ATZUMI- dihydroergotamine mesylate powder
ATZUMI by
Drug Labeling and Warnings
ATZUMI by is a Prescription medication manufactured, distributed, or labeled by Satsuma Pharmaceuticals, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use ATZUMI safely and effectively. See full prescribing information for ATZUMI.
ATZUMI™ (dihydroergotamine) nasal powder
Initial U.S. Approval: 1946WARNING: PERIPHERAL ISCHEMIA FOLLOWING COADMINISTRATION WITH STRONG CYP3A4 INHIBITORS
See full prescribing information for complete boxed warning.
Serious and/or life-threatening peripheral ischemia has been associated with the coadministration of dihydroergotamine with strong CYP3A4 inhibitors. Because CYP3A4 inhibition elevates the serum levels of dihydroergotamine, the risk for vasospasm leading to cerebral ischemia and/or ischemia of the extremities is increased. Hence, concomitant use of ATZUMI with strong CYP3A4 inhibitors is contraindicated. (4, 5.1, 7.1)
INDICATIONS AND USAGE
DOSAGE AND ADMINISTRATION
- ATZUMI is for nasal administration only. (2.1)
- The recommended dose of ATZUMI is 5.2 mg, the contents of one nasal device, administered into one nostril. (2.1)
- To administer a dose, the white air pump of the ATZUMI device must be squeezed three separate times into one nostril. (2.1)
- The dose may be repeated, if needed, a minimum of 1 hour after the first dose. The maximum dose in a 24-hour period is 10.4 mg (two doses of ATZUMI 5.2 mg). (2.1)
- The safety of taking more than 4 doses within a 7-day period or 12 doses within a 30-day period has not been established. (2.1)
- Prior to initiation, a cardiovascular evaluation is recommended. (2.2)
DOSAGE FORMS AND STRENGTHS
Nasal powder: 5.2 mg (3)
CONTRAINDICATIONS
- Concomitant use of strong CYP3A4 inhibitors. (4)
- Ischemic heart disease or coronary artery vasospasm (4)
- Uncontrolled hypertension, peripheral arterial diseases, sepsis, following vascular surgery, or severe hepatic or renal impairment (4)
- Hypersensitivity to ergot alkaloids (4)
- Concomitant use of other 5-HT1 agonists or ergotamine-containing or ergot-type medications within 24 hours (4)
- Concomitant use of peripheral and central vasoconstrictors (4)
WARNINGS AND PRECAUTIONS
- Myocardial Ischemia and/or Infarction, Other Cardiac Adverse Reactions, and Fatalities: In patients with risk factors predictive of coronary artery disease, consider first dose administration under medical supervision with electrocardiogram. (5.2)
- Cerebrovascular Adverse Reactions and Fatalities: Cerebral hemorrhage, subarachnoid hemorrhage, and stroke have been reported; discontinue ATZUMI if suspected. (5.3)
- Other Vasospasm Related Adverse Reactions: ATZUMI may cause vasospasm or elevation in blood pressure. Discontinue if signs or symptoms of vasoconstriction develop. (5.4, 5.5)
- Medication Overuse Headache: Detoxification may be necessary. (5.6)
- Preterm Labor: Advise pregnant women of the risk. (5.7, 8.1)
- Fibrotic Complications: Pleural and retroperitoneal fibrosis have been reported following prolonged daily use of dihydroergotamine. Administration of ATZUMI should not exceed the dosing guidelines or be used for chronic daily administration. (5.8)
- Local Irritation: If severe local irritation occurs for no other attributable reason, suspend ATZUMI until resolution. (5.9)
ADVERSE REACTIONS
Most common adverse reactions (incidence > 1%) were rhinitis, nausea, altered sense of taste, application site reactions, dizziness, vomiting, somnolence, pharyngitis, and diarrhea. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Satsuma Pharmaceuticals, Inc. at toll-free phone # 1-888-273-2480 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 4/2025
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: PERIPHERAL ISCHEMIA FOLLOWING COADMINISTRATION WITH STRONG CYP3A4 INHIBITORS
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Dosing Information
2.2 Assessment Prior to First Dose
2.3 Administration Instructions
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Peripheral Ischemia Following Coadministration with Strong CYP3A4 Inhibitors
5.2 Myocardial Ischemia and/or Infarction, Other Cardiac Adverse Reactions, and Fatalities
5.3 Cerebrovascular Adverse Reactions and Fatalities
5.4 Other Vasospasm Related Adverse Reactions
5.5 Increase in Blood Pressure
5.6 Medication Overuse Headache
5.7 Preterm Labor
5.8 Fibrotic Complications
5.9 Local Irritation
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 CYP3A4 Inhibitors
7.2 Triptans
7.3 Beta Blockers
7.4 Vasoconstrictors
7.5 Nicotine
7.6 Selective Serotonin Reuptake Inhibitors
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
9.2 Abuse
9.3 Dependence
10 OVERDOSAGE
10.1 Symptoms
10.2 Treatment
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: PERIPHERAL ISCHEMIA FOLLOWING COADMINISTRATION WITH STRONG CYP3A4 INHIBITORS
Serious and/or life-threatening peripheral ischemia has been associated with the coadministration of dihydroergotamine with strong CYP3A4 inhibitors. Because CYP3A4 inhibition elevates the serum levels of dihydroergotamine, the risk for vasospasm leading to cerebral ischemia and/or ischemia of the extremities is increased. Hence, concomitant use of ATZUMI with strong CYP3A4 inhibitors is contraindicated [see Contraindications (4), Warnings and Precautions (5.1), and Drug Interactions (7.1)].
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Dosing Information
ATZUMI is for nasal administration only.
The recommended dose of ATZUMI is 5.2 mg (the contents of one nasal device) and is administered as a powdered medicine into one nostril [see Dosage and Administration (2.3)].
The dose may be repeated, if needed, a minimum of 1 hour after the first dose. The maximum dose in a 24-hour period is 10.4 mg (two doses of ATZUMI 5.2 mg). The safety of taking more than 4 doses in a 7-day period or 12 doses within a 30-day period has not been established.
2.2 Assessment Prior to First Dose
Prior to initiation of ATZUMI, a cardiovascular evaluation is recommended [see Warnings and Precautions (5.2)]. For patients with risk factors predictive of coronary artery disease who are determined to have a satisfactory cardiovascular evaluation, it is strongly recommended that administration of the first dose of ATZUMI take place in the setting of an equipped healthcare facility.
2.3 Administration Instructions
- Priming is not required.
- To administer a dose of ATZUMI, remove the round blue tab from the blue nozzle, and insert the blue nozzle into one nostril. Squeeze the white air pump 3 separate times into 1 nostril while inhaling. Allow the white air pump to expand back to its original shape between squeezes [see Instructions for Use].
