BUPIVACAINE injection, suspension, liposomal
Bupivacaine by
Drug Labeling and Warnings
Bupivacaine by is a Prescription medication manufactured, distributed, or labeled by Jiangsu Hengrui Pharmaceuticals Co., Ltd., Jiangsu Hengrui Pharmaceuticals Co., Ltd. (Jinqiao Road Site), Jiangsu Hengrui Pharmaceuticals Co., Ltd. (Dongjin Road Site). Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use BUPIVACAINE LIPOSOME INJECTABLE SUSPENSION safely and effectively. See full prescribing information for BUPIVACAINE LIPOSOME INJECTABLE SUSPENSION.
BUPIVACAINE LIPOSOME injectable suspension, for infiltration or perineural use
Initial U.S. Approval: 1972INDICATIONS AND USAGE
Bupivacaine liposome injectable suspension contains bupivacaine, an amide local anesthetic, and is indicated to produce postsurgical:
- Local analgesia via infiltration in adults ( 1).
- Regional analgesia via an interscalene brachial plexus nerve block in adults ( 1).
Limitations of Use
The safety and effectiveness of bupivacaine liposome injectable suspension have not been established to produce postsurgical regional analgesia via other nerve blocks besides an interscalene brachial plexus nerve block.DOSAGE AND ADMINISTRATION
- Bupivacaine liposome injectable suspension is for single administration only ( 2.1).
- Bupivacaine liposome injectable suspension is not substitutable with other bupivacaine products even if the strength is the same. Therefore, it is not possible to convert a dose from other bupivacaine products to a bupivacaine liposome injectable suspension dose and vice versa ( 2.1, 2.5).
- Do not dilute bupivacaine liposome injectable suspension with water or other hypotonic solutions ( 2.1).
- The recommended dose of bupivacaine liposome injectable suspension for:
- Local infiltration in adults is up to a maximum dose of 266 mg. See Full Prescribing Information for guidance on dose selection ( 2.2).
- Interscalene brachial plexus nerve block in adults is 133 mg ( 2.3).
- For the nerve block, administer additional analgesics, which may include other immediate-release local anesthetics, as appropriate ( 2.3).
- See Full Prescribing Information for important preparation and administration instructions and compatibility considerations ( 2.4, 2.5).
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
Bupivacaine liposome injectable suspension is contraindicated in obstetrical paracervical block anesthesia ( 4).
WARNINGS AND PRECAUTIONS
- Monitor cardiovascular status, neurological status, and vital signs during and after injection of bupivacaine liposome injectable suspension ( 5.1).
- Because amide-type local anesthetics, such as bupivacaine, are metabolized by the liver, use bupivacaine liposome injectable suspension cautiously in patients with hepatic disease. Patients with severe hepatic disease, because of their inability to metabolize local anesthetics normally, are at a greater risk of developing toxic plasma concentrations ( 5.1).
- Methemoglobinemia: Cases of methemoglobinemia have been reported in association with local anesthetic use ( 5.1).
- Avoid additional use of local anesthetics within 96 hours following administration of bupivacaine liposome injectable suspension ( 5.2).
ADVERSE REACTIONS
Adverse reactions reported with an incidence greater than or equal to 10% following bupivacaine liposome injectable suspension administration via:
- Infiltration in adults were nausea, constipation, and vomiting ( 6.1).
- Nerve block in adults were nausea, pyrexia, headache, and constipation ( 6.1).
To report SUSPECTED ADVERSE REACTIONS, contact eVenus Pharmaceutical Laboratories, Inc. at 1-609-395-8625 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- Lidocaine or other non-bupivacaine local anesthetics:Do not admix with bupivacaine liposome injectable suspension. Bupivacaine liposome injectable suspension may be administered at least 20 minutes or more following local administration of lidocaine ( 7).
- Bupivacaine HCl:Do not exceed a milligram dose of bupivacaine HCl solution to bupivacaine liposome injectable suspension of 1:2 when admixing, as this may impact the pharmacokinetics and/or physicochemical properties of the drugs ( 7).
USE IN SPECIFIC POPULATIONS
- Pregnancy: May cause fetal harm ( 8.1).
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 7/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1. INDICATIONS AND USAGE
2. DOSAGE AND ADMINISTRATION
2.1 Important Dose, Preparation, and Administration Instructions
2.2 Recommended Dose for Local Analgesia via Infiltration
2.3 Recommended Dose for Regional Analgesia
2.4 Preparation and Administration Instructions
2.5 Compatibility Considerations
3. DOSAGE FORMS AND STRENGTHS
4. CONTRAINDICATIONS
5. WARNINGS AND PRECAUTIONS
5.1 Warnings and Precautions for Bupivacaine-Containing Products
5.2 Warnings and Precautions Specific for Bupivacaine Liposome Injectable Suspension
6. ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7. DRUG INTERACTIONS
8. USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 Renal Impairment
10. OVERDOSAGE
11. DESCRIPTION
12. CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13. NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14. CLINICAL STUDIES
14.1 Overview of Clinical Studies in Adult Patients
14.2 Studies in Adults to Produce Postsurgical Local Analgesia
14.3 Nerve Block Studies in Adults to Produce Postsurgical Regional Analgesia
14.4 Studies That Do Not Support an Indication for Certain Nerve Blocks in Adults
16. HOW SUPPLIED/STORAGE AND HANDLING
17. PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1. INDICATIONS AND USAGE
Bupivacaine liposome injectable suspension is indicated to produce postsurgical:
- Local analgesia via infiltration in adults
- Regional analgesia via an interscalene brachial plexus nerve block in adults
Limitations of Use
The safety and effectiveness of bupivacaine liposome injectable suspension have not been established to produce postsurgical regional analgesia via other nerve blocks besides an interscalene brachial plexus nerve block.
-
2. DOSAGE AND ADMINISTRATION
2.1 Important Dose, Preparation, and Administration Instructions
- Bupivacaine liposome injectable suspension is for single administration only.
- Bupivacaine liposome injectable suspension is not substitutable with other bupivacaine products even if the strength is the same. Therefore, it is not possible to convert a dose from other bupivacaine products to a bupivacaine liposome injectable suspension dose and vice versa.
- Do not dilute bupivacaine liposome injectable suspension with water or other hypotonic agents, as it will result in disruption of the liposomal particles.
- Do not administer bupivacaine liposome injectable suspension if it is suspected that the vial has been frozen or exposed to high temperature (greater than 40°C or 104°F) for an extended period.
- Inspect bupivacaine liposome injectable suspension visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not administer bupivacaine liposome injectable suspension if the product is discolored.
- Do not heat or autoclave before use.
- Do not filter during administration.
2.2 Recommended Dose for Local Analgesia via Infiltration
Local Analgesia via Infiltration in Adults
The recommended dose of bupivacaine liposome injectable suspension for local infiltration in adults is up to a maximum dose of 266 mg, and is based on the following factors:
- Size of the surgical site
- Volume required to cover the area
- Individual patient factors that may impact the safety of an amide local anesthetic
As general guidance in selecting the proper bupivacaine liposome injectable suspension dose for local infiltration in adults, two examples are provided [ see Clinical Studies (14.2)]. In adult patients undergoing:
- Bunionectomy, a total of 106 mg (8 mL) of bupivacaine liposome injectable suspension was administered, with 7 mL infiltrated into the tissues surrounding the osteotomy, and 1 mL infiltrated into the subcutaneous tissue.
- Hemorrhoidectomy, a total of 266 mg (20 mL) of bupivacaine liposome injectable suspension was diluted with 10 mL of saline, for a total of 30 mL, divided into six 5 mL aliquots, injected by visualizing the anal sphincter as a clock face and slowly infiltrating one aliquot to each of the even numbers to produce a field block.
2.3 Recommended Dose for Regional Analgesia
- The maximum recommended dose of bupivacaine liposome injectable suspension via perineural use for interscalene brachial plexus nerve block is 133 mg. For all nerve blocks, administer additional analgesics, which may include other immediate-release local anesthetics, as appropriate.
- Regional Analgesia via Interscalene Brachial Plexus Nerve Block in Adults
- The recommended dose of bupivacaine liposome injectable suspension for interscalene brachial plexus nerve block in adults is 133 mg and is based upon one study of patients undergoing either total shoulder arthroplasty or rotator cuff repair [ see Clinical Studies (14.3)].
2.4 Preparation and Administration Instructions
- Invert vials of bupivacaine liposome injectable suspension multiple times to re-suspend the particles immediately prior to withdrawal from the vial.
- Administer bupivacaine liposome injectable suspension (1) undiluted or (2) diluted to increase volume up to a final concentration of 0.89 mg/mL (i.e., 1:14 dilution by volume) with 0.9% preservative-free Sodium Chloride Injection or lactated Ringer’s solution. Use diluted bupivacaine liposome injectable suspension within 4 hours of preparation in a syringe.
- Administer bupivacaine liposome injectable suspension with a 25 gauge or larger bore needle to maintain the structural integrity of the liposomal bupivacaine particles.
- Administer bupivacaine liposome injectable suspension slowly via infiltration or perineural use with frequent aspiration to check for blood and minimize the risk of inadvertent intravascular injection.
- Discard unused portion.
2.5 Compatibility Considerations
Some physicochemical incompatibilities exist between bupivacaine liposome injectable suspension and certain other drugs. Direct contact of bupivacaine liposome injectable suspension with these drugs results in a rapid increase in free (unencapsulated) bupivacaine, altering bupivacaine liposome injectable suspension characteristics and potentially affecting the safety and efficacy of bupivacaine liposome injectable suspension. Therefore, admixing bupivacaine liposome injectable suspension with other drugs prior to administration is not recommended [ see Drug Interactions (7)].
