VESICARE- solifenacin succinate tablet, film coated
VESIcare by
Drug Labeling and Warnings
VESIcare by is a Prescription medication manufactured, distributed, or labeled by Carilion Materials Management. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use VESIcare® safely and effectively. See full prescribing information for VESIcare.
VESIcare (solifenacin succinate) tablets
Initial U.S. Approval: 2004INDICATIONS AND USAGE
VESIcare is a muscarinic antagonist indicated for the treatment of overactive bladder with symptoms of urge urinary incontinence, urgency, and urinary frequency (1).
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
Tablets: 5 mg and 10 mg (3).
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Angioedema and anaphylactic reactions: Reports of angioedema of the face, lips and/or larynx, in some cases occurring after the first dose, have been described. Anaphylactic reactions have been reported rarely (5.1).
- Urinary Retention: Administer with caution to patients with clinically significant bladder outflow obstruction (5.2).
- Gastrointestinal Disorders: Use with caution in patients with decreased gastrointestinal motility (5.3).
- Central Nervous System Effects: Somnolence has been reported with VESIcare. Advise patients not to drive or operate heavy machinery until they know how VESIcare affects them (5.4).
- Controlled Narrow-Angle Glaucoma: Use with caution in patients being treated for narrow-angle glaucoma (5.5).
- QT Prolongation: Use with caution in patients with a known history of QT prolongation or patients who are taking medications known to prolong the QT interval (5.8).
ADVERSE REACTIONS
The most common adverse reactions (> 4% and > placebo) were dry mouth, and constipation at both 5 mg and 10 mg doses; and urinary tract infection, and blurred vision at the 10 mg dose (6.1).
To report SUSPECTED ADVERSE REACTIONS, contact Astellas Pharma US, Inc at 1-800-727-7003 or FDA at 1-800-FDA-1088 or http://www.fda.gov/medwatch.DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
Pregnancy and Nursing Mothers: VESIcare should be used during pregnancy only if the potential benefit for the mother justifies the potential risk to the fetus. VESIcare should not be administered during nursing (8.1, 8.3).
Pediatric Use: The safety and effectiveness of VESIcare in pediatric patients have not been established (8.4).
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 12/2017
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Dosing Information
2.2 Dose Adjustment in Patients with Renal Impairment
2.3 Dose Adjustment in Patients with Hepatic Impairment
2.4 Dose Adjustment in Patients Taking CYP3A4 Inhibitors
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Angioedema and Anaphylactic Reactions
5.2 Urinary Retention
5.3 Gastrointestinal Disorders
5.4 Central Nervous System Effects
5.5 Controlled Narrow-Angle Glaucoma
5.6 Hepatic Impairment
5.7 Renal Impairment
5.8 Patients with Congenital or Acquired QT Prolongation
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Post-Marketing Experience
7 DRUG INTERACTIONS
7.1 Potent CYP3A4 Inhibitors
7.2 CYP3A4 Inducers
7.3 Drugs Metabolized by Cytochrome P450
7.4 Warfarin
7.5 Oral Contraceptives
7.6 Digoxin
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Labor and Delivery
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
8.8 Gender
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Dosing Information
The recommended dose of VESIcare is 5 mg once daily. If the 5 mg dose is well tolerated, the dose may be increased to 10 mg once daily.
VESIcare should be taken with water and swallowed whole. VESIcare can be administered with or without food.
2.2 Dose Adjustment in Patients with Renal Impairment
For patients with severe renal impairment (CLcr < 30 mL/min), a daily dose of VESIcare greater than 5 mg is not recommended [see Warnings and Precautions (5.7); Use in Specific Populations (8.6)].
2.3 Dose Adjustment in Patients with Hepatic Impairment
For patients with moderate hepatic impairment (Child-Pugh B), a daily dose of VESIcare greater than 5 mg is not recommended. Use of VESIcare in patients with severe hepatic impairment (Child-Pugh C) is not recommended [see Warnings and Precautions (5.6); Use in Specific Populations (8.7)].
2.4 Dose Adjustment in Patients Taking CYP3A4 Inhibitors
When administered with potent CYP3A4 inhibitors such as ketoconazole, a daily dose of VESIcare greater than 5 mg is not recommended [see Drug Interactions (7.1)].
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
VESIcare is contraindicated in patients with:
- urinary retention [see Warnings and Precautions (5.2)],
- gastric retention [see Warnings and Precautions (5.3)],
- uncontrolled narrow-angle glaucoma [see Warnings and Precautions (5.5)], and
- in patients who have demonstrated hypersensitivity to the drug [see Adverse Reactions (6.2)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Angioedema and Anaphylactic Reactions
Angioedema of the face, lips, tongue, and/or larynx have been reported with solifenacin. In some cases angioedema occurred after the first dose. Cases of angioedema have been reported to occur hours after the first dose or after multiple doses. Angioedema associated with upper airway swelling may be life threatening. If involvement of the tongue, hypopharynx, or larynx occurs, solifenacin should be promptly discontinued and appropriate therapy and/or measures necessary to ensure a patent airway should be promptly provided. Anaphylactic reactions have been reported rarely in patients treated with solifenacin succinate. Solifenacin succinate should not be used in patients with a known or suspected hypersensitivity to solifenacin succinate. In patients who develop anaphylactic reactions, solifenacin succinate should be discontinued and appropriate therapy and/or measures should be taken.
