TRAMADOL HYDROCHLORIDE tablet, extended release
TRAMADOL HYDROCHLORIDE by
Drug Labeling and Warnings
TRAMADOL HYDROCHLORIDE by is a Prescription medication manufactured, distributed, or labeled by Medsource Pharmaceuticals, LUPIN LIMITED. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use TRAMADOL HYDROCHLORIDE EXTENDED-RELEASE TABLETS safely and effectively. See full prescribing information for TRAMADOL HYDROCHLORIDE EXTENDED-RELEASE TABLETS.
TRAMADOL hydrochloride extended-release tablets for oral use, C IV
Initial U.S. Approval: 1995WARNING: SERIOUS AND LIFE-THREATENING RISKS FROM USE OF TRAMADOL HYDROCHLORIDE EXTENDED-RELEASE TABLETS
See full prescribing information for complete boxed warning.
- Tramadol hydrochloride extended-release tablet exposes users to risks of addiction, abuse, and misuse, which can lead to overdose and death. Assess patient's risk before prescribing and monitor regularly for these behaviors and conditions. ( 5.1)
- Serious, life-threatening, or fatal respiratory depression may occur. Monitor closely, especially upon initiation or following a dose increase. Instruct patients to swallow tramadol hydrochloride extended-release tablets whole to avoid exposure to a potentially fatal dose of tramadol. ( 5.2)
- Accidental ingestion of tramadol hydrochloride extended-release tablets, especially by children, can result in a fatal overdose of tramadol. ( 5.2)
- Concomitant use of opioids with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing for use in patients for whom alternative treatment options are inadequate; limit dosages and durations to the minimum required; and follow patients for signs and symptoms of respiratory depression and sedation. ( 5.3, 7)
- Prolonged use of tramadol hydrochloride extended-release tablets during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated. If prolonged opioid use is required in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available. ( 5.4)
- To ensure that the benefits of opioid analgesics outweigh the risks of addiction, abuse, and misuse, the Food and Drug Administration (FDA) has required a Risk Evaluation and Mitigation Strategy (REMS) for these products. ( 5.5)
- Life-threatening respiratory depression and death have occurred in children who received tramadol. Some of the reported cases followed tonsillectomy and/or adenoidectomy; in at least one case, the child had evidence of being an ultra-rapid metabolizer of tramadol due to a CYP2D6 polymorphism ( 5.6). Tramadol hydrochloride extended-release tablets are contraindicated in children younger than 12 years of age and in children younger than 18 years of age following tonsillectomy and/or adenoidectomy ( 4). Avoid the use of tramadol hydrochloride extended-release tablets in adolescents 12 to 18 years of age who have other risk factors that may increase their sensitivity to the respiratory depressant effects of tramadol. [see Warnings and Precautions ( 5.6)]
- The effects of concomitant use or discontinuation of cytochrome P450 3A4 inducers, 3A4 inhibitors, or 2D6 inhibitors with tramadol are complex. Use of cytochrome P450 3A4 inducers, 3A4 inhibitors, or 2D6 inhibitors with tramadol hydrochloride extended-release tablet requires careful consideration of the effects on the parent drug, tramadol, and the active metabolite, M1 ( 5.7, 7)
RECENT MAJOR CHANGES
INDICATIONS AND USAGE
Tramadol hydrochloride extended-release tablets are an opioid agonist indicated for the management of severe and persistent pain that requires an extended treatment period with a daily opioid analgesic and for which alternative treatment options are inadequate. ( 1)
Limitations of Use
- Because of the risks of addiction, abuse, and misuse with opioids, which can occur at any dosages or duration, and because of the greater risks of overdose and death with extended-release opioid formulations, reserve tramadol hydrochloride extended-release tablet for use in patients for whom alternative treatment options (e.g., non-opioid analgesics or immediate-release opioids) are ineffective, not tolerated or would be otherwise inadequate to provide sufficient management of pain. ( 1)
- Tramadol hydrochloride extended-release tablets is not indicated as an as-needed (prn) analgesic. ( 1)
DOSAGE AND ADMINISTRATION
- Tramadol hydrochloride extended-release tablets should be prescribed only by healthcare providers knowledgeable about the use of extended-release/long-acting opioids and how to mitigate the associated risks. ( 2.1)
- Use the lowest effective dosage for the shortest duration of time consistent with individual patient treatment goals. Reserve titration to higher doses of tramadol hydrochloride extended-release tablets for patients in whom lower doses are insufficiently effective and in whom the expected benefits of using a higher dose opioid clearly outweigh the substantial risks. ( 2.1, 5).
- Initiate the dosing regimen for each patient individually, taking into account the patient's underlying cause and severity of pain, prior analgesic treatment and response, and risk factors for addiction, abuse, and misuse. ( 5.1)
- Respiratory depression can occur at any time during opioid therapy, especially when initiating and following dosage increases with tramadol hydrochloride extended-release tablets. Consider this risk when selecting an initial dose and when making dose adjustments. ( 2.1, 5.2)
- Do not exceed a daily dose of 300 mg tramadol. Do not use with other tramadol products. ( 2.1)
- For opioid-naïve and opioid non-tolerant patients, initiate tramadol hydrochloride extended-release tablets at a dose of 100 mg once daily, then titrate up by 100 mg increments every 5 days according to need and tolerance. ( 2.3)
- For patients currently on tramadol IR, calculate total 24-hr IR dose, and initiate tramadol hydrochloride extended-release tablets at a dose rounded down to next lower 100 mg increment; then adjust dose according to need and tolerance. See full prescribing information for instructions on conversion, titration, and maintenance of therapy. ( 2.3, 2.4)
- Do not abruptly discontinue tramadol hydrochloride extended-release tablets in a physically-dependent patient. ( 2.5)
- Discuss availability of naloxone with the patient and caregiver and assess each patient's need for access to naloxone, both when initiating and renewing treatment with tramadol hydrochloride extended-release tablets. Consider prescribing naloxone based on the patient's risk factors for overdose [ 2.2, 5.1, 5.3, 5.7].
DOSAGE FORMS AND STRENGTHS
- Extended-release tablets 100 mg, 200 mg, and 300 mg (non-scored) ( 3)
CONTRAINDICATIONS
- Children younger than 12 years of age ( 4)
- Postoperative management in children younger than 18 years of age following tonsillectomy and/or adenoidectomy. ( 4)
- Significant respiratory depression ( 4)
- Acute or severe bronchial asthma in an unmonitored setting or in absence of resuscitative equipment ( 4)
- Known or suspected gastrointestinal obstruction, including paralytic ileus ( 4)
- Hypersensitivity to tramadol ( 4)
- Concurrent use of monoamine oxidase inhibitors (MAOIs) or use within the last 14 days ( 4)
WARNINGS AND PRECAUTIONS
- Opioid Induced Hyperalgesia (OIH) and Allodynia: Opioid-Induced Hyperalgesia (OIH) occurs when an opioid analgesic paradoxically causes an increase in pain, or an increase in sensitivity to pain. If OIH is suspected, carefully consider appropriately decreasing the dose of the current opioid analgesic, or opioid rotation. ( 5.8)
- Serotonin Syndrome with Concomitant Use of Serotonergic Drugs: Potentially life-threatening condition could result from concomitant serotonergic drug administration. Discontinue tramadol hydrochloride extended-release tablets if serotonin syndrome is suspected. ( 5.9)
- Risk of Seizure: Present within recommended dosage range. Risk is increased with higher than recommended doses and concomitant use of SSRIs, SNRIs, anorectics, tricyclic antidepressants and other tricyclic compounds, other opioids, MAOIs, neuroleptics, other drugs that reduce seizure threshold, in patients with epilepsy or at risk for seizures. ( 5.10, 7)
- Risk of Suicide: Do not use tramadol hydrochloride extended-release tablets in suicidal or addiction-prone patients. Use with caution in those taking tranquilizers, antidepressants or abuse alcohol. ( 5.11)
- Life-Threatening Respiratory Depression in Patients with Chronic Pulmonary Disease or in Elderly, Cachectic, or Debilitated Patients: Regularly evaluate closely, particularly during initiation and titration. ( 5.12)
- Adrenal Insufficiency: If diagnosed, treat with physiologic replacement of corticosteroids, and wean patient off of the opioid. ( 5.13)
- Severe Hypotension: Regularly evaluate during dosage initiation and titration. Avoid use of tramadol hydrochloride extended-release tablets in patients with circulatory shock. ( 5.14)
- Risks of Use in Patients with Increased Intracranial Pressure, Brain Tumors, Head Injury, or Impaired Consciousness: Regularly evaluate for sedation and respiratory depression. Avoid use of tramadol hydrochloride extended-release tablets in patients with impaired consciousness or coma. ( 5.15)
ADVERSE REACTIONS
Most common adverse reactions (≥10% and ≥2 x placebo rate): Dizziness, constipation, nausea, headache, somnolence, flushing, pruritus, vomiting, insomnia, dry mouth. ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Lupin Pharmaceuticals, Inc. at 1-800-399-2561 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 1/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: SERIOUS AND LIFE-THREATENING RISKS FROM USE OF TRAMADOL HYDROCHLORIDE EXTENDED-RELEASE TABLETS
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosage and Administration Instructions
2.2 Patient Access to Naloxone for the Emergency Treatment of Opioid Overdose
2.3 Initial Dosage
2.4 Titration and Maintenance of Therapy
2.5 Safe Reduction or Discontinuation Of Tramadol Hydrochloride Extended-Release Tablets
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Addiction, Abuse, and Misuse
5.2 Life Threatening Respiratory Depression
5.3 Risks from Concomitant Use with Benzodiazepines or Other CNS Depressants
5.4 Neonatal Opioid Withdrawal Syndrome (NOWS)
5.5 Opioid Analgesic Risk Evaluation and Mitigation Strategy (REMS)
5.6 Ultra-Rapid Metabolism of Tramadol and Other Risk Factors for Life-threatening Respiratory Depression in Children
5.7 Risks of Interactions with Drugs Affecting Cytochrome P450 Isoenzymes
5.8 Opioid-Induced Hyperalgesia and Allodynia
5.9 Serotonin Syndrome with Concomitant Use of Serotonergic Drugs
5.10 Increased Risk of Seizures
5.11 Suicide Risk
5.12 Life-Threatening Respiratory Depression in Patients with Chronic Pulmonary Disease or in Elderly, Cachectic, or Debilitated Patients
5.13 Adrenal Insufficiency
5.14 Severe Hypotension
5.15 Risks of Use in Patients with Increased Intracranial Pressure, Brain Tumors, Head Injury, or Impaired Consciousness
5.16 Risks of Use in Patients with Gastrointestinal Conditions
5.17 Anaphylaxis and Other Hypersensitivity Reactions
5.18 Withdrawal
5.19 Risks of Driving and Operating Machinery
5.20 Hyponatremia
5.21 Hypoglycemia
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 Renal Impairment
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
9.2 Abuse
9.3 Dependence
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: SERIOUS AND LIFE-THREATENING RISKS FROM USE OF TRAMADOL HYDROCHLORIDE EXTENDED-RELEASE TABLETS
Because the use of Tramadol hydrochloride extended-release tablet exposes patients and other users to the risks of opioid addiction, abuse, and misuse, which can lead to overdose and death, assess each patient's risk prior to prescribing and reassess all patients regularly for the development of these behaviors and conditions [see Warnings and Precautions ( 5.1)] .
Life-Threatening Respiratory Depression
Serious, life-threatening, or fatal respiratory depression may occur with use of tramadol hydrochloride extended-release tablets, especially during initiation or following a dosage increase. To reduce the risk of respiratory depression, proper dosing and titration of tramadol hydrochloride extended-release tablets are essential. Instruct patients to swallow tramadol hydrochloride extended-release tablets whole to avoid exposure to a potentially fatal dose of tramadol. [see Warnings and Precautions ( 5.2)] .
Accidental Ingestion
Accidental ingestion of even one dose of tramadol hydrochloride extended-release tablets, especially by children, can result in a fatal overdose of tramadol [see Warnings and Precautions ( 5.2)] .
Risks From Concomitant Use With Benzodiazepines Or Other CNS Depressants
Concomitant use of opioids with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing of tramadol hydrochloride extended-release tablets and benzodiazepines or other CNS depressants for use in patients for whom alternative treatment options are inadequate. [see Warnings and Precautions ( 5.3), Drug Interactions ( 7)] .
Neonatal Opioid Withdrawal Syndrome
If opioid use is required for an extended period of time in a pregnant woman, advise the patient of the risk of NOWS, which may be life-threatening if not recognized and treated. Ensure that management by neonatology experts will be available at delivery [see Warnings and Precautions ( 5.4)] .
Opioid Analgesic Risk Evaluation and Mitigation Strategy (REMS)
Healthcare providers are strongly encouraged to complete a REMS compliant education program and to counsel patients and caregivers on serious risks, safe use, and the importance of reading the Medication Guide with each prescription [see Warnings and Precautions ( 5.5)] .
Ultra-Rapid Metabolism Of Tramadol And Other Risk Factors For Life-Threatening Respiratory Depression In Children
Life-threatening respiratory depression and death have occurred in children who received tramadol. Some of the reported cases followed tonsillectomy and/or adenoidectomy; in at least one case, the child had evidence of being an ultra-rapid metabolizer of tramadol due to a CYP2D6 polymorphism [see Warnings and Precautions ( 5.6)] . Tramadol hydrochloride extended-release tablets are contraindicated in children younger than 12 years of age and in children younger than 18 years of age following tonsillectomy and/or adenoidectomy [see Contraindications ( 4)] . Avoid the use of tramadol hydrochloride extended-release tablets in adolescents 12 to 18 years of age who have other risk factors that may increase their sensitivity to the respiratory depressant effects of tramadol. [see Warnings and Precautions ( 5.6)]
Interactions with Drugs Affecting Cytochrome P450 Isoenzymes
The effects of concomitant use or discontinuation of cytochrome P450 3A4 inducers, 3A4 inhibitors, or 2D6 inhibitors with tramadol are complex. Use of cytochrome P450 3A4 inducers, 3A4 inhibitors, or 2D6 inhibitors with tramadol hydrochloride extended-release tabletrequires careful consideration of the effects on the parent drug, tramadol, and the active metabolite, M1 [see Warnings and Precautions ( 5.7), Drug Interactions ( 7)] .
-
1 INDICATIONS AND USAGE
Tramadol hydrochloride extended-release tablet is indicated for the management of severe and persistent pain that requires an extended treatment period with a daily opioid analgesic and for which alternative treatment options are inadequate.
Limitations of Use
- Because of the risks of addiction, abuse, and misuse with opioids, which can occur at any dosages or duration, and because of the greater risks of overdose and death with extended-release opioid formulations [see Warnings and Precautions ( 5.1)] , reserve tramadol hydrochloride extended-release tablets for use in patients for whom alternative treatment options (e.g., non-opioid analgesics or immediate-release opioids) are ineffective, not tolerated, or would be otherwise inadequate to provide sufficient management of pain.
- Tramadol hydrochloride extended-release tablet is not indicated as an as-needed (prn) analgesic.
-
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosage and Administration Instructions
Tramadol hydrochloride extended-release tablets should be prescribed only by healthcare professionals who are knowledgeable about the use of extended-release/long-acting opioids and how to mitigate the associated risks.
- Do not use tramadol hydrochloride extended-release tablets concomitantly with other tramadol products [see Warnings and Precautions ( 5.3), ( 5.15)] .
- Do not administer tramadol hydrochloride extended-release tablets at a dose exceeding 300 mg per day.
- Use the lowest effective dosage for the shortest duration of time consistent with individual patient treatment goals [ see Warnings and Precautions ( 5.5) ]. Because the risk of overdose increases as opioid doses increase, reserve titration to higher doses of tramadol hydrochloride extended-release tablets for patients in whom lower doses are insufficiently effective and in whom the expected benefits of using a higher dose opioid clearly outweigh the substantial risks.
- Initiate the dosing regimen for each patient individually, taking into account the patient's underlying cause and severity of pain, prior analgesic treatment and response, and risk factors for addiction, abuse, and misuse [see Warnings and Precautions ( 5.1)]
- Respiratory depression can occur at any time during opioid therapy, especially when initiating and following dosage increases with tramadol hydrochloride extended-release tablets. Consider this risk when selecting an initial dose and when making dose adjustments [ see Warnings and Precautions ( 5.5) ].