- Non-bupivacaine based local anesthetics, including lidocaine, may cause an immediate release of bupivacaine from bupivacaine liposome injectable suspension if administered together locally. The administration of bupivacaine liposome injectable suspension may follow the administration of lidocaine after a delay of 20 minutes or more.
- Bupivacaine HCl administered together with bupivacaine liposome injectable suspension may impact the pharmacokinetic and/or physicochemical properties of bupivacaine liposome injectable suspension, and this effect is concentration dependent. Therefore, bupivacaine HCl and bupivacaine liposome injectable suspension may be administered simultaneously in the same syringe, and bupivacaine HCl may be injected immediately before bupivacaine liposome injectable suspension if the ratio of the milligram dose of bupivacaine HCl solution to bupivacaine liposome injectable suspension does not exceed 1:2.
The toxic effects of these drugs are additive, and their administration should be used with caution including monitoring for neurologic and cardiovascular effects related to local anesthetic systemic toxicity [ see Warnings and Precautions (5.1) and Overdosage (10)].
- When a topical antiseptic such as povidone iodine (e.g., Betadine) is applied, the site should be allowed to dry before bupivacaine liposome injectable suspension is administered into the site. Bupivacaine liposome injectable suspension should not be allowed to come into contact with antiseptics such as povidone iodine in solution.
Studies conducted with bupivacaine liposome injectable suspension demonstrated that the most common implantable materials (polypropylene, PTFE, silicone, stainless steel, and titanium) are not affected by the presence of bupivacaine liposome injectable suspension any more than they are by saline. None of the materials studied had an adverse effect on bupivacaine liposome injectable suspension.
- 3. DOSAGE FORMS AND STRENGTHS
-
4. CONTRAINDICATIONS
Bupivacaine liposome injectable suspension is contraindicated in obstetrical paracervical block anesthesia [ see Use in Specific Populations (8.1)]. While bupivacaine liposome injectable suspension has not been tested with this technique, the use of bupivacaine HCl with this technique has resulted in fetal bradycardia and death.
-
5. WARNINGS AND PRECAUTIONS
5.1 Warnings and Precautions for Bupivacaine-Containing Products
The safety and effectiveness of bupivacaine liposome injectable suspension, other bupivacaine products, and other amide-containing products depend on proper dosage, correct technique, adequate precautions, and readiness for emergencies. As there is a potential risk of severe life-threatening adverse reactions associated with the administration of bupivacaine, any bupivacaine-containing product should be administered in a setting where trained personnel and equipment are available to promptly treat patients who show evidence of neurological or cardiac toxicity [ see Overdosage (10)].
Careful and constant monitoring of cardiovascular and respiratory (adequacy of ventilation) vital signs and the patient’s state of consciousness should be performed after injection of bupivacaine and other amide-containing products. Restlessness, anxiety, incoherent speech, lightheadedness, numbness and tingling of the mouth and lips, metallic taste, tinnitus, dizziness, blurred vision, tremors, twitching, depression, or drowsiness may be early warning signs of central nervous system toxicity.
Bupivacaine liposome injectable suspension, other bupivacaine products, and other amide-containing products should also be used with caution in patients with impaired cardiovascular function because they may be less able to compensate for functional changes associated with the prolongation of AV conduction produced by these drugs.
Injection of multiple doses of bupivacaine liposome injectable suspension, other bupivacaine products, and other amide-containing products may cause significant increases in plasma concentrations with each repeated dose due to slow accumulation of the drug or its metabolites, or to slow metabolic degradation. Tolerance to elevated blood concentrations varies with the status of the patient.
Because amide-type local anesthetics, such as bupivacaine, are metabolized by the liver, these drugs should be used cautiously in patients with hepatic disease. Patients with severe hepatic disease, because of their inability to metabolize local anesthetics normally, are at a greater risk of developing toxic plasma concentrations.
Central Nervous System Reactions
The incidences of adverse neurologic reactions associated with the use of local anesthetics may be related to the total dose of local anesthetic administered and are also dependent upon the particular drug used, the route of administration, and the physical status of the patient. Many of these effects may be related to local anesthetic techniques, with or without a contribution from the drug. Neurologic effects following infiltration of soft tissue may include persistent anesthesia, paresthesia, weakness, and paralysis, all of which may have slow, incomplete, or no recovery.
Central nervous system reactions are characterized by excitation and/or depression. Restlessness, anxiety, dizziness, tinnitus, blurred vision, or tremors may occur, possibly proceeding to convulsions. However, excitement may be transient or absent, with depression being the first manifestation of an adverse reaction. This may quickly be followed by drowsiness merging into unconsciousness and respiratory arrest. Other central nervous system effects may be nausea, vomiting, chills, and constriction of the pupils. The incidence of convulsions associated with the use of local anesthetics varies with the procedure used and the total dose administered.
Cardiovascular System Reactions
Toxic blood concentrations depress cardiac conductivity and excitability, which may lead to atrioventricular block, ventricular arrhythmias, and cardiac arrest, sometimes resulting in fatalities. In addition, myocardial contractility is depressed and peripheral vasodilation occurs, leading to decreased cardiac output and arterial blood pressure [ See Overdosage (10)].
Allergic Reactions
Allergic-type reactions are rare and may occur as a result of hypersensitivity to the local anesthetic or to other formulation ingredients. These reactions are characterized by signs such as urticaria, pruritus, erythema, angioneurotic edema (including laryngeal edema), tachycardia, sneezing, nausea, vomiting, dizziness, syncope, excessive sweating, elevated temperature, and possibly anaphylactoid-like symptoms (including severe hypotension). Cross-sensitivity among members of the amide-type local anesthetic group has been reported. The usefulness of screening for sensitivity has not been definitively established.
Chondrolysis
Intra-articular infusions of local anesthetics following arthroscopic and other surgical procedures is an unapproved use, and there have been postmarketing reports of chondrolysis in patients receiving such infusions. The majority of reported cases of chondrolysis have involved the shoulder joint; cases of gleno-humeral chondrolysis have been described in pediatric patients andadult patients following intra-articular infusions of local anesthetics with and without epinephrine for periods of 48 to 72 hours. There is insufficient information to determine whether shorter infusion periods are not associated with these findings. The time of onset of symptoms, such as joint pain, stiffness, and loss of motion can be variable, but may begin as early as the second month after surgery. Currently, there is no effective treatment for chondrolysis; patients who have experienced chondrolysis have required additional diagnostic and therapeutic procedures and some required arthroplasty or shoulder replacement.
Methemoglobinemia
Cases of methemoglobinemia have been reported in association with local anesthetic use. Although all patients are at risk for methemoglobinemia, patients with glucose-6-phosphate dehydrogenase deficiency, congenital or idiopathic methemoglobinemia, cardiac or pulmonary compromise, infants under 6 months of age, and concurrent exposure to oxidizing agents or their metabolites are more susceptible to developing clinical manifestations of the condition. If local anesthetics must be used in these patients, close monitoring for symptoms and signs of methemoglobinemia is recommended.
Signs of methemoglobinemia may occur immediately or may be delayed some hours after exposure, and are characterized by a cyanotic skin discoloration and/or abnormal coloration of the blood. Methemoglobin levels may continue to rise; therefore, immediate treatment is required to avert more serious central nervous system and cardiovascular adverse effects, including seizures, coma, arrhythmias, and death. Discontinue bupivacaine liposome injectable suspension and any oxidizing agents. Depending on the severity of the signs and symptoms, patients may respond to supportive care, i.e., oxygen therapy, hydration. A more severe clinical presentation may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen.
5.2 Warnings and Precautions Specific for Bupivacaine Liposome Injectable Suspension
As there is a potential risk of severe life-threatening adverse reactions associated with the administration of bupivacaine, bupivacaine liposome injectable suspension should be administered in a setting where trained personnel and equipment are available to promptly treat patients who show evidence of neurological or cardiac toxicity [ See Overdosage ( 10) ].
Caution should be taken to avoid accidental intravascular injection of bupivacaine liposome injectable suspension. Convulsions and cardiac arrest have occurred following accidental intravascular injection of bupivacaine and other amide-containing products.
Avoid additional use of local anesthetics within 96 hours following administration of bupivacaine liposome injectable suspension [ see Dosage and Administration (2.4) and Clinical Pharmacology ( 12.3) ].
Bupivacaine liposome injectable suspension has not been evaluated for the following uses and, therefore, is not recommended for these routes of administration or types of analgesia:
- epidural
- intrathecal
- intravascular or intra-articular use
- regional nerve blocks other than interscalene brachial plexus nerve block
Bupivacaine liposome injectable suspension has not been evaluated for use in the following patient populations and, therefore, is not recommended for administration to these groups.
- patients younger than 6 years old for infiltration
- patients younger than 18 years old for interscalene brachial plexus nerve block
- pregnant patients
The potential sensory and/or motor loss with bupivacaine liposome injectable suspension is temporary and varies in degree and duration depending on the site of injection and dose administered and may last for up to 5 days as seen in clinical trials.
