KESIMPTA- ofatumumab injection, solution
KESIMPTA by
Drug Labeling and Warnings
KESIMPTA by is a Prescription medication manufactured, distributed, or labeled by Novartis Pharmaceuticals Corporation. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use KESIMPTA safely and effectively. See full prescribing information for KESIMPTA.
KESIMPTA® (ofatumumab) injection, for subcutaneous use
Initial U.S. Approval: 2009INDICATIONS AND USAGE
KESIMPTA is a CD20-directed cytolytic antibody indicated for the treatment of relapsing forms of multiple sclerosis (MS), to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in adults. (1)
DOSAGE AND ADMINISTRATION
- Before initiating KESIMPTA, screen for Hepatitis B virus (HBV) and obtain serum quantitative immunoglobulins, aminotransferases, alkaline phosphatase, and bilirubin. (2.1)
- Administer KESIMPTA by subcutaneous injection only. (2.2, 2.3)
- Initial Dosing: 20 mg administered at Weeks 0, 1, and 2. (2.2)
- Subsequent Dosing: 20 mg administered monthly starting at Week 4. (2.2)
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Infections: Serious, including life-threatening and fatal infections, have occurred in patients treated with anti-CD20 therapies. Delay KESIMPTA administration in patients with an active infection until the infection is resolved. Vaccination with live-attenuated or live vaccines is not recommended during treatment with KESIMPTA and after discontinuation, until B-cell repletion. (5.1)
- Injection-Related Reactions and Hypersensitivity Reactions: Management for injection-related reactions and hypersensitivity reactions depends on the type and severity of the reaction. (4, 5.2)
- Reduction in Immunoglobulins: Monitor the level of immunoglobulins at the beginning, during, and after discontinuation of treatment with KESIMPTA until B-cell repletion. Consider discontinuing KESIMPTA if a patient develops a serious opportunistic infection or recurrent infections if immunoglobulin levels indicate immune compromise. (5.3)
- Liver Injury: Clinically significant liver injury has occurred. Obtain serum aminotransferases, alkaline phosphatase, and bilirubin levels before initiating KESIMPTA, and during treatment as clinically indicated. Discontinue KESIMPTA in patients with evidence of liver injury in the absence of an alternative etiology. (5.4)
- Fetal Risk: May cause fetal harm based on animal data. Advise females of reproductive potential of the potential risk to a fetus and to use an effective method of contraception during treatment and for 6 months after stopping KESIMPTA. (5.5, 8.1)
ADVERSE REACTIONS
Most common adverse reactions (incidence greater than 10%) are upper respiratory tract infection, headache, injection-related reactions, and local injection site reactions. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Novartis Pharmaceuticals Corporation at 1-888-669-6682 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 8/2025
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Assessments Prior to First Dose of KESIMPTA
2.2 Recommended Dosage
2.3 Administration Instructions
2.4 Preparation of KESIMPTA
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Infections
5.2 Injection-Related Reactions and Hypersensitivity Reactions
5.3 Reduction in Immunoglobulins
5.4 Liver Injury
5.5 Fetal Risk
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Immunogenicity
6.3 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Immunosuppressive or Immune-Modulating Therapies
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Assessments Prior to First Dose of KESIMPTA
Hepatitis B Virus Screening
Prior to initiating KESIMPTA, perform Hepatitis B virus (HBV) screening. KESIMPTA is contraindicated in patients with active HBV confirmed by positive results for Hepatitis B surface antigen [HBsAg] and anti-HBV tests. For patients who are negative for HBsAg and positive for Hepatitis B core antibody [HBcAb+] or are carriers of HBV [HBsAg+], consult liver disease experts before starting and during treatment with KESIMPTA [see Warnings and Precautions (5.1)].
Serum Immunoglobulins
Prior to initiating KESIMPTA, perform testing for quantitative serum immunoglobulins [see Warnings and Precautions (5.3)]. For patients with low serum immunoglobulins, consult immunology experts before initiating treatment with KESIMPTA.
Vaccinations
Because vaccination with live-attenuated or live vaccines is not recommended during treatment and after discontinuation until B-cell repletion, administer all immunizations according to immunization guidelines at least 4 weeks prior to initiation of KESIMPTA for live or live-attenuated vaccines, and whenever possible, at least 2 weeks prior to initiation of KESIMPTA for inactivated vaccines [see Warnings and Precautions (5.1)].
Liver Function Tests
Prior to initiating KESIMPTA, obtain serum aminotransferases (alanine aminotransferase [ALT] and aspartate aminotransferase [AST]), alkaline phosphatase, and bilirubin levels [see Warnings and Precautions (5.4)].
2.2 Recommended Dosage
The recommended dosage of KESIMPTA is:
- initial dosing of 20 mg by subcutaneous injection at Weeks 0, 1, and 2, followed by
- subsequent dosing of 20 mg by subcutaneous injection once monthly starting at Week 4.
Missed Doses
If an injection of KESIMPTA is missed, it should be administered as soon as possible without waiting until the next scheduled dose. Subsequent doses should be administered at the recommended intervals.
2.3 Administration Instructions
Administer by subcutaneous injection only.
KESIMPTA is intended for patient self-administration by subcutaneous injection.
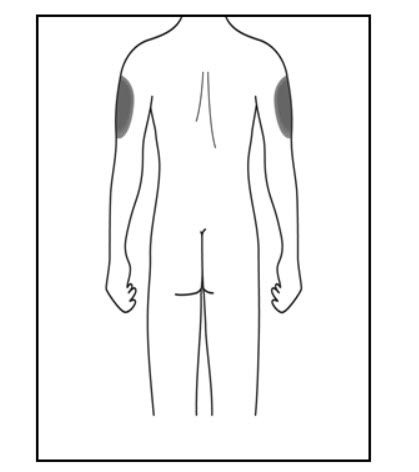
Administer KESIMPTA in the abdomen, thigh, or outer upper arm subcutaneously. Do not give injection into moles, scars, stretch marks, or areas where the skin is tender, bruised, red, scaly, or hard.
The first injection of KESIMPTA should be performed under the guidance of a healthcare professional [see Warnings and Precautions (5.2)].
KESIMPTA Sensoready® pens and syringes are for one-time use only and should be discarded after use. See Instructions for Use for complete administration instructions.
2.4 Preparation of KESIMPTA
The KESIMPTA “Instructions for Use” for each presentation contains more detailed instructions on the preparation of KESIMPTA.
Before administration, remove KESIMPTA Sensoready Pen or KESIMPTA prefilled syringe from the refrigerator and allow KESIMPTA to reach room temperature for about 15 to 30 minutes. DO NOT remove the needle cover while allowing the prefilled syringe to reach room temperature.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not use if the liquid contains visible particles or is cloudy.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
KESIMPTA is contraindicated in patients with:
- Active HBV infection [see Warnings and Precautions (5.1)].
- History of hypersensitivity to ofatumumab or life-threatening injection-related reaction to KESIMPTA. Hypersensitivity reactions have included anaphylaxis and angioedema [see Warnings and Precautions (5.2)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Infections
Serious, including life-threatening or fatal, bacterial, fungal, and new or reactivated viral infections have been observed during and following completion of treatment with anti-CD20 B-cell depleting therapies.
In KESIMPTA Study 1 and Study 2 [see Clinical Studies (14)], the overall rate of infections and serious infections in patients treated with KESIMPTA was similar to patients who were treated with teriflunomide (51.6% vs 52.7%, and 2.5% vs 1.8%, respectively). The most common infections reported by KESIMPTA-treated patients in the randomized clinical relapsing MS (RMS) trials included upper respiratory tract infection (39%) and urinary tract infection (10%). Delay KESIMPTA administration in patients with an active infection until the infection is resolved.
Possible Increased Risk of Immunosuppressant Effects with Other Immunosuppressants
When initiating KESIMPTA after an immunosuppressive therapy or initiating an immunosuppressive therapy after KESIMPTA, consider the potential for increased immunosuppressive effects [see Drug Interactions (7.1) and Clinical Pharmacology (12.2)]. KESIMPTA has not been studied in combination with other MS therapies.
Hepatitis B Virus
Reactivation
There were no reports of HBV reactivation in patients with MS treated with KESIMPTA. However, HBV reactivation, in some cases resulting in fulminant hepatitis, hepatic failure, and death, has occurred in patients being treated with ofatumumab for chronic lymphocytic leukemia (CLL) (at higher intravenous doses than the recommended dose in MS but for a shorter duration of treatment) and in patients treated with other anti-CD20 antibodies.
Infection
KESIMPTA is contraindicated in patients with active hepatitis B disease. Fatal infections caused by HBV in patients who have not been previously infected have occurred in patients being treated with ofatumumab for CLL (at higher intravenous doses than the recommended dose in MS but for a shorter duration of treatment). HBV screening should be performed in all patients before initiation of treatment with KESIMPTA. At a minimum, screening should include Hepatitis B surface antigen (HBsAg) and Hepatitis B Core Antibody (HBcAb) testing. These can be complemented with other appropriate markers as per local guidelines. For patients who are negative for HBsAg and positive for HB core antibody [HBcAb+] or are carriers of HBV [HBsAg+], consult liver disease experts before starting and during treatment with KESIMPTA. These patients should be monitored and managed following local medical standards to prevent HBV infection or reactivation.
Progressive Multifocal Leukoencephalopathy
Progressive multifocal leukoencephalopathy (PML) is an opportunistic viral infection of the brain caused by the JC virus (JCV) that typically occurs in patients who are immunocompromised, and that usually leads to death or severe disability.
