LANREOTIDE ACETATE injection
Lanreotide Acetate by
Drug Labeling and Warnings
Lanreotide Acetate by is a Prescription medication manufactured, distributed, or labeled by Cipla USA Inc., InvaGen Pharmaceuticals, Inc., Pharmathen International S.A.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use LANREOTIDE INJECTION safely and effectively. See full prescribing information for LANREOTIDE INJECTION.
LANREOTIDE injection, for subcutaneous use
Initial U.S. Approval: 2007RECENT MAJOR CHANGES
INDICATIONS AND USAGE
Lanreotide Injection is a somatostatin analog indicated for:
- the long-term treatment of acromegalic patients who have had an inadequate response to or cannot be treated with surgery and/or radiotherapy. (1.1)
- the treatment of adult patients with unresectable, well- or moderately- differentiated, locally advanced or metastatic gastroenteropancreatic neuroendocrine tumors (GEP-NETs) to improve progression-free survival. (1.2)
- the treatment of adults with carcinoid syndrome; when used, it reduces the frequency of short-acting somatostatin analog rescue therapy. (1.3)
DOSAGE AND ADMINISTRATION
Administration (2.1):
- For deep subcutaneous injection only.
- Intended for administration by a healthcare provider.
- Administer in the superior external quadrant of the buttock.
- Alternate injection sites.
Recommended Dosage (2.1)
- Acromegaly: 90 mg every 4 weeks for 3 months. Adjust thereafter based on GH and/or IGF-1 levels. See full prescribing information for titration regimen.
- GEP-NETs: 120 mg every 4 weeks.
- Carcinoid Syndrome: 120 mg every 4 weeks. If patients are already being treated with Lanreotide Injection for GEP-NET, do not administer an additional dose for carcinoid syndrome.
Dosage Adjustment:
DOSAGE FORMS AND STRENGTHS
Injection: 60 mg/0.2 mL, 90 mg/0.3 mL, and 120 mg/0.5 mL of lanreotide in single-dose prefilled syringes (3)
CONTRAINDICATIONS
Hypersensitivity to lanreotide. (4)
WARNINGS AND PRECAUTIONS
- Cholelithiasis and Complications of Cholelithiasis: Monitor periodically. Discontinue if complications of cholthiasis are suspected. Gallstones may occur; consider periodic monitoring. (5.1)
- Hyperglycemia and Hypoglycemia: Glucose monitoring is recommended and antidiabetic treatment adjusted accordingly. (5.2, 7.1)
- Cardiovascular Abnormalities: Decrease in heart rate may occur. Use with caution in at-risk patients. (5.3)
- Thyroid Function Abnormalities: Decreases in thyroid function may occur; perform tests where clinically indicated. (5.4)
- Steatorrhea and Malabsorption of Dietary Fats: New onset steatorrhea, stool discoloration, loose stools, abdominal bloating, and weight loss may occur. If new occurrence or worsening of these symptoms are reported, evaluate for potential pancreatic exocrine insufficiency. (5.6)
ADVERSE REACTIONS
Most common adverse reactions are:
- Acromegaly : (>5%): diarrhea, cholelithiasis, abdominal pain, nausea and injection site reactions. (6.1)
- GEP-NET : (>10%): abdominal pain, musculoskeletal pain, vomiting, headache, injection site reaction, hyperglycemia, hypertension, and cholelithiasis. (6.1)
- Carcinoid Syndrome: (≥5% and at least 5% greater than placebo): headache, dizziness and muscle spasm. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Cipla Ltd. Inc. at 1-866-604-3268 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
DRUG INTERACTIONS
- Cyclosporine: Lanreotide Injection may decrease the absorption of cyclosporine. Dosage adjustment of cyclosporine may be needed. (7.2)
- Bromocriptine: Lanreotide Injection may increase the absorption of bromocriptine. (7.3)
- Bradycardia-Inducing Drugs (e.g., beta-blockers): Lanreotide Injection may decrease heart rate. Dosage adjustment of the coadministered drug may be necessary. (7.3)
USE IN SPECIFIC POPULATIONS
Lactation: Advise women not to breastfeed during treatment and for 6 months after the last dose. (8.2)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 9/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Acromegaly
1.2 Gastroenteropancreatic Neuroendocrine Tumors
1.3 Carcinoid Syndrome
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
2.2 Dosage Adjustment in Renal Impairment
2.3 Dosage Adjustment in Hepatic Impairment
2.4 Important Preparation and Administration Instructions
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Cholelithiasis and Complications of Cholelithiasis
5.2 Hyperglycemia and Hypoglycemia
5.3 Cardiovascular Abnormalities
5.4 Thyroid Function Abnormalities
5.5 Monitoring: Laboratory Tests
5.6 Steatorrhea and Malabsorption of Dietary Fats
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Insulin and Oral Hypoglycemic Drugs
7.2 Cyclosporine
7.3 Bromocriptine
7.4 Bradycardia-Inducing Drugs
7.5 Drug Metabolism Interactions
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.6 Immunogenicity
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Acromegaly
14.2 Gastroenteropancreatic Neuroendocrine Tumors
14.3 Carcinoid Syndrome
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
1.1 Acromegaly
Lanreotide Injection is indicated for the long-term treatment of acromegalic patients who have had an inadequate response to surgery and/or radiotherapy, or for whom surgery and/or radiotherapy is not an option.
The goal of treatment in acromegaly is to reduce growth hormone (GH) and insulin growth factor-1 (IGF-1) levels to normal.
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
Acromegaly
The recommended starting dosage of Lanreotide Injection is 90 mg given via the deep subcutaneous route, at 4-week intervals for 3 months.
After 3 months, the Lanreotide injection dosage may be adjusted as follows:
- GH greater than 1 ng/mL to less than or equal to 2.5 ng/mL, IGF-1 normal, and clinical symptoms controlled: maintain dosage at 90 mg every 4 weeks.
- GH greater than 2.5 ng/mL, IGF-1 elevated, and/or clinical symptoms uncontrolled: increase dosage to 120 mg every 4 weeks.
- GH less than or equal to 1 ng/mL, IGF-1 normal, and clinical symptoms controlled: reduce dosage to 60 mg every 4 weeks.
Thereafter, the dosage should be adjusted according to the response of the patient as judged by a reduction in serum GH and/or IGF-1 levels; and/or changes in symptoms of acromegaly.
Patients who are controlled on Lanreotide Injection 60 or 90 mg may be considered for an extended dosing interval of Lanreotide Injection 120 mg every 6 or 8 weeks. GH and IGF-1 levels should be obtained 6 weeks after this change in dosing regimen to evaluate persistence of patient response.
Continued monitoring of patient response with dosage adjustments for biochemical and clinical symptom control, as necessary, is recommended.
Gastroenteropancreatic Neuroendocrine Tumors (GEP-NETs)
The recommended dosage of Lanreotide Injection is 120 mg administered every 4 weeks by deep subcutaneous injection.
Carcinoid Syndrome
The recommended dosage of Lanreotide Injection is 120 mg administered every 4 weeks by deep subcutaneous injection. If patients are already being treated with Lanreotide Injection for GEP-NETs, do not administer an additional dose for the treatment of carcinoid syndrome.
2.2 Dosage Adjustment in Renal Impairment
Acromegaly
The recommended starting dosage of Lanreotide Injection in acromegalic patients with moderate or severe renal impairment (creatinine clearance (CLcr) less than 60 mL/min) is 60 mg via the deep subcutaneous route at 4-week intervals for 3 months followed by dosage adjustment [see Dosage and Administration (2.1), Use in Specific Populations (8.6)].
2.3 Dosage Adjustment in Hepatic Impairment
Acromegaly
The recommended starting dosage of Lanreotide Injection in acromegalic patients with moderate or severe hepatic impairment (Child-Pugh Class B or C) is 60 mg via the deep subcutaneous route at 4-week intervals for 3 months followed by dosage adjustment [see Dosage and Administration (2.1), Use in Specific Populations (8.7)].
2.4 Important Preparation and Administration Instructions
The following instructions explain how to inject Lanreotide Injection:
- Read all instructions carefully before starting the injection. Follow this procedure exactly, as it may differ from your past experience.
- This is a single-dose pre-filled syringe with a single-use safety needle with a green needle shield (that cannot be removed) in a clear needle cap.
- ALL the medication must be injected SLOWLY over 20 seconds during the use.
- If you drop or damage the device in any way, please call 1-866-604-3268.
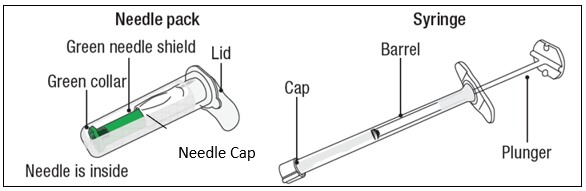
Figure 1
The box includes the following items:
- Sterile needle pack containing Sterile needle
- Sterile Laminated pouch with sterile syringe pre-filled with LANREOTIDE INJECTION
- Instructions for Use Leaflet
- Prescribing Information Leaflet
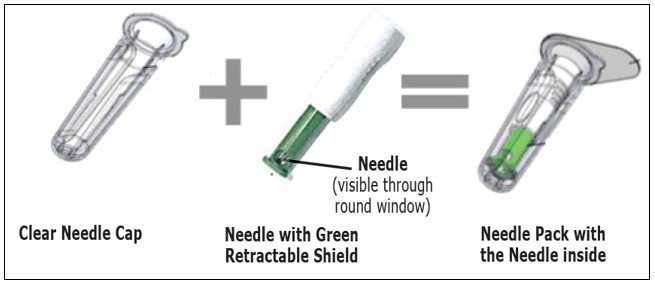
CAUTION
- NEVER TOUCH OR TRY TO OPEN THE GREEN NEEDLE SHIELD throughout the course of operation of the device.
- Green needle shield is NOT a removable cap or cover for the needle.
- Green needle shield will automatically activate once the injection is complete.
- Green needle shield is a self-operating safety lock mechanism.
- Needle is fully covered by green needle shield.
- Needle is visible only through a small window in the green needle shield.
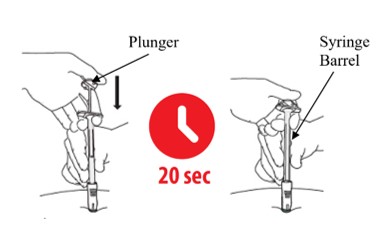
- Inject medication slowly over 20 seconds.
- DO NOT rush the injection.
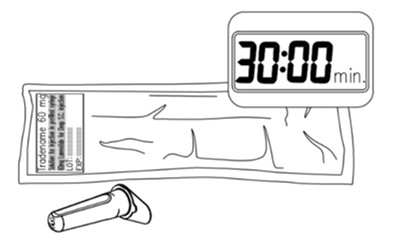
- Remove box from refrigerator 30 minutes prior to injecting.
- Product left in its sealed pouch at room temperature (not to exceed 104°F or 40°C) for up to 72 hours may be returned to the refrigerator for continued storage and usage at a later time.
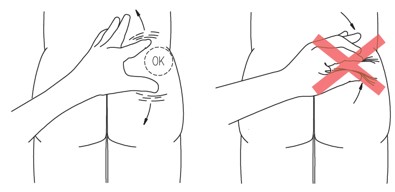
- Stretch out the skin around injection site to make it flat and tight using your thumb and index finger.
