STANDARDIZED MITE D FARINAE- dermatophagoides farinae injection, solution STANDARDIZED MITE D PTERONYSSINUS- dermatophagoides pteronyssinus injection, solution
STANDARDIZED MITE D PTERONYSSINUS by
Drug Labeling and Warnings
STANDARDIZED MITE D PTERONYSSINUS by is a Other medication manufactured, distributed, or labeled by Allergy Laboratories, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
-
BOXED WARNING
(What is this?)
WARNING
This product is intended for use by physicians who are experienced in the administration of allergenic extracts and the emergency care of anaphylaxis, or for use under the guidance of an allergy specialist.
Extracts standardized using the Allergy Unit may be more potent than extracts based on the weight to volume or PNU methods of expressing potency. Allergy Laboratories extract is not directly interchangeable with other allergenic extracts. The initial dose must be based on skin testing as described in the dosage and administration section of this insert. Patients being switched from other types of extracts to Allergy Laboratories should be started as though they were coming under treatment for the first time. Patients should be instructed to recognize adverse reaction symptoms and cautioned to contact physicians office if reaction symptoms occur. As with all allergenic extracts, severe systemic reactions may occur. In certain individuals these life threatening reactions may be fatal. Patients should be observed for at least 30 minutes following treatment and emergency measures as well as personnel trained in their use should be immediately available in the event of a life threatening reaction.
This product should not be injected intravenously. Subcutaneous injections are recommended.
Patients who are taking non-selective beta blockers may be more reactive to allergens given for testing or treatment and may be unresponsive to the usual doses of epinephrine used to treat allergic reactions.
Refer also to the warnings, precautions, adverse reactions and dosage sections below.
-
DESCRIPTION
The standardized mite extract contains the extractables of Dermatophagoides farinae or Dermatophagoides pteronyssinus. The standardized (Allergy Unit) extract in these vials is designed primarily for the physician equipped to prepare dilutions and mixtures as required. The extract is sterile and contains 50% (v/v) glycerine as a preservative. It is intended for subcutaneous injection. Source material for the mite extract is the whole bodies of the mite. The mites are grown on a medium containing yeast and pork and are processed in a manner to remove at least 99% of the growth medium. The medium contains no material of human origin. Several manufacturers submitted intradermal skin test data on an extract of mite medium from one supplier using patients who were puncture test reactive (∑ E ≥40mm) to mite extracts. By intradermal testing there was one reaction (∑ E ≥20mm) in 44 individuals at an estimated 1% level of medium content of mites, and 4 reactions in 40 individuals at an estimated 10% content. Two of the individuals who were skin test reactive to the mite extract and who were also skin test reactive to the mite medium extract were also skin tested by puncture method with an extract of yeast (Saccharomyces sp.) and were reactive.
The mite extract is standardized by assay using ELISA Competition (1) against a reference extract distributed by the Center for Biologics Evaluation and Research, U.S. Food and Drug Administration. Potency based on Allergy Units (AU/ml) is printed on the label. The F.D.A. reference extract has been assigned 10,000 AU/ml based on quantitative skin testing (2). The mite extract is labeled 10,000 AU/ml because it is statistically equivalent in potency to the reference extract.
- INACTIVE INGREDIENTS
-
CLINICAL PHARMACOLOGY
The allergic state is initiated by an immune response inducing B cells to produce IgE antibodies to specific allergens. IgE antibodies bind to surface receptors on mast cells and basophils.
When antigens gain access to the immune system they react with the bound IgE. The reacting antigen to the surface bound IgE stimulates a number of chemical mediators to be released from the mast cells and basophils. These include histamine, Eosinophil Chemotactic Factor (ECF-A) and leukotrienes. These chemical mediators are pharmacologically active at low concentrations and are partially responsible for the biological manifestation of the allergic response. (3)
The mechanism by which immunotherapy achieves hyposensitization is not completely understood. There is an increase in “blocking antibody” (IgG) titer and in some patients a decrease in specific IgE, a decrease in histamine release to specific allergen and an increase in suppressor cell population to specific allergen. These changes may occur only after prolonged therapy. (4)
-
INDICATIONS AND USAGE
Standardized mite extract is used for the diagnosis and treatment of allergic disease to mite. Diagnosis of allergic disease to mite is made through a combined medical history sufficiently complete to identify allergic symptoms to mite and identification of mite allergy by diagnostic skin testing.
