FLOVENT DISKUS- fluticasone propionate powder, metered
FLOVENT by
Drug Labeling and Warnings
FLOVENT by is a Prescription medication manufactured, distributed, or labeled by A-S Medication Solutions. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use FLOVENT DISKUS safely and effectively. See full prescribing information for FLOVENT DISKUS.
FLOVENT DISKUS (fluticasone propionate inhalation powder), for oral inhalation use
Initial U.S. Approval: 1994INDICATIONS AND USAGE
DOSAGE AND ADMINISTRATION
- For oral inhalation only. (2.1)
- Starting dosage is based on prior asthma therapy and disease severity. (2.2)
- Treatment of asthma in patients aged 12 years and older: 100 mcg twice daily up to a maximum recommended dosage of 1,000 mcg twice daily. (2.2)
- Treatment of asthma in patients aged 4 to 11 years: 50 mcg twice daily up to a maximum recommended dosage of 100 mcg twice daily. (2.2)
DOSAGE FORMS AND STRENGTHS
Inhalation powder: Inhaler containing fluticasone propionate (50, 100, or 250 mcg) as a powder formulation for oral inhalation. (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Candida albicans infection of the mouth and pharynx may occur. Monitor patients periodically. Advise the patient to rinse his/her mouth with water without swallowing after inhalation to help reduce the risk. (5.1)
- Potential worsening of infections (e.g., existing tuberculosis; fungal, bacterial, viral, or parasitic infection; ocular herpes simplex). Use with caution in patients with these infections. More serious or even fatal course of chickenpox or measles can occur in susceptible patients. (5.3)
- Risk of impaired adrenal function when transferring from systemic corticosteroids. Taper patients slowly from systemic corticosteroids if transferring to FLOVENT DISKUS. (5.4)
- Hypercorticism and adrenal suppression may occur with very high dosages or at the regular dosage in susceptible individuals. If such changes occur, discontinue FLOVENT DISKUS slowly. (5.5)
- Assess for decrease in bone mineral density initially and periodically thereafter. (5.7)
- Monitor growth of pediatric patients. (5.8)
- Glaucoma and cataracts may occur with long-term use of ICS. Consider referral to an ophthalmologist in patients who develop ocular symptoms or use FLOVENT DISKUS long term. (5.9)
ADVERSE REACTIONS
Most common adverse reactions (incidence >3%) include upper respiratory tract infection or inflammation, throat irritation, sinusitis, rhinitis, oral candidiasis, nausea and vomiting, gastrointestinal discomfort, fever, cough, bronchitis, and headache. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact GlaxoSmithKline at 1-888-825-5249 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
Strong cytochrome P450 3A4 inhibitors (e.g., ritonavir, ketoconazole): Use not recommended. May increase risk of systemic corticosteroid effects. (7.1)
USE IN SPECIFIC POPULATIONS
Hepatic impairment: Monitor patients for signs of increased drug exposure. (8.6)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 1/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Administration Information
2.2 Recommended Dosage
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Local Effects of Inhaled Corticosteroids
5.2 Acute Asthma Episodes
5.3 Immunosuppression
5.4 Transferring Patients from Systemic Corticosteroid Therapy
5.5 Hypercorticism and Adrenal Suppression
5.6 Immediate Hypersensitivity Reactions
5.7 Reduction in Bone Mineral Density
5.8 Effect on Growth
5.9 Glaucoma and Cataracts
5.10 Paradoxical Bronchospasm
5.11 Drug Interactions with Strong Cytochrome P450 3A4 Inhibitors
5.12 Eosinophilic Conditions and Churg-Strauss Syndrome
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Inhibitors of Cytochrome P450 3A4
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 Renal Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Adult and Adolescent Subjects Aged 12 Years and Older
14.2 Pediatric Subjects Aged 4 to 11 Years
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Administration Information
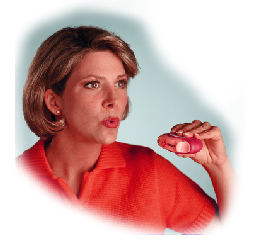
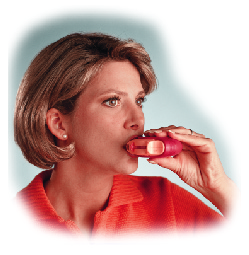
FLOVENT DISKUS should be administered by the orally inhaled route in patients aged 4 years and older. After inhalation, the patient should rinse his/her mouth with water without swallowing to help reduce the risk of oropharyngeal candidiasis.
2.2 Recommended Dosage
Adult and Adolescent Patients Aged 12 Years and Older
The starting dosage is based on previous asthma therapy and asthma severity, including consideration of patients’ current control of asthma symptoms and risk of future exacerbation. The recommended starting dosage for patients aged 12 years and older who are not on an inhaled corticosteroid (ICS) is 100 mcg twice daily, approximately 12 hours apart. For other patients, and for patients who do not respond adequately to the starting dosage after 2 weeks of therapy, higher dosages may provide additional asthma control. The maximum recommended dosage for patients aged 12 years and older is 1,000 mcg twice daily.
Pediatric Patients Aged 4 to 11 Years
The starting dosage is based on previous asthma therapy and asthma severity, including consideration of patients’ current control of asthma symptoms and risk of future exacerbation. For patients aged 4 to 11 years not on an ICS, the recommended starting dosage is 50 mcg twice daily, approximately 12 hours apart. For other patients, and for patients who do not respond adequately to the starting dosage after 2 weeks of therapy, increasing the dosage to 100 mcg twice daily may provide additional asthma control. The maximum recommended dosage for patients aged 4 to 11 years is 100 mcg twice daily.
General Dosing Recommendations
If symptoms arise between doses, an inhaled short-acting beta2-agonist should be used for immediate relief.
Individual patients will experience a variable time to onset and degree of symptom relief. Maximum benefit may not be achieved for 1 to 2 weeks or longer after starting treatment.
If a dosage regimen fails to provide adequate control of asthma, the therapeutic regimen should be re-evaluated and additional therapeutic options, e.g., replacing the current strength with a higher strength, initiating an ICS and long-acting beta2-agonist (LABA) combination product, or initiating oral corticosteroids, should be considered.
After asthma stability has been achieved, titrate to the lowest effective dosage to reduce the possibility of side effects.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
The use of FLOVENT DISKUS is contraindicated in the following conditions:
- Primary treatment of status asthmaticus or other acute episodes of asthma where intensive measures are required [see Warnings and Precautions (5.2)]
- Severe hypersensitivity to milk proteins or demonstrated hypersensitivity to fluticasone propionate [see Warnings and Precautions (5.6), Adverse Reactions (6.2), Description (11)]
-
5 WARNINGS AND PRECAUTIONS
5.1 Local Effects of Inhaled Corticosteroids
In clinical trials, the development of localized infections of the mouth and pharynx with Candida albicans has occurred in subjects treated with FLOVENT DISKUS. When such an infection develops, it should be treated with appropriate local or systemic (i.e., oral) antifungal therapy while treatment with FLOVENT DISKUS continues, but at times therapy with FLOVENT DISKUS may need to be interrupted. Advise the patient to rinse his/her mouth with water without swallowing following inhalation to help reduce the risk of oropharyngeal candidiasis.
5.2 Acute Asthma Episodes
FLOVENT DISKUS is not to be regarded as a bronchodilator and is not indicated for rapid relief of bronchospasm. Patients should be instructed to contact their physicians immediately when episodes of asthma that are not responsive to bronchodilators occur during the course of treatment with FLOVENT DISKUS. During such episodes, patients may require therapy with oral corticosteroids.
5.3 Immunosuppression
Persons who are using drugs that suppress the immune system are more susceptible to infections than healthy individuals. Chickenpox and measles, for example, can have a more serious or even fatal course in susceptible children or adults using corticosteroids. In such children or adults who have not had these diseases or been properly immunized, particular care should be taken to avoid exposure. How the dose, route, and duration of corticosteroid administration affect the risk of developing a disseminated infection is not known. The contribution of the underlying disease and/or prior corticosteroid treatment to the risk is also not known. If a patient is exposed to chickenpox, prophylaxis with varicella zoster immune globulin (VZIG) may be indicated. If a patient is exposed to measles, prophylaxis with pooled intramuscular immunoglobulin (IG) may be indicated. (See the respective package inserts for complete VZIG and IG prescribing information.) If chickenpox develops, treatment with antiviral agents may be considered.
ICS should be used with caution, if at all, in patients with active or quiescent tuberculosis infections of the respiratory tract; systemic fungal, bacterial, viral, or parasitic infections; or ocular herpes simplex.