- DO NOT pinch the skin around injection site.
A. BEFORE YOU START
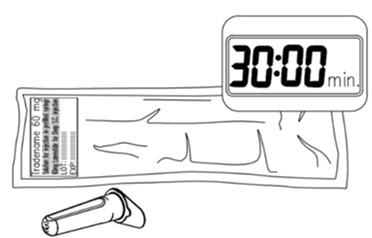
Figure 2
A1. Remove LANREOTIDE INJECTION from the refrigerator 30 minutes prior to injecting (Figure 2). Do not open the sterile pouch yet.
Note: Product left in its sealed pouch at room temperature (not to exceed 104° F or 40 °C) for up to 72 hours may be returned to the refrigerator for continued storage and use at a later time.

Figure 3
A2.Wash your hands with soap and dry your hands thoroughly before starting (Figure 3).
Follow the doctor or institution’s policy on the use of surgical gloves during the procedure 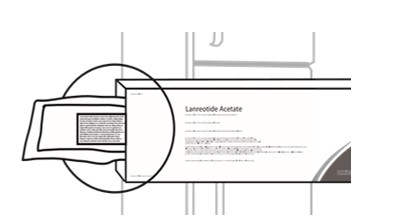
Figure 4
A3. Before opening the sterile pouch, confirm that it is intact, and that the medication has not expired. The Syringe is sterile only if the pouch is sealed and undamaged. Do not use if the pouch is opened, tampered with or damaged. The expiry date is printed on the outer carton and the pouch - Do not use if the medication has expired. (Figure 4). 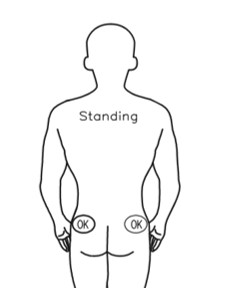
Or
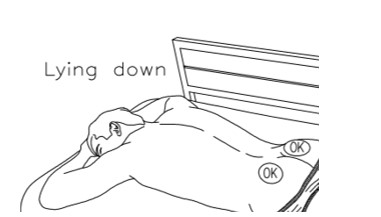
Figure 5
A4. Make sure there is a clean surface for preparation.
Find a clean, comfortable area for the patient to relax during procedure (Figure 5).
It's important that the patient remains as still as possible during the injection.
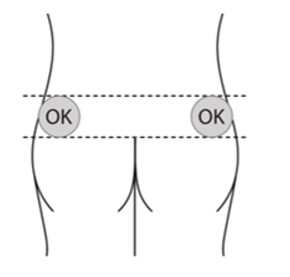
Figure 6
A5.Choose injection site - the sites are upper outer areas of the buttock as shown below
It is very important that you only inject in one of the areas marked OK in the picture (Figure 6).
Alternate the injection site between the right and left side each time an injection of LANREOTIDE INJECTION is administered.
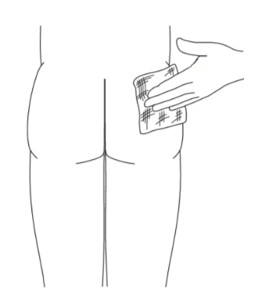
Figure 7
A6.Prepare the injection site by cleaning it with alcohol wipes (Figure 7).
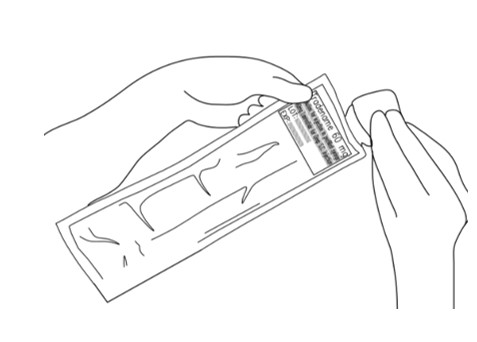
Figure 8
A7. Tear open the sterile pouch and take out the sterile pre-filled syringe (Figure 8).
B. PREPARE THE SYRINGE
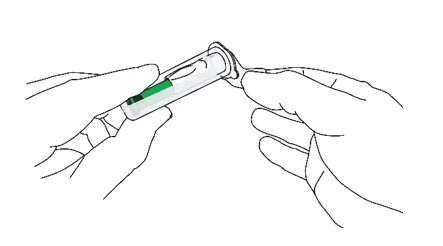
Figure 9
B1: Open the sterile needle cap (Figure 9)
- The needle is sterile only if the needle cap is sealed and undamaged. Do not use if the needle cap is opened, tampered with or damaged.
- Hold the clear needle cap and pull the lid off.
- DO NOT TOUCH THE OPEN END OF THE NEEDLE CAP TO MAINTAIN STERILITY.
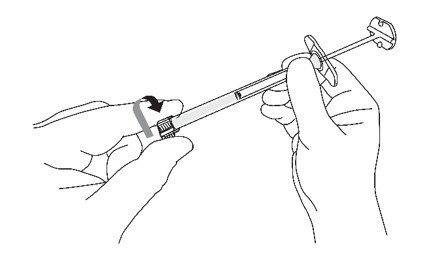
Figure 10
B2: Remove the cap from the sterile syringe (Figure 10)
- With one hand, hold the syringe barrel steady (not the plunger).
- With the other hand, remove the cap by twisting it.
B3: Prepare the assembly (Figure 11)
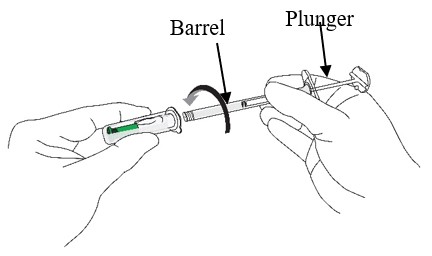
Figure 11
- Hold the needle cap with one hand and the syringe barrel (not the plunger) with the other
- Carefully insert the open end of the syringe into the open end of the needle cap
- Twist the syringe barrel clockwise until it is tight to make sure that the syringe is well connected to the safety needle.
- ENSURE THAT BOTH PARTS OF THE DEVICE (SYRINGE AND NEEDLE) ARE COMPLETELY CONNECTED.
B4: Remove the needle from the needle cap
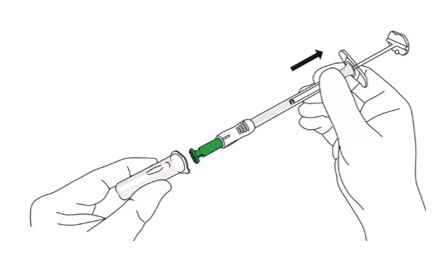
Figure 12
- Hold the syringe barrel (not the plunger).
- Pull the needle straight out from the needle cap without twisting or turning (Figure 12).
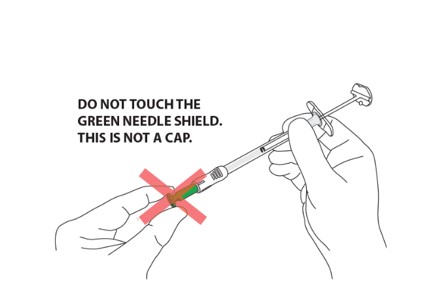
Figure 13
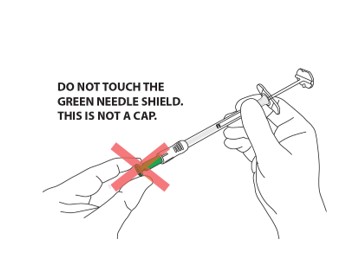
CAUTION: NEVER TOUCH THE GREEN NEEDLE SHIELD. THERE IS A RISK OF NEEDLE STICK INJURY. (Figure 13)
- Green needle shield is a self-operating safety lock mechanism and is not a removable cover or cap for the needle. It will activate once the injection is complete.
- The needle is fully covered by the green shield and is visible only through the small round window at the end of the shield.
C.PERFORM INJECTION
C1: Position the syringe assembly

Figure 14
- Stretch out the skin around the injection site to make it flat and tight using your thumb and index finger. (Figure 14)
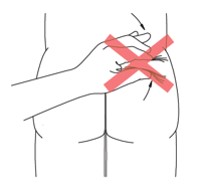
Figure 15
DO NOT pinch the skin(Figure 15) 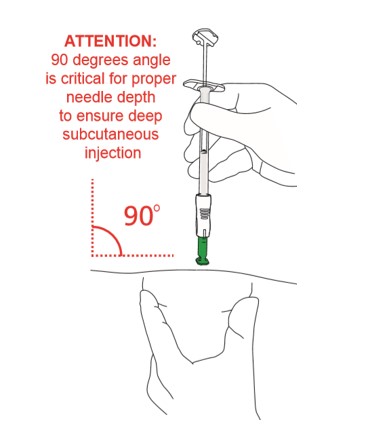
Figure 16
- Hold the assembly by the lower part of the syringe barrel (not the plunger) with your other hand.
- Position the syringe assembly at a 90-degree angle to the skin. The green collar at the bottom of the green shield should be perpendicular to the injection site (Figures 16 and 17)
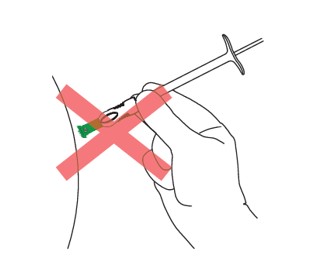
Figure 17
C2: Insert the needle (Figure 18)
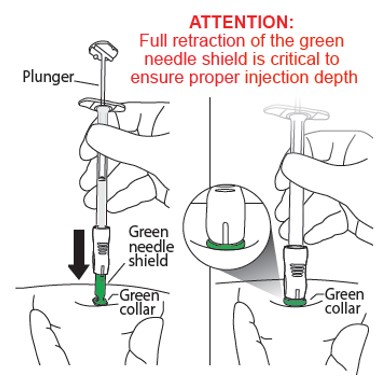
Figure 18
- Holding the skin flat and tight, push the syringe assembly firmly into the skin.
- Do NOT pinch the skin.
- Keep pushing until you reach a “hard stop” and only the green collar at the end of the green needle shield remains visible.
- Do NOT push the plunger yet.
- DO NOT aspirate.
- Keep pressing against the skin.
- During this step you should not see the needle.
C3: Push the top of the plunger (Figure 19)
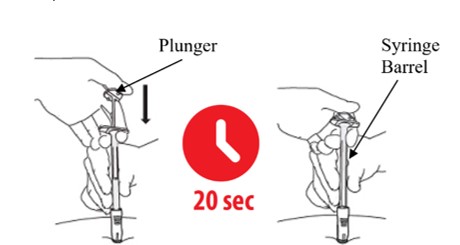
Figure 19
- Keep holding your hand on the syringe barrel to maintain a 90-degree angle throughout the injection.
- While keeping the syringe pressed against the skin, slowly press down the plunger. You may want to use both hands while applying pressure during the injection of drug.
- Continue slowly pushing the plunger over 20 seconds until the Plunger top touches the syringe end .
- DO NOT rush the injection. The medication is thicker and harder to push than you might expect. Pushing the plunger too fast may cause discomfort to the patient.
- While depressing the plunger, slowly count to 20 and CONTINUE STEADY PRESSURE on the plunger. You may find it helpful to say:
a “1 one-thousand”
b “2 one-thousand”
c “3 one-thousand” up to “20 one-thousand”
- During this step, as the needle is lowering, the green needle shield will retract. You should only see the green collar of the green needle shield.
