These highlights do not include all the information needed to use BLENREP safely and effectively. See full prescribing information for BLENREP.BLENREP (belantamab mafodotin-blmf) for injection, for intravenous useInitial U.S. Approval: 2020
Blenrep by
Drug Labeling and Warnings
Blenrep by is a Prescription medication manufactured, distributed, or labeled by GlaxoSmithKline LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
BLENREP- belantamab injection, powder, lyophilized, for solution
GlaxoSmithKline LLC
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use BLENREP safely and effectively. See full prescribing information for BLENREP.
BLENREP (belantamab mafodotin-blmf) for injection, for intravenous use Initial U.S. Approval: 2020 WARNING: OCULAR TOXICITYSee full prescribing information for complete boxed warning.
INDICATIONS AND USAGEBLENREP is a B-cell maturation antigen (BCMA)-directed antibody and microtubule inhibitor conjugate indicated for the treatment of adult patients with relapsed or refractory multiple myeloma who have received at least 4 prior therapies including an anti-CD38 monoclonal antibody, a proteasome inhibitor, and an immunomodulatory agent. This indication is approved under accelerated approval based on response rate. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trial(s). (1) DOSAGE AND ADMINISTRATIONDOSAGE FORMS AND STRENGTHSFor injection: 100 mg as a lyophilized powder in a single-dose vial for reconstitution and further dilution. (3) CONTRAINDICATIONSNone. (4) WARNINGS AND PRECAUTIONS
ADVERSE REACTIONS
To report SUSPECTED ADVERSE REACTIONS, contact GlaxoSmithKline at 1-888-825-5249 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. USE IN SPECIFIC POPULATIONSLactation: Advise not to breastfeed. (8.2) See 17 for PATIENT COUNSELING INFORMATION and Medication Guide. Revised: 2/2022 |
FULL PRESCRIBING INFORMATION
WARNING: OCULAR TOXICITY
BLENREP caused changes in the corneal epithelium resulting in changes in vision, including severe vision loss and corneal ulcer, and symptoms, such as blurred vision and dry eyes [see Warnings and Precautions (5.1)].
Conduct ophthalmic exams at baseline, prior to each dose, and promptly for worsening symptoms. Withhold BLENREP until improvement and resume, or permanently discontinue, based on severity [see Dosage and Administration (2.3), Warnings and Precautions (5.1)].
Because of the risk of ocular toxicity, BLENREP is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called the BLENREP REMS [see Warnings and Precautions (5.2)].
1 INDICATIONS AND USAGE
BLENREP is indicated for the treatment of adults with relapsed or refractory multiple myeloma who have received at least 4 prior therapies, including an anti-CD38 monoclonal antibody, a proteasome inhibitor, and an immunomodulatory agent.
This indication is approved under accelerated approval based on response rate [see Clinical Studies (14)]. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial(s).
2 DOSAGE AND ADMINISTRATION
2.1 Important Safety Information
Perform an ophthalmic exam prior to initiation of BLENREP and during treatment [see Warnings and Precautions (5.1)].
Advise patients to use preservative-free lubricant eye drops and avoid contact lenses unless directed by an ophthalmologist [see Warnings and Precautions (5.1)].
2.2 Recommended Dosage
The recommended dosage of BLENREP is 2.5 mg/kg of actual body weight given as an intravenous infusion over approximately 30 minutes once every 3 weeks until disease progression or unacceptable toxicity.
2.3 Dosage Modifications for Adverse Reactions
The recommended dose reduction for adverse reactions is:
- BLENREP 1.9 mg/kg intravenously once every 3 weeks.
Discontinue BLENREP in patients who are unable to tolerate a dose of 1.9 mg/kg (see Tables 1 and 2).
Corneal Adverse Reactions
The recommended dosage modifications for corneal adverse reactions, based on both corneal examination findings and changes in best-corrected visual acuity (BCVA), are provided in Table 1 [see Warnings and Precautions (5.1)]. Determine the recommended dosage modification of BLENREP based on the worst finding in the worst affected eye. Worst finding should be based on either a corneal examination finding or a change in visual acuity per the Keratopathy and Visual Acuity (KVA) scale.
