CLOBETASOL PROPIONATE aerosol, foam
Clobetasol Propionate by
Drug Labeling and Warnings
Clobetasol Propionate by is a Prescription medication manufactured, distributed, or labeled by Mylan Pharmaceuticals Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use CLOBETASOL PROPIONATE FOAM safely and effectively. See full prescribing information for CLOBETASOL PROPIONATE FOAM.
CLOBETASOL PROPIONATE foam, 0.05%
For topical use
Initial U.S. Approval: 1985RECENT MAJOR CHANGES
Warnings and Precautions, Ophthalmic Adverse Reactions (5.3) 5/2018
INDICATIONS AND USAGE
- Clobetasol propionate foam is a corticosteroid indicated for the treatment of inflammatory and pruritic manifestations of corticosteroid-responsive dermatoses in patients aged 12 years and older. (1)
DOSAGE AND ADMINISTRATION
Clobetasol propionate foam is not for oral, ophthalmic, or intravaginal use. (2)
DOSAGE FORMS AND STRENGTHS
Foam, 0.05%. (3)
CONTRAINDICATIONS
None. (4)
WARNINGS AND PRECAUTIONS
- Clobetasol propionate foam has been shown to suppress the HPA axis. Systemic absorption of clobetasol propionate foam may produce reversible HPA axis suppression, Cushing’s syndrome, hyperglycemia, and unmask latent diabetes. (5.1)
- Because of the potential for systemic absorption, use of topical corticosteroids may require that patients be periodically evaluated for HPA axis suppression. (5.1)
- Modify use should HPA axis suppression develop. (5.1)
- High potency corticosteroids, large treatment surface areas, prolonged use, use of occlusive dressings, altered skin barrier, and liver failure may predispose patients to HPA axis suppression. (5.1)
- May increase the risk of cataract and glaucoma. If visual symptoms occur, consider referral to an ophthalmologist for evaluation. (5.3)
- Pediatric patients may be more susceptible to systemic toxicity when treated with topical corticosteroids. (5.1, 8.4)
- The propellant in clobetasol propionate foam is flammable. Avoid fire, flame, or smoking during and immediately following application. (5.5)
ADVERSE REACTIONS
- The most common adverse reactions (incidence ≥ 1%) are application site atrophy and application site reaction. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Mylan at 1-877-446-3679 (1-877-4-INFO-RX) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 5/2018
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Effects on Endocrine System
5.2 Local Adverse Reactions with Topical Corticosteroids
5.3 Ophthalmic Adverse Reactions
5.4 Concomitant Skin Infections
5.5 Flammable Contents
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
- Apply a thin layer of clobetasol propionate foam to the affected area(s) twice daily, morning and evening, for up to 2 consecutive weeks; therapy should be discontinued when control has been achieved.
- The maximum weekly dose should not exceed 50 g or an amount greater than 21 capfuls per week.
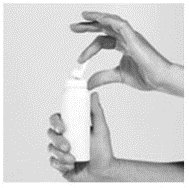
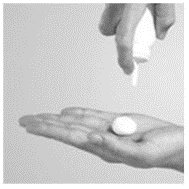
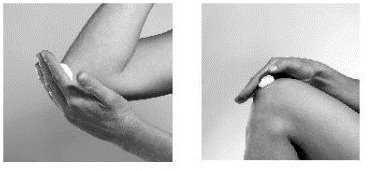
- For proper dispensing of foam, shake the can, hold it upside down, and depress the actuator.
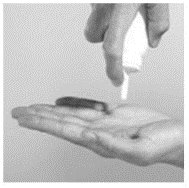
- Dispense a small amount of foam (about a capful) and gently massage the medication into the affected areas (excluding the face, groin, and axillae) until the foam is absorbed.
- Clobetasol propionate foam is not for oral, ophthalmic, or intravaginal use.
- Avoid contact with the eyes.
- Avoid use on face, axillae, and groin, or if skin atrophy is present at the treatment site.
- Wash hands after each application.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Effects on Endocrine System
Clobetasol propionate foam has been shown to suppress the hypothalamic-pituitary-adrenal (HPA) axis.
Systemic absorption of clobetasol propionate has caused reversible HPA axis suppression with the potential for clinical glucocorticoid insufficiency. This may occur during treatment or upon withdrawal of the topical corticosteroid. Use of clobetasol propionate foam for longer than 2 weeks may suppress the immune system [see Nonclinical Toxicology (13.1)].
