EDURANT- rilpivirine hydrochloride tablet, film coated
EDURANT by
Drug Labeling and Warnings
EDURANT by is a Prescription medication manufactured, distributed, or labeled by Janssen Products, LP, Janssen-Cilag SpA, Janssen Pharmaceutica NV, Janssen Pharmaceutical Sciences Unlimited Company, AndersonBrecon Inc. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use EDURANT® safely and effectively. See full prescribing information for EDURANT.
EDURANT (rilpivirine) tablets for oral use
Initial U.S. Approval: 2011RECENT MAJOR CHANGES
Warnings and Precautions, Immune Reconstitution Syndrome (5.6) 05/2019 INDICATIONS AND USAGE
EDURANT is a human immunodeficiency virus type 1 (HIV-1) specific, non-nucleoside reverse transcriptase inhibitor (NNRTI) indicated in combination with other antiretroviral agents for the treatment of HIV-1 infection in treatment-naïve patients 12 years of age and older and weighing at least 35 kg with HIV-1 RNA less than or equal to 100,000 copies/mL (1).
Limitations of Use:
DOSAGE AND ADMINISTRATION
- One tablet taken once daily with a meal. (2.1)
- For pregnant patients who are already on a stable EDURANT regimen prior to pregnancy and who are virologically suppressed (HIV-1 RNA less than 50 copies per mL) the recommended dosage is one 25 mg tablet once daily taken orally with a meal. (2.1, 12.3)
- Rifabutin coadministration: Take two 25-mg tablets of rilpivirine once daily with a meal for the duration of the rifabutin coadministration (2.2)
DOSAGE FORMS AND STRENGTHS
25 mg tablets (3)
CONTRAINDICATIONS
Coadministration of EDURANT is contraindicated with drugs where significant decreases in rilpivirine plasma concentrations may occur, which may result in loss of virologic response and possible resistance and cross-resistance. (4)
WARNINGS AND PRECAUTIONS
- Skin and Hypersensitivity Reactions: Severe skin and hypersensitivity reactions have been reported during postmarketing experience, including cases of Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), with rilpivirine-containing regimens. Immediately discontinue treatment if hypersensitivity or rash with systemic symptoms or elevations in hepatic serum biochemistries develop and closely monitor clinical status, including hepatic serum biochemistries. (5.1)
- Hepatotoxicity: Hepatic adverse events have been reported in patients with underlying liver disease, including hepatitis B or C virus co-infection, or in patients with elevated baseline transaminases. A few cases of hepatotoxicity have occurred in patients with no pre-existing hepatic disease. Monitor liver function tests before and during treatment with EDURANT in patients with underlying hepatic disease, such as hepatitis B or C virus co-infection, or marked elevations in transaminase. Also consider monitoring liver functions tests in patients without pre-existing hepatic dysfunction or other risk factors. (5.2)
- Depressive Disorders: Severe depressive disorders have been reported. Immediate medical evaluation is recommended for severe depressive disorders. (5.3)
- Patients may develop redistribution/accumulation of body fat (5.5) or immune reconstitution syndrome. (5.6)
ADVERSE REACTIONS
The most common adverse drug reactions to EDURANT (incidence > 2%) of at least moderate to severe intensity (≥ Grade 2) were depressive disorders, headache, insomnia and rash. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Janssen Products, LP at 1-800-JANSSEN (1-800-526-7736) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.DRUG INTERACTIONS
- Consider alternatives to EDURANT when coadministered with drugs with a known risk of torsade de pointes. (5.4)
- EDURANT should not be used in combination with NNRTIs. (4, 7)
- Coadministration of EDURANT with drugs that induce or inhibit CYP3A may affect the plasma concentrations of rilpivirine. (4, 7)
- Coadministration of EDURANT with drugs that increase gastric pH may decrease plasma concentrations of rilpivirine. (4, 7)
- Refer to the Full Prescribing Information for other drugs that should not be coadministered with EDURANT and for other drugs that may require a change in dose or regimen. (7)
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 5/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
2.2 Recommended Dosage with Rifabutin Coadministration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Skin and Hypersensitivity Reactions
5.2 Hepatotoxicity
5.3 Depressive Disorders
5.4 Risk of Adverse Reactions or Loss of Virologic Response Due to Drug Interactions
5.5 Fat Redistribution
5.6 Immune Reconstitution Syndrome
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Treatment-Naïve Adult Subjects
14.2 Treatment-Naïve Pediatric Subjects (12 to less than 18 years of age)
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
EDURANT®, in combination with other antiretroviral agents, is indicated for the treatment of human immunodeficiency virus type 1 (HIV-1) infection in antiretroviral treatment-naïve patients 12 years of age and older and weighing at least 35 kg with plasma HIV-1 RNA less than or equal to 100,000 copies/mL at the start of therapy.
Limitations of Use:
- More EDURANT treated subjects with HIV-1 RNA greater than 100,000 copies/mL at the start of therapy experienced virologic failure (HIV-1 RNA ≥ 50 copies/mL) compared to EDURANT treated subjects with HIV-1 RNA less than or equal to 100,000 copies/mL [see Clinical Studies (14.1)].
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
The recommended dosage of EDURANT in patients 12 years of age and older and weighing at least 35 kg is one 25 mg tablet taken orally once daily with a meal [see Use in Specific Populations (8.4) and Clinical Pharmacology (12.3)].
For pregnant patients who are already on a stable EDURANT regimen prior to pregnancy and who are virologically suppressed (HIV-1 RNA less than 50 copies per mL) the recommended dosage is one 25 mg tablet once daily taken orally with a meal. Lower exposures of rilpivirine were observed during pregnancy, therefore viral load should be monitored closely [see Use in Specific Populations (8.1) and Clinical Pharmacology (12.3)].
2.2 Recommended Dosage with Rifabutin Coadministration
If EDURANT is coadministered with rifabutin, the EDURANT dose should be increased to 50 mg (two tablets of 25 mg each) once daily, taken with a meal. When rifabutin coadministration is stopped, the EDURANT dose should be decreased to 25 mg once daily, taken with a meal [see Drug Interactions (7) and Clinical Pharmacology (12.3)].
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
EDURANT is contraindicated for coadministration with the drugs in Table 1 for which significant decreases in rilpivirine plasma concentrations may occur due to CYP3A enzyme induction or gastric pH increase, which may result in loss of virologic response and possible resistance to EDURANT or to the class of NNRTIs [see Drug Interactions (7) and Clinical Pharmacology (12.3)]
Table 1. Drugs That are Contraindicated with EDURANT Drug Class Contraindicated Drugs in Class Clinical Comment Anticonvulsants Carbamazepine
Oxcarbazepine
Phenobarbital
PhenytoinPotential for significant decreases in rilpivirine plasma concentrations due to CYP3A enzyme induction, which may result in loss of virologic response. Antimycobacterials Rifampin
RifapentineGlucocorticoid (systemic) Dexamethasone
(more than a single-dose treatment)Herbal Products St John's wort (Hypericum perforatum) Proton Pump Inhibitors e.g., Esomeprazole
Lansoprazole
Omeprazole
Pantoprazole RabeprazolePotential for significant decreases in rilpivirine plasma concentrations due to gastric pH increase, which may result in loss of virologic response. -
5 WARNINGS AND PRECAUTIONS
5.1 Skin and Hypersensitivity Reactions
Severe skin and hypersensitivity reactions have been reported during the postmarketing experience, including cases of Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), with rilpivirine-containing regimens. While some skin reactions were accompanied by constitutional symptoms such as fever, other skin reactions were associated with organ dysfunctions, including elevations in hepatic serum biochemistries. During the Phase 3 clinical trials, treatment-related rashes with at least Grade 2 severity were reported in 3% of subjects receiving EDURANT. No Grade 4 rash was reported. Overall, most rashes were Grade 1 or 2 and occurred in the first four to six weeks of therapy [see Adverse Reactions (6 and 6.2)]. Discontinue EDURANT immediately if signs or symptoms of severe skin or hypersensitivity reactions develop, including but not limited to, severe rash or rash accompanied by fever, blisters, mucosal involvement, conjunctivitis, facial edema, angioedema, hepatitis or eosinophilia. Clinical status including laboratory parameters should be monitored and appropriate therapy should be initiated.
5.2 Hepatotoxicity
Hepatic adverse events have been reported in patients receiving a rilpivirine-containing regimen. Patients with underlying hepatitis B or C virus infection, or marked elevations in transaminases prior to treatment may be at increased risk for worsening or development of transaminase elevations with use of EDURANT. A few cases of hepatic toxicity have been reported in adult patients receiving a rilpivirine-containing regimen who had no pre-existing hepatic disease or other identifiable risk factors. Appropriate laboratory testing prior to initiating therapy and monitoring for hepatotoxicity during therapy with EDURANT is recommended in patients with underlying hepatic disease such as hepatitis B or C virus infection, or in patients with marked elevations in transaminases prior to treatment initiation. Liver enzyme monitoring should also be considered for patients without pre-existing hepatic dysfunction or other risk factors.
5.3 Depressive Disorders
The adverse reaction depressive disorders (depressed mood, depression, dysphoria, major depression, mood altered, negative thoughts, suicide attempt, suicidal ideation) has been reported with EDURANT. Patients with severe depressive symptoms should seek immediate medical evaluation to assess the possibility that the symptoms are related to EDURANT, and if so, to determine whether the risks of continued therapy outweigh the benefits.
During the Phase 3 trials in adults (N = 1368) through 96 weeks, the incidence of depressive disorders (regardless of causality, severity) reported among EDURANT (n = 686) or efavirenz (n = 682) was 9% and 8%, respectively. Most events were mild or moderate in severity. The incidence of Grade 3 and 4 depressive disorders (regardless of causality) was 1% for both EDURANT and efavirenz. The incidence of discontinuation due to depressive disorders among EDURANT or efavirenz was 1% in each arm. Suicidal ideation was reported in 4 subjects in each arm while suicide attempt was reported in 2 subjects in the EDURANT arm.
During the Phase 2 trial in pediatric subjects 12 to less than 18 years of age (N = 36) receiving EDURANT through 48 weeks, the incidence of depressive disorders (regardless of causality, severity) was 19.4% (7/36). Most events were mild or moderate in severity. The incidence of Grade 3 and 4 depressive disorders (regardless of causality) was 5.6% (2/36). None of the subjects discontinued due to depressive disorders. Suicidal ideation and suicide attempt were reported in 1 subject.
5.4 Risk of Adverse Reactions or Loss of Virologic Response Due to Drug Interactions
The concomitant use of EDURANT and other drugs may result in potentially significant drug interactions, some of which may lead to [see Dosage and Administration (2.2), Contraindications (4), and Drug Interactions (7)]:
- Loss of therapeutic effect of EDURANT and possible development of resistance.
In healthy subjects, 75 mg once daily and 300 mg once daily (3 times and 12 times the dose in EDURANT) have been shown to prolong the QTc interval of the electrocardiogram. Consider alternatives to EDURANT when coadministered with a drug that is known to have a risk of torsade de pointes [see Drug Interactions (7) and Clinical Pharmacology (12.2)].
See Table 5 for steps to prevent or manage these possible and known significant drug interactions, including dosing recommendations. Consider the potential for drug interactions prior to and during EDURANT therapy and review concomitant medications during EDURANT therapy.
