PYRIDOSTIGMINE BROMIDE tablet
Pyridostigmine Bromide by
Drug Labeling and Warnings
Pyridostigmine Bromide by is a Prescription medication manufactured, distributed, or labeled by Surgeon General-Department of the Army (TSG-DA). Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use Pyridostigmine Bromide Tablets USP 30 mg safely and effectively. See full prescribing information for Pyridostigmine Bromide Tablets USP 30 mg.
Pyridostigmine Bromide USP Tablets 30 mg for Oral Use
Initial U.S. Approval: 1955CAUTION: USE PYRIDOSTIGMINE BROMIDE AS PRETREATMENT ONLY. AFTER EXPOSURE TO SOMAN, USE ATROPINE AND 2-PAM. ALWAYS USE PROTECTIVE GARMENT(S)
See full prescribing information for complete boxed warning.
- Pyridostigmine bromide is for use as a pretreatment for exposure to soman nerve agent. Pyridostigmine bromide alone will not protect against exposure to soman. The efficacy of pyridostigmine bromide is dependent upon the rapid use of atropine and pralidoxime (2-PAM) after soman exposure.
- Primary protection against exposure to chemical nerve agents is the wearing of protective garments.
- Pyridostigmine bromide must not be taken after exposure to soman. If taken immediately before soman exposure (e.g., when the gas attack alarm is given) or at the same time as poisoning by soman, it is not expected to be effective and may exacerbate the effects of a sub-lethal exposure to soman.
INDICATIONS AND USAGE
Pyridostigmine bromide is a reversible cholinesterase inhibitor indicated for pretreatment against the lethal effects of soman nerve agent poisoning. (1)
Pyridostigmine bromide is for use in conjunction with
- Protective garments, including a gas mask, and
- Immediate atropine and pralidoxime therapy at the first sign of nerve agent poisoning. (1)
DOSAGE AND ADMINISTRATION
- One 30 mg tablet every 8 hours. (2)
- Start at least one (1) hour prior to exposure to Soman. (2)
- At the first sign of Soman poisoning pyridostigmine must be stopped, and atropine and 2-PAM be administered. (2)
- Use beyond 14 consecutive days should be evaluated in the context of the likelihood of Soman exposure. (2)
- Store refrigerated between 2 and 8°C (36 to 46°F). Protect from light. Do not dispense after removal from refrigeration for more than a total of 3 months. (16)
DOSAGE FORMS AND STRENGTHS
- 30 mg tablets (round, white imprinted with letters "PBT") (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- At the first sign of Soman poisoning pyridostigmine must be stopped, atropine and 2-PAM must be administered immediately. (5.1)
- Use with caution in persons with increased risk of anticholinergic reactions, such as persons with bronchial asthma, chronic obstructive pulmonary disease, bradycardia, cardiac arrhythmias, beta blocker treatment (increased risk of anticholinergic reactions). (5.2)
- Use with caution in persons with bromide sensitivity. (5.3)
- In case of serious adverse reactions, advise personnel to temporarily discontinue pyridostigmine and seek immediate medical attention. (5.4)
ADVERSE REACTIONS
Most common adverse reactions ( ≥ 3% ) are diarrhea, abdominal pain, dysmenorrhea, and twitch. (6)
To report SUSPECTED ADVERSE REACTIONS, contact U.S. Army Medical Materiel Development Activity at 301-619-0317 (fax 301-619-0197) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- Mefloquine: Additive effect on gastrointestinal tract and atrial rate. (7.1)
- Anticholinesterase drugs for glaucoma treatment: Additive effects. (7.2)
- Narcotics: Exacerbation of bradycardia possible. (7.3)
- Depolarizing neuromuscular blocking agents: Increased effect. (7.4)
- Non-depolarizing neuromuscular blocking agents: Dose may need to be increased. (7.4)
- Aminoglycoside antibiotics, local and some general anesthetics, antiarrhythmic agents, and other drugs that interfere with neuromuscular transmission should be used cautiously, if at all. (7.4)
- Drugs converted to pantothenic acid (e.g., dexpanthenol): Additive effect. (7.5)
USE IN SPECIFIC POPULATIONS
- Renal impairment: Increased risk of side effects; careful dose selection. In persons with renal impairment, renal function monitoring may be useful. (8.6)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 1/2017
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
CAUTION: USE PYRIDOSTIGMINE BROMIDE AS PRETREATMENT ONLY. AFTER EXPOSURE TO SOMAN, USE ATROPINE AND 2-PAM. ALWAYS USE PROTECTIVE GARMENT(S).