Hyposensitization therapy to mite is treatment for patients exhibiting allergic reactions to mite. Immunotherapy is intended for patients whose symptoms cannot be satisfactorily controlled by avoidance of the offending allergen or by the use of symptomatic medications. (5)
-
CONTRAINDICATIONS
There are no known absolute contraindications to hyposensitization therapy. See precautions section for pregnancy risks.
A patient should not be treated with allergens unless a history of symptoms and a positive skin test reaction have been demonstrated. Allergenic extracts should only be administered to patients that show symptoms of allergy or asthma. The physician must determine if the benefits outweigh the risks in using these products for treating these patients.
Patients who are taking non-selective beta blockers may be more reactive to allergens given for testing or treatment and may be unresponsive to the usual doses of epinephrine used to treat allergic reactions.
WARNINGS See WARNINGS at the beginning of the instruction sheet.
Extracts standardized using the Allergy Unit may be more potent than extracts based on weight to volume or PNU methods of expressing potency. Comparative skin tests can be performed to determine the relative potency before initial use of new extracts. DO NOT GIVE ALLERGY INJECTIONS INTRAVENOUSLY. Subcutaneous injections are recommended. Injections may produce large local reactions that may be painful to the patient. DO NOT GIVE FULL STRENGTH INJECTIONS UNTIL THE COMPARATIVE STRENGTH IS DETERMINED. After inserting the needle, but before injecting extract, withdraw the plunger slightly. If blood appears in the syringe, re-insert the needle at another site. Careful selection of dose and injection should prevent most systemic reactions. -
PRECAUTIONS
(1) GENERAL:
The dosage should be reduced 50-75% from the previous dose when starting a patient on a new lot of standardized mite extract from the same manufacturer or from a different manufacturer. When changing from a non-standardized mite extract to a standardized mite extract the dose should be based upon comparative skin testing or the patient should be treated as though beginning treatment for the first time.
A separate sterile tuberculin type syringe should be used with each patient to prevent cross contamination of extracts. This will also prevent transmission of disease such as serum hepatitis, AIDS and other infectious diseases. Aseptic technique should always be used when injections of allergenic extracts are administered.
(2) INFORMATION FOR PATIENTS:
Because most serious reactions following the administration of allergenic extracts occur within 20 minutes of the injection, the patient should remain under observation for this period of time. The size of the local reaction should be recorded, because increasingly large local reaction may precede a subsequent systemic reaction with increasing dosage. The patient should be instructed to report any unusual reactions to the attention of the physician. In particular, this includes swelling and/or tenderness at the injection site or reactions such as rhinorrhea, sneezing, coughing, wheezing, shortness of breath, nausea, dizziness or faintness.
(3) DRUG INTERACTIONS:
Patients who are taking non-selective beta blockers may be more reactive to allergens given for testing or treatment and may be unresponsive to the usual doses of epinephrine used to treat allergic reactions. Antihistamines can significantly inhibit the immediate skin test reactions. Patients should be free of such medication for at least 48 hours before testing.
(4) CARCINOGENESIS, MUTAGENESIS, IMPAIRMENT OF FERTILITY:
Long term studies with extracts have not been conducted in animals to determine their potential for carcinogenesis, mutagenesis, or impairment of fertility.
(5) PREGNANCY: Pregnancy Category C.
Animal reproduction studies have not been conducted with allergenic extracts.
It is also not known whether allergenic extracts can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Allergenic extracts should be given to a pregnant woman only if clearly needed.
Controlled studies of hyposensitization with moderate to high doses of allergenic extracts in pregnant women have failed to demonstrate any risk to the mother or fetus. (6)
However, with histamines known ability to contract uterine muscles any reaction which would release significant amounts of histamine such as hyposensitization overdose should be avoided. The physician must weigh the benefits of immunotherapy against the risk of anaphylactic reactions that could result in harm to the mother and/or fetus.
Hyposensitization should be used during pregnancy only if clearly necessary and administered cautiously. If a woman is on maintenance dose, the occurrence of pregnancy is not an indication to stop injection therapy.