- During this step you should not see the needle.
D. REMOVE AND THROW AWAY THE SYRINGE ASSEMBLY
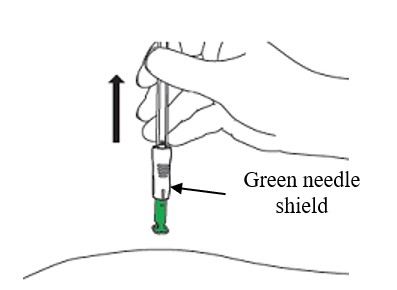
Figure 20
D1: Remove from the skin (Figure 20)
- Lift the syringe straight up and away from the body.
- The green needle shield will return to its original position and will fully cover the needle.
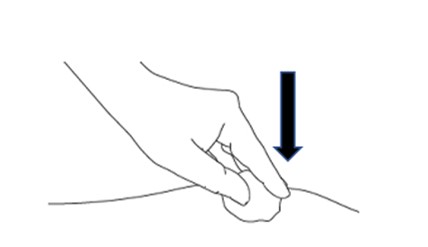
Figure 21
D2: Apply gentle pressure (Figure 21)
- Apply gentle pressure to the injection site with a dry cotton ball or sterile gauze to prevent any bleeding.
- Do NOT rub or massage the injection site after administration.

Figure 22
D3: Check needle (Figure 22)
- Check through the green needle shield’s round windows that the needle was not damaged during administration.
- If any damage or malfunction to the needle is suspected please contact 1-866-604-3268
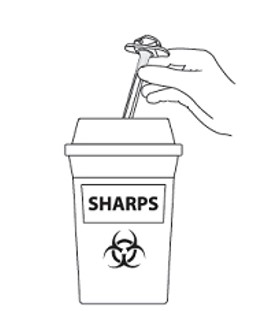
Figure 23
D4: Throw away / Disposal (Figure 23)
- DO NOT remove needle from syringe
- Dispose of complete product in sharps disposal container
- Do not dispose of the syringe or needle in the regular trash.
- The syringe and needle are not reusable.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Lanreotide Injection is contraindicated in patients with history of a hypersensitivity to lanreotide. Allergic reactions (including angioedema and anaphylaxis) have been reported following administration of lanreotide [see Adverse Reactions (6.3)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Cholelithiasis and Complications of Cholelithiasis
Lanreotide Injection may reduce gallbladder motility and lead to gallstone formation; therefore, patients may need to be monitored periodically [see Adverse Reactions (6.1), Clinical Pharmacology (12.2)]. There have been postmarketing reports of cholelithiasis (gallstones) resulting in complications, including cholecystitis, cholangitis, and pancreatitis, and requiring cholecystectomy in patients taking lanreotide. If complications of cholelithiasis are suspected, discontinue Lanreotide Injection and treat appropriately.
5.2 Hyperglycemia and Hypoglycemia
Pharmacological studies in animals and humans show that lanreotide, like somatostatin and other somatostatin analogs, inhibits the secretion of insulin and glucagon. Hence, patients treated with Lanreotide Injection may experience hypoglycemia or hyperglycemia. Blood glucose levels should be monitored when Lanreotide Injection treatment is initiated, or when the dose is altered, and antidiabetic treatment should be adjusted accordingly [see Adverse Reactions (6.1)].
5.3 Cardiovascular Abnormalities
The most common overall cardiac adverse reactions observed in three pooled lanreotide injection cardiac studies in patients with acromegaly were sinus bradycardia (12/217, 5.5%), bradycardia (6/217, 2.8%), and hypertension (12/217, 5.5%) [see Adverse Reactions (6.1)].
In 81 patients with baseline heart rates of 60 beats per minute (bpm) or greater treated with lanreotide in Study 3, the incidence of heart rate less than 60 bpm was 23% (19/81) as compared to 16% (15/94) of placebo treated patients; 10 patients (12%) had documented heart rates less than 60 bpm on more than one visit. The incidence of documented episodes of heart rate less than 50 bpm as well as the incidence of bradycardia reported as an adverse event was 1% in each treatment group. Initiate appropriate medical management in patients who develop symptomatic bradycardia.
In patients without underlying cardiac disease, Lanreotide Injection may lead to a decrease in heart rate without necessarily reaching the threshold of bradycardia. In patients suffering from cardiac disorders prior to Lanreotide Injection treatment, sinus bradycardia may occur. Care should be taken when initiating treatment with Lanreotide Injection in patients with bradycardia.
5.4 Thyroid Function Abnormalities
Slight decreases in thyroid function have been seen during treatment with lanreotide in acromegalic patients, though clinical hypothyroidism is rare (less than 1%). Thyroid function tests are recommended where clinically indicated.
5.5 Monitoring: Laboratory Tests
Acromegaly: Serum GH and IGF-1 levels are useful markers of the disease and the effectiveness of treatment [see Dosage and Administration (2.1)].
5.6 Steatorrhea and Malabsorption of Dietary Fats
New onset steatorrhea, stool discoloration and loose stools have been reported in patients receiving somatostatin analogs, including lanreotide products. Somatostatin analogs reversibly inhibit secretion of pancreatic enzymes and bile acids, which may result in malabsorption of dietary fats and subsequent symptoms of steatorrhea, loose stools, abdominal bloating, and weight loss. If new occurrence or worsening of these symptoms are reported in patients receiving Lanreotide Injection, evaluate patients for potential pancreatic exocrine insufficiency and manage accordingly.
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed in greater detail in other sections of the labeling:
- Cholelithiasis and Complications of Cholelithiasis [see Warnings and Precautions (5.1)]
- Hyperglycemia and Hypoglycemia [see Warnings and Precautions (5.2)]
- Cardiovascular Abnormalities [see Warnings and Precautions (5.3)]
- Thyroid Function Abnormalities [see Warnings and Precautions (5.4)]
- Steatorrhea and Malabsorption of Dietary Fats [see Warnings and Precautions (5.6)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of Lanreotide Injection was established from adequate and well-controlled studies of another lanreotide injection product [see Clinical Studies (14)]. Adverse reactions observed in these adequate and well-controlled studies are described below.
Acromegaly
The data described below reflect exposure to lanreotide injection in 416 acromegalic patients in seven studies. One study was a fixed-dose pharmacokinetic study. The other six studies were open-label or extension studies, one had a placebo-controlled, run-in period, and another had an active control. The population was mainly White (329/353, 93%) with a median age of 53 years of age (range 19 to 84 years). Fifty-four subjects (13%) were age 66 to 74 and 18 subjects (4.3%) were 75 years of age and older.
Patients were evenly matched for sex (205 males and 211 females). The median average monthly dose was 91.2 mg (e.g., 90 mg injected via the deep subcutaneous route every 4 weeks) over 385 days with a median cumulative dose of 1290 mg. Of the patients reporting acromegaly, severity at baseline (N=265), serum GH levels were less than 10 ng/mL for 69% (183/265) of the patients and 10 ng/mL or greater for 31% (82/265) of the patients.
The most commonly reported adverse reactions reported by greater than 5% of patients who received lanreotide (N=416) in the overall pooled safety studies in acromegaly patients were gastrointestinal disorders (diarrhea, abdominal pain, nausea, constipation, flatulence, vomiting, loose stools), cholelithiasis, and injection site reactions.
Tables 1 and 2 present adverse reaction data from clinical studies with lanreotide in acromegalic patients. The tables include data from a single clinical study and pooled data from seven clinical studies.
Adverse Reactions in Parallel Fixed-Dose Phase of Study 1
The incidence of treatment-emergent adverse reactions for lanreotide injection 60, 90, and 120 mg by dose as reported during the first 4 months (fixed-dose phase) of Study 1 [see Clinical Studies (14.1)] are provided in Table 1.
Table 1: Adverse Reactions in Patients with Acromegaly at an Incidence of Greater than 5% with Lanreotide Overall and Occurring at Higher Rate than Placebo: Placebo-Controlled and Fixed-Dose Phase of Study 1 By Dose A patient is counted only once for each body system and preferred term.
Dictionary = WHOART.Placebo-Controlled
Double-Blind Phase
Weeks 0 to 4Fixed-Dose Phase
Double-Blind + Single-Blind
Weeks 0 to 20Body System
Preferred TermPlacebo
(N=25)Lanreotide
Overall
(N=83)Lanreotide
60 mg
(N=34)Lanreotide
90 mg
(N=36)Lanreotide
120 mg
(N=37)Lanreotide
Overall
(N=107)N (%) N (%) N (%) N (%) N (%) N (%) Gastrointestinal System Disorders 1 (4%) 30 (36%) 12 (35%) 21 (58%) 27 (73%) 60 (56%) Diarrhea
Abdominal pain
Flatulence0
1 (4%)
026 (31%)
6 (7%)
5 (6%)9 (26%)
3 (9%)
0 (0%)15 (42%)
6 (17%)
3 (8%)24 (65%)
7 (19%)
5 (14%)48 (45%)
16 (15%)
8 (7%)Application Site Disorders
(Injection site mass/ pain/ reaction/ inflammation)0 (0%) 5 (6%) 3 (9%) 4 (11%) 8 (22%) 15 (14%) Liver and Biliary System Disorders 1 (4%) 3 (4%) 9 (26%) 7 (19%) 4 (11%) 20 (19%) Cholelithiasis 0 2 (2%) 5 (15%) 6 (17%) 3 (8%) 14 (13%) Heart Rate & Rhythm Disorders 0 8 (10%) 7 (21%) 2 (6%) 5 (14%) 14 (13%) Bradycardia 0 7 (8%) 6 (18%) 2 (6%) 2 (5%) 10 (9%) Red Blood Cell Disorders 0 6 (7%) 2 (6%) 5 (14%) 2 (5%) 9 (8%) Anemia 0 6 (7%) 2 (6%) 5 (14%) 2 (5%) 9 (8%) Metabolic & Nutritional Disorders 3 (12%) 13 (16%) 8 (24%) 9 (25%) 4 (11%) 21 (20%) Weight decrease 0 7 (8%) 3 (9%) 4 (11%) 2 (5%) 9 (8%) In Study 1, the adverse reactions of diarrhea, abdominal pain, and flatulence increased in incidence with increasing dose of lanreotide injection .
Adverse Reactions in Long-Term Clinical Trials
Table 2 provides the most common adverse reactions (greater than 5%) that occurred in 416 acromegalic patients treated with lanreotide injection pooled from 7 studies compared to those patients from the 2 efficacy studies (Studies 1 and 2). Patients with elevated GH and IGF-1 levels were either naive to somatostatin analog therapy or had undergone a 3-month washout [see Clinical Studies (14.1)].
