ALPRAZOLAM XR- alprazolam tablet, extended release
Alprazolam by
Drug Labeling and Warnings
Alprazolam by is a Prescription medication manufactured, distributed, or labeled by Greenstone LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
BOXED WARNING
(What is this?)
WARNING: RISKS FROM CONCOMITANT USE WITH OPIOIDS
Concomitant use of benzodiazepines and opioids may result in profound sedation, respiratory depression, coma, and death [see Warnings, Drug Interactions].
- Reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate.
- Limit dosages and durations to the minimum required.
- Follow patients for signs and symptoms of respiratory depression and sedation.
-
DESCRIPTION
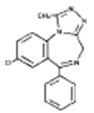
Alprazolam XR tablets contain alprazolam which is a triazolo analog of the 1,4 benzodiazepine class of central nervous system-active compounds.
The chemical name of alprazolam is 8-chloro-1-methyl-6-phenyl-4H-s-triazolo [4,3-α] [1,4] benzodiazepine. The molecular formula is C17H13ClN4 which corresponds to a molecular weight of 308.76.
The structural formula is represented below:
Alprazolam is a white crystalline powder, which is soluble in methanol or ethanol but which has no appreciable solubility in water at physiological pH.
Each Alprazolam XR extended-release tablet, for oral administration, contains 0.5 mg, 1 mg, 2 mg, or 3 mg of alprazolam. The inactive ingredients are lactose, magnesium stearate, colloidal silicon dioxide, and hypromellose. In addition, the 1 mg and 3 mg tablets contain D & C yellow No. 10 and the 2 mg and 3 mg tablets contain FD&C blue No. 2.
-
CLINICAL PHARMACOLOGY
Pharmacodynamics
CNS agents of the 1,4 benzodiazepine class presumably exert their effects by binding at stereospecific receptors at several sites within the central nervous system. Their exact mechanism of action is unknown. Clinically, all benzodiazepines cause a dose-related central nervous system depressant activity varying from mild impairment of task performance to hypnosis.
Pharmacokinetics
Absorption
Following oral administration of Alprazolam (immediate-release) tablets, alprazolam is readily absorbed. Peak concentrations in the plasma occur in one to two hours following administration. Plasma levels are proportional to the dose given; over the dose range of 0.5 to 3.0 mg, peak levels of 8.0 to 37 ng/mL were observed. Using a specific assay methodology, the mean plasma elimination half-life of alprazolam has been found to be about 11.2 hours (range: 6.3–26.9 hours) in healthy adults.
The mean absolute bioavailability of alprazolam from Alprazolam XR tablets is approximately 90%, and the relative bioavailability compared to Alprazolam tablets is 100%. The bioavailability and pharmacokinetics of alprazolam following administration of Alprazolam XR tablets are similar to that for Alprazolam tablets, with the exception of a slower rate of absorption. The slower absorption rate results in a relatively constant concentration that is maintained between 5 and 11 hours after the dosing. The pharmacokinetics of alprazolam and two of its major active metabolites (4-hydroxyalprazolam and α-hydroxyalprazolam) are linear, and concentrations are proportional up to the recommended maximum daily dose of 10 mg given once daily. Multiple dose studies indicate that the metabolism and elimination of alprazolam are similar for the immediate-release and the extended-release products.
Food has a significant influence on the bioavailability of Alprazolam XR tablets. A high-fat meal given up to 2 hours before dosing with Alprazolam XR tablets increased the mean Cmax by about 25%. The effect of this meal on Tmax depended on the timing of the meal, with a reduction in Tmax by about 1/3 for subjects eating immediately before dosing and an increase in Tmax by about 1/3 for subjects eating 1 hour or more after dosing. The extent of exposure (AUC) and elimination half-life (t1/2) were not affected by eating.
There were significant differences in absorption rate for the Alprazolam XR tablet, depending on the time of day administered, with the Cmax increased by 30% and the Tmax decreased by an hour following dosing at night, compared to morning dosing.
Distribution
The apparent volume of distribution of alprazolam is similar for Alprazolam XR and Alprazolam tablets. In vitro, alprazolam is bound (80%) to human serum protein. Serum albumin accounts for the majority of the binding.
Metabolism
Alprazolam is extensively metabolized in humans, primarily by cytochrome P450 3A4 (CYP3A4), to two major metabolites in the plasma: 4-hydroxyalprazolam and α-hydroxyalprazolam. A benzophenone derived from alprazolam is also found in humans. Their half-lives appear to be similar to that of alprazolam. The pharmacokinetic parameters at steady-state for the two hydroxylated metabolites of alprazolam (4-hydroxyalprazolam and α-hydroxyalprazolam) were similar for Alprazolam and Alprazolam XR tablets, indicating that the metabolism of alprazolam is not affected by absorption rate. The plasma concentrations of 4-hydroxyalprazolam and α-hydroxyalprazolam relative to unchanged alprazolam concentration after both Alprazolam XR and Alprazolam tablets were always less than 10% and 4%, respectively. The reported relative potencies in benzodiazepine receptor binding experiments and in animal models of induced seizure inhibition are 0.20 and 0.66, respectively, for 4-hydroxyalprazolam and α-hydroxyalprazolam. Such low concentrations and the lesser potencies of 4-hydroxyalprazolam and α-hydroxyalprazolam suggest that they are unlikely to contribute much to the pharmacological effects of alprazolam. The benzophenone metabolite is essentially inactive.
Elimination
Alprazolam and its metabolites are excreted primarily in the urine. The mean plasma elimination half-life of alprazolam following administration of Alprazolam XR tablet ranges from 10.7–15.8 hours in healthy adults.
Special Populations
While pharmacokinetic studies have not been performed in special populations with Alprazolam XR tablets, the factors (such as age, gender, hepatic or renal impairment) that would affect the pharmacokinetics of alprazolam after the administration of Alprazolam tablets would not be expected to be different with the administration of Alprazolam XR tablets.
Changes in the absorption, distribution, metabolism, and excretion of benzodiazepines have been reported in a variety of disease states including alcoholism, impaired hepatic function, and impaired renal function. Changes have also been demonstrated in geriatric patients. A mean half-life of alprazolam of 16.3 hours has been observed in healthy elderly subjects (range: 9.0–26.9 hours, n=16) compared to 11.0 hours (range: 6.3–15.8 hours, n=16) in healthy adult subjects. In patients with alcoholic liver disease the half-life of alprazolam ranged between 5.8 and 65.3 hours (mean: 19.7 hours, n=17) as compared to between 6.3 and 26.9 hours (mean=11.4 hours, n=17) in healthy subjects. In an obese group of subjects the half-life of alprazolam ranged between 9.9 and 40.4 hours (mean=21.8 hours, n=12) as compared to between 6.3 and 15.8 hours (mean=10.6 hours, n=12) in healthy subjects.
Because of its similarity to other benzodiazepines, it is assumed that alprazolam undergoes transplacental passage and that it is excreted in human milk.
Race
Maximal concentrations and half-life of alprazolam are approximately 15% and 25% higher in Asians compared to Caucasians.
Drug-Drug Interactions
Alprazolam is primarily eliminated by metabolism via cytochrome P450 3A (CYP3A). Most of the interactions that have been documented with alprazolam are with drugs that inhibit or induce CYP3A4.
Compounds that are potent inhibitors of CYP3A would be expected to increase plasma alprazolam concentrations. Drug products that have been studied in vivo, along with their effect on increasing alprazolam AUC, are as follows: ketoconazole, 3.98 fold; itraconazole, 2.70 fold; nefazodone, 1.98 fold; fluvoxamine, 1.96 fold; and erythromycin, 1.61 fold (see CONTRAINDICATIONS, WARNINGS, and PRECAUTIONS–Drug Interactions).
CYP3A inducers would be expected to decrease alprazolam concentrations and this has been observed in vivo. The oral clearance of alprazolam (given in a 0.8 mg single dose) was increased from 0.90±0.21 mL/min/kg to 2.13±0.54 mL/min/kg and the elimination t1/2 was shortened (from 17.1±4.9 to 7.7±1.7 h) following administration of 300 mg/day carbamazepine for 10 days (see PRECAUTIONS–Drug Interactions). However, the carbamazepine dose used in this study was fairly low compared to the recommended doses (1000–1200 mg/day); the effect at usual carbamazepine doses is unknown.