5.2 Urinary Retention
VESIcare, like other anticholinergic drugs, should be administered with caution to patients with clinically significant bladder outflow obstruction because of the risk of urinary retention [see Contraindications (4)].
5.3 Gastrointestinal Disorders
VESIcare, like other anticholinergics, should be used with caution in patients with decreased gastrointestinal motility [see Contraindications (4)].
5.4 Central Nervous System Effects
VESIcare is associated with anticholinergic central nervous system (CNS) effects [see Adverse Reactions (6.2)]. A variety of CNS anticholinergic effects have been reported, including headache, confusion, hallucinations and somnolence. Patients should be monitored for signs of anticholinergic CNS effects, particularly after beginning treatment or increasing the dose. Advise patients not to drive or operate heavy machinery until they know how VESIcare affects them. If a patient experiences anticholinergic CNS effects, dose reduction or drug discontinuation should be considered.
5.5 Controlled Narrow-Angle Glaucoma
VESIcare should be used with caution in patients being treated for narrow-angle glaucoma [see Contraindications (4)].
5.6 Hepatic Impairment
VESIcare should be used with caution in patients with hepatic impairment. Doses of VESIcare greater than 5 mg are not recommended in patients with moderate hepatic impairment (Child-Pugh B). VESIcare is not recommended for patients with severe hepatic impairment (Child-Pugh C) [see Dosage and Administration (2.3) and Use in Specific Populations (8.7)].
5.7 Renal Impairment
VESIcare should be used with caution in patients with renal impairment. Doses of VESIcare greater than 5 mg are not recommended in patients with severe renal impairment (CLcr < 30 mL/min) [see Dosage and Administration (2.2) and Use in Specific Populations (8.6)].
5.8 Patients with Congenital or Acquired QT Prolongation
In a study of the effect of solifenacin on the QT interval in 76 healthy women [see Clinical Pharmacology (12.2)] the QT prolonging effect appeared less with solifenacin 10 mg than with 30 mg (three times the maximum recommended dose), and the effect of solifenacin 30 mg did not appear as large as that of the positive control moxifloxacin at its therapeutic dose. This observation should be considered in clinical decisions to prescribe VESIcare for patients with a known history of QT prolongation or patients who are taking medications known to prolong the QT interval.
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
VESIcare has been evaluated for safety in 1811 patients in randomized, placebo-controlled trials. Expected adverse reactions of antimuscarinic agents are dry mouth, constipation, blurred vision (accommodation abnormalities), urinary retention, and dry eyes. The incidence of dry mouth and constipation in patients treated with VESIcare was higher in the 10 mg compared to the 5 mg dose group.
In the four 12-week double-blind clinical trials, severe fecal impaction, colonic obstruction, and intestinal obstruction were reported in one patient each, all in the VESIcare 10 mg group. Angioneurotic edema has been reported in one patient taking VESIcare 5 mg. Compared to 12 weeks of treatment with VESIcare, the incidence and severity of adverse reactions were similar in patients who remained on drug for up to 12 months.
The most frequent adverse reaction leading to study discontinuation was dry mouth (1.5%). Table 1 lists the rates of identified adverse reactions, derived from all reported adverse events, in randomized, placebo-controlled trials at an incidence greater than placebo and in 1% or more of patients treated with VESIcare 5 or 10 mg once daily for up to 12 weeks.
Table 1. Percentages of Patients with Identified Adverse Reactions, Derived from All Adverse Events Exceeding Placebo Rate and Reported by 1% or More Patients for Combined Pivotal Studies Placebo
(%)VESIcare
5 mg
(%)VESIcare
10 mg
(%)Number of Patients
1216
578
1233
GASTROINTESTINAL DISORDERS
Dry Mouth
4.2
10.9
27.6
Constipation
2.9
5.4
13.4
Nausea
2.0
1.7
3.3
Dyspepsia
1.0
1.4
3.9
Abdominal Pain Upper
1.0
1.9
1.2
Vomiting NOS
0.9
0.2
1.1
INFECTIONS AND INFESTATIONS
Urinary Tract Infection NOS
2.8
2.8
4.8
Influenza
1.3
2.2
0.9
Pharyngitis NOS
1.0
0.3
1.1
NERVOUS SYSTEM DISORDERS
Dizziness
1.8
1.9
1.8
EYE DISORDERS
Vision Blurred
1.8
3.8
4.8
Dry Eyes NOS
0.6
0.3
1.6
RENAL AND URINARY DISORDERS
Urinary Retention
0.6
0
1.4
GENERAL DISORDERS AND ADMINISTRATION SITE CONDITIONS
Edema Lower Limb
0.7
0.3
1.1
Fatigue
1.1
1.0
2.1
PSYCHIATRIC DISORDERS
Depression NOS
0.8
1.2
0.8
RESPIRATORY, THORACIC AND MEDIASTINAL DISORDERS
Cough
0.2
0.2
1.1
VASCULAR DISORDERS
Hypertension NOS
0.6
1.4
0.5
6.2 Post-Marketing Experience
Because these spontaneously reported events are from the worldwide postmarketing experience, the frequency of events and the role of solifenacin in their causation cannot be reliably determined.
