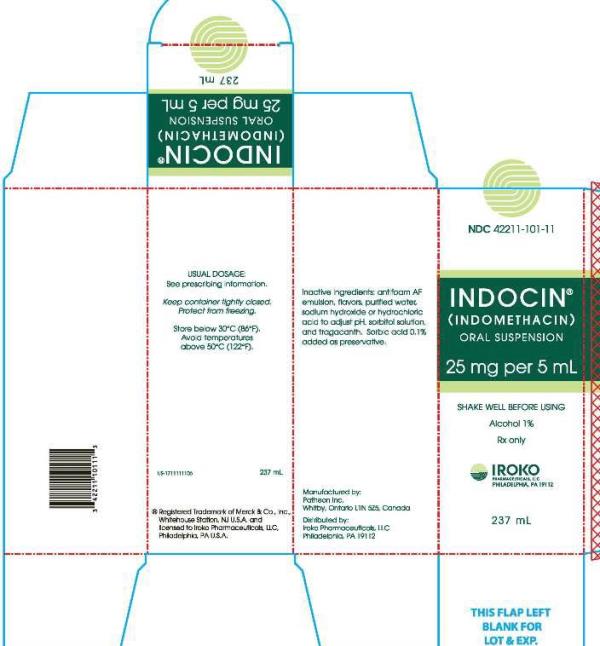
INDOCIN- indomethacin suspension
INDOCIN by
Drug Labeling and Warnings
INDOCIN by is a Prescription medication manufactured, distributed, or labeled by Iroko Pharmaceuticals, LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use INDOCIN® ORAL SUSPENSION safely and effectively. See full prescribing information for INDOCIN.
INDOCIN (indomethacin) Oral Suspension, for oral use
Initial U.S. Approval: 1965
WARNING: RISK OF SERIOUS CARDIOVASCULAR AND GASTROINTESTINAL EVENTS
See full prescribing information for complete boxed warning.
-
Nonsteroidal anti-inflammatory drugs (NSAIDs) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use (5.1)
-
INDOCIN is contraindicated in the setting of coronary artery bypass graft (CABG) surgery (4, 5.1)
- NSAIDs cause an increased risk of serious gastrointestinal (GI) adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients and patients with a prior history of peptic ulcer disease and/or GI bleeding are at greater risk for serious GI events (5.2)
RECENT MAJOR CHANGES
INDICATIONS AND USAGE
INDOCIN is a nonsteroidal anti-inflammatory drug indicated for:
- Moderate to severe rheumatoid arthritis including acute flares of chronic disease
- Moderate to severe ankylosing spondylitis
- Moderate to severe osteoarthritis
- Acute painful shoulder (bursitis and/or tendinitis)
- Acute gouty arthritis (1)
DOSAGE AND ADMINISTRATION
- Use the lowest effective dosage for shortest duration consistent with individual patient treatment goals (2.1)
- The dosage for moderate to severe rheumatoid arthritis including acute flares of chronic disease; moderate to severe ankylosing spondylitis; and moderate to severe osteoarthritis is INDOCIN 25 mg (5 mL) two or three times a day (2.2)
- The dosage for acute painful shoulder (bursitis and/or tendinitis) is 75-150 mg (15-30 mL) daily in 3 or 4 divided doses (2.3)
- The dosage for acute gouty arthritis is INDOCIN 50 mg (10 mL) three times a day (2.4)
DOSAGE FORMS AND STRENGTHS
INDOCIN (indomethacin) Oral Suspension: 25 mg of indocmethacin per 5mL (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
-
Hepatotoxicity: Inform patients of warning signs and symptoms of hepatotoxicity. Discontinue if abnormal liver tests persist or worsen or if clinical signs and symptoms of liver disease develop (5.3)
-
Hypertension: Patients taking some antihypertensive medications may have impaired response to these therapies when taking NSAIDs. Monitor blood pressure (5.4, 7)
-
Heart Failure and Edema: Avoid use of INDOCIN in patients with severe heart failure unless benefits are expected to outweigh risk of worsening heart failure (5.5)
-
Renal Toxicity: Monitor renal function in patients with renal or hepatic impairment, heart failure, dehydration, or hypovolemia. Avoid use of INDOCIN in patients with advanced renal disease unless benefits are expected to outweigh risk of worsening renal function (5.6)
-
Anaphylactic Reactions: Seek emergency help if an anaphylactic reaction occurs (5.7)
-
Exacerbation of Asthma Related to Aspirin Sensitivity: INDOCIN is contraindicated in patients with aspirin-sensitive asthma. Monitor patients with preexisting asthma (without aspirin sensitivity) (5.8)
-
Serious Skin Reactions: Discontinue INDOCIN at first appearance of skin rash or other signs of hypersensitivity (5.9)
-
Premature Closure of Fetal Ductus Arteriosus: Avoid use in pregnant women starting at 30 weeks gestation (5.10, 8.1)
- Hematologic Toxicity: Monitor hemoglobin or hematocrit in patients with any signs or symptoms of anemia (5.11, 7)
ADVERSE REACTIONS
Most common adverse reactions (incidence ≥ 3%) are headache, dizziness, dyspepsia, and nausea. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Iroko Pharmaceuticals, LLC at 1-877-757-0676 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.DRUG INTERACTIONS
-
Drugs that Interfere with Hemostasis (e.g. warfarin, aspirin, SSRIs/SNRIs): Monitor patients for bleeding who are concomitantly taking INDOCIN with drugs that interfere with hemostasis. Concomitant use of INDOCIN and analgesic doses of aspirin is not generally recommended (7)
-
ACE Iinhibitors, Angiotensin Receptor Blockers (ARB), or Beta-Blockers: Concomitant use with INDOCIN may diminish the antihypertensive effect of these drugs. Monitor blood pressure (7)
-
ACE Inhibitors and ARBs: Concomitant use with INDOCIN in elderly, volume depleted, or those with renal impairment may result in deterioration of renal function. In such high risk patients, monitor for signs of worsening renal function (7)
-
Diuretics: NSAIDs can reduce natriuretic effect of furosemide and thiazide diuretics. Monitor patients to assure diuretic efficacy including antihypertensive effects (7)
- Digoxin: Concomitant use with INDOCIN can increase serum concentration and prolong half-life of digoxin. Monitor serum digoxin levels (7)
USE IN SPECIFIC POPULATIONS
Pregnancy: Use of NSAIDs during the third trimester of pregnancy increases the risk of premature closure of the fetal ductus arteriosus. Avoid use of NSAIDs in pregnant women starting at 30 weeks gestation (5.10, 8.1)
Infertility: NSAIDs are associated with reversible infertility. Consider withdrawal of INDOCIN in women who have difficulties conceiving (8.3)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 5/2018
-
Nonsteroidal anti-inflammatory drugs (NSAIDs) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use (5.1)
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: RISK OF SERIOUS CARDIOVASCULAR AND GASTROINTESTINAL EVENTS
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 General Dosing Instructions
2.2 Moderate to severe rheumatoid arthritis including acute flares of chronic disease; moderate to severe ankylosing spondylitis; and moderate to severe osteoarthritis
2.3 Acute painful shoulder (bursitis and/or tendinitis)
2.4 Acute Gouty Arthritis
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Cardiovascular Thrombotic Events
5.2 Gastrointestinal Bleeding, Ulceration, and Perforation
5.3 Hepatotoxicity
5.4 Hypertension
5.5 Heart Failure and Edema
5.6 Renal Toxicity and Hyperkalemia
5.7 Anaphylactic Reactions
5.8 Exacerbation of Asthma Related to Aspirin Sensitivity
5.9 Serious Skin Reactions
5.10 Premature Closure of Fetal Ductus Arteriosus
5.11 Hematologic Toxicity
5.12 Masking of Inflammation and Fever
5.13 Laboratory Monitoring
5.14 Central Nervous System Effects
5.15 Ocular Effects
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: RISK OF SERIOUS CARDIOVASCULAR AND GASTROINTESTINAL EVENTS
Cardiovascular Thrombotic Events
-
Nonsteroidal anti-inflammatory drugs (NSAIDs) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use [see Warnings and Precautions (5.1)].