- Fast, complete, pulse-like squeezes are needed to deliver the complete dose. Do not squeeze slowly, partially or with any hesitation.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
ATZUMI is contraindicated in patients:
- with concomitant use of strong CYP3A4 inhibitors [see Warnings and Precautions (5.1) and Drug Interactions (7.1)]
- with ischemic heart disease (e.g., angina pectoris, history of myocardial infarction, or documented silent ischemia) or patients who have clinical symptoms or findings consistent with coronary artery vasospasm, including Prinzmetal's variant angina [see Warnings and Precautions (5.4)]
- with uncontrolled hypertension [see Warnings and Precautions (5.5)]
- with peripheral arterial disease
- with sepsis
- following vascular surgery
- with severe hepatic impairment
- with severe renal impairment
- with known hypersensitivity to ergot alkaloids
- with recent use (i.e., within 24 hours) of other 5-HT1 agonists or ergotamine-containing or ergot-type medications [see Drug Interactions (7.2)]
- with concomitant use of peripheral and central vasoconstrictors because the combination may result in additive or synergistic elevation of blood pressure [see Warnings and Precautions (5.5)]
-
5 WARNINGS AND PRECAUTIONS
5.1 Peripheral Ischemia Following Coadministration with Strong CYP3A4 Inhibitors
Serious and/or life-threatening peripheral ischemia has been associated with the coadministration of dihydroergotamine with strong CYP3A4 inhibitors, including protease inhibitors, macrolide antibiotics, and antifungals. Because CYP3A4 inhibition elevates the serum levels of dihydroergotamine, the risk for vasospasm leading to cerebral ischemia and/or ischemia of the extremities is increased. Hence, concomitant use of ATZUMI with strong CYP3A4 inhibitors is contraindicated [see Contraindications (4) and Drug Interactions (7.1)].
5.2 Myocardial Ischemia and/or Infarction, Other Cardiac Adverse Reactions, and Fatalities
The potential for cardiac adverse reactions exists with ATZUMI treatment. Serious adverse cardiac events, including some that have been fatal, have occurred following use of dihydroergotamine. These events have included acute myocardial infarction, life-threatening disturbances of cardiac rhythm (e.g., ventricular tachycardia and ventricular fibrillation), coronary artery vasospasm, and transient myocardial ischemia.
Prior to initiation of ATZUMI, a cardiovascular evaluation is recommended to determine if the patient is free of coronary artery and ischemic myocardial disease or other significant underlying cardiovascular disease. If, during the cardiovascular evaluation, the patient's medical history (including risk factors), or electrocardiographic investigation, findings are consistent with coronary artery vasospasm or myocardial ischemia, ATZUMI should not be administered [see Contraindications (4)].
For patients with risk factors predictive of coronary artery disease (e.g., hypertension, hypercholesterolemia, smoker, obesity, diabetes, strong family history of coronary artery disease, females who are surgically or physiologically postmenopausal, or males who are over 40 years of age) who are determined to have a satisfactory cardiovascular evaluation, it is strongly recommended that administration of the first dose of ATZUMI take place in the setting of an equipped healthcare facility, unless the patient has previously received dihydroergotamine. During the interval immediately following the first use of ATZUMI, an electrocardiogram is recommended in those patients with risk factors because ischemia can occur in the absence of clinical symptoms.
5.3 Cerebrovascular Adverse Reactions and Fatalities
The potential for adverse cerebrovascular adverse reactions exists with ATZUMI treatment. Cerebral hemorrhage, subarachnoid hemorrhage, stroke, and other cerebrovascular events have been reported in patients treated with dihydroergotamine; and some have resulted in fatalities. In a number of cases, it appears possible that the cerebrovascular events were primary, the dihydroergotamine having been administered in the incorrect belief that the symptoms experienced were a consequence of migraine, when they were not. It should be noted that patients with migraine may be at increased risk of certain cerebrovascular events (e.g., stroke, hemorrhage, transient ischemic attack).
Discontinue ATZUMI if a cerebrovascular event is suspected.
5.4 Other Vasospasm Related Adverse Reactions
ATZUMI, like other ergot alkaloids, may cause vasospastic reactions other than coronary artery vasospasm. Myocardial, peripheral vascular, and colonic ischemia have been reported with dihydroergotamine.
Dihydroergotamine associated vasospastic phenomena may also cause muscle pains, numbness, coldness, pallor, and cyanosis of the digits. In patients with compromised circulation, persistent vasospasm may result in gangrene or death. ATZUMI should be discontinued immediately if signs or symptoms of vasoconstriction develop.
Patients who experience other symptoms or signs suggestive of decreased arterial flow, such as ischemic bowel syndrome or Raynaud's syndrome, following the use of any 5-HT1 agonist, including ATZUMI, should be evaluated by a healthcare provider.
5.5 Increase in Blood Pressure
Significant elevation in blood pressure has been reported on rare occasions in patients with and without a history of hypertension treated with dihydroergotamine. ATZUMI is contraindicated in patients with uncontrolled hypertension [see Contraindications (4)].
An 18% increase in mean pulmonary artery pressure was seen following dosing with another 5-HT1 agonist in a study evaluating subjects undergoing cardiac catheterization.
5.6 Medication Overuse Headache
Overuse of acute migraine drugs (e.g., ergotamines, triptans, opioids, or a combination of these drugs for 10 or more days per month) may lead to exacerbation of headache (i.e., medication overuse headache). Medication overuse headache may present as migraine-like daily headaches or as a marked increase in frequency of migraine attacks. Detoxification of patients including withdrawal of the overused drugs and treatment of withdrawal symptoms (which often includes a transient worsening of headache) may be necessary.
5.7 Preterm Labor
Based on the mechanism of action of dihydroergotamine and findings from the published literature, ATZUMI may cause preterm labor. Avoid use of ATZUMI during pregnancy [see Use in Specific Populations (8.1) and Clinical Pharmacology (12.2)].
5.8 Fibrotic Complications
The potential for fibrotic complications exists with ATZUMI treatment. There have been reports of pleural and retroperitoneal fibrosis in patients following prolonged daily use of dihydroergotamine . Rarely, prolonged daily use of other ergot alkaloid drugs has been associated with cardiac valvular fibrosis. Rare cases have also been reported in association with the use of dihydroergotamine; however, in those cases, patients also received drugs known to be associated with cardiac valvular fibrosis.
Administration of ATZUMI should not exceed the dosing guidelines and should not be used for chronic daily administration [see Dosage and Administration (2.1)].
5.9 Local Irritation
Local irritative symptoms were reported in 29% of patients treated with at least one dose of ATZUMI in an open-labeled trial, which allowed repeated use of ATZUMI up to 12 months. The common local irritative symptoms (at least 1% of patients) were nasal discomfort (11%), altered taste (8%), nasal congestion (5%), nasopharyngitis (5%), rhinorrhea (4%), cough (3%), nasal pain (3%), epistaxis (2%), sneezing (2%), nasal pruritus (1%), and increased lacrimation (1%). If a severe local irritation event occurs for no other attributable reasons, avoid further use of ATZUMI until the event resolves. Monitor patients for severe recurrent local irritation.
Nasal tissue in animals treated with dihydroergotamine mesylate daily showed mild mucosal irritation characterized by mucous cell and transitional cell hyperplasia and squamous cell metaplasia. Changes in rat nasal mucosa at 64 weeks were less severe than at 13 weeks. Local effects on respiratory tissue after chronic intranasal dosing in animals have not been evaluated.
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Peripheral Ischemia Following Coadministration with Strong CYP3A4 Inhibitors [see Boxed Warning and Warnings and Precautions (5.1)]
- Myocardial Ischemia and/or Infarction, Other Adverse Cardiac Events, and Fatalities [see Warnings and Precautions (5.2)]
- Cerebrovascular Adverse Reactions and Fatalities [see Warnings and Precautions (5.3)]
- Other Vasospasm Related Adverse Reactions [see Warnings and Precautions (5.4)]
- Increase in Blood Pressure [see Warnings and Precautions (5.5)]
- Medication Overuse Headache [see Warnings and Precautions (5.6)]
- Preterm Labor [see Warnings and Precautions (5.7)]
- Fibrotic Complications [see Warnings and Precautions (5.8)]
- Local Irritation [see Warnings and Precautions (5.9)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The studies described below were conducted with dihydroergotamine mesylate nasal spray; adverse reactions with ATZUMI nasal powder are expected to be similar to adverse reactions with dihydroergotamine mesylate nasal spray.
