FLAXSEED injection, solution COFFEE injection, solution COTTONSEED injection, solution
Cottonseed by
Drug Labeling and Warnings
Cottonseed by is a Prescription medication manufactured, distributed, or labeled by Antigen Laboratories, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
BOXED WARNING
(What is this?)
WARNINGS
Allergenic extract is intended for use by physicians or under the guidance of physicians who are experienced in the administration of allergenic extracts for diagnosis and the emergency care of anaphylaxis. This extract is not directly interchangeable with other allergenic extracts. Patients should be instructed to recognize adverse reaction symptoms and cautioned to contact the physician's office if reaction symptoms occur. As with all allergenic extracts, severe systemic reactions may occur.In certain individuals, especially in steroid-dependent/unstable asthmatics, these life-threatening reactions may result in death.Patients should be observed for at least 20 minutes following testing. Emergency measures, as well as trained personnel, should be immediately available in the event of a life-threatening reaction.
This product should not be injected intravenously. See the "WARNINGS", "PRECAUTIONS", "ADVERSE REACTIONS" and "OVERDOSAGE" sections.
Sensitive patients may experience severe anaphylactic reactions resulting in respiratory obstruction, shock, coma and/or death.
Report serious adverse events to MedWatch, 5600 Fishers Lane, Rockville, MD 20852-9787, phone 1-800-FDA-1088.
Patients receiving beta-blockers may not be responsive to epinephrine or inhaled bronchodilators.Respiratory obstruction not responding to parenteral or inhaled bronchodilators may require theophylline, oxygen, intubation and the use of life support systems. Parenteral fluid and/or plasma expanders may be utilized for treatment of shock. Adrenocorticosteroids may be administered parenterally or intravenously. Refer to ''WARNINGS", "PRECAUTIONS" and "ADVERSE REACTIONS" sections below.
-
DESCRIPTION
Antigen Laboratories' allergenic extracts are manufactured from source material listed on the vial label. The extract is a sterile solution containing extractables of source materials obtained from biological collecting and/or processing firms. All source materials are inspected by Antigen Laboratories' technical personnel in accordance with 21 CFR 680.1 (b) (I).
The following "For Diagnostic Use Only" allergenic extracts are extracted at a 1:20 w/v or 1:50 w/v ratio of source material to extracting fluid:
The source material for Coffee is prepared by grinding the seed of the coffee plant (Coffea arabic).
The source material for Cottonseed is prepared by grinding the seed of the cotton plant (Gossypium spp.).
The source material for Flaxseed is prepared by grinding the seed of the flax plant (Linum usitatissimum).
Leafhopper source material is pulverized whole bodies of Leafhoppers (Cicadellidae).
Miller Moth source material is pulverized whole bodies of night flying moths (Lepidoptera).
Cricket source material is pulverized whole bodies of crickets (Gryllidae).
Moth source material is pulverized whole bodies of moths of the order Frenatae.
The routes of administration for diagnostic purposes are intradermal or prick-puncture of the skin.
FOR ALLERGENIC EXTRACTS CONTAINING 50% V/V GLYCERINE AS PRESERVATIVE AND STABILIZER:
Sodium chloride……………………………………………………………………...0.95%
Sodium bicarbonate………………………………………………………………….0.24%
USP Glycerine…………………………………………………………………50% (v/v)
Water for Injection…………………………………………………………q.s. to volume
Active allergens are described by common and scientific name on the stock concentrate container label.
-
CLINICAL PHARMACOLOGY
Studies indicate allergic individuals produce immunoglobulins of the IgE class in response to exposure to allergens. Subsequent exposure to the same allergen results in a complex of allergen with IgE antibody fixed on mast cells or basophil membranes. This cross-linking results in stimulation of mast cells which leads to release and generation of pharmacologically active substances that produce immediate hypersensitivity reaction.1
-
INDICATIONS AND USAGE
FOR DIAGNOSTIC USE ONLY. This product has not been shown by adequate data to be safe and effective for therapeutic use according to Federal Register Notice dated November 16, 1994, Vol. 59, No. 220. The following allergenic extracts are "For Diagnostic Use Only": Coffee (Coffea arabic), Cottonseed (Gossypium spp.), Flaxseed (Linum usitatissimum), Leafhopper (Cicadellidae), Miller Moth (Night Flying Lepidoptera), Cricket (Gryllidae) and Moth (Frenatae). These extracts are intended for diagnostic testing of patients whose histories indicate that upon natural exposure to the allergen, they experience allergic symptoms. Confirmation is determined by skin testing.