- Instruct patients to swallow tramadol hydrochloride extended-release tablets whole [see Patient Counseling Information ( 17)] , and to take it with liquid. Crushing, chewing, splitting, or dissolving tramadol hydrochloride extended-release tablets will result in uncontrolled delivery of tramadol and can lead to overdose or death [see Warnings and Precautions ( 5.1)] .
- Tramadol hydrochloride extended-release tablets may be taken without regard to food, It is recommended that tramadol hydrochloride extended-release tablets be taken in a consistent manner [see Clinical Pharmacology ( 12.3)] .
2.2 Patient Access to Naloxone for the Emergency Treatment of Opioid Overdose
Discuss the availability of naloxone for the emergency treatment of opioid overdose with the patient and caregiver and assess the potential need for access to naloxone, both when initiating and renewing treatment with tramadol hydrochloride extended release tablets [see Warnings and Precautions ( 5.3), Patient Counseling Information ( 17)].
Inform patients and caregivers about the various ways to obtain naloxone as permitted by individual state naloxone dispensing and prescribing requirements or guidelines (e.g., by prescription, directly from a pharmacist, or as part of a community-based program).
Consider prescribing naloxone, based on the patient's risk factors for overdose, such as concomitant use of CNS depressants, a history of opioid use disorder, or prior opioid overdose. The presence of risk factors for overdose should not prevent the proper management of pain in any given patient [see Warnings and Precautions ( 5.1, 5.3, 5.7)].
Consider prescribing naloxone if the patient has household members (including children) or other close contacts at risk for accidental ingestion or overdose .
2.3 Initial Dosage
Patients Not Currently on a Tramadol Product
The initial dose of tramadol hydrochloride extended-release tablets is 100 mg once daily.
Patients Currently on Tramadol Immediate-Release (IR) Products
Calculate the 24-hour tramadol IR dose and initiate a total daily dose of tramadol hydrochloride extended-release tablets rounded down to the next lower 100 mg increment. The dose may subsequently be individualized according to patient need.
Due to limitations in flexibility of dose selection with tramadol hydrochloride extended-release tablets, some patients maintained on tramadol IR products may not be able to convert to tramadol hydrochloride extended-release tablets.
Conversion from Other Opioids to Tramadol Hydrochloride Extended-Release Tablets
When tramadol hydrochloride extended-release tablets therapy is initiated, discontinue all other opioid analgesics other than those used on an as needed basis for breakthrough pain when appropriate drugs.
2.4 Titration and Maintenance of Therapy
Individually titrate tramadol hydrochloride extended-release tablets by 100 mg every five days to a dose that provides adequate analgesia and minimizes adverse reactions. The maximum daily dose of tramadol hydrochloride extended-release tablets is 300 mg per day.
Continually reevaluate patients receiving tramadol hydrochloride extended-release tablets to assess the maintenance of pain control, signs and symptoms of opioids withdrawal and other adverse reactions, as well as to reassess for the development of addiction, abuse, or misuse [see Warnings and Withdrawal ( 5.1, 5.18)] . Frequent communication is important among the prescriber, other members of the healthcare team, the patient, and the caregiver/family during periods of changing analgesic requirements, including initial titration. During use of opioid therapy for an extended period of time, periodically reassess the continued need for the use of opioid analgesics.
Patients who experience breakthrough pain may require a dosage adjustment of tramadol hydrochloride extended-release tablets, or may need rescue medication with an appropriate dose of an immediate-release analgesic. If the level of pain increases after dosage stabilization, attempt to identify the source of increased pain before increasing the tramadol hydrochloride extended-release tablets dosage.
If after increasing the dosage, unacceptable opioid-related adverse reactions are observed (including an increase in pain after dosage increase), consider reducing the dosage [see Warnings and Precautions ( 5)] . Adjust the dosage to obtain an appropriate balance between management of pain and opioid-related adverse reactions.
2.5 Safe Reduction or Discontinuation Of Tramadol Hydrochloride Extended-Release Tablets
Do not abruptly discontinue tramadol hydrochloride extended-release tablets in patients who may be physically dependent on opioids. Rapid discontinuation of opioid analgesics in patients who are physically dependent on opioids has resulted in serious withdrawal symptoms, uncontrolled pain, and suicide. Rapid discontinuation has also been associated with attempts to find other sources of opioid analgesics, which may be confused with drug-seeking for abuse. Patients may also attempt to treat their pain or withdrawal symptoms with illicit opioids, such as heroin, and other substances.
When a decision has been made to decrease the dose or discontinue therapy in an opioid-dependent patient taking tramadol hydrochloride extended-release tablets, there are a variety of factors that should be considered, including the total daily dose of opioid (including tramadol hydrochloride extended-release tablets) the patient has been taking, the duration of treatment, the type of pain being treated, and the physical and psychological attributes of the patient. It is important to ensure ongoing care of the patient and to agree on an appropriate tapering schedule and follow-up plan so that patient and provider goals and expectations are clear and realistic. When opioid analgesics are being discontinued due to a suspected substance use disorder, evaluate and treat the patient, or refer for evaluation and treatment of the substance use disorder. Treatment should include evidence-based approaches, such as medication assisted treatment of opioid use disorder. Complex patients with co-morbid pain and substance use disorders may benefit from referral to a specialist.
There are no standard opioid tapering schedules that are suitable for all patients. Good clinical practice dictates a patient-specific plan to taper the dose of the opioid gradually. For patients on tramadol hydrochloride extended-release tablets who are physically opioid-dependent, initiate the taper by a small enough increment (e.g., no greater than 10% to 25% of the total daily dose) to avoid withdrawal symptoms, and proceed with dose-lowering at an interval of every 2 to 4 weeks. Patients who have been taking opioids for briefer periods of time may tolerate a more rapid taper.
It may be necessary to provide the patient with lower dosage strengths to accomplish a successful taper. Reassess the patient frequently to manage pain and withdrawal symptoms, should they emerge. Common withdrawal symptoms include restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, myalgia, and mydriasis. Other signs and symptoms also may develop, including irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, or increased blood pressure, respiratory rate, or heart rate. If withdrawal symptoms arise, it may be necessary to pause the taper for a period of time or raise the dose of the opioid analgesic to the previous dose, and then proceed with a slower taper. In addition, evaluate patients for any changes in mood, emergence of suicidal thoughts, or use of other substances.
When managing patients taking opioid analgesics, particularly those who have been treated for an extended period of time and/or with high doses for chronic pain, ensure that a multimodal approach to pain management, including mental health support (if needed), is in place prior to initiating an opioid analgesic taper. A multimodal approach to pain management may optimize the treatment of chronic pain, as well as assist with the successful tapering of the opioid analgesic [see Warnings and Precautions ( 5.17), Drug Abuse and Dependence ( 9.3)].
-
3 DOSAGE FORMS AND STRENGTHS
Extended-release tablets are available as:
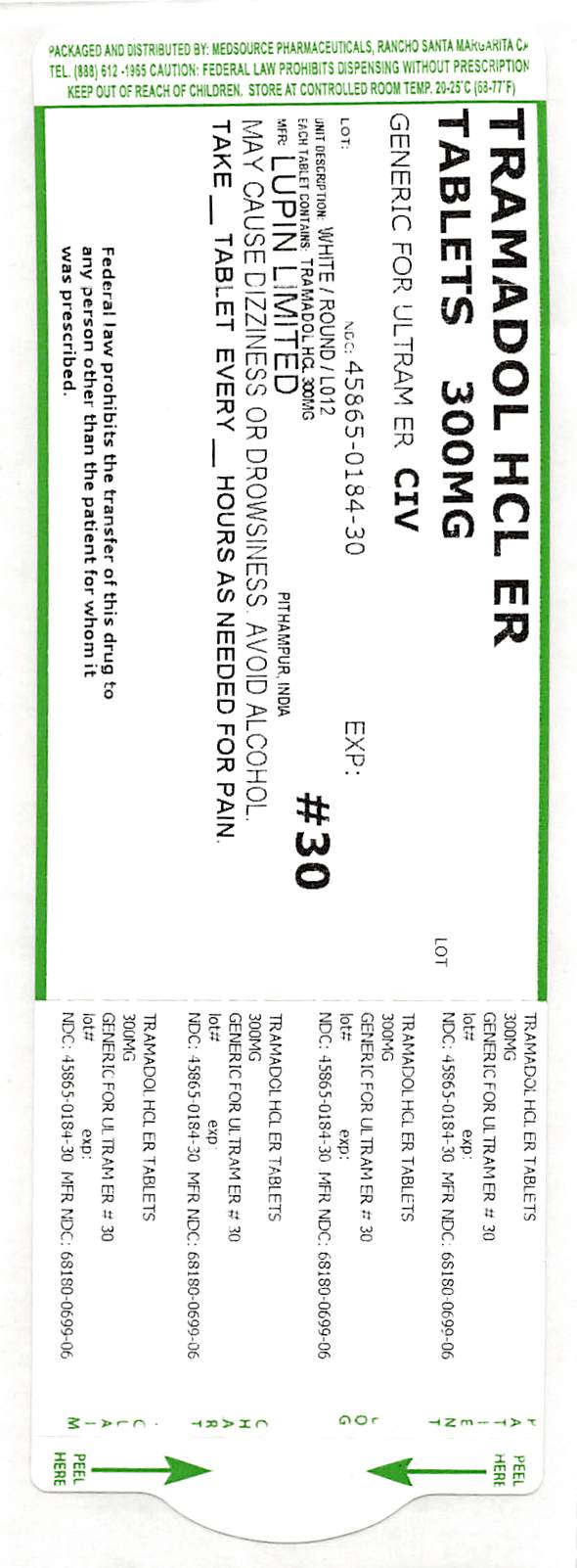
100 mg tablets: White to off-white circular, biconvex, beveled edge coated tablets imprinted with 'L010' on one side and plain on the other side.
200 mg tablets: White to off-white circular, biconvex, beveled edge coated tablets imprinted with 'L011' on one side and plain on the other side.
300 mg tablets: White to off-white circular, biconvex, beveled edge coated tablets imprinted with 'L012' on one side and plain on the other side.
-
4 CONTRAINDICATIONS
Tramadol hydrochloride extended-release tablets are contraindicated for:
- all children younger than 12 years of age [see Warnings and Precautions ( 5.4)]
- post-operative management in children younger than 18 years of age following tonsillectomy and/or adenoidectomy [see Warnings and Precautions ( 5.4)] .
Tramadol hydrochloride extended-release tablets are also contraindicated in patients with:
- Significant respiratory depression [see Warnings and Precautions ( 5.3)]
- Acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment [see Warnings and Precautions ( 5.12)]
- Known or suspected gastrointestinal obstruction, including paralytic ileus [see Warnings and Precautions ( 5.15)]
- Hypersensitivity to tramadol (e.g., anaphylaxis) [see Warnings and Precautions (5.16), Adverse Reactions ( 6.2)]
- Concurrent use of monoamine oxidase inhibitors (MAOIs) or use within the last 14 days [see Drug Interactions ( 7)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Addiction, Abuse, and Misuse
Tramadol hydrochloride extended-release tablet contains tramadol, a Schedule IV controlled substance. As an opioid, tramadol hydrochloride extended-release tablet exposes users to the risks of addiction, abuse, and misuse. Because extended-release products such as tramadol hydrochloride extended-release tablets deliver the opioid over an extended period of time, there is a greater risk for overdose and death due to the larger amount of tramadol present [see Drug Abuse and Dependence( 9)] .
Although the risk of addiction in any individual is unknown, it can occur in patients appropriately prescribed tramadol hydrochloride extended-release tablets. Addiction can occur at recommended dosages and if the drug is misused or abused.
Assess each patient's risk for opioid addiction, abuse, or misuse prior to prescribing tramadol hydrochloride extended-release tablets, and reassess all patients receiving tramadol hydrochloride extended-release tablets for the development of these behaviors and conditions. Risks are increased in patients with a personal or family history of substance abuse (including drug or alcohol abuse or addiction) or mental illness (e.g., major depression). The potential for these risks should not, however, prevent the proper management of pain in any given patient. Patients at increased risk may be prescribed opioids such as tramadol hydrochloride extended-release tablets, but use in such patients necessitates intensive counseling about the risks and proper use of tramadol hydrochloride extended-release tablets along with frequent reevaluation for signs of addiction, abuse, and misuse. Consider prescribing naloxone for the emergency treatment of opioid overdose [see Dosage and Administration ( 2.2), Warnings and Precautions ( 5.3)] .
Abuse or misuse of tramadol hydrochloride extended-release tablets by cutting, breaking, chewing, crushing, snorting, or injecting the dissolved product will result in the uncontrolled delivery of tramadol and can result in overdose and death [see Overdosage ( 10)] .
Opioids are sought for non-medical use and are subject to diversion from legitimate prescribed use. Consider these risks when prescribing or dispensing tramadol hydrochloride extended-release tablets. Strategies to reduce these risks include prescribing the drug in the smallest appropriate quantity and advising the patient on careful storage of the drug during the course of treatment and proper disposal of unused drug. Contact local state professional licensing board or state-controlled substances authority for information on how to prevent and detect abuse or diversion of this product.
5.2 Life Threatening Respiratory Depression
Serious, life-threatening, or fatal respiratory depression has been reported with the use of opioids, even when used as recommended. Respiratory depression, if not immediately recognized and treated, may lead to respiratory arrest and death. Management of respiratory depression may include close observation, supportive measures, and use of opioid antagonists, depending on the patient's clinical status [see Overdosage ( 10)] . Carbon dioxide (CO 2) retention from opioid-induced respiratory depression can exacerbate the sedating effects of opioids.
While serious, life-threatening, or fatal respiratory depression can occur at any time during the use of tramadol hydrochloride extended-release tablets, the risk is greatest during the initiation of therapy or following a dosage increase of tramadol hydrochloride extended-release tablets.
To reduce the risk of respiratory depression, proper dosing and titration of tramadol hydrochloride extended-release tablets are essential [see Dosage and Administration ( 2)] . Overestimating the tramadol hydrochloride extended-release tablets dosage when converting patients from another opioid product can result in a fatal overdose with the first dose.
Accidental ingestion of even one dose of tramadol hydrochloride extended-release tablets, especially by children, can result in respiratory depression and death due to an overdose of tramadol.
Educate patients and caregivers on how to recognize respiratory depression and emphasize the importance of calling 911 or getting emergency medical help right away in the event of a known or suspected overdose [see Patient Counseling Information (17)].
Opioids can cause sleep-related breathing disorders including central sleep apnea (CSA) and sleep-related hypoxemia. Opioid use increases the risk of CSA in a dose-dependent fashion. In patients who present with CSA, consider decreasing the opioid dosage using best practices for opioid taper [see Dosage and Administration ( 2.5)].
Patient Access to Naloxone for the Emergency Treatment of Opioid Overdose
Discuss the availability of naloxone for the emergency treatment of opioid overdose with the patient and caregiver and assess the potential need for access to naloxone, both when initiating and renewing treatment with tramadol hydrochloride extended release tablets. Inform patients and caregivers about the various ways to obtain naloxone as permitted by individual state naloxone dispensing and prescribing requirements or guidelines (e.g., by prescription, directly from a pharmacist, or as part of a community-based program). Educate patients and caregivers on how to recognize respiratory depression and emphasize the importance of calling 911 or getting emergency medical help, even if naloxone is administered [see Patient Counseling Information ( 17)].
Consider prescribing naloxone, based on the patient's risk factors for overdose, such as concomitant use of CNS depressants, a history of opioid use disorder, or prior opioid overdose. The presence of risk factors for overdose should not prevent the proper management of pain in any given patient. Also consider prescribing naloxone if the patient has household members (including children) or other close contacts at risk for accidental ingestion or overdose. If naloxone is prescribed, educate patients and caregivers on how to treat with naloxone. [see Dosage and Administration ( 2.2), Warnings and Precautions ( 5.1, 5.3, Overdosage ( 10)].
5.3 Risks from Concomitant Use with Benzodiazepines or Other CNS Depressants
Profound sedation, respiratory depression, coma, and death may result from the concomitant use of tramadol hydrochloride extended-release tablets with benzodiazepines and/or other CNS depressants, including alcohol (e.g., non-benzodiazepine sedatives/hypnotics, anxiolytics, tranquilizers, muscle relaxants, general anesthetics, antipsychotics, other opioids). Because of these risks, reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate.
