CIMETIDINE tablet, film coated
Cimetidine by
Drug Labeling and Warnings
Cimetidine by is a Prescription medication manufactured, distributed, or labeled by Blenheim Pharmacal, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
DESCRIPTION
Cimetidine is a histamine H 2-receptor antagonist. Chemically it is N”-cyano- N-methyl- N’-[2-[[(5-methyl-1 H-imidazol-4-yl)methyl]thio]-ethyl], guanidine.
The molecular formula for cimetidine is C 10H 16N 6S; and the molecular weight is 252.35. The structural formula for cimetidine is:
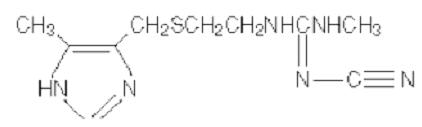
Cimetidine contains an imidazole ring, and is chemically related to histamine. Cimetidine has a bitter taste and characteristic odor.
Solubility Characteristics
Cimetidine is soluble in alcohol, slightly soluble in water, very slightly soluble in chloroform and insoluble in ether.
Each tablet, for oral administration, contains 300 mg, 400 mg, or 800 mg cimetidine. In addition, each tablet contains the following inactive ingredients: corn starch, magnesium stearate, microcrystalline cellulose, povidone, sodium lauryl sulfate and sodium starch glycolate. The coating for the tablets contains: carnauba wax, hypromellose, polyethylene glycol, polysorbate 80, talc, titanium dioxide, and triethyl citrate. The coating for the 300 mg and 400 mg tablets also contains D&C Yellow No. 10 Aluminum Lake, FD&C Blue No. 1 Aluminum Lake, and FD&C Yellow No. 6 Aluminum Lake.
-
CLINICAL PHARMACOLOGY
Cimetidine competitively inhibits the action of histamine at the histamine H 2 receptors of the parietal cells and thus is a histamine H 2-receptor antagonist.
Cimetidine is not an anticholinergic agent. Studies have shown that cimetidine inhibits both daytime and nocturnal basal gastric acid secretion. Cimetidine also inhibits gastric acid secretion stimulated by food, histamine, pentagastrin, caffeine and insulin.
Antisecretory Activity
1) Acid Secretion
Nocturnal
Cimetidine 800 mg orally at bedtime reduces mean hourly H + activity by greater than 85% over an eight-hour period in duodenal ulcer patients, with no effect on daytime acid secretion. Cimetidine 1600 mg orally at bedtime produces 100% inhibition of mean hourly H + activity over an eight-hour period in duodenal ulcer patients, but also reduces H + activity by 35% for an additional five hours into the following morning. Cimetidine 400 mg twice daily and 300 mg four times daily decrease nocturnal acid secretion in a dose-related manner, i.e., 47% to 83% over a six- to eight-hour period and 54% over a nine-hour period, respectively.
Food stimulated
During the first hour after a standard experimental meal, oral cimetidine 300 mg inhibited gastric acid secretion in duodenal ulcer patients by at least 50%. During the subsequent two hours cimetidine inhibited gastric acid secretion by at least 75%.
The effect of a 300 mg breakfast dose of cimetidine continued for at least four hours and there was partial suppression of the rise in gastric acid secretion following the luncheon meal in duodenal ulcer patients. This suppression of gastric output was enhanced and could be maintained by another 300 mg dose of cimetidine given with lunch.
In another study, cimetidine 300 mg given with the meal increased gastric pH as compared with placebo.
Table 1. Mean Gastric pH Cimetidine Placebo 1 hour 3.5 2.6 2 hours 3.1 1.6 3 hours 3.8 1.9 4 hours 6.1 2.2 24-Hour mean H + activity
Cimetidine 800 mg at bedtime, 400 mg twice daily and 200 mg four times daily all provide a similar, moderate (less than 60%) level of 24-hour acid suppression. However, the 800 mg at bedtime regimen exerts its entire effect on nocturnal acid, and does not affect daytime gastric physiology.
