SUBOXONE- buprenorphine and naloxone film, soluble
Suboxone by
Drug Labeling and Warnings
Suboxone by is a Prescription medication manufactured, distributed, or labeled by Bryant Ranch Prepack, Monosol Rx LLC, Reckitt Benckiser Healthcare (UK) Ltd. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use SUBOXONE sublingual film safely and effectively. See full prescribing information for SUBOXONE sublingual film. SUBOXONE (buprenorphine and naloxone) sublingual film for sublingual administration CIII Initial U.S. Approval: 2002
INDICATIONS AND USAGE
SUBOXONE sublingual film is indicated for maintenance treatment of opioid dependence. Prescription use of this product is limited under the Drug Addiction Treatment Act. (1)
DOSAGE AND ADMINISTRATION
Administer SUBOXONE sublingual film sublingually as a single daily dose. (2)
The recommended daily dose for maintenance is 16/4 mg.
DOSAGE FORMS AND STRENGTHS
Sublingual film: 2 mg buprenorphine with 0.5 mg naloxone and 8 mg buprenorphine with 2 mg naloxone. (3)
CONTRAINDICATIONS
Hypersensitivity to buprenorphine or naloxone. (4)
WARNINGS AND PRECAUTIONS
- Buprenorphine can be abused in a similar manner to other opioids. Clinical monitoring appropriate to the patient's level of stability is essential. Multiple refills should not be prescribed early in treatment or without appropriate patient follow-up visits. (5.1)
- Significant respiratory depression and death have occurred in association with buprenorphine, particularly when taken by the intravenous (IV) route in combination with benzodiazepines or other CNS depressants (including alcohol). (5.2)
- Consider dose reduction of CNS depressants, SUBOXONE sublingual film or both in situations of concomitant prescription. (5.3)
- Store SUBOXONE sublingual film safely out of the sight and reach of children. Buprenorphine can cause severe, possibly fatal, respiratory depression in children. (5.4)
- Chronic administration produces opioid-type physical dependence. Abrupt discontinuation or rapid dose taper may result in opioid withdrawal syndrome. (5.5)
- Monitor liver function tests prior to initiation and during treatment and evaluate suspected hepatic events. (5.6)
- Do not administer SUBOXONE sublingual film to patients with known hypersensitivity to buprenorphine or naloxone. (5.7)
- A marked and intense opioid withdrawal syndrome is highly likely to occur with parenteral misuse of SUBOXONE sublingual film by individuals physically dependent on full opioid agonists or by sublingual administration before the agonist effects of other opioids have subsided. (5.8)
- Neonatal withdrawal has been reported following use of buprenorphine by the mother during pregnancy. (5.9)
- SUBOXONE sublingual film is not appropriate as an analgesic. There have been reported deaths of opioid naïve individuals who received a 2 mg sublingual dose. (5.10)
- Caution patients about the risk of driving or operating hazardous machinery. (5.11)
ADVERSE REACTIONS
Adverse events commonly observed with the sublingual administration of the SUBOXONE sublingual film was oral hypoesthesia, glossodynia, oral mucosal erythema, headache, nausea, vomiting, hyperhidrosis, constipation, signs and symptoms of withdrawal, insomnia, pain and peripheral edema. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Reckitt Benckiser Pharmaceuticals Inc. at 1-877-782-6966, FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
- SUBOXONE sublingual film is not indicated for use during pregnancy unless potential benefit justifies potential risk. (8.1)
- Buprenorphine passes into the mother's milk. Breast-feeding is not advised while taking SUBOXONE sublingual film. (8.3)
- Safety and effectiveness of SUBOXONE sublingual film in patients below the age of 16 has not been established. (8.4)
- Administer SUBOXONE sublingual film with caution to elderly or debilitated patients. (8.5)
- Administer SUBOXONE sublingual film with caution in patients with liver dysfunction. (8.6)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 9/2010
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Maintenance
2.2 Method of Administration
2.3 Clinical Supervision
2.4 Unstable Patients
2.5 Stopping Treatment
2.6 Switching between SUBOXONE (buprenorphine and naloxone) Sublingual Tablets and SUBOXONE Sublingual film
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Abuse Potential
5.2 Respiratory Depression
5.3 CNS Depression
5.4 Unintentional Pediatric Exposure
5.5 Dependence
5.6 Hepatitis, Hepatic Events
5.7 Allergic Reactions
5.8 Precipitation of Opioid Withdrawal Signs and Symptoms
5.9 Neonatal Withdrawal
5.10 Use in Opioid Naïve Patients
5.11 Impairment of Ability to Drive or Operate Machinery
5.12 Orthostatic Hypotension
5.13 Elevation of Cerebrospinal Fluid Pressure
5.14 Elevation of Intracholedochal Pressure
5.15 Effects in Acute Abdominal Conditions
5.16 General Precautions
6 ADVERSE REACTIONS
6.1 Adverse Events in Clinical Trials - SUBOXONE Sublingual film
6.2 Adverse Events – Post-marketing Experience with SUBOXONE Sublingual Tablets
7 DRUG INTERACTIONS
7.1 Cytochrome P-450 3A4 (CYP3A4) Inhibitors and Inducers
7.2 Antiretrovirals
7.3 Benzodiazepines
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 Renal Impairment
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
9.2 Abuse
9.3 Dependence
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
17 PATIENT COUNSELING INFORMATION
17.1 Safe Use
17.2 Disposal of Unused SUBOXONE Sublingual Film
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
SUBOXONE sublingual film is indicated for maintenance treatment of opioid dependence and should be used as part of a complete treatment plan to include counseling and psychosocial support.
Under the Drug Addiction Treatment Act (DATA) codified at 21 U.S.C. 823(g), prescription use of this product in the treatment of opioid dependence is limited to physicians who meet certain qualifying requirements, and who have notified the Secretary of Health and Human Services (HHS) of their intent to prescribe this product for the treatment of opioid dependence and have been assigned a unique identification number that must be included on every prescription.
-
2 DOSAGE AND ADMINISTRATION
SUBOXONE sublingual film is administered sublingually as a single daily dose. SUBOXONE sublingual film should be used in patients who have been initially inducted using SUBUTEX® (buprenorphine) sublingual tablets.
2.1 Maintenance
- SUBOXONE sublingual film is indicated for maintenance treatment. The recommended target dosage of SUBOXONE sublingual film is 16/4 mg buprenorphine/naloxone/day, as a single daily dose.
- The dosage of SUBOXONE sublingual film should be progressively adjusted in increments/decrements of 2/0.5 mg or 4/1 mg buprenorphine/naloxone to a level that holds the patient in treatment and suppresses opioid withdrawal signs and symptoms.
- The maintenance dose of SUBOXONE sublingual film is generally in the range of 4/1 mg buprenorphine/naloxone to 24/6 mg buprenorphine/naloxone per day depending on the individual patient. Dosages higher than this have not been demonstrated to provide any clinical advantage.
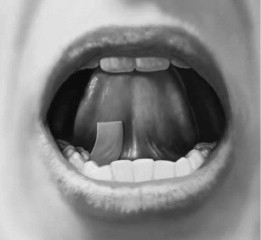
2.2 Method of Administration
Place the SUBOXONE sublingual film under the tongue. If an additional SUBOXONE sublingual film is necessary to achieve the prescribed dose, place the additional sublingual film sublingually on the opposite side from the first film. Place the sublingual film in a manner to minimize overlapping as much as possible. The sublingual film must be kept under the tongue until the film is completely dissolved. SUBOXONE sublingual film should NOT be chewed, swallowed, or moved after placement.
Proper administration technique should be demonstrated to the patient.
2.3 Clinical Supervision
Treatment should be initiated with supervised administration, progressing to unsupervised administration as the patient's clinical stability permits. SUBOXONE sublingual film is subject to diversion and abuse. When determining the prescription quantity for unsupervised administration, consider the patient's level of stability, the security of his or her home situation, and other factors likely to affect the ability to manage supplies of take-home medication.
Ideally patients should be seen at reasonable intervals (e.g., at least weekly during the first month of treatment) based upon the individual circumstances of the patient. Medication should be prescribed in consideration of the frequency of visits. Provision of multiple refills is not advised early in treatment or without appropriate patient follow-up visits. Periodic assessment is necessary to determine compliance with the dosing regimen, effectiveness of the treatment plan, and overall patient progress.
