KETALAR- ketamine hydrochloride injection
Ketalar by
Drug Labeling and Warnings
Ketalar by is a Prescription medication manufactured, distributed, or labeled by Par Pharmaceutical, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
-
SPECIAL NOTE
EMERGENCE REACTIONS HAVE OCCURRED IN APPROXIMATELY 12 PERCENT OF PATIENTS.
THE PSYCHOLOGICAL MANIFESTATIONS VARY IN SEVERITY BETWEEN PLEASANT DREAM-LIKE STATES, VIVID IMAGERY, HALLUCINATIONS, AND EMERGENCE DELIRIUM. IN SOME CASES THESE STATES HAVE BEEN ACCOMPANIED BY CONFUSION, EXCITEMENT, AND IRRATIONAL BEHAVIOR WHICH A FEW PATIENTS RECALL AS AN UNPLEASANT EXPERIENCE. THE DURATION ORDINARILY IS NO MORE THAN A FEW HOURS; IN A FEW CASES, HOWEVER, RECURRENCES HAVE TAKEN PLACE UP TO 24 HOURS POSTOPERATIVELY. NO RESIDUAL PSYCHOLOGICAL EFFECTS ARE KNOWN TO HAVE RESULTED FROM USE OF KETALAR.
THE INCIDENCE OF THESE EMERGENCE PHENOMENA IS LEAST IN THE ELDERLY (OVER 65 YEARS OF AGE) PATIENT. ALSO, THEY ARE LESS FREQUENT WHEN THE DRUG IS GIVEN INTRAMUSCULARLY AND THE INCIDENCE IS REDUCED AS EXPERIENCE WITH THE DRUG IS GAINED.
THE INCIDENCE OF PSYCHOLOGICAL MANIFESTATIONS DURING EMERGENCE, PARTICULARLY DREAM-LIKE OBSERVATIONS AND EMERGENCE DELIRIUM, MAY BE REDUCED BY USING LOWER RECOMMENDED DOSAGES OF KETALAR IN CONJUNCTION WITH INTRAVENOUS DIAZEPAM DURING INDUCTION AND MAINTENANCE OF ANESTHESIA. (See DOSAGE AND ADMINISTRATION Section). ALSO, THESE REACTIONS MAY BE REDUCED IF VERBAL, TACTILE, AND VISUAL STIMULATION OF THE PATIENT IS MINIMIZED DURING THE RECOVERY PERIOD. THIS DOES NOT PRECLUDE THE MONITORING OF VITAL SIGNS.
IN ORDER TO TERMINATE A SEVERE EMERGENCE REACTION, THE USE OF A SMALL HYPNOTIC DOSE OF A SHORT-ACTING OR ULTRA SHORT-ACTING BARBITURATE MAY BE REQUIRED.
WHEN KETALAR IS USED ON AN OUTPATIENT BASIS, THE PATIENT SHOULD NOT BE RELEASED UNTIL RECOVERY FROM ANESTHESIA IS COMPLETE AND THEN SHOULD BE ACCOMPANIED BY A RESPONSIBLE ADULT.
-
DESCRIPTION
KETALAR is a nonbarbiturate general anesthetic chemically designated dl 2-(0-chlorophenyl)-2-(methylamino) cyclohexanone hydrochloride. It is formulated as a slightly acid (pH 3.5-5.5) sterile solution for intravenous or intramuscular injection in concentrations containing the equivalent of either 10, 50 or 100 mg ketamine base per milliliter and contains not more than 0.1 mg/mL Phemerol® (benzethonium chloride) added as a preservative. The 10 mg/mL solution has been made isotonic with sodium chloride.

-
CLINICAL PHARMACOLOGY
KETALAR is a rapid-acting general anesthetic producing an anesthetic state characterized by profound analgesia, normal pharyngeal-laryngeal reflexes, normal or slightly enhanced skeletal muscle tone, cardiovascular and respiratory stimulation, and occasionally a transient and minimal respiratory depression. The mechanism of action is primarily due to antagonism of N-methyl-D-aspartate (NMDA receptors) in the central nervous system.
A patent airway is maintained partly by virtue of unimpaired pharyngeal and laryngeal reflexes. (See WARNINGS and PRECAUTIONS Sections).
