BOSULIF- bosutinib monohydrate tablet, film coated
BOSULIF by
Drug Labeling and Warnings
BOSULIF by is a Prescription medication manufactured, distributed, or labeled by Pfizer Laboratories Div Pfizer Inc, Pfizer Manufacturing Deutschland GmbH, Pfizer Ireland Pharmaceuticals. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use BOSULIF safely and effectively. See full prescribing information for BOSULIF.
BOSULIF® (bosutinib) tablets, for oral use
Initial U.S. Approval: 2012RECENT MAJOR CHANGES
INDICATIONS AND USAGE
BOSULIF is a kinase inhibitor indicated for the treatment of adult patients with
- Newly-diagnosed chronic phase Ph+ chronic myelogenous leukemia (CML). This indication is approved under accelerated approval based on molecular and cytogenetic response rates. Continued approval for this indication may be contingent upon verification and confirmation of clinical benefit in an ongoing long-term follow up trial. (1, 14)
- Chronic, accelerated, or blast phase Ph+ CML with resistance or intolerance to prior therapy. (1)
DOSAGE AND ADMINISTRATION
- Newly-diagnosed chronic phase Ph+ CML: 400 mg orally once daily with food. (2.1)
- Chronic, accelerated, or blast phase Ph+ CML with resistance or intolerance to prior therapy: 500 mg orally once daily with food. (2.1)
- Consider dose escalation by increments of 100 mg once daily to a maximum of 600 mg daily in patients who do not reach complete hematologic, cytogenetic, or molecular response and do not have Grade 3 or greater adverse reactions. (2.2)
- Adjust dosage for toxicity and organ impairment (2)
DOSAGE FORMS AND STRENGTHS
Tablets: 100 mg, 400 mg, and 500 mg. (3)
CONTRAINDICATIONS
Hypersensitivity to BOSULIF. (4)
WARNINGS AND PRECAUTIONS
- Gastrointestinal Toxicity: Monitor and manage as necessary. Withhold, dose reduce, or discontinue BOSULIF. (2.3, 5.1)
- Myelosuppression: Monitor blood counts and manage as necessary. (2.4, 5.2)
- Hepatic Toxicity: Monitor liver enzymes at least monthly for the first 3 months and as needed. Withhold, dose reduce, or discontinue BOSULIF. (2.3, 5.3)
- Cardiac Failure: Monitor and manage as necessary. (5.4)
- Fluid Retention: Monitor patients and manage using standard of care treatment. Withhold, dose reduce, or discontinue BOSULIF. (2.3, 5.5)
- Renal Toxicity: Monitor patients for renal function at baseline and during therapy with BOSULIF. (5.6)
- Embryo-Fetal Toxicity: BOSULIF can cause fetal harm. Advise patients of potential risk to a fetus and to use effective contraception. (5.7)
ADVERSE REACTIONS
Most common adverse reactions in patients with newly-diagnosed CML (incidence ≥20%) are diarrhea, nausea, thrombocytopenia, rash, increased alanine aminotransferase, abdominal pain, increased aspartate aminotransferase. (6)
Most common adverse reactions in patients with CML who were resistant or intolerant to prior therapy (incidence ≥20%) are diarrhea, nausea, abdominal pain, rash, thrombocytopenia, vomiting, anemia, fatigue, pyrexia, cough, headache, alanine aminotransferase, and edema. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Pfizer Inc. at 1-800-438-1985 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 10/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosing
2.2 Dose Escalation
2.3 Dose Adjustments for Non-Hematologic Adverse Reactions
2.4 Dose Adjustments for Myelosuppression
2.5 Dose Adjustments for Renal Impairment or Hepatic Impairment
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Gastrointestinal Toxicity
5.2 Myelosuppression
5.3 Hepatic Toxicity
5.4 Cardiac Failure
5.5 Fluid Retention
5.6 Renal Toxicity
5.7 Embryo-Fetal Toxicity
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Post-Marketing Experience
7 DRUG INTERACTIONS
7.1 Effect of Other Drugs on BOSULIF
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Newly-Diagnosed CP Ph+ CML
14.2 Imatinib-Resistant or -Intolerant Ph+ CP, AP, and BP CML
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage
16.3 Handling and Disposal
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
BOSULIF is indicated for the treatment of adult patients with:
- Newly-diagnosed chronic phase (CP) Philadelphia chromosome-positive chronic myelogenous leukemia (Ph+ CML). This indication is approved under accelerated approval based on molecular and cytogenetic response rates [see Clinical Studies (14.1)]. Continued approval for this indication may be contingent upon verification and confirmation of clinical benefit in an ongoing long-term follow up trial.
- Chronic phase, accelerated phase (AP), or blast phase (BP) Ph+ CML with resistance or intolerance to prior therapy.
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosing
The recommended dose is taken orally once daily with food. The tablet is to be swallowed whole and should not be broken or cut. Continue treatment with BOSULIF until disease progression or intolerance to therapy.
If a dose is missed beyond 12 hours, the patient should skip the dose and take the usual prescribed dose on the following day.
2.2 Dose Escalation
In clinical studies of adult Ph+ CML patients, dose escalation by increments of 100 mg once daily to a maximum of 600 mg once daily was allowed in patients who did not achieve or maintain a hematologic, cytogenetic, or molecular response and who did not have Grade 3 or higher adverse reactions at the recommended starting dosage.
2.3 Dose Adjustments for Non-Hematologic Adverse Reactions
Elevated liver transaminases: If elevations in liver transaminases greater than 5×institutional upper limit of normal (ULN) occur, withhold BOSULIF until recovery to less than or equal to 2.5×ULN and resume at 400 mg once daily thereafter. If recovery takes longer than 4 weeks, discontinue BOSULIF. If transaminase elevations greater than or equal to 3×ULN occur concurrently with bilirubin elevations greater than 2×ULN and alkaline phosphatase less than 2×ULN (Hy's law case definition), discontinue BOSULIF [see Warnings and Precautions (5.3)].
Diarrhea: For National Cancer Institute Common Terminology Criteria for Adverse Events (NCI CTCAE) Grade 3–4 diarrhea (increase of greater than or equal to 7 stools/day over baseline/pretreatment), withhold BOSULIF until recovery to Grade less than or equal to 1. BOSULIF may be resumed at 400 mg once daily [see Warnings and Precautions (5.1)].
For other clinically significant, moderate or severe non-hematological toxicity, withhold BOSULIF until the toxicity has resolved, then consider resuming BOSULIF at a dose reduced by 100 mg taken once daily. If clinically appropriate, consider re-escalating the dose of BOSULIF to the starting dose taken once daily. Doses less than 300 mg/day have been used in patients; however, efficacy has not been established.
2.4 Dose Adjustments for Myelosuppression
Dose reductions for severe or persistent neutropenia and thrombocytopenia are described below (Table 1).
Table 1: Dose Adjustments for Neutropenia and Thrombocytopenia - * Absolute Neutrophil Count
ANC* less than 1000×106/L
or
Platelets less than 50,000×106/LWithhold BOSULIF until ANC greater than or equal to1000×106/L and platelets greater than or equal to 50,000×106/L.
Resume treatment with BOSULIF at the same dose if recovery occurs within 2 weeks. If blood counts remain low for greater than 2 weeks, upon recovery, reduce dose by 100 mg and resume treatment.
If cytopenia recurs, reduce dose by an additional 100 mg upon recovery and resume treatment.
Doses less than 300 mg/day have been used in patients; however, efficacy has not been established.2.5 Dose Adjustments for Renal Impairment or Hepatic Impairment
The recommended starting doses for patients with renal and hepatic impairment are described in Table 2 below.
Table 2: Dose Adjustments for Renal and Hepatic Impairment Recommended Starting Dosage Newly-diagnosed chronic phase Ph+ CML2 Chronic, accelerated, or blast phase Ph+ CML with resistance or intolerance to prior therapy [see Use in Specific Populations (8.6, 8.7) and Clinical Pharmacology (12.3)]. Abbreviations: CML=chronic myelogenous leukemia; Ph+=Philadelphia chromosome-positive. - * There are no clinical data for efficacy at the dose of 200 mg once daily in patients with CML.
Normal renal and hepatic function 400 mg daily 500 mg daily Renal impairment Creatinine clearance 30 to 50 mL/min 300 mg daily 400 mg daily Creatinine clearance less than 30 mL/min 200 mg daily 300 mg daily Hepatic impairment Mild (Child-Pugh A), Moderate (Child-Pugh B) or Severe (Child-Pugh C) 200 mg daily* 200 mg daily* -
3 DOSAGE FORMS AND STRENGTHS
- 100 mg tablets: yellow, oval, biconvex, film-coated tablets debossed with "Pfizer" on one side and "100" on the other.
- 400 mg tablets: orange, oval, biconvex, film-coated tablets debossed with "Pfizer" on one side and "400" on the other.
- 500 mg tablets: red, oval, biconvex, film-coated tablets debossed with "Pfizer" on one side and "500" on the other.
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Gastrointestinal Toxicity
Diarrhea, nausea, vomiting, and abdominal pain occur with BOSULIF treatment. Monitor and manage patients using standards of care, including antidiarrheals, antiemetics, and fluid replacement.
In the randomized clinical trial in patients with newly-diagnosed Ph+ CML, the median time to onset for diarrhea (all grades) was 3 days and the median duration per event was 3 days.
