TRUBREXA- lidocaine and capsaicin patch
Trubrexa by
Drug Labeling and Warnings
Trubrexa by is a Prescription medication manufactured, distributed, or labeled by Strand Health Group. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
- 1. INDICATIONS & USAGE
-
2. DOSAGE & ADMINISTRATION
2.1 Important Dosage and Administration Instructions
- Unintended exposure to capsaicin can cause severe irritation of the eyes, mucous membranes, respiratory tract, and skin in healthcare providers and others.
- Because unintended exposure to capsaicin can cause severe irritation of eyes, mucous membranes, respiratory tract, and skin, when administering Trubrexa
TM Transdermal Patch it is important to follow these procedures:
- Keep Trubrexa TM Transdermal Patch in the sealed pouch until immediately before use.
- Use Trubrexa TM Transdermal Patch only on dry, intact (unbroken) skin.
- During administration, avoid unnecessary contact with any items in the room, including items that the patient may later have contact with, such as horizontal surfaces and bedsheets.
- Immediately after use, clean all areas of skin that had contact with Trubrexa TM Transdermal Patch.
- Ensure all used and unused pieces Trubrexa TM Transdermal Patch are properly disposed of.
2.2 Dosing and Instructions for Use
- Tear open pouch bag and remove one patch. Place remaining patches back in pouch bag and seal the pouch bag closed.
- Peel the clear plastic film away and apply Trubrexa TM Transdermal Patch to intact skin to cover the most painful area. Apply one patch per day for up to 12 hours within a 24 hour period (12 on, 12 off). One single Trubrexa TM Transdermal Patch may be used twice per day. To re-use after first application, place the clear plastic film back on to medicated hydrogel pad.
- Clothing may be worn over the area of application.
- Wash hands with soap and water after handling the patch.
- If irritation or a burning sensation occurs during application, remove the patch and do not reapply until the irritation subsides.
- When Trubrexa TM Transdermal Patch is used concomitantly with other products containing local anesthetic agents, the amount absorbed from all formulations must be considered.
-
3. DOSAGE FORMS & STRENGTHS
Trubrexa TM Transdermal Patch contains 4.75% lidocaine and 0.025% capsaicin. Each patch is 2 in x 2 in (5.08 cm x 5.08 cm) and consists of an adhesive side containing the active/inactive ingredients and an outer surface backing layer. The adhesive side is covered with a removable, clear, unprinted, plastic film. The outer surface of the backing layer is imprinted with the Trubrexa TM Transdermal Patch logo.
- 4. CONTRAINDICATIONS
-
5. WARNINGS, PRECAUTIONS & ADVERSE REACTIONS
5.1 Risk of Methemoglobinemia
Inform patients that use of local anesthetics may cause methemoglobinemia, a serious condition that must be treated promptly. Advise patients or caregivers to stop use and seek immediate medical attention if they or someone in their care experience the following signs or symptoms: pale, gray, or blue colored skin (cyanosis); headache; rapid heart rate; shortness of breath; fatigue; or lightheadedness.
Cases of methemoglobinemia have been reported in association with local anesthetic use. Although all patients are at risk for methemoglobinemia, patients with glucose-6-phosphate dehydrogenase deficiency, congenital or idiopathic methemoglobinemia, cardiac or pulmonary compromise, infants under 6 months of age, and concurrent exposure to oxidizing agents or their metabolites are more susceptible to developing clinical manifestations of the condition. If local anesthetics must be used in these patients, close monitoring for symptoms and signs of methemoglobinemia is recommended.
Signs of methemoglobinemia may occur immediately or may be delayed some hours after exposure and are characterized by cyanotic skin discoloration and/or abnormal coloration of the blood. Methemoglobin levels may continue to rise; therefore, immediate treatment is required to avert more serious central nervous system and cardiovascular adverse effects, including seizures, coma, arrhythmias, and death. Discontinue Trubrexa TM Transdermal Patch and any other oxidizing agents. Depending on the severity of the signs and symptoms, patients may respond to supportive care, i.e., oxygen therapy, hydration, etc. A more severe clinical presentation may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen.