- INDOCIN is contraindicated in the setting of coronary artery bypass graft (CABG) surgery [see Contraindications (4) and Warnings and Precautions (5.1)].
Gastrointestinal Bleeding, Ulceration, and Perforation
- NSAIDs cause an increased risk of serious gastrointestinal (GI) adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients and patients with a prior history of peptic ulcer disease and/or GI bleeding are at greater risk for serious GI events [see Warnings and Precautions (5.2)].
-
Nonsteroidal anti-inflammatory drugs (NSAIDs) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use [see Warnings and Precautions (5.1)].
- 1 INDICATIONS AND USAGE
-
2
DOSAGE AND ADMINISTRATION
2.1 General Dosing Instructions
Carefully consider the potential benefits and risks of INDOCIN and other treatment options before deciding to use INDOCIN. Use the lowest effective dosage for the shortest duration consistent with individual patient treatment goals [see Warnings and Precautions (5)].
After observing the response to initial therapy with indomethacin, the dose and frequency should be adjusted to suit an individual patient’s needs.
Adverse reactions generally appear to correlate with the dose of indomethacin. Therefore, every effort should be made to determine the lowest effective dosage for the individual patient.
Dosage recommendations for active stages of the following:
2.2 Moderate to severe rheumatoid arthritis including acute flares of chronic disease; moderate to severe ankylosing spondylitis; and moderate to severe osteoarthritis
INDOCIN 25 mg (5 mL) twice a day or three times a day. If this is well tolerated, increase the daily dosage by 25 mg (5 mL) or by 50 mg (10 mL), if required by continuing symptoms, at weekly intervals until a satisfactory response is obtained or until a total daily dose of 150- 200 mg (30 - 40 mL) is reached. Doses above this amount generally do not increase the effectiveness of the drug.
In patients who have persistent night pain and/or morning stiffness, the giving of a large portion, up to a maximum of 100 mg (20 mL), of the total daily dose at bedtime may be helpful in affording relief. The total daily dose should not exceed 200 mg (40 mL). In acute flares of chronic rheumatoid arthritis, it may be necessary to increase the dosage by 25 mg (5 mL) or, if required, by 50 mg (10 mL) daily.
If minor adverse effects develop as the dosage is increased, reduce the dosage rapidly to a tolerated dose and observe the patient closely.
If severe adverse reactions occur, stop the drug. After the acute phase of the disease is under control, an attempt to reduce the daily dose should be made repeatedly until the patient is receiving the smallest effective dose or the drug is discontinued.
Careful instructions to, and observations of, the individual patient are essential to the prevention of serious, irreversible, including fatal, adverse reactions.
As advancing years appear to increase the possibility of adverse reactions, INDOCIN should be used with greater care in the elderly [see Use in Specific Populations (8.5)].
2.3 Acute painful shoulder (bursitis and/or tendinitis)
INDOCIN 75-150 mg (15-30 mL) daily in 3 or 4 divided doses.
The drug should be discontinued after the signs and symptoms of inflammation have been controlled for several days. The usual course of therapy is 7-14 days.
2.4 Acute Gouty Arthritis
INDOCIN 50 mg (10 mL) three times a day until pain is tolerable. The dose should then be rapidly reduced to complete cessation of the drug. Definite relief of pain has been reported within 2 to 4 hours. Tenderness and heat usually subside in 24 to 36 hours, and swelling gradually disappears in 3 to 5 days.
- 3 DOSAGE FORMS AND STRENGTHS
-
4
CONTRAINDICATIONS
INDOCIN is contraindicated in the following patients:
- Known hypersensitivity (e.g., anaphylactic reactions and serious skin reactions) to indomethacin or any components of the drug product [see Warnings and Precautions (5.7, 5.9)]
- History of asthma, urticaria, or other allergic-type reactions after taking aspirin or other NSAIDs. Severe, sometimes fatal, anaphylactic reactions to NSAIDs have been reported in such patients [see Warnings and Precautions (5.7, 5.8)]
- In the setting of coronary artery bypass graft (CABG) surgery [see Warnings and Precautions (5.1)]
- Known hypersensitivity (e.g., anaphylactic reactions and serious skin reactions) to indomethacin or any components of the drug product [see Warnings and Precautions (5.7, 5.9)]
-
5
WARNINGS AND PRECAUTIONS
5.1 Cardiovascular Thrombotic Events
Clinical trials of several COX-2 selective and nonselective NSAIDs of up to three years duration have shown an increased risk of serious cardiovascular (CV) thrombotic events, including myocardial infarction (MI) and stroke, which can be fatal. Based on available data, it is unclear that the risk for CV thrombotic events is similar for all NSAIDs. The relative increase in serious CV thrombotic events over baseline conferred by NSAID use appears to be similar in those with and without known CV disease or risk factors for CV disease. However, patients with known CV disease or risk factors had a higher absolute incidence of excess serious CV thrombotic events, due to their increased baseline rate. Some observational studies found that this increased risk of serious CV thrombotic events began as early as the first weeks of treatment. The increase in CV thrombotic risk has been observed most consistently at higher doses.
To minimize the potential risk for an adverse CV event in NSAID-treated patients, use the lowest effective dose for the shortest duration possible. Physicians and patients should remain alert for the development of such events, throughout the entire treatment course, even in the absence of previous CV symptoms. Patients should be informed about the symptoms of serious CV events and the steps to take if they occur.
There is no consistent evidence that concurrent use of aspirin mitigates the increased risk of serious CV thrombotic events associated with NSAID use. The concurrent use of aspirin and an NSAID, such as indomethacin, increases the risk of serious gastrointestinal (GI) events [see Warnings and Precautions (5.2)].
Status Post Coronary Artery Bypass Graft (CABG) Surgery
Two large, controlled clinical trials of a COX-2 selective NSAID for the treatment of pain in the first 10–14 days following CABG surgery found an increased incidence of myocardial infarction and stroke. NSAIDs are contraindicated in the setting of CABG [see Contraindications (4)].
Post-MI Patients
Observational studies conducted in the Danish National Registry have demonstrated that patients treated with NSAIDs in the post-MI period were at increased risk of reinfarction, CV-related death, and all-cause mortality beginning in the first week of treatment. In this same cohort, the incidence of death in the first year post-MI was 20 per 100 person years in NSAID-treated patients compared to 12 per 100 person years in non-NSAID exposed patients. Although the absolute rate of death declined somewhat after the first year post-MI, the increased relative risk of death in NSAID users persisted over at least the next four years of follow-up.
Avoid the use of INDOCIN in patients with a recent MI unless the benefits are expected to outweigh the risk of recurrent CV thrombotic events. If INDOCIN is used in patients with a recent MI, monitor patients for signs of cardiac ischemia.