Among 546 patients in a single-arm study in patients with CML who were resistant or intolerant to prior therapy, the median time to onset for diarrhea (all grades) was 2 days and the median duration per event was 2 days. Among the patients who experienced diarrhea, the median number of episodes of diarrhea per patient during treatment with BOSULIF was 3 (range 1–268).
To manage gastrointestinal toxicity, withhold, dose reduce, or discontinue BOSULIF as necessary [see Dosage and Administration (2.3) and Adverse Reactions (6)].
5.2 Myelosuppression
Thrombocytopenia, anemia and neutropenia occur with BOSULIF treatment. Perform complete blood counts weekly for the first month of therapy and then monthly thereafter, or as clinically indicated. To manage myelosuppression, withhold, dose reduce, or discontinue BOSULIF as necessary [see Dosage and Administration (2.4) and Adverse Reactions (6)].
5.3 Hepatic Toxicity
Bosutinib may cause elevations in serum transaminases (alanine aminotransferase [ALT], aspartate aminotransferase [AST]).
One case consistent with drug induced liver injury (defined as concurrent elevations in ALT or AST greater than or equal to 3×ULN with total bilirubin greater than 2×ULN and alkaline phosphatase less than 2×ULN) occurred without alternative causes in a breast cancer (a disease for which BOSULIF is not indicated) trial of BOSULIF in combination with letrozole. The patient recovered fully following discontinuation of BOSULIF. This case represented 1 out of 1611 patients in BOSULIF clinical trials.
In the 268 patients from the safety population in the randomized clinical trial in patients with newly-diagnosed CML in the BOSULIF treatment group, the incidence of ALT elevation was 31% and AST elevation was 23%. Of patients who experienced transaminase elevations of any grade, 79% experienced their first event within the first 3 months. The median time to onset of increased ALT and AST was 32 and 43 days, respectively, and the median duration was 20 and 15 days, respectively.
Among the 546 patients in a single-arm study in patients with CML who were resistant or intolerant to prior therapy, the incidence of ALT elevation was 18% and AST elevation was 15%. Twenty percent of the patients experienced an increase in either ALT or AST. Most cases of transaminase elevations in this study occurred early in treatment; of patients who experienced transaminase elevations of any grade, more than 80% experienced their first event within the first 3 months. The median time to onset of increased ALT and AST was 35 and 33 days, respectively, and the median duration for each was 21 days.
Perform hepatic enzyme tests monthly for the first 3 months of BOSULIF treatment and as clinically indicated. In patients with transaminase elevations, monitor liver enzymes more frequently. Withhold, dose reduce, or discontinue BOSULIF as necessary [see Dosage and Administration (2.3) and Adverse Reactions (6)].
5.4 Cardiac Failure
Cardiac failure and left ventricular dysfunction have been reported in patients taking BOSULIF. These events occurred more frequently in previously treated patients than in patients with newly diagnosed CML and were more frequent in patients with advanced age or risk factors, including previous medical history of cardiac failure.
In a randomized study with newly diagnosed CML, cardiac failure occurred in 1.5% of patients treated with BOSULIF compared to 0.8% of patients treated with imatinib.
In a single-arm study in patients with CML who were resistant or intolerant to prior therapy, cardiac failure was observed in 5.3% of patients treated with BOSULIF.
Monitor patients for signs and symptoms consistent with cardiac failure and treat as clinically indicated. Interrupt, dose reduce, or discontinue BOSULIF as necessary [see Dosage and Administration (2.3)].
5.5 Fluid Retention
Fluid retention occurs with BOSULIF and may manifest as pericardial effusion, pleural effusion, pulmonary edema, and/or peripheral edema.
In the randomized clinical trial of 268 patients with newly-diagnosed CML in the bosutinib treatment group, 1 patient (0.4%) experienced severe fluid retention of Grade 3 pericardial effusion. Among 546 patients in a single-arm study in patients with Ph+ CML who were resistant or intolerant to prior therapy, Grade 3 or 4 fluid retention was reported in 26 patients (5%). Some patients experienced more than one fluid retention event. Specifically, 21 patients experienced Grade 3 or 4 pleural effusions, 7 patients experienced Grade 3 or Grade 4 pericardial effusions, and 6 patients experienced Grade 3 edema.
Monitor and manage patients using standards of care. Interrupt, dose reduce or discontinue BOSULIF as necessary [see Dosage and Administration (2.3) and Adverse Reactions (6)].
5.6 Renal Toxicity
An on-treatment decline in estimated glomerular filtration rate (eGFR) has occurred in patients treated with BOSULIF. Table 3 identifies the shift from baseline to lowest observed eGFR during BOSULIF therapy for patients in the pooled leukemia studies regardless of line of therapy. The median duration of therapy with BOSULIF was approximately 14 months (range, 0.03 to 123) for patients in these studies.
Table 3: Shift From Baseline to Lowest Observed eGFR Group During Treatment Safety Population in Clinical Studies (N=1272)* Baseline Follow-Up Renal Function Status N Normal
n (%)Mild
n (%)Mild to Moderate
n (%)Moderate to Severe
n (%)Severe
n (%)Kidney Failure
n (%)Abbreviations: eGFR=estimated glomerular filtration rate; N/n=number of patients. Notes: Grading is based on Modification in Diet in Renal Disease method (MDRD). Kidney Disease: Improving Global Outcomes (KDIGO) Classification by eGFR: Normal: greater than or equal to 90, Mild: 60 to less than 90, Mild to Moderate: 45 to less than 60, Moderate to Severe: 30 to less than 45, Severe: 15 to less than 30, Kidney Failure: less than 15 ml/min/1.73 m2. - * Among the 1272 patients, eGFR was missing in 9 patients at baseline or on-therapy. There were no patients with kidney failure at baseline.
Normal 468 102 (21.8) 298 (63.7) 46 (9.8) 16 (3.4) 2 (0.4) 2 (0.4) Mild 639 11 (1.7) 266 (41.6) 250 (39.1) 83 (13.0) 21 (3.3) 3 (0.5) Mild to Moderate 128 0 8 (6.3) 45 (35.2) 57 (44.5) 18 (14.1) 0 Moderate to Severe 32 0 1 (3.1) 1 (3.1) 9 (28.1) 17 (53.1) 3 (9.4) Severe 1 0 0 0 0 0 1 (100) Total 1268 113 (8.9) 573 (45.2) 342 (27.0) 165 (13.0) 58 (4.6) 9 (0.7) Monitor renal function at baseline and during therapy with BOSULIF, with particular attention to those patients who have preexisting renal impairment or risk factors for renal dysfunction. Consider dose adjustment in patients with baseline and treatment emergent renal impairment [see Dosage and Administration (2.5)].
5.7 Embryo-Fetal Toxicity
Based on findings from animal studies and its mechanism of action, BOSULIF can cause fetal harm when administered to a pregnant woman. There are no available data in pregnant women to inform the drug-associated risk. In animal reproduction studies conducted in rats and rabbits, oral administration of bosutinib during organogenesis caused adverse developmental outcomes, including structural abnormalities, embryo-fetal mortality, and alterations to growth at maternal exposures (AUC) as low as 1.2 times the human exposure at the dose of 500 mg/day (see Data). Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment and for at least 2 weeks after the last dose [see Use in Specific Populations (8.1, 8.3) and Clinical Pharmacology (12.1)].
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are discussed in greater detail in other sections of the labeling:
- Gastrointestinal toxicity [see Warnings and Precautions (5.1)].
- Myelosuppression [see Warnings and Precautions (5.2)].
- Hepatic toxicity [see Warnings and Precautions (5.3)].
- Cardiac Failure [see Warnings and Precautions (5.4)]
- Fluid retention [see Warnings and Precautions (5.5)].
- Renal toxicity [see Warnings and Precautions (5.6)].
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Serious adverse reactions reported include anaphylactic shock [see Contraindications (4)], myelosuppression, gastrointestinal toxicity (diarrhea), fluid retention, hepatotoxicity and rash.
Adverse Reactions in Patients With Newly-Diagnosed CP CML
The clinical trial randomized and treated 533 patients with newly-diagnosed CP CML to receive BOSULIF 400 mg daily or imatinib 400 mg daily as single agents (Newly-Diagnosed CP CML Study) [see Clinical Studies (14.1)]. The safety population (received at least 1 dose of BOSULIF) included:
- two hundred sixty-eight (268) patients with newly-diagnosed CP CML had a median duration of BOSULIF treatment of 14.1 months (range: 0.3 to 24.7 months) and a median dose intensity of 391.8 mg/day.
Adverse reactions reported for greater than or equal to 20% of bosutinib patients with newly-diagnosed CML (N=268) were diarrhea (70%), nausea (35%), thrombocytopenia (35%), rash (34%), increased ALT (31%), abdominal pain (25%), and increased AST (23%) [see Clinical Studies (14.1)].
Table 4 identifies adverse reactions greater than or equal to 10% for All Grades and Grades 3 or 4 (3/4) for the Phase 3 CP CML safety population.
Table 4: Adverse Reactions (10% or Greater) in Patients With Newly-Diagnosed CML in Bosutinib 400 mg Study Adverse Reaction Bosutinib 400 mg Chronic Phase CML
N=268Imatinib 400 mg Chronic Phase CML
N=265All Grades
(%)Grade 3/4
(%)All Grades
(%)Grade 3/4
(%)Abbreviation: CML=Chronic myelogenous leukemia, N=number of patients. - * Thrombocytopenia includes the following preferred terms: Platelet count decreased, Thrombocytopenia.