5.5 Fat Redistribution
Redistribution/accumulation of body fat, including central obesity, dorsocervical fat enlargement (buffalo hump), peripheral wasting, facial wasting, breast enlargement, and "cushingoid appearance" have been observed in patients receiving antiretroviral therapy. The mechanism and long-term consequences of these events are currently unknown. A causal relationship has not been established.
5.6 Immune Reconstitution Syndrome
Immune reconstitution syndrome has been reported in patients treated with combination antiretroviral therapy, including EDURANT. During the initial phase of combination antiretroviral treatment, patients whose immune system responds may develop an inflammatory response to indolent or residual opportunistic infections (such as Mycobacterium avium infection, cytomegalovirus, Pneumocystis jirovecii pneumonia or tuberculosis), which may necessitate further evaluation and treatment.
Autoimmune disorders (such as Graves' disease, polymyositis, and Guillain-Barré syndrome, and autoimmune hepatitis) have also been reported to occur in the setting of immune reconstitution; however, the time to onset is more variable, and can occur many months after initiation of treatment.
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed below and in other sections of the labeling:
- Skin and Hypersensitivity Reactions [see Warnings and Precautions (5.1)]
- Hepatotoxicity [see Warnings and Precautions (5.2)]
- Depressive Disorders [see Warnings and Precautions (5.3)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Clinical Trials Experience in Adults
The safety assessment is based on the Week 96 pooled data from 1368 patients in the Phase 3 controlled trials TMC278-C209 (ECHO) and TMC278-C215 (THRIVE) in antiretroviral treatment-naïve HIV-1 infected adult patients, 686 of whom received EDURANT (25 mg once daily) [see Clinical Studies (14.1)]. The median duration of exposure for patients in the EDURANT arm and efavirenz arm was 104.3 and 104.1 weeks, respectively. Most ADRs occurred in the first 48 weeks of treatment. The proportion of subjects who discontinued treatment with EDURANT or efavirenz due to ADR, regardless of severity, was 2% and 4%, respectively. The most common ADRs leading to discontinuation were psychiatric disorders: 10 (1%) subjects in the EDURANT arm and 11 (2%) subjects in the efavirenz arm. Rash led to discontinuation in 1 (0.1%) subject in the EDURANT arm and 10 (1.5%) subjects in the efavirenz arm.
Common Adverse Drug Reactions
ADRs of at least moderate intensity (≥ Grade 2) reported in at least 2% of adult subjects are presented in Table 2. Selected laboratory abnormalities are included in Table 3.
Table 2: Selected Adverse Drug Reactions of at least Moderate Intensity* (Grades 2–4) Occurring in at Least 2% of Antiretroviral Treatment-Naïve HIV-1 Infected Adult Subjects (Week 96 Analysis) System Organ Class,
Preferred Term,
%Pooled Data from the Phase 3 TMC278-C209 and TMC278-C215 Trials EDURANT + BR
N=686Efavirenz + BR
N=682N = total number of subjects per treatment group; BR = background regimen - * Intensities are defined as follows: Moderate (discomfort enough to cause interference with usual activity); Severe (incapacitating with inability to work or do usual activity).
- † Includes adverse drug reactions reported as depressed mood, depression, dysphoria, major depression, mood altered, negative thoughts, suicide attempt, suicide ideation.
Gastrointestinal Disorders Abdominal pain 2% 2% Nausea 1% 3% Vomiting 1% 2% General Disorders and Administration Site Conditions Fatigue 2% 2% Nervous System Disorders Headache 3% 4% Dizziness 1% 7% Psychiatric Disorders Depressive disorders† 5% 4% Insomnia 3% 4% Abnormal dreams 2% 4% Skin and Subcutaneous Tissue Disorders Rash 3% 11% No new ADR terms were identified in adult subjects in the Phase 3 TMC278-C209 and TMC278-C215 trials between 48 weeks and 96 weeks nor in the Phase 2b TMC278-C204 trial through 240 weeks. The incidence of adverse events in the Phase 2b TMC278-C204 trial was similar to the Phase 3 trials through 96 weeks.
Less Common Adverse Drug Reactions
ADRs of at least moderate intensity (≥ Grade 2) occurring in less than 2% of antiretroviral treatment-naïve subjects receiving EDURANT are listed below by System Organ Class. Some adverse events have been included because of investigator's assessment of potential causal relationship and were considered serious or have been reported in more than 1 subject treated with EDURANT.
Gastrointestinal Disorders: diarrhea, abdominal discomfort
Hepatobiliary Disorders: cholecystitis, cholelithiasis
Metabolism and Nutrition Disorders: decreased appetite
Nervous System Disorders: somnolence
Psychiatric Disorders: sleep disorders, anxiety
Renal and Urinary Disorders: glomerulonephritis membranous, glomerulonephritis mesangioproliferative, nephrolithiasis
Laboratory Abnormalities in Treatment-Naïve Subjects
The percentage of subjects treated with EDURANT or efavirenz in the Phase 3 trials with selected laboratory abnormalities (Grades 1 to 4), representing worst Grade toxicity are shown in Table 3.
Table 3: Selected Changes in Laboratory Parameters (Grades 1 to 4) Observed in Antiretroviral Treatment-Naïve HIV-1-Infected Adult Subjects (Week 96 Analysis) Laboratory Parameter Abnormality, (%) DAIDS Toxicity Range Pooled Data from the Phase 3 TMC278-C209 and TMC278-C215 Trials EDURANT + BR
N=686Efavirenz + BR
N=682BIOCHEMISTRY BR = background regimen; ULN = upper limit of normal N = number of subjects per treatment group Note: Percentages were calculated versus the number of subjects in ITT. Increased Creatinine Grade 1 ≥ 1.1–≤ 1.3 × ULN 6% 1% Grade 2 > 1.3–≤ 1.8 × ULN 1% 1% Grade 3 > 1.8–≤ 3.4 × ULN <1% 0 Grade 4 > 3.4 × ULN 0 <1% Increased AST Grade 1 ≥ 1.25–≤ 2.5 × ULN 16% 19% Grade 2 > 2.5–≤ 5.0 × ULN 4% 7% Grade 3 > 5.0–≤ 10.0 × ULN 2% 2% Grade 4 > 10.0 × ULN 1% 1% Increased ALT Grade 1 ≥ 1.25–≤ 2.5 × ULN 18% 20% Grade 2 > 2.5–≤ 5.0 × ULN 5% 7% Grade 3 > 5.0–≤ 10.0 × ULN 1% 2% Grade 4 > 10.0 × ULN 1% 1% Increased Total Bilirubin Grade 1 ≥ 1.1–≤ 1.5 × ULN 5% <1% Grade 2 > 1.5–≤ 2.5 × ULN 3% 1% Grade 3 > 2.5–≤ 5.0 × ULN 1% <1% Grade 4 > 5.0 × ULN 0 0 Increased Total Cholesterol (fasted) Grade 1 5.18–6.19 mmol/L
200–239 mg/dL17% 31% Grade 2 6.20–7.77 mmol/L
240–300 mg/dL7% 19% Grade 3 > 7.77 mmol/L
> 300 mg/dL<1% 3% Increased LDL Cholesterol (fasted) Grade 1 3.37–4.12 mmol/L
130–159 mg/dL14% 26% Grade 2 4.13–4.90 mmol/L
160–190 mg/dL5% 13% Grade 3 ≥ 4.91 mmol/L
≥ 191 mg/dL1% 5% Increased Triglycerides (fasted) Grade 2 5.65–8.48 mmol/L
500–750 mg/dL2% 2% Grade 3 8.49–13.56 mmol/L
751–1,200 mg/dL1% 3% Grade 4 > 13.56 mmol/L
> 1,200 mg/dL0 1% Adrenal Function
In the pooled Phase 3 trials, at Week 96, there was an overall mean change from baseline in basal cortisol of -0.69 (-1.12, 0.27) micrograms/dL in the EDURANT group and of -0.02 (-0.48, 0.44) micrograms/dL in the efavirenz group.
In the EDURANT group, 43/588 (7.3%) of subjects with a normal 250 micrograms ACTH stimulation test at baseline developed an abnormal 250 micrograms ACTH stimulation test (peak cortisol level < 18.1 micrograms/dL) during the trial compared to 18/561 (3.2%) in the efavirenz group. Of the subjects who developed an abnormal 250 micrograms ACTH stimulation test during the trial, fourteen subjects in the EDURANT group and nine subjects in the efavirenz group had an abnormal 250 micrograms ACTH stimulation test at Week 96. Overall, there were no serious adverse events, deaths, or treatment discontinuations that could clearly be attributed to adrenal insufficiency. The clinical significance of the higher abnormal rate of 250 micrograms ACTH stimulation tests in the EDURANT group is not known.
Serum Creatinine
In the pooled Phase 3 trials, an increase in serum creatinine was observed over the 96 weeks of treatment with EDURANT. Most of this increase occurred within the first four weeks of treatment, with a mean change of 0.1 mg/dL (range: -0.3 mg/dL to 0.6 mg/dL) observed after 96 weeks of treatment. In subjects who entered the trial with mild or moderate renal impairment, the serum creatinine increase observed was similar to that seen in subjects with normal renal function. These changes are not considered to be clinically relevant and no subject discontinued treatment due to increases in serum creatinine. Serum creatinine increases occurred regardless of the background N(t)RTI regimen.
Serum Lipids
Changes from baseline in total cholesterol, LDL-cholesterol, HDL-cholesterol and triglycerides are presented in Table 4. The clinical benefit of these findings has not been demonstrated.
Table 4: Lipid Values, Mean Change from Baseline* Pooled Data from the Week 96 Analysis of the Phase 3 TMC278-C209 and TMC278-C215 Trials EDURANT + BR Efavirenz + BR N Baseline Week 96 N Baseline Week 96 Mean
(95% CI)Mean
(mg/dL)Mean
(mg/dL)Mean Change†
(mg/dL)Mean
(mg/dL)Mean
(mg/dL)Mean Change†
(mg/dL)N = number of subjects per treatment group; BR = background regimen - * Excludes subjects who received lipid lowering agents during the treatment period
- † The change from baseline is the mean of within-patient changes from baseline for patients with both baseline and Week 96 values
Total Cholesterol
(fasted)546 161
166
5
507 160
187
28
HDL-cholesterol
(fasted)545 41
46
4
505 40
51
11
LDL-cholesterol
(fasted)543 96
98
1
503 95
109
14
Triglycerides
(fasted)546 122
116
-6
507 130
141
11
Subjects co-infected with hepatitis B and/or hepatitis C virus
In subjects co-infected with hepatitis B or C virus receiving EDURANT, the incidence of hepatic enzyme elevation was higher than in subjects receiving EDURANT who were not co-infected. This observation was the same in the efavirenz arm. The pharmacokinetic exposure of rilpivirine in co-infected subjects was comparable to that in subjects without co-infection.
Clinical Trials Experience in Pediatric Patients
The safety assessment is based on the Week 48 analysis of the single-arm, open-label, Phase 2 trial, TMC278-C213, in which 36 antiretroviral treatment-naïve HIV-1 infected patients 12 to less than 18 years of age and weighing at least 32 kg received EDURANT (25 mg once daily) in combination with other antiretroviral agents [see Clinical Studies (14.2)]. The median duration of exposure was 63.5 weeks. There were no patients who discontinued treatment due to ADRs. No new ADRs were identified compared to those seen in adults.
ADRs were reported in nineteen pediatric subjects (52.8%). Most ADRs were Grade 1 or 2. The most common ADRs reported in at least 2 subjects (regardless of severity) include headache (19.4%), depression (19.4%), somnolence (13.9%), nausea (11.1%), dizziness (8.3%), abdominal pain (8.3), vomiting (5.6%) and rash (5.6%).
