ZANOSAR- streptozocin powder, for solution
Zanosar by
Drug Labeling and Warnings
Zanosar by is a Prescription medication manufactured, distributed, or labeled by Teva Parenteral Medicines, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
-
BOXED WARNING
(What is this?)
WARNING
ZANOSAR should be administered under the supervision of a physician experienced in the use of cancer chemotherapeutic agents.
A patient need not be hospitalized but should have access to a facility with laboratory and supportive resources sufficient to monitor drug tolerance and to protect and maintain a patient compromised by drug toxicity. Renal toxicity is dose-related and cumulative and may be severe or fatal. Other major toxicities are nausea and vomiting which may be severe and at times treatment-limiting. In addition, liver dysfunction, diarrhea, and hematological changes have been observed in some patients. Streptozocin is mutagenic. When administered parenterally, it has been found to be tumorigenic or carcinogenic in some rodents.
The physician must judge the possible benefit to the patient against the known toxic effects of this drug in considering the advisability of therapy with ZANOSAR. The physician should be familiar with the following text before making a judgment and beginning treatment.
-
DESCRIPTION
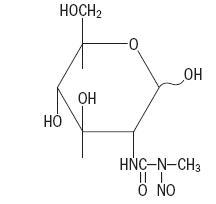
Each vial of ZANOSAR contains 1 g of the active ingredient streptozocin 2-deoxy-2 [[(methylnitrosoamino)carbonyl]amino]-α (and ß)-D-glucopyranose and 220 mg citric acid anhydrous. ZANOSAR is available as a sterile, pale yellow, freeze-dried preparation for intravenous administration. The pH was adjusted with sodium hydroxide. When reconstituted as directed, the pH of the solution will be between 3.5 and 4.5. Streptozocin is a synthetic antineoplastic agent that is chemically related to other nitrosoureas used in cancer chemotherapy. Streptozocin is an ivory-colored crystalline powder with a molecular weight of 265.2. It is very soluble in water or physiological saline and is soluble in alcohol. The structural formula is represented below:
-
CLINICAL PHARMACOLOGY
Streptozocin inhibits DNA synthesis in bacterial and mammalian cells. In bacterial cells, a specific interaction with cytosine moieties leads to degradation of DNA. The biochemical mechanism leading to mammalian cell death has not been definitely established; streptozocin inhibits cell proliferation at a considerably lower level than that needed to inhibit precursor incorporation into DNA or to inhibit several of the enzymes involved in DNA synthesis. Although streptozocin inhibits the progression of cells into mitosis, no specific phase of the cell cycle is particularly sensitive to its lethal effects.
Streptozocin is active in the L1210 leukemic mouse over a fairly wide range of parenteral dosage schedules. In experiments in many animal species, streptozocin induced a diabetes that resembles human hyperglycemic nonketotic diabetes mellitus. This phenomenon, which has been extensively studied, appears to be mediated through a lowering of beta cell nicotinamide adenine dinucleotide (NAD) and consequent histopathologic alteration of pancreatic islet beta cells.
The metabolism and the chemical dissociation of streptozocin that occurs under physiologic conditions has not been extensively studied. When administered intravenously to a variety of experimental animals, streptozocin disappears from the blood very rapidly. In all species tested, it was found to concentrate in the liver and kidney. As much as 20% of the drug (or metabolites containing an N-nitrosourea group) is metabolized and/or excreted by the kidney. Metabolic products have not yet been identified.
-
INDICATIONS AND USAGE
ZANOSAR is indicated in the treatment of metastatic islet cell carcinoma of the pancreas. Responses have been obtained with both functional and nonfunctional carcinomas. Because of its inherent renal toxicity, therapy with this drug should be limited to patients with symptomatic or progressive metastatic disease.