The following events have been reported in association with solifenacin use in worldwide postmarketing experience:
General: peripheral edema, hypersensitivity reactions, including angioedema with airway obstruction, rash, pruritus, urticaria, and anaphylactic reaction;
Central Nervous: headache, confusion, hallucinations, delirium and somnolence;
Cardiovascular: QT prolongation; Torsade de Pointes, atrial fibrillation, tachycardia, palpitations;
Hepatic: liver disorders mostly characterized by abnormal liver function tests, AST (aspartate aminotransferase), ALT (alanine aminotransferase), GGT (gamma-glutamyl transferase);
Renal: renal impairment;
Metabolism and nutrition disorders: decreased appetite, hyperkalemia;
Dermatologic: exfoliative dermatitis and erythema multiforme;
Eye disorders: glaucoma;
Gastrointestinal disorders: gastroesophageal reflux disease and ileus;
Respiratory, thoracic and mediastinal disorders: dysphonia;
Musculoskeletal and connective tissue disorders: muscular weakness.
-
7 DRUG INTERACTIONS
7.1 Potent CYP3A4 Inhibitors
Following the administration of 10 mg of VESIcare in the presence of 400 mg of ketoconazole, a potent inhibitor of CYP3A4, the mean Cmax and AUC of solifenacin increased by 1.5 and 2.7-fold, respectively. Therefore, it is recommended not to exceed a 5 mg daily dose of VESIcare when administered with therapeutic doses of ketoconazole or other potent CYP3A4 inhibitors [see Dosage and Administration (2.4) and Clinical Pharmacology (12.3)]. The effects of weak or moderate CYP3A4 inhibitors were not examined.
7.2 CYP3A4 Inducers
There were no in vivo studies conducted to evaluate the effect of CYP3A4 inducers on VESIcare. In vitro drug metabolism studies have shown that solifenacin is a substrate of CYP3A4. Therefore, inducers of CYP3A4 may decrease the concentration of solifenacin.
7.3 Drugs Metabolized by Cytochrome P450
At therapeutic concentrations, solifenacin does not inhibit CYP1A1/2, 2C9, 2C19, 2D6, or 3A4 derived from human liver microsomes.
7.4 Warfarin
Solifenacin has no significant effect on the pharmacokinetics of R-warfarin or S-warfarin [see Clinical Pharmacology (12.3)].
7.5 Oral Contraceptives
In the presence of solifenacin there are no significant changes in the plasma concentrations of combined oral contraceptives (ethinyl estradiol/levonorgestrel) [see Clinical Pharmacology (12.3)].
7.6 Digoxin
Solifenacin had no significant effect on the pharmacokinetics of digoxin (0.125 mg/day) in healthy subjects [see Clinical Pharmacology (12.3)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C
There are no adequate and well-controlled studies in pregnant women.
Reproduction studies have been performed in mice, rats and rabbits. After oral administration of 14C-solifenacin succinate to pregnant mice, drug-related material was shown to cross the placental barrier. No embryotoxicity or teratogenicity was observed in mice treated with 1.2 times (30 mg/kg/day) the expected exposure at the maximum recommended human dose [MRHD] of 10 mg. Administration of solifenacin succinate to pregnant mice at 3.6 times and greater (100 mg/kg/day and greater) the exposure at the MRHD, during the major period of organ development resulted in reduced fetal body weights. Administration of 7.9 times (250 mg/kg/day) the MRHD to pregnant mice resulted in an increased incidence of cleft palate. In utero and lactational exposures to maternal doses of solifenacin succinate of 3.6 times (100 mg/kg/day) the MRHD resulted in reduced peripartum and postnatal survival, reductions in body weight gain, and delayed physical development (eye opening and vaginal patency). An increase in the percentage of male offspring was also observed in litters from offspring exposed to maternal doses of 250 mg/kg/day. No embryotoxic effects were observed in rats at up to 50 mg/kg/day (< 1 times the exposure at the MRHD) or in rabbits at up to 1.8 times (50 mg/kg/day) the exposure at the MRHD. Because animal reproduction studies are not always predictive of human response, VESIcare should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
8.2 Labor and Delivery
The effect of VESIcare on labor and delivery in humans has not been studied.
There were no effects on natural delivery in mice treated with 1.2 times (30 mg/kg/day) the expected exposure at the maximum recommended human dose [MRHD] of 10 mg. Administration of solifenacin succinate at 3.6 times (100 mg/kg/day) the exposure at the MRHD or greater increased peripartum pup mortality.