The biotransformation of KETALAR includes N-dealkylation (metabolite I), hydroxylation of the cyclohexone ring (metabolites III and IV), conjugation with glucuronic acid and dehydration of the hydroxylated metabolites to form the cyclohexene derivative (metabolite II).
Following intravenous administration, the ketamine concentration has an initial slope (alpha phase) lasting about 45 minutes with a half-life of 10 to 15 minutes. This first phase corresponds clinically to the anesthetic effect of the drug. The anesthetic action is terminated by a combination of redistribution from the CNS to slower equilibrating peripheral tissues and by hepatic biotransformation to metabolite I. This metabolite is about 1/3 as active as ketamine in reducing halothane requirements (MAC) of the rat. The later half-life of ketamine (beta phase) is 2.5 hours.
The anesthetic state produced by KETALAR has been termed "dissociative anesthesia" in that it appears to selectively interrupt association pathways of the brain before producing somatesthetic sensory blockade. It may selectively depress the thalamoneocortical system before significantly obtunding the more ancient cerebral centers and pathways (reticular-activating and limbic systems).
Elevation of blood pressure begins shortly after injection, reaches a maximum within a few minutes and usually returns to preanesthetic values within 15 minutes after injection. In the majority of cases, the systolic and diastolic blood pressure peaks from 10% to 50% above preanesthetic levels shortly after induction of anesthesia, but the elevation can be higher or longer in individual cases (see CONTRAINDICATIONS Section).
Ketamine has a wide margin of safety; several instances of unintentional administration of overdoses of KETALAR (up to ten times that usually required) have been followed by prolonged but complete recovery.
KETALAR has been studied in over 12,000 operative and diagnostic procedures, involving over 10,000 patients from 105 separate studies. During the course of these studies KETALAR was administered as the sole agent, as induction for other general agents, or to supplement low-potency agents.
Specific areas of application have included the following:
1. debridement, painful dressings, and skin grafting in burn patients, as well as other superficial surgical procedures.
2. neurodiagnostic procedures such as pneumonencephalograms, ventriculograms, myelograms, and lumbar punctures. See also Precaution concerning increased intracranial pressure.
3. diagnostic and operative procedures of the eye, ear, nose, and mouth, including dental extractions.
4. diagnostic and operative procedures of the pharynx, larynx, or bronchial tree. NOTE: Muscle relaxants, with proper attention to respiration, may be required (see PRECAUTIONS Section).
5. sigmoidoscopy and minor surgery of the anus and rectum, and circumcision.
6. extraperitoneal procedures used in gynecology such as dilatation and curettage.
7. orthopedic procedures such as closed reductions, manipulations, femoral pinning, amputations, and biopsies.
8. as an anesthetic in poor-risk patients with depression of vital functions.
9. in procedures where the intramuscular route of administration is preferred.
10. in cardiac catheterization procedures.
In these studies, the anesthesia was rated either "excellent" or "good" by the anesthesiologist and the surgeon at 90% and 93%, respectively; rated "fair" at 6% and 4%, respectively; and rated "poor" at 4% and 3%, respectively. In a second method of evaluation, the anesthesia was rated "adequate" in at least 90%, and "inadequate" in 10% or less of the procedures.
-
INDICATIONS AND USAGE
KETALAR is indicated as the sole anesthetic agent for diagnostic and surgical procedures that do not require skeletal muscle relaxation.
KETALAR is best suited for short procedures but it can be used, with additional doses, for longer procedures.
KETALAR is indicated for the induction of anesthesia prior to the administration of other general anesthetic agents.
KETALAR is indicated to supplement low-potency agents, such as nitrous oxide.
Specific areas of application are described in the CLINICAL PHARMACOLOGY Section.
- CONTRAINDICATIONS
-
WARNINGS
Cardiac function should be continually monitored during the procedure in patients found to have hypertension or cardiac decompensation.
Postoperative confusional states may occur during the recovery period. (See Special Note).
Respiratory depression may occur with overdosage or too rapid a rate of administration of KETALAR, in which case supportive ventilation should be employed. Mechanical support of respiration is preferred to administration of analeptics.