-
CONTRAINDICATIONS
Do not administer in the presence of diseases characterized by bleeding diathesis. Individuals with autoimmune disease may be at risk of exacerbating symptoms of the underlying condition, possibly due to routine immunization. Children with nephrotic syndrome should not receive injections due to immunization exacerbating nephrotic diseases.
Allergenic extracts are not intended for diagnosing patients who do not manifest immediate hypersensitivity reactions to the allergenic extract when skin tested.
-
WARNINGS
Extreme caution is necessary when using diagnostic skin tests in highly sensitive patients who have experienced severe symptoms or anaphylaxis by natural exposure or previous skin testing or treatment. IN THESE CASES THE POTENCY FOR SKIN TESTS MUST BE ADJUSTED TO THE PATIENT'S SENSITIVITY AND TOLERANCE. Refer to boxed “WARNINGS" and “OVERDOSAGE" sections.
Epinephrine 1:1000 should be available when a new lot of allergenic extract is utilized. Patient re-evaluation may be necessary. Injections should never be given intravenously. Adverse reactions to allergenic extracts are usually apparent within 20-30 minutes following skin testing. Patients should be observed for 20-30 minutes after skin testing.
-
PRECAUTIONS
Sterile solutions, vials, syringes, etc. must be used. Aseptic technique should be observed in making dilutions for skin testing.
Observe caution in making test injection to minimize adverse reactions. The usual precautions in administering allergenic extracts are necessary (refer to boxed "WARNINGS" and "OVERDOSAGE" sections). A disposable, sterile syringe and needle should be used for each individual patient to prevent transmission of serum hepatitis, Human Immunodeficiency Virus (HIV) and other infectious agents.
It cannot be overemphasized that, under certain unpredictable combinations of circumstances, anaphylactic shock is always a possibility. Other possible systemic reaction symptoms are, in varying degrees of severity: fainting, pallor, bradycardia, hypotension, angioedema, cough, wheezing, conjunctivitis, rhinitis, and urticaria.4,5
With careful attention to administration, such reactions occur infrequently, but it must be remembered that allergenic extracts are highly potent to sensitive individuals and overdose could result in anaphylactic symptoms. Therefore, it is imperative that physicians administering allergenic extracts understand and be prepared for the treatment of severe reactions.
Refer to "OVERDOSAGE" section for a description of the treatment of anaphylactic reactions.
Patients should remain under observation of nurse, physician, or other personnel trained in emergency measures for at least 20 minutes following testing. Any adverse reactions during or after leaving the office should be reported to the physician or their qualified personnel.
Carcinogenesis, Mutagenesis, Impairment of Fertility:
Long term studies in animals have not been conducted with allergenic extract to determine their potential for carcinogenicity, mutagenicity or impairment of fertility.
Animal reproduction studies have not been conducted with allergenic extracts. It is not known whether allergenic extracts cause fetal harm during pregnancy or affect reproductive capacity. A systemic reaction to allergenic extract could cause uterine contractions leading to spontaneous abortion or premature labor. Allergenic extracts should be used during pregnancy only if potential benefit justifies potential risk to fetus.3
It is not known whether allergenic extracts are excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when allergenic extracts are administered to a nursing woman.
Allergenic extracts have been used routinely in children, and no special safety problems or specific hazards have been found.7,8
Antihistamines. Antihistamines inhibit the wheal and flare reaction. The inhibitory effect of conventional antihistamines varies from 1 day up to 10 days, according to the drug and patient's sensitivity. Long acting antihistamines (e.g., astemizole) may inhibit the wheal and flare for up to forty days.