5.4 Transferring Patients from Systemic Corticosteroid Therapy
Particular care is needed for patients who have been transferred from systemically active corticosteroids to ICS because deaths due to adrenal insufficiency have occurred in patients with asthma during and after transfer from systemic corticosteroids to less systemically available ICS. After withdrawal from systemic corticosteroids, a number of months are required for recovery of hypothalamic-pituitary-adrenal (HPA) function.
Patients who have been previously maintained on 20 mg or more of prednisone (or its equivalent) may be most susceptible, particularly when their systemic corticosteroids have been almost completely withdrawn. During this period of HPA suppression, patients may exhibit signs and symptoms of adrenal insufficiency when exposed to trauma, surgery, or infection (particularly gastroenteritis) or other conditions associated with severe electrolyte loss. Although FLOVENT DISKUS may control asthma symptoms during these episodes, in recommended doses it supplies less than normal physiological amounts of glucocorticoid systemically and does NOT provide the mineralocorticoid activity that is necessary for coping with these emergencies.
During periods of stress or a severe asthma attack, patients who have been withdrawn from systemic corticosteroids should be instructed to resume oral corticosteroids (in large doses) immediately and to contact their physicians for further instruction. These patients should also be instructed to carry a warning card indicating that they may need supplementary systemic corticosteroids during periods of stress or a severe asthma attack.
Patients requiring oral corticosteroids should be weaned slowly from systemic corticosteroid use after transferring to FLOVENT DISKUS. Prednisone reduction can be accomplished by reducing the daily prednisone dose by 2.5 mg on a weekly basis during therapy with FLOVENT DISKUS. Lung function (mean forced expiratory volume in 1 second [FEV1] or morning peak expiratory flow [AM PEF]), beta-agonist use, and asthma symptoms should be carefully monitored during withdrawal of oral corticosteroids. In addition, patients should be observed for signs and symptoms of adrenal insufficiency, such as fatigue, lassitude, weakness, nausea and vomiting, and hypotension.
Transfer of patients from systemic corticosteroid therapy to FLOVENT DISKUS may unmask allergic conditions previously suppressed by the systemic corticosteroid therapy (e.g., rhinitis, conjunctivitis, eczema, arthritis, eosinophilic conditions).
During withdrawal from oral corticosteroids, some patients may experience symptoms of systemically active corticosteroid withdrawal (e.g., joint and/or muscular pain, lassitude, depression) despite maintenance or even improvement of respiratory function.
5.5 Hypercorticism and Adrenal Suppression
Fluticasone propionate will often help control asthma symptoms with less suppression of HPA function than therapeutically equivalent oral doses of prednisone. Since fluticasone propionate is absorbed into the circulation and can be systemically active at higher doses, the beneficial effects of FLOVENT DISKUS in minimizing HPA dysfunction may be expected only when recommended dosages are not exceeded and individual patients are titrated to the lowest effective dose. A relationship between plasma levels of fluticasone propionate and inhibitory effects on stimulated cortisol production has been shown after 4 weeks of treatment with fluticasone propionate inhalation aerosol. Since individual sensitivity to effects on cortisol production exists, physicians should consider this information when prescribing FLOVENT DISKUS.
Because of the possibility of significant systemic absorption of ICS in sensitive patients, patients treated with FLOVENT DISKUS should be observed carefully for any evidence of systemic corticosteroid effects. Particular care should be taken in observing patients postoperatively or during periods of stress for evidence of inadequate adrenal response.
It is possible that systemic corticosteroid effects such as hypercorticism and adrenal suppression (including adrenal crisis) may appear in a small number of patients who are sensitive to these effects. If such effects occur, FLOVENT DISKUS should be reduced slowly, consistent with accepted procedures for reducing systemic corticosteroids, and other treatments for management of asthma symptoms should be considered.
5.6 Immediate Hypersensitivity Reactions
Immediate hypersensitivity reactions (e.g., urticaria, angioedema, rash, bronchospasm, hypotension), including anaphylaxis, may occur after administration of FLOVENT DISKUS. There have been reports of anaphylactic reactions in patients with severe milk protein allergy after inhalation of powder products containing lactose; therefore, patients with severe milk protein allergy should not use FLOVENT DISKUS [see Contraindications (4)].
5.7 Reduction in Bone Mineral Density
Decreases in bone mineral density (BMD) have been observed with long-term administration of products containing ICS. The clinical significance of small changes in BMD with regard to long-term consequences such as fracture is unknown. Patients with major risk factors for decreased bone mineral content, such as prolonged immobilization, family history of osteoporosis, postmenopausal status, tobacco use, advanced age, poor nutrition, or chronic use of drugs that can reduce bone mass (e.g., anticonvulsants, oral corticosteroids), should be monitored and treated with established standards of care.
A 2-year trial in 160 subjects (females aged 18 to 40 years, males 18 to 50) with asthma receiving chlorofluorocarbon (CFC)-propelled fluticasone propionate inhalation aerosol 88 or 440 mcg twice daily demonstrated no statistically significant changes in BMD at any time point (24, 52, 76, and 104 weeks of double-blind treatment) as assessed by dual-energy x-ray absorptiometry at lumbar regions L1 through L4.
5.8 Effect on Growth
Orally inhaled corticosteroids may cause a reduction in growth velocity when administered to pediatric patients. Monitor the growth of pediatric patients receiving FLOVENT DISKUS routinely (e.g., via stadiometry). To minimize the systemic effects of orally inhaled corticosteroids, including FLOVENT DISKUS, titrate each patient’s dosage to the lowest dosage that effectively controls his/her symptoms [see Dosage and Administration (2.2), Use in Specific Populations (8.4)].
5.9 Glaucoma and Cataracts
Glaucoma, increased intraocular pressure, and cataracts have been reported in patients following the long-term administration of ICS, including fluticasone propionate. Consider referral to an ophthalmologist in patients who develop ocular symptoms or use FLOVENT DISKUS long term.
5.10 Paradoxical Bronchospasm
As with other inhaled medicines, bronchospasm may occur with an immediate increase in wheezing after dosing. If bronchospasm occurs following dosing with FLOVENT DISKUS, it should be treated immediately with an inhaled, short-acting bronchodilator; FLOVENT DISKUS should be discontinued immediately; and alternative therapy should be instituted.
5.11 Drug Interactions with Strong Cytochrome P450 3A4 Inhibitors
The use of strong cytochrome P450 3A4 (CYP3A4) inhibitors (e.g., ritonavir, atazanavir, clarithromycin, indinavir, itraconazole, nefazodone, nelfinavir, saquinavir, ketoconazole, telithromycin) with FLOVENT DISKUS is not recommended because increased systemic corticosteroid adverse effects may occur [see Drug Interactions (7.1), Clinical Pharmacology (12.3)].
5.12 Eosinophilic Conditions and Churg-Strauss Syndrome
In rare cases, patients on inhaled fluticasone propionate may present with systemic eosinophilic conditions. Some of these patients have clinical features of vasculitis consistent with Churg-Strauss syndrome, a condition that is often treated with systemic corticosteroid therapy. These events usually, but not always, have been associated with the reduction and/or withdrawal of oral corticosteroid therapy following the introduction of fluticasone propionate. Cases of serious eosinophilic conditions have also been reported with other ICS in this clinical setting. Physicians should be alert to eosinophilia, vasculitic rash, worsening pulmonary symptoms, cardiac complications, and/or neuropathy presenting in their patients. A causal relationship between fluticasone propionate and these underlying conditions has not been established.
-
6 ADVERSE REACTIONS
Systemic and local corticosteroid use may result in the following:
- Candida albicans infection [see Warnings and Precautions (5.1)]
- Immunosuppression [see Warnings and Precautions (5.3)]
- Hypercorticism and adrenal suppression [see Warnings and Precautions (5.5)]
- Reduction in bone mineral density [see Warnings and Precautions (5.7)]
- Growth effects [see Warnings and Precautions (5.8)]
- Glaucoma and cataracts [see Warnings and Precautions (5.9)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The incidence of common adverse reactions in Table 1 is based upon 7 placebo-controlled U.S. clinical trials in which 1,176 pediatric, adolescent, and adult subjects (466 females and 710 males) previously treated with as-needed bronchodilators and/or ICS were treated twice daily for up to 12 weeks with FLOVENT DISKUS (doses of 50 to 500 mcg) or placebo.
