SPIRONOLACTONE AND HYDROCHLOROTHIAZIDE tablet
Spironolactone and Hydrochlorothiazide by
Drug Labeling and Warnings
Spironolactone and Hydrochlorothiazide by is a Prescription medication manufactured, distributed, or labeled by Mylan Pharmaceuticals Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
DESCRIPTION
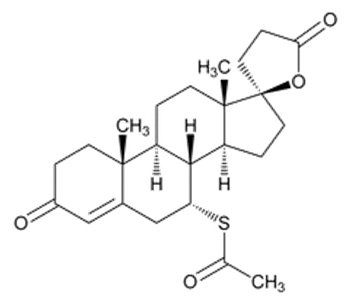
Each tablet of spironolactone and hydrochlorothiazide contains 25 mg of spironolactone, USP and 25 mg of hydrochlorothiazide, USP. Spironolactone, an aldosterone antagonist, is 17-Hydroxy-7α-mercapto-3-oxo-17α-pregn-4-ene-21-carboxylic acid, γ-lactone acetate and has the following structural formula, molecular formula and molecular weight:
C24H32O4S
M.W. = 416.57Spironolactone is practically insoluble in water, soluble in alcohol, and freely soluble in benzene and in chloroform.
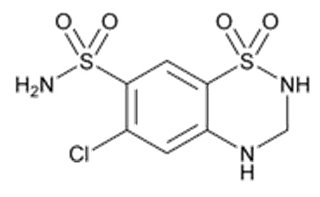
Hydrochlorothiazide, a diuretic and antihypertensive, is 6-Chloro-3,4-dihydro-2H-1,2,4-benzothiadiazine-7-sulfonamide 1,1-dioxide and has the following structural formula, molecular formula and molecular weight:
C7H8ClN3O4S2
M.W. = 297.74Hydrochlorothiazide is slightly soluble in water and freely soluble in sodium hydroxide solution.
Each tablet for oral administration contains 25 mg of spironolactone and 25 mg of hydrochlorothiazide and the following inactive ingredients: colloidal silicon dioxide, corn starch, D&C Yellow No. 10 Aluminum Lake, FD&C Yellow No. 6 Aluminum Lake, lactose monohydrate, magnesium stearate, L-menthol, microcrystalline cellulose, peppermint oil, sodium lauryl sulfate and sodium starch glycolate (potato).
-
ACTIONS/CLINICAL PHARMACOLOGY
Mechanism of Action
Spironolactone and hydrochlorothiazide tablets are a combination of two diuretic agents with different but complementary mechanisms and sites of action, thereby providing additive diuretic and antihypertensive effects. Additionally, the spironolactone component helps to minimize the potassium loss characteristically induced by the thiazide component.
The diuretic effect of spironolactone is mediated through its action as a specific pharmacologic antagonist of aldosterone, primarily by competitive binding of receptors at the aldosterone-dependent sodium-potassium exchange site in the distal convoluted renal tubule. Hydrochlorothiazide promotes the excretion of sodium and water primarily by inhibiting their reabsorption in the cortical diluting segment of the distal renal tubule.
Spironolactone and hydrochlorothiazide tablets are effective in significantly lowering the systolic and diastolic blood pressure in many patients with essential hypertension, even when aldosterone secretion is within normal limits.
Both spironolactone and hydrochlorothiazide reduce exchangeable sodium, plasma volume, body weight, and blood pressure. The diuretic and antihypertensive effects of the individual components are potentiated when spironolactone and hydrochlorothiazide are given concurrently.
Pharmacokinetics
Spironolactone is rapidly and extensively metabolized. Sulfur-containing products are the predominant metabolites and are thought to be primarily responsible, together with spironolactone, for the therapeutic effects of the drug. The following pharmacokinetic data were obtained from 12 healthy volunteers following the administration of 100 mg of spironolactone (as tablets) daily for 15 days. On the 15th day, spironolactone was given immediately after a low fat breakfast and blood was drawn thereafter.