5.2 Excessive Dosing
Excessive dosing by applying Trubrexa TM Transdermal Patch to larger areas or for longer than the recommended wearing time could result in increased absorption of lidocaine and capsaicin and high blood concentrations. Lidocaine toxicity could b e expected at lidocaine blood concentrations above 5 mcg/mL. The blood concentration of lidocaine is determined by the rate of systemic absorption and elimination. Longer duration of application, application of more than the recommended number of patches, smaller patients, or impaired elimination may all contribute to increasing the blood concentration of lidocaine and capsaicin.
5.3 Severe Irritation with Unintended Capsaicin Exposure
Unintended exposure to capsaicin can cause severe irritation of eyes, mucous membranes, respiratory tract, and skin.
Eye and Mucous Membrane Exposure
- Do not apply Trubrexa TM Transdermal Patch to the face, eyes, mouth, nose, or scalp to avoid risk of exposure to eyes or mucous membranes.
- Accidental exposure to the eyes and mucous membranes can occur from touching Trubrexa TM Transdermal Patch or items exposed to capsaicin, then touching the eyes and mucous membranes.
- If irritation of eyes or mucous membranes occurs, remove the affected individual from the vicinity of Trubrexa TM Transdermal Patch and flush eyes and mucous membranes with cool water.
Respiratory Tract Exposure
- Inhalation of airborne capsaicin can result in coughing or sneezing. If irritation of airways occurs, remove the affected individual from the vicinity of Trubrexa TM Transdermal Patch. Provide supportive medical care if shortness of breath develops.
Skin Exposure
- Thoroughly clean all areas that had contact with Trubrexa TM Transdermal Patch and properly dispose of all patch components.
5.4 Application-Associated Pain
During or immediately after treatment with Trubrexa TM Transdermal Patch, the skin at the site of application may develop blisters, bruising, burning sensation, depigmentation, dermatitis, discoloration, edema, erythema, exfoliation, irritation, papules, petechia, pruritus, vesicles, or may be the locus of abnormal sensation. These reactions are generally mild and transient, resolving spontaneously within a few minutes to hours.
5.5 Increase in Blood Pressure
Patient with unstable or poorly controlled hypertension, or a recent history of cardiovascular or cerebrovascular events, may be at increased risk of adverse cardiovascular effects. Consider these factors prior to initiating Trubrexa TM Transdermal Patch treatment. Monitor blood pressure periodically during and following the treatment procedure and provide adequate support for treatment-related pain.
5.6 Sensory Function
Decreases in sensory functions are generally minor and temporary (including to thermal and other harmful stimuli). All patients with pre-existing sensory deficits should be clinically assessed for signs of sensory deterioration or loss prior to each prescription of Trubrexa TM Transdermal Patch. If sensory deterioration or loss is detected or pre-existing sensory deficit worsens, continued use of Trubrexa TM Transdermal Patch treatment should be reconsidered.
5.7 Precautions
Allergic Reactions
Allergic and anaphylactoid reactions associated with lidocaine can occur. They are characterized by angioedema, bronchospasm, dermatitis, dyspnea, hypersensitivity, laryngospasm, pruritus, chock, and urticaria. If they occur, they should be managed by conventional means. Patients allergic to para-aminobenzoic acid derivates (procaine, tetracaine, benzocaine, etc.) have not shown cross-sensitivity to lidocaine. However, Trubrexa TM Transdermal Patch should be used with caution in patients with a history of drug sensitivities, especially if the etiologic agent is uncertain.
External Heat Sources
Placement of external heat sources, such as heating pads or electric blankets, over Trubrexa TM Transdermal Patch is not recommended.
Eye Exposure
The contact of Trubrexa TM Transdermal Patch with eyes should be avoided based on finding from previous studies with use of similar products. If eye contact occurs, immediately wash out the eye with water and saline and protect the eye until sensation returns.
Hepatic Disease
Patients with severe hepatic disease are at greater risk of developing toxic blood concentrations of lidocaine, because of their inability to metabolize lidocaine normally.
Non-Intact Skin
Trubrexa TM Transdermal Patch is only recommended for use on intact skin. Application to broken or inflamed skin may result in increased irritation and/or increased absorption of ingredients.