Chemically stimulated
Oral cimetidine significantly inhibited gastric acid secretion stimulated by betazole (an isomer of histamine), pentagastrin, caffeine and insulin as follows:
Table 2 Stimulant Stimulant Dose Cimetidine % Inhibition Betazole 1.5 mg/kg (sc) 300 mg (po) 85% at 2 ½ hours Pentagastrin 6 mcg/kg/hr (iv) 100 mg/hr (iv) 60% at 1 hour Caffeine 5 mg/kg/hr (iv) 300 mg (po) 100% at 1 hour Insulin 0.03 units/kg/hr (iv) 100 mg/hr (iv) 82% at 1 hour When food and betazole were used to stimulate secretion, inhibition of hydrogen ion concentration usually ranged from 45 to 75% and the inhibition of volume ranged from 30 to 65%.
Other
Lower Esophageal Sphincter Pressure and Gastric Emptying
Cimetidine has no effect on lower esophageal sphincter (LES) pressure or the rate of gastric emptying.
Pharmacokinetics
Cimetidine is rapidly absorbed after oral administration and peak levels occur in 45 to 90 minutes. The half-life of cimetidine is approximately 2 hours. Blood concentrations remain above that required to provide 80% inhibition of basal gastric acid secretion for 4 to 5 hours following a dose of 300 mg.
The principal route of excretion of cimetidine is the urine. Following oral administration, the drug is extensively metabolized, the sulfoxide being the major metabolite. Following a single oral dose, 48% of the drug is recovered from the urine after 24 hours as the parent compound.
Clinical Trials
Duodenal Ulcer
Cimetidine has been shown to be effective in the treatment of active duodenal ulcer and, at reduced dosage, in maintenance therapy following healing of active ulcers.
Active duodenal ulcer
Cimetidine accelerates the rate of duodenal ulcer healing. Healing rates reported in U.S. and foreign controlled trials with oral cimetidine are summarized below, beginning with the regimen providing the lowest nocturnal dose.
Table 3. Duodenal Ulcer Healing Rates with Various Oral Cimetidine Dosage Regimens * Regimen 300 mg four times daily 400 mg twice daily 800 mg at bedtime 1600 mg at bedtime - * Averages from controlled clinical trials.
week 4 68% 73% 80% 86% week 6 80% 80% 89% - week 8 - 92% 94% - A U.S., double-blind, placebo-controlled, dose-ranging study demonstrated that all once-daily at bedtime cimetidine regimens were superior to placebo in ulcer healing and that cimetidine 800 mg at bedtime healed 75% of patients at four weeks. The healing rate with 800 mg at bedtime was significantly superior to 400 mg at bedtime (66%) and not significantly different from 1600 mg at bedtime (81%).
In the U.S. dose-ranging trial, over 80% of patients receiving cimetidine 800 mg at bedtime experienced nocturnal pain relief after one day. Relief from daytime pain was reported in 70% of patients after two days. As with ulcer healing, the 800 mg at bedtime dose was superior to 400 mg at bedtime and not different from 1600 mg at bedtime.
In foreign, double-blind studies with cimetidine 800 mg at bedtime, 79 to 85% of patients were healed at four weeks.
While short-term treatment with cimetidine can result in complete healing of the duodenal ulcer, acute therapy will not prevent ulcer recurrence after cimetidine has been discontinued. Some follow-up studies have reported that the rate of recurrence once therapy was discontinued was slightly higher for patients healed on cimetidine than for patients healed on other forms of therapy; however, the cimetidine-treated patients generally had more severe disease.
Maintenance therapy in duodenal ulcer
Treatment with a reduced dose of cimetidine has been proven effective as maintenance therapy following healing of active duodenal ulcers.
In numerous placebo-controlled studies conducted worldwide, the percent of patients with observed ulcers at the end of one year’s therapy with cimetidine 400 mg at bedtime was significantly lower (10% to 45%) than in patients receiving placebo (44% to 70%). Thus, from 55% to 90% of patients were maintained free of observed ulcers at the end of one year with cimetidine 400 mg at bedtime.
Factors such as smoking, duration and severity of disease, gender, and genetic traits may contribute to variations in actual percentages.
Trials of other anti-ulcer therapy, whether placebo-controlled, positive-controlled or open, have demonstrated a range of results similar to that seen with cimetidine.
Active Benign Gastric Ulcer
Cimetidine has been shown to be effective in the short-term treatment of active benign gastric ulcer.
