Ulspira by Airgas Therapeutics, LLC ULSPIRA gas
Ulspira by
Drug Labeling and Warnings
Ulspira by is a Prescription medication manufactured, distributed, or labeled by Airgas Therapeutics, LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use ULSPIRA™ safely and effectively. See full prescribing information for ULSPIRA.
ULSPIRA™ (nitric oxide) gas, for inhalation Initial U.S. Approval: 1999INDICATIONS AND USAGE
ULSPIRA is a vasodilator indicated to improve oxygenation and reduce the need for extracorporeal membrane oxygenation in term and near- term (>34 weeks gestation) neonates with hypoxic respiratory failure associated with clinical or echocardiographic evidence of pulmonary hypertension in conjunction with ventilatory support and other appropriate agents. (1)
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
ULSPIRA (nitric oxide) is a gas available in a 800 ppm concentration (3). (3)
CONTRAINDICATIONS
Neonates dependent on right-to-left shunting of blood (4). (4)
WARNINGS AND PRECAUTIONS
Rebound: Abrupt discontinuation of ULSPIRA may lead to worsening oxygenation and increasing pulmonary artery pressure (5.1). (5)
Methemoglobinemia: Methemoglobin increases with the dose of nitric oxide; following discontinuation or reduction of nitric oxide, methemoglobin levels return to baseline over a period of hours (5.2). (5)
Elevated NO 2Levels: Monitor NO 2levels (5.3). (5)
Heart Failure: In patients with pre-existing left ventricular dysfunction, ULSPIRA may increase pulmonary capillary wedge pressure leading to pulmonary edema (5.4). (5)
ADVERSE REACTIONS
DRUG INTERACTIONS
Nitric oxide donor compounds may increase the risk of developing methemoglobinemia (7). (7)
Revised: 11/2023
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
6 ADVERSE REACTIONS
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
13 NONCLINICAL TOXICOLOGY
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
ULSPIRA™ is indicated to improve oxygenation and reduce the need for extracorporeal membrane oxygenation in term and near-term (>34 weeks gestation) neonates with hypoxic respiratory failure associated with clinical or echocardiographic evidence of pulmonary hypertension in conjunction with ventilatory support and other appropriate agents.
-
2 DOSAGE AND ADMINISTRATION
2.1 Dosage
Term and near-term neonates with hypoxic respiratory failure
The recommended dose of ULSPIRA is 20 ppm. Maintain treatment up to 14 days or until the underlying oxygen desaturation has resolved and the neonate is ready to be weaned from ULSPIRA therapy.
Doses greater than 20 ppm are not recommended [see Warnings and Precautions (5.2)].
2.2 Administration
Nitric Oxide Delivery Systems
ULSPIRA must be administered using a calibrated FDA-cleared Nitric Oxide Delivery System (NODS). There are various FDA-cleared NODS; refer to the NODS labeling to determine which NODS to use with this drug product and for needed information on training and technical support for users of this drug product with the NODS. Do not use ULSPIRA with Inomax DSIR Plus and DSIR Plus MRI NODS.
Do not use ULSPIRA in the MRI suite.
Keep available a backup battery power supply and an independent reserve nitric oxide delivery system to address power and system failures .
Monitoring
Measure methemoglobin within 4-8 hours after initiation of treatment with ULSPIRA and periodically throughout treatment [see Warnings and Precautions (5.2)].
Monitor for PaO2 and inspired NO2 during ULSPIRA administration [seeWarnings andPrecautions 5.3)].
Weaning and Discontinuation
Avoid abrupt discontinuation of ULSPIRA [see Warnings and Precautions (5.1)].To wean ULSPIRA, downtitrate in several steps, pausing several hours at each step to monitor for hypoxemia.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Rebound Pulmonary Hypertension Syndrome following Abrupt Discontinuation
Wean from ULSPIRA [see Dosage and Administration (2.2)].Abrupt discontinuation of ULSPIRA may lead to worsening oxygenation and increasing pulmonary artery pressure, i.e., Rebound Pulmonary Hypertension Syndrome. Signs and symptoms of Rebound Pulmonary Hypertension Syndrome include hypoxemia, systemic hypotension, bradycardia, and decreased cardiac output. If Rebound Pulmonary Hypertension occurs, reinstate ULSPIRA therapy immediately.