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Stopping Pyridostigmine Bromide and Using Atropine and 2-PAM in the Event of Soman Exposure
5.2 Individuals at Increased Risk of Anticholinergic Adverse Reactions
5.3 Use in Bromide-Sensitive Individuals
5.4 Action in Case of Serious Adverse Reactions
6 ADVERSE REACTIONS
6.1 Clinical Studies Experience
7 DRUG INTERACTIONS
7.1 Mefloquine
7.2 Other Anticholinesterase Drugs
7.3 Narcotics
7.4 Drugs that Interfere with Neuromuscular Transmission
7.5 Drugs Converted to Pantothenic Acid (e.g., Dexpanthenol)
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Persons with Renal Impairment
8.7 Persons with Hepatic Impairment
9 DRUG ABUSE AND DEPENDENCE
9.2 Abuse
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology and/or Pharmacology
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
17.1 Indication and Conditions of Use
17.2 Dosage and Administration
17.3 Contraindications and Precautions
17.4 Side Effects (Adverse Reactions)
17.5 Collection of Information
17.6 Questions and Requests for Information
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
CAUTION: USE PYRIDOSTIGMINE BROMIDE AS PRETREATMENT ONLY. AFTER EXPOSURE TO SOMAN, USE ATROPINE AND 2-PAM. ALWAYS USE PROTECTIVE GARMENT(S).
- Pyridostigmine bromide is for use as a pretreatment for exposure to soman nerve agent. Pyridostigmine bromide alone will not protect against exposure to soman. The efficacy of pyridostigmine bromide is dependent upon the rapid use of atropine and pralidoxime (2 PAM) after soman exposure. [See Dosage and Administration (2).]
- Primary protection against exposure to chemical nerve agents is the wearing of protective garments including masks, hoods, and overgarments designed specifically for this use.
Individuals must not rely solely upon pretreatment with pyridostigmine bromide and on the antidotes atropine and pralidoxime (2-PAM) to provide complete protection from poisoning by soman nerve agent. - Pyridostigmine bromide must not be taken after exposure to soman. If pyridostigmine bromide is taken immediately before exposure (e.g., when the gas attack alarm is given) or at the same time as poisoning by soman, it is not expected to be effective and may exacerbate the effects of a sub-lethal exposure to soman. [See Clinical Pharmacology (12.2).]
FOR MILITARY MEDICAL USE ONLY
-
1 INDICATIONS AND USAGE
Pyridostigmine bromide is indicated for pretreatment against the lethal effects of soman nerve agent poisoning. Pyridostigmine bromide is intended for use in conjunction with protective garments, including a mask. At the first sign of nerve agent poisoning, pyridostigmine bromide should be stopped, and atropine and pralidoxime therapy started immediately.
The evidence for the effectiveness of pyridostigmine bromide as pretreatment against soman-induced toxicity was derived from animal studies alone. [See Nonclinical Toxicology (13.2).]
FOR MILITARY MEDICAL USE ONLY
-
2 DOSAGE AND ADMINISTRATION
Pyridostigmine bromide is for use as a pretreatment for exposure to soman nerve agent. Pyridostigmine bromide alone will not protect against exposure to soman. The efficacy of pyridostigmine bromide is dependent upon the rapid use of atropine and pralidoxime (2-PAM) after soman exposure.
The primary protection against exposure to chemical nerve agents consists of wearing protective garments including masks, hoods, and overgarments designed specifically for this use.
Individuals must not rely solely upon pretreatment with pyridostigmine bromide and the antidotes atropine and pralidoxime (2-PAM) to provide complete protection from poisoning by soman nerve agent.
Pyridostigmine bromide must not be taken after exposure to soman. If pyridostigmine bromide is taken immediately before exposure (eg, when the gas attack alarm is given) or at the same time as poisoning by soman, it is not expected to be effective and may exacerbate the effects of a sublethal exposure to soman. [See Clinical Pharmacology (12.2).]
The dose of pyridostigmine bromide is one 30-mg tablet every 8 hours, started at least several hours prior to exposure to soman. At the first sign of nerve agent poisoning (runny nose; watery eyes; small, pinpoint pupils; eye pain; blurred vision; drooling and excessive sweating; cough; chest tightness; rapid breathing; diarrhea; increased urination; confusion; drowsiness; weakness; headache; nausea, vomiting, and/or abdominal pain; slow or fast heart rate; and/or abnormally low or high blood pressure), pyridostigmine bromide should be discontinued and treatment with atropine and pralidoxime should be instituted immediately.
