GAMMAGARD LIQUID ERC (immune globulin infusion- human injection, solution
GAMMAGARD Liquid ERC by
Drug Labeling and Warnings
GAMMAGARD Liquid ERC by is a Other medication manufactured, distributed, or labeled by Takeda Pharmaceuticals America, Inc., Baxalta Belgium Manufacturing SA. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use GAMMAGARD LIQUID® ERC safely and effectively. See full prescribing information for GAMMAGARD LIQUID ERC.
GAMMAGARD LIQUID ERC [immune globulin infusion (human)]
10% solution for intravenous, or subcutaneous use
Initial U.S. Approval: 2025WARNING: THROMBOSIS, RENAL DYSFUNCTION and ACUTE RENAL FAILURE
See full prescribing information for complete boxed warning.
- Thrombosis may occur with immune globulin products, including GAMMAGARD LIQUID ERC. Risk factors include advanced age, prolonged immobilization, hypercoagulable conditions, history of venous or arterial thrombosis, use of estrogens, indwelling vascular catheters, hyperviscosity and cardiovascular risk factors. (5.4)
- Renal dysfunction, acute renal failure, osmotic nephrosis, and death may occur in predisposed patients with immune globulin intravenous (IGIV) products including GAMMAGARD LIQUID ERC. Renal dysfunction and acute failure occur more commonly with IGIV products containing sucrose. GAMMAGARD LIQUID ERC does not contain sucrose. (5.2)
- For patients at risk of thrombosis, administer GAMMAGARD LIQUID ERC at the minimum dose and infusion rate practicable. Ensure adequate hydration in patients before administration. Monitor for signs and symptoms of thrombosis and assess blood viscosity in patients at risk of hyperviscosity. (5.4)
INDICATIONS AND USAGE
GAMMAGARD LIQUID ERC is a replacement therapy for primary humoral immunodeficiency (PI) in adult and pediatric patients two years of age and older. (1)
DOSAGE AND ADMINISTRATION
Intravenous (IV) Administration: (2.1)
Dose Initial Infusion Rate Maintenance Infusion Rate 300 to 600 milligrams (mg)/kilograms (kg) every 3 to 4 weeks based on clinical response (2.1) 0.5 milliliters (mL)/kg/hour (hr)
(0.8 mg/kg/ minutes (min) for 30 minutesIncrease every 30 minutes
(if tolerated) up to 5 mL/kg/hr (8 mg/kg/min)Subcutaneous (SC) Administration: (2.1)
Dose Initial Infusion Rate Maintenance Infusion Rate Initial dose: 1.37 × previous IV dose divided by # of weeks between IV doses.
Maintenance dose: Based on clinical response and target immunoglobulin G (IgG) trough level. (2.1)40 kg body weight (BW) and greater: 30 mL/site at 20 mL/hr/site
Under 40 kg BW: 20 mL/site at 15 mL/hr/site40 kg BW and greater: 30 mL/site at 20 to 30 mL/hr/site
Under 40 kg BW: 20 mL/site at 15 to 20 mL/hr/siteDOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
- History of anaphylactic or severe systemic hypersensitivity reactions to the administration of GAMMAGARD LIQUID ERC. (4)
WARNINGS AND PRECAUTIONS
- Hypersensitivity Reactions: In case of a severe hypersensitivity reaction, discontinue GAMMAGARD LIQUID ERC infusion, and manage as appropriate. (5.1)
- Renal Injury: Ensure patients are not volume depleted before administering GAMMAGARD LIQUID ERC. Monitor renal function, including blood urea nitrogen, serum creatinine, and urine output in patients receiving GAMMAGARD LIQUID ERC prior to initial infusion and at appropriate intervals thereafter. (5.2)
- Hyperproteinemia, hyperviscosity, and hyponatremia may occur. (5.3)
- Thrombosis: Monitor for signs and symptoms of thrombosis. (5.4)
- Aseptic Meningitis Syndrome (AMS): Conduct neurological examination on patients exhibiting symptoms and signs of AMS. (5.5)
- Hemolysis: Monitor for clinical signs and symptoms of hemolysis. (5.6)
- Transfusion-Related Acute Lung Injury (TRALI): Monitor patients for symptoms of TRALI and manage using oxygen therapy with adequate ventilatory support as appropriate. (5.7)
- Transmission of infectious disease: GAMMAGARD LIQUID ERC is made from human blood, it may carry a risk of transmitting infectious agents. (5.8)
ADVERSE REACTIONS
The most common adverse reactions (incidence ≥5%) were: (6.1)
Intravenous Administration: Headache, fatigue, pyrexia, chills, nausea, pain in extremity, diarrhea, migraine, vomiting, dizziness, urticaria, cough, asthma, oropharyngeal pain, infusion site extravasation, arthralgia, rash, myalgia, pruritus, and cardiac murmur. (6.1)
Subcutaneous Administration: Infusion site (local) event, headache, pyrexia, fatigue, heart rate increased, abdominal pain upper, vomiting, arthralgia, nausea, asthma, blood pressure systolic increased, diarrhea, ear pain, aphthous ulcer, migraine, oropharyngeal pain, and pain in extremity. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Takeda Pharmaceuticals U.S.A., Inc. at 1-877-TAKEDA-7 (1-877-825-3327) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
Passive transfer of antibodies may transiently interfere with immune responses to live virus vaccines, such as measles, mumps, rubella, and varicella. (7)
USE IN SPECIFIC POPULATIONS
Geriatric: In patients over age 65 or in any patient at risk of developing renal insufficiency, do not exceed the recommended dose. Infuse GAMMAGARD LIQUID ERC at the minimum infusion rate practicable. (8.5)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 10/2025
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: THROMBOSIS, RENAL DYSFUNCTION and ACUTE RENAL FAILURE
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
2.2 Preparation and Handling
2.3 Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity Reactions
5.2 Renal Injury
5.3 Hyperproteinemia, Hyperviscosity, and Hyponatremia
5.4 Thrombosis
5.5 Aseptic Meningitis Syndrome
5.6 Hemolysis
5.7 Transfusion-Related Acute Lung Injury
5.8 Transmission Infectious Agents
5.9 Monitoring Laboratory Tests
5.10 Interference with Laboratory Tests
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology and/or Pharmacology
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: THROMBOSIS, RENAL DYSFUNCTION and ACUTE RENAL FAILURE
- Thrombosis may occur with immune globulin products, including GAMMAGARD LIQUID ERC. Risk factors may include advanced age, prolonged immobilization, hypercoagulable conditions, history of venous or arterial thrombosis, use of estrogens, indwelling vascular catheters, hyperviscosity and cardiovascular risk factors. Thrombosis may occur in the absence of known risk factors [see Warnings and Precautions (5.4)].
- Renal dysfunction, acute renal failure, osmotic nephrosis, and death may occur in predisposed patients with immune globulin intravenous (IGIV) products. Patients predisposed to renal dysfunction include those with any degree of pre-existing renal insufficiency, diabetes mellitus, age greater than 65, volume depletion, sepsis, paraproteinemia, or patients receiving known nephrotoxic drugs. Renal dysfunction and acute renal failure occur more commonly in patients receiving IGIV products containing sucrose. GAMMAGARD LIQUID ERC does not contain sucrose [see Warnings and Precautions (5.2)].
- For patients at risk of thrombosis, administer GAMMAGARD LIQUID ERC at the minimum dose and infusion rate practicable. Ensure adequate hydration in patients before administration. Monitor for signs and symptoms of thrombosis and assess blood viscosity in patients at risk of hyperviscosity [see Dosage and Administration (2.3), Warnings and Precautions (5.4)].
-
1 INDICATIONS AND USAGE
GAMMAGARD LIQUID ERC is indicated as replacement therapy for primary humoral immunodeficiency (PI) in adult and pediatric patients two years of age and older. This includes, but is not limited to, common variable immunodeficiency (CVID), X-linked agammaglobulinemia, congenital agammaglobulinemia, Wiskott-Aldrich syndrome, and severe combined immunodeficiencies.
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
For intravenous (IV) or subcutaneous (SC) use only.
Intravenous Administration
Table 1: Recommended Dosage for Intravenous Administration Dosage Initial Infusion Rate Maintenance Infusion Rate 300 to 600 milligrams (mg)/kilograms (kg) every 3 to 4 weeks 0.5 milliliters (mL)/kg/hour (hr) (0.8 mg/kg/minutes (min) for 30 minutes Increase every 30 minutes
(if tolerated) up to 5 mL/kg/hr (8 mg/kg/min)- Adjust frequency and dosage to achieve target serum immunoglobulin G (IgG) levels and clinical response.
- If a patient misses a dose, administer the missed dose as soon as possible, and then resume scheduled treatments every 3 or 4 weeks, as applicable.
Dose Adjustments for Measles Exposure
If a patient has been exposed to measles, it may be prudent to administer an extra dose of GAMMAGARD LIQUID ERC intravenously as soon as possible and within 6 days of exposure. A dose of 400 mg/kg should provide a serum level >240 milli–International Units (mIU)/mL of measles antibodies for at least two weeks.
If a patient is at risk of future measles exposure and receives a dose of less than 530 mg/kg every 3 to 4 weeks, the dose should be increased to at least 530 mg/kg. This should provide a serum level of 240 mIU/mL of measles antibodies for at least 22 days after infusion.
Subcutaneous Administration
- Prior to switching from IV to SC treatment, obtain the patient's serum IgG trough level to guide subsequent dose adjustments.
- Start the initial SC dose approximately one week after the last IV infusion.
Table 2: Recommended Dosage for Subcutaneous Administration Dosage Initial Infusion Rate Maintenance Infusion Rate Initial dose:
Initial dose is 1.37 × previous IV dose divided by # of weeks between IV doses.
Maintenance dose:
Maintenance dose is based on clinical response and target IgG trough level.40 kg BW and greater: 30 mL/site at 20 mL/hr/site.
Under 40 kg BW: 20 mL/site at 15 mL/hr/site.40 kg BW and greater: 30 mL/site at 20 to 30 mL/hr/site.
Under 40 kg BW: 20 mL/site at 15 to 20 mL/hr/site.Dose Adjustments
Based on the results of clinical studies with GAMMAGARD LIQUID, the expected increase in serum IgG trough level during weekly SC treatment at the dose adjusted to provide a comparable area under the curve (AUC), is approximately 281 mg/ deciliter (dL) higher than the last IgG trough level during prior stable IV treatment. To calculate the target trough IgG level for SC treatment, add 281 mg/dL to the IgG trough level obtained after the last IV treatment.
To guide dose adjustment, calculate the difference between the patient's target serum IgG trough level and the IgG trough level during SC treatment. Find this difference in the columns of Table 3 and the corresponding amount (in mL) by which to increase (or decrease) the weekly dose based on the patient's body weight. If the difference between measured and target trough levels is less than 100 mg/dL, then no adjustment is necessary. However, the patient's clinical response should be the primary consideration in dose adjustment.
