NITYR- nitisinone tablet
NITYR by
Drug Labeling and Warnings
NITYR by is a Prescription medication manufactured, distributed, or labeled by Cycle Pharmaceuticals Ltd., Rivopharm SA, Penn Pharmaceutical Services Limited, Catalent Nottingham Limited, Pharmaron Manufacturing Services (UK) Limited, Central Pharma Contract Packing Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use NITYR safely and effectively. See full prescribing information for NITYR.
NITYR™ (nitisinone) tablets, for oral use
Initial U.S. Approval: 2002RECENT MAJOR CHANGES
Dosage and Administration, Preparation and Administration Instructions (2.2) 10/2018
INDICATIONS AND USAGE
NITYR is a hydroxyphenyl-pyruvate dioxygenase inhibitor indicated for the treatment of hereditary tyrosinemia type 1 (HT-1) in combination with dietary restriction of tyrosine and phenylalanine. (1)
DOSAGE AND ADMINISTRATION
Recommended Dosage (2.1):
- The recommended initial dosage is 0.5 mg/kg orally twice daily.
- Titrate the dose based on biochemical and/or clinical response, as described in the full prescribing information.
- The maximum dosage is 1 mg/kg orally twice daily.
Preparation and Administration Instructions (2.2):
- Maintain dietary restriction of tyrosine and phenylalanine.
- Take with or without food.
- For patients who have difficulties swallowing intact tablets, including pediatric patients, the tablets can be disintegrated in water and administered using an oral syringe. If patients can swallow semi-solid foods, the tablets can also be crushed and mixed with applesauce. For preparation and administration instructions, see the full prescribing information.
DOSAGE FORMS AND STRENGTHS
Tablets: 2 mg, 5 mg, 10 mg. (3)
CONTRAINDICATIONS
None (4).
WARNINGS AND PRECAUTIONS
- Elevated Plasma Tyrosine Levels, Ocular Symptoms, Developmental Delay and Hyperkeratotic Plaques: Inadequate restriction of tyrosine and phenylalanine intake can lead to elevations in plasma tyrosine, which at levels above 500 micromol/L can result in symptoms, intellectual disability and developmental delay or painful hyperkeratotic plaques on the soles and palms; do not adjust the dosage of NITYR in order to lower the plasma tyrosine concentration. Obtain slit-lamp examination prior to treatment and re-examination if symptoms develop. Assess plasma tyrosine levels in patients with an abrupt change in neurologic status. (5.1)
- Leukopenia and Severe Thrombocytopenia: Monitor platelet and white blood cell counts. (5.2)
ADVERSE REACTIONS
Most common adverse reactions (>1%) are elevated tyrosine levels, thrombocytopenia, leukopenia, conjunctivitis, corneal opacity, keratitis, photophobia, eye pain, blepharitis, cataracts, granulocytopenia, epistaxis, pruritus, exfoliative dermatitis, dry skin, maculopapular rash and alopecia. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Cycle Pharmaceuticals Ltd. at 1-855-831-5413 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.DRUG INTERACTIONS
CYP2C9 Substrates: Potential for increased systemic exposure of these co-administered drugs, additional monitoring may be warranted. (7.1)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 11/2018
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Dosage
2.2 Preparation and Administration Instructions
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Elevated Plasma Tyrosine Levels, Ocular Symptoms, Developmental Delay and Hyperkeratotic Plaques
5.2 Leukopenia and Severe Thrombocytopenia
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
7 DRUG INTERACTIONS
7.1 Interaction with CYP2C9 Substrates
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Dosage
Starting Dosage
The recommended starting dosage of NITYR is 0.5 mg/kg orally twice daily. Round up to the nearest dosage that can be administered using the available tablet strengths [see Dosage Forms and Strengths (3)]. Titrate the dosage for individual patients, as needed based on biochemical and/or clinical response.
Dosage Titration
- Monitor plasma and/or urine succinylacetone concentrations, liver function parameters and alpha-fetoprotein levels.
- If succinylacetone is still detectable one month after the start of nitisinone treatment, increase the nitisinone dosage to 0.75 mg/kg twice daily. A maximum dosage of 1 mg/kg orally twice daily may be needed based on the evaluation of all biochemical parameters. Round up to the nearest dosage that can be administered using the available tablet strengths.
- If the biochemical response is satisfactory, the dosage should be adjusted only according to body weight gain.
- During the initiation of therapy or if there is a deterioration in the patient’s condition, it may be necessary to follow all available biochemical parameters more closely (i.e., plasma succinylacetone, urine 5-aminolevulinate (ALA) and erythrocyte porphobilinogen (PBG)-synthase activity).
2.2 Preparation and Administration Instructions
- Maintain dietary restriction of tyrosine and phenylalanine when taking NITYR.
- NITYR can be taken with or without food.
- For patients, including pediatric patients, who have difficulty swallowing intact tablets, NITYR can be disintegrated in water and administered using an oral syringe. If patients can swallow semi-solid foods, NITYR tablets can be crushed and mixed with applesauce. Administration of NITYR with other liquids or foods has not been studied and is not recommended.
Preparation and Administration of NITYR with Water in an Oral Syringe:
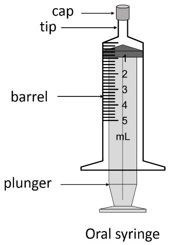
- A 5-mL oral syringe with a cap will be provided by a pharmacist.
- Follow the instructions below for one or two intact tablets, depending on the number of tablets needed to achieve the patient’s individual dosage.
- Do not prepare more than two tablets at once within the same oral syringe.
- If patient’s dosage requires more than two tablets, follow the steps below using multiple oral syringes to achieve the required dose.
One Tablet
- Remove the plunger from the 5-mL oral syringe and insert a single, intact tablet.
