These highlights do not include all the information needed to use ANECTINE safely and effectively. See full prescribing information for ANECTINE NOV. ANECTINE ®(succinylcholine chloride) injection, for intravenous or intramuscular use Initial U.S. Approval: 1952
ANECTINE NOV by
Drug Labeling and Warnings
ANECTINE NOV by is a Prescription medication manufactured, distributed, or labeled by Delpharm Boucherville Canada Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
ANECTINE NOV- succinylcholine chloride injection, solution
Delpharm Boucherville Canada Inc.
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use ANECTINE safely and effectively. See full prescribing information for ANECTINE NOV. ANECTINE
®(succinylcholine chloride) injection, for intravenous or intramuscular use
Initial U.S. Approval: 1952
WARNING
|
FULL PRESCRIBING INFORMATION: CONTENTS*WARNING: RISK OF VENTRICULAR DYSRHYTHMIAS, CARDIAC ARREST AND DEATH FROM HYPERKALEMIC RHABDOMYOLYSIS IN PEDIATRIC PATIENTSDESCRIPTIONCLINICAL PHARMACOLOGYPharmacogenomicsINDICATIONS AND USAGECONTRAINDICATIONSWARNINGSAnaphylaxisHyperkalemiaMalignant HyperthermiaOtherReduced Plasma Cholinesterase ActivityDrug InteractionsPregnancyADVERSE REACTIONSOVERDOSAGEDOSAGE AND ADMINISTRATIONPediatricsHOW SUPPLIED |
FULL PRESCRIBING INFORMATION
WARNING: RISK OF VENTRICULAR DYSRHYTHMIAS, CARDIAC ARREST AND DEATH FROM HYPERKALEMIC RHABDOMYOLYSIS IN PEDIATRIC PATIENTS
This drug should be used only by individuals familiar with its actions, characteristics, and hazards.
DESCRIPTION
ANECTINE (succinylcholine chloride) is an ultra short-acting depolarizingtype, skeletal muscle relaxant for intravenous (IV) administration.
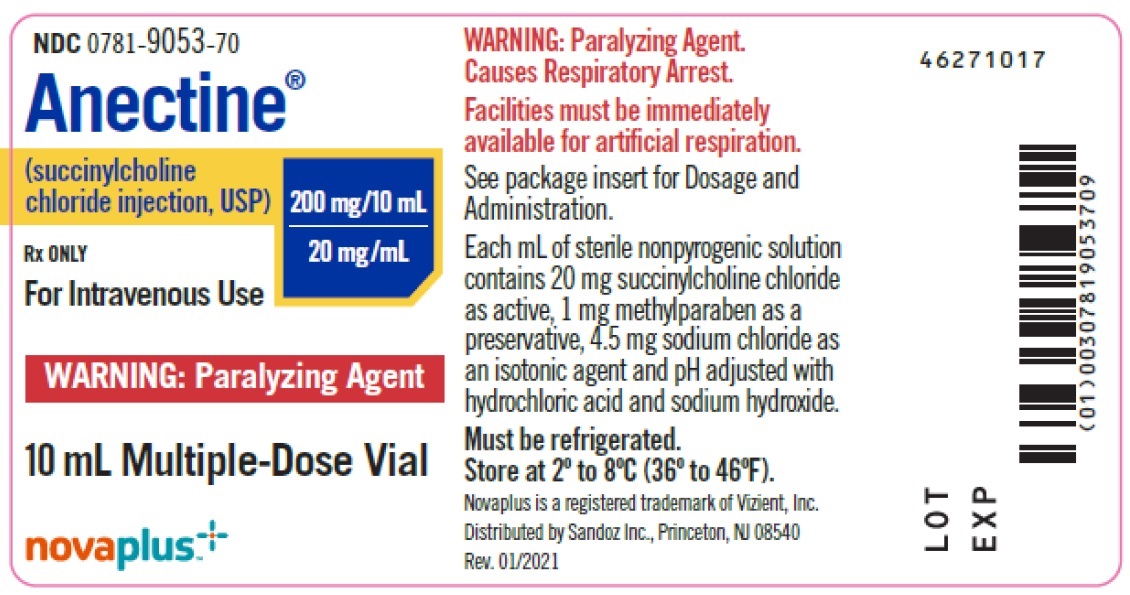
Succinylcholine chloride is a white, odorless, slightly bitter powder and very soluble in water. The drug is unstable in alkaline solutions but relatively stable in acid solutions, depending upon the concentration of the solution and the storage temperature. Solutions of succinylcholine chloride should be stored under refrigeration to preserve potency. ANECTINE injection is a sterile nonpyrogenic solution for intravenous injection where each mL contains 20 mg succinylcholine chloride as active, 1 mg methylparaben as a preservative, 4.5 mg sodium chloride as an isotonic agent and pH adjusted to 3.5 with hydrochloric acid and sodium hydroxide.