-
WARNINGS
Renal Toxicity
Many patients treated with ZANOSAR have experienced renal toxicity, as evidenced by azotemia, anuria, hypophosphatemia, glycosuria and renal tubular acidosis. Such toxicity is dose-related and cumulative and may be severe or fatal. Renal function must be monitored before and after each course of therapy. Serial urinalysis, blood urea nitrogen, plasma creatinine, serum electrolytes and creatinine clearance should be obtained prior to, at least weekly during, and for four weeks after drug administration. Serial urinalysis is particularly important for the early detection of proteinuria and should be quantitated with a 24 hour collection when proteinuria is detected. Mild proteinuria is one of the first signs of renal toxicity and may herald further deterioration of renal function. Reduction of the dose of ZANOSAR or discontinuation of treatment is suggested in the presence of significant renal toxicity. Adequate hydration may help reduce the risk of nephrotoxicity to renal tubular epithelium by decreasing renal and urinary concentration of the drug and its metabolites.
Use of ZANOSAR in patients with preexisting renal disease requires a judgment by the physician of potential benefit as opposed to the known risk of serious renal damage.
This drug should not be used in combination with or concomitantly with other potential nephrotoxins.
When exposed dermally, some rats developed benign tumors at the site of application of streptozocin. Consequently, streptozocin may pose a carcinogenic hazard following topical exposure if not properly handled. (See DOSAGE AND ADMINISTRATION.) See additional warnings at the beginning of this insert.
-
PRECAUTIONS
Injection-Site Reactions
ZANOSAR sterile powder is irritating to tissues. Extravasation may cause severe tissue lesions and necrosis.
Drug Interactions
ZANOSAR may demonstrate additive toxicity when used in combination with other cytotoxic drugs. Streptozocin has been reported to prolong the elimination half-life of doxorubicin and may lead to severe bone marrow suppression; a reduction of the doxorubicin dosage should be considered in patients receiving ZANOSAR concurrently. The concurrent use of streptozocin and phenytoin has been reported in one case to result in reduced streptozocin cytotoxicity.
Information for Patients
Confusion, lethargy, and depression have been reported in a limited number of patients receiving continuous intravenous infusion of ZANOSAR for 5 days. Patients should be informed that there may be a potential risk in driving or using complex machinery.
Laboratory Tests
Patients who are treated with ZANOSAR must be monitored closely, particularly for evidence of renal, hepatic, and hematopoietic toxicity. Renal function tests are described in the WARNINGS section. Patients should also be monitored closely for evidence of hematopoietic and hepatic toxicities. Complete blood counts and liver function tests should be done at least weekly. Dosage adjustments or discontinuance of the drug may be indicated, depending upon the degree of toxicity noted.
Mutagenesis, Carcinogenesis, Impairment of Fertility
Streptozocin is mutagenic in bacteria, plants, and mammalian cells. When administered parenterally, it has been shown to induce renal tumors in rats and to induce liver tumors and other tumors in hamsters. Stomach and pancreatic tumors were observed in rats treated orally with streptozocin. Streptozocin has also been shown to be carcinogenic in mice.
Streptozocin adversely affected fertility when administered to male and female rats.
Reproduction studies revealed that streptozocin is teratogenic in the rat and has abortifacient effects in rabbits. When administered intravenously to pregnant monkeys, it appears rapidly in the fetal circulation. There are no studies in pregnant women. ZANOSAR should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nursing Mothers
It is not known whether streptozocin is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants, nursing should be discontinued in patients receiving ZANOSAR.
Geriatric Use
Clinical studies of streptozocin did not include sufficient numbers of patients aged 65 years and older to determine whether there was a difference in either efficacy or toxicity as compared to younger patients. Other reported clinical experience has not identified differences in efficacy or safety between the elderly and younger patient populations. In general, dose selection for elderly patients should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
-
ADVERSE REACTIONS
Gastrointestinal
Most patients treated with ZANOSAR have experienced severe nausea and vomiting, occasionally requiring discontinuation of drug therapy. Some patients experienced diarrhea. A number of patients have experienced hepatic toxicity, as characterized by elevated liver enzyme (SGOT and LDH) levels and hypoalbuminemia.
