VITRAKVI- larotrectinib capsule VITRAKVI- larotrectinib solution, concentrate
VITRAKVI by
Drug Labeling and Warnings
VITRAKVI by is a Prescription medication manufactured, distributed, or labeled by Bayer HealthCare Pharmaceuticals Inc., Penn Pharmaceutical Services Ltd, Albemarle Corporation, Sharp Corporation. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use VITRAKVI safely and effectively. See full prescribing information for VITRAKVI.
VITRAKVI® (larotrectinib) capsules, for oral use
VITRAKVI® (larotrectinib) oral solution
Initial U.S. Approval: 2018INDICATIONS AND USAGE
VITRAKVI is a kinase inhibitor indicated for the treatment of adult and pediatric patients with solid tumors that:
- have a neurotrophic receptor tyrosine kinase (NTRK) gene fusion without a known acquired resistance mutation,
- are metastatic or where surgical resection is likely to result in severe morbidity, and
- have no satisfactory alternative treatments or that have progressed following treatment.
This indication is approved under accelerated approval based on overall response rate and duration of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials (1,14).
DOSAGE AND ADMINISTRATION
- Select patients for treatment with VITRAKVI based on the presence of a NTRK gene fusion (2.1, 14).
- Recommended Dosage in Adult and Pediatric Patients with Body Surface Area of at Least 1.0 Meter-Squared: 100 mg orally twice daily (2.2)
- Recommended Dosage in Pediatric Patients with Body Surface Area of Less Than 1.0 Meter-Squared: 100 mg/m2 orally twice daily (2.2)
CONTRAINDICATIONS
None. (4)
WARNINGS AND PRECAUTIONS
- Neurotoxicity: Advise patients and caretakers of the risk of neurologic adverse reactions. Advise patients not to drive or operate hazardous machinery if experiencing neurotoxicity. Withhold and modify dosage, or permanently discontinue VITRAKVI based on severity. (2.3, 5.1)
- Hepatotoxicity: Monitor liver tests including ALT and AST every 2 weeks during the first month of treatment, then monthly thereafter and as clinically indicated. Withhold and modify dosage, or permanently discontinue VITRAKVI based on severity. (2.6, 5.2)
- Embryo-Fetal Toxicity: Can cause fetal harm. Advise females with reproductive potential of potential risk to the fetus and to use effective contraception. (5.3, 8.3)
ADVERSE REACTIONS
The most common adverse reactions (≥ 20%) with VITRAKVI were fatigue, nausea, dizziness, vomiting, increased AST, cough, increased ALT, constipation, and diarrhea. (6).
To report SUSPECTED ADVERSE REACTIONS, contact Bayer HealthCare Pharmaceuticals Inc. at 1-888-842-2937 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- Strong CYP3A4 Inhibitors: Avoid coadministration of strong CYP3A4 inhibitors with VITRAKVI. If coadministration cannot be avoided, reduce the VITRAKVI dose. (2.4, 7.1)
- Strong CYP3A4 Inducers: Avoid coadministration of strong CYP3A4 inducers with VITRAKVI. If coadministration cannot be avoided, increase the VITRAKVI dose. (2.5, 7.1)
- Sensitive CYP3A4 Substrates: Avoid coadministration of sensitive CYP3A4 substrates with VITRAKVI. (7.2)
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 7/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Patient Selection
2.2 Recommended Dosage
2.3 Dosage Modifications for Adverse Reactions
2.4 Dosage Modifications for Coadministration with Strong CYP3A4 Inhibitors
2.5 Dosage Modifications for Coadministration with Strong CYP3A4 Inducers
2.6 Dosage Modifications for Patients with Hepatic Impairment
2.7 Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Neurotoxicity
5.2 Hepatotoxicity
5.3 Embryo-Fetal Toxicity
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience
7 DRUG INTERACTIONS
7.1 Effects of Other Drugs on VITRAKVI
7.2 Effects of VITRAKVI on Other Drugs
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 Renal Impairment
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology and/or Pharmacology
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
VITRAKVI is indicated for the treatment of adult and pediatric patients with solid tumors that:
- have a neurotrophic receptor tyrosine kinase (NTRK) gene fusion without a known acquired resistance mutation,
- are metastatic or where surgical resection is likely to result in severe morbidity, and
- have no satisfactory alternative treatments or that have progressed following treatment.
This indication is approved under accelerated approval based on overall response rate and duration of response [see Clinical Studies (14)]. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
-
2 DOSAGE AND ADMINISTRATION
2.1 Patient Selection
Select patients for treatment with VITRAKVI based on the presence of a NTRK gene fusion in tumor specimens [see Clinical Studies (14)]. An FDA-approved test for the detection of NTRK gene fusion is not currently available.
2.2 Recommended Dosage
Recommended Dosage in Adult and Pediatric Patients with Body Surface Area of at Least 1.0 Meter-Squared
The recommended dosage of VITRAKVI is 100 mg orally twice daily, with or without food, until disease progression or until unacceptable toxicity.
Recommended Dosage in Pediatric Patients with Body Surface Area Less Than 1.0 Meter-Squared
The recommended dosage of VITRAKVI is 100 mg/m2 orally twice daily, with or without food, until disease progression or until unacceptable toxicity.
2.3 Dosage Modifications for Adverse Reactions
For Grade 3 or 4 adverse reactions:
- Withhold VITRAKVI until adverse reaction resolves or improves to baseline or Grade 1. Resume at the next dosage modification if resolution occurs within 4 weeks.
- Permanently discontinue VITRAKVI if an adverse reaction does not resolve within 4 weeks.
The recommended dosage modifications for VITRAKVI for adverse reactions are provided in Table 1.
Table 1 Recommended Dosage Modifications for VITRAKVI for Adverse Reactions
Dosage
ModificationAdult and
Pediatric Patients with Body
Surface Area of at Least 1.0 m2Pediatric Patients with Body
Surface Area Less Than 1.0 m2First
75 mg orally twice daily
75 mg/m2 orally twice daily
Second
50 mg orally twice daily
50 mg/m2 orally twice daily
Third
100 mg orally once daily
25 mg/m2 orally twice daily
Permanently discontinue VITRAKVI in patients who are unable to tolerate VITRAKVI after three dose modifications.
2.4 Dosage Modifications for Coadministration with Strong CYP3A4 Inhibitors
Avoid coadministration of strong CYP3A4 inhibitors with VITRAKVI. If coadministration of a strong CYP3A4 inhibitor cannot be avoided, reduce the VITRAKVI dose by 50%. After the inhibitor has been discontinued for 3 to 5 elimination half-lives, resume the VITRAKVI dose taken prior to initiating the CYP3A4 inhibitor [see Drug Interactions (7.1), Clinical Pharmacology (12.3)].
2.5 Dosage Modifications for Coadministration with Strong CYP3A4 Inducers
Avoid coadministration of strong CYP3A4 inducers with VITRAKVI. If coadministration of a strong CYP3A4 inducer cannot be avoided, double the VITRAKVI dose. After the inducer has been discontinued for 3 to 5 elimination half-lives, resume the VITRAKVI dose taken prior to initiating the CYP3A4 inducer [see Drug Interactions (7.1), Clinical Pharmacology (12.3)].
2.6 Dosage Modifications for Patients with Hepatic Impairment
Reduce the starting dose of VITRAKVI by 50% in patients with moderate (Child-Pugh B) to severe (Child-Pugh C) hepatic impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)].
2.7 Administration
VITRAKVI capsule or oral solution may be used interchangeably.
Do not make up a missed dose within 6 hours of the next scheduled dose.
If vomiting occurs after taking a dose of VITRAKVI, take the next dose at the scheduled time.