8.3 Nursing Mothers
After oral administration of 14C-solifenacin succinate to lactating mice, radioactivity was detected in maternal milk. There were no adverse observations in mice treated with 1.2 times (30 mg/kg/day) the expected exposure at the maximum recommended human dose [MRHD]. Pups of female mice treated with 3.6 times (100 mg/kg/day) the exposure at the MRHD or greater revealed reduced body weights, postpartum pup mortality or delays in the onset of reflex and physical development during the lactation period.
It is not known whether solifenacin is excreted in human milk. Because many drugs are excreted in human milk, VESIcare should not be administered during nursing. A decision should be made whether to discontinue nursing or to discontinue VESIcare in nursing mothers.
8.4 Pediatric Use
The safety and effectiveness of VESIcare in pediatric patients have not been established.
8.5 Geriatric Use
In placebo-controlled clinical studies, similar safety and effectiveness were observed between older (623 patients ≥ 65 years and 189 patients ≥ 75 years) and younger patients (1188 patients < 65 years) treated with VESIcare.
Multiple dose studies of VESIcare in elderly volunteers (65 to 80 years) showed that Cmax, AUC and t1/2 values were 20-25% higher as compared to the younger volunteers (18 to 55 years).
8.6 Renal Impairment
VESIcare should be used with caution in patients with renal impairment. There is a 2.1-fold increase in AUC and 1.6-fold increase in t1/2 of solifenacin in patients with severe renal impairment. Doses of VESIcare greater than 5 mg are not recommended in patients with severe renal impairment (CLcr < 30 mL/min) [see Warnings and Precautions (5.7); Dosage and Administration (2.2)].
8.7 Hepatic Impairment
VESIcare should be used with caution in patients with reduced hepatic function. There is a 2-fold increase in the t1/2 and 35% increase in AUC of solifenacin in patients with moderate hepatic impairment. Doses of VESIcare greater than 5 mg are not recommended in patients with moderate hepatic impairment (Child-Pugh B). VESIcare is not recommended for patients with severe hepatic impairment (Child-Pugh C) [see Warnings and Precautions (5.6); Dosage and Administration (2.3)].
-
10 OVERDOSAGE
Overdosage with VESIcare can potentially result in severe anticholinergic effects and should be treated accordingly. The highest dose ingested in an accidental overdose of solifenacin succinate was 280 mg in a 5-hour period. This case was associated with mental status changes. Some cases reported a decrease in the level of consciousness.
Intolerable anticholinergic side effects (fixed and dilated pupils, blurred vision, failure of heel-to-toe exam, tremors and dry skin) occurred on day 3 in normal volunteers taking 50 mg daily (5 times the maximum recommended therapeutic dose) and resolved within 7 days following discontinuation of drug.
In the event of overdose with VESIcare, treat with gastric lavage and appropriate supportive measures. ECG monitoring is also recommended.
-
11 DESCRIPTION
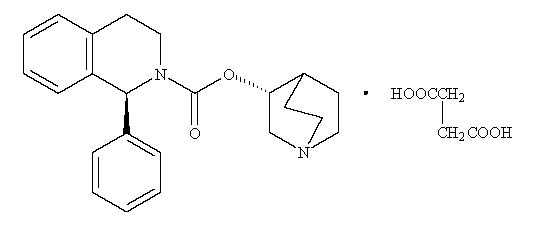
VESIcare (solifenacin succinate) is a muscarinic receptor antagonist. Chemically, solifenacin succinate is butanedioic acid, compounded with (1S)-(3R)-1-azabicyclo[2.2.2]oct-3-yl 3,4-dihydro-1-phenyl-2(1H)-iso-quinolinecarboxylate (1:1) having an empirical formula of C23H26N2O2C4H6O4, and a molecular weight of 480.55. The structural formula of solifenacin succinate is:
Solifenacin succinate is a white to pale-yellowish-white crystal or crystalline powder. It is freely soluble at room temperature in water, glacial acetic acid, dimethyl sulfoxide, and methanol. Each VESIcare tablet contains 5 or 10 mg of solifenacin succinate and is formulated for oral administration. In addition to the active ingredient solifenacin succinate, each VESIcare tablet also contains the following inert ingredients: lactose monohydrate, corn starch, hypromellose 2910, magnesium stearate, talc, polyethylene glycol 8000 and titanium dioxide with yellow ferric oxide (5 mg VESIcare tablet) or red ferric oxide (10 mg VESIcare tablet).
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Solifenacin is a competitive muscarinic receptor antagonist. Muscarinic receptors play an important role in several major cholinergically mediated functions, including contractions of urinary bladder smooth muscle and stimulation of salivary secretion.
12.2 Pharmacodynamics
Cardiac Electrophysiology
The effect of 10 mg and 30 mg solifenacin succinate on the QT interval was evaluated at the time of peak plasma concentration of solifenacin in a multi-dose, randomized, double-blind, placebo and positive-controlled (moxifloxacin 400 mg) trial. Subjects were randomized to one of two treatment groups after receiving placebo and moxifloxacin sequentially. One group (n=51) went on to complete 3 additional sequential periods of dosing with solifenacin 10, 20, and 30 mg while the second group (n=25) in parallel completed a sequence of placebo and moxifloxacin. Study subjects were female volunteers aged 19 to 79 years. The 30 mg dose of solifenacin succinate (three times the highest recommended dose) was chosen for use in this study because this dose results in a solifenacin exposure that covers those observed upon co-administration of 10 mg VESIcare with potent CYP3A4 inhibitors (e.g. ketoconazole, 400 mg). Due to the sequential dose escalating nature of the study, baseline EKG measurements were separated from the final QT assessment (of the 30 mg dose level) by 33 days.