Interactions involving HIV protease inhibitors (eg, ritonavir) and alprazolam are complex and time dependent. Short-term low doses of ritonavir (4 doses of 200 mg) reduced alprazolam clearance to 41% of control values, prolonged its elimination half-life (mean values, 30 versus 13 h) and enhanced clinical effects. However, upon extended exposure to ritonavir (500 mg, twice daily), CYP3A induction offset this inhibition. Alprazolam AUC and Cmax was reduced by 12% and 16%, respectively, in the presence of ritonavir (see WARNINGS).
The ability of alprazolam to induce or inhibit human hepatic enzyme systems has not been determined. However, this is not a property of benzodiazepines in general. Further, alprazolam did not affect the prothrombin or plasma warfarin levels in male volunteers administered sodium warfarin orally.
-
CLINICAL EFFICACY TRIALS
The efficacy of Alprazolam XR tablets in the treatment of panic disorder was established in two 6-week, placebo-controlled studies of Alprazolam XR in patients with panic disorder.
In two 6-week, flexible-dose, placebo-controlled studies in patients meeting DSM-III criteria for panic disorder, patients were treated with Alprazolam XR in a dose range of 1 to 10 mg/day, on a once-a-day basis. The effectiveness of Alprazolam XR was assessed on the basis of changes in various measures of panic attack frequency, on various measures of the Clinical Global Impression, and on the Overall Phobia Scale. In all, there were seven primary efficacy measures in these studies, and Alprazolam XR was superior to placebo on all seven outcomes in both studies. The mean dose of Alprazolam XR at the last treatment visit was 4.2 mg/day in the first study and 4.6 mg/day in the second.
In addition, there were two 8-week, fixed-dose, placebo-controlled studies of Alprazolam XR in patients with panic disorder, involving fixed Alprazolam XR doses of 4 and 6 mg/day, on a once-a-day basis, that did not show a benefit for either dose of Alprazolam XR.
The longer-term efficacy of Alprazolam XR in panic disorder has not been systematically evaluated.
Analyses of the relationship between treatment outcome and gender did not suggest any differential responsiveness on the basis of gender.
-
INDICATIONS AND USAGE
Alprazolam XR tablets are indicated for the treatment of panic disorder, with or without agoraphobia.
This claim is supported on the basis of two positive studies with Alprazolam XR conducted in patients whose diagnoses corresponded closely to the DSM-III-R/IV criteria for panic disorder (see CLINICAL EFFICACY TRIALS).
Panic disorder (DSM-IV) is characterized by recurrent unexpected panic attacks, ie, a discrete period of intense fear or discomfort in which four (or more) of the following symptoms develop abruptly and reach a peak within 10 minutes: (1) palpitations, pounding heart, or accelerated heart rate; (2) sweating; (3) trembling or shaking; (4) sensations of shortness of breath or smothering; (5) feeling of choking; (6) chest pain or discomfort; (7) nausea or abdominal distress; (8) feeling dizzy, unsteady, lightheaded, or faint; (9) derealization (feelings of unreality) or depersonalization (being detached from oneself); (10) fear of losing control; (11) fear of dying; (12) paresthesias (numbness or tingling sensations); (13) chills or hot flushes.
The longer-term efficacy of Alprazolam XR has not been systematically evaluated. Thus, the physician who elects to use this drug for periods longer than 8 weeks should periodically reassess the usefulness of the drug for the individual patient.
-
CONTRAINDICATIONS
Alprazolam XR tablets are contraindicated in patients with known sensitivity to this drug or other benzodiazepines.
Alprazolam XR is contraindicated with ketoconazole and itraconazole, since these medications significantly impair the oxidative metabolism mediated by cytochrome P450 3A (CYP3A) (see CLINICAL PHARMACOLOGY, WARNINGS and PRECAUTIONS–Drug Interactions).
-
WARNINGS
Risks from Concomitant Use with Opioids
Concomitant use of benzodiazepines, including Alprazolam XR, and opioids may result in profound sedation, respiratory depression, coma, and death. Because of these risks, reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate.
Observational studies have demonstrated that concomitant use of opioid analgesics and benzodiazepines increases the risk of drug-related mortality compared to use of opioids alone. If a decision is made to prescribe Alprazolam XR concomitantly with opioids, prescribe the lowest effective dosages and minimum durations of concomitant use, and follow patients closely for signs and symptoms of respiratory depression and sedation. In patients already receiving an opioid analgesic, prescribe a lower initial dose of Alprazolam XR than indicated in the absence of an opioid and titrate based on clinical response. If an opioid is initiated in a patient already taking Alprazolam XR, prescribe a lower initial dose of the opioid and titrate based upon clinical response.
Advise both patients and caregivers about the risks of respiratory depression and sedation when Alprazolam XR is used with opioids. Advise patients not to drive or operate heavy machinery until the effects of concomitant use with the opioid have been determined (see Drug Interactions).
Dependence and Withdrawal Reactions, Including Seizures
Certain adverse clinical events, some life-threatening, are a direct consequence of physical dependence to alprazolam. These include a spectrum of withdrawal symptoms; the most important is seizure (see DRUG ABUSE AND DEPENDENCE). Even after relatively short-term use at doses of ≤ 4 mg/day, there is some risk of dependence. Spontaneous reporting system data suggest that the risk of dependence and its severity appear to be greater in patients treated with doses greater than 4 mg/day and for long periods (more than 12 weeks). However, in a controlled postmarketing discontinuation study of panic disorder patients who received Alprazolam tablets, the duration of treatment (3 months compared to 6 months) had no effect on the ability of patients to taper to zero dose. In contrast, patients treated with doses of Alprazolam tablets greater than 4 mg/day had more difficulty tapering to zero dose than those treated with less than 4 mg/day.
Relapse or return of illness was defined as a return of symptoms characteristic of panic disorder (primarily panic attacks) to levels approximately equal to those seen at baseline before active treatment was initiated. Rebound refers to a return of symptoms of panic disorder to a level substantially greater in frequency, or more severe in intensity than seen at baseline. Withdrawal symptoms were identified as those which were generally not characteristic of panic disorder and which occurred for the first time more frequently during discontinuation than at baseline.
The rate of relapse, rebound, and withdrawal in patients with panic disorder who received Alprazolam XR tablets has not been systematically studied. Experience in randomized placebo-controlled discontinuation studies of patients with panic disorder who received Alprazolam tablets showed a high rate of rebound and withdrawal symptoms compared to placebo treated patients.
In a controlled clinical trial in which 63 patients were randomized to Alprazolam tablets and where withdrawal symptoms were specifically sought, the following were identified as symptoms of withdrawal: heightened sensory perception, impaired concentration, dysosmia, clouded sensorium, paresthesias, muscle cramps, muscle twitch, diarrhea, blurred vision, appetite decrease, and weight loss. Other symptoms, such as anxiety and insomnia, were frequently seen during discontinuation, but it could not be determined if they were due to return of illness, rebound, or withdrawal.
In two controlled trials of 6 to 8 weeks duration where the ability of patients to discontinue medication was measured, 71%–93% of patients treated with Alprazolam tablets tapered completely off therapy compared to 89%–96% of placebo treated patients. In a controlled postmarketing discontinuation study of panic disorder patients treated with Alprazolam tablets, the duration of treatment (3 months compared to 6 months) had no effect on the ability of patients to taper to zero dose.
Seizures were reported for three patients in panic disorder clinical trials with Alprazolam XR. In two cases, the patients had completed 6 weeks of treatment with Alprazolam XR6 mg/day before experiencing a single seizure. In one case, the patient abruptly discontinued Alprazolam XR, and in both cases, alcohol intake was implicated. The third case involved multiple seizures after the patient completed treatment with Alprazolam XR 4 mg/day and missed taking the medication on the first day of taper. All three patients recovered without sequelae.
