MEKINIST- trametinib tablet, film coated
Mekinist by
Drug Labeling and Warnings
Mekinist by is a Prescription medication manufactured, distributed, or labeled by Novartis Pharmaceuticals Corporation. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use MEKINIST safely and effectively. See full prescribing information for MEKINIST.
MEKINIST® (trametinib) tablets, for oral use
Initial U.S. Approval: 2013RECENT MAJOR CHANGES
INDICATIONS AND USAGE
MEKINIST is a kinase inhibitor indicated as a single agent for the treatment of BRAF-inhibitor treatment-naïve patients with unresectable or metastatic melanoma with BRAF V600E or V600K mutations as detected by an FDA-approved test. (1.1, 2.1)
MEKINIST is indicated, in combination with dabrafenib, for:
- the treatment of patients with unresectable or metastatic melanoma with BRAF V600E or V600K mutations as detected by an FDA-approved test. (1.1, 2.1)
- the adjuvant treatment of patients with melanoma with BRAF V600E or V600K mutations, as detected by an FDA-approved test, and involvement of lymph node(s), following complete resection. (1.2, 2.1)
- the treatment of patients with metastatic non-small cell lung cancer (NSCLC) with BRAF V600E mutation as detected by an FDA-approved test. (1.3, 2.1)
- the treatment of patients with locally advanced or metastatic anaplastic thyroid cancer (ATC) with BRAF V600E mutation and with no satisfactory locoregional treatment options. (1.4, 2.1)
DOSAGE AND ADMINISTRATION
- The recommended dosage of MEKINIST is 2 mg orally once daily. Take MEKINIST at least 1 hour before or at least 2 hours after a meal. (2)
DOSAGE FORMS AND STRENGTHS
Tablets: 0.5 mg, 2 mg (3)
CONTRAINDICATIONS
None. (4)
WARNINGS AND PRECAUTIONS
-
New Primary Malignancies, Cutaneous, and Non-cutaneous, can occur when MEKINIST is used with dabrafenib. Monitor patients for new malignancies prior to initiation of therapy, while on therapy, and following discontinuation of treatment. (5.1)
-
Hemorrhage: Major hemorrhagic events can occur. Monitor for signs and symptoms of bleeding. (5.2)
-
Colitis and Gastrointestinal Perforation: Colitis and gastrointestinal perforation can occur in patients receiving MEKINIST. (5.3)
-
Venous Thromboembolism: Deep vein thrombosis and pulmonary embolism (PE) can occur in patients receiving MEKINIST. (5.4, 2.7)
-
Cardiomyopathy: Assess left ventricular ejection fraction (LVEF) before treatment, after one month of treatment, then every 2 to 3 months thereafter. (5.5, 2.7)
-
Ocular Toxicities: Perform ophthalmologic evaluation for any visual disturbances. For Retinal Vein Occlusion (RVO), permanently discontinue MEKINIST. (5.6, 2.7)
-
Interstitial Lung Disease (ILD): Withhold MEKINIST for new or progressive unexplained pulmonary symptoms. Permanently discontinue MEKINIST for treatment-related ILD or pneumonitis. (5.7, 2.7)
-
Serious Febrile Reactions, can occur when MEKINIST is used with dabrafenib. (5.8, 2.7)
-
Serious Skin Toxicity: Monitor for skin toxicities and for secondary infections. Permanently discontinue MEKINIST for intolerable Grade 2, or Grade 3 or 4 rash not improving within 3 weeks despite interruption of MEKINIST. (5.9, 2.7)
-
Hyperglycemia: Monitor serum glucose levels in patients with preexisting diabetes or hyperglycemia. (5.10)
- Embryo-Fetal Toxicity: Can cause fetal harm. Advise females of reproductive potential of potential risk to a fetus and to use effective contraception. (5.12, 8.1, 8.3)
ADVERSE REACTIONS
Most common adverse reactions (≥ 20%) for MEKINIST as a single agent include rash, diarrhea, and lymphedema. (6.1)
Most common adverse reactions (≥ 20%) for MEKINIST with dabrafenib include:
- Unresectable or metastatic melanoma: pyrexia, nausea, rash, chills, diarrhea, vomiting, hypertension, and peripheral edema. (6.1)
- Adjuvant treatment of melanoma: pyrexia, fatigue, nausea, headache, rash, chills, diarrhea, vomiting, arthralgia, and myalgia. (6.1)
- NSCLC: pyrexia, fatigue, nausea, vomiting, diarrhea, dry skin, decreased appetite, edema, rash, chills, hemorrhage, cough, and dyspnea. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Novartis Pharmaceuticals Corporation at 1-888-669-6682 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 10/2019
- the treatment of patients with unresectable or metastatic melanoma with BRAF V600E or V600K mutations as detected by an FDA-approved test. (1.1, 2.1)
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 BRAF V600E or V600K Mutation-Positive Unresectable or Metastatic Melanoma
1.2 Adjuvant Treatment of BRAF V600E or V600K Mutation-Positive Melanoma
1.3 BRAF V600E Mutation-Positive Metastatic NSCLC
1.4 BRAF V600E Mutation-Positive Locally Advanced or Metastatic Anaplastic Thyroid Cancer
2 DOSAGE AND ADMINISTRATION
2.1 Patient Selection
2.2 Recommended Dosage for Unresectable or Metastatic Melanoma
2.3 Recommended Dosage for the Adjuvant Treatment of Melanoma
2.4 Recommended Dosage for NSCLC
2.5 Recommended Dosage for ATC
2.6 Administration
2.7 Dosage Modifications for Adverse Reactions
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 New Primary Malignancies
5.2 Hemorrhage
5.3 Colitis and Gastrointestinal Perforation
5.4 Venous Thromboembolism
5.5 Cardiomyopathy
5.6 Ocular Toxicities
5.7 Interstitial Lung Disease
5.8 Serious Febrile Reactions
5.9 Serious Skin Toxicity
5.10 Hyperglycemia
5.11 Risks Associated with Combination Treatment
5.12 Embryo-Fetal Toxicity
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 BRAF V600E or V600K Mutation-Positive Unresectable or Metastatic Melanoma
14.2 Adjuvant Treatment of BRAF V600E or V600K Mutation-Positive Melanoma
14.3 BRAF V600E Mutation-Positive Metastatic Non-Small Cell Lung Cancer
14.4 BRAF V600E Mutation-Positive Locally Advanced or Metastatic Anaplastic Thyroid Cancer
14.5 Lack of Clinical Activity in Metastatic Melanoma Following BRAF-Inhibitor Therapy
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1
INDICATIONS AND USAGE
1.1 BRAF V600E or V600K Mutation-Positive Unresectable or Metastatic Melanoma
MEKINIST® is indicated, as a single agent in BRAF-inhibitor treatment-naïve patients or in combination with dabrafenib, for the treatment of patients with unresectable or metastatic melanoma with BRAF V600E or V600K mutations, as detected by an FDA-approved test [see Dosage and Administration (2.1)].
1.2 Adjuvant Treatment of BRAF V600E or V600K Mutation-Positive Melanoma
MEKINIST is indicated, in combination with dabrafenib, for the adjuvant treatment of patients with melanoma with BRAF V600E or V600K mutations as detected by an FDA-approved test, and involvement of lymph node(s), following complete resection [see Dosage and Administration (2.1)].
1.3 BRAF V600E Mutation-Positive Metastatic NSCLC
MEKINIST is indicated, in combination with dabrafenib, for the treatment of patients with metastatic non-small cell lung cancer (NSCLC) with BRAF V600E mutation as detected by an FDA-approved test [see Dosage and Administration (2.1)].
1.4 BRAF V600E Mutation-Positive Locally Advanced or Metastatic Anaplastic Thyroid Cancer
MEKINIST is indicated, in combination with dabrafenib, for the treatment of patients with locally advanced or metastatic anaplastic thyroid cancer (ATC) with BRAF V600E mutation and with no satisfactory locoregional treatment options [see Dosage and Administration (2.1)].
-
2
DOSAGE AND ADMINISTRATION
2.1 Patient Selection
Melanoma
- Confirm the presence of BRAF V600E or V600K mutation in tumor specimens prior to initiation of treatment with MEKINIST as a single agent or in combination with dabrafenib [see Clinical Studies (14.1, 14.2)].
- Information on FDA-approved tests for the detection of BRAF V600 mutations in melanoma is available at: http://www.fda.gov/CompanionDiagnostics.
NSCLC
- Confirm the presence of BRAF V600E mutation in tumor specimens prior to initiation of treatment with MEKINIST and dabrafenib [see Clinical Studies (14.3)].
- Information on FDA-approved tests for the detection of BRAF V600E mutations in NSCLC is available at: http://www.fda.gov/CompanionDiagnostics.
ATC
- Confirm the presence of BRAF V600E mutation in tumor specimens prior to initiation of treatment with MEKINIST and dabrafenib [see Clinical Studies (14.4)]. An FDA-approved test for the detection of BRAF V600E mutation in ATC is not currently available.
2.2 Recommended Dosage for Unresectable or Metastatic Melanoma
The recommended dosage of MEKINIST is 2 mg orally taken once daily, as a single agent or in combination with dabrafenib, until disease progression or unacceptable toxicity. Refer to the dabrafenib prescribing information for recommended dabrafenib dosing information.
2.3 Recommended Dosage for the Adjuvant Treatment of Melanoma
The recommended dosage of MEKINIST is 2 mg orally taken once daily in combination with dabrafenib until disease recurrence or unacceptable toxicity for up to 1 year. Refer to the dabrafenib prescribing information for recommended dabrafenib dosing information.
2.4 Recommended Dosage for NSCLC
The recommended dosage of MEKINIST is 2 mg orally taken once daily in combination with dabrafenib until disease recurrence or unacceptable toxicity. Refer to the dabrafenib prescribing information for recommended dabrafenib dosing information.
2.5 Recommended Dosage for ATC
The recommended dosage of MEKINIST is 2 mg orally taken once daily in combination with dabrafenib until disease recurrence or unacceptable toxicity. Refer to the dabrafenib prescribing information for recommended dabrafenib dosing information.
2.6 Administration
- Take MEKINIST doses approximately 24 hours apart.
- Take MEKINIST at least 1 hour before or 2 hours after a meal [see Clinical Pharmacology (12.3)].
- Do not take a missed dose of MEKINIST within 12 hours of the next dose of MEKINIST.
2.7 Dosage Modifications for Adverse Reactions
Dose reductions for adverse reactions associated with MEKINIST are presented in Table 1.
Table 1. Recommended Dose Reductions for MEKINIST for Adverse Reactions Action Recommended Dose First Dose Reduction 1.5 mg orally once daily Second Dose Reduction 1 mg orally once daily Subsequent Modification Permanently discontinue if unable to tolerate MEKINIST 1 mg orally once daily Dosage modifications for adverse reactions associated with MEKINIST are presented in Table 2.
Table 2. Recommended Dosage Modifications for MEKINIST for Adverse Reactions aNational Cancer Institute Common Terminology Criteria for Adverse Events (NCI CTCAE) version 4.0.
bSee Table 1 for recommended dose reductions of MEKINIST.
cDose modifications are not recommended for MEKINIST when administered with dabrafenib for the following adverse reactions of dabrafenib: non-cutaneous malignancies and uveitis. Dose modification of MEKINIST is not required for new primary cutaneous malignancies.Severity of Adverse Reactiona Dosage Modification for MEKINISTb Venous Thromboembolism [see Warnings and Precautions (5.4)] - Uncomplicated deep venous thrombosis (DVT) or pulmonary embolism (PE)
Withhold MEKINIST for up to 3 weeks.
- If improved to Grade 0-1, resume MEKINIST at lower dose.
- If not improved, permanently discontinue MEKINIST.
- Life threatening PE
Permanently discontinue MEKINIST. Cardiomyopathy [see Warnings and Precautions (5.5)] - Asymptomatic, absolute decrease in left ventricular ejection fraction (LVEF) of 10% or greater from baseline and is below institutional lower limit of normal (LLN) from pretreatment value
Withhold MEKINIST for up to 4 weeks. - If improved to normal LVEF value, resume MEKINIST at lower dose.
- If not improved to normal LVEF value, permanently discontinue MEKINIST.
- Symptomatic cardiomyopathy
- Absolute decrease in LVEF of greater than 20% from baseline that is below LLN
Permanently discontinue MEKINIST. Ocular Toxicities [see Warnings and Precautions (5.6)] - Retinal pigment epithelial detachments (RPED)
Withhold MEKINIST for up to 3 weeks. - If improved, resume MEKINIST at same or lower dose.
- If not improved, permanently discontinue MEKINIST or resume MEKINIST at lower dose.
- Retinal vein occlusion (RVO)
Permanently discontinue MEKINIST.