Adverse Reactions in Placebo-Controlled Trials with Dihydroergotamine Mesylate Nasal Spray [see Clinical Studies (14)]
Of the 1,796 patients and subjects treated with dihydroergotamine mesylate nasal spray doses 2 mg or less in U.S. and foreign clinical studies, 26 (1.4%) discontinued because of adverse events. The adverse events associated with discontinuation were, in decreasing order of frequency: rhinitis (13), dizziness (2), facial edema (2), and one patient each due to cold sweats, accidental trauma, depression, elective surgery, somnolence, allergy, vomiting, hypotension, and paraesthesia.
Table 1 summarizes the incidence rates of adverse reactions reported by at least 1% of patients who received dihydroergotamine mesylate nasal spray for the treatment of migraine during placebo-controlled, double-blind clinical studies and were more frequent than in those patients receiving placebo. The most commonly reported adverse reactions (greater than 1% of patients who received dihydroergotamine mesylate nasal spray) were rhinitis, nausea, altered sense of taste, application site reactions, dizziness, vomiting, somnolence, pharyngitis, and diarrhea. In most instances these events were transient and self-limited and did not result in patient discontinuation from a study.
Table 1 Adverse Reactions Reported by at Least 1% of the Dihydroergotamine Mesylate Nasal Spray Treated Patients and Occurred more Frequently than in the Placebo-Group in the Migraine Placebo-Controlled Trials Dihydroergotamine Mesylate Nasal Spray
N=597
%Placebo
N=631
%Respiratory System Rhinitis 26 7 Pharyngitis 3 1 Gastrointestinal System Nausea 10 4 Vomiting 4 1 Diarrhea 2 <1 Special Senses, Other Altered Sense of Taste 8 1 Application Site Application Site Reaction 6 2 Central and Peripheral Nervous System Dizziness 4 2 Somnolence 3 2 Body as a Whole, General Hot Flashes 1 <1 Asthenia 1 0 Musculoskeletal System Stiffness 1 <1 Adverse Reactions in Studies with ATZUMI
An open-label study in adults was conducted to evaluate the safety and tolerability of ATZUMI, with repeated use of ATZUMI over the course of 6 to 12 months. A total of 344 patients with migraine received at least one dose of ATZUMI. One hundred and eighty-eight patients treated on average at least two migraines per month for at least 6 months, and 86 patients treated at least two migraines per month for at least one year. Of the patients who received at least one dose of ATZUMI, 99 (29%) experienced local irritative symptoms. Of these, the most common local irritative symptoms (at least 5% of patients) were nasal discomfort, altered taste, nasal congestion, and nasopharyngitis [see Warnings and Precautions (5.9)]. The most common adverse reaction resulting in discontinuation in the long-term safety study was nasal discomfort (1.5%).
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of dihydroergotamine. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure:
- Vasospasm, paresthesia, hypertension, dizziness, anxiety, dyspnea, headache, flushing, diarrhea, rash, increased sweating, and pleural and retroperitoneal fibrosis after long-term use of dihydroergotamine. Cases of myocardial infarction and stroke have been reported following the use of dihydroergotamine [see Warnings and Precautions (5.2)].
-
7 DRUG INTERACTIONS
7.1 CYP3A4 Inhibitors
There have been rare reports of serious adverse events in connection with the coadministration of intravenous administration of dihydroergotamine and strong CYP3A4 inhibitors, resulting in vasospasm that led to cerebral ischemia and/or ischemia of the extremities [see Warnings and Precautions (5.1)]. The use of strong CYP3A4 inhibitors with ATZUMI is contraindicated [see Contraindications (4)]. Administer moderate CYP3A4 inhibitors with caution.
7.2 Triptans
Triptans (serotonin [5-HT] 1B/1D receptor agonists) have been reported to cause coronary artery vasospasm, and its effects could be additive with ATZUMI. Therefore, triptans and ATZUMI should not be taken within 24 hours of each other [see Contraindications (4)].
7.3 Beta Blockers
There have been reports that propranolol may potentiate the vasoconstrictive action of ergotamine by blocking the vasodilating property of epinephrine.
7.4 Vasoconstrictors
ATZUMI is contraindicated for use with peripheral and central vasoconstrictors because the combination may cause synergistic elevation of blood pressure [see Warnings and Precautions (5.5)].
7.5 Nicotine
Nicotine may provoke vasoconstriction in some patients, predisposing to a greater ischemic response to ergot therapy [see Warnings and Precautions (5.2, 5.4)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Available data from published literature indicate an increased risk of preterm delivery with dihydroergotamine, the active moiety in ATZUMI, use during pregnancy. Avoid use of ATZUMI during pregnancy [see Warnings and Precautions (5.7)]. Data collected over decades have shown no increased risk of major birth defects or miscarriage with the use of dihydroergotamine during pregnancy.
In animal reproduction studies, adverse effects on development were observed following intranasal administration of dihydroergotamine mesylate during pregnancy (decreased fetal body weight and/or skeletal ossification) in rats and rabbits or during pregnancy and lactation in rats (decreased body weight and impaired reproductive function in the offspring) at doses that were not associated with maternal toxicity (see Data).
All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriages in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. The estimated rate of major birth defects (2.2% to 2.9%) and miscarriage (17%) among deliveries to women with migraine are similar to rates reported in women without migraine.
Data
Animal Data
Intranasal administration of dihydroergotamine mesylate to pregnant rats throughout the period of organogenesis resulted in decreased fetal body weight and/or skeletal ossification at doses of 0.16 mg/day and greater. A no-effect level for adverse effects on embryofetal development was not identified in rats.
Intranasal administration of dihydroergotamine mesylate to pregnant rabbits throughout organogenesis resulted in decreased skeletal ossification at 3.6 mg/day. The no-effect dose for adverse effects on embryofetal development in rabbits was 1.2 mg/day.
Intranasal administration of dihydroergotamine mesylate to female rats throughout pregnancy and lactation resulted in decreased body weight and impaired reproductive function (decreased mating indices) in the offspring at doses of 0.16 mg/day or greater. A no-effect dose for adverse effects on pre- and postnatal development in rats was not established. Effects on offspring development occurred at doses below those that produced evidence of significant maternal toxicity in these studies.
Dihydroergotamine-induced intrauterine growth retardation has been attributed to reduced uteroplacental blood flow resulting from prolonged vasoconstriction of the uterine vessels and/or increased myometrial tone.
8.2 Lactation
Risk Summary
There are no data on the presence of dihydroergotamine in human milk; however, ergotamine, a related drug, is present in human milk. There are reports of diarrhea, vomiting, weak pulse, and unstable blood pressure in breastfed infants exposed to ergotamine. ATZUMI may reduce milk supply because it may decrease prolactin levels. Because of the potential for reduced milk supply and serious adverse events in the breastfed infant, including diarrhea, vomiting, weak pulse, and unstable blood pressure, advise patients not to breastfeed during treatment with ATZUMI and for 3 days after the last dose. Breast milk supply during this time should be pumped and discarded.
8.4 Pediatric Use
The safety and effectiveness of ATZUMI have not been established in pediatric patients.
8.5 Geriatric Use
Clinical studies of ATZUMI and other dihydroergotamine products did not include sufficient numbers of subjects aged 65 and older to determine whether they respond differently from younger subjects. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or other drug therapy.