5.2 Hypoxemia from Methemoglobinemia
Nitric oxide combines with hemoglobin to form methemoglobin, which does not transport oxygen. Methemoglobin levels increase with the dose of ULSPIRA; it can take 8 hours or more before steady-state methemoglobin levels are attained. Monitor methemoglobin and adjust the dose of ULSPIRA to optimize oxygenation.
If methemoglobin levels do not resolve with decrease in dose or discontinuation of ULSPIRA, additional therapy may be warranted to treat methemoglobinemia [see Overdosage (10)].
5.3 Airway Injury from Nitrogen Dioxide
Nitrogen dioxide (NO2) forms in gas mixtures containing NO and O2. Nitrogen dioxide may cause airway inflammation and damage to lung tissues.
If there is an unexpected change in NO2 concentration, or if the NO2 concentration reaches 3 ppm when measured in the breathing circuit, then the delivery system should be assessed in accordance with the Nitric Oxide Delivery System O&M Manual troubleshooting section, and the NO2 analyzer should be recalibrated. The dose of ULSPIRA and/or FiO2 should be adjusted as appropriate.
5.4 Worsening Heart Failure
Patients with left ventricular dysfunction treated with ULSPIRA may experience pulmonary edema, increased pulmonary capillary wedge pressure, worsening of left ventricular dysfunction, systemic hypotension, bradycardia and cardiac arrest. Discontinue ULSPIRA gas while providing symptomatic care.
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed elsewhere in the label;
Hypoxemia [see Warnings and Precautions (5.2)]
Worsening Heart Failure [see Warnings and Precautions (5.4)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The adverse reaction information from the clinical studies does, however, provide a basis for identifying the adverse events that appear to be related to drug use and for approximating rates.
Controlled studies have included 325 patients on nitric oxide doses of 5 to 80 ppm and 251 patients on placebo. Total mortality in the pooled trials was 11% on placebo and 9% on nitric oxide, a result adequate to exclude nitric oxide mortality being more than 40% worse than placebo.
In both the NINOS and CINRGI studies, the duration of hospitalization was similar in nitric oxide and placebo-treated groups.
From all controlled studies, at least 6 months of follow-up is available for 278 patients who received nitric oxide and 212 patients who received placebo. Among these patients, there was no evidence of an adverse effect of treatment on the need for rehospitalization, special medical services, pulmonary disease, or neurological sequelae.
In the NINOS study, treatment groups were similar with respect to the incidence and severity of intracranial hemorrhage, Grade IV hemorrhage, periventricular leukomalacia, cerebral infarction, seizures requiring anticonvulsant therapy, pulmonary hemorrhage, or gastrointestinal hemorrhage.
In CINRGI, the only adverse reaction (>2% higher incidence on nitric oxide than on placebo) was hypotension (14% vs. 11%).
6.2 Post-Marketing Experience
Post marketing reports of accidental exposure to nitric oxide for inhalation in hospital staff has been associated with chest discomfort, dizziness, dry throat, dyspnea, and headache.
- 7 DRUG INTERACTIONS
-
8 USE IN SPECIFIC POPULATIONS
8.4 Pediatric Use
The safety and efficacy of nitric oxide for inhalation has been demonstrated in term and near- term neonates with hypoxic respiratory failure associated with evidence of pulmonary hypertension [see Clinical Studies (14.1)].Additional studies conducted in premature neonates for the prevention of bronchopulmonary dysplasia have not demonstrated substantial evidence of efficacy [see Clinical Studies (14.3)].No information about its effectiveness in other age populations is available.
8.5 Geriatric Use
Nitric oxide is not indicated for use in the adult population.
-
10 OVERDOSAGE
Overdosage with nitric oxide is manifest by elevations in methemoglobin and pulmonary toxicities associated with inspired NO2. Elevated NO2 may cause acute lung injury. Elevations in methemoglobin reduce the oxygen delivery capacity of the circulation. In clinical studies, NO2 levels >3 ppm or methemoglobin levels >7% were treated by reducing the dose of, or discontinuing, nitric oxide.
Methemoglobinemia that does not resolve after reduction or discontinuation of therapy can be treated with intravenous vitamin C, intravenous methylene blue, or blood transfusion, based upon the clinical situation.
-
11 DESCRIPTION
ULSPIRA (nitric oxide gas) is adrug administered by inhalation. Nitric oxide, the active substance in ULSPIRA, is a pulmonary vasodilator. ULSPIRA is a gaseous blend of nitric oxide and nitrogen (0.08% and 99.92%, respectively for 800 ppm).
