EMROSI- minocycline hydrochloride extended-release capsule
EMROSI by
Drug Labeling and Warnings
EMROSI by is a Prescription medication manufactured, distributed, or labeled by Journey Medical Corporation, Dr. Reddy’s Laboratories Limited, Dr. Reddy’s Laboratories Limited-FTO SEZ PU-1. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use EMROSI safely and effectively. See full prescribing information for EMROSI.
EMROSI TM (minocycline hydrochloride) extended-release capsules, for oral use
Initial U.S. Approval: 1971INDICATIONS AND USAGE
EMROSI is a tetracycline-class drug indicated to treat inflammatory lesions (papules and pustules) of rosacea in adults. ( 1)
Limitations of Use
This formulation of minocycline has not been evaluated in the treatment or prevention of infections. To reduce the development of drug-resistant bacteria and to maintain the effectiveness of other antibacterial drugs, use EMROSI only as indicated. ( 1)
DOSAGE AND ADMINISTRATION
The recommended dosage of EMROSI is 40 mg orally, once daily. ( 2)
DOSAGE FORMS AND STRENGTHS
Extended-release capsules: 40 mg. ( 3)
CONTRAINDICATIONS
Known hypersensitivity to any of the tetracyclines. ( 4)
WARNINGS AND PRECAUTIONS
- Serious Skin/Hypersensitivity Reactions:Minocycline has been associated with anaphylaxis, serious skin reactions, erythema multiforme, and drug rash with eosinophilia and systemic symptoms (DRESS) syndrome. Discontinue EMROSI immediately if symptoms occur. ( 5.1)
- Tooth Discoloration and Enamel Hypoplasia:The use of EMROSI during tooth development (second and third trimesters of pregnancy, infancy, and childhood up to the age of 8 years) may cause permanent discoloration of the teeth (yellow-gray-brown). ( 5.2)
- Inhibition of Bone Growth:Use during the second and third trimesters of pregnancy, infancy, and childhood up to the age of 8 years may cause reversible inhibition of bone growth. ( 5.3)
- Clostridioides difficile-Associated Diarrhea (Antibiotic-Associated Colitis): Discontinue if Clostridioides difficile-associated diarrhea (antibiotic-associated colitis) occurs. ( 5.4)
- Hepatotoxicity:Discontinue EMROSI if liver injury is suspected. ( 5.5)
- Central Nervous System Effects:May cause central nervous system side effects including light-headedness, dizziness, or vertigo. ( 5.6)
- Idiopathic Intracranial Hypertension:May cause idiopathic intracranial hypertension in adults and adolescents. Discontinue EMROSI if symptoms occur. ( 5.7)
- Autoimmune Syndromes:Minocycline has been associated with autoimmune syndromes; discontinue EMROSI immediately if symptoms occur. ( 5.8)
- Metabolic Effects:If renal impairment exists, monitor serum levels of EMROSI during treatment, discontinue EMROSI if necessary. ( 5.9)
ADVERSE REACTIONS
The most commonly observed adverse reaction (incidence ≥1%) is dyspepsia. ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Journey Medical Corporation at 1-855-531-1859 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
Patients who are on anticoagulant therapy may require downward adjustment of their anticoagulant dosage. ( 7.1)
USE IN SPECIFIC POPULATIONS
Lactation: Breastfeeding is not recommended. ( 8.2)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 11/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity Reaction and Serious Skin Reactions
5.2 Tooth Discoloration and Enamel Hypoplasia
5.3 Inhibition of Bone Growth
5.4 Clostridioides difficile-Associated Diarrhea (Antibiotic-Associated Colitis)
5.5 Hepatotoxicity
5.6 Central Nervous System Effects
5.7 Idiopathic Intracranial Hypertension
5.8 Autoimmune Syndromes
5.9 Metabolic Effects
5.10 Photosensitivity
5.11 Tissue Hyperpigmentation
5.12 Development of Drug-Resistant Bacteria
5.13 Superinfection
5.14 Laboratory Monitoring
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Anticoagulants
7.2 Penicillin
7.3 Antacids and Iron Preparations
7.4 Drug/Laboratory Test Interactions
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
EMROSI is indicated to treat inflammatory lesions (papules and pustules) of rosacea in adults.
Limitations of Use
- This formulation of minocycline has not been evaluated in the treatment or prevention of infections.
- To reduce the development of drug-resistant bacteria as well as to maintain the effectiveness of other antibacterial drugs, use EMROSI only as indicated.
-
2 DOSAGE AND ADMINISTRATION
The recommended dosage of EMROSI is one capsule taken orally, once daily. Higher doses have not shown to be of additional benefit in the treatment of rosacea.
EMROSI may be taken with or without food [see Clinical Pharmacology (12.3)] . Ingestion of food along with EMROSI may help to reduce the risk of esophageal irritation and ulceration.
Swallow the capsule whole. Do not crush or chew the extended-release capsule.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
EMROSI is contraindicated in patients with a history of hypersensitivity to any of the tetracyclines [see Warnings and Precautions (5.1)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity Reaction and Serious Skin Reactions
Cases of anaphylaxis, serious skin reactions (e.g., Stevens-Johnson syndrome), erythema multiforme, and drug rash with eosinophilia and systemic symptoms (DRESS) syndrome have been reported postmarketing with minocycline use in patients with acne. DRESS syndrome consists of cutaneous reaction (such as rash or exfoliative dermatitis), eosinophilia, and one or more of the following visceral complications such as: hepatitis, pneumonitis, nephritis, myocarditis, and pericarditis. Fever and lymphadenopathy may be present. In some cases, death has been reported. If this syndrome is recognized, discontinue EMROSI immediately.
