XALKORI- crizotinib capsule
Xalkori by
Drug Labeling and Warnings
Xalkori by is a Prescription medication manufactured, distributed, or labeled by Pfizer Laboratories Div Pfizer Inc, Pfizer Inc, Pfizer Pharmaceuticals LLC, Pfizer Ireland Pharmaceuticals, Pfizer Manufacturing Deutschland GmbH, Upjohn Manufacturing Ireland Unlimited Company, Pfizer Asia Manufacturing Pte Ltd. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use XALKORI® safely and effectively. See full prescribing information for XALKORI.
XALKORI® (crizotinib) capsules, for oral use
Initial U.S. Approval: 2011INDICATIONS AND USAGE
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
Capsules: 250 mg, 200 mg. (3)
CONTRAINDICATIONS
None. (4)
WARNINGS AND PRECAUTIONS
- Hepatotoxicity: Fatal hepatotoxicity occurred in 0.1% of patients. Monitor with periodic liver testing. Temporarily suspend, dose reduce, or permanently discontinue XALKORI. (2.3, 5.1)
- Interstitial Lung Disease (ILD)/Pneumonitis: Occurred in 2.9% of patients. Permanently discontinue in patients with ILD/pneumonitis. (5.2)
- QT Interval Prolongation: Occurred in 2.1% of patients. Monitor electrocardiograms and electrolytes in patients who have a history of or predisposition for QTc prolongation, or who are taking medications that prolong QT. Temporarily suspend, dose reduce, or permanently discontinue XALKORI. (2.3, 5.3)
- Bradycardia: XALKORI can cause bradycardia. Monitor heart rate and blood pressure regularly. Temporarily suspend, dose reduce, or permanently discontinue XALKORI. (2.3, 5.4)
- Severe Visual Loss: Reported in 0.2% of patients. Discontinue XALKORI in patients with severe visual loss. Perform an ophthalmological evaluation. (5.5)
- Embryo-Fetal Toxicity: Can cause fetal harm. Advise females of reproductive potential of the potential risk to a fetus and use of effective contraception. (5.6, 8.1, 8.3)
ADVERSE REACTIONS
The most common adverse reactions (≥25%) are vision disorders, nausea, diarrhea, vomiting, edema, constipation, elevated transaminases, fatigue, decreased appetite, upper respiratory infection, dizziness, and neuropathy. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Pfizer Inc. at 1-800-438-1985 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 6/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Patient Selection
2.2 Recommended Dosage
2.3 Dosage Modifications for Adverse Reactions
2.4 Dosage Modifications for Moderate and Severe Hepatic Impairment
2.5 Dosage Modification for Severe Renal Impairment
2.6 Dosage Modification for Concomitant Use of Strong CYP3A Inhibitors
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hepatotoxicity
5.2 Interstitial Lung Disease/Pneumonitis
5.3 QT Interval Prolongation
5.4 Bradycardia
5.5 Severe Visual Loss
5.6 Embryo-Fetal Toxicity
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Effect of Other Drugs on XALKORI
7.2 Effect of XALKORI on Other Drugs
7.3 Drugs That Prolong the QT Interval
7.4 Drugs That Cause Bradycardia
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 Renal Impairment
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 ALK-Positive Metastatic NSCLC
14.2 ROS1-Positive Metastatic NSCLC
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
XALKORI is indicated for the treatment of patients with metastatic non-small cell lung cancer (NSCLC) whose tumors are anaplastic lymphoma kinase (ALK) or ROS1-positive as detected by an FDA-approved test [see Dosage and Administration (2.1)].
-
2 DOSAGE AND ADMINISTRATION
2.1 Patient Selection
Select patients for the treatment of metastatic NSCLC with XALKORI based on the presence of ALK or ROS1 positivity in tumor specimens [see Clinical Studies (14.1, 14.2)].
Information on FDA-approved tests for the detection of ALK and ROS1 rearrangements in NSCLC is available at http://www.fda.gov/companiondiagnostics.
2.2 Recommended Dosage
The recommended dosage of XALKORI is 250 mg orally twice daily, with or without food, until disease progression or no longer tolerated by the patient.
Swallow capsules whole. If a dose of XALKORI is missed, make up that dose unless the next dose is due within 6 hours. If vomiting occurs after taking a dose of XALKORI, take the next dose at the regular time.
2.3 Dosage Modifications for Adverse Reactions
The recommended dose reductions are:
- First dose reduction: XALKORI 200 mg taken orally twice daily
- Second dose reduction: XALKORI 250 mg taken orally once daily
- Permanently discontinue if unable to tolerate XALKORI 250 mg taken orally once daily.
Dosage modifications for adverse reactions for XALKORI are provided in Tables 1 and 2.
Table 1. XALKORI Dosage Modification – Hematologic Toxicities* Severity of Adverse Reaction† XALKORI Dosage Modification - * Except lymphopenia (unless associated with clinical events, e.g., opportunistic infections).
- † Grade based on National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events (CTCAE), version 4.0.
Grade 3 Withhold until recovery to Grade 2 or less, then resume at the same dosage Grade 4 Withhold until recovery to Grade 2 or less, then resume at next lower dosage Monitor complete blood counts including differential white blood cell counts monthly and as clinically indicated, with more frequent repeat testing if Grade 3 or 4 abnormalities are observed, or if fever or infection occurs.
Table 2. XALKORI Dosage Modification – Non-Hematologic Toxicities Severity of Adverse Reaction* XALKORI Dosage Modification - * Grade based on National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events (CTCAE), version 4.0.
- † Heart rate less than 60 beats per minute (bpm).
- ‡ Permanently discontinue for recurrence.
Hepatotoxicity [see Warnings and Precautions (5.1)] Alanine aminotransferase (ALT) or aspartate aminotransferase (AST) greater than 5 times upper limit of normal (ULN) with total bilirubin less than or equal to 1.5 times ULN Withhold until recovery to baseline or less than or equal to 3 times ULN, then resume at next lower dosage. ALT or AST greater than 3 times ULN with concurrent total bilirubin greater than 1.5 times ULN (in the absence of cholestasis or hemolysis) Permanently discontinue. Interstitial Lung Disease (Pneumonitis) [see Warnings and Precautions (5.2)] Any grade drug-related interstitial lung disease/pneumonitis Permanently discontinue. QT Interval Prolongation [see Warnings and Precautions (5.3)] QT corrected for heart rate (QTc) greater than 500 ms on at least 2 separate electrocardiograms (ECGs) Withhold until recovery to baseline or to a QTc less than 481 ms, then resume at next lower dosage. QTc greater than 500 ms or greater than or equal to 60 ms change from baseline with Torsade de pointes or polymorphic ventricular tachycardia or signs/symptoms of serious arrhythmia Permanently discontinue. Bradycardia [see Warnings and Precautions (5.4)] Bradycardia† (symptomatic, may be severe and medically significant, medical intervention indicated) Withhold until recovery to asymptomatic bradycardia or to a heart rate of 60 bpm or above.
Evaluate concomitant medications known to cause bradycardia, as well as antihypertensive medications.
If contributing concomitant medication is identified and discontinued, or its dose is adjusted, resume at previous dose upon recovery to asymptomatic bradycardia or to a heart rate of 60 bpm or above.
If no contributing concomitant medication is identified, or if contributing concomitant medications are not discontinued or dose modified, resume at reduced dose upon recovery to asymptomatic bradycardia or to a heart rate of 60 bpm or above.Bradycardia†,‡ (life-threatening consequences, urgent intervention indicated) Permanently discontinue if no contributing concomitant medication is identified.
If contributing concomitant medication is identified and discontinued, or its dose is adjusted, resume at 250 mg once daily upon recovery to asymptomatic bradycardia or to a heart rate of 60 bpm or above, with frequent monitoring.Severe Vision Loss [see Warnings and Precautions (5.5)] Visual Loss (Grade 4 Ocular Disorder) Discontinue during evaluation of severe vision loss. 2.4 Dosage Modifications for Moderate and Severe Hepatic Impairment
The recommended dose of XALKORI in patients with pre-existing moderate hepatic impairment [any aspartate aminotransferase (AST) and total bilirubin greater than 1.5 times the upper limit of normal (ULN) and less than or equal to 3 times ULN] is 200 mg orally twice daily.
The recommended dose of XALKORI in patients with pre-existing severe hepatic impairment (any AST and total bilirubin greater than 3 times ULN) is 250 mg orally once daily [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)].
2.5 Dosage Modification for Severe Renal Impairment
The recommended dosage of XALKORI in patients with severe renal impairment [creatinine clearance (CLcr) less than 30 mL/min, calculated using the modified Cockcroft-Gault equation] not requiring dialysis is 250 mg orally once daily [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)].