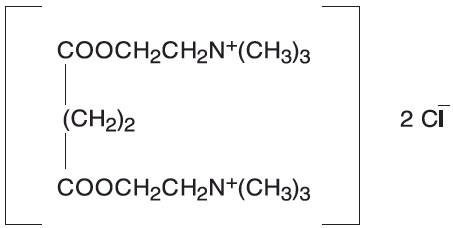
The chemical name for succinylcholine chloride is 2,2’-[(1,4-dioxo-1,4- butanediyl)bis(oxy)]bis[N,N,N-trimethylethanaminium] dichloride, and the structural formula is:
CLINICAL PHARMACOLOGY
Succinylcholine is a depolarizing skeletal muscle relaxant. As does acetylcholine, it combines with the cholinergic receptors of the motor end plate to produce depolarization. This depolarization may be observed as fasciculations. Subsequent neuromuscular transmission is inhibited so long as adequate concentration of succinylcholine remains at the receptor site. Onset of flaccid paralysis is rapid (less than 1 minute after IV administration), and with single administration lasts approximately 4 to 6 minutes.
Succinylcholine is rapidly hydrolyzed by plasma cholinesterase to succinylmonocholine (which possesses clinically insignificant depolarizing muscle relaxant properties) and then more slowly to succinic acid and choline (see PRECAUTIONS). About 10% of the drug is excreted unchanged in the urine. The paralysis following administration of muscles. This initially involves consecutively the levator muscles of the face, muscles of the glottis, and finally, the intercostals and the diaphragm and all other skeletal muscles.
Succinylcholine has no direct action on the uterus or other smooth muscle structures. Because it is highly ionized and has low fat solubility, it does not readily cross the placenta.
Tachyphylaxis occurs with repeated administration (see
PRECAUTIONS).
Depending on the dose and duration of succinylcholine administration, the characteristic depolarizing neuromuscular block (Phase I block) may change to a block with characteristics superficially resembling a nondepolarizing block (Phase II block). This may be associated with prolonged respiratory muscle paralysis or weakness in patients who manifest the transition to Phase II block. When this diagnosis is confirmed by peripheral nerve stimulation, it may sometimes be reversed with anticholinesterase drugs such as neostigmine (see PRECAUTIONS). Anticholinesterase drugs may not always be effective. If given before succinylcholine is metabolized by cholinesterase, anticholinesterase drugs may prolong rather than shorten paralysis.
Succinylcholine has no direct effect on the myocardium. Succinylcholine stimulates both autonomic ganglia and muscarinic receptors which may
cause changes in cardiac rhythm, including cardiac arrest. Changes in rhythm, including cardiac arrest, may also result from vagal stimulation, which may occur during surgical procedures, or from hyperkalemia, particularly in pediatric patients (see PRECAUTIONS: Pediatric Use). These effects are enhanced by halogenated anesthetics.
Succinylcholine causes an increase in intraocular pressure immediately after its injection and during the fasciculation phase, and slight increases
which may persist after onset of complete paralysis (see WARNINGS). Succinylcholine may cause slight increases in intracranial pressure
immediately after its injection and during the fasciculation phase (see
PRECAUTIONS).
As with other neuromuscular blocking agents, the potential for releasing histamine is present following succinylcholine administration. Signs and
symptoms of histamine-mediated release such as flushing, hypotension, and bronchoconstriction are, however, uncommon in normal clinical usage.
