MYLERAN® (busulfan) Tablets
MYLERAN by
Drug Labeling and Warnings
MYLERAN by is a Prescription medication manufactured, distributed, or labeled by Woodward Pharma Services LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
MYLERAN- busulfan tablet, film coated
Woodward Pharma Services LLC
----------
MYLERAN®
(busulfan) Tablets
WARNING
MYLERAN is a potent drug. It should not be used unless a diagnosis of chronic myelogenous leukemia has been adequately established and the responsible physician is knowledgeable in assessing response to chemotherapy.
MYLERAN can induce severe bone marrow hypoplasia. Reduce or discontinue the dosage immediately at the first sign of any unusual depression of bone marrow function as reflected by an abnormal decrease in any of the formed elements of the blood. A bone marrow examination should be performed if the bone marrow status is uncertain.
SEE WARNINGS FOR INFORMATION REGARDING BUSULFAN-INDUCED LEUKEMOGENESIS IN HUMANS.
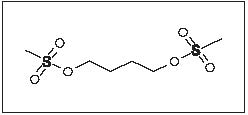
DESCRIPTION
MYLERAN (busulfan) is a bifunctional alkylating agent. Busulfan is known chemically as 1,4-butanediol dimethanesulfonate and has the following structural formula:
CH3SO2O(CH2)4OSO2CH3
Busulfan is not a structural analog of the nitrogen mustards. MYLERAN is available in tablet form for oral administration. Each film-coated tablet contains 2 mg busulfan and the inactive ingredients hypromellose, lactose (anhydrous), magnesium stearate, pregelatinized starch, triacetin, and titanium dioxide.
The activity of busulfan in chronic myelogenous leukemia was first reported by D.A.G. Galton in 1953.
CLINICAL PHARMACOLOGY
Busulfan is a small, highly lipophilic molecule that easily crosses the blood brain barrier. Following absorption, 32% and 47% of busulfan are bound to plasma proteins and red blood cells, respectively.
Busulfan absorption from the gastrointestinal tract is essentially complete. This has been demonstrated in radioactive studies after both intravenous and oral administration of 35S-busulfan, 14C-busulfan, and 3H-busulfan. Following intravenous administration of a single therapeutic dose of 35S-busulfan, there was rapid disappearance of radioactivity from the blood and 90% to 95% of the 35S-label disappeared within 3 to 5 minutes after injection. After either oral or intravenous administration of 35S-busulfan, 45% to 60% of the radioactivity was recovered in the urine in the 48 hours after administration; the majority of the total urinary excretion occurring in the first 24 hours. Over 95% of the urinary 35S-label occurs as 35S-methanesulfonic acid. Oral and intravenous administration of 1,4-14C-busulfan showed the same rapid initial disappearance of plasma radioactivity as observed following the administration of 35S-labeled drug. Cumulative radioactivity in the urine after 48 hours was 25% to 30% of the administered dose (contrasting with 45% to 60% for 35S-busulfan), and suggests a slower excretion of the alkylating portion of the molecule and its metabolites than for the sulfonoxymethyl moieties.
Regardless of the route of administration, 1,4-14C-busulfan yielded a complex mixture of at least 12 radiolabeled metabolites in urine; the main metabolite being 3-hydroxytetrahydrothiophene-1,1-dioxide.
Pharmacokinetic studies employing 3H-busulfan labeled on the tetramethylene chain confirmed a rapid initial clearance of the radioactivity from plasma, irrespective of whether the drug was given orally or intravenously.
A study compared a 2-mg single IV bolus injection to a single oral dose of a 2-mg tablet of nonradioactive busulfan in 8 adult patients 13 to 60 years of age. The study demonstrated that the mean ± SD absolute bioavailability was 80% ± 20% in adults. However, the absolute bioavailability for 8 children 1.5 to 6 years of age was 68% ± 31%.