Once a stable dosage has been achieved and patient assessment (e.g., urine drug screening) does not indicate illicit drug use, less frequent follow-up visits may be appropriate. A once-monthly visit schedule may be reasonable for patients on a stable dosage of medication who are making progress toward their treatment objectives. Continuation or modification of pharmacotherapy should be based on the physician's evaluation of treatment outcomes and objectives such as:
- Absence of medication toxicity.
- Absence of medical or behavioral adverse effects.
- Responsible handling of medications by the patient.
- Patient's compliance with all elements of the treatment plan (including recovery-oriented activities, psychotherapy, and/or other psychosocial modalities).
- Abstinence from illicit drug use (including problematic alcohol and/or benzodiazepine use).
If treatment goals are not being achieved, the physician should re-evaluate the appropriateness of continuing the current treatment.
2.4 Unstable Patients
Physicians will need to decide when they cannot appropriately provide further management for particular patients. For example, some patients may be abusing or dependent on various drugs, or unresponsive to psychosocial intervention such that the physician does not feel that he/she has the expertise to manage the patient. In such cases, the physician may want to assess whether to refer the patient to a specialist or more intensive behavioral treatment environment. Decisions should be based on a treatment plan established and agreed upon with the patient at the beginning of treatment.
Patients who continue to misuse, abuse, or divert buprenorphine products or other opioids should be provided with, or referred to, more intensive and structured treatment.
2.5 Stopping Treatment
The decision to discontinue therapy with SUBOXONE sublingual film after a period of maintenance should be made as part of a comprehensive treatment plan. Both gradual and abrupt discontinuation of buprenorphine has been used, but the data are insufficient to determine the best method of dose taper at the end of treatment.
2.6 Switching between SUBOXONE (buprenorphine and naloxone) Sublingual Tablets and SUBOXONE Sublingual film
Patients being switched between SUBOXONE (buprenorphine and naloxone) sublingual tablets and SUBOXONE sublingual film should be started on the same dosage as the previously administered product. However, dosage adjustments may be necessary when switching between products. Because of the potentially greater relative bioavailability of SUBOXONE sublingual film compared to SUBOXONE (buprenorphine and naloxone) sublingual tablets, patients switching from SUBOXONE (buprenorphine and naloxone) sublingual tablets to SUBOXONE sublingual film should be monitored for over-medication. Those switching from SUBOXONE sublingual film to SUBOXONE (buprenorphine and naloxone) sublingual tablets should be monitored for withdrawal or other indications of under-dosing. In clinical studies, pharmacokinetics of SUBOXONE sublingual film was similar to the respective dosage strengths of SUBOXONE (buprenorphine and naloxone) sublingual tablets, although not all doses and dose combinations met bioequivalence criteria.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
SUBOXONE sublingual film should not be administered to patients who have been shown to be hypersensitive to buprenorphine or naloxone as serious adverse reactions, including anaphylactic shock, have been reported [see Warnings and Precautions (5.7)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Abuse Potential
Buprenorphine can be abused in a manner similar to other opioids, legal or illicit. Prescribe and dispense buprenorphine with appropriate precautions to minimize risk of misuse, abuse, or diversion, and ensure appropriate protection from theft, including in the home. Clinical monitoring appropriate to the patient's level of stability is essential. Multiple refills should not be prescribed early in treatment or without appropriate patient follow-up visits. [see Drug Abuse and Dependence (9.2)].
5.2 Respiratory Depression
Buprenorphine, particularly when taken by the IV route, in combination with benzodiazepines or other CNS depressants (including alcohol), has been associated with significant respiratory depression and death. Many, but not all post-marketing reports regarding coma and death associated with the concomitant use of buprenorphine and benzodiazepines, involved misuse by self-injection. Deaths have also been reported in association with concomitant administration of buprenorphine with other depressants such as alcohol or other CNS depressant drugs. Patients should be warned of the potential danger of self-administration of benzodiazepines or other depressants while under treatment with SUBOXONE sublingual film. [see Drug Interactions (7.3)]
In the case of overdose, the primary management should be the re-establishment of adequate ventilation with mechanical assistance of respiration, if required. Naloxone may be of value for the management of buprenorphine overdose. Higher than normal doses and repeated administration may be necessary.
SUBOXONE sublingual film should be used with caution in patients with compromised respiratory function (e.g., chronic obstructive pulmonary disease, cor pulmonale, decreased respiratory reserve, hypoxia, hypercapnia, or pre-existing respiratory depression).
5.3 CNS Depression
Patients receiving buprenorphine in the presence of opioid analgesics, general anesthetics, benzodiazepines, phenothiazines, other tranquilizers, sedative/hypnotics or other CNS depressants (including alcohol) may exhibit increased CNS depression. Consider dose reduction of CNS depressants, SUBOXONE sublingual film, or both in situations of concomitant prescription. [see Drug Interactions (7.3)].
5.4 Unintentional Pediatric Exposure
Buprenorphine can cause severe, possibly fatal, respiratory depression in children who are accidentally exposed to it. Store buprenorphine-containing medications safely out of the sight and reach of children and destroy any unused medication appropriately [see Disposal of Unused SUBOXONE Sublingual Film (17.2)].
5.5 Dependence
Buprenorphine is a partial agonist at the mu-opioid receptor and chronic administration produces physical dependence of the opioid type, characterized by withdrawal signs and symptoms upon abrupt discontinuation or rapid taper. The withdrawal syndrome is typically milder than seen with full agonists and may be delayed in onset. Buprenorphine can be abused in a manner similar to other opioids. This should be considered when prescribing or dispensing buprenorphine in situations when the clinician is concerned about an increased risk of misuse, abuse, or diversion. [see Drug Abuse and Dependence (9.3)]
5.6 Hepatitis, Hepatic Events
Cases of cytolytic hepatitis and hepatitis with jaundice have been observed in individuals receiving buprenorphine in clinical trials and through post-marketing adverse event reports. The spectrum of abnormalities ranges from transient asymptomatic elevations in hepatic transaminases to case reports of death, hepatic failure, hepatic necrosis, hepatorenal syndrome, and hepatic encephalopathy. In many cases, the presence of pre-existing liver enzyme abnormalities, infection with hepatitis B or hepatitis C virus, concomitant usage of other potentially hepatotoxic drugs, and ongoing injecting drug use may have played a causative or contributory role. In other cases, insufficient data were available to determine the etiology of the abnormality. Withdrawal of buprenorphine has resulted in amelioration of acute hepatitis in some cases; however, in other cases no dose reduction was necessary. The possibility exists that buprenorphine had a causative or contributory role in the development of the hepatic abnormality in some cases. Liver function tests, prior to initiation of treatment is recommended to establish a baseline. Periodic monitoring of liver function during treatment is also recommended. A biological and etiological evaluation is recommended when a hepatic event is suspected. Depending on the case, SUBOXONE sublingual film may need to be carefully discontinued to prevent withdrawal signs and symptoms and a return by the patient to illicit drug use, and strict monitoring of the patient should be initiated.
5.7 Allergic Reactions
Cases of hypersensitivity to buprenorphine and naloxone containing products have been reported both in clinical trials and in the post-marketing experience. Cases of bronchospasm, angioneurotic edema, and anaphylactic shock have been reported. The most common signs and symptoms include rashes, hives, and pruritus. A history of hypersensitivity to buprenorphine or naloxone is a contraindication to the use of SUBOXONE sublingual film.
5.8 Precipitation of Opioid Withdrawal Signs and Symptoms
Because it contains naloxone, SUBOXONE sublingual film is highly likely to produce marked and intense withdrawal signs and symptoms if misused parenterally by individuals dependent on full opioid agonists such as heroin, morphine, or methadone. Because of the partial agonist properties of buprenorphine, SUBOXONE sublingual film may precipitate opioid withdrawal signs and symptoms in such persons if administered sublingually before the agonist effects of the opioid have subsided.
5.9 Neonatal Withdrawal
Neonatal withdrawal has been reported in the infants of women treated with buprenorphine during pregnancy. From post-marketing reports, the time to onset of neonatal withdrawal signs ranged from Day 1 to Day 8 of life with most cases occurring on Day 1. Adverse events associated with the neonatal withdrawal syndrome included hypertonia, neonatal tremor, neonatal agitation, and myoclonus, and there have been reports of convulsions, apnea, respiratory depression, and bradycardia.
5.10 Use in Opioid Naïve Patients
There have been reported deaths of opioid naive individuals who received a 2 mg dose of buprenorphine as a sublingual tablet for analgesia. SUBOXONE sublingual film is not appropriate as an analgesic.
