SPRIX- ketorolac tromethamine spray, metered
Sprix by
Drug Labeling and Warnings
Sprix by is a Prescription medication manufactured, distributed, or labeled by Zyla Life Sciences US LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use SPRIX® safely and effectively. See full prescribing information for SPRIX®.
SPRIX® (ketorolac tromethamine) Nasal Spray
Initial U.S. Approval: 1989WARNING: RISK OF SERIOUS CARDIOVASCULAR AND GASTROINTESTINAL EVENTS
See full prescribing information for complete boxed warning.- Nonsteroidal anti-inflammatory drugs (NSAIDS) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use (5.1)
- SPRIX® is contraindicated in the setting of coronary artery bypass graft (CABG) surgery (4, 5.1)
- NSAIDS cause an increased risk of serious gastrointestinal (GI) adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients and patients with a prior history of peptic ulcer disease and/or GI bleeding are at greater risk for serious GI events (5.2)
RECENT MAJOR CHANGES
Indications and Usage (1) 01/2018 INDICATIONS AND USAGE
SPRIX is a nonsteroidal anti-inflammatory drug indicated in adult patients for the short term (up to 5 days) management of moderate to moderately severe pain that requires analgesia at the opioid level. (1)
DOSAGE AND ADMINISTRATION
- Use the lowest effective dosage for shortest duration consistent with individual patient treatment goals. (2.1)
- SPRIX is not an inhaled product. For adult patients < 65 years of age: 31.5 mg (one 15.75 mg spray in each nostril) every 6 to 8 hours. The maximum daily dose is 126 mg. (2.2, 2.3)
- For patients ≥ 65 years of age, renally impaired patients, and patients less than 50 kg (110 lbs): 15.75 mg (one 15.75 mg spray in only one nostril) every 6 to 8 hours. The maximum daily dose is 63 mg. (2.4)
- SPRIX nasal spray should be discarded within 24 hours of taking the first dose, even if the bottle still contains some medication. (2.5)
DOSAGE FORMS AND STRENGTHS
SPRIX (ketorolac tromethamine) Nasal Spray: 15.75 mg of ketorolac tromethamine in each 100 μL spray. Each 1.7 g bottle contains 8 sprays. (3)
CONTRAINDICATIONS
- Known hypersensitivity to ketorolac or any components of the drug product (4)
- History of asthma, urticaria, or other allergic-type reactions after taking aspirin or other NSAIDs (4)
- In the setting of CABG surgery (4)
- Use in patients with active peptic ulcer disease or with recent GI bleeding or perforation (4)
- Use as a prophylactic analgesic before any major surgery (4)
- Use in patients with advanced renal disease or patients at risk for renal failure due to volume depletion (4)
- Use in patients with suspected or confirmed cerebrovascular bleeding, patients with hemorrhagic diathesis, incomplete hemostasis, and those at high risk of bleeding (4)
- Use in labor and delivery (4)
WARNINGS AND PRECAUTIONS
- Hepatotoxicity: Inform patients of warning signs and symptoms of hepatotoxicity. Discontinue if abnormal liver tests persist or worsen or if clinical signs and symptoms of liver disease develop. (5.3)
- Hypertension: Patients taking some antihypertensive medications may have impaired response to these therapies when taking NSAIDs. Monitor blood pressure. (5.4, 7)
- Heart Failure and Edema: Avoid use of SPRIX in patients with severe heart failure unless benefits are expected to outweigh risk of worsening heart failure. (5.5)
- Renal Toxicity: Monitor renal function in patients with renal or hepatic impairment, heart failure, dehydration, or hypovolemia. Avoid use of SPRIX in patients with advanced renal disease unless benefits are expected to outweigh risk of worsening renal function. (5.6)
- Anaphylactic Reactions: Seek emergency help if an anaphylactic reaction occurs. (5.7)
- Exacerbation of Asthma Related to Aspirin Sensitivity: SPRIX is contraindicated in patients with aspirin-sensitive asthma. Monitor patients with preexisting asthma (without aspirin sensitivity). (5.8)
- Serious Skin Reactions: Discontinue SPRIX at first appearance of skin rash or other signs of hypersensitivity. (5.9)
- Premature Closure of Fetal Ductus Arteriosus: Avoid use in pregnant women starting at 30 weeks gestation. (5.10, 8.1)
- Hematologic Toxicity: Monitor hemoglobin or hematocrit in patients with any signs or symptoms of anemia. Do not use SPRIX in patients for whom hemostasis is critical. (5.11, 7)
- Limitations of Use: SPRIX should not be used concomitantly with IM/IV or oral ketorolac, aspirin, or other NSAIDs. (5.15)
ADVERSE REACTIONS
Most common adverse reactions (incidence ≥2%) in patients treated with SPRIX and occurring at a rate at least twice that of placebo are nasal discomfort, rhinalgia, increased lacrimation, throat irritation, oliguria, rash, bradycardia, decreased urine output, increased ALT and/or AST, hypertension, and rhinitis. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Zyla Life Sciences US Inc. at 1-800-518-1084 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- Drugs that Interfere with Hemostasis (e.g. warfarin, aspirin, SSRIs/SNRIs): Monitor patients for bleeding who are concomitantly taking SPRIX with drugs that interfere with hemostasis. Concomitant use of SPRIX and analgesic doses of aspirin is not generally recommended. (7)
- ACE inhibitors, Angiotensin Receptor Blockers (ARB), or Beta-Blockers: Concomitant use with SPRIX may diminish the antihypertensive effect of these drugs. Monitor blood pressure. (7)
- ACE Inhibitors and ARBs: Concomitant use with SPRIX in elderly, volume depleted, or those with renal impairment may result in deterioration of renal function. In such high risk patients, monitor for signs of worsening renal function. (7)
- Diuretics: NSAIDs can reduce natriuretic effect of furosemide and thiazide diuretics. Monitor patients to assure diuretic efficacy including antihypertensive effects. (7)
- Digoxin: Concomitant use with SPRIX can increase serum concentration and prolong half-life of digoxin. Monitor serum digoxin levels. (7)
USE IN SPECIFIC POPULATIONS
Pregnancy: Use of NSAIDs during the third trimester of pregnancy increases the risk of premature closure of the fetal ductus arteriosus. Avoid use of NSAIDs in pregnant women starting at 30 weeks gestation. (5.10, 8.1)
Infertility: NSAIDs are associated with reversible infertility. Consider withdrawal of SPRIX in women who have difficulties conceiving. (8.3)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 9/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: RISK OF SERIOUS CARDIOVASCULAR AND GASTROINTESTINAL EVENTS
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 General Dosing Instructions
2.2 Administration
2.3 Adult Patients < 65 Years of Age
2.4 Reduced Doses for Special Populations
2.5 Discard Used SPRIX Bottle after 24 Hours
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Cardiovascular Thrombotic Events
5.2 Gastrointestinal Bleeding, Ulceration, and Perforation
5.3 Hepatotoxicity
5.4 Hypertension
5.5 Heart Failure and Edema
5.6 Renal Toxicity and Hyperkalemia
5.7 Anaphylactic Reactions
5.8 Exacerbation of Asthma Related to Aspirin Sensitivity
5.9 Serious Skin Reactions
5.10 Premature Closure of Fetal Ductus Arteriosus
5.11 Hematologic Toxicity
5.12 Masking of Inflammation and Fever
5.13 Laboratory Monitoring
5.14 Eye Exposure
5.15 Limitations of Use
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Postoperative Pain
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: RISK OF SERIOUS CARDIOVASCULAR AND GASTROINTESTINAL EVENTS
Cardiovascular Thrombotic Events
- Nonsteroidal anti-inflammatory drugs (NSAIDS) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use [see Warnings and Precautions (5.1)].
- SPRIX® is contraindicated in the setting of coronary artery bypass graft (CABG) surgery [see Contraindications (4) and Warnings and Precautions (5.1)].
Gastrointestinal Bleeding, Ulceration, and Perforation
- NSAIDS cause an increased risk of serious gastrointestinal (GI) adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients and patients with a prior history of peptic ulcer disease and/or GI bleeding are at greater risk for serious GI events [see Warnings and Precautions (5.2)].
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 General Dosing Instructions
Use the lowest effective dosage for the shortest duration consistent with individual patient treatment goals [see Warnings and Precautions (5)].
The total duration of use of SPRIX alone or sequentially with other formulations of ketorolac (IM/IV or oral) must not exceed 5 days because of the potential for increasing the frequency and severity of adverse reactions associated with the recommended doses [see Warnings and Precautions (5.15)].
Do not use SPRIX concomitantly with other formulations of ketorolac or other NSAIDs [see Warnings and Precautions (5.15)].
2.2 Administration
SPRIX is not an inhaled product. Do not inhale when administering this product.
Instruct patients to administer as follows:
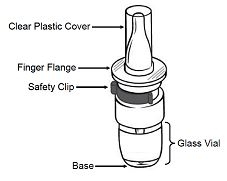
1. First hold the finger flange with fingers, and remove the clear plastic cover with opposite hand; then remove the blue plastic safety clip. Keep the clear plastic cover; and throw away the blue plastic safety clip.
2. Before using the bottle for the FIRST time, activate the pump. To activate the pump, hold the bottle at arm’s length away from the body with index finger and middle finger resting on the top of the finger flange and thumb supporting the base.
