Metolazone by Eon Labs, Inc. METOLAZONE tablet
Metolazone by
Drug Labeling and Warnings
Metolazone by is a Prescription medication manufactured, distributed, or labeled by Eon Labs, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
SPL UNCLASSIFIED SECTION
Rx only
DO NOT lNTERCHANGE:
DO NOT INTERCHANGE ZAROXOLYN® TABLETS AND OTHER FORMULATIONS OF METOLAZONE THAT SHARE ITS SLOW AND INCOMPLETE BIOAVAILABILITY AND ARE NOT THERAPEUTICALLY EQUIVALENT AT THE SAME DOSES TO MYKROX® TABLETS, A MORE RAPIDLY AVAILABLE AND COMPLETELY BIOAVAILABLE METOLAZONE PRODUCT. FORMULATIONS BIOEQUIVALENT TO ZAROXOLYN® AND FORMULATIONS BIOEQUIVALENT TO MYKROX® SHOULD NOT BE INTERCHANGED FOR ONE ANOTHER.
-
DESCRIPTION
Metolazone Tablets, USP for oral administration contain 2.5 mg, 5 mg or 10 mg of metolazone USP, a diuretic/saluretic/antihypertensive drug of the quinazoline class.
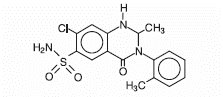
Metolazone has the molecular formula C16H16ClN3O3S, the chemical name 7-chloro-1,2,3,4-tetrahydro-2-methyl-4-oxo-3-o-tolyl-6-quinazolinesulfonamide, and a molecular weight of 365.84. The structural formula is:
Metolazone is only sparingly soluble in water, but more soluble in plasma, blood, alkali, and organic solvents.
Inactive Ingredients: colloidal silicon dioxide, magnesium stearate, microcrystalline cellulose and dye: 2.5 mg - D&C red No. 30 and FD&C blue No. 2; 5 mg - FD&C blue No. 2; 10 mg - D&C yellow No. 10 and FD&C yellow No. 6.
-
CLINICAL PHARMACOLOGY
Metolazone is a quinazoline diuretic, with properties generally similar to the thiazide diuretics. The actions of metolazone result from interference with the renal tubular mechanism of electrolyte reabsorption. Metolazone acts primarily to inhibit sodium reabsorption at the cortical diluting site and to a lesser extent in the proximal convoluted tubule. Sodium and chloride ions are excreted in approximately equivalent amounts. The increased delivery of sodium to the distal tubular exchange site results in increased potassium excretion. Metolazone does not inhibit carbonic anhydrase. A proximal action of metolazone has been shown in humans by increased excretion of phosphate and magnesium ions and by a markedly increased fractional excretion of sodium in patients with severely compromised glomerular filtration. This action has been demonstrated in animals by micropuncture studies.
When Metolazone Tablets are given, diuresis and saluresis usually begin within one hour and may persist for 24 hours or more. For most patients, the duration of effect can be varied by adjusting the daily dose. High doses may prolong the effect. A single daily dose is recommended. When a desired therapeutic effect has been obtained, it may be possible to reduce dosage to a lower maintenance level.
The diuretic potency of metolazone at maximum therapeutic dosage is approximately equal to thiazide diuretics. However, unlike thiazides, metolazone may produce diuresis in patients with glomerular filtration rates below 20 mL/min.
Metolazone and furosemide administered concurrently have produced marked diuresis in some patients where edema or ascites was refractory to treatment with maximum recommended doses of these or other diuretics administered alone. The mechanism of this interaction is unknown (see WARNINGSand PRECAUTIONS, Drug Interactions).
Maximum blood levels of metolazone are found approximately eight hours after dosing. A small fraction of metolazone is metabolized. Most of the drug is excreted in the unconverted form in the urine.
-
INDICATIONS AND USAGE
Metolazone is indicated for the treatment of salt and water retention including:
edema accompanying congestive heart failure;
edema accompanying renal diseases, including the nephrotic syndrome and states of diminished renal function.