Hematological
Hematological toxicity has been rare, most often involving mild decreases in hematocrit values. However, fatal hematological toxicity with substantial reductions in leukocyte and platelet count has been observed.
Metabolic
Mild to moderate abnormalities of glucose tolerance have been noted in some patients treated with ZANOSAR. These have generally been reversible, but insulin shock with hypoglycemia has been observed.
- OVERDOSAGE
-
DOSAGE AND ADMINISTRATION
ZANOSAR sterile powder should be administered intravenously by rapid injection or short/prolonged infusion. It is not active orally. Although it has been administered intraarterially, this is not recommended pending further evaluation of the possibility that adverse renal effects may be evoked more rapidly by this route of administration.
Two different dosage schedules have been employed successfully with ZANOSAR.
Daily Schedule—The recommended dose for daily intravenous administration is 500 mg/m2 of body surface area for five consecutive days every six weeks until maximum benefit or until treatment-limiting toxicity is observed. Dose escalation on this schedule is not recommended.
Weekly Schedule—The recommended initial dose for weekly intravenous administration is 1000 mg/m2 of body surface area at weekly intervals for the first two courses (weeks). In subsequent courses, drug doses may be escalated in patients who have not achieved a therapeutic response and who have not experienced significant toxicity with the previous course of treatment. However, A SINGLE DOSE OF 1500 mg/m2 BODY SURFACE AREA SHOULD NOT BE EXCEEDED as a greater dose may cause azotemia. When administered on this schedule, the median time to onset of response is about 17 days and the median time to maximum response is about 35 days. The median total dose to onset of response is about 2000 mg/m2 body surface area and the median total dose to maximum response is about 4000 mg/m2 body surface area.
The ideal duration of maintenance therapy with ZANOSAR has not yet been clearly established for either of the above schedules.
For patients with functional tumors, serial monitoring of fasting insulin levels allows a determination of biochemical response to therapy. For patients with either functional or nonfunctional tumors, response to therapy can be determined by measurable reductions of tumor size (reduction of organomegaly, masses, or lymph nodes).
Reconstitute ZANOSAR with 9.5 mL of dextrose injection, USP, or 0.9% sodium chloride injection, USP. The resulting pale-gold solution will contain 100 mg of streptozocin and 22 mg of citric acid per mL. Where more dilute infusion solutions are desirable, further dilution in the above vehicles is recommended. The total storage time for streptozocin after it has been placed in solution should not exceed 12 hours. This product contains no preservatives and is not intended as a multiple-dose vial.
Caution in the handling and preparation of the powder and solution should be exercised, and the use of gloves is recommended. If the sterile powder of ZANOSAR or a solution prepared from ZANOSAR contacts the skin or mucosae, immediately wash the affected area with soap and water.
Procedures for proper handling and disposal of anticancer drugs should be considered. Several guidelines on this subject have been published.1–7 There is no general agreement that all of the procedures recommended in the guidelines are necessary or appropriate.
- HOW SUPPLIED
-
REFERENCES
- Recommendations for the Safe Handling of Parenteral Antineoplastic Drugs, NIH Publication No. 83-2621. For sale by the Superintendent of Documents, U. S. Government Printing Office, Washington, DC 20402.
- AMA Council Report. Guidelines for Handling Parenteral Antineoplastics. JAMA. 1985; 2.53(11):1590–1592.
- National Study Commission on Cytotoxic Exposure-Recommendations for Handling Cytotoxic Agents. Available from Louis P. Jeffrey, ScD. , Chairman, National Study Commission on Cytotoxic Exposure, Massachusetts College of Pharmacy and Allied Health Sciences, 179 Longwood Avenue, Boston, Massachusetts 02115.