There is no known advantage to taking pyridostigmine bromide just prior to or concurrent with soman exposure. According to the mechanism of action of pyridostigmine bromide [See Clinical Pharmacology (12.2)], pyridostigmine bromide is effective when it is given sufficiently in advance of soman poisoning to provide a pool of protected enzyme. Therefore, it is expected that pyridostigmine bromide will not be effective if administered just prior to or during exposure to soman.
The benefits and risks of use beyond 14 consecutive days have not been definitively established; therefore, continued use beyond 14 consecutive days should be evaluated in the context of the likelihood of exposure to soman nerve agent.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Stopping Pyridostigmine Bromide and Using Atropine and 2-PAM in the Event of Soman Exposure
See Dosage and Administration (2) and Boxed Caution statement (at beginning of Full Prescribing Information).
- - Pyridostigmine bromide pretreatment offers no benefit against the nerve agent soman unless the nerve agent antidotes atropine and pralidoxime (2-PAM) are administered once symptoms of poisoning appear. Pyridostigmine should be discontinued at the first sign of nerve agent poisoning (runny nose; watery eyes; small, pinpoint pupils; eye pain; blurred vision; drooling and excessive sweating; cough; chest tightness; rapid breathing; diarrhea; increased urination; confusion; drowsiness; weakness; headache; nausea, vomiting, and/or abdominal pain; slow or fast heart rate; and/or abnormally low or high blood pressure) because it may exacerbate the effects of a sub-lethal exposure to soman.
5.2 Individuals at Increased Risk of Anticholinergic Adverse Reactions
Pyridostigmine bromide should be used with caution in persons with bronchial asthma, chronic obstructive pulmonary disease, bradycardia, or cardiac arrhythmias and, for example, in people being treated for hypertension or glaucoma with beta adrenergic receptor blockers.
5.3 Use in Bromide-Sensitive Individuals
Caution should be taken when administering pyridostigmine bromide to individuals with known bromide sensitivity. The risks and benefits of administration must be weighed against the potential for rash or other adverse reactions in these individuals. [See Adverse Reactions (6).]
5.4 Action in Case of Serious Adverse Reactions
If personnel experience serious adverse reactions such as difficult breathing, severe dizziness, or loss of consciousness as a result of ingestion of pyridostigmine bromide, they should temporarily discontinue use of product and seek immediate medical attention. Personnel should report serious adverse events to their commander and responsible medical officer.
-
6 ADVERSE REACTIONS
The most common adverse reactions (≥ 3%) are diarrhea, abdominal pain, dysmenorrhea, and twitch.
The adverse reactions to pyridostigmine bromide are typically of two varieties: muscarinic and nicotinic. Muscarinic adverse reactions include abdominal cramps, bloating, flatulence, diarrhea, emesis, increased peristalsis, nausea, hypersalivation, urinary incontinence, increased bronchial secretion, diaphoresis, miosis, and lacrimation. Nicotinic adverse reactions are comprised chiefly of muscle cramps, fasciculations, and weakness.
Pyridostigmine bromide is a quaternary ammonium compound and does not readily cross the blood-brain barrier. Compared to the peripheral effects of pyridostigmine bromide, central nervous system manifestations are less frequent and less serious, primarily consisting of headache and vertigo, with minor and clinically insignificant changes in heart rate, blood pressure, and respiratory function.
Extremely high doses may produce central nervous system (CNS) symptoms of agitation, restlessness, confusion, visual hallucinations, and paranoid delusions. Electrolyte abnormalities, possibly resulting from high serum bromide concentrations, also have been reported. Death may result from cardiac arrest or respiratory paralysis and pulmonary edema.
As with any compound containing bromide, a skin rash may be observed in an occasional patient, which usually subsides promptly upon discontinuance of the medication.
6.1 Clinical Studies Experience
In a controlled study of 90 healthy volunteers comparing pyridostigmine bromide 30 mg every 8 hours to placebo for 21 days, the following incidences of adverse reactions was reported.
Table 1 Incidence of Adverse Reactions ≥ 2% Reaction: %
Pyridostigmine
N = 60%
Placebo
N = 30Diarrhea 7 0 Abdominal Pain 7 0 Dysmenorrhea 5 0 Twitch 3 0 Myalgia 2 0 Dry Skin 2 0 Urinary Frequency 2 0 Epistaxis 2 0 Amblyopia 2 0 Hypesthesia 2 0 Neck pain 2 0 Other less common adverse reactions seen during controlled and uncontrolled clinical trials for pyridostigmine include the following:
- Pulmonary: Exacerbation of acute bronchitis and asthma
- Cardiovascular: Elevated blood pressure, decreased heart rate (4-6 beats per minute), chest tightness
- Eyes: Change in vision, eye pain
- Neurologic: Headache, hypertonia, difficulty in concentrating, confusion, disturbed sleep, tingling of extremities, numbness of the tongue
- Skin: Increased sweating, rash, alopecia
- Digestive: Vomiting, borborygmi, nausea, bloating, flatulence
- General: Warm sensation, lethargy/drowsiness, depressed mood
During safety studies at the recommended dosage, there were two reports of loss of consciousness, one of which also included urinary and fecal incontinence, stiffness of the upper torso and arms, post-syncopal skin pallor, post-syncopal confusion, and post-syncopal weakness (suggesting a seizure event).