5.11 Impairment of Ability to Drive or Operate Machinery
SUBOXONE sublingual film may impair the mental or physical abilities required for the performance of potentially dangerous tasks such as driving a car or operating machinery, especially during treatment induction and dose adjustment. Patients should be cautioned about driving or operating hazardous machinery until they are reasonably certain that SUBOXONE sublingual film therapy does not adversely affect his or her ability to engage in such activities.
5.12 Orthostatic Hypotension
Like other opioids, SUBOXONE sublingual film may produce orthostatic hypotension in ambulatory patients.
5.13 Elevation of Cerebrospinal Fluid Pressure
Buprenorphine, like other opioids, may elevate cerebrospinal fluid pressure and should be used with caution in patients with head injury, intracranial lesions and other circumstances when cerebrospinal pressure may be increased. Buprenorphine can produce miosis and changes in the level of consciousness that may interfere with patient evaluation.
5.14 Elevation of Intracholedochal Pressure
Buprenorphine has been shown to increase intracholedochal pressure, as do other opioids, and thus should be administered with caution to patients with dysfunction of the biliary tract.
5.15 Effects in Acute Abdominal Conditions
As with other opioids, buprenorphine may obscure the diagnosis or clinical course of patients with acute abdominal conditions.
5.16 General Precautions
SUBOXONE sublingual film should be administered with caution in debilitated patients and those with myxedema or hypothyroidism, adrenal cortical insufficiency (e.g., Addison's disease); CNS depression or coma; toxic psychoses; prostatic hypertrophy or urethral stricture; acute alcoholism; delirium tremens; or kyphoscoliosis.
-
6 ADVERSE REACTIONS
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
6.1 Adverse Events in Clinical Trials - SUBOXONE Sublingual film
The safety of SUBOXONE sublingual film is supported by clinical trials using SUBUTEX (buprenorphine) sublingual tablets and SUBOXONE (buprenorphine and naloxone) sublingual tablets, and other trials using buprenorphine sublingual solutions, as well as an open-label study in 194 patients treated with SUBOXONE sublingual film. In total, safety data from clinical studies are available from over 3000 opioid-dependent subjects exposed to buprenorphine at doses in the range used in the treatment of opioid dependence. Few differences in the adverse event profile were noted among SUBOXONE sublingual film, SUBOXONE (buprenorphine and naloxone) sublingual tablets, SUBUTEX (buprenorphine) sublingual tablets and a buprenorphine ethanolic sublingual solution.
The most common adverse event (>1%) associated with the sublingual administration of the SUBOXONE sublingual film was oral hypoesthesia. Other adverse events were constipation, glossodynia, oral mucosal erythema, vomiting, intoxication, disturbance in attention, palpitations, insomnia, withdrawal syndrome, hyperhidrosis, and blurred vision.
Other adverse event data were derived from larger, controlled studies of SUBOXONE (buprenorphine and naloxone) and SUBUTEX (buprenorphine) tablets and of buprenorphine sublingual solution. In a comparative study of SUBOXONE (buprenorphine and naloxone) and SUBUTEX (buprenorphine) sublingual tablets, adverse event profiles were similar for subjects treated with 16/4 mg SUBOXONE (buprenorphine and naloxone) sublingual tablets or 16 mg SUBUTEX (buprenorphine) sublingual tablets. The following adverse events were reported to occur by at least 5% of patients in a 4-week study of SUBOXONE (buprenorphine and naloxone) sublingual tablets and SUBUTEX (buprenorphine) sublingual tablets.
Table 1. Adverse Events (≥5%) by Body System and Treatment Group in a 4-week Study Abbreviations: COSTART = Coding Symbols for Thesaurus of Adverse Reaction Terms.
Body System/ Adverse Event (COSTART Terminology) SUBOXONE (buprenorphine and naloxone) sublingual tablets
16/4 mg/day
N=107
n (%)SUBUTEX (buprenorphine) sublingual tablets
16 mg/day
N=103
n (%)Placebo
N=107
n (%)Body as a Whole Asthenia 7 (6.5%) 5 (4.9%) 7 (6.5%) Chills 8 (7.5%) 8 (7.8%) 8 (7.5%) Headache 39 (36.4%) 30 (29.1%) 24 (22.4%) Infection 6 (5.6%) 12 (11.7%) 7 (6.5%) Pain 24 (22.4%) 19 (18.4%) 20 (18.7%) Pain abdomen 12 (11.2%) 12 (11.7%) 7 (6.5%) Pain back 4 (3.7%) 8 (7.8%) 12 (11.2%) Withdrawal syndrome 27 (25.2%) 19 (18.4%) 40 (37.4%) Cardiovascular System Vasodilation 10 (9.3%) 4 (3.9%) 7 (6.5%) Digestive System Constipation 13 (12.1%) 8 (7.8%) 3 (2.8%) Diarrhea 4 (3.7%) 5 (4.9%) 16 (15.0%) Nausea 16 (15.0%) 14 (13.6%) 12 (11.2%) Vomiting 8 (7.5%) 8 (7.8%) 5 (4.7%) Nervous System Insomnia 15 (14.0%) 22 (21.4%) 17 (15.9%) Respiratory System Rhinitis 5 (4.7%) 10 (9.7%) 14 (13.1%) Skin And Appendages Sweating 15 (14.0%) 13 (12.6%) 11 (10.3%) The adverse event profile of buprenorphine was also characterized in the dose-controlled study of a buprenorphine ethanolic solution, over a range of doses in four months of treatment. Table 2 shows adverse events reported by at least 5% of subjects in any dose group in the dose-controlled trial.
Table 2. Adverse Events (≥5%) by Body System and Treatment Group in a 16-week Study *Sublingual solution. Doses in this table cannot necessarily be delivered in tablet form, but for comparison purposes:
1 mg solution would be less than a tablet dose of 2 mg
4 mg solution approximates a 6 mg tablet dose
8 mg solution approximates a 12 mg tablet dose
16 mg solution approximates a 24 mg tablet dose
Body System/ Adverse Event
(COSTART Terminology)Buphrenorphine Dose Very Low*
N=184
n (%)Low*
N=180
n (%)Moderate*
N=186
n (%)High*
N=181
n (%)Total*
N=731
n (%)Body as a Whole Abscess 9 (5%) 2 (1%) 3 (2%) 2 (1%) 16 (2%) Asthenia 26 (14%) 28 (16%) 26 (14%) 24 (13%) 104 (14%) Chills 11 (6%) 12 (7%) 9 (5%) 10 (6%) 42 (6%) Fever 7 (4%) 2 (1%) 2 (1%) 10 (6%) 21 (3%) Flu syndrome 4 (2%) 13 (7%) 19 (10%) 8 (4%) 44 (6%) Headache 51 (28%) 62 (34%) 54 (29%) 53 (29%) 220 (30%) Infection 32 (17%) 39 (22%) 38 (20%) 40 (22%) 149 (20%) Injury accidental 5 (3%) 10 (6%) 5 (3%) 5 (3%) 25 (3%) Pain 47 (26%) 37 (21%) 49 (26%) 44 (24%) 177 (24%) Pain back 18 (10%) 29 (16%) 28 (15%) 27 (15%) 102 (14%) Withdrawal syndrome 45 (24%) 40 (22%) 41 (22%) 36 (20%) 162 (22%) Digestive System Constipation 10 (5%) 23 (13%) 23 (12%) 26 (14%) 82 (11%) Diarrhea 19 (10%) 8 (4%) 9 (5%) 4 (2%) 40 (5%) Dyspepsia 6 (3%) 10 (6%) 4 (2%) 4 (2%) 24 (3%) Nausea 12 (7%) 22 (12%) 23 (12%) 18 (10%) 75 (10%) Vomiting 8 (4%) 6 (3%) 10 (5%) 14 (8%) 38 (5%) Nervous System Anxiety 22 (12%) 24 (13%) 20 (11%) 25 (14%) 91 (12%) Depression 24 (13%) 16 (9%) 25 (13%) 18 (10%) 83 (11%) Dizziness 4 (2%) 9 (5%) 7 (4%) 11 (6%) 31 (4%) Insomnia 42 (23%) 50 (28%) 43 (23%) 51 (28%) 186 (25%) Nervousness 12 (7%) 11 (6%) 10 (5%) 13 (7%) 46 (6%) Somnolence 5 (3%) 13 (7%) 9 (5%) 11 (6%) 38 (5%) Respiratory System Cough increase 5 (3%) 11 (6%) 6 (3%) 4 (2%) 26 (4%) Pharyngitis 6 (3%) 7 (4%) 6 (3%) 9 (5%) 28 (4%) Rhinitis 27 (15%) 16 (9%) 15 (8%) 21 (12%) 79 (11%) Skin and Appendages Sweat 23 (13%) 21 (12%) 20 (11%) 23 (13%) 87 (12%) Special Senses Runny eyes 13 (7%) 9 (5%) 6 (3%) 6 (3%) 34 (5%) -
7 DRUG INTERACTIONS
7.1 Cytochrome P-450 3A4 (CYP3A4) Inhibitors and Inducers
Buprenorphine is metabolized to norbuprenorphine primarily by cytochrome CYP3A4; therefore, potential interactions may occur when SUBOXONE sublingual film is given concurrently with agents that affect CYP3A4 activity. The concomitant use of SUBOXONE sublingual film with CYP3A4 inhibitors (e.g., azole antifungals such as ketoconazole, macrolide antibiotics such as erythromycin, and HIV protease inhibitors) should be monitored and may require dose-reduction of one or both agents.