5.8 Other Adverse Events
Due to the nature and limitation of spontaneous reports in postmarketing surveillance, causality has not been established for additional reported adverse events including: asthenia, confusion, disorientation, dizziness, headache, hyperesthesia, hypoesthesia, lightheadedness, metallic taste, nausea, nervousness, pain exacerbated, paresthesia, somnolence, taste alteration, vomiting, visual disturbances such as blurred vision, flushing, tinnitus, and tremor.
5.9 Systemic (Dose-Related) Reactions
Systemic adverse reactions following appropriate use of Trubrexa TM Transdermal Patch are unlikely due to the small dose absorbed. Systemic adverse effects of lidocaine are similar in nature to those observed with other amide local anesthetic agents, including CNS excitation and/or depression (light headedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold, or numbness, twitching tremors, convulsions, unconsciousness, respiratory depression, and arrest). Excitatory CNS reactions may be brief or not occur at all, in which case the first manifestations may include bradycardia, hypotension, and cardiovascular collapse leading to arrest.
-
6. DRUG INTERACTIONS
Antiarrhythmic Drugs
Trubrexa TM Transdermal Patch should be used with caution in patients receiving Class I antiarrhythmic drugs (such as tocainide and mexiletine) since the toxic effects are additive and potentially synergistic.
Local Anesthetics
When Trubrexa TM Transdermal Patch is used concomitantly with other products containing local anesthetic agents, the amount absorbed from all formulations must be considered.
Drugs That May Cause Methemoglobinemia
Patients who are administered local anesthetics are at increased risk of developing methemoglobinemia when concurrently exposed to the following drugs, which could include other local anesthetics:
Nitrates/Nitrites (nitric oxide, nitroglycerin, nitroprusside, nitrous oxide)
Local anesthetics (benzocaine, bupivacaine, lidocaine, prilocaine, procaine, tetracaine)
Antineoplastic Agents (cyclophosphamide, flutamide, hydroxyurea, ifosfamide, rasburicase)
Antibiotics (dapsone, nitrofurantoin, para-aminosalicylic acid, sulfonamides)
Antimalarials (chloroquine, primaquine)
Anticonvulsants (Phenobarbital, phenytoin, sodium valproate)
Other Drugs (acetaminophen, metoclopramide, quinine, sulfasalazine)
-
7. USE IN SPECIFIC POPULATIONS
7.1 Pregnancy
Trubrexa TM Transdermal Patch has not been studied in pregnancy. Maternal use is not expected to result in fetal exposure. Animal studies have shown no adverse effects when lidocaine and capsaicin are administered and absorbed. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, Trubrexa TM Transdermal Patch should only be used during pregnancy if clearly needed or advised by a healthcare professional. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes.
7.2 Lactation
Trubrexa TM Transdermal Patch has not been studied in nursing mothers. Lidocaine is excreted in human milk, and the milk:plasma ration of lidocaine is 0.4. Capsaicin is negligibly absorbed systemically by the mother following topical administration of Trubrexa TM Transdermal Patch. Caution should be exercised when Trubrexa TM Transdermal Patch is administered to a nursing woman. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for Trubrexa TM Transdermal Patch and any potential adverse effects on the breastfed infant.
7.3 Pediatric Use
Safety and effectiveness in pediatric patients under the age of 12 have not been studied or established.
7.4 Geriatric Use
Safety and effectiveness are similar in geriatric patients and younger patients. No dose adjustments are required in geriatric patients.
-
8. OVERDOSAGE
Lidocaine overdose from cutaneous absorption is rare but could occur. If there is any suspicion of lidocaine overdose, drug blood concentration should be checked. The management of overdose includes close monitoring, supportive care, and symptomatic treatment. Dialysis is of negligible value in the treatment of acute overdose with lidocaine. In the absence of massive topical overdose or oral ingestion, evaluation of symptoms of toxicity should include consideration of other etiologies for the clinical effects, or overdosage from other sources of lidocaine or other local anesthetics. There is no specific antidote for overdose with capsaicin. In case of suspected overdose, remove Trubrexa TM Transdermal Patch and gently wash the area with soap and water. Use supportive measures and treat symptoms as clinically warranted.