Imipramines, phenothiazines, and tranquilizers. Tricyclic antidepressants exert a potent and sustained decrease of skin reactions to histamine that may last for a few weeks. Tranquilizers and antiemetic agents of the phenothiazine class have H1 antihistaminic activity and can block skin tests.2
Corticosteroids. Short-term (less than 1 week) administration of corticosteroids at the therapeutic doses used in asthmatic patients does not modify the cutaneous reactivity to histamine, compound 48/80, or allergen. Long-term corticosteroid therapy modifies the skin texture and makes the interpretation of immediate skin tests more difftcult.2
Theophylline. It appears that theophylline need not be stopped prior to skin testing. 2
Beta-adrenergic agents. Inhaled beta2 agonists in the routine doses for the treatment of asthma do not usually inhibit allergen-induced skin tests. However, oral terbutaline and parenteral ephedrine were shown to decrease the allergen-induced wheal.2
Cromolyn. Cromolyn inhaled or injected prior to skin tests with allergens or degranulating agents does not alter the skin whealing response.2
Other drugs. Other drugs have been shown to decrease skin test reactivity. Among them, dopamine is the best-documented compound.2
-
ADVERSE REACTIONS
Adverse reactions include, but are not necessarily limited to urticaria, itching, edema of the extremities, respiratory wheezing or asthma, dyspnea, cyanosis, tachycardia, lacrimation, marked perspiration, flushing of the face, neck or upper chest, mild persistent clearing of the throat, hacking cough or persistent sneezing.
A small amount of erythema and swelling at the site of injection is common, the extent varying with the patient. Such reactions should not be considered significant unless they persist for at least 24 hours or exceed 50 mm in diameter.
Large, persistent local reactions or minor exacerbations of the patient's allergic symptoms may be treated by local cold applications and/or the use of oral antihistamines, but they should be considered a warning of possible severe systemic reactions.
A mild burning immediately after the injection is to be expected; this usually is relieved in 10-20 seconds.
Systemic reactions may range from mild exaggeration of the patient's allergic symptoms to anaphylactic reactions. Very sensitive patients may show a rapid response. In some instances, a severe systemic reaction with blood pressure fall and/or shock may occur. Quantitation of patient's sensitivity combined with careful early observation is essential for safe skin testing.9
Patients receiving beta-blockers may not be responsive to epinephrine or inhaled bronchodilators. The following are commonly prescribed beta-blockers: Levatol, Lopressor, Propanolol Intersol, Propanolol HCL, Blocadren, Propanolol, Inderal-LA, Visken, Corgard, Ipran, Tenormin, Timoptic. Ophthalmic beta-blockers: Betaxolol, Levobunolol, Timolol, Timoptic. Chemicals that are beta-blockers and may be components of other drugs: Acebutolol, Atenolol, Esmolol, Metoprolol, Nadolol, Penbutolol, Pindolol, Propanolol, Timolol, Labetalol, Carteolol.
-
OVERDOSAGE
Refer to “WARNINGS," "PRECAUTIONS" and "ADVERSE REACTIONS" sections for signs and symptoms of an overdose.
If a systemic or anaphylactic reaction does occur, the first treatment should be injection intramuscularly or subcutaneously 0.3 to 0.5 ml of 1:1000 epinephrine-hydrochloride into the opposite arm or gluteal area. Apply tourniquet above site of allergenic extract injection and loosen briefly at 5 minute intervals to prevent circulatory impairment. If oxygen is indicated, it may be administered by nasal cannula or ambu bag.
The epinephrine HCL 1:1000 dose for infants to 2 years is 0.05 to 0.1 ml; for children 2 to 6 years it is 0.15 ml; for children 6 to 12 years it is 0.2 ml.
Symptoms of progressive anaphylaxis include airway obstruction and/or vascular collapse.
After administration of epinephrine, profound shock and vasomotor collapse should be treated with intravenous fluids and possibly vasoactive drugs. Monitor airways for obstruction. Oxygen should be given by mask if indicated.