Table 1. Adverse Reactions with FLOVENT DISKUS with >3% Incidence and More Common than Placebo in Subjects with Asthma
Adverse Event
FLOVENT DISKUS 50 mcg
Twice Daily
(n = 178)
%
FLOVENT DISKUS 100 mcg
Twice Daily
(n = 305)
%
FLOVENT DISKUS 250 mcg
Twice Daily
(n = 86)
%
FLOVENT DISKUS 500 mcg
Twice Daily
(n = 64)
%
Placebo
(n = 543)
%
Ear, nose, and throat
- Upper respiratory tract infection
20
18
21
14
16
- Throat irritation
13
13
3
22
8
- Sinusitis/sinus infection
9
10
6
6
6
- Upper respiratory inflammation
5
5
0
5
3
- Rhinitis
4
3
1
2
2
- Oral candidiasis
<1
9
6
5
7
Gastrointestinal
- Nausea and vomiting
8
4
1
2
4
- Gastrointestinal discomfort and pain
4
3
2
2
3
- Viral gastrointestinal infection
4
3
3
5
1
Non-site specific
- Fever
7
7
1
2
4
- Viral infection
2
2
0
5
2
Lower respiratory
- Viral respiratory infection
4
5
1
2
4
- Cough
3
5
1
5
4
- Bronchitis
2
3
0
8
1
Neurological
- Headache
12
12
2
14
7
Musculoskeletal and trauma
- Muscle injury
2
0
1
5
1
- Musculoskeletal pain
4
3
2
5
2
- Injury
2
<1
0
5
<1
Table 1 includes all events (whether considered drug-related or nondrug-related by the investigator) that occurred at a rate of over 3% in any of the groups treated with FLOVENT DISKUS and were more common than in the placebo group. Less than 2% of subjects discontinued from the trials because of adverse reactions. The average duration of exposure was 73 to 79 days in the active treatment groups compared with 56 days in the placebo group.
Additional Adverse Reactions
Other adverse reactions not previously listed, whether considered drug-related or not by the investigators, that were reported more frequently by subjects with asthma treated with FLOVENT DISKUS compared with subjects treated with placebo include the following: palpitations; soft tissue injuries; contusions and hematomas; wounds and lacerations; burns; poisoning and toxicity; pressure-induced disorders; hoarseness/dysphonia; epistaxis; ear, nose, throat, and tonsil signs and symptoms; ear, nose, and throat polyps; allergic ear, nose, and throat disorders; throat constriction; fluid disturbances; weight gain; appetite disturbances; keratitis and conjunctivitis; blepharoconjunctivitis; gastrointestinal signs and symptoms; oral ulcerations; dental discomfort and pain; oral erythema and rashes; mouth and tongue disorders; oral discomfort and pain; tooth decay; cholecystitis; arthralgia and articular rheumatism; muscle cramps and spasms; musculoskeletal inflammation; dizziness; sleep disorders; migraines; paralysis of cranial nerves; edema and swelling; bacterial infections; fungal infections; mobility disorders; mood disorders; bacterial reproductive infections; photodermatitis; dermatitis and dermatosis; viral skin infections; eczema; pruritus; acne and folliculitis; urinary infections.
Three (3) of the 7 placebo-controlled U.S. clinical trials were pediatric trials. A total of 592 subjects aged 4 to 11 years were treated with FLOVENT DISKUS (dosages of 50 or 100 mcg twice daily) or placebo; an additional 174 subjects aged 4 to 11 years received FLOVENT ROTADISK (fluticasone propionate inhalation powder) at the same doses. There were no clinically relevant differences in the pattern or severity of adverse events in children compared with those reported in adults.
In the first 16 weeks of a 52-week clinical trial in adult subjects with asthma who previously required oral corticosteroids (daily doses of 5 to 40 mg oral prednisone), the effects of FLOVENT DISKUS 500 mcg twice daily (n = 41) and 1,000 mcg twice daily (n = 36) were compared with placebo (n = 34) for the frequency of reported adverse events. The average duration of exposure for subjects taking FLOVENT DISKUS was 105 days compared with 75 days for placebo. Adverse events, whether or not considered drug related by the investigators, reported in more than 5 subjects in the group taking FLOVENT DISKUS and that occurred more frequently with FLOVENT DISKUS than with placebo are shown below (percent FLOVENT DISKUS and percent placebo).
Ear, Nose, and Throat: Hoarseness/dysphonia (9% and 0%), nasal congestion/blockage (16% and 0%), oral candidiasis (31% and 21%), rhinitis (13% and 9%), sinusitis/sinus infection (33% and 12%), throat irritation (10% and 9%), and upper respiratory tract infection (31% and 24%).
Gastrointestinal: Nausea and vomiting (9% and 0%).
Lower Respiratory: Cough (9% and 3%) and viral respiratory infections (9% and 6%).
Musculoskeletal: Arthralgia and articular rheumatism (17% and 3%) and muscle pain (12% and 0%).
Non-Site Specific: Malaise and fatigue (16% and 9%) and pain (10% and 3%).
Skin: Pruritus (6% and 0%) and skin rashes (8% and 3%).
6.2 Postmarketing Experience
In addition to adverse reactions reported from clinical trials, the following adverse reactions have been identified during postapproval use of fluticasone propionate. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. These events have been chosen for inclusion due to either their seriousness, frequency of reporting, or causal connection to fluticasone propionate or a combination of these factors.
Ear, Nose, and Throat
Aphonia, facial and oropharyngeal edema, and throat soreness.
Endocrine and Metabolic
Cushingoid features, growth velocity reduction in children/adolescents, hyperglycemia, and osteoporosis.
Eye
Cataracts.
Immune System Disorders
Immediate and delayed hypersensitivity reactions, including anaphylaxis, rash, angioedema, and bronchospasm, have been reported. Anaphylactic reactions in patients with severe milk protein allergy have been reported.
Infections and Infestations
Esophageal candidiasis.
Psychiatry
Agitation, aggression, anxiety, depression, and restlessness. Behavioral changes, including hyperactivity and irritability, have been reported very rarely and primarily in children.
Respiratory
Asthma exacerbation, bronchospasm, chest tightness, dyspnea, immediate bronchospasm, pneumonia, and wheeze.
Skin
Contusions and ecchymoses.
-
7 DRUG INTERACTIONS
7.1 Inhibitors of Cytochrome P450 3A4
Fluticasone propionate is a substrate of CYP3A4. The use of strong CYP3A4 inhibitors (e.g., ritonavir, atazanavir, clarithromycin, indinavir, itraconazole, nefazodone, nelfinavir, saquinavir, ketoconazole, telithromycin) with FLOVENT DISKUS is not recommended because increased systemic corticosteroid adverse effects may occur.
Ritonavir
A drug interaction trial with fluticasone propionate aqueous nasal spray in healthy subjects has shown that ritonavir (a strong CYP3A4 inhibitor) can significantly increase plasma fluticasone propionate exposure, resulting in significantly reduced serum cortisol concentrations [see Clinical Pharmacology (12.3)]. During postmarketing use, there have been reports of clinically significant drug interactions in patients receiving fluticasone propionate and ritonavir, resulting in systemic corticosteroid effects including Cushing’s syndrome and adrenal suppression.
Ketoconazole
Coadministration of orally inhaled fluticasone propionate (1,000 mcg) and ketoconazole (200 mg once daily) resulted in a 1.9-fold increase in plasma fluticasone propionate exposure and a 45% decrease in plasma cortisol area under the curve (AUC), but had no effect on urinary excretion of cortisol.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are insufficient data on the use of FLOVENT DISKUS in pregnant women. There are clinical considerations with the use of FLOVENT DISKUS in pregnant women. (See Clinical Considerations.) In animals, teratogenicity characteristic of corticosteroids, decreased fetal body weight, and/or skeletal variations in rats, mice, and rabbits were observed with subcutaneously administered maternal toxic doses of fluticasone propionate less than the maximum recommended human daily inhaled dose (MRHDID) on a mcg/m2 basis. (See Data.) However, fluticasone propionate administered via inhalation to rats decreased fetal body weight, but did not induce teratogenicity at a maternal toxic dose less than the MRHDID on a mcg/m2 basis. (See Data.) Experience with oral corticosteroids suggests that rodents are more prone to teratogenic effects from corticosteroids than humans.
The estimated risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Disease-Associated Maternal and/or Embryofetal Risk: In women with poorly or moderately controlled asthma, there is an increased risk of several perinatal outcomes such as pre-eclampsia in the mother and prematurity, low birth weight, and small for gestational age in the neonate. Pregnant women with asthma should be closely monitored and medication adjusted as necessary to maintain optimal asthma control.