Accumulation Factor:
AUC (0-24 hr, day 15)/
AUC (0-24 hr, day 1)Mean Peak Serum Concentration Mean (SD) Post-Steady State Half-Life 7-α-(thiomethyl) spironolactone (TMS)
1.25
391 ng/mL at 3.2 hr
13.8 hr (6.4) (terminal)
6-β-hydroxy-7-α-(thiomethyl) spironolactone (HTMS)
1.50
125 ng/mL at 5.1 hr
15.0 hr (4.0) (terminal)
Canrenone (C)
1.41
181 ng/mL at 4.3 hr
16.5 hr (6.3) (terminal)
Spironolactone
1.30
80 ng/mL at 2.6 hr
Approximately 1.4 hr (0.5) (β half-life)
The pharmacological activity of spironolactone metabolites in man is not known. However, in the adrenalectomized rat the antimineralocorticoid activities of the metabolites C, TMS, and HTMS, relative to spironolactone, were 1.10, 1.28, and 0.32, respectively. Relative to spironolactone, their binding affinities to the aldosterone receptors in rat kidney slices were 0.19, 0.86, and 0.06, respectively.
In humans, the potencies of TMS and 7-α-thiospirolactone in reversing the effects of the synthetic mineralocorticoid, fludrocortisone, on urinary electrolyte composition were 0.33 and 0.26, respectively, relative to spironolactone. However, since the serum concentrations of these steroids were not determined, their incomplete absorption and/or first-pass metabolism could not be ruled out as a reason for their reduced in vivo activities.
Spironolactone and its metabolites are more than 90% bound to plasma proteins. The metabolites are excreted primarily in the urine and secondarily in bile.
The effect of food on spironolactone absorption (two 100 mg spironolactone tablets) was assessed in a single dose study of 9 healthy, drug-free volunteers. Food increased the bioavailability of unmetabolized spironolactone by almost 100%. The clinical importance of this finding is not known.
Hydrochlorothiazide is rapidly absorbed following oral administration. Onset of action of hydrochlorothiazide is observed within one hour and persists for 6 to 12 hours. Hydrochlorothiazide plasma concentrations attain peak levels at 1 to 2 hours and decline with a half-life of 4 to 5 hours. Hydrochlorothiazide undergoes only slight metabolic alteration and is excreted in urine. It is distributed throughout the extracellular space, with essentially no tissue accumulation except in the kidney.
-
INDICATIONS AND USAGE
Spironolactone, an ingredient of spironolactone and hydrochlorothiazide tablets, has been shown to be a tumorigen in chronic toxicity studies in rats (see PRECAUTIONS section). Spironolactone and hydrochlorothiazide tablets should be used only in those conditions described below. Unnecessary use of this drug should be avoided.
Spironolactone and hydrochlorothiazide tablets are indicated for:
Edematous conditions for patients with:
Congestive heart failure:
- For the management of edema and sodium retention when the patient is only partially responsive to, or is intolerant of, other therapeutic measures;
- The treatment of diuretic-induced hypokalemia in patients with congestive heart failure when other measures are considered inappropriate;
- The treatment of patients with congestive heart failure taking digitalis when other therapies are considered inadequate or inappropriate.
Cirrhosis of the liver accompanied by edema and/or ascites:
- Aldosterone levels may be exceptionally high in this condition. Spironolactone and hydrochlorothiazide tablets are indicated for maintenance therapy together with bed rest and the restriction of fluid and sodium.
The nephrotic syndrome:
- For nephrotic patients when treatment of the underlying disease, restriction of fluid and sodium intake, and the use of other diuretics do not provide an adequate response.
Essential hypertension:
- For patients with essential hypertension in whom other measures are considered inadequate or inappropriate;
- In hypertensive patients for the treatment of a diuretic-induced hypokalemia when other measures are considered inappropriate;
- Spironolactone and hydrochlorothiazide tablets are indicated for the treatment of hypertension, to lower blood pressure. Lowering blood pressure reduces the risk of fatal and nonfatal cardiovascular events, primarily strokes and myocardial infarctions. These benefits have been seen in controlled trials of antihypertensive drugs from a wide variety of pharmacologic classes, including the classes to which this drug principally belongs. There are no controlled trials demonstrating risk reduction with spironolactone and hydrochlorothiazide tablets.
Control of high blood pressure should be part of comprehensive cardiovascular risk management, including, as appropriate, lipid control, diabetes management, antithrombotic therapy, smoking cessation, exercise, and limited sodium intake. Many patients will require more than one drug to achieve blood pressure goals. For specific advice on goals and management, see published guidelines, such as those of the National High Blood Pressure Education Program’s Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC).