Pulmonary [see Warnings and Precautions (5.7)] - Interstitial lung disease (ILD)/pneumonitis
Permanently discontinue MEKINIST. Febrile Reactions [see Warnings and Precautions (5.8)] - Fever higher than 104°F
- Fever complicated by rigors, hypotension, dehydration, or renal failure
Withhold MEKINIST until fever resolves, then resume MEKINIST at same or lower dose. Skin Toxicity [see Warnings and Precautions (5.9)] - Intolerable Grade 2
- Grade 3 or 4
Withhold MEKINIST for up to 3 weeks. - If improved, resume MEKINIST at lower dose.
- If not improved, permanently discontinue.
Other Adverse Reactionsc, including Hemorrhage [see Warnings and Precautions (5.2)] - Intolerable Grade 2
- Any Grade 3
Withhold MEKINIST - If improved to Grade 0-1, resume at lower dose.
- If not improved, permanently discontinue.
- First occurrence of any Grade 4
- Withhold MEKINIST until improves to Grade 0-1, then resume at lower dose.
- Permanently discontinue MEKINIST.
- Recurrent Grade 4
Permanently discontinue MEKINIST. Refer to the dabrafenib prescribing information for dose modifications for adverse reactions associated with dabrafenib.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5
WARNINGS AND PRECAUTIONS
5.1 New Primary Malignancies
Cutaneous Malignancies
In the COMBI-d study in patients with unresectable or metastatic melanoma, the incidence of basal-cell carcinoma (BCC) in patients receiving MEKINIST and dabrafenib was 3.3%. Among the 7 patients receiving MEKINIST with dabrafenib who developed BCC, 2 experienced more than one occurrence (range: 1 to 3). Cutaneous squamous cell carcinomas and keratoacanthoma (cuSCC) and new primary melanoma occurred in 3% and 0.5% of patients receiving MEKINIST and dabrafenib, respectively.
In the COMBI-AD study in the adjuvant treatment of melanoma, cuSCC and new primary melanoma occurred in 1% and < 1% of patients receiving MEKINIST plus dabrafenib, respectively.
In Study BRF113928 in patients with NSCLC, cuSCC occurred in 3.2% of patients receiving MEKINIST plus dabrafenib.
Perform dermatologic evaluations prior to initiation of MEKINIST when used with dabrafenib, every 2 months while on therapy, and for up to 6 months following discontinuation of the combination.
Non-Cutaneous Malignancies
Based on its mechanism of action, dabrafenib may promote growth and development of malignancies with activation of RAS through mutation or other mechanisms; refer to the Prescribing Information for dabrafenib. In the COMBI-d, COMBI-AD, and BRF113928 studies, non-cutaneous malignancies occurred in 1.4%, 1%, and 1.1% of patients receiving MEKINIST plus dabrafenib, respectively.
Monitor patients receiving MEKINIST and dabrafenib closely for signs or symptoms of non-cutaneous malignancies. No dose modification is required for MEKINIST in patients who develop non-cutaneous malignancies.
5.2 Hemorrhage
Hemorrhages, including major hemorrhages defined as symptomatic bleeding in a critical area or organ, can occur with MEKINIST.
In the COMBI-d study, the incidence of hemorrhagic events in patients receiving MEKINIST and dabrafenib was 19%. Gastrointestinal hemorrhage occurred in 6% of patients receiving MEKINIST in combination with dabrafenib. In the COMBI-d study, 1.4% of patients receiving MEKINIST and dabrafenib developed fatal intracranial hemorrhage. No fatal hemorrhagic events were observed in the COMBI-AD study. In Study BRF113928, fatal hemorrhagic events occurred in 2.2% of patients receiving MEKINIST with dabrafenib; these events were retroperitoneal hemorrhage and subarachnoid hemorrhage.
Permanently discontinue MEKINIST for all Grade 4 hemorrhagic events and for any Grade 3 hemorrhagic events that do not improve. Withhold MEKINIST for Grade 3 hemorrhagic events; if improved, resume at the next lower dose level.
5.3 Colitis and Gastrointestinal Perforation
Colitis and gastrointestinal perforation, including fatal outcomes, have been reported in patients taking MEKINIST as a single-agent and when administered with dabrafenib. Across clinical trials of MEKINIST, colitis occurred in 0.6% of patients and gastrointestinal perforation occurred in 0.3% of patients.
Monitor patients closely for colitis and gastrointestinal perforations.
5.4 Venous Thromboembolism
In the COMBI-d study, deep venous thrombosis (DVT) and pulmonary embolism (PE) occurred in 2.8% of patients receiving MEKINIST and dabrafenib. In the COMBI-AD study, DVT and PE occurred in 2% of patients receiving MEKINIST and dabrafenib. In Study BRF113928, DVT and PE occurred in 4.3% of patients receiving MEKINIST and dabrafenib.
Advise patients to immediately seek medical care if they develop symptoms of DVT or PE, such as shortness of breath, chest pain, or arm or leg swelling. Permanently discontinue MEKINIST for life-threatening PE. Withhold MEKINIST for uncomplicated DVT and PE for up to 3 weeks; if improved, MEKINIST may be resumed at a lower dose level [see Dosage and Administration (2.7)].
5.5 Cardiomyopathy
Cardiomyopathy, including cardiac failure, can occur with MEKINIST.
In the METRIC study in patients with unresectable or metastatic melanoma, cardiomyopathy [defined as cardiac failure, left ventricular dysfunction, or decreased left ventricular ejection fraction (LVEF)] occurred in 7% of patients receiving MEKINIST; no chemotherapy-treated patient developed cardiomyopathy. Four percent of patients required discontinuation and/or dose reduction of MEKINIST. Cardiomyopathy resolved in 10 of 14 patients.
Across clinical trials of MEKINIST as a single agent, 11% of patients developed evidence of cardiomyopathy [decrease in LVEF below institutional lower limit of normal (LLN) with an absolute decrease in LVEF ≥ 10% below baseline] and 5% demonstrated a decrease in LVEF below institutional LLN with an absolute decrease in LVEF of ≥ 20% below baseline.
In the COMBI-d study, evidence of cardiomyopathy (defined as decrease in LVEF below the institutional LLN with an absolute decrease in LVEF ≥ 10% below baseline) occurred in 6% of patients receiving MEKINIST and dabrafenib and resulted in dose interruption (4.4%), dose reduction (2.4%), and permanent discontinuation (1.5%) of MEKINIST. Cardiomyopathy resolved in 10 of 12 patients receiving MEKINIST and dabrafenib.
In the COMBI-AD study, cardiomyopathy (defined as a decrease in LVEF below the institutional LLN with an absolute decrease in LVEF > 10% below screening) occurred in 3% of patients receiving MEKINIST with dabrafenib and resulted in discontinuation, dose reduction, and dose interruption of drug in 0.2%, 1.6%, and 2.1% of patients, respectively. Cardiomyopathy resolved in 12 of 14 patients receiving MEKINIST with dabrafenib.
In Study BRF113928, cardiomyopathy (defined as a decrease in LVEF below the institutional LLN with an absolute decrease in LVEF > 10% below baseline) occurred in 9% of patients receiving MEKINIST with dabrafenib and resulted in dose interruption and permanent discontinuation of MEKINIST in 5% and 2.2% of patients, respectively. Cardiomyopathy resolved in 4 of 8 patients receiving MEKINIST and dabrafenib.
Assess LVEF by echocardiogram or multi-gated acquisition (MUGA) scan before initiation of MEKINIST as a single agent or with dabrafenib, one month after initiation, and then at 2- to 3-month intervals while on treatment. For an asymptomatic absolute decrease in LVEF of 10% or greater from baseline that is below the LLN, withhold MEKINIST for up to 4 weeks. If improved to normal LVEF value, resume at a lower dose. If no improvement to normal LVEF value within 4 weeks, permanently discontinue MEKINIST. For symptomatic cardiomyopathy or an absolute decrease in LVEF of greater than 20% from baseline that is below LLN, permanently discontinue MEKINIST [see Dosage and Administration (2.7)].
5.6 Ocular Toxicities
Retinal Vein Occlusion
Across clinical trials with MEKINIST, the incidence of retinal vein occlusion (RVO) was 0.2%. RVO may lead to macular edema, decreased visual function, neovascularization, and glaucoma.
Urgently (within 24 hours) perform ophthalmological evaluation for patient-reported loss of vision or other visual disturbances. Permanently discontinue MEKINIST in patients with documented RVO [see Dosage and Administration (2.7)].
Retinal Pigment Epithelial Detachment
Retinal pigment epithelial detachment (RPED) can occur with MEKINIST. Retinal detachments may be bilateral and multifocal, occurring in the central macular region of the retina or elsewhere in the retina. In melanoma and NSCLC trials, routine monitoring of patients to detect asymptomatic RPED was not conducted; therefore, the true incidence of this finding is unknown.
Perform ophthalmological evaluation periodically and at any time a patient reports visual disturbances. Withhold MEKINIST if RPED is diagnosed. If resolution of the RPED is documented on repeat ophthalmological evaluation within 3 weeks, resume MEKINIST at same or reduced dose. If no improvement after 3 weeks, resume at reduced dose or permanently discontinue MEKINIST [see Dosage and Administration (2.7)].
5.7 Interstitial Lung Disease
In clinical trials of single-agent MEKINIST, interstitial lung disease (ILD) or pneumonitis occurred in 2% of patients. In the METRIC study, 2.4% of patients treated with MEKINIST developed ILD or pneumonitis; all five patients required hospitalization. In the COMBI-d, COMBI-AD, and BRF113928 studies, 1.0%, < 1%, and 2.2% of patients receiving MEKINIST and dabrafenib developed pneumonitis, respectively.
Withhold MEKINIST in patients presenting with new or progressive pulmonary symptoms and findings including cough, dyspnea, hypoxia, pleural effusion, or infiltrates, pending clinical investigations. Permanently discontinue MEKINIST for patients diagnosed with treatment-related ILD or pneumonitis [see Dosage and Administration (2.7)].
5.8 Serious Febrile Reactions
Serious febrile reactions and fever of any severity accompanied by hypotension, rigors or chills, dehydration, or renal failure, can occur when MEKINIST is administered with dabrafenib.
Fever (serious and non-serious) occurred in 57% of patients with unresectable or metastatic melanoma receiving MEKINIST and dabrafenib. Approximately one-half of the patients who received MEKINIST and dabrafenib and experienced pyrexia had three or more discrete episodes.
Across clinical trials of MEKINIST administered with dabrafenib in patients with unresectable or metastatic melanoma, serious febrile reactions or fever of any severity complicated by severe rigors/chills, hypotension, dehydration, renal failure, or syncope, occurred in 17% of patients receiving MEKINIST and dabrafenib. Fever was complicated by severe chills/rigors in 0.4%, dehydration in 1.8%, renal failure in 0.5%, and syncope in 0.7% of patients.
Withhold MEKINIST for fever higher than 104ºF or fever accompanied by hypotension, rigors or chills, dehydration, or renal failure, and evaluate for signs and symptoms of infection. Monitor serum creatinine and other evidence of renal function during and following severe pyrexia. Upon resolution, resume at same or lower dose [see Dosage and Administration (2.7)]. Administer antipyretics as secondary prophylaxis when resuming MEKINIST if patient had a prior episode of severe febrile reaction or fever associated with complications. Administer corticosteroids (e.g., prednisone 10 mg daily) for at least 5 days for second or subsequent pyrexia if temperature does not return to baseline within 3 days of onset of pyrexia, or for pyrexia associated with complications such as dehydration, hypotension renal failure, or severe chills/rigors, and there is no evidence of active infection.
5.9 Serious Skin Toxicity
In the METRIC study, the overall incidence of any skin toxicity, the most frequent of which were rash, dermatitis acneiform rash, palmar-plantar erythrodysesthesia syndrome, and erythema, was 87% in patients receiving MEKINIST. Severe skin toxicity occurred in 12% of patients treated with MEKINIST. Skin toxicity requiring hospitalization occurred in 6% of patients treated with MEKINIST, most frequently for secondary infections of the skin requiring intravenous antibiotics or severe skin toxicity without secondary infection. Reductions in the dose of MEKINIST were required in 12% and permanent discontinuation of MEKINIST was required in 1% of patients with skin toxicity.
In the COMBI-d study, the overall incidence of any skin toxicity was 55% for patients receiving MEKINIST and dabrafenib. No serious or severe cases of skin toxicity occurred in patients treated with MEKINIST and dabrafenib. Reductions in the dose of MEKINIST were required in 5% of patients receiving MEKINIST and dabrafenib and no patients required permanent discontinuation of MEKINIST for skin toxicity.
Across clinical trials of MEKINIST administered with dabrafenib in patients with unresectable or metastatic melanoma, serious skin toxicity occurred in 0.7% of patients.
Withhold MEKINIST for intolerable or severe skin toxicity. Resume MEKINIST at a lower dose in patients with improvement or recovery from skin toxicity within 3 weeks. Permanently discontinue MEKINIST if skin toxicity has not improved in 3 weeks [see Dosage and Administration (2.7)].
5.10 Hyperglycemia
In the COMBI-d study, 27% of patients with a history of diabetes who received MEKINIST and dabrafenib required more intensive hypoglycemic therapy. Grade 3 and Grade 4 hyperglycemia based on laboratory values occurred in 5% and 0.5% of patients receiving MEKINIST and dabrafenib, respectively.