In another study of 2, 4, and 6 mg of busulfan, given as a single oral dose on consecutive days (starting with the lowest dose) in 5 adult patients, the mean dose-normalized (to 2 mg dose) area under the plasma concentration-time curve (AUC) was about 130 nghr/mL, while the mean intra- and inter-patient variability was about 16% and 21%, respectively. Busulfan was eliminated with a plasma terminal elimination half-life (t1/2) of about 2.6 hours, and demonstrated linear kinetics within the range of 2 to 6 mg for both the maximum plasma concentration (Cmax) and AUC. The mean Cmax for the 2-, 4-, and 6-mg doses (after dose normalization to 2 mg) was about 30 ng/mL. A recent study of 4 to 8 mg as single oral doses in 12 patients showed that the mean ± SD Cmax (after dose normalization to 4 mg) was 68.2 ± 24.4 ng/mL, occurring at about 0.9 hours and the mean ± SD AUC (after dose normalization to 4 mg) was 269 ± 62 nghr/mL. These results are consistent with previous results. In addition, the mean ± SD elimination half-life was 2.69 ± 0.49 hours.
The elimination of busulfan appears to be independent of renal function. This probably reflects the extensive metabolism of the drug in the liver, since less than 2% of the administered dose is excreted in the urine unchanged within 24 hours. The drug is metabolized by enzymatic activity to at least 12 metabolites, among which tetrahydrothiophene, tetrahydrothiophene 12-oxide, sulfolane, and 3-hydroxysulfolane were identified. These metabolites do not have cytotoxic activity.
There is no experience with the use of dialysis in an attempt to modify the clinical toxicity of busulfan. One technical difficulty would derive from the extremely poor water solubility of busulfan.
Additionally, all studies of the metabolism of busulfan employing radiolabeled materials indicate rapid chemical reactivity of the parent compound with prolonged retention of some of the metabolites (particularly the metabolites arising from the “alkylating” portion of the molecule). The effectiveness of dialysis at removing significant quantities of unreacted drug would be expected to be minimal in such a situation. Currently, there are no available data on the effect of food on busulfan bioavailability.
Pharmacokinetics in Hemodialysis Patients
The impact of hemodialysis on the clearance of busulfan was determined in a patient with chronic renal failure undergoing autologous stem cell transplantation. The apparent oral clearance of busulfan during a 4-hour hemodialysis session was increased by 65%, but the 24-hour oral clearance of busulfan was increased by only 11%.
The incidence of veno-occlusive disease was higher (33.3% versus 3.0%) in patients with busulfan AUC0-6hr >1,500 μM.min (Css >900 mcg/L) compared to patients with busulfan AUC0-6hr <1,500 μM.min (Css <900 mcg/L) (see WARNINGS).
Drug Interactions
Itraconazole reduced busulfan clearance by up to 25% in patients receiving itraconazole compared to patients who did not receive itraconazole. Higher busulfan exposure due to concomitant itraconazole could lead to toxic plasma levels in some patients. Fluconazole had no effect on the clearance of busulfan. Patients treated with concomitant cyclophosphamide and busulfan with phenytoin pretreatment have increased cyclophosphamide and busulfan clearance, which may lead to decreased concentrations of both cyclophosphamide and busulfan. However, busulfan clearance may be reduced in the presence of cyclophosphamide alone, presumably due to competition for glutathione.
Diazepam had no effect on the clearance of busulfan.
No information is available regarding the penetration of busulfan into brain or cerebrospinal fluid.
Biochemical Pharmacology
In aqueous media, busulfan undergoes a wide range of nucleophilic substitution reactions. While this chemical reactivity is relatively non-specific, alkylation of the DNA is felt to be an important biological mechanism for its cytotoxic effect. Coliphage T7 exposed to busulfan was found to have the DNA crosslinked by intrastrand crosslinkages, but no interstrand linkages were found.