Numerous antihypertensive drugs, from a variety of pharmacologic classes and with different mechanisms of action, have been shown in randomized controlled trials to reduce cardiovascular morbidity and mortality, and it can be concluded that it is blood pressure reduction, and not some other pharmacologic property of the drugs, that is largely responsible for those benefits. The largest and most consistent cardiovascular outcome benefit has been a reduction in the risk of stroke, but reductions in myocardial infarction and cardiovascular mortality also have been seen regularly.
Elevated systolic or diastolic pressure causes increased cardiovascular risk, and the absolute risk increase per mmHg is greater at higher blood pressures, so that even modest reductions of severe hypertension can provide substantial benefit. Relative risk reduction from blood pressure reduction is similar across populations with varying absolute risk, so the absolute benefit is greater in patients who are at higher risk independent of their hypertension (for example, patients with diabetes or hyperlipidemia), and such patients would be expected to benefit from more aggressive treatment to a lower blood pressure goal.
Some antihypertensive drugs have smaller blood pressure effects (as monotherapy) in black patients, and many antihypertensive drugs have additional approved indications and effects (e.g., on angina, heart failure, or diabetic kidney disease). These considerations may guide selection of therapy.
Usage in Pregnancy
The routine use of diuretics in an otherwise healthy woman is inappropriate and exposes mother and fetus to unnecessary hazard. Diuretics do not prevent development of toxemia of pregnancy, and there is no satisfactory evidence that they are useful in the treatment of developing toxemia.
Edema during pregnancy may arise from pathologic causes or from the physiologic and mechanical consequences of pregnancy. Spironolactone and hydrochlorothiazide tablets are indicated in pregnancy when edema is due to pathologic causes just as it is in the absence of pregnancy (however, see PRECAUTIONS: Pregnancy). Dependent edema in pregnancy, resulting from restriction of venous return by the expanded uterus, is properly treated through elevation of the lower extremities and use of support hose; use of diuretics to lower intravascular volume in this case is unsupported and unnecessary. There is hypervolemia during normal pregnancy which is not harmful to either the fetus or the mother (in the absence of cardiovascular disease), but which is associated with edema, including generalized edema, in the majority of pregnant women. If this edema produces discomfort, increased recumbency will often provide relief. In rare instances, this edema may cause extreme discomfort that is not relieved by rest. In these cases, a short course of diuretics may provide relief and may be appropriate.
-
CONTRAINDICATIONS
Spironolactone and hydrochlorothiazide tablets are contraindicated in patients with anuria, acute renal insufficiency, significant impairment of renal excretory function, hypercalcemia, hyperkalemia, Addison’s disease, and in patients who are allergic to thiazide diuretics or to other sulfonamide-derived drugs. Spironolactone and hydrochlorothiazide may also be contraindicated in acute or severe hepatic failure.
-
WARNINGS
Potassium supplementation, either in the form of medication or as a diet rich in potassium, should not ordinarily be given in association with spironolactone and hydrochlorothiazide therapy. Excessive potassium intake may cause hyperkalemia in patients receiving spironolactone and hydrochlorothiazide (see PRECAUTIONS: General).
Concomitant administration of spironolactone and hydrochlorothiazide with the following drugs or potassium sources may lead to severe hyperkalemia:
- other potassium-sparing diuretics
- ACE inhibitors
- angiotensin II receptor antagonists
- aldosterone blockers
- non-steroidal anti-inflammatory drugs (NSAIDs), e.g., indomethacin
- heparin and low molecular weight heparin
- other drugs or conditions known to cause hyperkalemia
- potassium supplements
- diet rich in potassium
- salt substitutes containing potassium
Spironolactone and hydrochlorothiazide should not be administered concurrently with other potassium-sparing diuretics. Spironolactone, when used with ACE inhibitors or indomethacin, even in the presence of a diuretic, has been associated with severe hyperkalemia. Extreme caution should be exercised when spironolactone and hydrochlorothiazide tablets are given concomitantly with these drugs (see PRECAUTIONS: Drug Interactions).
Spironolactone and hydrochlorothiazide should be used with caution in patients with impaired hepatic function because minor alterations of fluid and electrolyte balance may precipitate hepatic coma.
Lithium generally should not be given with diuretics (see PRECAUTIONS: Drug Interactions).
Thiazides should be used with caution in severe renal disease. In patients with renal disease, thiazides may precipitate azotemia. Cumulative effects of the drug may develop in patients with impaired renal function.
Thiazides may add to or potentiate the action of other antihypertensive drugs.
Sensitivity reactions to thiazides may occur in patients with or without a history of allergy or bronchial asthma.