-
7 DRUG INTERACTIONS
7.1 Mefloquine
A potential interaction between the antimalarial drug mefloquine and pyridostigmine bromide exists through a possible additive effect on the gastrointestinal tract. The most common complaint about both drugs is loose bowels. It has been reported that simple additive effects on the atrial rate occur when mefloquine and pyridostigmine bromide are combined.
7.2 Other Anticholinesterase Drugs
Because anticholinesterase drugs are often used in the treatment of glaucoma, the use of pyridostigmine bromide in such situations may have an additive effect that may cause or exacerbate problems with night vision.
7.3 Narcotics
The bradycardia associated with the use of narcotics may exacerbate pyridostigmine-induced bradycardia.
7.4 Drugs that Interfere with Neuromuscular Transmission
Particular caution should be observed in the administration of depolarizing neuromuscular blocking agents (eg, succinylcholine) during surgery since the degree of neuromuscular blockade that ensues may be enhanced by previously administered pyridostigmine bromide. Doses of non-depolarizing neuromuscular blocking agents (eg, pancuronium bromide) may need to be increased in patients previously administered pyridostigmine bromide. Atropine antagonizes the muscarinic effects of pyridostigmine bromide, and this interaction is utilized to counteract the muscarinic symptoms of pyridostigmine bromide toxicity. Anticholinesterase agents are sometimes effective in reversing neuromuscular block induced by aminoglycoside antibiotics. However, aminoglycoside antibiotics, local and some general anesthetics, antiarrhythmic agents, and other drugs that interfere with neuromuscular transmission should be used cautiously, if at all, during treatment with pyridostigmine bromide.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category B
Pyridostigmine bromide produced no teratogenic effects in rats given up to 30 mg/kg/day and in rabbits given up to 45 mg/kg/day orally during the period of organogenesis. These doses are 3 and 10 times, respectively, the recommended human dose of 90 mg on an mg/m2 basis. In rats, a slight degree of delayed skeletal ossification was seen at 30 mg/kg, a dose which caused maternal toxicity, and a slight increase in the incidence of hydronephrosis was seen at all dose levels (lowest dose tested was 3 mg/kg). In rabbits, a slight increase in the incidence of hydronephrosis was seen at 45 mg/kg, a dose that caused maternal toxicity and increased incidences of blood vessel variations were seen at all doses (lowest dose tested was 5 mg/kg). There are no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
8.3 Nursing Mothers
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when pyridostigmine bromide is administered to a nursing woman.
8.5 Geriatric Use
Clinical studies of pyridostigmine bromide did not contain sufficient numbers of subjects aged 65 and over to determine whether they respond differently than younger subjects. In general, dose selection for an elderly patient should be cautious, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
In the elderly (71 to 85 years of age) the elimination half-life, volume of distribution (central and steady state) were comparable with the young (21to 51 years of age). However, the systemic plasma clearance was significantly lower in the elderly compared to the young (6.7 ± 2.2 vs. 9.5 ± 2.7 mL/min/kg).
This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
8.6 Persons with Renal Impairment
This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Caution should be observed, and dosage be selected carefully, when administering pyridostigmine bromide to patients with impaired renal function. In anephric patients, a 3-fold increase in the elimination half-life and a 75% decrease in systemic clearance were observed. [See Clinical Pharmacology (12.3).] It may be useful to monitor renal function.
-
9 DRUG ABUSE AND DEPENDENCE
9.2 Abuse
Although the abuse potential of pyridostigmine bromide has not been specifically assessed, no abuse of, tolerance to, withdrawal from, or drug-seeking behavior was observed in patients who received pyridostigmine bromide in clinical trials. Cholinesterase inhibitors are not believed to be associated with drug abuse.
-
10 OVERDOSAGE
As is true of all cholinergic drugs, overdosage of pyridostigmine bromide may result in cholinergic crisis, a state characterized by increasing muscle weakness that, through involvement of the muscles of respiration, may lead to death. Overdosage with pyridostigmine bromide must be differentiated from the acute manifestations of nerve agent poisoning, which may also be characterized by a cholinergic crisis. Atropine should be used to treat pyridostigmine bromide overdosage.