- † Rash includes the following preferred terms: Acne, Dermatitis, Dermatitis acneiform, Dermatitis allergic, Dermatitis exfoliative, Drug reaction with eosinophilia and systemic symptoms, Photosensitivity reaction, Rash, Rash erythematous, Rash generalised, Rash macular, Rash maculo-papular, Rash papular, Rash pruritic, Urticaria.
- ‡ Abdominal pain includes the following preferred terms: Abdominal discomfort, Abdominal pain, Abdominal pain lower, Abdominal pain upper, Abdominal tenderness, Gastrointestinal pain.
- § Anemia includes the following preferred terms: Anemia, Hemoglobin decreased
- ¶ Fatigue includes the following preferred terms: Fatigue, Malaise.
- # Lipase increased includes the following preferred terms: Hyperlipasemia, Lipase increased.
- Þ Respiratory tract infection includes the following preferred terms: Lower respiratory tract infection, Respiratory tract infection, Respiratory tract infection viral, Upper respiratory tract infection, Viral upper respiratory tract infection.
- ß Neutropenia includes the following preferred terms: Neutropenia, Neutrophil count decreased.
Diarrhea 70 8 34 <1 Nausea 35 0 38 0 Thrombocytopenia* 35 14 20 6 Rash† 34 1 21 2 Alanine aminotransferase increased 31 19 6 2 Abdominal pain‡ 25 2 15 <1 Aspartate aminotransferase increased 23 10 6 2 Anemia§ 19 3 19 5 Headache 19 1 13 1 Fatigue¶ 19 <1 19 0 Vomiting 18 1 16 0 Lipase increased# 13 10 8 5 Pyrexia 13 <1 8 0 Respiratory tract infectionÞ 12 <1 12 <1 Neutropeniaß 11 7 21 12 Arthralgia 11 <1 13 0 Asthenia 11 0 6 0 Appetite decreased 10 <1 6 0 In the randomized study in patients with newly-diagnosed CP CML, one patient in the group treated with BOSULIF experienced a Grade 3 QTc prolongation (>500 msec). Patients with uncontrolled or significant cardiovascular disease including QT interval prolongation were excluded by protocol.
Table 5 identifies the clinically relevant or severe Grade 3/4 laboratory test abnormalities for the Phase 3 newly-diagnosed CML safety population.
Table 5: Number (%) of Patients With Clinically Relevant or Grade 3/4 Laboratory Test Abnormalities in Patients With Newly-Diagnosed CML in Bosutinib 400 mg Study, Safety Population Bosutinib
Chronic Phase CML
N=268
n (%)Imatinib
Chronic Phase CML
N=265
n (%)Abbreviations: ALT=alanine aminotransferase; AST=aspartate aminotransferase; CML=chronic myelogenous leukemia; SGPT=serum glutamic-pyruvic transaminase; SGOT=serum glutamic-oxaloacetic transaminase; N/n=number of patients; ULN=upper limit of normal. Hematology Parameters Platelet Count (Low) less than 50×109/L 38 (14.2) 17 (6.4) Absolute Neutrophil Count less than 1×109/L 24 (9.0) 49 (18.5) Hemoglobin (Low) less than 80 g/L 19 (7.1) 15 (5.7) White Blood Cell Count (Low) less than 2×109/L 15 (5.6) 20 (7.5) Biochemistry Parameters SGPT/ALT greater than 5.0×ULN 62 (23.1) 7 (2.6) SGOT/AST greater than 5.0×ULN 32 (11.9) 8 (3.0) Lipase greater than 2×ULN 35 (13.1) 16 (6.0) Phosphorus (Low) less than 0.6 mmol/L 12 (4.5) 45 (17.0) Total Bilirubin greater than 3.0×ULN 3 (1.1) 2 (0.8) Amylase greater than 2×ULN 6 (2.2) 4 (1.5) Creatinine greater than 3.0×baseline; greater than 3.0×ULN 0 2 (0.8) Adverse Reactions in Patients With Imatinib-Resistant or -Intolerant Ph+ CP, AP, and BP CML
The single-arm clinical trial enrolled patients with Ph+ CP, AP, or BP CML and with resistance or intolerance to prior therapy [see Clinical Studies (14)]. The safety population (received at least 1 dose of BOSULIF) included 546 CML patients:
- two hundred eighty-four (284) patients with CP CML previously treated with imatinib only who had a median duration of BOSULIF treatment of 26 months, and a median dose intensity of 442 mg/day.
- one hundred nineteen (119) patients with CP CML previously treated with both imatinib and at least 1 additional tyrosine kinase inhibitor (TKI) who had a median duration of BOSULIF treatment of 9 months and a median dose intensity of 442 mg/day.
- one hundred forty-three (143) patients with advanced phase CML including 79 patients with AP CML and 64 patients with BP CML. In the patients with AP CML and BP CML, the median duration of BOSULIF treatment was 10 months and 3 months, respectively. The median dose intensity was 425 mg/day, and 456 mg/day, in the AP CML and BP CML cohorts, respectively.
Adverse reactions of any toxicity grade reported for greater than or equal to 20% of patients in the safety population of the single-arm trial in patients with CP CML (N=546) who were resistant or intolerant to prior therapy were diarrhea (85%), nausea (47%), abdominal pain (42%), rash (42%), thrombocytopenia (40%), vomiting (37%), anemia (27%), fatigue (26%), pyrexia (23%), cough (22%), headache (21%), ALT (20%), and edema (20%) [see Clinical Studies (14.2)].
Table 6 identifies adverse reactions greater than or equal to 10% for All Grades and Grades 3 or 4 for the Phase 1/2 CML safety population based on long-term follow-up.
Table 6: Adverse Reactions (10% or Greater) in Patients With CML Who Were Resistant or Intolerant to Prior Therapy in Single-Arm Trial* Chronic Phase CML
N=403Advanced Phase CML
N=143All Grades
(%)Grade 3/4
(%)All Grades
(%)Grade 3/4
(%)Abbreviations: CML=chronic myelogenous leukemia; N=number of patients. Advanced Phase CML includes patients with Accelerated Phase and Blast Phase CML. - * Based on a Minimum of 48 Months of Follow-up.
- † Abdominal pain includes the following preferred terms: Abdominal discomfort, Abdominal pain, Abdominal pain lower, Abdominal pain upper, Abdominal tenderness, Gastrointestinal pain
- ‡ Rash includes the following preferred terms: Acne, Dermatitis, Dermatitis acneiform, Dermatitis allergic, Drug eruption, Exfoliative rash, Photosensitivity reaction, Rash, Rash erythematous, Rash generalised, Rash macular, Rash maculo-papular, Rash papular, Rash pruritic, Urticaria
- § Thrombocytopenia includes the following preferred terms: Platelet count decreased, Thrombocytopenia
- ¶ Anemia includes the following preferred terms: Anemia, Hemoglobin decreased.
- # Fatigue includes the following preferred terms: Fatigue, Malaise.
- Þ Neutropenia includes the following preferred terms: Neutropenia, Neutrophil count decreased
- ß Edema includes the following preferred terms containing: Edema, Edema peripheral, Face edema, Localized edema.
- à Respiratory tract infection includes the following preferred terms: Lower respiratory tract infection, Respiratory tract infection, Respiratory tract infection viral, Upper respiratory tract infection, Viral upper respiratory tract infection.
- è Leukopenia includes the following preferred terms: Leukopenia, White blood cell count decreased.
- ð Chest pain included the following preferred terms: Chest discomfort, Chest pain.
Diarrhea 85 9 76 4 Nausea 47 1 48 2 Abdominal Pain† 42 2 31 6 Rash‡ 42 9 38 5 Thrombocytopenia§ 40 26 45 39 Vomiting 37 3 43 3 Anemia¶ 27 11 38 27 Fatigue# 26 2 21 5 Pyrexia 23 <1 37 2 Cough 22 0 22 0 Headache 21 <1 17 4 Alanine aminotransferase increased 20 8 10 5 NeutropeniaÞ 18 12 22 20 Arthralgia 17 <1 14 0 Aspartate aminotransferase increased 16 3 11 3 Edemaß 20 1 17 2 Respiratory tract infectionà 15 <1 10 0 Decreased appetite 14 <1 13 0 Back pain 13 <1 8 1 Nasopharyngitis 13 0 6 0 Asthenia 13 2 10 <1 Pleural effusion 12 4 9 4 Dyspnea 12 2 20 6 Pruritus 12 <1 7 0 Dizziness 11 0 13 <1 Leukopeniaè 10 4 15 12 Blood creatinine increased 10 <1 6 <1 Influenza 10 <1 3 0 Chest painð 7 1 12 1 In the single-arm study in patients with CML who were resistant or intolerant to prior therapy, 1 patient (0.2%) experienced QTcF interval of greater than 500 milliseconds. Patients with uncontrolled or significant cardiovascular disease including QT interval prolongation were excluded by protocol.
Table 7 identifies the clinically relevant or severe Grade 3/4 laboratory test abnormalities for the safety population of the study in patients with CML who were resistant or intolerant to prior therapy based on long-term follow-up.