ULSPIRA is supplied in aluminum cylinders as a compressed gas under high pressure (2000 pounds per square inch gauge [psig]).
The structural formula of nitric oxide (NO) is shown below:

-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Nitric oxide relaxes vascular smooth muscle by binding to the heme moiety of cytosolic guanylate cyclase, activating guanylate cyclase and increasing intracellular levels of cyclic guanosine 3',5'-monophosphate, which then leads to vasodilation. When inhaled, nitric oxide selectively dilates the pulmonary vasculature, and because of efficient scavenging by hemoglobin, has minimal effect on the systemic vasculature.
Nitric oxide appears to increase the partial pressure of arterial oxygen (PaO2) by dilating pulmonary vessels in better ventilated areas of the lung, redistributing pulmonary blood flow away from lung regions with low ventilation/perfusion (V/Q) ratios toward regions with normal ratios.
12.2 Pharmacodynamics
Effects on Pulmonary Vascular Tone in PPHN
Persistent pulmonary hypertension of the newborn (PPHN) occurs as a primary developmental defect or as a condition secondary to other diseases such as meconium aspiration syndrome (MAS), pneumonia, sepsis, hyaline membrane disease, congenital diaphragmatic hernia (CDH), and pulmonary hypoplasia. In these states, pulmonary vascular resistance (PVR) is high, which results in hypoxemia secondary to right-to-left shunting of blood through the patent ductus arteriosus and foramen ovale. In neonates with PPHN, nitric oxide improves oxygenation (as indicated by significant increases in PaO2).
12.3 Pharmacokinetics
The pharmacokinetics of nitric oxide has been studied in adults.
Absorption and Distribution
Nitric oxide is absorbed systemically after inhalation. Most of it traverses the pulmonary capillary bed where it combines with hemoglobin that is 60% to 100% oxygen-saturated. At this level of oxygen saturation, nitric oxide combines predominantly with oxyhemoglobin to produce methemoglobin and nitrate. At low oxygen saturation, nitric oxide can combine with deoxyhemoglobin to transiently form nitrosylhemoglobin, which is converted to nitrogen oxides and methemoglobin upon exposure to oxygen. Within the pulmonary system, nitric oxide can combine with oxygen and water to produce nitrogen dioxide and nitrite, respectively, which interact with oxyhemoglobin to produce methemoglobin and nitrate. Thus, the end products of nitric oxide that enter the systemic circulation are predominantly methemoglobin and nitrate.
Metabolism
Methemoglobin disposition has been investigated as a function of time and nitric oxide exposure concentration in neonates with respiratory failure. The methemoglobin (MetHb) concentration- time profiles during the first 12 hours of exposure to 0, 5, 20, and 80 ppm nitric oxide are shown in Figure 1.
Figure 1: Methemoglobin Concentration-Time Profiles Neonates Inhaling 0, 5, 20 or 80 ppm Nitric Oxide
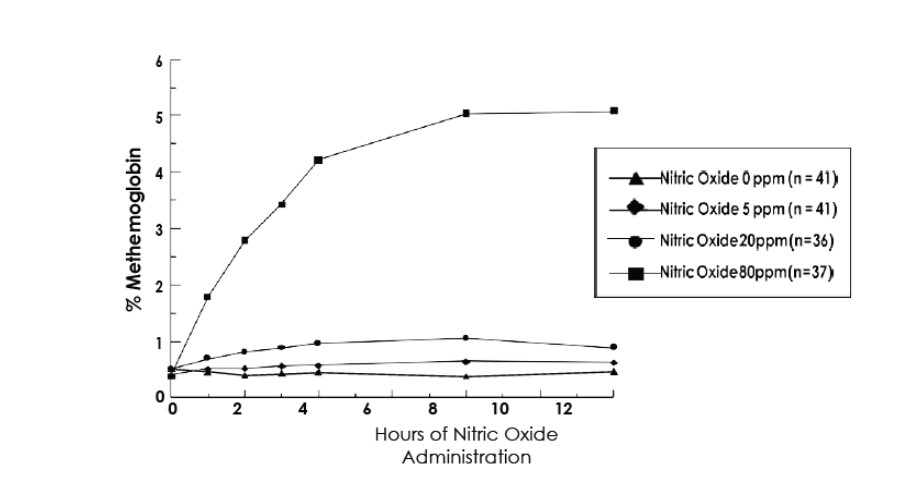
Methemoglobin concentrations increased during the first 8 hours of nitric oxide exposure. The mean methemoglobin level remained below 1% in the placebo group and in the 5 ppm and 20 ppm nitric oxide groups, but reached approximately 5% in the 80 ppm nitric oxide group.