-
6. ADVERSE REACTIONS
The following serious adverse reactions have been associated with bupivacaine hydrochloride in clinical trials and are described in greater detail in other sections of the labeling:
- Central Nervous System Reactions [ see Warnings and Precautions ( 5.1) ]
- Cardiovascular System Reactions [ see Warnings and Precautions (5.1) ]
- Allergic Reactions [ see Warnings and Precautions ( 5.1) ]
- Chondrolysis [ see Warnings and Precautions ( 5.1) ]
- Methemoglobinemia [ see Warnings and Precautions ( 5.1) ]
- Accidental intravascular injection [ see Warnings and Precautions ( 5.2) ]
6.1 Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice.
Adverse Reactions Reported in All Local Infiltration Clinical Studies in Adults
- The safety of bupivacaine liposome injectable suspension (local administration into the surgical site) was evaluated in 10 randomized, double-blind, clinical studies (including Studies 1 and 2 [ see Clinical Studies (14.2)]) that included 823 adult patients who had various surgical procedures. Patients were administered a bupivacaine liposome injectable suspension dose ranging from 66 to 532 mg (two times the maximum recommended dose of 266 mg). In these studies, following bupivacaine liposome injectable suspension administration, the: Most common adverse reactions (incidence greater than or equal to 10%) were nausea, constipation, and vomiting.
- Common adverse reactions (incidence greater than or equal to 2% to less than 10%) were pyrexia, dizziness, peripheral edema, anemia, hypotension, pruritus, tachycardia, headache, insomnia, postoperative anemia, muscle spasms, hemorrhagic anemia, back pain, somnolence, and procedural pain.
- Less common adverse reactions (incidence less than 2%) were chills, erythema, bradycardia, anxiety, urinary retention, pain, edema, tremor, postural dizziness, paresthesia, syncope, incision site edema, procedural hypertension, procedural hypotension, procedural nausea, muscular weakness, neck pain, generalized pruritus, pruritic rash, hyperhidrosis, cold sweat, urticaria, palpitations, sinus bradycardia, supraventricular extrasystoles, ventricular extrasystoles, ventricular tachycardia, hypertension, pallor, anxiety, confusional state, depression, agitation, restlessness, hypoxia, laryngospasm, apnea, respiratory depression, respiratory failure, increased body temperature, increased blood pressure (BP),decreased BP, decreased oxygen saturation, urinary incontinence, blurred vision, tinnitus, drug hypersensitivity, and hypersensitivity.
Neurological and Cardiac Adverse Reactions
In the bupivacaine liposome injectable suspension surgical site infiltration studies, following bupivacaine liposome injectable suspension administration adverse reactions with an incidence greater than or equal to 1% in the:
- Nervous System Disorders system organ class were dizziness (6.2%), headache (3.8%), somnolence (2.1%), hypoesthesia (1.5%), and lethargy (1.3%).
- Cardiac Disorders system organ class were tachycardia (3.9%) and bradycardia (1.6%).
Adverse Reactions Reported in All Local Infiltration Placebo-Controlled Trials in Adults
Adverse reactions with an incidence greater than or equal to 2% reported by adult patients in clinical studies who underwent a bunionectomy (Study 1) or hemorrhoidectomy (Study 2) [ see Clinical Studies (14.2)] that compared 106 mg of bupivacaine liposome injectable suspension (8 mL) to placebo and 266 mg of bupivacaine liposome injectable suspension (20 mL) to placebo are shown in Table 1.
Table 1: Treatment-Emergent Adverse Reactions with an Incidence Greater than or Equal to 2%: Local Infiltration Placebo-Controlled Studies in Adults (Studies 1 and 2) a Study 1: Bunionectomy
b Study 2: Hemorrhoidectomy; TEAE = treatment-emergent adverse event.
At each level of summation (overall, system organ class, preferred term), patients are only counted once.
Preferred terms are included where at least 2% of patients reported the event in any treatment group.
STUDY 1 a STUDY 2 b Bupivacaine Liposome
Injectable Suspension
Placebo Bupivacaine Liposome
Injectable Suspension
Placebo System Organ Class
Preferred Term(106 mg)
(N=97)
n (%)
(N=96)
n (%)(266 mg)
(N=95)
n (%)(N=94)
n (%)Any TEAE 53 (54.6) 59 (61.5) 10 (10.5) 17 (18.1) Gastrointestinal Disorders 41 (42.3) 38 (39.6) 7 (7.4) 13 (13.8) Nausea 39 (40.2) 36 (37.5) 2 (2.1) 1 (1.1) Vomiting 27 (27.8) 17 (17.7) 2 (2.1) 4 (4.3) Constipation 2 (2.1) 1 (1.0) 2 (2.1) 2 (2.1) Anal Hemorrhage 0 (0.0) 0 (0.0) 3 (3.2) 4 (4.3) Painful Defecation 0 (0.0) 0 (0.0) 2 (2.1) 5 (5.3) Rectal Discharge 0 (0.0) 0 (0.0) 1 (1.1) 3 (3.2) Nervous System Disorders 20 (20.6) 30 (31.3) 0 (0.0) 0 (0.0) Dizziness 11 (11.3) 25 (26.0) 0 (0.0) 0 (0.0) Headache 5 (5.2) 8 (8.3) 0 (0.0) 0 (0.0) Somnolence 5 (5.2) 1 (1.0) 0 (0.0) 0 (0.0) Syncope 2 (2.1) 0 (0.0) 0 (0.0) 0 (0.0) Skin And Subcutaneous Tissue Disorders 8 (8.2) 7 (7.3) 0 (0.0) 0 (0.0) Generalized Pruritus 5 (5.2) 6 (6.3) 0 (0.0) 0 (0.0) Pruritus 3 (3.1) 1 (1.0) 0 (0.0) 0 (0.0) Investigations 5 (5.2) 3 (3.1) 4 (4.2) 3 (3.2) Increased Alanine Aminotransferase 3 (3.1) 3 (3.1) 1 (1.1) 0 (0.0) Increased Aspartate Aminotransferase 3 (3.1) 2 (2.1) 0 (0.0) 0 (0.0) Increased Blood Creatinine 2 (2.1) 0 (0.0) 0 (0.0) 0 (0.0) Increased Body Temperature 0 (0.0) 0 (0.0) 3 (3.2) 3 (3.2) General Disorders and Administration Site Conditions 4 (4.1) 0 (0.0) 1 (1.1) 1 (1.1) Feeling Hot 2 (2.1) 0 (0.0) 0 (0.0) 0 (0.0) Pyrexia 2 (2.1) 0 (0.0) 1 (1.1) 1 (1.1) Infections And Infestations 2 (2.1) 1 (1.0) 0 (0.0) 0 (0.0) Fungal Infection 2 (2.1) 1 (1.0) 0 (0.0) 0 (0.0) Injury, Poisoning and Procedural Complications 2 (2.1) 0 (0.0) 0 (0.0) 0 (0.0) Post Procedural Swelling 2 (2.1) 0 (0.0) 0 (0.0) 0 (0.0) Metabolism And Nutrition Disorders 2 (2.1) 2 (2.1) 0 (0.0) 0 (0.0) Decreased Appetite 2 (2.1) 2 (2.1) 0 (0.0) 0 (0.0) Adverse Reactions Reported in Placebo-Controlled Nerve Block Clinical Studies in Adults
The safety of bupivacaine liposome injectable suspension was evaluated in four randomized, double-blind, placebo-controlled nerve block clinical studies (Studies 3, 6, 7, 8) [ see Clinical Studies (14.3, 14.4)] involving 469 bupivacaine liposome injectable suspension-treated adult patients and 357 placebo-treated patients who had various surgical procedures. Patients were administered placebo or a bupivacaine liposome injectable suspension dose of either 133 or 266 mg (two times the maximum recommended dose for these nerve blocks). In these studies, following bupivacaine liposome injectable suspension administration via nerve block (perineural use) the:
- Most Common adverse reactions (incidence greater than or equal to 10%) were nausea, pyrexia, and constipation.
- Common adverse reactions (incidence greater than or equal to 2% to less than 10%) were muscle twitching, dysgeusia, urinary retention, fatigue, headache, confusional state, hypotension, hypertension, oral hypoesthesia, generalized pruritus, hyperhidrosis, tachycardia, sinus tachycardia, anxiety, fall, increased body temperature, peripheral edema, sensory loss, increased hepatic enzyme, hiccups, hypoxia, and post-procedural hematoma.
- Less common adverse reactions (incidence less than 2%) were arrhythmia, atrial fibrillation, first degree atrioventricular block, bradycardia, left bundle branch block, right bundle branch block, cardiac arrest, impaired hearing, blurred vision, visual impairment, asthenia, chills, hyperthermia, cellulitis, lung infection, pneumonia, procedural nausea, wound dehiscence, wound secretion, electrocardiogram QT prolonged, white blood cell count increased, arthralgia, back pain, joint swelling, decreased mobility, muscle spasms, muscular weakness, musculoskeletal pain, paraesthesia, presyncope, sedation, somnolence, syncope, delirium, dysuria, urinary incontinence, atelectasis, cough, dyspnea, lung infiltration, blister, drug eruption, erythema, rash, urticaria, deep vein thrombosis, hematoma, and orthostatic hypotension.
The most common and common adverse reactions for the four randomized, double-blind, placebo-controlled nerve block clinical studies (Studies 3, 6, 7, 8) are shown in Table 3.
Neurological and Cardiac Adverse Reactions
In the bupivacaine liposome injectable suspension nerve block placebo-controlled studies, following bupivacaine liposome injectable suspension administration adverse reactions with an incidence greater than or equal to 1% in the:
- Nervous System Disorders system organ class were motor dysfunction (14.9%), dysgeusia (7.2%), headache (5.1%), hypoesthesia (2.3%), and sensory loss (2.3%).