-
9. DESCRIPTION
Trubrexa TM Transdermal Patch is comprised of an adhesive material containing 4.75% lidocaine and 0.025% capsaicin. Each patch is 2 in x 2 in (5.08 cm x 5.08 cm) and consists of an adhesive side containing the active/inactive ingredients and an outer surface backing layer with breathable fabric. The adhesive side is covered with a removable, clear, unprinted, plastic film. The outer surface of the backing layer is imprinted with the Trubrexa TM Transdermal Patch logo. 4 patches are included in each pouch bag. The inactive ingredients include: Arnica, Magnesium, Polyacrylate, Vegan Glycerol, and Water. Trubrexa TM Transdermal Patch is Latex Free, Paraben Free, and Vegan.
-
10. CLINICAL PHARMACOLOGY
10.1 Pharmacodynamics
Lidocaine is chemically designated as acetamide, 2-(diethylamino)-N-(2,6-dimethylphenyl), has an octanol:water partition ratio of 43 at pH 7.4. Capsaicin is soluble in alcohol, acetone, and ethyl acetate and very slightly soluble in water. Lidocaine is an amide-type local anesthetic agent and is suggested to stabilize neuronal membranes by inhibiting the ionic fluxes required for the initiation and conduction of impulses. The penetration of lidocaine into intact skin after application of Trubrexa TM Transdermal Patch is sufficient to produce an analgesic effect, but less than the amount necessary to produce a complete sensory block. Capsaicin is an agonist for the transient receptor potential vanilloid 1 receptor (TRPV1), which is an ion channel-receptor complex expressed on nociceptive nerve fibers in the skin. Topical administration of capsaicin causes an initial enhanced stimulation of the TRPV1-expressing cutaneous nociceptors that may be associated with painful sensations. This is followed by pain relief thought to be mediated by a reduction in TRPV1-expressing nociceptive nerve endings.
10.2 Pharmacokinetics
The amount of lidocaine and capsaicin systemically absorbed from Trubrexa TM Transdermal Patch is directly related to both the duration of application and the surface area over which it is applied. Systemic exposure decreases upon removal of Trubrexa TM Transdermal Patch. Lidocaine crosses the placental and blood brain barriers, presumably by passive diffusion. It is not known if lidocaine is metabolized in the skin. Lidocaine is metabolized rapidly by the liver to a number of metabolites, including monoethylglycinexylidide (MEGX) and glycinexylidide (GX), both of which have pharmacologic activity similar to, but less potent than that of lidocaine. Lidocaine and its metabolites are excreted by the kidneys.
-
11. NONCLINICAL TOXICOLOGY
11.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
A minor metabolite, 2,6-xylidine, has been found to be carcinogenic in rats. The blood concentration of this metabolite is negligible following application of Trubrexa TM Transdermal Patch.
Mutagenesis
Lidocaine HCl is not mutagenic in Salmonella/mammalian microsome test nor clastogenic in chromosome aberration assay with human lymphocytes and mouse micronucleus test.
Impairment of Fertility
The effect of Trubrexa TM Transdermal Patch on fertility has not been studied.
-
12. HOW SUPPLIED / STORAGE & HANDLING
12.1 How Supplied
Trubrexa TM Transdermal Patch comes in a sealed pouch bag. Each patch is 2 in x 2 in (5.08 cm x 5.08 cm) and consists of an adhesive side containing the active/inactive ingredients and an outer surface backing layer. The adhesive side is covered with a removable, clear, unprinted, plastic film. The outer surface of the backing layer is imprinted with the Trubrexa TM Transdermal Patch logo.
Trubrexa TM Transdermal Patch is available as a unit box containing 32 patches (8 pouch bags). NDC: 83295-4000-1
12.2 Storage
Store unit box between 68 o-77 o F (20 o-25 o C). Excursions between 15 o-30 o C (59 o-86 o F) are allowed. Keep Trubrexa TM Transdermal Patch in the sealed pouch bags until immediately before use.