Although no cases of PML have been reported for KESIMPTA in the RMS clinical studies, PML resulting in death has occurred in patients being treated with ofatumumab for CLL (at substantially higher intravenous doses than the recommended dose in MS but for a shorter duration of treatment). In addition, JCV infection resulting in PML has also been observed in patients treated with other anti-CD20 antibodies and other MS therapies. At the first sign or symptom suggestive of PML, withhold KESIMPTA and perform an appropriate diagnostic evaluation. Magnetic resonance imaging (MRI) findings may be apparent before clinical signs or symptoms. Typical symptoms associated with PML are diverse, progress over days to weeks, and include progressive weakness on one side of the body or clumsiness of limbs, disturbance of vision, and changes in thinking, memory, and orientation leading to confusion and personality changes.
If PML is confirmed, treatment with KESIMPTA should be discontinued.
Vaccinations
Administer all immunizations according to immunization guidelines at least 4 weeks prior to initiation of KESIMPTA for live or live-attenuated vaccines, and whenever possible, at least 2 weeks prior to initiation of KESIMPTA for inactivated vaccines.
KESIMPTA may interfere with the effectiveness of inactivated vaccines.
The safety of immunization with live or live-attenuated vaccines following KESIMPTA therapy has not been studied. Vaccination with live or live-attenuated vaccines is not recommended during treatment and after discontinuation until B-cell repletion [see Clinical Pharmacology (12.2)].
Vaccination of Infants Born to Mothers Treated with KESIMPTA During Pregnancy
In infants of mothers treated with KESIMPTA during pregnancy, do not administer live or live-attenuated vaccines before confirming the recovery of B-cell counts. Depletion of B-cells in these infants may increase the risks from live or live-attenuated vaccines.
Inactivated vaccines may be administered, as indicated, prior to recovery from B-cell depletion, but an assessment of vaccine immune responses, including consultation with a qualified specialist, should be considered to determine whether a protective immune response was mounted.
5.2 Injection-Related Reactions and Hypersensitivity Reactions
KESIMPTA can result in systemic injection-related reactions and hypersensitivity reactions, which may be serious or life-threatening.
In Study 1 and Study 2, systemic and local injection reactions were reported in 21% and 11% of patients treated with KESIMPTA, compared to 15% and 6% of patients treated with teriflunomide who received matching placebo injections, respectively [see Adverse Reactions (6.1) and Clinical Studies (14)].
Injection-related reactions with systemic symptoms observed in clinical studies occurred most commonly within 24 hours of the first injection, but were also observed with later injections. Symptoms observed included fever, headache, myalgia, chills, and fatigue, and were predominantly (99.8%) mild to moderate in severity. There were no life-threatening injection reactions in the RMS clinical studies.
In the post-marketing setting, additional systemic injection-related reactions and hypersensitivity reactions have been reported, including anaphylaxis, angioedema, pruritus, rash, urticaria, erythema, bronchospasm, throat irritation, oropharyngeal pain, dyspnea, pharyngeal or laryngeal edema, flushing, hypotension, dizziness, nausea, and tachycardia. Most cases were non-serious and occurred with the first injection. Most serious cases resulted in permanent discontinuation of KESIMPTA.
Symptoms of systemic injection-related reactions may be clinically indistinguishable from acute hypersensitivity reactions. A hypersensitivity reaction may occur with any injection. New or more severe symptoms compared to those experienced with previous injections should prompt consideration of a potential hypersensitivity reaction.
Only limited benefit of premedication with corticosteroids, antihistamines, or acetaminophen was observed in RMS clinical studies. The first injection of KESIMPTA should be performed under the guidance of an appropriately trained healthcare professional. If systemic injection-related reactions occur, initiate appropriate therapy. Patients who experience symptoms of systemic injection-related reactions or hypersensitivity reactions with KESIMPTA should be instructed to seek immediate medical attention.
If a hypersensitivity reaction or life-threatening systemic injection-related reaction occurs, immediately and permanently discontinue KESIMPTA [see Contraindications (4)]. If restarting KESIMPTA after a severe (but not life-threatening) systemic injection-related reaction or other event after which rechallenge is considered appropriate, administer the next KESIMPTA injection under clinical observation. If a mild to moderate injection-related reaction occurs, consider rechallenge under clinical observation.
Local injection-site reaction symptoms observed in clinical studies included erythema, swelling, itching, and pain. If local injection-related reactions occur, symptomatic treatment is recommended.
5.3 Reduction in Immunoglobulins
As expected with any B-cell depleting therapy, decreased immunoglobulin levels were observed. Decrease in immunoglobulin M (IgM) was reported in 7.7% of patients treated with KESIMPTA compared to 3.1% of patients treated with teriflunomide in RMS clinical trials [see Adverse Reactions (6.1)]. Treatment was discontinued because of decreased immunoglobulins in 3.4% of patients treated with KESIMPTA and in 0.8% of patients treated with teriflunomide. No decline in immunoglobulin G (IgG) was observed at the end of the study. Monitor the levels of quantitative serum immunoglobulins during treatment, especially in patients with opportunistic or recurrent infections, and after discontinuation of therapy until B-cell repletion. Consider discontinuing KESIMPTA therapy if a patient with low immunoglobulins develops a serious opportunistic infection or recurrent infections, or if prolonged hypogammaglobulinemia requires treatment with intravenous immunoglobulins.
5.4 Liver Injury
Clinically significant liver injury, without findings of viral hepatitis, has been reported in the postmarketing setting in patients treated with anti-CD20 B-cell depleting therapies approved for the treatment of MS, including KESIMPTA. Signs of liver injury, including markedly elevated serum hepatic enzymes with elevated total bilirubin, have occurred weeks to months after administration.
Patients treated with KESIMPTA found to have an alanine aminotransferase (ALT) or aspartate aminotransferase (AST) greater than 3x the upper limit of normal (ULN) with serum total bilirubin greater than 2x ULN, are potentially at risk for severe drug-induced liver injury.
Obtain liver function tests prior to initiating treatment with KESIMPTA [see Dosage and Administration (2.1)], and monitor for signs and symptoms of any hepatic injury during treatment. Measure serum aminotransferases, alkaline phosphatase, and bilirubin levels promptly in patients who report symptoms that may indicate liver injury, including new or worsening fatigue, anorexia, nausea, vomiting, right upper abdominal discomfort, dark urine, or jaundice. If liver injury is present and an alternative etiology is not identified, discontinue KESIMPTA.
5.5 Fetal Risk
Based on animal data, KESIMPTA can cause fetal harm due to B-cell lymphopenia and reduce antibody response in offspring exposed to KESIMPTA in utero. Transient peripheral B-cell depletion and lymphocytopenia have been reported in infants born to mothers exposed to other anti-CD20 B-cell depleting antibodies during pregnancy. Advise females of reproductive potential to use effective contraception while receiving KESIMPTA and for at least 6 months after the last dose [see Use in Specific Populations (8.1)].
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are discussed in greater detail elsewhere in the labeling:
- Infections [see Warnings and Precautions (5.1)]
- Injection-Related Reactions and Hypersensitivity Reactions [see Warnings and Precautions (5.2)]
- Reduction in Immunoglobulins [see Warnings and Precautions (5.3)]
- Liver Injury [see Warnings and Precautions (5.4)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Approximately 1500 patients with RMS received KESIMPTA in clinical studies. In Study 1 and Study 2, 1882 patients with RMS were randomized, 946 of whom were treated with KESIMPTA for a median duration of 85 weeks; 33% of patients receiving KESIMPTA were treated for up to 120 weeks [see Clinical Studies (14.1)]. The most common adverse reactions occurring in greater than 10% of patients treated with KESIMPTA and more frequently than in patients treated with teriflunomide were upper respiratory tract infections, injection-related reactions (systemic), headache, and injection-site reactions (local). The most common cause of discontinuation in patients treated with KESIMPTA was low immunoglobulin M (3.3%), defined in trial protocols as IgM at 10% below the lower limit of normal (LLN).
Table 1 summarizes the adverse drug reactions that occurred in Study 1 and Study 2.
Table 1: Adverse Reactions in Patients With RMS With an Incidence of at Least 5% With KESIMPTA and a Greater Incidence Than Teriflunomide (Pooled Study 1 and Study 2) aIncludes the following: nasopharyngitis, upper respiratory tract infection, influenza, sinusitis, pharyngitis, rhinitis, viral upper respiratory infection, tonsillitis, acute sinusitis, pharyngotonsillitis, laryngitis, pharyngitis streptococcal, viral rhinitis, sinusitis bacterial, tonsillitis bacterial, viral pharyngitis, viral tonsillitis, chronic sinusitis, nasal herpes, tracheitis. Adverse reactions KESIMPTA 20 mg
N = 946
%Teriflunomide 14 mg
N = 936
%Upper respiratory tract infectionsa 39 38 Injection-related reactions (systemic) 21 15 Headache 13 12 Injection-site reactions (local) 11 6 Urinary tract infection 10 8 Back pain 8 6 Blood immunoglobulin M decreased 6 2 Injection-Related Reactions and Injection-Site Reactions
The incidence of injection-related reactions (systemic) was highest with the first injection (14.4%), decreasing with subsequent injections (4.4% with second, less than 3% with third injection). Injection-related reactions were mostly (99.8%) mild to moderate in severity. Two (0.2%) patients treated with KESIMPTA reported serious injection-related reactions. There were no life-threatening injection-related reactions. Most frequently reported symptoms (2% or greater) included fever, headache, myalgia, chills, and fatigue.