Sulfonamide derivatives, including thiazides, have been reported to exacerbate or activate systemic lupus erythematosus.
Acute Myopia and Secondary Angle-Closure Glaucoma
Hydrochlorothiazide, a sulfonamide, can cause an idiosyncratic reaction, resulting in acute transient myopia and acute angle-closure glaucoma. Symptoms include acute onset of decreased visual acuity or ocular pain and typically occur within hours to weeks of drug initiation. Untreated acute angle-closure glaucoma can lead to permanent vision loss. The primary treatment is to discontinue hydrochlorothiazide as rapidly as possible. Prompt medical or surgical treatments may need to be considered if the intraocular pressure remains uncontrolled. Risk factors for developing acute angle-closure glaucoma may include a history of sulfonamide or penicillin allergy.
-
PRECAUTIONS
General
Serum Electrolyte Abnormalities
Spironolactone can cause hyperkalemia. The risk of hyperkalemia may be increased in patients with renal insufficiency, diabetes mellitus or with concomitant use of drugs that raise serum potassium (see Drug Interactions). Hydrochlorothiazide can cause hypokalemia and hyponatremia. The risk of hypokalemia may be increased in patients with cirrhosis, brisk diuresis, or with concomitant use of drugs that lower serum potassium. Hypomagnesemia can result in hypokalemia which appears difficult to treat despite potassium repletion. Monitor serum electrolytes periodically.
Other Metabolic Disturbances
Hydrochlorothiazide may alter glucose tolerance and raise serum levels of cholesterol and triglycerides.
Hydrochlorothiazide may raise the serum uric acid level due to reduced clearance of uric acid and may cause or exacerbate hyperuricemia and precipitate gout in susceptible patients.
Hydrochlorothiazide decreases urinary calcium excretion and may cause elevations of serum calcium. Monitor calcium levels in patients with hypercalcemia receiving spironolactone and hydrochlorothiazide.
Gynecomastia
Gynecomastia may develop in association with the use of spironolactone; physicians should be alert to its possible onset. The development of gynecomastia appears to be related to both dosage level and duration of therapy and is normally reversible when spironolactone and hydrochlorothiazide tablets are discontinued. In rare instances, some breast enlargement may persist when spironolactone and hydrochlorothiazide tablets are discontinued.
Information for Patients
Patients who receive spironolactone and hydrochlorothiazide should be advised to avoid potassium supplements and foods containing high levels of potassium including salt substitutes.
Laboratory Tests
Periodic determination of serum electrolytes to detect possible electrolyte imbalance should be done at appropriate intervals, particularly in the elderly and those with significant renal or hepatic impairments.
Drug Interactions
ACE Inhibitors, Angiotensin II Receptor Antagonists, Aldosterone Blockers, Potassium Supplements, Heparin, Low Molecular Weight Heparin, and Other Drugs Known to Cause Hyperkalemia
Concomitant administration may lead to severe hyperkalemia.
Antidiabetic Drugs (e.g., oral agents, insulin)
Dosage adjustment of the antidiabetic drug may be required (see PRECAUTIONS).
Pressor Amines (e.g., norepinephrine)
Both spironolactone and hydrochlorothiazide reduce the vascular responsiveness to norepinephrine. Therefore, caution should be exercised in the management of patients subjected to regional or general anesthesia while they are being treated with spironolactone and hydrochlorothiazide.
Skeletal Muscle Relaxants, Nondepolarizing (e.g., tubocurarine)
Possible increased responsiveness to the muscle relaxant may result.
Lithium
Lithium generally should not be given with diuretics. Diuretic agents reduce the renal clearance of lithium and add a high risk of lithium toxicity.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
In some patients, the administration of an NSAID can reduce the diuretic, natriuretic, and antihypertensive effects of loop, potassium-sparing, and thiazide diuretics. Combination of NSAIDs, e.g., indomethacin, with potassium-sparing diuretics has been associated with severe hyperkalemia. Therefore, when spironolactone and hydrochlorothiazide tablets and NSAIDs are used concomitantly, the patient should be observed closely to determine if the desired effect of the diuretic is obtained.
Acetylsalicylic Acid
Acetylsalicylic acid may reduce the efficacy of spironolactone. Therefore, when spironolactone and hydrochlorothiazide tablets and acetylsalicylic acid are used concomitantly, spironolactone and hydrochlorothiazide tablets may need to be titrated to higher maintenance dose and the patient should be observed closely to determine if the desired effect is obtained.