Data
Human Data: Following inhaled administration, fluticasone propionate was detected in the neonatal cord blood after delivery.
Animal Data: In embryofetal development studies with pregnant rats and mice dosed by the subcutaneous route throughout the period of organogenesis, fluticasone propionate was teratogenic in both species. Omphalocele, decreased body weight, and skeletal variations were observed in rat fetuses, in the presence of maternal toxicity, at a dose approximately 0.5 times the MRHDID (on a mcg/m2 basis with a maternal subcutaneous dose of 100 mcg/kg/day). The rat no observed adverse effect level (NOAEL) was observed at approximately 0.15 times the MRHDID (on a mcg/m2 basis with a maternal subcutaneous dose of 30 mcg/kg/day). Cleft palate and fetal skeletal variations were observed in mouse fetuses at a dose approximately 0.1 times the MRHDID (on a mcg/m2 basis with a maternal subcutaneous dose of 45 mcg/kg/day). The mouse NOAEL was observed with a dose approximately 0.04 times the MRHDID (on a mcg/m2 basis with a maternal subcutaneous dose of 15 mcg/kg/day).
In an embryofetal development study with pregnant rats dosed by the inhalation route throughout the period of organogenesis, fluticasone propionate produced decreased fetal body weights and skeletal variations, in the presence of maternal toxicity, at a dose approximately 0.13 times the MRHDID (on a mcg/m2 basis with a maternal inhalation dose of 25.7 mcg/kg/day); however, there was no evidence of teratogenicity. The NOAEL was observed with a dose approximately 0.03 times the MRHDID (on a mcg/m2 basis with a maternal inhalation dose of 5.5 mcg/kg/day).
In an embryofetal development study in pregnant rabbits that were dosed by the subcutaneous route throughout organogenesis, fluticasone propionate produced reductions of fetal body weights, in the presence of maternal toxicity, at doses approximately 0.006 times the MRHDID and higher (on a mcg/m2 basis with a maternal subcutaneous dose of 0.57 mcg/kg/day). Teratogenicity was evident based upon a finding of cleft palate for 1 fetus at a dose approximately 0.04 times the MRHDID (on a mcg/m2 basis with a maternal subcutaneous dose of 4 mcg/kg/day). The NOAEL was observed in rabbit fetuses with a dose approximately 0.001 times the MRHDID (on a mcg/m2 basis with a maternal subcutaneous dose of 0.08 mcg/kg/day).
Fluticasone propionate crossed the placenta following subcutaneous administration to mice and rats and oral administration to rabbits.
In a pre- and post-natal development study in pregnant rats dosed from late gestation through delivery and lactation (Gestation Day 17 to Postpartum Day 22), fluticasone propionate was not associated with decreases in pup body weight, and had no effects on developmental landmarks, learning, memory, reflexes, or fertility at doses up to 0.2 times the MRHDID (on a mcg/m2 basis with maternal subcutaneous doses up to 50 mcg/kg/day).
8.2 Lactation
Risk Summary
There are no available data on the presence of fluticasone propionate in human milk, the effects on the breastfed child, or the effects on milk production. Other corticosteroids have been detected in human milk. However, fluticasone propionate concentrations in plasma after inhaled therapeutic doses are low and therefore concentrations in human breast milk are likely to be correspondingly low [see Clinical Pharmacology (12.3)]. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for FLOVENT DISKUS and any potential adverse effects on the breastfed child from FLOVENT DISKUS or from the underlying maternal condition.
Data
Animal Data: Subcutaneous administration of tritiated fluticasone propionate at a dose of 10 mcg/kg/day to lactating rats resulted in measurable levels in milk.
8.4 Pediatric Use
The safety and effectiveness of FLOVENT DISKUS in children aged 4 years and older have been established [see Adverse Reactions (6.1), Clinical Pharmacology (12.3), Clinical Studies (14.2)]. The safety and effectiveness of FLOVENT DISKUS in children younger than 4 years have not been established.
Effects on Growth
Orally inhaled corticosteroids may cause a reduction in growth velocity when administered to pediatric patients. A reduction of growth velocity in children or teenagers may occur as a result of poorly controlled asthma or from use of corticosteroids, including ICS. The effects of long-term treatment of children and adolescents with ICS, including fluticasone propionate, on final adult height are not known.
Controlled clinical trials have shown that ICS may cause a reduction in growth in pediatric patients. In these trials, the mean reduction in growth velocity was approximately 1 cm/year (range: 0.3 to 1.8 cm/year) and appeared to depend upon dose and duration of exposure. This effect was observed in the absence of laboratory evidence of HPA axis suppression, suggesting that growth velocity is a more sensitive indicator of systemic corticosteroid exposure in pediatric patients than some commonly used tests of HPA axis function. The long‑term effects of this reduction in growth velocity associated with orally inhaled corticosteroids, including the impact on final adult height, are unknown. The potential for “catch-up” growth following discontinuation of treatment with orally inhaled corticosteroids has not been adequately studied. The effects on growth velocity of treatment with orally inhaled corticosteroids for over 1 year, including the impact on final adult height, are unknown. The growth of children and adolescents receiving orally inhaled corticosteroids, including FLOVENT DISKUS, should be monitored routinely (e.g., via stadiometry). The potential growth effects of prolonged treatment should be weighed against the clinical benefits obtained and the risks associated with alternative therapies. To minimize the systemic effects of orally inhaled corticosteroids, including FLOVENT DISKUS, each patient should be titrated to the lowest dose that effectively controls his/her symptoms.
A 52-week placebo-controlled trial to assess the potential growth effects of fluticasone propionate inhalation powder (FLOVENT ROTADISK) at 50 and 100 mcg twice daily was conducted in the U.S. in 325 prepubescent children (244 males and 81 females) aged 4 to 11 years. The mean growth velocities at 52 weeks observed in the intent-to-treat population were 6.32 cm/year in the placebo group (n = 76), 6.07 cm/year in the 50-mcg group (n = 98), and 5.66 cm/year in the 100‑mcg group (n = 89). An imbalance in the proportion of children entering puberty between groups and a higher dropout rate in the placebo group due to poorly controlled asthma may be confounding factors in interpreting these data. A separate subset analysis of children who remained prepubertal during the trial revealed growth rates at 52 weeks of 6.10 cm/year in the placebo group (n = 57), 5.91 cm/year in the 50-mcg group (n = 74), and 5.67 cm/year in the 100‑mcg group (n = 79). In children aged 8.5 years, the mean age of children in this trial, the range for expected growth velocity is: boys – 3rd percentile = 3.8 cm/year, 50th percentile = 5.4 cm/year, and 97th percentile = 7.0 cm/year; girls – 3rd percentile = 4.2 cm/year, 50th percentile = 5.7 cm/year, and 97th percentile = 7.3 cm/year. The clinical relevance of these growth data is not certain.
8.5 Geriatric Use
Safety data have been collected on 280 subjects (FLOVENT DISKUS n = 83, FLOVENT ROTADISK n = 197) aged 65 years and older and 33 subjects (FLOVENT DISKUS n = 14, FLOVENT ROTADISK n = 19) aged 75 years and older who have been treated with fluticasone propionate inhalation powder in U.S. and non-U.S. clinical trials. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger subjects, but greater sensitivity of some older individuals cannot be ruled out.
8.6 Hepatic Impairment
Formal pharmacokinetic studies using FLOVENT DISKUS have not been conducted in patients with hepatic impairment. Since fluticasone propionate is predominantly cleared by hepatic metabolism, impairment of liver function may lead to accumulation of fluticasone propionate in plasma. Therefore, patients with hepatic disease should be closely monitored.
-
10 OVERDOSAGE
Chronic overdosage may result in signs/symptoms of hypercorticism [see Warnings and Precautions (5.5)]. Inhalation by healthy volunteers of a single dose of 4,000 mcg of fluticasone propionate inhalation powder or single doses of 1,760 or 3,520 mcg of fluticasone propionate CFC inhalation aerosol was well tolerated. Fluticasone propionate given by inhalation aerosol at dosages of 1,320 mcg twice daily for 7 to 15 days to healthy human volunteers was also well tolerated. Repeat oral doses up to 80 mg daily for 10 days in healthy volunteers and repeat oral doses up to 20 mg daily for 42 days in subjects were well tolerated. Adverse reactions were of mild or moderate severity, and incidences were similar in active and placebo treatment groups.