The metabolic fate of busulfan has been studied in rats and humans using 14C- and 35S-labeled materials. In humans, as in the rat, almost all of the radioactivity in 35S-labeled busulfan is excreted in the urine in the form of 35S-methanesulfonic acid. Roberts and Warwick demonstrated that the formation of methanesulfonic acid in vivo in the rat is not due to a simple hydrolysis of busulfan to 1,4-butanediol, since only about 4% of 2,3-14C-busulfan was excreted as carbon dioxide, whereas 2,3-14C-1,4-butanediol was converted almost exclusively to carbon dioxide. The predominant reaction of busulfan in the rat is the alkylation of sulfhydryl groups (particularly cysteine and cysteine-containing compounds) to produce a cyclic sulfonium compound which is the precursor of the major urinary metabolite of the 4-carbon portion of the molecule, 3-hydroxytetrahydrothiophene-1,1-dioxide. This has been termed a “sulfur-stripping” action of busulfan and it may modify the function of certain sulfur-containing amino acids, polypeptides, and proteins; whether this action makes an important contribution to the cytotoxicity of busulfan is unknown.
The biochemical basis for acquired resistance to busulfan is largely a matter of speculation. Although altered transport of busulfan into the cell is one possibility, increased intracellular inactivation of the drug before it reaches the DNA is also possible. Experiments with other alkylating agents have shown that resistance to this class of compounds may reflect an acquired ability of the resistant cell to repair alkylation damage more effectively.
Clinical Studies
Although not curative, busulfan reduces the total granulocyte mass, relieves symptoms of the disease, and improves the clinical state of the patient. Approximately 90% of adults with previously untreated chronic myelogenous leukemia will obtain hematologic remission with regression or stabilization of organomegaly following the use of busulfan. It has been shown to be superior to splenic irradiation with respect to survival times and maintenance of hemoglobin levels, and to be equivalent to irradiation at controlling splenomegaly.
It is not clear whether busulfan unequivocally prolongs the survival of responding patients beyond the 31 months experienced by an untreated group of historical controls. Median survival figures of 31 to 42 months have been reported for several groups of patients treated with busulfan, but concurrent control groups of comparable, untreated patients are not available. The median survival figures reported from different studies will be influenced by the percentage of “poor risk” patients initially entered into the particular study. Patients who are alive 2 years following the diagnosis of chronic myelogenous leukemia, and who have been treated during that period with busulfan, are estimated to have a mean annual mortality rate during the second to fifth year which is approximately two thirds that of patients who received either no treatment, conventional x-ray or 32P-irradiation, or chemotherapy with minimally active drugs.
Busulfan is clearly less effective in patients with chronic myelogenous leukemia who lack the Philadelphia (Ph1) chromosome. Also, the so-called “juvenile” type of chronic myelogenous leukemia, typically occurring in young children and associated with the absence of a Philadelphia chromosome, responds poorly to busulfan. The drug is of no benefit in patients whose chronic myelogenous leukemia has entered a “blastic” phase.
MYLERAN should not be used in patients whose chronic myelogenous leukemia has demonstrated prior resistance to this drug.
MYLERAN is of no value in chronic lymphocytic leukemia, acute leukemia, or in the “blastic crisis” of chronic myelogenous leukemia.
INDICATIONS AND USAGE
MYLERAN (busulfan) is indicated for the palliative treatment of chronic myelogenous (myeloid, myelocytic, granulocytic) leukemia.
CONTRAINDICATIONS
MYLERAN is contraindicated in patients in whom a definitive diagnosis of chronic myelogenous leukemia has not been firmly established.
MYLERAN is contraindicated in patients who have previously suffered a hypersensitivity reaction to busulfan or any other component of the preparation.