Press down evenly and release the pump 5 times. Patient may not see a spray the first few times he/she presses down.
The bottle is now ready to use. There is no need to activate the pump again if more doses are used from the bottle.
3. It’s important to get the medication to the correct place in the nose so it will be most effective.
- Blow nose gently to clear nostrils.
- Sit up straight or stand. Tilt head slightly forward.
- Insert the tip of the container into your right nostril.
- Point the container away from the center of your nose.
- Hold your breath and spray once into your right nostril, pressing down evenly on both sides.
- Immediately after administration, resume breathing through mouth to reduce expelling the product. Also pinch the nose to help retain the spray if it starts to drip.If only one spray per dose is prescribed, administration is complete; skip to Step 5 below.
4. If a dose of 2 sprays is prescribed, repeat the process in Step 3 for the left nostril. Again, be sure to point the spray away from the center of nose. Spray once into the left nostril.
5. Replace the clear plastic cover and place the bottle in a cool, dry location out of direct sunlight, such as inside a medication cabinet. Keep out of reach of children.
2.3 Adult Patients < 65 Years of Age
The recommended dose is 31.5 mg SPRIX (one 15.75 mg spray in each nostril) every 6 to 8 hours. The maximum daily dose is 126 mg (four doses).
2.4 Reduced Doses for Special Populations
For patients ≥ 65 years of age, renally impaired patients, and adult patients less than 50 kg (110 lbs), the recommended dose is 15.75 mg SPRIX (one 15.75 mg spray in only one nostril) every 6 to 8 hours. The maximum daily dose is 63 mg (four doses) [see Warnings and Precautions (5.2, 5.6)].
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
SPRIX is contraindicated in the following patients:
- Known hypersensitivity (e.g., anaphylactic reactions and serious skin reactions) to ketorolac or any components of the drug product [see Warning and Precautions (5.7, 5.9)]
- History of asthma, urticaria, or other allergic-type reactions after taking aspirin or other NSAIDs. Severe, sometimes fatal, anaphylactic reactions to NSAIDs have been reported in such patients [see Warnings and Precautions (5.7, 5.8)]
- In the setting of coronary artery bypass graft (CABG) surgery [see Warnings and Precautions (5.1)]
- Use in patients with active peptic ulcer disease and in patients with recent gastrointestinal bleeding or perforation [see Warnings and Precautions (5.2)]
- Use as a prophylactic analgesic before any major surgery [see Warnings and Precautions (5.11)]
- Use in patients with advanced renal disease or patients at risk for renal failure due to volume depletion [see Warnings and Precautions (5.6)]
- Use in labor and delivery. Through its prostaglandin synthesis inhibitory effect, ketorolac may adversely affect fetal circulation and inhibit uterine contractions, thus increasing the risk of uterine hemorrhage [see Use in Specific Populations (8.1)]
- Use in patients with suspected or confirmed cerebrovascular bleeding, hemorrhagic diathesis, incomplete hemostasis, or those for whom hemostasis is critical [see Warnings and Precautions (5.11), Drug Interactions (7)]
- Concomitant use with probenecid [see Drug Interactions (7)]
- Concomitant use with pentoxifylline [see Drug Interactions (7)]
-
5 WARNINGS AND PRECAUTIONS
5.1 Cardiovascular Thrombotic Events
Clinical trials of several COX-2 selective and nonselective NSAIDs of up to three years duration have shown an increased risk of serious cardiovascular (CV) thrombotic events, including myocardial infarction (MI) and stroke, which can be fatal. Based on available data, it is unclear that the risk for CV thrombotic events is similar for all NSAIDs. The relative increase in serious CV thrombotic events over baseline conferred by NSAID use appears to be similar in those with and without known CV disease or risk factors for CV disease. However, patients with known CV disease or risk factors had a higher absolute incidence of excess serious CV thrombotic events, due to their increased baseline rate. Some observational studies found that this increased risk of serious CV thrombotic events began as early as the first weeks of treatment. The increase in CV thrombotic risk has been observed most consistently at higher doses.
To minimize the potential risk for an adverse CV event in NSAID-treated patients, use the lowest effective dose for the shortest duration possible. Physicians and patients should remain alert for the development of such events, throughout the entire treatment course, even in the absence of previous CV symptoms. Patients should be informed about the symptoms of serious CV events and the steps to take if they occur.
There is no consistent evidence that concurrent use of aspirin mitigates the increased risk of serious CV thrombotic events associated with NSAID use. The concurrent use of aspirin and an NSAID, such as ketorolac, increases the risk of serious gastrointestinal (GI) events [see Warnings and Precautions (5.2)].
Status Post Coronary Artery Bypass Graft (CABG) Surgery
Two large, controlled clinical trials of a COX-2 selective NSAID for the treatment of pain in the first 10–14 days following CABG surgery found an increased incidence of myocardial infarction and stroke. NSAIDs are contraindicated in the setting of CABG [see Contraindications (4)].
Post-MI Patients
Observational studies conducted in the Danish National Registry have demonstrated that patients treated with NSAIDs in the post-MI period were at increased risk of reinfarction, CV-related death, and all-cause mortality beginning in the first week of treatment. In this same cohort, the incidence of death in the first year post-MI was 20 per 100 person years in NSAID-treated patients compared to 12 per 100 person years in non-NSAID exposed patients. Although the absolute rate of death declined somewhat after the first year post-MI, the increased relative risk of death in NSAID users persisted over at least the next four years of follow-up.
Avoid the use of SPRIX in patients with a recent MI unless the benefits are expected to outweigh the risk of recurrent CV thrombotic events. If SPRIX is used in patients with a recent MI, monitor patients for signs of cardiac ischemia.
5.2 Gastrointestinal Bleeding, Ulceration, and Perforation
SPRIX is contraindicated in patients with active peptic ulcers and/or GI bleeding and in patients with recent gastrointestinal bleeding or perforation [see Contraindications (4)].
NSAIDs, including ketorolac, cause serious gastrointestinal (GI) adverse events including inflammation, bleeding, ulceration, and perforation of the esophagus, stomach, small intestine, or large intestine, which can be fatal. These serious adverse events can occur at any time, with or without warning symptoms, in patients treated with NSAIDs. Only one in five patients who develop a serious upper GI adverse event on NSAID therapy is symptomatic. Upper GI ulcers, gross bleeding, or perforation caused by NSAIDs occurred in approximately 1% of patients treated for 3-6 months, and in about 2%-4% of patients treated for one year. However, even short-term NSAID therapy is not without risk.
Risk Factors for GI Bleeding, Ulceration, and Perforation
Patients with a prior history of peptic ulcer disease and/or GI bleeding who used NSAIDs had a greater than 10-fold increased risk for developing a GI bleed compared to patients without these risk factors. Other factors that increase the risk of GI bleeding in patients treated with NSAIDs include longer duration of NSAID therapy; concomitant use of oral corticosteroids, aspirin, anticoagulants, or selective serotonin reuptake inhibitors (SSRIs); smoking; use of alcohol; older age; and poor general health status. Most postmarketing reports of fatal GI events occurred in elderly or debilitated patients. Additionally, patients with advanced liver disease and/or coagulopathy are at increased risk for GI bleeding.
Strategies to Minimize the GI Risks in NSAID-treated patients:
- Use the lowest effective dosage for the shortest possible duration.
- Avoid administration of more than one NSAID at a time.
- Avoid use in patients at higher risk unless benefits are expected to outweigh the increased risk of bleeding. For such patients, consider alternate therapies other than NSAIDs. Do not use Sprix in those with active GI bleeding.
- Remain alert for signs and symptoms of GI ulceration and bleeding during NSAID therapy.
- If a serious GI adverse event is suspected, promptly initiate evaluation and treatment, and discontinue SPRIX until a serious GI adverse event is ruled out.
- In the setting of concomitant use of low-dose aspirin for cardiac prophylaxis, monitor patients more closely for evidence of GI bleeding [see Drug Interactions (7)].
- Use great care when giving SPRIX to patients with a history of inflammatory bowel disease (ulcerative colitis, Crohn’s disease) as their condition may be exacerbated.
5.3 Hepatotoxicity
Elevations of ALT or AST (three or more times the upper limit of normal [ULN]) have been reported in approximately 1% of NSAID-treated patients in clinical trials. In addition, rare, sometimes fatal, cases of severe hepatic injury, including fulminant hepatitis, liver necrosis, and hepatic failure have been reported.
Elevations of ALT or AST (less than three times ULN) may occur in up to 15% of patients treated with NSAIDs including ketorolac.
Inform patients of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, diarrhea, pruritus, jaundice, right upper quadrant tenderness, and "flu-like" symptoms). If clinical signs and symptoms consistent with liver disease develop, or if systemic manifestations occur (e.g., eosinophilia, rash, etc.), discontinue SPRIX immediately, and perform a clinical evaluation of the patient.
5.4 Hypertension
NSAIDs, including SPRIX, can lead to new onset of hypertension or worsening of preexisting hypertension, either of which may contribute to the increased incidence of CV events. Patients taking angiotensin converting enzyme (ACE) inhibitors, thiazide diuretics, or loop diuretics may have impaired response to these therapies when taking NSAIDs [see Drug Interactions (7)].
Monitor blood pressure (BP) during the initiation of NSAID treatment and throughout the course of therapy.