Observational studies have demonstrated that concomitant use of opioid analgesics and benzodiazepines increases the risk of drug-related mortality compared to use of opioid analgesics alone. Because of similar pharmacological properties, it is reasonable to expect similar risk with the concomitant use of other CNS depressant drugs with opioid analgesics [see Drug Interactions ( 7)] .
If the decision is made to prescribe a benzodiazepine or other CNS depressant concomitantly with an opioid analgesic, prescribe the lowest effective dosages and minimum durations of concomitant use. In patients already receiving an opioid analgesic, prescribe a lower initial dose of the benzodiazepine or other CNS depressant than indicated in the absence of an opioid, and titrate based on clinical response. If an opioid analgesic is initiated in a patient already taking a benzodiazepine or other CNS depressant, prescribe a lower initial dose of the opioid analgesic, and titrate based on clinical response. Inform patients and caregivers of this potential interaction, educate them on the signs and symptoms of respiratory depression (including sedation).
If concomitant use is warranted, consider prescribing naloxone for the emergency treatment of opioid overdose [see Dosage and Administration ( 2.2), Warnings and Precautions ( 5.3)] .
5.4 Neonatal Opioid Withdrawal Syndrome (NOWS)
Use of tramadol hydrochloride extended-release tablets for an extended period of time during pregnancy can result in withdrawal in the neonate. Neonatal opioid withdrawal syndrome, unlike opioid withdrawal syndrome in adults, may be life-threatening if not recognized and treated, and requires management according to protocols developed by neonatology experts. Observe newborns for signs of neonatal opioid withdrawal syndrome and manage accordingly. Advise pregnant women using opioids for an extended period of time of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available [see Use in Specific Populations ( 8.1), Patient Counseling Information ( 17)] .
5.5 Opioid Analgesic Risk Evaluation and Mitigation Strategy (REMS)
To ensure that the benefits of opioid analgesics outweigh the risks of addiction, abuse, and misuse, the Food and Drug Administration (FDA) has required a Risk Evaluation and Mitigation Strategy (REMS) for these products. Under the requirements of the REMS, drug companies with approved opioid analgesic products must make REMS compliant education programs available to healthcare providers. Healthcare providers are strongly encouraged to do all of the following:
- Complete a REMS-compliant education programoffered by an accredited provider of continuing education (CE) or another education program that includes all the elements of the FDA Education Blueprint for Health Care Providers Involved in the Management or Support of Patients with Pain.
- Discuss the safe use, serious risks, and proper storage and disposal of opioid analgesics with patients and/or their caregivers every time these medicines are prescribed. The Patient Counseling Guide (PCG) can be obtained at this link: www.fda.gov/OpioidAnalgesicREMSPCG.
- Emphasize to patients and their caregivers the importance of reading the Medication Guide that they will receive from their pharmacist every time an opioid analgesic is dispensed to them.
- Consider using other tools to improve patient, household, and community safety, such as patient-prescriber agreements that reinforce patient-prescriber responsibilities.
To obtain further information on the opioid analgesic REMS and for a list of accredited REMS CME/CE, call 800-503-0784, or log on to www.opioidanalgesicrems.com. The FDA Blueprint can be found at www.fda.gov/OpioidAnalgesicREMSBlueprint.
5.6 Ultra-Rapid Metabolism of Tramadol and Other Risk Factors for Life-threatening Respiratory Depression in Children
Life-threatening respiratory depression and death have occurred in children who received tramadol. Tramadol and codeine are subject to variability in metabolism based upon CYP2D6 genotype (described below), which can lead to increased exposure to an active metabolite. Based upon postmarketing reports with tramadol or with codeine, children younger than 12 years of age may be more susceptible to the respiratory depressant effects of tramadol. Furthermore, children with obstructive sleep apnea who are treated with opioids for post-tonsillectomy and/or adenoidectomy pain may be particularly sensitive to their respiratory depressant effect. Because of the risk of life-threatening respiratory depression and death:
- Tramadol hydrochloride extended-release tablets are contraindicated for all children younger than 12 years of age [see Contraindications ( 4)].
- Tramadol hydrochloride extended-release tablets are contraindicated for post-operative management in pediatric patients younger than 18 years of age following tonsillectomy and/or adenoidectomy [see Contraindications ( 4)] .
- Avoid the use of tramadol hydrochloride extended-release tablets in adolescents 12 to 18 years of age who have other risk factors that may increase their sensitivity to the respiratory depressant effects of tramadol unless the benefits outweigh the risks. Risk factors include conditions associated with hypoventilation, such as postoperative status, obstructive sleep apnea, obesity, severe pulmonary disease, neuromuscular disease, and concomitant use of other medications that cause respiratory depression.
- As with adults, when prescribing opioids for adolescents, healthcare providers should choose the lowest effective dose for the shortest period of time and inform patients and caregivers about these risks and the signs of opioid overdose [see Use in Specific Populations ( 8.4), Overdosage ( 10)].
Tramadol is subject to the same polymorphic metabolism as codeine, with ultra-rapid metabolizers of CYP2D6 substrates being potentially exposed to life-threatening levels of O-desmethyltramadol (M1). At least one death was reported in a nursing infant who was exposed to high levels of morphine in breast milk because the mother was an ultra-rapid metabolizer of codeine. A baby nursing from an ultra-rapid metabolizer mother taking tramadol hydrochloride extended-release tablets could potentially be exposed to high levels of M1, and experience life-threatening respiratory depression. For this reason, breastfeeding is not recommended during treatment with tramadol hydrochloride extended-release tablets [see Use in Specific Populations ( 8.2)] .
CYP2D6 Genetic Variability: Ultra-rapid metabolizer
Some individuals may be ultra-rapid metabolizers because of a specific CYP2D6 genotype (e.g., gene duplications denoted as *1/*1xN or *1/*2xN). The prevalence of this CYP2D6 phenotype varies widely and has been estimated at 1 to 10% for Whites (European, North American), 3 to 4% for Blacks (African Americans), 1 to 2% for East Asians (Chinese, Japanese, Korean), and may be greater than 10% in certain racial/ethnic groups (i.e., Oceanian, Northern African, Middle Eastern, Ashkenazi Jews, Puerto Rican). These individuals convert tramadol into its active metabolite, O-desmethyltramadol (M1), more rapidly and completely than other people. This rapid conversion results in higher than expected serum M1 levels. Even at labeled dosage regimens, individuals who are ultra-rapid metabolizers may have life-threatening or fatal respiratory depression or experience signs of overdose (such as extreme sleepiness, confusion, or shallow breathing) [see Overdosage ( 10)] . Therefore, individuals who are ultra-rapid metabolizers should not use tramadol hydrochloride extended-release tablets.
5.7 Risks of Interactions with Drugs Affecting Cytochrome P450 Isoenzymes
The effects of concomitant use or discontinuation of cytochrome P450 3A4 inducers, 3A4 inhibitors, or 2D6 inhibitors on levels of tramadol and M1 from tramadol hydrochloride extended-release tablets are complex. Use of cytochrome P450 3A4 inducers, 3A4 inhibitors, or 2D6 inhibitors with tramadol hydrochloride extended-release tablet requires careful consideration of the effects on the parent drug, tramadol which is a weak serotonin and norepinephrine reuptake inhibitor and µ-opioid agonist, and the active metabolite, M1, which is more potent than tramadol in µ-opioid receptor binding [see Drug Interactions ( 7)] .
Risks of Concomitant Use or Discontinuation of Cytochrome P450 2D6 Inhibitors
The concomitant use of tramadol hydrochloride extended-release tablets with all cytochrome P450 2D6 inhibitors (e.g., amiodarone, quinidine) may result in an increase in tramadol plasma levels and a decrease in the levels of the active metabolite, M1. A decrease in M1 exposure in patients who have developed physical dependence to tramadol, may result in signs and symptoms of opioid withdrawal and reduced efficacy. The effect of increased tramadol levels may be an increased risk for serious adverse events including seizures and serotonin syndrome.
Discontinuation of a concomitantly used cytochrome P450 2D6 inhibitor may result in a decrease in tramadol plasma levels and an increase in active metabolite M1 levels, which could increase or prolong adverse reactions related to opioid toxicity and may cause potentially fatal respiratory depression.
Evaluate patients receiving tramadol hydrochloride extended-release tablets and any CYP2D6 inhibitor at frequent intervals for the risk of serious adverse events including seizures and serotonin syndrome, signs and symptoms that may reflect opioid toxicity, and opioid withdrawal when tramadol hydrochloride extended-release tablets are used in conjunction with inhibitors of CYP2D6 [see Drug Interactions ( 7)] .
Cytochrome P450 3A4 Interaction
The concomitant use of tramadol hydrochloride extended-release tablets with cytochrome P450 3A4 inhibitors, such as macrolide antibiotics (e.g., erythromycin), azole-antifungal agents (e.g., ketoconazole), and protease inhibitors (e.g., ritonavir) or discontinuation of a cytochrome P450 3A4 inducer such as rifampin, carbamazepine, and phenytoin, may result in an increase in tramadol plasma concentrations, which could increase or prolong adverse reactions, increase the risk for serious adverse events including seizures and serotonin syndrome, and may cause potentially fatal respiratory depression.
The concomitant use of tramadol hydrochloride extended-release tablets with all cytochrome P450 3A4 inducers or discontinuation of a cytochrome P450 3A4 inhibitor may result in lower tramadol levels. This may be associated with a decrease in efficacy, and in some patients, may result in signs and symptoms of opioid withdrawal.
Evaluate patients receiving tramadol hydrochloride extended-release tablets and any CYP3A4 inhibitor at frequent intervals for the risk for serious adverse events including seizures and serotonin syndrome, signs and symptoms that may reflect opioid toxicity and opioid withdrawal when tramadol hydrochloride extended-release tablets are used in conjunction with inhibitors and inducers of CYP3A4 [see Drug Interactions ( 7)] .
5.8 Opioid-Induced Hyperalgesia and Allodynia
Opioid-Induced Hyperalgesia (OIH) occurs when an opioid analgesic paradoxically causes an increase in pain, or an increase in sensitivity to pain. This condition differs from tolerance, which is the need for increasing doses of opioids to maintain a defined effect [ see Dependence ( 9.3) ]. Symptoms of OIH include (but may not be limited to) increased levels of pain upon opioid dosage increase, decreased levels of pain upon opioid dosage decrease, or pain from ordinarily non-painful stimuli (allodynia). These symptoms may suggest OIH only if there is no evidence of underlying disease progression, opioid tolerance, opioid withdrawal, or addictive behavior.
Cases of OIH have been reported, both with short-term and longer-term use of opioid analgesics. Though the mechanism of OIH is not fully understood, multiple biochemical pathways have been implicated. Medical literature suggests a strong biologic plausibility between opioid analgesics and OIH and allodynia. If a patient is suspected to be experiencing OIH, carefully consider appropriately decreasing the dose of the current opioid analgesic, or opioid rotation (safely switching the patient to a different opioid moiety) [ see Dosage and Administration ( 2.2); Warnings and Precautions ( 5.7) ].
5.9 Serotonin Syndrome with Concomitant Use of Serotonergic Drugs
Cases of serotonin syndrome, a potentially life-threatening condition, have been reported with the use of tramadol, including tramadol hydrochloride extended-release tablets, particularly during concomitant use with serotonergic drugs. Serotonergic drugs include selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), triptans, 5-HT3 receptor antagonists, drugs that affect the serotonergic neurotransmitter system (e.g., mirtazapine, trazodone, tramadol), certain muscle relaxants (i.e., cyclobenzaprine, metaxalone), and drugs that impair metabolism of serotonin (including MAO inhibitors, both those intended to treat psychiatric disorders and also others, such as linezolid and intravenous methylene blue) [see Drug Interactions ( 7)] . This may occur within the recommended dosage range.
Serotonin syndrome symptoms may include mental status changes (e.g., agitation, hallucinations, coma), autonomic instability (e.g., tachycardia, labile blood pressure, hyperthermia), neuromuscular aberrations (e.g., hyperreflexia, incoordination, rigidity), and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). The onset of symptoms generally occurs within several hours to a few days of concomitant use, but may occur later than that. Discontinue tramadol hydrochloride extended-release tablets if serotonin syndrome is suspected.
5.10 Increased Risk of Seizures
Seizures have been reported in patients receiving tramadol within the recommended dosage range. Spontaneous post-marketing reports indicate that seizure risk is increased with doses of tramadol above the recommended range.
Concomitant use of tramadol increases the seizure risk in patients taking: [see Drug Interactions ( 7)] .
- Selective serotonin re-uptake inhibitors (SSRIs) and Serotonin-norepinephrine re-uptake inhibitors (SNRIs) antidepressants or anorectics,
- Tricyclic antidepressants (TCAs), and other tricyclic compounds (e.g., cyclobenzaprine, promethazine, etc.),
- Other opioids,
- MAO inhibitors [see Warnings and Precautions ( 5.8), Drug Interactions ( 7)]
- Neuroleptics, or
- Other drugs that reduce the seizure threshold.
Risk of seizures may also increase in patients with epilepsy, those with a history of seizures, or in patients with a recognized risk for seizure (such as head trauma, metabolic disorders, alcohol and drug withdrawal, CNS infections).
In tramadol overdose, naloxone administration may increase the risk of seizure.
5.11 Suicide Risk
- Do not prescribe tramadol hydrochloride extended-release tablets for patients who are suicidal or addiction-prone. Consideration should be given to the use of non-narcotic analgesics in patients who are suicidal or depressed. [see Drug Abuse and Dependence ( 9.2)]
- Prescribe tramadol hydrochloride extended-release tablets with caution for patients with a history of misuse and/or are currently taking CNS-active drugs including tranquilizers, or antidepressant drugs, or alcohol in excess, and patients who suffer from emotional disturbance or depression [see Drug Interactions ( 7)] .
- Inform patients not to exceed the recommended dose and to limit their intake of alcohol [see Dosage and Administration ( 2.1), Warnings and Precautions ( 5.7, 5.8, 5.14)] .
5.12 Life-Threatening Respiratory Depression in Patients with Chronic Pulmonary Disease or in Elderly, Cachectic, or Debilitated Patients
The use of tramadol hydrochloride extended-release tablets in patients with acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment is contraindicated.
Patients with Chronic Pulmonary Disease:Tramadol hydrochloride extended-release tablets-treated patients with significant chronic obstructive pulmonary disease or cor pulmonale, and those with a substantially decreased respiratory reserve, hypoxia, hypercapnia, or pre-existing respiratory depression are at increased risk of decreased respiratory drive including apnea, even at recommended dosages of tramadol hydrochloride extended-release tablets [see Warnings and Precautions ( 5.3)] .
Elderly, Cachectic, or Debilitated Patients:Life-threatening respiratory depression is more likely to occur in elderly, cachectic, or debilitated patients because they may have altered pharmacokinetics or altered clearance compared to younger, healthier patients [see Warnings and Precautions ( 5.3)].
Regularly evaluate patients, particularly when initiating and titrating tramadol hydrochloride extended-release tablets and when tramadol hydrochloride extended-release tablets are given concomitantly with other drugs that depress respiration [see Warnings and Precautions ( 5.3, 5.6)] . Alternatively, consider the use of non-opioid analgesics in these patients.
5.13 Adrenal Insufficiency
Cases of adrenal insufficiency have been reported with opioid use, more often following greater than one month of use. Presentation of adrenal insufficiency may include non-specific symptoms and signs including nausea, vomiting, anorexia, fatigue, weakness, dizziness, and low blood pressure. If adrenal insufficiency is suspected, confirm the diagnosis with diagnostic testing as soon as possible. If adrenal insufficiency is diagnosed, treat with physiologic replacement doses of corticosteroids. Wean the patient off of the opioid to allow adrenal function to recover and continue corticosteroid treatment until adrenal function recovers. Other opioids may be tried as some cases reported use of a different opioid without recurrence of adrenal insufficiency. The information available does not identify any particular opioids as being more likely to be associated with adrenal insufficiency.