The interaction of buprenorphine with CYP3A4 inducers has not been studied; therefore, it is recommended that patients receiving SUBOXONE sublingual film be monitored for signs and symptoms of opioid withdrawal if inducers of CYP3A4 (e.g., efavirenz, phenobarbital, carbamazepine, phenytoin, rifampicin) are co-administered [see Clinical Pharmacology (12.3)].
7.2 Antiretrovirals
Three classes of antiretroviral agents have been evaluated for CYP3A4 interactions with buprenorphine. Nucleoside reverse transcriptase inhibitors (NRTIs) do not appear to induce or inhibit the P450 enzyme pathway, thus no interactions with buprenorphine are expected. Non-nucleoside reverse transcriptase inhibitors (NNRTIs) are metabolized principally by CYP3A4. Efavirenz, nevirapine and etravirine are known CYP3A inducers whereas delaviridine is a CYP3A inhibitor. Significant pharmacokinetic interactions between NNRTIs (e.g., efavirenz and delavirdine) and buprenorphine have been shown in clinical studies, but these pharmacokinetic interactions did not result in any significant pharmacodynamic effects. It is recommended that patients who are on chronic buprenorphine treatment have their dose monitored if NNRTIs are added to their treatment regimen. Studies have shown some antiretroviral protease inhibitors (PIs) with CYP3A4 inhibitory activity (nelfinavir, lopinavir/ritonavir, ritonavir) have little effect on buprenorphine pharmacokinetic and no significant pharmacodynamic effects. Other PIs with CYP3A4 inhibitory activity (atazanavir and atazanavir/ritonavir) resulted in elevated levels of buprenorphine and norbuprenorphine and patients in one study reported increased sedation. Symptoms of opioid excess have been found in post-marketing reports of patients receiving buprenorphine and atazanavir with and without ritonavir concomitantly. Monitoring of patients taking buprenorphine and atazanavir with and without ritonavir is recommended, and dose reduction of buprenorphine may be warranted.
7.3 Benzodiazepines
There have been a number of post-marketing reports regarding coma and death associated with the concomitant use of buprenorphine and benzodiazepines. In many, but not all, of these cases, buprenorphine was misused by self-injection. Preclinical studies have shown that the combination of benzodiazepines and buprenorphine altered the usual ceiling effect on buprenorphine-induced respiratory depression, making the respiratory effects of buprenorphine appear similar to those of full opioid agonists. SUBOXONE sublingual film should be prescribed with caution to patients taking benzodiazepines or other drugs that act on the CNS, regardless of whether these drugs are taken on the advice of a physician or are being abused/misused. Patients should be warned that it is extremely dangerous to self-administer non-prescribed benzodiazepines while taking SUBOXONE sublingual film, and should also be cautioned to use benzodiazepines concurrently with SUBOXONE sublingual film only as directed by their physician.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C.
There are no adequate and well-controlled studies of SUBOXONE sublingual film or buprenorphine/naloxone in pregnant women. SUBOXONE sublingual film should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Teratogenic Effects:
Effects on embryo-fetal development were studied in Sprague-Dawley rats and Russian white rabbits following oral (1:1) and intramuscular (IM) (3:2) administration of mixtures of buprenorphine and naloxone. Following oral administration to rats and rabbits, no teratogenic effects were observed at buprenorphine doses up to 250 mg/kg/day and 40 mg/kg/day, respectively (estimated exposure approximately 150 times and 50 times, respectively, the recommended human daily sublingual dose of 16 mg on a mg/m2 basis). No definitive drug-related teratogenic effects were observed in rats and rabbits at IM doses up to 30 mg/kg/day (estimated exposure approximately 20 times and 35 times, respectively, the recommended human daily dose of 16 mg on a mg/m2 basis). Acephalus was observed in one rabbit fetus from the low-dose group and omphalocele was observed in two rabbit fetuses from the same litter in the mid-dose group; no findings were observed in fetuses from the high-dose group. Following oral administration of buprenorphine to rats, dose-related post-implantation losses, evidenced by increases in the numbers of early resorptions with consequent reductions in the numbers of fetuses, were observed at doses of 10 mg/kg/day or greater (estimated exposure approximately 6 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis). In the rabbit, increased post-implantation losses occurred at an oral dose of 40 mg/kg/day. Following IM administration in the rat and the rabbit, post-implantation losses, as evidenced by decreases in live fetuses and increases in resorptions, occurred at 30 mg/kg/day.
Buprenorphine was not teratogenic in rats or rabbits after IM or subcutaneous (SC) doses up to 5 mg/kg/day (estimated exposure was approximately 3 and 6 times, respectively, the recommended human daily sublingual dose of 16 mg on a mg/m2 basis), after IV doses up to 0.8 mg/kg/day (estimated exposure was approximately 0.5 times and equal to, respectively, the recommended human daily sublingual dose of 16 mg on a mg/m2 basis), or after oral doses up to 160 mg/kg/day in rats (estimated exposure was approximately 95 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis) and 25 mg/kg/day in rabbits (estimated exposure was approximately 30 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis). Significant increases in skeletal abnormalities (e.g., extra thoracic vertebra or thoraco-lumbar ribs) were noted in rats after SC administration of 1 mg/kg/day and up (estimated exposure was approximately 0.6 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis), but were not observed at oral doses up to 160 mg/kg/day. Increases in skeletal abnormalities in rabbits after IM administration of 5 mg/kg/day (estimated exposure was approximately 6 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis) or oral administration of 1 mg/kg/day or greater (estimated exposure was approximately equal to the recommended human daily sublingual dose of 16 mg on a mg/m2 basis) were not statistically significant.
In rabbits, buprenorphine produced statistically significant pre-implantation losses at oral doses of 1 mg/kg/day or greater and post-implantation losses that were statistically significant at IV doses of 0.2 mg/kg/day or greater (estimated exposure approximately 0.3 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis).
Non-teratogenic Effects:
Dystocia was noted in pregnant rats treated intramuscularly with buprenorphine 5 mg/kg/day (approximately 3 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis). Fertility, peri-, and post-natal development studies with buprenorphine in rats indicated increases in neonatal mortality after oral doses of 0.8 mg/kg/day and up (approximately 0.5 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis), after IM doses of 0.5 mg/kg/day and up (approximately 0.3 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis), and after SC doses of 0.1 mg/kg/day and up (approximately 0.06 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis). Delays in the occurrence of righting reflex and startle response were noted in rat pups at an oral dose of 80 mg/kg/day (approximately 50 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis).
8.3 Nursing Mothers
Buprenorphine passes into breast milk. Breast-feeding is not advised in mothers treated with buprenorphine products.
An apparent lack of milk production during general reproduction studies with buprenorphine in rats caused decreased viability and lactation indices.
8.4 Pediatric Use
The safety and effectiveness of SUBOXONE sublingual film have not been established in pediatric patients.