Monitor serum glucose levels upon initiation and as clinically appropriate when MEKINIST is administered with dabrafenib in patients with pre-existing diabetes or hyperglycemia. Initiate or optimize anti-hyperglycemic medications as clinically indicated.
5.11 Risks Associated with Combination Treatment
MEKINIST is indicated for use in combination with dabrafenib. Review the Prescribing Information for dabrafenib for information on the serious risks of dabrafenib prior to initiation of MEKINIST with dabrafenib.
5.12 Embryo-Fetal Toxicity
Based on findings from animal studies and its mechanism of action, MEKINIST can cause fetal harm when administered to a pregnant woman. Trametinib was embryotoxic and abortifacient in rabbits at doses greater than or equal to those resulting in exposures approximately 0.3 times the human exposure at the recommended clinical dose. Advise pregnant women of the potential risk to a fetus. Advise female patients of reproductive potential to use effective contraception during treatment with MEKINIST and for 4 months after treatment [see Use in Specific Populations (8.1, 8.3)].
-
6
ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling:
- New Primary Malignancies [see Warnings and Precautions (5.1)]
- Hemorrhage [see Warnings and Precautions (5.2)]
- Colitis and Gastrointestinal Perforation [see Warnings and Precautions (5.3)]
- Venous Thromboembolism [see Warnings and Precautions (5.4)]
- Cardiomyopathy [see Warnings and Precautions (5.5)]
- Ocular Toxicities [see Warnings and Precautions (5.6)]
- Interstitial Lung Disease [see Warnings and Precautions (5.7)]
- Serious Febrile Reactions [see Warnings and Precautions (5.8)]
- Serious Skin Toxicity [see Warnings and Precautions (5.9)]
- Hyperglycemia [see Warnings and Precautions (5.10)]
There are additional adverse reactions associated with dabrafenib. Refer to the dabrafenib prescribing information for additional information.
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The data described in the Warnings and Precautions section reflect exposure to MEKINIST administered as a single agent in 329 patients with various solid tumors and exposure to MEKINIST administered with dabrafenib in 559 patients with unresectable or metastatic melanoma and 93 patients with NSCLC. MEKINIST as a single agent was evaluated in 329 patients including 107 (33%) exposed for ≥ 6 months and 30 (9%) exposed for ≥ one year. MEKINIST as a single agent was studied in open-label, single-arm trials (N = 118) and in an open-label, randomized, active-controlled trial (N = 211; the METRIC study). The median age was 54 years, 60% were male, > 99% were white, and all patients had unresectable or metastatic melanoma. All patients received 2 mg once-daily doses of MEKINIST.
Unresectable or Metastatic BRAF V600E or V600K Mutation-Positive Melanoma
MEKINIST as a Single Agent
The safety of MEKINIST was evaluated in the METRIC study, a randomized, open-label trial of patients with BRAF V600E or V600K mutation-positive unresectable or metastatic melanoma receiving MEKINIST (N = 211) 2 mg orally once daily or chemotherapy (N = 99) (either dacarbazine 1000 mg/m2 every 3 weeks or paclitaxel 175 mg/m2 every 3 weeks) [see Clinical Studies (14.1)]. Patients with abnormal LVEF, history of acute coronary syndrome within 6 months, or current evidence of Class II or greater congestive heart failure (New York Heart Association) were excluded. The median duration of treatment with MEKINIST was 4.3 months.
In this study, 9% of patients receiving MEKINIST experienced adverse reactions resulting in permanent discontinuation of trial medication. The most frequent adverse reactions resulting in permanent discontinuation of MEKINIST were decreased LVEF, pneumonitis, renal failure, diarrhea, and rash. Adverse reactions led to dose reductions in 27% of patients treated with MEKINIST. Rash and decreased LVEF were the most frequent reasons cited for dose reductions of MEKINIST. Tables 3 and 4 present adverse reactions and laboratory abnormalities, respectively, of MEKINIST as a single agent in the METRIC study.
Table 3. Select Adverse Reactions Occurring in ≥ 10% of Patients Receiving MEKINIST and at a Higher Incidence (≥ 5%) Than in the Chemotherapy Arm or ≥ 2% (Grades 3 or 4) Adverse Reactions in METRIC aNational Cancer Institute Common Terminology Criteria for Adverse Events, version 4.0.
bGrade 4 adverse reactions limited to rash (n = 1) in trametinib arm and diarrhea (n = 1) in chemotherapy arm.
cIncludes stomatitis, aphthous stomatitis, mouth ulceration, and mucosal inflammation.
dIncludes abdominal pain, lower abdominal pain, upper abdominal pain, and abdominal tenderness.
eIncludes lymphedema, edema, and peripheral edema.
fIncludes epistaxis, gingival bleeding, hematochezia, rectal hemorrhage, melena, vaginal hemorrhage, hemorrhoidal hemorrhage, hematuria, and conjunctival hemorrhage.Adverse Reactions MEKINIST Chemotherapy N = 211 N = 99 All
GradesaGrades
3 and 4bAll
GradesaGrades
3 and 4bSkin and subcutaneous tissue Rash 57 8 10 0 Acneiform dermatitis 19 < 1 1 0 Dry skin 11 0 0 0 Pruritus 10 2 1 0 Paronychia 10 0 1 0 Gastrointestinal Diarrhea 43 0 16 2 Stomatitisc 15 2 2 0 Abdominal paind 13 1 5 1 Vascular Lymphedemae 32 1 4 0 Hypertension 15 12 7 3 Hemorrhagef 13 < 1 0 0 Other clinically important adverse reactions observed in ≤ 10% of patients (N = 329) receiving MEKINIST were:
Cardiac: Bradycardia
Gastrointestinal: Dry mouth
Infections: Folliculitis, rash pustular, cellulitis
Musculoskeletal and Connective Tissue: Rhabdomyolysis
Nervous System: Dizziness, dysgeusia
Ocular: Blurred vision, dry eye
Table 4. Laboratory Abnormalities Occurring at a Higher Incidence in Patients Treated With MEKINIST in the METRIC Study [Between-arm Difference of ≥ 5% (All Grades) or ≥ 2% (Grades 3 or 4)a] aOnly Grade 3 adverse reactions were reported in either treatment arm. Laboratory Abnormality MEKINIST Chemotherapy N = 211 N = 99 All
GradesGrades
3 and 4All
GradesGrades
3 and 4Increased aspartate aminotransferase (AST) 60 2 16 1 Hypoalbuminemia 42 2 23 1 Increased alanine aminotransferase (ALT) 39 3 20 3 Anemia 38 2 26 3 Increased alkaline phosphatase 24 2 18 3 MEKINIST with Dabrafenib
The safety of MEKINIST, administered with dabrafenib, was evaluated in 559 patients with previously untreated, unresectable or metastatic, BRAF V600 mutation-positive melanoma who received MEKINIST in two trials, the COMBI-d study (n = 209), a multicenter, double-blind, randomized (1:1), active-controlled trial and the COMBI-v study (n = 350), a multicenter, open-label, randomized (1:1), active-controlled trial. In both trials, patients received MEKINIST 2 mg orally once daily and dabrafenib 150 mg orally twice daily until disease progression or unacceptable toxicity. The trials excluded patients with abnormal LVEF, history of acute coronary syndrome within 6 months, history of Class II or greater congestive heart failure (New York Heart Association), history of RVO or RPED, QTcB interval ≥ 480 msec, uncontrolled hypertension, uncontrolled arrhythmias, active brain metastases, or known history of glucose-6-phosphate dehydrogenase deficiency.
Among these 559 patients, 197 (35%) were exposed to MEKINIST for > 6 months to 12 months, while 185 (33%) were exposed to MEKINIST for > 1 year. The median age was 55 years (range: 18 to 91), 57% were male, and 98% were white, 72% had baseline ECOG performance status 0 and 28% had ECOG performance status 1, 64% had M1c stage disease, 35% had elevated lactate dehydrogenase (LDH) at baseline, and 0.5% had a history of brain metastases.
The most common adverse reactions (≥ 20%) for MEKINIST in patients receiving MEKINIST plus dabrafenib were: pyrexia, nausea, rash, chills, diarrhea, vomiting, hypertension, and peripheral edema.
The demographics and baseline tumor characteristics of patients enrolled in the COMBI-d study are summarized in Clinical Studies [see Clinical Studies (14.1)]. Patients receiving MEKINIST plus dabrafenib had a median duration of exposure of 11 months (range: 3 days to 30 months) to MEKINIST. Among the 209 patients receiving MEKINIST plus dabrafenib, 26% were exposed to MEKINIST for > 6 months to 12 months while 46% were exposed to MEKINIST for > 1 year.
In the COMBI-d study, adverse reactions leading to discontinuation of MEKINIST occurred in 11% of patients receiving MEKINIST plus dabrafenib; the most frequent were pyrexia (1.4%) and decreased ejection fraction (1.4%). Adverse reactions leading to dose reductions of MEKINIST occurred in 18% of patients receiving MEKINIST plus dabrafenib; the most frequent were pyrexia (2.9%), neutropenia (1.9%), decreased ejection fraction (1.9%), and rash (1.9%). Adverse reactions leading to dose interruptions of MEKINIST occurred in 46% of patients receiving MEKINIST plus dabrafenib; the most frequent were pyrexia (18%), chills (7%), vomiting (6%), and decreased ejection fraction (4.8%).
Table 5 and Table 6 present selected adverse reactions and laboratory abnormalities, respectively, of MEKINIST observed in the COMBI-d study.
Table 5. Adverse Reactions Occurring in ≥ 10% (All Grades) of Patients Receiving MEKINIST With Dabrafenib and at a Higher Incidence* Than in Patients Receiving Single-Agent Dabrafenib in COMBI-da *≥ 5% for All Grades or ≥ 2% for Grades 3–4 incidence in patients receiving MEKINIST with dabrafenib compared with patients receiving dabrafenib as a single agent.
aNational Cancer Institute Common Terminology Criteria for Adverse Events, version 4.0.
bIncludes peripheral edema, edema, lymphedema, localized edema, and generalized edema.
cIncludes abdominal pain, upper abdominal pain, lower abdominal pain, and abdominal discomfort.
dIncludes rash, generalized rash, pruritic rash, erythematous rash, papular rash, vesicular rash, macular rash, maculo-papular, and folliculitis rash.
eMost common events (≥ 1%) include epistaxis, hematochezia, decreased hemoglobin, purpura, and rectal hemorrhage. Grade 4 events were limited to hepatic hematoma and duodenal ulcer hemorrhage (each n = 1 in the pooled combination arm).Adverse Reactions Pooled MEKINIST plus
Dabrafenib
N = 559COMBI-d Study MEKINIST plus
Dabrafenib N = 209Dabrafenib
N = 211All
Grades
(%)Grades
3 and 4
(%)All
Grades
(%)Grades
3 and 4
(%)All
Grades
(%)Grades
3 and 4
(%)General Pyrexia 54 5 57 7 33 1.9 Chills 31 0.5 31 0 17 0.5 Peripheral edemab 21 0.7 25 1.4 11 0.5 Gastrointestinal Nausea 35 0.4 34 0.5 27 1.4 Diarrhea 31 1.3 30 1.4 16 0.9 Vomiting 27 1.1 25 1.0 14 0.5 Abdominal painc 18 0.9 26 1.0 14 2.4 Skin Rashd 32 1.1 42 0 27 1.4 Vascular Hypertension 26 11 25 6 16 6 Hemorrhagee 18 2.0 19 1.9 15 1.9 Nervous system Dizziness 11 0.2 14 0 7 0 Other clinically important adverse reactions for MEKINIST observed in less than 10% of patients receiving MEKINIST in combination with dabrafenib (N = 559) were:
Cardiac: Bradycardia
Musculoskeletal: Rhabdomyolysis
Table 6. Laboratory Abnormalities Worsening From Baseline Occurring at ≥ 10% (All Grades) of Patients Receiving MEKINIST With Dabrafenib and at a Higher Incidence* Than in Patients Receiving Single-Agent Dabrafenib in COMBI-d Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase.
