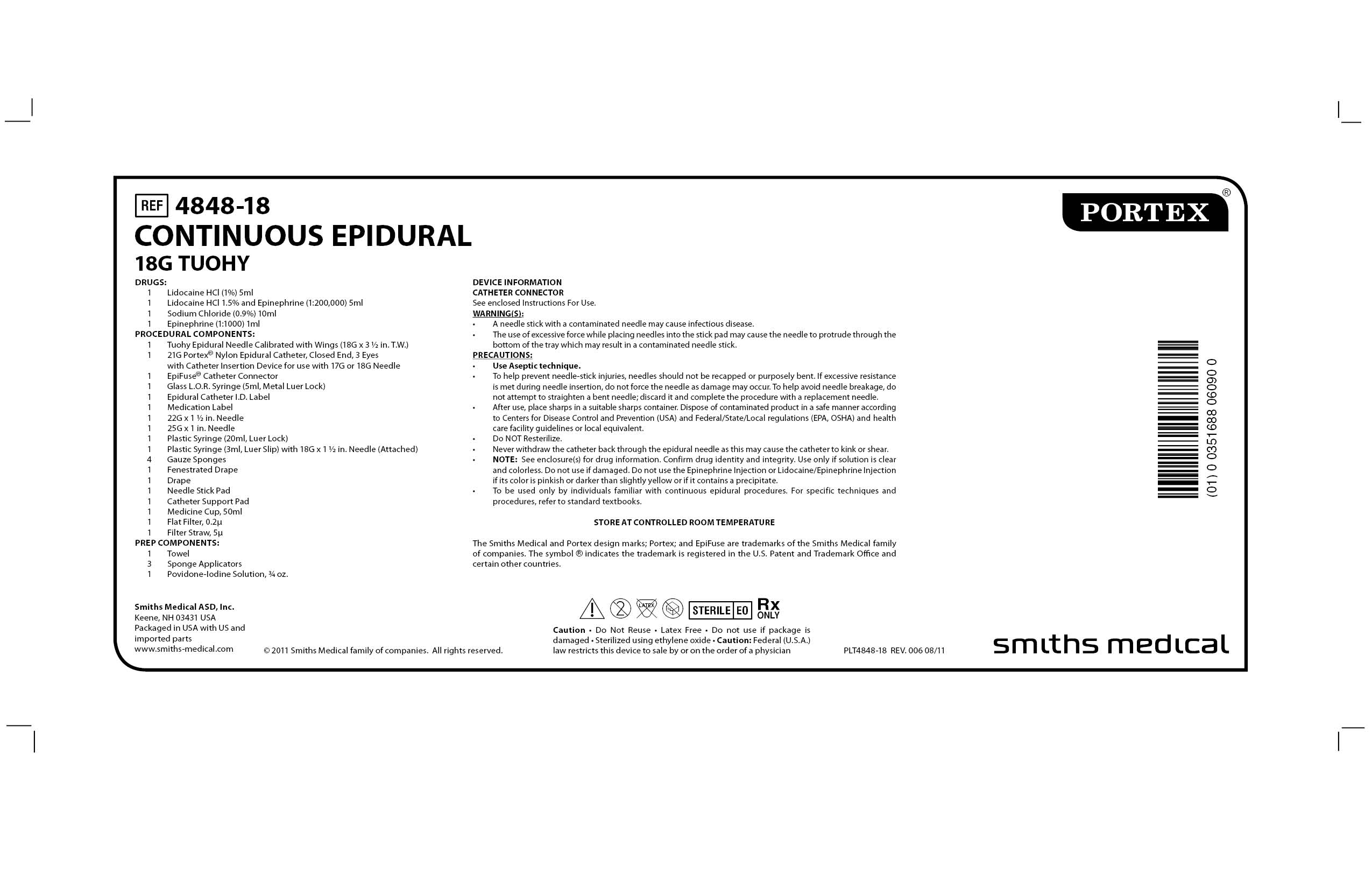
4848-18 CONTINUOUS EPIDURAL 18G TUOHY by Smiths Medical ASD, Inc. / Hospira, Inc. / Kwang Myung Pharm. Co., Ltd. / Aplicare, Inc.
4848-18 CONTINUOUS EPIDURAL 18G TUOHY by
Drug Labeling and Warnings
4848-18 CONTINUOUS EPIDURAL 18G TUOHY by is a Other medication manufactured, distributed, or labeled by Smiths Medical ASD, Inc., Hospira, Inc., Kwang Myung Pharm. Co., Ltd., Aplicare, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
4848-18 CONTINUOUS EPIDURAL 18G TUOHY- regional anesthesia kit
Smiths Medical ASD, Inc.
----------
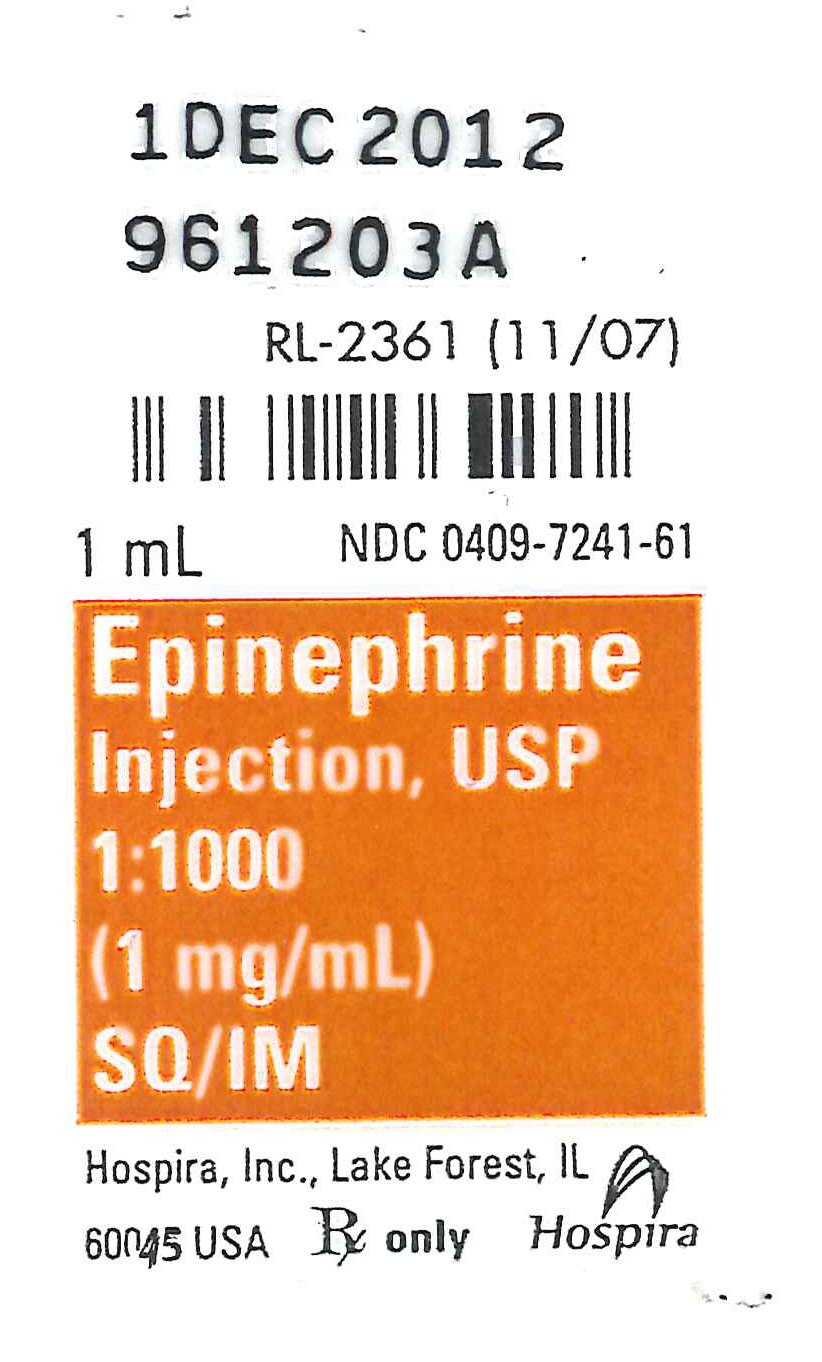
EPINEPHRINE injection, USP
1:1000 (1 mg/mL)
Ampul
Protect from light until ready to use.
Rx only
DescriptionEpinephrine Injection, USP 1:1000 is a sterile, nonpyrogenic solution.
Each mL contains epinephrine 1 mg; sodium chloride 9 mg; sodium
metabisulfite 0.9 mg added. May contain
hydrochloric acid for pH
adjustment. The solution contains no bacteriostat or antimicrobial
agent. It is administered by the following routes: intravenous,
intracardiac (left ventricular chamber), via endotracheal tube into the
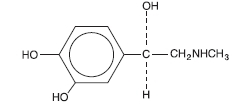
bronchial tree, subcutaneous or intramuscular. Epinephrine, USP is a
sympathomimetic (adrenergic) agent designated chemically as
4-[1-hydroxy-2 (methylamino) ethyl]-1,2 benzenediol, a white,
microcrystalline powder. It has the following structural formula:
Sodium Chloride, USP is chemically designated NaCl, a white, crystalline compound freely soluble in water.
The actions of epinephrine resemble the effects of
stimulation of adrenergic nerves. To a variable degree it acts on both
alpha and beta receptor sites of sympathetic effector cells. Its most
prominent actions are on the beta receptors of the heart, vascular and
other smooth muscle. When given by rapid intravenous injection, it
produces a rapid rise in blood pressure, mainly systolic, by (1) direct
stimulation of cardiac muscle which increases the strength of
ventricular contraction, (2) increasing the heart rate and (3)
constriction of the arterioles in the skin, mucosa and splanchnic areas
of the circulation. When given by slow intravenous injection epinephrine
usually produces only a moderate rise in systolic and a fall in
diastolic pressure. Although some increase in pulse pressure occurs,
there is usually no great elevation in mean blood pressure. Accordingly,
the compensatory reflex mechanisms that come into play with a
pronounced increase in blood pressure do not antagonize the direct
cardiac actions of epinephrine as much as with catecholamines that have a
predominant action on alpha receptors.
Total peripheral resistance
decreases by action of epinephrine on beta receptors of the skeletal
muscle vasculature and blood flow is thereby enhanced. Usually this
vasodilator effect of the drug on the circulation predominates so that
the modest rise in systolic pressure which follows slow injection or
absorption is mainly the result of direct cardiac stimulation and
increase in cardiac output. In some instances peripheral resistance is
not altered or may even rise owing to a greater ratio of alpha to beta
activity in different vascular areas. Epinephrine relaxes the smooth
muscles of the bronchi and iris and is a physiologic antagonist of
histamine. The drug also produces an increase in blood sugar and
glycogenolysis in the liver. Intravenous injection produces an immediate
and intensified response. Following intravenous injection epinephrine
disappears rapidly from the blood stream. Epinephrine is rapidly
inactivated in the body and is degraded by enzymes in the liver and
other tissues. The large portion of injection doses is excreted in the
urine as inactivated compounds. The remainder is excreted in the urine
as unchanged or conjugated compounds.
Epinephrine is used to relieve respiratory distress due to bronchospasm, to provide rapid relief of hypersensitivity reactions to drugs and other allergens, and to prolong the action of anesthetics. Its cardiac effects may be of use in restoring cardiac rhythm in cardiac arrest due to various causes, but it is not used in cardiac failure or in hemorrhagic, traumatic, or cardiogenic shock. Epinephrine is used as a hemostatic agent. It is also used in treating mucosal congestion of hay fever, rhinitis, and acute sinusitis; to relieve bronchial asthmatic paroxysms; in syncope due to complete heart block or carotid sinus hypersensitivity; for symptomatic relief of serum sickness, urticaria, angioneurotic edema; for resuscitation in cardiac arrest following anesthetic accidents; in simple (open angle) glaucoma; for relaxation of uterine musculature and to inhibit uterine contractions. Epinephrine Injection can be utilized to prolong the action of anesthetics used in local and regional anesthesia.
Epinephrine is contraindicated in patients with known
hypersensitivity to sympathomimetic amines, in patients with angle
closure glaucoma, and patients in shock (nonanaphylactic). It should
not
be used in patients anesthetized with agents such as cyclopropane or
halothane as these may sensitize the heart to the arrhythmic action of
sympathomimetic drugs. Addition of epinephrine to local anesthetics for
injection of certain areas (e.g., fingers, toes, ears, etc.) is
contraindicated because of danger that vasoconstriction may result in
sloughing of tissue.
Except as diluted for admixture with local
anesthetics to reduce absorption and prolong action, epinephrine should
not ordinarily be used in those cases where vasopressor drugs may be
contraindicated,
e.g., in thyrotoxicosis, diabetes, in obstetrics when maternal blood
pressure is in excess of 130/80 and in hypertension and other
cardiovascular disorders.