Table 2: Adverse Reactions in Lanreotide -Treated Patients with Acromegaly at an Incidence Greater than 5% in Overall Group Versus Adverse Reactions Reported in Studies 1 and 2 Dictionary = MedDRA 7.1 System Organ Class Number and Percentage of Patients Studies 1 & 2
(N=170)Overall Pooled Data
(N=416)N % N % Patients with any Adverse Reactions 157 92 356 86 Gastrointestinal disorders 121 71 235 57 Diarrhea 81 48 155 37 Abdominal pain 34 20 79 19 Nausea 15 9 46 11 Constipation 9 5 33 8 Flatulence 12 7 30 7 Vomiting 8 5 28 7 Loose stools 16 9 23 6 Hepatobiliary disorders 53 31 99 24 Cholelithiasis 45 27 85 20 General disorders and administration site conditions 51 30 91 22 (Injection site pain /mass /induration/
nodule/pruritus)28 17 37 9 Musculoskeletal and connective tissue disorders 44 26 70 17 Arthralgia 17 10 30 7 Nervous system disorders 34 20 80 19 Headache 9 5 30 7 In addition to the adverse reactions listed in Table 2, the following reactions were also seen:
- Sinus bradycardia occurred in 7% (12) of patients in the pooled Study 1 and 2 and in 3% (13) of patients in the overall pooled studies.
- Hypertension occurred in 7% (11) of patients in the pooled Study 1 and 2 and in 5% (20) of patients in the overall pooled studies.
- Anemia occurred in 7% (12) of patients in the pooled Study 1 and 2 and in 3% (14) of patients in the overall pooled studies.
Gastrointestinal Adverse Reactions
In the pooled clinical studies of lanreotide therapy, a variety of gastrointestinal (GI) reactions occurred, the majority of which were mild to moderate in severity. One percent of acromegalic patients treated with lanreotide in the pooled clinical studies discontinued treatment because of gastrointestinal reactions.
Pancreatitis was reported in less than 1% of patients.
Gallbladder Adverse Reactions
In clinical studies involving 416 acromegalic patients treated with lanreotide, cholelithiasis and gallbladder sludge were reported in 20% of the patients. Among 167 acromegalic patients treated with lanreotide who underwent routine evaluation with gallbladder ultrasound, 17% had gallstones at baseline. New cholelithiasis was reported in 12% of patients. Cholelithiasis may be related to dose or duration of exposure [see Warnings and Precautions (5.1)].
Injection Site Reactions
In the pooled clinical studies, injection site pain (4%) and injection site mass (2%) were the most frequently reported local adverse drug reactions that occurred with the administration of lanreotide. In a specific analysis, 20 of 413 patients (5%) presented indurations at the injection site. Injection site adverse reactions were more commonly reported soon after the start of treatment and were less commonly reported as treatment continued. Such adverse reactions were usually mild or moderate but did lead to withdrawal from clinical studies in two subjects.
Glucose Metabolism Adverse Reactions
In the clinical studies in acromegalic patients treated with lanreotide, adverse reactions of dysglycemia (hypoglycemia, hyperglycemia, diabetes) were reported by 14% (47/332) of patients and were considered related to study drug in 7% (24/332) of patients [see Warnings and Precautions (5.2)].
Cardiac Adverse Reactions
In the pooled clinical studies, sinus bradycardia (3%) was the most frequently observed heart rate and rhythm disorder. All other cardiac adverse drug reactions were observed in less than 1% of patients. The relationship of these events to lanreotide could not be established because many of these patients had underlying cardiac disease [see Warnings and Precautions (5.3)].
A comparative echocardiography study of lanreotide and another somatostatin analog demonstrated no difference in the development of new or worsening valvular regurgitation between the 2 treatments over 1 year. The occurrence of clinically significant mitral regurgitation (i.e., moderate or severe in intensity) or of clinically significant aortic regurgitation (i.e., at least mild in intensity) was low in both groups of patients throughout the study.
Other Adverse Reactions
For the most commonly occurring adverse reactions in the pooled analysis, diarrhea, abdominal pain, and cholelithiasis, there was no apparent trend for increasing incidence with age. GI disorders and renal and urinary disorders were more common in patients with documented hepatic impairment; however, the incidence of cholelithiasis was similar between groups.
Gastroenteropancreatic Neuroendocrine Tumors
The safety of lanreotide injection 120 mg for the treatment of patients with gastroenteropancreatic neuroendocrine tumors (GEP-NETs) was evaluated in Study 3, a double-blind, placebo-controlled trial. Patients in Study 3 were randomized to receive lanreotide (N=101) or placebo (N=103) administered by deep subcutaneous injection once every 4 weeks. The data below reflect exposure to lanreotide in 101 patients with GEP-NETs, including 87 patients exposed for at least 6 months and 72 patients exposed for at least 1 year (median duration of exposure 22 months). Patients treated with lanreotide had a median age of 64 years (range 30 to 83 years), 53% were men and 96% were White. Eighty-one percent of patients (83/101) in the lanreotide arm and 82% of patients (82/103) in the placebo arm did not have disease progression within 6 months of enrollment and had not received prior therapy for GEP-NETs. The rates of discontinuation due to treatment-emergent adverse reactions were 5% (5/101 patients) in the lanreotide arm and 3% (3/103 patients) in the placebo arm.
Table 3 compares the adverse reactions reported with an incidence of 5% and greater in patients receiving lanreotide injection 120 mg administered every 4 weeks and reported more commonly than placebo.
Table 3: Adverse Reactions Occurring in 5% and Greater of Lanreotide -Treated Patients with GEP-NETs and at a Higher Rate Than in Placebo -Treated Patients in Study 3 1Includes preferred terms of abdominal pain, abdominal pain upper/lower, abdominal discomfort
2 Includes preferred terms of myalgia, musculoskeletal discomfort, musculoskeletal pain, back pain
3 Includes preferred terms of infusion site extravasation, injection site discomfort, injection site granuloma, injections site hematoma, injection site hemorrhage, injection site induration, injection site mass, injections site nodule, injection site pain, injection site pruritus, injection site rash, injection site reaction, injection site swelling
4 Includes preferred terms of diabetes mellitus, glucose tolerance impaired, hyperglycemia, type 2 diabetes mellitus
5 Includes preferred terms of hypertension, hypertensive crisis
6 Includes preferred terms of depression, depressed mood
* Includes one or more serious adverse events (SAEs) defined as any event that results in death, is life threatening, results in hospitalization or prolongation of hospitalization, results in persistent or significant disability, results in congenital anomaly/birth defect, or may jeopardize the patient and may require medical or surgical intervention to prevent one of the outcomes listed.** Defined as hazardous to well-being, significant impairment of function or incapacitation
Adverse Reaction Lanreotide 120 mg
N=101Placebo
N=103Any (%) Severe** (%) Any (%) Severe** (%) Any Adverse Reactions 88 26 90 31 Abdominal pain1 34* 6* 24* 4 Musculoskeletal pain2 19* 2* 13* 2 Vomiting 19* 2* 9* 2* Headache 16 0 11 1 Injection site reaction3 15 0 7 0 Hyperglycemia4 14* 0 5 0 Hypertension5 14* 1* 5 0 Cholelithiasis 14* 1* 7 0 Dizziness 9 0 2* 0 Depression6 7 0 1 0 Dyspnea 6 0 1 0 Carcinoid Syndrome
The safety of lanreotide injection 120 mg in patients with histopathologically confirmed neuroendocrine tumors and a history of carcinoid syndrome (flushing and/or diarrhea) was evaluated in Study 4, a double-blind, placebo-controlled trial. Patients were randomized to receive lanreotide injection (N=59) or placebo (N=56) administered by deep subcutaneous injection once every 4 weeks. Patients in both arms of Study 4 had access to subcutaneous octreotide as rescue medication for symptom control.
Adverse reactions reported in Study 4 were generally similar to those reported in Study 3 for the GEP-NETs population shown in Table 3 above. Adverse reactions occurring in Study 4 in 5% and greater of lanreotide-treated patients and occurring at least 5% more than in placebo-treated patients were headache (12% vs 5%, respectively), dizziness (7% vs 0%, respectively), and muscle spasm (5% vs 0%, respectively) by week 16.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of lanreotide. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Gastrointestinal disorders: pancreatic exocrine insufficiency
Hepatobiliary: steatorrhea; cholecystitis, cholangitis, pancreatitis, which have sometimes required cholecystectomy
Hypersensitivity: angioedema and anaphylaxis
Injection site reactions: injection site abscess
-
7 DRUG INTERACTIONS
7.1 Insulin and Oral Hypoglycemic Drugs
Lanreotide, like somatostatin and other somatostatin analogs, inhibits the secretion of insulin and glucagon. Therefore, blood glucose levels should be monitored when Lanreotide Injection treatment is initiated or when the dose is altered, and antidiabetic treatment should be adjusted accordingly [see Warnings and Precautions (5.2)].
7.2 Cyclosporine
Concomitant administration of cyclosporine with Lanreotide Injection may decrease the absorption of cyclosporine, and therefore, may necessitate adjustment of cyclosporine dose to maintain therapeutic drug concentrations. [see Clinical Pharmacology (12.3)]
7.3 Bromocriptine
Limited published data indicate that concomitant administration of a somatostatin analog and bromocriptine may increase the absorption of bromocriptine [see Clinical Pharmacology (12.3)].
7.4 Bradycardia-Inducing Drugs
Concomitant administration of bradycardia-inducing drugs (e.g., beta-blockers) may have an additive effect on the reduction of heart rate associated with lanreotide. Dosage adjustments of concomitant drugs may be necessary.
7.5 Drug Metabolism Interactions
The limited published data available indicate that somatostatin analogs may decrease the metabolic clearance of compounds known to be metabolized by cytochrome P450 enzymes, which may be due to the suppression of growth hormone. Since it cannot be excluded that Lanreotide Injection may have this effect, avoid other drugs mainly metabolized by CYP3A4 and which have a low therapeutic index (e.g., quinidine, terfenadine). Drugs metabolized by the liver may be metabolized more slowly during Lanreotide Injection treatment and dose reductions of the concomitantly administered medications should be considered [see Clinical Pharmacology (12.3)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Limited available data based on post-marketing case reports with lanreotide use in pregnant women are not sufficient to determine a drug-associated risk of adverse developmental outcomes. In animal reproduction studies, decreased embryo/fetal survival was observed in pregnant rats and rabbits at subcutaneous doses 5- and 2-times the maximum recommended human dose (MRHD) of 120 mg, respectively (see Data)
The background risk of major birth defects and miscarriage for the indicated populations is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Animal Data
A reproductive study in pregnant rats given 30 mg/kg of lanreotide by subcutaneous injection every 2 weeks (5 times the human dose, based on body surface area comparisons) resulted in decreased embryo/fetal survival. A study in pregnant rabbits given subcutaneous injections of 0.45 mg/kg/day (2 times the human therapeutic exposures at the maximum recommended dose of 120 mg, based on comparisons of relative body surface area) shows decreased fetal survival and increased fetal skeletal/soft tissue abnormalities.
8.2 Lactation
Risk Summary
There is no information available on the presence of lanreotide in human milk, the effects of the drug on the breastfed infant, or the effects of the drug on milk production. Studies show that lanreotide administered subcutaneously passes into the milk of lactating rats; however, due to specifies-specific differences in lactation physiology, animal data may not reliably predict drug levels in human milk. Because of the potential for serious adverse reactions in breastfed infants from Lanreotide Injection, including effects on glucose metabolism and bradycardia, advise women not to breastfeed during treatment with Lanreotide Injection and for 6 months (6 half-lives) following the last dose.
8.3 Females and Males of Reproductive Potential
Infertility
Females
Based on results from animal studies conducted in female rats, Lanreotide Injection may reduce fertility in females of reproductive potential [see Nonclinical Toxicology (13.1)].