Succinylcholine has no effect on consciousness, pain threshold, or cerebration. It should be used only with adequate anesthesia (see
WARNINGS).
Pharmacogenomics
RYR1 and CACNA1S are polymorphic genes, and multiple pathogenic variants have been associated with malignant hyperthermia susceptibility (MHS) in patients receiving succinylcholine, including Anectine. Case reports as well as ex-vivo studies have identified multiple variants in RYR1 and CACNA1S associated with MHS. Variant pathogenicity should be assessed based on prior clinical experience, functional studies, prevalence information, or other evidence (see CONTRAINDICATIONS, WARNINGS).
INDICATIONS AND USAGE
Succinylcholine chloride is indicated as an adjunct to general anesthesia, to facilitate tracheal intubation, and to provide skeletal muscle relaxation during surgery or mechanical ventilation.
CONTRAINDICATIONS
ANECTINE is contraindicated in patients with:
Known or suspected genetic susceptibility to malignant hyperthermia (see
WARNINGS; Malignant Hyperthermia, CLINICAL PHARMACOLOGY;
Pharmacogenomics)
Skeletal muscle myopathies
Known hypersensitivity to succinylcholine (see WARNINGS; Anaphylaxis)
After the acute phase of injury following major burns, multiple trauma, extensive denervation of the skeletal muscle, or upper neuron injury because succinylcholine administered to such individuals may result in severe hyperkalemia, which may result in cardiac arrest (see
WARNINGS; Hyperkalemia)
WARNINGS
Succinylcholine should be used only by those skilled in the management of artificial respiration and only when facilities are instantly available for tracheal intubation and for providing adequate ventilation of the patient, including the administration of oxygen under positive pressure and the elimination of carbon dioxide. The clinician must be prepared to assist or control respiration.
To avoid distress to the patient, succinylcholine should not be administered before unconsciousness has been induced. In emergency situations, however, it may be necessary to administer succinylcholine before unconsciousness is induced.
Succinylcholine is metabolized by plasma cholinesterase and should be used with caution, if at all, in patients known to be or suspected of being homozygous for the atypical plasma cholinesterase gene.
Anaphylaxis
Severe anaphylactic reactions to neuromuscular blocking agents, including ANECTINE, have been reported. These reactions have in some cases been life-threatening and fatal. Due to the potential severity of these reactions, the necessary precautions, such as the immediate availability of appropriate emergency treatment, should be taken. Precautions should also be taken in those individuals who have had previous anaphylactic reactions to other neuromuscular blocking agents since cross-reactivity between neuromuscular blocking agents, both depolarizing and non-depolarizing, has been reported in this class of drugs.
Risk of Death due to Medication Errors
Administration of ANECTINE results in paralysis, which may lead to respiratory arrest and death; this progression may be more likely to occur in a patient for whom it is not intended. Confirm proper selection of intended product and avoid confusion with other injectable solutions that are present in critical care and other clinical settings. If another healthcare provider is administering the product, ensure that the intended dose is clearly labeled and communicated.
Hyperkalemia
(SEE BOX WARNING.)Succinylcholine should be administered with GREAT CAUTIONto patients suffering from electrolyte abnormalities and those who may have massive digitalis toxicity, because in these circumstances succinylcholine may induce serious cardiac arrhythmias or cardiac arrest due to hyperkalemia.
GREAT CAUTIONshould be observed if succinylcholine is administered to patients during the acute phase of injury following major burns, multiple trauma, extensive denervation of skeletal muscle, or upper motor neuron injury (see CONTRAINDICATIONS). The risk of hyperkalemia in these patients increases over time and usually peaks at 7 to 10 days after the injury. The risk is dependent on the extent and location of the injury. The precise time of onset and the duration of the risk period are undetermined. Patients with chronic abdominal infection, subarachnoid hemorrhage, or conditions causing degeneration of central and peripheral nervous systems should receive succinylcholine with GREAT CAUTIONbecause of the potential for developing severe hyperkalemia.
Malignant Hyperthermia
In susceptible individuals, succinylcholine may trigger malignant hyperthermia, a skeletal muscle hypermetabolic state leading to high oxygen demand. Fatal outcomes of malignant hyperthermia have been reported.