| KVA = Keratopathy and Visual Acuity, BCVA = best corrected visual acuity. a Mild superficial keratopathy (documented worsening from baseline), with or without symptoms. b Changes in visual acuity due to treatment-related corneal findings. c Moderate superficial keratopathy with or without patchy microcyst-like deposits, sub-epithelial haze (peripheral), or a new peripheral stromal opacity. d Severe superficial keratopathy with or without diffuse microcyst-like deposits, sub-epithelial haze (central), or a new central stromal opacity. e Corneal epithelial defect such as corneal ulcers. |
||
|
Corneal Adverse Reaction |
Recommended Dosage Modifications |
|
|
Grade 1 |
Corneal examination finding(s): Mild superficial keratopathya Change in BCVAb: Decline from baseline of 1 line on Snellen Visual Acuity |
Continue treatment at current dose. |
|
Grade 2 |
Corneal examination finding(s): Moderate superficial keratopathyc Change in BCVAb: Decline from baseline of 2 or 3 lines on Snellen Visual Acuity and not worse than 20/200 |
Withhold BLENREP until improvement in both corneal examination findings and change in BCVA to Grade 1 or better and resume at same dose. |
|
Grade 3 |
Corneal examination finding(s): Severe superficial keratopathyd Change in BCVAb: Decline from baseline by more than 3 lines on Snellen Visual Acuity and not worse than 20/200 |
Withhold BLENREP until improvement in both corneal examination findings and change in BCVA to Grade 1 or better and resume at reduced dose. |
|
Grade 4 |
Corneal examination finding(s): Corneal epithelial defecte Change in BCVAb: Snellen Visual Acuity worse than 20/200 |
Consider permanent discontinuation of BLENREP. If continuing treatment, withhold BLENREP until improvement in both corneal examination findings and change in BCVA to Grade 1 or better and resume at reduced dose. |
Other Adverse Reactions
The recommended dosage modifications for other adverse reactions are provided in Table 2.
|
Adverse Reaction |
Severity |
Recommended Dosage Modifications |
|
Thrombocytopenia [see Warnings and Precautions (5.3)] |
Platelet count 25,000 to less than 50,000/mcL |
Consider withholding BLENREP and/or reducing the dose of BLENREP. |
|
Platelet count less than 25,000/mcL |
Withhold BLENREP until platelet count improves to Grade 3 or better. Consider resuming at a reduced dose. |
|
|
Infusion-related reactions [see Warnings and Precautions (5.4)] |
Grade 2 (moderate) or Grade 3 (severe) |
Interrupt infusion and provide supportive care. Once symptoms resolve, resume at lower infusion rate; reduce the infusion rate by at least 50%. |
|
Grade 4 (life-threatening) |
Permanently discontinue BLENREP and provide emergency care. |
|
|
Other Adverse Reactions [see Adverse Reactions (6.1)] |
Grade 3 |
Withhold BLENREP until improvement to Grade 1 or better. Consider resuming at a reduced dose. |
|
Grade 4 |
Consider permanent discontinuation of BLENREP. If continuing treatment, withhold BLENREP until improvement to Grade 1 or better and resume at reduced dose. |
2.4 Preparation and Administration
BLENREP is a hazardous drug. Follow applicable special handling and disposal procedures.1
Calculate the dose (mg), total volume (mL) of solution required, and the number of vials of BLENREP needed based on the patient’s actual body weight. More than 1 vial may be needed for a full dose. Do not round down for partial vials.
Reconstitution
- Remove the vial(s) of BLENREP from the refrigerator and allow to stand for approximately 10 minutes to reach room temperature (68°F to 77°F [20°C to 25°C]).
- Reconstitute each 100-mg vial of BLENREP with 2 mL of Sterile Water for Injection, USP, to obtain a final concentration of 50 mg/mL. Gently swirl the vial to aid dissolution. Do not shake.
- If the reconstituted solution is not used immediately, store refrigerated at 36ºF to 46ºF (2ºC to 8ºC) or at room temperature (68°F to 77°F [20°C to 25°C]) for up to 4 hours in the original container. Discard if not diluted within 4 hours. Do not freeze.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. The reconstituted solution should be clear to opalescent, colorless to yellow to brown liquid. Discard if extraneous particulate matter is observed.
Dilution
- Withdraw the calculated volume of BLENREP from the appropriate number of vials and dilute in a 250-mL infusion bag of 0.9% Sodium Chloride Injection, USP, to a final concentration of 0.2 mg/mL to 2 mg/mL. The infusion bags must be made of polyvinylchloride (PVC) or polyolefin (PO).
- Mix the diluted solution by gentle inversion. Do not shake.