Observed laboratory abnormalities were comparable to those in adults.
Adrenal Function
In trial TMC278 C213, at Week 48, the overall mean change from baseline in basal cortisol showed an increase of 1.59 (0.24, 2.93) micrograms/dL.
Six of 30 (20%) subjects with a normal 250 micrograms ACTH stimulation test at baseline developed an abnormal 250 micrograms ACTH stimulation test (peak cortisol level < 18.1 micrograms/dL) during the trial. Three of these subjects had an abnormal 250 micrograms ACTH stimulation test at Week 48. Overall, there were no serious adverse events, deaths, or treatment discontinuations that could clearly be attributed to adrenal insufficiency. The clinical significance of the abnormal 250 micrograms ACTH stimulation tests is not known.
6.2 Postmarketing Experience
Adverse reactions have been identified during postmarketing experience in patients receiving a rilpivirine containing regimen. Because these reactions are reported voluntarily from a population of unknown size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Renal and Genitourinary Disorders: nephrotic syndrome
Skin and Subcutaneous Tissue Disorders: Severe skin and hypersensitivity reactions including DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms)
-
7 DRUG INTERACTIONS
[see Dosage and Administration (2), Contraindications (4) and Clinical Pharmacology (12.3).]
Rilpivirine is primarily metabolized by cytochrome P450 (CYP)3A, and drugs that induce or inhibit CYP3A may thus affect the clearance of rilpivirine. Coadministration of EDURANT and drugs that induce CYP3A may result in decreased plasma concentrations of rilpivirine and loss of virologic response and possible resistance to rilpivirine or to the class of NNRTIs. Coadministration of EDURANT and drugs that inhibit CYP3A may result in increased plasma concentrations of rilpivirine. Coadministration of EDURANT with drugs that increase gastric pH may result in decreased plasma concentrations of rilpivirine and loss of virologic response and possible resistance to rilpivirine or to the class of NNRTIs.
EDURANT at a dose of 25 mg once daily is not likely to have a clinically relevant effect on the exposure of drugs metabolized by CYP enzymes.
Table 5 shows the established and other potentially significant drug interactions based on which alterations in dose or regimen of EDURANT and/or coadministered drug may be recommended. Drugs that are not recommended for coadministration with EDURANT are also included in Table 5.
Table 5: Established and Other Potentially Significant Drug Interactions: Alterations in Dose or Regimen May Be Recommended Based on Drug Interaction Studies or Predicted Interaction [see Clinical Pharmacology (12.3)] Concomitant Drug Class:
Drug NameEffect on Concentration of Rilpivirine or Concomitant Drug Clinical Comment ↑ = increase, ↓ = decrease, ↔ = no change
- * The interaction between EDURANT and the drug was evaluated in a clinical study. All other drug-drug interactions shown are predicted.
- † This interaction study has been performed with a dose higher than the recommended dose for EDURANT assessing the maximal effect on the coadministered drug. The dosing recommendation is applicable to the recommended dose of EDURANT 25 mg once daily.
Antacids:
antacids (e.g., aluminum or magnesium hydroxide, calcium carbonate)↔ rilpivirine (antacids taken at least 2 hours before or at least 4 hours after rilpivirine) The combination of EDURANT and antacids should be used with caution as coadministration may cause significant decreases in rilpivirine plasma concentrations (increase in gastric pH). Antacids should only be administered either at least 2 hours before or at least 4 hours after EDURANT. ↓ rilpivirine (concomitant intake) Anticonvulsants:
Carbamazepine
Oxcarbazepine
Phenobarbital
Phenytoin↓Rilpivirine Coadministration is contraindicated with EDURANT [see Contraindications (4)]. Antimycobacterials:
Rifampin
Rifapentine↓Rilpivirine Coadministration is contraindicated with EDURANT [see Contraindications (4)]. Antimycobacterials:
rifabutin*↓ rilpivirine Concomitant use of EDURANT with rifabutin may cause a decrease in the plasma concentrations of rilpivirine (induction of CYP3A enzymes). Throughout coadministration of EDURANT with rifabutin, the EDURANT dose should be increased from 25 mg once daily to 50 mg once daily. When rifabutin coadministration is stopped, the EDURANT dose should be decreased to 25 mg once daily. Azole Antifungal Agents:
fluconazole
itraconazole
ketoconazole*†
posaconazole
voriconazole↑ rilpivirine
↓ ketoconazoleConcomitant use of EDURANT with azole antifungal agents may cause an increase in the plasma concentrations of rilpivirine (inhibition of CYP3A enzymes). No rilpivirine dose adjustment is required when EDURANT is coadministered with azole antifungal agents. Clinically monitor for breakthrough fungal infections when azole antifungals are coadministered with EDURANT. Glucocorticoid (systemic):
Dexamethasone
(more than a single-dose treatment)↓Rilpivirine Coadministration is contraindicated with EDURANT [see Contraindications (4)]. H2-Receptor Antagonists:
cimetidine
famotidine*†
nizatidine
ranitidine↔ rilpivirine (famotidine taken 12 hours before rilpivirine or 4 hours after rilpivirine) The combination of EDURANT and H2-receptor antagonists should be used with caution as coadministration may cause significant decreases in rilpivirine plasma concentrations (increase in gastric pH). H2-receptor antagonists should only be administered at least 12 hours before or at least 4 hours after EDURANT. ↓ rilpivirine (famotidine taken 2 hours before rilpivirine) Herbal Products:
St John's wort (Hypericum perforatum)↓Rilpivirine Coadministration is contraindicated with EDURANT [see Contraindications (4)]. HIV-Antiviral Agents: Non-nucleoside Reverse Transcriptase Inhibitors (NNRTIs) NNRTI
(delavirdine)↑ rilpivirine
↔ delavirdineIt is not recommended to coadminister EDURANT with delavirdine and other NNRTIs. Other NNRTIs
(efavirenz, etravirine, nevirapine)↓ rilpivirine
↔ other NNRTIsHIV-Antiviral Agents: Nucleoside Reverse Transcriptase Inhibitors (NRTIs) didanosine*† ↔ rilpivirine
↔ didanosineNo dose adjustment is required when EDURANT is coadministered with didanosine. Didanosine is to be administered on an empty stomach and at least two hours before or at least four hours after EDURANT (which should be administered with a meal). HIV-Antiviral Agents: Protease Inhibitors (PIs)-Boosted (i.e., with coadministration of low-dose ritonavir) or Unboosted (i.e., without coadministration of low-dose ritonavir) darunavir/ritonavir*† ↑ rilpivirine
↔ boosted darunavirConcomitant use of EDURANT with darunavir/ritonavir may cause an increase in the plasma concentrations of rilpivirine (inhibition of CYP3A enzymes). No dose adjustment is required when EDURANT is coadministered with darunavir/ritonavir. lopinavir/ritonavir*† ↑ rilpivirine
↔ boosted lopinavirConcomitant use of EDURANT with lopinavir/ritonavir may cause an increase in the plasma concentrations of rilpivirine (inhibition of CYP3A enzymes). No dose adjustment is required when EDURANT is coadministered with lopinavir/ritonavir. other boosted PIs (atazanavir/ritonavir, fosamprenavir/ritonavir, saquinavir/ritonavir, tipranavir/ritonavir) ↑ rilpivirine
↔ boosted PIConcomitant use of EDURANT with boosted PIs may cause an increase in the plasma concentrations of rilpivirine (inhibition of CYP3A enzymes). EDURANT is not expected to affect the plasma concentrations of coadministered PIs. unboosted PIs (atazanavir, fosamprenavir, indinavir, nelfinavir) ↑ rilpivirine
↔ unboosted PIConcomitant use of EDURANT with unboosted PIs may cause an increase in the plasma concentrations of rilpivirine (inhibition of CYP3A enzymes). EDURANT is not expected to affect the plasma concentrations of coadministered PIs. Macrolide or ketolide antibiotics:
clarithromycin
erythromycin
telithromycin↑ rilpivirine
↔ clarithromycin
↔ erythromycin
↔ telithromycinConcomitant use of EDURANT with clarithromycin, erythromycin or telithromycin may cause an increase in the plasma concentrations of rilpivirine (inhibition of CYP3A enzymes). Where possible, alternatives such as azithromycin should be considered. Narcotic Analgesics:
methadone*↓ R(-) methadone
↓ S(+) methadoneNo dose adjustments are required when initiating coadministration of methadone with EDURANT. However, clinical monitoring is recommended as methadone maintenance therapy may need to be adjusted in some patients. Proton Pump Inhibitors:
e.g., Esomeprazole
Lansoprazole
Omeprazole
Pantoprazole
Rabeprazole↓Rilpivirine Coadministration is contraindicated with EDURANT [see Contraindications (4)]. In addition to the drugs included in Table 5, the interaction between EDURANT and the following drugs was evaluated in clinical studies and no dose adjustment is needed for either drug [see Clinical Pharmacology (12.3)]: acetaminophen, atorvastatin, chlorzoxazone, ethinylestradiol, norethindrone, raltegravir, sildenafil, simeprevir and tenofovir disoproxil fumarate. Rilpivirine did not have a clinically significant effect on the pharmacokinetics of digoxin or metformin. No clinically relevant drug-drug interaction is expected when EDURANT is coadministered with maraviroc, ribavirin or the NRTIs abacavir, emtricitabine, lamivudine, stavudine and zidovudine.
QT Prolonging Drugs
There is limited information available on the potential for a pharmacodynamic interaction between rilpivirine and drugs that prolong the QTc interval of the electrocardiogram. In a study of healthy subjects, 75 mg once daily and 300 mg once daily (3 times and 12 times the dose in EDURANT) have been shown to prolong the QTc interval of the electrocardiogram [see Clinical Pharmacology (12.2)]. Consider alternatives to EDURANT when coadministered with a drug with a known risk of torsade de pointes.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to EDURANT during pregnancy. Healthcare providers are encouraged to register patients by calling the Antiretroviral Pregnancy Registry (APR) 1-800-258-4263.
Risk Summary
Available data from the APR show no difference in the overall risk of birth defects for rilpivirine compared with the background rate for major birth defects of 2.7% in the Metropolitan Atlanta Congenital Defects Program (MACDP) reference population (see Data). The rate of miscarriage is not reported in the APR. The estimated background rate of miscarriage in clinically recognized pregnancies in the U.S. general population is 15% to 20%. The background risk for major birth defects and miscarriage for the indicated population is unknown. Methodologic limitations of the APR include the use of MACDP as the external comparator group. The MACDP population is not disease-specific, evaluates women and infants from a limited geographic area, and does not include outcomes for births that occurred at <20 weeks gestation. In a clinical trial, total rilpivirine exposures were generally lower during pregnancy compared to the postpartum period (see Data).
In animal reproduction studies, no evidence of adverse developmental outcomes was observed following oral administration of rilpivirine (see Data). During organogenesis, systemic exposures (AUC) to rilpivirine were up to 15 (rats) and 70 (rabbits) times the exposure in humans at the recommended daily dose of rilpivirine. In the rat pre- and post-natal developmental study, maternal systemic exposure (AUC) was approximately 63 times the exposure at the recommended daily dose of rilpivirine.