- Replace the plunger and draw up 2.6 mL of room temperature water.
- Cap the oral syringe and leave the oral syringe for at least 60 minutes.
- After 60 minutes, turn the oral syringe up and down for at least 30 seconds to suspend the material.
- Inspect the syringe to ensure the tablet has disintegrated prior to administration to the patient. Administer immediately. However, do not administer unless the tablet has fully disintegrated.
- If the tablet is not fully disintegrated, leave the oral syringe for an additional 10 minutes. Before administration of the suspension to the patient, turn the oral syringe up and down for 30 seconds to re-suspend the particles. Inspect the syringe again to ensure the tablet has disintegrated prior to administration to the patient. Do not administer unless the tablet has fully disintegrated.
- Administer immediately. However, if this is not possible, the suspension can be stored at room temperature in the capped oral syringe, protected from direct sunlight for up to 24 hours after adding water to the tablets. Discard after 24 hours.
- Uncap the oral syringe and administer the suspension into the patient's mouth. To facilitate full administration, avoid depressing the plunger to the end of the oral syringe and leave a gap between the plunger and the oral syringe.
- Rinse the oral syringe by drawing up 2 mL of water. Cap the oral syringe and shake well for 10 seconds to suspend any remaining particles.
- Uncap the oral syringe and administer the suspension into the patient’s mouth, this time fully depressing the plunger. If particles are still present in the syringe, repeat steps 9-10.
Two Tablets
- Remove the plunger from the 5-mL oral syringe and insert two intact tablets.
- Replace the plunger and draw up 5 mL of room temperature water.
- Cap the oral syringe and leave it for at least 60 minutes.
- After 60 minutes, turn the oral syringe up and down for at least 30 seconds to suspend the material.
- Inspect the syringe to ensure the tablets have disintegrated prior to administration to the patient. Administer immediately. However, do not administer unless the tablet has fully disintegrated.
- If the tablet is not fully disintegrated, leave the oral syringe for an additional 10 minutes. Before administration of the suspension to the patient, turn the oral syringe up and down for 30 seconds to re-suspend the particles. Inspect the syringe again to ensure the tablet has disintegrated prior to administration to the patient. Do not administer unless the tablet has fully disintegrated.
- Administer immediately. However, if this is not possible, the suspension can be stored at room temperature in the capped oral syringe, protected from direct sunlight for up to 24 hours after adding water to the tablets. Discard after 24 hours.
- Uncap the oral syringe and administer the suspension into the patient's mouth. To facilitate full administration, avoid depressing the plunger to the end of the oral syringe and leave a gap between the plunger and the oral syringe.
- Rinse the oral syringe by drawing up 2 mL of water. Cap the oral syringe and shake well for 10 seconds to suspend any remaining particles.
- Uncap the oral syringe and administer the suspension into the patient’s mouth, this time fully depressing the plunger and ensuring the syringe is empty. If particles are still present in the syringe, repeat steps 9-10.
Preparation and Administration of NITYR Mixed in Applesauce
For patients who can swallow semi-solid food, NITYR can be crushed and mixed with applesauce:
- Measure around one teaspoon of applesauce and transfer it into a clean container (e.g., clean glass).
- Always crush one tablet at a time. Position the tablet between two metal teaspoons and apply light pressure on the top spoon. The two teaspoons should overlap each other to form a fine powder.
- Press and rotate the two teaspoons against each other repeatedly until all of the tablet is in a fine powder.
- Carefully transfer the resulting powder to the applesauce container ensuring all the powder is transferred, and no powder residue remains on the teaspoons.
- If more than one tablet is needed, repeat the procedure starting from Step 2 and collect all the resulting powder together in the applesauce container.
- Mix the powder into the applesauce until the powder is well dispersed.
- Administer the entire NITYR-applesauce mixture to the patient’s mouth using a teaspoon. Administer immediately. However, if this is not possible, the mixture can be stored at room temperature, out of direct sunlight, for up to 2 hours after adding the crushed tablets to the applesauce. Discard any mixture that has not been given within 2 hours.
- To assure that any leftover applesauce mixture from the container is recovered, add around one teaspoon of applesauce to the same container and mix the fresh applesauce with the remaining mixture.
- Administer the additional NITYR-applesauce mixture immediately to the patient’s mouth using a teaspoon.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Elevated Plasma Tyrosine Levels, Ocular Symptoms, Developmental Delay and Hyperkeratotic Plaques
Nitisinone is an inhibitor of 4-hydroxyphenyl-pyruvate dioxygenase, an enzyme in the tyrosine metabolic pathway [see Clinical Pharmacology (12.1)]. Therefore, treatment with NITYR may cause an increase in plasma tyrosine levels in patients with HT-1. Maintain concomitant reduction in dietary tyrosine and phenylalanine while on NITYR. Do not adjust the dosage of NITYR in order to lower the plasma tyrosine concentration. Maintain plasma tyrosine levels below 500 micromol/L. Inadequate restriction of tyrosine and phenylalanine intake can lead to elevations in plasma tyrosine levels and levels greater than 500 micromol/L may lead to the following:
- Ocular signs and symptoms including corneal ulcers, corneal opacities, keratitis, conjunctivitis, eye pain, and photophobia have been reported in patients treated with nitisinone [see Adverse Reactions (6.1)]. Therefore, a baseline ophthalmologic examination including slit-lamp examination should be considered prior to initiating NITYR treatment. Patients who develop photophobia, eye pain, or signs of inflammation such as redness, swelling, or burning of the eyes during treatment with NITYR should undergo slit-lamp re-examination and immediate measurement of the plasma tyrosine concentration.
- Variable degrees of intellectual disability and developmental delay. In patients treated with NITYR who exhibit an abrupt change in neurologic status, perform a clinical laboratory assessment including plasma tyrosine levels.