-
11 DESCRIPTION
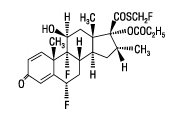
FLOVENT DISKUS inhalation powder is a dry powder inhaler for oral inhalation. The active component of FLOVENT DISKUS 50 mcg, FLOVENT DISKUS 100 mcg, and FLOVENT DISKUS 250 mcg is fluticasone propionate, a corticosteroid having the chemical name S-(fluoromethyl) 6α,9-difluoro-11β,17-dihydroxy-16α-methyl-3-oxoandrosta-1,4-diene-17β-carbothioate, 17-propionate and the following chemical structure:
Fluticasone propionate is a white powder with a molecular weight of 500.6, and the empirical formula is C25H31F3O5S. It is practically insoluble in water, freely soluble in dimethyl sulfoxide and dimethylformamide, and slightly soluble in methanol and 95% ethanol.
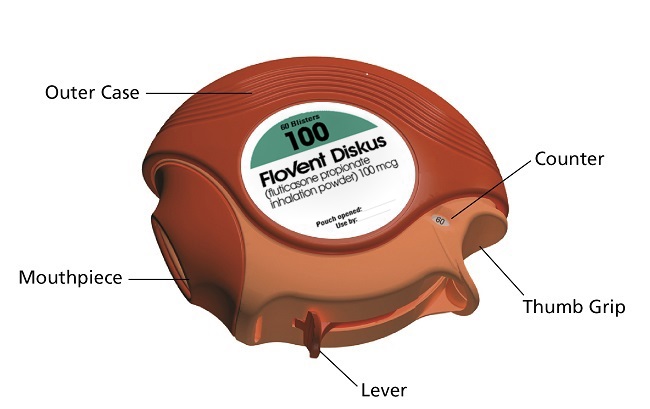
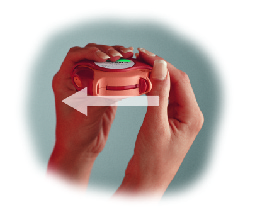
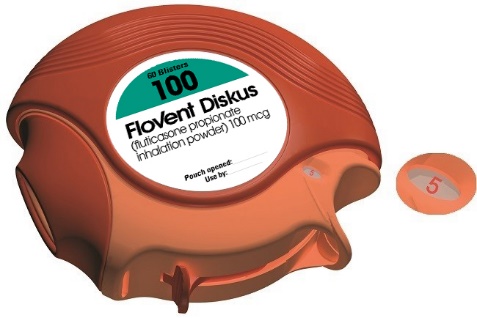
FLOVENT DISKUS is an orange plastic inhaler containing a foil blister strip. Each blister on the strip contains a white powder mix of micronized fluticasone propionate (50, 100, or 250 mcg) in 12.5 mg of formulation containing lactose monohydrate (which contains milk proteins). After the inhaler is activated, the powder is dispersed into the airstream created by the patient inhaling through the mouthpiece.
Under standardized in vitro test conditions, FLOVENT DISKUS delivers 46, 94, and 229 mcg of fluticasone propionate from FLOVENT DISKUS 50 mcg, FLOVENT DISKUS 100 mcg, and FLOVENT DISKUS 250 mcg, respectively, when tested at a flow rate of 60 L/min for 2 seconds.
In adult subjects with obstructive lung disease and severely compromised lung function (mean FEV1 20% to 30% of predicted), mean peak inspiratory flow (PIF) through the DISKUS inhaler was 82.4 L/min (range: 46.1 to 115.3 L/min). In children with asthma aged 4 and 8 years, mean PIF through FLOVENT DISKUS was 70 and 104 L/min, respectively (range: 48 to 123 L/min).
The actual amount of drug delivered to the lung will depend on patient factors, such as inspiratory flow profile.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Fluticasone propionate is a synthetic trifluorinated corticosteroid with anti-inflammatory activity. Fluticasone propionate has been shown in vitro to exhibit a binding affinity for the human glucocorticoid receptor that is 18 times that of dexamethasone, almost twice that of beclomethasone-17-monopropionate (BMP), the active metabolite of beclomethasone dipropionate, and over 3 times that of budesonide. Data from the McKenzie vasoconstrictor assay in man are consistent with these results. The clinical significance of these findings is unknown.
Inflammation is an important component in the pathogenesis of asthma. Corticosteroids have been shown to have a wide range of actions on multiple cell types (e.g., mast cells, eosinophils, neutrophils, macrophages, lymphocytes) and mediators (e.g., histamine, eicosanoids, leukotrienes, cytokines) involved in inflammation. These anti-inflammatory actions of corticosteroids contribute to their efficacy in asthma.
Though effective for the treatment of asthma, corticosteroids do not affect asthma symptoms immediately. Individual patients will experience a variable time to onset and degree of symptom relief. Maximum benefit may not be achieved for 1 to 2 weeks or longer after starting treatment. When corticosteroids are discontinued, asthma stability may persist for several days or longer.
Trials in subjects with asthma have shown a favorable ratio between topical anti-inflammatory activity and systemic corticosteroid effects with recommended doses of orally inhaled fluticasone propionate. This is explained by a combination of a relatively high local anti-inflammatory effect, negligible oral systemic bioavailability (<1%), and the minimal pharmacological activity of the only metabolite detected in man.
12.2 Pharmacodynamics
In clinical trials with fluticasone propionate inhalation powder using dosages up to and including 250 mcg twice daily, occasional abnormal short cosyntropin tests (peak serum cortisol <18 mcg/dL assessed by radioimmunoassay) were noted both in subjects receiving fluticasone propionate and in subjects receiving placebo. The incidence of abnormal tests at 500 mcg twice daily was greater than placebo. In a 2-year trial carried out with the DISKHALER inhalation device in 64 subjects with mild, persistent asthma (mean FEV1 91% of predicted) randomized to fluticasone propionate 500 mcg twice daily or placebo, no subject receiving fluticasone propionate had an abnormal response to 6-hour cosyntropin infusion (peak serum cortisol <18 mcg/dL). With a peak cortisol threshold of <35 mcg/dL, 1 subject receiving fluticasone propionate (4%) had an abnormal response at 1 year; repeat testing at 18 months and 2 years was normal. Another subject receiving fluticasone propionate (5%) had an abnormal response at 2 years. No subject on placebo had an abnormal response at 1 or 2 years.
In a placebo-controlled clinical trial conducted in subjects aged 4 to 11 years, a 30-minute cosyntropin stimulation test was performed in 41 subjects after 12 weeks of dosing with 50 or 100 mcg twice daily of fluticasone propionate via the DISKUS inhaler. One subject receiving fluticasone propionate via the DISKUS inhaler had a prestimulation plasma cortisol concentration <5 mcg/dL, and 2 subjects had a rise in cortisol of <7 mcg/dL. However, all poststimulation values were >18 mcg/dL.
The potential systemic effects of inhaled fluticasone propionate on the HPA axis were also studied in subjects with asthma. Fluticasone propionate given by inhalation aerosol at dosages of 220, 440, 660, or 880 mcg twice daily was compared with placebo or oral prednisone 10 mg given once daily for 4 weeks. For most subjects, the ability to increase cortisol production in response to stress, as assessed by 6-hour cosyntropin stimulation, remained intact with inhaled fluticasone propionate treatment. No subject had an abnormal response (peak serum cortisol <18 mcg/dL) after dosing with placebo or fluticasone propionate 220 mcg twice daily. For subjects treated with 440, 660, and 880 mcg twice daily, 10%, 16%, and 12%, respectively, had an abnormal response as compared with 29% of subjects treated with prednisone.
12.3 Pharmacokinetics
Absorption
Fluticasone propionate acts locally in the lung; therefore, plasma levels do not predict therapeutic effect. Trials using oral dosing of labeled and unlabeled drug have demonstrated that the oral systemic bioavailability of fluticasone propionate is negligible (<1%), primarily due to incomplete absorption and presystemic metabolism in the gut and liver. In contrast, the majority of the fluticasone propionate delivered to the lung is systemically absorbed. The absolute bioavailability of fluticasone propionate from the DISKUS inhaler in healthy volunteers averages 7.8%.
Peak steady-state fluticasone propionate plasma concentrations in adult subjects with asthma (N = 11) ranged from undetectable to 266 pg/mL after a 500-mcg twice-daily dose of fluticasone propionate inhalation powder using the DISKUS inhaler. The mean fluticasone propionate plasma concentration was 110 pg/mL.
Distribution
Following intravenous administration, the initial disposition phase for fluticasone propionate was rapid and consistent with its high lipid solubility and tissue binding. The volume of distribution averaged 4.2 L/kg.