- Discard any unused reconstituted solution of BLENREP left in the vial(s).
- If the diluted infusion solution is not used immediately, store refrigerated at 36ºF to 46ºF (2ºC to 8ºC) for up to 24 hours. Do not freeze. Once removed from refrigeration, administer the diluted infusion solution of BLENREP within 6 hours (including infusion time).
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. The diluted infusion solution should be clear and colorless. Discard if particulate matter is observed.
Administration
- If refrigerated, allow the diluted infusion solution to equilibrate to room temperature (68ºF to 77ºF [20ºC to 25ºC]) prior to administration. Diluted infusion solution may be kept at room temperature for no more than 6 hours (including infusion time).
- Administer by intravenous infusion over approximately 30 minutes using an infusion set made of polyvinyl chloride (PVC) or polyolefin (PO).
- Filtration of the diluted solution is not required; however, if the diluted solution is filtered, use a polyethersulfone (PES)-based filter (0.2 micron).
Do not mix or administer BLENREP as an infusion with other products. The product does not contain a preservative.
3 DOSAGE FORMS AND STRENGTHS
For injection: 100 mg of belantamab mafodotin-blmf as a white to yellow lyophilized powder in a single-dose vial for reconstitution and further dilution.
5 WARNINGS AND PRECAUTIONS
5.1 Ocular Toxicity
Ocular adverse reactions occurred in 77% of the 218 patients in the pooled safety population. Ocular adverse reactions included keratopathy (76%), changes in visual acuity (55%), blurred vision (27%), and dry eye (19%) [see Adverse Reactions (6.1)]. Among patients with keratopathy (n = 165), 49% had ocular symptoms, 65% had clinically relevant visual acuity changes (decline of 2 or more lines on Snellen Visual Acuity in any eye), and 34% had both ocular symptoms and visual acuity changes.
Keratopathy
Keratopathy was reported as Grade 1 in 7% of patients, Grade 2 in 22%, Grade 3 in 45%, and Grade 4 in 0.5% per the KVA scale. Cases of corneal ulcer (ulcerative and infective keratitis) have been reported. Most keratopathy events developed within the first 2 treatment cycles (cumulative incidence of 65% by Cycle 2). Of the patients with Grade 2 to 4 keratopathy (n = 149), 39% of patients recovered to Grade 1 or lower after median follow-up of 6.2 months. Of the 61% who had ongoing keratopathy, 28% were still on treatment, 9% were in follow-up, and in 24% the follow-up ended due to death, study withdrawal, or lost to follow up. For patients in whom events resolved, the median time to resolution was 2 months (range: 11 days to 8.3 months).
Visual Acuity Changes
A clinically significant decrease in visual acuity of worse than 20/40 in the better-seeing eye was observed in 19% of the 218 patients and of 20/200 or worse in the better-seeing eye in 1.4%. Of the patients with decreased visual acuity of worse than 20/40, 88% resolved and the median time to resolution was 22 days (range: 7 days to 4.2 months). Of the patients with decreased visual acuity of 20/200 or worse, all resolved and the median duration was 22 days (range: 15 to 22 days).
Monitoring and Patient Instruction
Conduct ophthalmic examinations (visual acuity and slit lamp) at baseline, prior to each dose, and promptly for worsening symptoms. Perform baseline examinations within 3 weeks prior to the first dose. Perform each follow-up examination at least 1 week after the previous dose and within 2 weeks prior to the next dose. Withhold BLENREP until improvement and resume at same or reduced dose, or consider permanently discontinuing based on severity [see Dosage and Administration (2.3)].
Advise patients to use preservative-free lubricant eye drops at least 4 times a day starting with the first infusion and continuing until end of treatment. Avoid use of contact lenses unless directed by an ophthalmologist [see Dosage and Administration (2.1)].
Changes in visual acuity may be associated with difficulty for driving and reading. Advise patients to use caution when driving or operating machinery.
BLENREP is only available through a restricted program under a REMS [see Warnings and Precautions (5.2)].
5.2 BLENREP REMS
BLENREP is available only through a restricted program under a REMS called the BLENREP REMS because of the risks of ocular toxicity [see Warnings and Precautions (5.1)].
Notable requirements of the BLENREP REMS include the following:
- Prescribers must be certified with the program by enrolling and completing training in the BLENREP REMS.
- Prescribers must counsel patients receiving BLENREP about the risk of ocular toxicity and the need for ophthalmic examinations prior to each dose.