In addition to systemic injection-related reactions, local reactions at the administration site were very common. Local injection-site reactions were all mild to moderate in severity. The most frequently reported symptoms (2% or greater) included erythema, pain, itching, and swelling [see Warnings and Precautions (5.2)].
Laboratory Abnormalities
Immunoglobulins
In Study 1 and Study 2, a decrease in the mean level of IgM was observed in KESIMPTA-treated patients but was not associated with an increased risk of infections [see Warnings and Precautions (5.3)]. In 14.3% of patients in Study 1 and Study 2, treatment with KESIMPTA resulted in a decrease in a serum IgM that reached a value below 0.34 g/L. KESIMPTA was associated with a decrease of 4.3% in mean IgG levels after 48 weeks of treatment and an increase of 2.2% after 96 weeks.
6.2 Immunogenicity
As with all therapeutic proteins, there is potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors, including assay methodology, sample handling, timing of sample collection, concomitant medication, and the underlying disease. For these reasons, comparison of the incidence of antibodies in the studies described below with the incidence of antibodies in other studies or to other ofatumumab products may be misleading.
Treatment-induced anti-drug antibodies (ADAs) were detected in 2 of 914 (0.2%) KESIMPTA-treated patients; no patients with treatment-enhancing or neutralizing ADAs were identified. There was no impact of positive ADA titers on pharmacokinetics, safety profile or B-cell kinetics in any patient; however, these data are not adequate to assess the impact of ADAs on the safety and efficacy of KESIMPTA.
6.3 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of KESIMPTA. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Immune System: Hypersensitivity reactions [see Warnings and Precautions (5.2)]
Hepatobiliary Disorders: Liver injury [see Warnings and Precautions (5.4)]
-
7 DRUG INTERACTIONS
7.1 Immunosuppressive or Immune-Modulating Therapies
Concomitant usage of KESIMPTA with immunosuppressant drugs, including systemic corticosteroids, may increase the risk of infection. Consider the risk of additive immune system effects when coadministering immunosuppressive therapies with KESIMPTA.
When switching from therapies with immune effects, the duration and mechanism of action of these therapies should be taken into account because of potential additive immunosuppressive effects when initiating KESIMPTA.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to KESIMPTA during pregnancy. Healthcare providers are encouraged to enroll pregnant patients, or pregnant women may register themselves in the MotherToBaby Pregnancy Study in Multiple Sclerosis by calling 1-877-311-8972, by sending an email to MotherToBaby@health.ucsd.edu, or by going to www.mothertobaby.org/join-study.
Risk Summary
There are no adequate data on the developmental risk associated with the use of KESIMPTA in pregnant women. Ofatumumab may cross the placenta and cause fetal B-cell depletion based on findings from animal studies (see Data).
Transient peripheral B-cell depletion and lymphocytopenia have been reported in infants born to mothers exposed to other anti-CD20 antibodies during pregnancy. B-cell levels in infants following maternal exposure to KESIMPTA have not been studied in clinical trials. The potential duration of B-cell depletion in infants exposed to ofatumumab in utero, and the impact of B-cell depletion on the safety and effectiveness of vaccines, are unknown. Avoid administering live vaccines to neonates and infants exposed to KESIMPTA in utero until B-cell recovery occurs [see Warnings and Precautions (5.2) and Clinical Pharmacology (12.2)].
Following administration of ofatumumab to pregnant monkeys, increased mortality, depletion of B-cell populations, and impaired immune function were observed in the offspring, in the absence of maternal toxicity, at plasma levels substantially higher than that in humans (see Data).
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. The background risk of major birth defects and miscarriage for the indicated population is unknown.
Data
Animal Data
Intravenous administration of ofatumumab (weekly doses of 0, 20, or 100 mg/kg) to pregnant monkeys during the period of organogenesis (gestations days 20 to 50) resulted in no adverse effects on embryofetal development; however, B-cell depletion was observed in fetuses at both doses when assessed on gestation day 100. Plasma exposure (Cave) at the no-effect dose (100 mg/kg) for adverse effects on embryofetal development was greater than 5000 times that in humans at the recommended human maintenance dose of 20 mg. A no-effect dose for effects on B-cells was not identified; plasma exposure (Cave) at the low-effect dose (20 mg/kg) was approximately 780 times that in humans at the recommended human maintenance dose (RHMD) of 20 mg/month.
Intravenous administration of ofatumumab (5 weekly doses of 0, 10, and 100 mg/kg, followed by biweekly doses of 0, 3, and 20 mg/kg) to pregnant monkeys throughout pregnancy resulted in no adverse effects on the development of the offspring. However, postnatal death, B-cell depletion, and impaired immune function were observed in the offspring at the high dose. The deaths at the high dose were considered secondary to B-cell depletion. Plasma exposure (Cave) in dams at the no-effect dose (100/20 mg/kg) for adverse developmental effects was approximately 500 times that in humans at RHMD. A no-effect level for mortality and immune effects in offspring was not established because of the limited number of evaluable offspring at the low dose.
8.2 Lactation
Risk Summary
There are no data on the presence of ofatumumab in human milk, the effects on the breastfed infant, or the effects of the drug on milk production. Human IgG is excreted in human milk, and the potential for absorption of ofatumumab to lead to B-cell depletion in the infant is unknown. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for KESIMPTA and any potential adverse effects on the breastfed infant from KESIMPTA or from the underlying maternal condition.
-
11 DESCRIPTION
Ofatumumab is a recombinant human monoclonal immunoglobulin G1 (IgG1) antibody that binds to human CD20 expressed on B-cells. Ofatumumab is produced in a murine NS0 cell line and consists of two IgG1 heavy chains and two kappa light chains with a molecular weight of approximately 146 kDa.
KESIMPTA (ofatumumab) injection is a sterile, preservative-free solution for subcutaneous use.
Each 20 mg/0.4 mL KESIMPTA Sensoready Pen or prefilled syringe delivers 0.4 mL of solution. Each 0.4 mL contains 20 mg of ofatumumab, and arginine (4 mg), disodium edetate (0.007 mg), polysorbate 80 (0.08 mg), sodium acetate trihydrate (2.722 mg), sodium chloride (1.192 mg), and Water for Injection, USP with a pH of 5.5. Hydrochloric acid may have been added to adjust pH.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The precise mechanism by which ofatumumab exerts its therapeutic effects in multiple sclerosis is unknown, but is presumed to involve binding to CD20, a cell surface antigen present on pre-B and mature B lymphocytes. Following cell surface binding to B lymphocytes, ofatumumab results in antibody-dependent cellular cytolysis and complement-mediated lysis.
12.2 Pharmacodynamics
B-cell Depletion
For B-cell counts, assays for CD19+ B-cells are used because the presence of ofatumumab interferes with the CD20 assay. In Study 1 and Study 2, KESIMPTA administered as recommended, resulted in a reduction of CD19+ B-cells to below the LLN in 77.0% and 78.8% of patients, respectively, one week after treatment initiation, and in 95.0% and 95.8% of patients, respectively, two weeks after treatment initiation [see Dosage and Administration (2.2) and Clinical Studies (14)]. In Study 1 and Study 2, at Week 12, 99.3% to 99.5% of patients had CD19+ B-cell counts below LLN. The CD19+ B-cell counts remained below LLN for approximately 97% of patients in Study 1 and 92% of patients in Study 2 from 12 weeks through 120 weeks while on KESIMPTA treatment.
In a study of bioequivalence using the same dosing regimen as in Study 1 and Study 2, before initiation of the maintenance phase, total CD19+ B-cell levels below the defined threshold of 10 cells/µL were achieved in 94% of patients starting at Week 4 and 98% of patients at Week 12.
B-cell Repletion
Data from Studies 1 and 2 indicate a median time to B-cell recovery to either LLN or baseline value of 24.6 weeks post-treatment discontinuation. Pharmacokinetics and pharmacodynamics modeling and simulation for B-cell repletion corroborate these data, predicting median time to B-cell recovery to LLN of 23 weeks post-treatment discontinuation.
12.3 Pharmacokinetics
Absorption
A subcutaneous dose of 20 mg every 4 weeks leads to a mean AUCtau of 483 mcg h/mL and a mean Cmax of 1.43 mcg/mL at steady state.
After subcutaneous administration, ofatumumab is believed to be predominantly absorbed via the lymphatic system similarly to other therapeutic monoclonal antibodies.
Distribution
The volume of distribution at steady-state was estimated to be 5.42 L following subcutaneous administration of repeated KESIMPTA 20 mg dose.
Elimination
Ofatumumab is eliminated by both linear catabolic pathways and a non-linear B-cell mediated pathway, resulting in non-constant elimination half-life. Initially, a higher baseline B-cell count results in greater B-cell-mediated elimination and shorter ofatumumab half-life. As the B-cells are depleted, the catabolic pathway predominates, resulting in a relatively longer ofatumumab half-life compared to earlier in therapy when both elimination pathways were available. Following B-cell depletion, clearance was estimated to be 0.34 L/day following repeated subcutaneous administration of KESIMPTA 20 mg injections. The half-life at steady state was estimated to be approximately 16 days following subcutaneous administration of repeated KESIMPTA 20 mg dosage.
Metabolism
Ofatumumab is a protein for which the expected metabolic pathway is degradation to small peptides and amino acids by ubiquitous proteolytic enzymes.
Excretion
Ofatumumab, a monoclonal antibody, is not likely to undergo renal excretion.