5.2 Gastrointestinal Bleeding, Ulceration, and Perforation
NSAIDs, including indomethacin, cause serious gastrointestinal (GI) adverse events including inflammation, bleeding, ulceration, and perforation of the esophagus, stomach, small intestine, or large intestine, which can be fatal. These serious adverse events can occur at any time, with or without warning symptoms, in patients treated with NSAIDs. Only one in five patients who develop a serious upper GI adverse event on NSAID therapy is symptomatic. Upper GI ulcers, gross bleeding, or perforation caused by NSAIDs occurred in approximately 1% of patients treated for 3-6 months, and in about 2%-4% of patients treated for one year. However, even short-term NSAID therapy is not without risk.
Risk Factors for GI Bleeding, Ulceration, and Perforation
Patients with a prior history of peptic ulcer disease and/or GI bleeding who used NSAIDs had a greater than 10-fold increased risk for developing a GI bleed compared to patients without these risk factors. Other factors that increase the risk of GI bleeding in patients treated with NSAIDs include longer duration of NSAID therapy; concomitant use of oral corticosteroids, aspirin, anticoagulants, or selective serotonin reuptake inhibitors (SSRIs); smoking; use of alcohol; older age; and poor general health status. Most postmarketing reports of fatal GI events occurred in elderly or debilitated patients. Additionally, patients with advanced liver disease and/or coagulopathy are at increased risk for GI bleeding.
Strategies to Minimize the GI Risks in NSAID-treated patients:
- Use the lowest effective dosage for the shortest possible duration.
- Avoid administration of more than one NSAID at a time.
- Avoid use in patients at higher risk unless benefits are expected to outweigh the increased risk of bleeding. For such patients, as well as those with active GI bleeding, consider alternate therapies other than NSAIDs.
- Remain alert for signs and symptoms of GI ulceration and bleeding during NSAID therapy.
- If a serious GI adverse event is suspected, promptly initiate evaluation and treatment, and discontinue INDOCIN until a serious GI adverse event is ruled out.
- In the setting of concomitant use of low-dose aspirin for cardiac prophylaxis, monitor patients more closely for evidence of GI bleeding [see Drug Interactions (7)].
5.3 Hepatotoxicity
Elevations of ALT or AST (three or more times the upper limit of normal [ULN]) have been reported in approximately 1% of NSAID-treated patients in clinical trials. In addition, rare, sometimes fatal, cases of severe hepatic injury, including fulminant hepatitis, liver necrosis, and hepatic failure have been reported.
Elevations of ALT or AST (less than three times ULN) may occur in up to 15% of patients treated with NSAIDs including indomethacin.
Inform patients of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, diarrhea, pruritus, jaundice, right upper quadrant tenderness, and "flu-like" symptoms). If clinical signs and symptoms consistent with liver disease develop, or if systemic manifestations occur (e.g., eosinophilia, rash, etc.), discontinue INDOCIN immediately, and perform a clinical evaluation of the patient.
5.4 Hypertension
NSAIDs, including INDOCIN, can lead to new onset of hypertension or worsening of preexisting hypertension, either of which may contribute to the increased incidence of CV events. Patients taking angiotensin converting enzyme (ACE) inhibitors, thiazide diuretics, or loop diuretics may have impaired response to these therapies when taking NSAIDs [see Drug Interactions (7)].
Monitor blood pressure (BP) during the initiation of NSAID treatment and throughout the course of therapy.
5.5 Heart Failure and Edema
The Coxib and traditional NSAID Trialists’ Collaboration meta-analysis of randomized controlled trials demonstrated an approximately two-fold increase in hospitalizations for heart failure in COX-2 selective-treated patients and nonselective NSAID-treated patients compared to placebo-treated patients. In a Danish National Registry study of patients with heart failure, NSAID use increased the risk of MI, hospitalization for heart failure, and death.
Additionally, fluid retention and edema have been observed in some patients treated with NSAIDs. Use of indomethacin may blunt the CV effects of several therapeutic agents used to treat these medical conditions (e.g., diuretics, ACE inhibitors, or angiotensin receptor blockers [ARBs]) [see Drug Interactions (7)].
Avoid the use of INDOCIN in patients with severe heart failure unless the benefits are expected to outweigh the risk of worsening heart failure. If INDOCIN is used in patients with severe heart failure, monitor patients for signs of worsening heart failure.
5.6 Renal Toxicity and Hyperkalemia
Renal Toxicity
Long-term administration of NSAIDs has resulted in renal papillary necrosis and other renal injury.
Renal toxicity has also been seen in patients in whom renal prostaglandins have a compensatory role in the maintenance of renal perfusion. In these patients, administration of an NSAID may cause a dose-dependent reduction in prostaglandin formation and, secondarily, in renal blood flow, which may precipitate overt renal decompensation. Patients at greatest risk of this reaction are those with impaired renal function, dehydration, hypovolemia, heart failure, liver dysfunction, those taking diuretics and ACE inhibitors or ARBs, and the elderly. Discontinuation of NSAID therapy is usually followed by recovery to the pretreatment state.
No information is available from controlled clinical studies regarding the use of INDOCIN in patients with advanced renal disease. The renal effects of INDOCIN may hasten the progression of renal dysfunction in patients with preexisting renal disease.
Correct volume status in dehydrated or hypovolemic patients prior to initiating INDOCIN. Monitor renal function in patients with renal or hepatic impairment, heart failure, dehydration, or hypovolemia during use of INDOCIN [see Drug Interactions (7)]. Avoid the use of INDOCIN in patients with advanced renal disease unless the benefits are expected to outweigh the risk of worsening renal function. If INDOCIN is used in patients with advanced renal disease, monitor patients for signs of worsening renal function.
It has been reported that the addition of the potassium-sparing diuretic, triamterene, to a maintenance schedule of indomethacin resulted in reversible acute renal failure in two of four healthy volunteers. Indomethacin and triamterene should not be administered together.
Hyperkalemia
Increases in serum potassium concentration, including hyperkalemia, have been reported with use of NSAIDs, even in some patients without renal impairment. In patients with normal renal function, these effects have been attributed to a hyporeninemic-hypoaldosteronism state.
Both Indomethacin and potassium-sparing diuretics may be associated with increased serum potassium levels. The potential effects of indomethacin and potassium-sparing diuretics on potassium levels and renal function should be considered when these agents are administered concurrently.
5.7 Anaphylactic Reactions
Indomethacin has been associated with anaphylactic reactions in patients with and without known hypersensitivity to indomethacin and in patients with aspirin-sensitive asthma [see Contraindications (4) and Warnings and Precautions (5.8)].
Seek emergency help if an anaphylactic reaction occurs.
5.8 Exacerbation of Asthma Related to Aspirin Sensitivity
A subpopulation of patients with asthma may have aspirin-sensitive asthma which may include chronic rhinosinusitis complicated by nasal polyps; severe, potentially fatal bronchospasm; and/or intolerance to aspirin and other NSAIDs. Because cross-reactivity between aspirin and other NSAIDs has been reported in such aspirin-sensitive patients, INDOCIN is contraindicated in patients with this form of aspirin sensitivity [see Contraindications (4)]. When INDOCIN is used in patients with preexisting asthma (without known aspirin sensitivity), monitor patients for changes in the signs and symptoms of asthma.
5.9 Serious Skin Reactions
NSAIDs, including indomethacin, can cause serious skin adverse reactions such as exfoliative dermatitis, Stevens-Johnson Syndrome (SJS), and toxic epidermal necrolysis (TEN), which can be fatal. These serious events may occur without warning. Inform patients about the signs and symptoms of serious skin reactions, and to discontinue the use of INDOCIN at the first appearance of skin rash or any other sign of hypersensitivity. INDOCIN is contraindicated in patients with previous serious skin reactions to NSAIDs [see Contraindications (4)].