Pediatric Neurotoxicity
Published animal studies demonstrate that the administration of anesthetic and sedation drugs that block NMDA receptors and/or potentiate GABA activity increase neuronal apoptosis in the developing brain and result in long-term cognitive deficits when used for longer than 3 hours. The clinical significance of these findings is not clear. However, based on the available data, the window of vulnerability to these changes is believed to correlate with exposures in the third trimester of gestation through the first several months of life, but may extend out to approximately three years of age in humans. (See PRECAUTIONS/Pregnancy).
Some published studies in children suggest that similar deficits may occur after repeated or prolonged exposures to anesthetic agents early in life and may result in adverse cognitive or behavioral effects. These studies have substantial limitations, and it is not clear if the observed effects are due to the anesthetic/sedation drug administration or other factors such as the surgery or underlying illness.
Anesthetic and sedation drugs are a necessary part of the care of children needing surgery, other procedures, or tests that cannot be delayed, and no specific medications have been shown to be safer than any other. Decisions regarding the timing of any elective procedures requiring anesthesia should take into consideration the benefits of the procedure weighed against the potential risks.
-
PRECAUTIONS
General
KETALAR should be used by or under the direction of physicians experienced in administering general anesthetics and in maintenance of an airway and in the control of respiration.
Because pharyngeal and laryngeal reflexes are usually active, KETALAR should not be used alone in surgery or diagnostic procedures of the pharynx, larynx, or bronchial tree. Mechanical stimulation of the pharynx should be avoided, whenever possible, if KETALAR is used alone. Muscle relaxants, with proper attention to respiration, may be required in both of these instances.
Resuscitative equipment should be ready for use.
The incidence of emergence reactions may be reduced if verbal and tactile stimulation of the patient is minimized during the recovery period. This does not preclude the monitoring of vital signs (see Special Note).
The intravenous dose should be administered over a period of 60 seconds. More rapid administration may result in respiratory depression or apnea and enhanced pressor response.
In surgical procedures involving visceral pain pathways, KETALAR should be supplemented with an agent which obtunds visceral pain.
Use with caution in the chronic alcoholic and the acutely alcohol-intoxicated patient.
An increase in cerebrospinal fluid pressure has been reported following administration of ketamine hydrochloride. Use with extreme caution in patients with preanesthetic elevated cerebrospinal fluid pressure.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Long-term animal studies have not been conducted to evaluate the carcinogenic potential of ketamine.
Mutagenesis
In a published report, ketamine was clastogenic in the in vitro chromosomal aberration assay.
Impairment of Fertility
Adequate studies to evaluate the impact of ketamine on male or female fertility have not been conducted. Male and female rats were treated with 10 mg/kg ketamine IV (0.8 times the average human induction dose of 2 mg/kg IV based on body surface area) on Days 11, 10, and 9 prior to mating. No impact on fertility was noted; however, this study design does not adequately characterize the impact of a drug on fertility endpoints.
Pregnancy
Risk Summary
There are no adequate and well-controlled studies of KETALAR in pregnant women. In animal reproduction studies in rats developmental delays (hypoplasia of skeletal tissues) were noted at 0.3 times the human intramuscular dose of 10 mg/kg. In rabbits, developmental delays and increased fetal resorptions were noted at 0.6 times the human dose. Published studies in pregnant primates demonstrate that the administration of anesthetic and sedation drugs that block NMDA receptors and/or potentiate GABA activity during the period of peak brain development increases neuronal apoptosis in the developing brain of the offspring when used for longer than 3 hours. There are no data on pregnancy exposures in primates corresponding to periods prior to the third trimester in humans.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Clinical Considerations
Since the safe use in pregnancy, including obstetrics (either vaginal or abdominal delivery), has not been established, such use is not recommended (see ANIMAL PHARMACOLOGY AND TOXICOLOGY).
Data
Animal Data
Pregnant rats were treated intramuscularly with 20 mg/kg ketamine (0.3 times the human dose of 10 mg/kg IM based on body surface area) on either Gestation Days 6 to 10 or Gestation Days 11 to 15. Ketamine treatment produced an increased incidence of hypoplastic skull, phalanges, and sternebrae in the pups.