In a trial including 37 subjects ages 12 years and older with atopic dermatitis of at least 30% body surface area (BSA), adrenal suppression was identified in 6 out of 37 subjects (16.2%) after 2 weeks of treatment with clobetasol propionate [see Clinical Pharmacology (12.2)].
Because of the potential for systemic absorption, use of clobetasol propionate may require that patients be periodically evaluated for HPA axis suppression. Factors that predispose a patient using a topical corticosteroid to HPA axis suppression include the use of more potent steroids, use over large surface areas, use over prolonged periods, use under occlusion, use on an altered skin barrier, and use in patients with liver failure.
An adrenocorticotrophic hormone (ACTH) stimulation test may be helpful in evaluating patients for HPA axis suppression. If HPA axis suppression is documented, an attempt should be made to gradually withdraw the drug, to reduce the frequency of application, or to substitute a less potent steroid. Manifestations of adrenal insufficiency may require systemic corticosteroids. Recovery of HPA axis function is generally prompt and complete upon discontinuation of topical corticosteroids.
Cushing’s syndrome, hyperglycemia, and unmasking of latent diabetes mellitus can also result from systemic absorption of topical corticosteroids.
Use of more than 1 corticosteroid-containing product at the same time may increase the total systemic corticosteroid exposure.
Pediatric patients may be more susceptible to systemic toxicity from equivalent doses because of their larger skin surface-to-body mass ratios [see Use in Specific Populations (8.4)].
5.2 Local Adverse Reactions with Topical Corticosteroids
Local adverse reactions may be more likely to occur with occlusive use, prolonged use, or use of higher potency corticosteroids. Reactions may include atrophy, striae, telangiectasias, burning, itching, irritation, dryness, folliculitis, acneiform eruptions, hypopigmentation, perioral dermatitis, allergic contact dermatitis, secondary infection, and miliaria. Some local adverse reactions may be irreversible.
Allergic contact dermatitis to any component of topical corticosteroids is usually diagnosed by a failure to heal rather than a clinical exacerbation. Clinical diagnosis of allergic contact dermatitis can be confirmed by patch testing.
If irritation develops, treatment with clobetasol propionate foam should be discontinued and appropriate therapy instituted.
5.3 Ophthalmic Adverse Reactions
Use of topical corticosteroids, including clobetasol propionate foam, may increase the risk of posterior subcapsular cataracts and glaucoma. Cataracts and glaucoma have been reported postmarketing with the use of topical corticosteroids, including topical clobetasol products [see Adverse Reactions (6.2)].
Avoid contact of clobetasol propionate foam with eyes. Advise patients to report any visual symptoms and consider referral to an ophthalmologist for evaluation.
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed in greater detail in other sections of the labeling:
- Effects on Endocrine System [see Warnings and Precautions (5.1)]
- Ophthalmic Adverse Reactions [see Warnings and Precautions (5.3)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
In controlled clinical trials involving 821 subjects exposed to clobetasol propionate foam and vehicle foam, the pooled incidence of local adverse reactions in trials for atopic dermatitis and psoriasis with clobetasol propionate foam was 1.9% for application site atrophy and 1.6% for application site reaction. Most local adverse events were rated as mild to moderate and they were not affected by age, race, or gender.
6.2 Postmarketing Experience
Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The following adverse reactions have been identified during post-approval use of clobetasol formulations: erythema, pruritus, burning, alopecia, and dryness.
The following additional local adverse reactions have been reported with topical corticosteroids: folliculitis, acneiform eruptions, hypopigmentation, perioral dermatitis, allergic contact dermatitis, secondary infection, irritation, striae, and miliaria. They may occur more frequently with the use of occlusive dressings and higher potency corticosteroids, such as clobetasol propionate.
Cushing’s syndrome has been reported in infants and adults as a result of prolonged use of topical clobetasol propionate formulations.
Ophthalmic adverse reactions may include cataracts, glaucoma, increased intraocular pressure, and central serous chorioretinopathy.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no available data on clobetasol propionate foam use in pregnant women to inform of a drug associated risk for adverse developmental outcomes.
Published data report a significantly increased risk of low birthweight with the use of greater than 300 grams of potent or very potent topical corticosteroid during a pregnancy. Advise pregnant women of the potential risk to a fetus and to use clobetasol propionate foam on the smallest area of skin and for the shortest duration possible (see Data).