Methemoglobin levels >7% were attained only in patients receiving 80 ppm, where they comprised 35% of the group. The average time to reach peak methemoglobin was 10 ± 9 (SD) hours (median, 8 hours) in these 13 patients, but one patient did not exceed 7% until 40 hours.
Elimination
Nitrate has been identified as the predominant nitric oxide metabolite excreted in the urine, accounting for >70% of the nitric oxide dose inhaled. Nitrate is cleared from the plasma by the kidney at rates approaching the rate of glomerular filtration.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No evidence of a carcinogenic effect was apparent, at inhalation exposures up to the recommended dose (20 ppm), in rats for 20 hr/day for up to two years. Higher exposures have not been investigated.
Nitric oxide has demonstrated genotoxicity in Salmonella (Ames Test), human lymphocytes, and after in vivoexposure in rats. There are no animal or human studies to evaluate nitric oxide for effects on fertility.
-
14 CLINICAL STUDIES
14.1 Treatment of Hypoxic Respiratory Failure (HRF)
The efficacy of nitric oxide has been investigated in term and near-term newborns with hypoxic respiratory failure resulting from a variety of etiologies. Inhalation of nitric oxide reduces the oxygenation index (OI= mean airway pressure in cm H2O × fraction of inspired oxygen concentration [FiO2]× 100 divided by systemic arterial concentration in mm Hg [PaO2]) and increases PaO2 [see Clinical Pharmacology (12.1)].
Control
(n=121)
NO
(n=114)
P value Death or ECMO*,† 77 (64%) 52 (46%) 0.006 Death 20 (17%) 16 (14%) 0.60 ECMO 66 (55%) 44 (39%) 0.014 Placebo Nitric Oxide P value ECMO*,† 51/89 (57%) 30/97 (31%) <0.001 Death 5/89 (6%) 3/97 (3%) 0.48 14.3 Ineffective in Prevention of Bronchopulmonary Dysplasia (BPD)
The safety and efficacy of nitric oxide for the prevention of chronic lung disease [bronchopulmonary dysplasia, (BPD)] in neonates ≤ 34 weeks gestational age requiring respiratory support has been studied in four large, multi-center, double-blind, placebo-controlled clinical trials in a total of 2,600 preterm infants. Of these, 1,290 received placebo, and 1,310 received inhaled nitric oxide at doses ranging from 5-20 ppm, for treatment periods of 7-24 days duration. The primary endpoint for these studies was alive and without BPD at 36 weeks postmenstrual age (PMA). The need for supplemental oxygen at 36 weeks PMA served as a surrogate endpoint for the presence of BPD. Overall, efficacy for the prevention of bronchopulmonary dysplasia in preterm infants was not established. There were no meaningful differences between treatment groups with regard to overall deaths, methemoglobin levels, or adverse events commonly observed in premature infants, including intraventricular hemorrhage, patent ductus arteriosus, pulmonary hemorrhage, and retinopathy of prematurity.
The use of nitric oxide for prevention of BPD in preterm neonates ≤ 34 weeks gestational age is not recommended.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Size D
Portable aluminum cylinders containing 362 liters at STP of nitric oxide gas in 800 ppm concentration in nitrogen (delivered volume 350 liters) (NDC: 82605-006-02)
Size 88
Aluminum cylinders containing 2138 liters at STP of nitric oxide gas in 800 ppm concentration in nitrogen (delivered volume 2083 liters) (NDC: 82605-006-01)
Distributed by
Airgas Therapeutics LLC Radnor, PA 19087 USA
AirGas Therapeutics
an Air Liquide company
© 2023 Airgas
ULSPI 01
-
PRINCIPAL DISPLAY PANEL
Ulspira TM
(nitric oxide for inhalation)
800 PPM
Rx Only
CAUTION: HIGH PRESSURE GAS. CAN CAUSE RAPID SUFFOCATION WITHOUT WARNING. Use equipment rated for cylinder pressure. Store and use with adequate ventilation. Secure cylinder in use and storage. Close valve after each use and when empty. USE IN ACCORDANCE WITH APPROPRIATE SDS.