2.6 Dosage Modification for Concomitant Use of Strong CYP3A Inhibitors
Avoid concomitant use of strong CYP3A inhibitors. If concomitant use of strong CYP3A inhibitors is unavoidable, reduce the dose of XALKORI to 250 mg orally once daily [see Drug Interactions (7.1)]. After discontinuation of a strong CYP3A inhibitor, resume the XALKORI dose used prior to initiating the strong CYP3A inhibitor.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Hepatotoxicity
Drug-induced hepatotoxicity with fatal outcome occurred in 0.1% of the 1719 patients treated with XALKORI across clinical trials [see Adverse Reactions (6.1)]. Concurrent elevations in ALT or AST ≥3 times the ULN and total bilirubin ≥2 times the ULN, with normal alkaline phosphatase, occurred in <1% treated with XALKORI. Increased ALT or AST >5 times the ULN occurred in 11% and 6% of patients, respectively. One percent (1.0%) of patients required permanent discontinuation due to elevated transaminases. Increased transaminases generally occurred within the first 2 months of treatment.
Monitor liver function tests, including ALT, AST, and total bilirubin, every 2 weeks during the first 2 months of treatment, then once a month, and as clinically indicated, with more frequent repeat testing for increased liver transaminases, alkaline phosphatase, or total bilirubin in patients who develop increased transaminases. Withhold, reduce dose, or permanently discontinue XALKORI for hepatotoxicity as recommended [see Dosage and Administration (2.3)].
5.2 Interstitial Lung Disease/Pneumonitis
Severe, life-threatening, or fatal interstitial lung disease (ILD)/pneumonitis can occur in patients treated with XALKORI. Across clinical trials (n=1719), 2.9% of XALKORI-treated patients had ILD of any grade, 1.0% had Grade 3 or 4 ILD, and 0.5% had fatal ILD [see Adverse Reactions (6.1)]. Interstitial lung disease generally occurred within 3 months after the initiation of XALKORI.
Monitor patients for pulmonary symptoms indicative of ILD/pneumonitis. Exclude other potential causes of ILD/pneumonitis, and permanently discontinue XALKORI in patients diagnosed with drug-related ILD/pneumonitis [see Dosage and Administration (2.3)].
5.3 QT Interval Prolongation
QTc prolongation can occur in patients treated with XALKORI. Across clinical trials, 2.1% of 1616 patients had QTcF (corrected QT for heart rate by the Fridericia method) greater than or equal to 500 ms and 5% of 1582 patients had an increase from baseline QTcF greater than or equal to 60 ms by automated machine-read evaluation of ECGs.
Avoid use of XALKORI in patients with congenital long QT syndrome. Monitor ECGs and electrolytes in patients with congestive heart failure, bradyarrhythmias, electrolyte abnormalities, or who are taking medications that are known to prolong the QT interval. Withhold, reduce dose, or permanently discontinue XALKORI for QT/QTc interval prolongation as recommended [see Dosage and Administration (2.3), Clinical Pharmacology (12.2)].
5.4 Bradycardia
Symptomatic bradycardia can occur in patients receiving XALKORI. Across clinical trials, bradycardia occurred in 13% of 1719 patients treated with XALKORI. Grade 3 syncope occurred in 2.4% of XALKORI-treated patients and in 0.6% of the chemotherapy-treated patients [see Adverse Reactions (6.1)].
Avoid using XALKORI in combination with other medications known to cause bradycardia (e.g., beta-blockers, non-dihydropyridine calcium channel blockers, clonidine, and digoxin) to the extent possible. Monitor heart rate and blood pressure regularly. If bradycardia occurs, re-evaluate for the use of concomitant medications known to cause bradycardia. Withhold, reduce dose, or permanently discontinue XALKORI for bradycardia as recommended [see Dosage and Administration (2.3)].
5.5 Severe Visual Loss
Across all clinical trials, the incidence of Grade 4 visual field defect with vision loss was 0.2% of 1719 patients [see Adverse Reactions (6.1)]. Optic atrophy and optic nerve disorder have been reported as potential causes of vision loss.
Discontinue XALKORI in patients with new onset of severe visual loss (best corrected vision less than 20/200 in one or both eyes). Perform an ophthalmological evaluation consisting of best corrected visual acuity, retinal photographs, visual fields, optical coherence tomography (OCT) and other evaluations as appropriate for new onset of severe visual loss. There is insufficient information to characterize the risks of resumption of XALKORI in patients with a severe visual loss; a decision to resume XALKORI should consider the potential benefits to the patient.
5.6 Embryo-Fetal Toxicity
Based on its mechanism of action, XALKORI can cause fetal harm when administered to a pregnant woman. In animal reproduction studies, oral administration of crizotinib in pregnant rats during organogenesis at exposures similar to those observed with the maximum recommended human dose resulted in embryotoxicity and fetotoxicity. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with XALKORI and for at least 45 days following the final dose. Advise males with female partners of reproductive potential to use condoms during treatment with XALKORI and for at least 90 days after the final dose [see Use in Specific Populations (8.1, 8.3), Nonclinical Toxicology (13.1)].
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Hepatotoxicity [see Warnings and Precautions (5.1)]
- Interstitial Lung Disease/Pneumonitis [see Warnings and Precautions (5.2)]
- QT Interval Prolongation [see Warnings and Precautions (5.3)]
- Bradycardia [see Warnings and Precautions (5.4)]
- Severe Visual Loss [see Warnings and Precautions (5.5)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
The data in the Warnings and Precautions reflect exposure to XALKORI in 1719 patients who received XALKORI 250 mg twice daily enrolled on Studies 1 (including an additional 109 patients who crossed over from the control arm), 2, 3, a single arm trial (n=1063) of ALK-positive NSCLC, and an additional ALK-positive NSCLC expansion cohort of a dose finding study (n=154).
The data described below is based primarily on 343 patients with ALK-positive metastatic NSCLC who received XALKORI 250 mg orally twice daily from 2 open-label, randomized, active-controlled trials (Studies 1 and 2). The safety of XALKORI was also evaluated in 50 patients with ROS1-positive metastatic NSCLC from a single-arm study (Study 3).
The most common adverse reactions (≥25%) of XALKORI are vision disorders, nausea, diarrhea, vomiting, edema, constipation, elevated transaminases, fatigue, decreased appetite, upper respiratory infection, dizziness, and neuropathy.
Previously Untreated ALK-Positive Metastatic NSCLC - Study 1 (PROFILE 1014)
The data in Table 3 are derived from 340 patients with ALK-positive metastatic NSCLC who had not received previous systemic treatment for advanced disease who received treatment in a randomized, multicenter, open-label, active-controlled trial (Study 1). Patients in the XALKORI arm (n=171) received XALKORI 250 mg orally twice daily until documented disease progression, intolerance to therapy, or the investigator determined that the patient was no longer experiencing clinical benefit. A total of 169 patients in the chemotherapy arm received pemetrexed 500 mg/m2 with cisplatin 75 mg/m2 (n=91) or carboplatin at a dose calculated to produce an AUC of 5 or 6 mg×min/mL (n=78). Chemotherapy was given by intravenous infusion every 3 weeks for up to 6 cycles, in the absence of dose-limiting chemotherapy-related toxicities. After 6 cycles, patients remained on study with no additional anticancer treatment, and tumor assessments continued until documented disease progression.
The median duration of study treatment was 10.9 months for patients in the XALKORI arm and 4.1 months for patients in the chemotherapy arm. Median duration of treatment was 5.2 months for patients who received XALKORI after cross over from chemotherapy. Across the 340 patients who were treated in Study 1, the median age was 53 years; 16% of patients were older than 65 years. A total of 62% of patients were female and 46% were Asian.
Serious adverse events were reported in 34% of patients treated with XALKORI. The most frequent serious adverse events reported in patients treated with XALKORI were dyspnea (4.1%) and pulmonary embolism (2.9%). Fatal adverse events in XALKORI-treated patients occurred in 2.3% patients, consisting of septic shock, acute respiratory failure, and diabetic ketoacidosis.
Dose reductions due to adverse reactions were required in 6% of XALKORI-treated patients. The most frequent adverse reactions that led to dose reduction in these patients were nausea (1.8%) and elevated transaminases (1.8%).
Permanent discontinuation of XALKORI treatment for adverse reactions was 8%. The most frequent adverse reactions that led to permanent discontinuation in XALKORI-treated patients were elevated transaminases (1.2%), hepatotoxicity (1.2%), and ILD (1.2%).
Tables 3 and 4 summarize common adverse reactions and laboratory abnormalities in XALKORI-treated patients.