5.10 Premature Closure of Fetal Ductus Arteriosus
Indomethacin may cause premature closure of the fetal ductus arteriosus. Avoid use of NSAIDs, including INDOCIN, in pregnant women starting at 30 weeks of gestation (third trimester) [see Use in Specific Populations (8.1)].
5.11 Hematologic Toxicity
Anemia has occurred in NSAID-treated patients. This may be due to occult or gross blood loss, fluid retention, or an incompletely described effect on erythropoiesis. If a patient treated with INDOCIN has any signs or symptoms of anemia, monitor hemoglobin or hematocrit.
NSAIDs, including INDOCIN, may increase the risk of bleeding events. Co-morbid conditions, such as coagulation disorders, or concomitant use of warfarin, other anticoagulants, antiplatelet agents (e.g., aspirin), serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs) may increase this risk. Monitor these patients for signs of bleeding [see Drug Interactions (7)].
5.12 Masking of Inflammation and Fever
The pharmacological activity of INDOCIN in reducing inflammation, and possibly fever, may diminish the utility of diagnostic signs in detecting infections.
5.13 Laboratory Monitoring
Because serious GI bleeding, hepatotoxicity, and renal injury can occur without warning symptoms or signs, consider monitoring patients on long-term NSAID treatment with a CBC and a chemistry profile periodically [see Warnings and Precautions (5.2, 5.3, 5.6)].
5.14 Central Nervous System Effects
INDOCIN may aggravate depression or other psychiatric disturbances, epilepsy, and parkinsonism, and should be used with considerable caution in patients with these conditions. Discontinue INDOCIN if severe CNS adverse reactions develop.
INDOCIN may cause drowsiness; therefore, caution patients about engaging in activities requiring mental alertness and motor coordination, such as driving a car. Indomethacin may also cause headache. Headache which persists despite dosage reduction requires cessation of therapy with INDOCIN.
5.15 Ocular Effects
Corneal deposits and retinal disturbances, including those of the macula, have been observed in some patients who had received prolonged therapy with INDOCIN. Be alert to the possible association between the changes noted and INDOCIN. It is advisable to discontinue therapy if such changes are observed. Blurred vision may be a significant symptom and warrants a thorough ophthalmological examination. Since these changes may be asymptomatic, ophthalmologic examination at periodic intervals is desirable in patients receiving prolonged therapy. INDOCIN is not indicated for long-term treatment.
- Use the lowest effective dosage for the shortest possible duration.
-
6
ADVERSE REACTIONS
The following adverse reactions are discussed in greater detail in other sections of the labeling:
- Cardiovascular Thrombotic Events [see Warnings and Precautions (5.1)]
- GI Bleeding, Ulceration and Perforation [see Warnings and Precautions (5.2)]
- Hepatotoxicity [see Warnings and Precautions (5.3)]
- Hypertension [see Warnings and Precautions (5.4)]
- Heart Failure and Edema [see Warnings and Precautions (5.5)]
- Renal Toxicity and Hyperkalemia [see Warnings and Precautions (5.6)]
- Anaphylactic Reactions [see Warnings and Precautions (5.7)]
- Serious Skin Reactions [see Warnings and Precautions (5.9)]
- Hematologic Toxicity [see Warnings and Precautions (5.11)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
In a gastroscopic study in 45 healthy subjects, the number of gastric mucosal abnormalities was significantly higher in the group receiving INDOCIN Capsules than in the group taking INDOCIN Suppositories or placebo.
In a double-blind comparative clinical study involving 175 patients with rheumatoid arthritis, however, the incidence of upper gastrointestinal adverse effects with INDOCIN Suppositories or Capsules was comparable. The incidence of lower gastrointestinal adverse effects was greater in the suppository group.
The adverse reactions for INDOCIN Capsules listed in the following table have been arranged into two groups: (1) incidence greater than 1%; and (2) incidence less than 1%. The incidence for group (1) was obtained from 33 double-blind controlled clinical trials reported in the literature (1,092 patients). The incidence for group (2) was based on reports in clinical trials, in the literature, and on voluntary reports since marketing. The probability of a causal relationship exists between INDOCIN and these adverse reactions, some of which have been reported only rarely.
The adverse reactions reported with INDOCIN Capsules may also occur with use of the suspension.
Table 1 Summary of Adverse Reactions for INDOCIN Capsules
Incidence greater than 1% Incidence less than 1% GASTROINTESTINAL nausea* with or without vomiting
dyspepsia* (including
indigestion, heartburn and
epigastric pain)
diarrhea
abdominal distress or pain
constipationanorexia
bloating (includes distension)
flatulence
peptic ulcer
gastroenteritis
rectal bleeding
proctitis
single or multiple ulcerations,
including perforation and hemorrhage
of the esophagus, stomach,
duodenum or small and large
intestines
intestinal ulceration associated with
stenosis and obstructiongastrointestinal bleeding without
obvious ulcer formation and
perforation of preexisting
sigmoid lesions (diverticulum,
carcinoma, etc.) development
of ulcerative colitis and
regional ileitis
ulcerative stomatitis
toxic hepatitis and jaundice
(some fatal cases have been
reported)
intestinal strictures
(diaphragms)
pancreatitisCENTRAL NERVOUS SYSTEM headache (11.7%)
dizziness*
vertigo
somnolence
depression and fatigue
(including malaise and
listlessness)anxiety (includes nervousness)
muscle weakness
involuntary muscle movements
insomnia
muzziness
psychic disturbances including
psychotic episodes
mental confusion
drowsinesslight-headedness
syncope
paresthesia
aggravation of epilepsy and
parkinsonism
depersonalization
coma
peripheral neuropathy
convulsion
dysarthriaSPECIAL SENSES tinnitus ocular — corneal deposits and retinal
disturbances, including those of
the macula, have been reported in
some patients on prolonged therapy with INDOCINblurred vision
diplopia
hearing disturbances, deafnessCARDIOVASCULAR None hypertension
hypotension
tachycardia
chest paincongestive heart failure
arrhythmia; palpitationsMETABOLIC None edema
weight gain
fluid retention
flushing or sweatinghyperglycemia
glycosuria
hyperkalemiaINTEGUMENTARY none pruritus
rash; urticaria
petechiae or ecchymosisexfoliative dermatitis
erythema nodosum
loss of hair
Stevens-Johnson syndrome
erythema multiforme
toxic epidermal necrolysisHEMATOLOGIC None leukopenia
bone marrow depression
anemia secondary to obvious or occult
gastrointestinal bleedingaplastic anemia
hemolytic anemia
agranulocytosis
thrombocytopenic purpura
disseminated intravascular
coagulationHYPERSENSITIVITY None acute anaphylaxis
acute respiratory distress
rapid fall in blood pressure resembling
a shock-like state
angioedemadyspnea
asthma
purpura
angiitis
pulmonary edema
feverGENITOURINARY None hematuria
vaginal bleeding
proteinuria
nephrotic syndrome
interstitial nephritisBUN elevation
renal insufficiency, including renal failureMISCELLANEOUS None epistaxis
breast changes, including enlargement
and tenderness, or gynecomastia* Reactions occurring in 3% to 9% of patients treated with INDOCIN. (Those reactions occurring in less than 3% of the patients are unmarked.) Causal relationship unknown: Other reactions have been reported but occurred under circumstances where a causal relationship could not be established. However, in these rarely reported events, the possibility cannot be excluded. Therefore, these observations are being listed to serve as alerting information to physicians:
Cardiovascular: Thrombophlebitis
Hematologic: Although there have been several reports of leukemia, the supporting information is weak
Genitourinary: Urinary frequency
A rare occurrence of fulminant necrotizing fasciitis, particularly in association with Group Aβ hemolytic streptococcus, has been described in persons treated with nonsteroidal anti-inflammatory agents, including indomethacin, sometimes with fatal outcome
- Cardiovascular Thrombotic Events [see Warnings and Precautions (5.1)]
-
7
DRUG INTERACTIONS
See Table 2 for clinically significant drug interactions with indomethacin.