Capsules
Swallow capsules whole with water. Do not chew or crush the capsules.
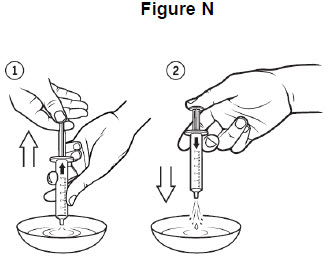
Oral Solution
- Store the glass bottle of VITRAKVI oral solution in the refrigerator. Discard any unused VITRAKVI oral solution remaining after 90 days of first opening the bottle.
- Prior to preparing an oral dose for administration, refer to the Instructions for Use.
-
3 DOSAGE FORMS AND STRENGTHS
Capsules
- 25 mg: white opaque hard gelatin capsule, size 2, with blue printing of "BAYER" cross and "25 mg" on body of capsules. 25 mg larotrectinib is equivalent to 30.7 mg larotrectinib sulfate.
- 100 mg: white opaque hard gelatin capsule, size 0, with blue printing of "BAYER" cross and "100 mg" on body of capsule. 100 mg larotrectinib is equivalent to 123 mg larotrectinib sulfate.
Oral Solution
- 20 mg/mL: clear yellow to orange solution. 20 mg/mL larotrectinib is equivalent to 24.6 mg/mL larotrectinib sulfate.
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Neurotoxicity
Among the 176 patients who received VITRAKVI, neurologic adverse reactions of any grade occurred in 53% of patients, including Grade 3 and Grade 4 neurologic adverse reactions in 6% and 0.6% of patients, respectively [see Adverse Reactions (6.1)]. The majority (65%) of neurologic adverse reactions occurred within the first three months of treatment (range: 1 day to 2.2 years). Grade 3 neurologic adverse reactions included delirium (2%), dysarthria (1%), dizziness (1%), gait disturbance (1%), and paresthesia (1%). Grade 4 encephalopathy (0.6%) occurred in a single patient. Neurologic adverse reactions leading to dose modification included dizziness (3%), gait disturbance (1%), delirium (1%), memory impairment (1%), and tremor (1%).
Advise patients and caretakers of these risks with VITRAKVI. Advise patients not to drive or operate hazardous machinery if they are experiencing neurologic adverse reactions. Withhold or permanently discontinue VITRAKVI based on the severity. If withheld, modify the VITRAKVI dosage when resumed [see Dosage and Administration (2.3)].
5.2 Hepatotoxicity
Among the 176 patients who received VITRAKVI, increased transaminases of any grade occurred in 45%, including Grade 3 increased AST or ALT in 6% of patients [see Adverse Reactions (6.1)]. One patient (0.6%) experienced Grade 4 increased ALT. The median time to onset of increased AST was 2 months (range: 1 month to 2.6 years). The median time to onset of increased ALT was 2 months (range: 1 month to 1.1 years). Increased AST and ALT leading to dose modifications occurred in 4% and 6% of patients, respectively. Increased AST or ALT led to permanent discontinuation in 2% of patients.
Monitor liver tests, including ALT and AST, every 2 weeks during the first month of treatment, then monthly thereafter, and as clinically indicated. Withhold or permanently discontinue VITRAKVI based on the severity. If withheld, modify the VITRAKVI dosage when resumed [see Dosage and Administration (2.3)].
5.3 Embryo-Fetal Toxicity
Based on literature reports in human subjects with congenital mutations leading to changes in TRK signaling, findings from animal studies, and its mechanism of action, VITRAKVI can cause fetal harm when administered to a pregnant woman. Larotrectinib resulted in malformations in rats and rabbits at maternal exposures that were approximately 11- and 0.7-times, respectively, those observed at the clinical dose of 100 mg twice daily. Advise women of the potential risk to a fetus. Advise females of reproductive potential to use an effective method of contraception during treatment and for 1 week after the final dose of VITRAKVI [see Use in Specific Populations (8.1, 8.3)].
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Neurotoxicity [see Warnings and Precautions (5.1)]
- Hepatotoxicity [see Warnings and Precautions (5.2)]
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Data in WARNINGS AND PRECAUTIONS and below reflects exposure to VITRAKVI in 176 patients, including 70 (40%) patients exposed for greater than 6 months and 35 (20%) patients exposed for greater than 1 year. VITRAKVI was studied in one adult dose-finding trial [LOXO-TRK-14001 (n = 70)], one pediatric dose-finding trial [SCOUT (n = 43)], and one single arm trial [NAVIGATE (n = 63)]. All patients had an unresectable or metastatic solid tumor and no satisfactory alternative treatment options or disease progression following treatment.
Across these 176 patients, the median age was 51 years (range: 28 days to 82 years); 25% were 18 years or younger; 52% were male; and 72% were White, 11% were Hispanic/Latino, 8% were Black, and 3% were Asian. The most common tumors in order of decreasing frequency were soft tissue sarcoma (16%), salivary gland (11%), lung (10%), thyroid (9%), colon (8%), infantile fibrosarcoma (8%), primary central nervous system (CNS) (7%), or melanoma (5%). NTRK gene fusions were present in 60% of VITRAKVI-treated patients. Most adults (80%) received VITRAKVI 100 mg orally twice daily and 68% of pediatrics (18 years or younger) received VITRAKVI 100 mg/m2 twice daily up to a maximum dose of 100 mg twice daily. The dose ranged from 50 mg daily to 200 mg twice daily in adults and 9.6 mg/m2 twice daily to 120 mg/m2 twice daily in pediatrics [see Pediatric Use (8.4)].
The most common adverse reactions (≥ 20%) in order of decreasing frequency were fatigue, nausea, dizziness, vomiting, anemia, increased AST, cough, increased ALT, constipation, and diarrhea.
The most common serious adverse reactions (≥ 2%) were pyrexia, diarrhea, sepsis, abdominal pain, dehydration, cellulitis, and vomiting. Grade 3 or 4 adverse reactions occurred in 51% of patients; adverse reactions leading to dose interruption or reduction occurred in 37% of patients and 13% permanently discontinued VITRAKVI for adverse reactions.
The most common adverse reactions (1-2% each) that resulted in discontinuation of VITRAKVI were brain edema, intestinal perforation, pericardial effusion, pleural effusion, small intestinal obstruction, dehydration, fatigue, increased ALT, increased AST, enterocutaneous fistula, increased amylase, increased lipase, muscular weakness, abdominal pain, asthenia, decreased appetite, dyspnea, hyponatremia, jaundice, syncope, vomiting, acute myeloid leukemia, and nausea.
The most common adverse reactions (≥ 3%) resulting in dose modification (interruption or reduction) were increased ALT (6%), increased AST (6%), and dizziness (3%). Most (82%) adverse reactions leading to dose modification occurred during the first three months of exposure.
Adverse reactions of VITRAKVI occurring in ≥ 10% of patients and laboratory abnormalities worsening from baseline in ≥ 5% of patients are summarized in Table 2 and Table 3, respectively.
Table 2 Adverse Reactions Occurring in ≥ 10% of Patients Treated with VITRAKVI
Adverse Reaction VITRAKVI
N = 176All Grades*
(%)Grade 3-4†
(%)- * National Cancer Institute-Common Terminology Criteria for Adverse Events (NCI-CTCAE) v 4.03.
- † One Grade 4 adverse reaction of pyrexia.