- Patients must be enrolled in the BLENREP REMS and comply with monitoring.
- Healthcare facilities must be certified with the program and verify that patients are authorized to receive BLENREP.
- Wholesalers and distributors must only distribute BLENREP to certified healthcare facilities.
Further information is available, at www.BLENREPREMS.com and 1-855-209-9188.
5.3 Thrombocytopenia
Thrombocytopenia occurred in 69% of 218 patients in the pooled safety population, including Grade 2 in 13%, Grade 3 in 10%, and Grade 4 in 17% [see Adverse Reactions (6.1)]. The median time to onset of the first thrombocytopenic event was 26.5 days. Thrombocytopenia resulted in dose reduction, dose interruption, or discontinuation in 9%, 2.8%, and 0.5% of patients, respectively.
Grade 3 to 4 bleeding events occurred in 6% of patients, including Grade 4 in 1 patient. Fatal adverse reactions included cerebral hemorrhage in 2 patients.
Perform complete blood cell counts at baseline and during treatment as clinically indicated. Consider withholding and/or reducing the dose based on severity [see Dosage and Administration (2.3)].
5.4 Infusion-Related Reactions
Infusion-related reactions occurred in 18% of 218 patients in the pooled safety population, including Grade 3 in 1.8% [see Adverse Reactions (6.1)].
Monitor patients for infusion-related reactions. For Grade 2 or 3 reactions, interrupt the infusion and provide supportive treatment. Once symptoms resolve, resume at a lower infusion rate [see Dosage and Administration (2.3)]. Administer premedication for all subsequent infusions. Discontinue BLENREP for life-threatening infusion-related reactions and provide appropriate emergency care.
5.5 Embryo-Fetal Toxicity
Based on its mechanism of action, BLENREP can cause fetal harm when administered to a pregnant woman because it contains a genotoxic compound (the microtubule inhibitor, monomethyl auristatin F [MMAF]) and it targets actively dividing cells.
Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with BLENREP and for 4 months after the last dose. Advise males with female partners of reproductive potential to use effective contraception during treatment with BLENREP and for 6 months after the last dose [see Use in Specific Populations (8.1, 8.3)].
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Ocular toxicity [see Warnings and Precautions (5.1)].
- Thrombocytopenia [see Warnings and Precautions (5.3)].
- Infusion-related reactions [see Warnings and Precautions (5.4)].
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The pooled safety population described in Warnings and Precautions reflects exposure to BLENREP at a dosage of 2.5 mg/kg or 3.4 mg/kg (1.4 times the recommended dose) administered intravenously once every 3 weeks in 218 patients in DREAMM-2. Of these patients, 194 received a liquid formulation (not the approved dosage form) rather than the lyophilized powder. Among the 218 patients, 24% were exposed for 6 months or longer.
Relapsed or Refractory Multiple Myeloma
The safety of BLENREP as a single agent was evaluated in DREAMM-2 [see Clinical Studies (14.1)]. Patients received BLENREP at the recommended dosage of 2.5 mg/kg administered intravenously once every 3 weeks (n = 95). Among these patients, 22% were exposed for 6 months or longer.
Serious adverse reactions occurred in 40% of patients who received BLENREP. Serious adverse reactions in >3% of patients included pneumonia (7%), pyrexia (6%), renal impairment (4.2%), sepsis (4.2%), hypercalcemia (4.2%), and infusion-related reactions (3.2%). Fatal adverse reactions occurred in 3.2% of patients, including sepsis (1%), cardiac arrest (1%), and lung infection (1%).
Permanent discontinuation due to an adverse reaction occurred in 8% of patients who received BLENREP; keratopathy (2.1%) was the most frequent adverse reaction resulting in permanent discontinuation.
Dosage interruptions due to an adverse reaction occurred in 54% of patients who received BLENREP. Adverse reactions which required a dosage interruption in >3% of patients included keratopathy (47%), blurred vision (5%), dry eye (3.2%), and pneumonia (3.2%).
Dose reductions due to an adverse reaction occurred in 29% of patients. Adverse reactions which required a dose reduction in >3% of patients included keratopathy (23%) and thrombocytopenia (5%).
The most common adverse reactions (≥20%) were keratopathy, decreased visual acuity, nausea, blurred vision, pyrexia, infusion-related reactions, and fatigue. The most common Grade 3 or 4 (≥5%) laboratory abnormalities were lymphocytes decreased, platelets decreased, hemoglobin decreased, neutrophils decreased, creatinine increased, and gamma-glutamyl transferase increased.