5.5 Heart Failure and Edema
The Coxib and traditional NSAID Trialists’ Collaboration meta-analysis of randomized controlled trials demonstrated an approximately two-fold increase in hospitalizations for heart failure in COX-2 selective-treated patients and nonselective NSAID-treated patients compared to placebo-treated patients. In a Danish National Registry study of patients with heart failure, NSAID use increased the risk of MI, hospitalization for heart failure, and death.
Additionally, fluid retention and edema have been observed in some patients treated with NSAIDs. Use of ketorolac may blunt the CV effects of several therapeutic agents used to treat these medical conditions (e.g., diuretics, ACE inhibitors, or angiotensin receptor blockers [ARBs]) [see Drug Interactions (7)].
Avoid the use of SPRIX in patients with severe heart failure unless the benefits are expected to outweigh the risk of worsening heart failure. If SPRIX is used in patients with severe heart failure, monitor patients for signs of worsening heart failure.
5.6 Renal Toxicity and Hyperkalemia
Ketorolac and its metabolites are eliminated primarily by the kidneys. Patients with reduced creatinine clearance will have diminished clearance of the drug [see Clinical Pharmacology (12.3)]. SPRIX is contraindicated in patients with advanced renal impairment [see Contraindications (4)].
Renal Toxicity
Long-term administration of NSAIDs has resulted in renal papillary necrosis and other renal injury. Renal toxicity has also been seen in patients in whom renal prostaglandins have a compensatory role in the maintenance of renal perfusion. In these patients, administration of an NSAID may cause a dose-dependent reduction in prostaglandin formation and, secondarily, in renal blood flow, which may precipitate overt renal decompensation. Patients at greatest risk of this reaction are those with impaired renal function, dehydration, hypovolemia, heart failure, liver dysfunction, those taking diuretics and ACE inhibitors or ARBs, and the elderly. Discontinuation of NSAID therapy is usually followed by recovery to the pretreatment state.
No information is available from controlled clinical studies regarding the use of SPRIX in patients with advanced renal disease. The renal effects of SPRIX may hasten the progression of renal dysfunction in patients with preexisting renal disease.
Correct volume status in dehydrated or hypovolemic patients prior to initiating SPRIX. Monitor renal function in patients with renal or hepatic impairment, heart failure, dehydration, or hypovolemia during use of SPRIX [see Drug Interactions (7)]. Avoid the use of SPRIX in patients with advanced renal disease unless the benefits are expected to outweigh the risk of worsening renal function. If SPRIX is used in patients with advanced renal disease, monitor patients for signs of worsening renal function.
Hyperkalemia
Increases in serum potassium concentration, including hyperkalemia, have been reported with use of NSAIDs, even in some patients without renal impairment. In patients with normal renal function, these effects have been attributed to a hyporeninemic-hypoaldosteronism state.
5.7 Anaphylactic Reactions
Ketorolac has been associated with anaphylactic reactions in patients with and without known hypersensitivity to ketorolac and in patients with aspirin-sensitive asthma [see Contraindications (4) and Warnings and Precautions (5.8)].
Seek emergency help if an anaphylactic reaction occurs.
5.8 Exacerbation of Asthma Related to Aspirin Sensitivity
A subpopulation of patients with asthma may have aspirin-sensitive asthma which may include chronic rhinosinusitis complicated by nasal polyps; severe, potentially fatal bronchospasm; and/or intolerance to aspirin and other NSAIDs. Because cross-reactivity between aspirin and other NSAIDs has been reported in such aspirin-sensitive patients, SPRIX is contraindicated in patients with this form of aspirin sensitivity [see Contraindications (4)]. When SPRIX is used in patients with preexisting asthma (without known aspirin sensitivity), monitor patients for changes in the signs and symptoms of asthma.
5.9 Serious Skin Reactions
NSAIDs, including ketorolac, can cause serious skin adverse reactions such as exfoliative dermatitis, Stevens-Johnson Syndrome (SJS), and toxic epidermal necrolysis (TEN), which can be fatal. These serious events may occur without warning. Inform patients about the signs and symptoms of serious skin reactions, and to discontinue the use of SPRIX at the first appearance of skin rash or any other sign of hypersensitivity. SPRIX is contraindicated in patients with previous serious skin reactions to NSAIDs [see Contraindications (4)].
5.10 Premature Closure of Fetal Ductus Arteriosus
Ketorolac may cause premature closure of the fetal ductus arteriosus. Avoid use of NSAIDs, including SPRIX, in pregnant women starting at 30 weeks of gestation (third trimester) [see Use in Specific Populations (8.1)].
5.11 Hematologic Toxicity
Anemia has occurred in NSAID-treated patients. This may be due to occult or gross blood loss, fluid retention, or an incompletely described effect upon erythropoiesis. If a patient treated with SPRIX has any signs or symptoms of anemia, monitor hemoglobin or hematocrit. Do not use SPRIX in patients for whom hemostasis is critical [see Contraindications (4), Drug Interactions (7)].
NSAIDs, including SPRIX, may increase the risk of bleeding events. Co-morbid conditions such as coagulation disorders or concomitant use of warfarin, other anticoagulants, antiplatelet agents (e.g., aspirin), serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs) may increase this risk. Monitor these patients for signs of bleeding [see Drug Interactions (7)].
The concurrent use of ketorolac and therapy that affects hemostasis, including prophylactic low dose heparin (2500 to 5000 units q12h), warfarin and dextrans, has not been studied extensively, but may also be associated with an increased risk of bleeding. Until data from such studies are available, carefully weigh the benefits against the risks and use such concomitant therapy in these patients only with extreme caution. Monitor patients receiving therapy that affects hemostasis closely.
In clinical trials, serious adverse events related to bleeding were more common in patients treated with SPRIX than placebo. In clinical trials and in postmarketing experience with ketorolac IV and IM dosing, postoperative hematomas and other signs of wound bleeding have been reported in association with peri-operative use. Therefore, use SPRIX with caution in the postoperative setting when hemostasis is critical.
5.12 Masking of Inflammation and Fever
The pharmacological activity of SPRIX in reducing inflammation, and possibly fever, may diminish the utility of diagnostic signs in detecting infections.
5.13 Laboratory Monitoring
Because serious GI bleeding, hepatotoxicity, and renal injury can occur without warning symptoms or signs, consider monitoring patients on long-term NSAID treatment with a CBC and a chemistry profile periodically [see Warnings and Precautions (5.2, 5.3, 5.6)].
5.14 Eye Exposure
Avoid contact of SPRIX with the eyes. If eye contact occurs, wash out the eye with water or saline, and consult a physician if irritation persists for more than an hour.
5.15 Limitations of Use
The total duration of use of SPRIX alone or sequentially with other forms of ketorolac is not to exceed 5 days. SPRIX must not be used concomitantly with other forms of ketorolac or other NSAIDs [see Dosage and Administration (2.1)].
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed in greater detail in other sections of the labeling:
- Cardiovascular Thrombotic Events [see Warnings and Precautions (5.1)]
- GI Bleeding, Ulceration and Perforation [see Warnings and Precautions (5.2)]
- Hepatotoxicity [see Warnings and Precautions (5.3)]
- Hypertension [see Warnings and Precautions (5.4)]
- Heart Failure and Edema [see Warnings and Precautions (5.5)]
- Renal Toxicity and Hyperkalemia [see Warnings and Precautions (5.6)]
- Anaphylactic Reactions [see Warnings and Precautions (5.7)]
- Serious Skin Reactions [see Warnings and Precautions (5.9)]
- Hematologic Toxicity [see Warnings and Precautions (5.11)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The data described below reflect exposure to SPRIX in patients enrolled in placebo-controlled efficacy studies of acute pain following major surgery. The studies enrolled 828 patients (183 men, 645 women) ranging from 18 years to over 75 years of age.
The patients in the postoperative pain studies had undergone major abdominal, orthopedic, gynecologic, or other surgery; 455 patients received SPRIX (31.5 mg) three or four times a day for up to 5 days, and 245 patients received placebo. Most patients were receiving concomitant opioids, primarily PCA morphine.
The most frequently reported adverse reactions were related to local symptoms, i.e., nasal discomfort or irritation. These reactions were generally mild and transient in nature.
The most common drug-related adverse events leading to premature discontinuation were nasal discomfort or nasal pain (rhinalgia).
Table 1: Post-Operative Patients with Adverse Reactions Observed at a Rate of 2% or More and at Least Twice the Incidence of the Placebo Group. SPRIX
(N = 455)Placebo
(N = 245)Nasal discomfort 15% 2% Rhinalgia 13% <1% Lacrimation increased 5% 0% Throat irritation 4% <1% Oliguria 3% 1% Rash 3% <1% Bradycardia 2% <1% Urine output decreased 2% <1% ALT and/or AST increased 2% 1% Hypertension 2% 1% Rhinitis 2% <1% In controlled clinical trials in major surgery, primarily knee and hip replacements and abdominal hysterectomies, seven patients (N=455, 1.5%) treated with SPRIX experienced serious adverse events of bleeding (4 patients) or hematoma (3 patients) at the operative site versus one patient (N=245, 0.4%) treated with placebo (hematoma). Six of the seven patients treated with SPRIX underwent a surgical procedure and/or blood transfusion and the placebo patient subsequently required a blood transfusion.