- Painful hyperkeratotic plaques on the soles and palms.
In patients with HT-1 treated with dietary restrictions and NITYR who develop elevated plasma tyrosine levels, assess dietary tyrosine and phenylalanine intake.
5.2 Leukopenia and Severe Thrombocytopenia
In clinical trials, patients treated with another oral formulation of nitisinone and dietary restriction developed transient leukopenia (3%), thrombocytopenia (3%), or both (1.5%) [see Adverse Reactions (6.1)]. No patients developed infections or bleeding as a result of the episodes of leukopenia and thrombocytopenia. Monitor platelet and white blood cell counts during therapy with NITYR.
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of NITYR has been established based on studies of another oral formulation of nitisinone in patients with HT-1 [see Clinical Studies (14)]. Below is a display of the adverse reactions of nitisinone in these studies.
Nitisinone was studied in one open-label, uncontrolled study of 207 patients with HT-1, ages 0 to 22 years at enrollment (median age 9 months), who were diagnosed with HT-1 by the presence of succinylacetone in the urine or plasma. The starting dose of nitisinone was 0.3 to 0.5 mg/kg twice daily, and the dose was increased in some patients to 1 mg/kg twice daily based on weight, biochemical, and enzyme markers. The recommended starting dosage of NITYR is 0.5 mg/kg twice daily [see Dosage and Administration (2.1)]. Median duration of treatment was 22 months (range 0.1 to 80 months).
The most serious adverse reactions reported during nitisinone treatment were thrombocytopenia, leukopenia, porphyria, and ocular/visual complaints associated with elevated tyrosine levels [see Warnings and Precautions (5.1, 5.2)]. Fourteen patients experienced ocular/visual events. The duration of the symptoms varied from 5 days to 2 years. Six patients had thrombocytopenia, three of which had platelet counts 30,000/microL or lower. In 4 patients with thrombocytopenia, platelet counts gradually returned to normal (duration up to 47 days) without change in the nitisinone dose. No patients developed infections or bleeding as a result of the episodes of leukopenia and thrombocytopenia.
Patients with HT-1 are at increased risk of developing porphyric crises, hepatic neoplasms, and liver failure requiring liver transplantation. These complications of HT-1 were observed in patients treated with nitisinone for a median of 22 months during the clinical trial (liver transplantation 13%, liver failure 7%, malignant hepatic neoplasms 5%, benign hepatic neoplasms 3%, porphyria 1%).
The most common adverse reactions reported in the clinical trial are summarized in Table 1.
*reported in at least 1% of patients; ** another oral formulation of nitisinone TABLE 1
Most Common Adverse Reactions* in Patients with HT-1 Treated with Nitisinone**Elevated tyrosine levels >10% Leukopenia 3% Thrombocytopenia 3% Conjunctivitis 2% Corneal Opacity 2% Keratitis 2% Photophobia 2% Eye Pain 1% Blepharitis 1% Cataracts 1% Granulocytopenia 1% Epistaxis 1% Pruritus 1% Exfoliative Dermatitis 1% Dry Skin 1% Maculopapular Rash 1% Alopecia 1% Adverse reactions reported in less than 1% of the patients, included death, seizure, brain tumor, encephalopathy, hyperkinesia, cyanosis, abdominal pain, diarrhea, enanthema, gastrointestinal hemorrhage, melena, elevated hepatic enzymes, liver enlargement, hypoglycemia, septicemia, and bronchitis.
-
7 DRUG INTERACTIONS
7.1 Interaction with CYP2C9 Substrates
If NITYR is co-administered with drugs that are metabolized by CYP2C9, additional monitoring may be warranted because of a potential for increased systemic exposure of these drugs [see Clinical Pharmacology (12.3)]. The risk is dependent upon the particular 2C9 substrate and its adverse reaction profile.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Limited available data with nitisinone use in pregnant women are not sufficient to determine a drug-associated risk of adverse developmental outcomes. Animal reproduction studies have been conducted for nitisinone. In these studies, nitisinone was administered to mice and rabbits during organogenesis with oral doses of nitisinone up to 20 and 8-times respectively, the recommended initial dose of 1 mg/kg/day. In mice, nitisinone caused incomplete skeletal ossification of fetal bones and decreased pup survival at doses 0.4 times the recommended initial dose, and increased gestational length at doses 4 times the recommended initial dose. In rabbits, nitisinone caused maternal toxicity and incomplete skeletal ossification of fetal bones at doses 1.6 times the recommended initial dose [see Data].The background risk of major birth defects and miscarriage for the indicated population are unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Animal DataReproduction studies have been performed in mice at oral doses of about 0.4, 4 and 20 times the recommended initial dose (1 mg/kg/day) and in rabbits at oral doses of about 1.6, 4 and 8 times the recommended initial dose based on the body surface area. In mice, nitisinone has been shown to cause incomplete skeletal ossification of fetal bones at 0.4, 4 and 20 times the recommended initial dose, increased gestational length at 4 and 20 times the recommended initial dose, and decreased pup survival at 0.4 times the recommended initial dose based on the body surface area. In rabbits, nitisinone caused incomplete skeletal ossification of fetal bones at 1.6, 4 and 8 times the recommended initial dose based on the body surface area.
8.2 Lactation
Risk Summary
There are no data on the presence of nitisinone in human milk, the effects on the breastfed infant, or the effects on milk production. Data suggest that nitisinone is present in rat milk due to findings of ocular toxicity and lower body weight seen in drug naive nursing rat pups. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for NITYR and any potential adverse effects on the breastfed infant from NITYR or from the underlying maternal condition.8.4 Pediatric Use
Pediatric patients with HT-1, ages birth to 17 years have been treated with nitisinone in an open-label, uncontrolled clinical study [see Clinical Studies (14)]. Monitoring of plasma and urine succinylacetone levels are recommended in the pediatric patients to ensure adequate control [see Dosage and Administration (2)]. A nutritionist skilled in managing children with inborn errors of metabolism should be employed to design a low-protein diet deficient in tyrosine and phenylalanine.
