FLUDARABINE PHOSPHATE tablet, film coated
Drug Labeling and Warnings
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
Fludarabine Phosphate Film-Coated Tablets
WARNING: CNS TOXICITY, HEMOLYTIC ANEMIA, AND PULMONARY TOXICITY
See full prescribing information for complete boxed warning.
- Severe central nervous system toxicity occurred in 36% of patients treated with doses approximately four times greater (96 mg/m2/day for 5 days to 7 days) than the recommended intravenous dose. This toxicity was seen in ≤0.2% of patients treated at the recommended intravenous dose levels (25 mg/m2). (5.1)
- Life-threatening and sometimes fatal autoimmune hemolytic anemia has been reported after one or more cycles of treatment. (5.2)
- High incidence of fatal pulmonary toxicity was observed in a clinical investigation of the combination of fludarabine phosphate with pentostatin (deoxycoformycin) for the treatment of refractory chronic lymphocytic leukemia (CLL). (5.3)
INDICATIONS AND USAGE
Fludarabine phosphate is a nucleotide metabolic inhibitor indicated as a single agent for the treatment of adult patients with B-cell chronic lymphocytic leukemia (CLL) whose disease has not responded to or has progressed during or after treatment with at least one standard alkylating-agent containing regimen. Studies demonstrating clinical benefit such as prolongation of survival or relief of symptoms have not been performed. A direct comparison of the clinical efficacy and safety of orally administered fludarabine phosphate relative to intravenously administered fludarabine phosphate has not been studied. (1)
DOSAGE AND ADMINISTRATION
Note: The oral dose is different than the intravenous dose.
Chronic Lymphocytic Leukemia (CLL) (2.1):
- The recommended adult dose is 40 mg/m2 administered daily for five consecutive days by the oral route.
- Begin each 5-day course of treatment every 28 days.
Renal Impairment (2.2): - Reduce dose by 20% in patients with mild to moderate renal impairment (creatinine clearance 30 to 70 mL/min/1.73 m2).
- Reduce dose by 50% in patients with severe renal impairment (creatinine clearance < 30 mL/min/1.73 m2)
DOSAGE FORMS AND STRENGTHS
- 10 milligram film-coated tablets. (see 3)
CONTRAINDICATIONS
- None
WARNINGS AND PRECAUTIONS
- Severe bone marrow suppression, notably anemia, thrombocytopenia and neutropenia. Monitor blood counts before and during treatment. (5.2)
- Infections. Monitor for signs or symptoms of infection. (5.3)
- Tumor lysis syndrome. Take precautions for patients at high risk. (5.4)
- Transfusion-associated graft-versus-host disease. Use only irradiated blood products for transfusions. (5.6)
- Fludarabine phosphate dose should be adjusted in patients with mild to moderate (creatinine clearance 30 to 70 mL/min/1.73 m2) or severe (creatinine clearance < 30 mL/min/1.73 m2) renal impairment. (5.7)
- Fetal harm may occur when administered to a pregnant woman. Women of childbearing potential and fertile males must take contraceptive measures during and at least for 6 months after the cessation of therapy. (5.9)
ADVERSE REACTIONS
Most common adverse reactions (incidence > 30%) include myelosuppression (neutropenia, thrombocytopenia and anemia). Fever, weakness, infection, pain, cough and anorexia were also reported as common adverse reactions. (6)
DRUG INTERACTIONS
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 2/2009
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: CNS TOXICITY, HEMOLYTIC ANEMIA, AND PULMONARY TOXICITY
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Chronic Lymphocytic Leukemia (CLL)
2.2 Renal Impairment
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Neurotoxicity
5.2 Bone Marrow Suppression
5.3 Pulmonary Toxicity
5.4 Infections
5.5 Tumor Lysis Syndrome
5.6 Use of Transfusions
5.7 Renal Impairment
5.8 Monitoring
5.9 Pregnancy
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Post Marketing Experience
7 DRUG INTERACTIONS
7.1 Pentostatin
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Patients with Renal Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
17.1 Bone Marrow Suppression
17.2 Infections
17.3 Pregnancy
17.4 Handling and Disposal
- * Sections or subsections omitted from the full prescribing information are not listed.
- N/A - Section Title Not Found In Database
-
BOXED WARNING
(What is this?)
WARNING: CNS TOXICITY, HEMOLYTIC ANEMIA, AND PULMONARY TOXICITY
Severe neurologic effects, including blindness, coma, and death were observed in dose-ranging studies in patients with acute leukemia when fludarabine phosphate was administered at high doses. This severe central nervous system toxicity occurred in 36% of patients treated with doses approximately four times greater (96 mg/m2/day for 5 days to 7 days) than the recommended intravenous dose (25 mg/m2/day). Similar severe central nervous system toxicity has been rarely (≤0.2%) reported in patients treated at doses in the range of the dose recommended for chronic lymphocytic leukemia. [See Warnings and Precautions (5.1)] Periodic neurological assessments are recommended.
Instances of life-threatening and sometimes fatal autoimmune hemolytic anemia have been reported after one or more cycles of treatment with fludarabine phosphate. Patients undergoing treatment with fludarabine phosphate should be evaluated and closely monitored for hemolysis. [See Warnings and Precautions (5.2)]
High incidence of fatal pulmonary toxicity was observed in a clinical investigation using fludarabine phosphate in combination with pentostatin (deoxycoformycin) for the treatment of refractory chronic lymphocytic leukemia (CLL). Therefore, the use of fludarabine phosphate in combination with pentostatin is not recommended [See Warnings and Precautions (5.3)]
-
1 INDICATIONS AND USAGE
Fludarabine phosphate is indicated as a single agent for the treatment of adult patients with B-cell chronic lymphocytic leukemia (CLL) whose disease has not responded to or has progressed during or after treatment with at least one standard alkylating-agent containing regimen. Studies demonstrating clinical benefit such as prolongation of survival or relief of symptoms have not been performed. Studies providing a direct comparison of the clinical efficacy and safety of orally administered fludarabine phosphate relative to intravenously administered fludarabine phosphate have not been performed.