In animal reproduction studies, increased malformations, such as cleft palate and skeletal abnormalities, were observed after subcutaneous administration of clobetasol propionate to pregnant mice and rabbits. No comparison of animal exposure with human exposure was computed.
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Human Data
Multiple observational studies found no significant associations between maternal use of topical corticosteroids of any potency and congenital malformations, preterm delivery, or fetal mortality. However, when the dispensed amount of potent or very potent topical corticosteroid exceeded 300 g during the entire pregnancy, use was associated with an increase in low birth weight infants (adjusted RR, 7.74 [95% CI, 1.49–40.11]). In addition, a small cohort study, in which 28 sub-Saharan women using potent topical corticosteroids (27/28 used clobetasol propionate 0.05%) for skin lightening during pregnancy, noted a higher incidence of low birth weight infants in the exposed group. The majority of exposed subjects treated large areas of the body (a mean quantity of 60 g/month [range, 12–170 g]) over long periods of time.
Animal Data
Embryofetal development studies conducted with clobetasol propionate in mice using the subcutaneous route resulted in fetotoxicity at the highest dose tested (1 mg/kg) and malformations at all dose levels tested down to 0.03 mg/kg. Malformations seen included cleft palate and skeletal abnormalities.
In an embryofetal development study in rabbits, subcutaneous administration of clobetasol propionate resulted in malformations at doses of 0.003 and 0.01 mg/kg. Malformations seen included cleft palate, cranioschisis, and other skeletal abnormalities.
8.2 Lactation
Risk Summary
There is no information regarding the presence of clobetasol propionate in breast milk or its effects on the breastfed infant or on milk production. Systemically administered corticosteroids appear in human milk and could suppress growth, interfere with endogenous corticosteroid production, or cause other untoward effects. It is not known whether topical administration of clobetasol propionate could result in sufficient systemic absorption to produce detectable quantities in human milk. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for clobetasol propionate foam and any potential adverse effects on the breastfed infant from clobetasol propionate foam or from the underlying maternal condition.
Clinical Considerations
To minimize potential exposure to the breastfed infant via breast milk, use clobetasol propionate foam on the smallest area of skin and for the shortest duration possible while breastfeeding. Advise breastfeeding women not to apply clobetasol propionate foam directly to the nipple and areola to avoid direct infant exposure.
8.4 Pediatric Use
Use in pediatric patients younger than 12 years is not recommended because of the risk of HPA axis suppression.
After two weeks of twice-daily treatment with clobetasol propionate foam, 7 of 15 subjects (47%) aged 6 to 11 years demonstrated HPA axis suppression. The laboratory suppression was transient; in all subjects serum cortisol levels returned to normal when tested 4 weeks post-treatment.
In 92 subjects aged 12 to 17 years, safety was similar to that observed in the adult population. Based on these data, no adjustment of dosage of clobetasol propionate foam in adolescent patients aged 12 to 17 years is warranted [see Warnings and Precautions (5.1)].
Because of a higher ratio of skin surface area to body mass, pediatric patients are at a greater risk than adults of HPA axis suppression and Cushing’s syndrome when they are treated with topical corticosteroids. They are therefore also at greater risk of adrenal insufficiency during and/or after withdrawal of treatment.
HPA axis suppression, Cushing’s syndrome, linear growth retardation, delayed weight gain, and intracranial hypertension have been reported in children receiving topical corticosteroids. Manifestations of adrenal suppression in children include low plasma cortisol levels and an absence of response to ACTH stimulation. Manifestations of intracranial hypertension include bulging fontanelles (in infants), headaches, and bilateral papilledema. Administration of topical corticosteroids to children should be limited to the least amount compatible with an effective therapeutic regimen. Chronic corticosteroid therapy may interfere with the growth and development of children.
Adverse effects, including striae, have been reported with inappropriate use of topical corticosteroids in infants and children.
8.5 Geriatric Use
A limited number of subjects aged 65 years or older have been treated with clobetasol propionate foam (n = 58) in U.S. clinical trials. While the number of subjects is too small to permit separate analysis of efficacy and safety, the adverse reactions reported in this population were similar to those reported by younger subjects. Based on available data, no adjustment of dosage of clobetasol propionate foam in geriatric patients is warranted.