General
Fatigue
37
3
Pyrexia
18
1
Edema peripheral
15
0
Gastrointestinal
Nausea
29
1
Vomiting
26
1
Constipation
23
1
Diarrhea
22
2
Abdominal pain
13
2
Nervous System
Dizziness
28
1
Headache
14
0
Respiratory, Thoracic and Mediastinal
Cough
26
0
Dyspnea
18
2
Nasal congestion
10
0
Investigations
Increased weight
15
4
Musculoskeletal and Connective Tissue
Arthralgia
14
1
Myalgia
14
1
Muscular weakness
13
0
Back pain
12
1
Pain in extremity
12
1
Metabolism and Nutrition
Decreased appetite
13
2
Vascular
Hypertension
11
2
Injury, Poisoning and Procedural Complications
Fall
10
1
Table 3 Laboratory Abnormalities Occurring in ≥ 5% Patients Treated with VITRAKVI
Laboratory Abnormality VITRAKVI* All Grades†
(%)Grade 3-4
(%)- * Denominator for each laboratory parameter is based on the number of patients with a baseline and post-treatment laboratory value available which ranged from 170 to 174 patients.
- † NCI-CTCAE v 4.03.
Chemistry
Increased ALT
45
3
Increased AST
45
3
Hypoalbuminemia
35
2
Increased alkaline phosphatase
30
3
Hematology
Anemia
42
10
Neutropenia
23
7
-
7 DRUG INTERACTIONS
7.1 Effects of Other Drugs on VITRAKVI
Strong CYP3A4 Inhibitors
Coadministration of VITRAKVI with a strong CYP3A4 inhibitor may increase larotrectinib plasma concentrations, which may result in a higher incidence of adverse reactions [see Clinical Pharmacology (12.3)]. Avoid coadministration of VITRAKVI with strong CYP3A4 inhibitors, including grapefruit or grapefruit juice. If coadministration of strong CYP3A4 inhibitors cannot be avoided, modify VITRAKVI dose as recommended [see Dosage and Administration (2.4)].
Strong CYP3A4 Inducers
Coadministration of VITRAKVI with a strong CYP3A4 inducer may decrease larotrectinib plasma concentrations, which may decrease the efficacy of VITRAKVI [see Clinical Pharmacology (12.3)]. Avoid coadministration of VITRAKVI with strong CYP3A4 inducers, including St. John’s wort. If coadministration of strong CYP3A4 inducers cannot be avoided, modify VITRAKVI dose as recommended [see Dosage and Administration (2.5)].
7.2 Effects of VITRAKVI on Other Drugs
Sensitive CYP3A4 Substrates
Coadministration of VITRAKVI with sensitive CYP3A4 substrates may increase their plasma concentrations, which may increase the incidence or severity of adverse reactions [see Clinical Pharmacology (12.3)]. Avoid coadministration of VITRAKVI with sensitive CYP3A4 substrates. If coadministration of these sensitive CYP3A4 substrates cannot be avoided, monitor patients for increased adverse reactions of these drugs.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Based on literature reports in human subjects with congenital mutations leading to changes in TRK signaling, findings from animal studies, and its mechanism of action [see Clinical Pharmacology (12.1)], VITRAKVI can cause embryo-fetal harm when administered to a pregnant woman. There are no available data on VITRAKVI use in pregnant women. Administration of larotrectinib to pregnant rats and rabbits during the period of organogenesis resulted in malformations at maternal exposures that were approximately 11- and 0.7-times, respectively, those observed at the clinical dose of 100 mg twice daily (see Data). Advise pregnant women of the potential risk to a fetus.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Human Data
Published reports of individuals with congenital mutations in TRK pathway proteins suggest that decreases in TRK-mediated signaling are correlated with obesity, developmental delays, cognitive impairment, insensitivity to pain, and anhidrosis.
Animal Data
Larotrectinib crosses the placenta in animals. Larotrectinib did not result in embryolethality at maternally toxic doses [up to 40 times the human exposure based on area under the curve (AUC) at the clinical dose of 100 mg twice daily] in embryo-fetal development studies in pregnant rats dosed during the period of organogenesis; however, larotrectinib was associated with fetal anasarca in rats from dams treated at twice-daily doses of 40 mg/kg [11 times the human exposure (AUC) at the clinical dose of 100 mg twice daily]. In pregnant rabbits, larotrectinib administration was associated with omphalocele at twice-daily doses of 15 mg/kg (0.7 times the human exposure at the clinical dose of 100 mg twice daily).
8.2 Lactation
Risk Summary
There are no data on the presence of larotrectinib or its metabolites in human milk and no data on its effects on the breastfed child or on milk production. Because of the potential for serious adverse reactions in breastfed children, advise women not to breastfeed during treatment with larotrectinib and for 1 week after the final dose.
8.3 Females and Males of Reproductive Potential
Pregnancy Testing
Verify pregnancy status in females of reproductive potential prior to initiating VITRAKVI [see Use in Specific Populations (8.1)].
Contraception
VITRAKVI can cause embryo-fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)].
Females
Advise female patients of reproductive potential to use effective contraception during treatment with VITRAKVI and for at least 1 week after the final dose.
Males
Advise males with female partners of reproductive potential to use effective contraception during treatment with VITRAKVI and for 1 week after the final dose.
Infertility
Females
Based on histopathological findings in the reproductive tracts of female rats in a 1-month repeated-dose study, VITRAKVI may reduce fertility [See Nonclinical Toxicology (13.1)].
8.4 Pediatric Use
The safety and effectiveness of VITRAKVI in pediatric patients was established based upon data from three multicenter, open-label, single-arm clinical trials in adult or pediatric patients 28 days and older [see Adverse Reactions (6.1), Clinical Studies (14)].
The efficacy of VITRAKVI was evaluated in 12 pediatric patients and is described in the Clinical Studies section [see Clinical Studies (14)]. The safety of VITRAKVI was evaluated in 44 pediatric patients who received VITRAKVI. Of these 44 patients, 27% were 1 month to < 2 years (n = 12), 43% were 2 years to < 12 years (n = 19), and 30% were 12 years to < 18 years (n = 13); 43% had metastatic disease and 57% had locally advanced disease; and 91% had received prior treatment for their cancer, including surgery, radiotherapy, or systemic therapy. The most common cancers were infantile fibrosarcoma (32%), soft tissue sarcoma (25%), primary CNS tumors (20%), and thyroid cancer (9%). The median duration of exposure was 5.4 months (range: 9 days to 1.9 years).
Due to the small number of pediatric and adult patients, the single arm design of clinical studies of VITRAKVI, and confounding factors such as differences in susceptibility to infections between pediatric and adult patients, it is not possible to determine whether differences in the incidence of adverse reactions to VITRAKVI are related to patient age or other factors. Adverse reactions and laboratory abnormalities of Grade 3 or 4 severity occurring more frequently (at least a 5% increase in per-patient incidence) in pediatric patients compared to adult patients were increased weight (11% vs. 2%) and neutropenia (20% vs. 2%). One of the 44 pediatric patients discontinued VITRAKVI due to an adverse reaction (Grade 3 increased ALT).
The pharmacokinetics of VITRAKVI in the pediatric population were similar to those seen in adults [see Clinical Pharmacology (12.3)].
Juvenile Animal Toxicity Data
Larotrectinib was administered in a juvenile toxicity study in rats at twice daily doses of 0.2, 2 and 7.5 mg/kg from postnatal day (PND) 7 to 27 and at twice daily doses of 0.6, 6 and 22.5mg/kg between PND 28 and 70. The dosing period was equivalent to human pediatric populations from newborn to adulthood. The doses of 2/6 mg/kg twice daily [approximately 0.7 times the human exposure (AUC) at the clinical dose of 100 mg twice daily] and 7.5/22.5 mg/kg twice daily (approximately 4 times the human exposure at the clinical dose of 100 mg twice daily) resulted in mortality between PND 9 to 99; a definitive cause of death was not identified in the majority of cases.