Digoxin
Spironolactone has been shown to increase the half-life of digoxin. This may result in increased serum digoxin levels and subsequent digitalis toxicity. Monitor serum digoxin levels and adjust dose accordingly. Thiazide-induced electrolyte disturbances, i.e. hypokalemia, hypomagnesemia, increase the risk of digoxin toxicity, which may lead to fatal arrhythmic events (see PRECAUTIONS).
Drug/Laboratory Test Interactions
Thiazides should be discontinued before carrying out tests for parathyroid function (see PRECAUTIONS: General). Thiazides may also decrease serum PBI levels without evidence of alteration of thyroid function.
Several reports of possible interference with digoxin radioimmunoassays by spironolactone or its metabolites have appeared in the literature. Neither the extent nor the potential clinical significance of its interference (which may be assay specific) has been fully established.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Spironolactone
Orally administered spironolactone has been shown to be a tumorigen in dietary administration studies performed in rats, with its proliferative effects manifested on endocrine organs and the liver. In an 18-month study using doses of about 50, 150, and 500 mg/kg/day, there were statistically significant increases in benign adenomas of the thyroid and testes and, in male rats, a dose-related increase in proliferative changes in the liver (including hepatocytomegaly and hyperplastic nodules). In a 24-month study in which the same strain of rat was administered doses of about 10, 30 and 100 mg spironolactone/kg/day, the range of proliferative effects included significant increases in hepatocellular adenomas and testicular interstitial cell tumors in males, and significant increases in thyroid follicular cell adenomas and carcinomas in both sexes. There was also a statistically significant, but not dose-related, increase in benign uterine endometrial stromal polyps in females.
A dose-related (above 30 mg/kg/day) incidence of myelocytic leukemia was observed in rats fed daily doses of potassium canrenoate (a compound chemically similar to spironolactone and whose primary metabolite, canrenone, is also a major product of spironolactone in man) for a period of one year. In two year studies in the rat, oral administration of potassium canrenoate was associated with myelocytic leukemia and hepatic, thyroid, testicular, and mammary tumors.
Neither spironolactone nor potassium canrenoate produced mutagenic effects in tests using bacteria or yeast. In the absence of metabolic activation, neither spironolactone nor potassium canrenoate has been shown to be mutagenic in mammalian tests in vitro. In the presence of metabolic activation, spironolactone has been reported to be negative in some mammalian mutagenicity tests in vitro and inconclusive (but slightly positive) for mutagenicity in other mammalian tests in vitro. In the presence of metabolic activation, potassium canrenoate has been reported to test positive for mutagenicity in some mammalian tests in vitro, inconclusive in others, and negative in still others.
In a three-litter reproduction study in which female rats received dietary doses of 15 and 500 mg spironolactone/kg/day, there were no effects on mating and fertility, but there was a small increase in incidence of stillborn pups at 500 mg/kg/day. When injected into female rats (100 mg/kg/day for 7 days, i.p.), spironolactone was found to increase the length of the estrous cycle by prolonging diestrus during treatment and inducing constant diestrus during a two week posttreatment observation period. These effects were associated with retarded ovarian follicle development and a reduction in circulating estrogen levels, which would be expected to impair mating, fertility, and fecundity. Spironolactone (100 mg/kg/day), administered i.p. to female mice during a two week cohabitation period with untreated males, decreased the number of mated mice that conceived (effect shown to be caused by an inhibition of ovulation) and decreased the number of implanted embryos in those that became pregnant (effect shown to be caused by an inhibition of implantation), and at 200 mg/kg, also increased the latency period to mating.
Hydrochlorothiazide
Two year feeding studies in mice and rats conducted under the auspices of the National Toxicology Program (NTP) uncovered no evidence of a carcinogenic potential of hydrochlorothiazide in female mice (at doses of up to approximately 600 mg/kg/day) or in male and female rats (at doses of up to approximately 100 mg/kg/day). The NTP, however, found equivocal evidence for hepatocarcinogenicity in male mice.