- 10 OVERDOSAGE
-
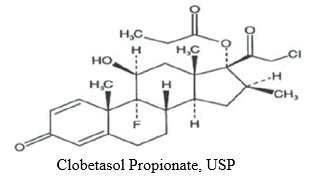
11 DESCRIPTION
Clobetasol propionate foam, is a white to off-white petrolatum-based emulsion aerosol foam, containing the active ingredient clobetasol propionate, USP, a synthetic corticosteroid for topical dermatologic use. Clobetasol, an analog of prednisolone, has a high degree of glucocorticoid activity and a slight degree of mineralocorticoid activity.
Clobetasol propionate is 21-chloro-9-fluoro-11ß,17-dihydroxy-16ß-methylpregna-1,4-diene-3,20-dione 17-propionate, with the empirical formula C25H32ClFO5, and a molecular weight of 466.97.
The following is the chemical structure:
Clobetasol propionate is a white to almost white crystalline powder, practically insoluble in water.
Each gram of clobetasol propionate foam contains 0.5 mg clobetasol propionate, USP. The foam also contains anhydrous citric acid, cetyl alcohol, cyclomethicone, isopropyl myristate, light mineral oil, polyoxyl 20 cetostearyl ether, potassium citrate monohydrate, propylene glycol, purified water, sorbitan monolaurate, white petrolatum, and phenoxyethanol as a preservative.
Clobetasol propionate foam is dispensed from an aluminum can pressurized with a hydrocarbon (propane/butane) propellant.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Corticosteroids play a role in cellular signaling, immune function, inflammation, and protein regulation; however, the precise mechanism of action in corticosteroid-responsive dermatoses is unknown.
12.2 Pharmacodynamics
In a trial evaluating the potential for HPA axis suppression, using the cosyntropin stimulation test, clobetasol propionate foam demonstrated reversible adrenal suppression after two weeks of twice-daily use in subjects with atopic dermatitis of at least 30% body surface area (BSA). The proportion of subjects aged 12 years and older demonstrating HPA axis suppression was 16.2% (6 out of 37). In this trial HPA axis suppression was defined as serum cortisol level ≤18 mcg/dL 30 minutes post cosyntropin stimulation. The laboratory suppression was transient; in all subjects serum cortisol levels returned to normal when tested 4 weeks post treatment [see Warnings and Precautions (5.1), Use in Specific Populations (8.4)].
12.3 Pharmacokinetics
Topical corticosteroids can be absorbed from intact healthy skin. The extent of percutaneous absorption of topical corticosteroids is determined by many factors, including the product formulation and the integrity of the epidermal barrier. Occlusion, inflammation, and/or other disease processes in the skin may increase percutaneous absorption. The use of pharmacodynamic endpoints for assessing the systemic exposure of topical corticosteroids may be necessary due to the fact that circulating levels are often below the level of detection. Once absorbed through the skin, topical corticosteroids are metabolized primarily in the liver and are then excreted by the kidneys. Some corticosteroids and their metabolites are also excreted in the bile.
Following twice-daily application of clobetasol propionate foam for one week to 32 adult subjects with mild to moderate plaque-type psoriasis, mean peak plasma concentrations (±SD) of 59 ± 36 pg/mL of clobetasol were observed at around 5 hours post dose on Day 8.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term animal studies have not been performed to evaluate the carcinogenic potential of clobetasol propionate foam or clobetasol propionate.
In a 90-day repeat-dose toxicity study in rats, topical administration of clobetasol propionate foam at dose concentrations from 0.001% to 0.1% or from 0.03 to 0.3 mg/kg/day of clobetasol propionate resulted in a toxicity profile consistent with long term exposure to corticosteroids including adrenal atrophy, histopathological changes in several organ systems indicative of severe immune suppression and opportunistic fungal and bacterial infections. A no observable adverse effect level could not be determined in this study. Although the clinical relevance of the findings in animals to humans is not clear, sustained glucocorticoid-related immune suppression may increase the risk of infection and possibly the risk for carcinogenesis.
Clobetasol propionate was non-mutagenic in the Ames test, the mouse lymphoma test, the Saccharomyces cerevisiae gene conversion assay, and the E. coli B WP2 fluctuation test. In the in vivo mouse micronucleus test, a positive finding was observed at 24 hours, but not at 48 hours, following oral administration at a dose of 2,000 mg/kg.
Studies in the rat following subcutaneous administration of clobetasol propionate at dosage levels up to 0.05 mg/kg per day revealed that the females exhibited an increase in the number of resorbed embryos and a decrease in the number of living fetuses at the highest dose.