Adverse Reactions Reported in Clinical Trials with Other Dosage Forms of Ketorolac or Other NSAIDs
Adverse reaction rates increase with higher doses of ketorolac. It is necessary to remain alert for the severe complications of treatment with ketorolac, such as GI ulceration, bleeding, and perforation, postoperative bleeding, acute renal failure, anaphylactic and anaphylactoid reactions, and liver failure. These complications can be serious in certain patients for whom ketorolac is indicated, especially when the drug is used inappropriately.
In patients taking ketorolac or other NSAIDs in clinical trials, the most frequently reported adverse experiences in approximately 1% to 10% of patients are:
*Incidence greater than 10% Gastrointestinal (GI) experiences including: abdominal pain
flatulence
gross bleeding/perforation
stomatitisconstipation/diarrhea
GI fullness
heartburn
vomitingdyspepsia
GI ulcers (gastric/duodenal)
nausea*Other experiences: abnormal renal function
drowsiness
headache*
injection site pain
rashanemia
edema
hypertension
pruritus
tinnitusdizziness
elevated liver enzymes
increased bleeding time
purpura
sweatingAdditional adverse experiences reported occasionally (<1% in patients taking ketorolac or other NSAIDs in clinical trials) include:
Body as a Whole: fever, infection, sepsis
Cardiovascular System: congestive heart failure, palpitation, pallor, tachycardia, syncope
Digestive System: anorexia, dry mouth, eructation, esophagitis, excessive thirst, gastritis, glossitis, hematemesis, hepatitis, increased appetite, jaundice, melena, rectal bleeding
Hemic and Lymphatic: ecchymosis, eosinophilia, epistaxis, leukopenia, thrombocytopenia
Metabolic and Nutritional: weight change
Nervous System: abnormal dreams, abnormal thinking, anxiety, asthenia, confusion, depression, euphoria, extrapyramidal symptoms, hallucinations, hyperkinesis, inability to concentrate, insomnia, nervousness, paresthesia, somnolence, stupor, tremors, vertigo, malaise
Respiratory: asthma, dyspnea, pulmonary edema, rhinitis
Special Senses: abnormal taste, abnormal vision, blurred vision, hearing loss
Urogenital: cystitis, dysuria, hematuria, increased urinary frequency, interstitial nephritis, oliguria/polyuria, proteinuria, renal failure, urinary retention
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of ketorolac or other NSAIDs. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Other observed reactions (reported from postmarketing experience in patients taking ketorolac or other NSAIDs) are:
Body as a Whole: angioedema, death, hypersensitivity reactions such as anaphylaxis, anaphylactoid reaction, laryngeal edema, tongue edema, myalgia
Cardiovascular: arrhythmia, bradycardia, chest pain, flushing, hypotension, myocardial infarction, vasculitis
Dermatologic: exfoliative dermatitis, erythema multiforme, Lyell's syndrome, bullous reactions including Stevens-Johnson syndrome and toxic epidermal necrolysis
Gastrointestinal: acute pancreatitis, liver failure, ulcerative stomatitis, exacerbation of inflammatory bowel disease (ulcerative colitis, Crohn’s disease)
Hemic and Lymphatic: agranulocytosis, aplastic anemia, hemolytic anemia, lymphadenopathy, pancytopenia, postoperative wound hemorrhage (rarely requiring blood transfusion)
Metabolic and Nutritional: hyperglycemia, hyperkalemia, hyponatremia
Nervous System: aseptic meningitis, convulsions, coma, psychosis
Respiratory: bronchospasm, respiratory depression, pneumonia
Special Senses: conjunctivitis
Urogenital: flank pain with or without hematuria and/or azotemia, hemolytic uremic syndrome
-
7 DRUG INTERACTIONS
See Table 2 for clinically significant drug interactions with ketorolac.
Table 2: Clinically Significant Drug Interactions with Ketorolac Drugs that Interfere with Hemostasis Clinical Impact: - Ketorolac and anticoagulants such as warfarin have a synergistic effect on bleeding. The concomitant use of ketorolac and anticoagulants have an increased risk of serious bleeding compared to the use of either drug alone [see Clinical Pharmacology (12.3)].
- Serotonin release by platelets plays an important role in hemostasis. Case-control and cohort epidemiological studies showed that concomitant use of drugs that interfere with serotonin reuptake and an NSAID may potentiate the risk of bleeding more than an NSAID alone.
- When ketorolac is administered concurrently with pentoxifylline, there is an increased risk of bleeding.
Intervention: Monitor patients with concomitant use of SPRIX with anticoagulants (e.g., warfarin), antiplatelet agents (e.g., aspirin), selective serotonin reuptake inhibitors (SSRIs), and serotonin norepinephrine reuptake inhibitors (SNRIs) for signs of bleeding [see Warnings and Precautions (5.11)]. Concomitant use of SPRIX and pentoxifylline is contraindicated [see Contraindications (4) and Warnings and Precautions (5.11)]. Aspirin Clinical Impact: Controlled clinical studies showed that the concomitant use of NSAIDs and analgesic doses of aspirin does not produce any greater therapeutic effect than the use of NSAIDs alone. In a clinical study, the concomitant use of an NSAID and aspirin was associated with a significantly increased incidence of GI adverse reactions as compared to use of the NSAID alone [see Warnings and Precautions (5.2)]. Intervention: Concomitant use of SPRIX and analgesic doses of aspirin is not generally recommended because of the increased risk of bleeding [see Warnings and Precautions (5.11)]. SPRIX is not a substitute for low dose aspirin for cardiovascular protection. ACE Inhibitors, Angiotensin Receptor Blockers, and Beta-blockers Clinical Impact: - NSAIDs may diminish the antihypertensive effect of angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), or beta-blockers (including propranolol).
- In patients who are elderly, volume-depleted (including those on diuretic therapy), or have renal impairment, co-administration of an NSAID with ACE inhibitors or ARBs may result in deterioration of renal function, including possible acute renal failure. These effects are usually reversible.
Intervention: - During concomitant use of SPRIX and ACE-inhibitors, ARBs, or beta-blockers, monitor blood pressure to ensure that the desired blood pressure is obtained.
- During concomitant use of SPRIX and ACE-inhibitors or ARBs in patients who are elderly, volume-depleted, or have impaired renal function, monitor for signs of worsening renal function [see Warnings and Precautions (5.6)].
- When these drugs are administered concomitantly, patients should be adequately hydrated. Assess renal function at the beginning of the concomitant treatment and periodically thereafter.
Diuretics Clinical Impact: Clinical studies, as well as post-marketing observations, showed that NSAIDs reduced the natriuretic effect of loop diuretics (e.g., furosemide) and thiazide diuretics in some patients. This effect has been attributed to the NSAID inhibition of renal prostaglandin synthesis Intervention: During concomitant use of SPRIX with diuretics, observe patients for signs of worsening renal function, in addition to assuring diuretic efficacy including antihypertensive effects [see Warnings and Precautions (5.6)]. Digoxin Clinical Impact: The concomitant use of ketorolac with digoxin has been reported to increase the serum concentration and prolong the half-life of digoxin. Intervention: During concomitant use of SPRIX and digoxin, monitor serum digoxin levels. Lithium Clinical Impact: NSAIDs have produced elevations in plasma lithium levels and reductions in renal lithium clearance. The mean minimum lithium concentration increased 15%, and the renal clearance decreased by approximately 20%. This effect has been attributed to NSAID inhibition of renal prostaglandin synthesis. Intervention: During concomitant use of SPRIX and lithium, monitor patients for signs of lithium toxicity. Methotrexate Clinical Impact: Concomitant use of NSAIDs and methotrexate may increase the risk for methotrexate toxicity (e.g., neutropenia, thrombocytopenia, renal dysfunction). Intervention: During concomitant use of SPRIX and methotrexate, monitor patients for methotrexate toxicity. Cyclosporine Clinical Impact: Concomitant use of SPRIX and cyclosporine may increase cyclosporine’s nephrotoxicity. Intervention: During concomitant use of SPRIX and cyclosporine, monitor patients for signs of worsening renal function. NSAIDs and Salicylates Clinical Impact: Concomitant use of ketorolac with other NSAIDs or salicylates (e.g., diflunisal, salsalate) increases the risk of GI toxicity, with little or no increase in efficacy [see Warnings and Precautions (5.2) and Clinical Pharmacology (12.3)]. Intervention: The concomitant use of ketorolac with other NSAIDs or salicylates is not recommended. Pemetrexed Clinical Impact: Concomitant use of SPRIX and pemetrexed may increase the risk of pemetrexed-associated myelosuppression, renal, and GI toxicity (see the pemetrexed prescribing information). Intervention: During concomitant use of SPRIX and pemetrexed, in patients with renal impairment whose creatinine clearance ranges from 45 to 79 mL/min, monitor for myelosuppression, renal and GI toxicity.
NSAIDs with short elimination half-lives (e.g., diclofenac, indomethacin) should be avoided for a period of two days before, the day of, and two days following administration of pemetrexed.
In the absence of data regarding potential interaction between pemetrexed and NSAIDs with longer half-lives (e.g., meloxicam, nabumetone), patients taking these NSAIDs should interrupt dosing for at least five days before, the day of, and two days following pemetrexed administration.