In a multicenter, double-blind U.S. study, patients with endoscopically confirmed benign gastric ulcer were treated with cimetidine 300 mg four times a day or with placebo for six weeks. Patients were limited to those with ulcers ranging from 0.5 to 2.5 cm in size. Endoscopically confirmed healing at six weeks was seen in significantly a more cimetidine-treated patients than in patients receiving the placebo, as shown below:
Table 4. Rate of Endoscopically Confirmed Gastric Ulcer Healing Cimetidine Placebo - * p < 0.05
week 2 14/63 (22%) 7/63 (11%) total at week 6 43/65 (66%) * 30/67 (45%) In a similar multicenter U.S. study of the 800 mg at bedtime oral regimen, the endoscopically confirmed healing rates were:
Table 5. Rate of Endoscopically Confirmed Gastric Ulcer Healing Cimetidine Placebo - * p = 0.005
total at week 6 63/83 (76%) * 44/80 (55%) Similarly, in worldwide double-blind clinical studies, endoscopically evaluated benign gastric ulcer healing rates were consistently higher with cimetidine than with placebo.
Gastroesophageal Reflux Disease
In two multicenter, double-blind, placebo-controlled studies in patients with gastroesophageal reflux disease (GERD) and endoscopically proven erosions and/or ulcers, cimetidine was significantly more effective than placebo in healing lesions. The endoscopically confirmed healing rates were:
Table 6. Rate of Endoscopically Confirmed Healing of Erosions and/or Ulcers Trial Cimetidine (800 mg twice daily) Cimetidine (400 mg four times daily) Placebo p-Value (800 mg twice daily vs placebo) 1 Week 6 45% 52% 26% 0.02 Week 12 60% 66% 42% 0.02 2 Week 6 50% 20% < 0.01 Week 12 67% 36% < 0.01 In these trials cimetidine was superior to placebo by most measures in improving symptoms of day- and night-time heartburn, with many of the differences statistically significant. The four times daily regimen was generally somewhat better than the twice daily regimen where these were compared.
Pathological Hypersecretory Conditions (such as Zollinger-Ellison Syndrome)
Cimetidine significantly inhibited gastric acid secretion and reduced occurrence of diarrhea, anorexia and pain in patients with pathological hypersecretion associated with Zollinger-Ellison Syndrome, systemic mastocytosis and multiple endocrine adenomas. Use of cimetidine was also followed by healing of intractable ulcers.
-
INDICATIONS AND USAGE
Cimetidine tablets are indicated in:
- Short-term treatment of active duodenal ulcer. Most patients heal within 4 weeks and there is rarely reason to use cimetidine at full dosage for longer than 6 to 8 weeks (see DOSAGE AND ADMINISTRATION, Duodenal Ulcer). Concomitant antacids should be given as needed for relief of pain. However, simultaneous administration of oral cimetidine and antacids is not recommended, since antacids have been reported to interfere with the absorption of oral cimetidine.
- Maintenance therapy for duodenal ulcer patients at reduced dosage after healing of active ulcer. Patients have been maintained on continued treatment with cimetidine 400 mg at bedtime for periods of up to five years.
- Short-term treatment of active benign gastric ulcer. There is no information concerning usefulness of treatment periods of longer than 8 weeks.
- Erosive gastroesophageal reflux disease (GERD). Erosive esophagitis diagnosed by endoscopy. Treatment is indicated for 12 weeks for healing of lesions and control of symptoms. The use of cimetidine beyond 12 weeks has not been established [see DOSAGE AND ADMINISTRATION, Erosive Gastroesophageal Reflux ( GERD)].
- The treatment of pathological hypersecretory conditions (i.e., Zollinger-Ellison Syndrome, systemic mastocytosis, multiple endocrine adenomas).
- CONTRAINDICATIONS
-
PRECAUTIONS
General
Rare instances of cardiac arrhythmias and hypotension have been reported following the rapid administration of cimetidine hydrochloride by intravenous bolus.
Symptomatic response to cimetidine therapy does not preclude the presence of a gastric malignancy. There have been rare reports of transient healing of gastric ulcers despite subsequently documented malignancy.
Reversible confusional states (see ADVERSE REACTIONS) have been observed on occasion, predominantly, but not exclusively, in severely ill patients. Advancing age (50 or more years) and preexisting liver and/or renal disease appear to be contributing factors. In some patients these confusional states have been mild and have not required discontinuation of cimetidine therapy. In cases where discontinuation was judged necessary the condition was usually cleared within 3 to 4 days of drug withdrawal.