- Clinical Oncological Society of Australia, Guidelines and Recommendations for Safe Handling of Antineoplastic Agents. Med J Australia, 1983; 1:426–428.
- Jones RB, et al: Safe Handling of Chemotherapeutic Agents: A Report from the Mount Sinai Medical Center. CA—A Cancer Journal for Clinicians, 1983; (Sept/Oct) 258–263.
- American Society of Hospital Pharmacists Technical Assistance Bulletin on Handling Cytotoxic and Hazardous Drugs. AM J. Hosp Pharm, 1990; 47:1033–1049.
- Controlling Occupational Exposure to Hazardous Drugs. (OSHA Work-Practice Guidelines), Am J Health-Syst Pharm, 1996; 53:1669–1685.
- SPL UNCLASSIFIED SECTION
-
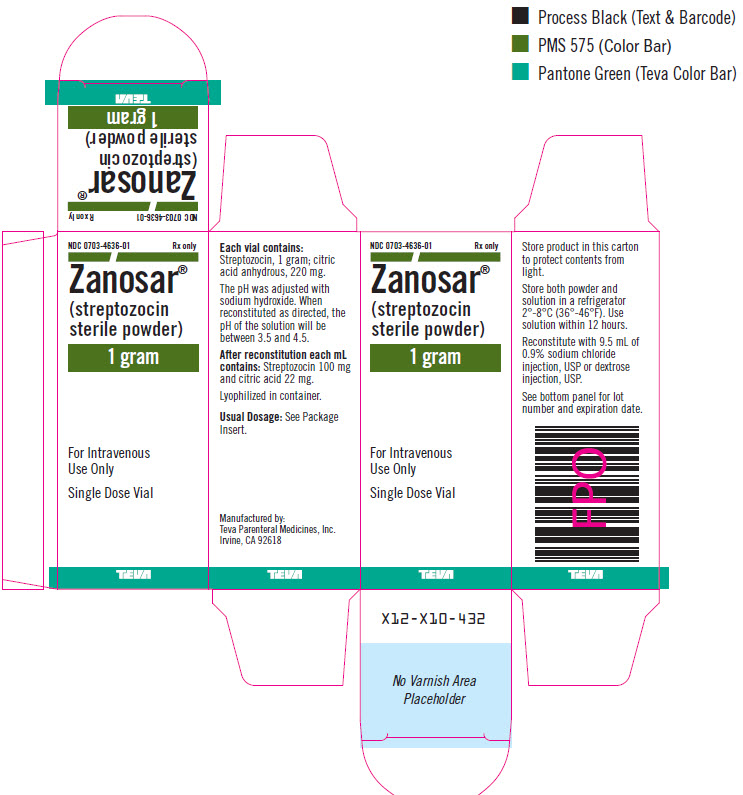
PRINCIPAL DISPLAY PANEL - 1 gram Vial Carton
NDC: 0703-4636-01 Rx only
Zanosar®
(streptozocin
sterile powder)1 gram
For Intravenous
Use OnlySingle Dose Vial
TEVA
-
INGREDIENTS AND APPEARANCE
ZANOSAR
streptozocin powder, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0703-4636 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength STREPTOZOCIN (UNII: 5W494URQ81) (STREPTOZOCIN - UNII:5W494URQ81) STREPTOZOCIN 100 mg in 1 mL Inactive Ingredients Ingredient Name Strength ANHYDROUS CITRIC ACID (UNII: XF417D3PSL) SODIUM HYDROXIDE (UNII: 55X04QC32I) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0703-4636-01 10 mL in 1 VIAL; Type 0: Not a Combination Product 12/03/2003 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA050577 12/03/2003 Labeler - Teva Parenteral Medicines, Inc. (794362533)
Trademark Results [Zanosar]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 ZANOSAR 73069901 1042644 Live/Registered |
UPJOHN COMPANY, THE 1975-11-24 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.