The main findings were transient central nervous system-related signs including head flick, tremor, and circling in both sexes. An increase in the number of errors in a maze swim test occurred in females at exposures of approximately 4 times the human exposure (AUC) at the clinical dose of 100 mg twice daily. Decreased growth and delays in sexual development occurred in the mid- and high-dose groups. Mating was normal in treated animals, but a reduction in pregnancy rate occurred at the high-dose of 7.5/22.5 mg/kg twice daily (approximately 4 times the human exposure at the clinical dose of 100 mg twice daily).
8.5 Geriatric Use
Of 176 patients in the overall safety population who received VITRAKVI, 22% of patients were ≥ 65 years of age and 5% of patients were ≥ 75 years of age. Clinical studies of VITRAKVI did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects.
8.6 Hepatic Impairment
No dose adjustment is recommended for patients with mild hepatic impairment (Child-Pugh A). Larotrectinib clearance was reduced in subjects with moderate (Child-Pugh B) to severe (Child-Pugh C) hepatic impairment [see Clinical Pharmacology (12.3)]. Reduce VITRAKVI dose as recommended [see Dosage and Administration (2.6)].
8.7 Renal Impairment
No dose adjustment is recommended for patients with renal impairment of any severity [see Clinical Pharmacology (12.3)].
-
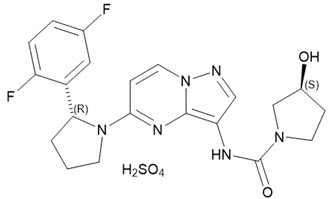
11 DESCRIPTION
Larotrectinib is a kinase inhibitor. VITRAKVI (larotrectinib) capsules and oral solution are formulated using larotrectinib sulfate. The molecular formula for larotrectinib sulfate is C21H24F2N6O6S and the molecular weight is 526.51 g/mol for the sulfate salt and 428.44 g/mol for the free base. The chemical name is (3S)-N-{5-[(2R)-2-(2,5-difluorophenyl)-1-pyrrolidinyl]pyrazolo[1,5-a]pyrimidin-3-yl}-3-hydroxy-1-pyrrolidinecarboxamide sulfate. Larotrectinib sulfate has the following chemical structure:
Larotrectinib sulfate is an off-white to pinkish yellow solid that is not hygroscopic. The aqueous solubility of larotrectinib at 37°C is pH dependent (very soluble at pH 1.0 and freely soluble at pH 6.8, according to USP descriptive terms of solubility).
VITRAKVI (larotrectinib) capsules and oral solution are for oral use. Each capsule contains 25 mg or 100 mg larotrectinib (30.7 mg and 123 mg larotrectinib sulfate, respectively) in a hard gelatin capsule. The capsule is composed of gelatin, titanium dioxide, and edible ink.
The oral solution contains 20 mg/mL larotrectinib (24.6 mg/mL larotrectinib sulfate) and the following inactive ingredients: purified water, hydroxypropyl betadex, sucrose, glycerin, sorbitol, citric acid, sodium phosphate, sodium citrate dihydrate, propylene glycol and flavoring. Preserved with methylparaben and potassium sorbate.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Larotrectinib is an inhibitor of the tropomyosin receptor kinases (TRK), TRKA, TRKB, and TRKC. In a broad panel of purified enzyme assays, larotrectinib inhibited TRKA, TRKB, and TRKC with IC50 values between 5-11 nM. One other kinase TNK2 was inhibited at approximately 100-fold higher concentration. TRKA, B, and C are encoded by the genes NTRK1, NTRK2, and NTRK3. Chromosomal rearrangements involving in-frame fusions of these genes with various partners can result in constitutively-activated chimeric TRK fusion proteins that can act as an oncogenic driver, promoting cell proliferation and survival in tumor cell lines.
In in vitro and in vivo tumor models, larotrectinib demonstrated anti-tumor activity in cells with constitutive activation of TRK proteins resulting from gene fusions, deletion of a protein regulatory domain, or in cells with TRK protein overexpression. Larotrectinib had minimal activity in cell lines with point mutations in the TRKA kinase domain, including the clinically identified acquired resistance mutation, G595R. Point mutations in the TRKC kinase domain with clinically identified acquired resistance to larotrectinib include G623R, G696A, and F617L.
12.2 Pharmacodynamics
Cardiac Electrophysiology
At a dose 9-fold higher than the recommended adult dose, VITRAKVI does not prolong QTc intervals to any clinically relevant extent.
12.3 Pharmacokinetics
The pharmacokinetics of larotrectinib were studied in healthy subjects and adult and pediatric patients with locally advanced or metastatic solid tumors. In healthy subjects who received a single dose of VITRAKVI capsules, systemic exposure (Cmax and AUC) of larotrectinib was dose proportional over the dose range of 100 mg to 400 mg (1 to 4 times the recommended adult dose) and slightly greater than proportional at doses of 600 mg to 900 mg (6 to 9 times the recommended adult dose). In adult patients who received VITRAKVI capsules 100 mg twice daily in Study LOXO-TRK-14001, peak plasma levels (Cmax) of larotrectinib were achieved at approximately 1 hour after dosing and steady-state was reached within 3 days. Mean steady-state larotrectinib [coefficient of variation (CV%)] for Cmax was 788 (81%) ng/mL and AUC0-24hr was 4351 (97%) ng*h/mL.
Absorption
The mean absolute bioavailability of VITRAKVI capsules was 34% (range: 32% to 37%). In healthy subjects, the AUC of VITRAKVI oral solution was similar to that of the capsules and the Cmax was 36% higher with the oral solution.
Effect of Food
The AUC of larotrectinib was similar and the Cmax was reduced by 35% after oral administration of a single 100 mg capsule of VITRAKVI to healthy subjects taken with a high-fat meal (approximately 900 calories, 58 grams carbohydrate, 56 grams fat and 43 grams protein) compared to the Cmax and AUC in the fasted state.
Distribution
The mean (CV%) volume of distribution (Vss) of larotrectinib is 48 (38%) L following intravenous administration of larotrectinib in healthy subjects.
Larotrectinib is 70% bound to human plasma proteins in vitro and binding is independent of drug concentrations. The blood-to-plasma concentration ratio is 0.9.
Elimination
The mean (CV%) clearance (CL/F) of larotrectinib is 98 (44%) L/h and the half-life is 2.9 hours following oral administration of VITRAKVI in healthy subjects.
Metabolism
Larotrectinib is metabolized predominantly by CYP3A4. Following oral administration of a single [14C] radiolabeled 100 mg dose of larotrectinib to healthy subjects, unchanged larotrectinib constituted 19% and an O-linked glucuronide constituted 26% of the major circulating radioactive drug components in plasma.
Excretion
Following oral administration of a single [14C] radiolabeled 100 mg dose of larotrectinib to healthy subjects, 58% (5% unchanged) of the administered radioactivity was recovered in feces and 39% (20% unchanged) was recovered in urine.
Specific Populations
Age (range: 28 days to 82 years), sex, and body weight (range: 3.8 kg to 179 kg) had no clinically meaningful effect on the pharmacokinetics of larotrectinib.
Pediatric Patients
In pediatric patients, the larotrectinib geometric mean (%CV) AUC0-24hr by age subgroup was: 3348 (66%) ng*h/mL in patients 1 month to < 2 years (n = 9), 4135 (36%) ng*h/mL in patients 2 to < 12 years (n = 15), and 3108 (69%) ng*h/mL and in patients 12 to < 18 years (n = 9).
Patients with Renal Impairment
Following oral administration of a single 100 mg dose of VITRAKVI capsules in subjects with end-stage renal disease (e.g., subjects who required dialysis), the AUC0-INF of larotrectinib increased 1.5-fold and Cmax increased 1.3-fold as compared to that in subjects with normal renal function (creatinine clearance ≥ 90 mL/min as estimated by Cockcroft-Gault). The pharmacokinetics of VITRAKVI in patients with moderate to severe renal impairment (creatinine clearance ≤ 60 mL/min) have not been studied.