(6) NURSING MOTHERS:
It is not known if allergenic extracts are excreted in human milk therefore caution should be exercised when extracts are administered in nursing women.
(7) PEDIATRIC USE:
Standardized mite extract has not been studied in children, so the safety in children has not been established. Doses of allergenic extracts for children are generally the same as those for adults. The extracts may cause some pain or discomfort when injected. The maximum tolerated dose may be less than the adult dose due to the smaller size of the child. Therefore the volume of the dose may need to be adjusted from the adult schedules provided.
-
ADVERSE REACTIONS
(1). Local Reactions:
Some swelling and redness at the site of injection is not unusual. Mild burning that occurs immediately after the injection is normal; this usually subsides in 10 to 20 seconds. If the swelling and redness persist for a period of 24 hours or longer this should be a sign to proceed with caution in increasing the dosage. With the next injection the dosage should remain the same or be decreased. Large local reactions may indicate that a systemic reaction could occur with the next injection if the dosage was increased. If a patient continues to have reactions at the maintenance dose, the patient is considered to have exceeded the maximum tolerated dosage.
(2). Systemic Reactions:
Systemic reactions occur infrequently but must be looked for in all patients, especially highly sensitive patients. Anaphylactic shock and death are always possible, therefore, physicians must be prepared for the treatment of these reactions. Systemic reactions can also be characterized by one or more of the following symptoms: angioedema, tachycardia, conjunctivitis, cough, fainting, hypotension, pallor, rhinitis, urticaria and wheezing.
Systemic reaction can be treated by the immediate application of a tourniquet above the site of injection and the administration of 0.3 to 0.5ml of 1:1000 Epinephrine-Hydrochloride subcutaneously or intramuscularly at the site of allergen injection. The dosage may be repeated two times at 15 minute intervals. Loosen the tourniquet at least every 10 minutes.
The pediatric dosage for 1:1000 Epinephrine-Hydrochloride is 0.05 to 0.1ml for infants to 2 years of age; 0.15ml for children 2 to 6 years; and 0.2ml for children 6 to 12 years.
Patients should always be observed for at least 30 minutes after any injection. Hypotension can be reversed by using vasopressor agents and volume expanders. Parenteral aminophylline and inhalation bronchodilators may be required for bronchospasm. Oxygen may also be needed. Maintenance of an open airway is critical if upper airway obstruction is present. Adrenal corticosteroids and intravenous antihistamine can be given after adequate epinephrine and circulatory support has been administered. Physicians must be familiar with these systemic reactions and have all the equipment and drugs necessary for proper treatment. (7)
-
DOSAGE AND ADMINISTRATION
DIAGNOSTIC SKIN TESTING:
Puncture tests performed on 15 highly sensitive patients with 2 separate lots of 10,000 AU/ml Mite Extract (D. farinae) showed a mean sum of diameter wheal of 15.93mm ± 4.92 and a mean sum of diameter erythema of 63.70mm ± 16.46. Puncture tests performed on 10 highly sensitive patients with 10,000 AU/ml Mite Extract (D. pteronyssinus) showed a mean sum of diameter wheal of 17.00mm ± 3.39 and a mean sum of diameter erythema of 84.80mm ± 5.80.
Intradermal skin test results in highly sensitive patients is shown below using the same lots as used in the puncture tests above.
AU/ml to elicit 50mm sum of
Diameter of Erythema Reaction
ExtractsNumber
of Patients
MeanRange D. farinae 15 1.328 0.0024-9.410 D. pteronyssinus 10 0.008 0.0009-0.0287 Puncture tests with the mite growth medium as control were negative in 15 patients sensitive to mite.
These products are used to determine a patient’s sensitivity to specific antigens and aid in the diagnosis and treatment of atopic diseases. After a thorough history a decision can be made as to which allergens will be appropriate to use for testing. The recommended procedure is to initially perform puncture tests, then follow with intradermal tests. See recommended dosage below.