Pregnant rabbits were treated intramuscularly with 20 mg/kg ketamine (0.6 times the human dose of 10 mg/kg IM based on body surface area) on either Gestation Days 6 to 10 or Gestation Days 11 to 15. An increase in resorptions and skeletal hypoplasia of the fetuses were noted. Additional pregnant rabbits were treated intramuscularly with a single dose 60 mg/kg (1.9 times the human dose of 10 mg/kg IM based on body surface area) on Gestation Day 6 only. Skeletal hypoplasia was reported in the fetuses.
In a study where pregnant rats were treated intramuscularly with 20 mg/kg ketamine (0.3 times the human dose of 10 mg/kg IM based on body surface area) from Gestation Day 18 to 21. There was a slight increase in incidence of delayed parturition by one day in treated dams of this group. No adverse effects on the litters or pups were noted; however, learning and memory assessments were not completed.
Three pregnant beagle dogs were treated intramuscularly with 25 mg/kg ketamine (1.3 times the human dose of 10 mg/kg IM based on body surface area) twice weekly for the three weeks of the first, second, and third trimesters of pregnancy, respectively, without the development of adverse effects in the pups.
In a published study in primates, administration of an anesthetic dose of ketamine for 24 hours on Gestation Day 122 increased neuronal apoptosis in the developing brain of the fetus. In other published studies, administration of either isoflurane or propofol for 5 hours on Gestation Day 120 resulted in increased neuronal and oligodendrocyte apoptosis in the developing brain of the offspring. With respect to brain development, this time period corresponds to the third trimester of gestation in the human. The clinical significance of these findings is not clear; however, studies in juvenile animals suggest neuroapoptosis correlates with long-term cognitive deficits. (See WARNINGS/Pediatric Neurotoxicity, Pediatric Use, and ANIMAL TOXICOLOGY AND PHARMACOLOGY).
Information for Patients
Risk of Drowsiness
As appropriate, especially in cases where early discharge is possible, the duration of KETALAR and other drugs employed during the conduct of anesthesia should be considered. The patients should be cautioned that driving an automobile, operating hazardous machinery or engaging in hazardous activities should not be undertaken for 24 hours or more (depending upon the dosage of KETALAR and consideration of other drugs employed) after anesthesia.
Effect of anesthetic and sedation drugs on early brain development
Studies conducted in young animals and children suggest repeated or prolonged use of general anesthetic or sedation drugs in children younger than 3 years may have negative effects on their developing brains. Discuss with parents and caregivers the benefits, risks, and timing and duration of surgery or procedures requiring anesthetic and sedation drugs (See WARNINGS/Pediatric Neurotoxicity).
Drug Interactions
Prolonged recovery time may occur if barbiturates and/or narcotics are used concurrently with KETALAR.
KETALAR is clinically compatible with the commonly used general and local anesthetic agents when an adequate respiratory exchange is maintained.
Geriatric Use
Clinical studies of ketamine hydrochloride did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Pediatric Use
Safety and effectiveness in pediatric patients below the age of 16 have not been established.
Published juvenile animal studies demonstrate that the administration of anesthetic and sedation drugs, such as KETALAR, that either block NMDA receptors or potentiate the activity of GABA during the period of rapid brain growth or synaptogenesis, results in widespread neuronal and oligodendrocyte cell loss in the developing brain and alterations in synaptic morphology and neurogenesis. Based on comparisons across species, the window of vulnerability to these changes is believed to correlate with exposures in the third trimester of gestation through the first several months of life, but may extend out to approximately 3 years of age in humans.
In primates, exposure to 3 hours of ketamine that produced a light surgical plane of anesthesia did not increase neuronal cell loss, however, treatment regimens of 5 hours or longer of isoflurane increased neuronal cell loss. Data from isoflurane-treated rodents and ketamine-treated primates suggest that the neuronal and oligodendrocyte cell losses are associated with prolonged cognitive deficits in learning and memory. The clinical significance of these nonclinical findings is not known, and healthcare providers should balance the benefits of appropriate anesthesia in pregnant women, neonates, and young children who require procedures with the potential risks suggested by the nonclinical data. (See WARNINGS/Pediatric Neurotoxicity, Pregnancy).
-
ADVERSE REACTIONS
Cardiovascular: Blood pressure and pulse rate are frequently elevated following administration of KETALAR alone. However, hypotension and bradycardia have been observed. Arrhythmia has also occurred.