The percentage of fluticasone propionate bound to human plasma proteins averages 99%. Fluticasone propionate is weakly and reversibly bound to erythrocytes and is not significantly bound to human transcortin.
Metabolism
The total clearance of fluticasone propionate is high (average, 1,093 mL/min), with renal clearance accounting for <0.02% of the total. The only circulating metabolite detected in man is the 17β-carboxylic acid derivative of fluticasone propionate, which is formed through the CYP3A4 pathway. This metabolite had less affinity (approximately 1/2,000) than the parent drug for the glucocorticoid receptor of human lung cytosol in vitro and negligible pharmacological activity in animal studies. Other metabolites detected in vitro using cultured human hepatoma cells have not been detected in man.
Elimination
Following intravenous dosing, fluticasone propionate showed polyexponential kinetics and had a terminal elimination half-life of approximately 7.8 hours. Less than 5% of a radiolabeled oral dose was excreted in the urine as metabolites, with the remainder excreted in the feces as parent drug and metabolites.
Specific Populations
Male and Female Patients: Full pharmacokinetic profiles were obtained from 9 female and 16 male subjects given 500 mcg twice daily. No overall differences in fluticasone propionate pharmacokinetics were observed.
Pediatric Patients: In a clinical trial conducted in subjects aged 4 to 11 years with mild to moderate asthma, fluticasone propionate concentrations were obtained in 61 subjects at 20 and 40 minutes after dosing with 50 and 100 mcg twice daily of fluticasone propionate inhalation powder using the DISKUS. Plasma concentrations were low and ranged from undetectable (about 80% of the plasma samples) to 88 pg/mL. Mean peak fluticasone propionate plasma concentrations at the 50- and 100-mcg dose levels were 5 and 8 pg/mL, respectively.
Patients with Hepatic and Renal Impairment: Formal pharmacokinetic studies using FLOVENT DISKUS have not been conducted in patients with hepatic or renal impairment. However, since fluticasone propionate is predominantly cleared by hepatic metabolism, impairment of liver function may lead to accumulation of fluticasone propionate in plasma. Therefore, patients with hepatic disease should be closely monitored.
Drug Interaction Studies
Inhibitors of Cytochrome P450 3A4: Ritonavir: Fluticasone propionate is a substrate of CYP3A4. Coadministration of fluticasone propionate and the strong CYP3A4 inhibitor ritonavir is not recommended based upon a multiple-dose, crossover drug interaction trial in 18 healthy subjects. Fluticasone propionate aqueous nasal spray (200 mcg once daily) was coadministered for 7 days with ritonavir (100 mg twice daily). Plasma fluticasone propionate concentrations following fluticasone propionate aqueous nasal spray alone were undetectable (<10 pg/mL) in most subjects, and when concentrations were detectable, peak levels (Cmax) averaged 11.9 pg/mL (range: 10.8 to 14.1 pg/mL) and AUC(0-τ) averaged 8.43 pgh/mL (range: 4.2 to 18.8 pgh/mL). Fluticasone propionate Cmax and AUC(0-τ) increased to 318 pg/mL (range: 110 to 648 pg/mL) and 3,102.6 pgh/mL (range: 1,207.1 to 5,662.0 pgh/mL), respectively, after coadministration of ritonavir with fluticasone propionate aqueous nasal spray. This significant increase in plasma fluticasone propionate exposure resulted in a significant decrease (86%) in serum cortisol AUC.
Ketoconazole: In a placebo-controlled, crossover trial in 8 healthy adult volunteers, coadministration of a single dose of orally inhaled fluticasone propionate (1,000 mcg) with multiple doses of ketoconazole (200 mg) to steady state resulted in increased plasma fluticasone propionate exposure, a reduction in plasma cortisol AUC, and no effect on urinary excretion of cortisol.
Following orally inhaled fluticasone propionate alone, AUC(2-last) averaged 1.559 ngh/mL (range: 0.555 to 2.906 ngh/mL) and AUC(2-∞) averaged 2.269 ngh/mL (range: 0.836 to 3.707 ngh/mL). Fluticasone propionate AUC(2-last) and AUC(2-∞) increased to 2.781 ngh/mL (range: 2.489 to 8.486 ngh/mL) and 4.317 ngh/mL (range: 3.256 to 9.408 ngh/mL), respectively, after coadministration of ketoconazole with orally inhaled fluticasone propionate. This increase in plasma fluticasone propionate concentration resulted in a decrease (45%) in serum cortisol AUC.
Erythromycin: In a multiple-dose drug interaction trial, coadministration of orally inhaled fluticasone propionate (500 mcg twice daily) and erythromycin (333 mg 3 times daily) did not affect fluticasone propionate pharmacokinetics.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Fluticasone propionate demonstrated no tumorigenic potential in mice at oral doses up to 1,000 mcg/kg (approximately 2 and 10 times the MRHDID for adults and children aged 4 to 11 years, respectively, on a mcg/m2 basis) for 78 weeks or in rats at inhalation doses up to 57 mcg/kg (approximately 0.2 times and approximately equivalent to the MRHDID for adults and children aged 4 to 11 years, respectively, on a mcg/m2 basis) for 104 weeks.
Fluticasone propionate did not induce gene mutation in prokaryotic or eukaryotic cells in vitro. No significant clastogenic effect was seen in cultured human peripheral lymphocytes in vitro or in the in vivo mouse micronucleus test.
Fertility and reproductive performance were unaffected in male and female rats at subcutaneous doses up to 50 mcg/kg (approximately 0.2 times the MRHDID for adults on a mcg/m2 basis).
-
14 CLINICAL STUDIES
14.1 Adult and Adolescent Subjects Aged 12 Years and Older
Four randomized, double-blind, parallel-group, placebo-controlled, U.S. clinical trials were conducted in 1,036 adult and adolescent subjects (aged 12 years and older) with asthma to assess the efficacy and safety of FLOVENT DISKUS in the treatment of asthma. Fixed dosages of 100, 250, and 500 mcg twice daily were compared with placebo to provide information about appropriate dosing to cover a range of asthma severity. Subjects in these trials included those inadequately controlled with bronchodilators alone and those already maintained on daily ICS. All doses were delivered by inhalation of the contents of 1 or 2 blisters from FLOVENT DISKUS twice daily.
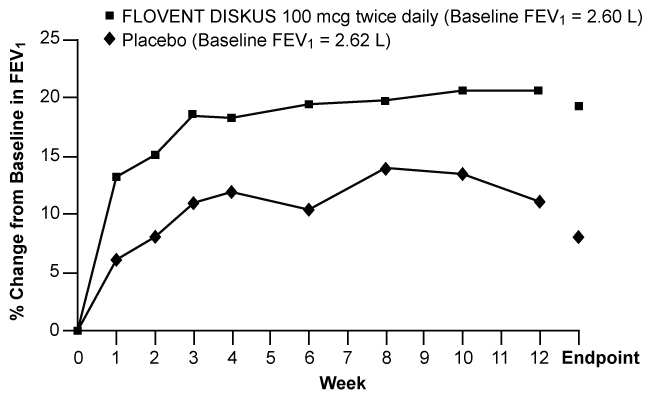
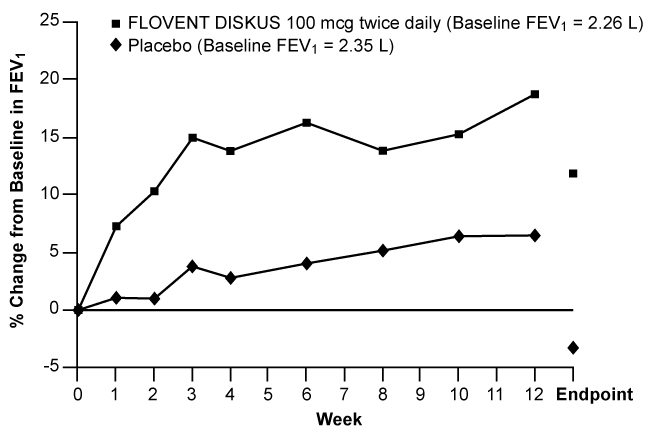
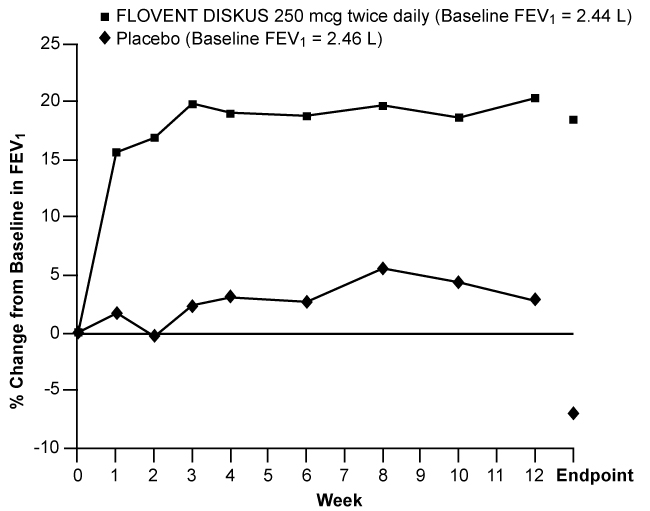
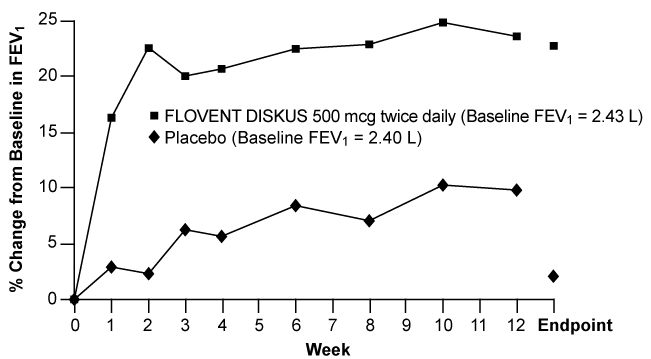
Figures 1 through 4 display results of pulmonary function tests (mean percent change from baseline in FEV1 prior to AM dose) for 3 recommended dosages of FLOVENT DISKUS (100, 250, and 500 mcg twice daily) and placebo from the four 12-week trials in adolescents and adults. These trials used predetermined criteria for lack of efficacy (indicators of worsening asthma), resulting in withdrawal of more patients in the placebo group. Therefore, pulmonary function results at Endpoint (the last evaluable FEV1 result, including most patients’ lung function data) are also displayed. Pulmonary function, as determined by percent change from baseline in FEV1 at recommended dosages of FLOVENT DISKUS improved significantly compared with placebo by the first week of treatment, and improvement was maintained for up to 1 year or more.