The risk of developing malignant hyperthermia increases with the concomitant administration of succinylcholine and volatile anesthetic agents. Anectine can induce malignant hyperthermia in patients with known or suspected susceptibility based on genetic factors or family history, including those with certain inherited ryanodine receptor (RYR1) or dihydropyridine receptor (CACNA1S) variants. (see CONTRAINDICATIONS, CLINICAL PHARMACOLOGY; Pharmacogenomics)
Signs consistent with malignant hyperthermia may include hyperthermia, hypoxia, hypercapnia, muscle rigidity (e.g., jaw muscle spasm), tachycardia (e.g., particularly that unresponsive to deepening anesthesia or analgesic medication administration), tachypnea, cyanosis, arrhythmias, hypovolemia, and hemodynamic instability. Skin mottling, coagulopathies, and renal failure may occur later in the course of the hypermetabolic process.
Successful treatment of malignant hyperthermia depends on early recognition of the clinical signs. If malignant hyperthermia is suspected, discontinue all triggering agents (i.e., volatile anesthetic agents and succinylcholine), administer intravenous dantrolene sodium, and initiate supportive therapies. Consult prescribing information for intravenous dantrolene sodium for additional information on patient management. Supportive therapies include administration of supplemental oxygen and respiratory support based on clinical need, maintenance of hemodynamic stability and adequate urinary output, management of fluid and electrolyte balance, correction of acid base derangements, and institution of measures to control rising temperature.
Other
In both adults and pediatric patients, the incidence of bradycardia, which may progress to asystole, is higher following a second dose of succinylcholine. The incidence and severity of bradycardia is higher in pediatric patients than in adults. Pretreatment with anticholinergic agents (e.g., atropine) may reduce the occurrence of bradyarrhythmias.
Succinylcholine causes an increase in intraocular pressure. It should not be used in instances in which an increase in intraocular pressure is undesirable (e.g., narrow angle glaucoma, penetrating eye injury) unless the potential benefit of its use outweighs the potential risk.
Succinylcholine is acidic (pH=3.5) and should not be mixed with alkaline solutions having a pH greater than 8.5 (e.g., barbiturate solutions).
(SEE BOX WARNING.)
General
When succinylcholine is given over a prolonged period of time, the characteristic depolarization block of the myoneural junction (Phase I block) may change to a block with characteristics superficially resembling a nondepolarizing block (Phase II block). Prolonged respiratory muscle paralysis or weakness may be observed in patients manifesting this transition to Phase II block. The transition from Phase I to Phase II block has been reported in seven of seven patients studied under halothane anesthesia after an accumulated dose of 2 to 4 mg/kg succinylcholine (administered in repeated, divided doses). The onset of Phase II block coincided with the onset of tachyphylaxis and prolongation of spontaneous recovery. In another study, using balanced anesthesia (N2O/O2/narcoticthiopental) and succinylcholine infusion, the transition was less abrupt, with great individual variability in the dose of succinylcholine required to produce Phase II block. Of 32 patients studied, 24 developed Phase II block. Tachyphylaxis was not associated with the transition to Phase II block, and 50% of the patients who developed Phase II block experienced prolonged recovery.
When Phase II block is suspected in cases of prolonged neuromuscular blockade, positive diagnosis should be made by peripheral nerve stimulation prior to administration of any anticholinesterase drug. Reversal of Phase II block is a medical decision which must be made upon the basis of the individual, clinical pharmacology, and the experience and judgment of the physician. The presence of Phase II block is indicated by fade of responses to successive stimuli (preferably “train-of-four”). The use of an anticholinesterase drug to reverse Phase II block should be accompanied by appropriate doses of an anticholinergic drug to prevent disturbances of cardiac rhythm. After adequate reversal of Phase II block with an anticholinesterase agent, the patient should be continually observed for at least 1 hour for signs of return of muscle relaxation. Reversal should not be attempted unless: (1) a peripheral nerve stimulator is used to determine the presence of Phase II block (since anticholinesterase agents will potentiate succinylcholine-induced Phase I block), and (2) spontaneous recovery of muscle twitch has been observed for at least 20 minutes and has reached a plateau with further recovery proceeding slowly; this delay is to ensure complete hydrolysis of succinylcholine by plasma cholinesterase prior to administration of the anticholinesterase agent. Should the type of block be misdiagnosed, depolarization of the type initially induced by succinylcholine (i.e., Phase I block) will be prolonged by an anticholinesterase agent.