*≥ 5% for All Grades or ≥ 2% for Grades 3–4 incidence in patients receiving MEKINIST with dabrafenib compared with patients receiving dabrafenib as a single agent.
aFor these laboratory tests the denominator is 556.
bFor these laboratory tests the denominator is 208 for the combination arm, 207-209 for the dabrafenib arm.
cGrade 4 adverse reactions limited to lymphopenia and hyperglycemia (each n = 4), increased ALT and increased AST (each n = 3), neutropenia (n = 2), and hyponatremia (n = 1), in the pooled combination arm; neutropenia, lymphopenia, increased ALT, increased AST, hyperglycemia (each n = 1) in the COMBI-d study combination arm; neutropenia, thrombocytopenia, increased ALT, and increased AST (each n = 1) in the dabrafenib arm.Laboratory Abnormality Pooled MEKINIST plus
Dabrafenib
N = 559aCOMBI-d Study MEKINIST plus
Dabrafenib N = 209bDabrafenib
N = 211bAll
Grades
(%)Grades
3 and 4c
(%)All
Grades
(%)Grades
3 and 4c
(%)All
Grades
(%)Grades
3 and 4c
(%)Chemistry Hyperglycemia 60 4.7 65 6 57 4.3 Hypoalbuminemia 48 1.1 53 1.4 27 0 Hyponatremia 25 8 24 6 14 2.9 Hepatic Increased AST 59 4.1 60 4.3 21 1.0 Increased blood alkaline phosphatase 49 2.7 50 1.0 25 0.5 Increased ALT 48 4.5 44 3.8 28 1.0 Hematology Neutropenia 46 7 50 6 16 1.9 Anemia 43 2.3 43 2.4 38 4.3 Lymphopenia 32 8 38 9 28 7 Thrombocytopenia 21 0.7 19 0.5 10 0.5 Adjuvant Treatment of BRAF V600E or V600K Mutation-Positive Melanoma
The safety of MEKINIST when administered with dabrafenib was evaluated in 435 patients with Stage III melanoma with BRAF V600E or V600K mutations following complete resection who received at least one dose of study therapy in the COMBI-AD study [see Clinical Studies (14.2)]. Patients received MEKINIST 2 mg orally once daily and dabrafenib 150 mg orally twice daily for 12 months. The trial excluded patients with abnormal LVEF; history of acute coronary syndromes, coronary angioplasty, or stenting within 6 months; Class II or greater congestive heart failure (New York Heart Association); QTc interval ≥ 480 msec; treatment refractory hypertension; uncontrolled arrhythmias; or history of RVO.
Patients receiving MEKINIST in combination with dabrafenib had a median duration of exposure of 11 months (range: 0 to 12) to MEKINIST. Among the 435 patients receiving MEKINIST in combination with dabrafenib, 72% were exposed to MEKINIST for > 6 months. The median age of patients who received MEKINIST in combination with dabrafenib was 50 years (range: 18 to 89), 56% were male, 99% were white, 92% had baseline ECOG performance status 0, and 8% had baseline ECOG performance status 1.
The most common adverse reactions (≥ 20%) in patients receiving MEKINIST in combination with dabrafenib were: pyrexia, fatigue, nausea, headache, rash, chills, diarrhea, vomiting, arthralgia, and myalgia.
Adverse reactions resulting in discontinuation and dose interruptions of MEKINIST occurred in 24% and 54% of patients, respectively; the most frequent for each were pyrexia and chills. Adverse reactions leading to dose reductions of MEKINIST occurred in 23% of patients; the most frequent were pyrexia and decreased ejection fraction.
Table 7 summarizes adverse reactions that occurred in at least 20% of the patients receiving MEKINIST in combination with dabrafenib.
Table 7. Adverse Reactions Occurring in ≥ 20% of Patients in COMBI-ADa aNCI CTCAE version 4.0.
bIncludes pyrexia and hyperpyrexia.
cIncludes fatigue, asthenia, and malaise.
dIncludes headache and tension headache.
eIncludes rash, rash maculo-papular, rash macular, rash generalized, rash erythematous, rash papular, rash pruritic, nodular rash, rash vesicular, and rash pustular.
fIncludes myalgia, musculoskeletal pain, and musculoskeletal chest pain.Adverse Reactions MEKINIST plus Dabrafenib
N = 435Placebo
N = 432All
Grades
(%)Grades
3 and 4
(%)All
Grades
(%)Grades
3 and 4
(%)General Pyrexiab 63 5 11 < 1 Fatiguec 59 5 37 < 1 Chills 37 1 4 0 Gastrointestinal Nausea 40 < 1 20 0 Diarrhea 33 < 1 15 < 1 Vomiting 28 < 1 10 0 Nervous system Headached 39 1 24 0 Skin Rashe 37 < 1 16 < 1 Musculoskeletal Arthralgia 28 < 1 14 0 Myalgiaf 20 < 1 14 0 Other clinically important adverse reactions observed in less than 20% of patients in the COMBI-AD study receiving MEKINIST in combination with dabrafenib were: blurred vision (6%), decreased ejection fraction (5%), and rhabdomyolysis (< 1%).
The laboratory abnormalities are summarized in Table 8.
Table 8. Laboratory Abnormalities Worsening From Baseline Occurring in ≥ 20% of Patients in COMBI-AD Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase.
aThe incidence is based on the number of patients who had both a baseline and at least one on-study laboratory measurement:
MEKINIST plus dabrafenib (range: 429 to 431) and placebo arm (range: 426 to 428).Laboratory Abnormality MEKINIST plus Dabrafeniba
N = 435Placeboa
N = 432All
Grades
(%)Grades
3 and 4
(%)All
Grades
(%)Grades
3 and 4
(%)Chemistry Hyperglycemia 63 3 47 2 Hypophosphatemia 42 7 10 < 1 Hypoalbuminemia 25 < 1 < 1 0 Hepatic Increased AST 57 6 11 < 1 Increased ALT 48 5 18 < 1 Increased blood alkaline phosphatase 38 1 6 < 1 Hematology Neutropenia 47 6 12 < 1 Lymphopenia 26 5 6 < 1 Anemia 25 < 1 6 < 1 Metastatic, BRAF V600E Mutation-Positive Non-Small Cell Lung Cancer
The safety of MEKINIST when administered with dabrafenib was evaluated in 93 patients with previously untreated (n = 36) and previously treated (n = 57) metastatic BRAF V600E mutation-positive NSCLC in a multicenter, multi-cohort, non-randomized, open-label trial (Study BRF113928). Patients received MEKINIST 2 mg orally once daily and dabrafenib 150 mg orally twice daily until disease progression or unacceptable toxicity. The trial excluded patients with abnormal LVEF, history of acute coronary syndrome within 6 months, history of Class II or greater congestive heart failure (New York Heart Association), QTc interval ≥ 480 msec, treatment refractory hypertension, uncontrolled arrhythmias, active brain metastases, history of ILD or pneumonitis, or history or current RVO [see Clinical Studies (14.3)].
Among these 93 patients, 53 (57%) were exposed to MEKINIST and dabrafenib for > 6 months and 27 (29%) were exposed to MEKINIST and dabrafenib for ≥ 1 year. The median age was 65 years (range: 41 to 91), 46% were male, 85% were white; 32% had baseline ECOG performance status 0 and 61% had ECOG performance status 1; 98% had non-squamous histology; and 12% were current smokers, 60% were former smokers, and 28% had never smoked.
The most common adverse reactions (≥ 20%) in these 93 patients were: pyrexia, fatigue, nausea, vomiting, diarrhea, dry skin, decreased appetite, edema, rash, chills, hemorrhage, cough, and dyspnea.
Adverse reactions resulting in discontinuation of MEKINIST occurred in 19% of patients; the most frequent were pyrexia (2.2%), decreased ejection fraction (2.2%), and respiratory distress (2.2%). Adverse reactions leading to dose reductions of MEKINIST occurred in 30% of patients receiving MEKINIST plus dabrafenib; the most frequent were pyrexia (5%), nausea (4.3%), vomiting (4.3%), diarrhea (3.2%), and neutropenia (3.2%). Adverse reactions leading to dose interruptions of MEKINIST occurred in 57% of patients receiving MEKINIST plus dabrafenib; the most frequent were pyrexia (16%), vomiting (10%), neutropenia (8%), nausea (5%), and decreased ejection fraction (5%).
Table 9 and Table 10 present adverse reactions and laboratory abnormalities, respectively, of MEKINIST in combination with dabrafenib in Study BRF113928.
Table 9. Adverse Reactions Occurring in ≥ 20% (All Grades) of Patients Treated With MEKINIST plus Dabrafenib in Study BRF113928a aNCI CTCAE version 4.0.
bIncludes fatigue, malaise, and asthenia.
cIncludes peripheral edema, edema, and generalized edema.
dIncludes rash, rash generalized, rash papular, rash macular, rash maculo-papular, and rash pustular.
eIncludes hemoptysis, hematoma, epistaxis, purpura, hematuria, subarachnoid hemorrhage, gastric hemorrhage, urinary bladder hemorrhage, contusion, hematochezia, injection site hemorrhage, pulmonary hemorrhage, and retroperitoneal hemorrhage.Adverse Reactions MEKINIST plus Dabrafenib
N = 93All
Grades
(%)Grades
3 and 4b
(%)General Pyrexia 55 5 Fatigueb 51 5 Edemac 28 0 Chills 23 1.1 Gastrointestinal Nausea 45 0 Vomiting 33 3.2 Diarrhea 32 2.2 Decreased appetite 29 0 Skin Dry skin 31 1.1 Rashd 28 3.2 Vascular Hemorrhagee 23 3.2 Respiratory system Cough 22 0 Dyspnea 20 5 Table 10. Treatment-Emergent Laboratory Abnormalities Occurring in ≥ 20% (All Grades) of Patients Receiving MEKINIST plus Dabrafenib in Study BRF113928 Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase.
aFor these laboratory tests the denominator is 90.
bFor these laboratory tests the denominator is 91.Laboratory Abnormality MEKINIST plus Dabrafenib
N = 93All
Grades
(%)Grades
3 and 4
(%)Chemistrya Hyperglycemia 71 9 Hyponatremia 57 17 Hypophosphatemia 36 7 Increased creatinine 21 1.1 Hepatica Increased blood alkaline phosphatase 64 0 Increased AST 61 4.4 Increased ALT 32 6 Hematologyb Leukopenia 48 8 Anemia 46 10 Neutropenia 44 8 Lymphopenia 42 14 Locally Advanced or Metastatic, BRAF V600E Mutation-Positive, Anaplastic Thyroid Cancer
The safety of MEKINIST when administered with dabrafenib was evaluated in a nine-cohort, multicenter, non-randomized, open-label study in patients with rare cancers with the BRAF V600E mutation, including locally advanced or metastatic ATC (Study BRF117019). At the time of the safety analysis, a total of 100 patients were enrolled in the trial, 16 of whom were enrolled in the ATC cohort. The primary safety population included all patients who received at least one dose of MEKINIST or dabrafenib. Patients received MEKINIST 2 mg orally once daily and dabrafenib 150 mg orally twice daily until disease progression or unacceptable toxicity.
Among these 100 patients, 46 (46%) were exposed to MEKINIST and dabrafenib for > 6 months and 23 (23%) were exposed to MEKINIST and dabrafenib for ≥ 1 year. The median age was 59.5 years (range: 18 to 85); 62% were male; 85% were white; and 31% had baseline ECOG performance status 0, and 59% had ECOG performance status 1.
The adverse reaction profile among all patients and among patients in the ATC cohort was similar to that observed in other approved indications.
- New Primary Malignancies [see Warnings and Precautions (5.1)]
- 7 DRUG INTERACTIONS
-
8
USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Based on its mechanism of action [see Clinical Pharmacology (12.1)] and findings from animal reproduction studies, MEKINIST can cause fetal harm when administered to a pregnant woman. There is insufficient data in pregnant women exposed to MEKINIST to assess the risks. Trametinib was embryotoxic and abortifacient in rabbits at doses greater than or equal to those resulting in exposures approximately 0.3 times the human exposure at the recommended clinical dose (see Data). Advise pregnant women of the potential risk to the fetus.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2%-4% and 15%-20%, respectively.
Data
Animal Data
In reproductive toxicity studies, administration of trametinib to rats during the period of organogenesis resulted in decreased fetal weights at doses greater than or equal to 0.031 mg/kg/day [approximately 0.3 times the human exposure at the recommended dose based on area under the curve (AUC)]. In rats, at a dose resulting in exposures 1.8-fold higher than the human exposure at the recommended dose, there was maternal toxicity and an increase in post-implantation loss.
In pregnant rabbits, administration of trametinib during the period of organogenesis resulted in decreased fetal body weight and increased incidence of variations in ossification at doses greater than or equal to 0.039 mg/kg/day (approximately 0.08 times the human exposure at the recommended dose based on AUC). In rabbits administered trametinib at 0.15 mg/kg/day (approximately 0.3 times the human exposure at the recommended dose based on AUC) there was an increase in post-implantation loss, including total loss of pregnancy, compared with control animals.
8.2 Lactation
Risk Summary
There are no data on the presence of trametinib in human milk, or the effects of trametinib on the breastfed infant or on milk production. Because of the potential for serious adverse reactions in breastfed infants, advise women not to breastfeed during treatment with MEKINIST and for 4 months following the last dose.
8.3 Females and Males of Reproductive Potential
Pregnancy Testing
Verify pregnancy status in females of reproductive potential prior to initiating MEKINIST.
Contraception
Based on data from animal studies and its mechanism of action, MEKINIST can cause fetal harm when administered to pregnant women [see Use in Specific Populations (8.1)].
Females
Advise female patients of reproductive potential to use effective contraception during treatment with MEKINIST and for 4 months after the last dose.