Figure 1. A 12-Week Clinical Trial Evaluating FLOVENT DISKUS 100 mcg Twice Daily in Adults and Adolescents Receiving Bronchodilators Alone
Figure 2. A 12-Week Clinical Trial Evaluating FLOVENT DISKUS 100 mcg Twice Daily in Adults and Adolescents Receiving Inhaled Corticosteroids
Figure 3. A 12-Week Clinical Trial Evaluating FLOVENT DISKUS 250 mcg Twice Daily in Adults and Adolescents Receiving Inhaled Corticosteroids or Bronchodilators Alone
Figure 4. A 12-Week Clinical Trial Evaluating FLOVENT DISKUS 500 mcg Twice Daily in Adults and Adolescents Receiving Inhaled Corticosteroids or Bronchodilators Alone
In all 4 efficacy trials, measures of pulmonary function (FEV1) were statistically significantly improved as compared with placebo at all twice-daily doses. Subjects on all dosages of FLOVENT DISKUS were also less likely to discontinue study participation due to asthma deterioration (as defined by predetermined criteria for lack of efficacy including lung function and subject-recorded variables such as AM PEF, albuterol use, and nighttime awakenings due to asthma) compared with placebo.
In a clinical trial of 111 subjects with severe asthma requiring chronic oral prednisone therapy (average baseline daily prednisone dose was 14 mg), fluticasone propionate given by inhalation powder at doses of 500 and 1,000 mcg twice daily was evaluated. Both doses enabled a statistically significantly larger percentage of subjects to wean from oral prednisone as compared with placebo (75% of the subjects on 500 mcg twice daily and 89% of the subjects on 1,000 mcg twice daily as compared with 9% of subjects on placebo). Accompanying the reduction in oral corticosteroid use, subjects treated with fluticasone propionate had significantly improved lung function and fewer asthma symptoms as compared with the placebo group.
14.2 Pediatric Subjects Aged 4 to 11 Years
A 12-week, placebo-controlled clinical trial was conducted in 437 pediatric subjects (177 received FLOVENT DISKUS), approximately half of whom were receiving ICS at baseline. In this trial, doses of fluticasone propionate inhalation powder 50 and 100 mcg twice daily significantly improved FEV1 (15% and 18% change from baseline at Endpoint, respectively) compared with placebo (7% change). AM PEF was also significantly improved with doses of fluticasone propionate 50 and 100 mcg twice daily (26% and 27% change from baseline at Endpoint, respectively) compared with placebo (14% change). In this trial, subjects on active treatment were significantly less likely to discontinue treatment due to asthma deterioration (as defined by predetermined criteria for lack of efficacy including lung function and subject-recorded variables such as AM PEF, albuterol use, and nighttime awakenings due to asthma).
Two other 12-week placebo-controlled clinical trials were conducted in 504 pediatric subjects with asthma, approximately half of whom were receiving ICS at baseline. In these trials, FLOVENT DISKUS was efficacious at doses of 50 and 100 mcg twice daily when compared with placebo on major endpoints including lung function and symptom scores. Pulmonary function improved significantly compared with placebo by the first week of treatment, and subjects treated with FLOVENT DISKUS were also less likely to discontinue trial participation due to asthma deterioration. One hundred ninety-two (192) subjects received FLOVENT DISKUS for up to 1 year during an open-label extension. Data from this open-label extension suggested that lung function improvements could be maintained up to 1 year.
- 16 HOW SUPPLIED/STORAGE AND HANDLING
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information and Instructions for Use).
Local Effects
Inform patients that localized infections with Candida albicans occurred in the mouth and pharynx in some patients. If oropharyngeal candidiasis develops, treat it with appropriate local or systemic (i.e., oral) antifungal therapy while still continuing therapy with FLOVENT DISKUS, but at times therapy with FLOVENT DISKUS may need to be temporarily interrupted under close medical supervision. Advise patients to rinse the mouth with water without swallowing after inhalation to help reduce the risk of thrush.
Status Asthmaticus and Acute Asthma Symptoms
Inform patients that FLOVENT DISKUS is not a bronchodilator and is not intended for use as rescue medicine for acute asthma exacerbations. Advise patients to treat acute asthma symptoms with an inhaled, short-acting beta2-agonist such as albuterol. Instruct patients to contact their physicians immediately if there is deterioration of their asthma.
Immunosuppression
Warn patients who are on immunosuppressant doses of corticosteroids to avoid exposure to chickenpox or measles and, if exposed, to consult their physicians without delay. Inform patients of potential worsening of existing tuberculosis; fungal, bacterial, viral, or parasitic infections; or ocular herpes simplex.
Hypercorticism and Adrenal Suppression
Advise patients that FLOVENT DISKUS may cause systemic corticosteroid effects of hypercorticism and adrenal suppression. Additionally, inform patients that deaths due to adrenal insufficiency have occurred during and after transfer from systemic corticosteroids. Patients should taper slowly from systemic corticosteroids if transferring to FLOVENT DISKUS.
Immediate Hypersensitivity Reactions
Advise patients that immediate hypersensitivity reactions (e.g., urticaria, angioedema, rash, bronchospasm, hypotension), including anaphylaxis, may occur after administration of FLOVENT DISKUS. Patients should discontinue FLOVENT DISKUS if such reactions occur. There have been reports of anaphylactic reactions in patients with severe milk protein allergy after inhalation of powder products containing lactose; therefore, patients with severe milk protein allergy should not take FLOVENT DISKUS.
Reduction in Bone Mineral Density
Advise patients who are at an increased risk for decreased BMD that the use of corticosteroids may pose an additional risk.
Reduced Growth Velocity
Inform patients that orally inhaled corticosteroids, including FLOVENT DISKUS, may cause a reduction in growth velocity when administered to pediatric patients. Physicians should closely follow the growth of children and adolescents taking corticosteroids by any route.
Glaucoma and Cataracts
Advise patients that long-term use of ICS may increase the risk of some eye problems (cataracts or glaucoma); consider regular eye examinations.
Use Daily for Best Effect
Patients should use FLOVENT DISKUS at regular intervals as directed. Individual patients will experience a variable time to onset and degree of symptom relief and the full benefit may not be achieved until treatment has been administered for 1 to 2 weeks or longer. Patients should not increase the prescribed dosage but should contact their physicians if symptoms do not improve or if the condition worsens. Instruct patients not to stop use of FLOVENT DISKUS abruptly. Patients should contact their physicians immediately if they discontinue use of FLOVENT DISKUS.