Inadvertently induced high arterial blood pressure may result in angina pectoris, aortic rupture or cerebral hemorrhage. Epinephrine may induce potentially serious cardiac arrhythmias in patients not suffering from heart disease and in patients with organic heart disease or who are receiving drugs that sensitize the myocardium. Parenterally administered epinephrine initially may produce constriction of renal blood vessels and decrease urine formation. Epinephrine Injection, USP is subject to oxidation and should be protected against exposure to light and stored in light-resistant containers. Epinephrine is the preferred treatment for serious allergic or other emergency situations even though this product contains sodium metabisulfite, a sulfite that may in other products cause allergic-type reactions including anaphylactic symptoms or life-threatening or less severe asthmatic episodes in certain susceptible persons. The alternatives to using epinephrine in a life-threatening situation may not be satisfactory. The presence of a sulfite in this product should not deter administration of the drug for treatment of serious allergic or other emergency situations.
Do not use the Injection if its color is pinkish or
darker than slightly yellow or if it contains a precipitate. Do not
administer unless solution is clear and container is intact. Discard
unused portion. Although epinephrine can produce ventricular
fibrillation, its actions in restoring electrical activity in asystole
and in enhancing defibrillation of the fibrillating ventricle are well
documented. The drug, however, should be used with caution in patients
with ventricular fibrillation. Epinephrine should be used cautiously in
patients with hyperthyroidism, hypertension and
cardiac arrhythmias.
All vasopressors should be used cautiously in patients taking monoamine
oxidase (MAO) inhibitors. Epinephrine should not be administered
concomitantly with other sympathomimetic drugs (such as isoproterenol)
because of possible additive effects and increased toxicity. Combined
effects may induce serious cardiac arrhythmias. They may be administered
alternately when the preceding effect of other such drugs has subsided.
Administration of epinephrine to patients receiving cyclopropane or
halogenated hydrocarbon general anesthetics such as halothane which
sensitize the myocardium, may induce cardiac arrhythmia. (See
CONTRAINDICATIONS.) When encountered, such arrhythmias may respond to
administration of a beta-adrenergic blocking drug. Epinephrine also
should be used cautiously with other drugs (e.g., digitalis glycosides)
that sensitize the myocardium to the actions of
sympathomimetic
agents. Diuretic agents may decrease vascular response to pressor drugs
such as epinephrine. Epinephrine may antagonize the neuron blockade
produced by guanethidine resulting in decreased antihypertensive effect
and requiring increased dosage of the latter.
Pregnancy Category C. Animal reproduction
studies have not been conducted with epinephrine. It is also not known
whether epinephrine can cause fetal harm when administered to a
pregnant woman or can affect reproduction capacity. Epinephrine should be given to a pregnant woman only if clearly needed.
Labor and Delivery. Parenteral
administration of epinephrine if used to support blood pressure during
low or other spinal anesthesia for delivery can cause acceleration of
fetal heart rate and
should not be used in obstetrics when maternal blood pressure exceeds 130/80. (See CONTRAINDICATIONS.)
Transient and minor side effects of anxiety, headache, fear and palpitations occur only with systemic therapeutic doses, especially in hyperthyroid individuals. Adverse effects such as cardiac arrhythmias and excessive rise in blood pressure may occur with systemic therapeutic doses or with inadvertent overdosage. Other adverse reactions include cerebral hemorrhage, hemiplegia, subarachnoid hemorrhage, anginal pain in patients with angina pectoris, anxiety, restlessness, headache, tremor, weakness, dizziness, pallor and respiratory difficulty. Such reactions are unlikely when epinephrine is diluted to 1:200,000 for injection with local anesthetic agents.
Erroneous administration of large doses of epinephrine may lead to precordial distress, vomiting, headache, dyspnea, as well as unusually elevated blood pressure. (See WARNINGS.) Toxic effects of overdosage can be counteracted by injection of an alpha-adrenergic blocker and a betaadrenergic blocker. In the event of a sharp rise in blood pressure, rapid-acting vasodilators such as the nitrites, or alpha-adrenergic blocking agents can be given to counteract the marked pressor effect of large doses of epinephrine.
Subcutaneously or intramuscularly – 0.2 to 1 mL (mg). Start with a small dose and increase if required.
Note: The subcutaneous is the preferred route
of administration. If given intramuscularly, injection into the buttocks
should be avoided.
Hypersensitivity Reactions
For bronchial asthma and certain allergic manifestations, e.g.,
angioedema, urticaria, serum sickness, anaphylactic shock, use
epinephrine subcutaneously. The adult intravenous dose for
hypersensitivity
reactions or to relieve bronchospasm usually ranges from 0.1 to 0.25 mg
injected slowly. Neonates may be given a dose of 0.01 mg per kg of body
weight; for the infant 0.05 mg is an adequate initial dose and this may
be repeated at 20 to 30 minute intervals in the management of asthma
attacks.
Cardiac Resuscitation
A dose of 0.5 mL (0.5 mg) diluted to 10 mL with sodium chloride
injection can be administered intravenously or intracardially to restore
myocardial contractility. Intracardiac injection should only be
administered by personnel well trained in the technique, if there has
not been sufficient time to establish an intravenous route. External
cardiac massage should follow intracardial administration to permit the
drug to enter coronary circulation. The drug should be used secondarily
to unsuccessful attempts with physical or electromechanical methods.
Ophthalmologic Use
Ophthalmologic use (for producing conjunctival decongestion, to
control hemorrhage, produce mydriasis and reduce intraocular pressure) –
use a concentration of 1:10,000 (0.1 mg/mL) to
1:1000 (1 mg/mL).
Regional Anesthesia
A final concentration of 1:200,000 of epinephrine injection is
recommended for infiltration injection, nerve block, caudal or other
epidural blocks. From 0.3 to 0.4 mg of epinephrine (0.3 to
0.4 mL of
1:1000 solution) may be mixed with spinal anesthetic agents. Parenteral
drug products should be inspected visually for particulate matter and
discoloration prior to administration. (See PRECAUTIONS.)
<paragraph>How SuppliedEpinephrine Injection, USP 1:1000 (1 mg/mL) is supplied in a 1 mL ampul single-dose container (NDC: 0409-7241-61).
Store at 20 to 25°C (68 to 77°F). [See USP Controlled Room Temperature.]
Protect from light.
Revised: October, 2008
Printed in USA EN-1927
Hospira, Inc., Lake Forest, IL 60045 USA<paragraph>
<paragraph>Spectra Medical Devices, Inc.
SODIUM CHLORIDE
INJECTION, USP, 0.9%
DESCRIPTION
Sodium Chloride Injection, USP is a sterile, nonpyrogenic, isotonic solution of sodium chloride 0.9% (9 mg/mL) in Water for Injection containing no antimicrobial agent or other added substance. The pH is between 4.5 and 7.0. Its chloride and sodium ion concentrates are approximately 0.154 mEq of each per milliliter and its calculated osmolality is 0.308 milliosmols per mL.
Sodium chloride occurs as colorless cubic crystals or white crystalline powder and has a saline taste. Sodium Chloride is freely soluble in water. It is soluble in glycerin and slightly soluble in alcohol. The empirical formula for sodium chloride is NaCl, and the molecular weight is 58.44.<paragraph>
CLINICAL PHARMACOLOGY
Sodium chloride comprises over 90% of the inorganic constituents of
the blood serum. Sodium chloride in water dissociates to provide sodium
(Na+) and chloride (Cl-) ions. Theses ions are normal constituents of
the body fluids (principally extracellular) and are essential for
maintaining electrolyte balance. The small volume of fluid and amount
of sodium chloride provided by Sodium Chloride Injection, USP, 0.9% when
used only as a vehicle for parenteral injection of drugs, is unlikely
to exert a significant effect on fluid and electrolyte balance except
possibly in very small infants.
INDICATIONS AND USAGE
Sodium Chloride Injection is used to flush intravascular catheters
or as a sterile, isontonic single dose vehicle, solvent, or diluent for
substances to administered intravenously, intramuscularly or
sub-cutaneously and for other extemporaneously prepared single dose
sterile solutions according to instructions of the manufacture of the
drug to be administered.
WARNING
Sodium Chloride must be used with caution in the presence of
congestive heart failure, circulatory insufficiency, kidney dysfunction
or hypoproteinemia.
Excessive amounts of sodium chloride by any route may cause hypokalemia and acidosis. Excessive amounts by parental routes may precipitate congestive heart failure and acute pulmonary edema, especially seen in patients with preexisting cardiovascular disease and those receiving corticos-teroids, corticotrophin or other drugs that may give rise to sodium retention. For use in newborns, when a Sodium Chloride solution is required for preparation or diluting medications, or in flushing intravenous catheters, only preservative-free Sodium Chloride Injection, USP, 0.9% should be used.
<paragraph>PRECAUTIONS
GENERAL
Since Sodium Chloride Injection does not contain antimicrobial agents and is intended for single use, any unused amount must be discarded immediately following withdrawal of any portion of the contents of the vial or ampul. Do not open ampul until it is to be used.
Consult the manufacturers instructions for choice of vehicle, appropriate dilution or volume for dissolving the drug to be injected, including the route and rate of injection.<paragraph>
PREGNANCY
CATEGORY C-Animal reproduction
studies have not been conducted with Sodium Chloride Injection. It is
also not known whether Sodium Chloride Injection can cause fetal harm
when administered to a pregnant woman or can effect reproduction
capacity. Sodium Chloride Injection should be given to a pregnant woman
only if clearly needed.
<paragraph>ADVERSE REACTION
Reactions which may occur because of this solution, added drugs or the technique of reconstitution or administration include febrile response, local tenderness, abscess, tissue necrosis or infection at the site of injection, venous thrombosis or phlebitis extending from the site of injection and extravasations.
If an adverse reaction does occur, discontinue the infusion, evaluate the patient, institute appropriate countermeasures and if possible, retrieve and save the remainder of unused vehicle for examination.<paragraph>
OVERDOSAGE
When used as a diluent, solvent or intravascular flushing solution,
this parental preparation is unlikely to pose a threat of sodium
chloride or fluid overload except possible in very small infants. In
the event these should occur, reevaluate the patient and institute
appropriate corrective measures
DOSAGE AND ADMINISTRATION
Before Sodium Chloride Injection, USP, 0.9% is used as a vehicle for
the administration of a drug;specific references should be checked for
any possible incompatibility with sodium chloride. The volume of the
preparation to be used for diluting or dissolving any drug for injection
is dependent on the vehicle concentration, dose and route of
administration as recommended by the manufacture.
Sodium Chloride Injection, USP, 0.9% is also indicated for use in flushing intravenous catheters. Prior to and after administration of the medication, the intravenous catheter should be flushed in its entirety with Sodium Chloride Injection, USP, 0.9%. Use in accord with any warnings or precautions appropriate to the medication being administered as recommended by the manufacture. Parental drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
HOW SUPPLIED
5 mL ampuls packaged in box of 50 each (NDC-65282-1505-1)
10 mL ampuls packaged in box of 50 each (NDC-65282-1510-1)
30 mL ampuls packaged in box of 30 each (NDC-65282-1530-3)
<paragraph>STORAGE
Store at controlled room temperature 15-30 C (59-86 F). Avoid freezing.