-
2 DOSAGE AND ADMINISTRATION
2.1 Chronic Lymphocytic Leukemia (CLL)
The oral dose is different than the intravenous dose.
The recommended adult dose of fludarabine phosphate is 40 mg/m2 administered by mouth daily for five consecutive days. Each 5-day course of treatment should commence every 28 days. Dosage may be decreased or delayed based on evidence of hematologic or nonhematologic toxicity. Physicians should consider delaying or discontinuing the drug if neurotoxicity occurs. Fludarabine phosphate film-coated tablets can be taken either on an empty stomach or with food. The tablets have to be swallowed whole with water; they should not be chewed or broken.
The following table provides guidance for determining the number of tablets of fludarabine phosphate to be administered based on body surface area (BSA):
TABLE 1: SUGGESTED NUMBER OF TABLETS TO BE ADMINISTERED Body Surface Area (BSA) Calculated Total Dose Equivalent to
40 mg/m2 BSA (rounded up or down
to nearest 10 mg)Total Number of Tablets 0.75 – 0.88 30 mg 3 0.89 – 1.13 40 mg 4 1.14 – 1.38 50 mg 5 1.39 – 1.63 60 mg 6 1.64 – 1.88 70 mg 7 1.89 – 2.13 80 mg 8 2.14 – 2.38 90 mg 9 2.39 – 2.50 100 mg 10 A number of clinical settings may predispose to increased toxicity from fludarabine phosphate. These include advanced age, renal insufficiency, and bone marrow impairment. Such patients should be monitored closely for excessive toxicity and the dose modified accordingly. The optimal duration of treatment has not been clearly established. It is recommended that three additional cycles of fludarabine phosphate be administered following the achievement of a maximal response and then the drug should be discontinued.
2.2 Renal Impairment
-
Reduce dose by 20% in patients with mild to moderate renal impairment (creatinine clearance 30 to 70 mL/min/1.73 m2). [See Warnings and Precautions (5.7)]
-
Reduce dose by 50% in patients with severe renal impairment (creatinine clearance < 30 mL/min/1.73 m2). [See Warnings and Precautions (5.7)]
-
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Neurotoxicity
Dose-dependent neurotoxicity has been observed with fludarabine phosphate. Dose levels approximately 4 times greater (96 mg/m2/day for 5 days to 7 days) than the recommended intravenous dose (25 mg/m2/day for 5 days) were associated with a syndrome characterized by delayed blindness, coma and death. Symptoms appeared from 21 days to 60 days following the last dose. Thirteen of 36 patients (36.1%) who received fludarabine phosphate intravenously at high doses (≥ 96 mg/m2/day for 5 days to 7 days per course) developed severe neurotoxicity, while only one of 443 patients (0.2%) who received the drug intravenously at low doses (≤ 40 mg/m2/day for 5 days per course) developed toxicity. In the pivotal clinical study conducted with fludarabine phosphate film-coated tablets administered at 40 mg/m2, severe impairment of consciousness was reported in one patient. The effect of chronic administration of fludarabine phosphate on the central nervous system is unknown; however, patients have received the recommended dose for up to 15 courses of therapy. Physicians should consider delaying or discontinuing the drug if neurotoxicity occurs.
5.2 Bone Marrow Suppression
Severe bone marrow suppression, notably anemia, thrombocytopenia and neutropenia, has been reported in patients treated with fludarabine phosphate. In a study in adult solid tumor patients, the median time to nadir counts was 13 days (range, 3 days to 25 days) for granulocytes and 16 days (range, 2 days to 32 days) for platelets. Most patients had hematologic impairment at baseline either as a result of disease or as a result of prior myelosuppressive therapy. Cumulative myelosuppression may be seen. While chemotherapy-induced myelosuppression is often reversible, administration of fludarabine phosphate requires careful hematologic monitoring.
Several instances of trilineage bone marrow hypoplasia or aplasia resulting in pancytopenia, sometimes resulting in death, have been reported in adult patients. The duration of clinically significant cytopenia in the reported cases has ranged from approximately 2 months to approximately 1 year. These episodes have occurred both in previously treated or untreated patients. One case of pancytopenia was reported in the pivotal clinical study conducted with oral fludarabine phosphate tablets.
Instances of life-threatening and sometimes fatal autoimmune hemolytic anemia have been reported to occur after one or more cycles of treatment with fludarabine phosphate in patients with or without a previous history of autoimmune hemolytic anemia or a positive Coombs’ test and who may or may not be in remission from their disease. Steroids may or may not be effective in controlling these hemolytic episodes. The majority of patients rechallenged with fludarabine phosphate developed a recurrence in the hemolytic process. The mechanism(s) which predispose patients to the development of this complication has not been identified. Patients undergoing treatment with fludarabine phosphate should be evaluated and closely monitored for hemolysis.
5.3 Pulmonary Toxicity
A high incidence of fatal pulmonary toxicity was observed in a clinical investigation using fludarabine phosphate in combination with pentostatin (deoxycoformycin) for the treatment of refractory chronic lymphocytic leukemia (CLL) in adults. Therefore, the use of fludarabine phosphate in combination with pentostatin is not recommended.