Table 3: Change in Weekly Dose of GAMMAGARD LIQUID ERC and Difference Between Measured and Target IgG Trough Levels * Body Weight 100 mg/dL 200 mg/dL 300 mg/dL 400 mg/dL - * Derived using a linear approximation to the nomogram method with a slope of 5.3 kg/dL.
10 kg 2 mL 4 mL 6 mL 8 mL 20 kg 4 mL 8 mL 11 mL 15 mL 30 kg 6 mL 11 mL 17 mL 23 mL 40 kg 8 mL 15 mL 23 mL 30 mL 50 kg 9 mL 19 mL 28 mL 38 mL 60 kg 11 mL 23 mL 34 mL 45 mL 70 kg 13 mL 26 mL 40 mL 53 mL 80 kg 15 mL 30 mL 45 mL 60 mL 90 kg 17 mL 34 mL 51 mL 68 mL 100 kg 19 mL 38 mL 57 mL 75 mL 110 kg 21 mL 42 mL 62 mL 83 mL 120 kg 23 mL 45 mL 68 mL 91 mL 130 kg 25 mL 49 mL 74 mL 98 mL 140 kg 26 mL 53 mL 79 mL 106 mL Example 1: A patient with a body weight of 80 kg has a measured IgG trough level of 800 mg/dL and the target trough level is 1000 mg/dL. The desired target trough level difference is 200 mg/dL (1000 mg/dL minus 800 mg/dL). The weekly dose of GAMMAGARD LIQUID ERC should be increased by 30 mL (3.0 g).
Example 2: A patient with a body weight of 60 kg has a measured IgG trough of 1000 mg/dL and the target trough level is 800 mg/dL. The desired target trough level difference is 200 mg/dL (800 mg/dL minus 1000 mg/dL). The weekly dose of GAMMAGARD LIQUID ERC should be decreased by 23 mL (2.3 g).
Dose Adjustments for Measles Exposure
If a patient has been exposed to measles, administer a dose of GAMMAGARD LIQUID ERC intravenously as soon as possible and within 6 days of exposure. A dose of 400 mg/kg IV should provide a serum level >240 mIU/mL of measles antibodies for at least two weeks.
If a patient is at risk of future measles exposure and receives a dose of less than 242 mg/kg subcutaneously per week, the dose should be increased to 242 mg/kg subcutaneously weekly while at risk.
2.2 Preparation and Handling
- Inspect the drug product visually for particulate matter and discoloration prior to administration. GAMMAGARD LIQUID ERC is a clear or slightly opalescent, colorless, or pale-yellow solution. Do not use if the solution is cloudy, turbid, or if it contains particulates.
- GAMMAGARD LIQUID ERC is for single-dose only. Partially used vials should be discarded. GAMMAGARD LIQUID ERC contains no preservatives.
- Allow refrigerated products to come to room temperature before use. DO NOT MICROWAVE.
- Do not shake.
- Do not mix with other products.
- Do not use normal saline as a diluent. If dilution is desired, 5% dextrose in water (D5W) should be used as a diluent.
- The infusion line may be flushed with normal saline. An in-line filter is optional.
- Record the name and lot number of the product in the recipient's records.
2.3 Administration
Intravenous Administration
- For rate of IV infusion, refer to Table 1
- Monitor patient vital signs throughout the infusion. Certain adverse reactions (ARs) such as headaches, flushing, and changes in pulse rate and blood pressure may be related to the rate of infusion. Slow or stop infusion if adverse reactions occur. If symptoms subside promptly, the infusion may be resumed at a lower rate that does not result in recurrence of the symptoms.
- Adverse reactions may occur more frequently in patients receiving immune globulin for the first time, upon switching brands or if there has been a long interval since the previous infusion. In such cases, start at lower infusion rates and gradually increase as tolerated.
- Ensure that patients with pre-existing renal insufficiency are not volume depleted. For patients over 65 years of age or judged to be at risk for renal dysfunction or thrombotic events, administer GAMMAGARD LIQUID ERC at the minimum infusion rate practicable. In such cases, the maximal rate should be less than 3.3 mg/kg/min (<2 mL/kg/hr); consider discontinuation of administration if renal function deteriorates [see Warnings and Precautions (5.2, 5.4), Use In Specific Populations (8.5)].
Subcutaneous Administration
Patients with a history of allergic reactions to immunoglobulin products should not be treated subcutaneously at home until 2 to 3 treatments have been administered and tolerated under medical supervision.
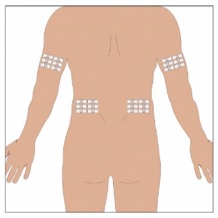
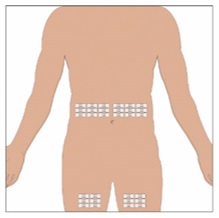
Selection of Infusion Site: Suggested areas for SC infusion of GAMMAGARD LIQUID ERC are abdomen, thighs, upper arms, or lower back. Infusion sites should be at least two inches apart, avoiding bony prominences. Rotate sites each week.
Volume per Site: The weekly dose (mL) should be divided by 30 or 20, based on patient weight above, to determine the number of sites required. Simultaneous SC infusion at multiple sites can be facilitated by using a multi-needle administration set.
Rate of Infusion
- For rate of SC infusion, refer to Table 2
- Patients 40 kg (88 lbs) and Greater: If multiple sites are used, the rate set on the pump should be the rate per site multiplied by the number of sites (e.g., 30 mL x 4 sites = 120 mL/hr). The number of simultaneous sites should be limited to 8, or maximum infusion rate of 240 mL/hr.
- Patients Under 40 kg (88 lbs): If multiple sites are used, the rate set on the pump should be the rate per site multiplied by the number of sites (e.g., 20 mL x 3 sites = 60 mL/hr). The number of simultaneous sites should be limited to 8, or maximum infusion rate of 160 mL/hr.
Instructions for Subcutaneous Administration: Instruct patients and/or caregivers to observe the following procedures:
1. Aseptic technique - Use aseptic technique when preparing and infusing GAMMAGARD LIQUID ERC.
2. Assemble supplies - Set up a clean work area and gather all supplies necessary for the SC infusion: vial(s) of GAMMAGARD LIQUID ERC, ancillary supplies, sharps container and pump. If GAMMAGARD LIQUID ERC has already been pooled into a bag or a syringe, skip to Step 6.
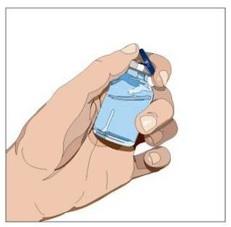
3. Product preparation - Remove the protective cap from the vial to expose the center of the vial (Figure 1).
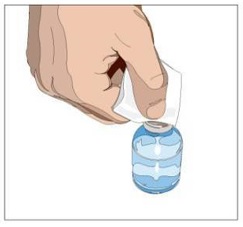
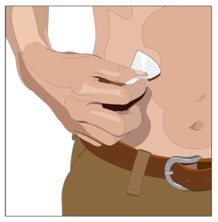
4. Wipe the stopper – Wipe the stopper with an alcohol pad and allow it to dry (Figure 2).
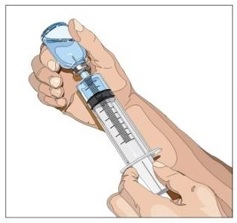
5. Withdraw GAMMAGARD LIQUID ERC from the vials - Attach a sterile syringe to a needle and draw air into the syringe barrel equal to the amount of product to be withdrawn. Inject the air into the vial and withdraw the desired volume of GAMMAGARD LIQUID ERC (Figure 3). If multiple vials are required to achieve the desired dose, repeat this step.
6. Prepare the infusion pump and tubing - Follow the manufacturer's instructions for preparing the pump and administration tubing, if needed. Be sure to prime the pump tubing to ensure that no air is left in the tubing and needle.
7. Select the infusion sites - Select the number of infusion sites depending on the volume of the total dose. [see Table 2] for recommended maximum volumes and rates. Potential sites for infusion include the back of arms, abdomen, thighs, and lower back (Figure 4, Figure 5). Ensure sites are at least 2 inches apart; avoid bony prominences.
8. Cleanse the infusion site(s) - Cleanse the infusion site(s) with an antiseptic skin preparation (e.g., alcohol pad) using a circular motion working from the center of the site and moving to the outside. Allow to dry (Figure 6).
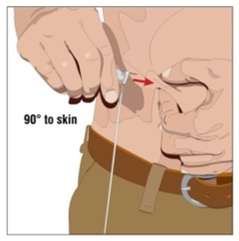
9. Insert the needle - Choose the correct needle length to assure that GAMMAGARD LIQUID ERC is delivered into the SC space. Grasp the skin and pinch at least one inch of skin between two fingers. Insert needle at a 90-degree angle with a darting motion into the SC tissue. Secure the needle (Figure 7).
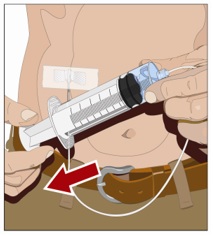
10. Check for proper needle placement - Prior to the start of infusion, check each needle for correct placement to make sure that a blood vessel has not been punctured. Gently pull back on the attached syringe plunger and monitor for any blood return in the needle set. If you see any blood, remove and discard the needle set. Repeat priming and needle insertion steps in a different infusion site with a new needle set (Figure 8).
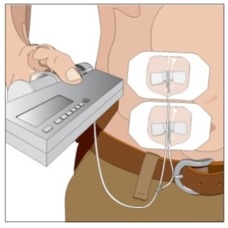
11. Secure the needle to the skin - Secure the needle(s) in place by applying a sterile protective dressing over the site (Figure 9).
12. Start the infusion of GAMMAGARD LIQUID ERC - Follow the manufacturer's instructions to turn the pump on (Figure 9).
13. Document the infusion - Remove the peel-off label with product lot number and expiration date from the GAMMAGARD LIQUID ERC vial and place in treatment diary/logbook to keep track of the product lots used. Keep the treatment diary/logbook current by recording the time, date, dose, product label and any reactions after each infusion.
14. Remove needle set - After the infusion is complete, remove the needle set and gently press a small piece of gauze over the needle insertion site and cover with a protective dressing. Discard any unused solution and disposable supplies in accordance with local requirements.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
GAMMAGARD LIQUID ERC is contraindicated in patients who have a history of anaphylactic or severe systemic hypersensitivity reactions to the administration of GAMMAGARD LIQUID ERC [see Warnings and Precautions (5.1)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity Reactions
Severe hypersensitivity reactions may occur after treatment with immune globulin products, including GAMMAGARD LIQUID ERC, even in patients previously treated with immune globulin products. Patients with known antibodies to IgA may have a greater risk of developing potentially severe hypersensitivity and anaphylactic reactions. In case of severe hypersensitivity, discontinue GAMMAGARD LIQUID ERC infusion immediately and manage with appropriate medications which may include epinephrine for immediate treatment.