Succinylcholine should be employed with caution in patients with fractures or muscle spasm because the initial muscle fasciculations may cause additional trauma.
Succinylcholine may cause a transient increase in intracranial pressure; however, adequate anesthetic induction prior to administration of succinylcholine will minimize this effect.
Succinylcholine may increase intragastric pressure, which could result in regurgitation and possible aspiration of stomach contents.
Neuromuscular blockade may be prolonged in patients with hypokalemia or hypocalcemia.
Since allergic cross-reactivity has been reported in this class, request information from your patients about previous anaphylactic reactions to other neuromuscular blocking agents. In addition, inform your patients that severe anaphylactic reactions to neuromuscular blocking agents, including ANECTINE have been reported.
Reduced Plasma Cholinesterase Activity
Succinylcholine should be used carefully in patients with reduced plasma cholinesterase (pseudocholinesterase) activity. The likelihood of prolonged neuromuscular block following administration of succinylcholine must be considered in such patients (see DOSAGE AND ADMINISTRATION).
Plasma cholinesterase activity may be diminished in the presence of genetic abnormalities of plasma cholinesterase (e.g., patients heterozygous or homozygous for atypical plasma cholinesterase gene), pregnancy, severe liver or kidney disease, malignant tumors, infections, burns, anemia, decompensated heart disease, peptic ulcer, or myxedema. Plasma cholinesterase activity may also be diminished by chronic administration of oral contraceptives, glucocorticoids, or certain monoamine oxidase inhibitors, and by irreversible inhibitors of plasma cholinesterase (e.g., organophosphate insecticides, echothiophate, and certain antineoplastic drugs).
Patients homozygous for atypical plasma cholinesterase gene (1 in 2500 patients) are extremely sensitive to the neuromuscular blocking effect of succinylcholine. In these patients, a 5- to 10-mg test dose of succinylcholine may be administered to evaluate sensitivity to succinylcholine, or neuromuscular blockade may be produced by the cautious administration of a 1-mg/mL solution of succinylcholine by slow IV infusion. Apnea or prolonged muscle paralysis should be treated with controlled respiration.
Drug Interactions
Drugs which may enhance the neuromuscular blocking action of succinylcholine include: promazine, oxytocin, aprotinin, certain nonpenicillin antibiotics, quinidine, ß-adrenergic blockers, procainamide, lidocaine, trimethaphan, lithium carbonate, magnesium salts, quinine, chloroquine, diethylether, isoflurane, desflurane, metoclopramide, and terbutaline. The neuromuscular blocking effect of succinylcholine may be enhanced by drugs that reduce plasma cholinesterase activity (e.g., chronically administered oral contraceptives, glucocorticoids, or certain monoamine oxidase inhibitors) or by drugs that irreversibly inhibit plasma cholinesterase (see PRECAUTIONS).
If other neuromuscular blocking agents are to be used during the same procedure, the possibility of a synergistic or antagonistic effect should be considered.
Carcinogenesis, Mutagenesis, Impairment of Fertility
There have been no long-term studies performed in animals to evaluate carcinogenic potential of succinylcholine. Genetic toxicology studies have not been completed to evaluate the genotoxic potential of succinylcholine. There are no studies to evaluate the potential impact of succinylcholine on fertility.
Pregnancy
Risk Summary
It is also not known whether succinylcholine can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Animal reproduction studies have not been conducted with succinylcholine chloride. Succinylcholine should be given to a pregnant woman only if clearly needed.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background
risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Plasma cholinesterase levels are decreased by approximately 24% during pregnancy and for several days postpartum. Therefore, a higher proportion of patients may be expected to show increased sensitivity (prolonged apnea) to succinylcholine when pregnant than when nonpregnant.