Patients with Hepatic Impairment
Following oral administration of a single 100 mg dose of VITRAKVI capsules, the AUC0-INF of larotrectinib increased 1.3-fold in subjects with mild hepatic impairment (Child-Pugh A), 2-fold in subjects with moderate hepatic impairment (Child-Pugh B) and 3.2-fold in subjects with severe hepatic impairment (Child-Pugh C) as compared to that in subjects with normal hepatic function. The Cmax was similar in subjects with mild and moderate hepatic impairment and the Cmax of larotrectinib increased 1.5-fold in subjects with severe hepatic impairment as compared to that in subjects with normal hepatic function [see Dosage and Administration (2.6), Use in Specific Populations (8.6)].
Drug Interaction Studies
Clinical Studies
Effect of Strong CYP3A Inhibitors: Coadministration of a single 100 mg dose of VITRAKVI capsules with a strong CYP3A inhibitor (itraconazole) increased the AUC0-INF of larotrectinib by 4.3-fold and the Cmax by 2.8-fold as compared to VITRAKVI administered alone [see Dosage and Administration (2.4), Drug Interactions (7.1)]. The effects of CYP3A moderate and weak inhibitors on the pharmacokinetics of larotrectinib have not been studied.
Effect of Strong CYP3A Inducers: Coadministration of a single 100 mg dose of VITRAKVI capsules with a strong CYP3A inducer (rifampin) decreased the AUC0-INF of larotrectinib by 81% and of Cmax by 71% as compared to VITRAKVI administered alone [see Dosage and Administration (2.5), Drug Interactions (7.1)]. The effects of CYP3A weak and moderate inducers on the pharmacokinetics of larotrectinib have not been studied.
Effect of Strong P-glycoprotein (P-gp) Inhibitors: Coadministration of a single 100 mg dose of VITRAKVI capsules with a P-gp inhibitor (rifampin) increased the AUC0-INF of larotrectinib by 1.7-fold and the Cmax by 1.8-fold as compared to VITRAKVI administered alone.
Effect of Larotrectinib on CYP3A4 Substrates: Coadministration of VITRAKVI capsules 100 mg twice daily with a sensitive CYP3A4 substrate (midazolam) increased both the AUC0-INF and Cmax of midazolam by 1.7-fold as compared to midazolam administered alone. The AUC0-INF and Cmax of 1-hydroxymidazolam, the main metabolite of midazolam, were both increased 1.4-fold as compared to when midazolam was administered alone [see Drug Interactions (7.2)].
In Vitro Studies
Effect of Transporter on Larotrectinib: Larotrectinib is a substrate for P-gp and BCRP. Larotrectinib is not a substrate of OAT1, OAT3, OCT1, OCT2, OATP1B1, or OATP1B3.
Effect of Larotrectinib on Transporters: Larotrectinib is not an inhibitor of BCRP, P-gp, OAT1, OAT3, OCT1, OCT2, OATP1B1, OATP1B3, BSEP, MATE1 and MATE2-K at clinically relevant concentrations.
Effect of Larotrectinib on CYP Substrates: Larotrectinib is not an inhibitor or inducer of CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, or CYP2D6 at clinically relevant concentrations.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies have not been conducted with larotrectinib. Larotrectinib was not mutagenic in the in vitro bacterial reverse mutation (Ames) assays, with or without metabolic activation, or in the in vitro mammalian mutagenesis assays, with or without metabolic activation. In vivo, larotrectinib was negative in the mouse micronucleus test.
Fertility studies with larotrectinib have not been conducted. In a 3-month repeat-dose toxicity study in the rat, larotrectinib had no effects on spermatogenesis at 75 mg/kg/day (approximately 7 times the human exposure at the 100 mg twice daily dose). Additionally, larotrectinib had no histological effects on the male reproductive tract in rats or monkeys at doses resulting in exposures up to 10 times the human exposure (AUC0-24hr) at the 100 mg twice daily clinical dose.
In a 1-month repeat-dose study in the rat, decreased uterine weight and uterine atrophy were seen at 200 mg/kg/day [approximately 45 times the human exposure (AUC) at the 100 mg twice daily dose]. Fewer corpora lutea and increased incidence of anestrus were also noted at doses ≥ 60 mg/kg/day (approximately 10 times the human exposure at the 100 mg twice daily dose). Decreased fertility occurred in a juvenile animal study [see Use in Specific Populations (8.4)]. There were no findings in female reproductive organs in repeat-dose studies in monkeys at exposures up to 22 times the human exposure at the 100 mg twice daily dose.
13.2 Animal Toxicology and/or Pharmacology
In general toxicology studies conducted in rats and monkeys and in reproductive toxicology studies conducted in rats and rabbits, administration of larotrectinib led to increased food consumption and increased body weight at doses resulting in exposures 0.6 times the human exposure at the 100 mg twice daily clinical dose. Obesity has also been one phenotypic outcome of some human syndromes resulting from congenital mutations in NTRK2 resulting in altered TRK signaling.
-
14 CLINICAL STUDIES
The efficacy of VITRAKVI was evaluated in pediatric and adult patients with unresectable or metastatic solid tumors with a NTRK gene fusion enrolled in one of three multicenter, open-label, single-arm clinical trials: Study LOXO-TRK-14001 (NCT02122913), SCOUT (NCT02637687), and NAVIGATE (NCT02576431). All patients were required to have progressed following systemic therapy for their disease, if available, or would have required surgery with significant morbidity for locally advanced disease.
Adult patients received VITRAKVI 100 mg orally twice daily and pediatric patients (18 years or younger) received VITRAKVI 100 mg/m2 up to a maximum dose of 100 mg orally twice daily until unacceptable toxicity or disease progression. Identification of positive NTRK gene fusion status was prospectively determined in local laboratories using next generation sequencing (NGS) or fluorescence in situ hybridization (FISH). NTRK gene fusions were inferred in three patients with infantile fibrosarcoma who had a documented ETV6 translocation identified by FISH. The major efficacy outcome measures were overall response rate (ORR) and duration of response (DOR), as determined by a blinded independent review committee (BIRC) according to RECIST v1.1.
The assessment of efficacy was based on the first 55 patients with solid tumors with an NTRK gene fusion enrolled across the three clinical trials. Baseline characteristics were: median age 45 years (range 4 months to 76 years); 22% <18 years of age, and 78% ≥18 years of age; 53% male; 67% White; 7% Hispanic/Latino, 4% Asian, 4% Black; and ECOG performance status 0-1 (93%) or 2 (7%). Eighty-two percent of patients had metastatic disease and 18% had locally advanced, unresectable disease. Ninety-eight percent of patients had received prior treatment for their cancer, including surgery, radiotherapy, or systemic therapy. Of these, 82% (n = 45) received prior systemic therapy with a median of two prior systemic regimens and 35% (n = 19) received three or more prior systemic regimens. The most common cancers were salivary gland tumors (22%), soft tissue sarcoma (20%), infantile fibrosarcoma (13%), and thyroid cancer (9%). A total of 50 patients had NTRK gene fusions detected by NGS and 5 patients had NTRK gene fusions detected by FISH.
Efficacy results are summarized in Tables 4, 5, and 6.
- Table 4 Efficacy Results for Patients with Solid Tumors Harboring NTRK Gene Fusions
Efficacy Parameter VITRAKVI
N = 55- * Includes one pediatric patient with unresectable infantile fibrosarcoma who underwent resection following partial response and who remained disease-free at data cutoff.