5.14 Severe Hypotension
Tramadol hydrochloride extended-release tablets may cause severe hypotension including orthostatic hypotension and syncope in ambulatory patients. There is increased risk in patients whose ability to maintain blood pressure has already been compromised by a reduced blood volume or concurrent administration of certain CNS depressant drugs (e.g., phenothiazines or general anesthetics) [see Drug Interactions ( 7)] . Regularly evaluate these patients for signs of hypotension after initiating or titrating the dosage of tramadol hydrochloride extended-release tablets. In patients with circulatory shock, tramadol hydrochloride extended-release tablets may cause vasodilation that can further reduce cardiac output and blood pressure. Avoid the use of tramadol hydrochloride extended-release tablets in patients with circulatory shock.
5.15 Risks of Use in Patients with Increased Intracranial Pressure, Brain Tumors, Head Injury, or Impaired Consciousness
In patients who may be susceptible to the intracranial effects of CO 2retention (e.g., those with evidence of increased intracranial pressure or brain tumors), tramadol hydrochloride extended-release tablets may reduce respiratory drive, and the resultant CO 2retention can further increase intracranial pressure. Monitor such patients for signs of sedation and respiratory depression, particularly when initiating therapy with tramadol hydrochloride extended-release tablets.
Opioids may also obscure the clinical course in a patient with a head injury. Avoid the use of tramadol hydrochloride extended-release tablets in patients with impaired consciousness or coma.
5.16 Risks of Use in Patients with Gastrointestinal Conditions
Tramadol hydrochloride extended-release tablets are contraindicated in patients with known or suspected gastrointestinal obstruction, including paralytic ileus.
The tramadol in tramadol hydrochloride extended-release tablets may cause spasm of the sphincter of Oddi. Opioids may cause increases in serum amylase. Regularly evaluate patients with biliary tract disease, including acute pancreatitis, for worsening symptoms.
5.17 Anaphylaxis and Other Hypersensitivity Reactions
Serious and rarely fatal hypersensitive reactions have been reported in patients receiving therapy with tramadol. When these events do occur it is often following the first dose. Other reported hypersensitivity reactions include pruritus, hives, bronchospasm, angioedema, toxic epidermal necrolysis and Stevens-Johnson syndrome. Patients with a history of hypersensitivity reactions to tramadol and other opioids may be at increased risk and therefore should not receive tramadol hydrochloride extended-release tablets. If anaphylaxis or other hypersensitivity occurs, stop administration of tramadol hydrochloride extended-release tablets immediately, discontinue tramadol hydrochloride extended-release tablets permanently, and do not rechallenge with any formulation of tramadol. Advise patients to seek immediate medical attention if they experience any symptoms of a hypersensitivity reaction [see Patient Counseling Information ( 17)] .
5.18 Withdrawal
Do not abruptly discontinue tramadol hydrochloride extended-release tablets in a patient physically dependent on opioids. When discontinuing tramadol hydrochloride extended-release tablets in a physically dependent patient, gradually taper the dosage. Rapid tapering of tramadol hydrochloride extended-release tablets in a patient physically dependent on opioids may lead to a withdrawal syndrome and return of pain [ see Dosage and Administration( 2.5), Drug Abuse and Dependence ( 9) ].
Additionally, avoid the use of mixed agonist/antagonist (e.g., pentazocine, nalbuphine, and butorphanol) or partial agonist (e.g., buprenorphine) analgesics in patients who are receiving a full opioid agonist analgesic, including tramadol hydrochloride extended-release tablets. In these patients, mixed agonist/antagonist and partial agonist analgesics may reduce the analgesic effect and/or precipitate withdrawal symptoms [ see Drug Interactions( 7)].
5.19 Risks of Driving and Operating Machinery
Tramadol hydrochloride extended-release tablets may impair the mental or physical abilities needed to perform potentially hazardous activities such as driving a car or operating machinery. Warn patients not to drive or operate dangerous machinery unless they are tolerant to the effects of tramadol hydrochloride extended-release tablets and know how they will react to the medication [see Patient Counseling Information ( 17)] .
5.20 Hyponatremia
Hyponatremia (serum sodium < 135 mmol/L) has been reported with the use of tramadol, and many cases are severe (sodium level < 120 mmol/L). Most cases of hyponatremia occurred in females over the age of 65 and within the first week of therapy. In some reports, hyponatremia resulted from the syndrome of inappropriate antidiuretic hormone secretion (SIADH). Monitor for signs and symptoms of hyponatremia (e.g., confusion, disorientation), during treatment with tramadol hydrochloride extended-release tablets, especially during initiation of therapy. If signs and symptoms of hyponatremia are present, initiate appropriate treatment (e.g., fluid restriction) and discontinue tramadol hydrochloride extended-release tablets [ seeDosage and Administration: Safe Reduction or Discontinuation of tramadol hydrochloride extended-release tablets ( 2.5)].
5.21 Hypoglycemia
Cases of tramadol- associated hypoglycemia have been reported, some resulting in hospitalization. In most cases, patients had predisposing risk factors (e.g. diabetes). If hypoglycemia is suspected, monitor blood glucose levels and consider drug discontinuation as appropriate [ seeDosage and Administration: Safe Reduction or Discontinuation of tramadol hydrochloride extended-release tablets ( 2.5)].
-
6 ADVERSE REACTIONS
The following serious adverse reactions are described in greater detail, in other sections:
- Addiction, Abuse, and Misuse [see Warnings and Precautions ( 5.1)]
- Life-Threatening Respiratory Depression [see Warnings and Precautions ( 5.2)]
- Interactions with Benzodiazepines and Other CNS Depressants [see Warnings and Precautions ( 5.3)]
- Neonatal Opioid Withdrawal Syndrome [see Warnings and Precautions ( 5.4)]
- Ultra-Rapid Metabolism of Tramadol and Other Risk Factors for Life-Threatening Respiratory Depression in Children [see Warnings and Precautions ( 5.6)]
- Opioid-Induced Hyperalgesia and Allodynia [See Warnings and Precautions ( 5.8)]
- Serotonin Syndrome [see Warnings and Precautions ( 5.9)]
- Seizures [see Warnings and Precautions ( 5.10)]
- Suicide [see Warnings and Precautions ( 5.11)]
- Adrenal Insufficiency [see Warnings and Precautions ( 5.13)]
- Severe Hypotension [see Warnings and Precautions ( 5.14)]
- Gastrointestinal Adverse Reactions [see Warnings and Precautions ( 5.16)]
- Hypersensitivity Reactions [see Warnings and Precautions ( 5.17)]
- Withdrawal [see Warnings and Precautions ( 5.18)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Tramadol hydrochloride extended-release tablet was administered to a total of 3108 patients during studies conducted in the U.S. These included four double-blind studies in patients with osteoarthritis and/or chronic low back pain and one open-label study in patients with chronic non-malignant pain. A total of 901 patients were 65 years or older. The frequency of adverse reactions generally increased with doses from 100 mg to 400 mg in the two pooled, twelve-week, randomized, double-blind, placebo-controlled studies in patients with chronic non-malignant pain (see Table 1). The most common adverse reactions from Table 1 occurring in ≥10% and ≥2 x placebo rate of the patients treated with tramadol hydrochloride extended-release tablets are dizziness (not vertigo), nausea, constipation, headache, somnolence, flushing, pruritus, vomiting, insomnia, and dry mouth.
Table 1: Incidence (%) of patients with adverse reaction rates ≥ 5% from two 12-week placebo-controlled studies in patients with moderate to moderately severe chronic pain by dose (N=1811). MedDRA Preferred Term
Tramadol Hydrochloride Extended-Release Tablets
Placebo
100 mg (N=403)
n (%)
200 mg (N=400)
n (%)
300 mg (N=400)
n (%)
400 mg (N=202)
n (%)
(N=406)
n (%)
Dizziness (not vertigo)
64 (16)
81 (20)
90 (23)
57 (28)
28 (7)
Nausea
61 (15)
90 (23)
102 (26)
53 (26)
32 (8)
Constipation
49 (12)
68 (17)
85 (21)
60 (30)
17 (4)
Headache
49 (12)
62 (16)
46 (12)
32 (16)
43 (11)
Somnolence
33 (8)
45 (11)
29 (7)
41 (20)
7 (2)
Flushing
31 (8)
40 (10)
35 (9)
32 (16)
18 (4)
Pruritus
25 (6)
34 (9)
30 (8)
24 (12)
4 (1)
Vomiting
20 (5)
29 (7)
34 (9)
19 (9)
11 ( 3)
Insomnia
26 (7)
32 (8)
36 (9)
22 (11)
13 (3)
Dry Mouth
20 (5)
29 (7)
39 (10)
18 (9)
6 (2)
Diarrhea
15 (4)
27 (7)
37 (9)
10 (5)
17 (4)
Asthenia
14 (4)
24 (6)
26 (7)
13 (6)
7 (2)
Postural hypotension
7 (2)
17 (4)
8 (2)
11 (5)
9 (2)
Sweating increased
6 (2)
8 (2)
15 (4)
13 (6)
1 (0)
Anorexia
3 (1)
7 (2)
21 (5)
12 (6)
1 (0)
Adverse reactions With Incidence Rates of 1.0% to <5.0% During Clinical Trials
The following adverse reactions were reported from all the chronic pain studies (N=3108).
The lists below include adverse reactions not otherwise noted in Table 1.
Eye disorders: vision blurred
Gastrointestinal disorders: abdominal pain upper, dyspepsia, abdominal pain, sore throat
General disorders: weakness, pain, feeling hot, influenza like illness, fall, rigors, lethargy, pyrexia, chest pain
Infections and infestations: nasopharyngitis, upper respiratory tract infection, sinusitis, influenza, gastroenteritis viral, urinary tract infection, bronchitis
Investigations: blood creatine phosphokinase increased, weight decreased
Metabolism and nutrition disorders: appetite decreased
Musculoskeletal, connective tissue and bone disorders: arthralgia, back pain, pain in limb, neck pain
Nervous system disorders: tremor, paresthesia, hypoesthesia
Psychiatric disorders: nervousness, anxiety, depression, restlessness
Respiratory, thoracic and mediastinal disorders: sneezing, cough, rhinorrhea, nasal congestion, dyspnea, sinus congestion
Skin and subcutaneous tissue disorders: sweating increased, dermatitis
Vascular disorders: hot flushes, vasodilatation
Adverse Reactions With Incidence Rates of 0.5% to <1.0% and Serious Adverse Reactions Reported in at Least 2 patients During Clinical Trials
Cardiac disorders: palpitations, myocardial infarction
Ear and labyrinth disorders: tinnitus, vertigo
Gastrointestinal disorders: flatulence, toothache, constipation aggravated, appendicitis, pancreatitis
General disorders: feeling jittery, edema lower limb, shivering, joint swelling, malaise, drug withdrawal syndrome, peripheral swelling
Hepato-biliary disorders: cholelithiasis, cholecystitis
Infections and infestations: cellulitis, ear infection, gastroenteritis, pneumonia, viral infection
Injury and poisoning: joint sprain, muscle injury
Investigations: alanine aminotransferase increased, blood pressure increased, aspartate aminotransferase increased, heart rate increased, blood glucose increased, liver function tests abnormal
Musculoskeletal, connective tissue and bone disorders: muscle cramps, muscle spasms, joint stiffness, muscle twitching, myalgia, osteoarthritis aggravated
Nervous system disorders: migraine, sedation, syncope, disturbance in attention, dizziness aggravated
Psychiatric disorders: euphoric mood, irritability, libido decreased, sleep disorder, agitation, disorientation, abnormal dreams
Renal and urinary disorders: difficulty in micturition, urinary frequency, hematuria, dysuria, urinary retention
Respiratory, thoracic and mediastinal disorders: yawning
Skin and subcutaneous tissue disorders: contusion, piloerection, clamminess, night sweats, urticaria
Vascular disorders: hypertension aggravated, hypertension, peripheral ischemia
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of tramadol. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Serotonin syndrome: Cases of serotonin syndrome, a potentially life-threatening condition, have been reported during concomitant use of opioids with serotonergic drugs.
Adrenal insufficiency: Cases of adrenal insufficiency have been reported with opioid use, more often following greater than one month of use.
Anaphylaxis: Anaphylaxis has been reported with ingredients contained in tramadol hydrochloride extended-release tablets.
Androgen deficiency: Cases of androgen deficiency have occurred with use of opioids for an extended period of time. [see Clinical Pharmacology ( 12.2)].
QT prolongation/torsade de pointes: Cases of QT prolongation and/or torsade de pointes have been reported with tramadol use. Many of these cases were reported in patients taking another drug labeled for QT prolongation, in patients with a risk factor for QT prolongation (e.g., hypokalemia), or in overdose setting.
Metabolism and nutrition disorders:
Hyponatremia: cases of severe hyponatremia and/or SIADH have been reported in patients taking tramadol, most often in females over the age of 65, and within the first week of therapy [see Warnings and Precautions ( 5.20)].
Hypoglycemia: Cases of hypoglycemia have been reported in patients taking tramadol. Most reports were in patients with predisposing risk factors, including diabetes or renal insufficiency, or in elderly patients [see Warnings and Precautions ( 5.21)].
Hyperalgesia and Allodynia: cases of hyperalgesia and allodynia have been reported with opioid therapy of any duration. [see Warnings and Precautions ( 5.8)]
-
7 DRUG INTERACTIONS
Table 2 includes clinically significant drug interactions with tramadol hydrochloride extended-release tablets.
Inhibitors of CYP2D6
Clinical Impact:
The concomitant use of tramadol hydrochloride extended-release tablets and CYP2D6 inhibitors may result in an increase in the plasma concentration of tramadol and a decrease in the plasma concentration of M1, particularly when an inhibitor is added after a stable dose of tramadol hydrochloride extended-release tablets is achieved. Since M1 is a more potent µ-opioid agonist, decreased M1 exposure could result in decreased therapeutic effects, and may result in signs and symptoms of opioid withdrawal in patients who had developed physical dependence to tramadol. Increased tramadol exposure can result in increased or prolonged therapeutic effects and increased risk for serious adverse events including seizures and serotonin syndrome.
After stopping a CYP2D6 inhibitor, as the effects of the inhibitor decline, the tramadol plasma concentration will decrease and the M1 plasma concentration will increase which could increase or prolong therapeutic effects but also increase adverse reactions related to opioid toxicity and may cause potentially fatal respiratory depression [see Clinical Pharmacology ( 12.3)] .
Intervention:
If concomitant use of a CYP2D6 inhibitor is necessary, follow patients closely for adverse reactions including opioid withdrawal, seizures, and serotonin syndrome.
If a CYP2D6 inhibitor is discontinued, consider lowering tramadol hydrochloride extended-release tablets dosage until stable drug effects are achieved. Evaluate patients at frequent intervals for adverse events including respiratory depression and sedation.
Examples
Quinidine, fluoxetine, paroxetine and bupropion
Inhibitors of CYP3A4
Clinical Impact:
The concomitant use of tramadol hydrochloride extended-release tablets and CYP3A4 inhibitors can increase the plasma concentration of tramadol and may result in a greater amount of metabolism via CYP2D6 and greater levels of M1. Follow patients closely for increased risk of serious adverse events including seizures and serotonin syndrome, and adverse reactions related to opioid toxicity including potentially fatal respiratory depression, particularly when an inhibitor is added after a stable dose of tramadol hydrochloride extended-release tablets is achieved.
After stopping a CYP3A4 inhibitor, as the effects of the inhibitor decline, the tramadol plasma concentration will decrease [see Clinical Pharmacology ( 12.3)] , resulting in decreased opioid efficacy and possibly signs and symptoms of opioid withdrawal in patients who had developed physical dependence to tramadol.
Intervention:
If concomitant use is necessary, consider dosage reduction of tramadol hydrochloride extended-release tablets until stable drug effects are achieved. Inform patients and caregivers of this potential interaction, educate them on the signs and symptoms of seizures, serotonin syndrome, and signs of respiratory depression and sedation.
If a CYP3A4 inhibitor is discontinued, consider increasing the tramadol hydrochloride extended-release tablets dosage until stable drug effects are achieved and evaluate patients at frequent intervals for signs and symptoms of opioid withdrawal.
Examples
Macrolide antibiotics (e.g., erythromycin), azole-antifungal agents (e.g. ketoconazole), protease inhibitors (e.g., ritonavir)
CYP3A4 Inducers
Clinical Impact:
The concomitant use of tramadol hydrochloride extended-release tablets and CYP3A4 inducers can decrease the plasma concentration of tramadol [see Clinical Pharmacology ( 12.3)] , resulting in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence to tramadol, [see Warnings and Precautions ( 5.7)] .