- Cardiac Disorders system organ class were tachycardia (3%), sinus tachycardia (2.3%), and bradycardia (1.3%).
Table 3: Treatment-Emergent Adverse Reactions with an Incidence Greater than or Equal to 2%: Nerve Block Placebo-Controlled Studies (Studies 3, 6, 7, and 8) At each level of summation (overall, system organ class, preferred term), patients are only counted once.
Preferred terms are included where at least 2% of patients reported the event in any treatment group.
TEAE = treatment-emergent adverse event.
SYSTEM ORGAN CLASS
Preferred TermBupivacaine
Liposome
Injectable
Suspension
133 mg
(N=168)
n (%)Bupivacaine
Liposome
Injectable
Suspension
266 mg
(N=301)
n (%)Placebo
(N=357)
n (%)Number of Patients with at Least One TEAE 152 (90.5) 260 (86.4) 299 (83.8) Blood and Lymphatic System Disorders 2 (1.2) 22 (7.3) 15 (4.2) Anemia 2 (1.2) 18 (6.0) 13 (3.6) Cardiac Disorders 13 (7.7) 34 (11.3) 38 (10.6) Atrial Fibrillation 1 (0.6) 4 (1.3) 8 (2.2) Sinus Tachycardia 3 (1.8) 8 (2.7) 4 (1.1) Tachycardia 3 (1.8) 11 (3.7) 10 (2.8) Gastrointestinal Disorders 84 (50.0) 154 (51.2) 184 (51.5) Constipation 29 (17.3) 66 (21.9) 68 (19.0) Dyspepsia 3 (1.8) 7 (2.3) 7 (2.0) Oral Hypoesthesia 6 (3.6) 8 (2.7) 7 (2.0) Nausea 62 (36.9) 111 (36.9) 133 (37.3) Vomiting 17 (10.1) 55 (18.3) 73 (20.4) General Disorders and Administration Site Conditions 52 (31.0) 102 (33.9) 91 (25.5) Fatigue 7 (4.2) 15 (5.0) 15 (4.2) Feeling Cold 0 10 (3.3) 8 (2.2) Peripheral Edema 4 (2.4) 6 (2.0) 8 (2.2) Peripheral Swelling 3 (1.8) 8 (2.7) 4 (1.1) Pyrexia 36 (21.4) 70 (23.3) 64 (17.9) Injury, Poisoning and Procedural Complications 18 (10.7) 44 (14.6) 32 (9.0) Postoperative Anemia 0 8 (2.7) 10 (2.8) Contusion 4 (2.4) 1 (0.3) 0 Fall 4 (2.4) 8 (2.7) 1 (0.3) Post Procedural Hematoma 4 (2.4) 1 (0.3) 0 Procedural Hypotension 2 (1.2) 13 (4.3) 7 (2.0) Investigations 18 (10.7) 31 (10.3) 31 (8.7) Increased Body Temperature 1 (0.6) 10 (3.3) 4 (1.1) Increased Hepatic Enzyme 7 (4.2) 1 (0.3) 3 (0.8) Metabolism and Nutrition Disorders 13 (7.7) 18 (6.0) 25 (7.0) Hypokalemia 7 (4.2) 9 (3.0) 14 (3.9) Musculoskeletal and Connective Tissue Disorders 22 (13.1) 47 (15.6) 41 (11.5) Decreased Mobility 0 6 (2.0) 5 (1.4) Muscle Twitching 14 (8.3) 21 (7.0) 25 (7.0) Nervous System Disorders 72 (42.9) 101 (33.6) 112 (31.4) Dizziness 8 (4.8) 28 (9.3) 40 (11.2) Dysgeusia 12 (7.1) 22 (7.3) 21 (5.9) Headache 14 (8.3) 10 (3.3) 10 (2.8) Hypoesthesia 6 (3.6) 5 (1.7) 2 (0.6) Motor Dysfunction 35 (20.8) 35 (11.6) 37 (10.4) Sensory Loss 4 (2.4) 7 (2.3) 1 (0.3) Psychiatric Disorders 10 (6.0) 33 (11.0) 44 (12.3) Anxiety 3 (1.8) 9 (3.0) 6 (1.7) Confusional State 3 (1.8) 15 (5.0) 14 (3.9) Insomnia 5 (3.0) 10 (3.3) 19 (5.3) Renal and Urinary Disorders 9 (5.4) 31 (10.3) 31 (8.7) Urinary Retention 5 (3.0) 23 (7.6) 22 (6.2) Respiratory, Thoracic and Mediastinal Disorders 18 (10.7) 30 (10.0) 31 (8.7) Dyspnea 2 (1.2) 4 (1.3) 8 (2.2) Hiccups 4 (2.4) 4 (1.3) 1 (0.3) Hypoxia 4 (2.4) 3 (1.0) 3 (0.8) Skin and Subcutaneous Tissue Disorders 24 (14.3) 63 (20.9) 84 (23.5) Hyperhidrosis 1 (0.6) 14 (4.7) 15 (4.2) Pruritus 10 (6.0) 45 (15.0) 55 (15.4) Generalized Pruritus 6 (3.6) 7 (2.3) 14 (3.9) Vascular Disorders 16 (9.5) 30 (10.0) 44 (12.3) Hypertension 3 (1.8) 15 (5.0) 21 (5.9) Hypotension 11 (6.5) 8 (2.7) 19 (5.3) 6.2 Postmarketing Experience
Because adverse reactions reported during postmarketing are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
These adverse reactions are consistent with those observed in clinical studies and most commonly involve the following system organ classes: Injury, Poisoning, and Procedural Complications (e.g., drug-drug interaction, procedural pain), Nervous System Disorders (e.g., palsy, seizure), General Disorders And Administration Site Conditions (e.g., lack of efficacy, pain), Skin And Subcutaneous Tissue Disorders (e.g., erythema, rash), and Cardiac Disorders (e.g., bradycardia, cardiac arrest).
-
7. DRUG INTERACTIONS
The toxic effects of local anesthetics are additive and concomitant use should be used with caution including monitoring for neurologic and cardiovascular effects related to local anesthetic systemic toxicity [ See Dosage and Administration ( 2.2), Warnings and Precautions ( 5.1), and Overdosage ( 10) ]. Avoid additional use of local anesthetics within 96 hours following administration of bupivacaine liposome injectable suspension.
Patients who are administered local anesthetics, including bupivacaine liposome injectable suspension, may be at increased risk of developing methemoglobinemia when concurrently exposed to the following drugs, which could include other local anesthetics:
Class Examples Nitrates/Nitrites nitric oxide, nitroglycerin, nitroprusside, nitrous oxide Local anesthetics articaine, benzocaine, bupivacaine, lidocaine, mepivacaine, prilocaine, procaine, ropivacaine, tetracaine Antineoplastic agents cyclophosphamide, flutamide, hydroxyurea, ifosfamide, rasburicase Antibiotics dapsone, nitrofurantoin, para-aminosalicylic acid, sulfonamides Antimalarials chloroquine, primaquine Anticonvulsants Phenobarbital, phenytoin, sodium valproate Other drugs acetaminophen, metoclopramide, quinine, sulfasalazine Bupivacaine
Bupivacaine HCl administered together with bupivacaine liposome injectable suspension may impact the pharmacokinetic and/or physicochemical properties of bupivacaine liposome injectable suspension, and this effect is concentration dependent. Therefore, bupivacaine HCl and bupivacaine liposome injectable suspension may be administered simultaneously in the same syringe, and bupivacaine HCl may be injected immediately before bupivacaine liposome injectable suspension as long as the ratio of the milligram dose of bupivacaine HCl solution to bupivacaine liposome injectable suspension does not exceed 1:2.
Non-Bupivacaine Local Anesthetics
Bupivacaine liposome injectable suspension should not be admixed with local anesthetics other than bupivacaine. Non-bupivacaine based local anesthetics, including lidocaine, may cause an immediate release of bupivacaine from bupivacaine liposome injectable suspension if administered together locally. The administration of bupivacaine liposome injectable suspension may follow the administration of lidocaine after a delay of 20 minutes or more. There are no data to support administration of other local anesthetics prior to administration of bupivacaine liposome injectable suspension.
Other than bupivacaine as noted above, bupivacaine liposome injectable suspension should not be admixed with other drugs prior to administration.
Water and Hypotonic Agents
Do not dilute bupivacaine liposome injectable suspension with water or other hypotonic agents, as it will result in disruption of the liposomal particles.
-
8. USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no studies conducted with bupivacaine liposome injectable suspension in pregnant women. In animal reproduction studies, embryo-fetal deaths were observed with subcutaneous administration of bupivacaine to rabbits during organogenesis at a dose equivalent to 1.6 times the maximum recommended human dose (MRHD) of 266 mg. Subcutaneous administration of bupivacaine to rats from implantation through weaning produced decreased pup survival at a dose equivalent to 1.5 times the MRHD [ see Data]. Based on animal data, advise pregnant women of the potential risks to a fetus.
The background risk of major birth defects and miscarriage for the indicated population is unknown. However, the background risk in the U.S. general population of major birth defects is 2% to 4% and of miscarriage is 15% to 20% of clinically recognized pregnancies.
Clinical Considerations
Labor or Delivery
Bupivacaine is contraindicated for obstetrical paracervical block anesthesia. While bupivacaine liposome injectable suspension has not been studied with this technique, the use of bupivacaine for obstetrical paracervical block anesthesia has resulted in fetal bradycardia and death.