Table 7: Number (%) of Patients With Clinically Relevant or Grade 3/4 Laboratory Test Abnormalities in the Safety Population of the Study of Patients With CML Who Were Resistant or Intolerant to Prior Therapy* Chronic Phase (CP) CML
N=403
n (%)Advanced Phase (AdvP) CML
N=143
n (%)All CP and AdvP CML
N=546
n (%)Abbreviations: ALT=alanine aminotransferase; AST=aspartate aminotransferase; CML=chronic myelogenous leukemia; N/n=number of patients; SGPT=serum glutamate-pyruvate transaminase; SGOT=serum glutamate-oxaloacetate aminotransferase; ULN=upper limit of normal. - * Based on a Minimum of 48 Months of Follow-up.
Hematology Parameters Platelet Count (Low) less than 50×109/L 105 (26) 82 (57) 187 (34) Absolute Neutrophil Count less than 1×109/L 65 (16) 55 (39) 120 (22) Hemoglobin (Low) less than 80 g/L 51 (13) 54 (38) 105 (19) Biochemistry Parameters SGPT/ALT greater than 5.0×ULN 43 (11) 8 (6) 51 (9) SGOT/AST greater than 5.0×ULN 19 (5) 5 (4) 24 (4) Lipase greater than 2×ULN 42 (10) 9 (6) 51 (9) Phosphorus (Low) less than 0.6 mmol/L 30 (7) 10 (7) 40 (7) Total Bilirubin greater than 3.0×ULN 3 (1) 4 (3) 7 (1) Additional Adverse Reactions From Multiple Clinical Trials
The following adverse reactions were reported in patients in clinical trials with BOSULIF (less than 10% of BOSULIF-treated patients). They represent an evaluation of the adverse reaction data from all 1272 patients with leukemia who received at least 1 dose of single-agent BOSULIF. These adverse reactions are presented by system organ class and are ranked by frequency. These adverse reactions are included based on clinical relevance and ranked in order of decreasing seriousness within each category.
Blood and Lymphatic System Disorders: less than 0.01% - Febrile neutropenia, Granulocytopenia
Cardiac Disorders: 1% and less than 10% - Pericardial effusion; 0.1% and less than 1% - Pericarditis
Ear and Labyrinth Disorders: 1% and less than 10% - Tinnitus
Vascular Disorders: 1% and less than 10% - Hypertension
Gastrointestinal Disorders: 1% and less than 10% - Gastritis; 0.1% and less than 1% - Pancreatitis (includes Pancreatitis, Pancreatitis acute), Gastrointestinal hemorrhage (includes Anal hemorrhage, Gastric hemorrhage, Gastrointestinal hemorrhage, Intestinal hemorrhage, Lower gastrointestinal hemorrhage, Rectal hemorrhage)
General Disorders and Administrative Site Conditions: 1% and less than 10% - Pain
Hepatobiliary Disorders: 1% and less than 10% - Hepatotoxicity (includes Hepatotoxicity, Hepatitis, Hepatitis toxic, Liver disorder), Hepatic function abnormal (includes Hepatic function abnormal, Liver function test abnormal, Transaminases increased); 0.1% and less than 1% - Liver injury (includes Liver injury, Drug-induced liver injury)
Immune System Disorders: 0.1% and less than 1% - Anaphylactic shock, Drug hypersensitivity
Infections and Infestations: 1% and less than 10% - pneumonia (includes pneumonia, atypical pneumonia), influenza, bronchitis
Investigations: 1% and less than 10% - Electrocardiogram QT prolonged (includes Electrocardiogram QT prolonged, Long QT syndrome), Blood bilirubin increased (includes Blood bilirubin increased, Hyperbilirubinaemia), Blood creatine phosphokinase increased, Amylase increased, GGT increased
Metabolism and Nutrition Disorders: 1% and less than 10% - Hypophosphatemia (includes Hypophosphatemia, Blood phosphorus decreased), Hyperkalemia (includes Hyperkalemia, Blood potassium increased), Dehydration
Musculoskeletal and Connective Tissue Disorders: 1% and less than 10% - Myalgia
Nervous System Disorders: 1% and less than 10% - Dysgeusia
Renal and Urinary Disorders: 1% and less than 10% - Acute kidney injury, Renal impairment, Acute renal failure, Renal failure
Respiratory, Thoracic and Mediastinal Disorders: 0.1% and less than 1% - Acute pulmonary edema, Respiratory failure, Pulmonary hypertension
Skin and Subcutaneous Disorders: 0.1% and less than 1% - Erythema multiforme
6.2 Post-Marketing Experience
The following additional adverse reactions have been identified during post-approval use of BOSULIF. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Blood and Lymphatic System Disorders: Thrombotic microangiopathy
Skin and Subcutaneous Tissue Disorders: Stevens-Johnson syndrome
-
7 DRUG INTERACTIONS
7.1 Effect of Other Drugs on BOSULIF
Strong or Moderate CYP3A Inhibitors
Concomitant use with a strong or moderate CYP3A inhibitor increased bosutinib Cmax and AUC compared to BOSULIF alone [see Clinical Pharmacology (12.3)] which may increase the risk of toxicities. Avoid the concomitant use of strong or moderate CYP3A inhibitors with BOSULIF.
Strong CYP3A Inducers
Concomitant use with a strong CYP3A inducer decreased bosutinib Cmax and AUC compared to BOSULIF alone [see Clinical Pharmacology (12.3)] which may reduce BOSULIF efficacy. Avoid the concomitant use of strong CYP3A inducers with BOSULIF.
Proton Pump Inhibitors (PPI)
Concomitant use with a PPI decreased bosutinib Cmax and AUC compared to BOSULIF alone [see Clinical Pharmacology (12.3)] which may reduce BOSULIF efficacy. As an alternative to PPIs, use short-acting antacids or H2 blockers and separate dosing by more than 2 hours from BOSULIF dosing.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Based on findings from animal studies and its mechanism of action, BOSULIF can cause fetal harm when administered to a pregnant woman [see Clinical Pharmacology (12.1)].
There are no available data in pregnant women to inform the drug-associated risk. In animal reproduction studies conducted in rats and rabbits, oral administration of bosutinib during organogenesis caused adverse developmental outcomes, including structural abnormalities, embryo-fetal mortality, and alterations to growth at maternal exposures (AUC) as low as 1.2 times the human exposure at the dose of 500 mg/day (see Data). Advise pregnant women of the potential risk to a fetus.
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies are 2–4% and 15–20%, respectively.
Data
Animal Data
In a rat fertility and early embryonic development study, bosutinib was administered orally to female rats for approximately 3 to 6 weeks, depending on day of mating (2 weeks prior to cohabitation with untreated breeder males until gestation day [GD] 7). Increased embryonic resorptions occurred at greater than or equal to 10 mg/kg/day of bosutinib (1.6 and 1.2 times the human exposure at the recommended doses of 400 or 500 mg/day, respectively), and decreased implantations and reduced number of viable embryos at 30 mg/kg/day of bosutinib (3.4 and 2.5 times the human exposure at the recommended doses of 400 or 500 mg/day, respectively).
In an embryo-fetal development study conducted in rabbits, bosutinib was administered orally to pregnant animals during the period of organogenesis at doses of 3, 10, and 30 mg/kg/day. At the maternally-toxic dose of 30 mg/kg/day of bosutinib, there were fetal anomalies (fused sternebrae, and 2 fetuses had various visceral observations), and an approximate 6% decrease in fetal body weight. The dose of 30 mg/kg/day resulted in exposures (AUC) approximately 5.1 and 3.8 times the human exposures at the recommended doses of 400 and 500 mg/day, respectively.
Fetal exposure to bosutinib-derived radioactivity during pregnancy was demonstrated in a placental-transfer study in pregnant rats. In a rat pre- and postnatal development study, bosutinib was administered orally to pregnant animals during the period of organogenesis through lactation day 20 at doses of 10, 30, and 70 mg/kg/day. Reduced number of pups born occurred at greater than or equal to 30 mg/kg/day bosutinib (3.4 and 2.5 times the human exposure at the recommended doses of 400 or 500 mg/day, respectively), and increased incidence of total litter loss and decreased growth of offspring after birth occurred at 70 mg/kg/day bosutinib (6.9 and 5.1 times the human exposure at the recommended doses of 400 or 500 mg/day, respectively).
8.2 Lactation
Risk Summary
No data are available regarding the presence of bosutinib or its metabolites in human milk or its effects on a breastfed child or on milk production. However, bosutinib is present in the milk of lactating rats. Because of the potential for serious adverse reactions in a nursing child, breastfeeding is not recommended during treatment with BOSULIF and for at least 2 weeks after the last dose.
8.3 Females and Males of Reproductive Potential
Pregnancy
Based on findings from animal studies, BOSULIF can cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)]. Females of reproductive potential should have a pregnancy test prior to starting treatment with BOSULIF.
Contraception
Females
Based on findings from animal studies, BOSULIF can cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)]. Advise females of reproductive potential to use effective contraception (methods that result in less than 1% pregnancy rates) during treatment with BOSULIF and for at least 2 weeks after the last dose.
Infertility
The risk of infertility in females or males of reproductive potential has not been studied in humans. Based on findings from animal studies, BOSULIF may cause reduced fertility in females and males of reproductive potential [see Nonclinical Toxicology (13.1)].