Seizures have also been observed in association with dose reduction or discontinuation of Alprazolam tablets, the immediate release form of alprazolam. Seizures attributable to Alprazolam were seen after drug discontinuance or dose reduction in 8 of 1980 patients with panic disorder or in patients participating in clinical trials where doses of Alprazolam greater than 4 mg/day for over 3 months were permitted. Five of these cases clearly occurred during abrupt dose reduction, or discontinuation from daily doses of 2 to 10 mg. Three cases occurred in situations where there was not a clear relationship to abrupt dose reduction or discontinuation. In one instance, seizure occurred after discontinuation from a single dose of 1 mg after tapering at a rate of 1 mg every three days from 6 mg daily. In two other instances, the relationship to taper is indeterminate; in both of these cases the patients had been receiving doses of 3 mg daily prior to seizure. The duration of use in the above 8 cases ranged from 4 to 22 weeks. There have been occasional voluntary reports of patients developing seizures while apparently tapering gradually from Alprazolam. The risk of seizure seems to be greatest 24–72 hours after discontinuation (see DOSAGE AND ADMINISTRATION for recommended tapering and discontinuation schedule).
Status Epilepticus
The medical event voluntary reporting system shows that withdrawal seizures have been reported in association with the discontinuation of Alprazolam tablets. In most cases, only a single seizure was reported; however, multiple seizures and status epilepticus were reported as well.
Interdose Symptoms
Early morning anxiety and emergence of anxiety symptoms between doses of Alprazolam tablets have been reported in patients with panic disorder taking prescribed maintenance doses. These symptoms may reflect the development of tolerance or a time interval between doses which is longer than the duration of clinical action of the administered dose. In either case, it is presumed that the prescribed dose is not sufficient to maintain plasma levels above those needed to prevent relapse, rebound, or withdrawal symptoms over the entire course of the interdosing interval.
Risk of Dose Reduction
Withdrawal reactions may occur when dosage reduction occurs for any reason. This includes purposeful tapering, but also inadvertent reduction of dose (eg, the patient forgets, the patient is admitted to a hospital). Therefore, the dosage of Alprazolam XR should be reduced or discontinued gradually (see DOSAGE AND ADMINISTRATION).
CNS Depression and Impaired Performance
Because of its CNS depressant effects, patients receiving Alprazolam XR should be cautioned against engaging in hazardous occupations or activities requiring complete mental alertness such as operating machinery or driving a motor vehicle. For the same reason, patients should be cautioned about the simultaneous ingestion of alcohol and other CNS depressant drugs during treatment with Alprazolam XR.
Risk of Fetal Harm
Benzodiazepines can potentially cause fetal harm when administered to pregnant women. If alprazolam is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus. Because of experience with other members of the benzodiazepine class, alprazolam is assumed to be capable of causing an increased risk of congenital abnormalities when administered to a pregnant woman during the first trimester. Because use of these drugs is rarely a matter of urgency, their use during the first trimester should almost always be avoided. The possibility that a woman of childbearing potential may be pregnant at the time of institution of therapy should be considered. Patients should be advised that if they become pregnant during therapy or intend to become pregnant they should communicate with their physicians about the desirability of discontinuing the drug.
Alprazolam Interaction With Drugs That Inhibit Metabolism Via Cytochrome P450 3A
The initial step in alprazolam metabolism is hydroxylation catalyzed by cytochrome P450 3A (CYP3A). Drugs that inhibit this metabolic pathway may have a profound effect on the clearance of alprazolam. Consequently, alprazolam should be avoided in patients receiving very potent inhibitors of CYP3A. With drugs inhibiting CYP3A to a lesser but still significant degree, alprazolam should be used only with caution and consideration of appropriate dosage reduction. For some drugs, an interaction with alprazolam has been quantified with clinical data; for other drugs, interactions are predicted from in vitro data and/or experience with similar drugs in the same pharmacologic class.
The following are examples of drugs known to inhibit the metabolism of alprazolam and/or related benzodiazepines, presumably through inhibition of CYP3A.
Potent CYP3A Inhibitors
Azole antifungal agents
Ketoconazole and itraconazole are potent CYP3A inhibitors and have been shown in vivo to increase plasma alprazolam concentrations 3.98 fold and 2.70 fold, respectively. The coadministration of alprazolam with these agents is not recommended. Other azole-type antifungal agents should also be considered potent CYP3A inhibitors and the coadministration of alprazolam with them is not recommended (see CONTRAINDICATIONS).
Drugs demonstrated to be CYP3A inhibitors on the basis of clinical studies involving alprazolam (caution and consideration of appropriate alprazolam dose reduction are recommended during coadministration with the following drugs)
Fluvoxamine
Coadministration of fluvoxamine approximately doubled the maximum plasma concentration of alprazolam, decreased clearance by 49%, increased half-life by 71%, and decreased measured psychomotor performance.
Cimetidine
Coadministration of cimetidine increased the maximum plasma concentration of alprazolam by 86%, decreased clearance by 42%, and increased half-life by 16%.
HIV protease inhibitors
Interactions involving HIV protease inhibitors (eg, ritonavir) and alprazolam are complex and time dependent. Low doses of ritonavir resulted in a large impairment of alprazolam clearance, prolonged its elimination half-life and enhanced clinical effects. However, upon extended exposure to ritonavir, CYP3A induction offset this inhibition. This interaction will require a dose-adjustment or discontinuation of alprazolam.
Other Drugs Possibly Affecting Alprazolam Metabolism
Other drugs possibly affecting alprazolam metabolism by inhibition of CYP3A are discussed in the PRECAUTIONS section (see PRECAUTIONS–Drug Interactions).
-
PRECAUTIONS
General
Suicide
As with other psychotropic medications, the usual precautions with respect to administration of the drug and size of the prescription are indicated for severely depressed patients or those in whom there is reason to expect concealed suicidal ideation or plans. Panic disorder has been associated with primary and secondary major depressive disorders and increased reports of suicide among untreated patients.
Mania
Episodes of hypomania and mania have been reported in association with the use of Alprazolam tablets in patients with depression.
Uricosuric Effect
Alprazolam has a weak uricosuric effect. Although other medications with weak uricosuric effect have been reported to cause acute renal failure, there have been no reported instances of acute renal failure attributable to therapy with alprazolam.
Use in Patients with Concomitant Illness
It is recommended that the dosage be limited to the smallest effective dose to preclude the development of ataxia or oversedation which may be a particular problem in elderly or debilitated patients (see DOSAGE AND ADMINISTRATION). The usual precautions in treating patients with impaired renal, hepatic, or pulmonary function should be observed. There have been rare reports of death in patients with severe pulmonary disease shortly after the initiation of treatment with Alprazolam tablets. A decreased systemic alprazolam elimination rate (eg, increased plasma half-life) has been observed in both alcoholic liver disease patients and obese patients receiving Alprazolam tablets (see CLINICAL PHARMACOLOGY).
Information for Patients
To assure safe and effective use of Alprazolam XR, the physician should provide the patient with the following guidance.
- Advise both patients and caregivers about the risks of potentially fatal respiratory depression and sedation when Alprazolam XR is used with opioids and not to use such drugs concomitantly unless supervised by a health care provider.
- Advise patients not to drive or operate heavy machinery until the effects of concomitant use with the opioid have been determined (see Drug Interactions).
- Inform your physician about any alcohol consumption and medicine you are taking now, including medication you may buy without a prescription. Alcohol should generally not be used during treatment with benzodiazepines.
- Not recommended for use in pregnancy. Therefore, inform your physician if you are pregnant, if you are planning to have a child, or if you become pregnant while you are taking this medication.
- Inform your physician if you are nursing.
- Until you experience how this medication affects you, do not drive a car or operate potentially dangerous machinery, etc.
- Do not increase the dose even if you think the medication "does not work anymore" without consulting your physician. Benzodiazepines, even when used as recommended, may produce emotional and/or physical dependence.
- Do not stop taking this medication abruptly or decrease the dose without consulting your physician, since withdrawal symptoms can occur.
- Some patients may find it very difficult to discontinue treatment with Alprazolam XR due to severe emotional and physical dependence. Discontinuation symptoms, including possible seizures, may occur following discontinuation from any dose, but the risk may be increased with extended use at doses greater than 4 mg/day, especially if discontinuation is too abrupt. It is important that you seek advice from your physician to discontinue treatment in a careful and safe manner. Proper discontinuation will help to decrease the possibility of withdrawal reactions that can range from mild reactions to severe reactions such as seizure.