Drug Interactions
Cimetidine, apparently through an effect on certain microsomal enzyme systems, has been reported to reduce the hepatic metabolism of warfarin-type anticoagulants, phenytoin, propanolol, nifedipine, chlordiazepoxide, diazepam, certain tricyclic antidepressants, lidocaine, theophylline and metronidazole, thereby delaying elimination and increasing blood levels of these drugs.
Clinically significant effects have been reported with the warfarin anticoagulants; therefore, close monitoring of prothrombin time is recommended, and adjustment of the anticoagulant dose may be necessary when cimetidine is administered concomitantly. Interaction with phenytoin, lidocaine and theophylline has also been reported to produce adverse clinical effects.
However, a crossover study in healthy subjects receiving either cimetidine 300 mg four times daily or 800 mg at bedtime concomitantly with a 300 mg twice daily dosage of theophylline extended-release tablets (Theo-Dur ®*) demonstrated less alteration in steady-state theophylline peak serum levels with the 800 mg at bedtime regimen, particularly in subjects aged 54 years and older. Data beyond ten days are not available. (Note: All patients receiving theophylline should be monitored appropriately, regardless of concomitant drug therapy.)
Dosage of the drugs mentioned above and other similarly metabolized drugs, particularly those of low therapeutic ratio or in patients with renal and/or hepatic impairment, may require adjustment when starting or stopping concomitantly administered cimetidine to maintain optimum therapeutic blood levels.
Alteration of pH may affect absorption of certain drugs (e.g., ketoconazole). If these products are needed, they should be given at least 2 hours before cimetidine administration.
Additional clinical experience may reveal other drugs affected by the concomitant administration of cimetidine.
Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 24 month toxicity study conducted in rats, at dose levels of 150, 378 and 950 mg/kg/day (approximately 8 to 48 times the recommended human dose), there was a small increase in the incidence of benign Leydig cell tumors in each dose group; when the combined drug-treated groups and control groups were compared, this increase reached statistical significance. In a subsequent 24 month study, there were no differences between the rats receiving 150 mg/kg/day and the untreated controls. However, a statistically significant increase in benign Leydig cell tumor incidence was seen in the rats that received 378 and 950 mg/kg/day. These tumors were common in control groups as well as treated groups and the difference became apparent only in aged rats.
Cimetidine has demonstrated a weak antiandrogenic effect. In animal studies this was manifested as reduced prostate and seminal vesicle weights. However, there was no impairment of mating performance or fertility, nor any harm to the fetus in these animals at doses 8 to 48 times the full therapeutic dose of cimetidine, as compared with controls. The cases of gynecomoastia seen in patients treated for one month or longer may be related to this effect.
In human studies, cimetidine has been shown to have no effect on spermatogenesis, sperm count, motility, morphology or in vitro fertilizing capacity.
Pregnancy
Teratogenic Effects
Pregnancy category B
Reproduction studies have been performed in rats, rabbits and mice at doses up to 40 times the normal human dose and have revealed no evidence of impaired fertility or harm to the fetus due to cimetidine. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproductive studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Nursing Mothers
Cimetidine is secreted in human milk and, as a general rule, nursing should not be undertaken while a patient is on this drug.
Pediatric Use
Clinical experience in pediatric patients is limited. Therefore, cimetidine therapy cannot be recommended for pediatric patients under 16, unless, in the judgment of the physician, anticipated benefits outweigh the potential risks. In very limited experience, doses of 20 to 40 mg/kg/day have been used.
-
ADVERSE REACTIONS
Adverse effects reported in patients taking cimetidine are described below by body system. Incidence figures of 1 in 100 and greater are generally derived from controlled clinical studies.
CNS
Headaches, ranging from mild to severe, have been reported in 3.5% of 924 patients taking 1600 mg/day, 2.1% of 2,225 patients taking 800 mg/day and 2.3% of 1,897 patients taking placebo. Dizziness and somnolence (usually mild) have been reported in approximately 1 in 100 patients on either 1600 mg/day or 800 mg/day.
Reversible confusional states, e.g., mental confusion, agitation, psychosis, depression, anxiety, hallucinations, disorientation, have been reported predominantly, but not exclusively, in severely ill patients. They have usually developed within 2 to 3 days of initiation of cimetidine therapy and have cleared within 3 to 4 days of discontinuation of the drug.