Specific Populations
The following population characteristics do not have a clinically meaningful effect on the pharmacokinetics of ofatumumab: body weight, sex, age, race, or baseline B-cell count.
Patients with Renal/Hepatic Impairment
Pharmacokinetics of ofatumumab in patients with renal or hepatic impairment have not been studied.
Drug Interaction Studies
Ofatumumab does not share a common clearance pathway with chemical drugs that are metabolized by the cytochrome P450 system or other drug-metabolizing enzymes. Additionally, there is no evidence that CD20 monoclonal antibodies are involved in the regulation of the expression of drug-metabolizing enzymes. Interactions between KESIMPTA and other medicinal products have not been investigated in formal studies.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
No carcinogenicity studies have been conducted to assess the carcinogenic potential of ofatumumab.
Mutagenesis
No studies have been conducted to assess the mutagenic potential of ofatumumab. As an antibody, ofatumumab is not expected to interact directly with DNA.
Impairment of Fertility
No effects on reproductive parameters, including hormones, menstrual cycle, sperm analysis, or histopathological evaluation of reproductive organs, were observed in male or female monkeys administered ofatumumab by intravenous injection (5 weekly doses of 0, 10, and 100 mg/kg, followed by biweekly doses of 0, 3, and 20 mg/kg). Plasma exposures (Cave) at the high dose tested in monkeys are greater than 500 times that in humans at the recommended human maintenance dose of 20 mg/month.
-
14 CLINICAL STUDIES
The efficacy of KESIMPTA was demonstrated in two randomized, double-blind, double-dummy, active comparator-controlled clinical trials of identical design, in patients with relapsing forms of MS [Study 1 (NCT02792218) and Study 2 (NCT02792231)]. Both studies enrolled patients with at least one relapse in the previous year, 2 relapses in the previous 2 years, or the presence of a T1 gadolinium-enhancing (GdE) lesion in the previous year. Patients were also required to have an Expanded Disability Status Scale (EDSS) score from 0 to 5.5.
Patients were randomized to receive either KESIMPTA, 20 mg subcutaneously on Days 1, 7, and 14, followed by 20 mg every 4 weeks thereafter starting at Week 4 with a daily oral placebo, or the active comparator, teriflunomide, at a dose of 14 mg orally once daily with a placebo administered subcutaneously on Days 1, 7, 14, and every 4 weeks thereafter. The treatment duration for an individual patient was variable based on when the end-of-study criteria were met. The maximal duration of treatment for an individual patient was 120 weeks. Neurologic evaluations were performed at baseline, every 3 months during blinded treatment, and at the time of a suspected relapse. Brain MRI scans were performed at baseline, 1 year, and 2 years.
The primary endpoint of both trials was the annualized relapse rate (ARR) over the treatment period. Additional outcome measures included: 1) the time to 3-month confirmed disability progression for the pooled populations, 2) the number of T1 GdE lesions per scan at Weeks 48 and 96, and 3) the annualized rate of new or enlarging T2 MRI lesions. Disability progression was defined as an increase in EDSS of at least 1.5, 1, or 0.5 points in patients with a baseline EDSS of 0, 1 to 5, or 5.5 or greater, respectively.
In Study 1, a total of 927 patients were randomized to receive KESIMPTA (n = 465) or teriflunomide (n = 462). Of those randomized to KESIMPTA, 90% completed the study; of those randomized to teriflunomide, 81% completed the study. Demographics and disease characteristics were balanced across treatment arms. The mean age was 38 years, 89% were White, and 69% were female. The mean time since MS diagnosis was 5.7 years and the median EDSS score at baseline was 3.0; 60% had been treated with a non-steroid therapy for MS. At baseline, the mean number of relapses in the previous year was 1 and the mean number of T1 GdE lesions on MRI scan was 1.5.
In Study 2, a total of 955 patients were randomized to receive KESIMPTA (n = 481) or teriflunomide (n = 474). Of those randomized to KESIMPTA, 83% completed the study; of those randomized to teriflunomide, 82% completed the study. Demographics and disease characteristics were balanced across treatment arms. The mean age was 38 years, 87% were White, and 67% were female. The mean time since MS diagnosis was 5.5 years and the median EDSS score at baseline was 2.5; 61% had been treated with a non-steroid therapy for MS. At baseline, the mean number of relapses in the previous year was 1.3, and the mean number of T1 GdE lesions on MRI scan was 1.6.
In both studies, KESIMPTA significantly lowered the ARR compared to teriflunomide.
KESIMPTA significantly reduced the risk of 3-month confirmed disability progression compared to teriflunomide.
KESIMPTA significantly reduced the number of T1 GdE lesions and the rate of new or enlarging T2 lesions in both studies.
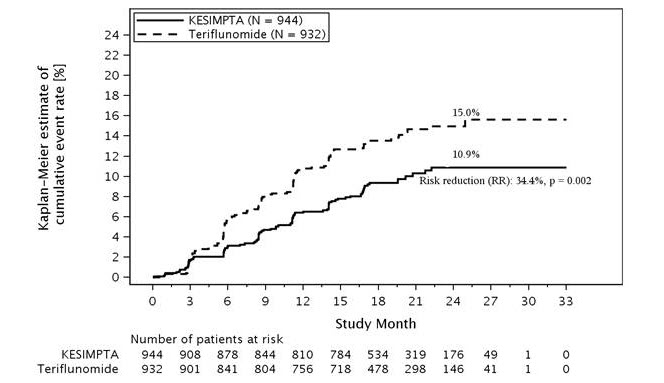
Key results for Study 1 and Study 2 are presented in Table 2 and Figure 1.
Table 2: Key Clinical and MRI Endpoints From Study 1 and Study 2 aDisability progression was defined as an increase in EDSS of at least 1.5, 1, or 0.5 points in patients with a baseline EDSS of 0, 1 to 5, or 5.5 or greater, respectively.
bProspective pooled analysis of Studies 1 and 2. Proportion of patients with 3-month confirmed disability progression refers to Kaplan-Meier estimates at Month 24.Study 1 Study 2 Endpoints KESIMPTA
20 mg
(n = 465)Teriflunomide
14 mg
(n = 462)KESIMPTA
20 mg
(n = 481)Teriflunomide
14 mg
(n = 474)Clinical Endpoints Annualized relapse rate (primary endpoint) 0.11 0.22 0.10 0.25 Relative reduction 51% (p < 0.001) 58% (p < 0.001) Proportion of patients with 3-month confirmed disability progressiona,b
Relative risk reduction10.9% KESIMPTA vs 15.0% teriflunomide
34.3% (p = 0.003)MRI Endpoints Mean number of T1 Gd-enhancing lesions per MRI scan 0.01 0.46 0.03 0.52 Relative reduction 98% (p < 0.001) 94% (p < 0.001) Number of new or enlarging T2 lesions per year 0.72 4.00 0.64 4.16 Relative reduction 82% (p < 0.001) 85% (p < 0.001) Figure 1: Time to First 3-month Confirmed Disability Progression by Treatment Full Analysis Set
A similar effect of KESIMPTA on the key efficacy results compared to teriflunomide was observed across the two studies in exploratory subgroups defined by sex, age, body weight, prior non-steroid MS therapy, and baseline disability and disease activity.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
KESIMPTA (ofatumumab) injection is a preservative-free, clear to slightly opalescent and colorless to slightly brownish-yellow solution for subcutaneous administration, which is supplied as follows:
KESIMPTA Sensoready Pen:
Carton of one 20 mg/0.4 mL single-dose prefilled Sensoready Pen NDC: 0078-1007-68
KESIMPTA Prefilled Syringe:
Carton of one 20 mg/0.4 mL single-dose prefilled syringe NDC: 0078-1007-69
16.2 Storage and Handling
KESIMPTA Sensoready pens and prefilled syringes must be refrigerated at 2ºC to 8ºC (36ºF to 46ºF). Keep the product in the original carton to protect from light until the time of use. Do not freeze. To avoid foaming, do not shake.
If necessary, KESIMPTA may be stored for up to 7 days at room temperature, not to exceed 30°C (86°F). Write the date removed from the refrigerator in the space provided on the carton labeling. If stored below 30°C (86°F), unused KESIMPTA may be returned to the refrigerator and must be used within the next 7 days or discarded after 7 days.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read FDA-approved patient labeling (Medication Guide and Instructions for Use).
Infections
Advise patients to contact their healthcare provider for any signs of infection during treatment or after the last dose. Signs include fever, chills, constant cough, or dysuria [see Warnings and Precautions (5.1)].
Advise patients that KESIMPTA may cause reactivation of hepatitis B infection and that monitoring will be required if they are at risk [see Warnings and Precautions (5.1)].
Advise patients that PML has happened with an intravenous form of ofatumumab administered at a higher intravenous dosage in patients with CLL, as well as with drugs that are similar to KESIMPTA, and may happen with KESIMPTA. Inform the patient that PML is characterized by a progression of deficits and usually leads to death or severe disability over weeks or months. Instruct the patient of the importance of contacting their healthcare provider if they develop any symptoms suggestive of PML. Inform the patient that typical symptoms associated with PML are diverse, progress over days to weeks, and include progressive weakness on one side of the body or clumsiness of limbs, disturbance of vision, and changes in thinking, memory, and orientation leading to confusion and personality changes [see Warnings and Precautions (5.1)].
Vaccinations
Advise patients to complete any required live or live-attenuated vaccinations at least 4 weeks and, whenever possible at least 2 weeks, prior to initiation of KESIMPTA for inactivated vaccines.