Laboratory Tests
Laboratory tests are not ordinarily required in otherwise healthy patients. However, when treatment is protracted, periodic blood counts, urinalysis, and blood chemistry analyses are advisable in keeping with good medical practice.
Drug Interactions
Use with Opioids
The concomitant use of benzodiazepines and opioids increases the risk of respiratory depression because of actions at different receptor sites in the CNS that control respiration. Benzodiazepines interact at GABAA sites and opioids interact primarily at mu receptors. When benzodiazepines and opioids are combined, the potential for benzodiazepines to significantly worsen opioid-related respiratory depression exists. Limit dosage and duration of concomitant use of benzodiazepines and opioids, and monitor patients closely for respiratory depression and sedation.
Use with Other CNS Depressants
If Alprazolam XR tablets are to be combined with other psychotropic agents or anticonvulsant drugs, careful consideration should be given to the pharmacology of the agents to be employed, particularly with compounds which might potentiate the action of benzodiazepines. The benzodiazepines, including alprazolam, produce additive CNS depressant effects when coadministered with other psychotropic medications, anticonvulsants, antihistaminics, ethanol and other drugs which themselves produce CNS depression.
Use with Digoxin
Increased digoxin concentrations have been reported when alprazolam was given, especially in elderly (>65 years of age). Patients who receive alprazolam and digoxin should therefore be monitored for signs and symptoms related to digoxin toxicity.
Use with Imipramine and Desipramine
The steady state plasma concentrations of imipramine and desipramine have been reported to be increased an average of 31% and 20%, respectively, by the concomitant administration of Alprazolam tablets in doses up to 4 mg/day. The clinical significance of these changes is unknown.
Drugs that inhibit alprazolam metabolism via cytochrome P450 3A
The initial step in alprazolam metabolism is hydroxylation catalyzed by cytochrome P450 3A (CYP3A). Drugs which inhibit this metabolic pathway may have a profound effect on the clearance of alprazolam (see CONTRAINDICATIONS and WARNINGS for additional drugs of this type).
Drugs demonstrated to be CYP3A inhibitors of possible clinical significance on the basis of clinical studies involving alprazolam (caution is recommended during coadministration with alprazolam)
Fluoxetine
Coadministration of fluoxetine with alprazolam increased the maximum plasma concentration of alprazolam by 46%, decreased clearance by 21%, increased half-life by 17%, and decreased measured psychomotor performance.
Drugs and other substances demonstrated to be CYP3A inhibitors on the basis of clinical studies involving benzodiazepines metabolized similarly to alprazolam or on the basis of in vitro studies with alprazolam or other benzodiazepines (caution is recommended during coadministration with alprazolam)
Available data from clinical studies of benzodiazepines other than alprazolam suggest a possible drug interaction with alprazolam for the following: diltiazem, isoniazid, macrolide antibiotics such as erythromycin and clarithromycin, and grapefruit juice. Data from in vitro studies of alprazolam suggest a possible drug interaction with alprazolam for the following: sertraline and paroxetine. However, data from an in vivo drug interaction study involving a single dose of alprazolam 1 mg and steady state doses of sertraline (50 to 150 mg/day) did not reveal any clinically significant changes in the pharmacokinetics of alprazolam. Data from in vitro studies of benzodiazepines other than alprazolam suggest a possible drug interaction for the following: ergotamine, cyclosporine, amiodarone, nicardipine, and nifedipine. Caution is recommended during the coadministration of any of these with alprazolam (see WARNINGS).
Drug/Laboratory Test Interactions
Although interactions between benzodiazepines and commonly employed clinical laboratory tests have occasionally been reported, there is no consistent pattern for a specific drug or specific test.
Carcinogenesis, Mutagenesis, Impairment of Fertility
No evidence of carcinogenic potential was observed during 2-year bioassay studies of alprazolam in rats at doses up to 30 mg/kg/day (150 times the maximum recommended daily human dose of 10 mg/day) and in mice at doses up to 10 mg/kg/day (50 times the maximum recommended daily human dose).
Alprazolam was not mutagenic in the rat micronucleus test at doses up to 100 mg/kg, which is 500 times the maximum recommended daily human dose of 10 mg/day. Alprazolam also was not mutagenic in vitro in the DNA Damage/Alkaline Elution Assay or the Ames Assay.
Alprazolam produced no impairment of fertility in rats at doses up to 5 mg/kg/day, which is 25 times the maximum recommended daily human dose of 10 mg/day.
Pregnancy
Nonteratogenic Effects
It should be considered that the child born of a mother who is receiving benzodiazepines may be at some risk for withdrawal symptoms from the drug during the postnatal period. Also, neonatal flaccidity and respiratory problems have been reported in children born of mothers who have been receiving benzodiazepines.
Nursing Mothers
Benzodiazepines are known to be excreted in human milk. It should be assumed that alprazolam is as well. Chronic administration of diazepam to nursing mothers has been reported to cause their infants to become lethargic and to lose weight. As a general rule, nursing should not be undertaken by mothers who must use alprazolam.
Pediatric Use
Safety and effectiveness of alprazolam in individuals below 18 years of age have not been established.
Geriatric Use
The elderly may be more sensitive to the effects of benzodiazepines. They exhibit higher plasma alprazolam concentrations due to reduced clearance of the drug as compared with a younger population receiving the same doses. The smallest effective dose of alprazolam should be used in the elderly to preclude the development of ataxia and oversedation (see CLINICAL PHARMACOLOGY and DOSAGE AND ADMINISTRATION).
-
ADVERSE REACTIONS
The information included in the subsection on Adverse Events Observed in Short-Term, Placebo-Controlled Trials with Alprazolam XR tablets is based on pooled data of five 6- and 8-week placebo-controlled clinical studies in panic disorder.
Adverse event reports were elicited either by general inquiry or by checklist, and were recorded by clinical investigators using terminology of their own choosing. The stated frequencies of adverse events represent the proportion of individuals who experienced, at least once, a treatment-emergent adverse event of the type listed. An event was considered treatment emergent if it occurred for the first time or worsened during therapy following baseline evaluation. In the tables and tabulations that follow, standard MedDRA terminology (version 4.0) was used to classify reported adverse events.
Adverse Events Observed in Short-Term, Placebo-Controlled Trials of Alprazolam XR
Adverse Events Reported as Reasons for Discontinuation of Treatment in Placebo-Controlled Trials
Approximately 17% of the 531 patients who received Alprazolam XR in placebo-controlled clinical trials for panic disorder had at least one adverse event that led to discontinuation compared to 8% of 349 placebo-treated patients. The most common events leading to discontinuation and considered to be drug-related (ie, leading to discontinuation in at least 1% of the patients treated with Alprazolam XR at a rate at least twice that of placebo) are shown in the following table.
Common Adverse Events Leading to Discontinuation of Treatment in Placebo-Controlled Trials System Organ Class/Adverse Event Percentage of Patients Discontinuing Due to Adverse Events Alprazolam XR
(n=531)Placebo
(n=349)Nervous system disorders Sedation 7.5 0.6 Somnolence 3.2 0.3 Dysarthria 2.1 0 Coordination abnormal 1.9 0.3 Memory impairment 1.5 0.3 General disorders/administration site conditions Fatigue 1.7 0.6 Psychiatric disorders Depression 2.5 1.2 Adverse Events Occurring at an Incidence of 1% or More Among Patients Treated with Alprazolam XR
The prescriber should be aware that adverse event incidence cannot be used to predict the incidence of adverse events in the course of usual medical practice where patient characteristics and other factors differ from those which prevailed in the clinical trials. Similarly, the cited frequencies cannot be compared with event incidence obtained from other clinical investigations involving different treatments, uses, and investigators. The cited values, however, do provide the prescribing physician with some basis for estimating the relative contribution of drug and non-drug factors to the adverse event incidence rate in the population studied.
The following table shows the incidence of treatment-emergent adverse events that occurred during 6- to 8-week placebo-controlled trials in 1% or more of patients treated with Alprazolam XR where the incidence in patients treated with Alprazolam XR was greater than the incidence in placebo-treated patients. The most commonly observed adverse events in panic disorder patients treated with Alprazolam XR (incidence of 5% or greater and at least twice the incidence in placebo patients) were: sedation, somnolence, memory impairment, dysarthria, coordination abnormal, ataxia, libido decreased (see table).