Manufactured for:
Spectra Medical Devices, Inc. 260-F Fordham Road, Wilmington, MA 01887
By: KM. Pharm. Co., LTD.<paragraph>
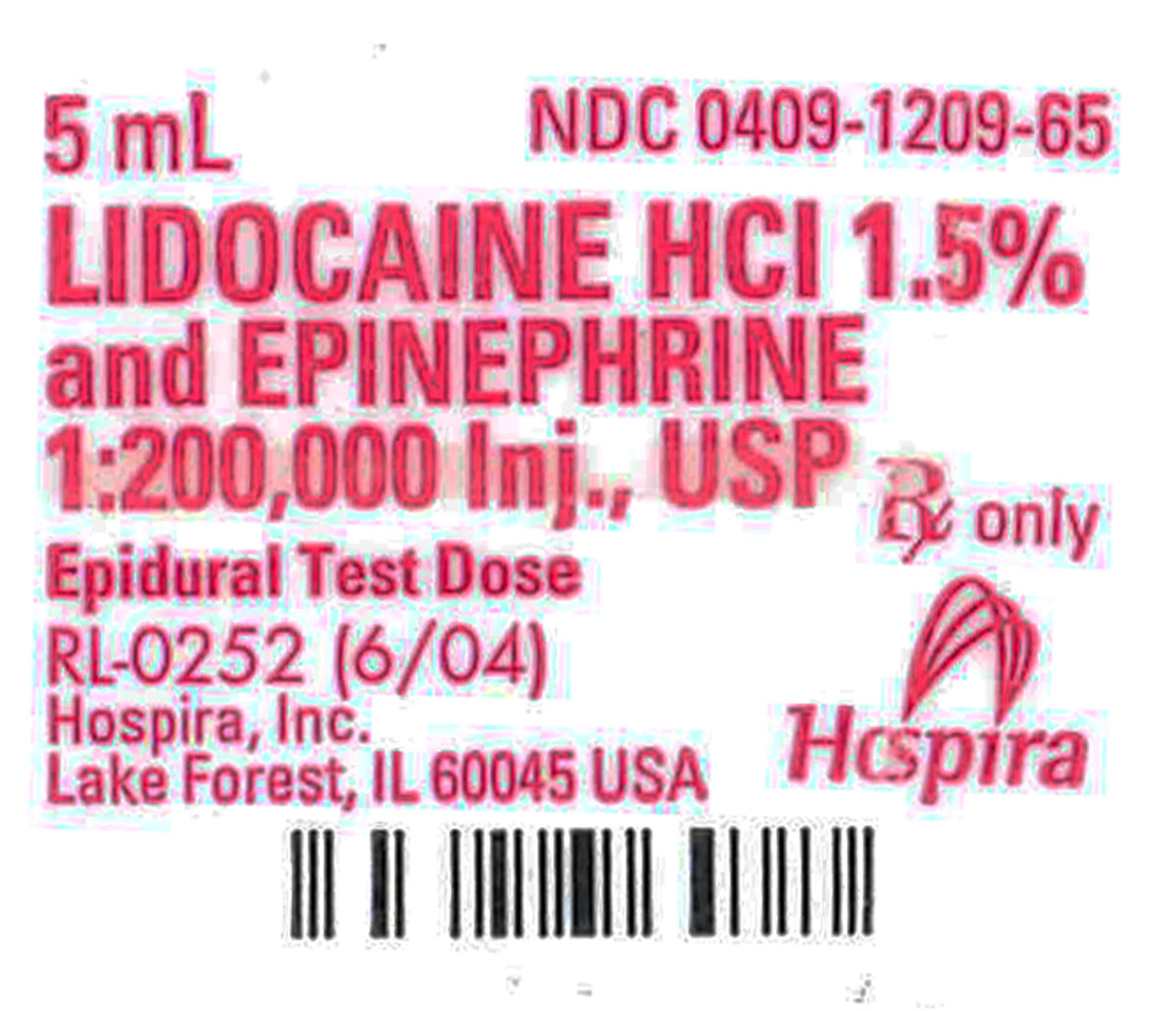
<paragraph>LIDOCAINE HYDROCHLORIDE AND EPINEPHRINE (lidocaine hydrochloride anhydrous and epinephrine) injection, solution
[Hospira, Inc.]
For Infiltration and Nerve Block.
Ampul
Fliptop Vial
Multiple-dose Fliptop Vial
Protect from light.
Rx only
DESCRIPTION
Lidocaine Hydrochloride and Epinephrine Injection, USP is a sterile, nonpyrogenic solution of lidocaine hydrochloride and epinephrine in water for injection for parenteral administration in various concentrations with characteristics as follows:
|
Concentration Lidocaine HCl |
Epinephrine |
Lidocaine HCl (anhyd.) mg/mL |
Epinephrine mcg/mL |
Sodium Chloride mg/mL |
|
0.5% |
1:200,000 |
5 |
5 |
8 |
|
1% |
1:200,000 |
10 |
5 |
7 |
|
1.5% |
1:200,000 |
15 |
5 |
6.5 |
|
2% |
1:200,000 |
20 |
5 |
6 |
|
1% |
1:100,000 |
10 |
10 |
7 |
|
2% |
1:100,000 |
20 |
10 |
6 |
Sodium metabisulfite 0.5 mg/mL and citric acid, anhydrous 0.2 mg/mL added as stabilizers. The headspace of Lists 1209, and 3179 are carbon dioxide gassed and Lists 3177, 3178, 3181, 3182 and 3183 are nitrogen gassed. May contain sodium hydroxide and/or hydrochloric acid to adjust pH; pH is 4.5 (3.3 to 5.5). See HOW SUPPLIED section for various sizes and strengths.
Multiple-dose vials contain methylparaben 1 mg/mL added as preservative.
Single-dose ampuls and vials contain no bacteriostat or antimicrobial agent. Discard unused portion.
Lidocaine is a local anesthetic of the amide type.
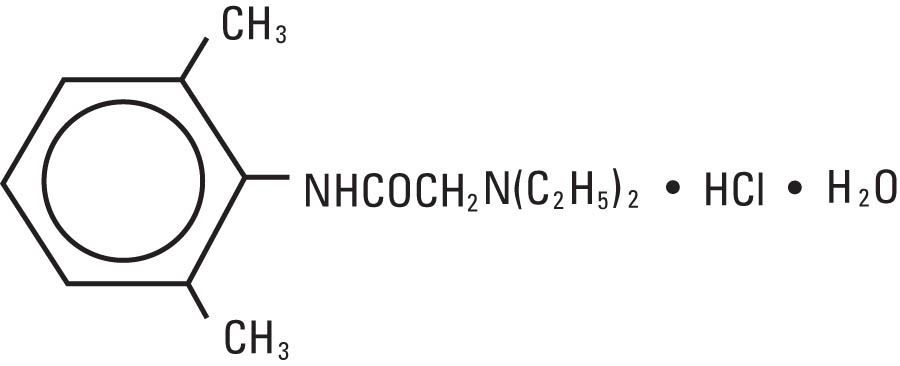
Lidocaine Hydrochloride, USP is chemically designated 2-(diethyl-amino)-2’,6’-acetoxylidide monohydrochloride monohydrate, a white powder freely soluble in water. It has the following structural formula:
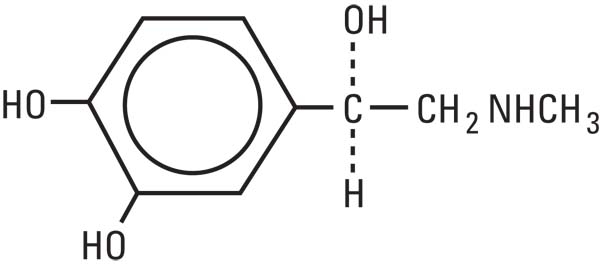
Epinephrine, USP is a sympathomimetic (adrenergic) agent designated chemically as 4-[1-hydroxy-2 (methylamino) ethyl]-1,2 benzenediol, a white, microcrystalline powder. It has the following structural formula:<paragraph>
<paragraph>CLINICAL PHARMACOLOGY
Mechanism of action: Lidocaine stabilizes the neuronal membrane by inhibiting the ionic fluxes required for the initiation and conduction of impulses, thereby effecting local anesthetic action.
Hemodynamics: Excessive blood levels may cause changes in cardiac output, total peripheral resistance, and mean arterial pressure. With central neural blockade these changes may be attributable to block of autonomic fibers, a direct depressant effect of the local anesthetic agent on various components of the cardiovascular system and/or the beta-adrenergic receptor stimulating action of epinephrine when present. The net effect is normally a modest hypotension when the recommended dosages are not exceeded.
Pharmacokinetics and metabolism: Information derived from diverse formulations, concentrations and usages reveals that lidocaine is completely absorbed following parenteral administration, its rate of absorption depending, for example, upon various factors such as the site of administration and the presence or absence of a vasoconstrictor agent. Except for intravascular administration, the highest blood levels are obtained following intercostal nerve block and the lowest after subcutaneous administration.
The plasma binding of lidocaine is dependent on drug concentration, and the fraction bound decreases with increasing concentration. At concentrations of 1 to 4 µg of free base per mL, 60 to 80 percent of lidocaine is protein bound. Binding is also dependent on the plasma concentration of the alpha-1-acid glycoprotein.
Lidocaine crosses the blood-brain and placental barriers, presumably by passive diffusion.
Lidocaine is metabolized rapidly by the liver, and metabolites and unchanged drug are excreted by the kidneys. Biotransformation includes oxidative N-dealkylation, ring hydroxylation, cleavage of the amide linkage, and conjugation. N-dealkylation, a major pathway of biotransformation, yields the metabolites monoethylglycinexylidide and glycinexylidide. The pharmacological/toxicological actions of these metabolites are similar to, but less potent than, those of lidocaine. Approximately 90% of lidocaine administered is excreted in the form of various metabolites, and less than 10% is excreted unchanged. The primary metabolite in urine is a conjugate of 4-hydroxy-2, 6-dimethylaniline.
The elimination half-life of lidocaine following an intravenous bolus injection is typically 1.5 to 2.0 hours. Because of the rapid rate at which lidocaine is metabolized, any condition that affects liver function may alter lidocaine kinetics. The half-life may be prolonged two-fold or more in patients with liver dysfunction. Renal dysfunction does not affect lidocaine kinetics but may increase the accumulation of metabolites.
Factors such as acidosis and the use of CNS stimulants and depressants affect the CNS levels of lidocaine required to produce overt systemic effects. Objective adverse manifestations become increasingly apparent with increasing venous plasma levels above 6.0 µg free base per mL. In the rhesus monkey arterial blood levels of 18-21 µg/mL have been shown to be threshold for convulsive activity.<paragraph>
<paragraph>INDICATIONS AND USAGE
Lidocaine Hydrochloride and Epinephrine Injection, USP is indicated for production of local or regional anesthesia by infiltration techniques such as percutaneous injection, by peripheral nerve block techniques such as brachial plexus and intercostal and by central neural techniques such as lumbar and caudal epidural blocks, when the accepted procedures for these techniques as described in standard textbooks are observed.<paragraph>
<paragraph>CONTRAINDICATIONS
Lidocaine is contraindicated in patients with a known history of hypersensitivity to local anesthetics of the amide type.<paragraph>
<paragraph>WARNINGS
LIDOCAINE HYDROCHLORIDE AND EPINEPHRINE INJECTION, USP FOR INFILTRATION AND NERVE BLOCK SHOULD BE EMPLOYED ONLY BY CLINICIANS WHO ARE WELL VERSED IN DIAGNOSIS AND MANAGEMENT OF DOSE-RELATED TOXICITY AND OTHER ACUTE EMERGENCIES THAT MIGHT ARISE FROM THE BLOCK TO BE EMPLOYED AND THEN ONLY AFTER ENSURING THE IMMEDIATE AVAILABILITY OF OXYGEN, OTHER RESUSCITATIVE DRUGS, CARDIOPULMONARY EQUIPMENT, AND THE PERSONNEL NEEDED FOR PROPER MANAGEMENT OF TOXIC REACTIONS AND RELATED EMERGENCIES (See also ADVERSE REACTIONS and PRECAUTIONS). DELAY IN PROPER MANAGEMENT OF DOSE-RELATED TOXICITY, UNDERVENTILATION FROM ANY CAUSE AND/OR ALTERED SENSITIVITY MAY LEAD TO THE DEVELOPMENT OF ACIDOSIS, CARDIAC ARREST AND, POSSIBLY, DEATH.
Intra-articular infusions of local anesthetics following arthroscopic and other surgical procedures is an unapproved use, and there have been post-marketing reports of chondrolysis in patients receiving such infusions. The majority of reported cases of chondrolysis have involved the shoulder joint; cases of gleno-humeral chondrolysis have been described in pediatric and adult patients following intra-articular infusions of local anesthetics with and without epinephrine for periods of 48 to 72 hours. There is insufficient information to determine whether shorter infusion periods are not associated with these findings. The time of onset of symptoms, such as joint pain, stiffness and loss of motion can be variable, but may begin as early as the 2nd month after surgery. Currently, there is no effective treatment for chondrolysis; patients who experienced chondrolysis have required additional diagnostic and therapeutic procedures and some required arthroplasty or shoulder replacement.
To avoid intravascular injection, aspiration should be performed before the local anesthetic solution is injected. The needle must be repositioned until no return of blood can be elicited by aspiration. Note, however, that the absence of blood in the syringe does not guarantee that intravascular injection has been avoided.
Local anesthetic solutions containing antimicrobial preservatives (e.g., methylparaben) should not be used for epidural or spinal anesthesia because the safety of these agents has not been established with regard to intrathecal injection, either intentional or accidental.
Lidocaine Hydrochloride and Epinephrine Injection contains sodium metabisulfite, a sulfite that may cause allergic-type reactions including anaphylactic symptoms and life-threatening or less severe asthmatic episodes in certain susceptible people. The overall prevalence of sulfite sensitivity in the general population is unknown and probably low. Sulfite sensitivity is seen more frequently in asthmatic than in nonasthmatic people.<paragraph>
<paragraph>PRECAUTIONS
General: The safety and effectiveness of lidocaine depend on proper dosage, correct technique, adequate precautions, and readiness for emergencies. Standard textbooks should be consulted for specific techniques and precautions for various regional anesthetic procedures.
Resuscitative equipment, oxygen, and other resuscitative drugs should be available for immediate use. (See WARNINGS and ADVERSE REACTIONS). The lowest dosage that results in effective anesthesia should be used to avoid high plasma levels and serious adverse effects. Syringe aspirations should also be performed before and during each supplemental injection when using indwelling catheter techniques. During the administration of epidural anesthesia, it is recommended that a test dose be administered initially and that the patient be monitored for central nervous system toxicity and cardiovascular toxicity, as well as for signs of unintended intrathecal administration before proceeding. When clinical conditions permit, consideration should be given to employing local anesthetic solutions that contain epinephrine for the test dose because circulatory changes compatible with epinephrine may also serve as a warning sign of unintended intravascular injection. An intravascular injection is still possible even if aspirations for blood are negative. Repeated doses of lidocaine may cause significant increases in blood levels with each repeated dose because of slow accumulation of the drug or its metabolites. Tolerance to elevated blood levels varies with the status of the patient. Debilitated, elderly patients, acutely ill patients and children should be given reduced doses commensurate with their age and physical condition. Lidocaine should also be used with caution in patients with severe shock or heart block.