Metolazone is also indicated for the treatment of hypertension, alone or in combination with other antihypertensive drugs of a different class. Mykrox® tablets, a more rapidly available form of metolazone, are intended for the treatment of new patients with mild to moderate hypertension. A dose titration is necessary if Mykrox® tablets are to be substituted for Zaroxolyn® tablets and other formulations of metolazone that share its slow and incomplete bioavailability, in the treatment of hypertension.
Usage In Pregnancy
The routine use of diuretics in an otherwise healthy woman is inappropriate and exposes mother and fetus to unnecessary hazard. Diuretics do not prevent development of toxemia of pregnancy, and there is no evidence that they are useful in the treatment of developed toxemia.
Edema during pregnancy may arise from pathologic causes or from the physiologic and mechanical consequence of pregnancy. Metolazone is indicated in pregnancy when edema is due to pathologic causes, just as it is in the absence of pregnancy (see PRECAUTIONS). Dependent edema in pregnancy resulting from restriction of venous return by the expanded uterus is properly treated through elevation of the lower extremities and use of support hose; use of diuretics to lower intravascular volume in this case is illogical and unnecessary. There is hypervolemia during normal pregnancy which is harmful to neither the fetus nor the mother (in the absence of cardiovascular disease), but which is associated with edema, including generalized edema, in the majority of pregnant women. If this edema produces discomfort, increased recumbency will often provide relief. In rare instances, this edema may cause extreme discomfort which is not relieved by rest. In these cases, a short course of diuretics may be appropriate.
- CONTRAINDICATIONS
-
WARNINGS
Rapid Onset Hyponatremia and/or Hypokalemia
Rarely, the rapid onset of severe hyponatremia and/or hypokalemia has been reported following initial doses of thiazide and non-thiazide diuretics. When symptoms consistent with severe electrolyte imbalance appear rapidly, drug should be discontinued and supportive measures should be initiated immediately. Parenteral electrolytes may be required. Appropriateness of therapy with this class of drugs should be carefully reevaluated.
Hypokalemia
Hypokalemia may occur with consequent weakness, cramps, and cardiac dysrhythmias. Serum potassium should be determined at regular and appropriate intervals, and dose reduction, potassium supplementation or addition of a potassium-sparing diuretic instituted whenever indicated. Hypokalemia is a particular hazard in patients who are digitalized or who have or have had a ventricular arrhythmia; dangerous or fatal arrhythmias may be precipitated. Hypokalemia is dose related.
Concomitant Therapy
Lithium
In general, diuretics should not be given concomitantly with lithium because they reduce its renal clearance and add a high risk of lithium toxicity. Read prescribing information for lithium preparations before use of such concomitant therapy.
Furosemide
Unusually large or prolonged losses of fluids and electrolytes may result when metolazone is administered concomitantly to patients receiving furosemide (see PRECAUTIONS, Drug Interactions).
-
PRECAUTIONS
DO NOT INTERCHANGE:
DO NOT INTERCHANGE ZAROXOLYN® TABLETS AND OTHER FORMULATIONS OF METOLAZONE THAT SHARE ITS SLOW AND INCOMPLETE BIOAVAILABILITY AND ARE NOT THERAPEUTICALLY EQUIVALENT AT THE SAME DOSES TO MYKROX® TABLETS, A MORE RAPIDLY AVAILABLE AND COMPLETELY BIOAVAILABLE METOLAZONE PRODUCT. FORMULATIONS BIOEQUIVALENT TO ZAROXOLYN® AND FORMULATIONS BIOEQUIVALENT TO MYKROX® SHOULD NOT BE INTERCHANGED FOR ONE ANOTHER.