Table 2 Clinically Significant Drug Interactions with Indomethacin
Drugs That Interfere with Hemostasis Clinical Impact: - Indomethacin and anticoagulants such as warfarin have a synergistic effect on bleeding. The concomitant use of indomethacin and anticoagulants have an increased risk of serious bleeding compared to the use of either drug alone.
- Serotonin release by platelets plays an important role in hemostasis. Case-control and cohort epidemiological studies showed that concomitant use of drugs that interfere with serotonin reuptake and an NSAID may potentiate the risk of bleeding more than an NSAID alone.
Intervention: Monitor patients with concomitant use of INDOCIN with anticoagulants (e.g., warfarin), antiplatelet agents (e.g., aspirin), selective serotonin reuptake inhibitors (SSRIs), and serotonin norepinephrine reuptake inhibitors (SNRIs) for signs of bleeding [see Warnings and Precautions (5.11)]. Aspirin Clinical Impact: Controlled clinical studies showed that the concomitant use of NSAIDs and analgesic doses of aspirin does not produce any greater therapeutic effect than the use of NSAIDs alone. In a clinical study, the concomitant use of an INDOCIN and aspirin was associated with a significantly increased incidence of GI adverse reactions as compared to use of the INDOCIN alone [see Warnings and Precautions (5.2)]. Intervention: Concomitant use of INDOCIN and analgesic doses of aspirin is not generally recommended because of the increased risk of bleeding [see Warnings and Precautions (5.11)].
INDOCIN is not a substitute for low dose aspirin for cardiovascular protection.ACE Inhibitors, Angiotensin Receptor Blockers, and Beta-Blockers Clinical Impact: - NSAIDs may diminish the antihypertensive effect of angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), or beta-blockers (including propranolol).
- In patients who are elderly, volume-depleted (including those on diuretic therapy), or have renal impairment, co-administration of an NSAID with ACE inhibitors or ARBs may result in deterioration of renal function, including possible acute renal failure. These effects are usually reversible.
Intervention: - During concomitant use of INDOCIN and ACE-inhibitors, ARBs, or beta-blockers, monitor blood pressure to ensure that the desired blood pressure is obtained.
- During concomitant use of INDOCIN and ACE-inhibitors or ARBs in patients who are elderly, volume-depleted, or have impaired renal function, monitor for signs of worsening renal function [see Warnings and Precautions (5.6)].
- When these drugs are administered concomitantly, patients should be adequately hydrated. Assess renal function at the beginning of the concomitant treatment and periodically thereafter.
Diuretics Clinical Impact: Clinical studies, as well as post-marketing observations, showed that NSAIDs reduced the natriuretic effect of loop diuretics (e.g., furosemide) and thiazide diuretics in some patients. This effect has been attributed to the NSAID inhibition of renal prostaglandin synthesis.
It has been reported that the addition of triamterene to a maintenance schedule of
INDOCIN resulted in reversible acute renal failure in two of four healthy volunteers. INDOCIN and triamterene should not be administered together.
Both INDOCIN and potassium-sparing diuretics may be associated with increased serum potassium levels. The potential effects of INDOCIN and potassium-sparing diuretics on potassium levels and renal function should be considered when these agents are administered concurrently.
Intervention: Indomethacin and triamterene should not be administered together.
During concomitant use of INDOCIN with diuretics, observe patients for signs of worsening renal function, in addition to assuring diuretic efficacy including antihypertensive effects.
Be aware that indomethacin and potassium-sparing diuretics may both be associated with increased serum potassium levels [see Warnings and Precautions (5.6)].Digoxin Clinical Impact: The concomitant use of INDOCIN with digoxin has been reported to increase the serum concentration and prolong the half-life of digoxin. Intervention: During concomitant use of INDOCIN and digoxin, monitor serum digoxin levels. Lithium Clinical Impact: NSAIDs have produced elevations in plasma lithium levels and reductions in renal lithium clearance. The mean minimum lithium concentration increased 15%, and the renal clearance decreased by approximately 20%. This effect has been attributed to NSAID inhibition of renal prostaglandin synthesis. Intervention: During concomitant use of INDOCIN and lithium, monitor patients for signs of lithium toxicity. Methotrexate Clinical Impact: Concomitant use of NSAIDs and methotrexate may increase the risk for methotrexate toxicity (e.g., neutropenia, thrombocytopenia, renal dysfunction). Intervention: During concomitant use of INDOCIN and methotrexate, monitor patients for methotrexate toxicity. Cyclosporine Clinical Impact: Concomitant use of INDOCIN and cyclosporine may increase cyclosporine’s nephrotoxicity. Intervention: During concomitant use of INDOCIN and cyclosporine, monitor patients for signs of worsening renal function. NSAIDs and Salicylates Clinical Impact: Concomitant use of indomethacin with other NSAIDs or salicylates (e.g., diflunisal, salsalate) increases the risk of GI toxicity, with little or no increase in efficacy [see Warnings and Precautions (5.2)].
Combined use with diflunisal may be particularly hazardous because diflunisal causes significantly higher plasma levels of indomethacin [ see Clinical Pharmacology (12.3)]. In some patients, combined use of indomethacin and diflunisal has been associated with fatal gastrointestinal hemorrhage.Intervention: The concomitant use of indomethacin with other NSAIDs or salicylates, especially diflunisal, is not recommended. Pemetrexed Clinical Impact: Concomitant use of INDOCIN and pemetrexed may increase the risk of pemetrexed-associated myelosuppression, renal, and GI toxicity (see the pemetrexed prescribing information). Intervention: During concomitant use of INDOCIN and pemetrexed, in patients with renal impairment whose creatinine clearance ranges from 45 to 79 mL/min, monitor for myelosuppression, renal and GI toxicity.
NSAIDs with short elimination half-lives (e.g., diclofenac, indomethacin) should be avoided for a period of two days before, the day of, and two days following administration of pemetrexed.
In the absence of data regarding potential interaction between pemetrexed and NSAIDs with longer half-lives (e.g., meloxicam, nabumetone), patients taking these NSAIDs should interrupt dosing for at least five days before, the day of, and two days following pemetrexed administration.Probenecid Clinical Impact: When indomethacin is given to patients receiving probenecid, the plasma levels of indomethacin are likely to be increased. Intervention: During the concomitant use of INDOCIN and probenecid, a lower total daily dosage of indomethacin may produce a satisfactory therapeutic effect. When increases in the dose of indomethacin are made, they should be made carefully and in small increments. Effects on Laboratory Tests
INDOCIN reduces basal plasma renin activity (PRA), as well as those elevations of PRA induced by furosemide administration, or salt or volume depletion. These facts should be considered when evaluating plasma renin activity in hypertensive patients.
False-negative results in the dexamethasone suppression test (DST) in patients being treated with indomethacin have been reported. Thus, results of the DST should be interpreted with caution in these patients.
- Indomethacin and anticoagulants such as warfarin have a synergistic effect on bleeding. The concomitant use of indomethacin and anticoagulants have an increased risk of serious bleeding compared to the use of either drug alone.