-
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
ATZUMI contains dihydroergotamine (as the mesylate salt), which is not a controlled substance.
9.2 Abuse
Abuse is the intentional, non-therapeutic use of a drug, even once, for its desirable psychological or physiological effects. Currently available data have not demonstrated drug abuse with dihydroergotamine. However, cases of drug abuse in patients on other forms of ergot therapy have been reported.
9.3 Dependence
Physical dependence is a state that develops as a result of physiological adaptation in response to repeated drug use, manifested by withdrawal signs and symptoms after abrupt discontinuation or a significant dose reduction of a drug. Currently available data have not demonstrated physical or psychological dependence with dihydroergotamine. However, cases of psychological dependence in patients on other forms of ergot therapy have been reported.
-
10 OVERDOSAGE
10.1 Symptoms
Excessive doses of dihydroergotamine may result in peripheral signs and symptoms of ergotism. In general, the symptoms of an acute ATZUMI overdose may be similar to those of an ergotamine overdose, although there may be less pronounced nausea and vomiting with ATZUMI. The symptoms of an ergotamine overdose include the following: numbness, tingling, pain, and cyanosis of the extremities associated with diminished or absent peripheral pulses; respiratory depression; an increase and/or decrease in blood pressure, usually in that order; confusion, delirium, convulsions, and coma; and/or some degree of nausea, vomiting, and abdominal pain.
In laboratory animals, dihydroergotamine mesylate was lethal when given at intravenous doses of 44 mg/kg in mice, 130 mg/kg in rats, and 37 mg/kg in rabbits.
10.2 Treatment
Treatment of an overdose of ATZUMI should consist of discontinuation of the drug, general supportive measures including monitoring of vital signs, and observation of the clinical status of the patient for at least 24 hours, or while symptoms or signs persist. Consider contacting the Poison Help line (1-800-222-1222) or a medical toxicologist for additional overdose management recommendations.
-
11 DESCRIPTION
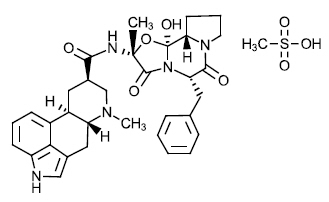
ATZUMI contains dihydroergotamine, an ergotamine derivative, as the mesylate salt. Dihydroergotamine mesylate is a white or almost white crystalline powder. It is slightly soluble in water and chloroform and sparingly soluble in methanol. The chemical designation for dihydroergotamine mesylate is (6aR,9R,10aR)-N-[(2R,5S,10aS,10bS)-5-benzyl-10b-hydroxy-2-methyl-3,6-dioxo-octahydro-8H-oxazolo[3,2-α]pyrrolo[2,1-c]pyrazin-2-yl]-7-methyl- 4,6,6a,7,8,9,10,10a-octahydroindolo[4,3-fg]quinoline-9-carboxamide methanesulphonate. The empirical formula is C33H37N5O5 ∙ CH4O3S. The molecular weight is 679.80, and it has the following structure:
ATZUMI contains dihydroergotamine 5.2 mg (equivalent to 6.0 mg dihydroergotamine mesylate).
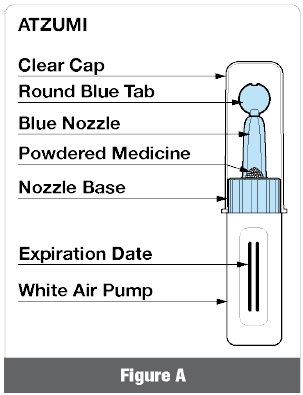
ATZUMI nasal powder is a drug-device combination product consisting of a powder prefilled in a single-dose delivery device for nasal administration into one nostril. ATZUMI does not need to be assembled or primed before use. Inactive ingredients are hypromellose, mannitol, and microcrystalline cellulose.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Dihydroergotamine binds with high affinity to 5-HT1Dα and 5-HT1Dβ receptors.
The therapeutic activity of dihydroergotamine in migraine is generally attributed to the agonist effects at 5-HT1D receptors.
12.2 Pharmacodynamics
Significant elevation in blood pressure has been reported in patients treated with dihydroergotamine with and without a history of hypertension [see Warnings and Precautions (5.5)].
Dihydroergotamine possesses oxytocic properties [see Warnings and Precautions (5.7)].
12.3 Pharmacokinetics
Absorption
Following ATZUMI administration, the mean maximum plasma concentration was 2.1 ng/mL, and the median time from dosing to maximum plasma concentration was approximately 0.5 hours.
Distribution
Dihydroergotamine is 93% plasma protein bound. The apparent steady-state volume of distribution is approximately 800 liters.
Elimination
The mean apparent half-life of dihydroergotamine following nasal administration of ATZUMI in healthy subjects is approximately 13 hours.
Metabolism
Four dihydroergotamine mesylate metabolites have been identified in human plasma following oral administration. The major metabolite, 8'-β-hydroxydihydroergotamine, exhibits affinity equivalent to its parent for adrenergic and 5-HT1 receptors and demonstrates equivalent potency in several venoconstrictor activity models, in vivo and in vitro. The other metabolites, (i.e., dihydrolysergic acid, dihydrolysergic amide) and a metabolite formed by oxidative opening of the proline ring are of minor importance.
Following nasal administration of ATZUMI, the 8'-β-hydroxydihydroergotamine metabolite plasma AUC was approximately 16% of the plasma AUC of dihydroergotamine, and the mean Cmax (5.7% of parent) was below the minimal concentrations required for receptor binding for adrenergic and 5-HT1 receptors.
Excretion
The major excretory route of dihydroergotamine is via the bile in the feces. The total body clearance following ATZUMI administration is 1.5 L/min which reflects mainly hepatic clearance. The renal clearance (0.1 L/min) is unaffected by the route of dihydroergotamine administration based on other dihydroergotamine products.
Specific Populations
No studies have been conducted on the effect of renal or hepatic impairment, gender, race, ethnicity, or pregnancy on dihydroergotamine pharmacokinetics [see Contraindications (4), Use in Specific Populations (8.1)].
Drug Interaction Studies
CYP3A4 Inhibitors
In a drug interaction study, administration of ATZUMI with itraconazole increased dihydroergotamine plasma exposure by 14% for Cmax and 19% for AUC while the plasma exposures (Cmax and AUC0-inf) of 8'-β-hydroxy dihydroergotamine (8'-OH-DHE, active metabolite) were increased by approximately 4-fold and 3-fold, respectively [see Contraindications (4), Warnings and Precautions (5.1), Drug Interactions (7.1)].
Other Drugs
The pharmacokinetics of dihydroergotamine did not appear to be significantly affected by the concomitant use of a local vasoconstrictor.
Multiple oral doses of the β-adrenoceptor antagonist propranolol, used for preventive treatment of migraine, had no significant influence on the Cmax, Tmax or AUC of dihydroergotamine doses up to 4 mg [see Drug Interactions (7.3)].
The effect of oral contraceptives on the pharmacokinetics of dihydroergotamine has not been studied.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
In a 2-year mouse carcinogenicity study, subcutaneous administration of dihydroergotamine mesylate (0, 0.5, 1.5, or 5 mg/kg/day) resulted in an increased incidence of fibrosarcoma at the injection sites in males and females at the high dose.
In a 2-year rat carcinogenicity study, intranasal administration of dihydroergotamine mesylate (0, 0.4, 0.8, or 1.6 mg/day for 13 weeks, followed by 0, 0.08, 0.24, or 0.8 mg/day for the remainder of the study) did not result in an increase in tumors.