12.3 Handling and Disposal
Unintended exposure to capsaicin can cause severe irritation of eyes, skin, respiratory tract, and mucous membranes. Avoid contact with your eyes, nose, or mouth. Keep used and unused patches out of the reach of children and pets. Pouch bags are not child resistant. Wash hands with soap and water after handling the patch. If irritation or a burning sensation occurs during application, remove the patch and do not reapply until the irritation subsides. After use, fold patches so that the adhesive side sticks to itself, then safely discard used patches where children and pets cannot get to them.
-
13. PATIENT COUNSELING INFORMATION
- Inform patients that accidental exposure to capsaicin from touching Trubrexa TM Transdermal Patch can cause severe irritation of eyes, mucous membranes, respiratory tract, and skin. If this occurs, patient should notify a healthcare professional immediately.
- Inform patients that the treated area may be sensitive to heat (e.g., hot showers/bath, direct sunlight, vigorous exercise) for a few days following treatment.
- Inform patients that as a result of treatment-related increases in pain, small transient increases in blood pressure may occur during and shortly after Trubrexa TM Transdermal Patch treatment and that blood pressure will be monitored during the treatment process. If any cardiovascular event occurs, patient should notify a healthcare professional immediately.
-
SPL UNCLASSIFIED SECTION
Manufactured for Strand Health Group, Las Vegas, NV 89102, USA.