8.5 Geriatric Use
Clinical studies of nitisinone did not include any subjects aged 65 and over. No pharmacokinetic studies of nitisinone have been performed in geriatric patients. In general, dose selection for an elderly patient should be cautious reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and concomitant disease or other drug therapy in this patient population.
-
10 OVERDOSAGE
Accidental ingestion of nitisinone by individuals eating normal diets not restricted in tyrosine and phenylalanine will result in elevated tyrosine levels. In healthy subjects given a single 1 mg/kg dose of nitisinone, the plasma tyrosine level reached a maximum of 1200 micromol/L from 48 to 120 hours after dosing. After a washout period of 14 days, the mean value of plasma tyrosine was still 808 micromol/L. Fasted follow-up samples obtained from subjects several weeks later showed tyrosine values back to normal. There were no reports of changes in vital signs or laboratory data of any clinical significance. One patient reported sensitivity to sunlight. Hyper-tyrosinemia has been reported with nitisinone treatment [see Warnings and Precautions (5.1)].
-
11 DESCRIPTION
NITYR contains nitisinone, which is a hydroxyphenyl-pyruvate dioxygenase inhibitor indicated as an adjunct to dietary restriction of tyrosine and phenylalanine in the treatment of hereditary tyrosinemia type 1 (HT-1).
Nitisinone occurs as white to yellowish-white, crystalline powder. It is practically insoluble in water, soluble in 2M sodium hydroxide and in methanol, and sparingly soluble in alcohol.
Chemically, nitisinone is 2-(2-nitro-4-trifluoromethylbenzoyl) cyclohexane-1,3-dione, and the structural formula is:
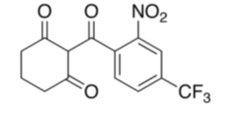
Figure 1. The molecular formula is C14H10F3NO5 and with a relative mass of 329.23.
Each NITYR (nitisinone) tablet contains 2, 5 or 10 mg of nitisinone. Inactive ingredients are: glyceryl dibehenate, and lactose monohydrate. NITYR tablets are intended for oral administration.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Nitisinone is a competitive inhibitor of 4-hydroxyphenyl-pyruvate dioxygenase, an enzyme upstream of fumarylacetoacetate hydrolase (FAH) in the tyrosine catabolic pathway. By inhibiting the normal catabolism of tyrosine in patients with HT-1, nitisinone prevents the accumulation of the catabolic intermediates maleylacetoacetate and fumarylacetoacetate. In patients with HT-1, these catabolic intermediates are converted to the toxic metabolites succinylacetone and succinylacetoacetate, which are responsible for the observed liver and kidney toxicity. Succinylacetone can also inhibit the porphyrin synthesis pathway leading to the accumulation of 5-aminolevulinate, a neurotoxin responsible for the porphyric crises characteristic of HT-1.Nitisinone inhibits catabolism of the amino acid tyrosine and can result in elevated plasma levels of tyrosine. Therefore, treatment with nitisinone requires restriction of the dietary intake of tyrosine and phenylalanine to prevent the toxicity associated with elevated plasma levels of tyrosine [see Warnings and Precautions (5.1)].
12.3 Pharmacokinetics
The single-dose pharmacokinetics of nitisinone have been studied for NITYR tablets in healthy adult subjects.
Absorption
The pharmacokinetic characteristics following single oral administration of 10 mg NITYR under fasting conditions are shown in Table 2.TABLE 2. Geometric Mean Pharmacokinetic Parameters in Healthy Subjects Following a Single Oral 10 mg Dose of NITYR Under Fasting Conditions Treatment Cmax (ng/mL)
[range]Tmax* (h)
[range]AUC0-120h (ng*h/mL)
[range]* presented as median [range]
Single 10 mg NITYR Tablet fasted (n=23) 1278
[780 to 1649]3.5
[1.0 to 4.0]
77874
[42335 to 104211]Food effect: In a food effect study, a high-fat and high-calorie breakfast (973.6 cal distributed in carbohydrate 250.1 cal, proteins 157 cal, fat 566.5 cal) did not significantly affect the total exposure (AUC0-120h) and Cmax of nitisinone following single oral administration of 10 mg NITYR. The median tmax was delayed to 6 hours under fed conditions [see Dosage and Administration (2.2)].
Distribution
In vitro binding of nitisinone to human plasma proteins is greater than 95% at 50 micromolar concentration. For NITYR, the arithmetic mean (SD) apparent volume of distribution of nitsinone is 8.2 (1.6) L in healthy subjects (n=23).Elimination
For NITYR, the arithmetic mean (SD) terminal half-life of nitisinone is 59.3 (8.9) hours in healthy subjects (n=23).Metabolism: In vitro studies have shown that nitisinone is relatively stable in human liver microsomes with minor metabolism possibly mediated by CYP3A4 enzyme.
Drug Interaction Studies
Based on in vitro studies, there is a potential for nitisinone to inhibit CYP2C9 [see Drug Interactions (7.1)]. Nitisinone is not expected to inhibit CYP 1A2, 2C19, or 3A4 based on in vitro studies. The potential for nitisinone to inhibit CYP2D6 and CYP2E1 at the recommended dosage is unknown due to limited data. -
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
The carcinogenic potential of nitisinone was assessed in a 26-week oral (gavage) carcinogenicity study in Tg.rasH2 mice. There were no drug-related neoplastic findings in male or female Tg.rasH2 mice at doses up to 100 mg/kg/ day nitisinone (approximately 8.1 times the recommended initial dose of 1 mg/kg/day on a body surface area basis).