Table 3. Adverse Reactions Reported at a Higher Incidence (≥5% Higher for All Grades or ≥2% Higher for Grades 3–4) with XALKORI than Chemotherapy in Study 1* Adverse Reaction XALKORI
(N=171)Chemotherapy
(Pemetrexed/Cisplatin or Pemetrexed/Carboplatin)
(N=169)All Grades
(%)Grade 3–4
(%)All Grades
(%)Grade 3–4
(%)- * Adverse reactions were graded using NCI CTCAE version 4.0.
Includes cases reported within the clustered terms:- † Bradycardia (Bradycardia, Sinus bradycardia).
- ‡ Vision Disorder (Diplopia, Photophobia, Photopsia, Reduced visual acuity, Blurred vision, Vitreous floaters, Visual impairment).
- § Abdominal pain (Abdominal discomfort, Abdominal pain, Lower abdominal pain, Upper abdominal pain, Abdominal tenderness).
- ¶ Esophagitis (Esophagitis, Esophageal ulcer).
- # Edema (Edema, Peripheral edema, Face edema, Generalized edema, Local swelling, Periorbital edema).
- Þ Upper respiratory infection (Nasopharyngitis, Pharyngitis, Rhinitis, Upper respiratory tract infection).
- ß Dizziness (Balance disorder, Dizziness, Postural dizziness, Presyncope).
Cardiac Bradycardia† 14 1 1 0 Electrocardiogram QT prolonged 6 2 2 0 Eye Vision disorder‡ 71 1 10 0 Gastrointestinal Diarrhea 61 2 13 1 Vomiting 46 2 36 3 Constipation 43 2 30 0 Abdominal pain§ 26 0 12 0 Dyspepsia 14 0 2 0 Dysphagia 10 1 2 1 Esophagitis¶ 6 2 1 0 General Edema# 49 1 12 1 Pyrexia 19 0 11 1 Infections Upper respiratory infectionÞ 32 0 12 1 Investigations Increased weight 8 1 2 0 Musculoskeletal and Connective Tissue Pain in extremity 16 0 7 0 Muscle spasm 8 0 2 1 Nervous System Dysgeusia 26 0 5 0 Headache 22 1 15 0 Dizzinessß 18 0 10 1 Additional adverse reactions occurring at an overall incidence between 1% and 60% in patients treated with XALKORI included nausea (56%), decreased appetite (30%), fatigue (29%), neuropathy (21%; gait disturbance, hypoesthesia, muscular weakness, neuralgia, neuropathy peripheral, paresthesia, peripheral sensory neuropathy, polyneuropathy, sensory disturbance), rash (11%), renal cyst (5%), ILD (1%; ILD, pneumonitis), syncope (1%), and decreased blood testosterone (1%; hypogonadism).
Table 4. Laboratory Abnormalities with Grade 3 or 4 Occurring in ≥4% of XALKORI-Treated Patients in Study 1 XALKORI Chemotherapy Laboratory Abnormality Any Grade
(%)Grade 3–4
(%)Any Grade
(%)Grade 3–4
(%)Additional laboratory test abnormality in patients treated with XALKORI was an increase in creatinine (Any Grade: 99%; Grade 3: 2%; Grade 4: 0%) compared to the chemotherapy arm (Any Grade: 92%; Grade 3: 0%; Grade 4: 1%). Hematology Neutropenia 52 11 59 16 Lymphopenia 48 7 53 13 Chemistry Increased ALT 79 15 33 2 Increased AST 66 8 28 1 Hypophosphatemia 32 10 21 6 Previously Treated ALK-Positive Metastatic NSCLC - Study 2 (PROFILE 1007)
The data in Table 5 are derived from 343 patients with ALK-positive metastatic NSCLC enrolled in a randomized, multicenter, active-controlled, open-label trial (Study 2). Patients in the XALKORI arm (n=172) received XALKORI 250 mg orally twice daily until documented disease progression, intolerance to therapy, or the investigator determined that the patient was no longer experiencing clinical benefit. A total of 171 patients in the chemotherapy arm received pemetrexed 500 mg/m2 (n=99) or docetaxel 75 mg/m2 (n=72) by intravenous infusion every 3 weeks until documented disease progression, intolerance to therapy, or the investigator determined that the patient was no longer experiencing clinical benefit. Patients in the chemotherapy arm received pemetrexed unless they had received pemetrexed as part of first-line or maintenance treatment.
The median duration of study treatment was 7.1 months for patients who received XALKORI and 2.8 months for patients who received chemotherapy. Across the 347 patients who were randomized to study treatment (343 received at least 1 dose of study treatment), the median age was 50 years; 14% of patients were older than 65 years. A total of 56% of patients were female and 45% of patients were Asian.
Serious adverse reactions were reported in 37% of patients treated with XALKORI and 23% of patients in the chemotherapy arm. The most frequent serious adverse reactions reported in patients treated with XALKORI were pneumonia (4.1%), pulmonary embolism (3.5%), dyspnea (2.3%), and ILD (2.9%). Fatal adverse reactions in XALKORI-treated patients in Study 2 occurred in 5% of patients, consisting of: acute respiratory distress syndrome, arrhythmia, dyspnea, pneumonia, pneumonitis, pulmonary embolism, ILD, respiratory failure, and sepsis.
Dose reductions due to adverse reactions were required in 16% of XALKORI-treated patients. The most frequent adverse reactions that led to dose reduction in the patients treated with XALKORI were increased ALT (8%) including some patients with concurrent increased AST, QTc prolongation (2.9%), and neutropenia (2.3%).
XALKORI was discontinued for adverse reactions in 15% of patients. The most frequent adverse reactions that led to discontinuation of XALKORI were ILD (1.7%), increased ALT and AST (1.2%), dyspnea (1.2%), and pulmonary embolism (1.2%).
Tables 5 and 6 summarize common adverse reactions and laboratory abnormalities in XALKORI-treated patients.
Table 5. Adverse Reactions Reported at a Higher Incidence (≥5% Higher for All Grades or ≥2% Higher for Grades 3/4) with XALKORI than Chemotherapy in Study 2* Adverse Reaction XALKORI
(N=172)Chemotherapy
(Pemetrexed or Docetaxel)
(N=171)All Grades
(%)Grade 3–4
(%)All Grades
(%)Grade 3–4
(%)- * Adverse reactions were graded using NCI CTCAE version 4.0.
Includes cases reported within the clustered terms:- † Dizziness (Balance disorder, Dizziness, Postural dizziness).
- ‡ Vision Disorder (Diplopia, Photophobia, Photopsia, Blurred vision, Reduced visual acuity, Visual impairment, Vitreous floaters).
- § Bradycardia (Bradycardia, Sinus bradycardia).
- ¶ Upper respiratory infection (Laryngitis, Nasopharyngitis, Pharyngitis, Rhinitis, Upper respiratory tract infection).
- # Pulmonary embolism (Pulmonary artery thrombosis, Pulmonary embolism).
- Þ Edema (Face edema, Generalized edema, Local swelling, Localized edema, Edema, Peripheral edema, Periorbital edema).
Nervous System Dysgeusia 26 0 9 0 Dizziness† 22 1 8 0 Syncope 3 3 0 0 Eye Vision disorder‡ 60 0 9 0 Cardiac Electrocardiogram QT prolonged 5 3 0 0 Bradycardia§ 5 0 0 0 Investigations Decreased weight 10 1 4 0 Gastrointestinal Diarrhea 60 0 19 1 Nausea 55 1 37 1 Vomiting 47 1 18 0 Constipation 42 2 23 0 Dyspepsia 8 0 3 0 Infections Upper respiratory infection¶ 26 0 13 1 Respiratory, Thoracic and Mediastinal Pulmonary embolism# 6 5 2 2 General EdemaÞ 31 0 16 0 Additional adverse reactions occurring at an overall incidence between 1% and 30% in patients treated with XALKORI included decreased appetite (27%), fatigue (27%), neuropathy (19%; dysesthesia, gait disturbance, hypoesthesia, muscular weakness, neuralgia, peripheral neuropathy, paresthesia, peripheral sensory neuropathy, polyneuropathy, burning sensation in skin), rash (9%), ILD (4%; acute respiratory distress syndrome, ILD, pneumonitis), renal cyst (4%), esophagitis (2%), hepatic failure (1%), and decreased blood testosterone (1%; hypogonadism).