Clinical Considerations
Dose adjustments during pregnancy and the postpartum period
Based on the experience of HIV-1-infected pregnant women who completed a clinical trial through the postpartum period with a rilpivirine-based regimen, no dose adjustments are required for pregnant patients who are already on a stable EDURANT regimen prior to pregnancy and who are virologically suppressed (HIV-1 RNA less than 50 copies per mL). The recommended dosage is one 25 mg tablet once daily taken orally with a meal. Lower exposures of rilpivirine were observed during pregnancy, therefore viral load should be monitored closely [see Clinical Pharmacology (12.3)].
Data
Human Data
Based on prospective reports to the APR of over 390 exposures to rilpivirine during pregnancy resulting in live births, (including over 247 exposed during first trimester), there was no significant difference between the overall risk of birth defects with rilpivirine compared to the background birth defect rate of 2.7% in the U.S. reference population of the MACDP. The prevalence of birth defects in live births was 1.2% (95% CI: 0.3% to 3.5%) and 1.4% (95% CI: 0.2% to 5.0%) following first and second/third trimester exposure, respectively, to rilpivirine-containing regimens.
Rilpivirine in combination with a background regimen was evaluated in a clinical trial of 19 HIV-1 infected pregnant women during the second and third trimesters and postpartum. Each of the women were on a rilpivirine-based regimen at the time of enrollment. Twelve subjects completed the trial through the postpartum period (6-12 weeks after delivery) and pregnancy outcomes are missing for six subjects. The exposure (C0h and AUC) of total rilpivirine was approximately 30 to 40% lower during pregnancy compared with postpartum (6 to 12 weeks). The protein binding of rilpivirine was similar (>99%) during second trimester, third trimester, and postpartum period. One subject discontinued the trial following spontaneous termination of the pregnancy at 25 weeks gestation due to suspected premature rupture of membranes. Among the 12 subjects who were virologically suppressed at baseline (less than 50 copies/mL), virologic response was preserved in 10 subjects (83.3%) through the third trimester visit and in 9 subjects (75%) through the 6-12 week postpartum visit. Virologic outcomes during the third trimester visit were missing for two subjects who were withdrawn (one subject was nonadherent to the study drug and one subject withdrew consent). Among the 10 infants with HIV test results available, born to 10 HIV-infected pregnant women, all had test results that were negative for HIV-1 at the time of delivery and up to 16 weeks postpartum. All 10 infants received antiretroviral prophylactic treatment with zidovudine. Rilpivirine was well tolerated during pregnancy and postpartum. There were no new safety findings compared with the known safety profile of rilpivirine in HIV–1-infected adults.
Animal Data
Rilpivirine was administered orally to pregnant rats (40, 120, or 400 mg per kg per day) and rabbits (5, 10, or 20 mg per kg per day) through organogenesis (on gestation Days 6 through 17, and 6 through 19, respectively). No significant toxicological effects were observed in embryo fetal toxicity studies performed with rilpivirine in rats and rabbits at exposures 15 (rats) and 70 (rabbits) times higher than the exposure in humans at the recommended dose of 25 mg once daily. In a pre/postnatal development study with rilpivirine, where rats were administered up to 400 mg per kg per day through lactation, no significant adverse effects directly related to drug were noted in the offspring.
8.2 Lactation
Risk Summary
The Centers for Disease Control and Prevention recommend that HIV-infected mothers not breastfeed their infants to avoid risking postnatal transmission of HIV. There are no data on the presence of rilpivirine in human milk, the effects on a breastfed infant, or the effects on milk production. Rilpivirine is present in rat milk (see Data). Because of the potential for (1) HIV transmission (in HIV-negative infants), (2) developing viral resistance (in HIV-positive infants), and (3) adverse reactions in nursing infants, mothers should not breastfeed if they are receiving EDURANT.
8.4 Pediatric Use
The safety, efficacy and pharmacokinetics of EDURANT were evaluated in a single arm, open label, Phase 2 trial that enrolled 36 antiretroviral treatment-naïve, HIV-1 infected pediatric subjects 12 to less than 18 years of age and weighing at least 32 kg [see Dosage and Administration (2.1), Adverse Reactions (6.2), Clinical Pharmacology (12.3) and Clinical Studies (14.2)].
Safety and effectiveness in pediatric patients less than 12 years of age or weighing less than 35 kg have not been established.
8.5 Geriatric Use
Clinical studies of EDURANT did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. In general, caution should be exercised in the administration and monitoring of EDURANT in elderly patients reflecting the greater frequency of decreased renal and hepatic function, and of concomitant disease or other drug therapy.
8.6 Renal Impairment
No dose adjustment is required in patients with mild or moderate renal impairment. However, in patients with severe renal impairment or end-stage renal disease, rilpivirine should be used with caution and with increased monitoring for adverse effects, as rilpivirine concentrations may be increased due to alteration of drug absorption, distribution, and metabolism secondary to renal dysfunction. As rilpivirine is highly bound to plasma proteins, it is unlikely that it will be significantly removed by hemodialysis or peritoneal dialysis [see Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
No dosage adjustment of EDURANT is required in patients with mild (Child-Pugh Class A) or moderate (Child-Pugh Class B) hepatic impairment. EDURANT has not been studied in patients with severe hepatic impairment (Child-Pugh Class C) [see Clinical Pharmacology (12.3)].
-
10 OVERDOSAGE
There is no specific antidote for overdose with EDURANT. Human experience of overdose with EDURANT is limited. Treatment of overdose with EDURANT consists of general supportive measures including monitoring of vital signs and ECG (QT interval) as well as observation of the clinical status of the patient. It is advisable to contact a poison control center to obtain the latest recommendations for the management of an overdose. Since rilpivirine is highly bound to plasma protein, dialysis is unlikely to result in significant removal of the active substance.
-
11 DESCRIPTION
EDURANT (rilpivirine) is a non-nucleoside reverse transcriptase inhibitor (NNRTI) of human immunodeficiency virus type 1 (HIV-1). EDURANT is available as a white to off-white, film-coated, round, biconvex, 6.4 mm tablet for oral administration. Each tablet contains 27.5 mg of rilpivirine hydrochloride, which is equivalent to 25 mg of rilpivirine.
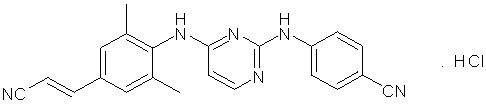
The chemical name for rilpivirine hydrochloride is 4-[[4-[[4-[(E)-2-cyanoethenyl]-2,6-dimethylphenyl]amino]-2-pyrimidinyl]amino]benzonitrile monohydrochloride. Its molecular formula is C22H18N6 ∙ HCl and its molecular weight is 402.88. Rilpivirine hydrochloride has the following structural formula:
Rilpivirine hydrochloride is a white to almost white powder. Rilpivirine hydrochloride is practically insoluble in water over a wide pH range.
Each EDURANT tablet also contains the inactive ingredients croscarmellose sodium, lactose monohydrate, magnesium stearate, polysorbate 20, povidone K30 and silicified microcrystalline cellulose. The tablet coating contains hypromellose 2910 6 mPa.s, lactose monohydrate, PEG 3000, titanium dioxide and triacetin.
-
12 CLINICAL PHARMACOLOGY
12.2 Pharmacodynamics
Effects on Electrocardiogram
The effect of EDURANT at the recommended dose of 25 mg once daily on the QTcF interval was evaluated in a randomized, placebo and active (moxifloxacin 400 mg once daily) controlled crossover study in 60 healthy adults, with 13 measurements over 24 hours at steady state. The maximum mean time-matched (95% upper confidence bound) differences in QTcF interval from placebo after baseline-correction was 2.0 (5.0) milliseconds (i.e., below the threshold of clinical concern).
When doses of 75 mg once daily and 300 mg once daily of EDURANT (3 times and 12 times the dose in EDURANT) were studied in healthy adults, the maximum mean time-matched (95% upper confidence bound) differences in QTcF interval from placebo after baseline-correction were 10.7 (15.3) and 23.3 (28.4) milliseconds, respectively. Steady-state administration of EDURANT 75 mg once daily and 300 mg once daily resulted in a mean steady-state Cmax approximately 2.6-fold and 6.7-fold, respectively, higher than the mean Cmax observed with the recommended 25 mg once daily dose of EDURANT [see Warnings and Precautions (5.4)].
12.3 Pharmacokinetics
Pharmacokinetics in Adults
The pharmacokinetic properties of rilpivirine have been evaluated in adult healthy subjects and in adult antiretroviral treatment-naïve HIV-1-infected subjects. Exposure to rilpivirine was generally lower in HIV-1 infected subjects than in healthy subjects.
Table 6: Population Pharmacokinetic Estimates of Rilpivirine 25 mg once daily in Antiretroviral Treatment-Naïve HIV-1-Infected Adult Subjects (Pooled Data from Phase 3 Trials through Week 96) Parameter Rilpivirine 25 mg once daily
N = 679AUC24h (ng∙h/mL) Mean ± Standard Deviation 2235 ± 851 Median (Range) 2096 (198 – 7307) C0h (ng/mL) Mean ± Standard Deviation 79 ± 35 Median (Range) 73 (2 – 288) Absorption and Bioavailability
After oral administration, the maximum plasma concentration of rilpivirine is generally achieved within 4–5 hours. The absolute bioavailability of EDURANT is unknown.
Effects of Food on Oral Absorption
The exposure to rilpivirine was approximately 40% lower when EDURANT was taken in a fasted condition as compared to a normal caloric meal (533 kcal) or high-fat high-caloric meal (928 kcal). When EDURANT was taken with only a protein-rich nutritional drink, exposures were 50% lower than when taken with a meal.
Distribution
Rilpivirine is approximately 99.7% bound to plasma proteins in vitro, primarily to albumin. The distribution of rilpivirine into compartments other than plasma (e.g., cerebrospinal fluid, genital tract secretions) has not been evaluated in humans.
Metabolism
In vitro experiments indicate that rilpivirine primarily undergoes oxidative metabolism mediated by the cytochrome P450 (CYP) 3A system.
Elimination
The terminal elimination half-life of rilpivirine is approximately 50 hours. After single dose oral administration of 14C-rilpivirine, on average 85% and 6.1% of the radioactivity could be retrieved in feces and urine, respectively. In feces, unchanged rilpivirine accounted for on average 25% of the administered dose. Only trace amounts of unchanged rilpivirine (< 1% of dose) were detected in urine.
Special Populations
Pregnancy and Postpartum
The exposure (C0h and AUC24h) to total rilpivirine after intake of rilpivirine 25 mg once daily as part of an antiretroviral regimen was 30 to 40% lower during pregnancy (similar for the second and third trimester), compared with postpartum (see Table 7). However, the exposure during pregnancy was not significantly different from exposures obtained in Phase 3 trials. Based on the exposure-response relationship for rilpivirine, this decrease is not considered clinically relevant in patients who are virollogically suppressed. The protein binding of rilpivirine was similar (>99%) during the second trimester, third trimester, and postpartum.