Nitisinone was not genotoxic in the Ames test and the in vivo mouse liver unscheduled DNA synthesis (UDS) test. Nitisinone was mutagenic in the mouse lymphoma cell (L5178Y/TK+/-) forward mutation test and in an in vivo mouse bone marrow micronucleus test.
In a single dose-group study in rats given 100 mg/kg (16.2 times the recommended initial dose of 1 mg/kg/day on a body surface area basis), reduced litter size, decreased pup weight at birth, and decreased survival of pups after birth was demonstrated.
-
14 CLINICAL STUDIES
The safety and efficacy of NITYR have been established based on studies of another oral formulation of nitisinone in patients with HT-1. Below is a display of the results of these studies.
The efficacy and safety of nitisinone in patients with HT-1 was evaluated in one open-label, uncontrolled study of 207 patients with HT-1, ages 0 to 22 years at enrollment (median age 9 months). Patients were diagnosed with HT-1 by the presence of succinylacetone in the urine or plasma. All patients were treated with nitisinone at a starting dose of 0.3 to 0.5 mg/kg twice daily, and the dose was increased in some patients to 1 mg/kg twice daily based on weight, liver and kidney function tests, platelet count, serum amino acids, urinary phenolic acid, plasma and urine succinylacetone, erythrocyte PBG- synthase, and urine 5-ALA. The median duration of treatment was 22 months (range less than 1 month to 80 months). Efficacy was assessed by comparison of survival and incidence of liver transplant to historical controls.
In this clinical study, for patients presenting with HT-1 younger than 2 months of age who were treated with dietary restriction and nitisinone, 2- and 4-year survival probabilities were 88% and 88%, respectively. Data from historical controls showed that patients presenting with HT-1 younger than 2 months of age treated with dietary restriction alone had 2- and 4-year survival probabilities of 29% and 29%, respectively. For patients presenting between 2 months and 6 months of age who were treated with dietary restrictions and nitisinone, 2-and 4-year survival probabilities were 94% and 94%, respectively. Data for historical controls showed that patients presenting with HT-1 between 2 months and 6 months of age treated with dietary restriction alone had 2-and 4-year survival probabilities of 74% and 60%, respectively.
The effects on urine and plasma succinylacetone, porphyrin metabolism, and urinary alpha-1-microglobulin were also assessed in this clinical study.
Urine succinylacetone was measured in 186 patients. In all 186 patients, urinary succinylacetone level decreased to less than 1 mmol/mol creatinine. The median time to normalization was 0.3 months. The probability of recurrence of abnormal values of urine succinylacetone was 1% at a nitisinone concentration of 37 micromol/L (95% confidence interval: 23, 51 micromol/L). Plasma succinylacetone was measured in 172 patients. In 150 patients (87%), plasma succinylacetone decreased to less than 0.1 micromol/L. The median time to normalization was 3.9 months.
Porphyria-like crisis were reported in 3 patients (0.3% of cases per year) during the clinical study. This compares to an incidence of 5 to 20% of cases per year expected as part of the natural history of the disorder. An assessment of porphyria-like crises was performed because these events are commonly reported in patients with HT-1 who are not treated with nitisinone.
Urinary alpha-1-microglobulin, a proposed marker of proximal tubular dysfunction, was measured in 100 patients at baseline. The overall median pretreatment level was 4.3 grams/mol creatinine. After one year of treatment in a subgroup of patients (N=100), overall median alpha-1-microglobulin decreased by 1.5 grams/mol creatinine. In patients 24 months of age and younger in whom multiple values were available (N=65), median alpha-1-microglobulin levels decreased from 5 to 3 grams/mol creatinine (reference value for age less than or equal to12 grams/mol creatinine). In patients older than 24 months in whom multiple values were available (N=35), median alpha-1-microglobulin levels decreased from 2.8 to 2 grams/mol creatinine (reference for age less than or equal to 6 grams/mol creatinine).
The long term effect of nitisinone on hepatic function was not assessed.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Tablets: White to beige, round, flat tablets, which may display light yellow to brown speckles, debossed with the “strength” in mg on one side and “L” on the other side. Each tablet contains 2, 5 or 10 mg nitisinone. NITYR tablets are packed in high-density polyethylene (HDPE) square bottles with a child-resistant tamper-evident polypropylene (PP) screw cap. Each bottle contains 60 tablets.
2 mg tablets: From white to beige, round, flat tablets, which may display light yellow to brown speckles, debossed “2” on one side and “L” on the other side, NDC: 70709-002-60
5 mg tablets: From white to beige, round, flat tablets, which may display light yellow to brown speckles, debossed “5” on one side and “L” on the other side, NDC: 70709-005-60
10 mg tablets: From white to beige, round, flat tablets, which may display light yellow to brown speckles, debossed “10” on one side and “L” on the other side, NDC: 70709-000-60
Store NITYR tablets at room temperature between 20°C to 25°C (68°F to 77°F), with excursions permitted between 15°C and 30°C (59°F and 86°F) [see USP Controlled Room Temperature].
Dispense in tight and light resistant container as defined in USP. -
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Instructions for Use).
Administration
- Maintain dietary restriction of tyrosine and phenylalanine.
- Take with or without food.
- For patients, including pediatric patients, who have difficulty swallowing the intact tablets, the tablets can be disintegrated in water and administered using an oral syringe. If patients can swallow semi-solid foods, the tablets can also be crushed and mixed with applesauce. See Instructions for Use for preparation and administration instructions.
- Store NITYR in the container that it is dispensed in and keep the container tightly closed [see How Supplied/Storage and Handling (16)].