In the treatment of pyridostigmine bromide overdosage, maintaining adequate respiration is of primary importance. Tracheostomy, bronchial aspiration, and postural drainage may be required to maintain an adequate airway; respiration can be assisted mechanically if required. Supplemental oxygen may be necessary. Pyridostigmine bromide should be discontinued immediately and 1 mg to 4 mg of atropine sulfate administered intravenously. Additional doses of atropine may be given every 5 to30 minutes as needed to control muscarinic symptoms. Atropine overdosage should be avoided, as tenacious secretions and bronchial plugs may result. It should be kept in mind that unlike muscarinic effects, the skeletal muscle effects and consequent respiratory paralysis (nicotinic effects), which can occur following pyridostigmine overdosage, are not alleviated by atropine.
-
11 DESCRIPTION
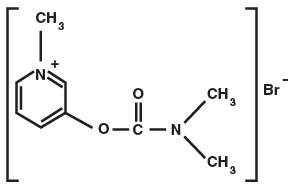
Pyridostigmine bromide is an orally active, reversible cholinesterase inhibitor. Its chemical name is: 3-hydroxy-1-methylpyridinium bromide dimethylcarbamate.
CAS registration number is 101-26-8.
Pyridostigmine bromide has a molecular formula of C9H13BrN2O2, a molecular weight of 261.12, and the following molecular structure:
Pyridostigmine bromide tablets, USP contain 30 mg of pyridostigmine bromide for oral administration. The inactive ingredients included in the tablet formula are colloidal silicon dioxide, lactose anhydrous, and stearic acid or, alternatively; lactose, starch, silica precipitated, talc, and magnesium stearate.
-
12 CLINICAL PHARMACOLOGY
12.2 Pharmacodynamics
The mechanism of soman-induced death is reasonably well understood. Death is believed to result primarily from respiratory failure due to irreversible inhibition of the enzyme acetylcholinesterase and the consequent increase in the level of the neurotransmitter acetylcholine 1) at nicotinic receptors at the neuromuscular junction, resulting in pathological stimulation and ultimate failure of the muscles of respiration, 2) at muscarinic receptors in secretory glands and smooth muscle, resulting in excessive respiratory secretions and bronchoconstriction, and 3) at cholinergic receptors in the brain, resulting in central respiratory depression.
The effect of pyridostigmine is presumed to result from its reversible inhibition of a critical number of acetylcholinesterase active sites in the peripheral nervous system, protecting them from irreversible inhibition by soman. (Pyridostigmine bromide is not thought to enter the brain in significant amounts.) When the pyridostigmine bromide-induced inhibition of the enzyme is subsequently reversed, there is a small residual amount of enzyme activity that is adequate to sustain life (provided atropine and 2-PAM are subsequently administered). An implication of this presumed mechanism is that it is not helpful to give pyridostigmine bromide either just before or during exposure to soman.
12.3 Pharmacokinetics
Pyridostigmine bromide is poorly absorbed from the gastrointestinal tract with an absolute bioavailability of 10% to 20%. Following a single oral dose of 30 mg pyridostigmine bromide in the fasting state, the TMAX was 2.2 ± 1.0 hours. The pharmacokinetics of pyridostigmine bromide is linear over the dose range of 30 mg to 60 mg. Following multiple doses of pyridostigmine bromide (30 mg every 8 hours for 21 days), the average steady-state trough concentration of pyridostigmine bromide was about ¼ of the peak concentration after a single dose.
The volume of distribution was about 19 ± 12 liters, indicating that pyridostigmine bromide distributes into tissues. No information on protein binding of pyridostigmine bromide is available.
Pyridostigmine bromide undergoes hydrolysis by cholinesterases and is metabolized in the liver. It is excreted in the urine as both unchanged drug and its metabolites. The systemic clearance of pyridostigmine bromide is 830 mL/min and the elimination half-life of pyridostigmine bromide is approximately 3 hours.
Renal Impairment
In anephric patients (n = 4), the elimination half-life increased 3 fold and the systemic clearance decreased by 75%. [See Use in Specific Populations (8.6).]
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Mutagenicity
Pyridostigmine bromide was mutagenic and clastogenic in an in vitro mammalian gene mutation assay in mouse lymphoma cells, in the presence of metabolic activation only. Pyridostigmine bromide was not mutagenic in an in vitro bacterial reverse mutation assay (Ames Test) or in an in vitro mammalian gene mutation assay in Chinese hamster ovary cells, and was not clastogenic in an in vitro assay in Chinese hamster ovary cells or in an in vivo mouse micronucleus assay.