Bupivacaine can rapidly cross the placenta, and when used for epidural, caudal, or pudendal block anesthesia, can cause varying degrees of maternal, fetal, and neonatal toxicity [ See Clinical Pharmacology ( 12.3)]. The incidence and degree of toxicity depend upon the procedure performed, the type, and amount of drug used, and the technique of drug administration. Adverse reactions in the parturient, fetus, and neonate involve alterations of the central nervous system, peripheral vascular tone, and cardiac function.
Data
Animal Data
Bupivacaine hydrochloride was administered subcutaneously to rats and rabbits during the period of organogenesis (implantation to closure of the hard plate). Rat doses were 4.4, 13.3, and 40 mg/kg/day (equivalent to 0.2, 0.5 and 1.5 times the MRHD, respectively, based on the BSA comparisons and a 60 kg human weight) and rabbit doses were 1.3, 5.8, and 22.2 mg/kg/day (equivalent to 0.1, 0.4 and 1.6 times the MRHD, respectively, based on the BSA comparisons and a 60 kg human weight). No embryo-fetal effects were observed in rats at the doses tested with the high dose causing increased maternal lethality. An increase in embryo-fetal deaths was observed in rabbits at the high dose in the absence of maternal toxicity.
Decreased pup survival was noted at 1.5 times the MRHD in a rat pre- and post-natal development study when pregnant animals were administered subcutaneous doses of 4.4, 13.3, and 40 mg/kg/day bupivacaine hydrochloride (equivalent to 0.2, 0.5 and 1.5 times the MRHD, respectively, based on the BSA comparisons and a 60 kg human weight) from implantation through weaning (during pregnancy and lactation).
8.2 Lactation
Risk Summary
Limited published literature reports that bupivacaine and its metabolite, pipecoloxylidide, are present in human milk at low levels. There is no available information on effects of the drug in the breastfed infant or effects of the drug on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for bupivacaine liposome injectable suspension and any potential adverse effects on the breastfed infant from bupivacaine liposome injectable suspension or from the underlying maternal condition.
8.4 Pediatric Use
Safety and effectiveness of bupivacaine liposome injectable suspension have not been established to produce postsurgical:
- Local analgesia via infiltration in pediatric patients aged less than 6 years old.
- Regional analgesia via interscalene brachial plexus nerve block in pediatric patients.
8.5 Geriatric Use
Of the total number of patients in the bupivacaine liposome injectable suspension local infiltration clinical studies (N=823), 171 patients were greater than or equal to 65 years of age and 47 patients were greater than or equal to 75 years of age. Of the total number of patients in the bupivacaine liposome injectable suspension nerve block clinical studies (N= 1046), 312 patients were greater than or equal to 65 years of age and 70 patients were greater than or equal to 75 years of age. No overall differences in safety or effectiveness of bupivacaine liposome injectable suspension have been observed between patients 65 years of age and older and younger adult patients.
In clinical studies, differences in various pharmacokinetic parameters have been observed between patients 65 years of age and older and younger adult patients. Bupivacaine is known to be substantially excreted by the kidney, and the risk of adverse reactions to bupivacaine may be greater in patients with renal impairment than in patients with normal renal function. Because patients 65 years of age and older are more likely to have renal impairment, increase monitoring for bupivacaine liposome injectable suspension -associated adverse reactions [ see Adverse Reactions (6)].
8.6 Hepatic Impairment
Amide-type local anesthetics, such as bupivacaine, are metabolized by the liver. Patients with severe hepatic disease, because of their inability to metabolize local anesthetics normally, are at a greater risk of developing toxic plasma concentrations, and potentially local anesthetic systemic toxicity [ see Clinical Pharmacology (12.3)]. Therefore, consider increased monitoring for local anesthetic systemic toxicity in patients with moderate to severe hepatic disease.
8.7 Renal Impairment
Bupivacaine is known to be substantially excreted by the kidney, and the risk of adverse reactions to bupivacaine liposome injectable suspension may be greater in patients with renal impairment than in patients with normal renal function. Therefore, in patients with renal impairment, increase monitoring for bupivacaine liposome injectable suspension-associated adverse reactions [ see Adverse Reactions (6)].
-
10. OVERDOSAGE
Clinical Presentation
Acute emergencies from local anesthetics are generally related to high plasma concentrations encountered during therapeutic use of local anesthetics or to unintended intravascular injection of local anesthetic solution [ See Warnings and Precautions ( 5) and Adverse Reactions ( 6)] .
Signs and symptoms of overdose include CNS symptoms (perioral paresthesia, dizziness, dysarthria, confusion, mental obtundation, sensory and visual disturbances, and eventually convulsions) and cardiovascular effects (that range from hypertension and tachycardia to myocardial depression, hypotension, bradycardia, and asystole).
Plasma levels of bupivacaine associated with toxicity can vary. Although concentrations of 2,500 to 4,000 ng/mL have been reported to elicit early subjective CNS symptoms of bupivacaine toxicity, symptoms of toxicity have been reported at levels as low as 800 ng/mL.
Management of Local Anesthetic Overdose
At the first sign of change, oxygen should be administered.
The first step in the management of convulsions, as well as underventilation or apnea, consists of immediate attention to the maintenance of a patent airway and assisted or controlled ventilation with oxygen and a delivery system capable of permitting immediate positive airway pressure by mask. Immediately after the institution of these ventilatory measures, the adequacy of the circulation should be evaluated, keeping in mind that drugs used to treat convulsions sometimes depress the circulation when administered intravenously. Should convulsions persist despite adequate respiratory support, and if the status of the circulation permits, small increments of an ultra-short acting barbiturate (such as thiopental or thiamylal) or a benzodiazepine (such as diazepam) may be administered intravenously. The clinician should be familiar, prior to the use of anesthetics, with these anticonvulsant drugs. Supportive treatment of circulatory depression may require administration of intravenous fluids and, when appropriate, a vasopressor dictated by the clinical situation (such as ephedrine to enhance myocardial contractile force).
If not treated immediately, both convulsions and cardiovascular depression can result in hypoxia, acidosis, bradycardia, arrhythmias, and cardiac arrest. If cardiac arrest should occur, standard cardiopulmonary resuscitative measures should be instituted.
Endotracheal intubation, employing drugs and techniques familiar to the clinician, may be indicated, after initial administration of oxygen by mask, if difficulty is encountered in the maintenance of a patent airway or if prolonged ventilatory support (assisted or controlled) is indicated.
-
11. DESCRIPTION
Bupivacaine liposome injectable suspension is a sterile, non-pyrogenic white to off-white preservative-free aqueous suspension consisting of multivesicular liposomes containing bupivacaine for infiltration and interscalene brachial plexus nerve block. Bupivacaine is present at a concentration of 13.3 mg/mL. After injection of bupivacaine liposome injectable suspension, bupivacaine is released from the multivesicular liposomes. Bupivacaine liposome injectable suspension is for infiltration or perineural use.
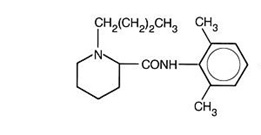
Active Ingredient
Bupivacaine is related chemically and pharmacologically to the amide-type local anesthetics. It is a homologue of mepivacaine and is related chemically to lidocaine. All three of these anesthetics contain an amide linkage between the aromatic nucleus and the amino, or piperidine group. They differ in this respect from the procaine-type local anesthetics, which have an ester linkage. Chemically, bupivacaine is 1-butyl-N-(2,6-dimethylphenyl)-2-piperidinecarboxamide with a molecular weight of 288.4. Bupivacaine has the following structural formula:
Bupivacaine Liposome Injectable Suspension
The median diameter of the liposome particles in bupivacaine liposome injectable suspension ranges from 22 to 30 μm. The liposomes are suspended in a 0.9% Sodium Chloride Injection. Each vial contains bupivacaine at a nominal concentration of 13.3 mg/mL. Inactive ingredients and their nominal concentrations are: cholesterol, 4.7 mg/mL; 1, 2-dipalmitoyl-sn-glycero-3 phospho-rac-(1-glycerol) sodium salt (DPPG), 0.9 mg/mL; tricaprylin, 2.0 mg/mL; 1, 2-dierucoylphosphatidylcholine (DEPC), 8.2 mg/mL; and phosphoric acid to adjust pH. The pH of bupivacaine liposome injectable suspension is in the range of 5.8 to 7.4.
Bupivacaine in bupivacaine liposome injectable suspension has different functional properties relative to those of the unencapsulated or nonlipid-associated bupivacaine products. Bupivacaine that is released from bupivacaine liposome injectable suspension has a different pharmacokinetic and systemic profile relative to other bupivacaine products. In addition, the nominal weight percent concentration of bupivacaine in bupivacaine liposome injectable suspension is based on bupivacaine free base rather than bupivacaine HCl (100 mg of bupivacaine HCl contains 88.6 mg of bupivacaine free base) [ see Dosage and Administration (2.1)].
-
12. CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Local anesthetics block the generation and the conduction of nerve impulses presumably by increasing the threshold for electrical excitation in the nerve, by slowing the propagation of the nerve impulse, and by reducing the rate of rise of the action potential. In general, the progression of anesthesia is related to the diameter, myelination, and conduction velocity of affected nerve fibers. Clinically, the order of loss of nerve function is as follows: (1) pain, (2) temperature, (3) touch, (4) proprioception, and (5) skeletal muscle tone.