- † Median duration of response not reached at time of data cutoff.
- ‡ 3 patients with an ongoing response were followed < 9 months from onset of response.
- § 10 patients with an ongoing response were followed < 12 months from onset of response.
Overall response rate (95% CI)
75% (61%, 85%)
Complete response rate
22%
Partial response rate*
53%
Duration of response†
N = 41
Range (months)
1.6+, 33.2+
% with duration ≥ 6 months
73%
% with duration ≥ 9 months‡
63%
% with duration ≥ 12 months§
39%
+ Denotes ongoing response.
Table 5 Efficacy Results by Tumor Type
Tumor Type Patients
(N=55)ORR DOR % 95% CI Range
(months)- * Observed values at data cutoff, not a range.
Soft tissue sarcoma
11
91%
(59%, 100%)
3.6, 33.2+
Salivary gland
12
83%
(52%, 98%)
7.7, 27.9+
Infantile fibrosarcoma
7
100%
(59%, 100%)
1.4+, 10.2+
Thyroid
5
100%
(48%, 100%)
3.7, 27.0+
Lung
4
75%
(19%, 99%)
8.2, 20.3+
Melanoma
4
50%
NA
1.9, 17.5+*
Colon
4
25%
NA
5.6*
Gastrointestinal stromal tumor
3
100%
(29%, 100%)
9.5, 17.3
Cholangiocarcinoma
2
SD, NE
NA
NA
Appendix
1
SD
NA
NA
Breast
1
PD
NA
NA
Pancreas
1
SD
NA
NA
NA = not applicable due to small numbers or lack of response; CR = complete response; PR = partial response; NE = not evaluable; SD = stable disease; PD = progressive disease.
+ Denotes ongoing response.
Table 6 Efficacy Results by NTRK Fusion Partner
NTRK Partner* Patients
(N=55)ORR DOR % 95% CI Range
(months)- * Fusion partners identified in the primary analysis set (N=55) may not represent all potential fusion partners.
- † Duration of response censored at the time of surgery for one pediatric patient with unresectable infantile fibrosarcoma who underwent resection following partial response and who remained disease-free at data cutoff.
- ‡ Observed values at data cutoff, not a range.
ETV6-NTRK3
25
84%
(64%, 96%)
3.7, 27.9+
TPM3-NTRK1
9
56%
(21%, 86%)
3.7, 10.3+
LMNA-NTRK1
5
40%
NA
5.6, 33.2+
Inferred ETV6-NTRK3
3
100%
(29%, 100%)
1.4+, 2.7†
IRF2BP2-NTRK1
2
CR, PR
NA
3.7, 20.3+
SQSTM1-NTRK1
2
PR, PR
NA
9.9, 12.9+
PDE4DIP-NTRK1
1
PR
NA
3.6+ ‡
PPL-NTRK1
1
CR
NA
12.0+ ‡
STRN-NTRK2
1
PR
NA
5.6‡
TPM4-NTRK3
1
CR
NA
23.6‡
TPR-NTRK1
1
PR
NA
8.2‡
TRIM63-NTRK1
1
PR
NA
1.9+ ‡
CTRC-NTRK1
1
SD
NA
NA
GON4L-NTRK1
1
NE
NA
NA
PLEKHA6-NTRK1
1
SD
NA
NA
CR = complete response; PR = partial response; NE = not evaluable; SD = stable disease; NA = not applicable.
+ Denotes ongoing response.
-
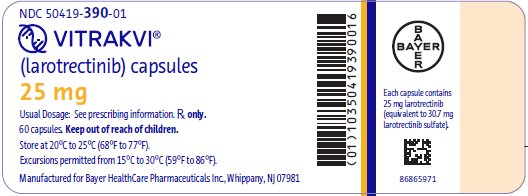
16 HOW SUPPLIED/STORAGE AND HANDLING
Capsules
25 mg: Hard gelatin opaque white capsule size #2 with blue printing of "BAYER" cross and "25 mg" on the body of the capsule.
- 60 count bottle NDC# 50419-390-01
100 mg: Hard gelatin opaque white capsule size #0 with blue printing of "BAYER" cross and "100 mg" on the body of the capsule.
- 60 count bottle NDC# 50419-391-01
Store capsules at room temperature 20°C to 25°C (68°F to 77°F); temperature excursions between 15°C and 30°C (59°F to 86°F) are permitted [see USP Controlled Room Temperature].
Oral Solution
20 mg/mL: Clear yellow to orange solution.
- 100 mL bottle NDC# 50419-392-01
Refrigerate oral solution at 2°C to 8°C (36°F to 46°F). Do not freeze.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information and Instructions for Use).
Neurotoxicity
Advise patients to notify their healthcare provider if they experience new or worsening neurotoxicity. Advise patients not to drive or operate hazardous machinery if they are experiencing neurologic adverse reactions [see Warnings and Precautions (5.1)].
Hepatotoxicity
Advise patients that they will need to undergo laboratory tests to monitor liver function [see Warnings and Precautions (5.2)].
Embryo-Fetal Toxicity
Advise males and females of reproductive potential of the potential risk to a fetus [see Warnings and Precautions (5.3), Use in Specific Populations (8.1)].
Advise females of reproductive potential to inform their healthcare provider of a known or suspected pregnancy and to use effective contraception during the treatment with VITRAKVI and for at least 1 week after the final dose [see Use in Specific Populations (8.3)].
Advise males with female partners of reproductive potential to use effective contraception during treatment with VITRAKVI and for at least 1 week after the final dose [see Use in Specific Populations (8.3)].
Lactation
Advise women not to breastfeed during treatment with VITRAKVI and for 1 week following the final dose [see Use in Specific Populations (8.2)].
Infertility
Advise females of reproductive potential that VITRAKVI may impair fertility [See Nonclinical Toxicology (13.1)].
Drug Interactions
Advise patients and caregivers to inform their healthcare provider of all concomitant medications, including prescription medicines, over-the-counter drugs, vitamins, and herbal products. Inform patients to avoid St. John’s wort, grapefruit or grapefruit juice while taking VITRAKVI [see Drug Interactions (7.1, 7.2)].
Manufactured for Bayer HealthCare Pharmaceuticals Inc.
Whippany, NJ 07981
-
PATIENT PACKAGE INSERT
PATIENT INFORMATION
VITRAKVI (vi trak vee)
(larotrectinib)
capsules and oral solutionWhat is VITRAKVI?
VITRAKVI is a prescription medicine that is used to treat adults and children with solid tumors (cancer) that:- are caused by certain abnormal NTRK genes and
- have spread or if surgery to remove their cancer is likely to cause severe complications, and
- there is no acceptable treatment option or the cancer grew or spread on other treatment.
Your healthcare provider will perform a test to make sure that VITRAKVI is right for you.
It is not known if VITRAKVI is safe and effective in children younger than 1 month of age.Before taking VITRAKVI, tell your healthcare provider about all of your medical conditions, including if you:
- have liver problems
- have nervous system (neurological) problems
-
are pregnant or plan to become pregnant. VITRAKVI can harm your unborn baby. You should not become pregnant during treatment with VITRAKVI.
- If you are able to become pregnant, your healthcare provider may do a pregnancy test before you start treatment with VITRAKVI.
- Females who are able to become pregnant should use effective birth control (contraception) during treatment and for at least 1 week after the final dose of VITRAKVI. Talk to your healthcare provider about birth control methods that may be right for you.
- Males with female partners who are able to become pregnant should use effective birth control during treatment with VITRAKVI and for at least 1 week after the final dose of VITRAKVI.