Mutagenesis
Dihydroergotamine mesylate was negative in an in vitro mutagenicity (Ames) assay and positive in in vitro chromosomal aberration (V79 Chinese hamster cell assay with metabolic activation, and human peripheral blood lymphocyte) assays. Dihydroergotamine was negative in in vivo micronucleus assays in mouse and hamster.
-
14 CLINICAL STUDIES
The efficacy of ATZUMI for the acute treatment of migraine with or without aura in adults was based on the relative bioavailability of ATZUMI nasal powder compared to dihydroergotamine mesylate nasal spray.
The clinical trials described below were conducted using dihydroergotamine mesylate nasal spray.
The efficacy of dihydroergotamine mesylate nasal spray for the acute treatment of migraine headaches was evaluated in four randomized, double-blind, placebo controlled studies in the U.S. The patient population for the trials was predominantly female (87%) and Caucasian (95%) with a mean age of 39 years (range 18 to 65 years). Patients treated a single moderate to severe migraine headache with a single dose of study medication and assessed pain severity over the 24 hours following treatment. Headache response was determined 0.5, 1, 2, 3 and 4 hours after dosing and was defined as a reduction in headache severity to mild or no pain. In studies 1 and 2, a four-point pain intensity scale was utilized; in studies 3 and 4, a five-point scale was used to record pain response. Although rescue medication was allowed in all four studies, patients were instructed not to use them during the four hour observation period. In studies 3 and 4, a total dose of 2 mg was compared to placebo. In studies 1 and 2, doses of 2 and 3 mg were evaluated, and showed no advantage of the higher dose for a single treatment. In all studies, patients received a regimen consisting of 0.5 mg in each nostril, repeated in 15 minutes (and again in another 15 minutes for the 3 mg dose in studies 1 and 2).
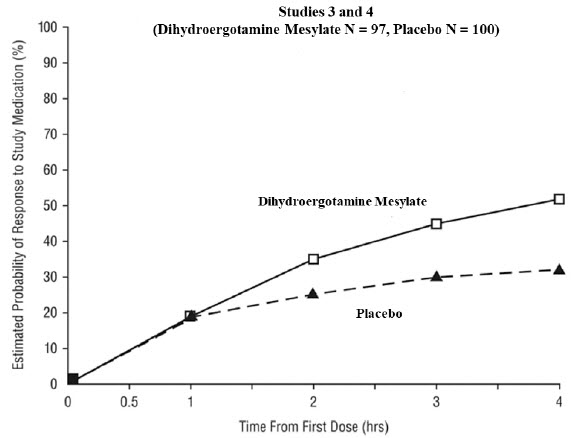
The percentage of patients achieving headache response 4 hours after treatment was significantly greater in patients receiving 2 mg doses of dihydroergotamine mesylate nasal spray compared to those receiving placebo in 3 of the 4 studies (see Table 2 and Table 3 and Figure 1 and Figure 2).
Table 2 Studies 1 and 2: Percentage of Patients with Headache Response* 2 and 4 Hours Following a Single Treatment of Study Medication (Dihydroergotamine Mesylate Nasal Spray or Placebo) N 2 hours 4 hours - * Headache response was defined as a reduction in headache severity to mild or no pain. Headache response was based on pain intensity as interpreted by the patient using a four-point pain intensity scale.
- † p value < 0.001
- ‡ p value < 0.01
Study 1 Dihydroergotamine mesylate nasal spray 105 61%† 70%† Placebo 98 23% 28% Difference from Placebo 37% 42% Study 2 Dihydroergotamine mesylate nasal spray 103 47% 56%‡ Placebo 102 33% 35% Difference from Placebo 14% 21% Table 3 Studies 3 and 4: Percentage of Patients with Headache Response* 2 and 4 Hours Following a Single Treatment of Study Medication (Dihydroergotamine Mesylate Nasal Spray or Placebo) N 2 hours 4 hours - * Headache response was defined as a reduction in headache severity to mild or no pain. Headache response was evaluated on a five-point scale that included pain response.
- † p value < 0.01
Study 3 Dihydroergotamine mesylate nasal spray 50 32% 48%† Placebo 50 20% 22% Difference from Placebo 12% 26% Study 4 Dihydroergotamine mesylate nasal spray 47 30% 47% Placebo 50 20% 30% Difference from Placebo 10% 17% The Kaplan-Meier plots below (Figure 1 and Figure 2) provides an estimate of the probability that a patient will have responded to a single 2 mg dose of dihydroergotamine mesylate nasal spray as a function of the time elapsed since initiation of treatment.
Figure 1 Estimated Probability of a Patient Responding During the Four Hours Following a Single 2 mg Dose of Dihydroergotamine Mesylate Nasal Spray as a Function of the Time Elapsed Since Initiation of Treatment* - * The figure shows the probability over time of obtaining a response following treatment with dihydroergotamine mesylate nasal spray. Headache response was based on pain intensity as interpreted by the patient using a four-point pain intensity scale. Patients not achieving response within 4 hours were censored to 4 hours.
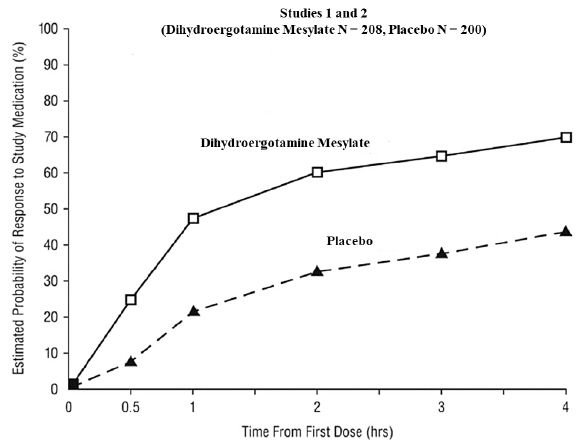
Figure 2 Estimated Probability of a Patient Responding to Dihydroergotamine Mesylate Nasal Spray During the Four Hours Following Dosing* - * The figure shows the probability over time of obtaining a response following treatment with dihydroergotamine mesylate nasal spray. Headache response was evaluated on a five-point scale that included pain response. Patients not achieving response within 4 hours were censored to 4 hours.
For patients with migraine-associated nausea, photophobia, and phonophobia at baseline, there was a lower incidence of these symptoms at 2 and 4 hours following administration of dihydroergotamine mesylate nasal spray compared to placebo.
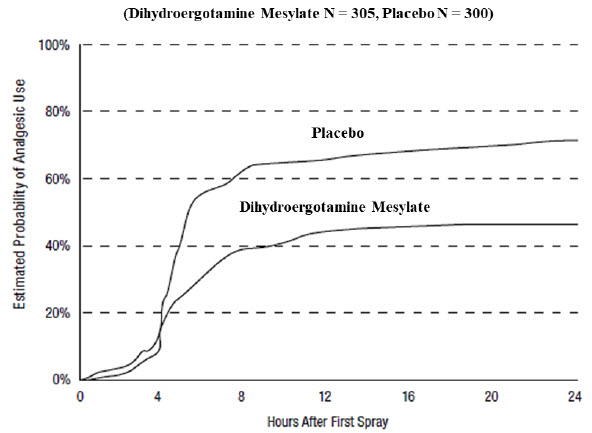
Patients were not allowed to use additional treatments for 8 hours prior to study medication dosing and during the 4-hour observation period following study treatment. Following the 4-hour observation period, patients were allowed to use additional treatments. For all studies, the estimated probability of patients using additional treatments for their migraines over the 24 hours following the single 2 mg dose of study treatment is summarized in Figure 3 below.