8.4 Pediatric Use
The safety and effectiveness of Lanreotide Injection in pediatric patients have not been established.
8.5 Geriatric Use
No overall differences in safety or effectiveness were observed between elderly patients with acromegaly compared with younger patients and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. Studies 3 and 4, conducted in patients with neuroendocrine tumors, did not include sufficient numbers of patients aged 65 and over to determine whether they respond differently from younger patients.
Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
8.6 Renal Impairment
Acromegaly
Lanreotide has been studied in patients with end-stage renal function on dialysis, but has not been studied in patients with mild, moderate, or severe renal impairment. It is recommended that patients with moderate or severe renal impairment receive a starting dose of Lanreotide Injection of 60 mg. Caution should be exercised when considering patients with moderate or severe renal impairment for an extended dosing interval of Lanreotide Injection 120 mg every 6 or 8 weeks [see Dosage and Administration (2.4) and Clinical Pharmacology (12.3)].
Neuroendocrine Tumors (NET) – Gastroenteropancreatic Neuroendocrine Tumors
No effect was observed in total clearance of lanreotide in patients with mild to moderate renal impairment receiving lanreotide injection 120 mg. Patients with severe renal impairment were not studied [see Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
Acromegaly
It is recommended that patients with moderate or severe hepatic impairment receive a starting dose of Lanreotide Injection 60 mg. Caution should be exercised when considering patients with moderate or severe hepatic impairment for an extended dosing interval of Lanreotide Injection 120 mg every 6 or 8 weeks [see Dosage and Administration (2.4) and Clinical Pharmacology (12.3)].
Neuroendocrine Tumors (NET) – Gastroenteropancreatic Neuroendocrine Tumors
Lanreotide has not been studied in patients with hepatic impairment.
-
11 DESCRIPTION
Lanreotide Injection 60 mg/0.2 mL, 90 mg/0.3 mL, and 120 mg/0.5 mL is a prolonged-release formulation for deep subcutaneous injection. It contains the drug substance lanreotide acetate, a synthetic octapeptide with a biological activity similar to naturally occurring somatostatin, water for injection and acetic acid (for pH adjustment).
Lanreotide Injection is available as sterile, ready-to-use, single-dose prefilled syringes containing lanreotide acetate supersaturated bulk solution of 24.6% w/w lanreotide base.
Each syringe contains: Lanreotide
Injection
60 mg/0.2 mLLanreotide
Injection
90 mg/0.3 mLLanreotide
Injection
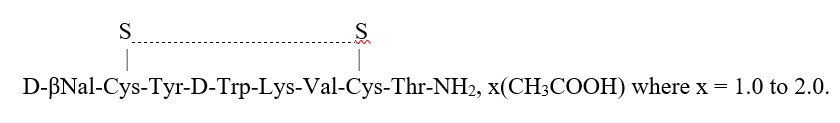
120 mg/0.5 mLLanreotide acetate 89.9 mg 123.2 mg 156.6 mg Acetic Acid q.s. q.s. q.s. Water for injection 236.4 mg 324.1 mg 411.6 mg Total Weight 328.9 mg 450.9 mg 572.8 mg Lanreotide acetate is a synthetic cyclical octapeptide analog of the natural hormone, somatostatin. Lanreotide acetate is chemically known as [cyclo S-S]-3-(2-naphthyl)-D alanyl-L-cysteinyl-L-tyrosyl-D-tryptophyl-L-lysyl-L-valyl-L-cysteinyl-L-threoninamide, acetate salt. Its molecular weight is 1096.34 (base) and its amino acid sequence is:
The Lanreotide Injection in the prefilled syringe is a white to pale yellow, semi-solid formulation.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Lanreotide, the active component of Lanreotide Injection, is an octapeptide analog of natural somatostatin. The mechanism of action of lanreotide is believed to be similar to that of natural somatostatin.
12.2 Pharmacodynamics
Lanreotide has a high affinity for human somatostatin receptors (SSTR) 2 and 5 and a reduced binding affinity for human SSTR1, 3, and 4. Activity at human SSTR2 and 5 is the primary mechanism believed responsible for GH inhibition. Like somatostatin, lanreotide is an inhibitor of various endocrine, neuroendocrine, exocrine, and paracrine functions.
The primary pharmacodynamic effect of lanreotide is a reduction of GH and/or IGF-1 levels enabling normalization of levels in acromegalic patients [see Clinical Studies (14.1)]. In acromegalic patients, lanreotide reduces GH levels in a dose-dependent way. After a single injection of lanreotide, plasma GH levels fall rapidly and are maintained for at least 28 days.
In Study 4, patients with carcinoid syndrome treated with lanreotide injection 120 mg every 4 weeks had reduced levels of urinary 5-hydroxyindoleacetic acid (5-HIAA) compared with placebo [see Clinical Studies (14.3)].
Lanreotide inhibits the basal secretion of motilin, gastric inhibitory peptide, and pancreatic polypeptide, but has no significant effect on the secretion of secretin. Lanreotide inhibits postprandial secretion of pancreatic polypeptide, gastrin, and cholecystokinin (CCK). In healthy subjects, lanreotide produces a reduction and a delay in postprandial insulin secretion, resulting in transient, mild glucose intolerance.
Lanreotide inhibits meal-stimulated pancreatic secretions, and reduces duodenal bicarbonate and amylase concentrations, and produces a transient reduction in gastric acidity.
Lanreotide has been shown to inhibit gallbladder contractility and bile secretion in healthy subjects [see Warnings and Precautions (5.1)].
In healthy subjects, lanreotide inhibits meal-induced increases in superior mesenteric artery and portal venous blood flow but has no effect on basal or meal-stimulated renal blood flow. Lanreotide has no effect on renal plasma flow or renal vascular resistance. However, a transient decrease in glomerular filtration rate (GFR) and filtration fraction has been observed after a single injection of lanreotide.
In healthy subjects, non-significant reductions in glucagon levels were seen after lanreotide administration. In diabetic non-acromegalic subjects receiving a continuous infusion (21-day) of lanreotide, serum glucose concentrations were temporarily decreased by 20% to 30% after the start and end of the infusion. Serum glucose concentrations returned to normal levels within 24 hours. A significant decrease in insulin concentrations was recorded between baseline and Day 1 only [see Warnings and Precautions (5.2)].
Lanreotide inhibits the nocturnal increase in thyroid-stimulating hormone (TSH) seen in healthy subjects. Lanreotide reduces prolactin levels in acromegalic patients treated on a long-term basis [see Warnings and Precautions (5.4)].
12.3 Pharmacokinetics
Lanreotide Injection is thought to form a drug depot at the injection site due to the interaction of the formulation with physiological fluids. The most likely mechanism of drug release is a passive diffusion of the precipitated drug from the depot towards the surrounding tissues, followed by the absorption to the bloodstream.
After a single, deep subcutaneous administration, the mean absolute bioavailability of lanreotide in healthy subjects was 73.4, 69.0, and 78.4% for the 60 mg, 90 mg, and 120 mg doses, respectively. Mean Cmax values ranged from 4.3 to 8.4 ng/mL during the first day. Single-dose linearity was demonstrated with respect to AUC and Cmax and showed high inter-subject variability. Lanreotide showed sustained release of lanreotide with a half-life of 23 to 30 days. Mean serum concentrations were > 1 ng/mL throughout 28 days at 90 mg and 120 mg and > 0.9 ng/mL at 60 mg.
In studies evaluating excretion, <5% of lanreotide was excreted in urine and less than 0.5% was recovered unchanged in feces, indicative of some biliary excretion.
Acromegaly
In a repeat-dose administration pharmacokinetics (PK) study in acromegalic patients, rapid initial release was seen giving peak levels during the first day after administration. At doses of lanreotide between 60 and 120 mg, linear pharmacokinetics were observed in acromegalic patients. At steady state, mean Cmax values were 3.8 ± 0.5, 5.7 ± 1.7, and 7.7 ± 2.5 ng/mL, increasing linearly with dose. The mean accumulation ratio index was 2.7, which is in line with the range of values for the half-life of lanreotide. The steady- state trough serum lanreotide concentrations in patients receiving lanreotide every 28 days were 1.8 ± 0.3; 2.5 ± 0.9 and 3.8 ± 1.0 ng/mL at 60 mg, 90 mg, and 120 mg doses, respectively. A limited initial burst effect and a low peak-to-trough fluctuation (81% to 108%) of the serum concentration at the plateau were observed.
For the same doses, similar values were obtained in clinical studies after at least four administrations (2.3 ± 0.9, 3.2 ± 1.1, and 4.0 ± 1.4 ng/mL, respectively).
Pharmacokinetic data from studies evaluating extended dosing use of lanreotide injection 120 mg demonstrated mean steady-state, Cmin values between 1.6 and 2.3 ng/mL for the 8- and 6-week treatment interval, respectively.
Gastroenteropancreatic Neuroendocrine Tumors
In patients with GEP-NETs treated with lanreotide 120 mg every 4 weeks, steady state concentrations were reached after 4 to 5 injections and the mean trough serum lanreotide concentrations at steady state ranged from 5.3 to 8.6 ng/mL.
Specific Populations
Lanreotide Injection has not been studied in specific populations. However, the pharmacokinetics of lanreotide in renal impaired, hepatic impaired, and geriatric subjects were evaluated after IV administration of lanreotide immediate release formulation (IRF) at 7 mcg/kg dose.
Geriatric Patients
Studies in healthy elderly subjects showed an 85% increase in half-life and a 65% increase in mean residence time (MRT) of lanreotide compared to those seen in healthy young subjects; however, there was no change in either AUC or Cmax of lanreotide in elderly as compared to healthy young subjects. Age has no effect on clearance of lanreotide based on population PK analysis in patients with GEP-NET which included 122 patients aged 65 to 85 years with neuroendocrine tumors.
Patients with Renal Impairment
An approximate 2-fold decrease in total serum clearance of lanreotide, with a consequent 2fold increase in half-life and AUC was observed [see Dosage and Administration (2.2) and Use in Specific Populations (8.6)].
Mild (CLcr 60-89 mL/min) or moderate (CLcr 30-59 mL/min) renal impairment has no effect on clearance of lanreotide in patients with GEP-NET based on population PK analysis which included 106 patients with mild and 59 patients with moderate renal impairment treated with lanreotide. GEP-NET patients with severe renal impairment (CLcr < 30 mL/min) were not studied.
Patients with Hepatic Impairment
In subjects with moderate to severe hepatic impairment, a 30% reduction in clearance of lanreotide was observed [see Dosage and Administration (2.3) and Use in Specific Populations (8.7)].
The effect of hepatic impairment on clearance of lanreotide has not been studied in patients with GEP-NET.
12.6 Immunogenicity
The observed incidence of anti-drug antibodies is highly dependent on the sensitivity and specificity of the assay. Differences in assay methods preclude meaningful comparisons of the incidence of anti-drug antibodies in the studies described below with the incidence of anti-drug antibodies in other studies, including those of Lanreotide Injection or of other lanreotide products.
Acromegaly
Laboratory investigations of acromegalic patients treated with lanreotide injection in clinical studies show that the percentage of patients with putative antibodies at any time point after treatment is low (less than 1% to 4% of patients in specific studies whose antibodies were tested). The antibodies did not appear to affect the efficacy or safety of lanreotide injection.