Administration of live-attenuated or live vaccines is not recommended during KESIMPTA treatment and until B-cell recovery [see Warnings and Precautions (5.1)].
Injection-Related Reactions and Hypersensitivity Reactions
Inform patients about the signs and symptoms of injection-related reactions and hypersensitivity reactions. Inform patients that injection-related reactions generally occur within 24 hours and predominantly following the first injection. A hypersensitivity reaction may occur with any injection, and any new or worsening symptoms with subsequent KESIMPTA injections should prompt consideration of a hypersensitivity reaction. Advise patients to seek immediate medical attention if they experience signs or symptoms of a severe or life-threatening injection-related reaction or hypersensitivity reaction, and to contact their healthcare provider if they experience any signs or symptoms of an injection-related reaction or hypersensitivity reaction [see Warnings and Precautions (5.2)].
Liver Injury
Inform patients that liver injury has been reported with anti-CD20 B-cell depleting therapies, including KESIMPTA. Instruct patients treated with KESIMPTA to promptly report any symptoms that may indicate liver injury, including fatigue, anorexia, nausea, vomiting, right upper abdominal discomfort, dark urine, or jaundice. A blood test should be obtained before patients start therapy, and during treatment as clinically indicated [see Warnings and Precautions (5.4)].
Contraception
Advise females of childbearing potential to use effective contraception while receiving KESIMPTA and for 6 months after the last treatment of KESIMPTA [see Warnings and Precautions (5.5) and Use in Specific Populations (8.3)].
Pregnancy Exposure Registry
Instruct patients that if they are pregnant or plan to become pregnant while taking KESIMPTA, they should inform their healthcare provider. Encourage patients to enroll in the MotherToBaby Pregnancy Study in Multiple Sclerosis if they become pregnant while taking KESIMPTA [see Use in Specific Populations (8.1)].
Instruction on Injection Technique
Patients or caregivers should be instructed by a healthcare professional on how to administer KESIMPTA [see Instructions for Use].
Instruct patients or caregivers in the technique of proper syringe and needle disposal, and advise them not to reuse these items. Instruct patients to inject the full amount of KESIMPTA according to the directions provided in the Instructions for Use. Dispose of pens and syringes in a puncture-resistant container.
Manufactured by:
Novartis Pharmaceuticals Corporation
East Hanover, NJ 07936
U.S. License No.: 1244KESIMPTA and SENSOREADY are [registered] trademarks of Novartis AG.
T2025-49
-
MEDICATION GUIDE
This Medication Guide has been approved by the U.S. Food and Drug Administration. Revised: 8/2025 MEDICATION GUIDE KESIMPTA® (KEY-simp-ta)
(ofatumumab)
injection, for subcutaneous useWhat is the most important information I should know about KESIMPTA?
KESIMPTA can cause serious side effects, including:
Infections. Serious infections, which can be life-threatening or cause death, can happen during treatment with KESIMPTA. If you have an active infection, your healthcare provider should delay your treatment with KESIMPTA until your infection is gone. KESIMPTA taken before or after other medicines that weaken the immune system may increase your risk of getting infections.
Tell your healthcare provider right away if you have any infections or get any symptoms, including painful and frequent urination, nasal congestion, runny nose, sore throat, fever, chills, cough, or body aches.- Hepatitis B virus (HBV) reactivation. Before starting treatment with KESIMPTA, your healthcare provider will do blood tests to check for HBV. If you have ever had HBV infection, the HBV may become active again during or after treatment with KESIMPTA. Hepatitis B virus becoming active again (called reactivation) may cause serious liver problems, including liver failure or death. You should not receive KESIMPTA if you have active hepatitis B liver disease. Your healthcare provider will monitor you for HBV infection during and after you stop using KESIMPTA.
- Progressive Multifocal Leukoencephalopathy (PML). PML may happen with KESIMPTA. PML is a rare, serious brain infection caused by a virus that may get worse over days or weeks. PML can result in death or severe disability. Tell your healthcare provider right away if you have any new or worsening neurologic signs or symptoms. These may include weakness on one side of your body, loss of coordination in arms and legs, vision problems, changes in thinking and memory which may lead to confusion and personality changes.
- Weakened immune system. KESIMPTA taken before or after other medicines that weaken the immune system could increase your risk of getting infections.
What is KESIMPTA?
KESIMPTA is a prescription medicine used to treat adults with relapsing forms of multiple sclerosis (MS), including:- clinically isolated syndrome
- relapsing-remitting disease
- active secondary progressive disease
Do not use KESIMPTA if you: - have an active hepatitis B virus infection.
- have had an allergic reaction to ofatumumab or life-threatening injection-related reaction to KESIMPTA. See the end of this Medication Guide for a complete list of ingredients in KESIMPTA.
Before using KESIMPTA, tell your healthcare provider about all of your medical conditions, including if you: - have or think you have an infection, including HBV or PML. See “What is the most important information I should know about KESIMPTA?”
- have ever taken, currently take, or plan to take medicines that affect your immune system. These medicines could increase your risk of getting an infection.
- have a history of liver problems.
- have had a recent vaccination or are scheduled to receive any vaccinations.
- You should receive any required ‘live’ or ‘live-attenuated’ vaccines at least 4 weeks before you start treatment with KESIMPTA. You should not receive ‘live’ or ‘live-attenuated’ vaccines while you are being treated with KESIMPTA and until your healthcare provider tells you that your immune system is no longer weakened.
- Whenever possible, you should receive any ‘non-live’ vaccines at least 2 weeks before you start treatment with KESIMPTA.
- Talk to your healthcare provider about vaccinations for your baby if you used KESIMPTA during your pregnancy.
- are pregnant, think that you might be pregnant, or plan to become pregnant. It is not known if KESIMPTA will harm your unborn baby. Females who can become pregnant should use birth control (contraception) during treatment with KESIMPTA and for 6 months after your last treatment. Talk with your healthcare provider about what birth control method is right for you during this time.
- Pregnancy Registry: There is a registry for women who become pregnant during treatment with KESIMPTA. If you become pregnant while taking KESIMPTA, tell your healthcare provider right away. Talk to your healthcare provider about registering with the MotherToBaby Pregnancy Study in Multiple Sclerosis. The purpose of the registry is to collect information about your health and your baby’s health. For more information or to register, contact MotherToBaby by calling 1-877-311-8972, by sending an email to MotherToBaby@health.ucsd.edu, or go to www.mothertobaby.org/join-study.
- are breastfeeding or plan to breastfeed. It is not known if KESIMPTA passes into your breast milk. Talk to your healthcare provider about the best way to feed your baby if you take KESIMPTA.
Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.How should I use KESIMPTA?
See the detailed Instructions for Use that comes with KESIMPTA for information about how to prepare and inject a dose of KESIMPTA and how to properly throw away (dispose of) used KESIMPTA Sensoready pens or prefilled syringes.- Use KESIMPTA exactly as your healthcare provider tells you to use it.
- KESIMPTA is given as an injection under your skin (subcutaneous injection), in your thigh or stomach-area (abdomen) by you or a caregiver. A caregiver may also give you an injection of KESIMPTA in your upper outer arm.
- Your healthcare provider will show you how to prepare and inject KESIMPTA the right way before you use it for the first time.
- Do not inject into areas where the skin is tender, bruised, red, scaly or hard. Avoid areas with moles, scars or stretch marks.
- The initial dosing is 20 mg of KESIMPTA given by subcutaneous injection at Weeks 0, 1, and 2. There is no injection at Week 3. Starting at Week 4 and then every month, the recommended dose is 20 mg of KESIMPTA administered by subcutaneous injection.
- If you miss an injection of KESIMPTA at Week 0, 1, or 2, talk to your healthcare provider. If you miss a monthly injection, give it as soon as possible without waiting until the next scheduled dose. After that, give your KESIMPTA injections a month apart.
What are the possible side effects of KESIMPTA?
KESIMPTA may cause serious side effects, including:
See “What is the most important information I should know about KESIMPTA?”-
Injection-related reactions. Injection-related reactions are a common side effect of KESIMPTA. Injecting KESIMPTA can cause injection-related reactions that can happen within 24 hours (1 day) following the first injection and with later injections. There are two kinds of reactions:
- at or near the injection site: redness of the skin, swelling, itching and pain. Talk with your healthcare provider if you have any of these signs and symptoms.
- that may happen when certain substances are released in your body: fever, headache, pain in the muscles, chills, tiredness, rash, hives, trouble breathing, swelling of the face, eyelids, lips, mouth, tongue and throat, and feeling faint, or chest tightness. Contact your healthcare provider right away if you experience any of these signs and symptoms, especially if they become worse or you have new severe signs of reactions after subsequent injections. It could be a sign of an allergic reaction, which can be serious.
- Low immunoglobulins. KESIMPTA may cause a decrease in some types of antibodies. Your healthcare provider will do blood tests to check your blood immunoglobulin levels.
-
Liver damage. KESIMPTA may cause liver damage. Your healthcare provider will do blood tests to check your liver before you start KESIMPTA and while you take KESIMPTA if needed. Tell your healthcare provider right away if you have any symptoms of liver damage, such as:
- yellowing of the skin and eyes (jaundice)
- nausea
- vomiting
- unusual darkening of the urine
- feeling tired or weak
- upper respiratory tract infection, with symptoms, such as sore throat and runny nose, and headache. See “What is the most important information I should know about KESIMPTA?”
- headache
You may report side effects to FDA at 1-800-FDA-1088.How should I store KESIMPTA? - Store KESIMPTA in a refrigerator between 36°F to 46°F (2°C to 8°C).