5.2 Tooth Discoloration and Enamel Hypoplasia
The use of tetracycline class drugs, including EMROSI during tooth development (second and third trimesters of pregnancy, infancy, and childhood up to the age of 8 years) may cause permanent discoloration of the teeth (yellow-gray-brown). Permanent discoloration of the teeth is more common during long-term use of tetracycline-class drugs but has been observed following repeated short-term courses. Enamel hypoplasia has also been reported. Use of EMROSI is not recommended during tooth development.
Advise the patient of the potential risk to the fetus if EMROSI is used during the second or third trimester of pregnancy [see Use in Specific Populations (8.1, 8.4)].
5.3 Inhibition of Bone Growth
The use of tetracycline-class drugs, including EMROSI, during the second and third trimesters of pregnancy, infancy, and childhood up to the age of 8 years may cause reversible inhibition of bone growth. All tetracyclines, including EMROSI, form a stable calcium complex in any bone-forming tissue. A decrease in fibula growth rate has been observed in premature human infants given oral tetracycline in doses of 25 mg/kg every 6 hours. This reaction was shown to be reversible when the drug was discontinued.
Advise the patient of the potential risk to the fetus if EMROSI is used during the second or third trimester of pregnancy [see Use in Specific Populations (8.1, 8.4)].
5.4 Clostridioides difficile-Associated Diarrhea (Antibiotic-Associated Colitis)
Clostridium difficileassociated diarrhea (CDAD) has been reported with nearly all antibacterial agents, including minocycline, and may range in severity from mild diarrhea to fatal colitis.
C. difficileproduces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficilecause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, discontinue EMROSI.
5.5 Hepatotoxicity
Postmarketing cases of serious liver injury, including irreversible drug-induced hepatitis and fulminant hepatic failure (sometimes fatal) have been reported with minocycline use in the treatment of acne. Discontinue EMROSI if liver injury is suspected.
5.6 Central Nervous System Effects
Central nervous system side effects including light-headedness, dizziness or vertigo have been reported with minocycline therapy. Caution patients who experience these symptoms about driving vehicles or using hazardous machinery while on EMROSI. These symptoms may disappear during therapy and usually rapidly disappear when the drug is discontinued.
5.7 Idiopathic Intracranial Hypertension
Idiopathic Intracranial hypertension has been associated with the use of tetracyclines. Clinical manifestations of idiopathic intracranial hypertension include headache, blurred vision, diplopia, and vision loss; papilledema can be found on fundoscopy. Women of childbearing age who are overweight or have a history of idiopathic intracranial hypertension are at a greater risk for developing idiopathic intracranial hypertension. Avoid concomitant use of isotretinoin and EMROSI because isotretinoin, a systemic retinoid, is also known to cause idiopathic intracranial hypertension.
Permanent visual loss may exist, even after the medication is discontinued. If visual disturbance occurs during treatment, prompt ophthalmologic evaluation is warranted. Because intracranial pressure can remain elevated for weeks after drug cessation, monitor patients until they stabilize.
5.8 Autoimmune Syndromes
Tetracyclines have been associated with the development of autoimmune syndromes. The long-term use of minocycline in the treatment of acne has been associated with drug-induced lupus-like syndrome, autoimmune hepatitis and vasculitis. Sporadic cases of serum sickness have presented shortly after minocycline use. Symptoms may be manifested by fever, rash, arthralgia, and malaise. Evaluate symptomatic patients. If symptoms occur, immediately discontinue EMROSI.
5.9 Metabolic Effects
The anti-anabolic action of the tetracyclines, including EMROSI, may cause an increase in blood urea nitrogen (BUN). In patients with significantly impaired renal function, higher serum levels of EMROSI may lead to azotemia, hyperphosphatemia, and acidosis. If renal impairment exists, monitor serum levels of EMROSI during treatment, and discontinue EMROSI if necessary.
5.10 Photosensitivity
Photosensitivity manifested by an exaggerated sunburn reaction has been observed in some individuals taking tetracyclines, including minocycline. Advise patients to minimize or avoid exposure to natural or artificial sunlight (tanning beds or UVA/B treatment) while using EMROSI. Instruct patients to use sunscreen products and wear protective apparel (e.g., hat) when exposure to sun cannot be avoided.
5.11 Tissue Hyperpigmentation
Tetracycline-class antibiotics are known to cause hyperpigmentation. EMROSI may induce hyperpigmentation in many organs, including nails, bone, skin, eyes, thyroid, visceral tissue, oral cavity (teeth, mucosa, alveolar bone), sclerae and heart valves. Skin and oral pigmentation has been reported to occur independently of time or amount of drug administration, whereas other tissue pigmentation has been reported to occur upon prolonged administration. Skin pigmentation includes diffuse pigmentation as well as over sites of scars or injury.