GAMMAGARD LIQUID ERC contains IgA less than or equal to 2 µg/mL in a 10% solution. The concentration of IgA that will not provoke a reaction is not known, and therefore all immunoglobulin products, including GAMMAGARD LIQUID ERC, carry the risk of inducing an anaphylactic reaction to IgA.
5.2 Renal Injury
Renal injury including acute renal failure, acute tubular necrosis, proximal tubular nephropathy, and osmotic nephrosis may occur after treatment with immune globulin products, including GAMMAGARD LIQUID ERC.
Ensure patients are not volume depleted before administering GAMMAGARD LIQUID ERC. In patients who are at risk of renal injury because of pre-existing renal insufficiency or predisposition to acute renal failure (such as diabetes mellitus, age greater than 65, volume depletion, sepsis, paraproteinemia, or patients receiving known nephrotoxic drugs, etc.), administer GAMMAGARD LIQUID ERC at the minimum rate of infusion practicable [see Dosage and Administration (2.3)].
Assess renal function, including measurement of blood urea nitrogen (BUN), serum creatinine, and urine output in patients receiving GAMMAGARD LIQUID ERC prior to initial infusion and at appropriate intervals thereafter. If renal function deteriorates, consider discontinuation of GAMMAGARD LIQUID ERC [see Dosage and Administration (2.3)].
5.3 Hyperproteinemia, Hyperviscosity, and Hyponatremia
Hyperproteinemia, hyperviscosity, and hyponatremia may occur in patients receiving immune globulin products, including GAMMAGARD LIQUID ERC. Distinguish true hyponatremia from pseudohyponatremia that is temporally or causally related to hyperproteinemia with concomitant decreased calculated serum osmolality or elevated osmolar gap. Treatment aimed at decreasing serum free water in patients with pseudohyponatremia may lead to volume depletion and hyperviscosity and a predisposition to thromboembolic events.
5.4 Thrombosis
Thrombosis may occur following treatment with immune globulin products, including GAMMAGARD LIQUID ERC. Risk factors include advanced age, prolonged immobilization, hypercoagulable conditions, history of venous or arterial thrombosis, use of estrogens, indwelling central vascular catheters, hyperviscosity, and cardiovascular risk factors. Thrombosis may occur in the absence of known risk factors.
Ensure adequate hydration in patients before administration of GAMMAGARD LIQUID ERC. For patients at risk of thrombosis, administer GAMMAGARD LIQUID ERC at the minimum dose and infusion rate practicable. Monitor patients for signs and symptoms of thrombosis.
Consider baseline assessment of blood viscosity in patients at risk for hyperviscosity, including patients with cryoglobulins, fasting chylomicronemia, high triacylglycerols (triglycerides), or monoclonal gammopathies [see Boxed Warning, Dosage and Administration (2.3)].
5.5 Aseptic Meningitis Syndrome
Aseptic meningitis syndrome (AMS) may occur with immune globulin products, including GAMMAGARD LIQUID ERC. The risk of AMS may be higher with high doses (2 g/kg) and/or rapid infusion of immunoglobulin products. Signs and symptoms of AMS include severe headache, nuchal rigidity, drowsiness, fever, photophobia, painful eye movements, nausea and vomiting. AMS usually begins within several hours to 2 days following immune globulin treatment. Conduct neurological examination on patients exhibiting symptoms and signs of AMS, including Cerebrospinal fluid (CSF) studies, to rule out other causes of meningitis. CSF studies frequently reveal pleocytosis up to several thousand cells per cubic millimeter, elevated protein levels up to several hundred mg/dL, and negative culture results. Discontinuation of immune globulin treatment has resulted in remission of AMS within several days without sequelae.
5.6 Hemolysis
Hemolysis may occur with immune globulin products, including GAMMAGARD LIQUID ERC due to the presence of blood group antibodies that may act as hemolysins and induce in vivo coating of red blood cells (RBC). This may cause a positive direct antiglobulin test [DAT (Coombs test)]. Delayed hemolytic anemia can develop after GAMMAGARD LIQUID ERC therapy due to enhanced RBC sequestration [see Adverse Reactions (6)].
The risk factors for hemolysis include high doses (e.g., ≥2 g/kg, either as a single administration or divided over several days), non-O blood group, and underlying inflammatory disease condition.
Monitor patients for signs and symptoms of hemolysis. Conduct appropriate laboratory testing in higher risk patients, including measurement of hemoglobin or hematocrit prior to infusion and within approximately 36 to 96 hours post-infusion. If signs and symptoms of hemolysis are observed, perform additional confirmatory laboratory testing [see Warnings and Precautions (5.9)].
5.7 Transfusion-Related Acute Lung Injury
Transfusion-Related Acute Lung Injury (TRALI) may occur following treatment with immune globulin products, including GAMMAGARD LIQUID ERC. Symptoms typically occur within 1 to 6 hours after treatment and may include severe respiratory distress, pulmonary edema, hypoxemia, normal left ventricular function, and fever.
Monitor patients for signs and symptoms of TRALI. If TRALI is suspected, perform appropriate tests for the presence of anti-neutrophil and anti-HLA antibodies in both the product and patient serum. Manage patients using oxygen therapy with ventilatory support as appropriate.
5.8 Transmission Infectious Agents
There is risk of transmission of infectious disease or agents including viruses, the variant Creutzfeldt-Jakob disease (vCJD) agent, and the Creutzfeldt-Jakob disease agent with GAMMAGARD LIQUID ERC administration because it is manufactured using human blood. The risk of infectious agent transmission is minimized by plasma donor screening, donation testing, and manufacturing steps proven to inactivate and remove bloodborne pathogens.
All infections thought by a physician to possibly have been transmitted by this product should be reported by to Takeda Pharmaceuticals U.S.A., Inc at 1-877-TAKEDA-7 (1-877-825-3327) (in the U.S.).
5.9 Monitoring Laboratory Tests
- Assess renal function including measurement of blood urea nitrogen (BUN) and serum creatinine before the initial infusion of GAMMAGARD LIQUID ERC and at appropriate intervals thereafter.
- Consider baseline assessment of blood viscosity in patients at risk for hyperviscosity, including those with cryoglobulins, fasting chylomicronemia, high triacylglycerols (triglycerides), or monoclonal gammopathies, because of the potentially increased risk of thrombosis.
- If signs and/or symptoms of hemolysis are present after an infusion of GAMMAGARD LIQUID ERC, perform appropriate laboratory testing for confirmation.
- If TRALI is suspected, perform appropriate tests for the presence of anti-neutrophil antibodies and anti-HLA antibodies in both the product and the patient's serum.
5.10 Interference with Laboratory Tests
False positive serological testing results including a positive direct or indirect antiglobulin (Coombs) test may occur after administration of immune globulin products, including GAMMAGARD LIQUID ERC due to the transitory rise of various passively transferred antibodies.
Administration of immune globulin products, including GAMMAGARD LIQUID ERC, can lead to false positive readings in assays that depend on detection of beta-D-glucans for diagnosis of fungal infections; this may persist during the weeks following infusion of the product.
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice.
No clinical studies have been conducted using GAMMAGARD LIQUID ERC. The safety of GAMMAGARD LIQUID ERC in patients with primary humoral immunodeficiency (PI) is supported by two clinical studies conducted on GAMMAGARD LIQUID, Study 1 and Study 2 as described below.
Study 1
The safety of GAMMAGARD LIQUID IV infusion was evaluated in Study 1. A total of 61 patients received 1,811 infusions of GAMMAGARD LIQUID at a dose of 300 to 600 mg/kg every 21 to 28 days for 12 months [see Clinical Studies 14].
A total of 5 serious adverse reactions were reported in 4 patients (28%), including two cases of aseptic meningitis in one patient, stent placement, gastrointestinal hemorrhage, and encephalopathy. Out of these 5 serious adverse reactions, only 1 case of aseptic meningitis was deemed to be related by the investigator. Two patients were discontinued, likely due to adverse reactions, which were pruritic papular rash and aseptic meningitis.
Table 4: summarizes the most common adverse reactions occurring in ≥5% of patients in Study 1.
Table 4: Adverse Reactions Occurring in ≥5% of Patients in Study 1 Adverse Reactions* By Infusion N (%)
(N=1,811 Infusions)By Patient N (%)
(N=61 Patients)- * Adverse reactions were defined as adverse events occurring during or within 72 hours of infusion or any causally related event occurring within the study period.
Headache 94 (5%) 29 (48%) Fatigue 33 (2%) 14 (23%) Pyrexia 28 (2%) 17 (28%) Chills 28 (2%) 12 (20%) Nausea 17 (0.9%) 11 (18%) Pain in extremity 13 (0.7%) 7 (11%) Diarrhea 12 (0.7%) 9 (15%) Migraine 12 (0.7%) 4 (7%) Vomiting 11 (0.6%) 9 (15%) Dizziness 11 (0.6%) 8 (13%) Urticaria 10 (0.6%) 6 (10%) Cough 9 (0.5%) 8 (13%) Asthma 7 (0.4%) 6 (10%) Oropharyngeal pain 7 (0.4%) 5 (8%) Infusion site extravasation 7 (0.4%) 4 (7%) Arthralgia 6 (0.3%) 5 (8%) Rash 6 (0.3%) 4 (7%) Myalgia 5 (0.3%) 5 (8%) Pruritus 5 (0.3%) 4 (7%) Cardiac murmur 4 (0.2%) 4 (7%) Study 2
The safety of GAMMAGARD LIQUID SC infusion was evaluated in Study 2. A total of 47 patients received 2,294 SC infusions of GAMMAGARD LIQUID at a mean dose of 182 to 191 mg/kg/week for a median duration of 379 days (range 57 to 477 days) [see Clinical Studies 14].
One serious adverse reaction of chest pain was reported in 1 patient (2%). One patient discontinued likely due to adverse reactions of fatigue and malaise.
Table 5 summarizes the most common adverse reactions occurring in ≥5% of patients in Study 2.
Table 5: Adverse Reactions Occurring in ≥5% of Patients in Study 2 Adverse Reactions* By Infusion N (%)
(N=2294 Infusions)By Patient N (%)
(N=47 Patients)- * Adverse reactions were defined as adverse events occurring during or within 72 hours of infusion or any causally related event occurring within the study period.
- † included rash, erythema, edema, hemorrhage, pain, hematoma, pruritus, and swelling.
Infusion site (local) event† 55 (2%) 21 (45%) Headache 31 (1%) 19 (40%) Pyrexia 11 (0.5%) 9 (19%) Fatigue 11 (0.5%) 7 (15%) Heart rate increased 11 (0.5%) 3 (6%) Abdominal pain upper 9 (0.4%) 5 (11%) Vomiting 7 (0.3%) 5 (11%) Arthralgia 7 (0.3%) 3 (6%) Nausea 7 (0.3%) 3 (6%) Asthma 6 (0.3%) 4 (9%) Blood pressure systolic increased 6 (0.3%) 3 (6%) Diarrhea 5 (0.2%) 3 (6%) Ear pain 4 (0.2%) 3 (6%) Aphthous ulcer 3 (0.1%) 3 (6%) Migraine 3 (0.1%) 3 (6%) Oropharyngeal pain 3 (0.1%) 3 (6%) Pain in extremity 3 (0.1%) 3 (6%) 6.2 Postmarketing Experience
Because adverse reactions are reported voluntarily post-approval from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to product exposure.