5.4 Infections
Of 133 adult patients with CLL who received intravenous fludarabine phosphate in two clinical trials, there were 29 fatalities during study. Approximately 50% of the fatalities were due to infection and 25% due to progressive disease. Of 183 adult patients with CLL that received oral fludarabine phosphate in two clinical trials, there were 13 deaths. Approximately 50% of the deaths were due to progressive disease, while two patient deaths (15%) were attributed to infection. Monitor for signs and symptoms of infection.
5.5 Tumor Lysis Syndrome
Tumor lysis syndrome associated with fludarabine phosphate treatment has been reported in patients with CLL with large tumor burdens. Since fludarabine phosphate can induce a response as early as the first week of treatment, precautions should be taken in those patients at risk of developing this complication.
5.6 Use of Transfusions
Transfusion-associated graft-versus-host disease has been observed rarely after transfusion of non-irradiated blood in fludarabine phosphate treated patients. Consideration should, therefore, be given to the use of irradiated blood products in those patients requiring transfusions while undergoing treatment with fludarabine phosphate.
5.7 Renal Impairment
Fludarabine phosphate must be administered cautiously in patients with renal impairment. Following dosing of the intravenous product, the total body clearance of 2-fluoro-ara-A has been shown to be directly correlated with creatinine clearance. Patients with mild to moderate impairment of renal function (creatinine clearance 30 to 70 mL/min/1.73 m2) should have their oral fludarabine phosphate dose reduced by 20% and be monitored closely. Patients with severe impairment of renal function (creatinine clearance < 30 mL/min/1.73 m2) should have their oral fludarabine phosphate dose reduced by 50% and be monitored closely.
5.8 Monitoring
-
Hematologic and Nonhematologic Toxicity
Fludarabine phosphate is an antineoplastic agent with potentially significant toxic side effects. Patients undergoing therapy should be closely observed for signs of hematologic and nonhematologic toxicity. Periodic assessment of peripheral blood counts is recommended to detect the development of anemia, neutropenia and thrombocytopenia.
-
Hematopoietic Suppression
During treatment, the patient’s hematologic profile (particularly neutrophils and platelets) should be monitored regularly to determine the degree of hematopoietic suppression.
-
Infections
Patients treated with fludarabine phosphate appear to be at an increased risk of infection. Monitor for signs and symptoms of infection.
5.9 Pregnancy
Based on its mechanism of action, fludarabine phosphate can cause fetal harm when administered to a pregnant woman. Fludarabine phosphate administered to rats and rabbits during organogenesis caused an increase in resorptions, skeletal and visceral malformation, and decreased fetal body weights. If fludarabine phosphate is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus. Women of childbearing potential should be advised to avoid becoming pregnant. Women of childbearing potential and fertile males must take contraceptive measures during and at least for 6 months after the cessation of therapy.
[see Use in Specific Populations (8.1)]. -
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The data described below reflect exposure to fludarabine phosphate tablets in 159 patients exposed to the drug. Fludarabine phosphate tablets were studied primarily in Study 1 in 78 patients with CLL who received prior therapy and in Study 2 in 81 patients with CLL who had not received prior therapy.
Based on experience with the intravenous and oral use of fludarabine phosphate, the most common adverse reactions include myelosuppression (neutropenia, thrombocytopenia and anemia), fever and chills, infection, and nausea and vomiting. Other commonly reported events include malaise, fatigue, anorexia, and weakness. Serious opportunistic infections have occurred in patients with CLL treated with fludarabine phosphate. The most frequently reported adverse reactions and those reactions which are more clearly related to the drug, as reported in clinical studies conducted with intravenous and oral fludarabine phosphate, are arranged below according to body system.
Hematopoietic Systems
Hematologic events (neutropenia, thrombocytopenia, and/or anemia) were reported in the majority of patients with CLL treated with fludarabine phosphate. During intravenous fludarabine phosphate treatment of 133 patients with CLL, the absolute neutrophil count decreased to less than 500/mm3 in 59% of patients, hemoglobin decreased from pretreatment values by at least 2 grams percent in 60%, and platelet count decreased from pretreatment values by at least 50% in 55%. Among 78 patients with B-CLL who were treated with oral fludarabine phosphate, the absolute neutrophil count decreased to less than 500/mm3 in 37% of patients, hemoglobin decreased from pretreatment values by at least 2 grams percent in 14%, and platelet count decreased from pretreatment values by at least 50% in 17% of patients. Myelosuppression may be severe, cumulative, and may affect multiple cell lines. Bone marrow fibrosis occurred in one CLL patient treated with fludarabine phosphate intravenously. In the pivotal oral fludarabine phosphate study (Study 1), there was one report of a non-fatal case of pancytopenia. Similarly, there was one case of non-fatal pancytopenia reported among the 133 patients with CLL treated with intravenous fludarabine phosphate.
Life-threatening and sometimes fatal autoimmune hemolytic anemias have been reported to occur in patients receiving fludarabine phosphate. [See Warnings and Precautions (5.2)] The majority of patients rechallenged with fludarabine phosphate developed a recurrence in the hemolytic process.
Metabolic
Tumor lysis syndrome has been reported in patients with CLL treated with fludarabine phosphate for injection. This complication may include hyperuricemia, hyperphosphatemia, hypocalcemia, metabolic acidosis, hyperkalemia, hematuria, urate crystalluria, and renal failure. The onset of this syndrome may be heralded by flank pain and hematuria.