GEP-NETs
In Study 3, development of anti-lanreotide antibodies was assessed using a radioimmunoprecipitation assay. In patients with GEP-NETs receiving lanreotide injection, the incidence of anti-lanreotide antibodies was 4% (3 of 82) at 24 weeks, 10% (7 of 67) at 48 weeks, 11% (6 of 57) at 72 weeks, and 10% (8 of 84) at 96 weeks. Assessment for neutralizing antibodies was not conducted.
Carcinoid Syndrome
In Study 4, less than 2% (2 of 108) of the patients treated with lanreotide injection developed anti-lanreotide antibodies.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Standard lifetime carcinogenicity bioassays were conducted in mice and rats. Mice were given daily subcutaneous doses of lanreotide at 0.5, 1.5, 5, 10, and 30 mg/kg for 104 weeks. Cutaneous and subcutaneous tumors of fibrous connective tissues at the injection sites were observed at the high dose of 30 mg/kg/day. Fibrosarcomas in both genders and malignant fibrous histiocytomas were observed in males at 30 mg/kg/day resulting in exposures 3 times higher than the clinical therapeutic exposure at the maximum therapeutic dose of 120 mg given by monthly subcutaneous injection based on the AUC values. Rats were given daily subcutaneous doses of lanreotide at 0.1, 0.2, and 0.5 mg/kg for 104 weeks. Increased cutaneous and subcutaneous tumors of fibrous connective tissues at the injection sites were observed at the dose of 0.5 mg/kg/day resulting in exposures less than the clinical therapeutic exposure at 120 mg given by monthly subcutaneous injection. The increased incidence of injection site tumors in rodents is likely related to the increased dosing frequency (daily) in animals compared to monthly dosing in humans and therefore may not be clinically relevant.
Lanreotide was not genotoxic in tests for gene mutations in a bacterial mutagenicity (Ames) assay, or mouse lymphoma cell assay with or without metabolic activation. Lanreotide was not genotoxic in tests for the detection of chromosomal aberrations in a human lymphocyte and in vivo mouse micronucleus assay.
In a fertility study conducted with lanreotide in rats, reduced female fecundity was observed at estimated exposure corresponding to approximately 10-fold the plasma exposure at the MRHD of 120 mg. The fertility of male rats was unaffected by the treatment up to an estimated exposure corresponding to approximately 11-fold the plasma exposure at the MRHD of 120 mg.
-
14 CLINICAL STUDIES
The safety and efficacy of Lanreotide Injection have been established based on adequate and well-controlled studies of another lanreotide injection product. Below is a description of the results of these adequate and well-controlled studies of lanreotide injection in these conditions.
14.1 Acromegaly
The effect of lanreotide on reducing GH and IGF-levels and control of symptoms in patients with acromegaly was studied in 2 long-term, multiple-dose, randomized, multicenter studies.
Study 1
This 1-year study included a 4-week, double-blind, placebo-controlled phase; a 16-week single-blind, fixed-dose phase; and a 32-week, open-label, dose-titration phase. Patients with active acromegaly, based on biochemical tests and medical history, entered a 12-week washout period if there was previous treatment with a somatostatin analog or a dopaminergic agonist.
Upon entry, patients were randomly allocated to receive a single, deep subcutaneous injection of lanreotide 60, 90, or 120 mg or placebo. Four weeks later, patients entered a fixed-dose phase where they received 4 injections of lanreotide followed by a dose-titration phase of 8 injections for a total of 13 injections over 52 weeks (including the placebo phase). Injections were given at 4-week intervals. During the dose-titration phase of the study, the dose was titrated twice (every fourth injection), as needed, according to individual GH and IGF-1 levels.
A total of 108 patients (51 males, 57 females) were enrolled in the initial placebo-controlled phase of the study. Half (54/108) of the patients had never been treated with a somatostatin analog or dopamine agonist or had stopped treatment for at least 3 months prior to their participation in the study, and were required to have a mean GH level greater than 5 ng/mL at their first visit. The other half of the patients had received prior treatment with a somatostatin analog or a dopamine agonist before study entry and at study entry were required to have a mean GH concentration greater than 3 ng/mL and at least a 100% increase in mean GH concentration after washout of medication.
One hundred and seven (107) patients completed the placebo-controlled phase, 105 patients completed the fixed-dose phase, and 99 patients completed the dose-titration phase. Patients not completing withdrew due to adverse events (5) or lack of efficacy (4).
In the double-blind phase of Study 1, a total of 52 (63%) of the 83 lanreotide-treated patients had a greater than 50% decrease in mean GH from baseline to Week 4, including 52%, 44%, and 90% of patients in the 60, 90, and 120 mg groups, respectively, compared to placebo (0%, 0/25). In the fixed-dose phase at Week 16, 72% of all 107 lanreotide-treated patients had a decrease from baseline in mean GH of greater than 50%, including 68% (23/34), 64% (23/36), and 84% (31/37) of patients in the 60, 90, and 120 mg lanreotide treatment groups, respectively. Efficacy achieved in the first 16 weeks was maintained for the duration of the study (see Table 4).
Table 4: Overall Efficacy Results Based on GH and IGF-1 Levels by Treatment Phase in Patients with Acromegaly in Study 1 1n=105, 2n=102, 3Age-adjusted
*Last Observation Carried ForwardBaseline
N=107Before Titration 1
(16 weeks)
N=107Before Titration 2
(32 weeks)
N=105Last Value Available*
N=107IGH ≤5.0 ng/mL Number of Responders (%) 20
(19%)72
(67%)76
(72%)74
(69%)≤2.5 ng/mL Number of Responders (%) 0
(0%)52
(49%)59
(56%)55
(51%)≤1.0 ng/mL Number of Responders (%) 0
(0%)15
(14%)18
(17%)17
(16%)Median GH ng/mL 10.27 2.53 2.20 2.43 GH Reduction Median % Reduction - 75.5 78.2 75.5 IGF-1 Normal3 Number of Responders (%) 9
(8%)58
(54%)57
(54%)62
(58%)Median IGF-1 ng/mL 775.0 332.01 316.52 326.0 IGF-1 Reduction Median % Reduction -- 52.31 54.52 55.4 IGF-1 Normal3 + GH ≤2.5 ng/mL Number of Responders (%) 0
(0%)41
(38%)46
(44%)44
(41%)Study 2
This was a 48-week, open-label, uncontrolled, multicenter study that enrolled patients who had an IGF-1 concentration 1.3 times or greater than the upper limit of the normal age- adjusted range. Patients receiving treatment with a somatostatin analog (other than lanreotide) or a dopaminergic agonist had to attain this IGF-1 concentration after a washout period of up to 3 months.
Patients were initially enrolled in a 4-month, fixed-dose phase where they received 4 deep subcutaneous injections of lanreotide 90 mg, at 4-week intervals. Patients then entered a dose-titration phase where the dose of lanreotide was adjusted based on GH and IGF-1 levels at the beginning of the dose-titration phase and, if necessary, again after another 4 injections. Patients titrated up to the maximum dose (120 mg) were not allowed to titrate down again.
A total of 63 patients (38 males, 25 females) entered the fixed-dose phase of the trial and 57 patients completed 48 weeks of treatment. Six patients withdrew due to adverse reactions (3), other reasons (2), or lack of efficacy (1).
After 48 weeks of treatment with lanreotide at 4-week intervals, 43% (27/63) of the acromegalic patients in this study achieved normal age-adjusted IGF-1 concentrations. Mean IGF-1 concentrations after treatment completion were 1.3 ± 0.7 times the upper limit of normal compared to 2.5 ± 1.1 times the upper limit of normal at baseline.
The reduction in IGF-1 concentrations over time correlated with a corresponding marked decrease in mean GH concentrations. The proportion of patients with mean GH concentrations less than 2.5 ng/mL increased significantly from 35% to 77% after the fixed- dose phase and 85% at the end of the study. At the end of treatment, 24/63 (38%) of patients had both normal IGF-1 concentrations and a GH concentration of less than or equal to 2.5 ng/mL (see Table 5) and 17/63 patients (27%) had both normal IGF-1 concentrations and a GH concentration of less than 1 ng/mL.
Table 5: Overall Efficacy Results Based on GH and IGF-1 Levels by Treatment Phase in Patients with Acromegaly in Study 2 1Age-adjusted, 2N= 62,
* Last Observation Carried ForwardBaseline
N=63Before Titration 1
(12 wks)
N=63Before Titration 2
(28 wks)
N=59Last Value Available*
N=63IGF-1 Normal1 Number of Responders (%) 0
(0%)17
(27%)22
(37%)27
(43%)Median IGF-1 ng/mL 689.0 382.0 334.0 317.0 IGF-1 Reduction Median % Reduction -- 41.0 51.0 50.3 GH ≤5.0 ng/mL Number of Responders (%) 40
(64%)59
(94%)57
(97%)62
(98%)≤2.5 ng/mL Number of Responders (%) 21
(33%)47
(75%)47
(80%)54
(86%)≤1.0 ng/mL Number of Responders (%) 8
(13%)19
(30%)18
(31%)28
(44%)Median GH ng/Ml 3.71 1.65 1.48 1.13 GH Reduction Median % Reduction -- 63.2 66.7 78.62 IGF-1 normal1 + GH ≤2.5 ng/mL Number of Responders (%) 0
(0%)14
(22%)20
(34%)24
(38%)Examination of age and gender subgroups did not identify differences in response to lanreotide among these subgroups. The limited number of patients in the different racial subgroups did not raise any concerns regarding efficacy of lanreotide in these subgroups.
14.2 Gastroenteropancreatic Neuroendocrine Tumors
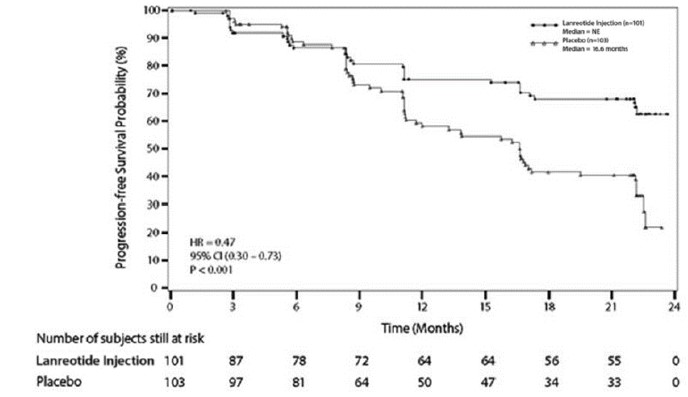
The efficacy of lanreotide was established in a multicenter, randomized, double-blind, placebo-controlled trial of 204 patients with unresectable, well or moderately differentiated, metastatic or locally advanced, GEP-NETs. Patients were required to have non-functioning tumors without hormone-related symptoms. Patients were randomized 1:1 to receive lanreotide injection 120 mg (n=101) or placebo (n=103) every 4 weeks until disease progression, unacceptable toxicity, or a maximum of 96 weeks of treatment. Randomization was stratified by the presence or absence of prior therapy and by the presence or absence of disease progression within 6 months of enrollment. The major efficacy outcome measure was progression-free survival (PFS), defined as time to disease progression as assessed by central independent radiological review using the Response Evaluation Criteria in Solid Tumors (RECIST 1.0) or death.