5.12 Development of Drug-Resistant Bacteria
Bacterial resistance to the tetracyclines may develop in patients using EMROSI, Because of the potential for drug-resistant bacteria to develop during the use of EMROSI, use EMROSI only as indicated.
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Serious Skin/Hypersensitivity Reactions [see Warnings and Precautions (5.1)]
- Clostridioides difficile-Associated Diarrhea (Antibiotic-Associated Colitis) [see Warnings and Precautions (5.4)]
- Hepatotoxicity [see Warnings and Precautions (5.5)]
- Central Nervous System Effects [see Warnings and Precautions (5.6)]
- Idiopathic Intracranial Hypertension [see Warnings and Precautions (5.7)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In two clinical trials, MVOR-1 and MVOR-2, a total of 638 adult subjects were analyzed under the safety population with 243 subjects in EMROSI group, 237 subjects in doxycycline (40 mg) group and 158 subjects in placebo group [see Clinical Studies (14)].
The most common adverse reaction reported by ≥1% of subjects treated with EMROSI and more frequently than in subjects receiving placebo was dyspepsia, which was reported in 2% of subjects treated with EMROSI and none of the subjects receiving placebo.
6.2 Postmarketing Experience
The following adverse reactions have been reported with post-approval use of minocycline hydrochloride in a variety of indications. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Skin and hypersensitivity reactions:anaphylaxis, angioedema, DRESS syndrome, erythema multiforme, Stevens-Johnson syndrome, acute febrile neutrophilic dermatosis (Sweet’s syndrome), fixed drug eruptions, balanitis, anaphylactoid purpura photosensitivity, pigmentation of skin and mucous membranes.
Autoimmune conditions:polyarthralgia, pericarditis, exacerbation of systemic lupus, pulmonary infiltrates with eosinophilia, lupus-like syndrome.
Central nervous system:idiopathic intracranial hypertension, bulging fontanels in infants, decreased hearing.
Endocrine:brown-black microscopic thyroid discoloration, abnormal thyroid function.
Oncology:thyroid cancer.
Oral:glossitis, dysphagia, tooth discoloration.
Gastrointestinal:enterocolitis, pancreatitis, hepatitis, liver failure.
Renal:acute renal failure.
Hematology:hemolytic anemia, thrombocytopenia, eosinophilia.
-
7 DRUG INTERACTIONS
7.1 Anticoagulants
Because tetracyclines have been shown to decrease plasma prothrombin activity, patients who are on anticoagulant therapy may require downward adjustment of their anticoagulant dosage.
7.2 Penicillin
Because bacteriostatic drugs may interfere with the bactericidal action of penicillin, avoid giving EMROSI in conjunction with penicillin.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Tetracycline-class drugs, including EMROSI, may cause permanent discoloration of deciduous teeth and reversible inhibition of bone growth when administered during the second and third trimesters of pregnancy [see Warnings and Precautions (5.2, 5.3) and Use in Specific Populations (8.4)]. A few postmarketing cases of limb reductions have been reported over decades of use; however, the association is unclear. The limited data from postmarketing reports are not sufficient to inform a drug-associated risk for birth defects or miscarriage.
In animal reproduction studies conducted in pregnant rats and rabbits, bent limb bones were observed following oral administration of minocycline hydrochloride during organogenesis at systemic exposure of approximately 7.1 and 4.8 times, respectively, the maximum recommended human dose (MRHD) based on AUC exposures (see Data).
If the patient becomes pregnant while taking this drug, advise the patient of the risk to the fetus and discontinue treatment.
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Human Data
The use of tetracycline class drugs, including EMROSI, during tooth development (second and third trimesters of pregnancy, infancy, and childhood up to the age of 8 years) may cause permanent discoloration of deciduous teeth (yellow-gray-brown). Permanent discoloration of the teeth is more common during long-term use of the drug but has been observed following repeated short-term courses [see Warnings and Precautions (5.2)].
Animal Data
Results of animal studies indicate that minocycline hydrochloride crosses the placenta, are found in fetal tissues, and can cause delayed skeletal development in the developing fetus. Evidence of embryotoxicity has been noted in animals treated early in pregnancy [see Warnings and Precautions (5.3)].
Minocycline hydrochloride induced skeletal malformations (bent limb bones) in fetuses when administered to pregnant rats and rabbits during the period of organogenesis at doses of 30 mg/kg/day and 100 mg/kg/day, respectively, (7.1 and 4.8 times, respectively, the MRHD based on AUC comparison). Reduced mean fetal body weight was observed in studies in which minocycline hydrochloride was administered to pregnant rats at an oral dose of 10 mg/kg/day (2.4 times the MRHD based on AUC comparison).
Minocycline hydrochloride was assessed for effects on peri- and post-natal development of rats in a study that involved oral administration to pregnant rats during the period of organogenesis through lactation at doses of 5, 10, or 50 mg/kg/day. In this study, body weight gain was significantly reduced in pregnant females that received 50 mg/kg/day (6 times the MRHD based on AUC comparison). No effects of treatment on the duration of the gestation period or the number of live pups born per litter were observed. Gross external anomalies observed in offspring of animals that received minocycline hydrochloride at 50 mg/kg/day included reduced body size, improperly rotated forelimbs, and reduced size of extremities. No effects were observed on the physical development, behavior, learning ability, or reproduction of the offspring of animals that received minocycline hydrochloride.