Table 6. Laboratory Abnormalities with Grade 3 or 4 Occurring in ≥4% of XALKORI-Treated Patients in Study 2 XALKORI Chemotherapy Laboratory Abnormality Any Grade
(%)Grade 3–4
(%)Any Grade
(%)Grade 3–4
(%)Additional laboratory test abnormality in patients treated with XALKORI was an increase in creatinine (Any Grade: 96%; Grade 3: 1%; Grade 4: 0%) compared to the chemotherapy arm (Any Grade: 72%; Grade 3: 0%; Grade 4: 0%). Hematology Lymphopenia 51 9 60 25 Neutropenia 49 12 28 12 Chemistry Increased ALT 76 17 38 4 Increased AST 61 9 33 0 Hypophosphatemia 28 5 25 6 Hypokalemia 18 4 10 1 ROS1-Positive Metastatic NSCLC - Study 3 (PROFILE 1001)
The safety profile of XALKORI from Study 3, which was evaluated in 50 patients with ROS1-positive metastatic NSCLC, was generally consistent with the safety profile of XALKORI evaluated in patients with ALK-positive metastatic NSCLC (n=1669). Vision disorders occurred in 92% of patients in Study 3; 90% were Grade 1 and 2% were Grade 2. The median duration of exposure to XALKORI was 34.4 months.
Description of Selected Adverse Reactions
Vision disorders
Vision disorders, most commonly visual impairment, photopsia, blurred vision, or vitreous floaters, occurred in 63% of 1719 patients. The majority (95%) of these patients had Grade 1 visual adverse reactions. There were 0.8% of patients with Grade 3 and 0.2% of patients with Grade 4 visual impairment.
Based on the Visual Symptom Assessment Questionnaire (VSAQ-ALK), patients treated with XALKORI in Studies 1 and 2 reported a higher incidence of visual disturbances compared to patients treated with chemotherapy. The onset of vision disorder generally was within the first week of drug administration. The majority of patients on the XALKORI arms in Studies 1 and 2 (>50%) reported visual disturbances which occurred at a frequency of 4–7 days each week, lasted up to 1 minute, and had mild or no impact (scores 0 to 3 out of a maximum score of 10) on daily activities as captured in the VSAQ-ALK questionnaire.
Neuropathy
Neuropathy, most commonly sensory in nature, occurred in 25% of 1719 patients. Most events (95%) were Grade 1 or Grade 2 in severity.
Renal cysts
Renal cysts were experienced by 3.0% of 1719 patients.
The majority of renal cysts in XALKORI-treated patients were complex. Local cystic invasion beyond the kidney occurred, in some cases with imaging characteristics suggestive of abscess formation. However, across clinical trials no renal abscesses were confirmed by microbiology tests.
Renal toxicity
The estimated glomerular filtration rate (eGFR) decreased from a baseline median of 96.42 mL/min/1.73 m2 (n=1681) to a median of 80.23 mL/min/1.73 m2 at 2 weeks (n=1499) in patients with ALK-positive advanced NSCLC who received XALKORI in clinical trials. No clinically relevant changes occurred in median eGFR from 12 to 104 weeks of treatment. Median eGFR slightly increased (83.02 mL/min/1.73 m2) 4 weeks after the last dose of XALKORI. Overall, 76% of patients had a decrease in eGFR to <90 mL/min/1.73 m2, 38% had a decrease to eGFR to <60 mL/min/1.73 m2, and 3.6% had a decrease to eGFR to <30 mL/min/1.73 m2.
6.2 Postmarketing Experience
The following additional adverse reaction has been identified during postapproval use of XALKORI. Because this reaction is reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate the frequency or establish a causal relationship to drug exposure.
-
7 DRUG INTERACTIONS
7.1 Effect of Other Drugs on XALKORI
Strong or Moderate CYP3A Inhibitors
Concomitant use of crizotinib with strong CYP3A inhibitors increases crizotinib plasma concentrations [see Clinical Pharmacology (12.3)], which may increase the risk of adverse reactions of XALKORI. Avoid concomitant use of strong CYP3A inhibitors. If concomitant use of strong CYP3A inhibitors is unavoidable, reduce the XALKORI dosage [see Dosage and Administration (2.4)]. Avoid grapefruit or grapefruit juice which may also increase plasma concentrations of crizotinib. Use caution with concomitant use of moderate CYP3A inhibitors.
Strong CYP3A Inducers
Concomitant use of crizotinib with strong CYP3A inducers decreases crizotinib plasma concentrations [see Clinical Pharmacology (12.3)], which may decrease the efficacy of XALKORI. Avoid concomitant use of strong CYP3A inducers.
7.2 Effect of XALKORI on Other Drugs
CYP3A Substrates
Concomitant use of crizotinib increases plasma concentrations of CYP3A substrates [see Clinical Pharmacology (12.3)], which may increase the risk of adverse reactions of these substrates. Avoid concomitant use of XALKORI with CYP3A substrates where minimal concentration changes may lead to serious adverse reactions. If concomitant use of XALKORI is unavoidable, decrease the CYP3A substrate dosage in accordance with approved product labeling.
7.3 Drugs That Prolong the QT Interval
XALKORI can prolong the QT/QTc interval. Avoid concomitant use of XALKORI with drugs that prolong the QT interval [see Warnings and Precautions (5.3), Clinical Pharmacology (12.2)].
7.4 Drugs That Cause Bradycardia
XALKORI can cause bradycardia. Avoid concomitant use of XALKORI with drugs that cause bradycardia (e.g., beta-blockers, non-dihydropyridine calcium channel blockers, clonidine, and digoxin) [see Warnings and Precautions (5.4)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Based on findings from animal studies and its mechanism of action, XALKORI can cause fetal harm when administered to a pregnant woman [see Clinical Pharmacology (12.1)]. There are no available data on the use of XALKORI during pregnancy. In animal reproduction studies, oral administration of crizotinib in pregnant rats during organogenesis at exposures similar to those expected with the maximum recommended human dose resulted in embryotoxicity and fetotoxicity (see Data). Advise pregnant women of the potential risk to fetus.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Animal Data
Crizotinib was administered to pregnant rats and rabbits during organogenesis to study the effects on embryo-fetal development. Postimplantation loss was increased at doses ≥50 mg/kg/day (approximately 0.6 times the recommended human dose based on AUC) in rats. No teratogenic effects were observed in rats at doses up to the maternally toxic dose of 200 mg/kg/day (approximately 2.7 times the recommended human dose based on AUC) or in rabbits at doses of up to 60 mg/kg/day (approximately 1.6 times the recommended human dose based on AUC), though fetal body weights were reduced at these doses.
8.2 Lactation
Risk Summary
There is no information regarding the presence of crizotinib or its metabolites in human milk, or the effects on the breastfed child or on milk production. Because of the potential for adverse reactions in breastfed children, advise women not to breastfeed during treatment with XALKORI and for 45 days after the final dose.
8.3 Females and Males of Reproductive Potential
Pregnancy Testing
Verify the pregnancy status of females of reproductive potential prior to initiating XALKORI [see Use in Specific Population (8.1)].
Contraception
XALKORI can cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)].
Females
Advise females of reproductive potential to use effective contraception during treatment with XALKORI and for at least 45 days after the final dose.
Males
Because of the potential for genotoxicity, advise males with female partners of reproductive potential to use condoms during treatment with XALKORI and for at least 90 days after the final dose [see Nonclinical Toxicology (13.1)].
Infertility
Based on reproductive organ findings in animals, XALKORI may cause reduced fertility in females and males of reproductive potential. It is not known whether these effects on fertility are reversible [see Nonclinical Toxicology (13.1)].
8.4 Pediatric Use
The safety and effectiveness of XALKORI in pediatric patients have not been established.
Juvenile Animal Toxicity Data
Decreased bone formation in growing long bones was observed in immature rats at 150 mg/kg/day following once daily dosing for 28 days (approximately 5.4 times the recommended human dose based on AUC). Other toxicities of potential concern to pediatric patients have not been evaluated in juvenile animals.
8.5 Geriatric Use
Of the total number of patients with ALK-positive metastatic NSCLC in clinical studies of XALKORI (n=1669), 16% were 65 years or older and 3.8% were 75 years or older. No overall differences in safety or effectiveness were observed between these patients and younger patients.
Clinical studies of XALKORI in patients with ROS1-positive metastatic NSCLC did not include sufficient numbers of patients age 65 years and older to determine whether they respond differently from younger patients.
8.6 Hepatic Impairment
Crizotinib concentrations increased in patients with pre-existing moderate (any AST and total bilirubin greater than 1.5 times ULN and less than or equal to 3 times ULN) or severe (any AST and total bilirubin greater than 3 times ULN) hepatic impairment [see Clinical Pharmacology (12.3)]. Reduce XALKORI dosage in patients with moderate or severe hepatic impairment [see Dosage and Administration (2.2)]. No dose adjustment is recommended in patients with pre-existing mild hepatic impairment (AST > ULN and total bilirubin less than or equal to 1 times ULN or any AST and total bilirubin greater than 1 times ULN but less than or equal to1.5 times ULN).