Antihistamines, H2 antagonist, bronchodilators, steroids and theophylline may be used as indicated after giving adequate epinephrine and circulatory support.6
Patients who have been taking a beta-blocker may be unresponsive to epinephrine. Epinephrine or beta-adrenergic drugs (Alupent) may be ineffective. These drugs should be administered even though a beta-blocker may have been taken. The following treatment will be effective whether or not patient is taking a beta-blocker: Aminophylline IV, slow push or drip, Atrovent (Ipratropium bromide) Inhaler, 3 inhalations repeated, Atropine, 0.4 mg/ml, 0.75 to 1.5 ml IM or IV, Solu-Cortef, 100-200 mg IM or IV, Solu-Medrol, 125 mg IM or IV, Glucagon, 0.5-1 mg IM or IV, Benadryl, 50 mg IM or IV, Cimetidine, 300 mg IM or IV, Oxygen via ambu bag.
-
DOSAGE AND ADMINISTRATION
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Some allergenic extracts naturally precipitate. This allergenic extract is "For Diagnostic Use Only". (Refer to STORAGE section.)
PRICK-PUNCTURE TESTING: To identify highly sensitive individuals and as a safety precaution, it is recommended that a prick-puncture test using a drop of the extract concentrate be performed prior to initiating very dilute intradermal testing. Prick-puncture testing is performed by placing a drop of extract concentrate on the skin and puncturing the skin through the drop with a small needle such as a bifurcated vaccinating needle. The most satisfactory sites on the back for skin testing are from the posterior axillary fold to 2.5 cm from the spinal column, and from the top of the scapula to the lower rib margins. The best areas on the arms are the volar surfaces from the axilla to 2.5 or 5 cm above the wrist, skipping the anticubital space. Skin testing should include a positive control of histamine phosphate and a negative control of 50% v/v glycerine in buffered saline. A positive reaction is approximately 10-15 mm erythema with 2.5 mm wheal. Smaller, less conclusive reactions may be considered positive in conjunction with a definitive history of symptoms on exposure to the allergen. Less sensitive individuals can be tested intradermally with an appropriately diluted extract (See "INTRADERMAL TESTING").
INTRADERMAL TESTING: The surface of the upper and lower arm is the usual location for skin testing. A sterile, disposable syringe and needle is used for each extract tested. Intracutaneous test dilutions, five-fold or ten-fold, may be prepared from stock concentrate using physiologic saline as a diluent. (1) Start testing with the most dilute allergenic extract concentration. (2) A volume of 0.02-0.05 ml should be injected slowly into the superficial skin layers making a small bleb (superficial wheal). (3) For patients without a history of extreme sensitivity, or a negative or weakly reactive prick-puncture test, the initial dilution for skin testing should be at least 1:12,500 w/v. This initial dilution can be prepared by diluting 1:20 to 1:50 w/v (2%-5%) extracts five-fold to 5-4 or 1:10 w/v (10%) extracts to 5-5. Dilute 1:10 w/v (10%) extracts to 10-3 if using ten-fold dilutions. (4) Sensitive patients with a positive prick-puncture test require a further dilution to at least 1:312,500 w/v. This dilution can be prepared by diluting 1:20 to 1:50 w/v (2%-5%) extracts to 5-6 or 1:10 w/v (10%) extracts to 5-7 (five-fold dilutions). Ten-fold dilution to 10-6 of a 1:10 w/v (10%) extract would be a safe starting dilution. For interpretation of skin reactions, refer to chart below. If after 20 minutes no skin reaction is observed, continue testing using increasing increments of the concentration until a reaction of 5-10 mm wheal and 11-30 mm erythema is obtained, or a concentration of 5-2 or 10-1 has been tested. A negative control, 50% glycerine diluted with diluent to 5-2 (1:25) or 10-1 (1:10) dilution and a positive control of histamine phosphate, should be tested and included in interpretation of skin reactions.2,4
GRADE mm ERYTHEMA mm WHEAL 0 less than 5 less than 5 ± 5-10 5-10 1+ 11-20 5-10 2+ 21-30 5-10 3+ 31-40 10-15 or with pseudopods 4+ greater than 40 greater than 15 or with many pseudopods INTRADERMAL TESTING–SKIN ENDPOINT TITRATION: The allergenic extracts to which the patient is sensitive and the patient's degree of sensitivity can be determined through the use of intracutaneous skin tests involving progressive five-fold dilutions of allergenic extracts. Intracutaneously inject 0.01 to 0.02 ml of the test allergen to form a 4 mm diameter superficial skin wheal. For patients demonstrating a negative or weakly reactive prick-puncture skin test, an initial screening dilution of 1:12,500 w/v is safe. For patients demonstrating a positive prick-puncture skin test, an initial screening dilution of 1:312,500 w/v is safe (see "Serial Dilution Titration Test Dilutions" chart below).When a sequence of five-fold or ten-fold dilutions of an allergen is injected, the endpoint is determined by noting the dilution that first produces a wheal or erythema (15 minutes after injection) that is 2 mm larger than wheals with erythema produced by weaker, non-reacting dilutions (5 mm negative wheal).