General
Fluid and Electrolytes
All patients receiving therapy with metolazone tablets should have serum electrolyte measurements done at appropriate intervals and be observed for clinical signs of fluid and/or electrolyte imbalance: namely, hyponatremia, hypochloremic alkalosis and hypokalemia. In patients with severe edema accompanying cardiac failure or renal disease, a low-salt syndrome may be produced, especially with hot weather and a low-salt diet. Serum and urine electrolyte determinations are particularly important when the patient has protracted vomiting, severe diarrhea or is receiving parenteral fluids. Warning signs of imbalance are: dryness of mouth, thirst, weakness, lethargy, drowsiness, restlessness, muscle pains or cramps, muscle fatigue, hypotension, oliguria, tachycardia and gastrointestinal disturbances such as nausea and vomiting. Hyponatremia may occur at any time during long term therapy and, on rare occasions, may be life threatening.
The risk of hypokalemia is increased when larger doses are used, when diuresis is rapid, when severe liver disease is present, when corticosteroids are given concomitantly, when oral intake is inadequate or when excess potassium is being lost extrarenally, such as with vomiting or diarrhea.
Thiazide-like diuretics have been shown to increase the urinary excretion of magnesium; this may result in hypomagnesemia.
Glucose Tolerance
Metolazone may raise blood glucose concentrations possibly causing hyperglycemia and glycosuria in patients with diabetes or latent diabetes.
Hyperuricemia
Metolazone regularly causes an increase in serum uric acid and can occasionally precipitate gouty attacks even in patients without a prior history of them.
Azotemia
Azotemia, presumably prerenal azotemia, may be precipitated during the administration of metolazone. If azotemia and oliguria worsen during treatment of patients with severe renal disease, metolazone should be discontinued.
Renal Impairment
Use caution when administering metolazone tablets to patients with severely impaired renal function. As most of the drug is excreted by the renal route, accumulation may occur.
Orthostatic Hypotension
Orthostatic hypotension may occur; this may be potentiated by alcohol, barbiturates, narcotics, or concurrent therapy with other antihypertensive drugs.
Information for Patients
Patients should be informed of possible adverse effects, advised to take the medication as directed, and promptly report any possible adverse reactions to the treating physician.
Drug Interactions
Diuretics
Furosemide and probably other loop diuretics given concomitantly with metolazone can cause unusually large or prolonged losses of fluid and electrolytes (see WARNINGS).
Other Antihypertensives
When metolazone tablets are used with other antihypertensive drugs, care must be taken, especially during initial therapy. Dosage adjustments of other antihypertensives may be necessary.
Alcohol, Barbiturates and Narcotics
The hypotensive effects of these drugs may be potentiated by the volume contraction that may be associated with metolazone therapy.
Digitalis Glycosides
Diuretic-induced hypokalemia can increase the sensitivity of the myocardium to digitalis. Serious arrhythmias can result.
Curariform Drugs
Diuretic-induced hypokalemia may enhance neuromuscular blocking effects of curariform drugs (such as tubocurarine) - the most serious effect would be respiratory depression which could proceed to apnea. Accordingly, it may be advisable to discontinue metolazone three days before elective surgery.
Salicylates and Other Non-Steroidal Anti-Inflammatory Drugs
May decrease the antihypertensive effects of metolazone tablets.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Mice and rats administered metolazone 5 days/week for up to 18 and 24 months, respectively, at daily doses of 2 mg/kg, 10 mg/kg and 50 mg/kg, exhibited no evidence of a tumorigenic effect of the drug. The small number of animals examined histologically and poor survival in the mice limit the conclusions that can be reached from these studies.
Metolazone was not mutagenic in vitro in the Ames Test using Salmonella typhimurium strains TA-97, TA-98, TA-100, TA-102, and TA-1535.
Reproductive performance has been evaluated in mice and rats. There is no evidence that metolazone possesses the potential for altering reproductive capacity in mice. In a rat study, in which males were treated orally with metolazone at doses of 2 mg/kg, 10 mg/kg and 50 mg/kg for 127 days prior to mating with untreated females, an increased number of resorption sites was observed in dams mated with males from the 50 mg/kg group. In addition, the birth weight of offspring was decreased and the pregnancy rate was reduced in dams mated with males from the 10 mg/kg and 50 mg/kg groups.