WARNINGS
The most frequent, serious side effect of treatment with busulfan is the induction of bone marrow failure (which may or may not be anatomically hypoplastic) resulting in severe pancytopenia. The pancytopenia caused by busulfan may be more prolonged than that induced with other alkylating agents. It is generally felt that the usual cause of busulfan-induced pancytopenia is the failure to stop administration of the drug soon enough; individual idiosyncrasy to the drug does not seem to be an important factor. MYLERAN should be used with extreme caution and exceptional vigilance in patients whose bone marrow reserve may have been compromised by prior irradiation or chemotherapy, or whose marrow function is recovering from previous cytotoxic therapy. Although recovery from busulfan-induced pancytopenia may take from 1 month to 2 years, this complication is potentially reversible, and the patient should be vigorously supported through any period of severe pancytopenia.
A rare, important complication of busulfan therapy is the development of bronchopulmonary dysplasia with pulmonary fibrosis. Symptoms have been reported to occur within 8 months to 10 years after initiation of therapy—the average duration of therapy being 4 years. The histologic findings associated with “busulfan lung” mimic those seen following pulmonary irradiation. Clinically, patients have reported the insidious onset of cough, dyspnea, and low-grade fever. In some cases, however, onset of symptoms may be acute. Pulmonary function studies have revealed diminished diffusion capacity and decreased pulmonary compliance. It is important to exclude more common conditions (such as opportunistic infections or leukemic infiltration of the lungs) with appropriate diagnostic techniques. If measures such as sputum cultures, virologic studies, and exfoliative cytology fail to establish an etiology for the pulmonary infiltrates, lung biopsy may be necessary to establish the diagnosis. Treatment of established busulfan-induced pulmonary fibrosis is unsatisfactory; in most cases the patients have died within 6 months after the diagnosis was established. There is no specific therapy for this complication. MYLERAN should be discontinued if this lung toxicity develops. The administration of corticosteroids has been suggested, but the results have not been impressive or uniformly successful.
Busulfan may cause cellular dysplasia in many organs in addition to the lung. Cytologic abnormalities characterized by giant, hyperchromatic nuclei have been reported in lymph nodes, pancreas, thyroid, adrenal glands, liver, and bone marrow. This cytologic dysplasia may be severe enough to cause difficulty in interpretation of exfoliative cytologic examinations from the lung, bladder, breast, and the uterine cervix.
In addition to the widespread epithelial dysplasia that has been observed during busulfan therapy, chromosome aberrations have been reported in cells from patients receiving busulfan. Busulfan is mutagenic in mice and, possibly, in humans. Malignant tumors and acute leukemias have been reported in patients who have received busulfan therapy, and this drug may be a human carcinogen. The World Health Organization has concluded that there is a causal relationship between busulfan exposure and the development of secondary malignancies. Four cases of acute leukemia occurred among 243 patients treated with busulfan as adjuvant chemotherapy following surgical resection of bronchogenic carcinoma. All 4 cases were from a subgroup of 19 of these 243 patients who developed pancytopenia while taking busulfan 5 to 8 years before leukemia became clinically apparent. These findings suggest that busulfan is leukemogenic, although its mode of action is uncertain.
Ovarian suppression and amenorrhea with menopausal symptoms commonly occur during busulfan therapy in premenopausal patients. Busulfan has been associated with ovarian failure including failure to achieve puberty in females. Busulfan interferes with spermatogenesis in experimental animals, and there have been clinical reports of sterility, azoospermia, and testicular atrophy in male patients.
Hepatic veno-occlusive disease, which may be life threatening, has been reported in patients receiving busulfan, usually in combination with cyclophosphamide or other chemotherapeutic agents prior to bone marrow transplantation. Possible risk factors for the development of hepatic veno-occlusive disease include: total busulfan dose exceeding 16 mg/kg based on ideal body weight, and concurrent use of multiple alkylating agents (see CLINICAL PHARMACOLOGY and Drug Interactions).
A clear cause-and-effect relationship with busulfan has not been demonstrated. Periodic measurement of serum transaminases, alkaline phosphatase, and bilirubin is indicated for early detection of hepatotoxicity. A reduced incidence of hepatic veno-occlusive disease and other regimen-related toxicities have been observed in patients treated with high-dose MYLERAN and cyclophosphamide when the first dose of cyclophosphamide has been delayed for >24 hours after the last dose of busulfan (see CLINICAL PHARMACOLOGY and Drug Interactions).