Endocrine
Gynecomastia has been reported in patients treated for one month or longer. In patients being treated for pathological hypersecretory states, this occurred in about 4% of cases while in all others the incidence was 0.3% to 1% in various studies. No evidence of induced endocrine dysfunction was found, and the condition remained unchanged or returned toward normal with continuing cimetidine treatment.
Reversible impotence has been reported in patients with pathological hypersecretory disorders, e.g., Zollinger-Ellison Syndrome, receiving cimetidine, particularly in high doses for at least 12 months (range 12 to 79 months, mean 38 months). However, in large-scale surveillance studies at regular dosage, the incidence has not exceeded that commonly reported in the general population.
Hematologic
Decreased white blood cell counts in cimetidine-treated patients (approximately 1 per 100,000 patients), including agranulocytosis (approximately 3 per million patients, have been reported, including a few reports of recurrence on rechallenge. Most of these reports were in patients who had serious concomitant illnesses and received drugs and/or treatment known to produce neutropenia. Thrombocytopenia (approximately 3 per million patients) and, very rarely, cases of pancytopenia or aplastic anemia have also been reported. As with some other H 2-receptor antagonists, there have been extremely rare reports of immune hemolytic anemia.
Hepatobiliary
Dose-related increases in serum transaminase have been reported. In most cases they did not progress with continued therapy and returned to normal at the end of therapy. There have been rare reports of cholestatic or mixed cholestatic-hepatocellular effects. These were usually reversible. Because of the predominance of cholestatic features, severe parenchymal injury is considered highly unlikely. However, as in the occasional liver injury with other H 2-receptor antagonists, in exceedingly rare circumstances fatal outcomes have been reported.
There has been reported a single case of biopsy-proven periportal hepatic fibrosis in a patient receiving cimetidine.
Rare cases of pancreatitis, which cleared on withdrawal of the drug, have been reported.
Hypersensitivity
Rare cases of fever and allergic reactions including anaphylaxis and hypersensitivity vasculitis, which cleared on withdrawal of the drug, have been reported.
Renal
Small, possibly dose-related increases in plasma creatinine, presumably due to competition for renal tubular secretion, are not uncommon and do not signify deteriorating renal function. Rare cases of interstitial nephritis and urinary retention, which cleared on withdrawal of the drug, have been reported.
Cardiovascular
Rare cases of bradycardia, tachycardia and A-V heart block have been reported with H 2-receptor antagonists.
Musculoskeletal
There have been rare reports of reversible arthralgia and myalgia; exacerbation of joint symptoms in patients with preexisting arthritis has also been reported. Such symptoms have usually been alleviated by a reduction in cimetidine dosage. Rare cases of polymyositis have been reported, but no causal relationship has been established.
Integumental
Mild rash and, very rarely, cases of severe generalized skin reactions including Stevens-Johnson syndrome, epidermal necrolysis, erythema multiforme, exfoliative dermatitis and generalized exfoliative erythroderma have been reported with H 2-receptor antagonists. Reversible alopecia has been reported very rarely.
Immune Function
There have been extremely rare reports of strongyloidiasis hyperinfection in immunocompromised patients.
Respiratory
A large epidemiological study suggested an increased risk of developing pneumonia in current users of histamine-2-receptor antagonists (H 2RAs) compared to patients who had stopped H 2RA treatment, with an observed adjusted relative risk of 1.63 (95% CI, 1.07 to 2.48). However, a causal relationship between use of H 2RAs and pneumonia has not been established.
-
OVERDOSAGE
Studies in animals indicate that toxic doses are associated with respiratory failure and tachycardia that may be controlled by assisted respiration and the administration of a beta-blocker.
Reported acute ingestions orally of up to 20 grams have been associated with transient adverse effects similar to those encountered in normal clinical experience. The usual measures to remove unabsorbed material from the gastrointestinal tract, clinical monitoring, and supportive therapy should be employed.
There have been reports of severe CNS symptoms, including unresponsiveness, following ingestion of between 20 and 40 grams of cimetidine, and extremely rare reports following concomitant use of multiple CNS active medications and ingestion of cimetidine at doses less than 20 grams. An elderly, terminally ill dehydrated patient with organic brain syndrome receiving concomitant antipsychotic agents and cimetidine 4800 mg intravenously over a 24 hour period experienced mental deterioration with reversal on cimetidine discontinuation.