8.2 Lactation
Risk Summary
Tetracycline-class antibiotics, including minocycline, are present in breast milk following oral administration. There are no data on the effects of minocycline on milk production. Because of the potential for serious adverse reactions, including tooth discoloration and inhibition of bone growth, advise patients that breastfeeding is not recommended during EMROSI therapy and for 4 days after the final dose [see Warnings and Precautions (5.2, 5.3)].
8.4 Pediatric Use
The safety and effectiveness of EMROSI have not been established in pediatric patients.
Tooth discoloration and inhibition of bone growth have been observed in pediatric patients with the use of tetracycline class antibiotics [see Warnings and Precaution (5.2, 5.3)].
8.5 Geriatric Use
Of the 653 subjects in the phase 3 clinical trials of EMROSI, 101 (15.5%) subjects were 65 years of age and older and 25 (3.8%) were 75 years of age and older. No overall differences in safety or effectiveness of EMROSI have been observed between subjects 65 years of age and older and younger adult subjects.
- 10 OVERDOSAGE
-
11 DESCRIPTION
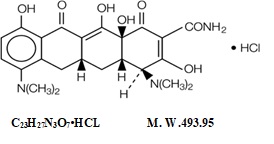
Minocycline hydrochloride, a semi synthetic derivative of tetracycline, is [4S-(4α,4aα,5aα,12aα)]-4,7-Bis(dimethylamino)-1,4,4a,5,5a,6,11,12a-octahydro-3,10,12,12a- tetrahydroxy-1,11-dioxo-2-naphthacenecarboxamide mono hydrochloride. Its molecular formula is C 23H 27N 3O 7HCl with a molecular weight of 493.95. Minocycline hydrochloride has the following structure:
Minocycline hydrochloride is a yellow, hygroscopic, crystalline powder. It is sparingly soluble in water, slightly soluble in ethanol (96%). A 1% w/v solution in water has pH between 3.5 and 4.5.
Each EMROSI extended-release capsule contains 40 mg of minocycline (equivalent to 43.19 mg of minocycline hydrochloride) as 10 mg immediate-release and 30 mg extended-release beads and the following inactive ingredients: ethyl cellulose, hypromellose, isopropyl alcohol, microcrystalline cellulose, Opadry ®clear, polyethylene glycol 400, triethyl citrate and talc. Opadry ®clear contains: hydroxypropyl cellulose and hypromellose. Capsule shell contains gelatin, iron oxide red and titanium dioxide. White ink contains ammonia, butyl alcohol, dehydrated alcohol, isopropyl alcohol, potassium hydroxide, propylene glycol, titanium dioxide and shellac.
-
12 CLINICAL PHARMACOLOGY
12.3 Pharmacokinetics
EMROSI is not bioequivalent to any other minocycline products. The pharmacokinetics of minocycline following administration of EMROSI was investigated in two studies that enrolled 32 healthy, adult subjects. In Study 1, the plasma pharmacokinetic parameters for EMROSI following single dose administration under fasting and fed states are presented in Table 1.
Table 1: Plasma Pharmacokinetic Parameters [Mean (%CV)] for EMROSI (40 mg)
N
C max
(ng/mL)
T max*
(hr)AUC inf
(ng.hr/mL)t 1/2
(hr)EMROSI (Fasting)
23
243.9
(37.3)1.50
(1.00 – 4.17)3933.6
(31.2)14.67
(26.7)EMROSI (Fed)
23
225.0
(16.7)4.50
(3.00 – 8.00)4404.1
(21.0)14.93
(21.5)Note: * Median (Range)
In Study 2, minocycline plasma PK following EMROSI single (Day 1) and after repeated (Day 21) once daily administrations in eight (8) subjects were found to be similar with overlapping ranges. The mean C maxwas 382.83 ng/mL versus 337.74 ng/mL and AUC 0-24was 3549.64 ng*hr/mL versus 3957.62 ng*hr/mL, respectively on Day 1 versus Day 21.Absorption:In Study 1, the median plasma T maxof minocycline from EMROSI was 1.50 hours (1.00 - 4.17). In Study 2, the median plasma T maxvalues of minocycline from EMROSI on Day 1 and Day 21 were 1.75 and 1.5 hours, respectively.
Effect of Food:Following administration of EMROSI with a high-fat meal (1011 Kcal, 53% fat), T maxwas delayed by approximately 3 hours. The high fat meal did not impact the C maxhowever, the AUC infwas increased by 15.26% ( Table 1) [see Dosage and Administration (2)].
Distribution:Minocycline is lipid soluble and distributes into the skin and sebum. In Study 1, the mean apparent volume of distribution (Vz/F) values of minocycline following oral administration of EMROSI at fasting and fed condition were 229.61 (±67.83) L and 199.83 (±43.71) L, respectively.
Elimination:The mean apparent elimination half-life (t ½) of minocycline from EMROSI was approximately 15 hours independent of fasting and fed dosing condition.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In an oral carcinogenicity study in rats in which minocycline hydrochloride was administered once daily for up to 104 weeks at doses up to 200 mg/kg/day, minocycline hydrochloride increased incidences of follicular cell tumors of the thyroid gland in both sexes, including adenomas, carcinomas, and the combined incidence of adenomas and carcinomas in males and adenomas and the combined incidence of adenomas and carcinomas in females. In an oral carcinogenicity study in mice in which minocycline hydrochloride was administered once daily for up to 104 weeks at doses up to 150 mg/kg/day, minocycline hydrochloride did not increase tumor incidence.