8.4 Pediatric Use
The safety and efficacy of BOSULIF in patients less than 18 years of age have not been established.
8.5 Geriatric Use
In the single-arm study in patients with CML who were resistant or intolerant to prior therapy of BOSULIF in patients with Ph+ CML, 20% were age 65 and over, 4% were 75 and over. No overall differences in safety or effectiveness were observed between these patients and younger patients, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
8.6 Renal Impairment
Reduce the BOSULIF starting dose in patients with moderate (creatinine clearance [CLcr] 30 to 50 mL/min, estimated by Cockcroft-Gault (C-G)) and severe (CLcr less than 30 mL/min, C-G) renal impairment at baseline. For patients who have declining renal function while on BOSULIF who cannot tolerate the starting dose, follow dose adjustment recommendations for toxicity [see Dosage and Administration (2.3, 2.5) and Clinical Pharmacology (12.3)]. BOSULIF has not been studied in patients undergoing hemodialysis.
8.7 Hepatic Impairment
Reduce the BOSULIF dosage in patients with hepatic impairment (Child-Pugh A, B, or C) [see Dosage and Administration (2.3, 2.5) and Clinical Pharmacology (12.3)].
- 10 OVERDOSAGE
-
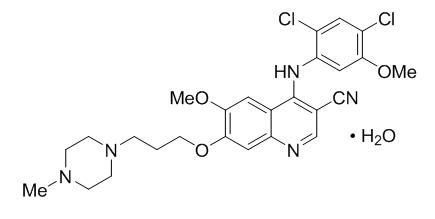
11 DESCRIPTION
Bosutinib is a kinase inhibitor. The chemical name for bosutinib monohydrate is 3-Quinolinecarbonitrile, 4-[(2,4-dichloro-5-methoxyphenyl)amino]-6-methoxy-7-[3-(4-methyl-1-piperazinyl) propoxy]-, hydrate (1:1). Its chemical formula is C26H29Cl2N5O3∙H2O (monohydrate); its molecular weight is 548.46 (monohydrate), equivalent to 530.46 (anhydrous). Bosutinib monohydrate has the following chemical structure:
Bosutinib monohydrate is a white to yellowish-tan powder. Bosutinib monohydrate has a pH dependent solubility across the physiological pH range. At or below pH 5, bosutinib monohydrate behaves as a highly soluble compound. Above pH 5, the solubility of bosutinib monohydrate reduces rapidly.
BOSULIF® (bosutinib) tablets are supplied for oral administration in 3 strengths: a 100 mg yellow, oval, biconvex, film-coated tablet debossed with "Pfizer" on one side and "100" on the other; a 400 mg orange, oval, biconvex, film-coated tablet debossed with "Pfizer" on one side and "400" on the other; and a 500 mg red, oval, biconvex, film-coated tablet debossed with "Pfizer" on one side and "500" on the other.
Each 100 mg BOSULIF tablet contains 103.40 mg of bosutinib monohydrate, equivalent to 100 mg of bosutinib; each 400 mg BOSULIF tablet contains 413.60 mg of bosutinib monohydrate, equivalent to 400 mg of bosutinib; each 500 mg BOSULIF tablet contains 516.98 mg of bosutinib monohydrate, equivalent to 500 mg of bosutinib. The following inactive ingredients are included in the tablets: microcrystalline cellulose, croscarmellose sodium, poloxamer, povidone, magnesium stearate, polyvinyl alcohol, titanium dioxide, polyethylene glycol, talc, and iron oxide yellow (for 100 mg, and 400 mg tablet) and iron oxide red (for 400 mg, and 500 mg tablet).
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Bosutinib is a TKI. Bosutinib inhibits the BCR-ABL kinase that promotes CML; it is also an inhibitor of Src-family kinases including Src, Lyn, and Hck. Bosutinib inhibited 16 of 18 imatinib-resistant forms of BCR-ABL kinase expressed in murine myeloid cell lines. Bosutinib did not inhibit the T315I and V299L mutant cells.
12.2 Pharmacodynamics
Based on the exposure response analyses for efficacy, a relationship between drug exposure and a greater likelihood of response was observed in clinical studies. Based on the exposure response analyses for safety, a relationship between drug exposure and a greater likelihood of safety events was observed in clinical studies.
12.3 Pharmacokinetics
The bosutinib pharmacokinetics following oral dosing was assessed with food, unless otherwise specified.
Bosutinib exhibits dose proportional increases in AUC and Cmax over the oral dose range of 200 to 800 mg (0.33 to 1.3 times the maximum approved recommended dosage of 600 mg). The mean (standard deviation [SD]) Cmax was 146 (20) ng/mL and the mean (SD) AUC was 2720 (442) ng∙h/mL following multiple oral doses of BOSULIF 400 mg in patients with CML; Cmax was 200 (12) ng/mL and AUC was 3650 (425) ng∙h/mL following multiple oral doses of BOSULIF 500 mg in patients with CML.
Absorption
Following administration of a single oral dose of BOSULIF 500 mg with food in patients with CML, the median (minimum, maximum) time-to-peak concentration (tmax) was 6.0 (6.0, 6.0) hours. The absolute bioavailability was 34% in healthy subjects.
Distribution
Following a single intravenous dose of bosutinib 120 mg (0.2 times the maximum approved recommended oral dosage of 600 mg) in healthy subjects, bosutinib had a mean (SD) volume of distribution of 2441 (796) L. The mean (SD) apparent volume of distribution after an oral dose of 500 mg of BOSULIF to patients with CML was 6080 (1230) L. Protein binding of bosutinib is 94% in vitro and 96% ex vivo, and is independent of concentration.
Elimination
Following a single intravenous dose of bosutinib 120 mg (0.2 times the maximum approved recommended oral dosage of 600 mg), the mean (SD) terminal phase elimination half-life (t½) was 35.5 (8.5) hours, and the mean (SD) clearance (Cl) was 63.6 (14.1) L/h. Following a single oral dose of BOSULIF in patients with CML, the mean (SD) t½ was 22.5 (1.7) hours, and the mean (SD) Cl was 189 (48) L/h.
Excretion
Following a single oral dose of [14C] radiolabeled bosutinib without food, 91.3% of the dose was recovered in feces and 3.3% of the dose recovered in urine.
Specific Populations
Patients with Renal Impairment
Following a single oral dose of BOSULIF 200 mg (0.33 times the maximum approved recommended dosage of 600 mg), bosutinib AUC increased 1.4-fold in subjects with moderate renal impairment (CLcr: 30 to 50 mL/min, estimated by Cockcroft-Gault (C-G)) and increased 1.6-fold in subjects with severe renal impairment (CLcr less than 30 mL/min) compared to subjects with normal renal function (CLcr > 80 mL/min, C-G). No clinically significant difference in the pharmacokinetics of bosutinib was observed in subjects with mild renal impairment (CLcr: 51 to 80 mL/min, C-G).
Patients with Hepatic Impairment
Following a single oral dose of BOSULIF 200 mg (0.33 times the maximum approved recommended dosage of 600 mg), bosutinib Cmax increased 2.4-fold, 2-fold, and 1.5-fold, and AUC increased 2.3-fold, 2-fold, and 1.9-fold in hepatic impairment Child-Pugh A, B, and C, respectively.
Drug Interaction Studies
Clinical Studies
The following interactions were evaluated in crossover studies of healthy subjects, unless otherwise specified.
Strong and Moderate CYP3A Inhibitors
A single oral dose of BOSULIF 100 mg (0.17 times the maximum approved recommended dosage) was administered alone or following multiple daily doses of 400 mg ketoconazole (a strong CYP3A inhibitor) without food. Ketoconazole increased bosutinib Cmax and AUC 5.2-fold and 8.6-fold, respectively.
A single oral dose of BOSULIF 500 mg was administered alone or in combination with 125 mg aprepitant (a moderate CYP3A inhibitor) with food. Aprepitant increased bosutinib Cmax 1.5-fold and AUC 2.0-fold.
Strong CYP3A Inducers
A single dose of BOSULIF 500 mg was administered alone or following multiple daily doses of 600 mg rifampin with food. Rifampin decreased bosutinib Cmax by 86% and AUC by 94%.
Proton Pump Inhibitors
BOSULIF displays pH-dependent aqueous solubility, in vitro. A single oral dose of BOSULIF 400 mg was administered alone or following multiple oral doses of lansoprazole 60 mg without food. Lansoprazole decreased bosutinib Cmax by 46% and AUC by 26%.
P-gp Substrates
A single oral dose of 500 mg BOSULIF was administered in combination with a single oral dose of 150 mg dabigatran etexilate mesylate (a P-glycoprotein (P-gp) substrate). No clinically significant difference in the pharmacokinetics of dabigatran was observed following bosutinib administration.
In Vitro Studies
Bosutinib Effect on Transporters
Bosutinib may have the potential to inhibit breast cancer resistance protein (BCRP) in the gastrointestinal tract but has a low potential to inhibit BCRP, systemically, or organic anion transporting polypeptide (OATP)1B1, OATP1B3, organic anion transporter (OAT)1, OAT3, organic cation transporter (OCT)1, and OCT2 at clinically relevant concentrations.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
A 2-year carcinogenicity study was conducted orally in rats at bosutinib doses up to 25 mg/kg/day in males and 15 mg/kg/day in females. The exposures achieved at the high dose were approximately 1.8 times (males) and 3.8 times (females) the human exposure at the recommended dose of 400 mg, and 1.4 times (males) and 2.8 times (females) the human exposure at the recommended dose of 500 mg. The study was negative for carcinogenic findings.