Elevated Plasma Tyrosine Levels, Ocular Symptoms, Developmental Delay and Hyperkeratotic Plaques
- Inform patients that inadequate dietary restriction may be associated with ocular signs and symptoms, intellectual disability and developmental delay, and painful hyperkeratotic plaques on the soles and palms. Advise patients and caregivers of the need to maintain dietary restriction of tyrosine and phenylalanine and to report any unexplained ocular, neurologic, or other symptoms promptly to their healthcare provider [see Warnings and Precautions (5.1)].
- SPL UNCLASSIFIED SECTION
-
PATIENT PACKAGE INSERT
Instructions for Use
NITYRTM (ni-TIR)
(nitisinone)
tabletsRead this Instructions for Use before you start taking NITYR tablets using an oral syringe or mixed in applesauce, and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or your treatment.
- People who have a problem swallowing NITYR tablets whole, including children, can take NITYR tablets mixed with water in an oral (by mouth) syringe or crushed and mixed with applesauce. NITYR tablets should not be mixed in any other liquid or food.
- Follow the diet restrictions for tyrosine and phenylalanine that your healthcare provider has given you during treatment with NITYR.
- NITYR can be taken with or without food.
Important information for taking NITYR using an oral syringe
- Prepare only 1 or 2 NITYR tablets in an oral syringe at one time.
- Each tablet is white to beige in color and can have yellow to brown tiny specks.
- Use a 5 mL oral syringe with a cap (see below) to prepare NITYR tablets in an oral syringe. Ask your pharmacist for your oral syringe. You may need more than one 5 mL oral syringe if you take more than 2 NITYR tablets for your prescribed dose.
- Use only room temperature water to prepare NITYR tablets in an oral syringe.
- Wash your hands well before preparing NITYR tablets using an oral syringe.
- Talk to your healthcare provider or pharmacist if you have questions about NITYR tablets or how to use the oral syringe. You can also contact the NITYR Patient Support Program by calling the United States (U.S.) toll free phone number, 1-800-847-8714.
How to prepare and take 1 NITYR tablet using a 5 mL oral syringe:
Step 1. Remove the cap from the 5 mL oral syringe.
Step 2. Remove the plunger from the oral syringe and place 1 whole NITYR tablet inside the oral syringe (See Figure A).
Step 3. Replace the plunger (See Figure B). 
Step 4. Draw up 2.6 mL of room temperature water into the oral syringe. Each line on the barrel of the syringe is 0.2 mL. There may be some air in the oral syringe. Leave the air in the oral syringe (See Figure C). 
Step 5. Replace the cap on the oral syringe. Let the oral syringe sit for at least 60 minutes (See Figure D). 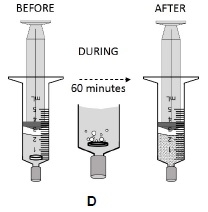
Step 6. Turn the oral syringe up and down for at least 30 seconds (See Figure E). 
Step 7. Check the oral syringe to see if the NITYR tablet has broken apart into very small pieces and the pieces are evenly spread through the water (suspension) (See Figure F). Do not take the suspension if there are any large pieces of the NITYR tablet in the suspension or if there are any pieces of the tablet that are not evenly spread through the water.
If there are any pieces of the tablet that are not evenly spread through the water, let the oral syringe sit for 10 minutes.
Before giving the suspension, turn the oral syringe up and down for 30 seconds to continue to spread the pieces of NITYR tablet in the suspension.
Step 8. Remove the cap from the oral syringe (See Figure G). 
Step 9. Place the tip of the oral syringe in the mouth right away. If giving to a child, place the tip of the oral syringe along the inner cheek of the child’s mouth (See Figure H). 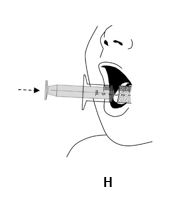
Step 10. While keeping the oral syringe in the mouth, slowly push down on the plunger until a small amount of air is left in the oral syringe, between the plunger and the tip of the oral syringe (See Figure I). Do not press the plunger all the way down to the end of the syringe. 
Step 11. Draw up an additional 2 mL of water into the oral syringe (See Figure J). 
Step 12. Replace the cap on the oral syringe. Shake the oral syringe well for 10 seconds to spread the remaining tablet pieces evenly through the water in the oral syringe (See Figure K). 
Step 13. Remove the cap from the oral syringe (See Figure L). 
Step 14. Place the tip of the oral syringe in the mouth right away. If giving to a child, place the tip of the oral syringe along the inner cheek of the child’s mouth (See Figure M). 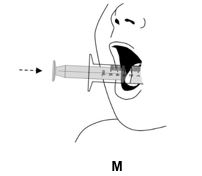
Step 15. While keeping the oral syringe in the mouth, slowly push down on the plunger until the oral syringe is empty (See Figure N). In case any pieces of the tablet are still present in the oral syringe, repeat steps 11 through 15. 
Step 16. After use, remove the plunger from the syringe barrel. Rinse the syringe and the plunger with water after each use and let it dry. Do not replace the plunger into the barrel of the oral syringe until ready to use again to allow it to dry. Do not throw away the oral syringe or plunger.
If you are not taking the water and NITYR tablet suspension as soon as it is prepared, complete steps 1 through 5. When you are ready to take the suspension, complete steps 6 through 16.
After adding water to the tablet in the oral syringe you can keep NITYR tablet suspension at room temperature for 24 hours. Store NITYR tablet suspension in the oral syringe with the cap on and out of direct sunlight until ready for use. The suspension does not need to be refrigerated. Throw away any suspension that is not used within 24 hours after adding water to the tablet in the oral syringe. Empty the syringe in the drain and throw away (dispose of) the syringe by placing it in a trash can.
How to prepare and take 2 NITYR tablets using a 5 mL oral syringe:
Step 1. Remove the cap from the 5 mL oral syringe.