-
8
USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Use of NSAIDs, including INDOCIN, during the third trimester of pregnancy increases the risk of premature closure of the fetal ductus arteriosus. Avoid use of NSAIDs, including INDOCIN, in pregnant women starting at 30 weeks of gestation (third trimester).
There are no adequate and well-controlled studies of INDOCIN in pregnant women.
Data from observational studies regarding potential embryofetal risks of NSAID use in women in the first or second trimesters of pregnancy are inconclusive. In the general U.S. population, all clinically recognized pregnancies, regardless of drug exposure, have a background rate of 2-4% for major malformations, and 15-20% for pregnancy loss. In animal reproduction studies retarded fetal ossification was observed with administration of indomethacin to mice and rats during organogenesis at doses 0.1 and 0.2 times, respectively, the maximum recommended human dose (MRHD, 200 mg (40 mL)). In published studies in pregnant mice, indomethacin produced maternal toxicity and death, increased fetal resorptions, and fetal malformations at 0.1 times the MRHD. When rat and mice dams were dosed during the last three days of gestation, indomethacin produced neuronal necrosis in the offspring at 0.1 and 0.05 times the MRHD, respectively [See Data]. Based on animal data, prostaglandins have been shown to have an important role in endometrial vascular permeability, blastocyst implantation, and decidualization. In animal studies, administration of prostaglandin synthesis inhibitors such as indomethacin, resulted in increased pre- and post-implantation loss.
Clinical Considerations
Labor or Delivery
There are no studies on the effects of INDOCIN during labor or delivery. In animal studies, NSAIDs, including indomethacin, inhibit prostaglandin synthesis, cause delayed parturition, and increase the incidence of stillbirth.
Data
Animal data
Reproductive studies were conducted in mice and rats at dosages of 0.5, 1.0, 2.0, and 4.0 mg/kg/day. Except for retarded fetal ossification at 4 mg/kg/day (0.1 times [mice] and 0.2 times [rats] the MRHD on a mg/m2 basis, respectively) considered secondary to the decreased average fetal weights, no increase in fetal malformations was observed as compared with control groups. Other studies in mice reported in the literature using higher doses (5 to 15 mg/kg/day, 0.1 to 0.4 times MRHD on a mg/m2 basis) have described maternal toxicity and death, increased fetal resorptions, and fetal malformations.
In rats and mice, maternal indomethacin administration of 4.0 mg/kg/day (0.2 times and 0.1 times the MRHD on a mg/m2 basis) during the last 3 days of gestation was associated with an increased incidence of neuronal necrosis in the diencephalon in the live-born fetuses however no increase in neuronal necrosis was observed at 2.0 mg/kg/day as compared to the control groups (0.1 times and 0.05 times the MRHD on a mg/m2 basis). Administration of 0.5 or 4.0 mg/kg/day to offspring during the first 3 days of life did not cause an increase in neuronal necrosis at either dose level.
8.2 Lactation
Risk Summary
Based on available published clinical data, indomethacin may be present in human milk. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for INDOCIN and any potential adverse effects on the breastfed infant from the INDOCIN or from the underlying maternal condition.
Data
In one study, levels of indomethacin in breast milk were below the sensitivity of the assay (<20 mcg/L) in 11 of 15 women using doses ranging from 75 mg orally to 300 mg rectally daily (0.94 to 4.29 mg/kg daily) in the postpartum period. Based on these levels, the average concentration present in breast milk was estimated to be 0.27% of the maternal weight-adjusted dose. In another study indomethacin levels were measured in breast milk of eight postpartum women using doses of 75 mg daily and the results were used to calculate an estimated infant daily dose. The estimated infant dose of indomethacin from breast milk was less than 30 mcg/day or 4.5 mcg/kg/day assuming breast milk intake of 150 mL/kg/day. This is 0.5% of the maternal weight-adjusted dosage or about 3% of the neonatal dose for treatment of patent ductus arteriosus.
8.3 Females and Males of Reproductive Potential
Infertility
Females
Based on the mechanism of action, the use of prostaglandin-mediated NSAIDs, including INDOCIN, may delay or prevent rupture of ovarian follicles, which has been associated with reversible infertility in some women. Published animal studies have shown that administration of prostaglandin synthesis inhibitors has the potential to disrupt prostaglandin-mediated follicular rupture required for ovulation. Small studies in women treated with NSAIDs have also shown a reversible delay in ovulation. Consider withdrawal of NSAIDs, including INDOCIN, in women who have difficulties conceiving or who are undergoing investigation of infertility.
8.4 Pediatric Use
Safety and effectiveness in pediatric patients 14 years of age and younger has not been established.
INDOCIN should not be prescribed for pediatric patients 14 years of age and younger unless toxicity or lack of efficacy associated with other drugs warrants the risk.
In experience with more than 900 pediatric patients reported in the literature or to the manufacturer who were treated with INDOCIN Capsules, side effects in pediatric patients were comparable to those reported in adults. Experience in pediatric patients has been confined to the use of INDOCIN Capsules.
If a decision is made to use indomethacin for pediatric patients two years of age or older, such patients should be monitored closely and periodic assessment of liver function is recommended. There have been cases of hepatotoxicity reported in pediatric patients with juvenile rheumatoid arthritis, including fatalities. If indomethacin treatment is instituted, a suggested starting dose is 1-2 mg/kg/day given in divided doses. Maximum daily dosage should not exceed 3 mg/kg/day or 150-200 mg/day, whichever is less. Limited data are available to support the use of a maximum daily dosage of 4 mg/kg/day or 150-200 mg/day, whichever is less. As symptoms subside, the total daily dosage should be reduced to the lowest level required to control symptoms, or the drug should be discontinued.
8.5 Geriatric Use
Elderly patients, compared to younger patients, are at greater risk for NSAID-associated serious cardiovascular, gastrointestinal, and/or renal adverse reactions. If the anticipated benefit for the elderly patient outweighs these potential risks, start dosing at the low end of the dosing range, and monitor patients for adverse effects [see Warnings and Precautions (5.1, 5.2, 5.3, 5.6, 5.13)].
Indomethacin may cause confusion or rarely, psychosis [see Adverse Reactions (6.1)]; physicians should remain alert to the possibility of such adverse effects in the elderly.
Indomethacin and its metabolites are known to be substantially excreted by the kidneys, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, use caution in this patient population, and it may be useful to monitor renal function [see Clinical Pharmacology (12.3)].
-
10
OVERDOSAGE
Symptoms following acute NSAID overdosages have been typically limited to lethargy, drowsiness, nausea, vomiting, and epigastric pain, which have been generally reversible with supportive care. Gastrointestinal bleeding has occurred. Hypertension, acute renal failure, respiratory depression, and coma have occurred, but were rare [see Warnings and Precautions (5.1, 5.2, 5.4, 5.6)].
Manage patients with symptomatic and supportive care following an NSAID overdosage. There are no specific antidotes. Consider emesis and/or activated charcoal (60 to 100 grams in adults, 1 to 2 grams per kg of body weight in pediatric patients) and/or osmotic cathartic in symptomatic patients seen within four hours of ingestion or in patients with a large overdosage (5 to 10 times the recommended dosage). Forced diuresis, alkalinization of urine, hemodialysis, or hemoperfusion may not be useful due to high protein binding.
For additional information about overdosage treatment contact a poison control center (1-800-222-1222).
-
11
DESCRIPTION
INDOCIN (indomethacin) Oral Suspension is a nonsteroidal anti-inflammatory drug, available as an oral suspension contain 25 mg of indomethacin per 5mL, alcohol 1%, and sorbic acid 0.1% added as a preservative for oral administration. The chemical name is -(4-chlorobenzoyl)-5-methoxy-2-methyl-1H-indole-3-acetic acid. The molecular weight is 357.8. Its molecular formula is C19H16ClNO4 , and it has the following chemical structure.