Minocycline hydrochloride was not mutagenic in vitro in a bacterial reverse mutation assay (Ames test) or CHO/HGPRT mammalian cell assay in the presence or absence of metabolic activation. Minocycline hydrochloride was not clastogenic in vitrousing human peripheral blood lymphocytes or in vivoin a mouse micronucleus test.
Male and female reproductive performance in rats was unaffected by oral doses of minocycline hydrochloride up to 300 mg/kg/day (95 times the MRHD based on AUC comparison). However, doses of 100 mg/kg/day (36 times the MRHD based on AUC comparison) and higher to male rats adversely affected spermatogenesis. At 100 mg/kg/day, minocycline increased morphological abnormalities, including absent heads, misshapen heads, and abnormal flagella. At 300 mg/kg/day, minocycline also reduced the number of sperm cells per gram of epididymis and reduced the percentage of motile sperm.
-
14 CLINICAL STUDIES
The safety and efficacy of EMROSI in the treatment of inflammatory lesions and erythema of rosacea was assessed in two 16-week, multi-center, randomized, double-blind, active- and placebo-controlled trials (MVOR-1 [NCT05296629] and MVOR-2 [NCT05343455]) in adults. In the two trials, a total of 653 subjects with papulopustular rosacea received EMROSI or doxycycline capsules 40 mg or placebo for up to 16 weeks.
Subjects were required to have an inflammatory lesion count (papules and pustules) in the range 15-60 lesions and an Investigator’s Global Assessment (IGA) score of 3 (“moderate”) or 4 (“severe”) at baseline.
The mean age of subjects was 49 years and subjects were from the following racial groups: White (93%), Asian (4%), Black or African American (2%), and Other (1%); for ethnicity, 38% of subjects identified as Hispanic or Latino. At baseline, subjects had a mean inflammatory lesion count of 25 (ranged 15 to 58), 88% were scored as moderate (IGA=3), and 12% were scored as severe (IGA=4).
The co-primary efficacy endpoints were the proportion of subjects with IGA ‛treatment success’ at Week 16 (defined as an IGA score of 0 [“clear”] or 1 [“near clear”] with at least a 2-grade reduction from baseline) and the absolute change from baseline in total inflammatory lesion counts at Week 16, in the EMROSI group compared to the placebo group. The efficacy results are presented in Table 2.
Table 2: Efficacy Results at Week 16 in Trials MVOR-1 and MVOR-2
Endpoint
Trial MVOR-1
Trial MVOR-2
EMROSI
(N=122)
Doxycycline
(N=121)
Placebo
(N=80)
EMROSI
(N=123)
Doxycycline
(N=125)
Placebo
(N=82)
IGA Treatment
Success 1
65%
46%
31%
60%
31%
27%
Difference from
Placebo (95% CI)
33% (20%, 46%)
34% (21%, 47%)
Difference from
Doxycycline (95% CI)
18% (5%, 31%)
28% (17%, 39%)
Inflammatory Lesion Counts
Mean 2Absolute Change from Baseline
-20.6
-15.6
-11.4
-18.1
-14.6
-11.2
Difference from
Placebo (95% CI)
-9.3 (-11.6, -6.9)
-6.9 (-9.1, -4.6)
Difference from
Doxycycline (95% CI)
-5.1 (-7.2, -2.9)
-3.4 (-5.4, -1.5)
Mean 2 Percent Change from Baseline
-79%
-63%
-47%
-75%
-60%
-46%
Difference from
Placebo (95% CI)
-33% (-41%, -24%)
-30% (-39%, -20%)
Difference from
Doxycycline (95% CI)
-16% (-24%, -8%)
-15% (-23%, -7%)
1Investigator’s Global Assessment (IGA) treatment success was defined as an IGA score of 0 or 1 with at least a 2-grade reduction from baseline.
2Means presented in table are Least Square (LS) means.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
How Supplied
EMROSI is an opaque, brownish-red colored, hard gelatin capsule, imprinted “MEC” on both cap and body with white ink.
Bottles of 30 capsules with child-resistant closure, NDC: 69489-131-30.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Advise patients taking EMROSI extended-release capsules of the following information and instructions:
Administration Instructions
- EMROSI should be taken exactly as directed.
- Advise patients to swallow EMROSI capsule whole and not to chew or crush the capsule [see Dosage and Administration (2)].
Serious Skin/Hypersensitivity Reactions
- Inform patients that serious skin reactions have occurred with minocycline use in patients with acne. Advise patients to discontinue use of EMROSI and contact their healthcare provider immediately at the first evidence of skin erythema [see Warnings and Precautions (5.1)].
Tooth Discoloration and Enamel Hypoplasia
- Advise patients that EMROSI use in pregnancy may cause permanent tooth discoloration of deciduous teeth. Advise patients to discontinue EMROSI during pregnancy and to inform their healthcare provider right away if they become pregnant during treatment [see Warnings and Precautions (5.2), Use in Specific Populations (8.1)].