The median difference from baseline in heart rate associated with the 10 and 30 mg doses of solifenacin succinate compared to placebo was -2 and 0 beats/minute, respectively. Because a significant period effect on QTc was observed, the QTc effects were analyzed utilizing the parallel placebo control arm rather than the pre-specified intra-patient analysis. Representative results are shown in Table 2.
Table 2. QTc changes in msec (90%CI) from baseline at Tmax (relative to placebo)* Drug/Dose Fridericia method
(using mean difference)- * Results displayed are those derived from the parallel design portion of the study and represent the comparison of Group 1 to time-matched placebo effects in Group 2
Solifenacin 10 mg
2 (-3,6)
Solifenacin 30 mg
8 (4,13)
Moxifloxacin was included as a positive control in this study and, given the length of the study, its effect on the QT interval was evaluated in 3 different sessions. The placebo subtracted mean changes (90% CI) in QTcF for moxifloxacin in the three sessions were 11 (7, 14), 12 (8, 17), and 16 (12, 21), respectively.
The QT interval prolonging effect appeared greater for the 30 mg compared to the 10 mg dose of solifenacin. Although the effect of the highest solifenacin dose (three times the maximum therapeutic dose) studied did not appear as large as that of the positive control moxifloxacin at its therapeutic dose, the confidence intervals overlapped. This study was not designed to draw direct statistical conclusions between the drugs or the dose levels.
12.3 Pharmacokinetics
Absorption
After oral administration of VESIcare to healthy volunteers, peak plasma levels (Cmax) of solifenacin are reached within 3 to 8 hours after administration, and at steady state ranged from 32.3 to 62.9 ng/mL for the 5 and 10 mg VESIcare tablets, respectively. The absolute bioavailability of solifenacin is approximately 90%, and plasma concentrations of solifenacin are proportional to the dose administered.
Effect of FoodVESIcare may be administered without regard to meals. A single 10 mg dose administration of VESIcare with food increased Cmax and AUC by 4% and 3%, respectively.
DistributionSolifenacin is approximately 98% (in vivo) bound to human plasma proteins, principally to ∝1-acid glycoprotein. Solifenacin is highly distributed to non-CNS tissues, having a mean steady-state volume of distribution of 600L.
MetabolismSolifenacin is extensively metabolized in the liver. The primary pathway for elimination is by way of CYP3A4; however, alternate metabolic pathways exist. The primary metabolic routes of solifenacin are through N-oxidation of the quinuclidin ring and 4R-hydroxylation of tetrahydroisoquinoline ring. One pharmacologically active metabolite (4R-hydroxy solifenacin), occurring at low concentrations and unlikely to contribute significantly to clinical activity, and three pharmacologically inactive metabolites (N-glucuronide and the N-oxide and 4R-hydroxy-N-oxide of solifenacin) have been found in human plasma after oral dosing.
ExcretionFollowing the administration of 10 mg of 14C-solifenacin succinate to healthy volunteers, 69.2% of the radioactivity was recovered in the urine and 22.5% in the feces over 26 days. Less than 15% (as mean value) of the dose was recovered in the urine as intact solifenacin. The major metabolites identified in urine were N-oxide of solifenacin, 4R-hydroxy solifenacin and 4R-hydroxy-N-oxide of solifenacin and in feces 4R-hydroxy solifenacin. The elimination half-life of solifenacin following chronic dosing is approximately 45-68 hours.
Drug Interactions
Potent CYP3A4 InhibitorsIn a crossover study, following blockade of CYP3A4 by coadministration of the potent CYP3A4 inhibitor, ketoconazole 400 mg, once daily for 21 days, the mean Cmax and AUC of solifenacin increased by 1.5 and 2.7-fold, respectively [see Dosage and Administration (2.4) and Drug Interactions (7.1)].
WarfarinIn a crossover study, subjects received a single oral dose of warfarin 25 mg on the 10th day of dosing with either solifenacin 10 mg or matching placebo once daily for 16 days. For R-warfarin when it was coadministered with solifenacin, the mean Cmax increased by 3% and AUC decreased by 2%. For S-warfarin when it was coadministered with solifenacin, the mean Cmax and AUC increased by 5% and 1%, respectively [see Drug Interactions (7.4)].
Oral ContraceptivesIn a crossover study, subjects received 2 cycles of 21 days of oral contraceptives containing 30 ug ethinyl estradiol and 150 ug levonorgestrel. During the second cycle, subjects received additional solifenacin 10 mg or matching placebo once daily for 10 days starting from 12th day of receipt of oral contraceptives. For ethinyl estradiol when it was administered with solifenacin, the mean Cmax and AUC increased by 2% and 3%, respectively. For levonorgestrel when it was administered with solifenacin, the mean Cmax and AUC decreased by 1% [see Drug Interactions (7.5)].