Table 3 summarizes the adverse reactions in DREAMM-2 for patients who received the recommended dosage of 2.5 mg/kg once every 3 weeks.
| a Keratopathy was based on slit lamp eye examination, characterized as corneal epithelium changes with or without symptoms. b Visual acuity changes were determined upon eye examination. c Blurred vision included diplopia, vision blurred, visual acuity reduced, and visual impairment. d Dry eyes included dry eye, ocular discomfort, and eye pruritus. e Fatigue included fatigue and asthenia. f Infusion-related reactions included infusion-related reaction, pyrexia, chills, diarrhea, nausea, asthenia, hypertension, lethargy, tachycardia. g Upper respiratory tract infection included upper respiratory tract infection, nasopharyngitis, rhinovirus infections, and sinusitis. |
||
|
Adverse Reactions |
BLENREP N = 95 |
|
|
All Grades (%) |
Grade 3-4 (%) |
|
|
Eye disorders | ||
|
Keratopathya |
71 |
44 |
|
Decreased visual acuityb |
53 |
28 |
|
Blurred visionc |
22 |
4 |
|
Dry eyesd |
14 |
1 |
|
Gastrointestinal disorders | ||
|
Nausea |
24 |
0 |
|
Constipation |
13 |
0 |
|
Diarrhea |
13 |
1 |
|
General disorders and administration site conditions | ||
|
Pyrexia |
22 |
3 |
|
Fatiguee |
20 |
2 |
|
Procedural complications | ||
|
Infusion-related reactionsf |
21 |
3 |
|
Musculoskeletal and connective tissue disorders | ||
|
Arthralgia |
12 |
0 |
|
Back pain |
11 |
2 |
|
Metabolic and nutritional disorders | ||
|
Decreased appetite |
12 |
0 |
|
Infections | ||
|
Upper respiratory tract infectiong |
11 |
0 |
Clinically relevant adverse reactions in <10% of patients included:
Eye Disorders: Photophobia, eye irritation, infective keratitis, ulcerative keratitis.
Gastrointestinal Disorders: Vomiting.
Infections: Pneumonia.
Renal and Urinary Disorders: Albuminuria.
Table 4 summarizes the laboratory abnormalities in DREAMM-2.
|
Laboratory Abnormality |
BLENREP N = 95 |
|
|
All Grades (%) |
Grades 3-4 (%) |
|
|
Hematology | ||
|
Platelets decreased |
62 |
21 |
|
Lymphocytes decreased |
49 |
22 |
|
Hemoglobin decreased |
32 |
18 |
|
Neutrophils decreased |
28 |
9 |
|
Chemistry | ||
|
Aspartate aminotransferase increased |
57 |
2 |
|
Albumin decreased |
43 |
4 |
|
Glucose increased |
38 |
3 |
|
Creatinine increased |
28 |
5 |
|
Alkaline phosphatase increased |
26 |
1 |
|
Gamma-glutamyl transferase increased |
25 |
5 |
|
Creatinine phosphokinase increased |
22 |
1 |
|
Sodium decreased |
21 |
2 |
|
Potassium decreased |
20 |
2 |
Clinically relevant adverse reactions from expanded access programs include: pneumonitis including fatal cases.
6.2 Immunogenicity
As with all therapeutic proteins, there is potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies in the studies described below with the incidence of antibodies in other studies or to other products may be misleading.
The immunogenicity of BLENREP was evaluated using an electrochemiluminescence (ECL)-based immunoassay to test for anti-belantamab mafodotin antibodies. In clinical studies of BLENREP, 2/274 patients (<1%) tested positive for anti-belantamab mafodotin antibodies after treatment. One of the 2 patients tested positive for neutralizing anti-belantamab mafodotin antibodies following 4 weeks on therapy. Due to the limited number of patients with antibodies against belantamab mafodotin-blmf, no conclusions can be drawn concerning a potential effect of immunogenicity on pharmacokinetics, efficacy, or safety.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Based on its mechanism of action, BLENREP can cause fetal harm when administered to a pregnant woman, because it contains a genotoxic compound (the microtubule inhibitor, MMAF) and it targets actively dividing cells [see Clinical Pharmacology (12.1), Nonclinical Toxicology (13.1)]. Human immunoglobulin G (IgG) is known to cross the placenta; therefore, belantamab mafodotin-blmf has the potential to be transmitted from the mother to the developing fetus. There are no available data on the use of BLENREP in pregnant women to evaluate for drug-associated risk. No animal reproduction studies were conducted with BLENREP. Advise pregnant women of the potential risk to a fetus.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcome. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Animal Data: Animal reproductive or developmental toxicity studies were not conducted with belantamab mafodotin-blmf. The cytotoxic component of BLENREP, MMAF, disrupts microtubule function, is genotoxic, and can be toxic to rapidly dividing cells, suggesting it has the potential to cause embryotoxicity and teratogenicity.