Figure 3 Estimated Probability of a Patient Using Additional Treatments for Migraine Over the 24 Hours Following Either Dihydroergotamine Mesylate Nasal Spray 2 mg (or Placebo)* - * Kaplan-Meier plot based on data obtained from all studies with patients not using additional treatments censored to 24 hours. All patients received a single treatment of study medication for their migraine attack. The plot also includes patients who had no response to the initial dose.
Neither age nor sex appear to affect the patient's response to dihydroergotamine mesylate nasal spray. The racial distribution of patients was insufficient to determine the effect of race on the efficacy of dihydroergotamine mesylate nasal spray.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
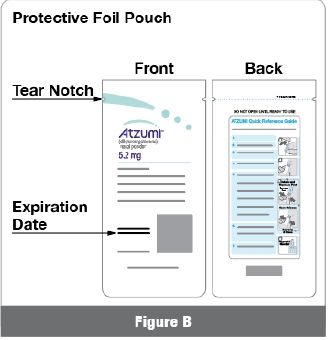
ATZUMI (dihydroergotamine) nasal powder is supplied in a single-dose nasal device with white powder containing 5.2 mg of dihydroergotamine. ATZUMI is available in a carton of 8 nasal devices each individually packaged in a protective foil pouch (NDC: 76978-101-08).
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide and Instructions for Use).
Serious and/or Life-Threatening Reactions with Coadministration of CYP3A4 Inhibitors
Inform patients that serious and/or life-threatening peripheral ischemia (cerebral ischemia and/or ischemia of the extremities) has been associated with the coadministration of dihydroergotamine and strong CYP3A4 inhibitors, such as macrolide antibiotics and protease inhibitors [see Contraindications (4), Warnings and Precautions (5.1), and Drug Interactions (7.1)].
Myocardial Ischemia and/or Infarction, Other Cardiac Events, Cerebrovascular Events, and Fatalities
Inform patients of the risk for serious cardiac, cerebrovascular, and other vasospasm related events. Advise patients to notify their healthcare provider if they develop any risk factors or symptoms while taking ATZUMI. Inform patients that nicotine may provoke vasoconstriction predisposing to a greater ischemic response [see Warnings and Precautions (5.2, 5.3, 5.4)].
Increase in Blood Pressure
Inform patients of the risk for significant elevation in blood pressure [see Warnings and Precautions (5.5)].
Medication Overuse Headache
Inform patients that use of drugs to treat migraine attacks for 10 or more days per month may lead to an exacerbation of headache, and encourage patients to record headache frequency and drug use (e.g., by keeping a headache diary) [see Warnings and Precautions (5.6)].
Local Irritation
Advise patients to notify their healthcare provider if they have bothersome local irritation [see Warning and Precautions (5.9)].
Drug Interactions
Advise patients to inform their healthcare providers if they are taking, or plan to take, any prescription or over-the-counter drugs, since there is a potential for interactions [see Drug Interactions (7)].
Pregnancy
Advise patients of the risk for preterm birth. Advise women to inform their healthcare provider if they are pregnant or intend to become pregnant [see Warnings and Precautions (5.7), Use in Specific Populations (8.1)].
Lactation
Advise patients not to breastfeed during treatment with ATZUMI [see Use In Specific Populations (8.2)].
Administration Instructions
Instruct patients not to squeeze ATZUMI before inserting it into the nostril because priming is not required. Inform patients that they will need to squeeze the air pump on the ATZUMI device three separate times into one nostril to give a dose. Instruct the patient to squeeze while inhaling, release to allow the air pump to expand back to its original shape, then repeat two more times [see Instructions for Use]. Tell patients to use fast, complete, pulse-like squeezes to deliver their dose. [see Dosage and Administration (2.3)].
- SPL UNCLASSIFIED SECTION
-
MEDICATION GUIDE
MEDICATION GUIDE
ATZUMI™ (at zoo' mee)
(dihydroergotamine)
nasal powderThis Medication Guide has been approved by the U.S. Food and Drug Administration. Issued: 04/2025 What is the most important information I should know about ATZUMI?
ATZUMI can cause serious side effects, including:-
Serious problems with blood circulation to your legs and feet (peripheral ischemia). ATZUMI can cause peripheral ischemia when you take it with certain medicines known as CYP3A4 inhibitors. Peripheral ischemia may lead to a stroke and death. Stop taking ATZUMI and get emergency medical help right away if you have any of the following symptoms:
- cramping and pain in your legs or hips
- feeling of heaviness or tightness in your leg muscles
- burning or aching pain in your feet or toes while resting
- numbness, tingling, or weakness in your legs
- cold feeling or color changes in 1 or both legs or feet
- slurred speech
- sudden weakness
- ritonavir
- nelfinavir
- erythromycin
- clarithromycin
- ketoconazole
- itraconazole
These are not all of the medicines that could affect how ATZUMI works. Your healthcare provider can tell you if it is safe to take ATZUMI with other medicines. What is ATZUMI?
ATZUMI is a prescription medicine used for the acute treatment of migraine with or without aura in adults.- ATZUMI is not used to prevent migraine.
- ATZUMI is not used to treat other types of headaches such as hemiplegic (that make you unable to move on one side of your body) or basilar (rare form of migraine with aura) migraines.
Who should not take ATZUMI?
Do not take ATZUMI if you:- are taking medicines known as strong CYP3A4 inhibitors.
- have heart problems or a history of heart problems.
- have uncontrolled high blood pressure.
- have narrowing of blood vessels in your legs, arms, stomach, or kidneys (peripheral vascular disease).
- have sepsis.
- have had vascular surgery.
- have severe liver problems.
- have severe kidney problems.
- are allergic to dihydroergotamine, ergot alkaloids, or any of the ingredients in ATZUMI. See the end of this Medication Guide for a complete list of ingredients in ATZUMI.
- have taken any of the following medicines in the last 24 hours:
- sumatriptan
- almotriptan
- eletriptan
- frovatriptan
- naratriptan
- rizatriptan
- zolmitriptan
- ergotamine or ergotamine-type medicines
- have taken any medicines that constrict your blood vessels or raise your blood pressure.
Your healthcare provider can tell you if it is safe to take ATZUMI with other medicines.Before you take ATZUMI, tell your healthcare provider about all of your medical conditions, including if you: - have high blood pressure.
- have liver problems.
- have kidney problems.
- have risk factors for heart disease. You have a higher risk for heart disease if you:
- have high blood pressure
- have high cholesterol levels
- smoke
- are overweight
- have diabetes
- have a family history of heart disease
- are taking medicines known as strong CYP3A4 inhibitors.
- are pregnant or plan to become pregnant. ATZUMI may cause preterm labor. ATZUMI should be avoided during pregnancy. Talk to your healthcare provider right away if you are pregnant or want to become pregnant.
- are breastfeeding or plan to breastfeed. ATZUMI may reduce breast milk supply and pass into your breast milk. ATZUMI may be harmful to your baby. Do not breastfeed your baby while taking ATZUMI and for 3 days after you use ATZUMI. Talk with your healthcare provider about the best way to feed your baby if you take ATZUMI.
How should I take ATZUMI? - ATZUMI is for nasal use only (use in the nose).
- Certain people should take their first dose of ATZUMI in their healthcare provider's office or in another medical setting. Ask your healthcare provider if you should take your first dose in a medical setting.
- Use ATZUMI exactly as your healthcare provider tells you to use it. Read and follow the instructions in the Instructions for Use or use the Quick Reference Guide located on the ATZUMI protective foil pouch.