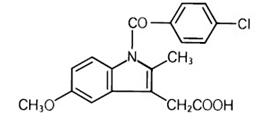
Indomethacin is a white to yellow crystalline powder. It is practically insoluble in water and sparingly soluble in alcohol. Indomethacin has a pKa of 4.5 and is stable in neutral or slightly acidic media and decomposes in strong alkali. The suspension has a pH of 4.0-5.0.
The inactive ingredients in INDOCIN include: antifoam AF emulsion, flavors, purified water, sodium hydroxide or hydrochloric acid to adjust pH, sorbitol solution, and tragacanth. INDOCIN Oral Suspension, 25 mg per 5 mL, is an off-white suspension with a pineapple coconut mint flavor.
-
12
CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Indomethacin has analgesic, anti-inflammatory, and antipyretic properties.
The mechanism of action of INDOCIN, like that of other NSAIDs, is not completely understood but involves inhibition of cyclooxygenase (COX-1 and COX-2).
Indomethacin is a potent inhibitor of prostaglandin synthesis in vitro. Indomethacin concentrations reached during therapy have produced in vivo effects. Prostaglandins sensitize afferent nerves and potentiate the action of bradykinin in inducing pain in animal models. Prostaglandins are mediators of inflammation. Because indomethacin is an inhibitor of prostaglandin synthesis, its mode of action may be due to a decrease of prostaglandins in peripheral tissues.
12.3 Pharmacokinetics
Absorption
Following single oral doses of INDOCIN Capsules 25 mg or 50 mg, indomethacin is readily absorbed, attaining peak plasma concentrations of about 1 and 2 mcg/mL, respectively, at about 2 hours. Orally administered INDOCIN Capsules are virtually 100% bioavailable, with 90% of the dose absorbed within 4 hours. A single 50 mg dose of INDOCIN Oral Suspension was found to be bioequivalent to a 50 mg INDOCIN Capsule when each was administered with food. With a typical therapeutic regimen of 25 or 50 mg three times a day, the steady-state plasma concentrations of indomethacin are an average 1.4 times those following the first dose.
Distribution
Indomethacin is highly bound to protein in plasma (about 99%) over the expected range of therapeutic plasma concentrations. Indomethacin has been found to cross the blood-brain barrier and the placenta, and appears in breast milk.
Elimination
Metabolism
Indomethacin exists in the plasma as the parent drug and its desmethyl, desbenzoyl, and desmethyldesbenzoyl metabolites, all in the unconjugated form. Appreciable formation of glucuronide conjugates of each metabolite and of indomethacin are formed.
Excretion
Indomethacin is eliminated via renal excretion, metabolism, and biliary excretion. Indomethacin undergoes appreciable enterohepatic circulation. About 60% of an oral dose is recovered in urine as drug and metabolites (26% as indomethacin and its glucuronide), and 33% is recovered in feces (1.5% as indomethacin). The mean half-life of indomethacin is estimated to be about 4.5 hours.
Specific Populations
Pediatric: The pharmacokinetics of INDOCIN has not been investigated in pediatric patients.
Race: Pharmacokinetic differences due to race have not been identified.
Hepatic Impairment: The pharmacokinetics of INDOCIN has not been investigated in patients with hepatic impairment.
Renal Impairment: The pharmacokinetics of INDOCIN has not been investigated in patients with renal impairment [see Warnings and Precautions (5.6)].
Drug Interaction Studies
Aspirin:
In a study in normal volunteers, it was found that chronic concurrent administration of 3.6 g of aspirin per day decreases indomethacin blood levels approximately 20% [see Drug Interactions (7)].
When NSAIDs were administered with aspirin, the protein binding of NSAIDs were reduced, although the clearance of free NSAID was not altered. The clinical significance of this interaction is not known. See Table 2 for clinically significant drug interactions of NSAIDs with aspirin [see Drug Interactions (7)].
Diflunisal:
In normal volunteers receiving indomethacin, the administration of diflunisal decreased the renal clearance and significantly increased the plasma levels of indomethacin [see Drug Interactions (7)].
-
13
NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
In an 81-week chronic oral toxicity study in the rat at doses up to 1 mg/kg/day (0.05 times the MRHD on a mg/m2 basis), indomethacin had no tumorigenic effect. Indomethacin produced no neoplastic or hyperplastic changes related to treatment in carcinogenic studies in the rat (dosing period 73 to 110 weeks) and the mouse (dosing period 62 to 88 weeks) at doses up to 1.5 mg/kg/day (0.04 times [mice] and 0.07 times [rats] the MRHD on a mg/m2 basis, respectively).
Mutagenesis
Indomethacin did not have any mutagenic effect in in vitro bacterial tests and a series of in vivo tests including the host-mediated assay, sex-linked recessive lethals in Drosophila, and the micronucleus test in mice.
Impairment of Fertility
Indomethacin at dosage levels up to 0.5 mg/kg/day had no effect on fertility in mice in a two generation reproduction study (0.01 times the MRHD on a mg/m2 basis) or a two litter reproduction study in rats (0.02 times the MRHD on a mg/m2 basis).
-
14
CLINICAL STUDIES
INDOCIN has been shown to be an effective anti-inflammatory agent, appropriate for long-term use in rheumatoid arthritis, ankylosing spondylitis, and osteoarthritis.
INDOCIN affords relief of symptoms; it does not alter the progressive course of the underlying disease.
INDOCIN suppresses inflammation in rheumatoid arthritis as demonstrated by relief of pain, and reduction of fever, swelling and tenderness. Improvement in patients treated with INDOCIN for rheumatoid arthritis has been demonstrated by a reduction in joint swelling, average number of joints involved, and morning stiffness; by increased mobility as demonstrated by a decrease in walking time; and by improved functional capability as demonstrated by an increase in grip strength. INDOCIN may enable the reduction of steroid dosage in patients receiving steroids for the more severe forms of rheumatoid arthritis. In such instances the steroid dosage should be reduced slowly and the patients followed very closely for any possible adverse effects.
- 16 HOW SUPPLIED/STORAGE AND HANDLING
-
17
PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide) that accompanies each prescription dispensed. Inform patients, families, or their caregivers of the following information before initiating therapy with INDOCIN and periodically during the course of ongoing therapy.
Cardiovascular Thrombotic Events
Advise patients to be alert for the symptoms of cardiovascular thrombotic events, including chest pain, shortness of breath, weakness, or slurring of speech, and to report any of these symptoms to their health care provider immediately [see Warnings and Precautions (5.1)].
Gastrointestinal Bleeding, Ulceration, and Perforation
Advise patients to report symptoms of ulcerations and bleeding, including epigastric pain, dyspepsia, melena, and hematemesis to their health care provider. In the setting of concomitant use of low-dose aspirin for cardiac prophylaxis, inform patients of the increased risk for and the signs and symptoms of GI bleeding [see Warnings and Precautions (5.2)].
Hepatotoxicity
Inform patients of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, pruritus, diarrhea, jaundice, right upper quadrant tenderness, and “flu-like” symptoms). If these occur, instruct patients to stop INDOCIN and seek immediate medical therapy [see Warnings and Precautions (5.3)].
Heart Failure and Edema
Advise patients to be alert for the symptoms of congestive heart failure including shortness of breath, unexplained weight gain, or edema and to contact their healthcare provider if such symptoms occur [see Warnings and Precautions (5.5)].