Hydrochlorothiazide was not genotoxic in in vitro assays using strains TA 98, TA 100, TA 1535, TA 1537, and TA 1538 of Salmonella typhimurium (Ames assay) and in the Chinese Hamster Ovary (CHO) test for chromosomal aberrations, or in in vivo assays using mouse germinal cell chromosomes, Chinese hamster bone marrow chromosomes, and the Drosophila sex-linked recessive lethal trait gene. Positive test results were obtained only in the in vitro CHO Sister Chromatid Exchange (clastogenicity) and in the Mouse Lymphoma Cell (mutagenicity) assays, using concentrations of hydrochlorothiazide from 43 to 1300 mcg/mL, and in the Aspergillus nidulans non-disjunction assay at an unspecified concentration.
Hydrochlorothiazide had no adverse effects on the fertility of mice and rats of either sex in studies wherein these species were exposed, via their diet, to doses of up to 100 and 4 mg/kg, respectively, prior to mating and throughout gestation.
Pregnancy
Teratogenic Effects
Hydrochlorothiazide
Studies in which hydrochlorothiazide was orally administered to pregnant mice and rats during their respective periods of major organogenesis at doses up to 3000 and 1000 mg hydrochlorothiazide/kg, respectively, provided no evidence of harm to the fetus. There are, however, no adequate and well-controlled studies in pregnant women.
Spironolactone
Teratology studies with spironolactone have been carried out in mice and rabbits at doses of up to 20 mg/kg/day. On a body surface area basis, this dose in the mouse is substantially below the maximum recommended human dose and, in the rabbit, approximates the maximum recommended human dose. No teratogenic or other embryotoxic effects were observed in mice, but the 20 mg/kg dose caused an increased rate of resorption and a lower number of live fetuses in rabbits. Because of its antiandrogenic activity and the requirement of testosterone for male morphogenesis, spironolactone may have the potential for adversely affecting sex differentiation of the male during embryogenesis. When administered to rats at 200 mg/kg/day between gestation days 13 and 21 (late embryogenesis and fetal development), feminization of male fetuses was observed. Offspring exposed during late pregnancy to 50 and 100 mg/kg/day doses of spironolactone exhibited changes in the reproductive tract including dose-dependent decreases in weights of the ventral prostate and seminal vesicle in males, ovaries and uteri that were enlarged in females, and other indications of endocrine dysfunction, that persisted into adulthood. There are no adequate and well-controlled studies with spironolactone and hydrochlorothiazide in pregnant women. Spironolactone has known endocrine effects in animals including progestational and antiandrogenic effects. The antiandrogenic effects can result in apparent estrogenic side effects in humans, such as gynecomastia. Therefore, the use of spironolactone and hydrochlorothiazide in pregnant women requires that the anticipated benefit be weighed against the possible hazards to the fetus.
Non-Teratogenic Effects
Spironolactone or its metabolites may, and hydrochlorothiazide does, cross the placental barrier and appear in cord blood. Therefore, the use of spironolactone and hydrochlorothiazide in pregnant women requires that the anticipated benefit be weighed against possible hazards to the fetus. The hazards include fetal or neonatal jaundice, thrombocytopenia, and possibly other adverse reactions that have occurred in adults.
Nursing Mothers
Canrenone, a major (and active) metabolite of spironolactone, appears in human breast milk. Because spironolactone has been found to be tumorigenic in rats, a decision should be made whether to discontinue the drug, taking into account the importance of the drug to the mother. If use of the drug is deemed essential, an alternative method of infant feeding should be instituted.
Thiazides are excreted in human milk in small amounts. Thiazides when given at high doses can cause intense diuresis which can in turn inhibit milk production. The use of spironolactone and hydrochlorothiazide during breast feeding is not recommended. If spironolactone and hydrochlorothiazide tablets are used during breast feeding, doses should be kept as low as possible.
-
ADVERSE REACTIONS
The following adverse reactions have been reported and, within each category (body system), are listed in order of decreasing severity.
Hydrochlorothiazide
Body as a whole: Weakness.
Cardiovascular: Hypotension including orthostatic hypotension (may be aggravated by alcohol, barbiturates, narcotics, or antihypertensive drugs).
Digestive: Pancreatitis, jaundice (intrahepatic cholestatic jaundice), diarrhea, vomiting, sialoadenitis, cramping, constipation, gastric irritation, nausea, anorexia.
Eye Disorders: acute myopia and acute angle-closure glaucoma (see WARNINGS).
Hematologic: Aplastic anemia, agranulocytosis, leukopenia, hemolytic anemia, thrombocytopenia.
Hypersensitivity: Anaphylactic reactions, necrotizing angitis (vasculitis and cutaneous vasculitis), respiratory distress including pneumonitis and pulmonary edema, photosensitivity, fever, urticaria, rash, purpura.