Males
To avoid potential drug exposure to pregnant partners and female partners of reproductive potential, advise male patients (including those who have had vasectomies) with female partners of reproductive potential to use condoms during treatment with MEKINIST and for at least 4 months after the last dose.
Infertility
Females
Advise female patients of reproductive potential that MEKINIST may impair fertility. Increased follicular cysts and decreased corpora lutea were observed in female rats at dose exposures equivalent to 0.3 times the human exposure at the recommended dose [see Nonclinical Toxicology (13.1)].
8.4 Pediatric Use
The safety and effectiveness of MEKINIST as a single agent or in combination with dabrafenib have not been established in pediatric patients.
Juvenile Animal Toxicity Data
In a repeat-dose toxicity study in juvenile rats, decreased bone length and corneal dystrophy were observed at doses resulting in exposures as low as 0.3 times the human exposure at the recommended adult dose based on AUC. Additionally, a delay in sexual maturation was noted at doses resulting in exposures as low as 1.6 times the human exposure at the recommended adult dose based on AUC.
8.5 Geriatric Use
Of the 214 patients with melanoma who received single agent MEKINIST in the METRIC study, 27% were aged 65 years and older and 4% were over 75 years old [see Clinical Studies (14.1)]. This study of single agent MEKINIST in melanoma did not include sufficient numbers of geriatric patients to determine whether they respond differently from younger adults.
Of the 994 patients with melanoma who received MEKINIST plus dabrafenib in the COMBI-d, COMBI-v, and COMBI-AD studies [see Clinical Studies (14.1, 14.2)], 21% were aged 65 years and older and 5% were aged 75 years and older. No overall differences in the effectiveness of MEKINIST plus dabrafenib were observed in geriatric patients as compared to younger adults across these melanoma studies. The incidences of peripheral edema (26% vs. 12%) and anorexia (21% vs. 9%) increased in geriatric patients as compared to younger adults in these studies.
Of the 93 patients with NSCLC who received MEKINIST in Study BRF113928, there were insufficient numbers of geriatric patients aged 65 and older to determine whether they respond differently from younger adults [see Clinical Studies (14.4)].
Of the 26 patients with ATC who received MEKINIST in Study BRF117019, 77% were aged 65 years and older and 31% were aged 75 years and older [see Clinical Studies (14.4)]. This study did not include sufficient numbers of younger adults to determine whether they respond differently compared to geriatric patients.
8.6 Renal Impairment
No dose adjustment is recommended in patients with mild (GFR 60 to 89 mL/min/1.73 m2) or moderate renal impairment (GFR 30 to 59 mL/min/1.73 m2) [see Clinical Pharmacology (12.3)]. The appropriate dose of MEKINIST has not been established in patients with severe renal impairment (GFR ≤ 30 mL/min/1.73 m2).
8.7 Hepatic Impairment
No dose adjustment is recommended in patients with mild (bilirubin ≤ upper limit of normal (ULN) and aspartate aminotransferase (AST) > ULN or bilirubin > 1x to 1.5x ULN and any AST) hepatic impairment [see Clinical Pharmacology (12.3)]. A recommended dosage of MEKINIST has not been established in patients with moderate (bilirubin > 1.5x to 3x ULN and any AST) or severe (bilirubin > 3x to 10x ULN and any AST) hepatic impairment.
-
10
OVERDOSAGE
The highest doses of MEKINIST evaluated in clinical trials were 4 mg orally once daily and 10 mg administered orally once daily on 2 consecutive days followed by 3 mg once daily. In seven patients treated on one of these two schedules, there were two cases of RPEDs for an incidence of 28%.
Since trametinib is highly bound to plasma proteins, hemodialysis is likely to be ineffective in the treatment of overdose with MEKINIST.
-
11
DESCRIPTION
Trametinib dimethyl sulfoxide is a kinase inhibitor. The chemical name is acetamide, N-[3-[3-cyclopropyl-5-[(2-fluoro-4- iodophenyl)amino]-3,4,6,7-tetrahydro-6,8-dimethyl- 2,4,7-trioxopyrido[4,3-d]pyrimidin-1(2H)-yl]phenyl]-, compound with 1,1’-sulfinylbis[methane] (1:1). It has a molecular formula C26H23FIN5O4C2H6OS with a molecular mass of 693.53 g/mol. Trametinib dimethyl sulfoxide has the following chemical structure:
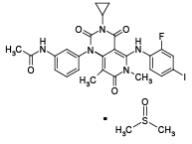
Trametinib dimethyl sulfoxide is a white to almost white powder. It is practically insoluble in the pH range of 2 to 8 in aqueous media.
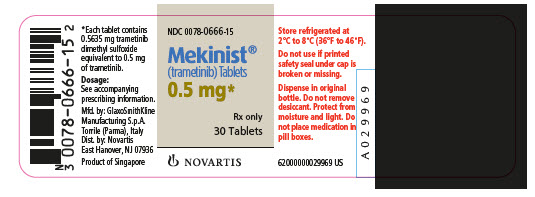
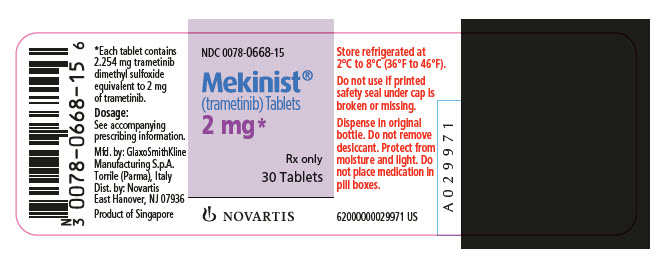
MEKINIST (trametinib) tablets for oral use are supplied as 0.5 mg and 2 mg tablets for oral administration. Each 0.5 mg tablet contains 0.5635 mg trametinib dimethyl sulfoxide equivalent to 0.5 mg of trametinib non-solvated parent. Each 2 mg tablet contains 2.254 mg trametinib dimethyl sulfoxide equivalent to 2 mg of trametinib non-solvated parent.
The inactive ingredients of MEKINIST tablets are: Tablet Core: colloidal silicon dioxide, croscarmellose sodium, hypromellose, magnesium stearate (vegetable source), mannitol, microcrystalline cellulose, and sodium lauryl sulfate. Coating: hypromellose, iron oxide red (2 mg tablets), iron oxide yellow (0.5 mg tablets), polyethylene glycol, polysorbate 80 (2 mg tablets), and titanium dioxide.
-
12
CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Trametinib is a reversible inhibitor of mitogen-activated extracellular signal-regulated kinase 1 (MEK1) and MEK2 activation and of MEK1 and MEK2 kinase activity. MEK proteins are upstream regulators of the extracellular signal-related kinase (ERK) pathway, which promotes cellular proliferation. BRAF V600E mutations result in constitutive activation of the BRAF pathway which includes MEK1 and MEK2. Trametinib inhibits cell growth of various BRAF V600 mutation-positive tumors in vitro and in vivo.
Trametinib and dabrafenib target two different kinases in the RAS/RAF/MEK/ERK pathway. Use of trametinib and dabrafenib in combination resulted in greater growth inhibition of BRAF V600 mutation-positive tumor cell lines in vitro and prolonged inhibition of tumor growth in BRAF V600 mutation positive tumor xenografts compared with either drug alone.
12.2 Pharmacodynamics
Administration of 1 mg and 2 mg MEKINIST to patients with BRAF V600 mutation-positive melanoma resulted in dose-dependent changes in tumor biomarkers including inhibition of phosphorylated ERK, inhibition of Ki67 (a marker of cell proliferation), and increases in p27 (a marker of apoptosis).
Cardiac Electrophysiology
The heart rate-corrected QT (QTc) prolongation potential of trametinib was assessed in a dedicated study in 32 patients who received placebo on day 1 and MEKINIST 2 mg once daily on days 2-14 followed by MEKINIST 3 mg on day 15. No clinically relevant QTc prolongation was detected in the study.
In clinical trials in patients receiving MEKINIST with dabrafenib, QTc prolongation > 500 ms occurred in 0.8% of patients and QTc increased by > 60 ms from baseline in 3.8% of patients.
12.3 Pharmacokinetics
The pharmacokinetics of trametinib were characterized following single- and repeat-oral administration in patients with solid tumors and BRAF V600 mutation-positive metastatic melanoma.
Absorption
After oral administration of MEKINIST, the median time to achieve peak plasma concentrations (Tmax) is 1.5 hours post-dose. The mean absolute bioavailability of a single oral dose of MEKINIST 2 mg is 72%. The increase in Cmax was dose proportional after a single dose of 0.125 mg (0.0625 times the approved recommended dosage) to 10 mg (5 times the approved recommended dosage) while the increase in AUC was greater than dose proportional. After repeat doses of 0.125 mg to 4 mg daily, both Cmax and AUC increase proportionally with dose. Inter-subject variability in AUC and Cmax at steady state is 22% and 28%, respectively.
Effect of Food
Administration of a single dose of MEKINIST with a high-fat, high-calorie meal (approximately 1000 calories) decreased trametinib AUC by 24%, Cmax by 70%, and delayed Tmax by approximately 4 hours as compared with fasted conditions.
Distribution
Trametinib is 97.4% bound to human plasma proteins. The apparent volume of distribution (Vc/F) is 214 L.
Elimination
The estimated elimination half-life of trametinib based on the population PK model is 3.9 to 4.8 days. The apparent clearance is 4.9 L/h.
Metabolism
Trametinib is metabolized predominantly via deacetylation alone or with mono-oxygenation or in combination with glucuronidation biotransformation pathways in vitro. Deacetylation is mediated by carboxylesterases (i.e., carboxylesterase 1b/c and 2) and may also be mediated by other hydrolytic enzymes.
Following a single dose of [14C]-trametinib, approximately 50% of circulating radioactivity is represented as the parent compound. However, based on metabolite profiling after repeat dosing of trametinib, ≥ 75% of drug-related material in plasma is the parent compound.
Excretion
Following oral administration of [14C]-trametinib, greater than 80% of excreted radioactivity was recovered in the feces while less than 20% of excreted radioactivity was recovered in the urine with less than 0.1% of the excreted dose as parent.
Specific Populations
Age, sex, and body weight do not have a clinically important effect on the exposure of trametinib. There are insufficient data to evaluate potential differences in the exposure of trametinib by race or ethnicity.
Patients with Hepatic Impairment: Based on a population pharmacokinetic analysis in 64 patients with mild hepatic impairment (total bilirubin ≤ ULN and AST > ULN or total bilirubin > 1 to 1.5 x ULN and any AST), mild hepatic impairment has no clinically important effect on the systemic exposure of trametinib. The pharmacokinetics of trametinib have not been studied in patients with moderate (bilirubin > 1.5x to 3x ULN and any AST) or severe (bilirubin >3x to 10x ULN and any AST) hepatic impairment.
Patients with Renal Impairment: Based on a population pharmacokinetic analysis in 223 patients with mild renal impairment (GFR 60 to 89 mL/min/1.73 m2) and 35 patients with moderate renal impairment (GFR 30 to 59 mL/min/1.73 m2), mild and moderate renal impairment have no clinically important effects on the systemic exposure of trametinib. The pharmacokinetics of trametinib have not been studied in patients with severe renal impairment (GFR ≤ 30 mL/min/1.73 m2).
Drug Interaction Studies
Effect of Dabrafenib on Trametinib: Coadministration of trametinib 2 mg daily with dabrafenib 150 mg twice daily resulted in no change in AUC of trametinib as compared with administration of trametinib.
Effect of Trametinib on CYP Substrates: Based on in vitro studies, trametinib is an inhibitor of CYP2C8, but is not an inhibitor of CYP1A2, CYP2A6, CYP2B6, CYP2C9, CYP2C19, CYP2D6, or CYP3A4 at a clinically relevant systemic concentration of 0.04 µM. Trametinib is an inducer of CYP3A in vitro. Based on cross-study comparisons, oral administration of MEKINIST 2 mg once daily with a sensitive CYP3A4 substrate had no clinically important effect on the AUC and Cmax of the sensitive CYP3A4 substrate.
Effect of Transporters on Trametinib: Trametinib is a substrate of P-glycoprotein (P-gp) and BSEP. Inhibition of P-gp is unlikely to result in a clinically important increase in trametinib concentrations as trametinib exhibits high passive permeability and bioavailability. Trametinib is not a substrate of BCRP, OATP1B1, OATP1B3, OATP2B1, OCT1, MRP2, or MATE1 in vitro.
Effect of Trametinib on Transporters: Based on in vitro studies, trametinib is not an inhibitor of P-gp, BCRP, OATP1B1, OATP1B3, OAT1, OAT3, OCT2, BSEP, MRP2, or MATE1 at a clinically relevant systemic concentration of 0.04 µM.
-
13
NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies with trametinib have not been conducted. Trametinib was not genotoxic in studies evaluating reverse mutations in bacteria, chromosomal aberrations in mammalian cells, and micronuclei in the bone marrow of rats.