12.2 Pharmacodynamics
Systemic absorption of local anesthetics produces effects on the cardiovascular and central nervous systems. At blood concentrations achieved with normal therapeutic doses, changes in cardiac conduction, excitability, refractoriness, contractility, and peripheral vascular resistance are minimal. However, toxic blood concentrations depress cardiac conductivity and excitability, which may lead to atrioventricular block, ventricular arrhythmias, and cardiac arrest, sometimes resulting in fatalities. In addition, myocardial contractility is depressed and peripheral vasodilation occurs, leading to decreased cardiac output and arterial blood pressure. Clinical reports and animal research suggest that these cardiovascular changes are more likely to occur after accidental intravascular injection of bupivacaine.
Following systemic absorption, local anesthetics can produce central nervous system stimulation, depression, or both. Apparent central stimulation is manifested as restlessness, tremors, and shivering progressing to convulsions, followed by depression and coma progressing ultimately to respiratory arrest. However, the local anesthetics have a primary depressant effect on the medulla and on higher centers. The depressed stage may occur without a prior excited state.
12.3 Pharmacokinetics
After administration of bupivacaine liposome injectable suspension, the systemic plasma levels of bupivacaine were observed for 96 hours after local infiltration and 120 hours after interscalene brachial plexus nerve block. [ see Warnings and Precautions ( 5.2) ]. In general, peripheral nerve blocks have shown systemic plasma levels of bupivacaine for extended duration when compared to local infiltration. Systemic plasma levels of bupivacaine following administration of bupivacaine liposome injectable suspension are not correlated with local efficacy.
Absorption
The rate of systemic absorption of bupivacaine is dependent upon the total dose of bupivacaine liposome injectable suspension administered, the route of administration, and the vascularity of the administration site.
Pharmacokinetic parameters of bupivacaine liposome injectable suspension after local infiltration and following an interscalene brachial plexus nerve block were evaluated following surgical procedures. Descriptive statistics of pharmacokinetic parameters of representative bupivacaine liposome injectable suspension doses in each study are provided in Table 5 for adult patients after administration of single doses of bupivacaine liposome injectable suspension via local infiltration; and Table 6 for adult patients after administration of single doses of bupivacaine liposome injectable suspension via nerve block.
Table 5: Summary of Pharmacokinetic Parameters for Bupivacaine after Administration of Single Doses of Bupivacaine Liposome Injectable Suspension via Local Infiltration in Adult Patients * Arithmetic mean (standard deviation) except T max where it is median (minimum, maximum).
1 Patients undergoing bunionectomy (Study 1)
2 Patients undergoing hemorrhoidectomy (Study 2)
3 Patients undergoing open posterior spinal fusion or reconstructive surgery
4 Patients undergoing posterolateral thoracotomy
5 AUC 0-last, 0-72h; 6 AUC 0-last, 0-96h ;
NE: Not evaluated
Parameters* Bunionectomy 1
106 mg (8 mL)Hemorrhoidectomy 2
266 mg (20 mL)Spine Surgery 3
266 mg (20 mL)Cardiothoracic Surgery 4
266 mg (20 mL)(N=26) (N=25) (N=11) (N=5) C max (ng/mL) 166 (93) 867 (353) 513 (268) 445 (120) T max (h) 2 (0.5, 24) 0.5 (0.25, 36) 0.6 (0.2, 37) 0.6 (0.6, 36) AUC 0-40h
(h x ng/mL)NE NE 13035 (8782) 9867 (1332) AUC (0-last)
(h x ng/mL)5864 (2038) 5 16867 (7868) 5 17214 (11621) 6 14277 (3449) 6 AUC (inf)
(h x ng/mL)7105 (2283) 18289 (7569) 17917 (12187) 15768 (4530) t ½ (h) 34 (17) 24 (39) 9 (2) 14 (6) Table 6: Summary of Pharmacokinetic Parameters for Bupivacaine after Administration of Single Doses of Bupivacaine Liposome Injectable Suspension via Nerve Block in Adult Patients (Study 3) * Arithmetic mean (standard deviation) except T max where it is median (minimum, maximum).
1 Patients undergoing total shouder arthroplasty (Study 3)
4 AUC 0-last, 0-120h; NE: Not evaluated
Parameters* Interscalene Brachial Plexus Nerve Block 1 Bupivacaine Liposome Injectable Suspension 133 mg (10 mL) (N = 12) C max (ng/mL) 207 (137) T max (h) 48 (3, 74) AUC (0-last) (h x ng/mL) 11484 (8615) 4 AUC (inf) (h x ng/mL) 11590 (8603) t ½ (h) 11 (5) Distribution
After bupivacaine has been released from bupivacaine liposome injectable suspension and is absorbed systemically, bupivacaine distribution is expected to be the same as for any bupivacaine HCl solution formulation.
Local anesthetics including bupivacaine are distributed to some extent to all body tissues, with high concentrations found in highly perfused organs such as the liver, lungs, heart, and brain.
Local anesthetics including bupivacaine appear to cross the placenta by passive diffusion. The rate and degree of diffusion is governed by (1) the degree of plasma protein binding, (2) the degree of ionization, and (3) the degree of lipid solubility. Fetal/maternal ratios of local anesthetics appear to be inversely related to the degree of plasma protein binding, because only the free, unbound drug is available for placental transfer. Bupivacaine with a high protein binding capacity (95%) has a low fetal/maternal ratio (0.2 to 0.4). The extent of placental transfer is also determined by the degree of ionization and lipid solubility of the drug. Lipid soluble, non-ionized drugs such as bupivacaine readily enter the fetal blood from the maternal circulation.
Elimination
Metabolism
Amide-type local anesthetics, such as bupivacaine, are metabolized primarily in the liver via conjugation with glucuronic acid. Pipecoloxylidide (PPX) is the major metabolite of bupivacaine; approximately 5% of bupivacaine is converted to PPX. Elimination of drug depends largely upon the availability of plasma protein binding sites in the circulation to carry it to the liver where it is metabolized.
Various pharmacokinetic parameters of the local anesthetics can be significantly altered by the presence of hepatic disease. Patients with hepatic disease, especially those with severe hepatic disease, may be more susceptible to the potential toxicities of the amide-type local anesthetics.
Excretion
After bupivacaine has been released from bupivacaine liposome injectable suspension and is absorbed systemically, bupivacaine excretion is expected to be the same as for other bupivacaine formulations.
The kidney is the main excretory organ for most local anesthetics and their metabolites. Only 6% of bupivacaine is excreted unchanged in the urine.
Urinary excretion is affected by urinary perfusion and factors affecting urinary pH. Acidifying the urine hastens the renal elimination of local anesthetics. Various pharmacokinetic parameters of the local anesthetics can be significantly altered by the presence of renal disease, factors affecting urinary pH, and renal blood flow.
Specific Populations
Hepatic Impairment
Because amide-type local anesthetics, such as bupivacaine, are metabolized by the liver, the effects of decreased hepatic function on bupivacaine pharmacokinetics following administration of bupivacaine liposome injectable suspension were studied in patients with moderate hepatic impairment. Consistent with the hepatic clearance of bupivacaine, mean plasma concentrations were higher in patients with moderate hepatic impairment than in the healthy control volunteers with approximately 1.5- and 1.6-fold increases in the mean values for C max and the area under the curve (AUC), respectively. [ See Warnings and Precautions ( 5.1) and Use in Specific Populations ( 8.6) ].
-
13. NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Long-term studies in animals to evaluate the carcinogenic potential of bupivacaine have not been conducted.
Mutagenesis
The mutagenic potential of bupivacaine has not been determined.
Impairment of Fertility
The effect of bupivacaine on fertility has not been determined.
-
14. CLINICAL STUDIES
14.1 Overview of Clinical Studies in Adult Patients
In three multicenter, randomized, double-blinded, placebo-controlled clinical studies in adults, the efficacy of bupivacaine liposome injectable suspension was established to produce postsurgical:
- Local analgesia via infiltration: One study evaluated the use of bupivacaine liposome injectable suspension in patients undergoing bunionectomy (Study 1); the other study evaluated the use of bupivacaine liposome injectable suspension in patients undergoing hemorrhoidectomy (Study 2) [ see Clinical Studies (14.2)].
- Regional analgesia via perineural use: one study (Study 3) evaluated the use of bupivacaine liposome injectable suspension as a brachial plexus nerve block via interscalene or supraclavicular approach in patients undergoing total shoulder arthroplasty (TSA) or rotator cuff repair (RCR) (only two patients had nerve blocks via the supraclavicular approach) [ see Clinical Studies (14.3)].
- Three additional studies (Studies 6, 7, and 8) [ see Clinical Studies (14.4)] did not provide sufficient efficacy and/or safety data to support an indication for the following nerve blocks: femoral block in patients undergoing total knee arthroplasty and intercostal nerve block in patients undergoing posterolateral thoracotomy [ see Indications and Usage (1)].
14.2 Studies in Adults to Produce Postsurgical Local Analgesia
Study 1: Infiltration for Bunionectomy in Adults
A multicenter, randomized, double-blind, placebo-controlled, parallel-group clinical trial (NCT00890682) (Study 1) evaluated the safety and efficacy of 106 mg (8 mL) bupivacaine liposome injectable suspension in 193 adult patients undergoing bunionectomy. The mean age was 43 years (range 18 to 72).
Study medication was administered directly into the site at the conclusion of the surgery, prior to closure. There was an infiltration of placebo or 7 mL of bupivacaine liposome injectable suspension into the tissues surrounding the osteotomy and 1 mL into the subcutaneous tissue.