Respiration: Although respiration is frequently stimulated, severe depression of respiration or apnea may occur following rapid intravenous administration of high doses of KETALAR. Laryngospasms and other forms of airway obstruction have occurred during KETALAR anesthesia.
Eye: Diplopia and nystagmus have been noted following KETALAR administration. It also may cause a slight elevation in intraocular pressure measurement.
Genitourinary: In individuals with history of chronic ketamine use or abuse, lower urinary tract and bladder symptoms including dysuria, increased urinary frequency, urgency, urge incontinence, and hematuria have been reported (see DOSAGE AND ADMINISTRATION Section). In addition, diagnostic studies performed to assess the cause of these symptoms have reported cystitis (including cystitis non-infective, cystitis interstitial, cystitis ulcerative, cystitis erosive and cystitis hemorrhagic) as well as hydronephrosis and reduced bladder capacity.
Psychological: (See Special Note).
Neurological: In some patients, enhanced skeletal muscle tone may be manifested by tonic and clonic movements sometimes resembling seizures (see DOSAGE AND ADMINISTRATION Section).
Gastrointestinal: Anorexia, nausea and vomiting have been observed; however, this is not usually severe and allows the great majority of patients to take liquids by mouth shortly after regaining consciousness (see DOSAGE AND ADMINISTRATION Section).
General: Anaphylaxis. Local pain and exanthema at the injection site have infrequently been reported. Transient erythema and/or morbilliform rash have also been reported.
For medical advice about adverse reactions contact your medical professional. To report SUSPECTED ADVERSE REACTIONS, contact Par Pharmaceutical at 1-800-828-9393 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
-
DRUG ABUSE AND DEPENDENCE
Ketamine has been reported being used as a drug of abuse.
Reports suggest that ketamine produces a variety of symptoms including, but not limited to anxiety, dysphoria, disorientation, insomnia, flashbacks, hallucinations, and psychotic episodes.
Ketamine dependence and tolerance are possible following prolonged administration. A withdrawal syndrome with psychotic features has been described following discontinuation of long-term ketamine use. Therefore, ketamine should be prescribed and administered with caution.
- OVERDOSAGE
-
DOSAGE AND ADMINISTRATION
Note: Barbiturates and KETALAR, being chemically incompatible because of precipitate formation, should not be injected from the same syringe.
If the KETALAR dose is augmented with diazepam, the two drugs must be given separately. Do not mix KETALAR and diazepam in syringe or infusion flask. For additional information on the use of diazepam, refer to the WARNINGS and DOSAGE AND ADMINISTRATION Sections of the diazepam insert.
Preoperative Preparations:
1. While vomiting has been reported following KETALAR administration, some airway protection may be afforded because of active laryngeal-pharyngeal reflexes. However, since aspiration may occur with KETALAR and since protective reflexes may also be diminished by supplementary anesthetics and muscle relaxants, the possibility of aspiration must be considered. KETALAR is recommended for use in the patient whose stomach is not empty when, in the judgment of the practitioner, the benefits of the drug outweigh the possible risks.
2. Atropine, scopolamine, or another drying agent should be given at an appropriate interval prior to induction.
Onset and Duration:
Because of rapid induction following the initial intravenous injection, the patient should be in a supported position during administration.
The onset of action of KETALAR is rapid; an intravenous dose of 2 mg/kg of body weight usually produces surgical anesthesia within 30 seconds after injection, with the anesthetic effect usually lasting five to ten minutes. If a longer effect is desired, additional increments can be administered intravenously or intramuscularly to maintain anesthesia without producing significant cumulative effects.
Intramuscular doses, in a range of 9 to 13 mg/kg usually produce surgical anesthesia within 3 to 4 minutes following injection, with the anesthetic effect usually lasting 12 to 25 minutes.
Dosage:
As with other general anesthetic agents, the individual response to KETALAR is somewhat varied depending on the dose, route of administration, and age of patient, so that dosage recommendation cannot be absolutely fixed. The drug should be titrated against the patient's requirements.
In individuals with a history of chronic ketamine use for off-label indications, there have been case reports of genitourinary pain that may be related to the ketamine treatment, not the underlying condition (see Adverse Reactions Section). Consider cessation of ketamine if genitourinary pain continues in the setting of other genitourinary symptoms.