Lumbar and caudal epidural anesthesia should be used with extreme caution in persons with the following conditions: existing neurological disease, spinal deformities, septicemia and severe hypertension.
Local anesthetic solutions containing a vasoconstrictor should be used cautiously and in carefully circumscribed quantities in areas of the body supplied by end arteries or having otherwise compromised blood supply. Patients with peripheral vascular disease and those with hypertensive vascular disease may exhibit exaggerated vasoconstrictor response. Ischemic injury or necrosis may result. Preparations containing a vasoconstrictor should be used with caution in patients during or following the administration of potent general anesthetic agents, since cardiac arrhythmias may occur under such conditions.
Careful and constant monitoring of cardiovascular and respiratory (adequacy of ventilation) vital signs and the patient’s state of consciousness should be accomplished after each local anesthetic injection. It should be kept in mind at such times that restlessness, anxiety, tinnitus, dizziness, blurred vision, tremors, depression or drowsiness may be early warning signs of central nervous system toxicity.
Since amide-type local anesthetics are metabolized by the liver, lidocaine injection should be used with caution in patients with hepatic disease. Patients with severe hepatic disease because of their inability to metabolize local anesthetics normally, are a greater risk of developing toxic plasma concentrations. Lidocaine should also be used with caution in patients with impaired cardiovascular function since they may be less able to compensate for functional changes associated with the prolongation of A-V conduction produced by these drugs.
Many drugs used during the conduct of anesthesia are considered potential triggering agents for familial malignant hyperthermia. Since it is not known whether amide-type local anesthetics may trigger this reaction and since the need for supplemental general anesthesia cannot be predicted in advance, it is suggested that a standard protocol for the management of malignant hyperthermia should be available. Early unexplained signs of tachycardia, tachypnea, labile blood pressure and metabolic acidosis may precede temperature elevation. Successful outcome is dependent on early diagnosis, prompt discontinuance of the suspect triggering agent(s) and institution of treatment, including oxygen therapy, indicated supportive measures and dantrolene (consult dantrolene sodium intravenous package insert before using).
Injections containing epinephrine or other vasoconstrictors should not be used for intravenous regional anesthesia.
Lidocaine should be used with caution in persons with known drug sensitivities. Patients allergic to para-amino-benzoic acid derivatives (procaine, tetracaine, benzocaine, etc.) have not shown cross sensitivity to lidocaine.
Use in the Head and Neck Area: Small doses of local anesthetics injected into the head and neck area, including retrobulbar, dental and stellate ganglion blocks, may produce adverse reactions similar to systemic toxicity seen with unintentional intravascular injections of larger doses. Confusion, convulsions, respiratory depression and/or respiratory arrest and cardiovascular stimulation or depression have been reported. These reactions may be due to intra-arterial injections of the local anesthetic with retrograde flow to the cerebral circulation. Patients receiving these blocks should have their circulation and respiration monitored and be constantly observed. Resuscitative equipment and personnel for treating adverse reactions should be immediately available. Dosage recommendations should not be exceeded. (See DOSAGE AND ADMINISTRATION).
Information for Patients: When appropriate, patients should be informed in advance that they may experience temporary loss of sensation and motor activity, usually in the lower half of the body following proper administration of epidural anesthesia.
Clinically Significant Drug Interactions: The administration of local anesthetic solutions containing epinephrine or norepinephrine to patients receiving monoamine oxidase inhibitors or tricyclic antidepressants may produce severe prolonged hypertension.
Phenothiazines and butyrophenones may reduce or reverse the pressor effect of epinephrine.
Concurrent use of these agents should generally be avoided. In situations when concurrent therapy is necessary, careful patient monitoring is essential.
Concurrent administration of vasopressor drugs (for the treatment of hypotension related to obstetric blocks) and ergot-type oxytocic drugs may cause severe persistent hypertension or cerebrovascular accidents.
Drug Laboratory Test Interactions: The intramuscular injection of lidocaine may result in an increase in creatine phosphokinase levels. Thus, the use of this enzyme determination without isoenzyme separation as a diagnostic test for the presence of acute myocardial infarction may be compromised by the intramuscular injection of lidocaine.
Carcinogenesis, Mutagenesis, Impairment of Fertility: Studies of lidocaine in animals to evaluate the carcinogenic and mutagenic potential or the effect on fertility have not been conducted.
Pregnancy: Teratogenic Effects. Pregnancy Category B. Reproduction studies have been performed in rats at doses up to 6.6 times the human dose and have revealed no evidence of harm to the fetus caused by lidocaine. There are, however, no adequate and well-controlled studies in pregnant women. Animal reproduction studies are not always predictive of human response. General consideration should be given to this fact before administering lidocaine to women of childbearing potential, especially during early pregnancy when maximum organogenesis takes place.
Labor and Delivery: Local anesthetics rapidly cross the placenta and when used for epidural, paracervical, pudendal or caudal block anesthesia, can cause varying degrees of maternal, fetal and neonatal toxicity (See CLINICAL PHARMACOLOGY-Pharmacokinetics). The potential for toxicity depends upon the procedure performed, the type and amount of drug used, and the technique of drug administration. Adverse reactions in the parturient, fetus and neonate involve alterations of the central nervous system peripheral vascular tone and cardiac function.
Maternal hypotension has resulted from regional anesthesia. Local anesthetics produce vasodilation by blocking sympathetic nerves. Elevating the patient’s legs and positioning her on her left side will help prevent decreases in blood pressure. The fetal heart rate also should be monitored continuously, and electronic fetal monitoring is highly advisable.
Epidural, spinal, paracervical, or pudendal anesthesia may alter the forces of parturition through changes in uterine contractility or maternal expulsive efforts. In one study, paracervical block anesthesia was associated with a decrease in the mean duration of first stage labor and facilitation of cervical dilation. However, spinal and epidural anesthesia have also been reported to prolong the second stage of labor by removing the parturient’s reflex urge to bear down or by interfering with motor function. The use of obstetrical anesthesia may increase the need for forceps assistance.
The use of some local anesthetic drug products during labor and delivery may be followed by diminished muscle strength and tone for the first day or two of life. The long term significance of these observations is unknown. Fetal bradycardia may occur in 20 to 30 percent of patients receiving paracervical nerve block anesthesia with the amide-type local anesthetics and may be associated with fetal acidosis. Fetal heart rate should always be monitored during paracervical anesthesia. The physician should weigh the possible advantages against risks when considering paracervical block in prematurity, toxemia of pregnancy and fetal distress. Careful adherence to recommended dosage is of the utmost importance in obstetrical paracervical block. Failure to achieve adequate analgesia with recommended doses should arouse suspicion of intravascular or fetal intracranial injection. Cases compatible with unintended fetal intracranial injection of local anesthetic solution have been reported following intended paracervical or pudendal block or both. Babies so affected present with unexplained neonatal depression at birth, which correlates with high local anesthetic serum levels, and often manifest seizures within six hours. Prompt use of supportive measures combined with forced urinary excretion of the local anesthetic has been used successfully to manage this complication.
Case reports of maternal convulsions and cardiovascular collapse following use of some local anesthetics for paracervical block in early pregnancy (as anesthesia for elective abortion) suggest that systemic absorption under these circumstances may be rapid. The recommended maximum dose of each drug should not be exceeded. Injection should be made slowly and with frequent aspiration. Allow a 5-minute interval between sides.
Nursing Mothers: It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when lidocaine is administered to a nursing woman.
Pediatric Use: Dosages in pediatric patients should be reduced, commensurate with age, body weight and physical condition. See DOSAGE AND ADMINISTRATION.<paragraph>
<paragraph>ADVERSE REACTIONS
Systemic: Adverse experiences following the administration of lidocaine are similar in nature to those observed with other amide local anesthetic agents. These adverse experiences are, in general, dose-related and may result from high plasma levels caused by excessive dosage, rapid absorption or inadvertent intravascular injection, or may result from a hypersensitivity, idiosyncrasy or diminished tolerance on the part of the patient. Serious adverse experiences are generally systemic in nature. The following types are those most commonly reported:
Central Nervous System: CNS manifestations are excitatory and/or depressant and may be characterized by lightheadedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression and arrest. The excitatory manifestations may be very brief or may not occur at all, in which case the first manifestation of toxicity may be drowsiness merging into unconsciousness and respiratory arrest.
Drowsiness following the administration of lidocaine is usually an early sign of a high blood level of the drug and may occur as a consequence of rapid absorption.
Cardiovascular System: Cardiovascular manifestations are usually depressant and are characterized by bradycardia, hypotension, and cardiovascular collapse, which may lead to cardiac arrest.
Allergic: Allergic reactions are characterized by cutaneous lesions, urticaria, edema or anaphylactoid reactions. Allergic reactions may occur as a result of sensitivity either to local anesthetic agents, to bisulfites or to the methylparaben used as a preservative in multiple dose vials. Allergic reactions as a result of sensitivity to lidocaine are extremely rare and, if they occur, should be managed by conventional means. The detection of sensitivity by skin testing is of doubtful value.
Neurologic: The incidences of adverse reactions associated with the use of local anesthetics may be related to the total dose of local anesthetic administered and are also dependent upon the particular drug used, the route of administration and the physical status of the patient. In a prospective review of 10,440 patients who received lidocaine for spinal anesthesia, the incidences of adverse reactions were reported to be about 3 percent each for positional headaches, hypotension and backache; 2 percent for shivering; and less than 1 percent each for peripheral nerve symptoms, nausea, respiratory inadequacy and double vision. Many of these observations may be related to local anesthetic techniques, with or without a contribution from the local anesthetic.
In the practice of caudal or lumbar epidural block, occasional unintentional penetration of the subarachnoid space by the catheter may occur. Subsequent adverse effects may depend partially on the amount of drug administered subdurally. These may include spinal block of varying magnitude (including total spinal block), hypotension secondary to spinal block, loss of bladder and bowel control, and loss of perineal sensation and sexual function. Persistent motor, sensory and/or autonomic (sphincter control) deficit of some lower spinal segments with slow recovery (several months) or incomplete recovery have been reported in rare instances when caudal or lumbar epidural block has been attempted. Backache and headache have also been noted following use of these anesthetic procedures.
There have been reported cases of permanent injury to extraocular muscles requiring surgical repair following retrobulbar administration.<paragraph>
<paragraph> OVERDOSAGE
Acute emergencies from local anesthetics are generally related to high plasma levels encountered during therapeutic use of local anesthetics or to unintended subarachnoid injection of local anesthetic solution (see ADVERSE REACTIONS, WARNINGS and PRECAUTIONS).
Management of Local Anesthetic Emergencies: The first consideration is prevention, best accomplished by careful monitoring of cardiovascular and respiratory vital signs and the patient’s state of consciousness after each local anesthetic injection. At the first sign of change, oxygen should be administered.
The first step in the management of convulsions, as well as under-ventilation or apnea due to unintended subarachnoid injection of drug solution, consists of immediate attention to the maintenance of a patent airway and assisted or controlled ventilation with oxygen and a delivery system capable of permitting immediate positive airway pressure by mask. Immediately after the institution of these ventilatory measures, the adequacy of the circulation should be evaluated, keeping in mind that drugs used to treat convulsions sometimes depress the circulation when administered intravenously. Should convulsions persist despite adequate respiratory support, and if the status of the circulation permits, small increments of an ultra-short acting barbiturate (such as thiopental or thiamylal) or a benzodiazepine (such as diazepam) may be administered intravenously. The clinician should be familiar, prior to use of local anesthetics, with these anticonvulsant drugs. Supportive treatment of circulatory depression may require administration of intravenous fluids and, when appropriate, a vasopressor as directed by the clinical situation (e.g., ephedrine).
If not treated immediately, both convulsions and cardiovascular depression can result in hypoxia, acidosis, bradycardia, arrhythmias and cardiac arrest. Underventilation or apnea due to unintentional subarachnoid injection of local anesthetic solution may produce these same signs and also lead to cardiac arrest if ventilatory support is not instituted. If cardiac arrest should occur standard cardiopulmonary resuscitative measures should be instituted.
Endotracheal intubation, employing drugs and techniques familiar to the clinician, may be indicated, after initial administration of oxygen by mask, if difficulty is encountered in the maintenance of a patent airway or if prolonged ventilatory support (assisted or controlled) is indicated.
Dialysis is of negligible value in the treatment of acute overdosage with lidocaine.