- Keep KESIMPTA in the original carton until ready for use to protect from light.
- If needed, KESIMPTA may be stored for up to 7 days at room temperature, up to 86°F (30°C).
- Write the date taken out of the refrigerator in the space provided on the carton.
- If stored below 86°F (30°C), unused KESIMPTA may be returned to the refrigerator and must be used within the next 7 days. If this KESIMPTA is not used within those 7 days, then discard the medicine.
- Do not freeze KESIMPTA.
- Do not shake KESIMPTA.
General information about the safe and effective use of KESIMPTA.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use KESIMPTA for a condition for which it was not prescribed. Do not give KESIMPTA to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about KESIMPTA that is written for health professionals.What are the ingredients in KESIMPTA?
Active ingredient: ofatumumab
Inactive ingredients: Sensoready Pen and prefilled syringe: arginine, disodium edetate, polysorbate 80, sodium acetate trihydrate, sodium chloride, and Water for Injection. Hydrochloric acid may be added.
Distributed by: Novartis Pharmaceuticals Corporation, East Hanover, New Jersey 07936
For more information, go to www.novartis.us or call 1-888-669-6682.T2025-50
-
INSTRUCTIONS FOR USE
This Instructions for Use has been approved by the U.S. Food and Drug Administration. Revised: 9/2022 INSTRUCTIONS FOR USE
KESIMPTA® [KEY-simp-ta]
(ofatumumab)
injection, for subcutaneous use
Sensoready® PenThis Instructions for Use contains information on how to inject KESIMPTA Sensoready Pen.
Be sure that you read, understand, and follow this Instructions for Use before injecting KESIMPTA. Your healthcare provider should show you how to prepare and inject KESIMPTA the right way using the Sensoready Pen before you use it for the first time. Talk to your healthcare provider if you have any questions before you use KESIMPTA for the first time.
Important Information You Need to Know Before Injecting KESIMPTA Sensoready Pen.- Do not use the KESIMPTA Sensoready Pen if either the seal on the outer carton or the seal on the KESIMPTA Sensoready Pen is broken. Keep the KESIMPTA Sensoready Pen in the sealed outer carton until you are ready to use it.
- Do not shake the KESIMPTA Sensoready Pen.
- If you drop your KESIMPTA Sensoready Pen, do not use it if it looks damaged, or if you dropped it with the cap removed.
How should I store KESIMPTA Sensoready Pen? - Store your carton of KESIMPTA Sensoready Pen in a refrigerator, between 36°F to 46°F (2°C to 8°C).
- Keep KESIMPTA Sensoready Pen in the original carton until ready to use to protect from light.
- If needed, KESIMPTA Sensoready Pen may be stored for up to 7 days at room temperature, up to 86°F (30°C).
- Write the date taken out of the refrigerator in the space provided on the carton.
- If stored below 86°F (30°C), unused KESIMPTA may be returned to the refrigerator and must be used within the next 7 days. If this KESIMPTA is not used within those 7 days, then discard the medicine.
- Do not freeze KESIMPTA Sensoready Pen.
KESIMPTA Sensoready Pen parts (see Figure A):
Figure A
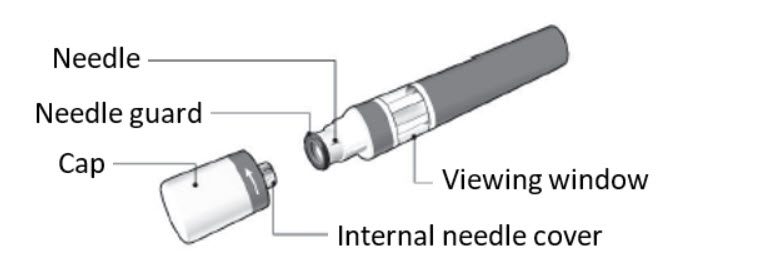
The KESIMPTA Sensoready Pen is shown with the cap removed. Do not remove the cap until you are ready to inject.
What you need for your injection:
Included in the carton:
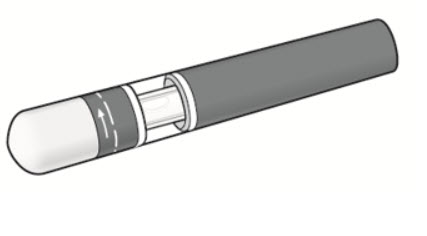
A new KESIMPTA Sensoready Pen (see Figure B).
Figure B
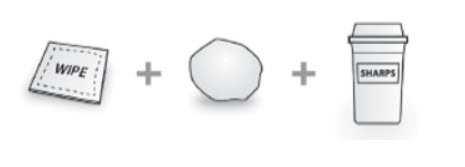
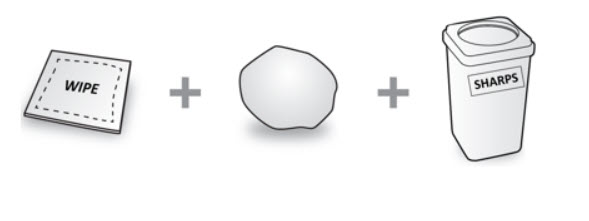
Not included in the carton (see Figure C): - 1 alcohol wipe
- 1 cotton ball or gauze
- Sharps disposal container
Figure C
Before your injection
Take the KESIMPTA Sensoready Pen out of the refrigerator 15 to 30 minutes before injecting to allow it to reach room temperature.
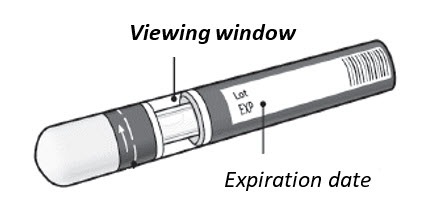
Step 1. Important safety checks before you inject (see Figure D):- Look through the viewing window. The liquid should be clear to slightly cloudy.
You may see a small air bubble, which is normal.- Look at the expiration date (EXP) on your KESIMPTA Sensoready Pen. Do not use your pen if the expiration date has passed.
Figure D
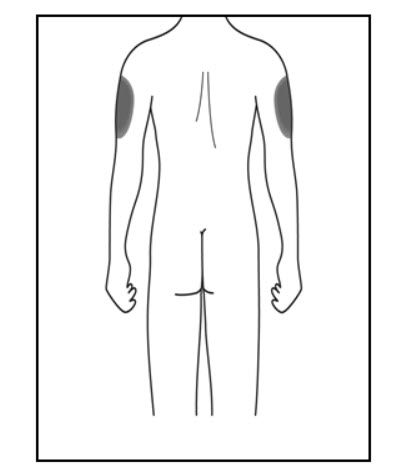
Step 2. Choose your injection site: - The recommended site is the front of the thighs. You may also use the lower stomach area (lower abdomen), but not the area 2 inches around the navel (belly button) (see Figure E).
- Do not inject into areas where the skin is tender, bruised, red, scaly, or hard. Avoid areas with moles, scars or stretch marks.
- If a caregiver or healthcare provider is giving you your injection, they may also inject into your outer upper arm (see Figure F).
Figure E

Figure F (Caregiver and healthcare provider only)
Step 3. Clean your injection site: - Wash your hands with soap and water.
- Using a circular motion, clean the injection site with the alcohol wipe. Leave it to dry before injecting (see Figure G).
- Do not touch the cleaned area again before injecting.
Figure G

Your injection
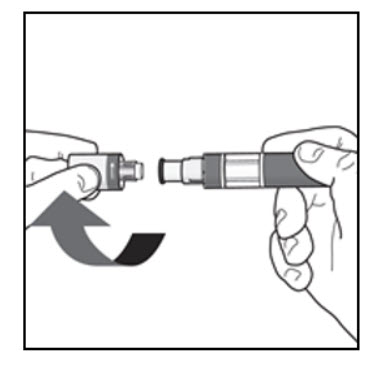
Step 4. Remove the cap:- Only remove the cap when you are ready to use the KESIMPTA Sensoready Pen.
- Twist off the cap in the direction of the arrow (see Figure H).
- Throw away the cap. Do not try to re-attach the cap.
- Use the KESIMPTA Sensoready Pen within 5 minutes of removing the cap.
Figure H
Step 5. Hold your KESIMPTA Sensoready Pen: - Hold the KESIMPTA Sensoready Pen at 90 degrees to the cleaned injection site (see Figure I).
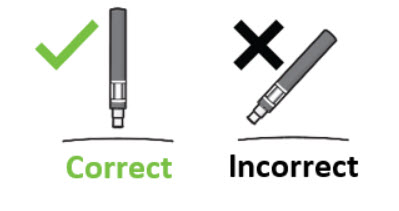
Figure I

Important: During the injection you will hear 2 loud clicks: - The 1st click indicates that the injection has started
- A 2nd click will indicate that the injection is almost complete
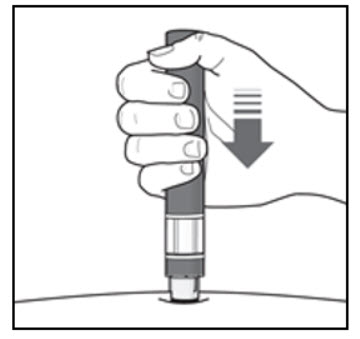
Step 6. Start your injection:- Press the KESIMPTA Sensoready Pen firmly against the skin to start the injection (see Figure J).
- The 1st click indicates the injection has started.
- Keep holding the KESIMPTA Sensoready Pen firmly against your skin.
- The green indicator shows the progress of the injection.