Labor and Delivery
Succinylcholine is commonly used to provide muscle relaxation during delivery by Cesarean section. While small amounts of succinylcholine are known to cross the placental barrier, under normal conditions the quantity of drug that enters fetal circulation after a single dose of 1 mg/kg to the mother should not endanger the fetus. However, since the amount of drug that crosses the placental barrier is dependent on the concentration gradient between the maternal and fetal circulations, residual neuromuscular blockade (apnea and flaccidity) may occur in the neonate after repeated high doses to, or in the presence of atypical plasma cholinesterase in, the mother.
Nursing Mothers
It is not known whether succinylcholine is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised following succinylcholine administration to a nursing woman.
Pediatric Use
There are rare reports of ventricular dysrhythmias and cardiac arrest secondary to acute rhabdomyolysis with hyperkalemia in apparently healthy pediatric patients who receive succinylcholine (see
BOX WARNING). Many of these pediatric patients were subsequently found to have a skeletal muscle myopathy such as Duchenne’s muscular dystrophy whose clinical signs were not obvious. The syndrome often presents as sudden cardiac arrest within minutes after the administration of succinylcholine. These pediatric patients are usually, but not exclusively, males, and most frequently 8 years of age or younger. There have also been reports in adolescents. There may be no signs or symptoms to alert the practitioner to which patients are at risk. A careful history and physical may identify developmental delays suggestive of a myopathy. A preoperative creatine kinase could identify some but not all patients at risk. Due to the abrupt onset of this syndrome, routine resuscitative measures are likely to be unsuccessful. Careful monitoring of the electrocardiogram may alert the practitioner to peaked T-waves (an early sign). Administration of IV calcium, bicarbonate, and glucose with insulin, with hyperventilation have resulted in successful resuscitation in some of the reported cases. Extraordinary and prolonged resuscitative efforts
have been effective in some cases. In addition, in the presence of signs of malignant hyperthermia, appropriate treatment should be initiated concurrently (see
WARNINGS). Since it is difficult to identify which patients are at risk, it is recommended that the use of succinylcholine in pediatric patients should be reserved for emergency intubation or instances where immediate securing of the airway is necessary, e.g., laryngospasm, difficult airway, full stomach, or for intramuscular use when a suitable vein is inaccessible.
As in adults, the incidence of bradycardia in pediatric patients is higher following the second dose of succinylcholine. The incidence and severity of bradycardia is higher in pediatric patients than in adults. Pretreatment with anticholinergic agents, e.g., atropine, may reduce the occurrence of bradyarrhythmias.
ADVERSE REACTIONS
Adverse reactions to succinylcholine consist primarily of an extension of its pharmacological actions. Succinylcholine causes profound muscle relaxation resulting in respiratory depression to the point of apnea; this effect may be prolonged. Hypersensitivity reactions, including anaphylaxis, may occur in rare instances. The following additional adverse reactions have been reported: cardiac arrest, malignant hyperthermia, arrhythmias, bradycardia, tachycardia, hypertension, hypotension, hyperkalemia, prolonged respiratory depression or apnea, increased intraocular pressure, muscle fasciculation, jaw rigidity, postoperative muscle pain, rhabdomyolysis with possible myoglobinuric acute renal failure, excessive salivation, and rash.
There have been post-marketing reports of severe allergic reactions (anaphylactic and anaphylactoid reactions) associated with use of neuromuscular blocking agents, including ANECTINE. These reactions, in some cases, have been life-threatening and fatal. Because these reactions were reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency (see WARNINGSand PRECAUTIONS).
OVERDOSAGE
Overdosage with succinylcholine may result in neuromuscular block beyond the time needed for surgery and anesthesia. This may be manifested by skeletal muscle weakness, decreased respiratory reserve, low tidal volume, or apnea. The primary treatment is maintenance of a patent airway and respiratory support until recovery of normal respiration is assured. Depending on the dose and duration of succinylcholine administration, the characteristic depolarizing neuromuscular block (Phase I) may change to a block with characteristics superficially resembling a nondepolarizing block (Phase II) (see PRECAUTIONS).
DOSAGE AND ADMINISTRATION
The dosage of succinylcholine should be individualized and should always be determined by the clinician after careful assessment of the patient (see WARNINGS).