GAMMAGARD LIQUID
The following adverse reactions have been identified during postmarketing use of GAMMAGARD LIQUID.
Intravenous Administration
Blood and Lymphatic System Disorders: Hemolysis
Immune System Disorders: Anaphylactic shock
Nervous System Disorders: Cerebral vascular accident, Transient ischemic attack, Tremor
Cardiac Disorders: Myocardial infarction
Vascular Disorders: Deep vein thrombosis, Hypotension
Respiratory, Thoracic and Mediastinal Disorders: Pulmonary embolism, Pulmonary edema, Chest pain, Transfusion-related acute lung injury
Skin and Subcutaneous Tissue Disorders: Hyperhidrosis
Investigations: Coombs direct test positive, Oxygen saturation decreased
Subcutaneous Administration
Immune System Disorders: Hypersensitivity
Musculoskeletal and Connective Tissue Disorders: Myalgia
General Disorders and Administration Site Conditions: Chills
GENERAL
In addition to the adverse reactions listed above, the following adverse reactions have been identified for immune globulin products.
Blood and Lymphatic System Disorder: Hemolytic anemia, Pancytopenia
Nervous System Disorders: Aseptic meningitis, Coma, Seizures, Loss of consciousness, Paresthesia, Lethargy
Cardiac Disorders: Arrhythmia, Tachycardia, Cardiac arrest
Vascular Disorders: Flushing, Vascular collapse
Respiratory, Thoracic and Mediastinal Disorders: Cyanosis, Hypoxemia, Bronchospasm, Apnea, Acute Respiratory Distress Syndrome (ARDS), Dyspnea, Laryngospasm, Renal and Urinary Disorders: Renal impairment, Osmotic nephropathy
Skin and Subcutaneous Tissue Disorders: Bullous dermatitis, Epidermolysis, Erythema multiforme, Stevens-Johnson Syndrome
Gastrointestinal Disorders: Hepatic dysfunction
General Disorders and Administration Site Conditions: Malaise, Fever, Injection site reaction (including induration, warmth)
-
7 DRUG INTERACTIONS
Immunoglobulin administration may transiently impair the efficacy of live attenuated virus vaccines such as mumps, rubella and varicella because of passively acquired antibodies. Inform the immunizing physician of recent therapy with GAMMAGARD LIQUID ERC so that appropriate precautions can be taken.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Animal reproduction studies have not been conducted with GAMMAGARD LIQUID ERC. It is not known whether GAMMAGARD LIQUID ERC can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Immune globulins cross the placenta from maternal circulation increasingly after 30 weeks of gestation. GAMMAGARD LIQUID ERC should be given to a pregnant woman only if clearly indicated.
The background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
8.2 Lactation
Risk Summary
There is no information regarding the presence of GAMMAGARD LIQUID ERC in human milk, its effects on the breast-fed infant or its effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for GAMMAGARD LIQUID ERC and any potential adverse effects on the breast-fed infant from GAMMAGARD LIQUID ERC or from the underlying maternal condition.
8.4 Pediatric Use
GAMMAGARD LIQUID clinical studies have established the safety and efficacy of the GAMMAGARD LIQUID ERC in pediatric patients with PI aged 2 years of age and older.
GAMMAGARD LIQUID administered intravenously was evaluated in 15 pediatric patients with PI (7 patients aged 2 to <12 years and 8 patients aged 12 to <16 years). GAMMAGARD LIQUID administered subcutaneously was evaluated in 18 pediatric patients with PI (14 patients aged 2 to <12 years and 4 patients aged 12 to <16 years) [see Adverse Reactions (6) and Clinical Studies (14)].
The safety and efficacy of GAMMAGARD LIQUID ERC in pediatric patients below the age of 2 have not been established.
8.5 Geriatric Use
Limited information is available for the geriatric use of GAMMAGARD LIQUID ERC. The geriatric use of GAMMAGARD LIQUID administered intravenously and subcutaneously was evaluated in two clinical studies (Study 1 and Study 2). The studies included 8 patients over the age of 65 years. No differences in safety or efficacy were observed for this group. Monitor patients who are at an increased risk for developing renal failure or thrombotic events. Do not exceed the recommended dose. Infuse at the minimum IV infusion rate practicable [see Boxed Warning, Warnings and Precautions (5.2, 5.4), Dosage and Administration (2.3)].
- 10 OVERDOSAGE
-
11 DESCRIPTION
GAMMAGARD LIQUID ERC (human immunoglobulin) is a single-dose sterile, liquid preparation of purified and concentrated IgG antibodies. GAMMAGARD LIQUID ERC has an IgA concentration less than or equal to 2 µg/mL, in a 10% solution.
The distribution of the IgG subclasses is similar to that of normal plasma with lower levels of IgG4 and IgG3. The Fc and Fab functions are maintained in GAMMAGARD LIQUID ERC. Pre-kallikrein activator activity is not detectable. GAMMAGARD LIQUID ERC contains 100 mg/mL protein. At least 98% of the protein is immune globulin, the average IgA concentration is less than or equal to 2 µg/mL, in a 10% solution and immunoglobulin M is present in trace amounts.
GAMMAGARD LIQUID ERC contains a broad spectrum of IgG antibodies against bacterial and viral agents. Glycine (0.25M) serves as a stabilizing and buffering agent. There are no added sugars, sodium, or preservatives. The pH is 4.6 to 5.1. The osmolality is 240 to 300 mOsmol/kg, which is similar to physiological osmolality (285 to 295 mOsmol/kg).
GAMMAGARD LIQUID ERC is manufactured from large pools of human plasma. IgG preparations are purified from plasma pools using a modified Cohn-Oncley cold ethanol fractionation process, as well as cation and anion exchange chromatography. GAMMAGARD LIQUID ERC shares its manufacturing process with GAMMAGARD LIQUID. The differentiation occurs with the modified parameters applied during the anion exchange chromatography step enhanced removal capability (ERC) to reduce IgA content, resulting in a product with IgA less than or equal to 2 µg/mL in a 10% solution.
Screening against potentially infectious agents begins with the donor selection process and continues throughout plasma collection and plasma preparation. Each individual plasma donation used in the manufacture of GAMMAGARD LIQUID ERC is collected only at FDA-approved blood establishments and is tested by FDA licensed serological tests for Hepatitis B Surface Antigen (HBsAg), and for antibodies to Human Immunodeficiency Virus (HIV-1/HIV-2) and Hepatitis C Virus (HCV) in accordance with U.S. regulatory requirements. As an additional safety measure, mini-pools of the plasma are tested for the presence of HIV-1 and HCV by FDA licensed Nucleic Acid Testing (NAT) and found to be negative.
To improve the margin of safety, validated virus inactivation/removal steps have been integrated into the manufacturing and formulation processes, namely solvent/detergent (S/D) treatment, nanofiltration, and a low pH incubation at elevated temperature (30° to 32°C). The S/D process includes treatment with an organic mixture of tri-n-butyl phosphate, octoxynol 9 and polysorbate 80 at 18° to 25°C for a minimum of 60 minutes. S/D treatment inactivates the lipid-enveloped viruses investigated to below detection limits within minutes.
In vitro virus spiking studies have been used to validate the capability of the manufacturing process to inactivate and remove viruses. To establish the minimum applicable virus clearance capacity of the manufacturing process, virus clearance studies were performed under extreme conditions (e.g., at minimum S/D concentrations, incubation time and temperature for the S/D treatment).
Virus clearance studies for GAMMAGARD LIQUID ERC performed in accordance with good laboratory practices are summarized in Table 6.
Table 6: Three Dedicated Independent Virus Inactivation/Removal Steps, Mean Log10 Reduction Factors* (RFs) for Each Virus and Manufacturing Step Virus Type Enveloped RNA Enveloped DNA Non-enveloped
RNANon-enveloped
DNAAbbreviations: HIV-1, Human Immunodeficiency Virus Type 1; BVDV, Bovine Viral Diarrhea Virus (model for Hepatitis C Virus and other lipid enveloped RNA viruses); WNV, West Nile Virus; PRV, Pseudorabies Virus (model for lipid enveloped DNA viruses, including Hepatitis B Virus); EMCV, Encephalomyocarditis Virus (model for non-lipid enveloped RNA viruses, including Hepatitis A Virus [HAV]); MMV, Mice Minute Virus (model for non-lipid enveloped DNA viruses, including B19 Virus [B19V]); n.d. (not done), n.a. (not applicable). - * For the calculation of these RF data from virus clearance study reports, applicable manufacturing conditions were used. Log10 RFs on the order of 4 or more are considered effective for virus clearance in accordance with the Committee for Medicinal Products for Human Use (CHMP, formerly CPMP) guidelines.
- † No RF obtained due to immediate neutralization of HAV by the anti-HAV antibodies present in the product.
Family Retroviridae Flaviviridae Herpesviridae Picornaviridae Parvoviridae Virus HIV-1 BVDV WNV PRV HAV EMCV MMV SD treatment >4.5 >6.2 n.a. >4.8 n.d. n.d. n.d. Nanofiltration >4.5 >5.1 >6.2 >5.6 5.7 1.4 2.0 Low pH treatment >5.8 >5.5 >6.0 >6.5 n.d.† >6.3 3.1 Overall log reduction factor (ORF) >14.8 >16.8 >12.2 >16.9 5.7† >7.7 5.1 -
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
GAMMAGARD LIQUID ERC supplies a broad spectrum of opsonizing and neutralizing IgG antibodies against a wide variety of bacterial and viral agents. GAMMAGARD LIQUID ERC also contains a spectrum of antibodies capable of interacting with and altering the activity of cells of the immune system as well as antibodies capable of reacting with cells such as erythrocytes. The role of these antibodies and the mechanism of action of IgG in GAMMAGARD LIQUID ERC have not been fully elucidated.
12.3 Pharmacokinetics
Study 1
Following IV infusion, IGIV products show a biphasic decay curve. The initial (α) phase is characterized by an immediate post-infusion peak in serum IgG and is followed by rapid decay due to equilibration between the plasma and extravascular fluid compartments. The second (β) phase is characterized by a slower and constant rate of decay.
The pharmacokinetics of immunoglobulins depend on their concentration.
The commonly cited "normal" half-life of 18 to 25 days is based on studies in which tiny quantities of radiolabeled IgG are injected into healthy individuals. When radiolabeled IgG was injected into patients with hypogammaglobulinemia or agammaglobulinemia, highly variable half-lives ranging from 12 to 40 days were observed. In other radiolabeled studies, high serum concentrations of IgG and hypermetabolism associated with fever and infection have been seen to coincide with a shortened IgG half-life.