Treatment-Emergent Adverse Events: Incidence in Short-Term, Placebo-Controlled Clinical Trials with Alprazolam XR System Organ Class/Adverse Event Percentage of Patients Reporting Adverse Event Alprazolam XR
(n=531)Placebo
(n=349)Nervous system disorders Sedation 45.2 22.6 Somnolence 23.0 6.0 Memory impairment 15.4 6.9 Dysarthria 10.9 2.6 Coordination abnormal 9.4 0.9 Mental impairment 7.2 5.7 Ataxia 7.2 3.2 Disturbance in attention 3.2 0.6 Balance impaired 3.2 0.6 Paresthesia 2.4 1.7 Dyskinesia 1.7 1.4 Hypoesthesia 1.3 0.3 Hypersomnia 1.3 0 General disorders/administration site conditions Fatigue 13.9 9.2 Lethargy 1.7 0.6 Infections and infestations Influenza 2.4 2.3 Upper respiratory tract infections 1.9 1.7 Psychiatric disorders Depression 12.1 9.2 Libido decreased 6.0 2.3 Disorientation 1.5 0 Confusion 1.5 0.9 Depressed mood 1.3 0.3 Anxiety 1.1 0.6 Metabolism and nutrition disorders Appetite decreased 7.3 7.2 Appetite increased 7.0 6.0 Anorexia 1.5 0 Gastrointestinal disorders Dry mouth 10.2 9.7 Constipation 8.1 4.3 Nausea 6.0 3.2 Pharyngolaryngeal pain 3.2 2.6 Investigations Weight increased 5.1 4.3 Weight decreased 4.3 3.7 Injury, poisoning, and procedural complications Road traffic accident 1.5 0 Reproductive system and breast disorders Dysmenorrhea 3.6 2.9 Sexual dysfunction 2.4 1.1 Premenstrual syndrome 1.7 0.6 Musculoskeletal and connective tissue disorders Arthralgia 2.4 0.6 Myalgia 1.5 1.1 Pain in limb 1.1 0.3 Vascular disorders Hot flushes 1.5 1.4 Respiratory, thoracic, and mediastinal disorders Dyspnea 1.5 0.3 Rhinitis allergic 1.1 0.6 Skin and subcutaneous tissue disorders Pruritis 1.1 0.9 Other Adverse Events Observed During the Premarketing Evaluation of Alprazolam XR tablets
Following is a list of MedDRA terms that reflect treatment-emergent adverse events reported by 531 patients with panic disorder treated with Alprazolam XR. All potentially important reported events are included except those already listed in the above table or elsewhere in labeling, those events for which a drug cause was remote, those event terms that were so general as to be uninformative, and those events that occurred at rates similar to background rates in the general population. It is important to emphasize that, although the events reported occurred during treatment with Alprazolam XR, they were not necessarily caused by the drug. Events are further categorized by body system and listed in order of decreasing frequency according to the following definitions: frequent adverse events are those occurring on 1 or more occasions in at least l/l00 patients; infrequent adverse events are those occurring in less than l/100 patients but at least l/1000 patients; rare events are those occurring in fewer than l/1000 patients.
Cardiac disorders: Frequent: palpitation; Infrequent: sinus tachycardia
Ear and Labyrinth disorders: Frequent: Vertigo; Infrequent: tinnitus, ear pain
Eye disorders: Frequent: blurred vision; Infrequent: mydriasis, photophobia
Gastrointestinal disorders: Frequent: diarrhea, vomiting, dyspepsia, abdominal pain; Infrequent: dysphagia, salivary hypersecretion
General disorders and administration site conditions: Frequent: malaise, weakness, chest pains; Infrequent: fall, pyrexia, thirst, feeling hot and cold, edema, feeling jittery, sluggishness, asthenia, feeling drunk, chest tightness, increased energy, feeling of relaxation, hangover, loss of control of legs, rigors
Musculoskeletal and connective tissue disorders: Frequent: back pain, muscle cramps, muscle twitching
Nervous system disorders: Frequent: headache, dizziness, tremor; Infrequent: amnesia, clumsiness, syncope, hypotonia, seizures, depressed level of consciousness, sleep apnea syndrome, sleep talking, stupor
Psychiatric system disorders: Frequent: irritability, insomnia, nervousness, derealization, libido increased, restlessness, agitation, depersonalization, nightmare; Infrequent: abnormal dreams, apathy, aggression, anger, bradyphrenia, euphoric mood, logorrhea, mood swings, dysphonia, hallucination, homicidal ideation, mania, hypomania, impulse control, psychomotor retardation, suicidal ideation
Renal and urinary disorders: Frequent: difficulty in micturition; Infrequent: urinary frequency, urinary incontinence
Respiratory, thoracic, and mediastinal disorders: Frequent: nasal congestion, hyperventilation; Infrequent: choking sensation, epistaxis, rhinorrhea
Skin and subcutaneous tissue disorders: Frequent: sweating increased; Infrequent: clamminess, rash, urticaria
Vascular disorders: Infrequent: hypotension
The categories of adverse events reported in the clinical development program for Alprazolam tablets in the treatment of panic disorder differ somewhat from those reported for Alprazolam XR tablets because the clinical trials with Alprazolam tablets and Alprazolam XR tablets used different standard medical nomenclature for reporting the adverse events. Nevertheless, the types of adverse events reported in the clinical trials with Alprazolam tablets were generally the same as those reported in the clinical trials with Alprazolam XR tablets.
Discontinuation-Emergent Adverse Events Occurring at an Incidence of 5% or More Among Patients Treated with Alprazolam XR
The following table shows the incidence of discontinuation-emergent adverse events that occurred during short-term, placebo-controlled trials in 5% or more of patients treated with Alprazolam XR where the incidence in patients treated with Alprazolam XR was two times greater than the incidence in placebo-treated patients.
Discontinuation-Emergent Symptoms: Incidence in Short-Term, Placebo-Controlled Trials with Alprazolam XR System Organ Class/AdverseEvent Percentage of Patients Reporting Adverse Event Alprazolam XR
(n=422)Placebo
(n=261)Nervous system disorders Tremor 28.2 10.7 Headache 26.5 12.6 Hypoesthesia 7.8 2.3 Paraesthesia 7.1 2.7 Psychiatric disorders Insomnia 24.2 9.6 Nervousness 21.8 8.8 Depression 10.9 5.0 Derealization 8.0 3.8 Anxiety 7.8 2.7 Depersonalization 5.7 1.9 Gastrointestinal disorders Diarrhea 12.1 3.1 Respiratory, thoracic and mediastinal disorders Hyperventilation 8.5 2.7 Metabolism and nutrition disorders Appetite decreased 9.5 3.8 Musculosketal and connective tissue disorders Muscle twitching 7.4 2.7 Vascular disorders Hot flushes 5.9 2.7 There have also been reports of withdrawal seizures upon rapid decrease or abrupt discontinuation of alprazolam (see WARNINGS).
To discontinue treatment in patients taking Alprazolam XR tablets, the dosage should be reduced slowly in keeping with good medical practice. It is suggested that the daily dosage of Alprazolam XR tablets be decreased by no more than 0.5 mg every three days (see DOSAGE AND ADMINISTRATION). Some patients may benefit from an even slower dosage reduction. In a controlled postmarketing discontinuation study of panic disorder patients which compared this recommended taper schedule with a slower taper schedule, no difference was observed between the groups in the proportion of patients who tapered to zero dose; however, the slower schedule was associated with a reduction in symptoms associated with a withdrawal syndrome.
As with all benzodiazepines, paradoxical reactions such as stimulation, increased muscle spasticity, sleep disturbances, hallucinations, and other adverse behavioral effects such as agitation, rage, irritability, and aggressive or hostile behavior have been reported rarely. In many of the spontaneous case reports of adverse behavioral effects, patients were receiving other CNS drugs concomitantly and/or were described as having underlying psychiatric conditions. Should any of the above events occur, alprazolam should be discontinued. Isolated published reports involving small numbers of patients have suggested that patients who have borderline personality disorder, a prior history of violent or aggressive behavior, or alcohol or substance abuse may be at risk for such events. Instances of irritability, hostility, and intrusive thoughts have been reported during discontinuation of alprazolam in patients with posttraumatic stress disorder.