- are breastfeeding or plan to breastfeed. It is not known if VITRAKVI passes into your breast milk. Do not breastfeed during treatment and for 1 week after the last dose of VITRAKVI.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Certain other medicines may affect how VITRAKVI works. Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.
How should I take VITRAKVI?
- Take VITRAKVI exactly as your healthcare provider tells you.
- Your healthcare provider may stop treatment or change your dose of VITRAKVI if you have side effects. Do not change your dose or stop taking VITRAKVI unless your healthcare provider tells you.
- VITRAKVI comes in capsules and as an oral solution.
-
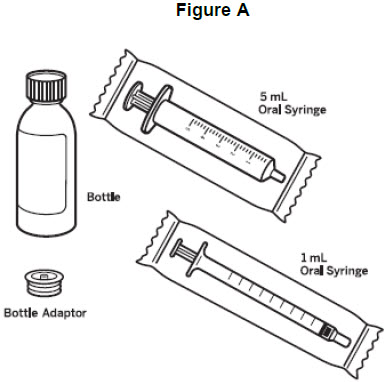
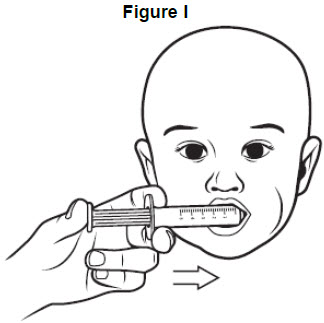
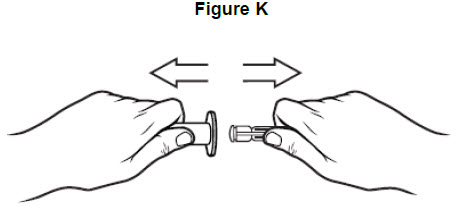
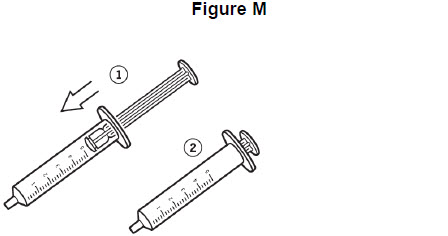
If your healthcare provider prescribes VITRAKVI oral solution:
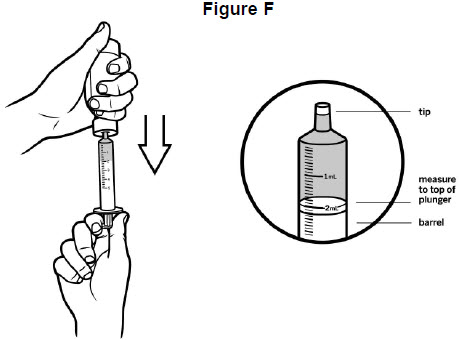
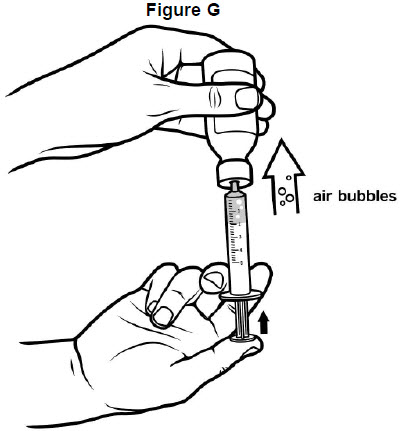
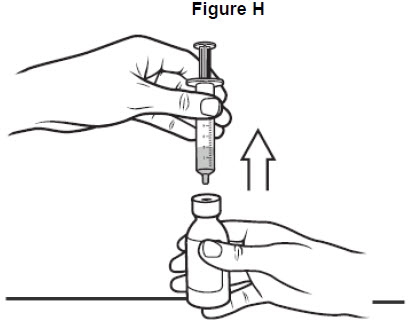
- Your healthcare provider will provide you with the VITRAKVI oral solution and oral syringes or send you to a pharmacy that can provide you with VITRAKVI oral solution and oral syringes.
- Your healthcare provider should show you how to correctly measure and give a dose of VITRAKVI oral solution.
- See the detailed Instructions for Use that comes with VITRAKVI oral solution for information about the correct way to measure and give a dose of VITRAKVI oral solution. If you have any questions, talk to your healthcare provider or pharmacist.
- VITRAKVI is usually taken by mouth 2 times a day.
- Swallow VITRAKVI capsules whole. Do not chew or crush the capsules.
- Take VITRAKVI with or without food.
- If you vomit after taking a dose of VITRAKVI, wait and take the next dose at your scheduled time
- If you miss a dose of VITRAKVI, take it as soon as you remember unless your next scheduled dose is due within 6 hours. Take the next dose at your regular time.
If you take too much VITRAKVI, call your healthcare provider.
What should I avoid while taking VITRAKVI?
- VITRAKVI can make you feel dizzy. Do not drive or operate machinery until you know how VITRAKVI affects you.
- Avoid taking St. John’s wort, eating grapefruit, or drinking grapefruit juice during treatment with VITRAKVI.
What are the possible side effects of VITRAKVI?
VITRAKVI may cause serious side effects, including:- Nervous system problems. Tell your healthcare provider if you develop any symptoms such as confusion, difficulty speaking, dizziness, coordination problems, tingling, numbness, or burning sensation in your hands and feet. Your healthcare provider may temporarily stop treatment, decrease your dose, or permanently stop VITRAKVI if you develop symptoms of a nervous system problem with VITRAKVI.
- Liver problems. Your healthcare provider will do blood tests to check your liver function during treatment with VITRAKVI. Tell your healthcare provider right away if you develop symptoms of liver problems including: loss of appetite, nausea or vomiting, or pain on the upper right side of your stomach area. Your healthcare provider may temporarily stop treatment, decrease your dose, or permanently stop VITRAKVI if you develop liver problems with VITRAKVI.
The most common side effects of VITRAKVI include:
- tiredness
- nausea
- dizziness
- vomiting
- cough
- constipation
- diarrhea
VITRAKVI may affect fertility in females and may affect your ability to become pregnant. Talk to your healthcare provider if this is a concern for you.
These are not all the possible side effects with VITRAKVI. Call your healthcare provider for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.How should I store VITRAKVI?
- Store VITRAKVI capsules at room temperature between 68°F to 77°F (20°C to 25°C).
- Store VITRAKVI oral solution in the refrigerator between 36° F to 46° F (2° C to 8° C). Do not freeze.
- Throw away (dispose of) any unused VITRAKVI oral solution remaining after 90 days of first opening the bottle.
Keep VITRAKVI and all medicines out of the reach of children.
General information about the safe and effective use of VITRAKVI.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use VITRAKVI for a condition for which it was not prescribed. Do not give VITRAKVI to other people, even if they have the same symptoms you have. It may harm them. You can ask your healthcare provider or pharmacist for more information about VITRAKVI that is written for health professionals.What are the ingredients in VITRAKVI?
Active ingredient: larotrectinib
Inactive ingredients:
Capsule: gelatin, titanium dioxide and edible ink
Oral Solution: purified water, hydroxypropyl betadex, sucrose, glycerin, sorbitol, citric acid, sodium phosphate, sodium citrate dihydrate, propylene glycol and flavoring. Preserved with methylparaben and potassium sorbate.
Manufactured for Bayer HealthCare Pharmaceuticals Inc., Whippany, NJ 07981
For more information, go to www.VITRAKVI.com or call 1-888-842-2937
This Patient Information has been approved by the U.S. Food and Drug Administration.