8.7 Renal Impairment
Increased exposure to crizotinib occurred in patients with pre-existing severe renal impairment (CLcr less than 30 mL/min calculated using the modified Cockcroft-Gault equation) not requiring dialysis, therefore reduce dosage of XALKORI in these patients [see Dosage and Administration (2.4), Clinical Pharmacology (12.3)]. No dose adjustment is recommended in patients with mild to moderate renal impairment (CLcr 30 to 89 mL/min).
-
11 DESCRIPTION
Crizotinib is a kinase inhibitor. The molecular formula for crizotinib is C21H22Cl2FN5O and the molecular weight is 450.34 daltons. Crizotinib is described chemically as (R)-3-[1-(2,6-Dichloro-3-fluorophenyl)ethoxy]-5-[1-(piperidin-4-yl)-1H-pyrazol-4-yl]pyridin-2-amine.
The chemical structure of crizotinib is shown below:
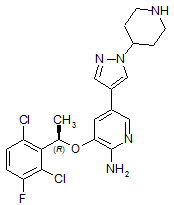
Crizotinib is a white to pale-yellow powder with a pKa of 9.4 (piperidinium cation) and 5.6 (pyridinium cation). The solubility of crizotinib in aqueous media decreases over the range pH 1.6 to pH 8.2 from greater than 10 mg/mL to less than 0.1 mg/mL. The log of the distribution coefficient (octanol/water) at pH 7.4 is 1.65.
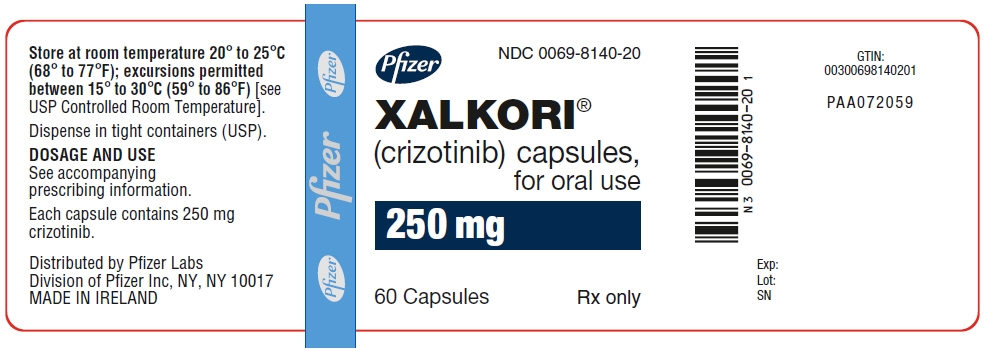
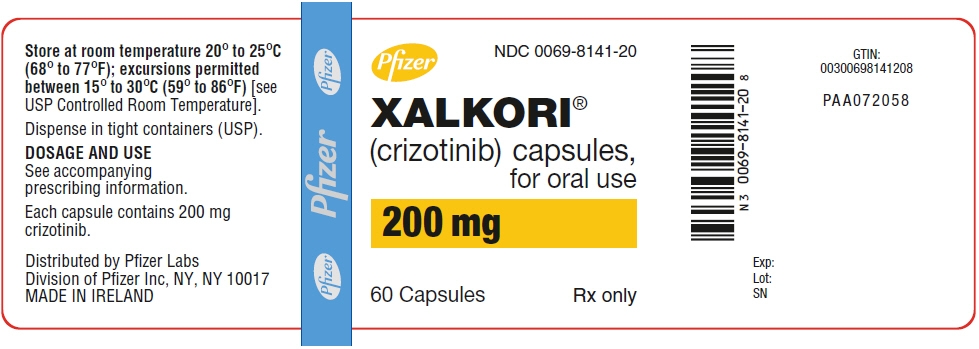
XALKORI (crizotinib) for oral administration is supplied as printed hard-shell capsules containing 250 mg or 200 mg of crizotinib together with colloidal silicon dioxide, microcrystalline cellulose, anhydrous dibasic calcium phosphate, sodium starch glycolate, magnesium stearate, and hard gelatin capsule shells as inactive ingredients.
The pink opaque capsule shell components contain gelatin, titanium dioxide, and red iron oxide. The white opaque capsule shell components contain gelatin and titanium dioxide. The printing ink contains shellac, propylene glycol, strong ammonia solution, potassium hydroxide, and black iron oxide.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Crizotinib is an inhibitor of receptor tyrosine kinases including ALK, Hepatocyte Growth Factor Receptor (HGFR, c-Met), ROS1 (c-ros), and Recepteur d'Origine Nantais (RON). Translocations can affect the ALK gene resulting in the expression of oncogenic fusion proteins. The formation of ALK fusion proteins results in activation and dysregulation of the gene's expression and signaling which can contribute to increased cell proliferation and survival in tumors expressing these proteins. Crizotinib demonstrated concentration-dependent inhibition of ALK, ROS1, and c-Met phosphorylation in cell-based assays using tumor cell lines and demonstrated antitumor activity in mice bearing tumor xenografts that expressed echinoderm microtubule-associated protein-like 4 (EML4)- or nucleophosmin (NPM)-ALK fusion proteins or c-Met.
12.2 Pharmacodynamics
Cardiac Electrophysiology
In an ECG substudy conducted in 52 patients with ALK-positive NSCLC, the maximum mean QTcF (corrected QT by the Fridericia method) change from baseline was 12.3 ms (2-sided 90% upper CI: 19.5 ms) following administration of XALKORI 250 mg orally twice daily. An exposure-QT analysis suggested a crizotinib plasma concentration-dependent increase in QTcF [see Warnings and Precautions (5.3)].
12.3 Pharmacokinetics
Following XALKORI 250 mg twice daily, steady-state was reached within 15 days and remained stable, with a median accumulation ratio of 4.8. Steady-state observed minimum concentration (Cmin) and AUC increased in a greater than dose-proportional manner over the dose range of 200 mg to 300 mg twice daily (0.8 to 1.2 times the approved recommended dosage).
Absorption
A single crizotinib dose was absorbed with median time to achieve peak concentration of 4 to 6 hours, and the mean absolute bioavailability of crizotinib was 43% (range: 32% to 66%).
Distribution
The geometric mean volume of distribution (Vss) of crizotinib was 1772 L following a single intravenous dose. Protein binding of crizotinib is 91% and is independent of drug concentration in vitro. Crizotinib is a substrate for P-glycoprotein (P-gp) in vitro. The blood-to-plasma concentration ratio is approximately 1.
Elimination
The mean apparent plasma terminal half-life of crizotinib was 42 hours following single doses of crizotinib in patients. The mean apparent clearance (CL/F) of crizotinib was lower at steady-state (60 L/h) after 250 mg twice daily than after a single 250 mg oral dose (100 L/h).
Specific Populations
No clinically significant difference in crizotinib pharmacokinetics were observed based on age, sex, ethnicity (Asian, non-Asian), or body weight.
Patients with Hepatic Impairment
Steady-state mean crizotinib AUC and Cmax decreased by 9% in patients with mild hepatic impairment (AST >ULN and total bilirubin ≤1 times ULN or any AST and total bilirubin >1 times ULN but ≤1.5 times ULN) compared to patients with normal hepatic function following XALKORI 250 mg orally twice daily.
Steady-state mean crizotinib AUC increased by 14% and Cmax increased by 9% in patients with moderate hepatic impairment (any AST and total bilirubin >1.5 times ULN and ≤3 times ULN) following XALKORI 200 mg orally twice daily compared with patients with normal hepatic function following XALKORI 250 mg orally twice daily.
Mean crizotinib AUC decreased by 35% and Cmax decreased by 27% in patients with severe hepatic impairment (any AST and total bilirubin >3 times ULN) following XALKORI 250 mg orally once daily compared with patients with normal hepatic function following XALKORI 250 mg orally twice daily [see Dosage and Administration (2.3) and Use in Specific Populations (8.6)].
Patients with Renal Impairment
Mild or moderate renal impairment (CLcr of 60–89 ml/min or 30–59 ml/min, respectively, calculated using the modified Cockcroft-Gault equation) has no clinically significant effect on the exposure of crizotinib. Following a single 250 mg dose, the mean AUC0–INF of crizotinib increased by 79% and the mean Cmax increased by 34% in patients with severe renal impairment (CLcr <30 mL/min) who did not require dialysis compared to those with normal renal function (CLcr ≥90 mL/min). Similar changes in AUC0–INF and Cmax were observed for the active metabolite of crizotinib [see Dosage and Administration (2. 4), Use in Specific Populations (8.7)].