Probenecid Clinical Impact: Concomitant administration of oral ketorolac and probenecid results in increased half-life and systemic exposure. [see Clinical Pharmacology (12.3)]. Intervention: Concomitant use of SPRIX and probenecid is contraindicated. Antiepileptic Drugs Clinical Impact: Sporadic cases of seizures have been reported during concomitant use of ketorolac and antiepileptic drugs (phenytoin, carbamazepine). Intervention: During concomitant use of SPRIX and antiepileptic drugs, monitor patients for seizures. Psychoactive Drugs Clinical Impact: Hallucinations have been reported when ketorolac was used in patients taking psychoactive drugs (fluoxetine, thiothixene, alprazolam). Intervention: During concomitant use of SPRIX and psychoactive drugs, monitor patients for hallucinations. Nondepolarizing Muscle Relaxants Clinical Impact: In postmarketing experience there have been reports of a possible interaction between ketorolac and nondepolarizing muscle relaxants that resulted in apnea. The concurrent use of ketorolac with muscle relaxants has not been formally studied. Intervention: During concomitant use of SPRIX and nondepolarizing muscle relaxants, monitor patients for apnea. -
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C prior to 30 weeks gestation; Category D starting at 30 weeks gestation.
Risk Summary
Use of NSAIDs, including SPRIX, during the third trimester of pregnancy increases the risk of premature closure of the fetal ductus arteriosus. Avoid use of NSAIDs, including SPRIX, in pregnant women starting at 30 weeks of gestation (third trimester).
There are no adequate and well-controlled studies of SPRIX in pregnant women. Data from observational studies regarding potential embryofetal risks of NSAID use in women in the first or second trimesters of pregnancy are inconclusive. In the general U.S. population, all clinically recognized pregnancies, regardless of drug exposure, have a background rate of 2-4% for major malformations, and 15-20% for pregnancy loss. In animal reproduction studies in rabbits and rats tested at 0.6 and 1.5 times the human systemic exposure, respectively, at the recommended maximum IN dose of 31.5 mg four times a day, there was no evidence of teratogenicity or other adverse developmental outcomes (see Data). Based on animal data, prostaglandins have been shown to have an important role in endometrial vascular permeability, blastocyst implantation, and decidualization. In animal studies, administration of prostaglandin synthesis inhibitors such as ketorolac, resulted in increased pre- and post-implantation loss.
Clinical Considerations
Labor or Delivery
There are no studies on the effects of SPRIX during labor or delivery. In animal studies, NSAIDs, including ketorolac, inhibit prostaglandin synthesis, cause delayed parturition, and increase the incidence of stillbirth.
Data
Human Data
There are no adequate and well-controlled studies of SPRIX in pregnant women.
Animal Data
Reproduction studies have been performed during organogenesis using daily oral doses of ketorolac tromethamine at 3.6 mg/kg (0.6 times the human systemic exposure at the recommended maximum IN dose of 31.5 mg qid, based on area-under-the-plasma-concentration curve [AUC]) in rabbits and at 10 mg/kg (1.5 times the human AUC) in rats. These studies did not reveal evidence of teratogenicity or other adverse developmental outcomes. However, because animal dosing was limited by maternal toxicity, these studies do not adequately assess ketorolac’s potential to cause adverse developmental outcomes in humans.
8.2 Lactation
Risk Summary
Ketorolac is excreted in human milk. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for SPRIX and any potential adverse effects on the breastfed infant from the SPRIX or from the underlying maternal condition.
Clinical Considerations
Exercise caution when administering SPRIX to a nursing woman. Available information has not shown any specific adverse events in nursing infants; however, instruct patients to contact their infant’s health care provider if they note any adverse events.
Data
Limited data from one published study involving ten nursing mothers 2-6 days postpartum showed low levels of ketorolac in breast milk. Levels were undetectable (less than 5 ng/mL) in 4 of the patients. After a single administration of 10 mg ketorolac, the maximum milk concentration observed was 7.3 ng/mL, and the maximum milk to plasma ratio was 0.037. After 1 day of dosing (10 mg every 6 hours), the maximum milk concentration was 7.9 ng/mL, and the maximum milk-to-plasma ratio was 0.025. Assuming a daily intake of 400-1000 mL of human milk per day and a maternal body weight of 60 kg, the calculated maximum daily infant exposure was 0.00263 mg/kg/day, which is 0.4% of the maternal weight adjusted dose.
8.3 Females and Males of Reproductive Potential
Infertility
Females
Based on the mechanism of action, the use of prostaglandin-mediated NSAIDs, including SPRIX, may delay or prevent rupture of ovarian follicles, which has been associated with reversible infertility in some women. Published animal studies have shown that administration of prostaglandin synthesis inhibitors has the potential to disrupt prostaglandin-mediated follicular rupture required for ovulation. Small studies in women treated with NSAIDs have also shown a reversible delay in ovulation. Consider withdrawal of NSAIDs, including SPRIX, in women who have difficulties conceiving or who are undergoing investigation of infertility.
8.4 Pediatric Use
Sprix is not for use in pediatric patients less than 2 years of age. The safety and effectiveness of ketorolac in pediatric patients 17 years of age and younger have not been established.
8.5 Geriatric Use
Exercise caution when treating the elderly (65 years and older) with SPRIX. Elderly patients, compared to younger patients, are at greater risk for NSAID-associated serious cardiovascular, gastrointestinal, and/or renal adverse reactions. If the anticipated benefit for the elderly patient outweighs these potential risks, start dosing at the low end of the dosing range, and monitor patients for adverse effects [see Dosage and Administration (2.4), Warnings and Precautions (5.1, 5.2, 5.3, 5.6, 5.13), Clinical Pharmacology (12.3)]. After observing the response to initial therapy with SPRIX, adjust the dose and frequency to suit an individual patient’s needs.
Ketorolac and its metabolites are known to be substantially excreted by the kidneys, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, use caution in this patient population, and it may be useful to monitor renal function [see Clinical Pharmacology (12.3)].
-
10 OVERDOSAGE
Symptoms following acute NSAID overdosages have been typically limited to lethargy, drowsiness, nausea, vomiting, and epigastric pain, which have been generally reversible with supportive care. Gastrointestinal bleeding has occurred. Hypertension, acute renal failure, respiratory depression, and coma have occurred, but were rare [see Warnings and Precautions (5.1, 5.2, 5.4, 5.6)].
There has been no experience with overdosage of SPRIX. In controlled overdosage studies with IM ketorolac injection, daily doses of 360 mg given for five days (approximately 3 times the maximum daily dose of SPRIX) caused abdominal pain and peptic ulcers, which healed after discontinuation of dosing. Single overdoses of ketorolac tromethamine have been variously associated with abdominal pain, nausea, vomiting, hyperventilation, peptic ulcers and/or erosive gastritis, and renal dysfunction.
Manage patients with symptomatic and supportive care following an NSAID overdosage. There are no specific antidotes. Consider emesis and/or activated charcoal (60 to 100 grams in adults, 1 to 2 grams per kg of body weight in pediatric patients) and/or osmotic cathartic in symptomatic patients seen within four hours of ingestion or in patients with a large overdosage (5 to 10 times the recommended dosage). Forced diuresis, alkalinization of urine, hemodialysis, or hemoperfusion may not be useful due to high protein binding.
For additional information about overdosage treatment contact a poison control center (1-800-222-1222).
-
11 DESCRIPTION
SPRIX (ketorolac tromethamine) Nasal Spray is a member of the pyrrolo-pyrrole group of nonsteroidal anti-inflammatory drugs, available as a clear, colorless to yellow solution packaged in a glass vial with a snap on spray pump that delivers 15.75 mg ketorolac tromethamine per spray and is intended for intranasal administration. The chemical name is (±)-5-benzoyl-2,3-dihydro-1H-pyrrolizine-1-carboxylic acid, compound with 2-amino-2-(hydroxymethyl)-1,3-propanediol (1:1). The molecular weight is 376.41.
Its molecular formula is C19H24N2O6(C15H13NO3C4H11NO3), and it has the following chemical structure.
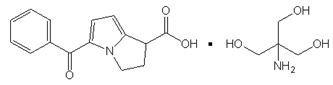
Ketorolac tromethamine is highly water-soluble, allowing its formulation in an aqueous nasal spray product at pH 7.2.
The inactive ingredients in SPRIX include: edetate disodium (EDTA), monobasic potassium phosphate, sodium hydroxide, and water for injection.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Ketorolac has analgesic, anti-inflammatory, and antipyretic properties.
The mechanism of action of SPRIX, like that of other NSAIDs, is not completely understood but involves inhibition of cyclooxygenase (COX-1 and COX-2), an early component of the arachidonic acid cascade, resulting in the reduced synthesis of prostaglandins, thromboxanes, and prostacyclin.
Ketorolac is a potent inhibitor of prostaglandin synthesis in vitro. Ketorolac concentrations reached during therapy have produced in vivo effects. Prostaglandins sensitize afferent nerves and potentiate the action of bradykinin in inducing pain in animal models. Prostaglandins are mediators of inflammation. Because ketorolac is an inhibitor of prostaglandin synthesis, its mode of action may be due to a decrease of prostaglandins in peripheral tissues.
12.3 Pharmacokinetics
The half-lives of ketorolac by the IN and IM routes were similar. The bioavailability of ketorolac by the IN route of administration of a 31.5 mg dose was approximately 60% compared to IM administration. (See Table 3).