Table 7: Pharmacokinetic Results of Total Rilpivirine After Administration of Rilpivirine 25 mg Once Daily as Part of an Antiretroviral Regimen, During the 2nd Trimester of Pregnancy, the 3rd Trimester of Pregnancy and Postpartum Pharmacokinetics of total rilpivirine
(mean ± SD, tmax: median [range])Postpartum
(6-12 Weeks)
(n=11)2nd Trimester of pregnancy
(n=15)3rd Trimester of pregnancy
(n=13)C0h, ng/mL 111 ± 69.2 65.0 ± 23.9 63.5 ± 26.2 Cmin, ng/mL 84.0 ± 58.8 54.3 ± 25.8 52.9 ± 24.4 Cmax, ng/mL 167 ± 101 121 ±45.9 123 ± 47.5 tmax, h 4.00 (2.03–25.08) 4.00 (1.00–9.00) 4.00 (2.00–24.93) AUC24h, ng.h/mL 2714 ± 1535 1792 ± 711 1762 ± 662 Pediatric Patients
The pharmacokinetics of rilpivirine in antiretroviral treatment-naïve HIV-1 infected pediatric subjects 12 to less than 18 years of age receiving EDURANT 25 mg once daily were comparable to those in treatment-naïve HIV-1 infected adults receiving EDURANT 25 mg once daily. There was no clinically significant impact of body weight on rilpivirine pharmacokinetics in pediatric subjects in trial C213 (33 to 93 kg).
Table 8: Population Pharmacokinetic Estimates of Rilpivirine 25 mg once daily in Antiretroviral Treatment-Naïve HIV-1-Infected Pediatric Subjects aged 12 to less than 18 years (Data from Phase 2 Trial through Week 48) Parameter Rilpivirine 25 mg once daily
N = 34AUC24h (ng∙h/mL) Mean ± Standard Deviation 2424 ± 1024 Median (Range) 2269 (417 – 5166) C0h (ng/mL) Mean ± Standard Deviation 85 ± 40 Median (Range) 79 (7 – 202) The pharmacokinetics and dosing recommendations of rilpivirine in pediatric patients who are less than 12 years of age and less than 35 kg have not been established [see Use in Specific Populations (8.4)].
Renal Impairment
Population pharmacokinetic analysis indicated that rilpivirine exposure was similar in HIV-1 infected subjects with mild renal impairment relative to HIV-1 infected subjects with normal renal function. No dose adjustment is required in patients with mild renal impairment. There is limited or no information regarding the pharmacokinetics of rilpivirine in patients with moderate or severe renal impairment or in patients with end-stage renal disease, and rilpivirine concentrations may be increased due to alteration of drug absorption, distribution, and metabolism secondary to renal dysfunction. The potential impact is not expected to be of clinical relevance for HIV-1-infected subjects with moderate renal impairment, and no dose adjustment is required in these patients. Rilpivirine should be used with caution and with increased monitoring for adverse effects in patients with severe renal impairment or end-stage renal disease. As rilpivirine is highly bound to plasma proteins, it is unlikely that it will be significantly removed by hemodialysis or peritoneal dialysis [see Use in Specific Populations (8.6)].
Hepatic Impairment
Rilpivirine is primarily metabolized and eliminated by the liver. In a study comparing 8 subjects with mild hepatic impairment (Child-Pugh score A) to 8 matched controls, and 8 subjects with moderate hepatic impairment (Child-Pugh score B) to 8 matched controls, the multiple dose exposure of rilpivirine was 47% higher in subjects with mild hepatic impairment and 5% higher in subjects with moderate hepatic impairment. EDURANT has not been studied in subjects with severe hepatic impairment (Child-Pugh score C) [see Use in Specific Populations (8.7)].
Drug Interactions
[see Contraindications (4) and Drug Interactions (7).]
Rilpivirine is primarily metabolized by cytochrome P450 (CYP)3A, and drugs that induce or inhibit CYP3A may thus affect the clearance of rilpivirine. Coadministration of EDURANT and drugs that induce CYP3A may result in decreased plasma concentrations of rilpivirine and loss of virologic response and possible resistance. Coadministration of EDURANT and drugs that inhibit CYP3A may result in increased plasma concentrations of rilpivirine. Coadministration of EDURANT with drugs that increase gastric pH may result in decreased plasma concentrations of rilpivirine and loss of virologic response and possible resistance to rilpivirine and to the class of NNRTIs.
EDURANT at a dose of 25 mg once daily is not likely to have a clinically relevant effect on the exposure of medicinal products metabolized by CYP enzymes.
Drug interaction studies were performed with EDURANT and other drugs likely to be coadministered or commonly used as probes for pharmacokinetic interactions. The effects of coadministration of other drugs on the Cmax, AUC, and Cmin values of rilpivirine are summarized in Table 9 (effect of other drugs on EDURANT). The effect of coadministration of EDURANT on the Cmax, AUC, and Cmin values of other drugs are summarized in Table 10 (effect of EDURANT on other drugs). [For information regarding clinical recommendations, see Drug Interactions (7).]
Table 9: Drug Interactions: Pharmacokinetic Parameters for Rilpivirine in the Presence of Coadministered Drugs Coadministered Drug Dose/Schedule N Mean Ratio of Rilpivirine
Pharmacokinetic Parameters
With/Without Coadministered Drug
(90% CI); No Effect = 1.00Coadministered Drug Rilpivirine Cmax AUC Cmin CI = Confidence Interval; N = maximum number of subjects with data; N.A. = not available; ↑ = increase; ↓ = decrease; ↔ = no change; q.d. = once daily; b.i.d. = twice daily - * This interaction study has been performed with a dose higher than the recommended dose for EDURANT (25 mg once daily) assessing the maximal effect on the coadministered drug.
- † comparison based on historic controls
CoAdministration With HIV Protease Inhibitors (PIs) Darunavir/ritonavir 800/100 mg q.d. 150 mg q.d.* 14 1.79
(1.56–2.06)2.30
(1.98–2.67)2.78
(2.39–3.24)Lopinavir/ritonavir (soft gel capsule) 400/100 mg b.i.d. 150 mg q.d.* 15 1.29
(1.18–1.40)1.52
(1.36–1.70)1.74
(1.46–2.08)CoAdministration With HIV Nucleoside or Nucleotide Reverse Transcriptase Inhibitors (NRTIs/N[t]RTIs) Didanosine 400 mg q.d.
delayed release capsules taken 2 hours before rilpivirine150 mg q.d.* 21 1.00
(0.90–1.10)1.00
(0.95–1.06)1.00
(0.92–1.09)Tenofovir disoproxil fumarate 300 mg q.d. 150 mg q.d.* 16 0.96
(0.81–1.13)1.01
(0.87–1.18)0.99
(0.83–1.16)CoAdministration With HIV Integrase Strand Transfer Inhibitors Raltegravir 400 mg b.i.d. 25 mg q.d. 23 1.12
(1.04–1.20)1.12
(1.05–1.19)1.03
(0.96–1.12)CoAdministration With other Antivirals Simeprevir 150 mg q.d. 25 mg q.d. 23 1.04
(0.95–1.13)1.12
(1.05–1.19)1.25
(1.16–1.35)CoAdministration With Drugs other than Antiretrovirals Acetaminophen 500 mg single dose 150 mg q.d.* 16 1.09
(1.01–1.18)1.16
(1.10–1.22)1.26
(1.16–1.38)Atorvastatin 40 mg q.d. 150 mg q.d.* 16 0.91
(0.79–1.06)0.90
(0.81–0.99)0.90
(0.84–0.96)Chlorzoxazone 500 mg single dose taken 2 hours after rilpivirine 150 mg q.d.* 16 1.17
(1.08–1.27)1.25
(1.16–1.35)1.18
(1.09–1.28)Ethinylestradiol/Norethindrone 0.035 mg q.d./
1 mg q.d.25 mg q.d. 15 ↔† ↔† ↔† Famotidine 40 mg single dose taken 12 hours before rilpivirine 150 mg single dose* 24 0.99
(0.84–1.16)0.91
(0.78–1.07)N.A. Famotidine 40 mg single dose taken 2 hours before rilpivirine 150 mg single dose* 23 0.15
(0.12–0.19)0.24
(0.20–0.28)N.A. Famotidine 40 mg single dose taken 4 hours after rilpivirine 150 mg single dose* 24 1.21
(1.06–1.39)1.13
(1.01–1.27)N.A. Ketoconazole 400 mg q.d. 150 mg q.d.* 15 1.30
(1.13–1.48)1.49
(1.31–1.70)1.76
(1.57–1.97)Methadone 60–100 mg q.d., individualised dose 25 mg q.d. 12 ↔† ↔† ↔† Omeprazole 20 mg q.d. 150 mg q.d.* 16 0.60
(0.48–0.73)0.60
(0.51–0.71)0.67
(0.58–0.78)Rifabutin 300 mg q.d. 25 mg q.d. 18 0.69
(0.62–0.76)0.58
(0.52–0.65)0.52
(0.46–0.59)Rifabutin 300 mg q.d. 50 mg q.d. 18 1.43
(1.30–1.56)1.16
(1.06–1.26)0.93
(0.85–1.01)(reference arm for comparison was 25 mg q.d. rilpivirine administered alone) Rifampin 600 mg q.d. 150 mg q.d.* 16 0.31
(0.27–0.36)0.20
(0.18–0.23)0.11
(0.10–0.13)Sildenafil 50 mg single dose 75 mg q.d.* 16 0.92
(0.85–0.99)0.98
(0.92–1.05)1.04
(0.98–1.09)Table 10: Drug Interactions: Pharmacokinetic Parameters for Coadministered Drugs in the Presence of EDURANT Coadministered Drug Dose/Schedule N Mean Ratio of Coadministered Drug
Pharmacokinetic Parameters
With/Without EDURANT
(90% CI); No Effect = 1.00Coadministered Drug Rilpivirine Cmax AUC Cmin CI = Confidence Interval; N = maximum number of subjects with data; N.A. = not available; ↑ = increase; ↓ = decrease; ↔ = no change; q.d. = once daily; b.i.d. = twice daily - * This interaction study has been performed with a dose higher than the recommended dose for EDURANT (25 mg once daily) assessing the maximal effect on the coadministered drug.
- † AUC(0–last)
- ‡ N (maximum number of subjects with data) for AUC(0–∞) = 15
CoAdministration With HIV Protease Inhibitors (PIs) Darunavir/ritonavir 800/100 mg q.d. 150 mg q.d.* 15 0.90
(0.81–1.00)0.89
(0.81–0.99)0.89
(0.68–1.16)Lopinavir/ritonavir
(soft gel capsule)400/100 mg b.i.d. 150 mg q.d.* 15 0.96
(0.88–1.05)0.99
(0.89–1.10)0.89
(0.73–1.08)CoAdministration With HIV Nucleoside or Nucleotide Reverse Transcriptase Inhibitors (NRTIs/N[t]RTIs) Didanosine 400 mg q.d.