Nervous System
Objective weakness, agitation, confusion, visual disturbances, and coma have occurred in patients with CLL treated with fludarabine phosphate at the recommended dose. Peripheral neuropathy and one case of wrist-drop have been observed with intravenous administration of fludarabine phosphate. In Study 1 for oral fludarabine phosphate, there was one report of severe impairment of consciousness that presented concurrent with hemolytic anemia. This patient had enrolled in the study with pre-existing peripheral neurotoxicity. [See Warnings and Precautions (5.1)]
Pulmonary System
Pneumonia, a frequent manifestation of infection in patients with CLL, was observed in two clinical trials conducted with intravenous fludarabine phosphate (16% and 22%) and in two clinical trials with oral fludarabine phosphate (8% and 3%). Pulmonary hypersensitivity reactions to fludarabine phosphate characterized by dyspnea, cough and interstitial pulmonary infiltrate have been observed. In Study 1 conducted with oral fludarabine phosphate, severe pulmonary toxicity was reported in 5 of 78 patients, often in conjunction with respiratory or pulmonary infections and hence not regarded as isolated drug related pulmonary toxicity.
Gastrointestinal System
Gastrointestinal disturbances such as nausea and vomiting, anorexia, diarrhea, stomatitis and gastrointestinal bleeding have been reported in patients treated with fludarabine phosphate. Nausea and vomiting occurred in up to 38% of patients following treatment with oral fludarabine phosphate in the clinical trials.
Cardiovascular
Edema has been frequently reported. One patient developed a pericardial effusion possibly related to treatment with fludarabine phosphate. No other severe cardiovascular events were considered to be drug related.
Genitourinary System
Hemorrhagic cystitis has been reported in patients treated intravenously with fludarabine phosphate.
Skin
Skin toxicity, consisting primarily of skin rashes, has been reported in patients treated with oral and intravenous fludarabine phosphate.
Data in Table 2 are derived from the 159 patients with CLL who received fludarabine phosphate in Study 1 and Study 2.
TABLE 2: Incidence (≥5%) of Non-Hematologic Adverse Reactions in Patients with CLL Treated with Fludarabine Phosphate Tablets ADVERSE REACTIONS Study 1
(N=78)
%Study 2
(N=81)
%ANY ADVERSE REACTION 82 89 BODY AS A WHOLE 59 77 FEVER 26 11 INFECTION 12 17 PAIN 5 19 FLU SYNDROME 8 5 DIAPHORESIS 8 0 NEUROLOGICAL 19 41 WEAKNESS/FATIGUE (ASTHENIA) 13 31 SWEATING INCREASED 0 14 HEADACHE 9 9 PULMONARY 37 53 COUGH 21 0 COUGH INCREASED 0 6 PNEUMONIA 8 3 DYSPNEA 1 5 SINUSITIS 1 5 UPPER RESPIRATORY INFECTION 9 14 RHINITIS 3 11 BRONCHITIS 6 9 METABOLIC AND NUTRITIONAL 3 31 WEIGHT DECREASED 1 6 LACTIC DEHYDROGENASE INCREASED 0 6 PERIPHERAL EDEMA 0 7 GASTROINTESTINAL 41 28 NAUSEA 5 1 DIARRHEA 6 5 ANOREXIA 19 0 ABDOMINAL PAIN 8 10 CUTANEOUS 22 25 RASH 5 4 SKIN DISORDER 0 6 HERPES SIMPLEX 8 7 GENITOURINARY 8 14 URINARY TRACT INFECTION 4 5 CARDIOVASCULAR 14 17 CHEST PAIN 0 5 MUSCULOSKELETAL 10 19 BACK PAIN 4 9 6.2 Post Marketing Experience
The following adverse reactions have been identified during post approval use of oral fludarabine phosphate. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possibly to reliably estimate their frequency or establish a causal relationship to drug exposure.
Hematopoietic Systems
Several instances of trilineage bone marrow hypoplasia or aplasia resulting in pancytopenia, sometimes resulting in death, have been reported in post-marketing surveillance. The duration of clinically significant cytopenia in the reported cases has ranged from approximately 2 months to approximately 1 year. These episodes have occurred both in previously treated or untreated patients.
Nervous System
In post-marketing experience, cases of progressive multifocal leukoencephalopathy have been reported. Most cases had a fatal outcome. Many of these cases were confounded by prior and/or concurrent chemotherapy. The median time to onset was approximately one year.
Pulmonary System
In post-marketing experience, cases of severe pulmonary toxicity have been observed with fludarabine phosphate use which resulted in acute respiratory distress syndrome, respiratory distress, pulmonary hemorrhage, pulmonary fibrosis, and respiratory failure. After exclusion of an infectious origin, some patients experienced symptom improvement with corticosteroids.
-
7 DRUG INTERACTIONS
7.1 Pentostatin
The use of fludarabine phosphate in combination with pentostatin is not recommended due to the risk of severe pulmonary toxicity. [See Warnings and Precautions (5.6)]
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
“Pregnancy Category D. See ‘Warnings and Precautions’ section.”
Based on its mechanism of action, fludarabine phosphate can cause fetal harm when administered to a pregnant woman. There are no adequate and well-controlled studies of fludarabine phosphate in pregnant women. Fludarabine phosphate was embryolethal and teratogenic in both rats and rabbits. If fludarabine phosphate is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus. Women of childbearing potential should be advised to avoid becoming pregnant. Women of childbearing potential and fertile males must take contraceptive measures during and at least for 6 months after the cessation of therapy.