Bosutinib was not mutagenic or clastogenic in a battery of tests, including the bacteria reverse mutation assay (Ames Test), the in vitro assay using human peripheral blood lymphocytes and the micronucleus test in orally treated male mice.
In a rat fertility study, drug-treated males were mated with untreated females, or untreated males were mated with drug-treated females. Females were administered the drug from pre-mating through early embryonic development. The dose of 70 mg/kg/day of bosutinib resulted in reduced fertility in males as demonstrated by 16% reduction in the number of pregnancies. There were no lesions in the male reproductive organs at this dose. This dose of 70 mg/kg/day resulted in exposure (AUC) in male rats approximately 1.5 times and equal to the human exposure at the recommended doses of 400 and 500 mg/day, respectively. Fertility (number of pregnancies) was not affected when female rats were treated with bosutinib. However, there were increased embryonic resorptions at greater than or equal to 10 mg/kg/day of bosutinib (1.6 and 1.2 times the human exposure at the recommended doses of 400 and 500 mg/day, respectively), and decreased implantations and reduced number of viable embryos at 30 mg/kg/day of bosutinib (3.4 and 2.5 times the human exposure at the recommended doses of 400 or 500 mg/day, respectively).
-
14 CLINICAL STUDIES
14.1 Newly-Diagnosed CP Ph+ CML
The efficacy of BOSULIF in patients with newly-diagnosed chronic phase Ph+ CML was evaluated in the Bosutinib trial in First-line chrOnic myelogenous leukemia tREatment (BFORE) Trial: "A Multicenter Phase 3, Open-Label Study of Bosutinib Versus Imatinib in Adult Patients With Newly Diagnosed Chronic Phase Chronic Myelogenous Leukemia" [NCT02130557].
The BFORE Trial is a 2-arm, open-label, randomized, multicenter trial conducted to investigate the efficacy and safety of BOSULIF 400 mg once daily alone compared with imatinib 400 mg once daily alone in adult patients with newly-diagnosed CP Ph+ CML. The trial randomized 536 patients (268 in each arm) with Ph+ or Ph- newly-diagnosed CP CML (intent-to-treat [ITT] population) including 487 patients with Ph+ CML harboring b2a2 and/or b3a2 transcripts at baseline and baseline BCR-ABL copies >0 (modified intent-to-treat [mITT] population). Randomization was stratified by Sokal score and geographical region. All patients are being treated and/or followed for up to 5 years. Efficacy was evaluated in the mITT population. The major efficacy outcome measure was MMR at 12 months defined as ≤0.1% BCR-ABL ratio on international scale (corresponding to ≥3 log reduction from standardized baseline) with a minimum of 3000 ABL transcripts as assessed by the central laboratory. Additional efficacy outcomes included CCyR by 12 months, defined as the absence of Ph+ metaphases in chromosome banding analysis of ≥20 metaphases derived from bone marrow aspirate or MMR if an adequate cytogenetic assessment was unavailable.
In the mITT population in this study, 57% of patients were males, 77% were Caucasian, and 19% were 65 years or older. The median age was 53 years. After a minimum of 12 months of follow-up, 77.6% of the 246 bosutinib-treated patients and 72.4% of the 239 imatinib-treated patients were still receiving treatment. The median treatment duration was 14.3 months for BOSULIF and 13.8 months for imatinib.
The efficacy results from the BFORE trial are summarized in Table 8.
Table 8: Summary of Major Molecular Response (MMR) at Month 12 and Complete Cytogenetic Response (CCyR) by Month 12, by Treatment Group in the Modified Intent-to-Treat (mITT) Population Response Bosutinib
N=246
n (%)Imatinib
N=241
n (%)2-sided p-value Abbreviations: CCyR=complete cytogenetic response; CI=confidence interval; CMH=Cochran-Mantel-Haenszel; MMR=major molecular response; N/n=number of patients. - * derived from CMH test stratified by Geographical region and Sokal score at randomization.
Major Molecular Response at Month 12 MMR 116 (47.2) 89 (36.9) 0.0200* (95% CI) (40.9, 53.4) (30.8, 43.0) Complete Cytogenetic Response by Month 12 CCyR 190 (77.2) 160 (66.4) 0.0075* (95% CI) (72.0, 82.5) (60.4, 72.4) The MMR rate at Month 12 for all randomized patients (ITT population) was consistent with the mITT population (46.6% [95% CI: 40.7, 52.6] in the bosutinib treatment group and 36.2% [95% CI: 30.4, 41.9] in the imatinib treatment group; odds ratio of 1.57 [95% CI: 1.10, 2.22]). After a minimum of 12 months of follow-up, 5 bosutinib patients and 7 imatinib patients transformed to AP CML or BP CML while on treatment.
14.2 Imatinib-Resistant or -Intolerant Ph+ CP, AP, and BP CML
Study 200 (NCT00261846), a single-arm, open-label, multicenter study in patients with CML who were resistant or intolerant to prior therapy was conducted to evaluate the efficacy and safety of BOSULIF 500 mg once daily in patients with imatinib-resistant or -intolerant CML with separate cohorts for CP, AP, and BP disease previously treated with 1 prior TKI (imatinib) or more than 1 TKI (imatinib followed by dasatinib and/or nilotinib). The definition of imatinib resistance included (1) failure to achieve or maintain any hematologic improvement within 4 weeks; (2) failure to achieve a CHR by 3 months, cytogenetic response by 6 months or major cytogenetic response (MCyR) by 12 months; (3) progression of disease after a previous cytogenetic or hematologic response; or (4) presence of a genetic mutation in the BCR-ABL gene associated with imatinib resistance. Imatinib intolerance was defined as inability to tolerate imatinib due to toxicity, or progression on imatinib and inability to receive a higher dose due to toxicity. The definitions of resistance and intolerance to both dasatinib and nilotinib were similar to those for imatinib. The protocol was amended to exclude patients with a known history of the T315I mutation after 396 patients were enrolled in the trial.
The efficacy endpoints for patients with CP CML previously treated with 1 prior TKI (imatinib) were the rate of attaining MCyR by Week 24 and the duration of MCyR. The efficacy endpoints for patients with CP CML previously treated with both imatinib and at least 1 additional TKI were the cumulative rate of attaining MCyR by Week 24 and the duration of MCyR. The efficacy endpoints for patients with previously treated AP and BP CML were confirmed CHR and overall hematologic response (OHR).
The study enrolled 546 patients with CP, AP or BP CML. Of the total patient population 73% were imatinib resistant and 27% were imatinib intolerant. In this trial, 53% of patients were males, 65% were Caucasian, and 20% were 65 years old or older. Of the 546 treated patients, 506 were considered evaluable for cytogenetic or hematologic efficacy assessment. Patients were evaluable for efficacy if they had received at least 1 dose of BOSULIF and had a valid baseline efficacy assessment. Among evaluable patients, there were 262 patients with CP CML previously treated with 1 prior TKI (imatinib), 112 patients with CP CML previously treated with both imatinib and at least 1 additional TKI, and 132 patients with advanced phase CML previously treated with at least 1 TKI.
Median duration of BOSULIF treatment was 26 months in patients with CP CML previously treated with 1 TKI (imatinib), 9 months in patients with CP CML previously treated with imatinib and at least 1 additional TKI, 10 months in patients with AP CML previously treated with at least imatinib, and 3 months in patients with BP CML previously treated with at least imatinib.
The 24 week efficacy and MCyR at any time results are summarized in Table 9.
Table 9: Efficacy Results in Patients with Ph+ CP CML With Resistance to or Intolerance to Imatinib Prior Treatment With Imatinib Only
(N=262 evaluable)
n (%)Prior Treatment With Imatinib and Dasatinib or Nilotinib
(N=112 evaluable)
n (%)Abbreviations: CI=confidence interval; CML=chronic myelogenous leukemia; CP=chronic phase; MCyR=major cytogenetic response; N/n=number of patients; Ph+=Philadelphia chromosome positive. By Week 24 MCyR 105 (40.1) 29 (25.9) (95% CI) (34.1, 46.3) (18.1, 35.0) MCyR any time 156 (59.5) 45 (40.2) (53.3, 65.5) (31.0, 49.9) The long term follow-up data analysis was based on a minimum of 60 months for patients with CP CML treated with 1 prior TKI (imatinib) and a minimum of 48 months for patients with CP CML treated with imatinib and at least 1 additional TKI. For the 59.5% of patients with CP CML treated with 1 prior TKI (imatinib) who achieved a MCyR at any time, the median duration of MCyR was not reached. Among these patients, 65.4% and 42.9% had a MCyR lasting at least 18 and 54 months, respectively. For the 40.2% of patients with CP CML treated with imatinib and at least 1 additional TKI who achieved a MCyR at any time, the median duration of MCyR was not reached. Among these patients, 64.4% and 35.6% had a MCyR lasting at least 9 and 42 months, respectively. Of the 403 treated patients with CP CML, 20 patients had confirmed disease transformation to AP or BP while on treatment with BOSULIF.
The 48 week efficacy results in patients with accelerated and blast phases CML previously treated with at least imatinib are summarized in Table 10.