Step 2. Remove the plunger from the oral syringe and place 2 whole NITYR tablets inside the oral syringe (See Figure A).
Step 3. Replace the plunger (See Figure B). 
Step 4. Draw up 5 mL of room temperature water into the oral syringe. There may be some air in the oral syringe. Leave the air in the oral syringe (See Figure C). 
Step 5. Replace the cap on the oral syringe. Let the oral syringe sit for at least 60 minutes (See Figure D). 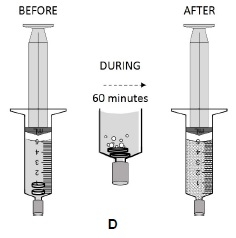
Step 6. Turn the oral syringe up and down for at least 30 seconds (See Figure E). 
Step 7. Check the oral syringe to see if the NITYR tablets have broken apart into very small pieces and the pieces are evenly spread through the water (suspension) (See Figure F). Do not take the suspension if there are any large pieces of the NITYR tablets in the suspension or if there are any pieces of the tablets that are not evenly spread through the water.
If there are any pieces of the tablets that are not evenly spread through the water, let the oral syringe sit for 10 minutes.
Before giving the suspension, turn the oral syringe up and down for 30 seconds to continue to spread the pieces of NITYR tablets in the suspension.
Step 8. Remove the cap from the oral syringe (See Figure G). 
Step 9. Place the tip of the oral syringe in the mouth right away. If giving to a child, place the tip of the oral syringe along the inner cheek of the child’s mouth (See Figure H). 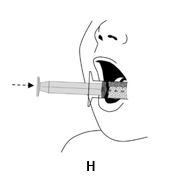
Step 10. While keeping the oral syringe in the mouth, slowly push down on the plunger until a small amount of air is left in the oral syringe, between the plunger and the tip of the oral syringe (See Figure I). Do not press all the way down on the plunger. 
Step 11. Draw up 2 mL of water into the oral syringe (See Figure J). 
Step 12. Replace the cap on the oral syringe. Shake the oral syringe well for 10 seconds to spread the remaining tablet pieces evenly through the water in the oral syringe (See Figure K). 
Step 13. Remove the cap from the oral syringe (See Figure L). 
Step 14. Place the tip of the oral syringe in the mouth right away. If giving to a child, place the tip of the oral syringe along the inner cheek of the child’s mouth (See Figure M). 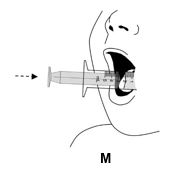
Step 15. While keeping the oral syringe in the mouth, slowly push down on the plunger until the oral syringe is empty (See Figure N). In case any pieces of the tablets are still present in the oral syringe, repeat steps 11 through 15. 
Step 16. After use, remove the plunger from the oral syringe barrel. Rinse the oral syringe with water after each use and let it dry. Do not replace the plunger into the barrel of the oral syringe until ready to use again to allow it to dry. Do not throw away the oral syringe.
If you are not taking the water and NITYR tablets suspension as soon as it is prepared, complete steps 1 through 5. When you are ready to take the suspension, complete steps 6 through 16.
After adding water to the tablet in the oral syringe you can keep NITYR tablet suspension at room temperature for 24 hours. Store the suspension in the oral syringe with the cap on and out of direct sunlight until use. The suspension does not need to be refrigerated. Throw away any suspension that is not used within 24 hours after adding water to the tablets in the oral syringe. Empty the syringe in the drain and throw away (dispose of) the syringe by placing it in a trash can.
How to prepare and take more than 2 NITYR tablets using an oral syringe:If more than two NITYR tablets are needed for the prescribed dose follow the instructions for "How to prepare and take 1 NITYR tablet using an oral syringe" and "How to prepare and take 2 NITYR tablets using an oral syringe" until you get your prescribed dose. You should not add more than 2 tablets to one syringe at a time.
How to prepare and take NITYR tablets in applesauce:
- Wash your hands well before preparing NITYR tablets in applesauce.
- Crush only 1 NITYR tablet at a time.
Step 1. Measure about 1 teaspoon of applesauce and put it into a clean container, such as a glass or bowl.
Step 2. Place 1 NITYR tablet onto a metal teaspoon (See Figure A).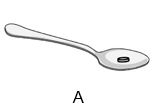
Step 3. Place a second teaspoon on top of the teaspoon holding the tablet. Apply light pressure with the second teaspoon by pressing and rotating the two teaspoons against each other (See Figure B) until the tablet is crushed to a fine powder (See Figure C). 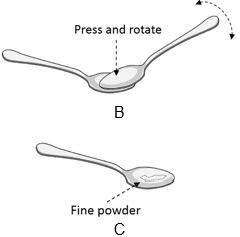
Step 4. Carefully place all of the NITYR tablet powder from the metal teaspoon into the clean container of applesauce. Be sure that no tablet powder remains on the teaspoon (See Figure D). 
Step 5. If the prescribed dose is more than 1 tablet, repeat Steps 2 and 3, placing all of the NITYR tablet powder together in the container with the applesauce. You do not need to add more applesauce at this time if you take more than 1 tablet.
Step 6. Stir the NITYR tablet powder and the applesauce until all of the tablet powder is mixed well in the applesauce (See Figure E).
Step 7. Remove the NITYR tablet powder and applesauce mixture from the container using a teaspoon and swallow the mixture right away (See Figure F). Repeat this step until no mixture is left in the container. 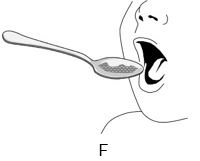
Step 8. Measure another 1 teaspoon of applesauce and place it in the container used to mix the NITYR tablet powder and applesauce (See Figure G). 
Step 9. Stir the fresh applesauce with the remaining NITYR tablet powder and applesauce mixture until they are mixed well (See Figure H). 