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit. Solutions which are not clear and colorless should not be used.
Risk of Medication Errors
Accidental administration of neuromuscular blocking agents may be fatal. Store ANECTINE with the cap and ferrule intact and in a manner that minimizes the possibility of selecting the wrong product.
Adults
For Short Surgical Procedures
The average dose required to produce neuromuscular blockade and to facilitate tracheal intubation is 0.6 mg/kg ANECTINE Injection given intravenously. The optimum dose will vary among individuals and may be from 0.3 to 1.1 mg/kg for adults. Following administration of doses in this range, neuromuscular blockade develops in about 1 minute; maximum blockade may persist for about 2 minutes, after which recovery takes place within 4 to 6 minutes. However, very large doses may result in more prolonged blockade. A 5- to 10-mg test dose may be used to determine the sensitivity of the patient and the individual recovery time (see
PRECAUTIONS).
For Long Surgical Procedures
The dose of succinylcholine administered by infusion depends upon the duration of the surgical procedure and the need for muscle relaxation. The average rate for an adult ranges between 2.5 and 4.3 mg per minute.
Solutions containing from 1 to 2 mg per mL succinylcholine have commonly been used for continuous infusion. The more dilute solution (1 mg per mL) is probably preferable from the standpoint of ease of control of the rate of administration of the drug and, hence, of relaxation. This IV solution containing 1 mg per mL may be administered at a rate of 0.5 mg (0.5 mL) to 10 mg (10 mL) per minute to obtain the required amount of relaxation. The amount required per minute will depend upon the individual response as well as the degree of relaxation required. Avoid overburdening the circulation with a large volume of fluid. It is recommended that neuromuscular function be carefully monitored with a peripheral nerve stimulator when using succinylcholine by infusion in order to avoid overdose, detect development of Phase II block, follow its rate of recovery, and assess the effects of reversing agents (see PRECAUTIONS).
Intermittent IV injections of succinylcholine may also be used to provide muscle relaxation for long procedures. An IV injection of 0.3 to 1.1 mg/kg may be given initially, followed, at appropriate intervals, by further injections of 0.04 to 0.07 mg/kg to maintain the degree of relaxation
required.
Pediatrics
For emergency tracheal intubation or in instances where immediate securing of the airway is necessary, the IV dose of succinylcholine is 2 mg/kg for infants and small pediatric patients; for older pediatric patients and adolescents the dose is 1 mg/kg (see BOX WARNING and PRECAUTIONS: Pediatric Use).
Rarely, IV bolus administration of succinylcholine in infants and pediatric patients may result in malignant ventricular arrhythmias and cardiac arrest secondary to acute rhabdomyolysis with hyperkalemia. In such situations, an underlying myopathy should be suspected.
Intravenous bolus administration of succinylcholine in infants or pediatric patients may result in profound bradycardia or, rarely, asystole. As in adults, the incidence of bradycardia in pediatric patients is higher following a second dose of succinylcholine. The occurrence of bradyarrhythmias may be reduced by pretreatment with atropine (see PRECAUTIONS: Pediatric Use).
Intramuscular Use
If necessary, succinylcholine may be given intramuscularly to infants, older pediatric patients, or adults when a suitable vein is inaccessible. A dose of up to 3 to 4 mg/kg may be given, but not more than 150 mg total dose should be administered by this route. The onset of effect of succinylcholine given intramuscularly is usually observed in about 2 to 3 minutes.
Compatibility and Admixtures
Succinylcholine is acidic (pH 3.5) and should not be mixed with alkaline solutions having a pH greater than 8.5 (e.g., barbiturate solutions). ANECTINE Injection is stable for 24 hours after dilution to a final concentration of 1 to 2 mg/mL in 5% Dextrose Injection, USP or 0.9% Sodium Chloride Injection, USP. Aseptic techniques should be used to prepare the diluted product. Admixtures of ANECTINE should be prepared for single patient use only. The unused portion of diluted ANECTINE should be discarded.