Post Introduction Reports
Various adverse drug reactions have been reported in association with the use of Alprazolam tablets since market introduction. The majority of these reactions were reported through the medical event voluntary reporting system. Because of the spontaneous nature of the reporting of medical events and the lack of controls, a causal relationship to the use of Alprazolam tablets cannot be readily determined. Reported events include: gastrointestinal disorder, hypomania, mania, liver enzyme elevations, hepatitis, jaundice, hepatic failure, Stevens-Johnson syndrome, photosensitivity reaction, angioedema, peripheral edema, menstruation irregular, hyperprolactinemia, gynecomastia, and galactorrhea (see PRECAUTIONS).
-
DRUG ABUSE AND DEPENDENCE
Physical and Psychological Dependence
Withdrawal symptoms similar in character to those noted with sedative/hypnotics and alcohol have occurred following discontinuance of benzodiazepines, including alprazolam. The symptoms can range from mild dysphoria and insomnia to a major syndrome that may include abdominal and muscle cramps, vomiting, sweating, tremors, and convulsions. Distinguishing between withdrawal emergent signs and symptoms and the recurrence of illness is often difficult in patients undergoing dose reduction. The long-term strategy for treatment of these phenomena will vary with their cause and the therapeutic goal. When necessary, immediate management of withdrawal symptoms requires re-institution of treatment at doses of alprazolam sufficient to suppress symptoms. There have been reports of failure of other benzodiazepines to fully suppress these withdrawal symptoms. These failures have been attributed to incomplete cross-tolerance but may also reflect the use of an inadequate dosing regimen of the substituted benzodiazepine or the effects of concomitant medications.
While it is difficult to distinguish withdrawal and recurrence for certain patients, the time course and the nature of the symptoms may be helpful. A withdrawal syndrome typically includes the occurrence of new symptoms, tends to appear toward the end of taper or shortly after discontinuation, and will decrease with time. In recurring panic disorder, symptoms similar to those observed before treatment may recur either early or late, and they will persist.
While the severity and incidence of withdrawal phenomena appear to be related to dose and duration of treatment, withdrawal symptoms, including seizures, have been reported after only brief therapy with alprazolam at doses within the recommended range for the treatment of anxiety (eg, 0.75 to 4 mg/day). Signs and symptoms of withdrawal are often more prominent after rapid decrease of dosage or abrupt discontinuance. The risk of withdrawal seizures may be increased at doses above 4 mg/day (see WARNINGS).
Patients, especially individuals with a history of seizures or epilepsy, should not be abruptly discontinued from any CNS depressant agent, including alprazolam. It is recommended that all patients on alprazolam who require a dosage reduction be gradually tapered under close supervision (see WARNINGS and DOSAGE AND ADMINISTRATION).
Psychological dependence is a risk with all benzodiazepines, including alprazolam. The risk of psychological dependence may also be increased at doses greater than 4 mg/day and with longer term use, and this risk is further increased in patients with a history of alcohol or drug abuse. Some patients have experienced considerable difficulty in tapering and discontinuing from alprazolam, especially those receiving higher doses for extended periods. Addiction-prone individuals should be under careful surveillance when receiving alprazolam. As with all anxiolytics, repeat prescriptions should be limited to those who are under medical supervision.
-
OVERDOSAGE
Clinical Experience
Overdosage reports with Alprazolam tablets are limited. Manifestations of alprazolam overdosage include somnolence, confusion, impaired coordination, diminished reflexes, and coma. Death has been reported in association with overdoses of alprazolam by itself, as it has with other benzodiazepines. In addition, fatalities have been reported in patients who have overdosed with a combination of a single benzodiazepine, including alprazolam, and alcohol; alcohol levels seen in some of these patients have been lower than those usually associated with alcohol-induced fatality.
Animal experiments have suggested that forced diuresis or hemodialysis are probably of little value in treating overdosage.
General Treatment of Overdose
As in all cases of drug overdosage, respiration, pulse rate, and blood pressure should be monitored. General supportive measures should be employed, along with immediate gastric lavage. Intravenous fluids should be administered and an adequate airway maintained. If hypotension occurs, it may be combated by the use of vasopressors. Dialysis is of limited value. As with the management of intentional overdosing with any drug, it should be borne in mind that multiple agents may have been ingested.
Flumazenil, a specific benzodiazepine receptor antagonist, is indicated for the complete or partial reversal of the sedative effects of benzodiazepines and may be used in situations when an overdose with a benzodiazepine is known or suspected. Prior to the administration of flumazenil, necessary measures should be instituted to secure airway, ventilation, and intravenous access. Flumazenil is intended as an adjunct to, not as a substitute for, proper management of benzodiazepine overdose. Patients treated with flumazenil should be monitored for re-sedation, respiratory depression, and other residual benzodiazepine effects for an appropriate period after treatment. The prescriber should be aware of a risk of seizure in association with flumazenil treatment, particularly in long-term benzodiazepine users and in cyclic antidepressant overdose. The complete flumazenil package insert including CONTRAINDICATIONS, WARNINGS, and PRECAUTIONS should be consulted prior to use.
-
DOSAGE AND ADMINISTRATION
Alprazolam XR tablets may be administered once daily, preferably in the morning. The tablets should be taken intact; they should not be chewed, crushed, or broken.
The suggested total daily dose ranges between 3 to 6 mg/day. Dosage should be individualized for maximum beneficial effect. While the suggested total daily dosages given will meet the needs of most patients, there will be some patients who require doses greater than 6 mg/day. In such cases, dosage should be increased cautiously to avoid adverse effects.
Dosing in Special Populations
In elderly patients, in patients with advanced liver disease, or in patients with debilitating disease, the usual starting dose of Alprazolam XR is 0.5 mg once daily. This may be gradually increased if needed and tolerated (see Dose Titration). The elderly may be especially sensitive to the effects of benzodiazepines.
Dose Titration
Treatment with Alprazolam XR may be initiated with a dose of 0.5 mg to 1 mg once daily. Depending on the response, the dose may be increased at intervals of 3 to 4 days in increments of no more than 1 mg/day. Slower titration to the dose levels may be advisable to allow full expression of the pharmacodynamic effect of Alprazolam XR.
Generally, therapy should be initiated at a low dose to minimize the risk of adverse responses in patients especially sensitive to the drug. Dose should be advanced until an acceptable therapeutic response (ie, a substantial reduction in or total elimination of panic attacks) is achieved, intolerance occurs, or the maximum recommended dose is attained.
Dose Maintenance
In controlled trials conducted to establish the efficacy of Alprazolam XR tablets in panic disorder, doses in the range of 1 to 10 mg/day were used. Most patients showed efficacy in the dose range of 3 to 6 mg/day. Occasional patients required as much as 10 mg/day to achieve a successful response.
The necessary duration of treatment for panic disorder patients responding to Alprazolam XR is unknown. However, periodic reassessment is advised. After a period of extended freedom from attacks, a carefully supervised tapered discontinuation may be attempted, but there is evidence that this may often be difficult to accomplish without recurrence of symptoms and/or the manifestation of withdrawal phenomena.
Dose Reduction
Because of the danger of withdrawal, abrupt discontinuation of treatment should be avoided (see WARNINGS, PRECAUTIONS, DRUG ABUSE AND DEPENDENCE).
In all patients, dosage should be reduced gradually when discontinuing therapy or when decreasing the daily dosage. Although there are no systematically collected data to support a specific discontinuation schedule, it is suggested that the daily dosage be decreased by no more than 0.5 mg every three days. Some patients may require an even slower dosage reduction.