In contrast, pharmacokinetic studies of GAMMAGARD LIQUID in immunodeficient patients are based on the decline of IgG concentrations following infusion of large quantities of immune globulin. In such studies, investigators have reported uniformly prolonged half-lives of 26 to 35 days. Pharmacokinetic parameters for GAMMAGARD LIQUID were determined from total IgG levels following the fourth infusion in patients with primary humoral immunodeficiency (N=61) treated intravenously with the product every 3 or 4 weeks according to the regimen used prior to entering the study. Of these, 57 had sufficient pharmacokinetic data to be included in the dataset. The median weight-adjusted dose per patient was 455 mg/kg/4 weeks with a range of 262 to 710 mg/kg/4 weeks. Pharmacokinetic parameters are presented in Table 7.
Table 7: Summary of Intravenous Pharmacokinetic Parameters in 57 Patients Parameter Median 95% Confidence Interval Abbreviations: AUC=area under the curve, Cmax=maximum concentration, Cmin=minimum concentration Dose of IgG (mg/kg/4 weeks) 455 Range: 262 to 710 Elimination Half-Life (T1/2 days) 35 (31, 42) AUC0-21d (milligram days/dL) 29139 (27494, 30490) Cmax (Peak, mg/dL) 2050 (1980, 2200) Cmin (Trough, mg/dL) 1030 (939, 1110) Incremental recovery (mg/dL)/(mg/kg) 2.3 (2.2, 2.6) Median IgG trough levels were maintained between 960 to 1120 mg/dL. These dosing regimens-maintained serum trough IgG levels generally considered adequate to prevent bacterial infections. The elimination of half-life of GAMMAGARD LIQUID (35 days) was similar to that reported for other IGIV products.
Study 2
Pharmacokinetic (PK) parameters of subcutaneously administered GAMMAGARD LIQUID were evaluated in patients with primary immunodeficiency (PI) who were 12 years of age and older during a clinical study [see Clinical Studies (14)].
Patients were treated intravenously for 12 weeks with GAMMAGARD LIQUID and then switched to weekly SC GAMMAGARD LIQUID infusions. Initially, all patients were treated for a minimum of 12 weeks at a SC dose that was 130% of the IV dose. A comparison of the AUC for IV and SC infusions done on the first 15 adult patients determined that the SC dose required to provide an exposure from SC administration that was not inferior to the exposure from IV administration was 137% of the IV dose. Subsequently, all patients were treated with this dose for 6 weeks after which the dose was individualized for all patients based on IgG trough levels, as described below. After a minimum of 8 weeks at this SC dose, a PK evaluation was conducted on patients 12 years of age or older (N=32).
The mean adjusted dose at the end of the study was 137.3% (125.7 to 150.8) of the IV dose for patients 12 years of age and older, and 141.0% (100.5 to 160.0) for patients under the age of 12. Thus, a significant dosing difference was not required for children. At this dose adjustment, the geometric mean ratio of the AUC for SC vs IV GAMMAGARD LIQUID administration was 95.2% (90% confidence limit (CI): 92.3 to 98.2). The peak IgG level occurred 2.9 (1.2 to 3.2) days after SC administration.
Pharmacokinetic parameters of GAMMAGARD LIQUID administered intravenously vs subcutaneously in clinical study are shown in Table 8. The mean peak IgG level was lower (1393 ± 289 mg/dL) during SC treatment than with IV treatment (2240 ± 536 mg/dL), consistent with lower weekly doses compared with doses administered every 3 or 4 weeks intravenously. In contrast, the mean trough level was higher when GAMMAGARD LIQUID was given subcutaneously (1202 ± 282 mg/dL) than when it was given intravenously (1050 ± 260 mg/dL), a result of both higher monthly dose and more frequent dosing. The median IgG trough level during IV treatment in this clinical study, 1010 mg/dL (95% CI: 940 to 1240), was similar to the median IgG trough level of 1030 mg/dL (95% CI: 939 to 1110) during IV treatment as shown in Table 8. By contrast, the median IgG trough level during SC treatment was higher, at 1260 mg/dL (95% CI: 1060 to 1400).
Table 8: Pharmacokinetic Parameters of Subcutaneously Administered GAMMAGARD LIQUID Compared with GAMMAGARD LIQUID Administered Intravenously in 32 Patients Pharmacokinetic Parameters Subcutaneous Administration Intravenous Administration - * Weekly equivalent dose
- † Standardized to a 7-day interval
Dose* (mg/kg) Mean ± SD 182.6 ± 48.4 133.2 ± 36.9 Range (min to max) 94.2 to 293.8 62.7 to 195.4 IgG Peak Levels (mg/dL) Mean ± SD 1393 ± 289 2240 ± 536 Range (min to max) 734 to 1900 1130 to 3610 IgG Trough Levels (mg/dL) Mean ± SD 1202 ± 282 1050 ± 260 Range (min to max) 621 to 1700 532 to 1460 AUC (days† mg/dL) Mean ± SD 9176 ± 1928 9958 ± 2274 Range (min to max) 4695 to 12468 5097 to 13831 Clearance (mL/kg/day) Mean ± SD 2.023 ± 0.528 1.355 ± 0.316 Range (min to max) 1.225 to 3.747 0.880 to 2.340 -
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
An in vitro mutagenicity test was performed with GAMMAGARD LIQUID. No evidence of mutagenicity was observed.
13.2 Animal Toxicology and/or Pharmacology
In single-dose toxicity studies GAMMAGARD LIQUID revealed no adverse effects at doses of 5000 mg/kg or 2000 mg/kg in mice and rats, respectively. Repeat-dose toxicity studies were not conducted.
In in-vitro immune cell activation, cytokine/chemokine release and complement activation assays with GAMMAGARD LIQUID ERC no increased potential to stimulate the immune system and associated risk for hypersensitivity reactions compared to GAMMAGARD LIQUID were revealed. No hypotensive or bronchospastic effects were observed with GAMMAGARD LIQUID ERC in safety pharmacology studies in spontaneously hypertensive rats and guinea pigs.
-
14 CLINICAL STUDIES
No clinical studies have been conducted with GAMMAGARD LIQUID ERC. The efficacy of GAMMAGARD LIQUID ERC for primary humoral immunodeficiency (PI) are supported by two clinical studies conducted on GAMMAGARD LIQUID, Study 1 with IV administration (NCT00157079) and Study 2 with both IV and SC administration (NCT00546871).
This was an open-label study to evaluate the efficacy of GAMMAGARD LIQUID in patients with PI. A total of 61 patients received IV infusion of GAMMAGARD LIQUID at the dose 300 to 600 mg/kg every 21 to 28 days for 12 months.
The population characteristics were as follows: The median age was 34 years (range 6 to 72 years), 54% were female 93% were Caucasian, 5% were African American, and 2% were Asian. Three patients were excluded from the per-protocol efficacy analysis due to study withdrawal for non-study product related reasons.
The primary efficacy outcome was the annualized rate of acute serious bacterial infections defined as the mean number of prespecified acute serious bacterial infections per patient per year. Secondary efficacy outcome measure was hospitalizations secondary to infection. Table 9 summarizes the efficacy results.
Table 9: Efficacy Outcomes from Study 1 (N=58) Efficacy Outcomes Number of Events - * Serious acute bacterial infections were defined by FDA and met specific diagnostic requirements
- † The rate of validated infections was compared with a rate of 1 per patient per year, in accordance with recommendations by the FDA Blood Products Advisory Committee
Serious Acute Bacterial Infections* Bacteremia/Sepsis 0 Bacterial Meningitis 0 Osteomyelitis/Septic Arthritis 0 Bacterial Pneumonia 0 Visceral Abscess 0 Total 0 Hospitalizations Secondary to Infection 0 Mean Number of Validated Infections per Patient per Year 0 p-value† p<0.0001 95% Confidence Interval† (0.000, 0.064) An open-label, non-controlled, multicenter study to determine the efficacy, tolerability and PK of GAMMAGARD LIQUID SC infusion in adult and pediatric patients with PI.
A total of 49 patients were treated for 12 weeks with GAMMAGARD LIQUID IV infusion every 3 or 4 weeks. Patients who were on IV treatment prior to entering the study were switched to GAMMAGARD LIQUID at the same dose and frequency. Patients who were receiving SC immune globulin were switched to GAMMAGARD LIQUID at the IV dose they had received prior to switching to SC treatment. A PK analysis was performed at the end of the IV period in all patients aged 12 years and older. One week after the last IV infusion, each patient began SC treatment with GAMMAGARD LIQUID at 130% of the weekly equivalent of the IV dose for a minimum of 12 weeks. The median dose determined from the PK studies of the first 15 adult patients exposed to SC treatment was 137% of the IV dose, and subsequently all patients were treated for a minimum of 6 weeks at this dose. After 6 SC infusions, a trough IgG level was obtained and used to individually adapt the SC dose of GAMMAGARD LIQUID to compensate for individual variation [see Clinical Pharmacology (12.3)]. All patients received a minimum of 12 infusions at this individually adapted dose and continued to receive SC treatment with GAMMAGARD LIQUID until the last patient completed the study. Patients (N=47) were treated with 2,294 SC infusions of GAMMAGARD LIQUID: 4 patients treated for up to 29 weeks, 17 patients for 30 to 52 weeks, and 26 patients for 53 weeks or longer. Two patients that completed the IV treatment part of the study did not continue to the SC treatment part of the study. The median duration of SC treatment was 379 days (range: 57 to 477 days).
The population characteristics were as follows: The median age was 20 years (range 3 to 77 years) including 18 pediatric patients, 45% were female, 94% were Caucasian, 4% were Black, and 2% were Hispanic.
Mean weekly SC doses ranged from 182 mg/kg to 191 mg/kg (at 130% to 137% of the IV dose). In the study, the number of infusion sites per infusion was dependent on the dose of IgG and ranged from 2 to 10. In 75% of infusions, the number of infusion sites was 5 or fewer.
The efficacy results are summarized in Table 10 below.
Table 10: Efficacy Outcomes from Study 2 (N = 47) during Subcutaneous Treatment Infections - * CI is lower than the minimal goal of achieving a rate of <1 bacterial infection per patient-year
- † Included systemic and topical antibacterial, anti-fungal, anti-viral, and anti-protozoal antimicrobials.
Number of patients (efficacy phase)
Total number of patients years
Number of patients with serious bacterial infections
Number of serious bacterial infections
Annual rate of serious bacterial infections
Annual rate of any infections47
44
3
3 (all bacterial pneumonias)
0.07 (99% upper CI 0.13)*
infections/patient year
4 (95% CI 3 to 5)
infections/patient yearAntibiotic use† (prophylaxis or treatment) Number of patients (%)
Annual rate40 (85%)
50 (95% CI 33 to 72) days/patient yearDays out of work/school/day care or unable to perform normal activities Number of patients (%)
Annual rate25 (53%)
4 (95% CI 2 to 6) days/patient yearHospitalizations due to infections Number of patients (%)
Annual rate0 (0%)
0 (95% CI 0.0 to 0.1) days/patient year -
16 HOW SUPPLIED/STORAGE AND HANDLING
GAMMAGARD LIQUID ERC is supplied in single-dose vials containing the labeled amount of functionally active IgG with less than or equal to 2 μg/mL IgA in a 10% solution.