- If your headache comes back after the first complete dose or you only get some relief from your headache, you can use a second dose 1 hour after the first complete dose. Use a new ATZUMI nasal powder device for the second dose, if needed.
- Do not take more than 2 doses of ATZUMI within a 24-hour period. It is not known if it is safe to take more than 4 doses of ATZUMI in a 7-day period or 12 doses in a 30-day period.
- Taking ATZUMI for 10 or more days in 1 month may make your headaches worse. You should write down when you have headaches and when you take ATZUMI so that you can talk with your healthcare provider about how ATZUMI is working for you. See "What are the possible side effects of ATZUMI?".
What are the possible side effects of ATZUMI?
ATZUMI can cause serious side effects, including:
See "What is the most important information I should know about ATZUMI?"-
Heart attack and other heart problems. Heart problems may lead to death. Stop taking ATZUMI and get emergency medical help right away if you have any of the following symptoms of a heart attack:
- discomfort in the center of your chest that lasts for more than a few minutes, or that goes away and comes back
- severe tightness, pain, pressure, or heaviness in your chest, throat, neck, or jaw
- pain or discomfort in your arms, back, neck, jaw, or stomach
- shortness of breath with or without chest discomfort
- breaking out in a cold sweat
- feeling lightheaded
- nausea or vomiting
ATZUMI is not for people with risk factors for heart disease unless a heart exam is done and shows no problem. See "Before you take ATZUMI, tell your healthcare provider about all of your medical conditions, including if you:" for the risk factors for heart disease. -
Stroke. Stop taking ATZUMI and get emergency medical help right away if you have any of the following symptoms of a stroke:
- face drooping
- unusual weakness or numbness
- slurred speech
- Changes in color or sensation in your fingers and toes (Raynaud's syndrome).
-
Stomach and intestinal problems (gastrointestinal and colonic ischemic events). Symptoms of gastrointestinal and colonic ischemic events include:
- sudden or severe stomach pain
- constipation or diarrhea
- stomach pain after meals
- bloody diarrhea
- weight loss
- fever
- nausea or vomiting
- Increased blood pressure.
- Medicine overuse headache. Some people who use too much ATZUMI may make their headaches worse (medicine overuse headache). If your headaches get worse, your healthcare provider may decide to stop your treatment with ATZUMI.
- Preterm labor.
- Tissue changes (fibrotic complications). Inflammation and fiber-like tissue that is not normal (fibrosis) can occur around the lungs and stomach.
- Nose irritation. Discomfort in your nose, change in taste, stuffy nose, and cold-type symptoms, (such as, runny nose, sneezing, and cough) can occur.
- runny nose
- nausea
- abnormal taste
- application site reactions
- dizziness
- vomiting
- sleepiness
- sore throat
- diarrhea
These are not all of the possible side effects of ATZUMI.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.How should I store ATZUMI? - Store ATZUMI at room temperature between 68°F to 77°F (20°C to 25°C).
- Store ATZUMI in its protective foil pouch until ready to use.
General information about the safe and effective use of ATZUMI.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use ATZUMI for a condition for which it was not prescribed. Do not give ATZUMI to other people, even if they have the same symptoms you have. It may harm them. You can ask your pharmacist or healthcare provider for information about ATZUMI that is written for health professionals.What are the ingredients in ATZUMI?
Active ingredient: Dihydroergotamine
Inactive ingredients: Hypromellose, mannitol, and microcrystalline cellulose
ATZUMI is a trademark of Satsuma Pharmaceuticals, Inc.
Manufactured for Satsuma Pharmaceuticals, Inc., Durham, NC 27703
© 2025. Satsuma Pharmaceuticals, Inc. All rights reserved.
For more information, go to www.atzumi.com or call 1-888-273-2480. -
Serious problems with blood circulation to your legs and feet (peripheral ischemia). ATZUMI can cause peripheral ischemia when you take it with certain medicines known as CYP3A4 inhibitors. Peripheral ischemia may lead to a stroke and death. Stop taking ATZUMI and get emergency medical help right away if you have any of the following symptoms:
-
INSTRUCTIONS FOR USE
ATZUMI™ (at zoo' mee)
(dihydroergotamine)
nasal powderFor Nasal Use Only
This Instructions for Use contains information on how to use ATZUMI.
Read this Instructions for Use before using ATZUMI.
Important Information You Need to Know Before Using ATZUMI
- ATZUMI contains 1 complete dose of medicine and should be thrown away after each use.
- ATZUMI is for nasal (nose) use only.
- Deliver all the powdered medicine into only 1 nostril.
- Do not use ATZUMI if it is damaged or expired.
- Do not squeeze ATZUMI before inserting it into the nostril. Priming is not required.
- Powdered medicine is inside the blue nozzle. When you squeeze the white air pump, air is pushed into the blue nozzle and pushes the powdered medicine into your nose.
- Do not squeeze slowly, partially or with any hesitation. When dosing, you must fully squeeze the white air pump as fast as you can. A fast, pulse-like squeezing action is needed.
How often can you use ATZUMI?
- If needed, you may take a second dose 1 hour after your first dose. Wait at least 1 hour before taking the second dose.
- Do not take more than 2 doses within a 24-hour period.
- It is not known if it is safe to take more than 4 doses of ATZUMI in a 7-day period or 12 doses in a 30-day period.
Storing ATZUMI
- Store ATZUMI at room temperature between 68°F to 77°F (20°C to 25°C).
- Store ATZUMI in its protective foil pouch until ready to use (Figure C).
-
Keep ATZUMI and all medicines out of the reach of children.

Step 1. Preparing to Use ATZUMI
-
1.1 Blow Your Nose
Blow your nose to clear your nostrils (Figure D).
-
1.2 Take Out ATZUMI
Open the protective foil pouch by tearing at the notch.

Remove ATZUMI from the protective foil pouch (Figure E). -
1.3 Check ATZUMI
Check the Expiration Date to make sure ATZUMI is not expired (Figure F).

Check ATZUMI for damage.
If ATZUMI is expired or damaged, throw it away in your household trash and get a new ATZUMI. -
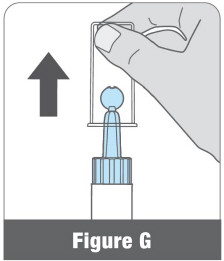
1.4 Remove Clear Cap
Pull the clear cap straight off (Figure G).
Step 2. Using ATZUMI
-
2.1 Remove Round Blue Tab
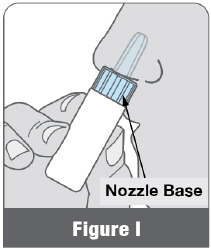
Hold the nozzle base in 1 hand.
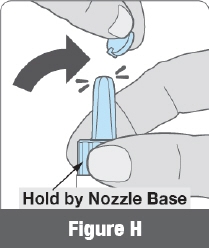
Remove the round blue tab by bending it back and forth or twisting it to break it off (Figure H).
This creates an opening for the powdered medicine to pass through.
Important: Do not squeeze the white air pump yet. Wait until Step 2.3. -
2.2 Insert Into Nostril
Hold the white air pump as shown in Figure I and insert the blue nozzle into 1 nostril as far as it will comfortably go. The nozzle base should touch your nose (Figure I).
- 2.3 Deliver All of the Powdered Medicine into Only 1 Nostril
- Squeeze the white air pump 3 separate times into 1 nostril. Inhale through your nose each time you squeeze (Figure J).