-
14 CLINICAL STUDIES
In a randomized trial of subjects 12 years and older with moderate to severe atopic dermatitis, 251 subjects were treated with clobetasol propionate foam and 126 subjects were treated with vehicle foam. Subjects were treated twice daily for 2 weeks. At the end of treatment, 131 of 251 subjects (52%) treated with clobetasol propionate foam compared with 18 of 126 subjects (14%) treated with vehicle foam achieved treatment success. Treatment success was defined by an Investigator’s Static Global Assessment (ISGA) score of clear (0) or almost clear (1) with at least 2 grades improvement from baseline, and scores of absent or minimal (0 or 1) for erythema and induration/papulation.
In an additional randomized trial of subjects 12 years and older with mild to moderate plaque-type psoriasis, 253 subjects were treated with clobetasol propionate foam and 123 subjects were treated with vehicle foam. Subjects were treated twice daily for 2 weeks. At the end of treatment, 41 of 253 subjects (16%) treated with clobetasol propionate foam compared with 5 of 123 subjects (4%) treated with vehicle foam achieved treatment success. Treatment success was defined by an ISGA score of clear (0) or almost clear (1) with at least 2 grades improvement from baseline, scores of none or faint/minimal (0 or 1) for erythema and scaling, and a score of none (0) for plaque thickness.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Clobetasol Propionate Foam, 0.05% contains 0.5 mg of clobetasol propionate, USP per gram. The white emulsion aerosol foam is available as follows:
NDC: 0378-8055-50
50 g aluminum canNDC: 0378-8055-01
100 g aluminum can16.2 Storage and Handling
Store at 20° to 25°C (68° to 77°F). [See USP Controlled Room Temperature.]
FLAMMABLE. AVOID FIRE, FLAME OR SMOKING DURING AND IMMEDIATELY FOLLOWING APPLICATION. Contents under pressure. Do not puncture or incinerate. Do not expose to heat or store at temperatures above 120°F (49°C).
Keep out of reach of children.
-
17 PATIENT COUNSELING INFORMATION
See FDA-Approved Patient Labeling (Patient Information)
Effects on Endocrine System
Clobetasol propionate foam may cause HPA axis suppression. Advise patients that use of topical corticosteroids, including clobetasol propionate foam, may require periodic evaluation for HPA axis suppression. Topical corticosteroids may have other endocrine effects. Concomitant use of multiple corticosteroid-containing products may increase the total systemic exposure to topical corticosteroids. Patients should inform their physician(s) that they are using clobetasol propionate foam if surgery is contemplated [see Warnings and Precautions (5.1)].
Ophthalmic Adverse Reactions
Advise patients to report any visual symptoms to their healthcare providers [see Warnings and Precautions (5.3)].
Local Adverse Reactions
Report any signs of local adverse reactions to the physician. Advise patients that local reactions and skin atrophy are more likely to occur with occlusive use or prolonged use [see Warnings and Precautions (5.2)].
Pregnancy
Advise a pregnant woman that use of clobetasol propionate foam may cause fetal harm and to use clobetasol propionate foam on the smallest area of skin and for the shortest duration possible [see Use in Specific Populations (8.1)].
Lactation
Advise a woman to use clobetasol propionate foam on the smallest area of skin and for the shortest duration possible while breastfeeding. Advise breastfeeding women not to apply clobetasol propionate foam directly to the nipple and areola to avoid direct infant exposure [see Use in Specific Populations (8.2)].
Important Administration Instructions
Patients using topical corticosteroids should receive the following information and instructions:
- This medication is to be used as directed by the physician. It is for external use only. Unless directed by the prescriber, it should not be used on the face or in skin-fold areas, such as the underarms or groin. Avoid contact with the eyes or other mucous membranes. Wash hands after use.
- As with other corticosteroids, therapy should be discontinued when control is achieved. If no improvement is seen within 2 weeks, contact the physician.
- Do not use for more than 50 grams per week of clobetasol propionate foam, or an amount greater than 21 capfuls per week. [see Dosage and Administration (2).]
- This medication is flammable; avoid heat, flame, or smoking when applying this product.
-
PATIENT INFORMATION
Clobetasol Propionate Foam
Important: For skin use only. Do not get clobetasol propionate foam in your eyes, mouth, or vagina.
What is clobetasol propionate foam?