The packaging of this product is not made with natural rubber latex.
The following presentations of GAMMAGARD LIQUID ERC are available:
NDC Number (Carton) NDC Number (Vial) Volume Protein 0944-2705-50 0944-2705-05 50 mL 5 g 0944-2705-10 0944-2705-01 100 mL 10 g - DO NOT freeze.
- Store GAMMAGARD LIQUID ERC in the refrigerator or at room temperature.
- Refrigerated Temperature: 2° to 8°C (36° to 46°F) for up to 36 months.
- Room Temperature: up to 25°C (77°F) for up to 24 months.
- Expiration dates for both storage conditions are printed on the outer carton and vial label.
- Do not use past the applicable expiration date.
- Discard unused portion.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information and Instructions for Use).
Discuss the following with the patient and/or caregivers.
- Hypersensitivity Reactions: Inform patients and/or caregivers that hypersensitivity reactions may occur with GAMMAGARD LIQUID ERC infusion. Prior to starting GAMMAGARD LIQUID ERC ask about a history of allergic reactions to immune globulin or other blood products. Advise patients and/or caregivers to seek immediate medical evaluation if any signs and symptoms of hypersensitivity or acute infusion reactions occur [see Warnings and Precautions (5.1)].
- Renal Injury: Inform patients and/or caregivers that renal injury may occur with GAMMAGARD LIQUID ERC infusion. Advise patients and/or caregivers to seek immediate medical evaluation if any signs and symptoms of renal injury occur such as decreased urine output, sudden weight gain, fluid retention/edema, and/or shortness of breath [see Warnings and Precautions (5.2)].
- Thrombosis: Inform patients and/or caregivers that thrombosis may occur after GAMMAGARD LIQUID ERC infusion. Advise patients and/or caregivers to seek immediate medical evaluation if any signs and symptoms of thrombosis occur such as pain and/or swelling of an arm or leg with warmth over the affected area, discoloration of an arm or leg, unexplained shortness of breath, chest pain or discomfort that worsens on deep breathing, unexplained rapid pulse, numbness or weakness on one side of the body [see Warnings and Precautions (5.4)].
- Aseptic meningitis syndrome (AMS): Inform patients and/or caregivers that AMS may occur after GAMMAGARD LIQUID ERC infusion. Advise patients and/or caregivers to seek immediate medical evaluation if any signs and symptoms of AMS occur such as severe headache, neck stiffness, drowsiness, fever, sensitivity to light, painful eye movements, nausea, and vomiting [see Warnings and Precautions (5.5)].
- Hemolysis: Inform patients and/or caregivers that hemolysis may occur after GAMMAGARD LIQUID ERC infusion. Advise patients and/or caregivers to seek immediate medical evaluation if any signs and symptoms of hemolysis occur such as increased heart rate, fatigue, yellowing of the skin or eyes, and dark-colored urine [see Warnings and Precautions (5.6)].
- Transfusion-Related Acute Lung Injury (TRALI): Inform patients and/or caregivers that TRALI may occur 1 to 6 hours after GAMMAGARD LIQUID ERC infusion. Advise patients and/or caregivers to seek immediate medical evaluation if any signs and symptoms of TRALI occur such as trouble breathing, chest pain, blue lips or extremities, or fever [see Warnings and Precautions (5.7)].
- Transmission of Infectious Agents: Inform patients and/or caregivers that GAMMAGARD LIQUID ERC is made from human plasma and may contain infectious agents that can cause disease (e.g., viruses and, theoretically, the vCJD agent). The risk of GAMMAGARD LIQUID ERC transmitting an infectious agent has been reduced by screening plasma donors for prior exposure, testing donated plasma, and inactivating or removing certain viruses during manufacturing. Patients should report any symptoms that concern them which might be caused by virus infections [see Warnings and Precautions (5.8)].
- Drug Interactions: Inform patients that GAMMAGARD LIQUID ERC can interfere with their immune response to live viral vaccines such as measles, mumps, rubella and varicella, and instruct patients to notify their healthcare professional of this potential interaction when they are receiving vaccinations [see Drug Interactions (7)].
Subcutaneous Administration Only
For self-administration provide clear instructions and training on SC infusion to the patient/caregiver and document the demonstration of their ability to independently administer SC infusions.
- Patients with a history of allergic reactions should not be treated subcutaneously at home until 2 to 3 treatments have been administered and tolerated under medical supervision.
- Ensure the patient understands the importance of consistent weekly SC infusion to maintain appropriate steady IgG levels.
- Instruct the patient to keep a treatment diary/logbook. This diary/logbook should include information about each infusion such as, the time, date, dose, lot number(s) and any reactions.
- Inform the patient that mild to moderate local infusion site reactions (e.g., swelling and redness) are a common side effect of SC treatment, but contact their healthcare professional if a local reaction increases in severity or persists for more than a few days.
Manufactured by:
Takeda Pharmaceuticals U.S.A., Inc.
Cambridge, MA 02142U.S. License Number: 1898
GAMMAGARD and GAMMAGARD LIQUID are registered trademarks of Baxalta Incorporated.
TAKEDA and
 are registered trademarks of Takeda Pharmaceutical Company Limited.
are registered trademarks of Takeda Pharmaceutical Company Limited.©2025 Takeda Pharmaceuticals U.S.A., Inc. All rights reserved.
GLQ 381 R1
-
PATIENT PACKAGE INSERT
PATIENT INFORMATION
GAMMAGARD LIQUID ERC
Immune Globulin Infusion (Human)
10% solution for intravenous or subcutaneous useThis Patient Information has been approved by the U.S. Food and Drug Administration.
Issued: 10/2025
GLQ 381 R1What is the most important information I need to know about GAMMAGARD LIQUID ERC?
GAMMAGARD LIQUID ERC can cause the following serious reactions:- Severe allergic reactions causing difficulty in breathing or skin rashes
- Decreased kidney function or kidney failure
- Blood clots in the heart, brain, lungs or elsewhere in the body
- Severe headache, drowsiness, fever, painful eye movements, or nausea and vomiting
- Dark colored urine, swelling, fatigue, or difficulty breathing
What is GAMMAGARD LIQUID ERC?
GAMMAGARD LIQUID ERC is a single-dose, liquid medicine that contains immunoglobulin G (Human) (IgG) antibodies, which protect the body against infection. GAMMAGARD LIQUID ERC is used to treat the following conditions:
Primary Immunodeficiency Diseases: There are many forms of PI. The most common types of PI result in an inability to make a very important type of protein called antibodies, which help the body fight off infections from bacteria or viruses. GAMMAGARD LIQUID ERC is made from human plasma that is donated by healthy people. GAMMAGARD LIQUID ERC contains antibodies collected from these healthy people that replace the missing antibodies in PI patients.Who should not use GAMMAGARD LIQUID ERC?
Do not use GAMMAGARD LIQUID ERC if you have a known history of a severe allergic reaction to immune globulin or other blood products. If you have such a history, discuss this with your healthcare provider to determine if GAMMAGARD LIQUID ERC can be given to you.How should I use GAMMAGARD LIQUID ERC?
GAMMAGARD LIQUID ERC is given into a vein (intravenously) or under the skin (subcutaneously). For patients with PI, infusions into the vein are usually given every 3 or 4 weeks whereas infusions under the skin are given every week. You and your healthcare provider will decide which way is best for you. Most of the time infusions under the skin are given at home by patients or caregivers. Although it is possible to give yourself infusions into the vein at home they are more often given in a hospital or infusion center by a nurse.
Instructions for giving GAMMAGARD LIQUID ERC under the skin (subcutaneously) are provided in the Instructions for Use brochure. Only use GAMMAGARD LIQUID ERC by yourself after you have been instructed by your healthcare provider.What should I avoid while taking GAMMAGARD LIQUID ERC?
GAMMAGARD LIQUID ERC can make vaccines (like measles/mumps/rubella or chickenpox vaccines) not work as well for you. Before you get any vaccines, tell your healthcare provider that you take GAMMAGARD LIQUID ERC.
Tell your healthcare provider if you are pregnant, or plan to become pregnant, or if you are nursing.What are the possible or reasonably likely side effects of GAMMAGARD LIQUID ERC?
The following one or more possible reactions may occur at the site of infusion. These generally go away within a few hours and are less likely after the first few infusions.- Mild or moderate pain
- Swelling
- Itching
- Rash
- Redness
- Bruising
- Warmth
- Bleeding
During the infusion of GAMMAGARD LIQUID ERC, look out for the first signs of the following common side effects: - Headache
- Migraine
- Fever
- Fatigue
- Itching
- Rash/Hives
- Cough
- Chest pain/tightness
- Pain in extremity
- Diarrhea
- Infusion site leakage
- Joint pain
- Chills/Shaking chills
- Dizziness
- Nausea/Vomiting
- Faster heart rate
- Upper abdominal pain
- Increased blood pressure
- Muscle cramps
- Sore throat
- Heart murmur
- Asthma
- Ear pain
- Mouth ulcer/sore
If any of the following problems occur after starting treatment with GAMMAGARD LIQUID ERC, stop the infusion immediately and contact your healthcare provider or call emergency services. These could be signs of a serious problem. - Hives, swelling in the mouth or throat, itching, trouble breathing, wheezing, fainting or dizziness. These could be signs of a serious allergic reaction.
- Bad headache with nausea, vomiting, stiff neck, fever, and sensitivity to light. These could be signs of irritation of the lining around your brain.
- Reduced urination, sudden weight gain, or swelling in your legs. These could be signs of a kidney problem.
- Pain, swelling, warmth, redness, or a lump in your legs or arms. These could be signs of blood clots.
- Brown or red urine, fast heart rate, yellow skin or eyes. These could be signs of a liver problem or a blood problem.
- Chest pain or trouble breathing, or blue lips or extremities. These could be signs of a serious heart or lung problem.
- Fever over 100°F. This could be a sign of an infection.
Whenever giving yourself treatment at home, you should have another responsible person present to help treat side effects or get help if you have a serious adverse reaction occur. Ask your healthcare provider whether you should have rescue medications, such as antihistamines or epinephrine.
Call your healthcare provider for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.How do I store GAMMAGARD LIQUID ERC?
Store vials in their original boxes to protect them from light. Do not freeze GAMMAGARD LIQUID ERC.
You can store GAMMAGARD LIQUID ERC in the refrigerator or at room temperature. The maximum storage time for GAMMAGARD LIQUID ERC depends on the storage temperature you choose.