In rats, repeated intravenous doses of fludarabine phosphate at 1.5 times and 4.5 times the recommended human oral dose (40 mg/m2) administered during organogenesis caused an increase in resorptions, skeletal and visceral malformations (cleft palate, exencephaly, and fetal vertebrae deformities) and decreased fetal body weights. Maternal toxicity was not apparent at 1.5 times the human oral dose, and was limited to slight body weight decreases at 4.5 times the human oral dose. In rabbits, repeated intravenous doses of fludarabine phosphate at 2.4 times the human oral dose administered during organogenesis increased embryo and fetal lethality as indicated by increased resorptions and a decrease in live fetuses. A significant increase in malformations including cleft palate, hydrocephaly, adactyly, brachydactyly, fusions of the digits, diaphragmatic hernia, heart/great vessel defects, and vertebrae/rib anomalies were seen in all dose levels (≥ 0.3 times the human oral dose).
8.3 Nursing Mothers
It is not known whether fludarabine phosphate is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions including tumorgenicity in nursing infants, a decision should be made to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.
8.5 Geriatric Use
Of 78 previously treated patients with B-CLL treated with oral fludarabine phosphate 50% were ≥ age 65 and 3% were ≥ age 75. The response rate was generally lower among patients age 65 and older. Among previously treated patients (Study 1) age 65 and older, the overall objective response, according to standardized response criteria developed by the National Cancer Institute CLL Working Group (NCI criteria), was 41%. The safety profile among younger and older patients on study was similar. Other reported clinical experience has not identified differences in responses or safety between older and younger patients.
8.6 Patients with Renal Impairment
In patients receiving intravenous fludarabine phosphate, the total body clearance of the metabolite 2-fluoro-ara-adenine (2F-ara-A) correlated with the creatinine clearance, indicating the importance of the renal excretion pathway for the elimination of the drug. Renal clearance represented approximately 40% of the total body clearance. Patients with mild to moderate renal impairment (30 to 70 mL/min/1.73 m2) receiving 20% reduced fludarabine phosphate dose had a similar exposure compared to patients with normal renal function receiving the recommended dose (AUC; 21 nMh/mL versus 20 nMh/mL). Two patients with severe renal impairment (< 30 mL/min/1.73 m2) receiving 40% reduced fludarabine phosphate dose had a 40% increase in exposure compared to patients with normal renal function receiving the recommended dose. The mean total body clearance was 172 mL/min for patients with normal renal function, 124 mL/min for patients with mild to moderately impaired renal function, and 71 mL/min for the two patients with severe renal impairment.
-
10 OVERDOSAGE
High doses of fludarabine phosphate [See Indications and Usage (1.1) and Warnings and Precautions (5.1)] have been associated with an irreversible central nervous system toxicity characterized by delayed blindness, coma and death. High doses are also associated with severe thrombocytopenia and neutropenia due to bone marrow suppression. There is no known specific antidote for fludarabine phosphate overdosage. Treatment consists of drug discontinuation and supportive therapy. In Study 2, two patients ingested an overdose of 20% to 33% of oral fludarabine phosphate. No serious side effects were reported.
-
11 DESCRIPTION
The chemical name for fludarabine phosphate is 9H-Purin-6-amine, 2-fluoro-9-(5-O-phosphono-ß-D-arabinofuranosyl)(2-fluoro-ara-AMP). The molecular formula of fludarabine phosphate is C10H13FN5O7P (MW 365.2) and the structure is provided in Figure 1
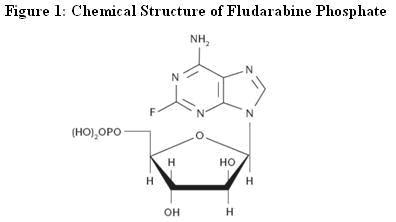
Fludarabine phosphate film-coated tablets for oral administration contain fludarabine phosphate, a fluorinated nucleotide analog of the antiviral agent vidarabine, 9-beta -D-arabinofuranosyladenine (ara-A) that is relatively resistant to deamination by adenosine deaminase. Each tablet contains 10 mg of the active ingredient fludarabine phosphate. The tablet core consists of microcrystalline cellulose, lactose monohydrate, colloidal anhydrous silicon dioxide, croscarmellose sodium and magnesium stearate. The film-coat contains hypromellose, talc, titanium dioxide (E171) and ferric oxide pigment (red/E172, yellow/E172).
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Fludarabine phosphate (2F-ara-AMP) is a synthetic purine nucleotide antimetabolite agent. Upon administration, 2F-ara-AMP is rapidly dephosphorylated in the plasma to 2F-ara-A, which then enters into the cell. Intracellularly, 2F-ara-A is converted to the 5'-triphosphate, 2-fluoro-ara-ATP (2F-ara-ATP). 2F-ara-ATP competes with deoxyadenosine triphosphate for incorporation into DNA. Once incorporated into DNA, 2F-ara-ATP functions as a DNA chain terminator, inhibits DNA polymerase alpha, gamma, and delta, and inhibits ribonucleoside diphosphate reductase. 2F-ara-A also inhibits DNA primase and DNA ligase I. The mechanism of action of this antimetabolite is not completely characterized and may be multi-faceted.
12.2 Pharmacodynamics
Cardiac Electrophysiology
In a randomized, uncontrolled, open-label, parallel study, patients with B-cell CLL were administered a single dose of oral fludarabine phosphate 40 mg/m2 (n = 42) or intravenous fludarabine phosphate 25 mg/m2 (n=14). The maximum increase in the baseline-corrected mean change in QTcI (individual-corrected QT interval) following treatment with oral fludarabine phosphate was less than 10 milliseconds.