Pregnancy
Teratogenic Effects
Pregnancy Category B.
Reproduction studies performed in mice, rabbits, and rats treated during the appropriate period of gestation at doses up to 50 mg/kg/day have revealed no evidence of harm to the fetus due to metolazone. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, metolazone tablets should be used during pregnancy only if clearly needed. Metolazone crosses the placental barrier and appears in cord blood.
Non-Teratogenic Effects
The use of metolazone tablets in pregnant women requires that the anticipated benefit be weighed against possible hazards to the fetus. These hazards include fetal or neonatal jaundice, thrombocytopenia and possibly other adverse reactions which have occurred in the adult. It is not known what effect the use of the drug during pregnancy has on the later growth, development and functional maturation of the child. No such effects have been reported with metolazone.
Labor and Delivery
Based on clinical studies in which women received metolazone in late pregnancy until the time of delivery, there is no evidence that the drug has any adverse effects on the normal course of labor or delivery.
Nursing Mothers
Metolazone appears in breast milk. Because of the potential for serious adverse reactions in nursing infants from metolazone, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established in controlled clinical trials. There is limited experience with the use of metolazone in pediatric patients with congestive heart failure, hypertension, bronchopulmonary dysplasia, nephrotic syndrome and nephrogenic diabetes insipidus. Doses used generally ranged from 0.05 mg/kg to 0.1 mg/kg administered once daily and usually resulted in a 1 kg to 2.8 kg weight loss and 150 cc to 300 cc increase in urine output. Not all patients responded and some gained weight. Those patients who did respond did so in the first few days of treatment. Prolonged use (beyond a few days) was generally associated with no further beneficial effect or a return to baseline status and is not recommended.
There is limited experience with the combination of metolazone and furosemide in pediatric patients with furosemide-resistant edema. Some benefited while others did not or had an exaggerated response with hypovolemia, tachycardia, and orthostatic hypotension requiring fluid replacement. Severe hypokalemia was reported and there was a tendency for diuresis to persist for up to 24 hours after metolazone was discontinued. Hyperbilirubinemia has been reported in 1 neonate. Close clinical and laboratory monitoring of all children treated with diuretics is indicated (see CONTRAINDICATIONS, WARNINGS, PRECAUTIONS).
Geriatric Use
Clinical studies of metolazone did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal or cardiac function and of concomitant disease or other drug therapy.
This drug is known to be substantially excreted by the kidney and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection and it may be useful to monitor renal function.
-
ADVERSE REACTIONS
Metolazone is usually well tolerated and most reported adverse reactions have been mild and transient. Many metolazone related adverse reactions represent extensions of its expected pharmacologic activity and can be attributed to either its antihypertensive action or its renal/metabolic actions. The following adverse reactions have been reported. Several are single or comparably rare occurrences. Adverse reactions are listed in decreasing order of severity within body systems.
Cardiovascular
Chest pain/discomfort, orthostatic hypotension, excessive volume depletion, hemoconcentration, venous thrombosis, palpitations.
Central and Peripheral Nervous System
Syncope, neuropathy, vertigo, paresthesias, psychotic depression, impotence, dizziness/lightheadedness, drowsiness, fatigue, weakness, restlessness (sometimes resulting in insomnia), headache.
Dermatologic/Hypersensitivity
Toxic epidermal necrolysis (TEN), Stevens-Johnson syndrome, necrotizing angiitis (cutaneous vasculitis), skin necrosis, purpura, petechiae, dermatitis (photosensitivity), urticaria, pruritus, skin rashes.
Gastrointestinal
Hepatitis, intrahepatic cholestatic jaundice, pancreatitis, vomiting, nausea, epigastric distress, diarrhea, constipation, anorexia, abdominal bloating, abdominal pain.
Metabolic
Hypokalemia, hyponatremia, hyperuricemia, hypochloremia, hypochloremic alkalosis, hyperglycemia, glycosuria, increase in serum urea nitrogen (BUN) or creatinine, hypophosphatemia, hypomagnesemia, hypercalcemia.