In any case, reduction of dose must be undertaken under close supervision and must be gradual. If significant withdrawal symptoms develop, the previous dosing schedule should be reinstituted and, only after stabilization, should a less rapid schedule of discontinuation be attempted. In a controlled postmarketing discontinuation study of panic disorder patients which compared this recommended taper schedule with a slower taper schedule, no difference was observed between the groups in the proportion of patients who tapered to zero dose; however, the slower schedule was associated with a reduction in symptoms associated with a withdrawal syndrome. It is suggested that the dose be reduced by no more than 0.5 mg every three days, with the understanding that some patients may benefit from an even more gradual discontinuation. Some patients may prove resistant to all discontinuation regimens.
Switch from alprazolam (immediate-release) tablets to Alprazolam XR (extended-release) tablets
Patients who are currently being treated with divided doses of alprazolam (immediate-release) tablets, for example 3 to 4 times a day, may be switched to Alprazolam XR tablets at the same total daily dose taken once daily. If the therapeutic response after switching is inadequate, the dosage may be titrated as outlined above.
-
HOW SUPPLIED
Alprazolam XR (extended-release) tablets are available as follows:
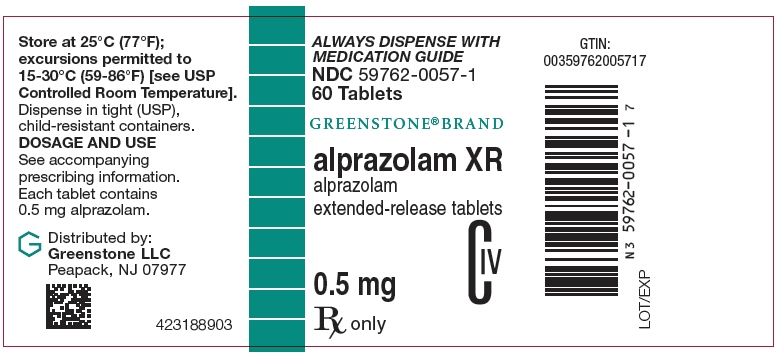
0.5 mg (white, pentagonal-shaped tablets debossed with an "G" on one side and "0.5" on the other side)
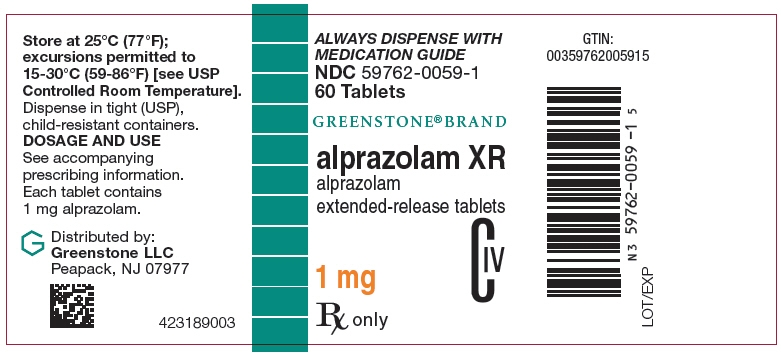
Bottles of 60 NDC: 59762-0057-1 1 mg (yellow, square-shaped tablets debossed with an "G" on one side and "1" on the other side)
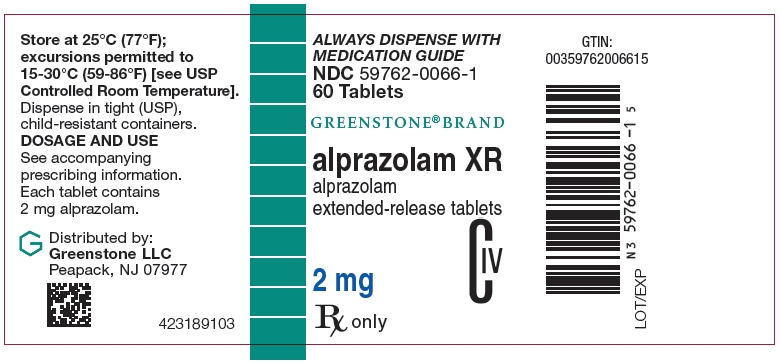
Bottles of 60 NDC: 59762-0059-1 2 mg (blue, round-shaped tablets debossed with an "G" on one side and "2" on the other side)
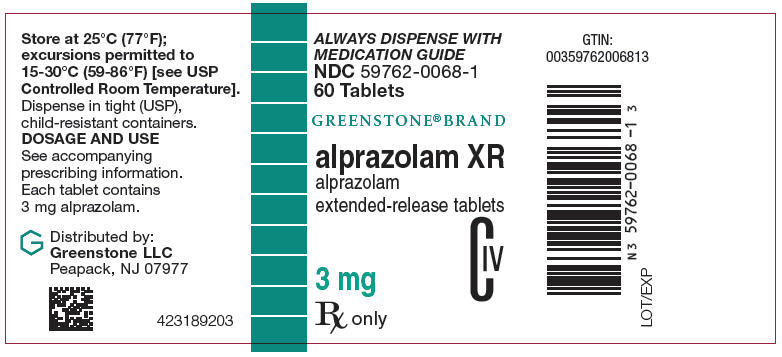
Bottles of 60 NDC: 59762-0066-1 3 mg (green, triangular-shaped tablets debossed with an "G" on one side and "3" on the other side)
Bottles of 60 NDC: 59762-0068-1 -
ANIMAL STUDIES
When rats were treated with alprazolam at 3, 10, and 30 mg/kg/day (15 to 150 times the maximum recommended human dose) orally for 2 years, a tendency for a dose related increase in the number of cataracts was observed in females and a tendency for a dose related increase in corneal vascularization was observed in males. These lesions did not appear until after 11 months of treatment.
This product's label may have been updated. For current full prescribing information, please visit www.greenstonellc.com.
- SPL UNCLASSIFIED SECTION
-
MEDICATION GUIDE
MEDICATION GUIDE
ALPRAZOLAM XR Tablets, C-IVWhat is the most important information I should know about Alprazolam XR? - Alprazolam XR is a benzodiazepine medicine. Taking benzodiazepines with opioid medicines, alcohol, or other central nervous system depressants (including street drugs) can cause severe drowsiness, breathing problems (respiratory depression), coma and death.
-
Alprazolam XR can make you sleepy or dizzy, and can slow your thinking and motor skills.
- Do not drive, operate heavy machinery, or do other dangerous activities until you know how Alprazolam XR affects you.
- Do not drink alcohol or take other drugs that may make you sleepy or dizzy while taking Alprazolam XR without first talking to your healthcare provider. When taken with alcohol or drugs that cause sleepiness or dizziness, Alprazolam XR may make your sleepiness or dizziness much worse.
- Do not take more Alprazolam XR than prescribed.
What is Alprazolam XR? - Alprazolam XR is a prescription medicine used to treat panic disorder, with or without a fear of places and situations that might cause panic, helplessness, or embarrassment (agoraphobia)
- Alprazolam XR is a federal controlled substance (C-IV) because it can be abused or lead to dependence. Keep Alprazolam XR in a safe place to prevent misuse and abuse. Selling or giving away Alprazolam XR may harm others, and is against the law. Tell your healthcare provider if you have abused or been dependent on alcohol, prescription medicines or street drugs.
- It is not known if Alprazolam XR is safe and effective in children.
- Elderly patients are especially susceptible to dose related adverse effects when taking Alprazolam XR.
- It is not known if Alprazolam XR is safe and effective in the treatment of panic disorder for use longer than 8 weeks.
Do not take Alprazolam XR if: - you are allergic to alprazolam, other benzodiazepines, or any of the ingredients in Alprazolam XR. See the end of this Medication Guide for a complete list of ingredients in Alprazolam XR.
- you are taking antifungal medicines including ketoconazole and itraconazole
Before you take Alprazolam XR, tell your healthcare provider about all of your medical conditions, including if you: - have or have had depression, mood problems, or suicidal thoughts or behavior
- have liver or kidney problems
- have lung disease or breathing problems
- are pregnant or plan to become pregnant. Alprazolam XR may harm your unborn baby. You and your healthcare provider should decide if you should take Alprazolam XR while you are pregnant.
- are breastfeeding or plan to breastfeed. Alprazolam XR passes into your breast milk and may harm your baby. Talk to your healthcare provider about the best way to feed your baby if you take Alprazolam XR. You should not breastfeed while taking Alprazolam XR.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Taking Alprazolam XR with certain other medicines can cause side effects or affect how well Alprazolam XR or the other medicines work. Do not start or stop other medicines without talking to your healthcare provider.