Refrigerator Temperature: at 2° to 8°C (36° to 46°F) for up to 36 months.
Room Temperature: up to 25°C (77°F) for up to 24 months.
The refrigerator and room temperature expiration dates are printed on the vial labels and the box. Always check the expiration date. You should not use the product after the expiration date.
Note: If you remove GAMMAGARD LIQUID ERC from the refrigerator and store it at room temperature, do not refrigerate again.General information about the safe and effective use of GAMMAGARD LIQUID ERC.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet.
Do not use GAMMAGARD LIQUID ERC for a condition for which it was not prescribed. Do not give GAMMAGARD LIQUID ERC to other people, even if they have the same symptoms you have. It may harm them.
This Patient Information leaflet summarizes the most important information about GAMMAGARD LIQUID ERC. If you would like more information, talk to your doctor. You can ask your pharmacist or doctor for information about GAMMAGARD LIQUID ERC that is written for health professionals.What are the ingredients in GAMMAGARD LIQUID ERC?
Active ingredients: Human normal immunoglobulin 10% solution with less than or equal to 2 µg/mL immunoglobulin A (IgA).
Inactive ingredients: Glycine, Water for Injection, Hydrochloric acid.Manufactured by:
Takeda Pharmaceuticals U.S.A., Inc.
Cambridge, MA 02142
U.S. License Number: 1898
GAMMAGARD and GAMMAGARD LIQUID are registered trademarks of Baxalta Incorporated.
TAKEDA and
 are registered trademarks of Takeda Pharmaceutical Company Limited.
are registered trademarks of Takeda Pharmaceutical Company Limited.
©2025 Takeda Pharmaceuticals U.S.A., Inc. All rights reserved.
For more information about GAMMAGARD LIQUID ERC call Takeda Pharmaceuticals U.S.A., Inc. at
1-877-TAKEDA-7 (1-877-825-3327). -
INSTRUCTIONS FOR USE
INSTRUCTIONS FOR USE
GAMMAGARD LIQUID ERC
Immune Globulin Infusion (Human)
10% solution for subcutaneous useThis "Instructions for Use" contains information on how to infuse GAMMAGARD LIQUID ERC
Important Information You Need to Know Before Preparing and Infusing GAMMAGARD LIQUID ERC
Do not use GAMMAGARD LIQUID ERC at home until you get instructions and training from your healthcare professional.
Preparing for your Infusion
Step 1 Prepare for your Infusion
Before you start- Find a quiet work area with as few distractions as possible.
- Clean a work area with an antibacterial cleaner.
- Remove GAMMAGARD LIQUID ERC from the refrigerator and take the vial out of the box.
- Allow vials to reach room temperature. This may take up to 60 minutes.
- Do not apply heat or place it in the microwave.
- Do not shake the vial(s).
- Take the vial out of the box, if stored at room temperature.
- Do not shake the vial(s).
Gather your supplies (Figure 1)
Collect all the items you will need for the infusion- Vial(s) of GAMMAGARD LIQUID ERC
- Infusion supplies
- Infusion pump
- Needle sets
- Transfer needles
- Alcohol swabs
- Syringes
- Gauze and tape
- Sharps container
- Treatment logbook

Figure 1Step 2 Wash your hands (Figure 2) - Wash your hands thoroughly.
- Put on clean gloves if your healthcare provider has instructed you to wear them.
Figure 2Step 3 Check the vial and liquid - Remove the vial from the box. Carefully look at the liquid in the vial of GAMMAGARD LIQUID ERC.
- GAMMAGARD LIQUID ERC is a clear, colorless to slightly yellowish liquid. Check for particles or color changes.
-
Do not use the vial if:
- The liquid looks cloudy, contains particles, or is dark yellow.
- The protective flip cap is missing or damaged.
- The expiration date on the label has passed.
Step 4 Vial(s) preparation 
Figure 3

Figure 4Step 5 Fill syringe from GAMMAGARD LIQUID ERC vial(s) - Remove sterile syringe from package and attach to a sterile needle.
- Pull back on plunger of the syringe to fill it with air, which should equal the amount of liquid you will be taking from the vial.
- Insert the needle into the center of the vial stopper. Inject air into the vial and withdraw GAMMAGARD LIQUID ERC into the syringe. (Example: If you withdraw 50 mL of GAMMAGARD LIQUID ERC, inject 50 mL of air into the vial). (Figure 5)
- If using a vented spike:
- It is not necessary to inject air into the vial with the syringe.
- Attach a sterile syringe to the spike, insert the spike into the center of the stopper, and pull back on the plunger to withdraw the desired volume.
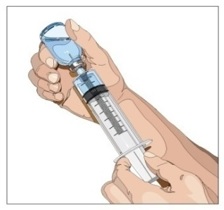
Figure 5Step 6 Prepare the infusion pump and tubing
- If you use a syringe driver pump, attach the syringe filled with GAMMAGARD LIQUID ERC to the needle set. On a hard surface, gently push down on the plunger to fill (prime) the pump tubing up to the needle hub. This will ensure that no air is left in the tubing and needle. (Figure 6)
- If using a portable pump with GAMMAGARD LIQUID ERC in a bag, follow manufacturer's instructions for preparing the pump and administration tubing, if needed.

Figure 6Infusing of GAMMAGARD LIQUID ERC
Step 7 Prepare the infusion site - Choose an infusion site(s): upper arms, abdomen, thighs, and lower back. (Figure 7, Figure 8)
- Make sure the sites are at least 2 inches apart.
- Avoid bony areas, visible blood vessels, scars and areas of inflammation (irritation) or infection.
- Select the number of infusion sites based on the volume of the total dose. It is recommended that you not inject more than 20 mL for children and 30 mL for adults into each infusion site.
- Rotate sites by choosing opposite sides of the body between future infusions.
- Wipe the infusion site(s) with a sterile alcohol wipe beginning at the center of each infusion site and moving outward in a circular motion.
- Allow the infusion site(s) to dry (at least 30 seconds). (Figure 9)
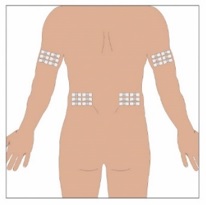
Figure 7
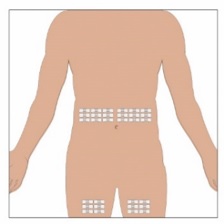
Figure 8
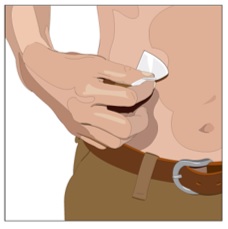
Figure 9Step 8 Insert the needle (Figure 10) - Remove the needle cover.
- Firmly grasp skin and pinch at least one inch of skin between two fingers.
- Insert needle with a rapid motion straight into the skin at a 90-degree angle. Tape the needle in place with sterile tape.
- Repeat this step for each infusion site.
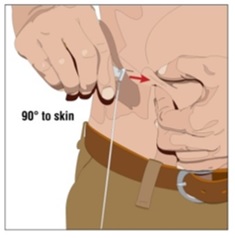
Figure 10Step 9 Check for proper needle placement - Before starting the infusion, check each needle for correct placement by gently pulling back on the attached syringe plunger and looking for any blood in the needle tubing. (Figure 11)
- If you see any blood, remove and throw away the needle into the Sharps container. Repeat filling (priming) and needle insertion steps in a different infusion site with a new needle.
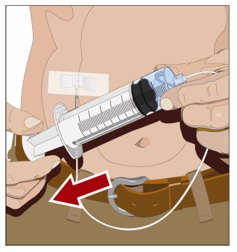
Figure 11Step 10 Secure the needle to the skin and start infusion - Secure the needle(s) in place by putting a sterile clear bandage over the needle. (Figure 12)
- Follow the manufacturer's instructions to turn pump on. Check infusion sites occasionally throughout the infusion.
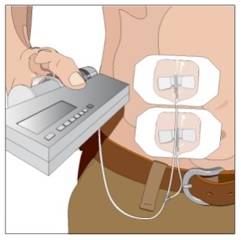
Figure 12Step 11 Remove needle set - After the infusion is complete, remove the needle set by pulling it straight out. Gently press a small piece of gauze over the needle site and cover with a protective dressing. (Figure 13)
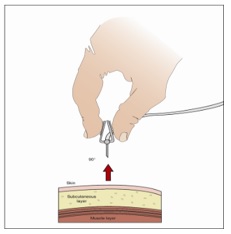
Figure 13Step 12 Record the infusion
- Remove the peel-off label from GAMMAGARD LIQUID ERC vial, which has the product lot number and expiration date, and place the label in your treatment diary/logbook. Write down the date, time, dose, and any reactions after each infusion.
Storing GAMMAGARD LIQUID ERC
Store vials in their original boxes to protect them from light. Do not freeze GAMMAGARD LIQUID ERC.
You can store GAMMAGARD LIQUID ERC in the refrigerator or at room temperature. The maximum storage time for GAMMAGARD LIQUID ERC depends on the storage temperature you choose.
Refrigerator Temperature: at 2° to 8°C (36° to 46°F) for up to 36 months.
Room Temperature: up to 25°C (77°F) for up to 24 months.
The refrigerator and room temperature expiration dates are printed on the vial labels and the box. Always check the expiration date. You should not use the product after the expiration date.
Note: If you remove GAMMAGARD LIQUID ERC from the refrigerator and store it at room temperature, do not refrigerate again.
Disposing of GAMMAGARD LIQUID ERC
Throw away any unused product in the vial(s) and the disposable supplies into the Sharps container. Dispose of the Sharps container using instructions provided with the container or contact your healthcare provider.
For more information about GAMMAGARD LIQUID ERC, including the current Prescribing Information, call Takeda Pharmaceuticals U.S.A., Inc. at 1-877-TAKEDA-7 (1-877-825-3327).
Manufactured by:
Takeda Pharmaceuticals U.S.A., Inc.
Cambridge, MA 02142U.S. License Number: 1898
GAMMAGARD and GAMMAGARD LIQUID are registered trademarks of Baxalta Incorporated.
TAKEDA and
 are registered trademarks of Takeda Pharmaceutical Company Limited.
are registered trademarks of Takeda Pharmaceutical Company Limited.©2025 Takeda Pharmaceuticals U.S.A., Inc. All rights reserved.
This Instructions for Use document has been approved by the U.S. Food and Drug Administration.
Issued: 10/2025
GLQ 381 R1
-
PRINCIPAL DISPLAY PANEL - 50 mL Bottle Label
NDC: 0944-2705-05 Single-dose vial
Immune Globulin Infusion (Human)
GAMMAGARD LIQUID ERC
10% Solution for Infusion
Less than or equal to 2 µg/mL IgA5 g
50 mLFor Intravenous or Subcutaneous Administration.
Not made with natural rubber latex.
Refrigeration: 2° to 8°C (36° to 46°F).
Do not freeze.
Room Temperature: up to 25°C (77°F).Takeda Pharmaceuticals
U.S.A., Inc.