Table 3: Pharmacokinetic Parameters of Ketorolac Tromethamine after Intramuscular (IM) and Intranasal (IN) Administration Cmax = maximum plasma concentration; tmax = time of Cmax; AUC0-∞ = complete area under the concentration-time curve; T½ = half-life; SD = standard deviation. All values are means, except tmax, for which medians are reported. Ketorolac Tromethamine Cmax
(SD)
ng/mLtmax
(range)
hoursAUC 0-∞
(SD)
ngh/mLT½
(SD)
hours30 mg IM
(1.0 mL of a 30 mg/mL solution)2382.2
(432.7)0.75
(0.25-1.03)11152.8
(4260.1)4.80
(1.18)31.5 mg IN (SPRIX)
(2 x 100 μL of a 15% w/w solution)1805.8
(882.8)0.75
(0.50-2.00)7477.3
(3654.4)5.24
(1.33)15 mg IM
(0.5 mL of a 30 mg/mL solution)1163.4
(279.9)0.75
(0.25-1.50)5196.3
(2076.7)5.00
(1.72)Absorption
In a study in which SPRIX (31.5 mg) was administered to healthy volunteers four times daily for 5 days, the Cmax, tmax, and AUC values following the final dose were comparable to those obtained in the single-dose study. Accumulation of ketorolac has not been studied in special populations, geriatric, pediatric, renal failure or hepatic disease patients.
Distribution
Scintigraphic assessment of drug disposition of ketorolac following SPRIX intranasal dosing demonstrated that most of the ketorolac was deposited in the nasal cavity and pharynx, with less than 20% deposited in the esophagus and stomach, and zero or negligible deposition in the lungs (<0.5%).
The mean apparent volume (Vβ) of ketorolac tromethamine following complete distribution was approximately 13 liters. This parameter was determined from single-dose data. The ketorolac tromethamine racemate has been shown to be highly protein bound (99.2%). Nevertheless, plasma concentrations as high as 10 mcg/mL will only occupy approximately 5% of the albumin binding sites. Thus, the unbound fraction for each enantiomer will be constant over the therapeutic range. A decrease in serum albumin, however, will result in increased free drug concentrations. Therapeutic concentrations of digoxin, warfarin, ibuprofen, naproxen, piroxicam, acetaminophen, phenytoin, and tolbutamide did not alter ketorolac protein binding. In vitro studies indicate that, at therapeutic concentrations of salicylate (300 mcg/mL), the binding of ketorolac was reduced from approximately 99.2% to 97.5%, representing a potential twofold increase in unbound ketorolac plasma levels.
The in vitro binding of warfarin to plasma proteins is only slightly reduced by ketorolac (99.5% control vs. 99.3%) when ketorolac plasma concentrations reach 5 to 10 mcg/mL.
Ketorolac tromethamine is excreted in human milk.
Elimination
Metabolism
Ketorolac tromethamine is largely metabolized in the liver. The metabolic products are hydroxylated and conjugated forms of the parent drug. The products of metabolism, and some unchanged drug, are excreted in the urine. There is no evidence in animal or human studies that ketorolac induces or inhibits hepatic enzymes capable of metabolizing itself or other drugs.
Excretion
The principal route of elimination of ketorolac and its metabolites is renal. About 92% of a given dose is found in the urine, approximately 40% as metabolites and 60% as unchanged ketorolac. Approximately 6% of a dose is excreted in the feces. A single-dose study with 10 mg ketorolac tromethamine (n = 9) demonstrated that the S-enantiomer is cleared approximately two times faster than the R-enantiomer and that the clearance was independent of the route of administration. This means that the ratio of S/R plasma concentrations decreases with time after each dose. There is little or no inversion of the R- to S- form in humans.
The half-life of the ketorolac tromethamine S-enantiomer was approximately 2.5 hours (SD ± 0.4) compared with 5 hours (SD ± 1.7) for the R-enantiomer. In other studies, the half-life for the racemate has been reported to lie within the range of 5 to 6 hours.
Specific Populations
Geriatric: A single-dose study was conducted to compare the pharmacokinetics of SPRIX (31.5 mg) in subjects ≥ age 65 to the pharmacokinetics in subjects < age 65. Exposure to ketorolac was increased by 23% for the ≥ 65 population as compared to subjects < 65. Peak concentrations of 2028 and 1840 ng/mL were observed for the elderly and nonelderly adult populations, respectively, at 0.75 h after dosing. In the elderly population a longer terminal half-life was observed as compared to the nonelderly adults (4.5 h vs. 3.3 h, respectively).
Race: Pharmacokinetic differences due to race have not been identified.
Hepatic Impairment: There was no significant difference in estimates of half-life, AUC∞ and Cmax in 7 patients with liver disease compared to healthy volunteers.
Renal Impairment: Based on single-dose data only, the mean half-life of ketorolac tromethamine in renally impaired patients is between 6 and 19 hours, and is dependent on the extent of the impairment. There is poor correlation between creatinine clearance and total ketorolac tromethamine clearance in the elderly and populations with renal impairment (r = 0.5).
In patients with renal disease, the AUC∞ of each enantiomer increased by approximately 100% compared with healthy volunteers. The volume of distribution doubles for the S-enantiomer and increases by 1/5th for the R-enantiomer. The increase in volume of distribution of ketorolac tromethamine implies an increase in unbound fraction. The AUC∞-ratio of the ketorolac tromethamine enantiomers in healthy subjects and patients remained similar, indicating there was no selective excretion of either enantiomer in patients compared to healthy subjects.
Allergic Rhinitis: Comparison of the pharmacokinetics of SPRIX in subjects with allergic rhinitis to data from a previous study in healthy subjects showed no differences that would be of clinical consequence for the efficacy or safety of SPRIX.
Drug Interaction Studies
Aspirin: When NSAIDs were administered with aspirin, the protein binding of NSAIDs were reduced, although the clearance of free NSAID was not altered. The clinical significance of this interaction is not known. See Table 2 for clinically significant drug interactions of NSAIDs with aspirin [see Drug Interactions (7)].
Other Nasal Spray Products: A study was conducted in subjects with symptomatic allergic rhinitis to assess the effects of the commonly used nasal spray products oxymetazoline hydrochloride and fluticasone propionate on the pharmacokinetics of SPRIX. Subjects received a single dose of oxymetazoline nasal spray followed by a single dose (31.5 mg) of SPRIX 30 min later. Subjects also received fluticasone nasal spray (200 mcg as 2 x 50 mcg in each nostril) for seven days, with a single dose (31.5 mg) of SPRIX on the 7th day. Administration of these common intranasal products had no effect of clinical significance on the rate or extent of ketorolac absorption.
Probenecid: Concomitant administration of oral ketorolac and probenecid resulted in decreased clearance and volume of distribution of ketorolac and significant increases in ketorolac plasma levels (total AUC increased approximately threefold from 5.4 to 17.8 mcg/h/mL), and terminal half-life increased approximately twofold from 6.6 to 15.1 hours [see Drug Interactions (7)].
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
An 18-month study in mice with oral doses of ketorolac at 2 mg/kg/day (approximately 1.3 times the human systemic exposure at the recommended maximum IN dose of 31.5 mg four times a day, based on area-under-the-plasma-concentration curve [AUC]), and a 24-month study in rats at 5 mg/kg/day (approximately 0.8 times the human AUC) showed no evidence of tumorigenicity.
Mutagenesis
Ketorolac was not mutagenic in the Ames test, unscheduled DNA synthesis and repair, or in forward mutation assays. Ketorolac did not cause chromosome breakage in the in vivo mouse micronucleus assay. At 1590 μg/mL and at higher concentrations, ketorolac increased the incidence of chromosomal aberrations in Chinese hamster ovarian cells.
Impairment of fertility
Impairment of fertility did not occur in male or female rats at oral doses of 9 mg/kg (approximately 1.3 times the human AUC) and 16 mg/kg (approximately 2.4 times the human AUC) of ketorolac, respectively.
-
14 CLINICAL STUDIES
14.1 Postoperative Pain
The effect of SPRIX on acute pain was evaluated in two multi-center, randomized, double-blind, placebo-controlled studies.
In a study of adults who had undergone elective abdominal or orthopedic surgery, 300 patients were randomized and treated with SPRIX or placebo administered every 8 hours and morphine administered via patient controlled analgesia on an as needed basis. Efficacy was demonstrated as a statistically significant greater reduction in the summed pain intensity difference over 48 hours in patients who received SPRIX as compared to those receiving placebo. The clinical relevance of this is reflected in the finding that patients treated with SPRIX required 36% less morphine over 48 hours than patients treated with placebo.