- Fast, complete, pulse-like squeezes are needed to push the powdered medicine and deliver the complete dose.
- Do not squeeze slowly, partially or with any hesitation.
-
Allow the white air pump to expand back to its original shape between squeezes (Figure J). Important:

Deliver all the powdered medicine into only 1 nostril.
Step 3. Inspecting ATZUMI
-
3.1 Check for Remaining Powdered Medicine
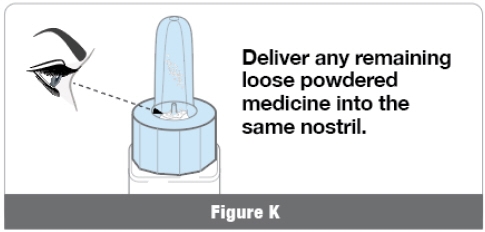
- Keep ATZUMI upright and look inside the blue nozzle to see if any loose powdered medicine remains at the bottom (Figure K).
-
If loose powdered medicine remains, repeat Step 2.3 to dose into the same nostril, but squeeze the white air pump faster. Repeat Step 2.3 until no loose powdered medicine remains.
Note: - It is normal to see a light coating of powdered medicine in the blue nozzle after delivering the complete dose.
- If you are not sure whether you have delivered all of the loose powdered medicine, then repeat Step 2.3 with the same ATZUMI device in the same nostril.
Step 4. Throwing Away ATZUMI
-
After use, throw away the protective foil pouch, the ATZUMI device, the round blue tab, and the clear cap in your household trash (Figure L).
Do not save ATZUMI after use. ATZUMI contains a one-time (single) dose.
This Instructions for Use has been approved by the U.S. Food and Drug Administration.
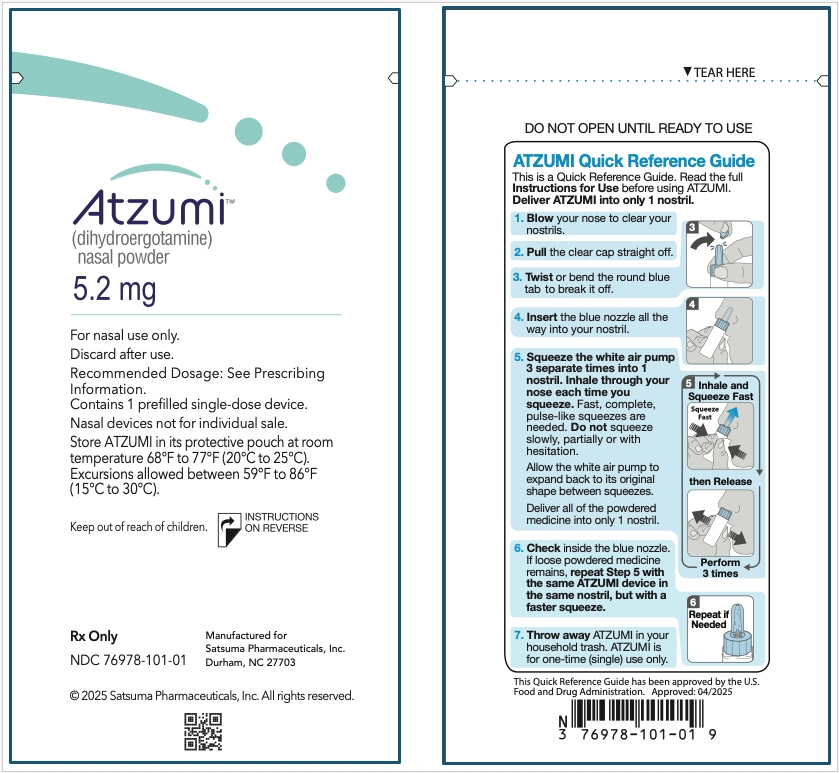
Approved: 4/2025Quick Reference Guide
This is a Quick Reference Guide. Read the full Instructions for Use before using ATZUMI. Deliver ATZUMI into only 1 nostril.
- Blow your nose to clear your nostrils.
- Pull the clear cap straight off.
-
Twist or bend the round blue tab to break it off.

-
Insert the blue nozzle all the way into your nostril.

-
Squeeze the white air pump 3 separate times into 1 nostril. Inhale through your nose each time you squeeze. Fast, complete, pulse-like squeezes are needed. Do not squeeze slowly, partially or with hesitation.
Allow the white air pump to expand back to its original shape between squeezes.
Deliver all of the powdered medicine into only 1 nostril.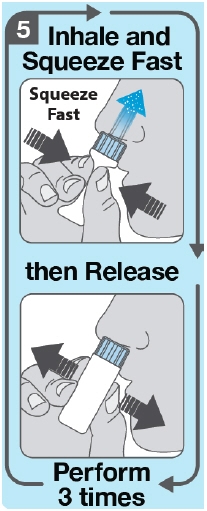
-
Check inside the blue nozzle. If loose powdered medicine remains, repeat Step 5 with the same ATZUMI device in the same nostril, but with a faster squeeze.

- Throw away ATZUMI in your household trash. ATZUMI is for one-time (single) use only.
This Quick Reference Guide has been approved by the U.S. Food and Drug Administration.
Approved: 04/2025 -
PRINCIPAL DISPLAY PANEL - 5.2 mg Bottle Carton
Atzumi™
(dihydroergotamine)
nasal powder5.2 mg
For nasal use only.
Discard after use.
Contains:- 8 prefilled single-dose devices
- Instructions for Use
- Medication Guide
- Prescribing Information
Nasal devices not for individual sale.
Dispense entire carton and accompanying Medication Guide to each patient.Rx Only
NDC: 76978-101-08© 2025 Satsuma Pharmaceuticals, Inc. All rights reserved.
-
PRINCIPAL DISPLAY PANEL - 5.2 mg Device Pouch Label
Atzumi™
(dihydroergotamine)
nasal powder5.2 mg
For nasal use only.
Discard after use.
Recommended Dosage: See Prescribing
Information.
Contains 1 prefilled single-dose device.
Nasal devices not for individual sale.
Store ATZUMI in its protective pouch at room
temperature 68°F to 77°F (20°C to 25°C).
Excursions allowed between 59°F to 86°F
(15°C to 30°C).Keep out of reach of children.
INSTRUCTIONS
ON REVERSERx Only
NDC: 76978-101-01Manufactured for
Satsuma Pharmaceuticals, Inc.
Durham, NC 27703© 2025 Satsuma Pharmaceuticals, Inc. All rights reserved.
-
INGREDIENTS AND APPEARANCE
ATZUMI
dihydroergotamine mesylate powderProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 76978-101 Route of Administration NASAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength DIHYDROERGOTAMINE MESYLATE (UNII: 81AXN7R2QT) (DIHYDROERGOTAMINE - UNII:436O5HM03C) DIHYDROERGOTAMINE MESYLATE 5.2 mg Inactive Ingredients Ingredient Name Strength MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) MANNITOL (UNII: 3OWL53L36A) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 76978-101-11 1 in 1 CARTON 04/30/2025 1 1 in 1 BOTTLE, UNIT-DOSE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) 2 NDC: 76978-101-08 8 in 1 CARTON 04/30/2025 2 1 in 1 BOTTLE, UNIT-DOSE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA217901 04/30/2025 Labeler - Satsuma Pharmaceuticals, Inc. (117333645)
Trademark Results [ATZUMI]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 ATZUMI 97365929 not registered Live/Pending |
Satsuma Pharmaceuticals, Inc. 2022-04-15 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.