8.5 Geriatric Use
Clinical studies of SUBOXONE sublingual film, SUBOXONE (buprenorphine and naloxone) sublingual tablets, or SUBUTEX (buprenorphine) sublingual tablets did not include sufficient numbers of subjects aged 65 and over to determine whether they responded differently than younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
8.6 Hepatic Impairment
The effect of hepatic impairment on the pharmacokinetics of buprenorphine and naloxone is unknown. Since both drugs are extensively metabolized, the plasma levels will be expected to be higher in patients with moderate and severe hepatic impairment. However, it is not known whether both drugs are affected to the same degree. Therefore, dosage should be adjusted and patients should be watched for signs and symptoms of precipitated opioid withdrawal.
-
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
Buprenorphine is a Schedule III narcotic under the Controlled Substances Act.
Under the Drug Addiction Treatment Act (DATA) codified at 21 U.S.C. 823(g), prescription use of this product in the treatment of opioid dependence is limited to physicians who meet certain qualifying requirements, and who have notified the Secretary of Health and Human Services (HHS) of their intent to prescribe this product for the treatment of opioid dependence and have been assigned a unique identification number that must be included on every prescription.
9.2 Abuse
Buprenorphine, like morphine and other opioids, has the potential for being abused and is subject to criminal diversion. This should be considered when prescribing or dispensing buprenorphine in situations when the clinician is concerned about an increased risk of misuse, abuse, or diversion. Healthcare professionals should contact their state professional licensing board or state controlled substances authority for information on how to prevent and detect abuse or diversion of this product.
Patients who continue to misuse, abuse, or divert buprenorphine products or other opioids should be provided with or referred for more intensive and structured treatment.
Abuse of buprenorphine poses a risk of overdose and death. This risk is increased with the abuse of buprenorphine and alcohol and other substances, especially benzodiazepines.
The physician may be able to more easily detect misuse or diversion by maintaining records of medication prescribed including date, dose, quantity, frequency of refills, and renewal requests of medication prescribed.
Proper assessment of the patient, proper prescribing practices, periodic re-evaluation of therapy, and proper handling and storage of the medication are appropriate measures that help to limit abuse of opioid drugs.
9.3 Dependence
Buprenorphine is a partial agonist at the mu-opioid receptor and chronic administration produces physical dependence of the opioid type, characterized by moderate withdrawal signs and symptoms upon abrupt discontinuation or rapid taper. The withdrawal syndrome is typically milder than seen with full agonists and may be delayed in onset [see Warnings and Precautions (5.5)].
A neonatal withdrawal syndrome has been reported in the infants of women treated with buprenorphine during pregnancy [see Warnings and Precautions (5.9)].
-
10 OVERDOSAGE
The manifestations of acute overdose include pinpoint pupils, sedation, hypotension, respiratory depression, and death.
In the event of overdose, the respiratory and cardiac status of the patient should be monitored carefully. When respiratory or cardiac functions are depressed, primary attention should be given to the re-establishment of adequate respiratory exchange through provision of a patent airway and institution of assisted or controlled ventilation. Oxygen, IV fluids, vasopressors, and other supportive measures should be employed as indicated.
In the case of overdose, the primary management should be the re-establishment of adequate ventilation with mechanical assistance of respiration, if required. Naloxone may be of value for the management of buprenorphine overdose. Higher than normal doses and repeated administration may be necessary.
-
11 DESCRIPTION
SUBOXONE (buprenorphine and naloxone) sublingual film is an orange film, imprinted with a logo identifying the product and strength in white ink. It contains buprenorphine HCl, a mu-opioid receptor partial agonist and a kappa-opioid receptor antagonist, and naloxone HCl dihydrate, an opioid receptor antagonist, at a ratio of 4:1 (ratio of free bases). It is intended for sublingual administration and is available in two dosage strengths, 2 mg buprenorphine with 0.5 mg naloxone and 8 mg buprenorphine with 2 mg naloxone. Each sublingual film also contains polyethylene oxide, hydroxypropyl methylcellulose, maltitol, acesulfame potassium, lime flavor, citric acid, sodium citrate, FD&C yellow #6, and white ink.
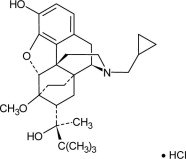
Chemically, buprenorphine HCl is (2S)-2-[17-Cyclopropylmethyl-4,5α-epoxy-3-hydroxy-6-methoxy-6α,14-ethano-14α-morphinan-7α-yl]-3,3-dimethylbutan-2-ol hydrochloride. It has the following chemical structure:
Buprenorphine HCl has the molecular formula C29 H41 NO4 HCl and the molecular weight is 504.10. It is a white or off-white crystalline powder, sparingly soluble in water, freely soluble in methanol, soluble in alcohol, and practically insoluble in cyclohexane.
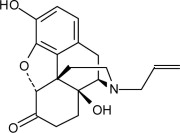
Chemically, naloxone HCl dihydrate is 17-Allyl-4,5 α -epoxy-3, 14-dihydroxymorphinan-6-one hydrochloride dihydrate. It has the following chemical structure:
Naloxone hydrochloride dihydrate has the molecular formula C19H21NO4 HCl 2H20 and the molecular weight is 399.87. It is a white to slightly off-white powder and is freely soluble in water, soluble in alcohol, and practically insoluble in toluene and ether.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
SUBOXONE sublingual film contains buprenorphine and naloxone. Buprenorphine is a partial agonist at the mu-opioid receptor and an antagonist at the kappa-opioid receptor. Naloxone is a potent antagonist at mu- opioid receptors and produces opioid withdrawal signs and symptoms in individuals physically dependent on full opioid agonists when administered parenterally.
12.2 Pharmacodynamics
Subjective Effects:
Comparisons of buprenorphine to full opioid agonists such as methadone and hydromorphone suggest that sublingual buprenorphine produces typical opioid agonist effects which are limited by a ceiling effect.
In opioid-experienced subjects who were not physically dependent, acute sublingual doses of buprenorphine/naloxone tablets produced opioid agonist effects which reached a maximum between doses of 8/2 mg and 16/4 mg buprenorphine/naloxone.
Opioid agonist ceiling-effects were also observed in a double-blind, parallel group, dose-ranging comparison of single doses of buprenorphine sublingual solution (1, 2, 4, 8, 16, or 32 mg), placebo and a full agonist control at various doses. The treatments were given in ascending dose order at intervals of at least one week to 16 opioid-experienced subjects who were not physically dependent. Both active drugs produced typical opioid agonist effects. For all measures for which the drugs produced an effect, buprenorphine produced a dose-related response. However, in each case, there was a dose that produced no further effect. In contrast, the highest dose of the full agonist control always produced the greatest effects. Agonist objective rating scores remained elevated for the higher doses of buprenorphine (8-32 mg) longer than for the lower doses and did not return to baseline until 48 hours after drug administration. The onset of effects appeared more rapidly with buprenorphine than with the full agonist control, with most doses nearing peak effect after 100 minutes for buprenorphine compared to 150 minutes for the full agonist control.
Physiologic Effects:
Buprenorphine in IV (2, 4, 8, 12 and 16 mg) and sublingual (12 mg) doses has been administered to opioid-experienced subjects who were not physically dependent to examine cardiovascular, respiratory, and subjective effects at doses comparable to those used for treatment of opioid dependence. Compared to placebo, there were no statistically significant differences among any of the treatment conditions for blood pressure, heart rate, respiratory rate, O2 saturation, or skin temperature across time. Systolic BP was higher in the 8 mg group than placebo (3-hour AUC values). Minimum and maximum effects were similar across all treatments. Subjects remained responsive to low voice and responded to computer prompts. Some subjects showed irritability, but no other changes were observed.
The respiratory effects of sublingual buprenorphine were compared with the effects of methadone in a double-blind, parallel group, dose ranging comparison of single doses of buprenorphine sublingual solution (1, 2, 4, 8, 16, or 32 mg) and oral methadone (15, 30, 45, or 60 mg) in non-dependent, opioid-experienced volunteers. In this study, hypoventilation not requiring medical intervention was reported more frequently after buprenorphine doses of 4 mg and higher than after methadone. Both drugs decreased O2 saturation to the same degree.