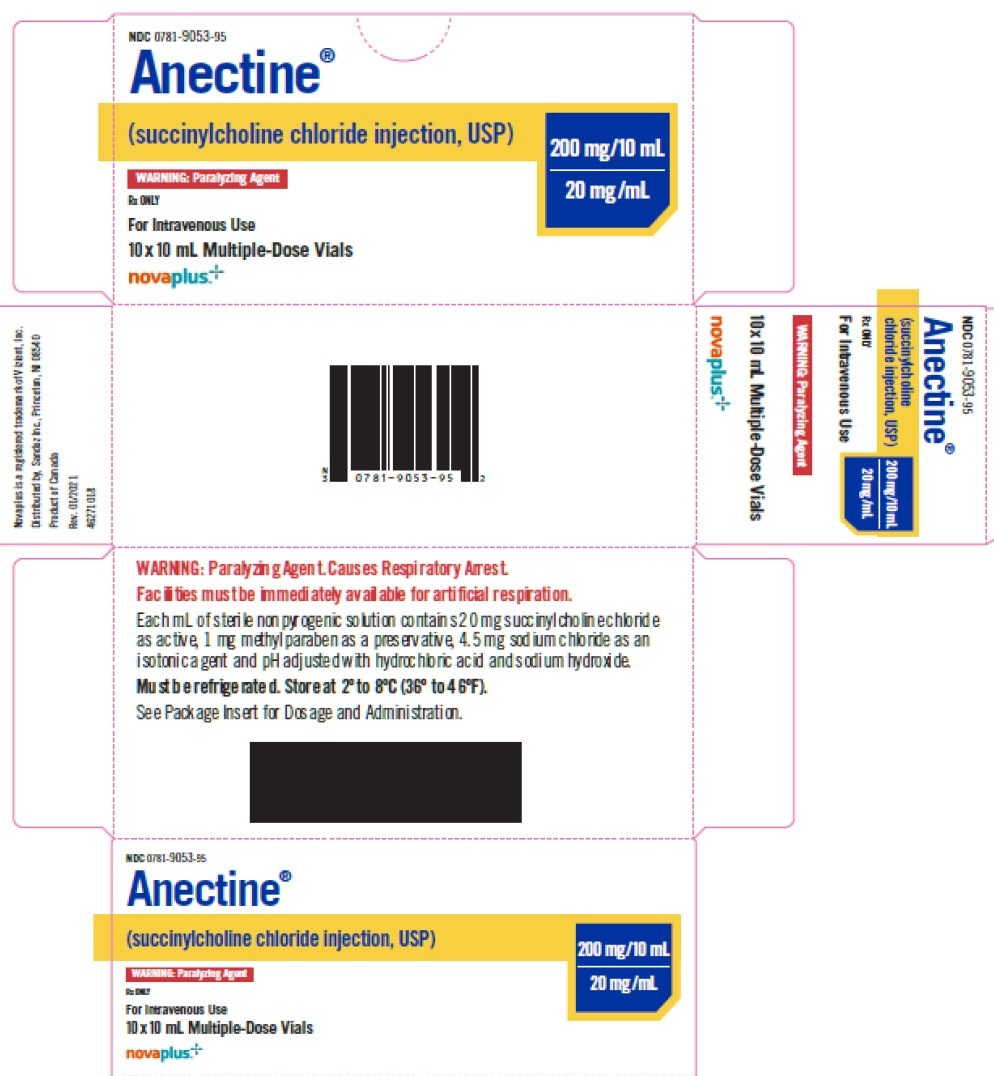
HOW SUPPLIED
ANECTINE (Succinylcholine Chloride Injection, USP) is supplied as a clear, colorless solution in Multiple-dose vials 200 mg/10 mL (20 mg/mL), box of 10 vials (NDC: 0781-9053-95).
Store in refrigerator at 2° to 8°C (36° to 46°F). The multi-dose vials are stable for up to 14 days at room temperature without significant loss of potency.
Novaplus is a registered trademark of Vizient, Inc.
Distributed by
Sandoz Inc., Princeton, NJ 08540
Rev. November 2022
46314243
| ANECTINE NOV
succinylcholine chloride injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Delpharm Boucherville Canada Inc. (242254227) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Delpharm Boucherville Canada Inc. | 242254227 | manufacture(82650-139) | |