The oral LD50 of lidocaine HCl in non-fasted female rats is 459 (346-773) mg/kg (as the salt) and 214 (159-324) mg/kg (as the salt) in fasted female rats.<paragraph>
<paragraph> DOSAGE AND ADMINISTRATION
Table I (Recommended Dosages) summarizes the recommended volumes and concentrations of Lidocaine Hydrochloride Injection, USP for various types of anesthetic procedures. The dosages suggested in this table are for normal healthy adults and refer to the use of epinephrine-free solutions. When larger volumes are required only solutions containing epinephrine should be used, except in those cases where vasopressor drugs may be contraindicated.
There have been adverse event reports of chondrolysis in patients receiving intra-articular infusions of local anesthetics following arthroscopic and other surgical procedures. Lidocaine is not approved for this use (see WARNINGS and DOSAGE AND ADMINISTRATION).
These recommended doses serve only as a guide to the amount of anesthetic required for most routine procedures. The actual volumes and concentrations to be used depend on a number of factors such as type and extent of surgical procedure, depth of anesthesia and degree of muscular relaxation required, duration of anesthesia required, and the physical condition of the patient. In all cases the lowest concentration and smallest dose that will produce the desired result should be given. Dosages should be reduced for children and for elderly and debilitated patients and patients with cardiac and/or liver disease.
The onset of anesthesia, the duration of anesthesia and the degree of muscular relaxation are proportional to the volume and concentration (i.e., total dose) of local anesthetic used. Thus, an increase in volume and concentration of Lidocaine Hydrochloride Injection, USP will decrease the onset of anesthesia, prolong the duration of anesthesia, provide a greater degree of muscular relaxation and increase the segmental spread of anesthesia. However, increasing the volume and concentration of Lidocaine Hydrochloride Injection, USP may result in a more profound fall in blood pressure when used in epidural anesthesia. Although the incidence of side effects with lidocaine is quite low, caution should be exercised when employing large volumes and concentrations, since the incidence of side effects is directly proportional to the total dose of local anesthetic agent injected.
Epidural Anesthesia
For an epidural test dose, only the following available specific product of Lidocaine Hydrochloride and Epinephrine Injection, USP by Hospira is recommended:
1.5% with epinephrine 1:200,000.................... 5 mL single-dose ampuls
For epidural anesthesia, only the following available specific products of Lidocaine Hydrochloride and Epinephrine Injection, USP by Hospira are recommended:
1% with epinephrine 1:200,000............................ 30 mL single-dose ampuls
30 mL single-dose vials
1.5% with epinephrine 1:200,000.......................... 30 mL single-dose ampuls
30 mL single-dose vials
2% with epinephrine 1:200,000................................ 20 mL single-dose vials
Although these solutions are intended specifically for epidural anesthesia, they may also be used for infiltration and peripheral nerve block provided they are employed as single-dose units. These solutions contain no bacteriostatic agent.
In epidural anesthesia, the dosage varies with the number of dermatomes to be anesthetized (generally 2-3 mL of the indicated concentration per dermatome).
Caudal and Lumbar Epidural Block: As a precaution against the adverse experiences sometimes observed following unintentional penetration of the subarachnoid space, a test dose such as 2-3 mL of 1.5% lidocaine injection should be administered at least 5 minutes prior to injecting the total volume required for a lumbar or caudal epidural block. The test dose should be repeated if the patient is moved in a manner that may have displaced the catheter. Epinephrine, if contained in the test dose (10-15 µg have been suggested), may serve as a warning of unintentional intravascular injection. If injected into a blood vessel, this amount of epinephrine is likely to produce a transient “epinephrine response” within 45 seconds, consisting of an increase in heart rate and systolic blood pressure, circumoral pallor, palpitations and nervousness in the unsedated patient. The sedated patient may exhibit only a pulse rate increase of 20 or more beats per minute for 15 or more seconds. Patients on beta-blockers may not manifest changes in heart rate, but blood pressure monitoring can detect an evanescent rise in systolic blood pressure. Adequate time should be allowed for onset of anesthesia after administration of each test dose. The rapid injection of a large volume of Lidocaine Hydrochloride and Epinephrine Injection, USP through the catheter should be avoided, and, when feasible, fractional doses should be administered.
In the event of the known injection of a large volume of local anesthetic solution into the subarachnoid space, after suitable resuscitation and if the catheter is in place, consider attempting the recovery of drug by draining a moderate amount of cerebrospinal fluid (such as 10 mL) through the epidural catheter.
Maximum Recommended Dosages
Adults: For normal healthy adults, the individual maximum dose of Lidocaine Hydrochloride and Epinephrine Injection, USP should not exceed 7 mg/kg (3.5 mg/lb) of body weight and in general it is recommended that the maximum total dose not exceed 500 mg. When used without epinephrine, the maximum individual dose should not exceed 4.5 mg/kg (2 mg per lb) of body weight, and in general it is recommended that the maximum total dose does not exceed 300 mg. For continuous epidural or caudal anesthesia, the maximum recommended dosage should not be administered at intervals of less than 90 minutes. When continuous lumbar or caudal epidural anesthesia is used for non-obstetrical procedures, more drug may be administered if required to produce adequate anesthesia.
The maximum recommended dose per 90 minute period of lidocaine hydrochloride for paracervical block in obstetrical patients and non-obstetrical patients is 200 mg total. One half of the total dose is usually administered to each side. Inject slowly five minutes between sides. (See also discussion of paracervical block in PRECAUTIONS).
Pediatric Population: It is difficult to recommend a maximum dose of any drug for pediatric patients, since this varies as a function of age and weight. For pediatric patients over 3 years of age who have a normal lean body mass and normal body development, the maximum dose is determined by the child’s age and weight. For example, in a child of 5 years weighing 50 lbs., the dose of lidocaine HCl should not exceed 75-100 mg (1.5-2 mg/lb).
In order to guard against systemic toxicity, the lowest effective concentration and lowest effective dose should be used at all times. In some cases it will be necessary to dilute available concentrations with 0.9% sodium chloride injection in order to obtain the required final concentration.
FOR EPIDURAL USE ONLY.
Note: Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever the solution and container permit. Do not use the injection if its color is pinkish or darker than slightly yellow or if it contains a precipitate.
|
Lidocaine Hydrochloride Injection, USP (without Epinephrine) |
|||
|
Procedure |
Conc. (%) |
Vol. (mL) |
Total Dose (mg) |
| InfiltrationPercutaneous Intravenous Regional |
0.5 or 1.0 0.5 |
1-60 10-60 |
5-300 50-300 |
|
Peripheral Nerve Blocks, e.g. Brachial Dental Intercostal Paravertebral Pudendal (each side) Paracervical Obstetrical Analgesia (each side) |
1.5 2.0 1.0 1.0 1.0 1.0 |
15-20 1-5 3 3-5 10 10 |
225-300 20-100 30 30-50 100 100 |
|
Sympathetic Nerve Blocks, e.g. Cervical (stellate ganglion) Lumbar |
1.0 1.0 |
5 5-10 |
50 50-100 |
|
Central Neural Blocks Epidural* Thoracic Lumbar Analgesia Anesthesia Caudal Obstetrical Analgesia Surgical Anesthesia |
1.0 1.0 1.5 2.0 1.0 1.5 |
20-30 25-30 15-20 10-15 20-30 15-20 |
200-300 250-300 225-300 200-300 200-300 225-300 |
|
*Dose determined by number of dermatomes to be anesthetized (2 to 3 mL/ dermatome). |
THE ABOVE SUGGESTED CONCENTRATIONS AND VOLUMES SERVE ONLY AS A GUIDE. OTHER VOLUMES AND CONCENTRATIONS MAY BE USED PROVIDED THE TOTAL MAXIMUM RECOMMENDED DOSE IS NOT EXCEEDED.
Sterilization, Storage and Technical Procedures: Disinfecting agents containing heavy metals, which cause release of respective ions (mercury, zinc, copper, etc.) should not be used for skin or mucous membrane disinfection as they have been related to incidence of swelling and edema. When chemical disinfection of multi-dose vials is desired, either isopropyl alcohol (91%) or 70% ethyl alcohol is recommended. Many commercially available brands of rubbing alcohol, as well as solutions of ethyl alcohol not of USP grade, contain denaturants which are injurious to rubber and, therefore, are not to be used. It is recommended that chemical disinfection be accomplished by wiping the vial stopper or ampul thoroughly with cotton or gauze that has been moistened with the recommended alcohol just prior to use.
Do not autoclave.<paragraph>
<paragraph> HOW SUPPLIED
Lidocaine Hydrochloride and Epinephrine Injection, USP is supplied in single-dose and multiple-dose containers as shown below:
|
NDC No. |
Container |
Size |
Drug Concentration |
|
|
Lidocaine HCl |
Epinephrine |
|||
|
Single-dose |
||||
|
0409-3181-01 |
Fliptop Vial |
30 mL |
1.5% |
1:200,000 |
|
0409-3183-01 |
Fliptop Vial |
20 mL |
2% |
1:200,000 |
|
Epidural Test Dose (single-dose) |
||||
|
0409-1209-01 |
Ampul |
5 mL |
1.5% |
1:200,000 |
|
0409-1209-05 |
Ampul |
5 mL |
1.5% |
1:200,000 |
|
0409-1209-65 |
Ampul |
5 mL |
1.5% |
1:200,000 |
|
Multiple-dose |
||||
|
0409-3177-01 |
Fliptop Vial |
50 mL |
0.5% |
1:200,000 |
|
0409-3178-01 |
Fliptop Vial |
20 mL |
1% |
1:100,000 |
|
0409-3178-02 |
Fliptop Vial |
30 mL |
1% |
1:100,000 |
|
0409-3178-03 |
Fliptop Vial |
50 mL |
1% |
1:100,000 |
|
0409-3182-01 |
Fliptop Vial |
20 mL |
2% |
1:100,000 |
|
0409-3182-02 |
Fliptop Vial |
30 mL |
2% |
1:100,000 |
|
0409-3182-03 |
Fliptop Vial |
50 mL |
2% |
1:100,000 |
Store at 20 to 25°C (68 to 77°F). [See USP Controlled Room Temperature.] Protect from light.
Revised: March, 2010
Printed in USA EN-2440
Hospira, Inc., Lake Forest, IL 60045 USA<paragraph>
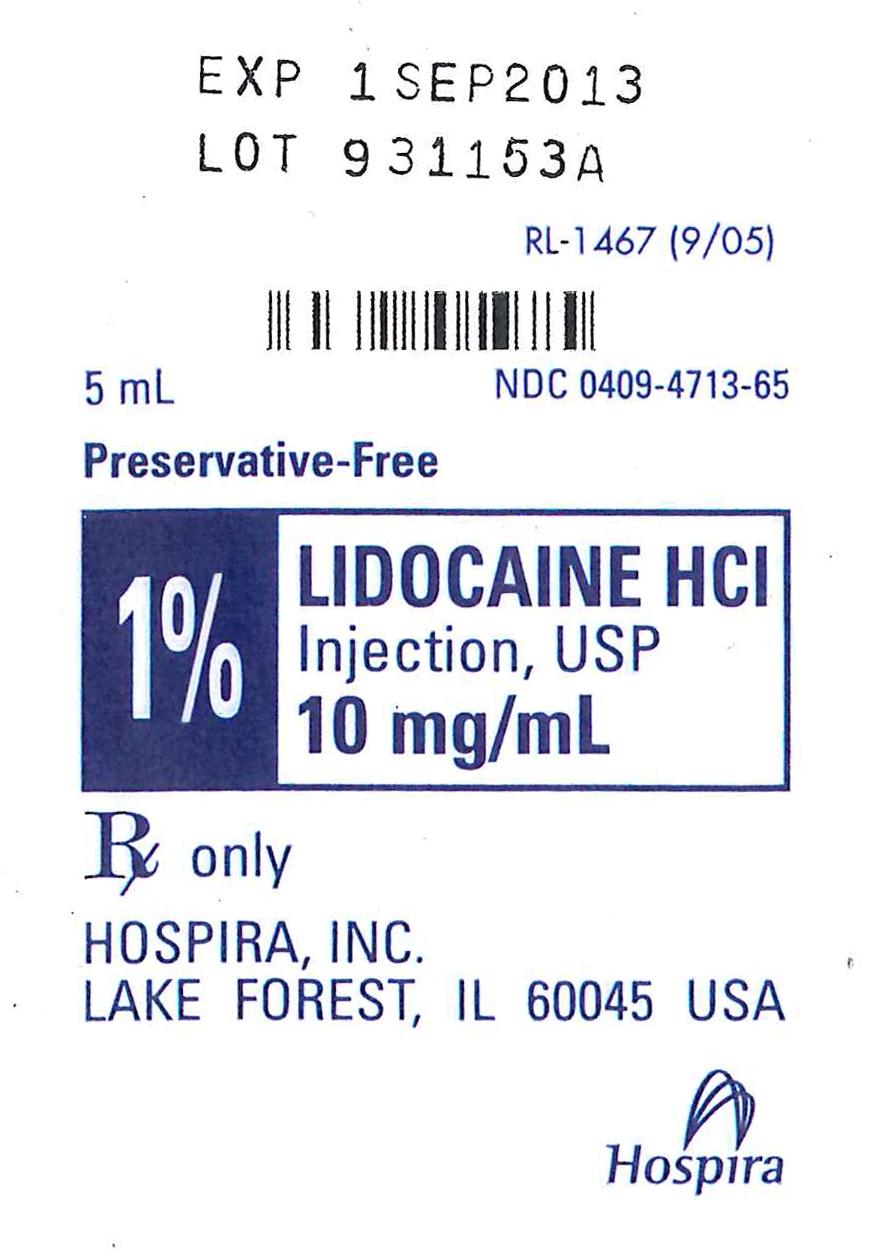
<paragraph>LIDOCAINE HYDROCHLORIDE (lidocaine hydrochloride anhydrous) injection, solution
[Hospira, Inc.]