Drug Interaction Studies
Clinical Studies
Gastric Acid Reducing Agents: No clinically significant differences in crizotinib pharmacokinetics were observed when used concomitantly with esomeprazole, a proton pump inhibitor.
Strong CYP3A Inhibitors: Coadministration of a single 150 mg oral dose of crizotinib with ketoconazole, a strong CYP3A inhibitor, increased crizotinib AUC0–INF by 216% and Cmax by 44% compared to crizotinib alone. Coadministration of XALKORI 250 mg orally once daily with itraconazole, a strong CYP3A inhibitor, increased crizotinib steady-state AUC by 57% and Cmax by 33% compared to crizotinib alone [see Drug Interactions (7.1)].
Strong CYP3A Inducers: Coadministration of XALKORI 250 mg orally twice daily with rifampin, a strong CYP3A inducer, decreased crizotinib steady-state AUC0–Tau by 84% and Cmax by 79%, compared to crizotinib alone [see Drug Interactions (7.1)].
CYP3A Substrates: Coadministration of XALKORI 250 mg orally twice daily for 28 days increased AUC0–INF of oral midazolam (CYP3A substrate) 3.7-fold compared to midazolam alone [see Drug Interactions (7.2)].
In Vitro Studies
CYP Enzymes: Crizotinib inhibits CYP2B6 in vitro. Crizotinib does not inhibit CYP1A2, CYP2C8, CYP2C9, CYP2C19, or CYP2D6. Crizotinib does not induce CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, or CYP3A.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies with crizotinib have not been conducted.
Crizotinib was genotoxic in an in vitro micronucleus assay in Chinese Hamster Ovary cultures, in an in vitro human lymphocyte chromosome aberration assay, and in in vivo rat bone marrow micronucleus assays. Crizotinib was not mutagenic in vitro in the bacterial reverse mutation (Ames) assay.
No specific studies with crizotinib have been conducted in animals to evaluate the effect on fertility; however, crizotinib is considered to have the potential to impair reproductive function and fertility in humans based on findings in repeat-dose toxicity studies in the rat. Findings observed in the male reproductive tract included testicular pachytene spermatocyte degeneration in rats given greater than or equal to 50 mg/kg/day for 28 days (greater than 1.7 times the recommended human dose based on AUC). Findings observed in the female reproductive tract included single-cell necrosis of ovarian follicles of a rat given 500 mg/kg/day (approximately 10 times the recommended human dose based on body surface area) for 3 days.
-
14 CLINICAL STUDIES
14.1 ALK-Positive Metastatic NSCLC
Previously Untreated ALK-Positive Metastatic NSCLC - Study 1 (PROFILE 1014; NCT01154140)
The efficacy of XALKORI for the treatment of patients with ALK-positive metastatic NSCLC, who had not received previous systemic treatment for advanced disease, was demonstrated in a randomized, multicenter, open-label, active-controlled study (Study 1). Patients were required to have ALK-positive NSCLC as identified by the FDA-approved assay, Vysis ALK Break-Apart fluorescence in situ hybridization (FISH) Probe Kit, prior to randomization. The major efficacy outcome measure was progression-free survival (PFS) according to Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1 as assessed by independent radiology review (IRR) committee. Additional efficacy outcome measures included objective response rate (ORR) as assessed by IRR, duration of response (DOR), and overall survival (OS). Patient-reported lung cancer symptoms were assessed at baseline and periodically during treatment.
Patients were randomized to receive XALKORI (n=172) or chemotherapy (n=171). Randomization was stratified by Eastern Cooperative Oncology Group (ECOG) performance status (0–1, 2), race (Asian, non-Asian), and brain metastases (present, absent). Patients in the XALKORI arm received XALKORI 250 mg orally twice daily until documented disease progression, intolerance to therapy, or the investigator determined that the patient was no longer experiencing clinical benefit. Chemotherapy consisted of pemetrexed 500 mg/m2 with cisplatin 75 mg/m2 or carboplatin AUC of 5 or 6 mg×min/mL by intravenous infusion every 3 weeks for up to 6 cycles. Patients in the chemotherapy arm were not permitted to receive maintenance chemotherapy. At the time of documented disease progression, as per independent radiology review, patients randomized to chemotherapy were offered XALKORI.
The demographic characteristics of the overall study population were 62% female, median age of 53 years, baseline ECOG performance status 0 or 1 (95%), 51% White and 46% Asian, 4% current smokers, 32% past smokers, and 64% never smokers. The disease characteristics of the overall study population were metastatic disease in 98% of patients, 92% of patients' tumors were classified as adenocarcinoma histology, 27% of patients had brain metastases, and 7% received systemic chemotherapy as adjuvant or neoadjuvant therapy. At the time of the final analysis of overall survival, 84% of patients randomized to the chemotherapy arm subsequently received XALKORI.
Study 1 demonstrated a statistically significant improvement in PFS in patients treated with XALKORI. There was no statistically significant difference in OS between patients treated with XALKORI and patients treated with chemotherapy. Table 7 and Figure 1 summarize the efficacy results. Exploratory patient-reported symptom measures of baseline and post-treatment dyspnea, cough, and chest pain suggested a delay in time to development of or worsening of dyspnea, but not cough or chest pain, in patients treated with XALKORI as compared to chemotherapy. The patient-reported delay in onset or worsening of dyspnea may be an overestimation, because patients were not blinded to treatment assignment.
Table 7. Previously Untreated ALK-Positive Metastatic NSCLC - Efficacy Results in Study 1 XALKORI
(N=172)Chemotherapy
(N=171)HR=hazard ratio; CI=confidence interval; IRR=independent radiology review; NR=not reached; CR=complete response; PR=partial response. - * Based on the Cox proportional hazards stratified analysis.
- † Based on the stratified log-rank test.
- ‡ Based on the stratified Cochran-Mantel-Haenszel test.
Progression-Free Survival (Based on IRR) Number of Events (%) 100 (58%) 137 (80%) Progressive Disease 89 (52%) 132 (77%) Death 11 (6%) 5 (3%) Median, Months (95% CI) 10.9 (8.3, 13.9) 7.0 (6.8, 8.2) HR (95% CI)* 0.45 (0.35, 0.60) p-value† <0.001 Overall Survival Number of Events (%) 71 (41%) 81 (47%) Median, Months (95% CI) NR (45.8, NR) 47.5 (32.2, NR) HR (95% CI)* 0.76 (0.55, 1.05) p-value† 0.098 Tumor Responses (Based on IRR) Objective Response Rate % (95% CI) 74% (67, 81) 45% (37, 53) CR, n (%) 3 (1.7%) 2 (1.2%) PR, n (%) 125 (73%) 75 (44%) p-value‡ <0.001 Duration of Response Median, Months (95% CI) 11.3 (8.1, 13.8) 5.3 (4.1, 5.8) Figure 1. Kaplan-Meier Curves of Progression-Free Survival as Assessed by IRR in Study 1 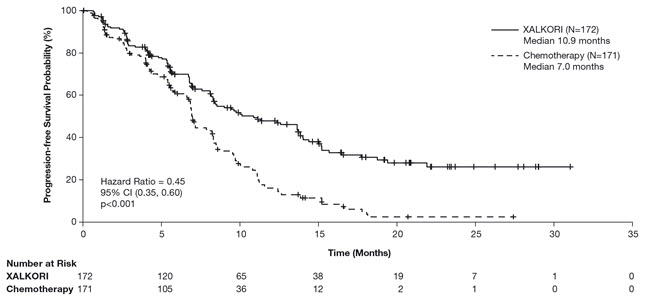
Previously Treated ALK-Positive Metastatic NSCLC - Study 2 (PROFILE 1007; NCT00932893)
The efficacy of XALKORI as monotherapy for the treatment of 347 patients with ALK-positive metastatic NSCLC, previously treated with 1 platinum-based chemotherapy regimen, were demonstrated in a randomized, multicenter, open-label, active-controlled study (Study 2). The major efficacy outcome was PFS according to RECIST version 1.1 as assessed by IRR. Additional efficacy outcomes included ORR as assessed by IRR, DOR, and OS.