Trademarks are owned by or licensed to the GSK group of companies.
GlaxoSmithKline
Durham, NC 27701
©2023 GSK group of companies or its licensor.
FLD:16PI
-
PATIENT PACKAGE INSERT
PATIENT INFORMATION
FLOVENT DISKUS (FLO vent DISK us)
(fluticasone propionate inhalation powder)
for oral inhalation use
What is FLOVENT DISKUS?
FLOVENT DISKUS is a prescription inhaled corticosteroid (ICS) medicine used for the long-term treatment of asthma in people aged 4 years and older.
- ICS medicines such as fluticasone propionate help to decrease inflammation in the lungs. Inflammation in the lungs can lead to breathing problems.
- FLOVENT DISKUS is not used to relieve sudden breathing problems and will not replace a rescue inhaler.
- It is not known if FLOVENT DISKUS is safe and effective in children younger than 4 years of age.
Do not use FLOVENT DISKUS:
- to relieve sudden breathing problems.
- as a rescue inhaler.
- if you have a severe allergy to milk proteins. Ask your healthcare provider if you are not sure.
- if you are allergic to fluticasone propionate.
Before using FLOVENT DISKUS, tell your healthcare provider about all of your medical conditions, including if you:
- have liver problems.
- have weak bones (osteoporosis).
- have an immune system problem.
- have or have had eye problems, such as glaucoma, increased pressure in your eye, cataracts, or other changes in vision.
- are allergic to milk proteins.
- have any type of viral, bacterial, or fungal infection.
- are exposed to chickenpox or measles.
- are pregnant or plan to become pregnant. It is not known if FLOVENT DISKUS may harm your unborn baby.
- are breastfeeding. It is not known if the medicine in FLOVENT DISKUS passes into your milk and if it can harm your baby.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. FLOVENT DISKUS and certain other medicines may interact with each other. This may cause serious side effects. Especially tell your healthcare provider if you take antifungal or anti-HIV medicines.
Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.
How should I use FLOVENT DISKUS?
Read the step-by-step instructions for using FLOVENT DISKUS at the end of this Patient Information.
- Do not use FLOVENT DISKUS unless your healthcare provider has taught you how to use the inhaler and you understand how to use it correctly.
- Children should use FLOVENT DISKUS with an adult’s help, as instructed by the child’s healthcare provider.
- FLOVENT DISKUS comes in 3 different strengths. Your healthcare provider prescribed the strength that is best for you.
- Use FLOVENT DISKUS exactly as your healthcare provider tells you to use it. Do not use FLOVENT DISKUS more often than prescribed.
- It may take 1 to 2 weeks or longer after you start FLOVENT DISKUS for your asthma symptoms to get better. You must use FLOVENT DISKUS regularly.
- Do not stop using FLOVENT DISKUS, even if you are feeling better, unless your healthcare provider tells you to.
- If you miss a dose of FLOVENT DISKUS, just skip that dose. Take your next dose at your usual time. Do not take 2 doses at 1 time.
- FLOVENT DISKUS does not relieve sudden breathing problems. Always have a rescue inhaler with you to treat sudden symptoms. If you do not have a rescue inhaler, call your healthcare provider to have one prescribed for you.
- Rinse your mouth with water without swallowing after each dose of FLOVENT DISKUS. This will help lessen the chance of getting a yeast infection (thrush) in your mouth and throat.
- Call your healthcare provider or get medical care right away if:
- your breathing problems get worse.
- you need to use your rescue inhaler more often than usual.
- your rescue inhaler does not work as well to relieve your symptoms.
- you need to use 4 or more inhalations of your rescue inhaler in 24 hours for 2 or more days in a row.
- you use 1 whole canister of your rescue inhaler in 8 weeks.
- your peak flow meter results decrease. Your healthcare provider will tell you the numbers that are right for you.
What are the possible side effects of FLOVENT DISKUS?
FLOVENT DISKUS can cause serious side effects, including:
- fungal infection in your mouth or throat (thrush). Rinse your mouth with water without swallowing after using FLOVENT DISKUS to help reduce your chance of getting thrush.
- weakened immune system and increased chance of getting infections (immunosuppression).
- reduced adrenal function (adrenal insufficiency). Adrenal insufficiency is a condition where the adrenal glands do not make enough steroid hormones. This can happen when you stop taking oral corticosteroid medicines (such as prednisone) and start taking a medicine containing an inhaled steroid (such as FLOVENT DISKUS). During this transition period, when your body is under stress such as from fever, trauma (such as a car accident), infection, or surgery, adrenal insufficiency can get worse and may cause death.
- Symptoms of adrenal insufficiency include:
ο feeling tired ο nausea and vomiting
ο lack of energy ο low blood pressure (hypotension)
ο weakness
- serious allergic reactions. Call your healthcare provider or get emergency medical care if you get any of the following symptoms of a serious allergic reaction:
ο rash ο swelling of your face, mouth and tongue
ο hives ο breathing problems
- bone thinning or weakness (osteoporosis).
- slowed growth in children. Your child’s growth should be checked regularly by the healthcare provider while using FLOVENT DISKUS.
- eye problems including glaucoma, increased pressure in your eye, cataracts, or other changes in vision. You should have regular eye exams while using FLOVENT DISKUS.
- increased wheezing (bronchospasm). Increased wheezing can happen right away after using FLOVENT DISKUS. Always have a rescue inhaler with you to treat sudden wheezing.
Common side effects of FLOVENT DISKUS include:
upper respiratory tract infection fever nose irritation
throat irritation headache upset stomach
nausea and vomiting sinus irritation
persistent cough cough
These are not all the possible side effects of FLOVENT DISKUS.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store FLOVENT DISKUS?
- Store FLOVENT DISKUS at room temperature between 68°F and 77°F (20°C and 25°C). Keep in a dry place away from heat and sunlight.
- Store FLOVENT DISKUS in the unopened foil pouch and only open when ready for use.
- Safely throw away FLOVENT DISKUS 50 mcg in the trash 6 weeks after you open the foil pouch or when the counter reads 0, whichever comes first.
- Safely throw away FLOVENT DISKUS 100 mcg and FLOVENT DISKUS 250 mcg in the trash 2 months after you open the foil pouch or when the counter reads 0, whichever comes first.
Keep FLOVENT DISKUS and all medicines out of the reach of children.
General information about the safe and effective use of FLOVENT DISKUS.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use FLOVENT DISKUS for a condition for which it was not prescribed. Do not give FLOVENT DISKUS to other people, even if they have the same symptoms that you have. It may harm them.
You can ask your healthcare provider or pharmacist for information about FLOVENT DISKUS that is written for health professionals.
What are the ingredients in FLOVENT DISKUS?
Active ingredient: fluticasone propionate
Inactive ingredient: lactose monohydrate (contains milk proteins)
For more information about FLOVENT DISKUS, call 1-888-825-5249.
Trademarks are owned by or licensed to the GSK group of companies.
GlaxoSmithKline, Durham, NC 27701
©2023 GSK group of companies or its licensor.
FLD:11PIL
- This Patient Information has been approved by the U.S. Food and Drug Administration Revised: August 2023
- fluticasone propionate
-
INGREDIENTS AND APPEARANCE
FLOVENT DISKUS
fluticasone propionate powder, meteredProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 50090-1245(NDC:0173-0600) Route of Administration RESPIRATORY (INHALATION) Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength FLUTICASONE PROPIONATE (UNII: O2GMZ0LF5W) (FLUTICASONE - UNII:CUT2W21N7U) FLUTICASONE PROPIONATE 50 ug Inactive Ingredients Ingredient Name Strength LACTOSE, UNSPECIFIED FORM (UNII: J2B2A4N98G) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 50090-1245-0 1 in 1 CARTON 11/28/2014 1 60 in 1 INHALER; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020833 05/08/2007 Labeler - A-S Medication Solutions (830016429) Establishment Name Address ID/FEI Business Operations A-S Medication Solutions 830016429 RELABEL(50090-1245)
Trademark Results [FLOVENT]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 FLOVENT 86010358 5047604 Live/Registered |
Levi's Nails & Screws, LP 2013-07-15 |
 FLOVENT 74396966 1864506 Live/Registered |
GLAXO GROUP LIMITED 1993-05-28 |
 FLOVENT 74209704 1779546 Live/Registered |
MENTOR GRAPHICS CORPORATION 1991-10-07 |
 FLOVENT 74109511 not registered Dead/Abandoned |
GLAXO GROUP LIMITED 1990-10-26 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.