Metabolic: Electrolyte imbalance (see PRECAUTIONS), hyperglycemia, glycosuria, hyperuricemia.
Musculoskeletal: Muscle spasm.
Nervous System/Psychiatric: Vertigo, paresthesias, dizziness, headache, restlessness.
Renal: Renal failure, renal dysfunction, interstitial nephritis (see WARNINGS).
Skin: Erythema multiforme, pruritus.
Special Senses: Transient blurred vision, xanthopsia.
Spironolactone
Digestive: Gastric bleeding, ulceration, gastritis, diarrhea and cramping, nausea, vomiting.
Reproductive: Gynecomastia (see PRECAUTIONS), inability to achieve or maintain erection, irregular menses or amenorrhea, postmenopausal bleeding, breast pain. Carcinoma of the breast has been reported in patients taking spironolactone but a cause and effect relationship has not been established.
Hematologic: Leukopenia (including agranulocytosis), thrombocytopenia.
Hypersensitivity: Fever, urticaria, maculopapular or erythematous cutaneous eruptions, anaphylactic reactions, vasculitis.
Metabolism:Hyperkalemia, electrolyte disturbances (see WARNINGS and PRECAUTIONS).
Musculoskeletal:Leg cramps.
Nervous System/Psychiatric: Lethargy, mental confusion, ataxia, dizziness, headache, drowsiness.
Liver/Biliary: A very few cases of mixed cholestatic/hepatocellular toxicity, with one reported fatality, have been reported with spironolactone administration.
Renal: Renal dysfunction (including renal failure).
Skin: Stevens-Johnson Syndrome (SJS), toxic epidermal necrolysis (TEN), drug rash with eosinophilia and systemic symptoms (DRESS), alopecia, pruritus.
-
OVERDOSAGE
The oral LD50 of spironolactone is greater than 1000 mg/kg in mice, rats, and rabbits. The oral LD50 of hydrochlorothiazide is greater than 10 g/kg in both mice and rats.
Acute overdosage of spironolactone may be manifested by drowsiness, mental confusion, maculopapular or erythematous rash, nausea, vomiting, dizziness, or diarrhea. Rarely, instances of hyponatremia, hyperkalemia (less commonly seen with spironolactone and hydrochlorothiazide because the hydrochlorothiazide component tends to produce hypokalemia), or hepatic coma may occur in patients with severe liver disease, but these are unlikely due to acute overdosage.
However, because spironolactone and hydrochlorothiazide tablets contain both spironolactone and hydrochlorothiazide, the toxic effects may be intensified, and signs of thiazide overdosage may be present. These include electrolyte imbalance such as hypokalemia and/or hyponatremia. The potassium-sparing action of spironolactone may predominate and hyperkalemia may occur, especially in patients with impaired renal function. BUN determinations have been reported to rise transiently with hydrochlorothiazide. There may be CNS depression with lethargy or even coma.
Treatment
Induce vomiting or evacuate the stomach by lavage. There is no specific antidote. Treatment is supportive to maintain hydration, electrolyte balance, and vital functions.
Patients who have renal impairment may develop spironolactone-induced hyperkalemia. In such cases, spironolactone and hydrochlorothiazide should be discontinued immediately. With severe hyperkalemia, the clinical situation dictates the procedures to be employed. These include the intravenous administration of calcium chloride solution, sodium bicarbonate solution, and/or the oral or parenteral administration of glucose with a rapid-acting insulin preparation. These are temporary measures to be repeated as required. Cationic exchange resins such as sodium polystyrene sulfonate may be orally or rectally administered. Persistent hyperkalemia may require dialysis.
-
DOSAGE AND ADMINISTRATION
Optimal dosage should be established by individual titration of the components.
Edema in Adults (Congestive Heart Failure, Hepatic Cirrhosis, or Nephrotic Syndrome)
The usual maintenance dose of spironolactone and hydrochlorothiazide tablets is 100 mg each of spironolactone and hydrochlorothiazide daily, administered in a single dose or in divided doses, but may range from 25 mg to 200 mg of each component daily depending on the response to the initial titration. In some instances it may be desirable to administer separate tablets of either spironolactone or hydrochlorothiazide in addition to spironolactone and hydrochlorothiazide tablets in order to provide optimal individual therapy.