Figure J
Step 7. Complete your injection: - Listen for the 2nd click. This indicates that the injection is almost complete.
- Check to see if the green indicator fills the window and has stopped moving (see Figure K).
- The KESIMPTA Sensoready Pen can now be removed (see Figure L).
Figure K
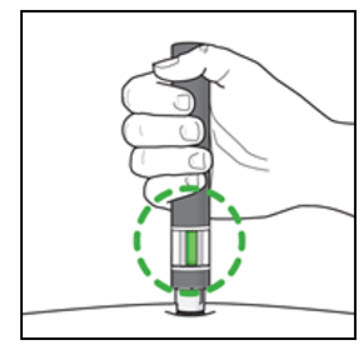
After your injection - In case the green indicator does not fill the window, it means the medicine has not been delivered. Contact your healthcare provider if the green indicator is not visible.
- There may be a small amount of blood at the injection site. You can press a cotton ball or gauze over the injection site and hold it for 10 seconds. Do not rub the injection site. You may cover the injection site with a small adhesive bandage, if needed.
Figure L

How should I dispose of used KESIMPTA Sensoready® Pens?
Step 8. Put your used KESIMPTA Sensoready Pen in an FDA-cleared sharps disposal container right away after use (see Figure M). Do not throw away (dispose of) your used KESIMPTA Sensoready Pen in your household trash.
If you do not have an FDA-cleared sharps disposal container, you may use a household container that is:- made of a heavy-duty plastic,
- can be closed with a tight-fitting, puncture-resistant lid, without sharps being able to come out,
- upright and stable during use,
- leak-resistant, and
- properly labeled to warn of hazardous waste inside the container.
When your sharps disposal container is almost full, you will need to follow your community guidelines for the right way to dispose of your sharps disposal container. There may be state or local laws about how you should throw away used needles, syringes and pens. For more information about safe sharps disposal, and for specific information about sharps disposal in the state that you live in, go to the FDA’s website at: http://www.fda.gov/safesharpsdisposal.
Keep the sharps container out of the reach of children.
Manufactured by:
Novartis Pharmaceuticals Corporation
East Hanover, NJ 07936
U.S. License No.: 1244Figure M

T2022-54
-
INSTRUCTIONS FOR USE
This Instructions for Use has been approved by the U.S. Food and Drug Administration. Revised: 4/2024 INSTRUCTIONS FOR USE
KESIMPTA® [KEY-simp-ta]
(ofatumumab)
injection, for subcutaneous use
Prefilled SyringeThis Instructions for Use contains information on how to inject KESIMPTA Prefilled Syringe.
Be sure that you read, understand, and follow this Instructions for Use before injecting KESIMPTA prefilled syringe. Your healthcare provider should show you how to prepare and inject KESIMPTA the right way before using the prefilled syringe the first time. Talk to your healthcare provider if you have any questions.
Important Information You Need to Know Before Injecting KESIMPTA prefilled syringe.- Do not use the KESIMPTA prefilled syringe if either the seal on the outer carton or the seal of the blister is broken. Keep the KESIMPTA prefilled syringe in the sealed carton until you are ready to use it.
- Do not shake the KESIMPTA prefilled syringe.
- The KESIMPTA prefilled syringe has a needle guard that will be activated to cover the needle after the injection is finished. The needle guard will help to prevent needle stick injuries to anyone who handles the KESIMPTA prefilled syringe after injection.
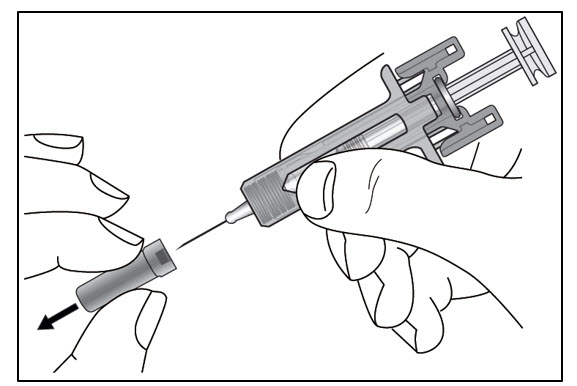
- Do not remove the needle cap until just before you give the injection.
- Avoid touching the syringe guard wings before use. Touching them may cause the needle guard to be activated too early.
- Do not use if the prefilled syringe has been dropped onto a hard surface or dropped after removing the needle cap.
- Throw away (dispose of) the used KESIMPTA prefilled syringe right away after use. Do not re-use a KESIMPTA prefilled syringe. See "How should I dispose of used KESIMPTA prefilled syringes?” at the end of these Instructions for Use.
How should I store KESIMPTA Prefilled Syringe? - Store your carton of the KESIMPTA prefilled syringe in a refrigerator, between 36°F to 46°F (2°C to 8°C).
- Keep the KESIMPTA prefilled syringe in the original carton until ready to use to protect from light.
- If needed, KESIMPTA prefilled syringe may be stored for up to 7 days at room temperature, up to 86°F (30°C).
- Write the date taken out of the refrigerator in the space provided on the carton.
- If stored below 86°F (30°C), unused KESIMPTA may be returned to the refrigerator and must be used within the next 7 days. If this KESIMPTA is not used within those 7 days, then discard the medicine.
- Do not freeze the KESIMPTA prefilled syringe.
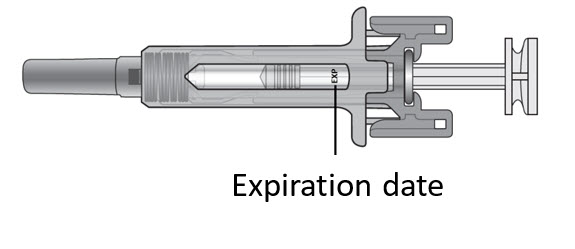
KESIMPTA prefilled syringe parts (see Figure A):
Figure A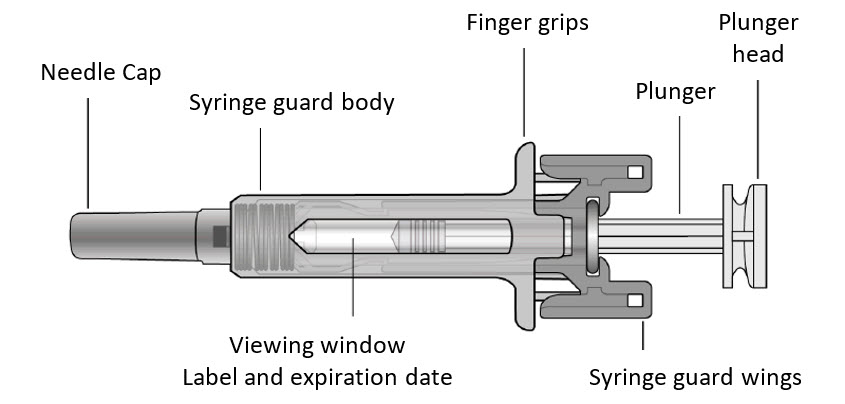
What you need for your injection
Included in the carton:
A new KESIMPTA prefilled syringe.
Not included in the carton (see Figure B):- 1 alcohol wipe
- 1 cotton ball or gauze
- Sharps disposal container
Figure B
Prepare the KESIMPTA prefilled syringe
Step 1. Find a clean, well-lit, flat work surface.
Step 2. Take the carton containing the KESIMPTA prefilled syringe out of the refrigerator and leave it unopened on your work surface for about 15 to 30 minutes so that it reaches room temperature.
Step 3. Wash your hands well with soap and water.
Step 4. Remove the KESIMPTA prefilled syringe from the outer carton and take it out of the blister by holding the syringe guard body.
Step 5. Look through the viewing window on the KESIMPTA prefilled syringe. The liquid inside should be clear to slightly cloudy. You may see a small air bubble in the liquid, which is normal. Do not use the KESIMPTA prefilled syringe if the liquid contains particles or is cloudy.
Step 6. Do not use the KESIMPTA prefilled syringe if it is broken. Return the KESIMPTA prefilled syringe and the package it came in to the pharmacy.
Step 7. Do not use the KESIMPTA prefilled syringe if the expiration date has passed (see Figure C). Return the expired KESIMPTA prefilled syringe and the package it came in to the pharmacy.Figure C
Choose and clean the injection site - Areas of your body that you may use as injection sites include:
- the front of your thighs (see Figure D)
- the lower stomach-area (abdomen), but not the area 2 inches around your navel (belly button) (see Figure D)
- your outer upper arms, if a healthcare provider or caregiver is giving you the injection (see Figure E)
- Do not inject into areas where the skin is tender, bruised, red, scaly, or hard. Avoid areas with moles, scars, or stretch marks.