SERIAL DILUTION TITRATION TEST DILUTIONS APPROXIMATE ALLERGENIC EXTRACT CONCENTRATION RESULTING FROM 1:5 DILUTION Titration Number Dilution Exponent Weight / Volume Allergenic Extract Concentrate 1:50 (2%) 1:40 (2 1/2%) 1:33 1/3 (3%) 1:20 (5%) 1:10 (10%) No. 1 5-1 1:5 1:250 1:200 1:167 1:100 1:50 No. 2 5-2 1:25 1:1,250 1:1,000 1:835 1:500 1:250 No. 3 5-3 1:125 1:6,250 1:5,000 1:4,175 1:2,500 1:1,250 No. 4 5-4 1:625 1:31,250 1:25,000 1:20,875 1:12,500 1:6,250 No. 5 5-5 1:3,125 1:156,250 1:125,000 1:104,375 1:62,500 1:31,250 No. 6 5-6 1:15,625 1:781,250 1:625,000 1:521,875 1:312,500 1:156,250 No. 7 5-7 1:78,125 1:3,906,250 1:3,125,000 1:2,609,375 1:1,562,500 1:781,250 No. 8 5-8 1:390,625 1:19,531,250 1:15,625,000 1:13,046,875 1:7,812,500 1:3,906,250 No. 9 5-9 1:1,953,125 1:97,656,250 1:78,125,000 1:65,234,375 1:39,062,500 1:19,531,250 No. 10 5-10 1:9,765,625 1:488,281,250 1:390,625,000 1:326,171,875 1:195,312,500 1:97,656,250 No. 11 5-11 1:48,828,125 1:2,441,406,250 1:1,953,125,000 1:1,630,859,375 1:976,562,500 1:488,281,250 No. 12 5-12 1:244,140,625 1:12,207,031,250 1:9,765,625,000 1:8,154,296,875 1:4,882,812,500 1:2,441,406,250 -
HOW SUPPLIED
The stock concentrate of allergenic extract is expressed in weight/volume, at 1:50 w/v (2%) or 1:20 w/v (5%). It is supplied in 10, 30 and 50 ml containers. Extracts in 5 ml sterile dropper bottles are available for prick-puncture testing. To insure maximum potency for the entire dating period, all stock concentrates contain 50% glycerine v/v.
-
STORAGE
Store all stock concentrates and dilutions at 2-8 degrees C and keep at this temperature during office use. The expiration date of the allergenic extract is listed on the container label. Dilutions of the allergenic extract concentration containing less then 50% glycerine are less stable. If loss of potency is suspected, potency can be checked using side by side skin testing with freshly prepared dilutions of equal concentration on individuals with known sensitivity to the allergen.
-
REFERENCES
1. Holgate, S.T., Robinson, C., Church, Mike: Mediators of Immediate Hypersensitivity, Third Edition, Allergy Principles and Practice, C.V. Mosby Co., Vol. I and II, pp 135-163, 1988.