Revised: 7/2019
-
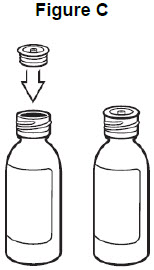
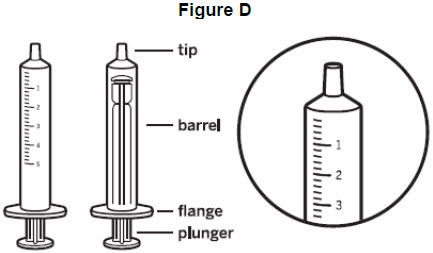
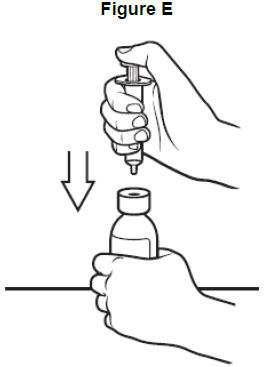
INSTRUCTIONS FOR USE
- PRINCIPAL DISPLAY PANEL
-
PRINCIPAL DISPLAY PANEL
Package Label - 25 mg - 60 CapsulesPRINCIPAL DISPLAY PANEL
NDC 71777-390-01
VITRAKVI®
(larotrectinib) capsules
25 mg
Usual Dosage: See prescribing information. Rx only.
60 capsules. Keep out of reach of children.
Store at 20°C to 25°C (68°F to 77°F).
Excursions permitted from 15°C to 30°C (59° to 86°F).Manufactured for Loxo Omcology, Inc. Stamford, CT 06901 86579626
(01)10371777390012
Bayer
LOXO
Each capsule contains
25 mg larotrectinib
(equivalent to 30.7 mg
larotrectinib sulfate). - PRINCIPAL DISPLAY PANEL
-
PRINCIPAL DISPLAY PANEL
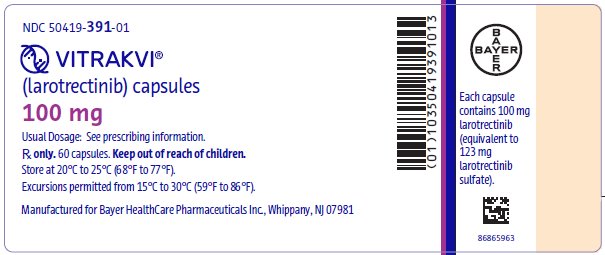
Package Label - 100 mg - 60 CapsulesPRINCIPAL DISPLAY PANEL
NDC 71777-391-01
VITRAKVI®
(larotrectinib) capsules
100 mg
Usual Dosage: See prescribing information.
Rx only. 60 capsules. Keep out of reach of children.
Store at 20°C to 25°C (68°F to 77°F).
Excursions permitted from 15°C to 30°C (59° to 86°F).Manufactured for Loxo Omcology, Inc. Stamford, CT 06901 86579634
(01)10371777391019
Bayer
LOXO
Each capsule
contains 100 mg
larotrectinib
(equivalent to
123 mg
larotrectinib
sulfate). - PRINCIPAL DISPLAY PANEL
-
PRINCIPAL DISPLAY PANEL
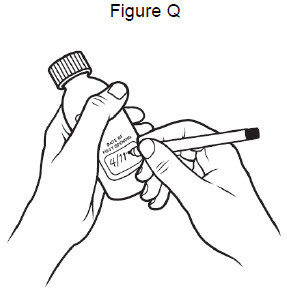
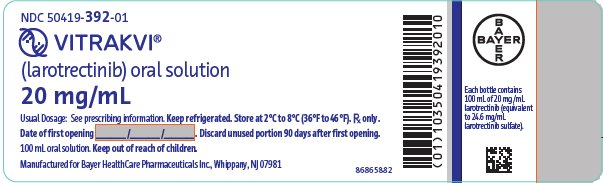
Package Label - 20 mg/mL - 100 mL Oral SolutionPRINCIPAL DISPLAY PANEL
NDC 71777-392-01
VITRAKVI®
(larotrectinib) oral solution
20 mg/mL
Usual Dosage: See prescribing information. Keep refrigerated. Store at 2°C to 8°C (36°F to 46°F). Rx only.
Date of first opening ____/____/____. Discard unused portion 90 days after first opening.
100 mL oral solution. Keep out of reach of children.Manufactured for Loxo Omcology, Inc. Stamford, CT 06901 86659069
(01)10371777392016
Bayer
LOXO
Each bottle contains
100 ml of 20 mg/mL
larotrectinib (equivalent
to 24.6 mg/mL
larotrectinib sulfate). -
INGREDIENTS AND APPEARANCE
VITRAKVI
larotrectinib capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 50419-390 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LAROTRECTINIB (UNII: PF9462I9HX) (LAROTRECTINIB - UNII:PF9462I9HX) LAROTRECTINIB 25 mg Inactive Ingredients Ingredient Name Strength GELATIN, UNSPECIFIED (UNII: 2G86QN327L) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) Product Characteristics Color WHITE (Opaque White) Score no score Shape CAPSULE Size 18mm Flavor Imprint Code BAYER;25mg Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 50419-390-01 60 in 1 BOTTLE; Type 0: Not a Combination Product 07/26/2019 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA authorized generic NDA210861 07/26/2019 VITRAKVI
larotrectinib capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 50419-391 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LAROTRECTINIB (UNII: PF9462I9HX) (LAROTRECTINIB - UNII:PF9462I9HX) LAROTRECTINIB 100 mg Inactive Ingredients Ingredient Name Strength GELATIN, UNSPECIFIED (UNII: 2G86QN327L) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) Product Characteristics Color WHITE (Opaque White) Score no score Shape CAPSULE Size 22mm Flavor Imprint Code BAYER;100mg Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 50419-391-01 60 in 1 BOTTLE; Type 0: Not a Combination Product 07/26/2019 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA210861 07/26/2019 VITRAKVI
larotrectinib solution, concentrateProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 50419-392 Route of Administration OROPHARYNGEAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LAROTRECTINIB (UNII: PF9462I9HX) (LAROTRECTINIB - UNII:PF9462I9HX) LAROTRECTINIB 20 mg in 1 mL Inactive Ingredients Ingredient Name Strength WATER (UNII: 059QF0KO0R) HYDROXYPROPYL BETADEX (0.6 HYDROXYPROPYL RESIDUES PER GLUCOSE) (UNII: 8W6Q67R6NX) SUCROSE (UNII: C151H8M554) GLYCERIN (UNII: PDC6A3C0OX) SORBITOL (UNII: 506T60A25R) CITRIC ACID MONOHYDRATE (UNII: 2968PHW8QP) SODIUM PHOSPHATE (UNII: SE337SVY37) TRISODIUM CITRATE DIHYDRATE (UNII: B22547B95K) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) METHYLPARABEN (UNII: A2I8C7HI9T) POTASSIUM SORBATE (UNII: 1VPU26JZZ4) Product Characteristics Color YELLOW (Clear Yellow to Orange) Score Shape Size Flavor BERRY (Citrus Berry) Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 50419-392-01 100 mL in 1 BOTTLE; Type 0: Not a Combination Product 07/26/2019 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA211710 07/26/2019 Labeler - Bayer HealthCare Pharmaceuticals Inc. (005436809) Establishment Name Address ID/FEI Business Operations Penn Pharmaceutical Services Ltd 226277259 MANUFACTURE(50419-390, 50419-391, 50419-392) Establishment Name Address ID/FEI Business Operations Albemarle Corporation 788779192 API MANUFACTURE(50419-392) Establishment Name Address ID/FEI Business Operations Sharp Corporation 143696495 PACK(50419-390, 50419-391, 50419-392) , LABEL(50419-390, 50419-391, 50419-392)
Trademark Results [VITRAKVI]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 VITRAKVI 87819990 5584983 Live/Registered |
Bayer Aktiengesellschaft 2018-03-05 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.