Trametinib may impair fertility in humans. In female rats given trametinib for up to 13 weeks, increased follicular cysts and decreased corpora lutea were observed at doses ≥ 0.016 mg/kg/day (approximately 0.3 times the human exposure at the recommended dose based on AUC). In rat and dog toxicity studies up to 13 weeks in duration, there were no treatment effects observed on male reproductive tissues [see Use in Specific Populations (8.3)].
-
14
CLINICAL STUDIES
14.1 BRAF V600E or V600K Mutation-Positive Unresectable or Metastatic Melanoma
MEKINIST as a Single Agent
The safety and efficacy of MEKINIST were evaluated in an international, multicenter, randomized (2:1), open-label, active-controlled trial (the METRIC study; NCT01245062) in 322 patients with BRAF V600E or V600K mutation-positive, unresectable or metastatic melanoma. In the METRIC study, patients were not permitted to have more than one prior chemotherapy regimen for advanced or metastatic disease; prior treatment with a BRAF inhibitor or MEK inhibitor was not permitted. Patients were randomized to receive MEKINIST 2 mg orally once daily (N = 214) or chemotherapy (N = 108) consisting of either dacarbazine 1000 mg/m2 intravenously every 3 weeks or paclitaxel 175 mg/m2 intravenously every 3 weeks. Treatment continued until disease progression or unacceptable toxicity. Randomization was stratified according to prior use of chemotherapy for advanced or metastatic disease (yes versus no) and LDH level (normal versus greater than ULN). Tumor tissue was evaluated for BRAF mutations at a central testing site using a clinical trial assay. Tumor samples from 289 patients (196 patients treated with MEKINIST and 93 chemotherapy-treated patients) were also tested retrospectively using an FDA-approved companion diagnostic test, THxID™-BRAF assay. The major efficacy outcome measure was progression-free survival (PFS).
The median age for randomized patients was 54 years, 54% were male, greater than 99% were white, and all patients had baseline ECOG performance status of 0 or 1. Most patients had metastatic disease (94%), were Stage M1c (64%), had elevated LDH (36%), had no history of brain metastasis (97%), and received no prior chemotherapy for advanced or metastatic disease (66%). The distribution of BRAF V600 mutations was BRAF V600E (87%), V600K (12%), or both (less than 1%). The median durations of follow-up prior to initiation of alternative treatment were 4.9 months for patients treated with MEKINIST and 3.1 months for patients treated with chemotherapy. Fifty-one (47%) patients crossed over from the chemotherapy arm at the time of disease progression to receive MEKINIST.
The METRIC study demonstrated a statistically significant increase in progression-free survival in the patients treated with MEKINIST. Table 11 and Figure 1 summarize the PFS results.
Table 11. Efficacy Results in the METRIC Study Abbreviations: CI, confidence interval; DoR, duration of response; HR, hazard ratio; NR, not reached.
aPike estimator.Investigator-Assessed Endpoints MEKINIST
N = 214Chemotherapy
N = 108Progression-Free Survival Number of Events (%) 117 (55%) 77 (71%) Progressive Disease 107 (50%) 70 (65%) Death 10 (5%) 7 (6%) Median, months (95% CI) 4.8 (4.3, 4.9) 1.5 (1.4, 2.7) HRa (95% CI) 0.47 (0.34, 0.65) P value (log-rank test) < 0.0001 Confirmed Tumor Responses Overall Response Rate (95% CI) 22% (17%, 28%) 8% (4%, 15%) Complete Response, n (%) 4 (2%) 0 Partial Response, n (%) 43 (20%) 9 (8%) Duration of Response Median DoR, months (95% CI) 5.5 (4.1, 5.9) NR (3.5, NR) 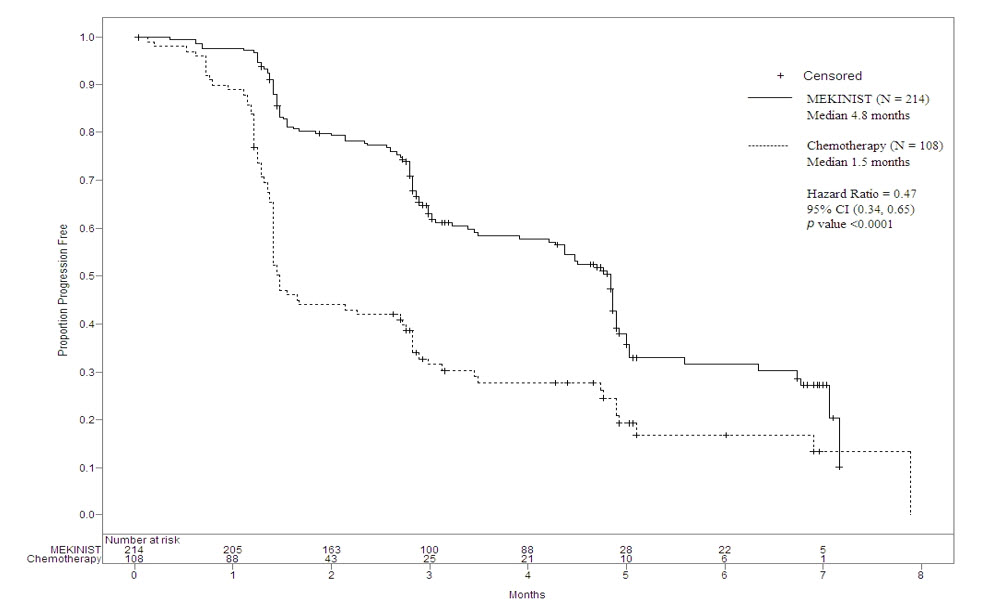
Figure 1. Kaplan-Meier Curves of Investigator-Assessed Progression-Free Survival (ITT Population) in the METRIC Study
In supportive analyses based on independent radiologic review committee (IRRC) assessment, the PFS results were consistent with those of the primary efficacy analysis.
MEKINIST with Dabrafenib
COMBI-d Study
The safety and efficacy of MEKINIST administered with dabrafenib were evaluated in an international, randomized, double-blind, active-controlled trial (the COMBI-d study; NCT01584648). The COMBI-d study compared dabrafenib plus MEKINIST to dabrafenib plus placebo as first-line treatment for patients with unresectable (Stage IIIc) or metastatic (Stage IV) BRAF V600E or V600K mutation-positive cutaneous melanoma. Patients were randomized (1:1) to receive MEKINIST 2 mg once daily plus dabrafenib 150 mg twice daily or dabrafenib 150 mg twice daily plus matching placebo. Randomization was stratified by LDH level (greater than the ULN vs. ≤ ULN) and BRAF mutation subtype (V600E vs. V600K). The major efficacy outcome was investigator-assessed progression-free survival (PFS) per RECIST v1.1 with additional efficacy outcome measures of overall survival (OS) and confirmed overall response rate (ORR).
In the COMBI-d study, 423 patients were randomized to MEKINIST plus dabrafenib (n = 211) or dabrafenib plus placebo (n = 212). The median age was 56 years (range: 22 to 89 years), 53% were male, > 99% were white, 72% had ECOG performance status of 0, 4% had Stage IIIc, 66% had M1c disease, 65% had a normal LDH, and 2 patients had a history of brain metastases. All patients had tumor containing BRAF V600E or V600K mutations as determined by centralized testing with the FDA-approved companion diagnostic test; 85% had BRAF V600E mutation-positive melanoma and 15% had BRAF V600K mutation-positive melanoma.
The COMBI-d study demonstrated statistically significant improvements in PFS and OS. Table 12 and Figure 2 summarize the efficacy results.
Table 12. Efficacy Results in the COMBI-d Study Abbreviations: CI, confidence interval; DoR, duration of response; HR, hazard ratio; NR, not reached; ORR, overall response rate.
aPFS and ORR were assessed by investigator.
bBased on stratified log-rank test.Endpoint MEKINIST plus Dabrafenib
N = 211Placebo plus Dabrafenib
N = 212Survivala Number of Events (%) 102 (48%) 109 (51%) Median, months (95% CI) 9.3 (7.7, 11.1) 8.8 (5.9, 10.9) HR (95% CI) 0.75 (0.57, 0.99) P valueb 0.035 Overall Survival Number of Deaths (%) 99 (47%) 123 (58%) Median, months (95% CI) 25.1 (19.2, NR) 18.7 (15.2, 23.1) HR (95% CI) 0.71 (0.55, 0.92) P valueb 0.01 Overall Response Ratea ORR (95% CI) 66% (60%, 73%) 51% (44%, 58%) P value < 0.001 Complete Response 10% 8% Partial Response 56% 42% Median DoR, months (95% CI) 9.2 (7.4, NR) 10.2 (7.5, NR) 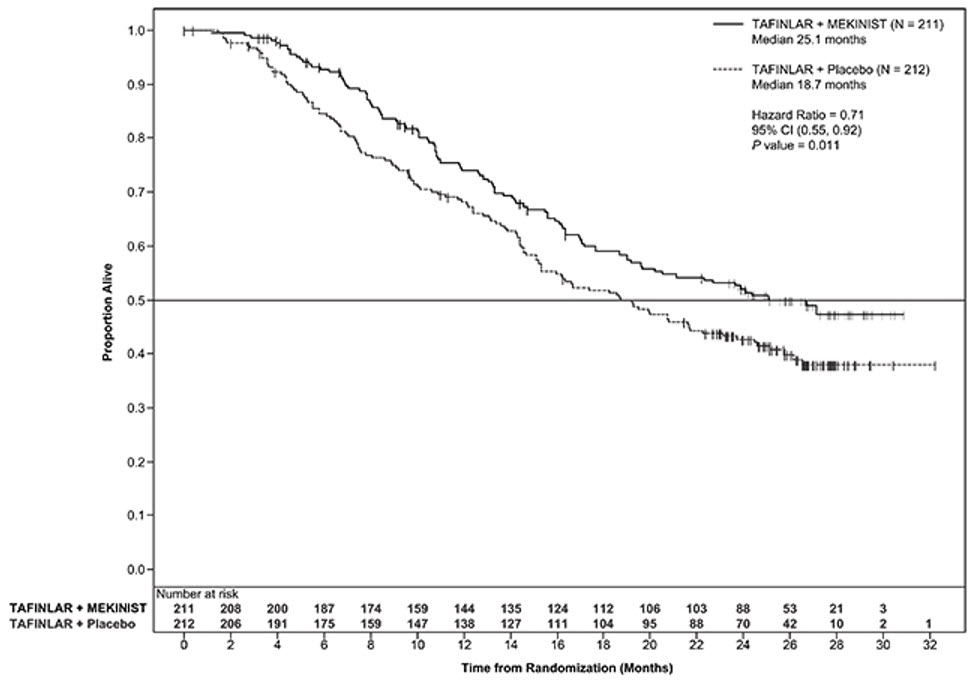
Figure 2. Kaplan-Meier Curves of Overall Survival in the COMBI-d Study
COMBI-MB Study
The activity of MEKINIST with dabrafenib for the treatment of BRAF V600E or V600K mutation-positive melanoma, metastatic to the brain, was evaluated in a non-randomized, open-label, multi-center, multi-cohort trial (the COMBI-MB study; NCT02039947). Eligible patients were required to have at least one measurable intracranial lesion and to have no leptomeningeal disease, parenchymal brain metastasis greater than 4 cm in diameter, ocular melanoma, or primary mucosal melanoma. Patients received MEKINIST 2 mg orally once daily and dabrafenib 150 mg orally twice daily until disease progression or unacceptable toxicity. The major efficacy outcome measure was intracranial response rate, defined as the percentage of patients with a confirmed intracranial response per RECIST v1.1, modified to allow up to five intracranial target lesions at least 5 mm in diameter, as assessed by independent review.
The COMBI-MB study enrolled 121 patients with a BRAF V600E (85%) or V600K (15%) mutation. The median age was 54 years (range: 23 to 84 years), 58% were male, 100% were white, 8% were from the United States, 65% had a normal LDH value at baseline, and 97% had an ECOG performance status of 0 or 1. Intracranial metastases were asymptomatic in 87% and symptomatic in 13% of patients, 22% received prior local therapy for brain metastases, and 87% also had extracranial metastases.
The intracranial response rate was 50% (95% CI: 40, 60), with a complete response rate of 4.1% and a partial response rate of 46%. The median duration of intracranial response was 6.4 months (range: 1 to 31 months). Of the patients with an intracranial response, 9% had stable or progressive disease as their best overall response.