Cardiac tamponade has been reported in a small number of patients with thalassemia (2% in one series) who received busulfan and cyclophosphamide as the preparatory regimen for bone marrow transplantation. In this series, the cardiac tamponade was often fatal. Abdominal pain and vomiting preceded the tamponade in most patients.
Pregnancy
Busulfan may cause fetal harm when administered to a pregnant woman. Although there have been a number of cases reported where apparently normal children have been born after busulfan treatment during pregnancy, one case has been cited where a malformed baby was delivered by a mother treated with busulfan. During the pregnancy that resulted in the malformed infant, the mother received x-ray therapy early in the first trimester, mercaptopurine until the third month, then busulfan until delivery. In pregnant rats, busulfan produces sterility in both male and female offspring due to the absence of germinal cells in testes and ovaries. Germinal cell aplasia or sterility in offspring of mothers receiving busulfan during pregnancy has not been reported in humans. There are no adequate and well-controlled studies in pregnant women. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus. Women of childbearing potential should be advised to avoid becoming pregnant.
PRECAUTIONS
General
The most consistent, dose-related toxicity is bone marrow suppression. This may be manifest by anemia, leukopenia, thrombocytopenia, or any combination of these. It is imperative that patients be instructed to report promptly the development of fever, sore throat, signs of local infection, bleeding from any site, or symptoms suggestive of anemia. Any one of these findings may indicate busulfan toxicity; however, they may also indicate transformation of the disease to an acute “blastic” form. Since busulfan may have a delayed effect, it is important to withdraw the medication temporarily at the first sign of an abnormally large or exceptionally rapid fall in any of the formed elements of the blood. Patients should never be allowed to take the drug without close medical supervision.
Seizures have been reported in patients receiving busulfan. As with any potentially epileptogenic drug, caution should be exercised when administering busulfan to patients with a history of seizure disorder, head trauma, or receiving other potentially epileptogenic drugs. Some investigators have used prophylactic anticonvulsant therapy in this setting.
Information for Patients
Patients beginning therapy with busulfan should be informed of the importance of having periodic blood counts and to immediately report any unusual fever or bleeding. Aside from the major toxicity of myelosuppression, patients should be instructed to report any difficulty in breathing, persistent cough, or congestion. They should be told that diffuse pulmonary fibrosis is an infrequent, but serious and potentially life-threatening complication of long-term busulfan therapy. Patients should be alerted to report any signs of abrupt weakness, unusual fatigue, anorexia, weight loss, nausea and vomiting, and melanoderma that could be associated with a syndrome resembling adrenal insufficiency. Patients should never be allowed to take the drug without medical supervision and they should be informed that other encountered toxicities to busulfan include infertility, amenorrhea, skin hyperpigmentation, drug hypersensitivity, dryness of the mucous membranes, and rarely, cataract formation. Women of childbearing potential should be advised to avoid becoming pregnant. The increased risk of a second malignancy should be explained to the patient.
Laboratory Tests
It is recommended that evaluation of the hemoglobin or hematocrit, total white blood cell count and differential count, and quantitative platelet count be obtained weekly while the patient is on busulfan therapy. In cases where the cause of fluctuation in the formed elements of the peripheral blood is obscure, bone marrow examination may be useful for evaluation of marrow status. A decision to increase, decrease, continue, or discontinue a given dose of busulfan must be based not only on the absolute hematologic values, but also on the rapidity with which changes are occurring. The dosage of busulfan may need to be reduced if this agent is combined with other drugs whose primary toxicity is myelosuppression. Occasional patients may be unusually sensitive to busulfan administered at standard dosage and suffer neutropenia or thrombocytopenia after a relatively short exposure to the drug. Busulfan should not be used where facilities for complete blood counts, including quantitative platelet counts, are not available at weekly (or more frequent) intervals.