Clobetasol propionate foam is a prescription corticosteroid medicine used on the skin (topical) to treat people 12 years of age and older with certain skin conditions that cause red, flaky, and itchy skin.
Clobetasol propionate foam is not recommended for use in children under 12 years of age.
Clobetasol propionate foam should not be used:
- on your face, underarms, or groin area
- if you have skin thinning (atrophy) at the treatment area
You should not use clobetasol propionate foam for longer than 2 weeks in a row.
You should not use more than 50 grams or 21 capfuls of clobetasol propionate foam in 1 week.
Before using clobetasol propionate foam, tell your healthcare provider about all of your medical conditions, including if you:
- have had irritation or other skin reaction to a steroid medicine in the past.
- have a skin infection. You may need medicine to treat the skin infection before using clobetasol propionate foam.
- have diabetes.
- have adrenal gland problems.
- have liver problems.
- plan to have surgery.
- are pregnant or plan to become pregnant. It is not known if clobetasol propionate foam will harm your unborn baby. If you use clobetasol propionate foam during pregnancy, use clobetasol propionate foam on the smallest area of skin and for the shortest time needed.
- are breastfeeding or plan to breastfeed. It is not known if clobetasol propionate passes into your breast milk. If you use clobetasol propionate foam while breastfeeding, use clobetasol propionate foam on the smallest area of skin and for the shortest time needed. Do not apply clobetasol propionate foam directly to the nipple and areola to avoid getting clobetasol propionate foam into your baby’s mouth.
Tell your healthcare provider about all the medicine you take including prescription and over-the-counter medicines, vitamins, and herbal supplements. Do not use other products containing a corticosteroid medicine during treatment with clobetasol propionate foam without talking to your healthcare provider first.
How should I use clobetasol propionate foam?
See the “Instructions for Use” for detailed information about the right way to apply clobetasol propionate foam.
- Use clobetasol propionate foam exactly as your healthcare provider tells you to use it.
- Apply a thin layer of clobetasol propionate foam to the affected area 2 times each day, 1 time in the morning and 1 time at night, or as directed by your healthcare provider.
- Do not bandage, wrap or cover your treated area unless your healthcare provider tells you to.
- Talk to your healthcare provider if your skin does not improve after 2 weeks of treatment with clobetasol propionate foam.
Wash your hands after using clobetasol propionate foam.
What should I avoid while using clobetasol propionate foam?
Clobetasol propionate foam is flammable. Avoid heat, flame, or smoking during and right after you apply clobetasol propionate foam to your skin.
What are the possible side effects of clobetasol propionate foam?
Clobetasol propionate foam may cause serious side effects, including:
- Clobetasol propionate foam can pass through your skin. Too much clobetasol propionate foam passing through your skin can cause adrenal glands to stop working.
- Cushing’s syndrome, a condition that happens when the body is exposed to too much of the hormone cortisol.
- High blood sugar (hyperglycemia)
- Vision problems. Clobetasol propionate foam may increase your chance of developing vision problems such as cataract(s) and glaucoma. Tell your healthcare provider if you develop blurred vision or other vision problems during your treatment with clobetasol propionate foam.
- Skin reactions at the treated site. Tell your healthcare provider if you get any skin reactions or skin infections.
- Effects on growth and weight in children.
Your healthcare provider may do certain blood tests to check for side effects.
The most common side effects of clobetasol propionate foam include:
- thinning of skin
- burning
- redness
- itching
- dryness
These are not all the side effects of clobetasol propionate foam.
Call your healthcare provider for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store clobetasol propionate foam?
- Store clobetasol propionate foam at room temperature between 68° to 77°F (20° to 25°C).
- Do not break through (puncture) clobetasol propionate foam can.
- Never throw the can into a fire, even if the can is empty.
- Do not store clobetasol propionate foam near heat or at temperatures above 120°F (49°C).
Keep clobetasol propionate foam and all medicines out of the reach of children.
General information about the safe and effective use of clobetasol propionate foam
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use clobetasol propionate foam for a condition for which it was not prescribed. Do not give clobetasol propionate foam to other people, even if they have the same condition that you have. It may harm them. You can ask your healthcare provider or pharmacist for information about clobetasol propionate foam that is written for health professionals.
What are the ingredients in clobetasol propionate foam?