After stopping a CYP3A4 inducer, as the effects of the inducer decline, the tramadol plasma concentration will increase [see Clinical Pharmacology ( 12.3)] , which could increase or prolong both the therapeutic effects and adverse reactions, and may cause seizures and serotonin syndrome, and potentially fatal respiratory depression.
Intervention:
If concomitant use is necessary, consider increasing the tramadol hydrochloride extended-release tablets dosage until stable drug effects are achieved. Evaluate for signs of opioid withdrawal.
If a CYP3A4 inducer is discontinued, consider tramadol hydrochloride extended-release tablets dosage reduction and evaluate patients at frequent intervals for signs of respiratory depression and sedation.
Patients taking carbamazepine, a CYP3A4 inducer, may have a significantly reduced analgesic effect of tramadol. Because carbamazepine increases tramadol metabolism and because of the seizure risk associated with tramadol, concomitant administration of tramadol hydrochloride extended-release tablets and carbamazepine is not recommended.
Examples:
Rifampin, carbamazepine, phenytoin
Benzodiazepines and Other Central Nervous System (CNS) Depressants
Clinical Impact:
Due to additive pharmacologic effect, the concomitant use of benzodiazepines or other CNS depressants, including alcohol, can increase the risk of hypotension, respiratory depression, profound sedation, coma, and death.
Intervention:
Reserve concomitant prescribing of these drugs for use in patients for whom alternative Inform patients and caregivers of this potential interaction, educate them on the signs and symptoms of respiratory depression (including sedation). If concomitant use is warranted, consider prescribing naloxone for the emergency treatment of opioid overdose [see Dosage and Administration ( 2.2), Warnings and Precautions ( 5.1, 5.2, 5.3)] .
Examples:
Benzodiazepines and other sedatives/hypnotics, anxiolytics, tranquilizers, muscle relaxants, general anesthetics, antipsychotics, other opioids, alcohol.
Serotonergic Drugs
Clinical Impact:
The concomitant use of opioids with other drugs that affect the serotonergic neurotransmitter system has resulted in serotonin syndrome.
Intervention:
If concomitant use is warranted, carefully observe the patient, particularly during treatment initiation and dose adjustment. Discontinue tramadol hydrochloride extended-release tablets if serotonin syndrome is suspected.
Examples:
Selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), triptans, 5-HT3 receptor antagonists, drugs that affect the serotonin neurotransmitter system (e.g., mirtazapine, trazodone, tramadol), certain muscle relaxants (i.e., cyclobenzaprine, metaxalone), monoamine oxidase (MAO) inhibitors (those intended to treat psychiatric disorders and also others, such as linezolid and intravenous methylene blue).
Monoamine Oxidase Inhibitors (MAOIs)
Clinical Impact:
MAOI interactions with opioids may manifest as serotonin syndrome [see Warnings and Precautions ( 5.3)] or opioid toxicity (e.g., respiratory depression, coma) [see Warnings and Precautions ( 5.2)] .
Intervention:
Do not use tramadol hydrochloride extended-release tablets in patients taking MAOIs or within 14 days of stopping such treatment.
Examples:
phenelzine, tranylcypromine, linezolid
Mixed Agonist/Antagonist and Partial Agonist Opioid Analgesics
Clinical Impact:
May reduce the analgesic effect of tramadol hydrochloride extended-release tablets and/or precipitate withdrawal symptoms.
Intervention:
Avoid concomitant use.
Examples:
butorphanol, nalbuphine, pentazocine, buprenorphine
Muscle Relaxants
Clinical Impact:
Tramadol may enhance the neuromuscular blocking action of skeletal muscle relaxants and produce an increased degree of respiratory depression.
Intervention:
Because respiratory depression may be greater than otherwise expected, decrease the dosage of tramadol hydrochloride extended-release tablets and/or the muscle relaxant as necessary. Due to the risk of respiratory depression with concomitant use of skeletal muscle relaxants and opioids, consider prescribing naloxone for the emergency treatment of opioid overdose [see Dosage and Administration (2.2), Warnings and Precautions ( 5.2, 5.3)]
Examples
cyclobenzaprine, metaxalone
Diuretics
Clinical Impact:
Opioids can reduce the efficacy of diuretics by inducing the release of antidiuretic hormone.
Intervention:
Evaluate patients for signs of diminished diuresis and/or effects on blood pressure and increase the dosage of the diuretic as needed.
Anticholinergic Drugs
Clinical Impact:
The concomitant use of anticholinergic drugs may increase risk of urinary retention and/or severe constipation, which may lead to paralytic ileus.
Intervention:
Evaluate patients for signs of urinary retention or reduced gastric motility when tramadol hydrochloride extended-release tablets are used concomitantly with anticholinergic drugs.
Digoxin
Clinical Impact:
Post-marketing surveillance of tramadol has revealed rare reports of digoxin toxicity.
Intervention:
Follow patients for signs of digoxin toxicity and adjust the dosage of digoxin as needed.
Warfarin
Clinical Impact:
Post-marketing surveillance of tramadol has revealed rare reports of alteration of warfarin effect, including elevation of prothrombin times.
Intervention:
Monitor the prothrombin time of patients on warfarin for signs of an interaction and adjust the dosage of warfarin as needed.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Use of opioid analgesics for an extended period of time during pregnancy may cause neonatal opioid withdrawal syndrome [see Warnings and Precautions ( 5.4)] . Available data with tramadol hydrochloride extended-release tablets in pregnant women are insufficient to inform a drug-associated risk for major birth defects and miscarriage.
In animal reproduction studies, tramadol administration during organogenesis decreased fetal weights and reduced ossification in mice, rats, and rabbits at 1.4, 0.6, and 3.6 times the maximum recommended human daily dosage (MRHD). Tramadol decreased pup body weight and increased pup mortality at 1.2 and 1.9 times the MRHD [see Data]. Based on animal data, advise pregnant women of the potential risk to a fetus.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Fetal/Neonatal Adverse Reactions
Use of opioid analgesics for an extended period of time during pregnancy for medical or nonmedical purposes can result in physical dependence in the neonate and neonatal opioid withdrawal syndrome shortly after birth. Neonatal opioid withdrawal syndrome presents as irritability, hyperactivity and abnormal sleep pattern, high pitched cry, tremor, vomiting, diarrhea, and failure to gain weight. The onset, duration, and severity of neonatal opioid withdrawal syndrome vary based on the specific opioid used, duration of use, timing and amount of last maternal use, and rate of elimination of the drug by the newborn. Observe newborns for symptoms and signs of neonatal opioid withdrawal syndrome and manage accordingly [see Warnings and Precautions ( 5.4)] .
Neonatal seizures, neonatal withdrawal syndrome, fetal death and stillbirth have been reported with tramadol during post-approval use of tramadol immediate-release products.
Labor or Delivery
Opioids cross the placenta and may produce respiratory depression and psycho-physiologic effects in neonates. An opioid antagonist, such as naloxone, must be available for reversal of opioid-induced respiratory depression in the neonate. Tramadol hydrochloride extended-release tablets are not recommended for use in pregnant women during or immediately prior to labor, when use of shorter-acting analgesics or other analgesic techniques are more appropriate. Opioid analgesics, including tramadol hydrochloride extended-release tablets, can prolong labor through actions which temporarily reduce the strength, duration, and frequency of uterine contractions. However, this effect is not consistent and may be offset by an increased rate of cervical dilation, which tends to shorten labor. Monitor neonates exposed to opioid analgesics during labor for signs of excess sedation and respiratory depression.
Tramadol has been shown to cross the placenta. The mean ratio of serum tramadol in the umbilical veins compared to maternal veins was 0.83 for 40 women given tramadol during labor.
The effect of tramadol hydrochloride extended-release tablets, if any, on the later growth, development, and functional maturation of the child is unknown.
Data
Animal Data
Tramadol has been shown to be embryotoxic and fetotoxic in mice, (120 mg/kg), rats (25 mg/kg) and rabbits (75 mg/kg) at maternally toxic dosages, but was not teratogenic at these dose levels. These doses on a mg/m 2basis are 1.9, 0.8, and 4.9 times the maximum recommended human daily dosage (MRHD) for mouse, rat and rabbit, respectively.
No drug-related teratogenic effects were observed in progeny of mice (up to 140 mg/kg), rats (up to 80 mg/kg) or rabbits (up to 300 mg/kg) treated with tramadol by various routes. Embryo and fetal toxicity consisted primarily of decreased fetal weights, decreased skeletal ossification, and increased supernumerary ribs at maternally toxic dose levels. Transient delays in developmental or behavioral parameters were also seen in pups from rat dams allowed to deliver. Embryo and fetal lethality were reported only in one rabbit study at 300 mg/kg, a dose that would cause extreme maternal toxicity in the rabbit. The dosages listed for mouse, rat, and rabbit are 2.3, 2.6, and 19 times the MRHD, respectively.
Tramadol was evaluated in pre- and post-natal studies in rats. Progeny of dams receiving oral (gavage) dose levels of 50 mg/kg (1.6 times the MRHD) or greater had decreased weights, and pup survival was decreased early in lactation at 80 mg/kg (2.6 times the MRHD).
8.2 Lactation
Tramadol hydrochloride extended-release tablets are not recommended for obstetrical preoperative medication or for post-delivery analgesia in nursing mothers because its safety in infants and newborns has not been studied.
Tramadol and its metabolite, O-desmethyl tramadol (M1), are present in human milk. There is no information on the effects of the drug on the breastfed infant or the effects of the drug on milk production. The M1 metabolite is more potent than tramadol in mu opioid receptor binding [see Clinical Pharmacology ( 12.1)] . Published studies have reported tramadol and M1 in colostrum with administration of tramadol to nursing mothers in the early post-partum period. Women who are ultra-rapid metabolizers of tramadol may have higher than expected serum levels of M1, potentially leading to higher levels of M1 in breast milk that can be dangerous in their breastfed infants. In women with normal tramadol metabolism, the amount of tramadol secreted into human milk is low and dose-dependent. Because of the potential for serious adverse reactions, including excess sedation and respiratory depression in a breastfed infant, advise patients that breastfeeding is not recommended during treatment with tramadol hydrochloride extended-release tablets.
Clinical Considerations
If infants are exposed to tramadol hydrochloride through breast milk, they should be monitored for excess sedation and respiratory depression. Withdrawal symptoms can occur in breastfed infants when maternal administration of an opioid analgesic is stopped, or when breast-feeding is stopped.
Data
Following a single IV 100 mg dose of tramadol, the cumulative excretion in breast milk within 16 hours post dose was 100 mcg of tramadol (0.1% of the maternal dose) and 27 mcg of M1.
8.3 Females and Males of Reproductive Potential
Use of opioids for an extended period of time may cause reduced fertility in females and males of reproductive potential. It is not known whether these effects on fertility are reversible [see Adverse Reactions ( 6.2), Clinical Pharmacology ( 12.2), Nonclinical Toxicology ( 13.1)] .
8.4 Pediatric Use
The safety and effectiveness of tramadol hydrochloride extended-release tablets in pediatric patients have not been established.
Life-threatening respiratory depression and death have occurred in children who received tramadol [see Warnings and Precautions ( 5.6)] . In some of the reported cases, these events followed tonsillectomy and/or adenoidectomy, and one of the children had evidence of being an ultra-rapid metabolizer of tramadol (i.e., multiple copies of the gene for cytochrome P450 isoenzyme 2D6). Children with sleep apnea may be particularly sensitive to the respiratory depressant effects of tramadol. Because of the risk of life-threatening respiratory depression and death:
- Tramadol hydrochloride extended-release tablets are contraindicated for all children younger than 12 years of age [see Contraindications ( 4)] .
- Tramadol hydrochloride extended-release tablets are contraindicated for post-operative management in pediatric patients younger than 18 years of age following tonsillectomy and/or adenoidectomy [see Contraindications ( 4)].
- Avoid the use of tramadol hydrochloride extended-release tablets in adolescents 12 to 18 years of age who have other risk factors that may increase their sensitivity to the respiratory depressant effects of tramadol unless the benefits outweigh the risks. Risk factors include conditions associated with hypoventilation, such as postoperative status, obstructive sleep apnea, obesity, severe pulmonary disease, neuromuscular disease, and concomitant use of other medications that cause respiratory depression. [see Warnings and Precautions ( 5.6)].
8.5 Geriatric Use
Nine-hundred-one elderly (65 years of age or older) subjects were exposed to tramadol hydrochloride extended-release tablets in clinical trials. Of those subjects, 156 were 75 years of age and older. In general, higher incidence rates of adverse events were observed for patients older than 65 years of age compared with patients 65 years and younger, particularly for the following adverse events: constipation, fatigue, weakness, postural hypotension and dyspepsia. For this reason, tramadol hydrochloride extended-release tablets should be used with caution in patients over 65 years of age, and with even greater caution in patients older than 75 years of age [see Dosage and Administration ( 2.5), Clinical Pharmacology ( 12.3)] .
Respiratory depression is the chief risk for elderly patients treated with opioids, and has occurred after large initial doses were administered to patients who were not opioid-tolerant or when opioids were co-administered with other agents that depress respiration. Titrate the dosage of tramadol hydrochloride extended-release tablets slowly in geriatric patients and frequently reevaluate the patient for signs of central nervous system and respiratory depression [see Warnings and Precautions ( 5.12)] .
Tramadol is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to regularly evaluate renal function.
8.6 Hepatic Impairment
Metabolism of tramadol and M1 is reduced in patients with advanced cirrhosis of the liver. Tramadol hydrochloride extended-release tablet has not been studied in patients with severe hepatic impairment. The limited availability of dose strengths and once daily dosing of tramadol hydrochloride extended-release tablets do not permit the dosing flexibility required for safe use in patients with severe hepatic impairment (Child-Pugh Class C). Therefore, tramadol hydrochloride extended-release tablets should not be used in patients with severe hepatic impairment [see Clinical Pharmacology ( 12.3)] .
8.7 Renal Impairment
Impaired renal function results in a decreased rate and extent of excretion of tramadol and its active metabolite, M1. Tramadol hydrochloride extended-release tablet has not been studied in patients with severe renal impairment (CLcr < 30 mL/min). The limited availability of dose strengths and once daily dosing of tramadol hydrochloride extended-release tablets do not permit the dosing flexibility required for safe use in patients with severe renal impairment (Child-Pugh Class C). Therefore, tramadol hydrochloride extended-release tablets should not be used in patients with severe renal impairment [see Clinical Pharmacology ( 12.3)] .
-
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
Tramadol hydrochloride extended-release tablet contains tramadol, a scheduled IV controlled substance.
9.2 Abuse
Tramadol hydrochloride extended-release tablet contains tramadol, a substance with high potential for misuse and abuse, which can lead to the development of substance use disorder, including addiction [see Warnings and Precautions ( 5.1)].
Misuse is the intentional use, for therapeutic purposes, of a drug by an individual in a way other than prescribed by a healthcare provider or for whom it was not prescribed.
Abuse is the intentional, non-therapeutic use of a drug, even once, for its desirable psychological or physiological effects.
Drug addiction is a cluster of behavioral, cognitive, and physiological phenomena that may include a strong desire to take the drug, difficulties in controlling drug use (e.g., continuing drug use despite harmful consequences, giving a higher priority to drug use than other activities and obligations), and possible tolerance or physical dependence.
Misuse and abuse of tramadol hydrochloride extended-release tablet increases risk of overdose, which may lead to central nervous system and respiratory depression, hypotension, seizures, and death. The risk is increased with concurrent abuse of tramadol hydrochloride extended-release tablet with alcohol and other CNS depressants. Abuse of and addiction to opioids in some individuals may not be accompanied by concurrent tolerance and symptoms of physical dependence. In addition, abuse of opioids can occur in the absence of addiction.
All patients treated with opioids require careful and frequent reevaluation for signs of misuse, abuse, and addiction, because use of opioid analgesic products carries the risk of addiction even under appropriate medical use. Patients at high risk of tramadol hydrochloride extended-release tablet abuse include those with a history of prolonged use of any opioid, including products containing tramadol, those with a history of drug or alcohol abuse, or those who use tramadol hydrochloride extended-release tablet in combination with other abused drugs.