SCRATCH OR PUNCTURE TEST:
Concentration AU/ml Dosage ml 10,000 0.05
INTRADERMAL TEST: A. Patients with a negative scratch or puncture test. Concentration AU/ml Dosage ml 1) 50 AU/ml or 0.02 2)100 AU/ml * if 0.02 50 AU/ml is negative B. Patients tested by intradermal only. Concentration AU/ml Dosage ml 0.05 AU/ml 0.02 If negative repeat tests with stronger concentrations until a maximum of 100 AU/ml* is reached 0.02 *The negative intradermal control used for the 100 AU/ml concentration should contain
0.05% (v/v) glycerine.FREQUENCY OF ADMINISTRATION:
The number of skin tests applied at one time will depend on the particular patient and their allergic history. These tests should be performed and observed in 15 to 20 minutes. Additional tests may be applied in sequence. Perform tests on the anterolateral aspect of the upper arm on an area that permits the effective application of a tourniquet proximal to the site of the test. The skin at the site of injection should be disinfected with rubbing alcohol before testing.
Puncture testing: Apply one drop (0.05ml) of extract to the skin. Pierce the drop of extract and skin using a sterile hypodermic needle or vaccinating needle. Maintain the needle perpendicular to the skin surface and rock the needle back and forth to produce a small hole without bleeding. Do not rotate or gouge the needle. Remove needle from skin and wipe excess extract from skin surface.
Scratch testing: Using a scarifier or needle, make a scratch 1/16 inch long on the epidermis penetrating the outer cornified area but being careful not to draw blood. Apply one drop (0.05ml) of allergen to the scratch.
Intradermal testing: Use a separate sterile syringe (tuberculin type equipped with a 27 gauge by 3/8 inch needle with intradermal bevel) for each antigen. The tests are made by injecting 0.02ml of allergen into the epidermis. If the test has been performed properly, the solution should raise a bleb 2 to 3mm in diameter. If the bleb does not appear, the injection was made too deeply.
A negative control consisting of the same solution that the extract was prepared in should be applied to one of the sites in the same manner as the tests being performed. For example, the negative intradermal control should contain 0.5% (v/v) glycerine, if a 100 AU/ml concentration mite is used for intradermal testing. Histamine phosphate should be used as a positive control for evaluation of skin testing. Histamine phosphate is available from other manufacturers. See their directions for use, for recommended dosage and interpretation of results.
A positive reaction usually develops in 15-20 minutes. The positive response is a wheal and flare reaction that is larger than the negative control and judged on the size of the reaction. Scratch or puncture tests may not elicit as large and well defined reaction as the intradermal. (5)
The following system is recommended (8):
Reaction Erythema Wheal 0 < 5mm < 5mm + 5-10mm 5-10mm 1+ 11-20mm 5-10mm 2+ 21-30mm 5-10mm 3+ 31-40mm 10-15mm or
with pseudopods
>15mm or with
many pseudopods
4+ >40mm IMMUNOTHERAPY:
The following are two methods of injection therapy:
1. Pre-seasonal in which treatment is begun three months before seasonal difficulty begins and brought to maintenance dose by injections 4 to 7 days apart and discontinued after that season ends.
2. Perennial treatment is the recommended mode of therapy in which the patient is, by injection therapy, brought up to tolerated maintenance dose and remains at that dose until amelioration of allergic symptoms occurs. Injections may be given at intervals of 4 to 7 days.
Allergenic extracts must be diluted before use. Normally immunotherapy can be started with a 1 AU/ml dilution. If a patient appears to be extremely sensitive, dilutions of the antigen can further be made before injections are started. The following are suggested procedures for making a proper dilution series. Recommended diluents contain 0.9% sodium chloride and 0.4% phenol as a preservative. Allergenic extracts should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
TEN FOLD DILUTION SERIES Extract
VolumeExtract
Concentration AU/mLDiluent
VolumeDilution
Concentration AU/mL1 part 10,000 + 9 parts= 1,000 1 part 1,000 + 9 parts= 100 1 part 100 + 9 parts= 10 1 part 10+ 9 parts= 1 Perennial treatment may be started using the following dosage and dilution schedule. THIS SCHEDULE IS ONLY ILLUSTRATIVE AND HAS NOT BEEN SUBJECTED TO ADEQUATE OR WELL-CONTROLLED TRIALS TO DETERMINE EITHER ITS SAFETY OR EFFICACY.