Induction:
Intravenous Route: The initial dose of KETALAR administered intravenously may range from 1 mg/kg to 4.5 mg/kg. The average amount required to produce five to ten minutes of surgical anesthesia has been 2 mg/kg.
Alternatively, in adult patients an induction dose of 1 mg to 2 mg/kg intravenous ketamine at a rate of 0.5 mg/kg/min may be used for induction of anesthesia. In addition, diazepam in 2 mg to 5 mg doses, administered in a separate syringe over 60 seconds, may be used. In most cases, 15 mg of intravenous diazepam or less will suffice. The incidence of psychological manifestations during emergence, particularly dream-like observations and emergence delirium, may be reduced by this induction dosage program.
Note: The 100 mg/mL concentration of KETALAR should not be injected intravenously without proper dilution. It is recommended the drug be diluted with an equal volume of either Sterile Water for injection, USP, Normal Saline, or 5% Dextrose in Water.
Maintenance of Anesthesia:
The maintenance dose should be adjusted according to the patient's anesthetic needs and whether an additional anesthetic agent is employed.
Increments of one-half to the full induction dose may be repeated as needed for maintenance of anesthesia. However, it should be noted that purposeless and tonic-clonic movements of extremities may occur during the course of anesthesia. These movements do not imply a light plane and are not indicative of the need for additional doses of the anesthetic.
It should be recognized that the larger the total dose of KETALAR administered, the longer will be the time to complete recovery.
Adult patients induced with KETALAR augmented with intravenous diazepam may be maintained on KETALAR given by slow microdrip infusion technique at a dose of 0.1 to 0.5 mg/minute, augmented with diazepam 2 to 5 mg administered intravenously as needed. In many cases 20 mg or less of intravenous diazepam total for combined induction and maintenance will suffice. However, slightly more diazepam may be required depending on the nature and duration of the operation, physical status of the patient, and other factors. The incidence of psychological manifestations during emergence, particularly dream-like observations and emergence delirium, may be reduced by this maintenance dosage program.
Dilution: To prepare a dilute solution containing 1 mg of ketamine per mL, aseptically transfer 10 mL from a 50 mg per mL vial or 5 mL from a 100 mg per mL vial to 500 mL of 5% Dextrose Injection, USP or Sodium Chloride (0.9%) Injection, USP (Normal Saline) and mix well. The resultant solution will contain 1 mg of ketamine per mL.
The fluid requirements of the patient and duration of anesthesia must be considered when selecting the appropriate dilution of KETALAR. If fluid restriction is required, KETALAR can be added to a 250 mL infusion as described above to provide a KETALAR concentration of 2 mg/mL.
KETALAR 10 mg/mL vials are not recommended for dilution.
Supplementary Agents:
KETALAR is clinically compatible with the commonly used general and local anesthetic agents when an adequate respiratory exchange is maintained.
The regimen of a reduced dose of KETALAR supplemented with diazepam can be used to produce balanced anesthesia by combination with other agents such as nitrous oxide and oxygen.
-
HOW SUPPLIED
KETALAR is supplied as the hydrochloride in concentrations equivalent to ketamine base.
NDC: 42023-113-10 — Each 20-mL multi-dose vial contains 10 mg/mL. Supplied in cartons of 10.
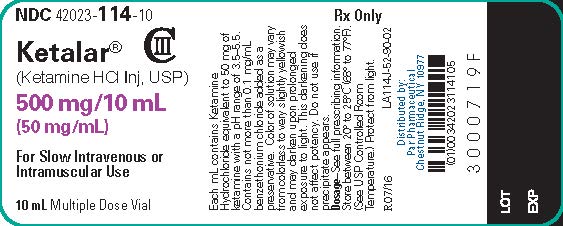
NDC: 42023-114-10 — Each 10-mL multi-dose vial contains 50 mg/mL. Supplied in cartons of 10.