Effect of Naloxone:
Physiologic and subjective effects following acute sublingual administration of buprenorphine tablets and buprenorphine/naloxone tablets were similar at equivalent dose levels of buprenorphine. Naloxone had no clinically significant effect when administered by the sublingual route, although blood levels of the drug were measurable. Buprenorphine/naloxone, when administered sublingually to an opioid-dependent cohort, was recognized as an opioid agonist, whereas when administered intramuscularly, combinations of buprenorphine with naloxone produced opioid antagonist actions similar to naloxone. This finding suggests that the naloxone in buprenorphine/naloxone tablets may deter injection of buprenorphine/naloxone tablets by persons with active substantial heroin or other full mu-opioid dependence. However, clinicians should be aware that some opioid-dependent persons, particularly those with a low level of full mu-opioid physical dependence or those whose opioid physical dependence is predominantly buprenorphine, abuse buprenorphine/naloxone combinations by the intravenous or intranasal route. In methadone-maintained patients and heroin-dependent subjects, IV administration of buprenorphine/naloxone combinations precipitated opioid withdrawal signs and symptoms and was perceived as unpleasant and dysphoric. In morphine-stabilized subjects, intravenously administered combinations of buprenorphine with naloxone produced opioid antagonist and withdrawal signs and symptoms that were ratio-dependent; the most intense withdrawal signs and symptoms were produced by 2:1 and 4:1 ratios, less intense by an 8:1 ratio.
12.3 Pharmacokinetics
Absorption:
Table 3 shows the pharmacokinetic parameters of buprenorphine, norbuprenorphine, and naloxone after administration of SUBOXONE sublingual film in randomized, crossover studies. The pharmacokinetics of the SUBOXONE sublingual film is similar to the pharmacokinetics of the respective dosage strengths of SUBOXONE (buprenorphine and naloxone) sublingual tablets, although not all doses and dose combinations met bioequivalence criteria.
Table 3 Pharmacokinetic parameters of buprenorphine, norbuprenorphine, and naloxone after the sublingual administration of SUBOXONE sublingual film *Naloxone Cmax expressed as pg/mL. Naloxone AUCinf expressed as hpg/mL
Dose Analyte Mean
SDCmax
(ng/mL)Tmax
(h)AUCinf
(hng/mL)t1/2
(h)2 mg/ 0.5 mg Buprenorphine Mean
SD0.947
0.3741.72
0.608.654
2.85433.41
13.01Norbuprenorphine Mean
SD0.312
0.1402.26
2.0314.52
5.77656.09
31.14Naloxone* Mean
SD54.1
23.00.77
0.26137.3
43.105.00
5.528 mg/ 2 mg Buprenorphine Mean
SD3.37
1.801.53
0.6630.45
13.0332.82
9.81Norbuprenorphine Mean
SD1.40
1.082.17
2.6354.91
36.0141.96
17.92Naloxone* Mean
SD193
91.20.81
0.19480.8
201.06.25
3.14Distribution:
Buprenorphine is approximately 96% protein bound, primarily to alpha and beta globulin.
Naloxone is approximately 45% protein bound, primarily to albumin.
Metabolism:
Buprenorphine undergoes both N-dealkylation to norbuprenorphine and glucuronidation. The N-dealkylation pathway is mediated primarily by the CYP3A4. Norbuprenorphine, the major metabolite, can further undergo glucuronidation. Norbuprenorphine has been found to bind opioid receptors in-vitro; however, it has not been studied clinically for opioid-like activity. Naloxone undergoes direct glucuronidation to naloxone-3-glucuronide as well as N-dealkylation, and reduction of the 6-oxo group.
Elimination:
A mass balance study of buprenorphine showed complete recovery of radiolabel in urine (30%) and feces (69%) collected up to 11 days after dosing. Almost all of the dose was accounted for in terms of buprenorphine, norbuprenorphine, and two unidentified buprenorphine metabolites. In urine, most of buprenorphine and norbuprenorphine was conjugated (buprenorphine, 1% free and 9.4% conjugated; norbuprenorphine, 2.7% free and 11% conjugated). In feces, almost all of the buprenorphine and norbuprenorphine were free (buprenorphine, 33% free and 5% conjugated; norbuprenorphine, 21% free and 2% conjugated). Based on all studies performed with SUBOXONE sublingual film, buprenorphine has a mean elimination half-life from plasma ranging from 24 to 42 hours and naloxone has a mean elimination half-life from plasma ranging from 2 to 12 hours.
Drug-drug Interactions:
CYP3A4 Inhibitors and Inducers: Subjects receiving SUBOXONE sublingual film should be monitored if inhibitors of CYP3A4 such as azole antifungal agents (e.g., ketoconazole), macrolide antibiotics (e.g., erythromycin) or HIV protease inhibitors and may require dose-reduction of one or both agents. The interaction of buprenorphine with all CYP3A4 inducers has not been studied, therefore it is recommended that patients receiving SUBOXONE sublingual film be monitored for signs and symptoms of opioid withdrawal if inducers of CYP3A4 (e.g., phenobarbital, carbamazepine, phenytoin, rifampicin) are co-administered [See Drug Interactions (7.1)].
Buprenorphine has been found to be a CYP2D6 and CYP3A4 inhibitor and its major metabolite, norbuprenorphine, has been found to be a moderate CYP2D6 inhibitor in in-vitro studies employing human liver microsomes. However, the relatively low plasma concentrations of buprenorphine and norbuprenorphine resulting from therapeutic doses are not expected to raise significant drug-drug interaction concerns.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity:
Carcinogenicity data on SUBOXONE sublingual film are not available.
A carcinogenicity study of buprenorphine/naloxone (4:1 ratio of the free bases) was performed in Alderley Park rats. Buprenorphine/naloxone was administered in the diet at doses of approximately 7, 31, and 123 mg/kg/day for 104 weeks (estimated exposure was approximately 4, 18, and 44 times the recommended human sublingual dose of 16/4 mg buprenorphine/naloxone based on buprenorphine AUC comparisons. A statistically significant increase in Leydig cell adenomas was observed in all dose groups. No other drug-related tumors were noted.
Carcinogenicity studies of buprenorphine were conducted in Sprague-Dawley rats and CD-1 mice. Buprenorphine was administered in the diet to rats at doses of 0.6, 5.5, and 56 mg/kg/day (estimated exposure was approximately 0.4, 3, and 35 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis) for 27 months. As in the buprenorphine/naloxone carcinogenicity study in rat, statistically significant dose-related increases in Leydig cell tumors occurred. In an 86-week study in CD-1 mice, buprenorphine was not carcinogenic at dietary doses up to 100 mg/kg/day (estimated exposure was approximately 30 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis).
Mutagenicity:
The 4:1 combination of buprenorphine and naloxone was not mutagenic in a bacterial mutation assay (Ames test) using four strains of S. typhimurium and two strains of E. coli. The combination was not clastogenic in an in vitro cytogenetic assay in human lymphocytes or in an IV micronucleus test in the rat.
Buprenorphine was studied in a series of tests utilizing gene, chromosome, and DNA interactions in both prokaryotic and eukaryotic systems. Results were negative in yeast (S. cerevisiae) for recombinant, gene convertant, or forward mutations; negative in Bacillus subtilis “rec” assay, negative for clastogenicity in CHO cells, Chinese hamster bone marrow and spermatogonia cells, and negative in the mouse lymphoma L5178Y assay.
Results were equivocal in the Ames test: negative in studies in two laboratories, but positive for frame shift mutation at a high dose (5mg/plate) in a third study. Results were positive in the Green-Tweets (E. coli) survival test, positive in a DNA synthesis inhibition (DSI) test with testicular tissue from mice, for both in vivo and in vitro incorporation of [3H]thymidine, and positive in unscheduled DNA synthesis (UDS) test using testicular cells from mice.
Impairment of Fertility:
Dietary administration of buprenorphine in the rat at dose levels of 500 ppm or greater (equivalent to approximately 47 mg/kg/day or greater; estimated exposure approximately 28 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis) produced a reduction in fertility demonstrated by reduced female conception rates. A dietary dose of 100 ppm (equivalent to approximately 10 mg/kg/day; estimated exposure approximately 6 times the recommended human daily sublingual dose of 16 mg on a mg/m2 basis) had no adverse effect on fertility.
-
17 PATIENT COUNSELING INFORMATION
17.1 Safe Use
Before initiating treatment with Suboxone, explain the points listed below to caregivers and patients. Instruct patients to read the Medication Guide each time Suboxone is dispensed because new information may be available.
- Patients should be warned that it is extremely dangerous to self-administer non-prescribed benzodiazepines or other CNS depressants (including alcohol) while taking SUBOXONE sublingual film. Patients prescribed benzodiazepines or other CNS depressants should be cautioned to use them only as directed by their physician. [see Warnings and Precautions (5.2), Drug Interactions (7.3)]
- Patients should be advised that SUBOXONE sublingual film contains an opioid that can be a target for people who abuse prescription medications or street drugs. Patients should be cautioned to keep their films in a safe place, and to protect them from theft.