DigoxinIn a crossover study, subjects received digoxin (loading dose of 0.25 mg on day 1, followed by 0.125 mg from days 2 to 8) for 8 days. Consecutively, they received solifenacin 10 mg or matching placebo with digoxin 0.125 mg for additional 10 days. When digoxin was coadministered with solifenacin, the mean Cmax and AUC increased by 13% and 4%, respectively [see Drug Interactions (7.6)].
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No increase in tumors was found following the administration of solifenacin succinate to male and female mice for 104 weeks at doses up to 200 mg/kg/day (5 and 9 times, respectively, of the exposure at the maximum recommended human dose [MRHD] of 10 mg), and male and female rats for 104 weeks at doses up to 20 and 15 mg/kg/day, respectively (< 1 times the exposure at the MRHD).
Solifenacin succinate was not mutagenic in the in vitro Salmonella typhimurium or Escherichia coli microbial mutagenicity test or chromosomal aberration test in human peripheral blood lymphocytes with or without metabolic activation, or in the in vivo micronucleus test in rats.
Solifenacin succinate had no effect on reproductive function, fertility or early embryonic development of the fetus in male and female mice treated with 250 mg/kg/day (13 times the exposure at the MRHD) of solifenacin succinate, and in male rats treated with 50 mg/kg/day (< 1 times the exposure at the MRHD) and female rats treated with 100 mg/kg/day (1.7 times the exposure at the MRHD) of solifenacin succinate.
-
14 CLINICAL STUDIES
VESIcare was evaluated in four twelve-week, double-blind, randomized, placebo-controlled, parallel group, multicenter clinical trials for the treatment of overactive bladder in patients having symptoms of urinary frequency, urgency, and/or urge or mixed incontinence (with a predominance of urge). Entry criteria required that patients have symptoms of overactive bladder for ≥ 3 months duration. These studies involved 3027 patients (1811 on VESIcare and 1216 on placebo), and approximately 90% of these patients completed the 12-week studies. Two of the four studies evaluated the 5 and 10 mg VESIcare doses and the other two evaluated only the 10 mg dose. All patients completing the 12-week studies were eligible to enter an open label, long term extension study and 81% of patients enrolling completed the additional 40-week treatment period. The majority of patients were Caucasian (93%) and female (80%) with a mean age of 58 years.
The primary endpoint in all four trials was the mean change from baseline to 12 weeks in number of micturitions/24 hours. Secondary endpoints included mean change from baseline to 12 weeks in number of incontinence episodes/24 hours, and mean volume voided per micturition. The efficacy of VESIcare was similar across patient age and gender. The mean reduction in the number of micturitions per 24 hours was significantly greater with VESIcare 5 mg (2.3; p < 0.001) and VESIcare 10 mg (2.7; p < 0.001) compared to placebo, (1.4).
The mean reduction in the number of incontinence episodes per 24 hours was significantly greater with VESIcare 5 mg (1.5; p < 0.001) and VESIcare 10 mg (1.8; p < 0.001) treatment groups compared to placebo (1.1). The mean increase in the volume voided per micturition was significantly greater with VESIcare 5 mg (32.3 mL; p < 0.001) and VESIcare 10 mg (42.5 mL; p < 0.001) compared with placebo (8.5 mL).
The results for the primary and secondary endpoints in the four individual 12-week clinical studies of VESIcare are reported in Tables 3 through 6.