Inhibition of Bone Growth
- Advise patients that EMROSI use in pregnancy may cause inhibition of fetal bone growth. Advise patients to discontinue EMROSI during pregnancy and to inform their healthcare provider right away if they become pregnant during treatment [see Warnings and Precautions (5.3), Use in Specific Populations (8.1)].
Clostridioides difficile-Associated Diarrhea (Antibiotic-Associated Colitis)
- Advise patients that Clostridioides difficile-associated diarrhea (antibiotic-associated colitis) can occur with minocycline therapy, including EMROSI. If patients develop watery or bloody stools, advise patients to seek medical attention [see Warnings and Precautions (5.4)].
Hepatotoxicity
- Inform patients about the possibility of hepatotoxicity. Advise patients to seek medical advice if they experience signs or symptoms of hepatotoxicity, including loss of appetite, tiredness, diarrhea, jaundice, bleeding easily, confusion, and sleepiness [see Warnings and Precautions (5.5)].
Central Nervous System Effects
- Inform patients that central nervous system adverse reactions including dizziness or vertigo have been reported with oral minocycline therapy. Caution patients about driving vehicles or using hazardous machinery if they experience such symptoms while on EMROSI [see Warnings and Precautions (5.6)].
Idiopathic Intracranial Hypertension
- Inform patients that idiopathic intracranial hypertension can occur with minocycline therapy. Advise patients to seek medical attention if they develop unusual headache, visual symptoms, such as blurred vision, diplopia, and vision loss [see Warnings and Precautions (5.7)].
Autoimmune Syndromes
- Inform patients that autoimmune syndromes, including drug-induced lupus-like syndrome, autoimmune hepatitis, vasculitis, and serum sickness have been observed with tetracycline-class drugs, including minocycline. Symptoms may be manifested by arthralgia, fever, rash, and malaise. Advise patients who experience such symptoms to immediately discontinue EMROSI and seek medical help [see Warnings and Precautions (5.8)].
Photosensitivity
- Inform patients that photosensitivity manifested by an exaggerated sunburn reaction has been observed in some individuals taking tetracyclines, including minocycline. Advise patients to minimize or avoid exposure to natural or artificial sunlight (i.e., tanning beds or UVA/B treatment) while using EMROSI. Instruct patients to use sunscreen and wear protective clothing (e.g., hat) over treated areas when exposure to sun cannot be avoided [see Warnings and Precautions (5.10)].
Tissue Hyperpigmentation
- Inform patients that EMROSI may cause discoloration of skin, scars, teeth, or gums [see Warnings and Precautions (5.11)] .
Lactation
- Advise patients that EMROSI therapy is not recommended during breast feeding for 4 days after the final dose [see Use in Specific Populations (8.2)].
Manufactured for:
Journey Medical Corporation
Scottsdale, AZ 85258EMR-P01-R01
EMROSI is a trademark of Journey Medical Corporation.
All other trademarks are the properties of their respective owners. Copyright © 2024, Journey Medical Corporation. All rights reserved.
-
PATIENT PACKAGE INSERT
PATIENT INFORMATION
EMROSI TM(em-ROH-see)
(minocycline hydrochloride)
extended-release capsules, for oral use
What is EMROSI?
EMROSI is a prescription medicine used to treat adults with pimples and bumps (inflammatory lesions) caused by a condition called rosacea.
It is not known if EMROSI is:
- safe and effective for the treatment of infections
- safe and effective in children under the age of 18 years
Who should not take EMROSI?
Do not take EMROSIif you are allergic to any tetracycline medicines. Ask your healthcare provider or pharmacist for a list of these medicines if you are not sure.
Before taking EMROSI, tell your healthcare provider about all of your medical conditions, including if you:
- have diarrhea or watery stools
- have liver problems
- have kidney problems
- have had increased pressure around your brain that may have cause vision problems
- are pregnant or plan to become pregnant. EMROSI may harm your unborn baby. Taking EMROSI while you are pregnant may cause serious side effects on the growth of bone and teeth of your baby. Stop taking EMROSI and call your healthcare provider right away if you become pregnant during treatment with EMROSI
- are breastfeeding or plan to breastfeed. EMROSI passes into your milk and may harm your baby. Do not breastfeed during treatment with EMROSI and for 4 days after your final dose
Tell your healthcare provider about all the other medicines you take,including prescription and over-the counter medicines, vitamins and herbal supplements.
EMROSI and other medicines may affect each other and cause serious side effects. EMROSI may affect the way other medicines work, and other medicines may affect how EMROSI works.
Especially tell your healthcare provider if you take:
- a blood thinner medicine
- penicillin antibiotic medicine
- antacids that contain aluminum, calcium, or magnesium or iron-containing medicines
- an acne medicine that contains isotretinoin
Ask your healthcare provider or pharmacist if you are not sure if your medicine is one that is listed above. Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist.
How should I take EMROSI?
- Take EMROSI exactly as your healthcare provider tells you
- Take EMROSI 1 time per day with or without food. Taking EMROSI with food may lower your chances of getting irritation or ulcers in your esophagus. Your esophagus is the tube that connects your mouth to your stomach
- Swallow EMROSI whole. Do not chew or crush the capsules
If you take too much EMROSI, call your healthcare provider or Poison Help line at 1-800-222-1222 or go to the nearest hospital emergency room right away.