2. Bousquet, Jean: "In vivo methods for study of allergy: Skin tests" Third Edition, Allergy Principles and Practice, C.V. Mosby Co., Vol. I and II, pp. 419-436, 1988.
3. Seebohm, P.M., et al: Panel on Review of Allergenic Extracts, Final Report, Food and Drug Administration, March 13, 1981, pp. 9-48.
4. Van Metre, T., Adkinson, N., Amodio, F., Lichtenstein, L., Mardinay, M., Norman, P., Rosenberg, G., Sobotka, A., Valentine, M.: "A Comparative Study of the Effectiveness of the Rinkel Method and the Current Standard Method of Immunology for Ragweed Pollen Hay Fever," The Journal of Clinical Allergy and Immunology, Vol. 66, No. 6, pg. 511, December 1980.
5. Wasserman, S.: The Mast Cell and the Inflammatory Response. The Mast CeIl–its role in health and disease. Edited by J. Pepys & A.M. Edwards, Proceedings of an International Symposium, Davos, Switzerland, Pitman Medical Publishing Co., 1979, pp. 9-20.
6. Wasserman, S., Marquart, D.: Anaphylaxis, Third Edition, Allergy Principles and Practice, Vol. I, Chapter 58, p. 1365, edited by Middleton et al.
7. Bullock, J., Frick, O.: Mite Sensitivity in House Dust Allergic Children, Am. J. Dis. Child.,pp. 123-222,1972.
8. Willoughby, J.W.: Inhalant Allergy Immunotherapy with Standardized and Nonstandardized Allergenic Extracts, American Academy of Otolaryngology-Head and Neck Surgery:
Instructional Courses, Vol. 1, Chapter 15, C.V. Mosby Co., St. Louis, Missouri, September 1988.
9. Reid, Michael J., Lockey, Richard F., Turkeltaub M.D., Paul C., Platts-Mills, Thomas: "Survey of Fatalities From Skin Testing and Immunotherapy 1985-1989," Journal of Allergy and Clinical Immunology, Vol. 92, No.1, pp. 6-15, 1993.
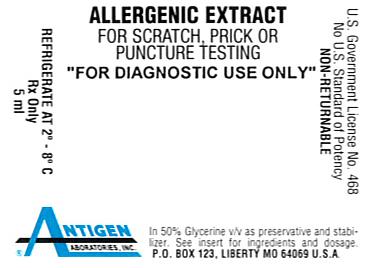
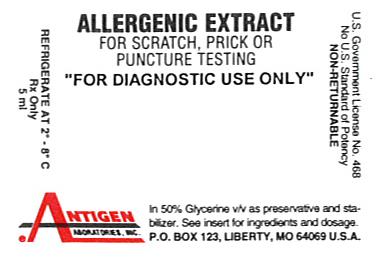
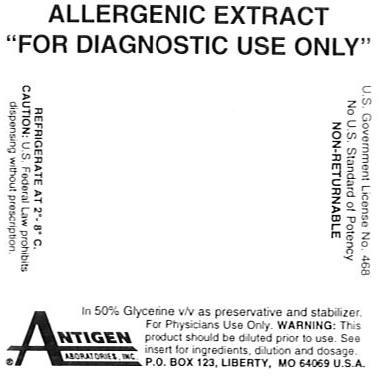
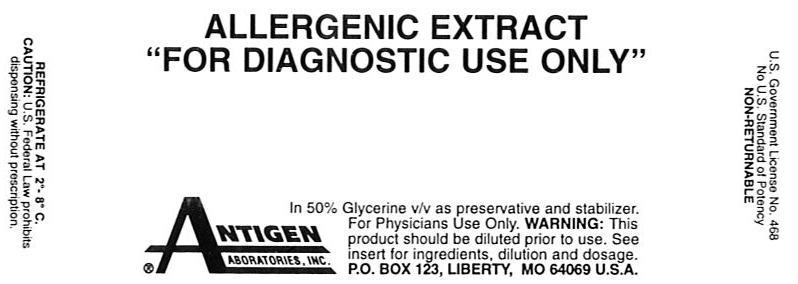
- CONTAINER LABELING
-
INGREDIENTS AND APPEARANCE
FLAXSEED
flaxseed injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 49288-0201 Route of Administration INTRADERMAL, SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength FLAX SEED (UNII: 4110YT348C) (FLAX SEED - UNII:4110YT348C) FLAX SEED 0.05 g in 1 mL Inactive Ingredients Ingredient Name Strength GLYCERIN (UNII: PDC6A3C0OX) 0.525 mL in 1 mL SODIUM CHLORIDE (UNII: 451W47IQ8X) 0.0095 g in 1 mL SODIUM BICARBONATE (UNII: 8MDF5V39QO) 0.0024 g in 1 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 49288-0201-1 2 mL in 1 VIAL, MULTI-DOSE 2 NDC: 49288-0201-2 5 mL in 1 VIAL, MULTI-DOSE 3 NDC: 49288-0201-3 10 mL in 1 VIAL, MULTI-DOSE 4 NDC: 49288-0201-4 30 mL in 1 VIAL, MULTI-DOSE 5 NDC: 49288-0201-5 50 mL in 1 VIAL, MULTI-DOSE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA102223 03/23/1974 COFFEE