8.2 Lactation
Risk Summary
There is no data on the presence of belantamab mafodotin-blmf in human milk or the effects on the breastfed child or milk production. Because of the potential for serious adverse reactions in the breastfed child, advise women not to breastfeed during treatment with BLENREP and for 3 months after the last dose.
8.3 Females and Males of Reproductive Potential
BLENREP can cause fetal harm when administered to pregnant women [see Use in Specific Populations (8.1)].
Pregnancy Testing
Pregnancy testing is recommended for females of reproductive potential prior to initiating BLENREP.
Contraception
Females: Advise women of reproductive potential to use effective contraception during treatment and for 4 months after the last dose.
Males: Because of the potential for genotoxicity, advise males with female partners of reproductive potential to use effective contraception during treatment with BLENREP and for 6 months after the last dose [see Nonclinical Toxicology (13.1)].
Infertility
Based on findings in animal studies, BLENREP may impair fertility in females and males. The effects were not reversible in male rats, but were reversible in female rats [see Nonclinical Toxicology (13.1)].
8.4 Pediatric Use
The safety and effectiveness of BLENREP in pediatric patients have not been established.
8.5 Geriatric Use
Of the 218 patients who received BLENREP in DREAMM-2, 43% were aged 65 to less than 75 years and 17% were aged 75 years and older. Clinical studies of BLENREP did not include sufficient numbers of patients aged 65 and older to determine whether the effectiveness differs compared with that of younger patients. Keratopathy occurred in 80% of patients aged less than 65 years and 73% of patients aged 65 years and older. Among the patients who received BLENREP at the 2.5-mg/kg dose in DREAMM-2 (n = 95), keratopathy occurred in 67% of patients aged less than 65 years and 73% of patients aged 65 years and older. Clinical studies did not include sufficient numbers of patients 75 years and older to determine whether they respond differently compared with younger patients.
8.6 Renal Impairment
No dose adjustment is recommended for patients with mild or moderate renal impairment (estimated glomerular filtration rate [eGFR] 30 to 89 mL/min/1.73m2 as estimated by the Modification of Diet in Renal Disease [MDRD] equation) [see Clinical Pharmacology (12.3)].
The recommended dosage has not been established in patients with severe renal impairment (eGFR 15 to 29 mL/min/1.73 m2) or end-stage renal disease (ESRD) with eGFR <15 mL/min/1.73 m2 not on dialysis or requiring dialysis [see Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
No dose adjustment is recommended for patients with mild hepatic impairment (total bilirubin ≤upper limit of normal [ULN] and aspartate aminotransferase (AST) >ULN or total bilirubin 1 to ≤1.5 × ULN and any AST).
The recommended dosage of BLENREP has not been established in patients with moderate or severe hepatic impairment (total bilirubin >1.5 × ULN and any AST) [see Clinical Pharmacology (12.3)].
11 DESCRIPTION
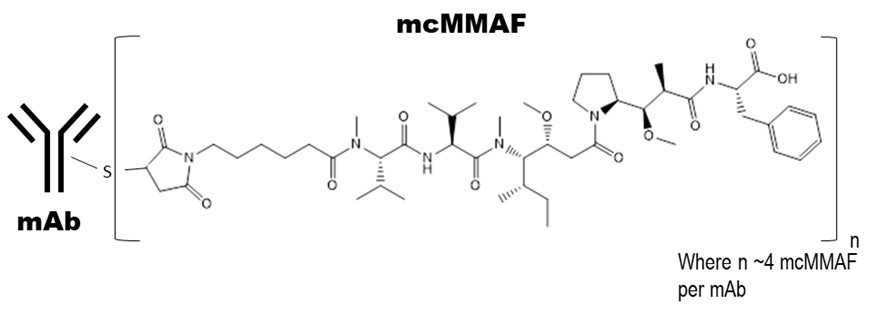
Belantamab mafodotin-blmf is a B-cell maturation antigen (BCMA)-directed antibody and microtubule inhibitor conjugate. Belantamab mafodotin-blmf is an antibody conjugate composed of 3 components: 1) afucosylated, humanized immunoglobulin G1 monoclonal antibody covalently linked to 2) the microtubule inhibitor MMAF via 3) a protease-resistant maleimidocaproyl linker.