Drug Interactions
Busulfan may cause additive myelosuppression when used with other myelosuppressive drugs.
In one study, 12 of approximately 330 patients receiving continuous busulfan and thioguanine therapy for treatment of chronic myelogenous leukemia were found to have portal hypertension and esophageal varices associated with abnormal liver function tests. Subsequent liver biopsies were performed in 4 of these patients, all of which showed evidence of nodular regenerative hyperplasia. Duration of combination therapy prior to the appearance of esophageal varices ranged from 6 to 45 months. With the present analysis of the data, no cases of hepatotoxicity have appeared in the busulfan-alone arm of the study. Long-term continuous therapy with thioguanine and busulfan should be used with caution.
Busulfan-induced pulmonary toxicity may be additive to the effects produced by other cytotoxic agents.
The concomitant systemic administration of itraconazole to patients receiving high-dose MYLERAN may result in reduced busulfan clearance (see CLINICAL PHARMACOLOGY). Patients should be monitored for signs of busulfan toxicity when itraconazole is used concomitantly with MYLERAN.
Carcinogenesis, Mutagenesis, Impairment of Fertility
See WARNINGS section. The World Health Organization has concluded that there is a causal relationship between busulfan exposure and the development of secondary malignancies.
Pregnancy
Teratogenic Effects: See WARNINGS section.
Nonteratogenic Effects: There have been reports in the literature of small infants being born after the mothers received busulfan during pregnancy, in particular, during the third trimester. One case was reported where an infant had mild anemia and neutropenia at birth after busulfan was administered to the mother from the eighth week of pregnancy to term.
Lactation
It is not known whether this drug is excreted in human milk. Because of the potential for tumorigenicity shown for busulfan in animal and human studies, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Geriatric Use
Clinical studies of busulfan did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
ADVERSE REACTIONS
To report SUSPECTED ADVERSE REACTIONS, contact Woodward Pharma Services LLC Toll-Free at 1-888-514-4727 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Hematological Effects
The most frequent, serious, toxic effect of busulfan is dose-related myelosuppression resulting in leukopenia, thrombocytopenia, and anemia. Myelosuppression is most frequently the result of a failure to discontinue dosage in the face of an undetected decrease in leukocyte or platelet counts.
Aplastic anemia (sometimes irreversible) has been reported rarely, often following long-term conventional doses and also high doses of MYLERAN.
Pulmonary
Interstitial pulmonary fibrosis has been reported rarely, but it is a clinically significant adverse effect when observed and calls for immediate discontinuation of further administration of the drug. The role of corticosteroids in arresting or reversing the fibrosis has been reported to be beneficial in some cases and without effect in others.
Cardiac
Cardiac tamponade has been reported in a small number of patients with thalassemia who received busulfan and cyclophosphamide as the preparatory regimen for bone marrow transplantation (see WARNINGS).
One case of endocardial fibrosis has been reported in a 79-year-old woman who received a total dose of 7,200 mg of busulfan over a period of 9 years for the management of chronic myelogenous leukemia. At autopsy, she was found to have endocardial fibrosis of the left ventricle in addition to interstitial pulmonary fibrosis.
Ocular
Busulfan is capable of inducing cataracts in rats and there have been several reports indicating that this is a rare complication in humans.
Dermatologic
Hyperpigmentation is the most common adverse skin reaction and occurs in 5% to 10% of patients, particularly those with a dark complexion.
Metabolic
In a few cases, a clinical syndrome closely resembling adrenal insufficiency and characterized by weakness, severe fatigue, anorexia, weight loss, nausea and vomiting, and melanoderma has developed after prolonged busulfan therapy. The symptoms have sometimes been reversible when busulfan was withdrawn. Adrenal responsiveness to exogenously administered ACTH has usually been normal. However, pituitary function testing with metyrapone revealed a blunted urinary 17-hydroxycorticosteroid excretion in 2 patients. Following the discontinuation of busulfan (which was associated with clinical improvement), rechallenge with metyrapone revealed normal pituitary-adrenal function.