Other
Transient blurred vision, chills, dry mouth.
In addition, adverse reactions reported with similar antihypertensive-diuretics, but which have not been reported to date for metolazone include: bitter taste, sialadenitis, xanthopsia, respiratory distress (including pneumonitis) and anaphylactic reactions. These reactions should be considered as possible occurrences with clinical usage of metolazone.
Whenever adverse reactions are moderate or severe, metolazone dosage should be reduced or therapy withdrawn.
-
OVERDOSAGE
Intentional overdosage has been reported rarely with metolazone and similar diuretic drugs.
Signs and Symptoms
Orthostatic hypotension, dizziness, drowsiness, syncope, electrolyte abnormalities, hemoconcentration and hemodynamic changes due to plasma volume depletion may occur. In some instances depressed respiration may be observed. At high doses, lethargy of varying degree may progress to coma within a few hours. The mechanism of CNS depression with thiazide overdosage is unknown. Also, GI irritation and hypermotility may occur. Temporary elevation of BUN has been reported, especially in patients with impairment of renal function. Serum electrolyte changes and cardiovascular and renal function should be closely monitored.
Treatment
There is no specific antidote available but immediate evacuation of stomach contents is advised. Dialysis is not likely to be effective. Care should be taken when evacuating the gastric contents to prevent aspiration, especially in the stuporous or comatose patient. Supportive measures should be initiated as required to maintain hydration, electrolyte balance, respiration and cardiovascular and renal function.
-
DOSAGE AND ADMINISTRATION
Effective dosage of metolazone tablets should be individualized according to indication and patient response. A single daily dose is recommended. Therapy with metolazone tablets should be titrated to gain an initial therapeutic response and to determine the minimal dose possible to maintain the desired therapeutic response.
Usual Single Daily Dosage Schedules
Suitable initial dosages will usually fall in the ranges given.
Edema of cardiac failure:
Metolazone tablets, 5 mg to 20 mg once daily.
Edema of renal disease:
Metolazone tablets, 5 mg to 20 mg once daily.
Mild to moderate essential hypertension:
Metolazone tablets, 2.5 mg to 5 mg once daily.
New patients - If considered desirable to switch patients currently on Zaroxolyn® tablets and other formulations of metolazone that share its slow and incomplete bioavailability to Mykrox®, the dose should be determined by titration starting at one tablet (0.5 mg) once daily and increasing to two tablets (1 mg) once daily if needed.
Treatment of Edematous States
The time interval required for the initial dosage to produce an effect may vary. Diuresis and saluresis usually begin within one hour and persist for 24 hours or longer. When a desired therapeutic effect has been obtained, it may be advisable to reduce the dose if possible. The daily dose depends on the severity of the patient's condition, sodium intake, and responsiveness. A decision to change the daily dose should be based on the results of thorough clinical and laboratory evaluations. If antihypertensive drugs or diuretics are given concurrently with metolazone, more careful dosage adjustment may be necessary. For patients who tend to experience paroxysmal nocturnal dyspnea, it may be advisable to employ a larger dose to ensure prolongation of diuresis and saluresis for a full 24-hour period.