12.3 Pharmacokinetics
Studies with the intravenous product have demonstrated that fludarabine phosphate is converted to the active metabolite, 2F-ara-A. Clinical pharmacology studies have focused on 2F-ara-A pharmacokinetics.
Following administration of the intravenous product, systemic plasma clearance of 2F-ara-A is approximately 117 mL/min to 145 mL/min. After five daily 30 minute intravenous infusions of 25 mg 2F-ara- AMP/m2 to cancer patients, trough concentrations of 2F-ara-A increased by a factor of about 2. The terminal half-life of 2F-ara-A was approximately 20 hours. Plasma protein binding of 2F-ara-A was approximately 19% to 29%. A correlation was noted between the degree of absolute granulocyte count nadir and increased area under the concentration x time curve (AUC).
2F-ara-A exhibits dose proportional increases in AUC and Cmax after single oral doses of 50 mg, 70 mg or 90 mg of 2F-ara-AMP. Cmax of 2F-ara-A occurs 1 hour to 2 hours after single or multiple oral doses and is approximately 20 % to 30 % of the maximum plasma concentrations produced at the end of a 30 minute intravenous infusion of the same dose. The absolute oral bioavailability of 2F-ara-A is 50 - 65% following single and repeated doses of the immediate release tablet formulation. Similar systemic exposure (AUC) was observed after a single 40 mg/m2 fludarabine phosphate oral dose and a single 25 mg/m2 fludarabine phosphate intravenous dose. The terminal half-life of 2F-ara-A was similar to that following intravenous administration; approximately 20 hours. The Cmax, AUC and terminal half-life of 2F-ara-A are unaffected when administered with a high fat meal, although Tmax is slightly delayed from 1.3 hours to 2.2 hours.
Following intravenous administration, renal clearance of 2F-ara-A represents approximately 40% of the total body clearance of fludarabine phosphate, and total body clearance is inversely correlated with serum creatinine and creatinine clearance. In two patients with median creatinine clearance of 22 mL/min/1.73 m2, 2F-ara-A clearance was reduced by 56%. Dosage adjustment based on creatinine clearance is recommended as follows:
Reduce dose by 20% in patients with mild to moderate renal impairment (creatinine clearance 30 to 70 mL/min/1.73 m2). [See Warnings and Precautions (5.7)]
Reduce dose by 50% in patients with severe renal impairment (creatinine clearance < 30 mL/min/1.73 m2). [See Warnings and Precautions (5.7)]
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No animal carcinogenicity studies with fludarabine phosphate have been conducted.
Fludarabine phosphate is a clastogen.
Fludarabine phosphate was clastogenic in vitro to Chinese hamster ovary cells (chromosome aberration assay) in the presence of metabolic activation and induced sister chromatid exchanges both in the presence and absence of metabolic activation. In addition, fludarabine phosphate was clastogenic in vivo (mouse micronucleus assay) but was not mutagenic to germ cells (dominant lethal test in male mice). Fludarabine phosphate was not mutagenic to bacteria (Ames test) or mammalian cells either in the presence or absence of metabolic activation.
Studies in mice, rats and dogs have demonstrated dose-related adverse effects on the male reproductive system. Observations consisted of a decrease in mean testicular weights in mice and rats with a trend toward decreased testicular weights in dogs and degeneration and necrosis of spermatogenic epithelium of the testes in mice, rats and dogs.
-
14 CLINICAL STUDIES
Study 1, a single-arm, open-label study of fludarabine phosphate film-coated tablets was conducted in 78 adult patients with CLL refractory to at least one prior standard alkylating-agent containing regimen. In this multicenter study patients were treated with oral fludarabine phosphate at a dose of 40 mg/m2 daily for 5 days every 28 days. The patient population median age was 64.5 years and consisted of 72% males and 28% females. Ninety-nine percent of the patients were Caucasian. The Rai stage for patients entering the study was: Stage 0 (3.9%), Stage I (20.5%), Stage II (32.1%), Stage III (11.5%), and Stage IV (32.1%). The mean number of treatment cycles was 5.1 with a mean daily dose of fludarabine phosphate of 38 mg/m2. The overall objective response, according to standardized response criteria developed by the National Cancer Institute CLL Working Group (NCI criteria), was 51 %, including 18% complete responses and 33% partial responses. The overall response rate, according to standardized criteria developed by the International Workshop on CLL (IWCLL criteria), was 46%, including 21% complete responses and 26% partial responses. Data on duration of response was not collected.
In Study 2, a supportive single-arm, open-label study, fludarabine phosphate tablets were administered to 81 previously untreated patients with B-CLL. In this multicenter study each patient was treated with oral fludarabine phosphate at a dose of 40 mg/m2 daily for 5 days every 28 days. The patient population median age was 64.0 years and consisted of 63% males and 37% females. Ninety-nine percent of the patients were Caucasian. The Rai stage for patients entering the study was: Stage 0 (3.7%), Stage I (37.0%), Stage II (37.0%), Stage III (9.9%), and Stage IV (12.3%). The mean number of treatment cycles was 5.9 with a mean daily dose per patient of 71 mg to 74 mg. The overall responses rate, according to NCI criteria, was 80%, including 12% complete responses and 68% partial responses. The overall response rate, according to IWCLL criteria, was 72%, including 37% complete responses and 35% partial responses. The median duration of response was 22.9 months.