AQUEOUS SOLUTIONS FOR INFILTRATION
AND NERVE BLOCK
Ampul
Plastic Multiple-dose Fliptop Vial
Glass Teartop Vial
Rx only
DESCRIPTION
Lidocaine Hydrochloride Injection, USP is a sterile, nonpyrogenic solution of lidocaine hydrochloride in water for injection for parenteral administration in various concentrations with characteristics as follows:
|
Concentration |
0.5% |
1% |
1.5% |
2% |
|
mg/mL lidocaine HCl (anhyd.) |
5 |
10 |
15 |
20 |
|
mg/mL sodium chloride |
8 |
7 |
6.5 |
6 |
Multiple-dose vials contain 0.1% of methylparaben added as preservative. May contain sodium hydroxide and/or hydrochloric acid for pH adjustment. The pH is 6.5 (5.0 to 7.0). See HOW SUPPLIED section for various sizes and strengths.
Lidocaine is a local anesthetic of the amide type.
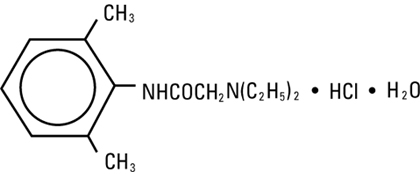
Lidocaine Hydrochloride, USP is chemically designated 2-(diethylamino)-N-(2,6-dimethylphenyl)-acetamide monohydrochloride monohydrate, a white powder freely soluble in water. The molecular weight is 288.82. It has the following structural formula:
The semi-rigid vial used for the plastic vials is fabricated from a specially formulated polyolefin. It is a copolymer of ethylene and propylene. The safety of the plastic has been confirmed by tests in animals according to USP biological standards for plastic containers. The container requires no vapor barrier to maintain the proper drug concentration.<paragraph>
<paragraph>CLINICAL PHARMACOLOGY
Mechanism of action: Lidocaine stabilizes the neuronal membrane by inhibiting the ionic fluxes required for the initiation and conduction of impulses, thereby effecting local anesthetic action.
Hemodynamics: Excessive blood levels may cause changes in cardiac output, total peripheral resistance, and mean arterial pressure. With central neural blockade these changes may be attributable to block of autonomic fibers, a direct depressant effect of the local anesthetic agent on various components of the cardiovascular system and/or the beta-adrenergic receptor stimulating action of epinephrine when present. The net effect is normally a modest hypotension when the recommended dosages are not exceeded.
Pharmacokinetics and metabolism: Information derived from diverse formulations, concentrations and usages reveals that lidocaine is completely absorbed following parenteral administration, its rate of absorption depending, for example, upon various factors such as the site of administration and the presence or absence of a vasoconstrictor agent. Except for intravascular administration, the highest blood levels are obtained following intercostal nerve block and the lowest after subcutaneous administration.
The plasma binding of lidocaine is dependent on drug concentration, and the fraction bound decreases with increasing concentration. At concentrations of 1 to 4 mcg of free base per mL, 60 to 80 percent of lidocaine is protein bound. Binding is also dependent on the plasma concentration of the alpha-1-acid glycoprotein.
Lidocaine crosses the blood-brain and placental barriers, presumably by passive diffusion.
Lidocaine is metabolized rapidly by the liver, and metabolites and unchanged drug are excreted by the kidneys. Biotransformation includes oxidative N-dealkylation, ring hydroxylation, cleavage of the amide linkage, and conjugation. N-dealkylation, a major pathway of biotransformation, yields the metabolites monoethylglycinexylidide and glycinexylidide. The pharmacological/toxicological actions of these metabolites are similar to, but less potent than, those of lidocaine. Approximately 90% of lidocaine administered is excreted in the form of various metabolites, and less than 10% is excreted unchanged. The primary metabolite in urine is a conjugate of 4-hydroxy-2, 6-dimethylaniline.
The elimination half-life of lidocaine following an intravenous bolus injection is typically 1.5 to 2.0 hours. Because of the rapid rate at which lidocaine is metabolized, any condition that affects liver function may alter lidocaine kinetics. The half-life may be prolonged two-fold or more in patients with liver dysfunction. Renal dysfunction does not affect lidocaine kinetics but may increase the accumulation of metabolites.
Factors such as acidosis and the use of CNS stimulants and depressants affect the CNS levels of lidocaine required to produce overt systemic effects. Objective adverse manifestations become increasingly apparent with increasing venous plasma levels above 6.0 mcg free base per mL. In the rhesus monkey arterial blood levels of 18-21 mcg/mL have been shown to be threshold for convulsive activity.<paragraph>
<paragraph>INDICATIONS AND USAGE
Lidocaine Hydrochloride Injection, USP is indicated for production of local or regional anesthesia by infiltration techniques such as percutaneous injection and intravenous regional anesthesia by peripheral nerve block techniques such as brachial plexus and intercostal and by central neural techniques such as lumbar and caudal epidural blocks, when the accepted procedures for these techniques as described in standard textbooks are observed.<paragraph>
<paragraph>CONTRAINDICATIONS
Lidocaine is contraindicated in patients with a known history of hypersensitivity to local anesthetics of the amide type.<paragraph>
<paragraph>WARNINGS
LIDOCAINE HYDROCHLORIDE INJECTION, FOR INFILTRATION AND NERVE BLOCK, SHOULD BE EMPLOYED ONLY BY CLINICIANS WHO ARE WELL VERSED IN DIAGNOSIS AND MANAGEMENT OF DOSE-RELATED TOXICITY AND OTHER ACUTE EMERGENCIES THAT MIGHT ARISE FROM THE BLOCK TO BE EMPLOYED AND THEN ONLY AFTER ENSURING THE IMMEDIATE AVAILABILITY OF OXYGEN, OTHER RESUSCITATIVE DRUGS, CARDIOPULMONARY EQUIPMENT, AND THE PERSONNEL NEEDED FOR PROPER MANAGEMENT OF TOXIC REACTIONS AND RELATED EMERGENCIES (See also ADVERSE REACTIONS and PRECAUTIONS). DELAY IN PROPER MANAGEMENT OF DOSE-RELATED TOXICITY, UNDERVENTILATION FROM ANY CAUSE AND/OR ALTERED SENSITIVITY MAY LEAD TO THE DEVELOPMENT OF ACIDOSIS, CARDIAC ARREST AND, POSSIBLY, DEATH.
Intra-articular infusions of local anesthetics following arthroscopic and other surgical procedures is an unapproved use, and there have been post-marketing reports of chondrolysis in patients receiving such infusions. The majority of reported cases of chondrolysis have involved the shoulder joint; cases of gleno-humeral chondrolysis have been described in pediatric and adult patients following intra-articular infusions of local anesthetics with and without epinephrine for periods of 48 to 72 hours. There is insufficient information to determine whether shorter infusion periods are not associated with these findings. The time of onset of symptoms, such as joint pain, stiffness and loss of motion can be variable, but may begin as early as the 2nd month after surgery. Currently, there is no effective treatment for chondrolysis; patients who experienced chondrolysis have required additional diagnostic and therapeutic procedures and some required arthroplasty or shoulder replacement.
To avoid intravascular injection, aspiration should be performed before the local anesthetic solution is injected. The needle must be repositioned until no return of blood can be elicited by aspiration. Note, however, that the absence of blood in the syringe does not guarantee that intravascular injection has been avoided.
Local anesthetic solutions containing antimicrobial preservatives (e.g., methylparaben) should not be used for epidural or spinal anesthesia because the safety of these agents has not been established with regard to intrathecal injection, either intentional or accidental.<paragraph>
<paragraph> PRECAUTIONSGeneral:
The safety and effectiveness of lidocaine depend on proper dosage, correct technique, adequate precautions, and readiness for emergencies. Standard textbooks should be consulted for specific techniques and precautions for various regional anesthetic procedures.
Resuscitative equipment, oxygen, and other resuscitative drugs should be available for immediate use. (See WARNINGS and ADVERSE REACTIONS). The lowest dosage that results in effective anesthesia should be used to avoid high plasma levels and serious adverse effects. Syringe aspirations should also be performed before and during each supplemental injection when using indwelling catheter techniques. During the administration of epidural anesthesia, it is recommended that a test dose be administered initially and that the patient be monitored for central nervous system toxicity and cardiovascular toxicity, as well as for signs of unintended intrathecal administration before proceeding. When clinical conditions permit, consideration should be given to employing local anesthetic solutions that contain epinephrine for the test dose because circulatory changes compatible with epinephrine may also serve as a warning sign of unintended intravascular injection. An intravascular injection is still possible even if aspirations for blood are negative. Repeated doses of lidocaine may cause significant increases in blood levels with each repeated dose because of slow accumulation of the drug or its metabolites. Tolerance to elevated blood levels varies with the status of the patient. Debilitated, elderly patients, acutely ill patients and children should be given reduced doses commensurate with their age and physical condition. Lidocaine should also be used with caution in patients with severe shock or heart block. Lumbar and caudal epidural anesthesia should be used with extreme caution in persons with the following conditions: existing neurological disease, spinal deformities, septicemia and severe hypertension.
Local anesthetic solutions containing a vasoconstrictor should be used cautiously and in carefully circumscribed quantities in areas of the body supplied by end arteries or having otherwise compromised blood supply. Patients with peripheral vascular disease and those with hypertensive vascular disease may exhibit exaggerated vasoconstrictor response. Ischemic injury or necrosis may result. Preparations containing a vasoconstrictor should be used with caution in patients during or following the administration of potent general anesthetic agents, since cardiac arrhythmias may occur under such conditions.
Careful and constant monitoring of cardiovascular and respiratory (adequacy of ventilation) vital signs and the patient’s state of consciousness should be accomplished after each local anesthetic injection. It should be kept in mind at such times that restlessness, anxiety, tinnitus, dizziness, blurred vision, tremors, depression or drowsiness may be early warning signs of central nervous system toxicity.
Since amide-type local anesthetics are metabolized by the liver, lidocaine should be used with caution in patients with hepatic disease. Patients with severe hepatic disease, because of their inability to metabolize local anesthetics normally, are at greater risk of developing toxic plasma concentrations. Lidocaine should also be used with caution in patients with impaired cardiovascular function since they may be less able to compensate for functional changes associated with the prolongation of A-V conduction produced by these drugs. Many drugs used during the conduct of anesthesia are considered potential triggering agents for familial malignant hyperthermia. Since it is not known whether amide-type local anesthetics may trigger this reaction and since the need for supplemental general anesthesia cannot be predicted in advance, it is suggested that a standard protocol for the management of malignant hyperthermia should be available. Early unexplained signs of tachycardia, tachypnea, labile blood pressure and metabolic acidosis may precede temperature elevation. Successful outcome is dependent on early diagnosis, prompt discontinuance of the suspect triggering agent(s) and institution of treatment, including oxygen therapy, indicated supportive measures and dantrolene (consult dantrolene sodium intravenous package insert before using).
Proper tourniquet technique, as described in publications and standard textbooks, is essential in the performance of intravenous regional anesthesia. Solutions containing epinephrine or other vasoconstrictors should not be used for this technique.
Lidocaine should be used with caution in persons with known drug sensitivities. Patients allergic to para-aminobenzoic acid derivatives (procaine, tetracaine, benzocaine, etc.) have not shown cross sensitivity to lidocaine.
Use in the Head and Neck Area: Small doses of local anesthetics injected into the head and neck area, including retrobulbar, dental and stellate ganglion blocks, may produce adverse reactions similar to systemic toxicity seen with unintentional intravascular injections of larger doses. Confusion, convulsions, respiratory depression and/or respiratory arrest and cardiovascular stimulation or depression have been reported. These reactions may be due to intra-arterial injections of the local anesthetic with retrograde flow to the cerebral circulation. Patients receiving these blocks should have their circulation and respiration monitored and be constantly observed. Resuscitative equipment and personnel for treating adverse reactions should be immediately available. Dosage recommendations should not be exceeded. (See DOSAGE AND ADMINISTRATION).
Information for Patients:
When appropriate, patients should be informed in advance that they may experience temporary loss of sensation and motor activity, usually in the lower half of the body following proper administration of epidural anesthesia.
Clinically Significant Drug Interactions:
The administration of local anesthetic solutions containing epinephrine or norepinephrine to patients receiving monoamine oxidase inhibitors or tricyclic antidepressants may produce severe prolonged hypertension.