What should I avoid while taking EMROSI?
- You should not drive or operate dangerous machinery until you know how EMROSI affects you. EMROSI may cause you to feel dizzy or lightheaded or have a spinning feeling (vertigo)
- Avoid sunlight or artificial sunlight, such as sunlamps and tanning beds during treatment with EMROSI. EMROSI can make your skin sensitive to the sun and artificial sunlight and you could get severe sunburn during treatment. Use sunscreen and wear a hat and protective clothing that covers your skin while out in the sunlight during treatment with EMROSI
What are the possible side effects of EMROSI?
EMROSI may cause serious side effects, including:
-
Serious skin and allergic reactionshave happened during treatment with minocycline. EMROSI may cause serious skin or allergic reactions that may also affect parts of your body such as your liver, lungs, kidneys, and heart. Sometimes these reactions can lead to death. Stop taking EMROSI and call your healthcare provider right away or go to the nearest hospital emergency room if you have any of the following signs or symptoms, including:
- skin redness, rash, hives, sores in your mouth, or your skin blisters and peels
- swelling of your face, eyes, lips, tongue, or throat
- trouble swallowing or breathing
- blood in your urine
- fever, yellowing of the skin or the whites of your eyes (jaundice), dark colored urine
- pain on the right side of the stomach area (abdominal pain)
- chest pain or abnormal heartbeats
- swelling in your legs, ankles, and feet
- Permanent tooth discoloration and problems with tooth enamel.EMROSI may permanently turn a baby or child's teeth yellow-grey-brown during tooth development. EMROSI may cause tooth enamel to not develop properly. You should not use EMROSI during tooth development. Tooth development happens in the second and third trimesters of pregnancy, and in children from birth to 8 years of age. See “Before taking EMROSI, tell your healthcare provider about all your medical conditions, including if you:”
- Slow bone growth.EMROSI may cause slow bone growth if it is used during the second and third trimesters of pregnancy and if it is used in infants and children up to 8 years of age. Slow bone growth is reversible after stopping treatment with EMROSI.
- Diarrhea (antibiotic associated colitis).Antibiotic associated colitis can happen with most antibiotics, including EMROSI. This type of diarrhea may be caused by an infection ( Clostridioides difficile) in your intestines and can be severe and lead to death. Call your healthcare provider right away if you get watery diarrhea, diarrhea that does not go away, or bloody stools.
-
Liver problems.EMROSI may cause serious liver problems that can lead to death.Stop taking EMROSI and call your healthcare provider right away if you get any of the following symptoms of liver problems:
- loss of appetite
- tiredness
- diarrhea
- yellowing of your skin or the whites of your eyes
- unexplained bleeding or bleeding easily than normal
- confusion
- sleepiness
- Central nervous system effects.See “ What should I avoid while taking EMROSI?” Central nervous system effects such as light headedness, dizziness, and a spinning feeling (vertigo) may go away during your treatment with EMROSI or if treatment is stopped.
- Increased pressure around the brain (idiopathic intracranial hypertension).This condition may lead to vision changes and permanent vision loss. You are more likely to get intracranial hypertension if you are a female who can have children, are overweight, and have already had intracranial hypertension. Stop taking EMROSI and tell your healthcare provider right away if you have unusual headaches, blurred vision, double vision, and vision loss.
- Immune system reactions including a lupus-like syndrome, hepatitis, and inflammation of blood or lymph vessels (vasculitis).Using EMROSI for a long time to treat acne may cause immune system reactions. Stop taking EMROSI and tell your healthcare provider right away if you get a fever, rash, joint pain, or body weakness.
- Sensitivity to sunlight (photosensitivity).See “ What should I avoid while taking EMROSI?”
- Discoloration (tissue hyperpigmentation).EMROSI may cause darkening of your nails, bone, skin, eyes, teeth, gums, scars, and internal organs.
The most common side effects of EMROSI includestomach upset or burning (dyspepsia) after eating or drinking.
Your healthcare provider may do blood tests and check you for side effects during treatment with EMROSI and may stop treatment if you develop certain side effects.
These are not all the side effects with EMROSI.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
You may also report side effects to Journey Medical Corporation at 1-855-531-1859.
How should I store EMROSI?
- Store EMROSI at room temperature between 68°F to 77°F (20°C to 25°C)
- EMROSI comes in a child-resistant package
- Keep EMROSI container tightly closed
- Keep EMROSI away from light, moisture, and excessive heat
- Do not eat desiccant
Keep EMROSI out of the reach of children
General information about the safe and effective use of EMROSI.
Medicines are sometimes prescribed for purposes other than those listed in the Patient Information leaflet. Do not use EMROSI for a condition for which it was not prescribed. Do not give EMROSI to other people, even if they have the same symptoms you have. It may harm them. You can ask your pharmacist or healthcare provider for information about EMROSI that is written for health professionals.What are the ingredients in EMROSI?
Active ingredient:minocycline hydrochloride
Inactive ingredients:ethyl cellulose, hypromellose, isopropyl alcohol, microcrystalline cellulose, Opadry clear, polyethylene glycol, triethyl citrate, and talc
Manufactured for:Journey Medical Corporation
Scottsdale, AZ 85258
For more information, go to www.journeymedicalcorp.comor call 1-855-531-1859This Patient Information has been approved by the U.S. Food and Drug Administration. Revised: 11/2024
EMR-P02-R01
EMROSI is a trademark of Journey Medical Corporation.