Copyright © 2023 Strand Health Group, LLC. All Rights Reserved.
For comments or questions, please email cs@strandhealthgroup.com.
NDC: 83295-4000-1
Trubrexa TM Transdermal Patch
Extended Time Release
Rx Only
[Trubrexa Logo]
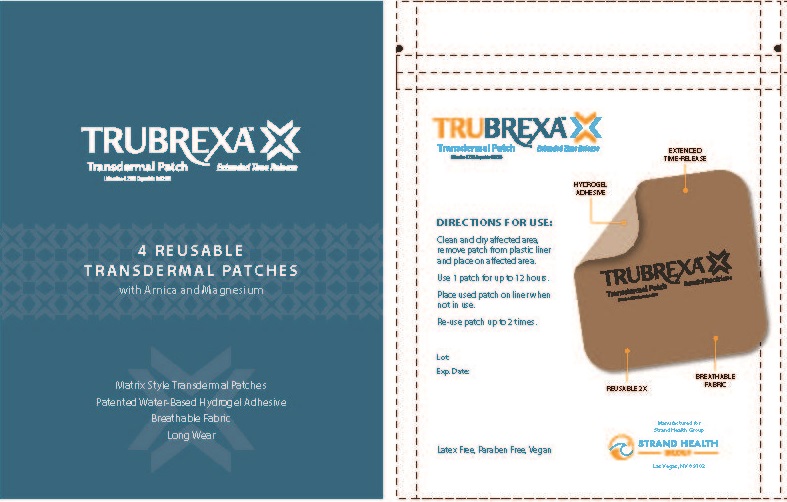
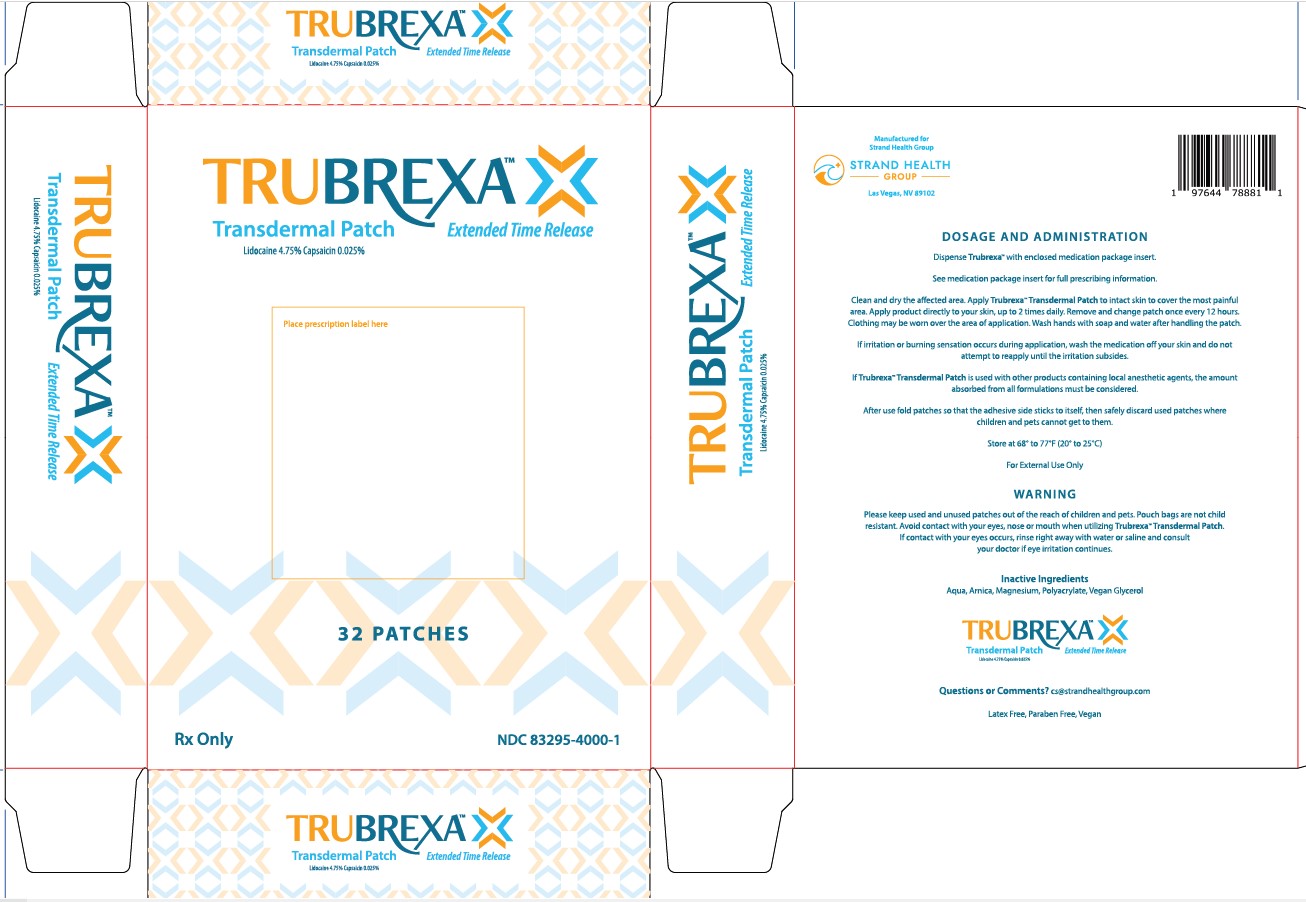
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
TRUBREXA
lidocaine and capsaicin patchProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 83295-4000 Route of Administration TRANSDERMAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CAPSAICIN (UNII: S07O44R1ZM) (CAPSAICIN - UNII:S07O44R1ZM) CAPSAICIN 0.00025 g in 1 g LIDOCAINE (UNII: 98PI200987) (LIDOCAINE - UNII:98PI200987) LIDOCAINE 0.0475 g in 1 g Inactive Ingredients Ingredient Name Strength GLYCERIN (UNII: PDC6A3C0OX) ARNICA MONTANA FLOWER (UNII: OZ0E5Y15PZ) POLYACRYLIC ACID (250000 MW) (UNII: 9G2MAD7J6W) MAGNESIUM (UNII: I38ZP9992A) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 83295-4000-1 8 in 1 BOX 10/03/2023 1 4 in 1 POUCH 1 2.7 g in 1 PATCH; Type 0: Not a Combination Product 2 NDC: 83295-4000-5 4 in 1 POUCH 10/03/2023 10/31/2023 2 2.7 g in 1 PATCH; Type 0: Not a Combination Product 3 NDC: 83295-4000-4 4 in 1 POUCH 10/03/2023 3 2.7 g in 1 PATCH; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date unapproved drug other 10/03/2023 Labeler - Strand Health Group (118929144)
Trademark Results [Trubrexa]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 TRUBREXA 98301732 not registered Live/Pending |
Strand Health Group LLC 2023-12-06 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.