"Drug-seeking" behavior is very common in persons with substance use disorders. Drug-seeking tactics include emergency calls or visits near the end of office hours, refusal to undergo appropriate examination, testing, or referral, repeated "loss" of prescriptions, tampering with prescriptions, and reluctance to provide prior medical records or contact information for other treating healthcare provider(s). "Doctor shopping" (visiting multiple prescribers to obtain additional prescriptions) is common among people who abuse drugs and people with substance use disorder. Preoccupation with achieving adequate pain relief can be appropriate behavior in a patient with inadequate pain control.
Tramadol hydrochloride extended-release tablets, like other opioids, can be diverted for nonmedical use into illicit channels of distribution. Careful record-keeping of prescribing information, including quantity, frequency, and renewal requests, as required by state and federal law, is strongly advised.
Proper assessment of the patient, proper prescribing practices, periodic reevaluation of therapy, and proper dispensing and storage are appropriate measures that help to limit abuse of opioid drugs.
Risks Specific to Abuse of Tramadol Hydrochloride Extended-Release Tablets
Abuse of tramadol hydrochloride extended-release tablets poses a risk of overdose and death. This is increased with concurrent use of tramadol hydrochloride extended-release tablets with alcohol and/or other CNS depressants.
Tramadol hydrochloride extended-release tablets are approved for oral use only. Inappropriate intravenous, intramuscular, or subcutaneous use of tramadol hydrochloride extended-release tablets can result in death, local tissue necrosis, infection, pulmonary granulomas, increased risk of endocarditis, and valvular heart injury, and embolism.
With parenteral abuse the inactive ingredients can result in local tissue necrosis, infection, pulmonary granulomas, increased risk of endocarditis and valvular heart injury, embolism, and death. Parenteral drug abuse is commonly associated with transmission of infectious diseases such as hepatitis and HIV.
9.3 Dependence
Both tolerance and physical dependence can develop during use of opioid therapy.
Tolerance is a physiological state characterized by a reduced response to a drug after repeated administration (i.e., a higher dose of a drug is required to produce the same effect that was once obtained at a lower dose).
Physical dependence is a state that develops as a result of a physiological adaptation in response to repeated drug use, manifested by withdrawal signs and symptoms after abrupt discontinuation or a significant dose reduction of a drug.
Withdrawal also may be precipitated through the administration of drugs with opioid antagonist activity (e.g., naloxone, nalmefene), mixed agonist/antagonist analgesics (e.g., pentazocine, butorphanol, nalbuphine), or partial agonists (e.g., buprenorphine). Physical dependence may not occur to a clinically significant degree until after several days to weeks of continued opioid usage.
Do not abruptly discontinue tramadol hydrochloride extended-release tablets in a patient physically dependent on opioids. Rapid tapering of tramadol hydrochloride extended-release tablets in a patient physically dependent on opioids may lead to serious withdrawal symptoms, uncontrolled pain, and suicide. Rapid discontinuation has also been associated with attempts to find other sources of opioid analgesics, which may be confused with drug-seeking for abuse.
When discontinuing tramadol hydrochloride extended-release tablets, gradually taper the dosage using a patient specific plan that considers the following: the dose of tramadol hydrochloride extended-release tablets the patient has been taking, the duration of treatment, and the physical and psychological attributes of the patient. To improve the likelihood of a successful taper and minimize withdrawal symptoms, it is important that the opioid tapering schedule is agreed upon by the patient. In patients taking opioids for a long duration at high doses, ensure that a multimodal approach to pain management, including mental health support (if needed), is in place prior to initiating an opioid analgesic taper [see Dosage and Administration ( 2.1), Warnings and Precautions ( 5.18)].
Infants born to mothers physically dependent on opioids will also be physically dependent and may exhibit respiratory difficulties and withdrawal signs [see Use in Specific Populations ( 8.1)].
-
10 OVERDOSAGE
Acute overdosage with tramadol hydrochloride extended-release tablets can be manifested by respiratory depression, somnolence progressing to stupor or coma, skeletal muscle flaccidity, cold and clammy skin, constricted pupils, and, in some cases, pulmonary edema, bradycardia, QT prolongation, hypotension, partial or complete airway obstruction, atypical snoring, and death. Marked mydriasis rather than miosis may be seen with hypoxia in overdose situations [see Clinical Pharmacology ( 12.2)] .
Treatment of Overdose
In case of overdose, priorities are the reestablishment of a patent and protected airway and institution of assisted or controlled ventilation, if needed. Employ other supportive measures (including oxygen and vasopressors) in the management of circulatory shock and pulmonary edema as indicated. Cardiac arrest or arrhythmias will require advanced life-support measures.
Opioid antagonists, such as naloxone, are specific antidotes to respiratory depression resulting from opioid overdose. For clinically significant respiratory or circulatory depression secondary to opiod overdose, administer an opioid antagonist.
While naloxone will reverse some, but not all, symptoms caused by overdosage with tramadol, the risk of seizures is also increased with naloxone administration. In animals, convulsions following the administration of toxic doses of tramadol hydrochloride extended-release tablets could be suppressed with barbiturates or benzodiazepines but were increased with naloxone. Naloxone administration did not change the lethality of an overdose in mice.
Hemodialysis is not expected to be helpful in an overdose because it removes less than 7% of the administered dose in a 4-hour dialysis period.
Because the duration of opioid reversal is expected to be less than the duration of action of tramadol in tramadol hydrochloride extended-release tablets, carefully monitor the patient until spontaneous respiration is reliably reestablished. Tramadol hydrochloride extended-release tablets will continue to release tramadol and add to the tramadol load for 24 to 48 hours or longer following ingestion, necessitating prolonged monitoring. If the response to an opioid antagonist is suboptimal or only brief in nature, administer additional antagonist as directed by the product's prescribing information.
In an individual physically dependent on opioids, administration of the recommended usual dosage of the antagonist will precipitate an acute withdrawal syndrome. The severity of the withdrawal symptoms experienced will depend on the degree of physical dependence and the dose of the antagonist administered. If a decision is made to treat serious respiratory depression in the physically dependent patient, administration of the antagonist should be initiated with care and by titration with smaller than usual doses of the antagonist.
-
11 DESCRIPTION
Tramadol hydrochloride is an opioid agonist in an extended-release tablet formulation for oral use. The chemical name is (±) cis-2-[(dimethylamino)methyl]-1-(3-methoxyphenyl) cyclohexanol hydrochloride. Its structural formula is:
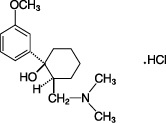
The molecular weight of tramadol HCl is 299.84. It is a white, bitter, crystalline and odorless powder that is readily soluble in water and ethanol and has a pKa of 9.41. The n-octanol/water log partition coefficient (logP) is 1.35 at pH 7.
Tramadol hydrochloride extended-release tablets USP contain 100, 200 or 300 mg of tramadol HCl in an extended-release formulation. The tablets are white to off-white in color and contain the inactive ingredients: colloidal silicon dioxide, dibutyl sebacate, ethyl cellulose, microcrystalline cellulose, povidone, and sodium stearyl fumarate.
The imprinting ink contains shellac, iron oxide black and propylene glycol.
Tramadol hydrochloride extended-release tablets USP meet USP Dissolution Test 3.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Tramadol hydrochloride extended-release tablet contains tramadol, an opioid agonist and an inhibitor of reuptake of norepinephrine and serotonin. Although the mode of action of tramadol is not completely understood, the analgesic effect of tramadol is believed to be due to both binding to µ-opioid receptors and weak inhibition of reuptake of norepinephrine and serotonin.
Opioid activity of tramadol is due to both low affinity binding of the parent compound and higher affinity binding of the O-desmethyl metabolite M1 to µ-opioid receptors. In animal models, M1 is up to 6 times more potent than tramadol in producing analgesia and 200 times more potent in µ-opioid binding. Tramadol-induced analgesia is only partially antagonized by the opioid antagonist naloxone in several animal tests. The relative contribution of both tramadol and M1 to human analgesia is dependent upon the plasma concentrations of each compound.
Tramadol has been shown to inhibit reuptake of norepinephrine and serotonin in vitro, as have some other opioid analgesics. These mechanisms may contribute independently to the overall analgesic profile of tramadol.
Apart from analgesia, tramadol administration may produce a constellation of symptoms (including dizziness, somnolence, nausea, constipation, sweating and pruritus) similar to that of other opioids. In contrast to morphine, tramadol has not been shown to cause histamine release. At therapeutic doses, tramadol has no effect on heart rate, left-ventricular function, or cardiac index. Orthostatic hypotension has been observed.
12.2 Pharmacodynamics
Effects on the Central Nervous System
Tramadol produces respiratory depression by direct action on brain stem respiratory centers. The respiratory depression involves a reduction in the responsiveness of the brain stem respiratory centers to both increases in carbon dioxide tension and electrical stimulation.
Tramadol causes miosis, even in total darkness. Pinpoint pupils are a sign of opioid overdose but are not pathognomonic (e.g., pontine lesions of hemorrhagic or ischemic origins may produce similar findings). Marked mydriasis rather than miosis may be seen due to hypoxia in overdose situations.
Effects on the Gastrointestinal Tract and Other Smooth Muscle
Tramadol causes a reduction in motility associated with an increase in smooth muscle tone in the antrum of the stomach and duodenum. Digestion of food in the small intestine is delayed and propulsive contractions are decreased. Propulsive peristaltic waves in the colon are decreased, while tone may be increased to the point of spasm, resulting in constipation. Other opioid-induced effects may include a reduction in biliary and pancreatic secretions, spasm of sphincter of Oddi, and transient elevations in serum amylase.
Effects on the Cardiovascular System
Tramadol produces peripheral vasodilation, which may result in orthostatic hypotension or syncope. Manifestations of histamine release and/or peripheral vasodilation may include pruritus, flushing, red eyes, sweating, and/or orthostatic hypotension.
The effect of oral tramadol on the QTcF interval was evaluated in a double-blind, randomized, four-way crossover, placebo- and positive- (moxifloxacin) controlled study in 68 adult male and female healthy subjects. At a 600 mg/day dose (1.5-fold the maximum immediate-release daily dose), the study demonstrated no significant effect on the QTcF interval.
Effects on the Endocrine System
Opioids inhibit the secretion of adrenocorticotropic hormone (ACTH), cortisol, and luteinizing hormone (LH) in humans [see Adverse Reactions ( 6.2)] . They also stimulate prolactin, growth hormone (GH) secretion, and pancreatic secretion of insulin and glucagon.
Use of opioids for an extended period of time may influence the hypothalamic-pituitary-gonadal axis, leading to androgen deficiency that may manifest as low libido, impotence, erectile dysfunction, amenorrhea, or infertility. The causal role of opioids in the clinical syndrome of hypogonadism is unknown because the various medical, physical, lifestyle, and psychological stressors that may influence gonadal hormone levels have not been adequately controlled for in studies conducted to date [see Adverse Reactions ( 6.2)] .
Effects on the Immune System
Opioids have been shown to have a variety of effects on components of the immune system in in vitroand animal models. The clinical significance of these findings is unknown. Overall, the effects of opioids appear to be modestly immunosuppressive.
Concentration–Efficacy Relationships
The minimum effective analgesic concentration will vary widely among patients, especially among patients who have been previously treated with opioid agonists. The minimum effective analgesic concentration of tramadol for any individual patient may increase over time due to an increase in pain, the development of a new pain syndrome, and/or the development of analgesic tolerance [see Dosage and Administration ( 2.1)] .
Concentration–Adverse Reaction Relationships
There is a relationship between increasing tramadol plasma concentration and increasing frequency of dose-related opioid adverse reactions such as nausea, vomiting, CNS effects, and respiratory depression. In opioid-tolerant patients, the situation may be altered by the development of tolerance to opioid-related adverse reactions [see Dosage and Administration ( 2.1, 2.3)] .
12.3 Pharmacokinetics
The analgesic activity of tramadol is due to both parent drug and the M1 metabolite. Tramadol hydrochloride extended-release tablet is administered as a racemate and both the [-] and [+] forms of both tramadol and M1 are detected in the circulation.
The pharmacokinetics of tramadol hydrochloride extended-release tablets are approximately dose-proportional over a 100 to 400 mg dose range in healthy subjects. The observed tramadol AUC values for the 400-mg dose were 26% higher than predicted based on the AUC values for the 200-mg dose. The clinical significance of this finding has not been studied and is not known.
Absorption
In healthy subjects, the bioavailability of a tramadol hydrochloride extended-release 200 mg tablet administered once daily relative to a 50 mg immediate-release (IR) tablet (tramadol hydrochloride) administered every six hours was approximately 85 to 90%. Consistent with the extended-release nature of the formulation, there is a lag time in drug absorption following tramadol hydrochloride extended-release tablets administration. The mean peak plasma concentrations of tramadol and M1 after administration of tramadol hydrochloride extended-release tablets to healthy volunteers are attained at about 12 h and 15 h, respectively, after dosing (see Table 3 and Figure 1). Following administration of the tramadol hydrochloride extended-release tablets, steady-state plasma concentrations of both tramadol and M1 are achieved within four days with once daily dosing.
The mean (%CV) pharmacokinetic parameter values for tramadol hydrochloride extended-release tablets 200 mg administered once daily and tramadol HCl IR (tramadol hydrochloride) 50 mg administered every six hours are provided in Table 3.
Table 3: Mean (%CV) Steady-State Pharmacokinetic Parameter Values (n=32) Tramadol
M1 Metabolite
Pharmacokinetic Parameter
Tramadol Hydrochloride Extended-Release
200-mg Tablet Once-Daily
Tramadol Hydrochloride
50-mg Tablet Every 6 Hours
Tramadol Hydrochloride Extended-Release
200-mg Tablet Once-Daily
Tramadol Hydrochloride
50-mg Tablet Every 6 Hours
AUC 0 to 24(ng∙h/mL)
5975 (34)
6613 (27)
1890 (25)
2095 (26)
C max(ng/mL)
335 (35)
383 (21)
95 (24)
104 (24)
C min(ng/mL)
187 (37)
228 (32)
69 (30)
82 (27)
T max(h)
12 (27)
1.5 (42)
15 (27)
1.9 (57)
% Fluctuation
61 (57)
59 (35)
34 (72)
26 (47)
AUC 0 to 24: Area Under the Curve in a 24-hour dosing interval; C max: Peak Concentration in a 24- hour dosing interval; C min: Trough Concentration in a 24-hour dosing interval; T max: Time to Peak Concentration
Figure 1: Mean Steady-State Tramadol (a) and M1 (b) Plasma Concentrations on Day 8 Post Dose after Administration of 200 mg Tramadol Hydrochloride Extended-Release Tablets Once-Daily and 50 mg Tramadol Hydrochloride Tablets Every 6 Hours.
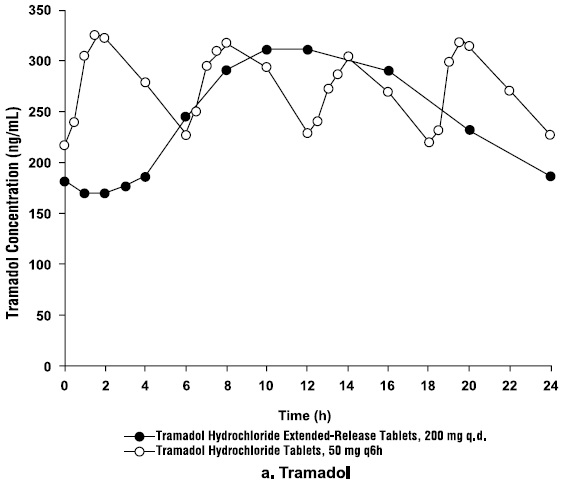
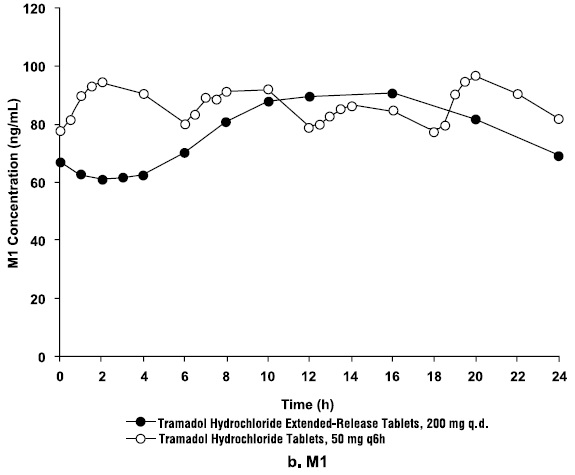
After a single dose administration of 200 mg tramadol hydrochloride extended-release tablet with a high fat meal, the C maxand AUC 0 to ∞of tramadol decreased 28% and 16%, respectively, compared to fasting conditions. Mean T maxwas increased by 3 hr (from 14 hr under fasting conditions to 17 hr under fed conditions). While tramadol hydrochloride extended-release tablets may be taken without regard to food, it is recommended that it be taken in a consistent manner [see Dosage and Administration ( 2.1)] .