dose #Dose
volume
Concentration1 0.05 1 AU/ml 2 0.10 3 0.20 4 0.30 5 0.40 6 0.50 7 0.05 10 AU/ml 8 0.10 9 0.20 10 0.30 11 0.40 12 0.50 13 0.05 100 AU/ml 14 0.10 15 0.20 16 0.30 17 0.40 18 0.50 19 0.05 1,000 AU/ml 20 0.10 21 0.20 22 0.30 23 0.40 24 0.50 25 0.05 10,000 AU/ml 26 0.10 27 0.20 28 0.30 29 0.40 30 0.50 Gradually increase the dose as outlined in the schedule. If you give a dose that causes a mild local reaction manifested by warmth or redness, repeat the same dose. If the reaction is severe or systemic (manifested as hives, asthma, or hay fever), drop back a dose in schedule and build again. If a severe local reaction or a systemic reaction is again encountered, this should be considered more than the maximum tolerance for this patient. The maintenance dose is the largest dose that relieves symptoms without producing local reactions. The size and interval of doses will vary and can be adjusted as necessary. The normal interval between doses is 4 to 7 days.
HOW SUPPLIED
Bulk extract (stock concentrate) in 50% (v/v) glycerine containing 10,000 AU/ml is supplied in 10ml, 30ml, and 50ml vials. Scratch testing in 50% (v/v) glycerine containing 10,000 AU/ml is supplied in 2ml dropper vials. Intradermal testing (aqueous) containing 100 AU/ml is supplied in 5ml vials.
STORAGE
These extracts should be stored at 2 to 8 degrees Celsius. Excessive heating (above room temperature) and repeated freeze-thawing should be avoided. The dating period (expiration date) is shown on the vial label. Once extracts are diluted the shelf life decreases. Extracts should be re-ordered when out of date. Please allow a minimum of three (3) weeks for delivery due to the holding period for sterility testing.
Revised 06/23/16
L-050-01
-
REFERENCES
1. ELISA Competition Assay, October 1993, In Methods of the Allergenics Products Testing Laboratory, Food and Drug Administration.
2. Turkeltaub, P., Rastogi, S.C., Baer, H.: Assignment of Allergy Units to Reference Preparations using the ID50EAL method, May 1986, In Methods of the Laboratory of Allergenic Products, Division of Bacterial Products, Food and Drug Administration.
3. Wasserman, S.I.: Biochemical mediators of allergic reactions. In Patterson, R. (ed): Allergic diseases: diagnosis and management, p. 86. Philadelphia, J.B. Lippincott Co. 1985.
4. Grammer, L.C.: Principle of immunologic management of allergic diseases due to extrinsic antigens. In Patterson, R. (ed): Allergic diseases: diagnosis and management, p. 358. Philadelphia, J.B. Lippincott Co. 1985.
5. Booth, B.H.: Diagnosis of Immediate Hypersensitivity. In Patterson, R. (ed): Allergic diseases: diagnosis and management, p. 102. Philadelphia, J.B. Lippincott Co. 1985.
6. Metzger, W.J., et al.: The safety of immunotherapy during pregnancy. J. Allergy Clin. Immunol., 64 (4): 268-272, 1978.
7. Patterson, R. et al.: Immunotherapy. In Middleton, E. Jr., Reed, C.E. and Ellis, E.F. (ed): Allergy; Principles and Practice, (Vol. 2) p. 1119, St. Louis, The C.V. Mosby Co. 1983.
8. Norman, P.S.: In vivo methods of study of allergy: Skin and Mucosal tests, techniques and interpretation. In Middleton, E Jr., Reed, C.E. and Ellis, E.F. (ed): Allergy Principles and Practice, (Vol 1), p. 258. St. Louis, The C.V. Mosby Co. 1978.
ALLERGY LABORATORIES, INC.