There have been two deaths in adults who have been reported to ingest over 40 grams orally on a single occasion.
-
DOSAGE AND ADMINISTRATION
Duodenal Ulcer
Active Duodenal Ulcer
Clinical studies have indicated that suppression of nocturnal acid is the most important factor in duodenal ulcer healing (see CLINICAL PHARMACOLOGY, Acid Secretion). This is supported by recent clinical trials (see Clinical Trials, Active duodenal ulcer). Therefore, there is no apparent rationale, except for familiarity with use, for treating with anything other than a once-daily at bedtime oral dosage regimen.
In a U.S. oral dose-ranging study of 400 mg at bedtime, 800 mg at bedtime and 1600 mg at bedtime, a continuous dose response relationship for ulcer healing was demonstrated.
However, 800 mg at bedtime is the dose of choice for most patients, as it provides a high healing rate (the difference between 800 mg at bedtime and 1600 mg at bedtime being small), maximal pain relief, a decreased potential for drug interactions (see PRECAUTIONS, Drug Interactions) and maximal patient convenience. Patients unhealed at four weeks, or those with persistent symptoms, have been shown to benefit from two to four weeks of continued therapy.
It has been shown that patients who both have an endoscopically demonstrated ulcer larger than 1 cm and are also heavy smokers (i.e., smoke one pack of cigarettes or more per day) are more difficult to heal. There is some evidence which suggests that more rapid healing can be achieved in this subpopulation with cimetidine 1600 mg at bedtime. While early pain relief with either 800 mg at bedtime or 1600 mg at bedtime is equivalent in all patients, 1600 mg at bedtime provides an appropriate alternative when it is important to ensure healing within four weeks for this subpopulation. Alternatively, approximately 94% of all patients will also heal in eight weeks with cimetidine 800 mg at bedtime.
Other cimetidine oral regimens in the U.S. which have been shown to be effective are: 300 mg four times daily, with meals and at bedtime, the original regimen with which U.S. physicians have the most experience, and 400 mg twice daily, in the morning and at bedtime (see Clinical Trials, Active duodenal ulcer).
Concomitant antacids should be given as needed for relief of pain. However, simultaneous administration of oral cimetidine and antacids is not recommended, since antacids have been reported to interfere with the absorption of cimetidine.
While healing with cimetidine often occurs during the first week or two, treatment should be continued for 4 to 6 weeks unless healing has been demonstrated by endoscopic examination.
Active Benign Gastric Ulcer
The recommended adult oral dosage for short-term treatment of active benign gastric ulcer is 800 mg at bedtime, or 300 mg four times a day with meals and at bedtime. Controlled clinical studies were limited to six weeks of treatment (see Clinical Trials). 800 mg at bedtime is the preferred regimen for most patients based upon convenience and reduced potential for drug interactions. Symptomatic response to cimetidine dose not preclude the presence of a gastric malignancy. It is important to follow gastric ulcer patients to assure rapid progress to complete healing.
Erosive Gastroesophageal Reflux Disease (GERD)
The recommended adult oral dosage for the treatment of erosive esophagitis that has been diagnosed by endoscopy is 1600 mg daily in divided doses (800 mg twice daily or 400 mg four times daily) for 12 weeks. The use of cimetidine beyond 12 weeks has not been established.
Pathological Hypersecretory Conditions (such as Zollinger-Ellison Syndrome)
Recommended adult oral dosage: 300 mg four times a day with meals at bedtime. In some patients it may be necessary to administer higher doses more frequently. Doses should be adjusted to individual patient needs, but should not usually exceed 2400 mg per day and should continue as long as clinically needed.
Dosage Adjustments for Patients with Impaired Renal Function
Patients with severely impaired renal function have been treated with cimetidine. However, such dosage has been very limited. On the basis of this experience the recommended dosage is 300 mg every 12 hours orally. Should the patient’s condition require, the frequency of dosing may be increased to every 8 hours or even further with caution. In severe renal failure, accumulation may occur and the lower frequency of dosing comparable with an adequate patient response should be used. When liver impairment is also present, further reductions in dosage may be necessary. Hemodialysis reduces the level of circulating cimetidine. Ideally, the dosage schedule should be adjusted so that the timing of a scheduled dose coincides with the end of hemodialysis.