Phenothiazines and butyrophenones may reduce or reverse the pressor effect of epinephrine.
Concurrent use of these agents should generally be avoided. In situations when concurrent therapy is necessary, careful patient monitoring is essential.
Concurrent administration of vasopressor drugs (for the treatment of hypotension related to obstetric blocks) and ergot-type oxytoxic drugs may cause severe persistent hypertension or cerebrovascular accidents.
Drug Laboratory Test Interactions:
The intramuscular injection of lidocaine may result in an increase in creatine phosphokinase levels. Thus, the use of this enzyme determination without isoenzyme separation as a diagnostic test for the presence of acute myocardial infarction may be compromised by the intramuscular injection of lidocaine.
Carcinogenesis, Mutagenesis, Impairment of Fertility:
Studies of lidocaine in animals to evaluate the carcinogenic and mutagenic potential or the effect on fertility have not been conducted.
Pregnancy:
Teratogenic Effects. Pregnancy Category B. Reproduction studies have been performed in rats at doses up to 6.6 times the human dose and have revealed no evidence of harm to the fetus caused by lidocaine. There are, however, no adequate and well-controlled studies in pregnant women. Animal reproduction studies are not always predictive of human response. General consideration should be given to this fact before administering lidocaine to women of childbearing potential, especially during early pregnancy when maximum organogenesis takes place.
Labor and Delivery:
Local anesthetics rapidly cross the placenta and when used for epidural, paracervical, pudendal or caudal block anesthesia, can cause varying degrees of maternal, fetal and neonatal toxicity (See CLINICAL PHARMACOLOGY—Pharmacokinetics). The potential for toxicity depends upon the procedure performed, the type and amount of drug used, and the technique of drug administration. Adverse reactions in the parturient, fetus and neonate involve alterations of the central nervous system peripheral vascular tone and cardiac function.
Maternal hypotension has resulted from regional anesthesia. Local anesthetics produce vasodilation by blocking sympathetic nerves. Elevating the patient’s legs and positioning her on her left side will help prevent decreases in blood pressure. The fetal heart rate also should be monitored continuously, and electronic fetal monitoring is highly advisable.
Epidural, spinal, paracervical, or pudendal anesthesia may alter the forces of parturition through changes in uterine contractility or maternal expulsive efforts. In one study, paracervical block anesthesia was associated with a decrease in the mean duration of first stage labor and facilitation of cervical dilation. However, spinal and epidural anesthesia have also been reported to prolong the second stage of labor by removing the parturient’s reflex urge to bear down or by interfering with motor function. The use of obstetrical anesthesia may increase the need for forceps assistance.
The use of some local anesthetic drug products during labor and delivery may be followed by diminished muscle strength and tone for the first day or two of life. The long-term significance of these observations is unknown. Fetal bradycardia may occur in 20 to 30 percent of patients receiving paracervical nerve block anesthesia with the amide-type local anesthetics and may be associated with fetal acidosis. Fetal heart rate should always be monitored during paracervical anesthesia. The physician should weigh the possible advantages against risks when considering paracervical block in prematurity, toxemia of pregnancy and fetal distress. Careful adherence to recommended dosage is of the utmost importance in obstetrical paracervical block. Failure to achieve adequate analgesia with recommended doses should arouse suspicion of intravascular or fetal intracranial injection. Cases compatible with unintended fetal intracranial injection of local anesthetic solution have been reported following intended paracervical or pudendal block or both. Babies so affected present with unexplained neonatal depression at birth, which correlates with high local anesthetic serum levels, and often manifest seizures within six hours. Prompt use of supportive measures combined with forced urinary excretion of the local anesthetic has been used successfully to manage this complication.
Case reports of maternal convulsions and cardiovascular collapse following use of some local anesthetics for paracervical block in early pregnancy (as anesthesia for elective abortion) suggest that systemic absorption under these circumstances may be rapid. The recommended maximum dose of each drug should not be exceeded. Injection should be made slowly and with frequent aspiration. Allow a 5-minute interval between sides.
Nursing Mothers:
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when lidocaine is administered to a nursing woman.
Pediatric Use:
Dosages in pediatric patients should be reduced, commensurate with age, body weight and physical condition. See DOSAGE AND ADMINISTRATION.<paragraph>
<paragraph>ADVERSE REACTIONS
Systemic: Adverse experiences following the administration of lidocaine are similar in nature to those observed with other amide local anesthetic agents. These adverse experiences are, in general, dose-related and may result from high plasma levels caused by excessive dosage, rapid absorption or inadvertent intravascular injection, or may result from a hypersensitivity, idiosyncrasy or diminished tolerance on the part of the patient. Serious adverse experiences are generally systemic in nature. The following types are those most commonly reported:
Central Nervous System: CNS manifestations are excitatory and/or depressant and may be characterized by lightheadedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression and arrest. The excitatory manifestations may be very brief or may not occur at all, in which case the first manifestation of toxicity may be drowsiness merging into unconsciousness and respiratory arrest.
Drowsiness following the administration of lidocaine is usually an early sign of a high blood level of the drug and may occur as a consequence of rapid absorption.
Cardiovascular System: Cardiovascular manifestations are usually depressant and are characterized by bradycardia, hypotension, and cardiovascular collapse, which may lead to cardiac arrest.
Allergic: Allergic reactions are characterized by cutaneous lesions, urticaria, edema or anaphylactoid reactions. Allergic reactions may occur as a result of sensitivity either to local anesthetic agents or to the methylparaben used as a preservative in multiple dose vials. Allergic reactions as a result of sensitivity to lidocaine are extremely rare and, if they occur, should be managed by conventional means. The detection of sensitivity by skin testing is of doubtful value.
Neurologic: The incidences of adverse reactions associated with the use of local anesthetics may be related to the total dose of local anesthetic administered and are also dependent upon the particular drug used, the route of administration and the physical status of the patient. In a prospective review of 10,440 patients who received lidocaine for spinal anesthesia, the incidences of adverse reactions were reported to be about 3 percent each for positional headaches, hypotension and backache; 2 percent for shivering; and less than 1 percent each for peripheral nerve symptoms, nausea, respiratory inadequacy and double vision. Many of these observations may be related to local anesthetic techniques, with or without a contribution from the local anesthetic.
In the practice of caudal or lumbar epidural block, occasional unintentional penetration of the subarachnoid space by the catheter may occur. Subsequent adverse effects may depend partially on the amount of drug administered subdurally.
These may include spinal block of varying magnitude (including total spinal block), hypotension secondary to spinal block, loss of bladder and bowel control, and loss of perineal sensation and sexual function. Persistent motor, sensory and/or autonomic (sphincter control) deficit of some lower spinal segments with slow recovery (several months) or incomplete recovery have been reported in rare instances when caudal or lumbar epidural block has been attempted. Backache and headache have also been noted following use of these anesthetic procedures.
There have been reported cases of permanent injury to extraocular muscles requiring surgical repair following retrobulbar administration.<paragraph>
<paragraph>OVERDOSAGE
Acute emergencies from local anesthetics are generally related to high plasma levels encountered during therapeutic use of local anesthetics or to unintended subarachnoid injection of local anesthetic solution (see ADVERSE REACTIONS, WARNINGS and PRECAUTIONS).
Management of Local Anesthetic Emergencies: The first consideration is prevention, best accomplished by careful monitoring of cardiovascular and respiratory vital signs and the patient’s state of consciousness after each local anesthetic injection. At the first sign of change, oxygen should be administered.
The first step in the management of convulsions, as well as underventilation or apnea due to unintended subarachnoid injection of drug solution, consists of immediate attention to the maintenance of a patent airway and assisted or controlled ventilation with oxygen and a delivery system capable of permitting immediate positive airway pressure by mask. Immediately after the institution of these ventilatory measures, the adequacy of the circulation should be evaluated, keeping in mind that drugs used to treat convulsions sometimes depress the circulation when administered intravenously. Should convulsions persist despite adequate respiratory support, and if the status of the circulation permits, small increments of an ultra-short acting barbiturate (such as thiopental or thiamylal) or a benzodiazepine (such as diazepam) may be administered intravenously. The clinician should be familiar, prior to use of local anesthetics, with these anticonvulsant drugs. Supportive treatment of circulatory depression may require administration of intravenous fluids and, when appropriate, a vasopressor as directed by the clinical situation (e.g., ephedrine).
If not treated immediately, both convulsions and cardiovascular depression can result in hypoxia, acidosis, bradycardia, arrhythmias and cardiac arrest. Underventilation or apnea due to unintentional subarachnoid injection of local anesthetic solution may produce these same signs and also lead to cardiac arrest if ventilatory support is not instituted. If cardiac arrest should occur standard cardiopulmonary resuscitative measures should be instituted.
Endotracheal intubation, employing drugs and techniques familiar to the clinician, may be indicated, after initial administration of oxygen by mask, if difficulty is encountered in the maintenance of a patent airway or if prolonged ventilatory support (assisted or controlled) is indicated.
Dialysis is of negligible value in the treatment of acute overdosage with lidocaine.
The oral LD50 of lidocaine HCl in non-fasted female rats is 459 (346−773) mg/kg (as the salt) and 214 (159−324) mg/kg (as the salt) in fasted female rats.<paragraph>
<paragraph>DOSAGE AND ADMINISTRATION
Table 1 (Recommended Dosages) summarizes the recommended volumes and concentrations of Lidocaine Hydrochloride Injection, USP for various types of anesthetic procedures. The dosages suggested in this table are for normal healthy adults and refer to the use of epinephrine-free solutions. When larger volumes are required only solutions containing epinephrine should be used, except in those cases where vasopressor drugs may be contraindicated.
There have been adverse event reports of chondrolysis in patients receiving intra-articular infusions of local anesthetics following arthroscopic and other surgical procedures. Lidocaine is not approved for this use (see WARNINGS and DOSAGE AND ADMINISTRATION).
These recommended doses serve only as a guide to the amount of anesthetic required for most routine procedures. The actual volumes and concentrations to be used depend on a number of factors such as type and extent of surgical procedure, depth of anesthesia and degree of muscular relaxation required, duration of anesthesia required, and the physical condition of the patient. In all cases the lowest concentration and smallest dose that will produce the desired result should be given. Dosages should be reduced for children and for elderly and debilitated patients and patients with cardiac and/or liver disease.
The onset of anesthesia, the duration of anesthesia and the degree of muscular relaxation are proportional to the volume and concentration (i.e., total dose) of local anesthetic used. Thus, an increase in volume and concentration of Lidocaine Hydrochloride Injection will decrease the onset of anesthesia, prolong the duration of anesthesia, provide a greater degree of muscular relaxation and increase the segmental spread of anesthesia. However, increasing the volume and concentration of Lidocaine Hydrochloride Injection may result in a more profound fall in blood pressure when used in epidural anesthesia. Although the incidence of side effects with lidocaine is quite low, caution should be exercised when employing large volumes and concentrations, since the incidence of side effects is directly proportional to the total dose of local anesthetic agent injected.
For intravenous regional anesthesia, only the 50 mL single-dose vial containing 0.5% Lidocaine Hydrochloride Injection, USP should be used.
Epidural Anesthesia
For epidural anesthesia, only the following available specific products of Lidocaine Hydrochloride Injection by Hospira are recommended:
1%. . . . . . . . . . . . . . . . . . . . 30 mL single-dose teartop vials
1.5%. . . . . . . . . . . . . . . . . . . . . . . 20 mL single-dose ampuls
2%. . . . . . . . . . . . . . . . . . . . . . . . . 10 mL single-dose ampuls
Although these solutions are intended specifically for epidural anesthesia, they may also be used for infiltration and peripheral nerve block provided they are employed as single dose units. These solutions contain no bacteriostatic agent. In epidural anesthesia, the dosage varies with the number of dermatomes to be anesthetized (generally 2−3 mL of the indicated concentration per dermatome).
Caudal and Lumbar Epidural Block: As a precaution against the adverse experiences sometimes observed following unintentional penetration of the subarachnoid space, a test dose such as 2−3 mL of 1.5% lidocaine hydrochloride should be administered at least 5 minutes prior to injecting the total volume required for a lumbar or caudal epidural block. The test dose should be repeated if the patient is moved in a manner that may have displaced the catheter. Epinephrine, if contained in the test dose (10−15 mcg have been suggested), may serve as a warning of unintentional intravascular injection. If injected into a blood vessel, this amount of epinephrine is likely to produce a transient "epinephrine response" within 45 seconds, consisting of an increase in heart rate and systolic blood pressure, circumoral pallor, palpitations and nervousness in the unsedated patient. The sedated patient may exhibit only a pulse rate increase of 20 or more beats per minute for 15 or more seconds. Patients on beta-blockers may not manifest changes in heart rate, but blood pressure monitoring can detect an evanescent rise in systolic blood pressure. Adequate time should be allowed for onset of anesthesia after administration of each test dose. The rapid injection of a large volume of Lidocaine Hydrochloride Injection through the catheter should be avoided, and, when feasible, fractional doses should be administered.