Oklahoma City, OK 73109U.S. License #103
(405) 235-1451 ∙ 800-654-3971
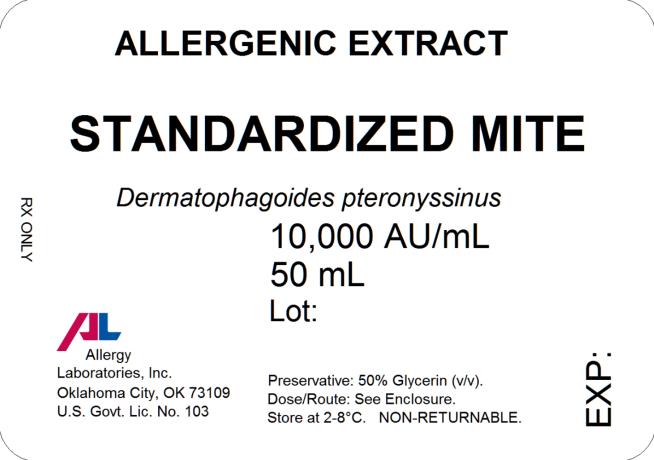
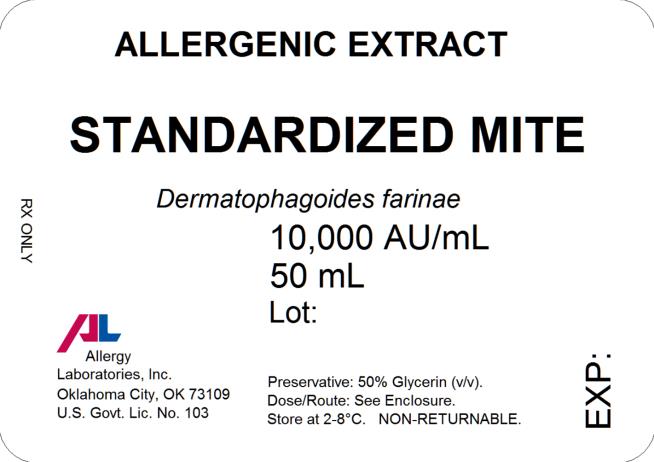
- PRINCIPAL DISPLAY PANEL
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
STANDARDIZED MITE D FARINAE
dermatophagoides farinae injection, solutionProduct Information Product Type STANDARDIZED ALLERGENIC Item Code (Source) NDC: 54575-325 Route of Administration PERCUTANEOUS, SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength DERMATOPHAGOIDES FARINAE (UNII: PR9U2YPF3Q) (DERMATOPHAGOIDES FARINAE - UNII:PR9U2YPF3Q) DERMATOPHAGOIDES FARINAE 10000 [AU] in 1 mL Inactive Ingredients Ingredient Name Strength GLYCERIN (UNII: PDC6A3C0OX) 0.5 mL in 1 mL SODIUM CHLORIDE (UNII: 451W47IQ8X) 0.00166 g in 1 mL SODIUM BICARBONATE (UNII: 8MDF5V39QO) 0.0091 g in 1 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 54575-325-02 2 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product 2 NDC: 54575-325-10 10 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product 3 NDC: 54575-325-30 30 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product 4 NDC: 54575-325-50 50 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA101377 01/25/1989 STANDARDIZED MITE D PTERONYSSINUS
dermatophagoides pteronyssinus injection, solutionProduct Information Product Type STANDARDIZED ALLERGENIC Item Code (Source) NDC: 54575-326 Route of Administration PERCUTANEOUS, SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength DERMATOPHAGOIDES PTERONYSSINUS (UNII: 57L1Z5378K) (DERMATOPHAGOIDES PTERONYSSINUS - UNII:57L1Z5378K) DERMATOPHAGOIDES PTERONYSSINUS 10000 [AU] in 1 mL Inactive Ingredients Ingredient Name Strength GLYCERIN (UNII: PDC6A3C0OX) 0.5 mL in 1 mL SODIUM CHLORIDE (UNII: 451W47IQ8X) 0.00166 g in 1 mL SODIUM BICARBONATE (UNII: 8MDF5V39QO) 0.0091 g in 1 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 54575-326-02 2 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product 2 NDC: 54575-326-10 10 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product 3 NDC: 54575-326-30 30 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product 4 NDC: 54575-326-50 50 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA101378 12/11/1991 Labeler - Allergy Laboratories, Inc. (007191810) Establishment Name Address ID/FEI Business Operations Allergy Laboratories, Inc. 007191810 MANUFACTURE(54575-325, 54575-326)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.