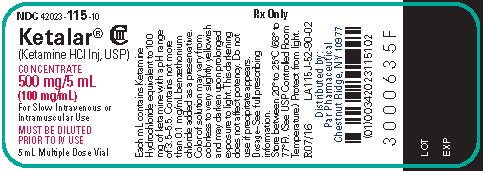
NDC: 42023-115-10 — Each 5-mL multi-dose vial contains 100 mg/mL. Supplied in cartons of 10. -
ANIMAL PHARMACOLOGY AND TOXICOLOGY
Published studies in animals demonstrate that the use of anesthetic agents during the period of rapid brain growth or synaptogenesis results in widespread neuronal and oligodendrocyte cell loss in the developing brain and alterations in synaptic morphology and neurogenesis. Based on comparisons across species, the window of vulnerability to these changes is believed to correlate with exposures in the third trimester through the first several months of life, but may extend out to approximately 3 years of age in humans.
In primates, exposure to 3 hours of an anesthetic regimen that produced a light surgical plane of anesthesia did not increase neuronal cell loss, however, treatment regimens of 5 hours or longer increased neuronal cell loss. Data in rodents and in primates suggest that the neuronal and oligodendrocyte cell losses are associated with subtle but prolonged cognitive deficits in learning and memory. The clinical significance of these nonclinical findings is not known, and healthcare providers should balance the benefits of appropriate anesthesia in neonates and young children who require procedures against the potential risks suggested by the nonclinical data. (See WARNINGS/Pediatric Neurotoxicity, Use in Pregnancy, and Pediatric Use).
In published studies, intraperitoneal administration of ketamine at doses greater than 40 mg/kg induced vacuolation in neuronal cells of the posterior cingulate and retrosplenial cortices in adult rats, similar to what has been reported in rodents administered other NMDA receptor antagonists. These vacuoles were demonstrated to be reversible and did not progress to degeneration or neuronal death up to doses of 80 mg/kg (1.2 times the human dose of 10 mg/kg based on body surface area). A no-effect level for neuronal vacuolation was 20 mg/kg intraperitoneal (0.3 times a human dose of 10 mg/kg on a body surface area basis). The window of vulnerability to these changes is believed to correlate with exposures in humans from the onset of puberty through adulthood. The relevance of this finding to humans is unknown.
- SPL UNCLASSIFIED SECTION
- PRINCIPAL DISPLAY PANEL - 20 mL Vial Label
- PRINCIPAL DISPLAY PANEL - 10 mL Vial Label
- PRINCIPAL DISPLAY PANEL - 5 mL Vial Label
-
INGREDIENTS AND APPEARANCE
KETALAR
ketamine hydrochloride injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 42023-113 Route of Administration INTRAMUSCULAR, INTRAVENOUS DEA Schedule CIII Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength KETAMINE HYDROCHLORIDE (UNII: O18YUO0I83) (KETAMINE - UNII:690G0D6V8H) KETAMINE 10 mg in 1 mL Inactive Ingredients Ingredient Name Strength BENZETHONIUM CHLORIDE (UNII: PH41D05744) SODIUM CHLORIDE (UNII: 451W47IQ8X) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 42023-113-10 10 in 1 CARTON 10/01/2007 1 20 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA016812 10/01/2007 KETALAR
ketamine hydrochloride injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 42023-114 Route of Administration INTRAMUSCULAR, INTRAVENOUS DEA Schedule CIII Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength KETAMINE HYDROCHLORIDE (UNII: O18YUO0I83) (KETAMINE - UNII:690G0D6V8H) KETAMINE 50 mg in 1 mL Inactive Ingredients Ingredient Name Strength BENZETHONIUM CHLORIDE (UNII: PH41D05744) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 42023-114-10 10 in 1 CARTON 10/01/2007 1 10 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA016812 10/01/2007 KETALAR
ketamine hydrochloride injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 42023-115 Route of Administration INTRAMUSCULAR, INTRAVENOUS DEA Schedule CIII Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength KETAMINE HYDROCHLORIDE (UNII: O18YUO0I83) (KETAMINE - UNII:690G0D6V8H) KETAMINE 100 mg in 1 mL Inactive Ingredients Ingredient Name Strength BENZETHONIUM CHLORIDE (UNII: PH41D05744) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 42023-115-10 10 in 1 CARTON 10/01/2007 1 5 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA016812 10/01/2007 Labeler - Par Pharmaceutical, Inc. (092733690)
Trademark Results [Ketalar]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 KETALAR 72276388 0840783 Live/Registered |
PARKE, DAVIS & COMPANY 1967-07-20 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.