- Patients should be instructed to keep SUBOXONE sublingual film in a secure place, out of the sight and reach of children. Accidental or deliberate ingestion by a child may cause respiratory depression that can result in death. Patients should be advised that if a child is exposed to SUBOXONE sublingual film, medical attention should be sought immediately.
- Patients should be advised never to give SUBOXONE sublingual film to anyone else, even if he or she has the same signs and symptoms. It may cause harm or death.
- Patients should be advised that selling or giving away this medication is against the law.
- Patients should be cautioned that SUBOXONE sublingual film may impair the mental or physical abilities required for the performance of potentially dangerous tasks such as driving or operating machinery. Caution should be taken especially during drug induction and dose adjustment and until individuals are reasonably certain that buprenorphine therapy does not adversely affect their ability to engage in such activities. [see Warnings and Precautions (5.11)]
- Patients should be advised not to change the dosage of SUBOXONE sublingual film without consulting their physician.
- Patients should be advised to take SUBOXONE sublingual film once a day.
- Patients should be informed that SUBOXONE sublingual film can cause drug dependence and that withdrawal signs and symptoms may occur when the medication is discontinued.
- Patients seeking to discontinue treatment with buprenorphine for opioid dependence should be advised to work closely with their physician on a tapering schedule and should be apprised of the potential to relapse to illicit drug use associated with discontinuation of opioid agonist/partial agonist medication-assisted treatment.
- Patients should be cautioned that, like other opioids, SUBOXONE sublingual film may produce orthostatic hypotension in ambulatory individuals. [see Warnings and Precautions. (5.12)]
- Patients should inform their physician if any other prescription medications, over-the-counter medications, or herbal preparations are prescribed or currently being used. [see Drug Interactions (7.1, 7.2 and 7.3)]
- Women of childbearing potential who become pregnant or are planning to become pregnant, should be advised to consult their physician regarding the possible effects of using SUBOXONE sublingual film during pregnancy. [see Use in Specific Populations (8.1)]
- Patients should be warned that buprenorphine passes into breast milk. Breast-feeding is not advised in mothers treated with buprenorphine products. [see Use in Specific Populations (8.3)].
- Patients should inform their family members that, in the event of emergency, the treating physician or emergency room staff should be informed that the patient is physically dependent on an opioid and that the patient is being treated with SUBOXONE sublingual film.
- Refer to the Medication Guide for additional information regarding the counseling information.
17.2 Disposal of Unused SUBOXONE Sublingual Film
Unopened SUBOXONE sublingual films should be disposed of as soon as they are no longer needed:
- Remove the SUBOXONE film from its foil pouch.
- Drop the SUBOXONE film into the toilet.
- Repeat steps 1 and 2 for each SUBOXONE film. Flush the toilet after all unneeded films have been put into the toilet.
Foil pouches or cartons should not be flushed down the toilet.
RA016 09/2010
Revised 9/7/2010Manufactured for Reckitt Benckiser
Pharmaceuticals Inc.,
Richmond, VA 23235 by:
MonoSol Rx, LLC,
Warren, NJ 07059Distributed by:
Reckitt Benckiser Pharmaceuticals Inc.
Richmond, VA 23235 -
MEDICATION GUIDE
MEDICATION GUIDE
SUBOXONE®(Sub-OX-own)
(buprenorphine and naloxone)
Sublingual Film (CIII)IMPORTANT: Keep SUBOXONE in a secure place away from children. Accidental use by a child is a medical emergency and can result in death. If a child accidentally uses SUBOXONE, get emergency help right away. Read this Medication Guide that comes with SUBOXONE before you start taking it and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking to your doctor. Talk to your doctor or pharmacist if you have questions about SUBOXONE.
Share the important information in this Medication Guide with members of your household.
What is the most important information I should know about SUBOXONE?
- SUBOXONE can cause serious and life-threatening breathing problems. Call your doctor right away or get emergency help if:
- You feel faint, dizzy, or confused
- Your breathing gets much slower than is normal for you
These can be signs of an overdose or other serious problems.
- SUBOXONE contains an opioid that can cause physical dependence.
- Do not stop taking SUBOXONE without talking to your doctor. You could become sick with uncomfortable withdrawal signs and symptoms because your body has become used to this medicine.
- Physical dependence is not the same as drug addiction.
- SUBOXONE is not for occasional or “as needed” use.
- An overdose and even death can happen if you take benzodiazepines, sedatives, tranquilizers, antidepressants, or alcohol while using SUBOXONE. Ask your doctor what you should do if you are taking one of these.
- Call a doctor or get emergency help right away if you:
- Feel sleepy and uncoordinated
- Have blurred vision
- Have slurred speech
- Cannot think well or clearly
- Have slowed reflexes and breathing
- Do not inject (“shoot-up”) SUBOXONE
- Injecting this medicine may cause life-threatening infections and other serious health problems.
- Injecting SUBOXONE may cause serious withdrawal symptoms such as pain, cramps, vomiting, diarrhea, anxiety, sleep problems, and cravings.
- In an emergency, have family members tell emergency department staff that you are physically dependent on an opioid and are being treated with SUBOXONE.
What is SUBOXONE?
- SUBOXONE is a prescription medicine used to treat adults who are addicted to (dependent on) opioid drugs (either prescription or illegal) as part of a complete treatment program that also includes counseling and behavioral therapy.
SUBOXONE is a controlled substance (CIII) because it contains buprenorphine, which can be a target for people who abuse prescription medicines or street drugs. Keep your SUBOXONE in a safe place to protect it from theft. Never give your SUBOXONE to anyone else; it can cause death or otherwise harm them. Selling or giving away this medicine is against the law. - It is not known if SUBOXONE is safe or effective in children.
Who should not take SUBOXONE?
Do not take SUBOXONE if you are allergic to buprenorphine or naloxone.
What should I tell my doctor before taking SUBOXONE?
SUBOXONE may not be right for you. Before taking SUBOXONE, tell your doctor if you:
- Have trouble breathing or lung problems
- Have an enlarged prostate gland (men)
- Have a head injury or brain problem
- Have problems urinating
- Have a curve in your spine that affects your breathing
- Have liver or kidney problems
- Have gallbladder problems
- Have adrenal gland problems
- Have Addison's disease
- Have low thyroid (hypothyroidism)
- Have a history of alcoholism
- Have mental problems such as hallucinations (seeing or hearing things that are not there)
- Have any other medical condition
- Are pregnant or plan to become pregnant. It is not known if SUBOXONE will harm your unborn baby. If you take SUBOXONE while pregnant, your baby may have symptoms of withdrawal at birth. Talk to your doctor if you are pregnant or plan to become pregnant.
- Are breast feeding or plan to breast feed. SUBOXONE can pass into your milk and may harm the baby. Talk to your doctor about the best way to feed your baby if you take SUBOXONE. Breast feeding is not recommended while taking SUBOXONE.
Tell your doctor about all the medicines you take, including prescription and nonprescription medicines, vitamins, and herbal supplements. SUBOXONE may affect the way other medicines work, and other medicines may affect how SUBOXONE works. Some medicines may cause serious or life-threatening medical problems when taken with SUBOXONE.
Sometimes the doses of certain medicines and SUBOXONE may need to be changed if used together. Do not take any medicine while using SUBOXONE until you have talked with your doctor. Your doctor will tell you if it is safe to take other medicines while you are using SUBOXONE.
Be especially careful about taking other medicines that may make you sleepy, such as pain medicines, tranquilizers, antidepressant medicines, sleeping pills, anxiety medicines or antihistamines.
Know the medicines you take. Keep a list of them to show your doctor or pharmacist each time you get a new medicine.
How should I take SUBOXONE sublingual film?
- Always take SUBOXONE exactly as your doctor tells you. Your doctor may change your dose after seeing how it affects you. Do not change your dose unless your doctor tells you to change it.
- Do not take SUBOXONE more often than prescribed by your doctor.
- Each SUBOXONE sublingual film comes in a sealed child-resistant foil pouch. Wait to open SUBOXONE until right before you use it.
- To open your SUBOXONE sublingual film foil pouch, fold along the dotted line and tear down at slit (see Figure 1) or cut with scissors along the arrow.
Figure 1
- Before taking SUBOXONE, drink water to moisten your mouth. This helps the film dissolve more easily.