Anaphylactic Reactions
Inform patients of the signs of an anaphylactic reaction (e.g., difficulty breathing, swelling of the face or throat). Instruct patients to seek immediate emergency help if these occur [see Contraindications (4) and Warnings and Precautions (5.7)].
Serious Skin Reactions
Advise patients to stop INDOCIN immediately if they develop any type of rash and to contact their healthcare provider as soon as possible [see Warnings and Precautions (5.9)].
Female Fertility
Advise females of reproductive potential who desire pregnancy that NSAIDs, including INDOCIN, may be associated with a reversible delay in ovulation [see Use in Specific Populations (8.3)].
Fetal Toxicity
Inform pregnant women to avoid use of INDOCIN and other NSAIDs starting at 30 weeks gestation because of the risk of the premature closing of the fetal ductus arteriosus [see Warnings and Precautions (5.10) and Use in Specific Populations (8.1)].
Avoid Concomitant Use of NSAIDs
Inform patients that the concomitant use of INDOCIN with other NSAIDs or salicylates (e.g., diflunisal, salsalate) is not recommended due to the increased risk of gastrointestinal toxicity, and little or no increase in efficacy [see Warnings and Precautions (5.2) and Drug Interactions (7)]. Alert patients that NSAIDs may be present in “over the counter” medications for treatment of colds, fever, or insomnia.
Use of NSAIDs and Low-Dose Aspirin
Inform patients not to use low-dose aspirin concomitantly with INDOCIN until they talk to their healthcare provider [see Drug Interactions (7)].
Manufactured by:
Patheon Inc.
Whitby, Ontario L1N 5Z5, Canada
Distributed by:
Iroko Pharmaceuticals, LLC
Philadelphia, PA 19112
Issued: May 2018
-
MEDICATION GUIDE
Medication Guide for Nonsteroidal Anti-inflammatory Drugs (NSAIDs) What is the most important information I should know about medicines called Nonsteroidal Anti-inflammatory Drugs (NSAIDs)?
NSAIDs can cause serious side effects, including:
-
Increased risk of a heart attack or stroke that can lead to death. This risk may happen early in treatment and may increase:
○ with increasing doses of NSAIDs
○ with longer use of NSAIDs
Avoid taking NSAIDs after a recent heart attack, unless your healthcare provider tells you to. You may have an increased risk of another heart attack if you take NSAIDs after a recent heart attack.
-
Increased risk of bleeding, ulcers, and tears (perforation) of the esophagus (tube leading from the mouth to the stomach), stomach and intestines:
○ anytime during use
○ without warning symptoms
○ that may cause death
○ past history of stomach ulcers, or stomach or intestinal bleeding with use of NSAIDs
○ taking medicines called “corticosteroids”, “anticoagulants”, “SSRIs”, or “SNRIs”○ increasing doses of NSAIDs ○ older age ○ longer use of NSAIDs ○ poor health ○ smoking ○ advanced liver disease ○ drinking alcohol ○ bleeding problems NSAIDs should only be used:
○ exactly as prescribed
○ at the lowest dose possible for your treatment
○ for the shortest time neededWhat are NSAIDs?
NSAIDs are used to treat pain and redness, swelling, and heat (inflammation) from medical conditions such as different types of arthritis, menstrual cramps, and other types of short-term pain.Who should not take NSAIDs?
Do not take NSAIDs:- if you have had an asthma attack, hives, or other allergic reaction with aspirin or any other NSAIDs.
- right before or after heart bypass surgery.
Before taking NSAIDs, tell your healthcare provider about all of your medical conditions, including if you:
- have liver or kidney problems
- have high blood pressure
- have asthma
- are pregnant or plan to become pregnant. Talk to your healthcare provider if you are considering taking NSAIDs during pregnancy. You should not take NSAIDs after 29 weeks of pregnancy.
- are breastfeeding or plan to breast feed.
What are the possible side effects of NSAIDs?
NSAIDs can cause serious side effects, including:
See “What is the most important information I should know about medicines called Nonsteroidal Anti-inflammatory Drugs (NSAIDs)?”
- new or worse high blood pressure
- heart failure
- liver problems including liver failure
- kidney problems including kidney failure
- low red blood cells (anemia)
- life-threatening skin reactions
- life-threatening allergic reactions
- Other side effects of NSAIDs include: stomach pain, constipation, diarrhea, gas, heartburn, nausea, vomiting, and dizziness.
shortness of breath or trouble breathing slurred speech chest pain swelling of the face or throat weakness in one part or side of your body Stop taking your NSAID and call your healthcare provider right away if you get any of the following symptoms: nausea vomit blood more tired or weaker than usual there is blood in your bowel movement or it is black and sticky like tar diarrhea unusual weight gain itching skin rash or blisters with fever your skin or eyes look yellow swelling of the arms, legs, hands and feet indigestion or stomach pain flu-like symptoms If you take too much of your NSAID, call your healthcare provider or get medical help right away.
These are not all the possible side effects of NSAIDs. For more information, ask your healthcare provider or pharmacist about NSAIDs.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.Other information about NSAIDs - Aspirin is an NSAID but it does not increase the chance of a heart attack. Aspirin can cause bleeding in the brain, stomach, and intestines. Aspirin can also cause ulcers in the stomach and intestines.
- Some NSAIDs are sold in lower doses without a prescription (over-the-counter). Talk to your healthcare provider before using over-the-counter NSAIDs for more than 10 days.
General information about the safe and effective use of NSAIDs
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use NSAIDs for a condition for which it was not prescribed. Do not give NSAIDs to other people, even if they have the same symptoms that you have. It may harm them.
If you would like more information about NSAIDs, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about NSAIDs that is written for health professionals.Manufactured by:
Patheon Inc.
111 Consumers Dr.
Whitby ON L1N 5Z5 Canada
Distributed by:
Iroko Pharmaceuticals, LLC
One Kew Place
150 Rouse Boulevard
Philadelphia, PA 19112
For more information, go to www.iroko.com or call 1-877-757-0676This Medication Guide has been approved by the U.S. Food and Drug Administration. Issued or Revised: May 2016
-
Increased risk of a heart attack or stroke that can lead to death. This risk may happen early in treatment and may increase:
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
INDOCIN
indomethacin suspensionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 42211-101 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength INDOMETHACIN (UNII: XXE1CET956) (INDOMETHACIN - UNII:XXE1CET956) INDOMETHACIN 25 mg in 5 mL Inactive Ingredients Ingredient Name Strength WATER (UNII: 059QF0KO0R) SODIUM HYDROXIDE (UNII: 55X04QC32I) HYDROCHLORIC ACID (UNII: QTT17582CB) SORBITOL (UNII: 506T60A25R) TRAGACANTH (UNII: 2944357O2O) ALCOHOL (UNII: 3K9958V90M) SORBIC ACID (UNII: X045WJ989B) Product Characteristics Color Score Shape Size Flavor PINEAPPLE, COCONUT (artificial mint flavor compound) Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 42211-101-11 1 in 1 CARTON 10/10/1985 1 237 mL in 1 BOTTLE; Type 0: Not a Combination Product 2 NDC: 42211-101-01 1 in 1 CARTON 10/10/1985 2 50 mL in 1 BOTTLE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA018332 10/10/1985 Labeler - Iroko Pharmaceuticals, LLC (796831217)
Trademark Results [INDOCIN]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 INDOCIN 73445422 not registered Dead/Abandoned |
Merck & Co., Inc. 1983-09-26 |
 INDOCIN 72159596 0758725 Live/Registered |
MERCK & CO., INC. 1962-12-21 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.