13.2 Animal Toxicology and/or Pharmacology
Evidence of the effectiveness of pyridostigmine bromide as a pretreatment for soman poisoning was obtained from studies in animals alone, because it is unethical to perform such studies in humans. While the results of these animal studies cannot be extrapolated to humans with certainty, the extrapolation is supported by the reasonably well understood pathophysiologic mechanisms of the toxicity of soman and the mechanism of the protective effect of pyridostigmine bromide pretreatment, as examined in various animal species. In addition, the results of these animal studies establish that pyridostigmine bromide is reasonably likely to produce clinical benefit in humans. The section below explains the current understanding of the mechanism of soman toxicity and the beneficial effect of pyridostigmine bromide pretreatment, as well as the basis for extrapolating the animal findings to humans.
Pyridostigmine bromide pretreatment has been shown in animals to decrease the lethality of the soman nerve agent, provided atropine and pralidoxime (2-PAM) are administered immediately after exposure to soman.
Rhesus monkeys were given oral doses of pyridostigmine bromide every 8 hours for a total of 6 doses and were challenged with soman given intramuscularly 5 hours after the last pyridostigmine bromide dose. Two dosage groups of pyridostigmine bromide were used: a low-dose group given 1.2 mg/kg for all 6 doses and a high-dose group given 1.2 and 1.8 mg/kg for the first and second doses, respectively, and 2.4 mg/kg for the final 4 doses. These animals were also given atropine and 2-PAM after exposure to soman. An untreated control group and a group given atropine and 2-PAM (but not pyridostigmine bromide) were also used. The primary endpoint in this study was a decrease in the lethality of soman expressed as an increase in the LD50 (the dose of soman that killed 50 % of the animals). The atropine/2-PAM control group showed a small but statistically significant 1.6-fold increase in the soman LD50 compared to the untreated control group. The groups given pyridostigmine bromide as well as atropine and 2 PAM showed increases in the soman LD50 of at least 40-fold compared to the untreated control group and at least 25 fold compared to the atropine/2-PAM group. The two dose levels of pyridostigmine bromide showed similar effectiveness.
Additional studies in rhesus monkeys and guinea pigs also showed effectiveness of pyridostigmine bromide (in the presence of post-soman administration of atropine and 2-PAM). The magnitude of effect in guinea pigs was smaller than that in monkeys (soman LD50 increased 4 to 7 fold compared to untreated control and 2- to 4-fold compared to atropine/ 2-PAM alone).
Pyridostigmine bromide produced only small and inconsistent effects in studies in rats, mice, and rabbits. It is thought that the effect of pyridostigmine bromide in rats and mice is masked by high blood levels of the enzyme carboxylesterase, which eliminates soman from blood and makes those species highly resistant to soman. In a study in which rats were given an inhibitor of carboxylesterase, pretreatment with pyridostigmine bromide plus atropine and 2 PAM increased the LD50 of soman 8.5-fold compared to untreated controls. Humans have little or no carboxylesterase in blood.
Animal studies have shown that pyridostigmine bromide pretreatment was effective only when animals were given atropine and 2-PAM after exposure to soman.
- 14 CLINICAL STUDIES
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Pyridostigmine bromide tablets, USP, 30 mg, are round, white tablets imprinted with the letters "PBT."
Immediate Container: Twenty-one (21) tablets individually sealed in a blister or strip package which is supplied in a protective sleeve.
NDC: 72458-128-01
NSN 6505-01-178-7903
The NSN refers to the actual unit that is ordered from supply (if someone orders 1 of this stock number they will get one package of 10 blister packs).
-
17 PATIENT COUNSELING INFORMATION
Pyridostigmine Bromide Tablets, USP, 30 mg are supplied with a Patient Information Sheet.
Personnel should be instructed to read the Patient Information Sheet before using Pyridostigmine Bromide Tablets, USP, 30 mg.
The following information and advice should be discussed with personnel when Pyridostigmine Bromide is issued.
17.1 Indication and Conditions of Use
- Pyridostigmine bromide is approved as a pretreatment for protection against the chemical nerve agent soman (GD). PB has not been approved for use against other chemical nerve agents including Sarin (GB), Tabun (GA), and VX. [See Indications and Usage (1).]