The onset of diuresis with spironolactone and hydrochlorothiazide tablets occurs promptly and, due to prolonged effect of the spironolactone component, persists for two to three days after spironolactone and hydrochlorothiazide tablets are discontinued.
Essential Hypertension
Although the dosage will vary depending on the results of titration of the individual ingredients, many patients will be found to have an optimal response to 50 mg to 100 mg each of spironolactone and hydrochlorothiazide daily, given in a single dose or in divided doses.
Concurrent potassium supplementation is not recommended when spironolactone and hydrochlorothiazide tablets are used in the long-term management of hypertension or in the treatment of most edematous conditions, since the spironolactone content of spironolactone and hydrochlorothiazide tablets is usually sufficient to minimize loss induced by the hydrochlorothiazide component.
-
HOW SUPPLIED
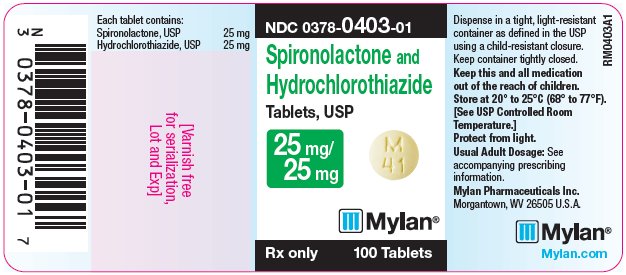
Spironolactone and Hydrochlorothiazide Tablets, USP are available containing 25 mg of spironolactone, USP and 25 mg of hydrochlorothiazide, USP.
The 25 mg/25 mg tablets are ivory, round, unscored tablets debossed with M over 41 on one side of the tablet and blank on the other side. They are available as follows:
NDC: 0378-0403-01
bottles of 100 tabletsNDC: 0378-0403-05
bottles of 500 tabletsStore at 20° to 25°C (68° to 77°F). [See USP Controlled Room Temperature.]
Protect from light.
Dispense in a tight, light-resistant container as defined in the USP using a child-resistant closure.
Mylan Pharmaceuticals Inc.
Morgantown, WV 26505 U.S.A.Revised: 11/2019
SPHZ:R22 -
PRINCIPAL DISPLAY PANEL - 25 mg/ 25 mg
NDC: 0378-0403-01
Spironolactone and
Hydrochlorothiazide
Tablets, USP
25 mg/
25 mgRx only 100 Tablets
Each tablet contains:
Spironolactone, USP 25 mg
Hydrochlorothiazide, USP 25 mgDispense in a tight, light-resistant
container as defined in the USP
using a child-resistant closure.Keep container tightly closed.
Keep this and all medication
out of the reach of children.Store at 20° to 25°C (68° to 77°F).
[See USP Controlled Room
Temperature.]Protect from light.
Usual Adult Dosage: See
accompanying prescribing
information.Mylan Pharmaceuticals Inc.
Morgantown, WV 26505 U.S.AMylan.com
RM0403A1
-
INGREDIENTS AND APPEARANCE
SPIRONOLACTONE AND HYDROCHLOROTHIAZIDE
spironolactone and hydrochlorothiazide tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0378-0403 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength SPIRONOLACTONE (UNII: 27O7W4T232) (SPIRONOLACTONE - UNII:27O7W4T232) SPIRONOLACTONE 25 mg HYDROCHLOROTHIAZIDE (UNII: 0J48LPH2TH) (HYDROCHLOROTHIAZIDE - UNII:0J48LPH2TH) HYDROCHLOROTHIAZIDE 25 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) D&C YELLOW NO. 10 (UNII: 35SW5USQ3G) FD&C YELLOW NO. 6 (UNII: H77VEI93A8) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MENTHOL, UNSPECIFIED FORM (UNII: L7T10EIP3A) MAGNESIUM STEARATE (UNII: 70097M6I30) MICROCRYSTALLINE CELLULOSE 102 (UNII: PNR0YF693Y) PEPPERMINT OIL (UNII: AV092KU4JH) SODIUM LAURYL SULFATE (UNII: 368GB5141J) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) STARCH, CORN (UNII: O8232NY3SJ) Product Characteristics Color WHITE (ivory) Score no score Shape ROUND Size 10mm Flavor Imprint Code M;41 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0378-0403-01 100 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 08/03/1979 2 NDC: 0378-0403-05 500 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 08/03/1979 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA086513 08/03/1979 Labeler - Mylan Pharmaceuticals Inc. (059295980)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.