The antibody is produced in a mammalian cell line (Chinese Hamster Ovary) using recombinant DNA technology and the microtubule inhibitor and linker are produced by chemical synthesis. Approximately 4 molecules of mafodotin are attached to each antibody molecule. The molecular weight of belantamab mafodotin-blmf is approximately 152 kDa. Belantamab mafodotin-blmf has the following structure:
BLENREP (belantamab mafodotin-blmf) for injection is a sterile, preservative-free, white to yellow, lyophilized powder in a single-dose vial for reconstitution and further dilution prior to intravenous use. BLENREP is supplied as 100 mg per vial and requires reconstitution with 2 mL of Sterile Water for Injection, USP, to obtain a concentration of 50 mg/mL. Each mL of reconstituted solution contains belantamab mafodotin-blmf (50 mg) and the inactive ingredients, citric acid (0.42 mg), disodium edetate dihydrate (0.019 mg), polysorbate 80 (0.2 mg), trehalose dihydrate (75.6 mg), and trisodium citrate dihydrate (6.7 mg). The pH of the reconstituted solution is 6.2.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Belantamab mafodotin-blmf is an antibody-drug conjugate (ADC). The antibody component is an afucosylated IgG1 directed against BCMA, a protein expressed on normal B lymphocytes and multiple myeloma cells. The small molecule component is MMAF, a microtubule inhibitor. Upon binding to BCMA, belantamab mafodotin-blmf is internalized followed by release of MMAF via proteolytic cleavage. The released MMAF intracellularly disrupts the microtubule network, leading to cell cycle arrest and apoptosis.
Belantamab mafodotin-blmf had antitumor activity in multiple myeloma cells and mediated killing of tumor cells through MMAF-induced apoptosis, as well as by tumor cell lysis through antibody-dependent cellular cytotoxicity (ADCC) and antibody-dependent cellular phagocytosis (ADCP).
12.2 Pharmacodynamics
Exposure-Response Relationships
Higher belantamab mafodotin-blmf exposure was associated with higher incidence of some adverse reactions (e.g., Grade ≥2 corneal toxicity). No exposure-response relationship for efficacy was observed at doses of 2.5 mg/kg or 3.4 mg/kg (1.4 times the recommended dose) after accounting for the effect of baseline disease-related characteristics, such as soluble BCMA, IgG, and ß2-microglobulin.
Cardiac Electrophysiology
Belantamab mafodotin-blmf had no large QTc prolongation (>10 ms) at the recommended dosage of 2.5 mg/kg once every 3 weeks.
12.3 Pharmacokinetics
Belantamab mafodotin-blmf exhibited dose-proportional pharmacokinetics, with a gradual decrease in clearance over time; the time to reach steady state was ~70 days. After a planned infusion duration of 0.5 hours, maximum belantamab mafodotin-blmf plasma concentrations occurred at or shortly after the end of the infusion. Accumulation of belantamab mafodotin-blmf was ~70% with a dosing regimen of every 3 weeks.
The pharmacokinetics of belantamab mafodotin-blmf after a dose of 2.5 mg/kg in Cycle 1 are shown in Table 5.
| AUC = Area under curve over the dosing interval; Cmax = Maximum observed plasma concentration; tmax = Time of Cmax; Ctrough = Observed plasma concentration prior to next dose. Data presented as geometric mean (%CV), except tmax, which is presented as median (minimum, maximum). |
||
|
Parameter |
Belantamab Mafodotin-blmf |
|
|
n |
Value |
|
|
AUC (mcg.h/mL) |
30 |
4,666 (46) |
|
Cmax (mcg/mL) |
32 |
42 (26) |
|
tmax (h) |
32 |
0.78 (0.4, 2.5) |
|
Ctrough (mcg/mL) |
69 |
2.4 (52) |
Distribution
The mean steady-state volume of distribution of belantamab mafodotin-blmf was 11 L (15%).