The median patient age was 63 years (range 30 to 92 years) and 95% were White. Disease progression was present in nine of 204 patients (4.4%) in the 6 months prior to enrollment and 29 patients (14%) received prior chemotherapy. Ninety-one patients (45%) had primary sites of disease in the pancreas, with the remainder originating in the midgut (35%), hindgut (7%), or unknown primary location (13%). The majority (69%) of the study population had grade 1 tumors. Baseline prognostic characteristics were similar between arms with one exception: there were 39% of patients in the lanreotide arm and 27% of patients in the placebo arm who had hepatic involvement by tumor of greater than 25%.
Patients in the lanreotide arm had a statistically significant improvement in PFS compared to patients receiving placebo (see Table 6 and Figure 1).
Table 6: Efficacy Results in Patients with GEP-NETs in Study 3 1NE = not reached at 22 months
2Hazard Ratio is derived from a Cox stratified proportional hazards modelLanreotide Placebo n=101 n=103 Number of Events (%) 32 (31.7%) 60 (58.3%) Median PFS (months)(95% CI) NE1 (NE, NE) 16.6 (11.2, 22.1) HR (95% CI) 0.47 (0.30, 0.73)2 Log-rank p-value <0.001 Figure 1: Kaplan-Meier Curves of Progression-Free Survival in Patients with GEP-NETs in Study 3
14.3 Carcinoid Syndrome
Study 4 was a multicenter, randomized, 16-week, double-blind, placebo-controlled trial in 115 patients with histopathologically-confirmed neuroendocrine tumors and a history of carcinoid syndrome (flushing and/or diarrhea) who were treatment naïve or stable on another somatostatin analog and who were randomized 1:1 to receive lanreotide injection 120 mg (n=59) or placebo (n=56) by deep subcutaneous injection every 4 weeks. Patients were instructed to self-administer a short-acting somatostatin analog (octreotide) as rescue medication as needed for symptom control. The use of rescue therapy and the severity and frequency of diarrhea and flushing symptoms were reported daily in electronic patient diaries. During the 16 week double-blind phase, the primary efficacy outcome measure was the percentage of days in which patients administered at least one injection of rescue medication for symptom control. Average daily frequencies of diarrhea and flushing events were assessed secondarily.
The patient population had a mean age of 59 years (range 27 to 85 years), 58% were female and 77% were White. Patients in the lanreotide arm experienced 15% fewer days on rescue medication compared to patients in the placebo arm (34% vs. 49% of days, respectively; p=0.02). The average daily frequencies of diarrhea and flushing events in patients treated with lanreotide (and rescue medication) were numerically lower relative to patients treated with placebo (and rescue medication), but were not statistically significantly different via hierarchical testing.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Lanreotide Injection is supplied in strengths of 60 mg/0.2 mL, 90 mg/0.3 mL, and 120 mg/0.5 mL lanreotide as a white to pale yellow, semi-solid formulation in a single-dose, sterile, prefilled, ready-to-use, polypropylene syringe and a safety needle device. The safety needle device is a sterile, single use needle system consisting of a needle (1.2 mm x 20 mm, stainless steel) held in protective plastic safety housing.
The single-dose prefilled syringe is contained in a plastic tray and is packed in a triple-layered aluminium pouch. The sterile safety needle is co-packaged along with the sealed aluminium pouch in the kit carton box and is attached to the former at the point of use.
NDC: 69097-880-67 60 mg/0.2 mL lanreotide, sterile, prefilled syringe
NDC: 69097-890-67 90 mg/0.3 mL lanreotide, sterile, prefilled syringe
NDC: 69097-870-67 120 mg/0.5 mL lanreotide, sterile, prefilled syringe
Storage and Handling
Store Lanreotide Injection in the refrigerator at 2°C to 8°C (36°F to 46°F). Protect from light.
Store in the original package.
Product left in its sealed pouch at room temperature (not to exceed 104°F or 40°C) for up to 72 hours may be returned to the refrigerator for continued storage and usage at a later time.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Hypersensitivity Reactions
Advise patients to immediately contact their healthcare provider if they experience serious hypersensitivity reactions, such as angioedema or anaphylaxis [see Contraindications (4)].
Cholelithiasis and Complications of Cholelithiasis
Advise patients to contact their healthcare provider if they experience signs or symptoms of gallstones (cholelithiasis) or complications of gallstones (e.g., cholecystitis, cholangitis, or pancreatitis) [see Warnings and Precautions (5.1)].
Hyperglycemia and Hypoglycemia
Advise patients to immediately contact their healthcare provider if they experience signs or symptoms of hyper- or hypoglycemia [see Warnings and Precautions (5.2)].
Cardiovascular Abnormalities
Advise patients to immediately contact their healthcare provider if they experience bradycardia [see Warnings and Precautions (5.3)].
Thyroid Function Abnormalities
Advise patients to contact their healthcare provider if they experience signs or symptoms of hypothyroidism [see Warnings and Precautions (5.4)].
Laboratory Tests
Advise patients with acromegaly that response to Lanreotide Injection should be monitored by periodic measurements of GH and IGF-1 levels, with a goal of decreasing these levels to the normal range [see Dosage and Administration (2.1)].
Steatorrhea and Malabsorption of Dietary Fats
Advise patients to contact their healthcare provider if they experience new or worsening symptoms of steatorrhea, stool discoloration, loose stools, abdominal bloating, and weight loss [see Warnings and Precautions (5.6)].
Lactation
Advise women not to breastfeed during treatment with Lanreotide Injection and for 6 months after the last dose [see Use in Specific Populations (8.2)].
Infertility
Advise females of reproductive potential of the potential for reduced fertility from Lanreotide Injection [see Use in Specific Populations (8.3)].
Manufactured by:
Pharmathen International S.A.
Industrial Park Sapes,
Rodopi Prefecture, Block No 5,
Rodopi 69300,
GreeceManufactured for:
Cipla USA Inc.
10 Independence Boulevard, Suite 300
Warren, NJ 07059 -
PATIENT PACKAGE INSERT
This Patient Information has been approved by the U.S. Food and Drug Administration. Revised: 09/2024 PATIENT INFORMATION
Lanreotide (lan-REE-oh-tide) Injection
for subcutaneous useRead this Patient Information before you receive your first Lanreotide injection and before each injection. There may be new information. This information does not take the place of talking with your healthcare provider about your medical condition or your treatment.
What is Lanreotide injection?
Lanreotide injection is a prescription medicine used for:
- the long-term treatment of people with acromegaly when:
⚬ surgery or radiotherapy have not worked well enough or
⚬ they are not able to have surgery or radiotherapy.
- the treatment of adults with a type of cancer known as neuroendocrine tumors, from the gastrointestinal tract or the pancreas (GEP-NETs) that has spread or cannot be removed by surgery.
- the treatment of adults with carcinoid syndrome to reduce the need for the use of short-acting somatostatin medicine
It is not known if Lanreotide injection is safe and effective in children.
Who should not receive Lanreotide injection?
Do not receive Lanreotide injection if you are allergic to lanreotide.
What should I tell my healthcare provider before receiving Lanreotide injection?
Before you receive Lanreotide injection, tell your healthcare provider about all of your medical conditions, including if you:
- have gallbladder problems.
- have diabetes.
- have heart problems.
- have thyroid problems.
- have kidney problems.
- have liver problems.
- are pregnant or plan to become pregnant. It is not known if Lanreotide injection will harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if Lanreotide injection passes into your breast milk. You should not breastfeed if you receive Lanreotide injection and for 6 months after your last dose of Lanreotide injection.
- are a person who can become pregnant. Lanreotide injection may affect fertility and may affect your ability to become pregnant. Talk to your healthcare provider if this is a concern for you.
Tell your healthcare provider about all the medicines you take, including prescription and over the-counter medicines, vitamins, and herbal supplements. Lanreotide injection and other medicines may affect each other, causing side effects. Lanreotide injection may affect the way other medicines work, and other medicines may affect how Lanreotide injection works. Your dose of Lanreotide injection or your other medicines may need to be changed.
Especially tell your healthcare provider if you take:
- insulin or other diabetes medicines.
- cyclosporine (Gengraf, Neoral, or Sandimmune).
- medicines that lower your heart rate such as beta blockers.
How will I receive Lanreotide injection?
- You will receive a Lanreotide injection dose every 4 weeks in your healthcare provider’s office.
- Your healthcare provider may change your dose of Lanreotide injection or the length of time between your injections. Your healthcare provider will tell you how long you need to receive Lanreotide injection.
- Lanreotide injection is injected deep under the skin of the upper outer area of your buttock. Your injection site should change (alternate) between your right and left buttock from one injection of Lanreotide injection to the next.
- During your treatment with Lanreotide injection for acromegaly, your healthcare provider may do certain blood tests to see if Lanreotide injection is working.
What should I avoid while receiving Lanreotide injection?
Lanreotide injection can cause dizziness. If you have dizziness, do not drive a car or operate machinery.
What are the possible side effects of Lanreotide injection?
Lanreotide injection may cause serious side effects, including:
- Gallstones (cholelithiasis) and complications that can happen if you have gallstones. Gallstones are a serious but common side effect in people who take Lanreotide injection and have acromegaly and GEP-NET. Your healthcare provider may check your gallbladder before and during treatment with Lanreotide injection. Possible complications of gallstones include inflammation and infection of the gallbladder and pancreatitis. Tell your healthcare provider if you get any symptoms of gallstones, including:
⚬ sudden pain in your upper right stomach area (abdomen)
⚬ yellowing of your skin and whites of your eyes
⚬ nausea⚬ sudden pain in your right shoulder between your shoulder blades
⚬ fever with chills- Changes in your blood sugar (high blood sugar or low blood sugar). If you have diabetes, test your blood sugar as your healthcare provider tells you to. Your healthcare provider may change your dose of diabetes medicine especially when you first start receiving Lanreotide injection or if your dose of Lanreotide injection changes. High blood sugar is a common side effect in people with GEP-NET.
Tell your healthcare provider right away if you have any signs or symptoms of high blood sugar or low blood sugar.
Signs and symptoms of high blood sugar may include:
⚬ increased thirst
⚬ increased appetite
⚬ nausea⚬ weakness or tiredness
⚬ urinating more often than normal
⚬ your breath smells like fruitSigns and symptoms of low blood sugar may include:
⚬ dizziness or lightheadedness
⚬ sweating
⚬ confusion
⚬ headache⚬ blurred vision
⚬ slurred speech
⚬ shakiness⚬ fast heartbeat
⚬ irritability or mood changes
⚬ hunger- Slow heart rate. Tell your healthcare provider right away if you have slowing of your heart rate or if you have symptoms of a slow heart rate, including:
⚬ dizziness or lightheadedness
⚬ fainting or near-fainting⚬ chest pain
⚬ shortness of breath⚬ confusion or memory
⚬ weakness, extreme tiredness- High blood pressure. High blood pressure can happen in people who receive Lanreotide injection and is a common side effect in people with GEP-NET.
- Changes in thyroid function. Lanreotide injection can cause the thyroid gland to not make enough thyroid hormones that the body needs (hypothyroidism) in people who have acromegaly. Tell your healthcare provider if you have signs and symptoms of low thyroid hormones levels, including:
⚬ fatigue
⚬ weight gain
⚬ a puffy face⚬ being cold all of the time
⚬ constipation
⚬ dry skin⚬ thinning, dry hair
⚬ decreased sweating
⚬ depression- Fatty stool. Lanreotide injection may cause your body to have issues absorbing dietary fats. Tell your healthcare provider if you have any new or worsening symptoms including fatty or oily stools, changes in the color of your stools, loose stools, stomach (abdominal) bloating or weight loss.