Table 3. Mean Change from Baseline to Endpoint for VESIcare (5 mg and 10 mg daily) and Placebo: Study 1 Parameter Placebo
(N=253)
Mean (SE)VESIcare
5 mg
(N=266)
Mean (SE)VESIcare
10 mg
(N=264)
Mean (SE)- * Primary endpoint
- † Secondary endpoint
Urinary Frequency (Number of Micturitions/24 hours)*
Baseline
Reduction
P value vs. placebo
12.2 (0.26)
1.2 (0.21)
12.1 (0.24)
2.2 (0.18)
< 0.001
12.3 (0.24)
2.6 (0.20)
< 0. 001
Number of Incontinence Episodes/24 hours†
Baseline
Reduction
P value vs. placebo
2.7 (0.23)
0.8 (0.18)
2.6 (0.22)
1.4 (0.15)
< 0.01
2.6 (0.23)
1.5 (0.18)
< 0.01
Volume Voided per Micturition [mL]†
Baseline
Increase
P value vs. placebo
143.8 (3.37)
7.4 (2.28)
149.6 (3.35)
32.9 (2.92)
< 0.001
147.2 (3.15)
39.2 (3.11)
< 0.001
Table 4. Mean Change from Baseline to Endpoint for VESIcare (5 mg and 10 mg daily) and Placebo: Study 2 Parameter Placebo
(N=281)
Mean (SE)VESIcare
5 mg
(N=286)
Mean (SE)VESIcare
10 mg
(N=290)
Mean (SE)- * Primary endpoint
- † Secondary endpoint
Urinary Frequency (Number of Micturitions/24 hours)*
Baseline
Reduction
P value vs. placebo
12.3 (0.23)
1.7 (0.19)
12.1 (0.23)
2.4 (0.17)
< 0.001
12.1 (0.21)
2.9 (0.18)
< 0. 001
Number of Incontinence Episodes/24 hours†
Baseline
Reduction
P value vs. placebo
3.2 (0.24)
1.3 (0.19)
2.6 (0.18)
1.6 (0.16)
< 0.01
2.8 (0.20)
1.6 (0.18)
0.016
Volume Voided per Micturition [mL]†
Baseline
Increase
P value vs. placebo
147.2 (3.18)
11.3 (2.52)
148.5 (3.16)
31.8 (2.94)
< 0.001
145.9 (3.42)
36.6 (3.04)
< 0.001
Table 5. Mean Change from Baseline to Endpoint for VESIcare (10 mg daily) and Placebo: Study 3 Parameter Placebo
(N=309)
Mean (SE)VESIcare
10 mg
(N=306)
Mean (SE)- * Primary endpoint
- † Secondary endpoint
Urinary Frequency (Number of Micturitions/24 hours)*
Baseline
Reduction
P value vs. placebo
11.5 (0.18)
1.5 (0.15)
11.7 (0.18)
3.0 (0.15)
< 0. 001
Number of Incontinence Episodes/24 hours†
Baseline
Reduction
P value vs. placebo
3.0 (0.20)
1.1 (0.16)
3.1 (0.22)
2.0 (0.19)
< 0.001
Volume Voided per Micturition [mL]†
Baseline
Increase
P value vs. placebo
190.3 (5.48)
2.7 (3.15)
183.5 (4.97)
47.2 (3.79)
< 0.001
Table 6. Mean Change from Baseline to Endpoint for VESIcare (10 mg daily) and Placebo: Study 4 Parameter Placebo
(N=295)
Mean (SE)VESIcare
10 mg
(N=298)
Mean (SE)- * Primary endpoint
- † Secondary endpoint
Urinary Frequency (Number of Micturitions/24 hours)*
Baseline
Reduction
P value vs. placebo
11.8 (0.18)
1.3 (0.16)
11.5 (0.18)
2.4 (0.15)
< 0. 001
Number of Incontinence Episodes/24 hours†
Baseline
Reduction
P value vs. placebo
2.9 (0.18)
1.2 (0.15)
2.9 (0.17)
2.0 (0.15)
< 0.001
Volume Voided per Micturition [mL]†
Baseline
Increase
P value vs. placebo
175.7 (4.44)
13.0 (3.45)
174.1 (4.15)
46.4 (3.73)
< 0.001
- 16 HOW SUPPLIED/STORAGE AND HANDLING
-
17 PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling (Patient Information).
Patients should be informed that antimuscarinic agents such as VESIcare have been associated with constipation and blurred vision. Patients should be advised to contact their physician if they experience severe abdominal pain or become constipated for 3 or more days. Because VESIcare may cause blurred vision, patients should be advised to exercise caution in decisions to engage in potentially dangerous activities until the drug’s effect on the patient’s vision has been determined. Heat prostration (due to decreased sweating) can occur when anticholinergic drugs, such as VESIcare, are used in a hot environment. Patients should read the patient leaflet entitled “Patient Information VESIcare” before starting therapy with VESIcare.
Patients should be informed that solifenacin may produce angioedema, which could result in life-threatening airway obstruction. Patients should be advised to promptly discontinue solifenacin therapy and seek immediate attention if they experience edema of the tongue or laryngopharynx, or difficulty breathing.
Rx Only
PRODUCT OF IRELAND
Marketed and Distributed by:
Astellas Pharma US, Inc.
Northbrook, IL 60062VESIcare is a registered trademark of Astellas Pharma Inc.
© 2016 Astellas Pharma US, Inc.
Revised: February 2016
16A001-VES
-
FDA Approved Patient Labeling
VESIcare® (VES-ih-care)
(solifenacin succinate)
Tablet
Read the Patient Information that comes with VESIcare before you start taking it and each time you get a refill. There may be new information. This leaflet does not take the place of talking with your doctor about your medical condition or treatment.
What is VESIcare?VESIcare is a prescription medicine for adults used to treat the following symptoms due to a condition called overactive bladder:
- Urge urinary incontinence: a strong need to urinate with leaking or wetting accidents
- Urgency: a strong need to urinate right away
- Frequency: urinating often
It is not known if VESIcare is safe and effective in children.
Who should NOT take VESIcare?Do not take VESIcare if you:
- are not able to empty your bladder (urinary retention)
- have delayed or slow emptying of your stomach (gastric retention)
- have an eye problem called “uncontrolled narrow-angle glaucoma”
-
are allergic to solifenacin succinate or any of the ingredients in VESIcare. See the end of this leaflet for a complete list of ingredients.
What should I tell my doctor before taking VESIcare?