The approval is based on safety studies in humans and effectiveness studies conducted in animals. The FDA has approved pyridostigmine bromide based only on animal studies of effectiveness because it is not ethical to do these studies in humans. Human studies would require exposing people to the deadly effects of nerve agents, risking poisoning them or even killing them. Studies in monkeys and guinea pigs show that pretreatment with pyridostigmine bromide makes the antidotes (atropine and 2-PAM) work better against soman (GD). [See Nonclinical Toxicology (13.2).] - The main protection against chemical weapons is the chemical protective mask and battle dress overgarments. [See boxed WARNINGS and Dosage and Administration (2).]
- Pyridostigmine bromide is used as a pretreatment against a soman nerve agent attack. Based on the animal studies, it is thought that any potential benefits from use of pyridostigmine bromide occur only if:
- (1) It is taken within 8 hours before, but not right before, exposure to the nerve agent soman. If it is taken right before (when the nerve gas attack alarm is given) or during nerve agent exposure, it may not work and may make the effects of soman worse.
- (2) Atropine and 2-PAM are used when symptoms of nerve agent poisoning occur. The two antidotes are part of the ATNAA (Antidote Treatment – Nerve Agent Autoinjector). See Dosage and Administration (2).
17.2 Dosage and Administration
- The chain of command will tell personnel when it is time to take pyridostigmine bromide, based on the threat of exposure to soman nerve agents.
- One tablet must be taken every 8 hours until the chain of command tells personnel to stop taking pyridostigmine bromide.
- Pyridostigmine bromide tablets must not be taken more often. The dose must not be doubled if a dose has been missed.
- There is no known advantage to taking extra pyridostigmine bromide right before soman exposure.
- No further pyridostigmine bromide should be taken after nerve agent exposure has occurred, instead:
- Persons experiencing most or all of the MILD symptoms of nerve agent poisoning (runny nose; watery eyes; small, pinpoint pupils; eye pain; blurred vision; drooling and excessive sweating; cough; chest tightness; rapid breathing; diarrhea; increased urination; confusion; drowsiness; weakness; headache; nausea, vomiting, and/ or abdominal pain; slow or fast heart rate; and/or abnormally low or high blood pressure) should IMMEDIATELY AVOID INHALATION (hold their breath) AND PUT ON THEIR PROTECTIVE MASK. Then atropine and 2 PAM (one ATNAA) must be administered.
See Dosage and Administration (2).
Personnel should contact their unit medical officer if adverse reactions from pyridostigmine bromide continue and limit duty performance.
17.3 Contraindications and Precautions
Pyridostigmine bromide must not be taken by persons with any of the following:
- Mechanical bowel or bladder obstruction
- Hypersensitivity to anticholinesterase medicines (certain drugs used during surgery like physostigmine, edrophonium, neostigmine, and ambenonium)
See Contraindications (4).
Personnel should be instructed to inform their doctor or medic before taking pyridostigmine bromide if they:
- Are pregnant
- Have asthma
- Are allergic to bromide
- Take a beta blocker (a medicine to treat, eg, high blood pressure)
- Have high eye pressure (glaucoma)
- Have any other medical condition, including heart problems or reflux esophagitis (GERD)
17.4 Side Effects (Adverse Reactions)
The following adverse reactions are possible (this list of adverse reactions is not complete.):
- Stomach cramps
- Gas
- Diarrhea
- Nausea
- Frequent urination
- Increased salivation
- Sweating
- Headaches
- Dizziness
- Watery eyes
- Blurred vision
- Runny nose
- Difficulty or tightness in breathing
- Acid stomach (including heartburn or reflux)
- Tingling of fingers, toes, arms, and legs
- Muscle twitching or weakness
- Muscle cramps
Most side effects are mild and will disappear without treatment.
Pyridostigmine bromide has been safely used and has been FDA approved for over 40 years in the US to treat a disease called myasthenia gravis (MG). Human studies of pyridostigmine bromide at doses intended for military use have found pyridostigmine bromide to be generally safe.
Personnel should contact their unit medical officer if side effects from pyridostigmine bromide continue and limit duty performance.
17.5 Collection of Information
The Department of Defense (DoD) may collect information on the use of pyridostigmine bromide to help decide how best to protect deployed forces in the future. Information that identifies individual persons will remain confidential. However, the FDA may review any data collected by DoD for the purpose of evaluating pyridostigmine bromide.
17.6 Questions and Requests for Information
Questions about personnel rights and welfare should be directed to the unit medical officer, or e-mailed to usamrmcregulatoryaffairs@mail.mil.
Personnel can receive information about pyridostigmine bromide from unit medical officers or medics. Questions about pyridostigmine bromide can also be e-mailed directly to the US Army Medical Research and Materiel Command at address usarmy.detrick.medcom-usammda.mbx.usamrmc-regulatory-affairs@mail.mil.