The most common side effects of Lanreotide injection in people with acromegaly include:
diarrhea
stomach area (abdominal) painnausea
pain, itching, or a lump at the injection siteThe most common side effects of Lanreotide injection in people with GEP-NET include:
stomach area (abdominal) pain
muscle and joint aches
vomitingheadache
pain, itching, or a lump at the injection siteThe most common side effects of Lanreotide Injection in people with carcinoid syndrome include:
headache dizziness muscle spasm
Tell your healthcare provider right away if you have signs of an allergic reaction after receiving Lanreotide injection, including:
swelling of your face, lips, mouth or tongue
breathing problems
fainting, dizziness, feeling lightheaded (low blood pressure)
itchingflushing or redness of your skin
rash
hivesThese are not all the possible side effects of Lanreotide injection. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
General information about the safe and effective use of Lanreotide injection.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not receive Lanreotide injection for a condition for which it was not prescribed. You can ask your healthcare provider for information about Lanreotide injection that is written for health professionals.
What are the ingredients in Lanreotide injection?
Active ingredient: lanreotide acetate
Inactive ingredients: water for injection and acetic acid (for pH adjustment)
Manufactured by: Pharmathen International S.A., Rodopi, Greece
Manufactured for: Cipla USA, Inc., 10 Independence Boulevard, Suite 300, Warren, NJ 07059
SAP Code: 99353071
For more information, go to www.ciplausa.com or call 1-886-604-3268.
-
PRINCIPAL DISPLAY PANEL - 60 mg/0.2 mL Carton Label
NDC: 69097-880-67 Rx Only
Lanreotide Injection
60 mg*/0.2 mL
For deep subcutaneous injection
Single dose only. Discard unused portion.
Lanreotide Injection should be administered by a healthcare professional.
Leave at room temperature for 30 minutes before administration.
CONTENTS: This box contains one (1) pre-filled syringe and one (1) safety needle.
Cipla
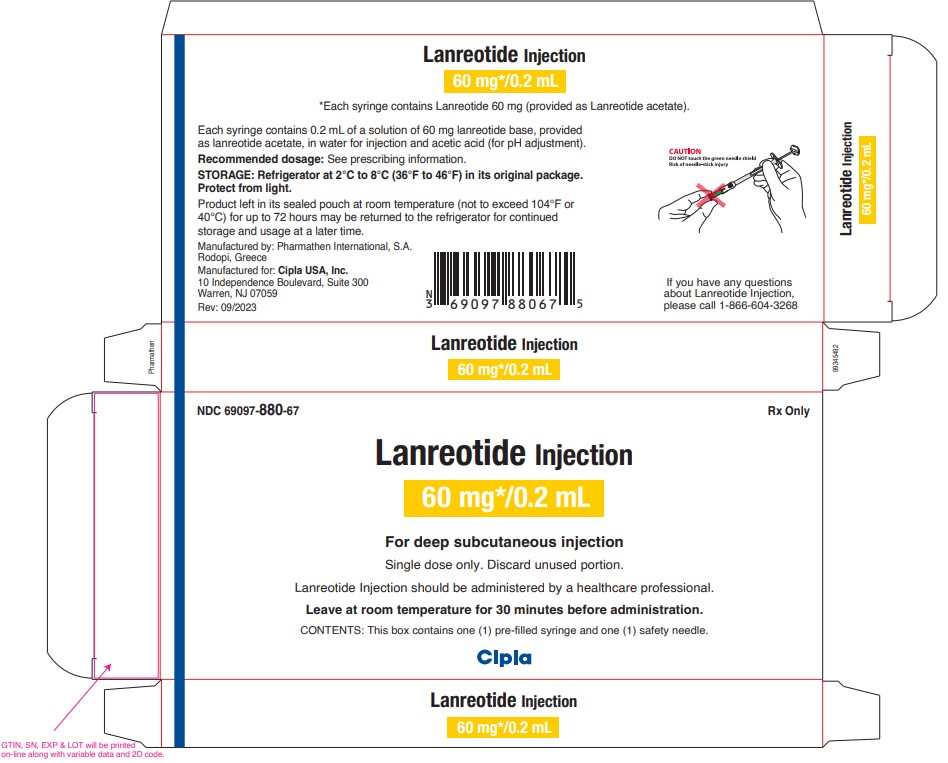
-
PRINCIPAL DISPLAY PANEL - 90 mg/0.3 mL Carton Label
NDC: 69097-890-67 Rx Only
Lanreotide Injection
90 mg*/0.3 mL
For deep subcutaneous injection
Single dose only. Discard unused portion.
Lanreotide Injection should be administered by a healthcare professional.
Leave at room temperature for 30 minutes before administration.
CONTENTS: This box contains one (1) pre-filled syringe and one (1) safety needle.
Cipla
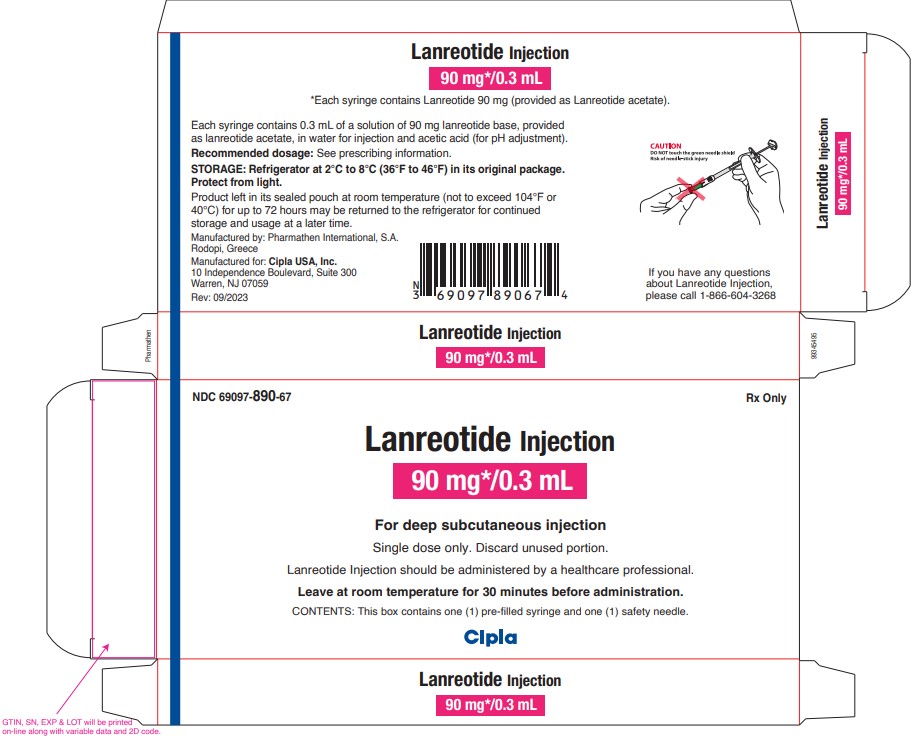
-
PRINCIPAL DISPLAY PANEL - 120 mg/0.5 mL Carton Label
NDC: 69097-870-67 Rx Only
Lanreotide Injection
120 mg*/0.5 mL
For deep subcutaneous injection
Single dose only. Discard unused portion.
Lanreotide Injection should be administered by a healthcare professional.
Leave at room temperature for 30 minutes before administration.
CONTENTS: This box contains one (1) pre-filled syringe and one (1) safety needle.
Cipla
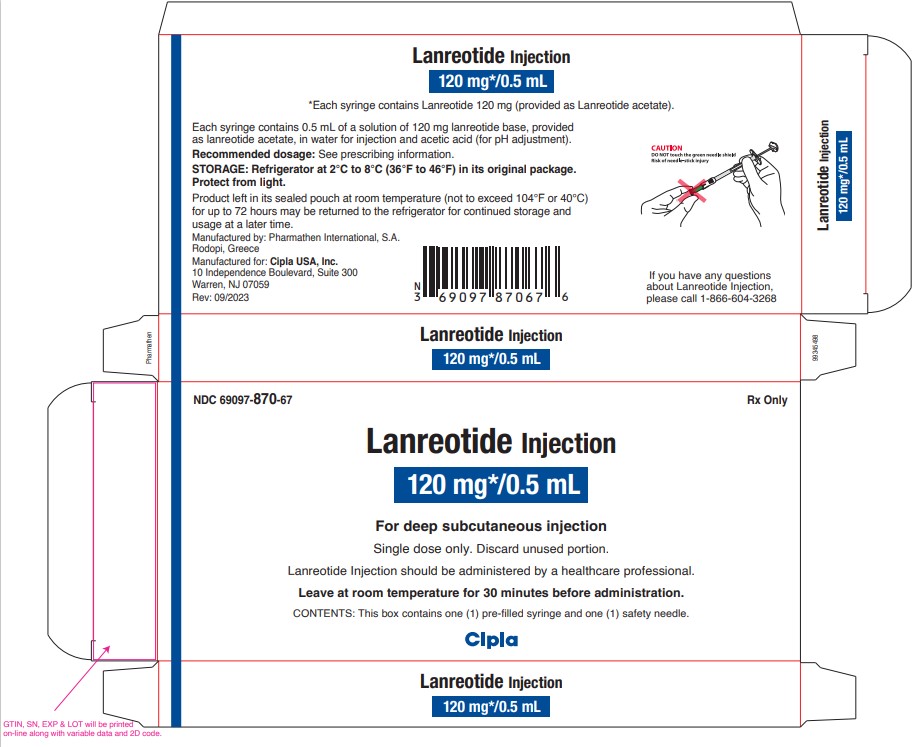
-
INGREDIENTS AND APPEARANCE
LANREOTIDE ACETATE
lanreotide acetate injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 69097-880 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LANREOTIDE ACETATE (UNII: IEU56G3J9C) (LANREOTIDE - UNII:0G3DE8943Y) LANREOTIDE 60 mg in 0.2 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 69097-880-67 1 in 1 CARTON 12/24/2021 1 0.2 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA215395 12/24/2021 LANREOTIDE ACETATE
lanreotide acetate injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 69097-890 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LANREOTIDE ACETATE (UNII: IEU56G3J9C) (LANREOTIDE - UNII:0G3DE8943Y) LANREOTIDE 90 mg in 0.3 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 69097-890-67 1 in 1 CARTON 12/24/2021 1 0.3 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA215395 12/24/2021 LANREOTIDE ACETATE
lanreotide acetate injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 69097-870 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LANREOTIDE ACETATE (UNII: IEU56G3J9C) (LANREOTIDE - UNII:0G3DE8943Y) LANREOTIDE 120 mg in 0.5 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 69097-870-67 1 in 1 CARTON 12/24/2021 1 0.5 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA215395 12/24/2021 Labeler - Cipla USA Inc. (078719707) Registrant - InvaGen Pharmaceuticals, Inc. (165104469) Establishment Name Address ID/FEI Business Operations Pharmathen International S.A. 503272186 manufacture(69097-880, 69097-890, 69097-870) , analysis(69097-880, 69097-890, 69097-870) , pack(69097-880, 69097-890, 69097-870)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.