Study 3 was a supportive randomized controlled open label study in patients with previously untreated B-CLL that included fludarabine phosphate monotherapy and fludarabine phosphate combination therapy arms. In this study 107 evaluable patients received fludarabine phosphate 40mg/m2 orally daily for 5 days every 28 days. The overall response rate according to modified NCI criteria was 74% and the CR plus nodular PR rate was 41%.
-
15 REFERENCES
-
Preventing Occupational Exposures to Antineoplastic and Other Hazardous Drugs in Health Care Settings. NIOSH Alert 2004-165.
-
OSHA Technical Manual, TED 1-0.15A, Section VI: Chapter 2. Controlling Occupational Exposure to Hazardous Drugs. OSHA, 1999.
http://www.osha.gov/dts/osta/otm/otm_vi/otm_vi_2.html
-
American Society of Health-System Pharmacists. ASHP guidelines on handling hazardous drugs. Am J Health-Syst Pharm. 2006;63:1172-1193.
-
Polovich, M., White, J. M., & Kelleher, L.O. (eds.) 2005. Chemotherapy and biotherapy guidelines and recommendations for practice (2nd. ed.) Pittsburgh, PA: Oncology Nursing Society.
-
-
16 HOW SUPPLIED/STORAGE AND HANDLING
HOW SUPPLIED
Fludarabine phosphate is supplied in 10 milligram tablets that are film-coated, capsule shaped, salmon pink in color, and marked on one side with ‘LN’ in a regular hexagon. Each film-coated tablet contains 10 mg fludarabine phosphate. The tablets are supplied in blisters, each blister strip containing 5 tablets. Packages of 15 and 20 tablets are available in child-resistant containers.
NDC: 45414-311-15: 15 - 10 milligram film-coated tablets per container. Each film-coated tablet is packaged in an individual blister package; 5 tablets per blister strip; 3 blister strips packaged in a plastic bottle with a child-resistant container closure; each bottle is packaged in an individual chip-board carton.
NDC: 45414-311-20: 20 - 10 milligram film-coated tablets per container. Each film-coated tablet is packaged in an individual blister package; 5 tablets per blister strip; 4 blister strips packaged in a plastic bottle with a child-resistant container closure; each bottle is packaged in an individual chip-board carton.
STORAGE
Store under normal lighting conditions at 25°C (77°F); excursions permitted to 15-30°C (59-86°F) [see USP controlled room temperature].
HANDLING AND DISPOSAL
Procedures for proper handling and disposal should be considered. Consideration should be given to handling and disposal according to guidelines issued for cytotoxic drugs. Several guidelines on this subject have been published.1-4 Caution should be exercised in the handling of fludarabine phosphate. Do not crush tablets. Avoid exposure by direct contact of the skin or mucous membranes or by inhalation. If contact occurs, wash thoroughly with soap and water or wash the eyes immediately with gently flowing water for at least 15 minutes. Consult healthcare provider in case of a skin reaction or if the drug gets in the eyes.
-
17 PATIENT COUNSELING INFORMATION
17.1 Bone Marrow Suppression
Inform patients that fludarabine phosphate decreases blood cell counts such as white blood cells, platelets, and red blood cells. Thus, it is important that periodic assessment of their blood count be performed to detect the development of neutropenia, thrombocytopenia and anemia. [See Warnings and Precautions (5.2)]
17.2 Infections
Instruct patients to notify their physician promptly if fever or other signs of infection such as chills, cough, or burning pain on urination occurs while on therapy. [See Warnings and Precautions (5.4)]
17.3 Pregnancy
Women of childbearing potential and fertile males must take contraceptive measures during and at least for 6 months after the cessation of therapy.
Fludarabine phosphate may cause fetal harm when administered to a pregnant woman. [See Warnings and Precautions (5.9)]
17.4 Handling and Disposal
Instruct patients that caution should be exercised in the handling of fludarabine phosphate. Do not crush tablets. Avoid exposure by direct contact of the skin or mucous membranes or by inhalation. If contact occurs, wash thoroughly with soap and water or wash the eyes immediately with gently flowing water for at least 15 minutes. Consult healthcare provider in case of a skin reaction or if the drug gets in the eyes. Ask your healthcare provider or pharmacist for directions about how to safely dispose of fludarabine phosphate.
Manufactured for: Antisoma Research Limited, Cambridge, MA 02139
Manufactured by: Bayer Schering Pharma AG, Berlin, Germany
Patient Package Insert
[TRADENAME] (phonetic spelling)
(oral fludarabine phosphate film-coated tablets)Read this Patient Information leaflet before you start taking [TRADENAME] and each time you get a refill. There may be new information. This information does not take the place of talking with your healthcare provider about your medical condition or your treatment.
What Is [TRADENAME]?
[TRADENAME] is a prescription anticancer medicine that slows or stops the growth of cancer cells in adults with chronic lymphocytic leukemia (CLL). [TRADENAME] also stops or slows the growth of some healthy cells. This can cause side effects that you should know about and report to your healthcare provider.
[TRADENAME] has not been studied in children.
What is the most important information I should know about [TRADENAME]?
On rare occasions people taking [TRADENAME] can have life-threatening symptoms. If you:
-
have problems seeing
-
feel very sleepy, tired, or confused
-
have shortness of breath or have trouble breathing
-
have yellow skin or dark urine
Tell your healthcare provider right away.
What should I tell my healthcare provider before taking [TRADENAME]?