- Pyridostigmine bromide is approved as a pretreatment for protection against the chemical nerve agent soman (GD). PB has not been approved for use against other chemical nerve agents including Sarin (GB), Tabun (GA), and VX. [See Indications and Usage (1).]
- SPL UNCLASSIFIED SECTION
-
PRINCIPAL DISPLAY PANEL - 21 Tablet Blister Pack
NDC: 72458-128-01
Rx Only
Quantity: 21 TabletsNSN 6505-01-178-7903
PYRIDOSTIGMINE BROMIDE TABLETS USP, 30 MG
[Soman Nerve Agent Pretreatment Pyridostgimine (SNAPP)]Date of issue_____/_____/_____Discard 3 months after issue.
Stop Taking Pyridostigmine Tablets:
- If You Are Exposed to Soman Nerve Agent
- If You Hear a Gas Attack Alarm
Manufactured by Bausch Health Companies Inc.,
Laval, Quebec H7L 4A8 for US Department of DefenseLOT: 0000000
EXP.: XXX 0000Dft_Fridge
(18-11-30)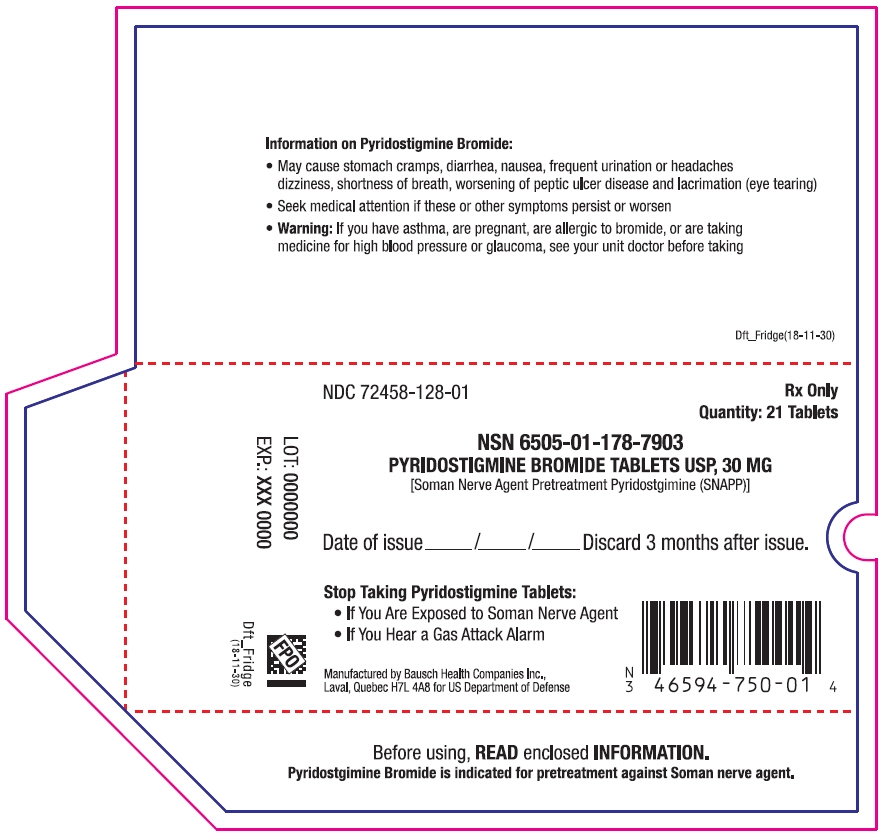
-
INGREDIENTS AND APPEARANCE
PYRIDOSTIGMINE BROMIDE
pyridostigmine bromide tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 72458-128 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Pyridostigmine Bromide (UNII: KVI301NA53) (Pyridostigmine - UNII:19QM69HH21) Pyridostigmine Bromide 30 mg Inactive Ingredients Ingredient Name Strength Anhydrous Lactose (UNII: 3SY5LH9PMK) Silicon Dioxide (UNII: ETJ7Z6XBU4) Stearic Acid (UNII: 4ELV7Z65AP) Product Characteristics Color WHITE Score no score Shape ROUND Size 8mm Flavor Imprint Code PBT Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 72458-128-02 10 in 1 BAG 12/05/1990 1 NDC: 72458-128-01 21 in 1 BLISTER PACK; Type 0: Not a Combination Product 2 NDC: 72458-128-04 10 in 1 BAG 07/14/2017 2 NDC: 72458-128-03 21 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020414 12/05/1990 Labeler - Surgeon General-Department of the Army (TSG-DA) (079859271)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.