In a study of adults who had undergone elective abdominal surgery, 321 patients were randomized and treated with SPRIX or placebo administered every 6 hours and morphine administered via patient controlled analgesia on an as needed basis. Efficacy was demonstrated as a statistically significant greater reduction in the summed pain intensity difference over 48 hours in patients who received SPRIX as compared to those receiving placebo. The clinical relevance of this is reflected in the finding that patients treated with SPRIX required 26% less morphine over 48 hours than patients treated with placebo.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
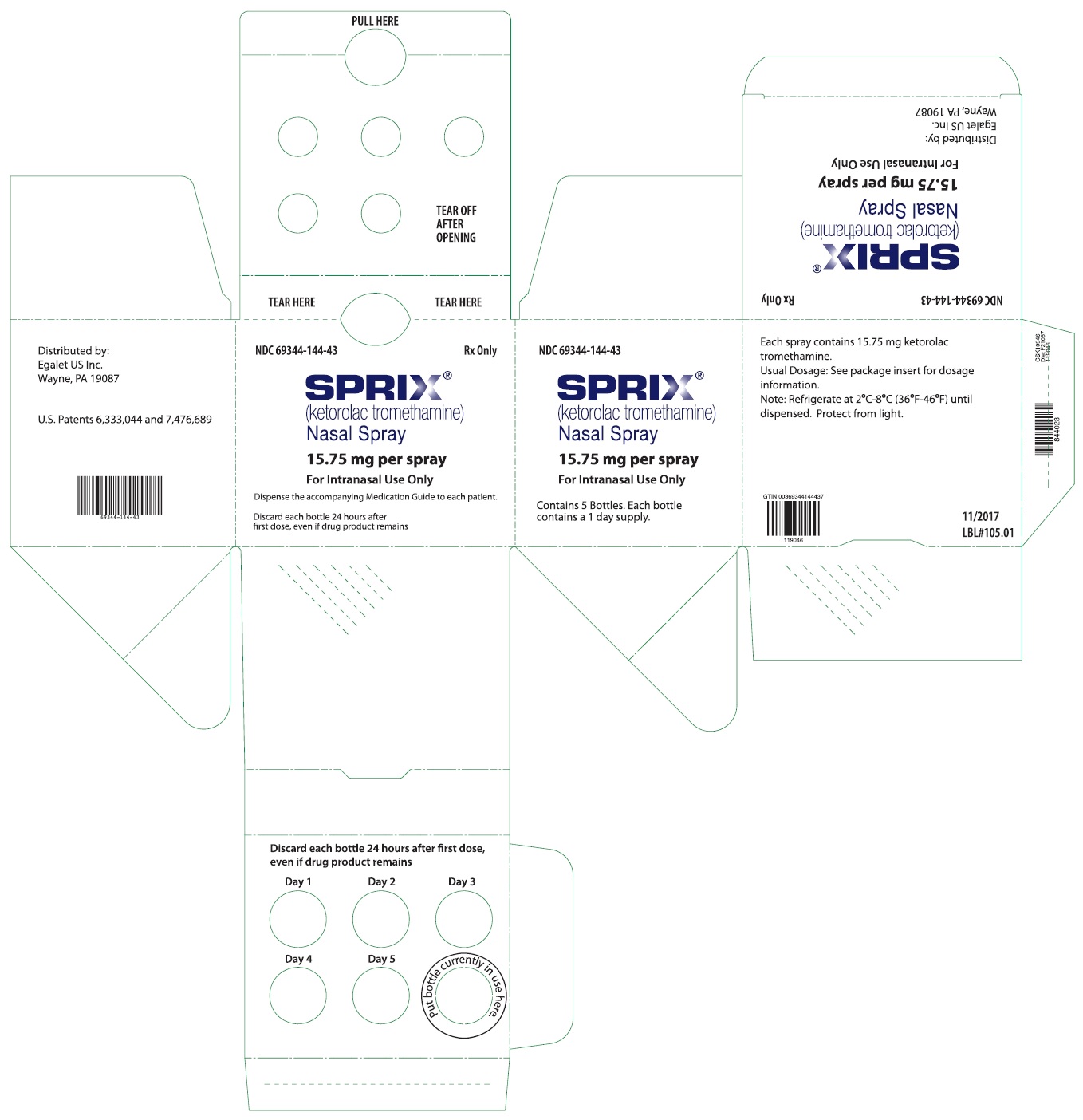
SPRIX (ketorolac tromethamine) Nasal Spray, 15.75 mg/spray, are single-day preservative-free spray bottles, supplied as:
NDC: 69344-144-43 Carton containing 5 single-day nasal spray bottles
NDC: 69344-144-53 Carton containing 1 single-day nasal spray bottleEach single-day nasal spray bottle contains a sufficient quantity of solution to deliver 8 sprays for a total of 126 mg of ketorolac tromethamine. Each spray delivers 15.75 mg of ketorolac tromethamine. The delivery system is designed to administer precisely metered doses of 100 µL per spray.
Storage
Protect from light and freezing. Store unopened SPRIX between 2°C to 8°C (36°F to 46°F). During use, keep containers of SPRIX Nasal Spray at controlled room temperature, between 15°C to 30°C (59°F to 86°F), out of direct sunlight. Bottles of SPRIX should be discarded within 24 hours of priming.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide and Instructions for Use) that accompanies each prescription dispensed. Instruct all patients to read and closely follow the FDA-approved SPRIX Patient Instructions to ensure proper administration of SPRIX. When prescribing SPRIX, inform patients or their caregivers of the potential risks of ketorolac treatment, instruct patients to seek medical advice if they develop treatment-related adverse events, advise patients not to give SPRIX to other family members, and advise patients to discard any unused drug. Inform patients, families, or their caregivers of the following information before initiating therapy with SPRIX and periodically during the course of ongoing therapy.
Cardiovascular Thrombotic Events
Advise patients to be alert for the symptoms of cardiovascular thrombotic events, including chest pain, shortness of breath, weakness, or slurring of speech, and to report any of these symptoms to their health care provider immediately [see Warnings and Precautions (5.1)].
Gastrointestinal Bleeding, Ulceration, and Perforation
Advise patients to report symptoms of ulcerations and bleeding, including epigastric pain, dyspepsia, melena, and hematemesis to their health care provider. In the setting of concomitant use of low-dose aspirin for cardiac prophylaxis, inform patients of the increased risk for and the signs and symptoms of GI bleeding [see Contraindications (4), Warnings and Precautions (5.2)].
Hepatotoxicity
Inform patients of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, pruritus, diarrhea, jaundice, right upper quadrant tenderness, and “flu-like” symptoms). If these occur, instruct patients to stop SPRIX and seek immediate medical therapy [see Warnings and Precautions (5.3)].
Heart Failure and Edema
Advise patients to be alert for the symptoms of congestive heart failure including shortness of breath, unexplained weight gain, or edema and to contact their healthcare provider if such symptoms occur [see Warnings and Precautions (5.5)].
Anaphylactic Reactions
Inform patients of the signs of an anaphylactic reaction (e.g., difficulty breathing, swelling of the face or throat). Instruct patients to seek immediate emergency help if these occur [see Contraindications (4) and Warnings and Precautions (5.7)].
Serious Skin Reactions
Advise patients to stop SPRIX immediately if they develop any type of rash and to contact their healthcare provider as soon as possible [see Warnings and Precautions (5.9)].
Female Fertility
Advise females of reproductive potential who desire pregnancy that NSAIDs, including SPRIX, may be associated with a reversible delay in ovulation [see Use in Specific Populations (8.3)].
Fetal Toxicity
Inform pregnant women to avoid use of SPRIX and other NSAIDs starting at 30 weeks gestation because of the risk of the premature closing of the fetal ductus arteriosus [see Warnings and Precautions (5.10) and Use in Specific Populations (8.1)].
Avoid Concomitant Use of NSAIDs
Inform patients that the concomitant use of SPRIX with other NSAIDs or salicylates (e.g., diflunisal, salsalate) is not recommended due to the increased risk of gastrointestinal toxicity, and little or no increase in efficacy [see Warnings and Precautions (5.2) and Drug Interactions (7)]. Alert patients that NSAIDs may be present in “over the counter” medications for treatment of colds, fever, or insomnia.
Use of NSAIDS and Low-Dose Aspirin
Inform patients not to use low-dose aspirin concomitantly with SPRIX until they talk to their healthcare provider [see Drug Interactions (7)].
Renal Effects
SPRIX is eliminated by the kidneys. Advise patients to maintain adequate fluid intake and request medical advice if urine output decreases significantly [see Contraindications (4), Warnings and Precautions (5.6)].
Limitations of Use
Instruct patients not to use SPRIX for more than 5 days. Use of SPRIX alone or in combination with any other ketorolac product for more than 5 days increases the risk for serious complications including GI bleeding and renal injury [see Dosage and Administration (2)].
Single-Day Container
Instruct patients not to use any single bottle of SPRIX for more than one day [see Dosage and Administration (2.5)].
Nasal Discomfort
Advise patients that they may experience transient, mild to moderate nasal irritation or discomfort upon dosing.
Manufactured for and Distributed by:
Zyla Life Sciences US Inc.
Wayne, PA 19087Issued: 09/2019
LBL # 101.03
-
MEDICATION GUIDE
Medication Guide for Nonsteroidal Anti-inflammatory Drugs (NSAIDs) What is the most important information I should know about medicines called Nonsteroidal Anti-inflammatory Drugs (NSAIDs)?
NSAIDs can cause serious side effects, including:-
Increased risk of a heart attack or stroke that can lead to death. This risk may happen early in treatment and may increase:
- with increasing doses of NSAIDs
- with longer use of NSAIDs
Avoid taking NSAIDs after a recent heart attack, unless your healthcare provider tells you to. You may have an increased risk of another heart attack if you take NSAIDs after a recent heart attack.-
Increased risk of bleeding, ulcers, and tears (perforation) of the esophagus (tube leading from the mouth to the stomach), stomach and intestines:
- anytime during use
- without warning symptoms
- that may cause death
- past history of stomach ulcers, or stomach or intestinal bleeding with use of NSAIDs
- taking medicines called “corticosteroids”, “anticoagulants”, “SSRIs”, or “SNRIs”
- increasing doses of NSAIDs
- longer use of NSAIDs
- smoking
- drinking alcohol
- older age
- poor health
- advanced liver disease
- bleeding problems
NSAIDs should only be used: - exactly as prescribed
- at the lowest dose possible for your treatment
- for the shortest time needed
What are NSAIDs?