Before you take VESIcare, tell your doctor if you:
- have any stomach or intestinal problems or problems with constipation
- have trouble emptying your bladder or you have a weak urine stream
- have an eye problem called "narrow angle glaucoma"
- have liver problems
- have kidney problems
- have a rare heart problem called "QT prolongation"
- are pregnant or plan to become pregnant. It is not known if VESIcare will harm your unborn baby. Talk to your doctor if you are pregnant or plan to become pregnant.
- are breastfeeding or plan to breastfeed. It is not known if VESIcare passes into your breast milk. You and your doctor should decide if you will take VESIcare or breastfeed. You should not do both.
Tell your doctor about all the medicines you take, including prescription and nonprescription medicines, vitamins, and herbal supplements. VESIcare may affect the way other medicines work, and other medicines may affect how VESIcare works.
How should I take VESIcare?- Take VESIcare exactly as your doctor tells you to take it.
- You should take 1 VESIcare tablet 1 time a day.
- You should take VESIcare with water and swallow the tablet whole.
- You can take VESIcare with or without food.
- If you miss a dose of VESIcare, begin taking VESIcare again the next day. Do not take 2 doses of VESIcare the same day.
-
If you take too much VESIcare, call your doctor or go to the nearest hospital emergency room right away.
What should I avoid while taking VESIcare?
VESIcare can cause blurred vision or drowsiness. Do not drive or operate heavy machinery until you know how VESIcare affects you.
What are the possible side effects of VESIcare?VESIcare may cause serious side effects including:
-
Serious allergic reaction. Stop taking VESIcare and get medical help right away if you have:
- o hives, skin rash or swelling
- o severe itching
- o swelling of your face, mouth or tongue
- o trouble breathing
The most common side effects of VESIcare include:
- dry mouth
- constipation. Call your doctor if you get severe stomach area (abdominal) pain or become constipated for 3 or more days.
- urinary tract infection
- blurred vision
-
heat exhaustion or heat-stroke. This can happen when VESIcare is used in hot environments. Symptoms may include:
- o decreased sweating
- o dizziness
- o tiredness
- o nausea
- o increase in body temperature
Tell your doctor if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of VESIcare. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store VESIcare?- Store VESIcare at 59°F to 86°F (15°C to 30°C). Keep the bottle closed.
- Safely throw away medicine that is out of date or that you no longer need.
Keep VESIcare and all medicines out of the reach of children.
General information about VESIcare.Medicines are sometimes prescribed for purposes other than those listed in Patient Information leaflets. Do not use VESIcare for a condition for which it was not prescribed. Do not give VESIcare to other people, even if they have the same symptoms you have. It may harm them.
This leaflet summarizes the most important information about VESIcare. If you would like more information, talk with your doctor. You can ask your doctor or pharmacist for information about VESIcare that is written for health professionals.
For more information, go to www.vesicare.com or call (800) 727-7003.
What are the ingredients in VESIcare?Active ingredient: solifenacin succinate
Inactive ingredients: lactose monohydrate, corn starch, hypromellose 2910, magnesium stearate, talc, polyethylene glycol 8000 and titanium dioxide with yellow ferric oxide (5 mg VESIcare tablet) or red ferric oxide (10 mg VESIcare tablet)
What is overactive bladder?Overactive bladder occurs when you cannot control your bladder contractions. When these muscle contractions happen too often or cannot be controlled you can get symptoms of overactive bladder, which are urinary frequency, urinary urgency, and urinary incontinence (leakage).
Rx OnlyPRODUCT OF IRELAND
Marketed and Distributed by:
Astellas Pharma US, Inc.
Northbrook, IL 60062VESIcare is a registered trademark of Astellas Pharma Inc.
© 2016 Astellas Pharma US, Inc.
Revised: February 2016
16A001-VES - VESICARE (SOLIFENACIN SUCCINATE) TABLET, FILM COATED
-
INGREDIENTS AND APPEARANCE
VESICARE
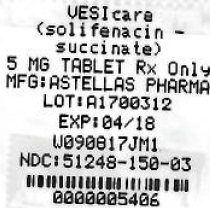
solifenacin succinate tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 68151-5406(NDC:51248-150) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength SOLIFENACIN SUCCINATE (UNII: KKA5DLD701) (SOLIFENACIN - UNII:A8910SQJ1U) SOLIFENACIN SUCCINATE 5 mg Product Characteristics Color yellow (YELLOW) Score no score Shape ROUND (ROUND) Size 8mm Flavor Imprint Code 150 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 68151-5406-1 1 in 1 BLISTER PACK; Type 0: Not a Combination Product 12/28/2017 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021518 01/05/2005 Labeler - Carilion Materials Management (079239644) Establishment Name Address ID/FEI Business Operations Carilion Materials Management 079239644 REPACK(68151-5406)
Trademark Results [VESIcare]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 VESICARE 88833757 not registered Live/Pending |
Astellas Pharma Inc. 2020-03-13 |
 VESICARE 75932952 2535639 Live/Registered |
ASTELLAS PHARMA INC. 2000-03-02 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.