coffee injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 49288-0100 Route of Administration INTRADERMAL, SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ARABICA COFFEE BEAN (UNII: 3SW678MX72) (ARABICA COFFEE BEAN - UNII:3SW678MX72) ARABICA COFFEE BEAN 0.05 g in 1 mL Inactive Ingredients Ingredient Name Strength GLYCERIN (UNII: PDC6A3C0OX) 0.525 mL in 1 mL SODIUM BICARBONATE (UNII: 8MDF5V39QO) 0.0024 g in 1 mL SODIUM CHLORIDE (UNII: 451W47IQ8X) 0.0095 g in 1 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 49288-0100-1 2 mL in 1 VIAL, MULTI-DOSE 2 NDC: 49288-0100-2 5 mL in 1 VIAL, MULTI-DOSE 3 NDC: 49288-0100-3 10 mL in 1 VIAL, MULTI-DOSE 4 NDC: 49288-0100-4 30 mL in 1 VIAL, MULTI-DOSE 5 NDC: 49288-0100-5 50 mL in 1 VIAL, MULTI-DOSE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA102223 03/23/1974 COTTONSEED
cottonseed injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 49288-0116 Route of Administration INTRADERMAL, SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength COTTON SEED (UNII: DI0ZRJ0MXN) (COTTON SEED - UNII:DI0ZRJ0MXN) COTTON SEED 0.05 g in 1 mL Inactive Ingredients Ingredient Name Strength GLYCERIN (UNII: PDC6A3C0OX) 0.525 mL in 1 mL SODIUM CHLORIDE (UNII: 451W47IQ8X) 0.0095 g in 1 mL SODIUM BICARBONATE (UNII: 8MDF5V39QO) 0.0024 g in 1 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 49288-0116-1 2 mL in 1 VIAL, MULTI-DOSE 2 NDC: 49288-0116-2 5 mL in 1 VIAL, MULTI-DOSE 3 NDC: 49288-0116-3 10 mL in 1 VIAL, MULTI-DOSE 4 NDC: 49288-0116-4 30 mL in 1 VIAL, MULTI-DOSE 5 NDC: 49288-0116-5 50 mL in 1 VIAL, MULTI-DOSE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA102223 03/23/1974 Labeler - Antigen Laboratories, Inc. (030705628) Registrant - Antigen Laboratories, Inc. (030705628) Establishment Name Address ID/FEI Business Operations Antigen Laboratories, Inc. 030705628 manufacture
Trademark Results [Cottonseed]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 COTTONSEED 77014268 3284376 Dead/Cancelled |
CottonSeed Clothing Company, LLC 2006-10-05 |
 COTTONSEED 75228385 2134227 Dead/Cancelled |
Club West Casual Wear, Inc. 1997-01-21 |
 COTTONSEED 73755672 1559914 Dead/Cancelled |
CLUB WEST CASUAL WEAR, INC. 1988-10-03 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.