Step 10. Remove the NITYR tablet and applesauce mixture from the container using a teaspoon and swallow the mixture right away (See Figure I). Repeat this step until no mixture or powder is left in the container. 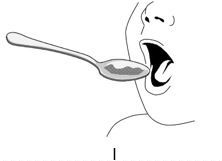
Take the NITYR tablet and applesauce mixture within 2 hours after adding the NITYR tablet powder to the applesauce. Store the NITYR tablet and applesauce mixture at room temperature and out of direct sunlight until use. The mixture does not need to be refrigerated. Throw away any mixture that is not used within 2 hours after mixing in a trash can.
How should I store NITYR?
- NITYR tablets do not need to be refrigerated.
- Store NITYR tablets at room temperature between 68°F to 77°F (20°C to 25°C).
- Store NITYR tablets in the container that it comes in and keep the container tightly closed.
- Keep NITYR tablets and NITYR that has been prepared in an oral syringe with water or in applesauce out of direct sunlight.
Take NITYR within 24 hours of adding water to NITYR tablets in an oral syringe. Throw away any unused NITYR tablets and water stored in the oral syringe after 24 hours of being mixed together.
Take NITYR within 2 hours of adding crushed NITYR tablets to applesauce. Throw away any crushed NITRY tablets and applesauce mixture that has not been used within 2 hours.
Talk to your healthcare provider or pharmacist if you have questions about NITYR tablets or how to use the oral syringe. You can also contact the NITYR Patient Support Program on the U.S. toll free number, 1-800-847-8714. For more information visit: www.nityr.us
Keep NITYR and all medicines out of the reach of children.
-
PRINCIPAL DISPLAY PANEL
Principal Display Panel - 2 mg Carton Label
NDC: 70709-002-60
NITYRTM
(nitisinone) tablets2 mg
For Oral Use
Store at room temperature between 20°C to 25°C (68°F to 77°F), excursions permitted to 15°C and 30°C (59° and 86°F). (See USP Controlled Room Temperature).
Rx only 60 tablets
-
PRINCIPAL DISPLAY PANEL
Principal Display Panel - Bottle Label
NDC: 70709-002-60
NITYRTM
(nitisinone) tablets2 mg
For Oral Use
Store at room temperature between 20°C to 25°C (68°F to 77°F).
Rx only CYCLE PHARMA 60 tablets

-
PRINCIPAL DISPLAY PANEL
Principal Display Panel - 5 mg Carton Label
NDC: 70709-005-60
NITYRTM
(nitisinone) tablets5 mg
For Oral Use
Store at room temperature between 20°C to 25°C (68°F to 77°F), excursions permitted to 15°C and 30°C (59° and 86°F). (See USP Controlled Room Temperature).
Rx only 60 tablets
-
PRINCIPAL DISPLAY PANEL
Principal Display Panel - Bottle Label
NDC: 70709-005-60
NITYRTM
(nitisinone) tablets5 mg
For Oral Use
Store at room temperature between 20°C to 25°C (68°F to 77°F).
Rx only CYCLE PHARMA 60 tablets

-
PRINCIPAL DISPLAY PANEL
Principal Display Panel - 10 mg Carton Label
NDC: 70709-000-60
NITYRTM
(nitisinone) tablets10 mg
For Oral Use
Store at room temperature between 20°C to 25°C (68°F to 77°F), excursions permitted to 15°C and 30°C (59° and 86°F). (See USP Controlled Room Temperature).
Rx only 60 tablets
-
PRINCIPAL DISPLAY PANEL
Principal Display Panel - Bottle Label
NDC: 70709-000-60
NITYRTM
(nitisinone) tablets10 mg
For Oral Use
Store at room temperature between 20°C to 25°C (68°F to 77°F).
Rx only CYCLE PHARMA 60 tablets

-
INGREDIENTS AND APPEARANCE
NITYR
nitisinone tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 70709-002 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength nitisinone (UNII: K5BN214699) (nitisinone - UNII:K5BN214699) nitisinone 2 mg Inactive Ingredients Ingredient Name Strength GLYCERYL DIBEHENATE (UNII: R8WTH25YS2) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) Product Characteristics Color white (white to beige which may display light yellow to brown speckles) Score no score Shape ROUND (round, flat) Size 7mm Flavor Imprint Code L;2 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 70709-002-60 1 in 1 CARTON 07/26/2017 1 60 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA209449 07/26/2017 NITYR
nitisinone tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 70709-005 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength nitisinone (UNII: K5BN214699) (nitisinone - UNII:K5BN214699) nitisinone 5 mg Inactive Ingredients Ingredient Name Strength GLYCERYL DIBEHENATE (UNII: R8WTH25YS2) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) Product Characteristics Color white (white to beige which may display light yellow to brown speckles) Score no score Shape ROUND (round, flat) Size 7mm Flavor Imprint Code L;5 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 70709-005-60 1 in 1 CARTON 07/26/2017 1 60 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA209449 07/26/2017 NITYR
nitisinone tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 70709-000 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength nitisinone (UNII: K5BN214699) (nitisinone - UNII:K5BN214699) nitisinone 10 mg Inactive Ingredients Ingredient Name Strength GLYCERYL DIBEHENATE (UNII: R8WTH25YS2) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) Product Characteristics Color white (white to beige which may display light yellow to brown speckles) Score no score Shape ROUND (round, flat) Size 7mm Flavor Imprint Code L;10 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 70709-000-60 1 in 1 CARTON 07/26/2017 1 60 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA209449 07/26/2017 Labeler - Cycle Pharmaceuticals Ltd. (218215530)
Trademark Results [NITYR]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 NITYR 87604011 5716643 Live/Registered |
Cycle Pharmaceuticals Ltd. 2017-09-11 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.