WARNING: Administration of this gas mixture may be hazardous or contraindicated. For use only by or under the supervision of a licensed practitioner who is experienced in the use and administration of gas mixtures, and is familiar with the indications, effects, dosages, methods, and frequency and duration of administration, and with the hazards, contraindications, and side effects and the precautions to be taken.
FIRST AID: IF INHALED, remove person to fresh air. If not breathing, give artificial respiration. If breathing is difficult, give oxygen. Get medical help.
RETURN WITH 25 PSIG.
TO BE REFILLED ONLY BY A PHARMACEUTICAL FACILITY
AUTHORIZED BY AIRGAS THERAPEUTICS, LLC
Manufactured Under Pharmaceutical Current Good Manufacturing Practices (cGmps).
DO NOT REMOVE THIS PRODUCT LABEL
Store at 25 C (77 F) with excursions permitted between 15 – 30 C (59 – 86 F).
Volume 2138 Liters
Airgas Therapeutics
An Air Liquide company
Manufactured by:
AIRGAS THERAPEUTICS, LLC
6141 Easton Road
Plumsteadville, PA 18949-0310
For Product Inquiry 1-833-ULSPIRA (857-7472)
UN1956
COMPRESSED GAS, N.O.S. (NITRIC OXIDE, NITROGEN) 2.2
Net Weight: 2.5 kg
LOT:
EXP:
NDC: 82605-006-01
-
PRINCIPAL DISPLAY PANEL
Ulspira TM
(nitric oxide for inhalation)
800 PPM
Rx Only
CAUTION: HIGH PRESSURE GAS. CAN CAUSE RAPID SUFFOCATION WITHOUT WARNING. Use equipment rated for cylinder pressure. Store and use with adequate ventilation. Secure cylinder in use and storage. Close valve after each use and when empty. USE IN ACCORDANCE WITH APPROPRIATE SDS.
WARNING: Administration of this gas mixture may be hazardous or contraindicated. For use only by or under the supervision of a licensed practitioner who is experienced in the use and administration of gas mixtures, and if familiar with the indications, effects, dosages, methods, and frequency and duration of administration, and with the hazards, contraindications and side effects and the precautions to be taken.
FIRST AID: IF INHALED, remove person to fresh air. If not breathing, give artificial respiration. If breathing is difficult, give oxygen. Get medical help.
RETURN WITH 25 PSIG.
TO BE REFILLED ONLY BY A PHARMACEUTICAL FACILITY
AUTHORIZED BY AIRGAS THERAPEUTICS, LLC
Manufactured Under Pharmaceutical Current Good Manufacturing Practices (cGMPs).
DO NOT REMOVE THIS PRODUCT LABELS
Store at 25 C (77 F) with excursions permitted between 15 - 30 C (59 – 86 F).
Volume 362 Liters
Airgas Therapeutics
An Air Liquide company
Manufactured by:
AIRGAS THERAPEUTICS, LLC
6141
Easton Road
Plumsteadville, PA 18949-0310
For Product Inquiry 1-833-ULSPIRA (857-7472)
UN 1956
COMPRESSED GAS, N.O.S. (NITRIC OXIDE, NITROGEN) 2.2
Net Weight: 0.4 kg
LOT:
EXP:
NDC: 82605-006-02
-
INGREDIENTS AND APPEARANCE
ULSPIRA
ulspira gasProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 82605-006 Route of Administration RESPIRATORY (INHALATION) Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength NITRIC OXIDE (UNII: 31C4KY9ESH) (NITRIC OXIDE - UNII:31C4KY9ESH) NITRIC OXIDE 0.8 mL in 100 L Inactive Ingredients Ingredient Name Strength NITROGEN (UNII: N762921K75) 999.2 mL in 100 L Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 82605-006-01 2138 L in 1 CYLINDER; Type 0: Not a Combination Product 08/04/2023 2 NDC: 82605-006-02 362 L in 1 CYLINDER; Type 0: Not a Combination Product 08/04/2023 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA203144 08/04/2023 Labeler - Airgas Therapeutics, LLC (118537769) Establishment Name Address ID/FEI Business Operations Airgas Therapeutics, LLC 118537769 manufacture(82605-006)
Trademark Results [Ulspira]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 ULSPIRA 98319577 not registered Live/Pending |
Airgas Therapeutics, LLC 2023-12-18 |
 ULSPIRA 97932397 not registered Live/Pending |
Airgas Therapeutics, LLC 2023-05-11 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.