Distribution
The volume of distribution of tramadol was 2.6 and 2.9 L/kg in male and female subjects, respectively, following a 100-mg intravenous dose. The binding of tramadol to human plasma proteins is approximately 20% and binding also appears to be independent of concentration up to 10 mcg/mL. Saturation of plasma protein binding occurs only at concentrations outside the clinically relevant range.
Elimination
Tramadol is eliminated primarily through metabolism by the liver and the metabolites are eliminated primarily by the kidneys. The mean terminal plasma elimination half-lives of racemic tramadol and racemic M1 after administration of tramadol hydrochloride extended-release tablets are approximately 7.9 and 8.8 hours, respectively.
Metabolism
Tramadol is extensively metabolized after oral administration. The metabolic pathways appear to be N – demethylation (mediated by CYP3A4 and CYP2D6), O – demethylation (mediated by CYP2D6) and glucuronidation or sulfation in the liver. The CYP2D6 metabolite, O-desmethyl tramadol, (denoted M1) is observed to be 6 times more potent than tramadol in producing analgesia and 200 times more potent in µ-opioid binding in animal models.
Excretion
Approximately 30% of the dose is excreted in the urine as unchanged drug, whereas 60% of the dose is excreted as metabolites. The remainder is excreted either as unidentified or as unextractable metabolites.
Special Populations
Hepatic Impairment
Pharmacokinetics of tramadol was studied in patients with mild or moderate hepatic impairment after receiving multiple doses of tramadol hydrochloride extended-release tablets 100 mg. The exposure of (+)- and (-)-tramadol was similar in mild and moderate hepatic impairment patients in comparison to patients with normal hepatic function. However, exposure of active metabolite (+)- and (-)-M1 decreased ~50% with increased severity of the hepatic impairment (from normal to mild and moderate). The pharmacokinetics of tramadol after the administration of tramadol hydrochloride extended-release tablets has not been studied in patients with severe hepatic impairment (Child-Pugh Class C). After the administration of tramadol IR tablets to patients with advanced cirrhosis of the liver, tramadol exposure was increased and the tramadol and M1 half-lives were longer than patients with normal hepatic function [see Use in Specific Populations ( 8.6)] .
Renal Impairment
Impaired renal function results in a decreased rate and extent of excretion of tramadol and its active metabolite, M1. The pharmacokinetics of tramadol were studied in patients with mild or moderate renal impairment after receiving multiple doses of tramadol hydrochloride extended-release tablets 100 mg. There is no consistent trend observed for tramadol exposure related to renal function in patients with mild (CLcr: 50 to 80 mL/min) or moderate (CLcr: 30 to 50 mL/min) renal impairment in comparison to patients with normal renal function. However, exposure of M1 increased 20 to 40% with increased severity of the renal impairment (from normal to mild and moderate). Tramadol hydrochloride extended-release tablet has not been studied in patients with severe renal impairment (CLcr < 30 mL/min). The total amount of tramadol and M1 removed during a 4-hour dialysis period is less than 7% of the administered dose [see Use in Specific Populations ( 8.7)].
Sex
Based on pooled multiple-dose pharmacokinetics studies for tramadol hydrochloride extended-release tablets in 166 healthy subjects (111 males and 55 females), the dose-normalized AUC values for tramadol were somewhat higher in females than in males. There was a considerable degree of overlap in values between male and female groups. Dosage adjustment based on sex is not recommended.
Age: Geriatric Population
The effect of age on pharmacokinetics of tramadol hydrochloride extended-release tablet has not been studied. Healthy elderly subjects aged 65 to 75 years administered an immediate-release formulation of tramadol, have plasma concentrations and elimination half-lives comparable to those observed in healthy subjects younger than 65 years of age. In subjects over 75 years, mean maximum plasma concentrations are elevated (208 vs. 162 ng/mL) and the mean elimination half-life is prolonged (7 vs. 6 hours) compared to subjects 65 to 75 years of age. Adjustment of the daily dose is recommended for patients older than 75 years [see Dosage and Administration ( 2.4].
Drug Interaction Studies
Potential for Tramadol to Affect Other Drugs
In vitrostudies indicate that tramadol is unlikely to inhibit the CYP3A4-mediated metabolism of other drugs when tramadol is administered concomitantly at therapeutic doses. Tramadol does not appear to induce its own metabolism in humans, since observed maximal plasma concentrations after multiple oral doses are higher than expected based on single-dose data.
Poor/Extensive Metabolizers, CYP2D6
The formation of the active metabolite, M1, is mediated by CYP2D6, a polymorphic enzyme. Approximately 7% of the population has reduced activity of the CYP2D6 isoenzyme of cytochrome P450 metabolizing enzyme system. These individuals are "poor metabolizers" of debrisoquine, dextromethorphan and tricyclic antidepressants, among other drugs. Based on a population PK analysis of Phase 1 studies with IR tablets in healthy subjects, concentrations of tramadol were approximately 20% higher in "poor metabolizers" versus "extensive metabolizers," while M1 concentrations were 40% lower.
CYP2D6 Inhibitors
In vitrodrug interaction studies in human liver microsomes indicate that concomitant administration with inhibitors of CYP2D6 such as fluoxetine, paroxetine, and amitriptyline could result in some inhibition of the metabolism of tramadol.
Quinidine
Tramadol is metabolized to active metabolite M1 by CYP2D6. Coadministration of quinidine, a selective inhibitor of CYP2D6, with tramadol hydrochloride extended-release tablets resulted in a 50 to 60% increase in tramadol exposure and a 50 to 60% decrease in M1 exposure. The clinical consequences of these findings are unknown.
To evaluate the effect of tramadol, a CYP2D6 substrate on quinidine, an in vitrodrug interaction study in human liver microsomes was conducted. The results from this study indicate that tramadol has no effect on quinidine metabolism [see Warnings and Precautions ( 5.7), Drug Interactions ( 7)] .
CYP3A4 Inhibitors and Inducers
Since tramadol is also metabolized by CYP3A4, administration of CYP3A4 inhibitors, such as ketoconazole and erythromycin, or CYP3A4 inducers, such as rifampin and St. John's Wort, with tramadol hydrochloride extended-release tablets may affect the metabolism of tramadol leading to altered tramadol exposure [see Warnings and Precautions ( 5.7), Drug Interactions ( 7)] .
Cimetidine
Concomitant administration of tramadol IR tablets with cimetidine, a weak CYP3A4 inhibitor, does not result in clinically significant changes in tramadol pharmacokinetics. No alteration of the tramadol hydrochloride extended-release tablets dosage regimen with cimetidine is recommended.
Carbamazepine
Carbamazepine, a CYP3A4 inducer, increases tramadol metabolism. Patients taking carbamazepine may have a significantly reduced analgesic effect of tramadol. Concomitant administration of tramadol hydrochloride extended-release tablets and carbamazepine is not recommended.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity assessment has been conducted in mice, rats and p53(+/-) heterozygous mice. A slight but statistically significant increase in two common murine tumors, pulmonary and hepatic, was observed in an NMRI mouse carcinogenicity study, particularly in aged mice. Mice were dosed orally up to 30 mg/kg in the drinking water (0.5 times the maximum recommended daily human dosage or MRHD) for approximately two years, although the study was not done with the Maximum Tolerated Dose. This finding is not believed to suggest risk in humans.
No evidence of carcinogenicity was noted in a rat 2-year carcinogenicity study testing oral doses of up to 30 mg/kg in the drinking water (1 times the MRHD). In a second rat study, no evidence of carcinogenicity was noted in rats at oral doses up to 75 mg/kg/day for males and 100 mg/kg/day for females (approximately 2-fold the maximum recommended human daily dose MRHD) for two years. However, the excessive decrease in body weight gain observed in the rat study might have reduced their sensitivity to any potential carcinogenic effect of the drug. No carcinogenic effect of tramadol was observed in p53(+/–)-heterozygous mice at oral doses up to 150 mg/kg/day for 26 weeks.
Mutagenesis
Tramadol was mutagenic in the presence of metabolic activation in the mouse lymphoma assay. Tramadol was not mutagenic in the in vitrobacterial reverse mutation assay using Salmonellaand E. coli(Ames), the mouse lymphoma assay in the absence of metabolic activation, the in vitrochromosomal aberration assay, or the in vivomicronucleus assay in bone marrow.
Impairment of Fertility
No effects on fertility were observed for tramadol at oral dose levels up to 50 mg/kg in male rats and 75 mg/kg in female rats. These dosages are 1.2 and 1.8 times the maximum recommended human daily dose based on body surface area, respectively.
-
14 CLINICAL STUDIES
Tramadol hydrochloride extended-release tablets were studied in patients with chronic, moderate to moderately severe pain due to osteoarthritis and/or low back pain in four 12-week, randomized, double-blind, placebo- controlled trials. To qualify for inclusion into these studies, patients were required to have moderate to moderately severe pain as defined by a pain intensity score of ≥40 mm, off previous medications, on a 0 to 100 mm visual analog scale (VAS). Adequate evidence of efficacy was demonstrated in the following two studies:
Study 1: Osteoarthritis of the Knee and/or Hip
In one 12-week randomized, double-blind, placebo-controlled study, patients with moderate to moderately severe pain due to osteoarthritis of the knee and/or hip were administered doses from 100 mg to 400 mg daily. Treatment was initiated at 100 mg QD for four days then increased by 100 mg per day increments every five days to the randomized fixed dose. Between 51% and 59% of patients in the tramadol hydrochloride extended-release tablets treatment groups completed the study and 56% of patients in the placebo group completed the study. Discontinuations due to adverse events were more common in the tramadol hydrochloride extended-release tablets 200 mg, 300 mg and 400 mg treatment groups (20%, 27%, and 30% of discontinuations, respectively) compared to 14% of the patients treated with tramadol hydrochloride extended-release tablets 100 mg and 10% of patients treated with placebo.
Pain, as assessed by the WOMAC Pain subscale, was measured at 1, 2, 3, 6, 9, and 12 weeks and change from baseline assessed. A responder analysis based on the percent change in WOMAC Pain subscale demonstrated a statistically significant improvement in pain for the 100 mg and 200 mg treatment groups compared to placebo (see Figure 2).
Figure 2
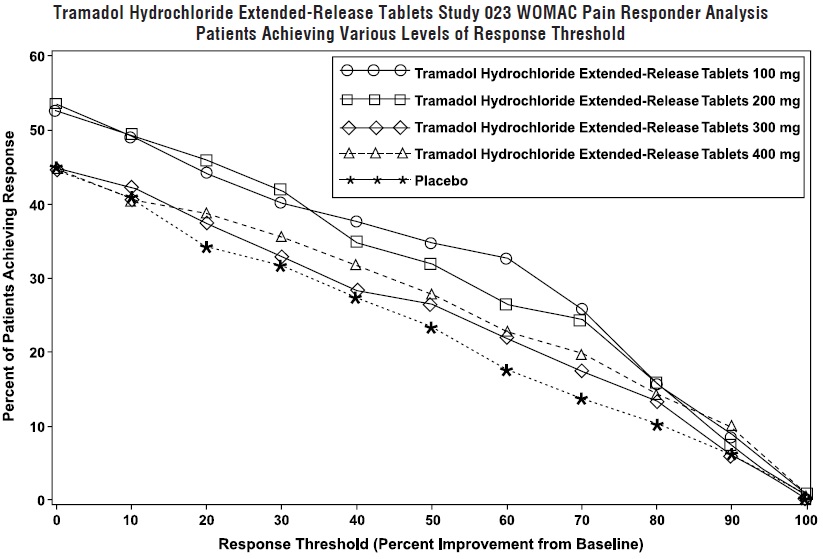
Study 2: Osteoarthritis of the Knee
In one 12-week randomized, double-blind, placebo-controlled flexible-dosing trial of tramadol hydrochloride extended-release tablets in patients with osteoarthritis of the knee, patients titrated to an average daily tramadol hydrochloride extended-release tablets dose of approximately 270 mg/day. Forty-nine percent of patients randomized to tramadol hydrochloride extended-release tablets completed the study, while 52% of patients randomized to placebo completed the study. Most of the early discontinuations in the tramadol hydrochloride extended-release tablets treatment group were due to adverse events, accounting for 27% of the early discontinuations in contrast to 7% of the discontinuations from the placebo group. Thirty-seven percent of the placebo-treated patients discontinued the study due to lack of efficacy compared to 15% of tramadol hydrochloride extended-release tablets-treated patients. The tramadol hydrochloride extended-release tablets group demonstrated a statistically significant decrease in the mean VAS score, and a statistically significant difference in the responder rate, based on the percent change from baseline in the VAS score, measured at 1, 2, 4, 8, and 12 weeks, between patients receiving tramadol hydrochloride extended-release tablets and placebo (see Figure 3).
Figure 3
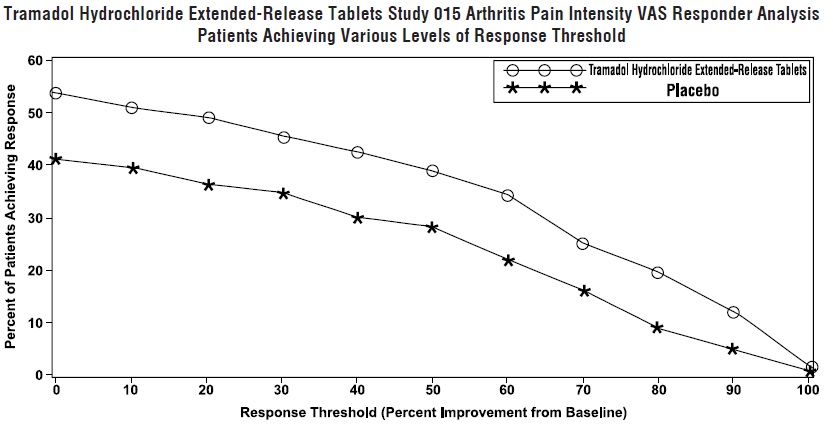
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Tramadol hydrochloride extended-release tablets USP are supplied in the following package and dose strength forms:
100 mg tablets (white to off-white circular, biconvex, beveled edge, coated) imprinted with 'L010' on one side and plain on the other side.
Bottles of 30 tablets: NDC: 68180-697-06
Bottles of 100 tablets: NDC: 68180-697-01
Bottles of 500 tablets: NDC: 68180-697-02
200 mg tablets (white to off-white circular, biconvex, beveled edge, coated) imprinted with 'L011' on one side and plain on the other side.
Bottles of 30 tablets: NDC: 68180-698-06
Bottles of 100 tablets: NDC: 68180-698-01
Bottles of 500 tablets: NDC: 68180-698-02
300 mg tablets (white to off-white circular, biconvex, beveled edge, coated) imprinted with 'L012' on one side and plain on the other side
Bottles of 30 tablets: NDC: 68180-699-06
Bottles of 100 tablets: NDC: 68180-699-01
Store at 25°C (77°F); excursions permitted to 15° to 30°C (59° to 86°F) [see USP Controlled Room Temperature].
Store tramadol hydrochloride extended release tablets securely and dispose of properly [ see Patient Counseling Information ( 17) ].
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Storage and Disposal:
Because of the risks associated with accidental ingestion, misuse, and abuse, advise patients to store tramadol hydrochloride extended-release tablets securely, out of sight and reach of children, and in a location not accessible by others, including visitors to the home .Inform patients that leaving tramadol hydrochloride extended-release tablets unsecured can pose a deadly risk to others in the home. [see Warnings and Precautions ( 5.1), Drug Abuse and Dependence ( 9)]
Advise patients and caregivers that when medicines are no longer needed, they should be disposed of promptly. Inform patients that medicine take-back options are the preferred way to safely dispose of most types of unneeded medicines. If no take back programs or DEA-registered collectors are available, instruct patients to dispose of tramadol hydrochloride extended-release tablets by following these four steps:
- Mix tramadol hydrochloride extended-release tablets (do not crush) with an unpalatable substance such as dirt, cat litter, or used coffee grounds;
- Place the mixture in a container such as a sealed plastic bag;
- Throw the container in the household trash;
- Delete all personal information on the prescription label of the empty bottle
Inform patients that they can visit www.fda.gov/drugdisposal for additional information on disposal of unused medicines.