14.2 Adjuvant Treatment of BRAF V600E or V600K Mutation-Positive Melanoma
The safety and efficacy of MEKINIST administered with dabrafenib were evaluated in an international, multi-center, randomized, double-blind, placebo-controlled trial (COMBI-AD; NCT01682083) that enrolled patients with Stage III melanoma with BRAF V600E or V600K mutations as detected by the THxIDTM-BRAF assay and pathologic involvement of regional lymph node(s). Enrollment required complete resection of melanoma with complete lymphadenectomy within 12 weeks prior to randomization. The trial excluded patients with mucosal or ocular melanoma, unresectable in-transit metastases, distant metastatic disease, or prior systemic anticancer treatment, including radiotherapy. Patients were randomized (1:1) to receive MEKINIST 2 mg once daily in combination with dabrafenib 150 mg twice daily or two placebos for up to 1 year. Randomization was stratified by BRAF mutation status (V600E or V600K) and American Joint Committee on Cancer (AJCC; 7th Edition) stage (IIIa, IIIb, or IIIc). The major efficacy outcome measure was relapse-free survival (RFS) defined as the time from randomization to disease recurrence (local, regional, or distant metastasis), new primary melanoma, or death from any cause, whichever occurred first as assessed by the investigator. Patients underwent imaging for tumor recurrence every 3 months for the first two years and every 6 months thereafter.
In COMBI-AD, a total of 870 patients were randomized: 438 to the MEKINIST in combination with dabrafenib and 432 to placebo. Median age was 51 years (range: 18 to 89), 55% were male, 99% were white, and 91% had an ECOG performance status of 0. Disease characteristics were AJCC Stage IIIa (18%), Stage IIIb (41%), Stage IIIc (40%), stage unknown (1%); BRAF V600E mutation (91%), BRAF V600K mutation (9%); macroscopic lymph nodes (65%); and tumor ulceration (41%). The median duration of follow-up (time from randomization to last contact or death) was 2.8 years.
COMBI-AD showed a statistically significant improvement in RFS in patients randomized to MEKINIST in combination with dabrafenib arm compared to those randomized to placebo. Efficacy results are presented in Table 13 and Figure 3.
Table 13. Efficacy Results in COMBI-AD in the Adjuvant Treatment of Melanoma Abbreviations: HR, hazard ratio; CI, confidence interval; NE, not estimable.
aPike estimator obtained from the stratified log-rank test.
bLog-rank test stratified by disease stage – IIIA vs. IIIB vs. IIIC – and BRAF V600 mutation type – V600E vs. V600K.MEKINIST plus Dabrafenib
N = 438Placebo
N = 432Relapse-Free Survival Number of Events (%) 166 (38) 248 (57) Median, months (95% CI) NE (44.5, NE) 16.6 (12.7, 22.1) HR (95% CI)a 0.47 (0.39, 0.58) P valueb < 0.0001 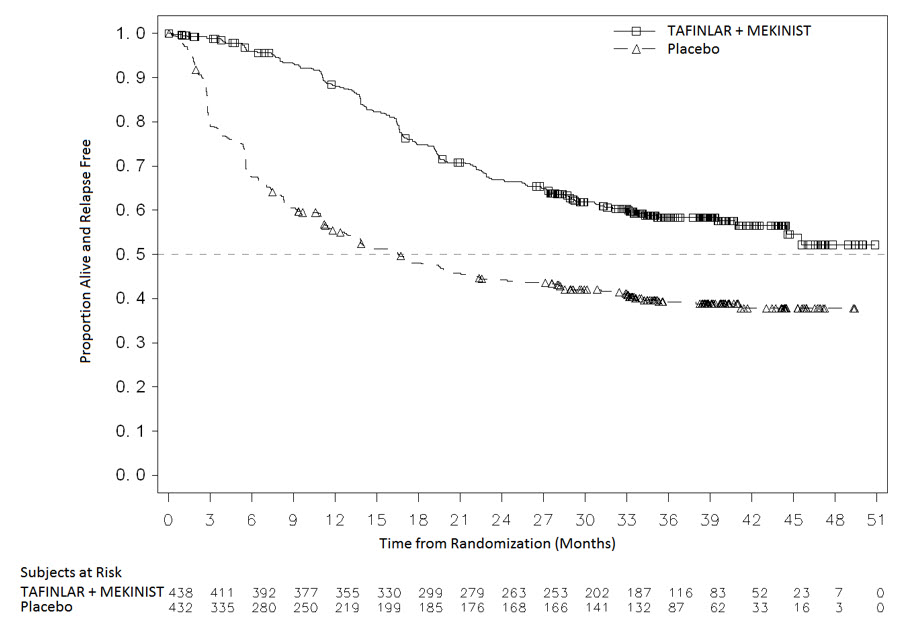
Figure 3. Kaplan-Meier Curves for Relapse-Free Survival in COMBI-AD in the Adjuvant Treatment of Melanoma
14.3 BRAF V600E Mutation-Positive Metastatic Non-Small Cell Lung Cancer
The safety and efficacy of dabrafenib alone or administered with MEKINIST were evaluated in a multicenter, three-cohort, non-randomized, activity-estimating, open-label trial (Study BRF113928; NCT01336634). Key eligibility criteria were locally confirmed BRAF V600E mutation-positive metastatic NSCLC, no prior exposure to BRAF or MEK inhibitor, and absence of EGFR mutation or ALK rearrangement (unless patients had progression on prior tyrosine kinase inhibitor therapy). Patients enrolled in Cohorts A and B were required to have received at least one previous platinum-based chemotherapy regimen with demonstrated disease progression but no more than three prior systemic regimens. Patients in Cohort C could not have received prior systemic therapy for metastatic disease. Patients in Cohort A received dabrafenib 150 mg twice daily. Patients in Cohorts B and C received MEKINIST 2 mg once daily and dabrafenib 150 mg twice daily. The major efficacy outcome was ORR per RECIST v1.1 as assessed by independent review committee (IRC) and duration of response.
There were a total of 171 patients enrolled, which included 78 patients enrolled in Cohort A, 57 patients enrolled in Cohort B, and 36 patients enrolled in Cohort C. The characteristics of the population were: a median age of 66 years; 48% male; 81% white, 14% Asian, 3% black, and 2% Hispanic; 60% former smokers, 32% never smokers, and 8% current smokers; 27% had ECOG performance status (PS) of 0, 63% had ECOG PS of 1, and 11% had ECOG PS of 2; 99% had metastatic disease of which 6% had brain metastasis at baseline and 14% had liver metastasis at baseline; 11% had systemic anti-cancer therapy in the adjuvant setting, 58% of the 135 previously treated patients had only one line of prior systemic therapy for metastatic disease; 98% had non-squamous histology.
Efficacy results are summarized in Table 14.
Table 14. Efficacy Results Based on Independent Review in Study BRF113928 Abbreviations: CI, confidence interval; DoR, duration of response; NE, not estimable. Treatment Dabrafenib MEKINIST plus Dabrafenib Population Previously Treated
N = 78Previously Treated
N = 57Treatment Naïve
N = 36Overall Response Rate ORR (95% CI) 27% (18%, 38%) 63% (49%, 76%) 61% (44%, 77%) Complete Response 1% 4% 3% Partial Response 26% 60% 58% Duration of Response n = 21 n = 36 n = 22 Median DoR, months (95% CI) 9.9 (4.2, NE) 12.6 (5.8, NE) NE (6.9, NE) % with DoR ≥ 6 months 52% 64% 59% In a subgroup analysis of patients with retrospectively centrally confirmed BRAF V600E mutation-positive NSCLC with the Oncomine™ Dx Target Test, the ORR results were similar to those presented in Table 14.
14.4 BRAF V600E Mutation-Positive Locally Advanced or Metastatic Anaplastic Thyroid Cancer
The safety and efficacy of MEKINIST administered with dabrafenib was evaluated in an activity-estimating, nine-cohort, multi-center, non-randomized, open-label trial (Study BRF117019; NCT02034110) in patients with rare cancers with the BRAF V600E mutation, including locally advanced, unresectable, or metastatic ATC with no standard locoregional treatment options. Trial BRF117019 excluded patients who could not swallow or retain the medication; who received prior treatment with BRAF or MEK inhibitors; with symptomatic or untreated CNS metastases; or who had airway obstruction. Patients received MEKINIST 2 mg once daily and dabrafenib 150 mg twice daily. The major efficacy outcome measure was ORR per RECIST v1.1 as assessed by independent review committee (IRC) and duration of response (DoR).
At the time of efficacy analysis, 23 patients were evaluable for response in the ATC cohort. Three additional patients were enrolled; however, there was insufficient time to assess response of these patients. Among the 26 patients enrolled, the median age was 70 years (range: 49-85); 50% were male, 50% white, 46% Asian; 100% had ECOG performance status of 0 or 1; and 54% had a prior history of differentiated thyroid cancer. Prior anti-cancer treatments included surgery (92%), external beam radiotherapy (81%), and systemic therapy (54%).
Efficacy results are summarized in Table 15.
Table 15. Efficacy Results in the ATC Cohort Based on Independent Review of Study BRF117019 Abbreviations: ATC, anaplastic thyroid cancer; CI, confidence interval; DoR, duration of response; ORR, overall response rate. ATC Cohort Population (evaluable for response) N = 23 Overall Response Rate ORR (95% CI) 61% (39%, 80%) Complete Response 4% Partial Response 57% Duration of Response % with DoR ≥ 6 months 64% 14.5 Lack of Clinical Activity in Metastatic Melanoma Following BRAF-Inhibitor Therapy
The clinical activity of MEKINIST as a single agent was evaluated in a single-arm, multicenter, international trial in 40 patients with BRAF V600E or V600K mutation-positive, unresectable or metastatic melanoma who had received prior treatment with a BRAF inhibitor. All patients received MEKINIST at a dose of 2 mg orally once daily until disease progression or unacceptable toxicity.
The median age was 58 years, 63% were male, all were white, 98% had baseline ECOG PS of 0 or 1, and the distribution of BRAF V600 mutations was V600E (83%), V600K (10%), and the remaining patients had multiple V600 mutations (5%), or unknown mutational status (2%). No patient achieved a confirmed partial or complete response as determined by the clinical investigators.
-
16
HOW SUPPLIED/STORAGE AND HANDLING
0.5 mg tablets: Yellow, modified oval, biconvex, film-coated tablets with ‘GS’ debossed on one face and ‘TFC’ on the opposing face and are available in bottles of 30 (NDC: 0078-0666-15).
2 mg tablets: Pink, round, biconvex, film-coated tablets with ‘GS’ debossed on one face and ‘HMJ’ on the opposing face and are available in bottles of 30 (NDC: 0078-0668-15).
Store refrigerated at 2°C to 8°C (36°F to 46°F). Dispense in original bottle. Do not remove desiccant. Protect from moisture and light. Do not place medication in pill boxes.
-
17
PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
New Cutaneous and Non-cutaneous Malignancies
Advise patients that MEKINIST administered with dabrafenib can result in the development of new primary cutaneous and non-cutaneous malignancies. Advise patients to contact their doctor immediately for any new lesions, changes to existing lesions on their skin, or other signs and symptoms of malignancies [see Warnings and Precautions (5.1)].
Hemorrhage
Advise patients that MEKINIST administered with dabrafenib increases the risk of intracranial and gastrointestinal hemorrhage. Advise patients to contact their healthcare provider to seek immediate medical attention for signs or symptoms of unusual bleeding or hemorrhage [see Warnings and Precautions (5.2)].
Colitis and Gastrointestinal Perforation
Advise patients that MEKINIST can cause colitis and gastrointestinal perforation and to contact their healthcare provider for signs or symptoms of colitis or gastrointestinal perforation [see Warnings and Precautions (5.3)].
Venous Thrombosis
Advise patients that MEKINIST administered with dabrafenib increases the risks of PE and DVT. Advise patients to seek immediate medical attention for sudden onset of difficulty breathing, leg pain, or swelling [see Warnings and Precautions (5.4)].
Cardiomyopathy
Advise patients that MEKINIST can cause cardiomyopathy and to immediately report any signs or symptoms of heart failure to their healthcare provider [see Warnings and Precautions (5.5)].
Retinal Pigment Epithelial Detachment
Advise patients that MEKINIST can cause severe visual disturbances that can lead to blindness and to contact their healthcare provider if they experience any changes in their vision [see Warnings and Precautions (5.6)].
Interstitial Lung Disease
Advise patients that MEKINIST can cause ILD (or pneumonitis). Advise patients to contact their healthcare provider as soon as possible if they experience signs such as cough or dyspnea [see Warnings and Precautions (5.7)].
Serious Febrile Reactions
Advise patients that MEKINIST administered with dabrafenib can cause serious febrile reactions. Instruct patients to contact their healthcare provider if they develop fever while taking MEKINIST with dabrafenib [see Warnings and Precautions (5.8)].
Serious Skin Toxicities
Advise patients that MEKINIST can cause serious skin toxicities which may require hospitalization and to contact their healthcare provider for progressive or intolerable rash [see Warnings and Precautions (5.9)].
Hypertension
Advise patients that MEKINIST can cause hypertension and that they need to undergo blood pressure monitoring and to contact their healthcare provider if they develop symptoms of hypertension such as severe headache, blurry vision, or dizziness.
Diarrhea
Advise patients that MEKINIST often causes diarrhea which may be severe in some cases. Inform patients of the need to contact their healthcare provider if severe diarrhea occurs during treatment.
Embryo-Fetal Toxicity
- Advise pregnant women and males of reproductive potential of the potential risk to a fetus [see Warnings and Precautions (5.12), Use in Specific Populations (8.1, 8.3)].