Cambridge, MA 02142
U.S. License No. 1898Rx Only
LE-07-59902
Takeda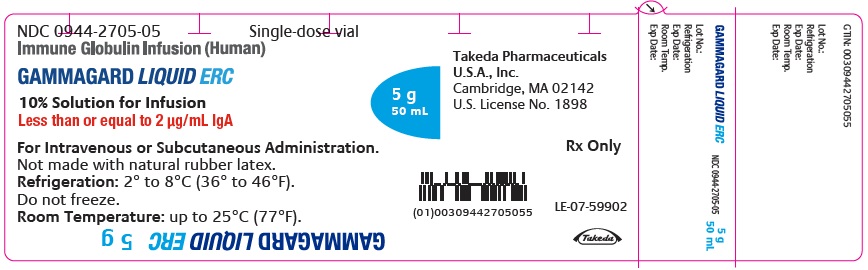
-
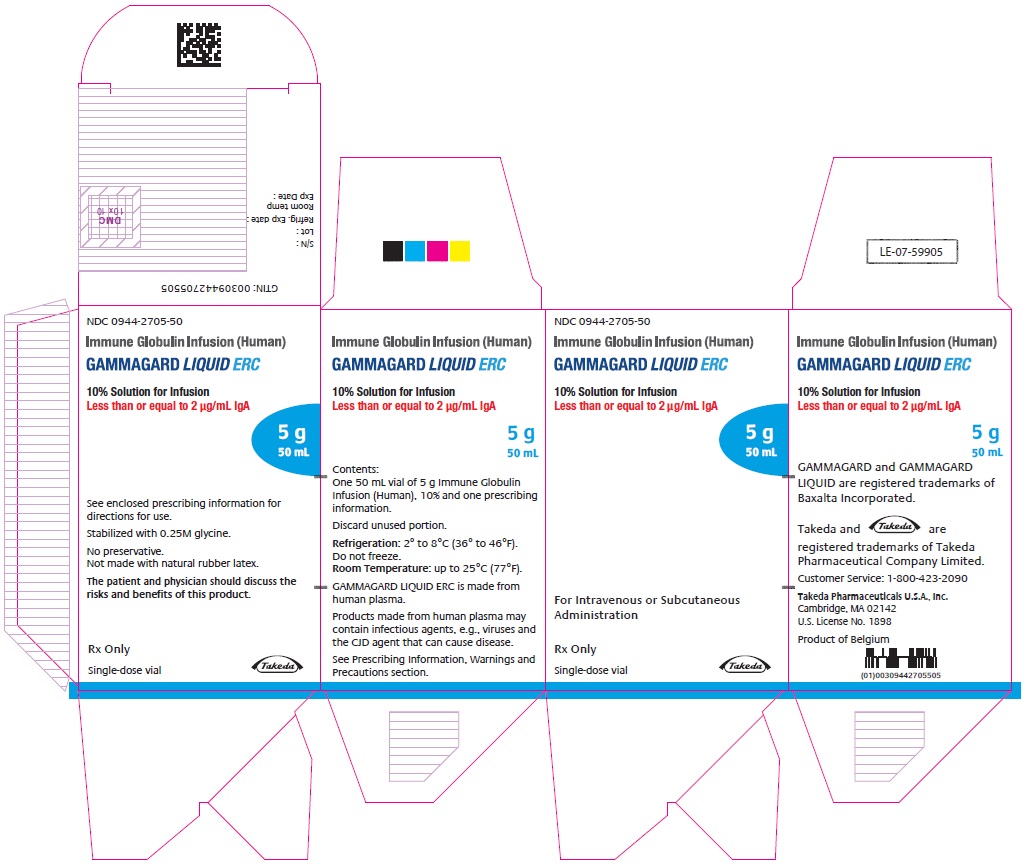
PRINCIPAL DISPLAY PANEL - 50 mL Bottle Carton
NDC: 0944-2705-50
Immune Globulin Infusion (Human)
GAMMAGARD LIQUID ERC
10% Solution for Infusion
Less than or equal to 2 µg/mL IgA5 g
50 mLFor Intravenous or Subcutaneous
AdministrationRx Only
Single-dose vial
Takeda
-
PRINCIPAL DISPLAY PANEL - 100 mL Bottle Label
NDC: 0944-2705-01 Single-dose vial
Immune Globulin Infusion (Human)
GAMMAGARD LIQUID ERC
10% Solution for Infusion
Less than or equal to 2 µg/mL IgA10 g
100 mLFor Intravenous or Subcutaneous Administration.
Not made with natural rubber latex.
Refrigeration: 2° to 8°C (36° to 46°F).
Do not freeze.
Room Temperature: up to 25°C (77°F).GTIN: 00309442705017
Takeda Pharmaceuticals
U.S.A., Inc.
Cambridge, MA 02142
U.S. License No. 1898Rx Only
LE-07-59906
Takeda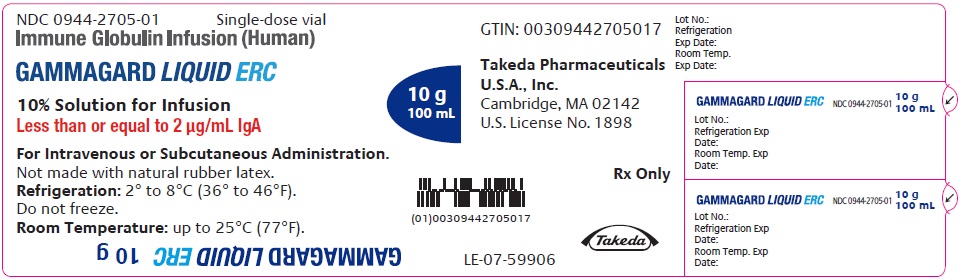
-
PRINCIPAL DISPLAY PANEL - 100 mL Bottle Carton
NDC: 0944-2705-10
Immune Globulin Infusion (Human)
GAMMAGARD LIQUID ERC
10% Solution for Infusion
Less than or equal to 2 µg/mL IgA10 g
100 mLSee enclosed prescribing
information for directions for use.Stabilized with 0.25M glycine.
No preservative.
Not made with natural rubber latex.The patient and physician should discuss
the risks and benefits of this product.Rx Only
Single-dose vial
Takeda
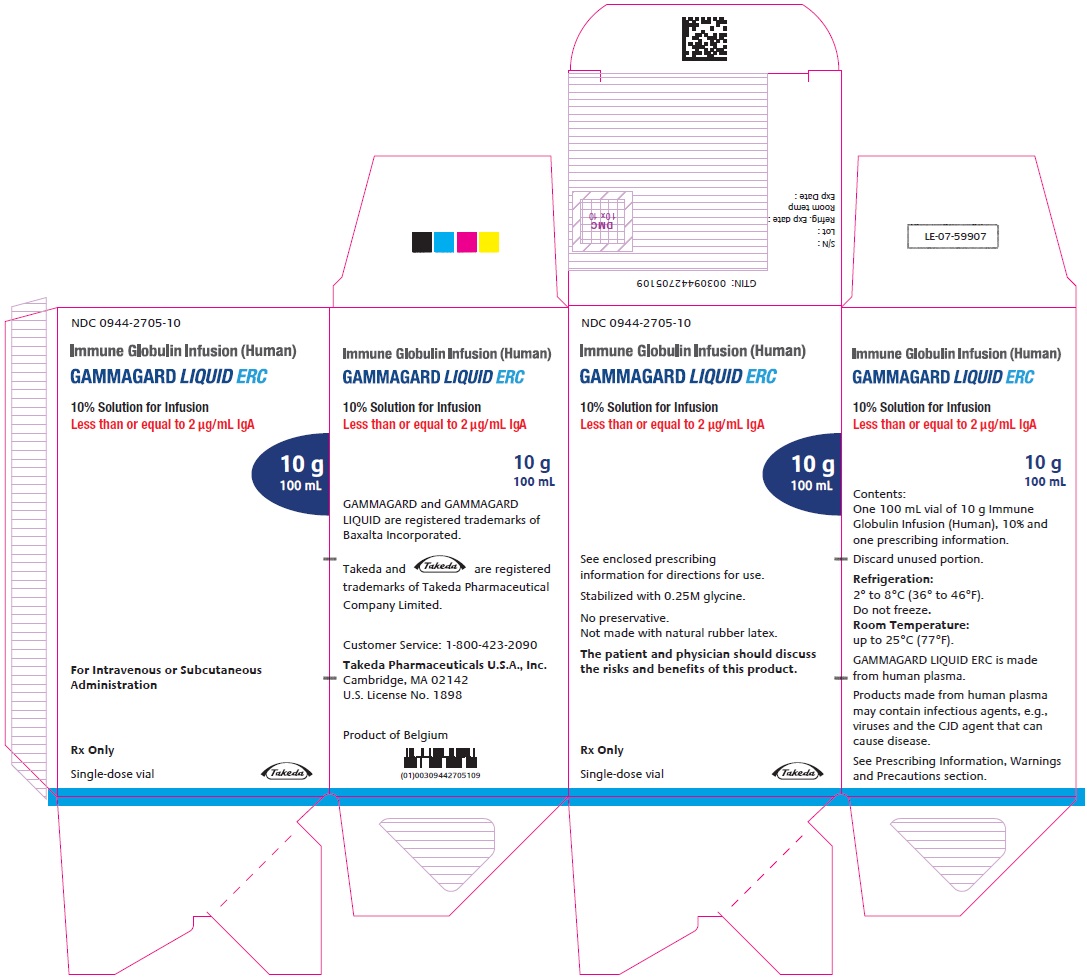
-
INGREDIENTS AND APPEARANCE
GAMMAGARD LIQUID ERC
immune globulin infusion (human) injection, solutionProduct Information Product Type PLASMA DERIVATIVE Item Code (Source) NDC: 0944-2705 Route of Administration INTRAVENOUS, SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength HUMAN IMMUNOGLOBULIN G (UNII: 66Y330CJHS) (HUMAN IMMUNOGLOBULIN G - UNII:66Y330CJHS) HUMAN IMMUNOGLOBULIN G 100 mg in 1 mL Inactive Ingredients Ingredient Name Strength GLYCINE (UNII: TE7660XO1C) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0944-2705-50 1 in 1 CARTON 1 NDC: 0944-2705-05 50 mL in 1 VIAL, GLASS; Type 0: Not a Combination Product 2 NDC: 0944-2705-10 1 in 1 CARTON 2 NDC: 0944-2705-01 100 mL in 1 VIAL, GLASS; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125105 07/14/2025 Labeler - Takeda Pharmaceuticals America, Inc. (039997266) Establishment Name Address ID/FEI Business Operations Baxalta Belgium Manufacturing SA 370634700 MANUFACTURE(0944-2705) , ANALYSIS(0944-2705) , API MANUFACTURE(0944-2705) , LABEL(0944-2705) , PACK(0944-2705)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.