Addiction, Abuse, and Misuse
Inform patients that the use of tramadol hydrochloride extended-release tablets, even when taken as recommended, can result in addiction, abuse, and misuse, which can lead to overdose and death [see Warnings and Precautions ( 5.1)]. Instruct patients not to share tramadol hydrochloride extended-release tablets with others and to take steps to protect tramadol hydrochloride extended-release tablets from theft or misuse.
Life-Threatening Respiratory Depression
Inform patients of the risk of life-threatening respiratory depression, including information that the risk is greatest when starting tramadol hydrochloride extended-release tablets or when the dosage is increased, and that it can occur even at recommended dosages. Advise patients how to recognize respiratory depression and to seek medical attention if breathing difficulties develop.
Educate patients and caregivers on how to recognize respiratory depression and emphasize the importance of calling 911 or getting emergency medical help right away in the event of a known or suspected overdose [see Warnings and Precautions ( 5.2)].
Accidental Ingestion (or Exposure)
Inform patients that accidental ingestion (or exposure), especially by (or in) children, may result in respiratory depression or death [see Warnings and Precautions( 5.1)] . Instruct patients to take steps to store tramadol hydrochloride extended-release tablets securely and to dispose of unused tramadol hydrochloride extended-release tablets in accordance with the local state guidelines and/or regulations.
Interactions with Benzodiazepines and Other CNS Depressants
Inform patients and caregivers that potentially fatal additive effects may occur if tramadol hydrochloride extended-release tablets are used with benzodiazepines or other CNS depressants, including alcohol, and not to use these concomitantly unless supervised by a healthcare provider [see Warnings and Precautions ( 5.3), Drug Interactions ( 7)].
Patient Access to Naloxone for the Emergency Treatment of Opioid Overdose
Discuss with the patient and caregiver the availability of naloxone for the emergency treatment of opioid overdose, both when initiating and renewing treatment with tramadol hydrochloride extended release tablets. Inform patients and caregivers about the various ways to obtain naloxone as permitted by individual state naloxone dispensing and prescribing requirements or guidelines (e.g., by prescription, directly from a pharmacist, or as part of a community-based program) [see Dosage and Administration ( 2.2), Warnings and Precautions ( 5.2)].
Educate patients and caregivers on how to recognize the signs and symptoms of an overdose.
Explain to patients and caregivers that naloxone's effects are temporary, and that they must call 911 or get emergency medical help right away in all cases of known or suspected opioid overdose, even if naloxone is administered [see Overdosage ( 10)].
If naloxone is prescribed, also advise patients and caregivers:
How to treat with naloxone in the event of an opioid overdose
To tell family and friends about their naloxone and to keep it in a place where family and friends can access it in an emergency
To read the Patient Information (or other educational material) that will come with their naloxone. Emphasize the importance of doing this before an opioid emergency happens, so the patient and caregiver will know what to do.
Ultra-Rapid Metabolism of Tramadol and Other Risk Factors for Life-threatening Respiratory Depression in Children
Advise caregivers that tramadol hydrochloride extended-release tablets are contraindicated in children younger than 12 years of age and in children younger than 18 years of age following tonsillectomy and/or adenoidectomy. Advise caregivers of children 12 to 18 years of age receiving tramadol hydrochloride extended-release tablets to monitor for signs of respiratory depression [see Warnings and Precautions ( 5.6)].
Hyperalgesia and Allodynia
Inform patients and caregivers not to increase opioid dosage without first consulting a clinician. Advise patients to seek medical attention if they experience symptoms of hyperalgesia, including worsening pain, increased sensitivity to pain, or new pain [see Warnings and Precautions ( 5.21); Adverse Reactions ( 6.2)] .
Serotonin Syndrome
Inform patients that tramadol could cause a rare but potentially life-threatening condition, particularly during concomitant use with serotonergic drugs. Warn patients of the symptoms of serotonin syndrome and to seek medical attention right away if symptoms develop. Instruct patients to inform their healthcare provider if they are taking, or plan to take serotonergic medications [see Warnings and Precautions ( 5.9), Drug Interactions ( 7)].
Seizures
Inform patients that tramadol hydrochloride extended-release tablets may cause seizures with concomitant use of serotonergic agents (including SSRIs, SNRIs, and triptans) or drugs that significantly reduce the metabolic clearance of tramadol [see Warnings and Precautions ( 5.10)].
MAOI Interaction
Inform patients not to take tramadol hydrochloride extended-release tablets while using any drugs that inhibit monoamine oxidase. Patients should not start MAOIs while taking tramadol hydrochloride extended-release tablets [see Drug Interactions ( 7)].
Important Administration Instructions
Instruct patients how to properly take tramadol hydrochloride extended-release tablets, including the following:
- Tramadol hydrochloride extended-release tablets are designed to work properly only if swallowed intact. Taking cut, broken, chewed, crushed, or dissolved tramadol hydrochloride extended-release tablets can result in a fatal overdose [see Dosage and Administration ( 2.1)].
- Advise patients not to exceed the single-dose and 24-hour dose limit and the time interval between doses, since exceeding these recommendations can result in respiratory depression, seizures, hepatic toxicity, and death. [see Dosage and Administration ( 2.1)].
- Do not discontinue tramadol hydrochloride extended-release tablets without first discussing the need for a tapering regimen with the prescriber [see Dosage and Administration ( 2.5)].
Important Discontinuation Instructions
In order to avoid developing withdrawal symptoms, instruct patients not to discontinue tramadol hydrochloride extended-release tablets without first discussing a tapering plan with the prescriber [see Dosage and Administration ( 2.5)]
Driving or Operating Heavy Machinery
Inform patients that tramadol hydrochloride extended-release tablets may impair the ability to perform potentially hazardous activities such as driving a car or operating heavy machinery. Advise patients not to perform such tasks until they know how they will react to the medication [see Warnings and Precautions ( 5.19)].
Constipation
Advise patients of the potential for severe constipation, including management instructions and when to seek medical attention [see Adverse Reactions ( 6), Clinical Pharmacology ( 12.1)].
Adrenal Insufficiency
Inform patients that opioids could cause adrenal insufficiency, a potentially life-threatening condition. Adrenal insufficiency may present with non-specific symptoms and signs such as nausea, vomiting, anorexia, fatigue, weakness, dizziness, and low blood pressure. Advise patients to seek medical attention if they experience a constellation of these symptoms [see Warnings and Precautions ( 5.13)].
Hypotension
Inform patients that tramadol hydrochloride extended-release tablets may cause orthostatic hypotension and syncope. Instruct patients how to recognize symptoms of low blood pressure and how to reduce the risk of serious consequences should hypotension occur (e.g., sit or lie down, carefully rise from a sitting or lying position) [see Warnings and Precautions ( 5.14)].
Anaphylaxis
Inform patients that anaphylaxis has been reported with ingredients contained in tramadol hydrochloride extended-release tablets. Advise patients how to recognize such a reaction and when to seek medical attention [see Contraindications ( 4), Warnings and Precautions ( 5.17), Adverse Reactions ( 6)].
Pregnancy
Neonatal Opioid Withdrawal Syndrome
Inform female patients of reproductive potential that use of tramadol hydrochloride extended-release tablets for an extended period of time during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated [see Warnings and Precautions ( 5.4), Use in Specific Populations ( 8.1)].
Embryo-Fetal Toxicity
Inform female patients of reproductive potential that tramadol hydrochloride extended-release tablets can cause fetal harm and to inform their healthcare provider of a known or suspected pregnancy [see Use in Specific Populations ( 8.1)].
Lactation
Advise nursing mothers to carefully observe infants for increased sleepiness (more than usual), breathing difficulties, or limpness. Instruct nursing mothers to seek immediate medical care if they notice these signs [see Use in Specific Populations ( 8.2)].
Infertility
Inform patients that use of opioids for an extended period of time may cause reduced fertility. It is not known whether these effects on fertility are reversible [see Adverse Reactions ( 6.2), Use in Specific Populations ( 8.3)].
Manufactured for:
Lupin Pharmaceuticals, Inc.
Baltimore, Maryland 21202
United States
Manufactured by:
Lupin Limited
Pithampur (M.P.) - 454 775
INDIA
Revised: January 2024 ID#: 274624
-
MEDICATION GUIDE
Tramadol Hydrochloride Extended-Release Tablets , CIV
(tram' a dol hye'' droe klor' ide)
Tramadol hydrochloride extended-release tablets are:
- A strong prescription pain medicine that contains an opioid (narcotic) that is used to manage severe and persistent pain that requires an extended treatment period with a daily opioid pain medicine, when other pain medicines do not treat your pain well enough or you cannot tolerate them.
- A long-acting (extended-release) opioid pain medicine that can put you at risk for overdose and death. Even if you take your dose correctly as prescribed you are at risk for opioid addiction, abuse, and misuse that can lead to death.
- Not to be taken on an "as needed" basis.
Important information about tramadol hydrochloride extended-release tablets:
- Get emergency help or call 911 right away if you take too much tramadol hydrochloride extended-release tablets (overdose).When you first start taking tramadol hydrochloride extended-release tablets, when your dose is changed, or if you take too much (overdose), serious or life-threatening breathing problems that can lead to death may occur. Talk to your healthcare provider about naloxone, a medicine for the emergency treatment of an opioid overdose.
- Taking tramadol hydrochloride extended-release tablets with other opioid medicines, benzodiazepines, alcohol, or other central nervous system depressants (including street drugs) can cause severe drowsiness, decreased awareness, breathing problems, coma, and death.
- Never give anyone else your tramadol hydrochloride extended-release tablets. They could die from taking it. Selling or giving away tramadol hydrochloride extended-release tablets is against the law.
- Store tramadol hydrochloride extended-release tablets securely, out of sight and reach of children, and in a location not accessible by others, including visitors to the home.
Important Information Guiding Use in Pediatric Patients:
- Do not give tramadol hydrochloride extended-release tablets to a child younger than 12 years of age.
- Do not give tramadol hydrochloride extended-release tablets to a child younger than 18 years of age after surgery to remove the tonsils and/or adenoids.
- Avoid giving tramadol hydrochloride extended-release tablets to children between 12 to 18 years of age who have risk factors for breathing problems such as obstructive sleep apnea, obesity, or underlying lung problems.
Do not take tramadol hydrochloride extended-release tablets if you have:
- severe asthma, trouble breathing, or other lung problems.
- a bowel blockage or have narrowing of the stomach or intestines.
Before taking tramadol hydrochloride extended-release tablets, tell your healthcare provider if you have a history of:
- head injury, seizures
- problems urinating
- abuse of street or prescription drugs, alcohol addiction, opioid overdose, or mental health problems.
- liver, kidney, thyroid problems
- pancreas or gallbladder problems
Tell your healthcare provider if you are:
- noticing your pain getting worse. If your pain gets worse after you take tramadol hydrochloride extended-release tablets, do not take more of tramadol hydrochloride extended-release tablets without first talking to your healthcare provider. Talk to your healthcare provider if the pain that you have increases, if you feel more sensitive to pain, or if you have new pain after taking tramadol hydrochloride extended-release tablets.
- Are pregnant or planning to become pregnant. Use of tramadol hydrochloride extended-release tablets for an extended period of time during pregnancy can cause withdrawal symptoms in your newborn baby that could be life-threatening if not recognized and treated.
- breastfeeding. Tramadol hydrochloride passes into breast milk and may harm your baby. Carefully observe infants for increased sleepiness (more than usual), breathing difficulties, or limpness. Seek immediate medical care if you notice these signs.
- living in a household where there are small children or someone who has abused street or prescription drugs
- taking prescription or over-the-counter medicines, vitamins, or herbal supplements. Taking tramadol hydrochloride extended-release tablets with certain other medicines can cause serious side effects that could lead to death.
When taking tramadol hydrochloride extended-release tablets:
- Do not change your dose. Take tramadol hydrochloride extended-release tablets exactly as prescribed by your healthcare provider. Use the lowest dose possible for the shortest time needed.
- Take your prescribed dose once a day at the same time every day as needed for pain. Do not take more than your prescribed dose. If you miss a dose, take your next dose at your usual time.
- Swallow tramadol hydrochloride extended-release tablets whole. Do not cut, break, chew, crush, dissolve, snort, or inject tramadol hydrochloride extended-release tablets because this may cause you to overdose and die.
- Call your healthcare provider if the dose you are taking does not control your pain.
- Do not stop taking tramadol hydrochloride extended-release tablets without talking to your healthcare provider.
- Dispose of expired, unwanted, or unused tramadol hydrochloride extended-release tablets by taking your drug to an authorized DEA-registered collector or drug take-back program. If one is not available, you can dispose of tramadol hydrochloride extended-release tablets by mixing the product with dirt, cat litter, or coffee grounds; placing the mixture in a sealed plastic bag, and throwing the bag in your trash. Visit www.fda.gov/drugdisposal for additional information on disposal of unused medicines.
While taking tramadol hydrochloride extended-release tablets DO NOT:
- Drive or operate heavy machinery, until you know how tramadol hydrochloride extended-release tablet affects you. Tramadol hydrochloride extended-release tablets can make you sleepy, dizzy, or lightheaded.
- Drink alcohol or use prescription or over-the-counter medicines that contain alcohol. Using products containing alcohol during treatment with tramadol hydrochloride extended-release tablets may cause you to overdose and die.
The possible side effects of tramadol hydrochloride extended-release tablets:
- constipation, nausea, sleepiness, vomiting, tiredness, headache, dizziness, abdominal pain, seizure. Call your healthcare provider if you have any of these symptoms and they are severe.
Get emergency medical help or call 911 right away if you have:
- trouble breathing, shortness of breath, fast heartbeat, chest pain, swelling of your face, tongue, or throat, extreme drowsiness, light-headedness when changing positions, feeling faint, agitation, high body temperature, trouble walking, stiff muscles, or mental changes such as confusion.
These are not all the possible side effects of tramadol hydrochloride extended-release tablets. Call your healthcare provider for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. For more information go to fda.reportor www.lupinpharmaceuticals.com or call Lupin Pharmaceuticals, Inc. at 1-800-399-2561.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Manufactured for:
Lupin Pharmaceuticals, Inc.
Baltimore, Maryland 21202
United States
Manufactured by:
Lupin Limited
Pithampur (M.P.) - 454 775
INDIA
Revised: January 2024 ID#: 274625
- Bottle of 30
-
INGREDIENTS AND APPEARANCE
TRAMADOL HYDROCHLORIDE
tramadol hydrochloride tablet, extended releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 45865-184(NDC:68180-699) Route of Administration ORAL DEA Schedule CIV Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TRAMADOL HYDROCHLORIDE (UNII: 9N7R477WCK) (TRAMADOL - UNII:39J1LGJ30J) TRAMADOL HYDROCHLORIDE 300 mg Inactive Ingredients Ingredient Name Strength CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) DIBUTYL SEBACATE (UNII: 4W5IH7FLNY) ETHYLCELLULOSES (UNII: 7Z8S9VYZ4B) FERROSOFERRIC OXIDE (UNII: XM0M87F357) POVIDONE (UNII: FZ989GH94E) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) SHELLAC (UNII: 46N107B71O) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) SODIUM STEARYL FUMARATE (UNII: 7CV7WJK4UI) Product Characteristics Color white (white to off-white) Score no score Shape ROUND (biconvex) Size 10mm Flavor Imprint Code L012 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 45865-184-30 30 in 1 BOTTLE; Type 0: Not a Combination Product 05/28/2021 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA200503 08/19/2014 Labeler - Medsource Pharmaceuticals (833685915) Registrant - LUPIN LIMITED (675923163) Establishment Name Address ID/FEI Business Operations LUPIN LIMITED 863645527 manufacture(45865-184) , pack(45865-184) Establishment Name Address ID/FEI Business Operations Medsource Pharmaceuticals 833685915 relabel(45865-184)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.