- Hold the film between two fingers by the outside edges.
-
Place SUBOXONE sublingual film under your tongue, close to the base either to the left or right of the center (see Figure 2).
Figure 2
- If your doctor tells you to take 2 films at a time, place the second film under your tongue on the opposite side. Try to avoid having the films touch as much as possible.
- Keep the films in place until they have completely dissolved.
- If you are directed to take a third film, place it under your tongue on either side after the first 2 films have dissolved.
- While SUBOXONE is dissolving, do not chew or swallow the film because the medicine will not work as well.
- Talking while the film is dissolving can affect how well the medicine in SUBOXONE is absorbed.
- If you miss a dose of SUBOXONE, take your medicine when you remember. If it is almost time for your next dose, skip the missed dose and take the next dose at your regular time. Do not take 2 doses at the same time unless your doctor tells you to. If you are not sure about your dosing, call your doctor.
- Do not stop taking SUBOXONE suddenly. You could become sick and have withdrawal symptoms because your body has become used to the medicine. Physical dependence is not the same as drug addiction. Your doctor can tell you more about the differences between physical dependence and drug addiction. To have fewer withdrawal symptoms, ask your doctor how to stop using SUBOXONE the right way.
- If you take too much SUBOXONE or overdose, call Poison Control or get emergency medical help right away.
What should I avoid while taking SUBOXONE?
- Do not drive, operate heavy machinery, or perform any other dangerous activities until you know how this medication affects you. Buprenorphine can cause drowsiness and slow reaction times. This may happen more often in the first few weeks of treatment when your dose is being changed, but can also happen if you drink alcohol or take other sedative drugs when you take SUBOXONE.
- You should not drink alcohol while using SUBOXONE, as this can lead to loss of consciousness or even death.
What are the possible side effects of SUBOXONE?
SUBOXONE can cause serious side effects, including:
- See “What is the most important information I should know about SUBOXONE?”
- Respiratory problems. You have a higher risk of death and coma if you take SUBOXONE with other medicines, such as benzodiazepines.
- Sleepiness, dizziness, and problems with coordination
- Dependency or abuse
- Liver problems. Call your doctor right away if you notice any of these signs of liver problems: Your skin or the white part of your eyes turning yellow (jaundice), urine turning dark, stools turning light in color, you have less of an appetite, or you have stomach (abdominal) pain or nausea. Your doctor should do tests before you start taking and while you take SUBOXONE.
- Allergic reaction. You may have a rash, hives, swelling of the face, wheezing, or a loss of blood pressure and consciousness. Call a doctor or get emergency help right away.
- Opioid withdrawal. This can include: shaking, sweating more than normal, feeling hot or cold more than normal, runny nose, watery eyes, goose bumps, diarrhea, vomiting, and muscle aches. Tell your doctor if you develop any of these symptoms.
- Decrease in blood pressure. You may feel dizzy if you get up too fast from sitting or lying down.
Common side effects of SUBOXONE sublingual film include:
- Nausea
- Vomiting
- Drug withdrawal syndrome
- Headache
- Sweating
- Numb mouth
- Constipation
- Painful tongue
- The inside of your mouth is more red than normal
- Intoxication (feeling lightheaded or drunk)
- Disturbance in attention
- Irregular heart beat (palpitations)
- Decrease in sleep (insomnia)
- Blurred vision
- Back pain
- Fainting
- Dizziness
- Sleepiness
Tell your doctor about any side effect that bothers you or that does not go away.
These are not all the possible side effects of SUBOXONE sublingual film. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store SUBOXONE?
- Store at 25°C (77°F), excursions permitted to 15-30°C (59-86°F).
- Keep SUBOXONE in a safe place, out of the sight and reach of children.
How should I dispose of unused SUBOXONE sublingual film?
- Dispose of unopened SUBOXONE sublingual films as soon as you no longer need them:
- Remove the SUBOXONE film from its foil pouch.
- Drop the SUBOXONE film into the toilet.
- Repeat steps 1 and 2 for each SUBOXONE film. Flush the toilet after all unneeded films have been put into the toilet.
- Do not flush foil pouches or cartons down the toilet.
General information about the safe and effective use of SUBOXONE
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not take SUBOXONE for a condition for which it was not prescribed. Do not give SUBOXONE to other people, even if they have the same symptoms you have. It may harm them and it is against the law.
This Medication Guide summarizes the most important information about SUBOXONE sublingual film. If you would like more information, talk to your doctor or pharmacist. You can ask your doctor or pharmacist for information that is written for healthcare professionals. For more information call 1-877-782-6966.
What are the ingredients in SUBOXONE sublingual film?
Active Ingredients: buprenorphine and naloxone.
Inactive Ingredients: polyethylene oxide, hydroxypropyl methylcellulose, maltitol, acesulfame potassium, lime flavor, citric acid, sodium citrate, FD&C yellow #6, and white ink.
Approved: August 2010
Manufactured for Reckitt Benckiser Pharmaceuticals Inc.
Richmond, VA 23235 by MonoSol Rx LLC, Warren, NJ 07059This Medication Guide has been approved by the US Food and Drug Administration.
SUBOXONE® is a registered trademark of Reckitt Benckiser Healthcare (UK) Ltd.
Copyright © 2010 Reckitt Benckiser Pharmaceuticals Inc.
Printed in USA
TF08054 Rev 09/2010 - SUBOXONE can cause serious and life-threatening breathing problems. Call your doctor right away or get emergency help if:
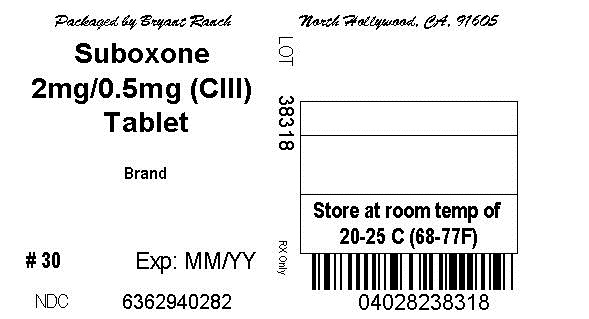
- Suboxone 2mg/0.5mg (CIII) Tablet
-
INGREDIENTS AND APPEARANCE
SUBOXONE
buprenorphine and naloxone film, solubleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 63629-4028(NDC:12496-1202) Route of Administration SUBLINGUAL DEA Schedule CIII Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength BUPRENORPHINE HYDROCHLORIDE (UNII: 56W8MW3EN1) (BUPRENORPHINE - UNII:40D3SCR4GZ) BUPRENORPHINE HYDROCHLORIDE 2 mg NALOXONE HYDROCHLORIDE (UNII: F850569PQR) (NALOXONE - UNII:36B82AMQ7N) NALOXONE HYDROCHLORIDE 0.5 mg Inactive Ingredients Ingredient Name Strength POLYETHYLENE GLYCOLS (UNII: 3WJQ0SDW1A) HYPROMELLOSES (UNII: 3NXW29V3WO) MALTITOL (UNII: D65DG142WK) ACESULFAME POTASSIUM (UNII: 23OV73Q5G9) CITRIC ACID MONOHYDRATE (UNII: 2968PHW8QP) SODIUM CITRATE (UNII: 1Q73Q2JULR) FD&C YELLOW NO. 6 (UNII: H77VEI93A8) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 63629-4028-1 10 in 1 BOTTLE 2 NDC: 63629-4028-2 30 in 1 BOTTLE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA022410 09/13/2010 Labeler - Bryant Ranch Prepack (171714327) Registrant - Bryant Ranch Prepack (171714327) Establishment Name Address ID/FEI Business Operations Monosol Rx LLC 785935235 PACK(63629-4028) Establishment Name Address ID/FEI Business Operations Reckitt Benckiser Healthcare (UK) Ltd 227363660 API MANUFACTURE(63629-4028) Establishment Name Address ID/FEI Business Operations Bryant Ranch Prepack 171714327 REPACK(63629-4028) , RELABEL(63629-4028)
Trademark Results [Suboxone]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 SUBOXONE 78303449 2917297 Dead/Cancelled |
Reckitt Benckiser Healthcare (UK) Limited 2003-09-22 |
 SUBOXONE 77727995 3917631 Live/Registered |
INDIVIOR UK LIMITED 2009-05-04 |
 SUBOXONE 75226449 2169133 Live/Registered |
INDIVIOR UK LIMITED 1997-01-16 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.