Active ingredient: clobetasol propionate
Inactive ingredients: anhydrous citric acid, cetyl alcohol, cyclomethicone, isopropyl myristate, light mineral oil, polyoxyl 20 cetostearyl ether, potassium citrate monohydrate, propylene glycol, purified water, sorbitan monolaurate, white petrolatum, and phenoxyethanol as a preservative, pressurized with a hydrocarbon (propane/butane) propellant.
Manufactured for: Mylan Pharmaceuticals Inc.,Morgantown, WV 26505 U.S.A.
For more information, call Mylan at 1-877-446-3679 (1-877-4-INFO-RX).
The Patient Information and Instructions for Use have been approved by the U.S. Food and Drug Administration.
Manufactured for:
Mylan Pharmaceuticals Inc.
Morgantown, WV 26505 U.S.A.Manufactured by:
DPT Laboratories, Ltd.
San Antonio, TX 78215 U.S.A.140952-0518
Revised: 5/2018
DPT:ECLOBFOG:R2 -
PRINCIPAL DISPLAY PANEL – 0.05%
NDC: 0378-8055-50
Clobetasol
Propionate
Foam
0.05%Emulsion
FormulationFOR TOPICAL USE ONLY.
NOT FOR OPHTHALMIC, ORAL,
OR INTRAVAGINAL USE.Shake can before use.
Invert can
and then
press firmly
to dispense.Description: Each gram of Clobetsol
Propionate Foam contains 0.5 mg
clobetasol propionate, USP.The foam also contains anhydrous
citric acid, cetyl alcohol,
cyclomethicone, isopropyl myristate,
light mineral oil, polyoxyl 20
cetostearyl ether, potassium citrate
monohydrate, propylene glycol,
purified water, sorbitan monolaurate,
white petrolatum, and phenoxyethanol
as a preservative, and is pressurized
with a hydrocarbon (propane/butane)
propellant.Usual Dosage: Use only as
prescribed by your physician. See
accompanying prescribing
information.Warning: FLAMMABLE. AVOID FIRE,
FLAME, OR SMOKING DURING AND
IMMEDIATELY FOLLOWING
APPLICATION.Contents under pressure. Do not
puncture or incinerate. Do not
expose to heat or store at
temperatures above 120°F (49°C).Avoid contact with eyes or other
mucous membranes. Keep this and
all medication out of the reach of
children.Store at 20° to 25°C (68° to 77°F).
[See USP Controlled Room
Temperature.]CFC FREE
Manufactured for:
Mylan Pharmaceuticals Inc.
Morgantown, WV 26505 U.S.A.Manufactured by:
DPT Laboratories, Ltd.
San Antonio, TX 78215 U.S.A.For more information, call
Mylan Pharmaceuticals Inc. at
1-877-446-3679 (1-877-4-INFO-RX).DPT:8055:50:1C:R1
117492-0917
Mylan.com
-
INGREDIENTS AND APPEARANCE
CLOBETASOL PROPIONATE
clobetasol propionate aerosol, foamProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0378-8055 Route of Administration TOPICAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CLOBETASOL PROPIONATE (UNII: 779619577M) (CLOBETASOL - UNII:ADN79D536H) CLOBETASOL PROPIONATE 0.5 mg in 1 g Inactive Ingredients Ingredient Name Strength ANHYDROUS CITRIC ACID (UNII: XF417D3PSL) CETYL ALCOHOL (UNII: 936JST6JCN) CYCLOMETHICONE (UNII: NMQ347994Z) ISOPROPYL MYRISTATE (UNII: 0RE8K4LNJS) LIGHT MINERAL OIL (UNII: N6K5787QVP) POLYOXYL 20 CETOSTEARYL ETHER (UNII: YRC528SWUY) POTASSIUM CITRATE (UNII: EE90ONI6FF) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) WATER (UNII: 059QF0KO0R) SORBITAN MONOLAURATE (UNII: 6W9PS8B71J) PETROLATUM (UNII: 4T6H12BN9U) PHENOXYETHANOL (UNII: HIE492ZZ3T) Product Characteristics Color WHITE Score Shape Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0378-8055-50 1 in 1 CARTON 11/14/2019 1 50 g in 1 CAN; Type 0: Not a Combination Product 2 NDC: 0378-8055-01 1 in 1 CARTON 01/14/2019 2 100 g in 1 CAN; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA authorized generic NDA022013 01/14/2019 Labeler - Mylan Pharmaceuticals Inc. (059295980)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.