- Advise females to contact their healthcare provider of a known or suspected pregnancy.
- Advise females of reproductive potential to use effective contraception during treatment with MEKINIST and for 4 months after the last dose.
- Advise male patients with female partners of reproductive potential to use condoms during treatment with MEKINIST and for at least 4 months after the last dose.
Lactation
Advise women not to breastfeed during treatment with MEKINIST and for 4 months after the last dose [see Use in Specific Populations (8.2)].
Infertility
Advise females of reproductive potential of the potential risk for impaired fertility [see Use in Specific Populations (8.3)].
Administration
MEKINIST should be taken at least 1 hour before or at least 2 hours after a meal [see Dosage and Administration (2.6)].
THxID BRAF™ assay is a trademark of bioMérieux.
Oncomine™ Dx Target Test is a trademark of Life Technologies Corporation, a part of Thermo Fisher Scientific Inc.
Distributed by:
Novartis Pharmaceuticals Corporation
East Hanover, New Jersey 07936© Novartis
T2019-114
-
PATIENT PACKAGE INSERT
This Patient Information has been approved by the U.S. Food and Drug Administration. Revised: July 2019 Patient Information
MEKINIST® (MEK-in-ist)
(trametinib)
tabletsImportant information: If your healthcare provider prescribes MEKINIST for you to be taken with dabrafenib, also read the Medication Guide that comes with dabrafenib. What is the most important information I should know about MEKINIST?
MEKINIST may cause serious side effects, including:
Risk of new skin cancers. MEKINIST, when used with dabrafenib, may cause skin cancers, called cutaneous squamous cell carcinoma, keratoacanthoma, basal cell carcinoma, or melanoma.
Talk to your healthcare provider about your risk for these cancers.
Check your skin and tell your healthcare provider right away about any skin changes including a:- new wart
- skin sore or reddish bump that bleeds or does not heal
- change in size or color of a mole
Your healthcare provider should also check for cancers that may not occur on the skin. Tell your healthcare provider about any new symptoms that develop during treatment with MEKINIST with dabrafenib.
See "What are the possible side effects of MEKINIST?" for more information about side effects.What is MEKINIST?
MEKINIST is a prescription medicine used:
- alone or in combination with a medicine called dabrafenib to treat a type of skin cancer called melanoma:
○ that has spread to other parts of the body or cannot be removed by surgery, and
○ that has a certain type of abnormal “BRAF” gene. - in combination with dabrafenib, to help prevent melanoma that has a certain type of abnormal “BRAF” gene from coming back after the cancer has been removed by surgery.
- in combination with dabrafenib to treat a type of lung cancer called non-small cell lung cancer (NSCLC)
○ that has spread to other parts of the body, and
○ that has a certain type of abnormal “BRAF” gene.
- in combination with dabrafenib to treat a type of thyroid cancer called anaplastic thyroid cancer (ATC)
○ that has spread to other parts of the body and you have no satisfactory treatment options, and
○ that has a certain type of abnormal “BRAF” gene
It is not known if MEKINIST alone or MEKINIST with dabrafenib is safe and effective in children.Before you take MEKINIST, tell your healthcare provider about all of your medical conditions, including if you:
- have had bleeding problems or blood clots
- have stomach problems
- have inflammation of the colon
- have heart problems
- have eye problems
- have lung or breathing problems
- have high blood pressure (hypertension)
- have liver or kidney problems
- have diabetes
- are a male (including one who has had a vasectomy) with a female partner of reproductive potential.
○ Males (including those who have had a vasectomy) should use condoms during sexual intercourse during treatment with MEKINIST and for at least 4 months after your last dose of MEKINIST. - are pregnant or plan to become pregnant. MEKINIST can harm your unborn baby.
○ Females who are able to become pregnant should use effective birth control (contraception) during treatment with MEKINIST and for 4 months after your last dose of MEKINIST.
○ Talk to your healthcare provider about birth control methods that may be right for you during this time.
○ Tell your healthcare provider right away if you become pregnant or think you might be pregnant during treatment with MEKINIST.
- are breastfeeding or plan to breastfeed. It is not known if MEKINIST passes into your breast milk.
○ Do not breastfeed during treatment and for 4 months after your last dose of MEKINIST. Talk to your healthcare provider about the best way to feed your baby during this time.
Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.How should I take MEKINIST? - Take MEKINIST exactly as your healthcare provider tells you to take it. Do not change your dose or stop MEKINIST unless your healthcare provider tells you.
- Your healthcare provider may change your dose of MEKINIST, temporarily stop, or completely stop your treatment with MEKINIST if you develop certain side effects.
- Take MEKINIST one time a day, about every 24 hours.
- Take MEKINIST at least 1 hour before or 2 hours after a meal.
- If you miss a dose, take it as soon as you remember. If it is less than 12 hours before your next scheduled dose, skip the missed dose. Just take the next dose at your regular time.
What are the possible side effects of MEKINIST?
MEKINIST may cause serious side effects, including:
-
See “What is the most important information I should know about MEKINIST?”
-
bleeding problems. MEKINIST can cause serious bleeding problems, especially in your brain or stomach, that can lead to death. Call your healthcare provider and get medical help right away if you have any signs of bleeding, including:
○ headaches, dizziness, or feeling weak
○ cough up blood or blood clots
○ vomit blood or your vomit looks like “coffee grounds”
○ red or black stools that look like tar
-
inflammation of the intestines, or tears (perforation) of the stomach or intestines. MEKINIST can cause inflammation of your intestines, or tears in the stomach or intestines that can lead to death. Tell your healthcare provider immediately if you have any of the following symptoms:
○ bleeding. see “bleeding problems” above
○ diarrhea (loose stools) or more bowel movements than usual
○ stomach-area (abdomen) pain or tenderness
○ fever
○ nausea
-
blood clots. MEKINIST can cause blood clots in your arms or legs, which can travel to your lungs and can lead to death. Get medical help right away if you have the following symptoms:
○ chest pain
○ sudden shortness of breath or trouble breathing
○ pain in your legs with or without swelling
○ swelling in your arms or legs
○ a cool pale arm or leg
-
heart problems, including heart failure. Your healthcare provider should check your heart function before and during treatment with MEKINIST. Call your healthcare provider right away if you have any of the following signs and symptoms of a heart problem:
○ feeling like your heart is pounding or racing
○ shortness of breath
○ swelling of your ankles and feet
○ feeling lightheaded
-
eye problems. MEKINIST can cause severe eye problems that might lead to blindness. Call your healthcare provider right away if you get these symptoms of eye problems:
○ blurred vision, loss of vision, or other vision changes
○ see color dots
○ halo (seeing blurred outline around objects)
○ eye pain, swelling, or redness
-
lung or breathing problems. MEKINIST can cause lung or breathing problems. Tell your healthcare provider if you have any new or worsening symptoms of lung or breathing problems, including:
○ shortness of breath
○ cough
-
fever. Fever is common during treatment with MEKINIST and dabrafenib, but it may also be serious. When taking MEKINIST with dabrafenib, fever may happen more often or may be more severe. In some cases, chills or shaking chills, too much fluid loss (dehydration), low blood pressure, dizziness, or kidney problems may happen with the fever. Call your healthcare provider right away if you get a fever during treatment with MEKINIST.
-
serious skin reactions. Rash is a common side effect of MEKINIST. MEKINIST can also cause other skin reactions. In some cases these rashes and other skin reactions can be severe or serious, and may need to be treated in a hospital. Call your healthcare provider if you get any of the following symptoms:
○ skin rash that bothers you or does not go away
○ acne
○ redness, swelling, peeling, or tenderness of hands or feet
○ skin redness
-
increased blood sugar (hyperglycemia). Some people may develop high blood sugar or worsening diabetes during treatment with MEKINIST and dabrafenib. If you are diabetic, your healthcare provider should check your blood sugar levels closely during treatment with MEKINIST and dabrafenib. Your diabetes medicine may need to be changed. Tell your healthcare provider if you have any of the following symptoms of severe high blood sugar:
○ increased thirst
○ urinating more often than normal or urinating an increased amount of urine
- rash
- diarrhea. Call your healthcare provider if you get severe diarrhea.
- swelling of the face, arms, or legs
fever diarrhea rash vomiting nausea high blood pressure (hypertension) chills swelling of the face, arms, or legs The most common side effects of MEKINIST when taken with dabrafenib to help prevent melanoma from coming back after the cancer has been removed by surgery include: fever chills fatigue diarrhea nausea vomiting headache joint aches rash muscle aches The most common side effects of MEKINIST when taken with dabrafenib in people with NSCLC include: fever rash fatigue swelling of face, arms, and legs nausea chills vomiting bleeding diarrhea cough dry skin shortness of breath decreased appetite MEKINIST can cause new or worsening high blood pressure (hypertension). Your healthcare provider should check your blood pressure during treatment with MEKINIST. Call your healthcare provider right away if you develop high blood pressure, your blood pressure worsens, or you have severe headache, lightheadedness, blurry vision, or dizziness.
MEKINIST may cause fertility problems in females. This could affect your ability to become pregnant. Talk to your healthcare provider if this is a concern for you.
These are not all the possible side effects of MEKINIST.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
You may also report side effects to Novartis Pharmaceuticals Corporation at 1-888-669-6682.How should I store MEKINIST?
- Store MEKINIST in the refrigerator between 36°F to 46°F (2°C to 8°C).
- Keep MEKINIST dry and away from moisture and light.
- The bottle of MEKINIST contains a desiccant packet to help keep your medicine dry. Do not throw away the desiccant packet.
- Keep MEKINIST in its original bottle. Do not place tablets in a pill box.
- Safely throw away MEKINIST that is out of date or no longer needed.
General information about the safe and effective use of MEKINIST.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use MEKINIST for a condition for which it was not prescribed. Do not give MEKINIST to other people, even if they have the same symptoms that you have. It may harm them. You can ask your healthcare provider or pharmacist for information about MEKINIST that is written for health professionals.What are the ingredients in MEKINIST?
Active ingredient: trametinib
Inactive ingredients:
Tablet Core: colloidal silicon dioxide, croscarmellose sodium, hypromellose, magnesium stearate (vegetable source), mannitol, microcrystalline cellulose, sodium lauryl sulfate.
Tablet Coating: hypromellose, iron oxide red (2 mg tablets), iron oxide yellow (0.5 mg tablets), polyethylene glycol, polysorbate 80 (2 mg tablets), titanium dioxide.
Novartis Pharmaceuticals Corporation, East Hanover, New Jersey 07936
For more information, go to www.MEKINIST.com or call 1-888-669-6682.
© Novartis
T2019-83 - new wart
-
PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL
NDC: 0078-0666-15
Mekinist®
(trametinib) Tablets
0.5 mg*
Rx only
30 Tablets
Novartis
-
PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL
NDC: 0078-0668-15
Mekinist®
(trametinib) Tablets
2 mg*
Rx only
30 Tablets
Novartis
-
INGREDIENTS AND APPEARANCE
MEKINIST
trametinib tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0078-0666 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TRAMETINIB DIMETHYL SULFOXIDE (UNII: BSB9VJ5TUT) (TRAMETINIB - UNII:33E86K87QN) TRAMETINIB .5 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) HYPROMELLOSES (UNII: 3NXW29V3WO) MAGNESIUM STEARATE (UNII: 70097M6I30) MANNITOL (UNII: 3OWL53L36A) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) SODIUM LAURYL SULFATE (UNII: 368GB5141J) FERRIC OXIDE RED (UNII: 1K09F3G675) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) POLYETHYLENE GLYCOL (UNII: 3WJQ0SDW1A) POLYSORBATE 80 (UNII: 6OZP39ZG8H) Product Characteristics Color YELLOW Score no score Shape OVAL Size 9mm Flavor Imprint Code GS;TFC Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0078-0666-15 30 in 1 BOTTLE; Type 0: Not a Combination Product 03/17/2016 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA204114 03/17/2016 MEKINIST
trametinib tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0078-0668 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TRAMETINIB DIMETHYL SULFOXIDE (UNII: BSB9VJ5TUT) (TRAMETINIB - UNII:33E86K87QN) TRAMETINIB 2 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) HYPROMELLOSES (UNII: 3NXW29V3WO) MAGNESIUM STEARATE (UNII: 70097M6I30) MANNITOL (UNII: 3OWL53L36A) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) SODIUM LAURYL SULFATE (UNII: 368GB5141J) FERRIC OXIDE RED (UNII: 1K09F3G675) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) Product Characteristics Color PINK Score no score Shape ROUND Size 8mm Flavor Imprint Code GS;HMJ Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0078-0668-15 30 in 1 BOTTLE; Type 0: Not a Combination Product 03/17/2016 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA204114 03/17/2016 Labeler - Novartis Pharmaceuticals Corporation (002147023)
Trademark Results [Mekinist]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 MEKINIST 85399275 4448207 Live/Registered |
NOVARTIS PHARMA AG 2011-08-16 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.