Hyperuricemia and/or hyperuricosuria are not uncommon in patients with chronic myelogenous leukemia. Additional rapid destruction of granulocytes may accompany the initiation of chemotherapy and increase the urate pool. Adverse effects can be minimized by increased hydration, urine alkalinization, and the prophylactic administration of a xanthine oxidase inhibitor such as allopurinol.
Hepatic Effects
Esophageal varices have been reported in patients receiving continuous busulfan and thioguanine therapy for treatment of chronic myelogenous leukemia (see PRECAUTIONS: Drug Interactions). Hepatic veno-occlusive disease has been observed in patients receiving busulfan (see WARNINGS).
Miscellaneous
Other reported adverse reactions include: urticaria, erythema multiforme, erythema nodosum, alopecia, porphyria cutanea tarda, excessive dryness and fragility of the skin with anhidrosis, dryness of the oral mucous membranes and cheilosis, gynecomastia, cholestatic jaundice, and myasthenia gravis. Most of these are single case reports, and in many, a clear cause-and-effect relationship with busulfan has not been demonstrated.
Seizures (see PRECAUTIONS: General) have been observed in patients receiving higher than recommended doses of busulfan.
Observed During Clinical Practice
The following events have been identified during post-approval use of busulfan. Because they are reported voluntarily from a population of unknown size, estimates of frequency cannot be made. These events have been chosen for inclusion due to a combination of their seriousness, frequency of reporting, or potential causal connection to busulfan.
Blood and Lymphatic: Aplastic anemia.
Eye: Cataracts, corneal thinning, lens changes.
Hepatobiliary Tract and Pancreas: Centrilobular sinusoidal fibrosis, hepatic veno-occlusive disease, hepatocellular atrophy, hepatocellular necrosis, hyperbilirubinemia (see WARNINGS).
Non-site Specific: Infection, mucositis, sepsis.
Respiratory: Pneumonia.
Skin: Rash. An increased local cutaneous reaction has been observed in patients receiving radiotherapy soon after busulfan.
OVERDOSAGE
There is no known antidote to busulfan. The principal toxic effects are bone marrow depression and pancytopenia. The hematologic status should be closely monitored and vigorous supportive measures instituted if necessary. Induction of vomiting or gastric lavage followed by administration of charcoal would be indicated if ingestion were recent. Dialysis may be considered in the management of overdose as there is 1 report of successful dialysis of busulfan (see CLINICAL PHARMACOLOGY).
Gastrointestinal toxicity with mucositis, nausea, vomiting, and diarrhea has been observed when MYLERAN was used in association with bone marrow transplantation.
Oral LD50 single doses in mice are 120 mg/kg. Two distinct types of toxic response are seen at median lethal doses given intraperitoneally. Within a matter of hours there are signs of stimulation of the central nervous system with convulsions and death on the first day. Mice are more sensitive to this effect than are rats. With doses at the LD50 there is also delayed death due to damage to the bone marrow. At 3 times the LD50, atrophy of the mucosa of the large intestine is found after a week, whereas that of the small intestine is little affected. After doses in the order of 10 times those used therapeutically were added to the diet of rats, irreversible cataracts were produced after several weeks. Small doses had no such effect.
DOSAGE AND ADMINISTRATION
Busulfan is administered orally. The usual adult dose range for remission induction is 4 to 8 mg, total dose, daily. Dosing on a weight basis is the same for both pediatric patients and adults, approximately 60 mcg/kg of body weight or 1.8 mg/m2 of body surface, daily. Since the rate of fall of the leukocyte count is dose related, daily doses exceeding 4 mg per day should be reserved for patients with the most compelling symptoms; the greater the total daily dose, the greater is the possibility of inducing bone marrow aplasia.