In the event of the known injection of a large volume of local anesthetic solutions into the subarachnoid space, after suitable resuscitation and if the catheter is in place, consider attempting the recovery of drug by draining a moderate amount of cerebrospinal fluid (such as 10 mL) through the epidural catheter.
Maximum Recommended Dosages
NOTE: The products accompanying this insert do not contain epinephrine.
Adults: For normal healthy adults, the individual maximum recommended dose of lidocaine HCl with epinephrine should not exceed 7 mg/kg (3.5 mg/lb) of body weight and in general it is recommended that the maximum total dose not exceed 500 mg. When used without epinephrine, the maximum individual dose should not exceed 4.5 mg/kg (2 mg/lb) of body weight and in general it is recommended that the maximum total dose does not exceed 300 mg. For continuous epidural or caudal anesthesia, the maximum recommended dosage should not be administered at intervals of less than 90 minutes. When continuous lumbar or caudal epidural anesthesia is used for non-obstetrical procedures, more drug may be administered if required to produce adequate anesthesia.
The maximum recommended dose per 90 minute period of lidocaine hydrochloride for paracervical block in obstetrical patients and non-obstetrical patients is 200 mg total. One-half of the total dose is usually administered to each side. Inject slowly five minutes between sides. (See also discussion of paracervical block in PRECAUTIONS).
For intravenous regional anesthesia, the dose administered should not exceed 4 mg/kg in adults.
Children: It is difficult to recommend a maximum dose of any drug for children, since this varies as a function of age and weight. For children over 3 years of age who have a normal lean body mass and normal body development, the maximum dose is determined by the child’s age and weight. For example, in a child of 5 years weighing 50 lbs., the dose of lidocaine HCl should not exceed 75 — 100 mg (1.5 — 2 mg/lb). The use of even more dilute solutions (i.e., 0.25 — 0.5%) and total dosages not to exceed 3 mg/kg (1.4 mg/lb) are recommended for induction of intravenous regional anesthesia in children.
In order to guard against systemic toxicity, the lowest effective concentration and lowest effective dose should be used at all times. In some cases it will be necessary to dilute available concentrations with 0.9% sodium chloride injection in order to obtain the required final concentration.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever the solution and container permit. Solutions that are discolored and/or contain particulate matter should not be used.
|
Table 1 |
|||
|
Recommended Dosages of Lidocaine Hydrochloride Injection, USP for Various Anesthetic |
|||
|
Procedures in Normal Healthy Adults |
|||
|
Lidocaine Hydrochloride Injection, USP (without Epinephrine) |
|||
|
Procedure |
Conc. (%) |
Vol. (mL) |
Total Dose (mg) |
|
Infiltration | |||
|
Percutaneous |
0.5 or 1.0 |
1−60 |
5−300 |
|
Intravenous Regional |
0.5 |
10−60 |
50−300 |
|
Peripheral Nerve Blocks, e.g. | |||
|
Brachial |
1.5 |
15−20 |
225−300 |
|
Dental |
2.0 |
1−5 |
20−100 |
|
Intercostal |
1.0 |
3 |
30 |
|
Paravertebral |
1.0 |
3−5 |
30−50 |
|
Pudendal (each side) |
1.0 |
10 |
100 |
|
Paracervical | |||
|
Obstetrical Analgesia | |||
|
(each side) |
1.0 |
10 |
100 |
|
Sympathetic Nerve Blocks, e.g. | |||
|
Cervical (stellate ganglion) |
1.0 |
5 |
50 |
|
Lumbar |
1.0 |
5−10 |
50−100 |
|
Central Neural Blocks | |||
|
Epidural* | |||
|
Thoracic |
1.0 |
20−30 |
200−300 |
|
Lumbar | |||
|
Analgesia |
1.0 |
25−30 |
250−300 |
|
Anesthesia |
1.5 |
15−20 |
225−300 |
|
2.0 |
10−15 |
200−300 |
|
|
Caudal | |||
|
Obstetrical Analgesia |
1.0 |
20−30 |
200−300 |
|
Surgical Anesthesia |
1.5 |
15−20 |
225−300 |
|
*Dose determined by number of dermatomes to be anesthetized (2 to 3 mL/dermatome). |
THE ABOVE SUGGESTED CONCENTRATIONS AND VOLUMES SERVE ONLY AS A GUIDE. OTHER VOLUMES AND CONCENTRATIONS MAY BE USED PROVIDED THE TOTAL MAXIMUM RECOMMENDED DOSE IS NOT EXCEEDED.
Sterilization, Storage and Technical Procedures: Disinfecting agents containing heavy metals, which cause release of respective ions (mercury, zinc, copper, etc.) should not be used for skin or mucous membrane disinfection as they have been related to incidence of swelling and edema. When chemical disinfection of multi-dose vials is desired, either isopropyl alcohol (91%) or 70% ethyl alcohol is recommended. Many commercially available brands of rubbing alcohol, as well as solutions of ethyl alcohol not of USP grade, contain denaturants which are injurious to rubber and, therefore, are not to be used. It is recommended that chemical disinfection be accomplished by wiping the vial stopper thoroughly with cotton or gauze that has been moistened with the recommended alcohol just prior to use.<paragraph>
<paragraph>HOW SUPPLIED
Lidocaine Hydrochloride Injection, USP is supplied as follows:
|
NDC |
Container |
Concentration |
Size |
Total (mg) |
|
Single-dose: | ||||
|
0409-4278-01 |
Glass Teartop Vial |
0.5% (5 mg/mL) |
50 mL |
250 |
|
0409-4713-01 |
Glass Ampul |
1% (10 mg/mL) |
2 mL (bulk – 400 units) |
20 |
|
0409-4713-02 |
Glass Ampul |
1% (10 mg/mL) |
5 mL |
50 |
|
0409-4713-05 |
Glass Ampul |
1% (10 mg/mL) |
5 mL (bulk – 400 units) |
50 |
|
0409-4713-20 |
Glass Ampul |
1% (10 mg/mL) |
20 mL |
200 |
|
0409-4713-32 |
Glass Ampul |
1% (10 mg/mL) |
2 mL |
20 |
|
0409-4713-62 |
Glass Ampul |
1% (10 mg/mL) |
2 mL (bulk – 800 units) |
20 |
|
0409-4713-65 |
Glass Ampul |
1% (10 mg/mL) |
5 mL (bulk – 800 units) |
50 |
|
0409-4279-02 |
Glass Teartop Vial |
1% (10 mg/mL) |
30 mL |
300 |
|
0409-4270-01 |
Sterile Glass Teartop Vial |
1% (10 mg/mL) |
30 mL |
300 |
|
0409-4776-01 |
Glass Ampul |
1.5% (15 mg/mL) |
20 mL |
300 |
|
0409-4056-01 |
Sterile Glass Ampul |
1.5% (15 mg/mL) |
20 mL |
300 |
|
0409-4282-01 |
Glass Ampul |
2% (20 mg/mL) |
2 mL |
40 |
|
0409-4282-02 |
Glass Ampul |
2% (20 mg/mL) |
10 mL |
200 |
|
Multiple-dose: | ||||
|
0409-4275-01 |
Plastic Fliptop Vial |
0.5% (5 mg/mL) |
50 mL |
250 |
|
0409-4276-01 |
Plastic Fliptop Vial |
1% (10 mg/mL) |
20 mL |
200 |
|
0409-4276-02 |
Plastic Fliptop Vial |
1% (10 mg/mL) |
50 mL |
500 |
|
0409-4277-01 |
Plastic Fliptop Vial |
2% (20 mg/mL) |
20 mL |
400 |
|
0409-4277-02 |
Plastic Fliptop Vial |
2% (20 mg/mL) |
50 mL |
1000 |
Single-dose products are preservative-free.
Store at 20 to 25°C (68 to 77°F). [See USP Controlled Room Temperature.]
Lidocaine Hydrochloride Injection, USP solutions packaged in ampuls and glass teartop vials may be autoclaved one time only. Autoclave at 15 pounds pressure, 121°C (250°F) for 15 minutes. DO NOT AUTOCLAVE PRODUCT IN PLASTIC VIALS.
Revised: February, 2010
Printed in USA EN-2421
Hospira, Inc., Lake Forest, IL 60045 USA
TY-0067<paragraph>
<paragraph>
3/4 Fluid Ounce Povidone Iodine
Povidone-iodine 10%
Antiseptic
Warnings
Do not use
- if allergic to iodine
- in the eyes
For external use only
Ask a doctor before use if injuries are
- deep or puncture wounds
- serious burns
Stop use and ask a doctor if
- redness, irritation, swelling or pain persists or increases
- infection occurs
Avoid pooling beneath patient
Keep out of reach of children.In case of accidental ingestion, seek professional assistance or consult a poison control center immediately.<paragraph>
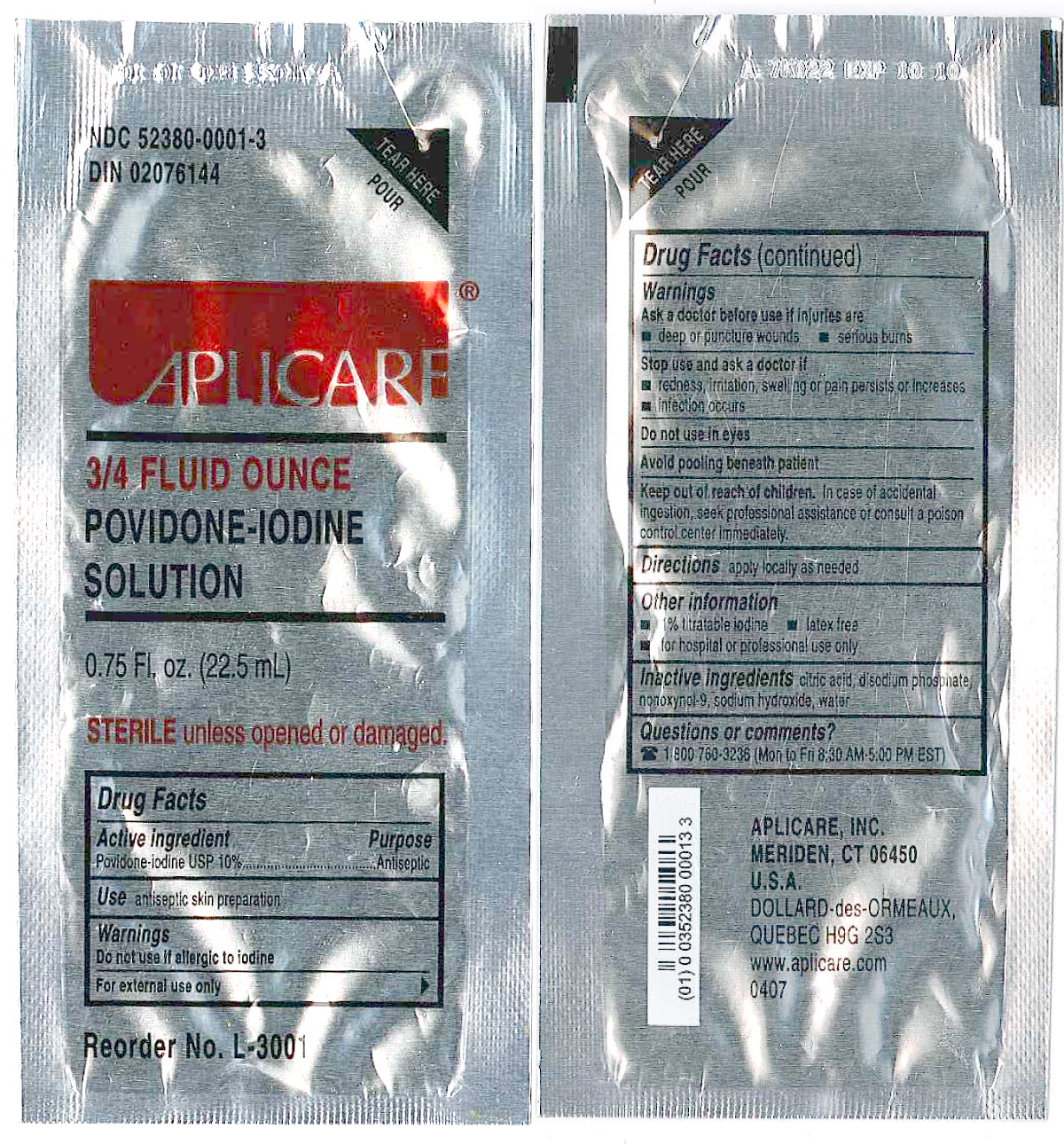
| 4848-18 CONTINUOUS EPIDURAL 18G TUOHY
regional anesthesia kit c47916 |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| Labeler - Smiths Medical ASD, Inc. (137835299) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Smiths Medical ASD, Inc. | 137835299 | relabel, manufacture | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Hospira, Inc. | 030606222 | manufacture | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Hospira, Inc. | 093132819 | manufacture | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Kwang Myung Pharm. Co., Ltd. | 631099384 | manufacture | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Aplicare, Inc. | 081054904 | manufacture | |