Figure D
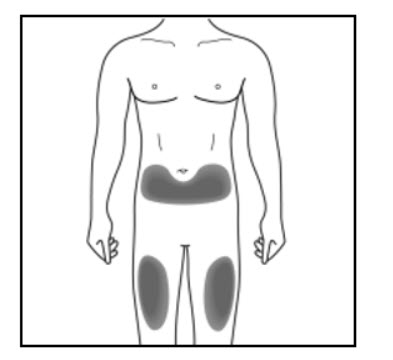
Figure E (Caregiver and healthcare provider only)
Giving your injection
Step 9. Carefully remove the needle cap from the KESIMPTA prefilled syringe (see Figure F). Throw away the needle cap. You may see a drop of liquid at the end of the needle. This is normal.Figure F
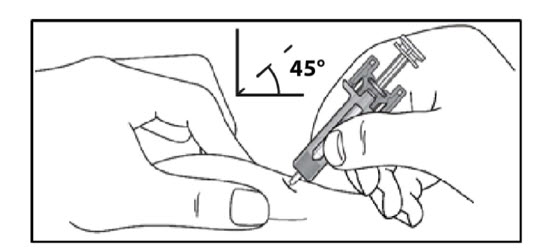
Step 10. With one hand, gently pinch the skin at the injection site. With your other hand insert the needle into your skin at an angle of about 45 degrees as shown (see Figure G). Push the needle all the way in to make sure that you inject your full dose. Figure G
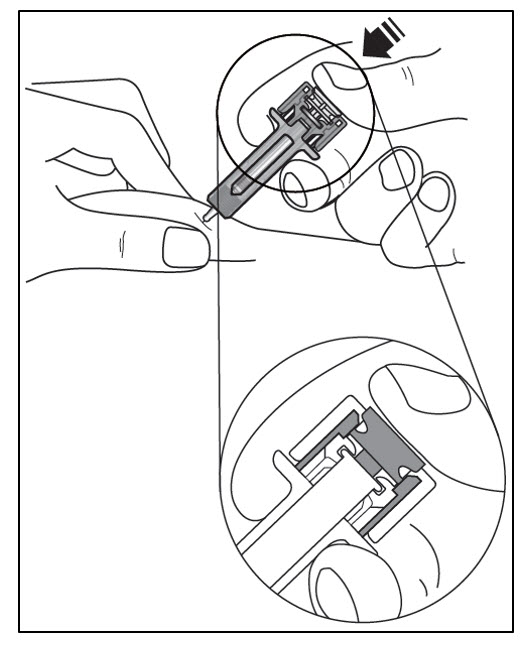
Step 11. Hold the KESIMPTA prefilled syringe finger grips as shown (see Figure H). Slowly press down on the plunger head as far as it will go, so that the plunger head is completely between the syringe guard wings.
Continue to press fully on the plunger head for an additional 5 seconds. Hold the syringe in place for the full 5 seconds.Figure H
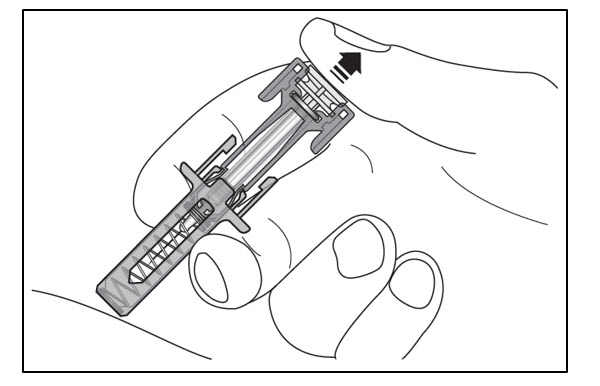
Step 12. Slowly release the plunger head until the needle is covered (see Figure I), and then remove the syringe from the injection site.
Step 13. There may be a small amount of blood at the injection site. You can press a cotton ball or gauze over the injection site and hold it for 10 seconds. Do not rub the injection site. You may cover the injection site with a small adhesive bandage, if needed.Figure I
How should I dispose of used KESIMPTA prefilled syringes?
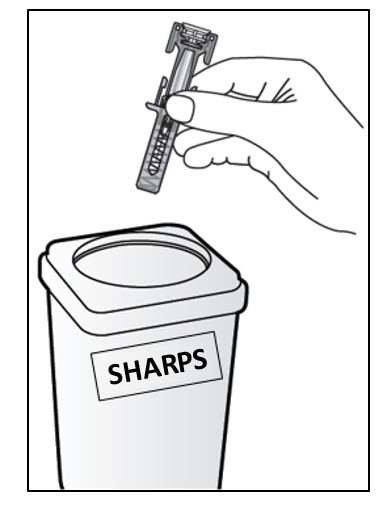
Step 14. Put your used KESIMPTA prefilled syringe in an FDA-cleared sharps disposal container right away after use (see Figure J). Do not throw away (dispose of) your used KESIMPTA prefilled syringe in your household trash. Never try to reuse your KESIMPTA prefilled syringe.
If you do not have an FDA-cleared sharps disposal container, you may use a household container that is:- made of a heavy-duty plastic,
- can be closed with a tight-fitting, puncture-resistant lid, without sharps being able to come out,
- upright and stable during use,
- leak-resistant, and
- properly labeled to warn of hazardous waste inside the container.
When your sharps disposal container is almost full, you will need to follow your community guidelines for the right way to dispose of your sharps disposal container. There may be state or local laws about how you should throw away used needles, syringes, and prefilled syringes. For more information about safe sharps disposal, and for specific information about sharps disposal in the state that you live in, go to the FDA’s website at: http://www.fda.gov/safesharpsdisposal.
Keep the sharps container out of the reach of children.
Manufactured by:
Novartis Pharmaceuticals Corporation
East Hanover, NJ 07936
U.S. License No.: 1244Figure J
T2024-33
-
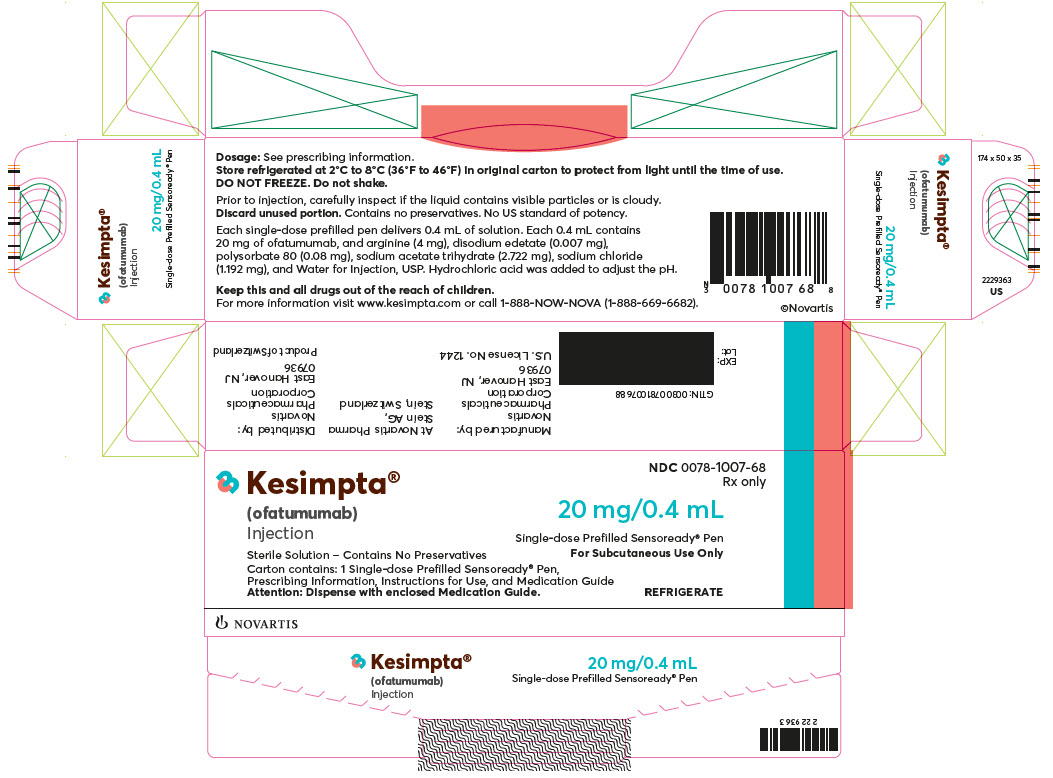
PRINCIPAL DISPLAY PANEL
NDC: 0078-1007-68
Rx only
Kesimpta®
(ofatumumab)
Injection20 mg/0.4 mL
Single-dose Prefilled Sensoready® Pen
For Subcutaneous Use OnlySterile Solution - Contains No Preservatives
Carton contains: 1 Single-dose Prefilled Sensoready® Pen,
Prescribing Information, Instructions for Use, and Medication GuideAttention: Dispense with enclosed Medication Guide.
REFRIGERATE
NOVARTIS
-
INGREDIENTS AND APPEARANCE
KESIMPTA
ofatumumab injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0078-1007 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength OFATUMUMAB (UNII: M95KG522R0) (OFATUMUMAB - UNII:M95KG522R0) OFATUMUMAB 20 mg in 0.4 mL Inactive Ingredients Ingredient Name Strength ARGININE (UNII: 94ZLA3W45F) 4.000 mg in 0.4 mL HYDROCHLORIC ACID (UNII: QTT17582CB) 5.5 mg in 0.4 mL EDETATE DISODIUM (UNII: 7FLD91C86K) 0.007 mg in 0.4 mL POLYSORBATE 80 (UNII: 6OZP39ZG8H) 0.080 mg in 0.4 mL SODIUM ACETATE (UNII: 4550K0SC9B) 2.722 mg in 0.4 mL SODIUM CHLORIDE (UNII: 451W47IQ8X) 1.192 mg in 0.4 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0078-1007-68 1 in 1 CARTON 08/20/2020 1 0.4 mL in 1 SYRINGE, GLASS; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) 2 NDC: 0078-1007-98 1 in 1 CARTON 08/20/2020 2 0.4 mL in 1 SYRINGE, GLASS; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125326 10/26/2009 Labeler - Novartis Pharmaceuticals Corporation (002147023)
Trademark Results [KESIMPTA]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 KESIMPTA 79227649 5537963 Live/Registered |
Novartis AG 2018-01-15 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.