A decrease in the leukocyte count is not usually seen during the first 10 to 15 days of treatment; the leukocyte count may actually increase during this period and it should not be interpreted as resistance to the drug, nor should the dose be increased. Since the leukocyte count may continue to fall for more than 1 month after discontinuing the drug, it is important that busulfan be discontinued prior to the total leukocyte count falling into the normal range. When the total leukocyte count has declined to approximately 15,000/mcL, the drug should be withheld.
With a constant dose of busulfan, the total leukocyte count declines exponentially; a weekly plot of the leukocyte count on semi-logarithmic graph paper aids in predicting the time when therapy should be discontinued. With the recommended dose of busulfan, a normal leukocyte count is usually achieved in 12 to 20 weeks.
During remission, the patient is examined at monthly intervals and treatment resumed with the induction dosage when the total leukocyte count reaches approximately 50,000/mcL. When remission is shorter than 3 months, maintenance therapy of 1 to 3 mg daily may be advisable in order to keep the hematological status under control and prevent rapid relapse.
Procedures for proper handling and disposal of anticancer drugs should be considered. Several guidelines on this subject have been published.1-8
There is no general agreement that all of the procedures recommended in the guidelines are necessary or appropriate.
HOW SUPPLIED
MYLERAN is supplied as white, film-coated, round, biconvex tablets containing 2 mg busulfan in amber glass bottles with child-resistant closures. One side is imprinted with "GX EF3" and the other side is imprinted with an "M.”
Bottle of 25 (NDC: 69784-620-25).
Store at 25°C (77°F); excursions permitted to 15° to 30°C (59° to 86°F) (see USP Controlled Room Temperature).
REFERENCES
1. ONS Clinical Practice Committee. Cancer Chemotherapy Guidelines and Recommendations for Practice. Pittsburgh, PA. Oncology Nursing Society; 1999:32-41.
2. Recommendations for the safe handling of parenteral antineoplastic drugs. Washington, DC: Division of Safety, Clinical Center Pharmacy Department and Cancer Nursing Services, National Institutes of Health and Human Services; 1992. US Dept of Health and Human Services, Public Health Service publication NIH 92-2621.
3. AMA Council on Scientific Affairs. Guidelines for handling parenteral antineoplastics. JAMA. 1985;253:1590-1591.
4. National Study Commission on Cytotoxic Exposure. Recommendations for handling cytotoxic agents. 1987. Available from Louis P. Jeffrey, Chairman, National Study Commission on Cytotoxic Exposure. Massachusetts College of Pharmacy and Allied Health Sciences, 179 Longwood Avenue, Boston, MA 02115.
5. Clinical Oncological Society of Australia. Guidelines and recommendations for safe handling of antineoplastic agents. Med J Australia. 1983;1:426-428.
6. Jones RB, Frank R, Mass T. Safe handling of chemotherapeutic agents: a report from the Mount Sinai Medical Center. CA-A Cancer J for Clin. 1983;33:258-263.
7. American Society of Hospital Pharmacists. ASHP technical assistance bulletin on handling cytotoxic and hazardous drugs. Am J Hosp Pharm. 1990;47:1033-1049.
8. Controlling Occupational Exposure to Hazardous Drugs. (OSHA Work-Practice Guidelines.) Am J. Health-Syst Pharm. 1996:53:1669-1685.
Principal Display Panel
NDC: 69784-620-25
MYLERAN®
(busulfan) Tablets
2 mg
25 Tablets
Each tablet contains 2 mg busulfan.
Rx only
| MYLERAN
busulfan tablet, film coated |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Labeler - Woodward Pharma Services LLC (080406260) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Woodward Pharma Services LLC | 080406260 | MANUFACTURE(69784-620) | |
Trademark Results [MYLERAN]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 MYLERAN 71644161 0596271 Live/Registered |
BURROUGHS WELLCOME & CO.(U. S. A.) INC. 1953-03-25 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.