Patients were randomized to receive XALKORI 250 mg orally twice daily (n=173) or chemotherapy (n=174). Chemotherapy consisted of pemetrexed 500 mg/m2 (if pemetrexed-naïve; n=99) or docetaxel 75 mg/m2 (n=72) intravenously (IV) every 21 days. Patients in both treatment arms continued treatment until documented disease progression, intolerance to therapy, or the investigator determined that the patient was no longer experiencing clinical benefit. Randomization was stratified by ECOG performance status (0–1, 2), brain metastases (present, absent), and prior EGFR tyrosine kinase inhibitor treatment (yes, no). Patients were required to have ALK-positive NSCLC as identified by the FDA-approved assay, Vysis ALK Break-Apart FISH Probe Kit, prior to randomization.
The demographic characteristics of the overall study population were 56% female, median age of 50 years, baseline ECOG performance status 0 or 1 (90%), 52% White and 45% Asian, 4% current smokers, 33% past smokers, and 63% never smokers. The disease characteristics of the overall study population were metastatic disease in at least 95% of patients and at least 93% of patients' tumors were classified as adenocarcinoma histology. At the time of the final analysis of overall survival, 89% of patients randomized to the chemotherapy arm subsequently received XALKORI.
Study 2 demonstrated a statistically significant improvement in PFS in the patients treated with XALKORI. Table 8 and Figure 2 summarize the efficacy results.
Table 8. Previously Treated ALK-Positive Metastatic NSCLC - Efficacy Results in Study 2 XALKORI
(N=173)Chemotherapy
(N=174)HR=hazard ratio; CI=confidence interval; IRR=independent radiology review; CR=complete response; PR=partial response. - * For pemetrexed, the median PFS was 4.2 months. For docetaxel, the median PFS was 2.6 months.
- † Based on the Cox proportional hazards stratified analysis.
- ‡ Based on the stratified log-rank test.
- § Based on the stratified Cochran-Mantel-Haenszel test.
Progression-Free Survival (Based on IRR) Number of Events (%) 100 (58%) 127 (73%) Progressive Disease 84 (49%) 119 (68%) Death 16 (9%) 8 (5%) Median, Months (95% CI) 7.7 (6.0, 8.8) 3.0* (2.6, 4.3) HR (95% CI)† 0.49 (0.37, 0.64) p-value‡ <0.001 Overall Survival Number of Events (%) 116 (67%) 126 (72%) Median, Months (95% CI) 21.7 (18.9,30.5) 21.9 (16.8,26.0) HR (95% CI)† 0.85 (0.66, 1.10) p-value‡ 0.229 Tumor Responses (Based on IRR) Objective Response Rate % (95% CI) 65% (58, 72) 20% (14, 26) CR, n (%) 1 (0.6%) 0 PR, n (%) 112 (65%) 34 (20%) p-value§ <0.001 Duration of Response Median, Months (95% CI) 7.4 (6.1, 9.7) 5.6 (3.4, 8.3) Figure 2. Kaplan-Meier Curves of Progression-Free Survival as Assessed by IRR in Study 2 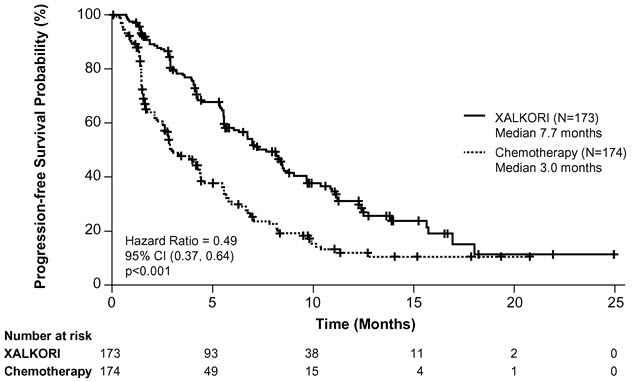
14.2 ROS1-Positive Metastatic NSCLC
ROS1-Positive Metastatic NSCLC - Study 3 (PROFILE 1001; NCT00585195)
The efficacy and safety of XALKORI was investigated in a multicenter, single-arm study (Study 3), in which patients with ROS1-positive metastatic NSCLC received XALKORI 250 mg orally twice daily. Patients were required to have histologically-confirmed advanced NSCLC with a ROS1 rearrangement, age 18 years or older, ECOG performance status of 0, 1, or 2, and measurable disease. The efficacy outcome measures were ORR and DOR according to RECIST version 1.0 as assessed by IRR and investigator, with imaging performed every 8 weeks for the first 60 weeks.
Baseline demographic and disease characteristics were female (56%), median age of 53 years, baseline ECOG performance status of 0 or 1 (98%), White (54%), Asian (42%), past smokers (22%), never smokers (78%), metastatic disease (92%), adenocarcinoma (96%), no prior systemic therapy for metastatic disease (14%), and prior platinum-based chemotherapy for metastatic disease (80%). The ROS1 status of NSCLC tissue samples was determined by laboratory-developed break-apart FISH (96%) or RT-PCR (4%) clinical trial assays. For assessment by FISH, ROS1 positivity required that ≥15% of a minimum of 50 evaluated nuclei contained a ROS1 gene rearrangement.
Efficacy results are summarized in Table 9.
Table 9. ROS1-Positive Metastatic NSCLC - Results* in Study 3 Efficacy Parameters IRR
(N=50)Investigator-Assessed
(N=50)IRR=independent radiology review; CI=confidence interval; NR=not reached. - * As assessed by RECIST version 1.0.
Objective Response Rate (95% CI) 66% (51, 79) 72% (58, 84) Complete Response, n 1 5 Partial Response, n 32 31 Duration of Response Median, Months (95% CI) 18.3 (12.7, NR) NR (14.5, NR) -
16 HOW SUPPLIED/STORAGE AND HANDLING
- 250 mg capsules
Hard gelatin capsule with pink opaque cap and body, printed with black ink "Pfizer" on the cap, "CRZ 250" on the body; available in:Bottles of 60 capsules: NDC: 0069-8140-20 - 200 mg capsules
Hard gelatin capsule with pink opaque cap and white opaque body, printed with black ink "Pfizer" on the cap, "CRZ 200" on the body; available in:Bottles of 60 capsules: NDC: 0069-8141-20
- 250 mg capsules
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Hepatotoxicity
Inform patients to immediately report symptoms of hepatotoxicity [see Warnings and Precautions (5.1)].
Interstitial Lung Disease (Pneumonitis)
Advise patients to immediately report any new or worsening pulmonary symptoms [see Warnings and Precautions (5.2)].
Bradycardia
Advise patients to report any symptoms of bradycardia and to inform their healthcare provider about the use of any heart or blood pressure medications [see Warnings and Precautions (5.4)].
Severe Visual Loss
Inform patients of the potential risk of severe visual loss and to immediately contact their healthcare provider if they develop severe visual loss. Inform patients that visual changes such as perceived flashes of light, blurry vision, light sensitivity, and floaters are commonly reported adverse reactions and may occur while driving or operating machinery. The onset of visual disorders most commonly occurs during the first week of treatment [see Warnings and Precautions (5.5), Adverse Reactions (6)].
Drug Interactions
Inform patients to avoid grapefruit or grapefruit juice while taking XALKORI. Advise patients to inform their healthcare providers of all concomitant medications, including prescription medicines, over-the-counter drugs, vitamins, and herbal products [see Drug Interactions (7)].
Dosage and Administration
Advise patients to take XALKORI with or without food and swallow XALKORI capsules whole.
If a patient misses a dose, advise the patient to take it as soon as remembered unless it is less than 6 hours until the next dose, in which case, advise the patient not to take the missed dose. If a patient vomits after taking a dose of XALKORI, advise the patient not to take an extra dose, but to take the next dose at the regular time.
Embryo-Fetal Toxicity
Advise females of reproductive potential of the potential risk to a fetus and to inform their healthcare provider of a known or suspected pregnancy [see Warnings and Precautions (5.6) and Use in Specific Populations (8.1)].
Females and Males of Reproductive Potential
Advise females of reproductive potential to use effective contraception during treatment with XALKORI and for at least 45 days after the final dose [see Use in Specific Populations (8.3)].
Advise males with female partners of reproductive potential to use condoms during treatment with XALKORI and for at least 90 days after the final dose [see Use in Specific Populations (8.3), Nonclinical Toxicology (13.1)].
Lactation
Advise females not to breastfeed during treatment with XALKORI and for 45 days after the final dose [see Use in Specific Populations (8.2)].
Infertility
Advise females and males of reproductive potential of the potential for reduced fertility from XALKORI [see Use in Specific Populations (8.3), Nonclinical Toxicology (13.1)].
- SPL UNCLASSIFIED SECTION
-
PATIENT PACKAGE INSERT
This Patient Information has been approved by the U.S. Food and Drug Administration. Revised: March 2016 PATIENT INFORMATION
XALKORI® (zal-KOR-ee)
(crizotinib)
capsulesWhat is the most important information I should know about XALKORI?