Pain intensity was rated by the patients on a 0 to 10 numeric rating scale (NRS) out to 72 hours. Postoperatively, patients were allowed rescue medication (5 mg oxycodone/325 mg acetaminophen orally every 4 to 6 hours as needed) or, if that was insufficient within the first 24 hours, ketorolac (15 to 30 mg IV). The primary outcome measure was the area under the curve (AUC) of the NRS pain intensity scores (cumulative pain scores) collected over the first 24-hour period. There was a significant treatment effect for bupivacaine liposome injectable suspension compared to placebo. Bupivacaine liposome injectable suspension demonstrated a significant reduction in pain intensity compared to placebo for up to 24 hours. There was no significant difference in the amount of morphine equivalents used through 72 hours post-surgery, 43 mg versus 42 mg for placebo and bupivacaine liposome injectable suspension, respectively. In addition, there was not a significant difference in the percentage of patients that used ketorolac, 43% versus 31% for placebo and bupivacaine liposome injectable suspension, respectively.
Study 2: Infiltration for Hemorrhoidectomy in Adults
A multicenter, randomized, double-blind, placebo-controlled, parallel-group clinical trial (NCT00890721) (Study 2) evaluated the safety and efficacy of 266 mg (20 mL) bupivacaine liposome injectable suspension in 189 adult patients undergoing hemorrhoidectomy. The mean age was 48 years (range 18 to 86).
Bupivacaine liposome injectable suspension or placebo were administered directly into the site (greater than or equal to 3 cm) at the conclusion of the surgery. Dilution of 20 mL of bupivacaine liposome injectable suspension with 10 mL of saline, for a total of 30 mL, was divided into six 5-mL aliquots. A field block was performed by visualizing the anal sphincter as a clock face and slowly infiltrating one aliquot to each of the even numbers.
Pain intensity was rated by the patients on a 0 to 10 NRS at multiple time points up to 72 hours. Postoperatively, patients were allowed rescue medication (morphine sulfate 10 mg intramuscular every 4 hours as needed).
The primary outcome measure was the AUC of the NRS pain intensity scores (cumulative pain scores) collected over the first 72-hour period.
There was a significant treatment effect for bupivacaine liposome injectable suspension compared to placebo. See Figure 1 for the mean pain intensity over time for the bupivacaine liposome injectable suspension and placebo treatment groups for the 72- hour efficacy period.
Figure 1. Mean Pain Intensity versus Time plot for hemorrhoidectomy study (C-316)
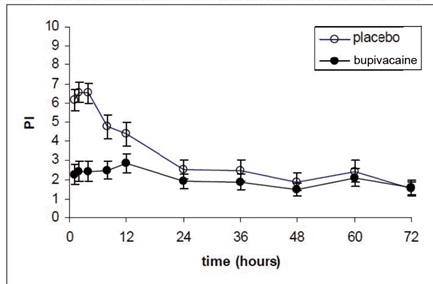
There were statistically significant, but small differences in the amount of opioid rescue analgesia used across the treatment groups, the clinical benefit of which has not been established. The median time to rescue analgesic use was 15 hours for patients treated with bupivacaine liposome injectable suspension and one hour for patients treated with placebo. Twenty-eight percent of patients treated with bupivacaine liposome injectable suspension required no rescue medication at 72 hours compared to 10% treated with placebo. For those patients who did require rescue medication, the mean amount of morphine sulfate intramuscular injections used over 72 hours was 22 mg for patients treated with bupivacaine liposome injectable suspension and 29 mg for patients treated with placebo.
14.3 Nerve Block Studies in Adults to Produce Postsurgical Regional Analgesia
Study 3: Interscalene Brachial Plexus Nerve Block for Total Shoulder Arthroplasty or Rotator Cuff Repair in Adults
A multicenter, randomized, double-blind, placebo-controlled study (NCT02713230) (Study 3) was conducted in 156 adult patients undergoing primary unilateral total shoulder arthroplasty or rotator cuff repair with general anesthesia. The mean age was 61 years (range 33 to 80). Prior to the surgical procedure, patients received 133 mg (10 mL) of bupivacaine liposome injectable suspension expanded with normal saline to 20 mL or placebo as a brachial plexus nerve block (perineural use) via interscalene or supraclavicular approach with ultrasound guidance. Only two patients received nerve block with bupivacaine liposome injectable suspension by supraclavicular approach. Postsurgically, patients were administered acetaminophen/paracetamol up to 1,000 mg orally or intravenously every 8 hours unless contraindicated. Patients were allowed opioid rescue medication administered initially as oral immediate-release oxycodone (initiating at 5 to 10 mg every 4 hours or as needed). If a patient could not tolerate oral medication, intravenous morphine (2.5 to 5 mg) or hydromorphone (0.5 to 1 mg) could be administered every 4 hours or as needed.
In Study 3, there was a statistically significant treatment effect for bupivacaine liposome injectable suspension compared to placebo in cumulative pain scores through 48 hours as measured by the AUC of the visual analog scale (VAS) pain intensity scores. There were statistically significant, but small differences in the amount of opioid consumption through 48 hours, the clinical benefit of which has not been demonstrated. For those patients who required rescue medication, the mean amount of morphine-equivalent opioid rescue used over 48 hours was 12 mg for bupivacaine liposome injectable suspension -treated patients and 54 mg for placebo- treated patients and 23 mg with bupivacaine liposome injectable suspension -treated patients vs. 70 mg for placebo -treated patients over 72 hours.
Although at 48 hours, 9 patients (13%) in the bupivacaine liposome injectable suspension group remained opioid-free compared to 1 patient (1%) in the placebo group, a difference which was statistically significant, at 72 hours, there were 4 (6%) patients in the bupivacaine liposome injectable suspension group who remained opioid-free compared to 1 (1%) patient in the placebo group, a difference that is not statistically significant.
14.4 Studies That Do Not Support an Indication for Certain Nerve Blocks in Adults
Studies 6 and 7: Inadequate Demonstration of Efficacy and Safety in Femoral Nerve Block in Total Knee Arthroplasty
Bupivacaine liposome injectable suspension was administered via a femoral nerve block in two placebo-controlled studies in adults (Studies 6 and 7). The results of these studies did not support a femoral nerve block indication due to inadequate safety data (Study 6) and/or due to inadequate efficacy findings (Study 7). In addition, patient falls were reported only in the bupivacaine liposome injectable suspension treatment groups, and none was reported in placebo groups.
Study 6
Study 6, a multicenter, randomized, double-blind, parallel-group, placebo-controlled study (NCT01683071), was conducted in 196 adult patients undergoing primary unilateral total knee arthroplasty (TKA) under general or spinal anesthesia. The mean age was 65 years (range 42 to 88). Prior to the surgical procedure, 266 mg (20 mL) of bupivacaine liposome injectable suspension or placebo was administered as a femoral nerve block with ultrasound guidance. Postsurgically, patients were allowed opioid rescue medication administered initially by intravenous injection of hydromorphone and subsequently by a patient-controlled analgesia (PCA) pump containing morphine or hydromorphone only. Once patients were tolerating oral medication, oral immediate-release oxycodone was administered on an as-needed basis (but not more than 10 mg every 4 hours) or, if that was insufficient, a third rescue of 1.25 mg/mL of 0.125% bupivacaine HCl was administered at a rate of 8 mL per hour via the previously placed femoral nerve catheter.
In this study, there was a statistically significant treatment effect for bupivacaine liposome injectable suspension compared to placebo in cumulative pain scores through 72 hours as measured by the AUC of the NRS pain (at rest) intensity scores.
There was a statistically significant, although small decrease in opioid consumption for the bupivacaine liposome injectable suspension treatment group compared to the placebo group, the clinical benefit of which has not been established. All patients in both the bupivacaine liposome injectable suspension and placebo treatment groups required opioid rescue medication during the first 72 hours. The mean amount of opioid rescue used over 72 hours was 76 mg for patients treated with bupivacaine liposome injectable suspension and 103 mg for patients treated with placebo.
The study was inadequate to fully characterize the safety of bupivacaine liposome injectable suspension when used for femoral nerve block due to patient falls, which occurred only in the bupivacaine liposome injectable suspension-treated patients and not in the placebo-treated patients.
Study 7
Study 7, a multicenter, randomized, double-blind, parallel-group, placebo-controlled study (NCT02713178), was conducted in 230 adult patients undergoing primary unilateral total knee arthroplasty (TKA) under general or spinal anesthesia. The mean age was 65 years (range 39 to 89). Prior to the surgical procedure, either 266 mg (20 mL) of bupivacaine liposome injectable suspension or 133 mg (10 mL) of bupivacaine liposome injectable suspension plus 10 mL of normal saline or placebo was administered as a femoral nerve block with ultrasound guidance. In addition to study drug, 8 mL of 0.5% bupivacaine HCl diluted with 8 mL of normal saline was administered by the surgeon as a periarticular infiltration to the posterior capsule (8 mL each behind the medial and lateral condyles) before placement of the prosthesis. Postsurgically, patients were allowed opioid rescue medication consisting of oral immediate-release oxycodone (initiated at 5 to 10 mg every 4 hours or as needed). If a patient could not tolerate oral medication, IV morphine (2.5 to 5 mg) or hydromorphone (0.5 to 1 mg) was permitted every 4 hours or as needed. Patient-controlled analgesia was not permitted. No other analgesic agents, including NSAIDs, were permitted through 108 hours.