All other trademarks are the properties of their respective owners.Copyright © 2024, Journey Medical Corporation. All rights reserved.
-
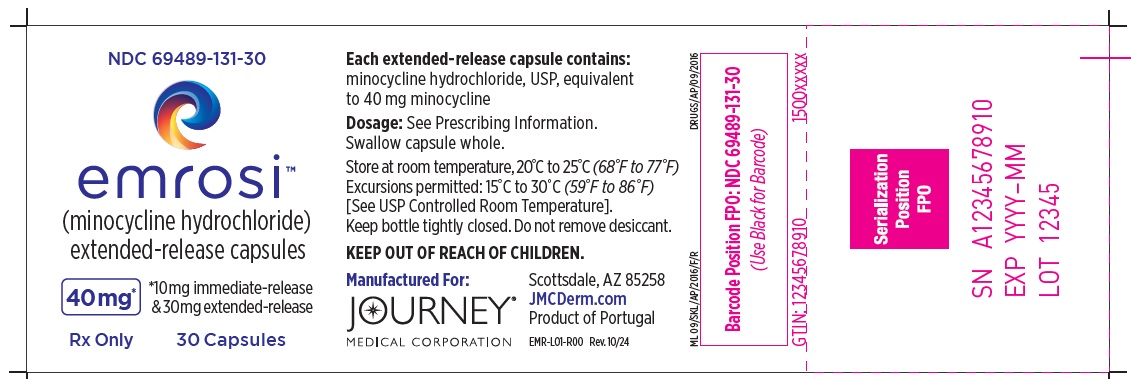
PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL
NDC: 69489-131-30
emrosi TM
(minocycline hydrochloride)
extended-release capsules
40mg*
*10mg immediate-release
& 30mg extended-releaseRx Only
30 Capsules
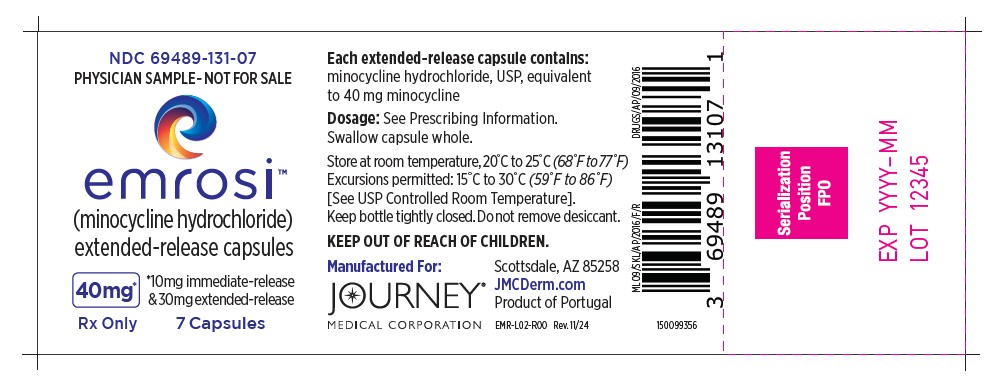
PRINCIPAL DISPLAY PANEL
NDC: 69489-131-07
PHYSICIAN SAMPLE-NOT FOR SALE
emrosi TM
(minocycline hydrochloride)
extended-release capsules
40mg*
*10mg immediate-release
& 30mg extended-releaseRx Only
7 Capsules
-
INGREDIENTS AND APPEARANCE
EMROSI
minocycline hydrochloride extended-release capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 69489-131 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength MINOCYCLINE HYDROCHLORIDE (UNII: 0020414E5U) (MINOCYCLINE - UNII:FYY3R43WGO) MINOCYCLINE 40 mg Inactive Ingredients Ingredient Name Strength ETHYLCELLULOSE, UNSPECIFIED (UNII: 7Z8S9VYZ4B) HYPROMELLOSES (UNII: 3NXW29V3WO) HYDROXYPROPYL CELLULOSE, UNSPECIFIED (UNII: 9XZ8H6N6OH) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) TRIETHYL CITRATE (UNII: 8Z96QXD6UM) TALC (UNII: 7SEV7J4R1U) GELATIN (UNII: 2G86QN327L) FERRIC OXIDE RED (UNII: 1K09F3G675) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) AMMONIA (UNII: 5138Q19F1X) SHELLAC (UNII: 46N107B71O) Product Characteristics Color brown (opaque, brownish-red color) Score no score Shape CAPSULE Size 16mm Flavor Imprint Code MEC;MEC Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 69489-131-30 30 in 1 BOTTLE; Type 0: Not a Combination Product 03/01/2025 2 NDC: 69489-131-07 7 in 1 BOTTLE; Type 0: Not a Combination Product 03/10/2025 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA219015 03/01/2025 Labeler - Journey Medical Corporation (079640860) Registrant - Dr. Reddy’s Laboratories Limited (862179079) Establishment Name Address ID/FEI Business Operations Dr. Reddy’s Laboratories Limited-FTO SEZ PU-1 860037244 analysis(69489-131) , manufacture(69489-131)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.