Table 10: Efficacy Results in Patients With Accelerated Phase and Blast Phase CML Previously Treated With at Least Imatinib AP CML
(N=72 evaluable)
n (%)BP CML
(N=60 evaluable)
n (%)Abbreviations: AP=accelerated phase; BP=blast phase; CHR=complete hematologic response; CI=confidence interval; CML=chronic myelogenous leukemia; CI=confidence interval, OHR=overall hematologic response, CHR=complete hematologic response, N/n=number of patients - * Overall hematologic response (OHR) = major hematologic response (complete hematologic response + no evidence of leukemia) or return to chronic phase (RCP). All responses were confirmed after 4 weeks. Complete hematologic response (CHR) for AP and BP CML: WBC less than or equal to institutional ULN, platelets greater than or equal to 100,000/mm3 and less than 450,000/mm3, absolute neutrophil count (ANC) greater than or equal to 1.0×109 /L, no blasts or promyelocytes in peripheral blood, less than 5% myelocytes + metamyelocytes in bone marrow, less than 20% basophils in peripheral blood, and no extramedullary involvement. No evidence of leukemia (NEL): Meets all other criteria for CHR except may have thrombocytopenia (platelets greater than or equal to 20,000/mm3 and less than 100,000/mm3) and/or neutropenia (ANC greater than or equal to 0.5×109 /L and less than 1.0×109 /L). Return to chronic phase (RCP) = disappearance of features defining accelerated or blast phases but still in chronic phase.
CHR* by Week 48 22 (30.6) 10 (16.7) (95% CI) (20.2, 42.5) (8.3, 28.5) OHR* by Week 48 41 (56.9) 17 (28.3) (95% CI) (44.7, 68.6) (17.5, 41.4) The long term follow-up data analysis was based on a minimum of 48 months for patients with AP CML and BP CML. Of the 79 treated patients with AP CML, 3 patients had confirmed disease transformation to BP while on BOSULIF treatment.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
BOSULIF (bosutinib) tablets are supplied for oral administration in 3 strengths: a 100 mg yellow, oval, biconvex, film-coated tablet debossed with "Pfizer" on one side and "100" on the other; a 400 mg orange, oval, biconvex, film coated tablet debossed with "Pfizer" on one side and "400" on the other; and a 500 mg red, oval, biconvex, film-coated tablet debossed with "Pfizer" on one side and "500" on the other. BOSULIF (bosutinib) tablets are available in the following packaging configurations (Table 11):
Table 11: Tablet Presentations BOSULIF Tablets Package Configuration Tablet Strength
(mg)NDC Tablet Description Abbreviation: NDC=National drug code. 120 tablets per bottle 100 mg 0069-0135-01 Yellow, oval, biconvex, film-coated tablets, debossed "Pfizer" on one side and "100" on the other. 30 tablets per bottle 400 mg 0069-0193-01 Orange, oval, biconvex, film-coated tablet debossed with "Pfizer" on one side and "400" on the other. 30 tablets per bottle 500 mg 0069-0136-01 Red, oval, biconvex, film-coated tablets, debossed "Pfizer" on one side and "500" on the other. -
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
- Dosage and Administration
Instruct patients to take BOSULIF exactly as prescribed, not to change their dose or to stop taking BOSULIF unless they are told to do so by their doctor. If patients miss a dose beyond 12 hours, they should be advised to take the next scheduled dose at its regular time. A double dose should not be taken to make up for any missed dose. Advise patients to take BOSULIF with food. Patients should be advised: "Do not crush, break, or cut tablet. Do not touch or handle crushed or broken tablets."
- Gastrointestinal Toxicity
Advise patients that they may experience diarrhea, nausea, vomiting, abdominal pain, or blood in their stools with BOSULIF and to seek medical attention promptly for these symptoms [see Warnings and Precautions (5.1)].
- Myelosuppression
Advise patients of the possibility of developing low blood cell counts and to immediately report fever, any suggestion of infection, or signs or symptoms suggestive of bleeding or easy bruising [see Warnings and Precautions (5.2)].
- Hepatic Toxicity
Advise patients of the possibility of developing liver function abnormalities and to immediately report jaundice [see Warnings and Precautions (5.3)].
- Cardiac Failure
Advise patients that cardiac failure and left ventricular dysfunction have been reported. Advise patients to seek immediate medical attention if any symptoms suggestive of cardiac failure occur, such as shortness of breath, weight gain, or fluid retention [see Warnings and Precautions (5.4)].
- Fluid Retention
Advise patients of the possibility of developing fluid retention (swelling, weight gain, or shortness of breath) and to seek medical attention promptly if these symptoms arise [see Warnings and Precautions (5.5)].
- Renal Toxicity
Advise patients of the possibility of developing renal problems and to immediately report frequent urination, polyuria or oliguria [see Warnings and Precautions (5.6)].
- Adverse Reactions
Advise patients that they may experience other adverse reactions such as respiratory tract infections, rash, fatigue, loss of appetite, headache, dizziness, back pain, arthralgia, or pruritus with BOSULIF and to seek medical attention if symptoms are significant. There is a possibility of anaphylactic shock [see Contraindications (4) and Adverse Reactions (6)].
- Embryo-Fetal Toxicity
Advise females to inform their healthcare provider if they are pregnant or become pregnant. Inform female patients of the risk to a fetus and potential loss of the pregnancy [see Use in Specific Populations (8.1)].
Advise females of reproductive potential, to use effective contraception during treatment and for at least 2 weeks after receiving the last dose of BOSULIF [see Warnings and Precautions (5.7) and Use in Specific Populations (8.1, 8.3)].
Advise lactating women not to breastfeed during treatment with BOSULIF and for at least 2 weeks after the last dose [see Use in Specific Populations (8.2)].
- Drug Interactions
Advise patients that BOSULIF and certain other medicines, including over the counter medications or herbal supplements (such as St. John's wort) can interact with each other and may alter the effects of BOSULIF [see Drug Interactions (7)].
- SPL UNCLASSIFIED SECTION
-
PATIENT PACKAGE INSERT
PATIENT INFORMATION
BOSULIF® (BAH-su-lif)
(bosutinib)
tabletsThis Patient Information has been approved by the U.S. Food and Drug Administration. Revised: October 2019 What is BOSULIF?
BOSULIF is a prescription medicine used to treat adults who have a certain type of leukemia called Philadelphia chromosome-positive chronic myelogenous leukemia (Ph+ CML) who are newly-diagnosed or who no longer benefit from or did not tolerate other treatment.
It is not known if BOSULIF is safe and effective in children less than 18 years of age.Do not take BOSULIF if you are allergic to bosutinib or any of the ingredients in BOSULIF. See the end of this leaflet for a complete list of ingredients of BOSULIF. Before taking BOSULIF, tell your doctor about all of your medical conditions, including if you: - have liver problems
- have heart problems
- have kidney problems
- are pregnant or plan to become pregnant. BOSULIF can harm your unborn baby. Females who are able to become pregnant should have a pregnancy test before starting treatment with BOSULIF. Tell your doctor right away if you become pregnant during treatment with BOSULIF.
- Females who are able to become pregnant should use effective birth control (contraception) during treatment with BOSULIF and for at least 2 weeks after the last dose. Talk to your doctor about birth control methods that may be right for you.
- are breastfeeding or plan to breastfeed. It is not known if BOSULIF passes into your breast milk or if it can harm your baby. Do not breastfeed during treatment with BOSULIF and for at least 2 weeks after the last dose.
Know the medicines you take. Keep a list of your medicines and show it to your doctor and pharmacist when you get a new medicine.How should I take BOSULIF? - Take BOSULIF exactly as prescribed by your doctor.
- Do not change your dose or stop taking BOSULIF without first talking with your doctor.
- Take BOSULIF with food.
- Swallow BOSULIF tablets whole. Do not crush, break, or cut BOSULIF tablets. Do not touch or handle crushed or broken BOSULIF tablets.
- If you take an antacid or H2 blocker medicine, take it at least 2 hours before or 2 hours after BOSULIF. If you take a Proton Pump Inhibitor (PPI) medicine, talk to your doctor or pharmacist.
- You should avoid grapefruit, grapefruit juice, and supplements that contain grapefruit extract during treatment with BOSULIF. Grapefruit products increase the amount of BOSULIF in your body.
- If you miss a dose of BOSULIF, take it as soon as you remember. If you miss a dose by more than 12 hours, skip that dose and take your next dose at your regular time. Do not take 2 doses at the same time.
- If you take too much BOSULIF, call your doctor or go to the nearest hospital emergency room right away.
What are the possible side effects of BOSULIF?
BOSULIF may cause serious side effects, including:- Stomach problems. BOSULIF may cause stomach (abdomen) pain, nausea, diarrhea, vomiting, or blood in your stools. Get medical help right away for any stomach problems.
- Low blood cell counts. BOSULIF may cause low platelet counts (thrombocytopenia), low red blood cell counts (anemia) and low white blood cell counts (neutropenia). Your doctor should do blood tests to check your blood cell counts regularly during your treatment with BOSULIF. Call your doctor right away if you have unexpected bleeding or bruising, blood in your urine or stools, fever, or any signs of an infection.