However, to reflect the current standard of care of postsurgical multimodal therapy, all patients received cyclobenzaprine (a single dose of 10 mg orally or as needed) and acetaminophen/paracetamol (up to 1,000 mg orally or IV every 8 hours for a maximum total daily dose of 3000 mg) postsurgically.
In this study there were no statistically significant treatment effects for the bupivacaine liposome injectable suspension group compared to the placebo group in cumulative pain intensity scores or total opioid consumption. All patients in the bupivacaine liposome injectable suspension and placebo treatment groups required opioid rescue medication over 72 hours. The median Tmax of bupivacaine observed in this study was 72 hours with a range of 2.5 to 108 hours. Similar to Study 6, patient falls only occurred in the bupivacaine liposome injectable suspension-treated patients and not the placebo-treated patients.
Study 8: Lack of Efficacy in Intercostal Nerve Block for Posterolateral Thoracotomy
A multicenter, randomized, double-blind, placebo-controlled study was conducted in 191 adult patients undergoing posterolateral thoracotomy under general anesthesia (NCT01802411) (Study 8). The mean age was 58 years (range 18 to 82).
After the surgical procedure was completed but prior to the surgical site closure, 266 mg (20 mL) of bupivacaine liposome injectable suspension was administered by the surgeon as an intercostal nerve block divided into three equal doses in three syringes of approximately 88 mg in 6.6 mL volume per nerve, and administered to each of three nerve segments (index nerve, nerve above, and nerve below). Postsurgically, patients were allowed opioid rescue medication administered initially by intravenous fentanyl 100 mcg, which was to be administered once via bolus only. For the US sites, the second rescue medication was to be PCA-administered morphine or hydromorphone. For the European sites, the second rescue medication was to be intramuscular administered morphine up to 10 mg every 4 hours. At all sites, once a patient was tolerating oral medication, oral immediate-release oxycodone was administered (but not more than 10 mg every 4 hours). Patients who did not achieve adequate pain relief with this regimen were to be withdrawn from the study and followed for safety only.
In this study there were no statistically significant treatment effects for bupivacaine liposome injectable suspension 266 mg compared to placebo in cumulative pain intensity scores or total opioid consumption. Four percent of patients treated with bupivacaine liposome injectable suspension required no rescue medication at 72 hours compared to 1% treated with placebo. For those patients who did require rescue medication, the mean amount of opioid rescue used over 72 hours was 71 mg for patients treated with bupivacaine liposome injectable suspension and 71 mg for patients treated with placebo. The median T max of bupivacaine observed in this study was 1 hour with a range of 0.5 hours to 50 hours.
-
16. HOW SUPPLIED/STORAGE AND HANDLING
Bupivacaine liposome injectable suspension is a white to off-white milky aqueous suspension that is available in the following single-dose vials.
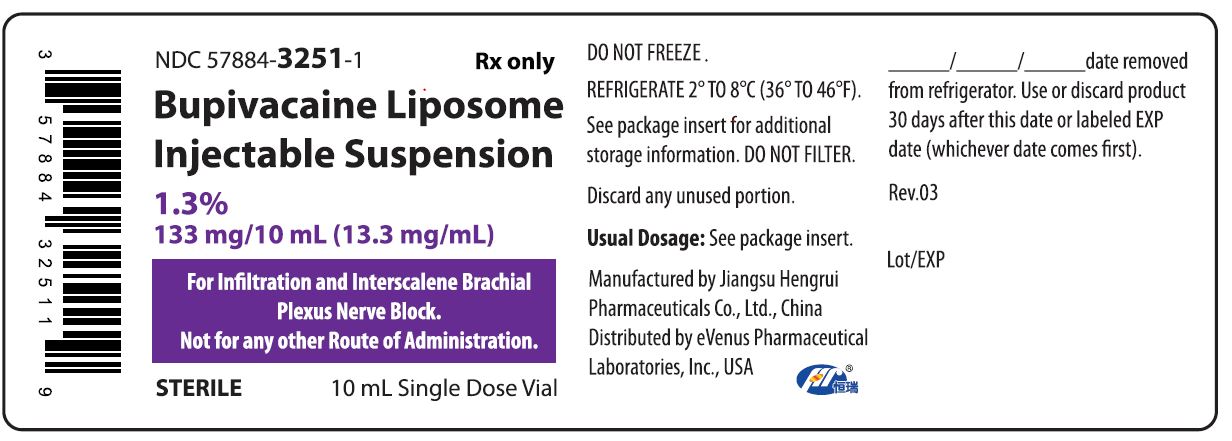
1.3% (133 mg/10 mL) (13.3 mg/mL) single-dose vial, (NDC: 57884-3251-1) packaged in cartons of 10 (NDC: 57884-3251-1)
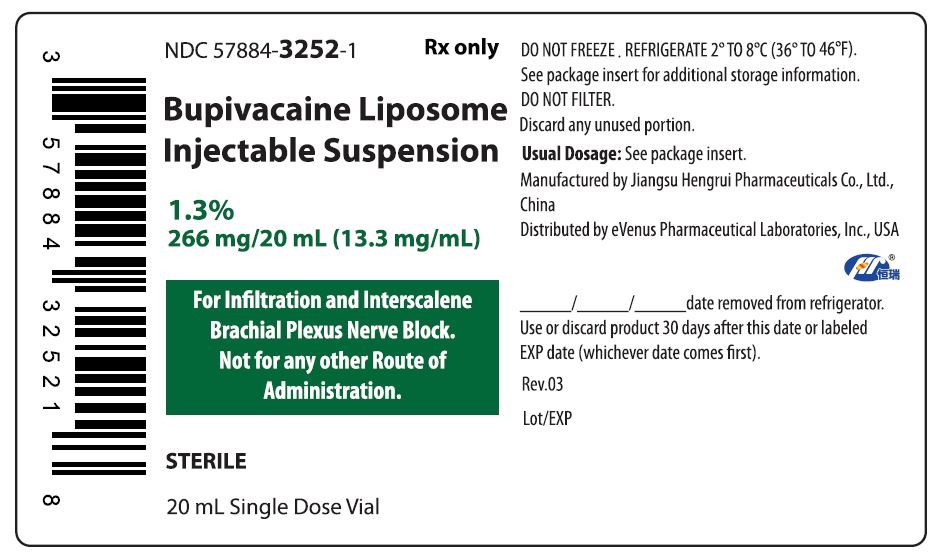
1.3% (266 mg/20 mL) (13.3 mg/mL) single-dose vial, (NDC: 57884-3252-1) packaged in cartons of 10 (NDC: 57884-3252-1)
Storage
Store bupivacaine liposome injectable suspension vials refrigerated between 2° to 8°C (36° to 46°F). Bupivacaine liposome injectable suspension may be held at a controlled room temperature of 20° to 25°C (68° to 77°F) for up to 30 days in sealed, intact (unopened) vials. Do not re-refrigerate vials.
Do not freeze or expose bupivacaine liposome injectable suspension to high temperatures (greater than 40°C or 104°F) for an extended period. Do not administer bupivacaine liposome injectable suspension if it is suspected of having been frozen or exposed to high temperatures. Do not use the vial if the stopper is bulging.
Handling
See Dosage and Administration ( 2.1, 2.4) for important preparation instructions.
-
17. PATIENT COUNSELING INFORMATION
Inform patients that use of local anesthetics may cause methemoglobinemia, a serious condition that must be treated promptly. Advise patients or caregivers to seek immediate medical attention if they or someone in their care experience the following signs or symptoms: pale, gray, or blue colored skin (cyanosis); headache; rapid heart rate; shortness of breath; lightheadedness; or fatigue.
Inform patients in advance that bupivacaine liposome injectable suspension can cause temporary loss of sensation or motor activity that may last for up to 5 days.
Manufactured by:
Jiangsu Hengrui Pharmaceuticals Co., Ltd.
Lianyungang, Jiangsu 222047, China
Distributed by:
eVenus Pharmaceutical Laboratories, Inc.
506 Carnegie Center, Suite 100,
Princeton, NJ 08540 USA
Revised: June 2024
Rev.06
- Container Label - 10 mL Vial Label
- Container Label - 20 mL Vial Label
-
INGREDIENTS AND APPEARANCE
BUPIVACAINE
bupivacaine injection, suspension, liposomalProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 57884-3251 Route of Administration INFILTRATION Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength BUPIVACAINE (UNII: Y8335394RO) (BUPIVACAINE - UNII:Y8335394RO) BUPIVACAINE 13.3 mg in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 57884-3251-1 10 in 1 CARTON 07/01/2024 1 10 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA214348 07/01/2024 BUPIVACAINE
bupivacaine injection, suspension, liposomalProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 57884-3252 Route of Administration INFILTRATION Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength BUPIVACAINE (UNII: Y8335394RO) (BUPIVACAINE - UNII:Y8335394RO) BUPIVACAINE 13.3 mg in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 57884-3252-1 10 in 1 CARTON 07/01/2024 1 20 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA214348 07/01/2024 Labeler - Jiangsu Hengrui Pharmaceuticals Co., Ltd. (654147255) Registrant - Jiangsu Hengrui Pharmaceuticals Co., Ltd. (654147255) Establishment Name Address ID/FEI Business Operations Jiangsu Hengrui Pharmaceuticals Co., Ltd. (Jinqiao Road Site) 699507972 api manufacture(57884-3251, 57884-3252) Establishment Name Address ID/FEI Business Operations Jiangsu Hengrui Pharmaceuticals Co., Ltd. (Dongjin Road Site) 421324417 manufacture(57884-3251, 57884-3252)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.