delayed release capsules taken 2 hours before rilpivirine150 mg q.d.* 13 0.96
(0.80–1.14)1.12
(0.99–1.27)N.A. Tenofovir disoproxil fumarate 300 mg q.d. 150 mg q.d.* 16 1.19
(1.06–1.34)1.23
(1.16–1.31)1.24
(1.10–1.38)CoAdministration With HIV Integrase Strand Transfer Inhibitors Raltegravir 400 mg b.i.d. 25 mg q.d. 23 1.10
(0.77–1.58)1.09
(0.81–1.47)1.27
(1.01–1.60)CoAdministration With other Antivirals Simeprevir 150 mg q.d. 25 mg q.d. 21 1.10
(0.97–1.26)1.06
(0.94–1.19)0.96
(0.83–1.11)CoAdministration With Drugs other than Antiretrovirals Acetaminophen 500 mg single dose 150 mg q.d.* 16 0.97
(0.86–1.10)0.91
(0.86–0.97)N.A. Atorvastatin 40 mg q.d. 150 mg q.d.* 16 1.35
(1.08–1.68)1.04
(0.97–1.12)0.85
(0.69–1.03)
2-hydroxy-atorvastatin 16 1.58
(1.33–1.87)1.39
(1.29–1.50)1.32
(1.10–1.58)
4-hydroxy-atorvastatin 16 1.28
(1.15–1.43)1.23
(1.13–1.33)N.A. Chlorzoxazone 500 mg single dose taken 2 hours after rilpivirine 150 mg q.d.* 16 0.98
(0.85–1.13)1.03
(0.95–1.13)N.A. Digoxin 0.5 mg single dose 25 mg q.d. 22 1.06
(0.97–1.17)0.98
(0.93–1.04)†N.A. Ethinylestradiol 0.035 mg q.d. 25 mg q.d. 17 1.17
(1.06–1.30)1.14
(1.10–1.19)1.09
(1.03–1.16)
Norethindrone 1 mg q.d. 17 0.94
(0.83–1.06)0.89
(0.84–0.94)0.99
(0.90–1.08)Ketoconazole 400 mg q.d. 150 mg q.d.* 14 0.85
(0.80–0.90)0.76
(0.70–0.82)0.34
(0.25–0.46)R(-) methadone 60–100 mg q.d., individualised dose 25 mg q.d. 13 0.86
(0.78–0.95)0.84
(0.74–0.95)0.78
(0.67–0.91)
S(+) methadone 13 0.87
(0.78–0.97)0.84
(0.74–0.96)0.79
(0.67–0.92)Metformin 850 mg single dose 25 mg q.d. 20 1.02
(0.95–1.10)0.97
(0.90–1.06)‡N.A. Omeprazole 20 mg q.d. 150 mg q.d.* 15 0.86
(0.68–1.09)0.86
(0.76–0.97)N.A. Rifampin 600 mg q.d. 150 mg q.d.* 16 1.02
(0.93–1.12)
0.99
(0.92–1.07)N.A.
25-desacetylrifampin 16 1.00
(0.87–1.15)0.91
(0.77–1.07)N.A. Sildenafil 50 mg single dose 75 mg q.d.* 16 0.93
(0.80–1.08)
0.97
(0.87–1.08)N.A.
N-desmethyl-sildenafil 16 0.90
(0.80–1.02)0.92
(0.85–0.99)†N.A. 12.4 Microbiology
Mechanism of Action
Rilpivirine is a diarylpyrimidine non-nucleoside reverse transcriptase inhibitor (NNRTI) of human immunodeficiency virus type 1 (HIV-1) and inhibits HIV-1 replication by non-competitive inhibition of HIV-1 reverse transcriptase (RT). Rilpivirine does not inhibit the human cellular DNA polymerases α, β and γ.
Antiviral Activity in Cell Culture
Rilpivirine exhibited activity against laboratory strains of wild-type HIV-1 in an acutely infected T-cell line with a median EC50 value for HIV-1IIIB of 0.73 nM (0.27 ng/mL). Rilpivirine demonstrated limited activity in cell culture against HIV-2 with a median EC50 value of 5220 nM (range 2510 to 10830 nM) (920 to 3970 ng/mL).
Rilpivirine demonstrated antiviral activity against a broad panel of HIV-1 group M (subtype A, B, C, D, F, G, H) primary isolates with EC50 values ranging from 0.07 to 1.01 nM (0.03 to 0.37 ng/mL) and was less active against group O primary isolates with EC50 values ranging from 2.88 to 8.45 nM (1.06 to 3.10 ng/mL).
The antiviral activity of rilpivirine was not antagonistic when combined with the NNRTIs efavirenz, etravirine or nevirapine; the N(t)RTIs abacavir, didanosine, emtricitabine, lamivudine, stavudine, tenofovir or zidovudine; the PIs amprenavir, atazanavir, darunavir, indinavir, lopinavir, nelfinavir, ritonavir, saquinavir or tipranavir; the fusion inhibitor enfuvirtide; the CCR5 co-receptor antagonist maraviroc, or the integrase strand transfer inhibitor raltegravir.
Resistance
In Cell Culture
Rilpivirine-resistant strains were selected in cell culture starting from wild-type HIV-1 of different origins and subtypes as well as NNRTI resistant HIV-1. The frequently observed amino acid substitutions that emerged and conferred decreased phenotypic susceptibility to rilpivirine included: L100I, K101E, V106I and A, V108I, E138K and G, Q, R, V179F and I, Y181C and I, V189I, G190E, H221Y, F227C and M230I and L.
In Treatment-Naïve Adult Subjects
In the Week 96 pooled resistance analysis of the Phase 3 trials C209 and C215, the emergence of resistance was greater among subjects' viruses in the EDURANT arm compared to the efavirenz arm, and was dependent on baseline viral load. In the pooled resistance analysis, 58% (57/98) of the subjects who qualified for resistance analysis (resistance analysis subjects) in the EDURANT arm had virus with genotypic and/or phenotypic resistance to rilpivirine compared to 45% (25/56) of the resistance analysis subjects in the efavirenz arm who had genotypic and/or phenotypic resistance to efavirenz. Moreover, genotypic and/or phenotypic resistance to a background drug (emtricitabine, lamivudine, tenofovir, abacavir or zidovudine) emerged in viruses from 52% (51/98) of the resistance analysis subjects in the rilpivirine arm compared to 23% (13/56) in the efavirenz arm.
Emerging NNRTI substitutions in the rilpivirine resistance analysis of subjects' viruses included V90I, K101E/P/T, E138K/A/Q/G, V179I/L, Y181C/I, V189I, H221Y, F227C/L and M230L, which were associated with a rilpivirine phenotypic fold change range of 2.6 – 621. The E138K substitution emerged most frequently during rilpivirine treatment commonly in combination with the M184I substitution. The emtricitabine and lamivudine resistance-associated substitutions M184I or V and NRTI resistance-associated substitutions (K65R/N, A62V, D67N/G, K70E, Y115F, T215S/T, or K219E/R) emerged more frequently in rilpivirine resistance analysis subjects compared to efavirenz resistance analysis subjects (see Table 11).
NNRTI- and NRTI-resistance substitutions emerged less frequently in resistance analysis of viruses from subjects with baseline viral load of ≤ 100,000 copies/mL compared to viruses from subjects with baseline viral load of > 100,000 copies/mL: 26% (14/54) compared to 74% (40/54) of NNRTI-resistance substitutions and 22% (11/50) compared to 78% (39/50) of NRTI-resistance substitutions. This difference was also observed for the individual emtricitabine/lamivudine and tenofovir resistance substitutions: 23% (11/47) compared to 77% (36/47) for M184I/V and 0% (0/8) compared to 100% (8/8) for K65R/N. Additionally, NNRTI- and NRTI-resistance substitutions emerged less frequently in the resistance analysis of viruses from subjects with baseline CD4+ cell counts ≥ 200 cells/mm3 compared to viruses from subjects with baseline CD4+ cell counts < 200 cells/mm3: 37% (20/54) compared to 63% (34/54) of NNRTI-resistance substitutions and 28% (14/50) compared to 72% (36/50) of NRTI-resistance substitutions.
Table 11: Proportion of Resistance Analysis Subjects* with Frequently Emerging Reverse Transcriptase Substitutions from the Pooled Phase 3 TMC278-C209 and TMC278-C215 Trials in the Week 96 Analysis C209 and C215
N = 1368EDURANT + BR
N = 686Efavirenz + BR
N = 682BR = background regimen - * Subjects who qualified for resistance analysis.
- † V90, L100, K101, K103, V106, V108, E138, V179, Y181, Y188, V189, G190, H221, P225, F227 or M230
- ‡ This combination of NNRTI and NRTI substitutions is a subset of those with the E138K.
- § A62V, K65R/N, D67N/G, K70E, L74I, V75I, Y115F, M184I/V, L210F, T215S/T, K219E/R
- ¶ These substitutions emerged in addition to the primary substitutions M184V/I or K65R/N; A62V (n=3), D67N/G (n=3), K70E (n=4), Y115F (n=2), T215S/T (n=1), K219E/R (n=8) in rilpivirine resistance analysis subjects.
Subjects who Qualified for Resistance Analysis 15% (98/652) 9% (56/604) Subjects with Evaluable Post-Baseline Resistance Data 87 43 Emerging NNRTI Substitutions† Any 62% (54/87) 53% (23/43) V90I 13% (11/87) 2% (1/43) K101E/P/T/Q 20% (17/87) 9% (4/43) K103N 1% (1/87) 40% (17/43) E138K/A/Q/G 40% (35/87) 2% (1/43) E138K+ M184I‡ 25% (22/87) 0 V179I/L/D 6% (5/87) 7% (3/43) Y181C/I/S 10% (9/87) 2% (1/43) V189I 8% (7/87) 2% (1/43) H221Y 9% (8/87) 0 Emerging NRTI Substitutions§ Any 57% (50/87) 30% (13/43) M184I/V 54% (47/87) 26% (11/43) K65R/N 9% (8/87) 5% (2/43) A62V, D67N/G, K70E, Y115F, T215S/T or K219E/R¶ 21% (18/87) 2% (1/43) Cross-Resistance
Site-Directed NNRTI Mutant Virus
Cross-resistance has been observed among NNRTIs. The single NNRTI substitutions K101P, Y181I and Y181V conferred 52-fold, 15-fold and 12-fold decreased susceptibility to rilpivirine, respectively. The combination of E138K and M184I showed 6.7-fold reduced susceptibility to rilpivirine compared to 2.8-fold for E138K alone. The K103N substitution did not result in reduced susceptibility to rilpivirine by itself. However, the combination of K103N and L100I resulted in a 7-fold reduced susceptibility to rilpivirine. Combinations of 2 or 3 NNRTI resistance-associated substitutions had decreased susceptibility to rilpivirine (fold change range of 3.7 – 554) in 38% and 66% of mutants analyzed, respectively.
Treatment-naïve HIV-1-infected adult subjects
Considering all available cell culture and clinical data, any of the following amino acid substitutions, when present at baseline, are likely to decrease the antiviral activity of rilpivirine: K101E, K101P, E138A, E138G, E138K, E138R, E138Q, V179L, Y181C, Y181I, Y181V, Y188L, H221Y, F227C, M230I or M230L.
Cross-resistance to efavirenz, etravirine and/or nevirapine is likely after virologic failure and development of rilpivirine resistance. In the Week 96 pooled analyses of the Phase 3 TMC278-C209 and TMC278-C215 clinical trials, 50 of the 87 (57%) rilpivirine resistance analysis subjects with post-baseline resistance data had virus with decreased susceptibility to rilpivirine (≥ 2.5-fold change). Of these, 86% (n= 43/50) were resistant to efavirenz (≥ 3.3-fold change), 90% (n= 45/50) were resistant to etravirine (≥ 3.2-fold change) and 62% (n= 31/50) were resistant to nevirapine (≥ 6-fold change). In the efavirenz arm, 3 of the 21 (14%) efavirenz resistance analysis subjects' viruses were resistant to etravirine and rilpivirine, and 95% (n= 20/21) were resistant to nevirapine. Virus from subjects experiencing virologic failure on EDURANT developed more NNRTI resistance-associated substitutions conferring more cross-resistance to the NNRTI class and had a higher likelihood of cross-resistance to all NNRTIs in the class compared to virus from subjects who failed on efavirenz.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis and Mutagenesis
Rilpivirine was evaluated for carcinogenic potential by oral gavage administration to mice and rats up to 104 weeks. Daily doses of 20, 60 and 160 mg/kg/day were administered to mice and doses of 40, 200, 500 and 1500 mg/kg/day were administered to rats. In rats, there were no drug related neoplasms. In mice, rilpivirine was positive for hepatocellular neoplasms in both males and females. The observed hepatocellular findings in mice may be rodent-specific. At the lowest tested doses in the carcinogenicity studies, the systemic exposures (based on AUC) to rilpivirine were 21-fold (mice) and 3-fold (rats), relative to those observed in humans at the recommended dose (25 mg q.d.).