NSAIDs are used to treat pain and redness, swelling, and heat (inflammation) from medical conditions such as different types of arthritis, menstrual cramps, and other types of short-term pain.Who should not take NSAIDs?
Do not take NSAIDs:- if you have had an asthma attack, hives, or other allergic reaction with aspirin or any other NSAIDs.
- right before or after heart bypass surgery.
Before taking NSAIDs, tell your healthcare provider about all of your medical conditions, including if you: - have liver or kidney problems
- have high blood pressure
- have asthma
- are pregnant or plan to become pregnant. Talk to your healthcare provider if you are considering taking NSAIDs during pregnancy. You should not take NSAIDs after 29 weeks of pregnancy.
- are breastfeeding or plan to breast feed.
What are the possible side effects of NSAIDs?
NSAIDs can cause serious side effects, including:
See “What is the most important information I should know about medicines called Nonsteroidal Anti-inflammatory Drugs (NSAIDs)?”- new or worse high blood pressure
- heart failure
- liver problems including liver failure
- kidney problems including kidney failure
- low red blood cells (anemia)
- life-threatening skin reactions
- life-threatening allergic reactions
- Other side effects of NSAIDs include: stomach pain, constipation, diarrhea, gas, heartburn, nausea, vomiting, and dizziness.
- shortness of breath or trouble breathing
- chest pain
- weakness in one part or side of your body
- slurred speech
- swelling of the face or throat
Stop taking your NSAID and call your healthcare provider right away if you get any of the following symptoms: - nausea
- more tired or weaker than usual
- diarrhea
- itching
- your skin or eyes look yellow
- indigestion or stomach pain
- flu-like symptoms
- vomit blood
- there is blood in your bowel movement or it is black and sticky like tar
- unusual weight gain
- skin rash or blisters with fever
- swelling of the arms, legs, hands and feet
If you take too much of your NSAID, call your healthcare provider or get medical help right away.
These are not all the possible side effects of NSAIDs. For more information, ask your healthcare provider or pharmacist about NSAIDs.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.Other information about NSAIDs - Aspirin is an NSAID but it does not increase the chance of a heart attack. Aspirin can cause bleeding in the brain, stomach, and intestines. Aspirin can also cause ulcers in the stomach and intestines.
- Some NSAIDs are sold in lower doses without a prescription (over-the-counter). Talk to your healthcare provider before using over-the-counter NSAIDs for more than 10 days.
General information about the safe and effective use of NSAIDs
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use NSAIDs for a condition for which it was not prescribed. Do not give NSAIDs to other people, even if they have the same symptoms that you have. It may harm them.
If you would like more information about NSAIDs, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about NSAIDs that is written for health professionals.Manufactured for: Zyla Life Sciences US Inc., Wayne, PA 19087
Distributed by: Zyla Life Sciences US Inc., Wayne, PA 19087
For more information, go to www.sprix.com or call 1-800-518-1084.This Medication Guide has been approved by the U.S. Food and Drug Administration. Issued or Revised: 09/2019
-
Increased risk of a heart attack or stroke that can lead to death. This risk may happen early in treatment and may increase:
-
INSTRUCTIONS FOR USE
Instructions for Use
SPRIX® (spriks)
(ketorolac tromethamine)
Nasal SprayRead this Instructions for Use before you start using SPRIX and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or your treatment.
Important information:
- SPRIX is for use in your nose only. Do not breathe in (inhale) SPRIX.
- Each SPRIX bottle has enough pain medicine for 1 day.
- Throw away each SPRIX bottle within 24 hours of taking your first dose, even if the bottle still contains unused medicine.
Your healthcare provider has prescribed SPRIX to treat moderate to severe pain.
- Use SPRIX exactly as your healthcare provider tells you to use it.
- Your healthcare provider will tell you how many sprays you should use each time you use SPRIX.
- Do not use SPRIX for more than 5 days. If you still have pain after 5 days, contact your healthcare provider.
- Do not use SPRIX more than every 6 hours.
- It is important that you drink plenty of fluids while you are using SPRIX. Tell your healthcare provider if you urinate less while using SPRIX.
You may have discomfort or irritation in your nose when using SPRIX. This usually lasts for a short time. Do not breathe in (inhale) SPRIX while spraying.
Using SPRIX Nasal Spray
Parts of your SPRIX bottle
Follow the instructions below to use SPRIX.
Before you use SPRIX for the first time, you will need to prime the bottle.
Priming SPRIX:
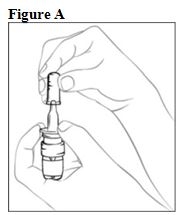
Step 1. Hold the finger flange with your fingers (see Figure A), and remove the clear plastic cover with your opposite hand. Keep the clear plastic cover for later. Remove and throw away the blue plastic safety clip.
If the clear plastic cover is improperly removed, the tip of the bottle may be pulled off of the glass vial. If this happens, place the tip back onto the glass vial by lining it up carefully and gently pushing it back on until it is back in the correct position (see Figure B). The SPRIX bottle should work properly again.
Step 2. Hold the SPRIX bottle upright at arm’s length away from you with your index finger and middle finger resting on the top of the finger flange and your thumb supporting the base (see Figure C).
Press down on the finger flange and release the pump 5 times. You may not see a spray the first few times you press down.
Now the pump is primed and ready to use. You do not need to prime the pump again if you use more doses from this bottle.
Step 3. Blow your nose to clear your nostrils.
Step 4. Sit up straight or stand.
Step 5. Keep your head tilted downward toward your toes.
Step 6. Place the tip of the SPRIX bottle into your right nostril.
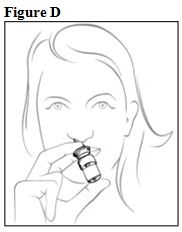
Step 7. Hold the SPRIX bottle upright and aim the tip toward the back of your nose (see Figure D).
Step 8. Hold your breath and spray 1 time into your right nostril, pressing down on both sides of the finger flange (see Figure D).
Step 9. Breathe in gently through your mouth after you use SPRIX. You may also pinch your nose to help keep the medicine in your nose.
Step 10. If your healthcare provider has prescribed only 1 spray per dose for you, you have now finished your dose, skip to Step 12 below.
Step 11. If your healthcare provider has prescribed 2 sprays for you, repeat steps 3 - 9 above for your left nostril. Be sure to point the spray away from the center of your nose. Spray 1 time into your left nostril.
Step 12. When you are finished using SPRIX, put the clear plastic cover back on the SPRIX bottle.
How should I store SPRIX?
- Store unopened SPRIX bottles between 36°F to 46°F (2°C to 8°C).
- Keep opened bottles of SPRIX at room temperature.
- Keep SPRIX out of direct sunlight.
- Do not freeze SPRIX.
- SPRIX does not contain a preservative. Throw away each SPRIX bottle within 24 hours of taking your first dose, even if the bottle still contains unused medicine.
Keep SPRIX and all medicines out of the reach of children.
General information about the safe and effective use of SPRIX.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not give SPRIX to other people, even if they have the same symptoms that you have. It may harm them.
You can ask your pharmacist or healthcare provider for information about SPRIX that is written for health professionals.
What are the ingredients in SPRIX?
Active ingredient: ketorolac tromethamine
Inactive ingredient: edetate disodium (EDTA), monobasic potassium phosphate, sodium hydroxide, and water for injection
This Instructions for Use has been approved by the U.S. Food and Drug Administration.
Distributed by:
Zyla Life Sciences US Inc.
Wayne, PA 19087LBL # 102.03
Revised: 09/2019
- PRINCIPAL DISPLAY PANEL - NDC: 69344-144-63 - Vial Label
- PRINCIPAL DISPLAY PANEL - NDC: 69344-144-43 - Carton Label
-
INGREDIENTS AND APPEARANCE
SPRIX
ketorolac tromethamine spray, meteredProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 69344-144 Route of Administration NASAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength KETOROLAC TROMETHAMINE (UNII: 4EVE5946BQ) (KETOROLAC - UNII:YZI5105V0L) KETOROLAC TROMETHAMINE 15.75 mg Inactive Ingredients Ingredient Name Strength EDETATE DISODIUM (UNII: 7FLD91C86K) POTASSIUM PHOSPHATE, MONOBASIC (UNII: 4J9FJ0HL51) SODIUM HYDROXIDE (UNII: 55X04QC32I) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 69344-144-43 5 in 1 CARTON 04/26/2011 1 NDC: 69344-144-53 1 in 1 CARTON 1 NDC: 69344-144-63 8 in 1 BOTTLE, SPRAY; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA022382 04/26/2011 Labeler - Zyla Life Sciences US Inc. (079581441)
Trademark Results [Sprix]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 SPRIX 97291727 not registered Live/Pending |
Sprix, Ltd. 2022-03-02 |
 SPRIX 85693913 5362215 Live/Registered |
SPRIX Co., Ltd. 2012-08-02 |
 SPRIX 77172987 3550920 Live/Registered |
ZYLA LIFE SCIENCES US INC. 2007-05-04 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.