- Liver problems. BOSULIF may cause liver problems. Your doctor should do blood tests to check your liver function regularly during your treatment with BOSULIF. Call your doctor right away if your skin or the white part of your eyes turns yellow (jaundice) or you have dark "tea color" urine.
- Heart problems. BOSULIF may cause heart problems, including heart failure. Get medical help right away if you get shortness of breath, weight gain or swelling in your hands, ankles or feet.
- Your body may hold too much fluid (fluid retention). Fluid may build up in the lining of your lungs, the sac around your heart, or your stomach cavity. Get medical help right away if you get any of the following symptoms during your treatment with BOSULIF:
- shortness of breath and cough
- chest pain
- swelling in your hands, ankles, or feet
- swelling all over your body
- weight gain
-
Kidney problems. BOSULIF may cause kidney problems. Your doctor should do tests to check your kidney function when you start treatment with BOSULIF and during your treatment. Call your doctor right away if you get any of the following symptoms during your treatment with BOSULIF:
- you urinate more often than normal
- you urinate less often than normal
- you make a much larger amount of urine than normal
- you make a much smaller amount of urine than normal
- diarrhea
- nausea
- low platelet counts
- rash
- changes in liver function test
- stomach (abdomen) pain
The most common side effects of BOSULIF in people with CML who no longer benefit from or did not tolerate other treatment include: - diarrhea
- nausea
- stomach (abdomen) pain
- rash
- low platelet counts
- vomiting
- low red blood cell counts
- tiredness
- fever
- cough
- headache
- change in liver function test
- swelling
Tell your doctor or get medical help right away if you get respiratory tract infections, loss of appetite, headache, dizziness, back pain, joint pain, or itching while taking BOSULIF. These may be symptoms of a severe allergic reaction.
Your doctor may change your dose, temporarily stop, or permanently stop treatment with BOSULIF if you have certain side effects.
BOSULIF may cause fertility problems in females and males. This may affect your ability to have a child. Talk to your doctor if this is a concern for you.
Tell your doctor if you have any side effect that bothers you or that does not go away.
These are not all of the possible side effects of BOSULIF. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.How should I store BOSULIF? - Store BOSULIF between 68°F to 77°F (20°C to 25°C).
- Ask your doctor or pharmacist about the right way to throw away outdated or unused BOSULIF.
General information about the safe and effective use of BOSULIF.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use BOSULIF for a condition for which it is not prescribed. Do not give BOSULIF to other people even if they have the same symptoms you have. It may harm them. You can ask your doctor or pharmacist for information about BOSULIF that is written for health professionals.What are the ingredients in BOSULIF?
Active ingredient: bosutinib.
Inactive ingredients: microcrystalline cellulose, croscarmellose sodium, poloxamer, povidone, magnesium stearate, polyvinyl alcohol, titanium dioxide, polyethylene glycol, talc, and iron oxide yellow (for 100 mg and 400 mg tablets) and iron oxide red (for 400 mg and 500 mg tablets).
LAB-0639-10.0
For more information, go to www.Bosulif.com or www.pfizermedicalinformation.com or call 1-800-438-1985. -
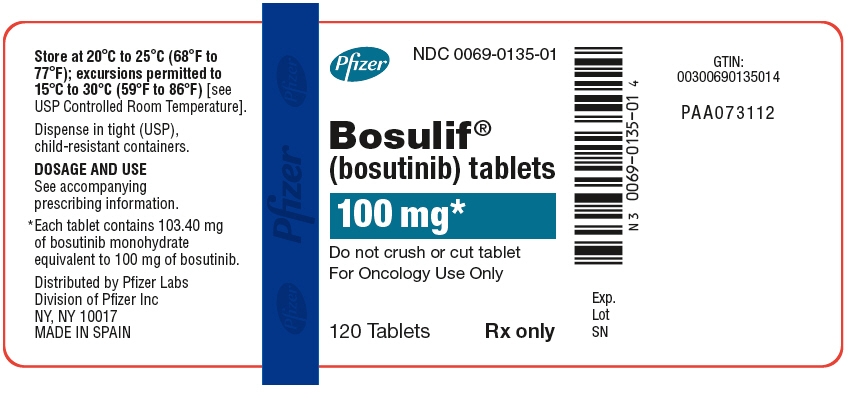
PRINCIPAL DISPLAY PANEL - 100 mg Bottle Label
Pfizer
NDC: 0069-0135-01
Bosulif®
(bosutinib) tablets100 mg*
Do not crush or cut tablet
For Oncology Use Only120 Tablets
Rx only
-
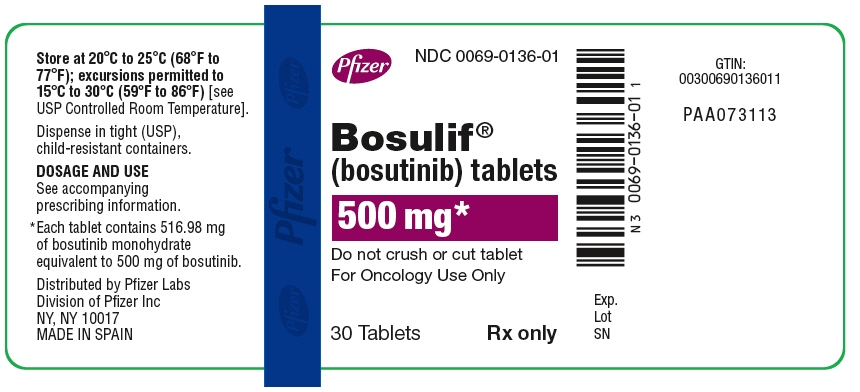
PRINCIPAL DISPLAY PANEL - 500 mg Bottle Label
Pfizer
NDC: 0069-0136-01
Bosulif®
(bosutinib) tablets500 mg*
Do not crush or cut tablet
For Oncology Use Only30 Tablets
Rx only
-
PRINCIPAL DISPLAY PANEL - 400 mg Tablet Bottle Label
Pfizer
NDC: 0069-0193-01
Bosulif®
(bosutinib) tablets400 mg*
Do not crush or cut tablet
For Oncology Use Only30 Tablets
Rx only

-
INGREDIENTS AND APPEARANCE
BOSULIF
bosutinib monohydrate tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0069-0135 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength BOSUTINIB MONOHYDRATE (UNII: 844ZJE6I55) (BOSUTINIB - UNII:5018V4AEZ0) BOSUTINIB MONOHYDRATE 100 mg Inactive Ingredients Ingredient Name Strength MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) POVIDONE K25 (UNII: K0KQV10C35) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL 3350 (UNII: G2M7P15E5P) TALC (UNII: 7SEV7J4R1U) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) POLOXAMER 188 (UNII: LQA7B6G8JG) Product Characteristics Color YELLOW Score no score Shape OVAL (biconvex) Size 11mm Flavor Imprint Code Pfizer;100 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0069-0135-01 120 in 1 BOTTLE; Type 0: Not a Combination Product 09/04/2012 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA203341 09/04/2012 BOSULIF
bosutinib monohydrate tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0069-0136 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength BOSUTINIB MONOHYDRATE (UNII: 844ZJE6I55) (BOSUTINIB - UNII:5018V4AEZ0) BOSUTINIB MONOHYDRATE 500 mg Inactive Ingredients Ingredient Name Strength MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) POVIDONE K25 (UNII: K0KQV10C35) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL 3350 (UNII: G2M7P15E5P) TALC (UNII: 7SEV7J4R1U) FERRIC OXIDE RED (UNII: 1K09F3G675) POLOXAMER 188 (UNII: LQA7B6G8JG) Product Characteristics Color RED Score no score Shape OVAL (biconvex) Size 18mm Flavor Imprint Code Pfizer;500 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0069-0136-01 30 in 1 BOTTLE; Type 0: Not a Combination Product 09/04/2012 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA203341 09/04/2012 BOSULIF
bosutinib monohydrate tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0069-0193 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength BOSUTINIB MONOHYDRATE (UNII: 844ZJE6I55) (BOSUTINIB - UNII:5018V4AEZ0) BOSUTINIB MONOHYDRATE 400 mg Inactive Ingredients Ingredient Name Strength MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) POVIDONE K25 (UNII: K0KQV10C35) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL 3350 (UNII: G2M7P15E5P) TALC (UNII: 7SEV7J4R1U) FERRIC OXIDE RED (UNII: 1K09F3G675) POLOXAMER 188 (UNII: LQA7B6G8JG) Product Characteristics Color ORANGE Score no score Shape OVAL (biconvex) Size 18mm Flavor Imprint Code Pfizer;400 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0069-0193-01 30 in 1 BOTTLE; Type 0: Not a Combination Product 12/18/2017 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA203341 12/18/2017 Labeler - Pfizer Laboratories Div Pfizer Inc (134489525) Establishment Name Address ID/FEI Business Operations Pfizer Manufacturing Deutschland GmbH 341970073 ANALYSIS(0069-0135, 0069-0136, 0069-0193) , LABEL(0069-0135, 0069-0136, 0069-0193) , MANUFACTURE(0069-0135, 0069-0136, 0069-0193) , PACK(0069-0135, 0069-0136, 0069-0193)
Trademark Results [BOSULIF]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 BOSULIF 85254857 4292873 Live/Registered |
Wyeth LLC 2011-03-01 |
 BOSULIF 77813503 3971238 Live/Registered |
WYETH LLC 2009-08-26 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.