Rilpivirine has tested negative in the absence and presence of a metabolic activation system in the in vitro Ames reverse mutation assay and the in vitro clastogenicity mouse lymphoma assay. Rilpivirine did not induce chromosomal damage in the in vivo micronucleus test in mice.
Impairment of Fertility
No human data on the effect of rilpivirine on fertility are available. In a study conducted in rats, there were no effects on mating or fertility with rilpivirine up to 400 mg/kg/day, a dose of rilpivirine that showed maternal toxicity. This dose is associated with an exposure that is approximately 40 times higher than the exposure in humans at the recommended dose of 25 mg once daily.
-
14 CLINICAL STUDIES
14.1 Treatment-Naïve Adult Subjects
The evidence of efficacy of EDURANT is based on the analyses of 48- and 96-week data from 2 randomized, double-blinded, active controlled, Phase 3 trials TMC278-C209 (ECHO) and TMC278-C215 (THRIVE) in antiretroviral treatment-naïve adults. Antiretroviral treatment-naïve HIV-1 infected subjects enrolled in the Phase 3 trials had a plasma HIV-1 RNA ≥ 5000 copies/mL and were screened for susceptibility to N(t)RTIs and for absence of specific NNRTI resistance-associated substitutions (RASs). The Phase 3 trials were identical in design, apart from the background regimen (BR). In TMC278-C209, the BR was fixed to the N(t)RTIs, tenofovir disoproxil fumarate plus emtricitabine. In TMC278-C215, the BR consisted of 2 investigator-selected N(t)RTIs: tenofovir disoproxil fumarate plus emtricitabine or zidovudine plus lamivudine or abacavir plus lamivudine. In both trials, randomization was stratified by screening viral load. In TMC278-C215, randomization was also stratified by N(t)RTI BR.
In the pooled analysis for TMC278-C209 and TMC278-C215, demographics and baseline characteristics were balanced between the EDURANT arm and the efavirenz arm. Table 12 displays selected demographic and baseline disease characteristics of the subjects in the EDURANT and efavirenz arms.
Table 12: Demographic and Baseline Disease Characteristics of Antiretroviral Treatment-Naïve HIV-1-Infected Adult Subjects in the TMC278-C209 and TMC278-C215 Trials (Pooled Analysis) Pooled Data from the Phase 3 TMC278-C209 and TMC278-C215 Trials EDURANT + BR
N=686Efavirenz + BR
N=682BR=background regimen Demographic Characteristics Median Age, years (range) 36 (18–78) 36 (19–69) Sex Male 76% 76% Female 24% 24% Race White 61% 60% Black/African American 24% 23% Asian 11% 14% Other 2% 2% Not allowed to ask per local regulations 1% 1% Baseline Disease Characteristics Median Baseline Plasma HIV-1 RNA (range), log10 copies/mL 5.0 (2–7) 5.0 (3–7) Percentage of Patients with Baseline Plasma Viral Load: ≤ 100,000 54% 48% > 100,000 to ≤ 500,000 36% 40% > 500,000 10% 12% Median Baseline CD4+ Cell Count (range), cells/mm3 249 (1–888) 260 (1–1137) Percentage of Subjects with: Hepatitis B/C Virus Co-infection 7% 10% Percentage of Patients with the Following Background Regimens: tenofovir disoproxil fumarate plus emtricitabine 80% 80% zidovudine plus lamivudine 15% 15% abacavir plus lamivudine 5% 5% Week 96 efficacy outcomes for subjects treated with EDURANT 25 mg once daily from the pooled analysis are shown in Table 13. The incidence of virologic failure was higher in the EDURANT arm than the efavirenz arm at Week 96. Virologic failures and discontinuations due to adverse events mostly occurred in the first 48 weeks of treatment. Regardless of HIV-1 RNA at the start of therapy, more EDURANT treated subjects with CD4+ cell count less than 200 cells/mm3 experienced virologic failure compared to EDURANT treated subjects with CD4+ cell count greater than or equal to 200 cells/mm3.
Table 13: Virologic Outcome of Randomized Treatment of Studies TMC278-C209 and TMC278-C215 (Pooled Data) at Week 96 EDURANT + BR
N=686Efavirenz + BR
N=682N = total number of subjects per treatment group; BR = background regimen. Note: Analysis was based on the last observed viral load data within the Week 96 window (Week 90–103), respectively. - * CI = Predicted difference (95% CI) of response rate is -0.2 (-4.7; 4.3) at Week 96.
- † Includes subjects who had ≥ 50 copies/mL in the Week 96 window, subjects who discontinued early due to lack or loss of efficacy, subjects who discontinued for reasons other than an adverse event, death or lack or loss of efficacy and at the time of discontinuation had a viral value of ≥ 50 copies/mL, and subjects who had a switch in background regimen that was not permitted by the protocol.
- ‡ Includes subjects who discontinued due to an adverse event or death if this resulted in no on-treatment virologic data in the Week 96 window.
- § Includes subjects who discontinued for reasons other than an adverse event, death or lack or loss of efficacy, e.g., withdrew consent, loss to follow-up, etc.
HIV-1 RNA < 50 copies/mL* 76% 77% HIV-1 RNA ≥ 50 copies/mL† 16% 10% No virologic data at Week 96 window
ReasonsDiscontinued study due to adverse event or death‡ 4% 8% Discontinued study for other reasons and last available HIV-1 RNA < 50 copies/mL (or missing)§ 4% 5% Missing data during window but on study < 1% < 1% HIV-1 RNA < 50 copies/mL by Baseline HIV-1 RNA (copies/mL) ≤ 100,000 82% 78% > 100,000 70% 75% HIV-1 RNA ≥ 50 copies/mL† by Baseline HIV-1 RNA (copies/mL) ≤ 100,000 9% 8% > 100,000 24% 11% HIV-1 RNA < 50 copies/mL by CD4+ cell count (cells/mm3) < 200 68% 74% ≥ 200 81% 77% HIV-1 RNA ≥ 50 copies/mL† by CD4+ cell count (cells/mm3) < 200 27% 10% ≥ 200 10% 9% At Week 96, the mean CD4+ cell count increase from baseline was 228 cells/mm3 for EDURANT-treated subjects and 219 cells/mm3 for efavirenz-treated subjects in the pooled analysis of the TMC278-C209 and TMC278-C215 trials.
Study TMC278-C204 was a randomized, active-controlled, Phase 2b trial in antiretroviral treatment-naïve HIV-1-infected adult subjects consisting of 2 parts: an initial 96 weeks, partially-blinded dose-finding part [EDURANT doses blinded] followed by a long-term, open-label part. After Week 96, subjects randomized to one of the 3 doses of EDURANT were switched to EDURANT 25 mg once daily. Subjects in the control arm received efavirenz 600 mg once daily in addition to a BR in both parts of the study. The BR consisted of 2 investigator-selected N(t)RTIs: zidovudine plus lamivudine or tenofovir disoproxil fumarate plus emtricitabine.
Study TMC278-C204 enrolled 368 HIV-1-infected treatment-naïve adult subjects who had a plasma HIV-1 RNA ≥ 5000 copies/ml, previously received ≤ 2 weeks of treatment with an N(t)RTI or protease inhibitor, had no prior use of NNRTIs, and were screened for susceptibility to N(t)RTI and for absence of specific NNRTI RASs.
At 96 weeks, the proportion of subjects with <50 HIV-1 RNA copies/ml receiving EDURANT 25 mg (N = 93) compared to subjects receiving efavirenz (N = 89) was 76% and 71%, respectively. The mean increase from baseline in CD4+ counts was 146 cells/mm3 in subjects receiving EDURANT 25 mg and 160 cells/mm3 in subjects receiving efavirenz.
At 240 weeks, 60% (56/93) of subjects who originally received 25 mg once daily achieved HIV RNA < 50 copies/mL compared to 57% (51/89) of subjects in the control group.
14.2 Treatment-Naïve Pediatric Subjects (12 to less than 18 years of age)
The pharmacokinetics, safety, tolerability and efficacy of EDURANT 25 mg once daily, in combination with an investigator-selected background regimen (BR) containing two NRTIs, was evaluated in trial TMC278-C213, a single-arm, open-label Phase 2 trial in antiretroviral treatment-naïve HIV-1 infected pediatric subjects 12 to less than 18 years of age and weighing at least 32 kg. Thirty six (36) subjects were enrolled in the trial to complete at least 48 weeks of treatment. The 36 subjects had a median age of 14.5 years (range: 12 to 17 years), and were 55.6% female, 88.9% Black and 11.1% Asian.
In the efficacy analysis, most subjects (75%; 28/36) had baseline HIV RNA <100,000 copies/mL. For these 28 subjects the median baseline plasma HIV-1 RNA was 44,250 (range: 2,060–92,600 copies/mL) and the median baseline CD4+ cell count was 445.5 cells/mm3 (range: 123 to 983 cells/mm3).
Among the subjects who had baseline HIV RNA ≤ 100,000, the proportion with HIV-1 RNA <50 copies/mL at Week 48 was 79% (22/28), versus 50.0% (4/8) in those with >100,000 copies/mL. The proportion of virologic failures among subjects with a baseline viral load ≤100,000 copies/mL was 21.4% (6/28), versus 37.5% (3/8) in those with >100,000 copies/mL. At Week 48, the mean increase in CD4+ cell count from baseline was 201.2 cells/mm3.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
EDURANT (rilpivirine) tablets are supplied as white to off-white, film-coated, round, biconvex, 6.4 mm tablets. Each tablet contains 27.5 mg of rilpivirine hydrochloride, which is equivalent to 25 mg of rilpivirine. Each tablet is debossed with "TMC" on one side and "25" on the other side.
EDURANT tablets are packaged in bottles in the following configuration: 25 mg tablets-bottles of 30 (NDC: 59676-278-01).
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Severe Skin and Hypersensitivity Reactions
Advise patients to immediately contact their healthcare provider if they develop a rash. Instruct patients to immediately stop taking EDURANT and seek medical attention if they develop a rash associated with any of the following symptoms as it may be a sign of more serious reactions such as DRESS severe hypersensitivity: fever, blisters, mucosal involvement, eye inflammation (conjunctivitis), severe allergic reaction causing a swelling of the face, eyes, lips, mouth, tongue or throat, which may lead to difficulty swallowing or breathing, and any signs and symptoms of liver problems as it may be a sign of a more serious reaction. Advise patients that if severe rash occurs, they will be closely monitored, laboratory tests will be performed and appropriate therapy will be initiated [see Warnings and Precautions (5.1)].
Hepatotoxicity
Inform patients that hepatotoxicity has been reported with EDURANT. Inform patients that laboratory monitoring for hepatotoxicity during therapy with EDURANT is recommended, especially for patients with underlying liver disease such as hepatitis B or C virus infection [see Warnings and Precautions (5.2)].