-
HOW SUPPLIED
Cimetidine tablets USP, 300 mg are dark-green, oval-shaped, film-coated tablets, debossed with N192 on one side and 300 on the reverse. They are supplied as follows:
NDC 0093-8192-01 bottles of 100
NDC 0093-8192-05 bottles of 500
Cimetidine tablets USP, 400 mg are dark-green, oval-shaped, film-coated tablets, debossed with N vertical bisect 204 on one side and partial bisect 400 on the reverse. They are supplied as follows:
NDC 0093-8204-01 bottles of 100
NDC 0093-8204-05 bottles of 500
Cimetidine tablets USP, 800 mg are white, oval-shaped, film-coated tablets, debossed with N vertical bisect 305 on one side and partial bisect 800 on the reverse. They are supplied as follows:
NDC 0093-8305-01 bottles of 100
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Dispense in a tight, light-resistant container, as defined in the USP, with a child-resistant closure (as required).
* Theo-Dur ® is a registered trademark of Key Pharmaceuticals Inc.
Manufactured In Canada By:
NOVOPHARM LIMITED
Toronto, Canada M1B 2K9
Manufactured For:
TEVA PHARMACEUTICALS USA
Sellersville, PA 18960
Rev. D 10/2010
- PRINCIPAL DISPLAY PANEL
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
CIMETIDINE
cimetidine tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 10544-627(NDC:0093-8192) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CIMETIDINE (UNII: 80061L1WGD) (CIMETIDINE - UNII:80061L1WGD) CIMETIDINE 300 mg Inactive Ingredients Ingredient Name Strength STARCH, CORN (UNII: O8232NY3SJ) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POVIDONE (UNII: FZ989GH94E) SODIUM LAURYL SULFATE (UNII: 368GB5141J) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) CARNAUBA WAX (UNII: R12CBM0EIZ) HYPROMELLOSES (UNII: 3NXW29V3WO) POLYETHYLENE GLYCOLS (UNII: 3WJQ0SDW1A) POLYSORBATE 80 (UNII: 6OZP39ZG8H) TALC (UNII: 7SEV7J4R1U) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) TRIETHYL CITRATE (UNII: 8Z96QXD6UM) D&C YELLOW NO. 10 (UNII: 35SW5USQ3G) FD&C BLUE NO. 1 (UNII: H3R47K3TBD) FD&C YELLOW NO. 6 (UNII: H77VEI93A8) ALUMINUM OXIDE (UNII: LMI26O6933) Product Characteristics Color green (dark green) Score no score Shape OVAL Size 14mm Flavor Imprint Code N192;300 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 10544-627-30 30 in 1 BOTTLE; Type 0: Not a Combination Product 01/14/2014 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA074151 01/14/2014 CIMETIDINE
cimetidine tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 10544-626(NDC:0093-8204) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CIMETIDINE (UNII: 80061L1WGD) (CIMETIDINE - UNII:80061L1WGD) CIMETIDINE 400 mg Inactive Ingredients Ingredient Name Strength STARCH, CORN (UNII: O8232NY3SJ) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POVIDONE (UNII: FZ989GH94E) SODIUM LAURYL SULFATE (UNII: 368GB5141J) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) CARNAUBA WAX (UNII: R12CBM0EIZ) HYPROMELLOSES (UNII: 3NXW29V3WO) POLYETHYLENE GLYCOLS (UNII: 3WJQ0SDW1A) POLYSORBATE 80 (UNII: 6OZP39ZG8H) TALC (UNII: 7SEV7J4R1U) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) TRIETHYL CITRATE (UNII: 8Z96QXD6UM) D&C YELLOW NO. 10 (UNII: 35SW5USQ3G) FD&C BLUE NO. 1 (UNII: H3R47K3TBD) FD&C YELLOW NO. 6 (UNII: H77VEI93A8) ALUMINUM OXIDE (UNII: LMI26O6933) Product Characteristics Color green (dark green) Score 2 pieces Shape OVAL Size 16mm Flavor Imprint Code N;204;400 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 10544-626-30 30 in 1 BOTTLE; Type 0: Not a Combination Product 01/14/2014 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA074151 01/14/2014 Labeler - Blenheim Pharmacal, Inc. (171434587) Registrant - Blenheim Pharmacal, Inc. (171434587) Establishment Name Address ID/FEI Business Operations Blenheim Pharmacal, Inc. 171434587 repack(10544-627, 10544-626)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.