How should I take Alprazolam XR? - See "What is the most important information I should know about Alprazolam XR?"
- Take Alprazolam XR exactly as your healthcare provider tells you to take it. Your healthcare provider will tell you how much Alprazolam XR to take and when to take it.
- If you take too much Alprazolam XR, call your healthcare provider or go to the nearest hospital emergency room right away.
- Swallow Alprazolam XR tablets whole. Do not crush, chew or break Alprazolam XR
What should I avoid while taking Alprazolam XR? - Alprazolam XR can cause you to be drowsy. Do not drive a car or operate heavy machinery until you know how Alprazolam XR affects you.
- You should not drink alcohol while taking Alprazolam XR. Drinking alcohol can increase your chances of having serious side effects.
What are the possible side effects of Alprazolam XR?
Alprazolam XR may cause serious side effects, including:
- See "What is the most important information I should know about Alprazolam XR?"
- Abuse and dependence. Taking Alprazolam XR can cause physical and psychological dependence. Physical and psychological dependence is not the same as drug addiction. Your healthcare provider can tell you more about the differences between physical and psychological dependence and drug addiction.
- Withdrawal symptoms. You may have withdrawal symptoms if you stop taking Alprazolam XR suddenly. Withdrawal symptoms can be serious and include seizures. Mild withdrawal symptoms include a depressed mood and trouble sleeping. Talk to your healthcare provider about slowly stopping Alprazolam XR to avoid withdrawal symptoms.
- Seizures. Stopping Alprazolam XR can cause seizures and seizures that will not stop (status epilepticus).
- Mania. Alprazolam XR may cause an increase in activity and talking (hypomania and mania) in people who have depression.
- sedation
- difficult or unclear ability to talk
- problems with coordination
- tiredness
- drowsiness
- depression
- memory problems
These are not all the possible side effects of Alprazolam XR. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. How should I store Alprazolam XR? - Store Alprazolam XR between 59°F to 86°F (15°C to 30°C)
- Keep Alprazolam XR and all medicines out of the reach of children.
- General information about the safe and effective use of Alprazolam XR.
- Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide.
- Do not use Alprazolam XR for a condition for which it was not prescribed.
- Do not give Alprazolam XR to other people, even if they have the same symptoms that you have. It may harm them.
- You can ask your pharmacist or healthcare provider for information about Alprazolam XR that is written for health professionals.
What are the ingredients in Alprazolam XR?
Active ingredient: alprazolam
Inactive ingredients: lactose, magnesium stearate, colloidal silicon dioxide, and hypromellose. In addition, the 1 mg and 3 mg tablets contain D & C yellow No. 10 and the 2 mg and 3 mg tablets contain FD&C blue No. 2.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
This product's label may have been updated. For current full prescribing information, please visit www.greenstonellc.com.
LAB-0823-1.0
January 2017 - PRINCIPAL DISPLAY PANEL - 0.5 mg Tablet Bottle Label
- PRINCIPAL DISPLAY PANEL - 1 mg Tablet Bottle Label
- PRINCIPAL DISPLAY PANEL - 2 mg Tablet Bottle Label
- PRINCIPAL DISPLAY PANEL - 3 mg Tablet Bottle Label
-
INGREDIENTS AND APPEARANCE
ALPRAZOLAM XR
alprazolam tablet, extended releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 59762-0057 Route of Administration ORAL DEA Schedule CIV Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ALPRAZOLAM (UNII: YU55MQ3IZY) (ALPRAZOLAM - UNII:YU55MQ3IZY) ALPRAZOLAM 0.5 mg Inactive Ingredients Ingredient Name Strength LACTOSE, UNSPECIFIED FORM (UNII: J2B2A4N98G) MAGNESIUM STEARATE (UNII: 70097M6I30) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) Product Characteristics Color WHITE Score no score Shape PENTAGON (5 SIDED) (pentagon) Size 9mm Flavor Imprint Code G;0;5 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 59762-0057-1 60 in 1 BOTTLE; Type 0: Not a Combination Product 01/17/2003 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA AUTHORIZED GENERIC NDA021434 01/17/2003 ALPRAZOLAM XR
alprazolam tablet, extended releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 59762-0059 Route of Administration ORAL DEA Schedule CIV Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ALPRAZOLAM (UNII: YU55MQ3IZY) (ALPRAZOLAM - UNII:YU55MQ3IZY) ALPRAZOLAM 1 mg Inactive Ingredients Ingredient Name Strength LACTOSE, UNSPECIFIED FORM (UNII: J2B2A4N98G) MAGNESIUM STEARATE (UNII: 70097M6I30) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) D&C YELLOW NO. 10 (UNII: 35SW5USQ3G) Product Characteristics Color YELLOW Score no score Shape SQUARE Size 8mm Flavor Imprint Code G;1 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 59762-0059-1 60 in 1 BOTTLE; Type 0: Not a Combination Product 01/17/2003 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA AUTHORIZED GENERIC NDA021434 01/17/2003 ALPRAZOLAM XR
alprazolam tablet, extended releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 59762-0066 Route of Administration ORAL DEA Schedule CIV Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ALPRAZOLAM (UNII: YU55MQ3IZY) (ALPRAZOLAM - UNII:YU55MQ3IZY) ALPRAZOLAM 2 mg Inactive Ingredients Ingredient Name Strength LACTOSE, UNSPECIFIED FORM (UNII: J2B2A4N98G) MAGNESIUM STEARATE (UNII: 70097M6I30) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) FD&C BLUE NO. 2 (UNII: L06K8R7DQK) Product Characteristics Color BLUE Score no score Shape ROUND Size 10mm Flavor Imprint Code G;2 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 59762-0066-1 60 in 1 BOTTLE; Type 0: Not a Combination Product 01/17/2003 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA AUTHORIZED GENERIC NDA021434 01/17/2003 ALPRAZOLAM XR
alprazolam tablet, extended releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 59762-0068 Route of Administration ORAL DEA Schedule CIV Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ALPRAZOLAM (UNII: YU55MQ3IZY) (ALPRAZOLAM - UNII:YU55MQ3IZY) ALPRAZOLAM 3 mg Inactive Ingredients Ingredient Name Strength LACTOSE, UNSPECIFIED FORM (UNII: J2B2A4N98G) MAGNESIUM STEARATE (UNII: 70097M6I30) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) D&C YELLOW NO. 10 (UNII: 35SW5USQ3G) FD&C BLUE NO. 2 (UNII: L06K8R7DQK) Product Characteristics Color GREEN Score no score Shape TRIANGLE Size 10mm Flavor Imprint Code G;3 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 59762-0068-1 60 in 1 BOTTLE; Type 0: Not a Combination Product 01/17/2003 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA AUTHORIZED GENERIC NDA021434 01/17/2003 Labeler - Greenstone LLC (825560733) Establishment Name Address ID/FEI Business Operations Pfizer Pharmaceuticals LLC 829084545 ANALYSIS(59762-0057, 59762-0059, 59762-0066, 59762-0068) , MANUFACTURE(59762-0057, 59762-0059, 59762-0066, 59762-0068) Establishment Name Address ID/FEI Business Operations Pharmacia and Upjohn Company LLC 618054084 API MANUFACTURE(59762-0057, 59762-0059, 59762-0066, 59762-0068) Establishment Name Address ID/FEI Business Operations Pfizer Pharmaceuticals LLC 829084552 PACK(59762-0057, 59762-0059, 59762-0066, 59762-0068) Establishment Name Address ID/FEI Business Operations Pfizer Italia S.r.l. 458521908 ANALYSIS(59762-0057, 59762-0059, 59762-0066, 59762-0068) , MANUFACTURE(59762-0057, 59762-0059, 59762-0066, 59762-0068) , PACK(59762-0057, 59762-0059, 59762-0066, 59762-0068) Establishment Name Address ID/FEI Business Operations Pfizer Ireland Pharmaceuticals 986019327 ANALYSIS(59762-0057, 59762-0059, 59762-0066, 59762-0068) , MANUFACTURE(59762-0057, 59762-0059, 59762-0066, 59762-0068)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.