Depressive Disorders
Inform patients that depressive disorders (depressed mood, depression, dysphoria, major depression, mood altered, negative thoughts, suicide attempt, suicidal ideation) have been reported with EDURANT. Advise patients to seek immediate medical evaluation if they experience depressive symptoms [see Warnings and Precautions (5.3)].
Drug Interactions
EDURANT may interact with many drugs; therefore, advise patients to report to their healthcare provider the use of any other prescription or nonprescription medication or herbal products, including St. John's wort [see Contraindications (4), Warnings and Precautions (5.4), and Drug Interactions (7)].
For patients concomitantly receiving rifabutin, the EDURANT dose should be increased to 50 mg once daily, taken with a meal. When rifabutin coadministration is stopped, the EDURANT dose should be decreased to 25 mg once daily, taken with a meal [see Dosage and Administration (2.2)].
Fat Redistribution
Inform patients that redistribution or accumulation of body fat may occur in patients receiving antiretroviral therapy, including EDURANT, and that the cause and long-term health effects of these conditions are not known at this time [see Warnings and Precautions (5.5)].
Immune Reconstitution Syndrome
Advise patients to inform their healthcare provider immediately of any signs or symptoms of infection as inflammation from previous infection may occur soon after combination antiretroviral therapy, including when EDURANT is started [see Warnings and Precautions (5.6)].
Administration Instruction
Advise patients to take EDURANT with a meal once a day as prescribed. A protein drink alone does not replace a meal. EDURANT must always be used in combination with other antiretroviral drugs. Advise patients not to alter the dose of EDURANT or discontinue therapy with EDURANT without consulting their physician. If the patient misses a dose of EDURANT within 12 hours of the time it is usually taken, advise the patient to take EDURANT with a meal as soon as possible and then take the next dose of EDURANT at the regularly scheduled time. If a patient misses a dose of EDURANT by more than 12 hours, advise the patient to not take the missed dose, but resume the usual dosing schedule. Inform the patient that he or she should not take more or less than the prescribed dose of EDURANT at any one time.
Pregnancy Registry
Advise patients that there is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to EDURANT during pregnancy [see Use in Specific Populations (8.1)].
Lactation
Instruct women with HIV-1 infection not to breastfeed because HIV-1 can be passed to the baby in the breast milk [see Use in Specific Populations (8.2)].
- SPL UNCLASSIFIED SECTION
-
PATIENT PACKAGE INSERT
This Patient Information has been approved by the U.S. Food and Drug Administration. Revised 05/2019 PATIENT INFORMATION
EDURANT® (ee' dur ant)
(rilpivirine)
TabletsImportant: Ask your healthcare provider or pharmacist about medicines that should not be taken with EDURANT. For more information, see "What should I tell my healthcare provider before taking EDURANT?" What is EDURANT? EDURANT is a prescription medicine that is used with other antiretroviral medicines to treat Human Immunodeficiency Virus (HIV-1) in people 12 years of age and older and who weigh at least 77 lbs (35 kg) who: - have never taken HIV medicines before, and
- have an amount of HIV-1 in their blood (this is called 'viral load') that is no more than 100,000 copies/mL.
HIV-1 is the virus that causes AIDS (Acquired Immune Deficiency Syndrome).
It is not known if EDURANT is safe and effective in children less than 12 years of age or who weigh less than 77 lbs (35 kg).Who should not take EDURANT? Do not take EDURANT if you also take: - anti-seizure medicines:
- carbamazepine
- oxcarbazepine
- phenobarbital
- phenytoin
- anti-tuberculosis (anti-TB) medicines:
- rifampin
- rifapentine
- proton pump inhibitor (PPI) medicine for certain stomach or intestinal problems:
- esomeprazole
- lansoprazole
- omeprazole
- pantoprazole sodium
- rabeprazole
- more than 1 dose of the steroid medicine dexamethasone or dexamethasone sodium phosphate
- St. John's wort (Hypericum perforatum)
What should I tell my healthcare provider before taking EDURANT? Before taking EDURANT, tell your healthcare provider about all your medical conditions, including if you: - have or had liver problems, including hepatitis B or C virus infection.
- have kidney problems
- have ever had a mental health problem.
- are pregnant or plan to become pregnant. It is not known if EDURANT will harm your unborn baby. Tell your healthcare provider if you become pregnant during treatment with EDURANT.
Pregnancy Registry: There is a pregnancy registry for women who take EDURANT during pregnancy. The purpose of this registry is to collect information about the health of you and your baby. Talk with your healthcare provider about how you can take part in this registry. - are breastfeeding or plan to breastfeed. Do not breastfeed if you take EDURANT.
- You should not breastfeed if you have HIV-1 because of the risk of passing HIV-1 to your baby.
- It is not known if EDURANT passes into your breast milk. Talk with your healthcare provider about the best way to feed your baby during EDURANT treatment.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Some medicines interact with EDURANT. Keep a list of your medicines to show your healthcare provider and pharmacist when you get a new medicine. You can ask your healthcare provider or pharmacist for a list of medicines that interact with EDURANT.
Do not start taking a new medicine without telling your healthcare provider. Your healthcare provider can tell you if it is safe to take EDURANT with other medicines.How should I take EDURANT? - Take EDURANT every day exactly as your healthcare provider tells you to.
- Take EDURANT 1 time each day with a meal. A protein drink alone does not replace a meal.
- Do not change your dose or stop taking EDURANT without first talking with your healthcare provider. Stay under the care of your healthcare provider during treatment with EDURANT.
- Do not miss a dose of EDURANT.
- If you take an H2-receptor antagonist (famotidine, cimetidine, nizatidine, or ranitidine), you should take these medicines at least 12 hours before or at least 4 hours after you take EDURANT.
- If you take antacids, or other products that contain aluminum, calcium carbonate, or magnesium hydroxide, you should take these medicines at least 2 hours before or at least 4 hours after you take EDURANT.
- If you miss a dose of EDURANT within 12 hours of the time you usually take it, take your dose of EDURANT with a meal as soon as possible. Then, take your next dose of EDURANT at the regularly scheduled time. If you miss a dose of EDURANT by more than 12 hours of the time you usually take it, wait and then take the next dose of EDURANT at the regularly scheduled time.
- Do not take more than your prescribed dose to make up for a missed dose.
- If you take too much EDURANT, call your healthcare provider or go to the nearest hospital emergency room right away.
- When your supply of EDURANT starts to run low, get more from your healthcare provider or pharmacy. It is important not to run out of EDURANT. The amount of HIV in your blood may increase if the medicine is stopped even for a short time.
What are the possible side effects of EDURANT? EDURANT can cause serious side effects including: -
Severe skin rash and allergic reactions. Skin rash is a common side effect of EDURANT. Skin rash can be serious. Call your healthcare provider right away if you get a rash. In some cases, rash and allergic reaction may need to be treated in a hospital.
If you get a rash with any of the following symptoms, stop taking EDURANT and get medical help right away:- fever
- skin blisters
- mouth sores
- redness or swelling of the eyes (conjunctivitis)
- swelling of the face, lips, mouth, tongue, or throat
- trouble breathing or swallowing
- pain on the right side of the stomach (abdominal) area
- dark colored urine "tea colored"
- Change in liver enzymes. People with a history of hepatitis B or C virus infection or who have certain liver function test changes may have an increased risk of developing new or worsening liver problems during treatment with EDURANT. Liver problems have also happened during treatment with EDURANT in people without a history of liver disease. Your healthcare provider may need to do tests to check your liver enzymes before and during treatment with EDURANT.
-
Depression or mood changes. Tell your healthcare provider right away if you have any of the following symptoms:
- feeling sad or hopeless
- feeling anxious or restless
- have thoughts of hurting yourself (suicide) or have tried to hurt yourself
- Changes in body fat can happen in people who take HIV medicine. These changes may include increased amount of fat in the upper back and neck ("buffalo hump"), breast, and around the middle of your body (trunk). Loss of fat from the legs, arms, and face may also happen. The exact cause and long- term health effects of these problems are not known.
- Changes in your immune system (Immune Reconstitution Syndrome) can happen when you start taking HIV medicines. Your immune system may get stronger and begin to fight infections that have been hidden in your body for a long time. Tell your healthcare provider right away if you start having any new symptoms after starting your HIV-1 medicine.
The most common side effects of EDURANT include depression, headache, trouble sleeping (insomnia) and rash.
These are not all the possible side effects with EDURANT.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.How should I store EDURANT? - Store EDURANT at room temperature between 68°F to 77°F (20°C to 25°C).
- Keep EDURANT in the original bottle to protect from light.
Keep EDURANT and all medicines out of the reach of children. General information about the safe and effective use of EDURANT Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use EDURANT for a condition for which it was not prescribed. Do not give EDURANT to other people even if they have the same condition you have. It may harm them. You can ask your healthcare provider or pharmacist for information about EDURANT that is written for health professionals. What are the ingredients in EDURANT? Active ingredient: rilpivirine. Inactive ingredients: croscarmellose sodium, lactose monohydrate, magnesium stearate, polysorbate 20, povidone K30 and silicified microcrystalline cellulose. The tablet coating contains hypromellose 2910 6 mPa.s, lactose monohydrate, PEG 3000, titanium dioxide, and triacetin. Manufactured by: Janssen-Cilag SpA, Latina, Italy
Manufactured for: Janssen Therapeutics, Division of Janssen Products, LP, Titusville NJ 08560
EDURANT® is a registered trademark of Johnson & Johnson
© Janssen Products, LP 2011
For more information go to www.EDURANT.com or call 1-800-526-7736 - PRINCIPAL DISPLAY PANEL - 25 mg Tablet Bottle Label
-
INGREDIENTS AND APPEARANCE
EDURANT
rilpivirine hydrochloride tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 59676-278 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength rilpivirine hydrochloride (UNII: 212WAX8KDD) (rilpivirine - UNII:FI96A8X663) rilpivirine 25 mg Inactive Ingredients Ingredient Name Strength CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) POVIDONE K30 (UNII: U725QWY32X) POLYSORBATE 20 (UNII: 7T1F30V5YH) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) HYPROMELLOSE 2910 (6 MPA.S) (UNII: 0WZ8WG20P6) POLYETHYLENE GLYCOL 3000 (UNII: SA1B764746) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) TRIACETIN (UNII: XHX3C3X673) Product Characteristics Color WHITE (white to off white) Score no score Shape ROUND (biconvex) Size 6mm Flavor Imprint Code TMC;25 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 59676-278-01 30 in 1 BOTTLE; Type 0: Not a Combination Product 05/20/2011 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA202022 05/20/2011 Labeler - Janssen Products, LP (804684207) Establishment Name Address ID/FEI Business Operations Janssen-Cilag SpA 542797928 MANUFACTURE(59676-278) , ANALYSIS(59676-278) Establishment Name Address ID/FEI Business Operations Janssen Pharmaceutica NV 374747970 API MANUFACTURE(59676-278) Establishment Name Address ID/FEI Business Operations Janssen Pharmaceutical Sciences Unlimited Company 985639841 API MANUFACTURE(59676-278) Establishment Name Address ID/FEI Business Operations Anderson Packaging, Inc. 053217022 LABEL(59676-278) , PACK(59676-278)
Trademark Results [EDURANT]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 EDURANT 85185858 not registered Dead/Abandoned |
JOHNSON & JOHNSON 2010-11-29 |
 EDURANT 85125575 4013848 Live/Registered |
JOHNSON & JOHNSON 2010-09-09 |
 EDURANT 76647698 not registered Dead/Abandoned |
JOHNSON & JOHNSON 2005-09-29 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.