XALKORI may cause serious side effects, including:
- Liver problems. XALKORI may cause life-threatening liver injury that may lead to death. Your healthcare provider should do blood tests at least every month to check your liver during treatment with XALKORI. Tell your healthcare provider right away if you get any of the following new or worsening symptoms:
- yellowing of your skin or the white part of your eyes
- severe tiredness
- dark or brown (tea color) urine
- nausea or vomiting
- decreased appetite
- pain on the right side of your stomach
- bleed or bruise more easily than normal
- itching
-
Lung problems (pneumonitis). XALKORI may cause life-threatening lung problems that may lead to death. Symptoms may be similar to those symptoms from lung cancer. Tell your healthcare provider right away if you have any new or worsening symptoms, including:
- trouble breathing or shortness of breath
- cough with or without mucous
- fever
- Heart problems. XALKORI may cause very slow, very fast, or abnormal heartbeats. Your healthcare provider may check your heart during treatment with XALKORI. Tell your healthcare provider right away if you feel dizzy or faint or have abnormal heartbeats. Tell your healthcare provider if you take any heart or blood pressure medicines.
- Vision problems. Vision problems are common with XALKORI. These problems usually happen within 1 week of starting treatment with XALKORI. Vision problems with XALKORI can be severe and may cause partial or complete loss of vision in one or both eyes. Your healthcare provider may stop XALKORI and refer you to an eye healthcare provider if you develop severe vision problems during treatment with XALKORI. Tell your healthcare provider right away if you have any loss of vision or any change in vision, including:
- double vision
- seeing flashes of light
- blurry vision
- light hurting your eyes
- new or increased floaters
- See "What are possible side effects of XALKORI?" for more information about side effects.
What is XALKORI?
XALKORI is a prescription medicine that is used to treat people with non-small cell lung cancer (NSCLC) that has spread to other parts of the body and is caused by a defect in either a gene called ALK (anaplastic lymphoma kinase) or a gene called ROS1.
It is not known if XALKORI is safe and effective in children.
What should I tell my healthcare provider before taking XALKORI?
Before you take XALKORI, tell your healthcare provider if you:
- have heart problems, including a condition called long QT syndrome
- have liver or kidney problems
- have vision or eye problems
- have any other medical conditions
- are pregnant, or plan to become pregnant. XALKORI can harm your unborn baby.
- Females who are able to become pregnant should use effective birth control during treatment with XALKORI and for at least 45 days after the final dose of XALKORI.
- Males who have female partners who can become pregnant should use condoms during treatment with XALKORI and for at least 90 days after the final dose of XALKORI.
- Talk to your healthcare provider about birth control methods that may be right for you.
- If you or your partner becomes pregnant, tell your healthcare provider right away.
- are breastfeeding or plan to breastfeed. It is not known if XALKORI passes into your breast milk. Do not breastfeed during treatment with XALKORI and for 45 days after the final dose. Talk to your healthcare provider about the best way to feed your baby during this time.
Tell your healthcare provider about the medicines you take, including prescription medicines, over-the-counter medicines, vitamins, and herbal supplements.
How should I take XALKORI?
- Take XALKORI exactly as your healthcare provider tells you.
- Swallow XALKORI capsules whole.
- You may take XALKORI with or without food.
- Your healthcare provider may change your dose, temporarily stop, or permanently stop treatment with XALKORI if you have certain side effects. Do not change your dose or stop taking XALKORI unless your healthcare provider tells you.
- If you miss a dose, take it as soon as you remember. If it is close to your next dose (within 6 hours), just take your next dose at your regular time.
- If you vomit after taking a dose of XALKORI, do not take an extra dose, just take your next dose at your regular time.
What should I avoid while taking XALKORI?
- You should not drink grapefruit juice or eat grapefruit during your treatment with XALKORI. It may increase the amount of XALKORI in your blood to a harmful level.
- XALKORI can cause changes in your vision, dizziness, and tiredness. If you have these symptoms avoid driving a car, using machinery, or doing anything that needs you to be alert.
What are the possible side effects of XALKORI?
XALKORI may cause serious side effects, including:
The most common side effects of XALKORI include:
- vision problems. See "What is the most important information I should know about XALKORI?"
- nausea
- diarrhea
- vomiting
- swelling of your hands, feet, face, and eyes
- constipation
- increased liver function blood test results. See "What is the most important information I should know about XALKORI?"
- tiredness
- decreased appetite
- upper respiratory infection
- dizziness
- feeling of numbness or tingling in the extremities
XALKORI may cause decreased fertility in females and males. In females, this could affect your ability to become pregnant. In males, this could affect your ability to father a child. Talk to your healthcare provider if you have concerns about fertility.
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all of the possible side effects of XALKORI. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store XALKORI?
- Store XALKORI at room temperature between 68°F to 77°F (20°C to 25°C).
Keep XALKORI and all medicines out of the reach of children.
General information about XALKORI
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use XALKORI for a condition for which it was not prescribed. Do not give XALKORI to other people, even if they have the same symptoms that you have. It may harm them. You can ask your healthcare provider or pharmacist for more information about XALKORI that is written for health professionals.
What are the ingredients in XALKORI?
Active ingredient: crizotinib
Inactive ingredients: colloidal silicon dioxide, microcrystalline cellulose, anhydrous dibasic calcium phosphate, sodium starch glycolate, and magnesium stearate.
Pink opaque capsule shell contains: gelatin, titanium dioxide, and red iron oxide.
White opaque capsule shell contains: gelatin and titanium dioxide.
Printing ink contains: shellac, propylene glycol, strong ammonia solution, potassium hydroxide, and black iron oxide.
LAB-0441-8.0
For more information, go to www.XALKORI.com.
- PRINCIPAL DISPLAY PANEL - 250 mg Capsule Bottle Label
- PRINCIPAL DISPLAY PANEL - 200 mg Capsule Bottle Label
-
INGREDIENTS AND APPEARANCE
XALKORI
crizotinib capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0069-8140 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CRIZOTINIB (UNII: 53AH36668S) (CRIZOTINIB - UNII:53AH36668S) CRIZOTINIB 250 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) ANHYDROUS DIBASIC CALCIUM PHOSPHATE (UNII: L11K75P92J) MAGNESIUM STEARATE (UNII: 70097M6I30) GELATIN, UNSPECIFIED (UNII: 2G86QN327L) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FERRIC OXIDE RED (UNII: 1K09F3G675) SHELLAC (UNII: 46N107B71O) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) AMMONIA (UNII: 5138Q19F1X) POTASSIUM HYDROXIDE (UNII: WZH3C48M4T) FERROSOFERRIC OXIDE (UNII: XM0M87F357) Product Characteristics Color PINK (opaque) Score no score Shape CAPSULE Size 21mm Flavor Imprint Code Pfizer;CRZ;250 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0069-8140-20 60 in 1 BOTTLE; Type 0: Not a Combination Product 08/26/2011 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA202570 08/26/2011 XALKORI
crizotinib capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0069-8141 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CRIZOTINIB (UNII: 53AH36668S) (CRIZOTINIB - UNII:53AH36668S) CRIZOTINIB 200 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) ANHYDROUS DIBASIC CALCIUM PHOSPHATE (UNII: L11K75P92J) MAGNESIUM STEARATE (UNII: 70097M6I30) GELATIN, UNSPECIFIED (UNII: 2G86QN327L) FERRIC OXIDE RED (UNII: 1K09F3G675) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) SHELLAC (UNII: 46N107B71O) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) AMMONIA (UNII: 5138Q19F1X) POTASSIUM HYDROXIDE (UNII: WZH3C48M4T) FERROSOFERRIC OXIDE (UNII: XM0M87F357) Product Characteristics Color PINK (opaque) , WHITE (opaque) Score no score Shape CAPSULE Size 19mm Flavor Imprint Code Pfizer;CRZ;200 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0069-8141-20 60 in 1 BOTTLE; Type 0: Not a Combination Product 08/26/2011 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA202570 08/26/2011 Labeler - Pfizer Laboratories Div Pfizer Inc (134489525) Registrant - Pfizer Inc (113480771) Establishment Name Address ID/FEI Business Operations Pfizer Pharmaceuticals LLC 829084552 REPACK(0069-8141, 0069-8140) Establishment Name Address ID/FEI Business Operations Pfizer Ireland Pharmaceuticals 985104227 API MANUFACTURE(0069-8140, 0069-8141)
Trademark Results [Xalkori]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 XALKORI 85069606 3967863 Live/Registered |
Pfizer Inc. 2010-06-23 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.