Before taking [TRADENAME], tell your healthcare provider about all of your medical conditions, including if you:
-
have kidney problems
-
have bleeding problems
-
are pregnant or plan to become pregnant. It is not known if [TRADENAME] will harm your unborn baby. Talk to your doctor if you are pregnant or plan to become pregnant. Women should not get pregnant during treatment with [TRADENAME] because the unborn baby may be harmed. Both men and women must take contraceptive measures during and for at least six months after cessation of therapy. Call your doctor right away if you become pregnant during or in the six months after treatment with [TRADENAME].
-
are breast- feeding or plan to breast-feed. It is not known if [TRADENAME] passes into your breast milk. You and your healthcare provider should decide if you will take [TRADENAME] or breast-feed. You should not do both.
Tell your healthcare provider about all the medicines you take including prescription and non-prescription medicines, vitamins, and herbal supplements. Using [TRADENAME] with certain other medicines may affect each other. Using [TRADENAME] with other medicines may cause serious side effects.
Know the medicines you take. Keep a list of them with you to show your healthcare provider.
How should I take [TRADENAME]?
-
Take [TRADENAME] exactly as your healthcare provider tells you to take it.
-
Your healthcare provider will tell you how much and when to take [TRADENAME].
-
[TRADENAME] can be taken with or without food.
-
[TRADENAME] have to be swallowed whole with water; they should never be chewed, crushed, or broken. If you cannot swallow [TRADENAME] whole, ask your healthcare provider if you can take another form of fludarabine.
-
If you miss a dose call your healthcare provider.
-
If you take too much call your healthcare provider.
What should I avoid while taking [TRADENAME]?
-
Do not allow other people or pets to touch or take [TRADENAME].
-
Avoid letting the tablets (whole or broken) touch your skin
-
Do not chew tablets or hold them in your mouth. Swallow tablets right away.
-
Do not breathe in any powder or residue from a broken tablet.
-
If you touch a broken tablet, wash the area thoroughly with soap and water.
-
If any [TRADENAME] gets in your eyes, wash your eyes right away with water for at least 15 minutes, and call your healthcare provider right away.
-
Call your healthcare provider right away in case of a skin reaction.
What are the possible side effects of [TRADENAME]?
See “What is the most important information I should know about [TRADENAME]?”
[TRADENAME] may cause serious side effects, including:
Low blood cell counts.
[TRADENAME] lessens the number of blood cells that fight infection, help your blood to clot, and carry oxygen throughout your body. This can result in
-
Infection
-
Bleeding
-
Tiredness.
Avoid activities that can raise your chances of these conditions. Your healthcare provider will check your blood counts so that you will know when you are most at risk for infection, bleeding, and tiredness.
Call your healthcare provider right away if you have a temperature of 100.5 F. or above or do not feel well. Do not take a fever medicine until you check with your healthcare provider.
[TRADENAME] may cause other side effects, including:
-
nausea and vomiting
-
loss of appetite
-
skin rash
-
swelling in your legs
-
diarrhea
-
redness and irritation inside your mouth (stomatitis)
-
abdominal and muscle pain.
Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of [TRADENAME]. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
How should I store and throw away [TRADENAME]?
-
Store [TRADENAME] at 59-86°F (15-30°C).
-
Keep under normal light in a child-resistant container.
-
Safely throw away medicine that is out of date or no longer needed.
-
Do not put [TRADENAME] in your regular household trash.
-
Ask your healthcare provider or pharmacist for directions about how to safely throw away and handle [TRADENAME].
Keep [TRADENAME] and all medicines out of the reach of children.
General information about [TRADENAME]
Medicines are sometimes prescribed for conditions that are not mentioned in patient information. Do not use [TRADENAME] for a condition for which it was not prescribed. Do not give [TRADENAME] to other people, even if they have the same symptoms you have. It may harm them.
This patient information leaflet summarizes the most important information about [TRADENAME]. For more information about [TRADENAME], talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about [TRADENAME] that is written for health professionals. For more information go to www.fludarabine.com or call 1-8XX-XXX-XXXX.
What are the ingredients in [TRADENAME]?
Active ingredients: fludarabine phosphate
Inactive ingredients: microcrystalline cellulose, lactose monohydrate, colloidal anhydrous silicon dioxide, croscarmellose sodium and magnesium stearate. The film-coat contains hypromellose, talc, titanium dioxide (E171) and ferric oxide pigment (red/E172, yellow/E172).
Rx only
PPI Issued August 11, 2008
Antisoma Research Ltd
-
-
INGREDIENTS AND APPEARANCE
FLUDARABINE PHOSPHATE
fludarabine phosphate tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 45414-311 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength FLUDARABINE PHOSPHATE (UNII: 1X9VK9O1SC) (FLUDARABINE - UNII:P2K93U8740) 10 mg Inactive Ingredients Ingredient Name Strength microcrystalline cellulose (UNII: OP1R32D61U) lactose monohydrate (UNII: EWQ57Q8I5X) colloidal anhydrous silicon dioxide () croscarmellose sodium (UNII: M28OL1HH48) magnesium stearate (UNII: 70097M6I30) hypromellose (UNII: 3NXW29V3WO) talc (UNII: 7SEV7J4R1U) titanium dioxide (E171) () ferric oxide pigment (red/E172, yellow/E172) () Product Characteristics Color pink (salmon pink) Score no score Shape OVAL (capsule shaped) Size Flavor Imprint Code LN Contains Coating true Symbol false Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 45414-311-15 1 in 1 CARTON 1 3 in 1 BOTTLE 1 5 in 1 BLISTER PACK 2 NDC: 45414-311-20 1 in 1 CARTON 2 4 in 1 BOTTLE 2 5 in 1 BLISTER PACK Labeler - Antisoma Research Limited
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.