-
HOW SUPPLIED
Metolazone Tablets, USP for oral administration are available as:
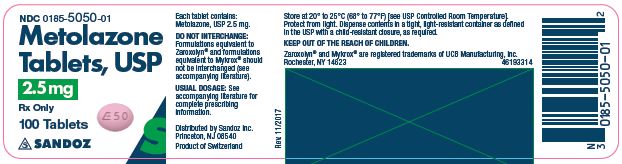
2.5 mg: Pink, shallow biconvex, modified oval tablets, debossed “E50” on one side, plain on the other side and supplied as:
NDC: 0185-5050-01 bottles of 100
NDC: 0185-5050-10 bottles of 1000
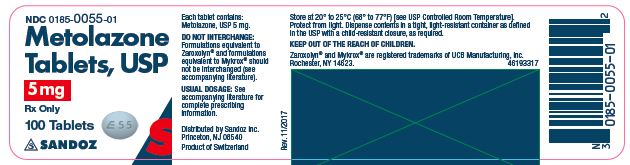
5 mg: Blue, shallow biconvex, modified oval tablets, debossed “E55” on one side, plain on the other side and supplied as:
NDC: 0185-0055-01 bottles of 100
NDC: 0185-0055-10 bottles of 1000
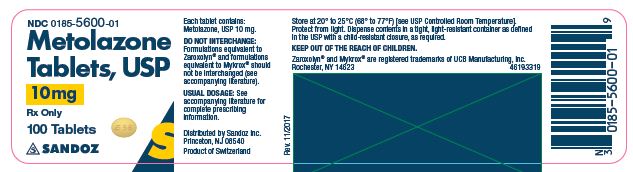
10 mg: Yellow, shallow biconvex, modified oval tablets, debossed “E56” on one side, plain on the other side and supplied as:
NDC: 0185-5600-01 bottles of 100
NDC: 0185-5600-10 bottles of 1000
Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature].
Protect from light.
Dispense contents in a tight, light-resistant container as defined in the USP with a child-resistant closure, as required.
Keep out of the reach of children.
Zaroxolyn® and Mykrox® are registered trademarks of UCB Manufacturing, Inc., Rochester, NY 14623.
To report SUSPECTED ADVERSE REACTIONS, contact Sandoz Inc. at 1-800-525-8747 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Sandoz Inc.
Princeton, NJ 08540
Rev. 06/17
MF0050REV06/17
- 2.5 mg Label
- 5 mg Label
- 10 mg Label
-
INGREDIENTS AND APPEARANCE
METOLAZONE
metolazone tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0185-5050 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength METOLAZONE (UNII: TZ7V40X7VX) (METOLAZONE - UNII:TZ7V40X7VX) METOLAZONE 2.5 mg Inactive Ingredients Ingredient Name Strength MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) D&C RED NO. 30 (UNII: 2S42T2808B) FD&C BLUE NO. 2 (UNII: L06K8R7DQK) MAGNESIUM STEARATE (UNII: 70097M6I30) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) Product Characteristics Color PINK Score no score Shape OVAL Size 6mm Flavor Imprint Code E50 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0185-5050-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 12/19/2003 2 NDC: 0185-5050-10 1000 in 1 BOTTLE; Type 0: Not a Combination Product 12/19/2003 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA076732 12/19/2003 METOLAZONE
metolazone tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0185-0055 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength METOLAZONE (UNII: TZ7V40X7VX) (METOLAZONE - UNII:TZ7V40X7VX) METOLAZONE 5 mg Inactive Ingredients Ingredient Name Strength MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) FD&C BLUE NO. 2 (UNII: L06K8R7DQK) MAGNESIUM STEARATE (UNII: 70097M6I30) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) Product Characteristics Color BLUE Score no score Shape OVAL Size 6mm Flavor Imprint Code E55 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0185-0055-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 12/19/2003 2 NDC: 0185-0055-10 1000 in 1 BOTTLE; Type 0: Not a Combination Product 12/19/2003 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA076466 12/19/2003 METOLAZONE
metolazone tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0185-5600 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength METOLAZONE (UNII: TZ7V40X7VX) (METOLAZONE - UNII:TZ7V40X7VX) METOLAZONE 10 mg Inactive Ingredients Ingredient Name Strength MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) D&C YELLOW NO. 10 (UNII: 35SW5USQ3G) FD&C YELLOW NO. 6 (UNII: H77VEI93A8) MAGNESIUM STEARATE (UNII: 70097M6I30) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) Product Characteristics Color YELLOW Score no score Shape OVAL Size 6mm Flavor Imprint Code E56 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0185-5600-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 12/19/2003 2 NDC: 0185-5600-10 1000 in 1 BOTTLE; Type 0: Not a Combination Product 12/19/2003 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA076466 12/19/2003 Labeler - Eon Labs, Inc. (012656273)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.