Elimination
Total plasma clearance (mean [CV%]) of belantamab mafodotin-blmf was approximately 22% lower at steady state (0.7 L/day [50%]) than after the first dose (0.9 L/day [42%]). The terminal phase half-life of belantamab mafodotin-blmf was 12 days after the first dose and 14 days at steady state.
Metabolism: The monoclonal antibody portion of belantamab mafodotin-blmf is expected to be metabolized into small peptides and individual amino acids by catabolic pathways. In vitro, cys-mcMMAF is mainly hydrolyzed and dehydrated to a cyclized isomeric form of cys-mcMMAF.
Specific Populations
No clinically significant differences in the pharmacokinetics of belantamab mafodotin-blmf were observed based on age (34 to 89 years), sex, race (White vs. Black), body weight (42 to 130 kg), mild or moderate renal impairment (eGFR 30 to 89 mL/min/1.73m2), or mild hepatic impairment (total bilirubin ≤ULN and AST >ULN or total bilirubin 1 to ≤1.5 x ULN and any AST).
The effects of severe renal impairment (eGFR 15 to 29 mL/min/1.73 m2) or ESRD with eGFR <15 mL/min/1.73 m2 not on dialysis or requiring dialysis, or moderate to severe hepatic impairment (total bilirubin >1.5 x ULN and any AST) on the pharmacokinetics of belantamab mafodotin-blmf are unknown.
Drug Interaction Studies
In Vitro Studies: Transporter Systems: Cys‑mcMMAF is a substrate of organic anion transporting polypeptide (OATP)1B1 and OATP1B3, multidrug resistance-associated protein (MRP)1, MRP2, MRP3, bile salt export pump (BSEP), and a possible substrate of P-glycoprotein (P‑gp).
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies have not been conducted with belantamab mafodotin-blmf.
Belantamab mafodotin-blmf was genotoxic in an in vitro micronucleus assay in human lymphocytes through an aneugenic mechanism. These results are consistent with the pharmacological effect of MMAF binding to tubulin causing microtubule depolymerization resulting in spindle disorganization during cell division. Cys-mcMMAF was not mutagenic in the bacterial reverse mutation assay (Ames test), the L5178Y mouse lymphoma forward mutation assay, or the in vivo rat bone marrow micronucleus assay.
Fertility studies have not been conducted with belantamab mafodotin-blmf. Results of repeat-dose toxicity studies with intravenous administration of belantamab mafodotin-blmf in rats indicate the potential for impaired male and female reproductive function and fertility. In rats, weekly dosing for 3 weeks at doses ≥10 mg/kg (approximately 4 times the exposure at the maximum recommended human dose [MRHD] of 2.5 mg/kg based on the AUC of belantamab mafodotin-blmf) resulted in degeneration and atrophy of seminiferous tubules in the testes and luteinized nonovulatory follicles in the ovaries. Findings in females were reversible; findings in the testes were not reversible at the end of the 12-week recovery period with weekly dosing or when given every 3 weeks for 13 weeks at doses ≥10 mg/kg. In male monkeys, the highest dose tested of 10 mg/kg (approximately 4 times the exposure at the MRHD based on AUC of belantamab mafodotin-blmf) given weekly for 13 weeks resulted in seminiferous tubules degeneration in the testes that was fully reversed following the 12-week recovery period.
14 CLINICAL STUDIES
14.1 Relapsed or Refractory Multiple Myeloma
The efficacy of BLENREP was evaluated in DREAMM-2, an open-label, multicenter study (NCT 03525678). Eligible patients had relapsed or refractory multiple myeloma, had previously received 3 or more prior therapies, including an anti-CD38 monoclonal antibody, and were refractory to an immunomodulatory agent and a proteasome inhibitor. Patients had measurable disease by International Myeloma Working Group (IMWG) criteria. Patients with corneal epithelial disease, except mild punctate keratopathy, at baseline were excluded from the study. Patients with mild or moderate renal impairment (eGFR 30 to 89 mL/min/1.73m2) at baseline were also eligible for the study. Patients received either BLENREP 2.5 mg/kg or 3.4 mg/kg intravenously once every 3 weeks until disease progression or unacceptable toxicity. The major efficacy outcome measure was overall response rate as evaluated by an Independent Review Committee (IRC) based on the IMWG Uniform Response Criteria for Multiple Myeloma. Only the results of the recommended dosage of 2.5 mg/kg are described below.
A total of 97 patients received BLENREP at a dose of 2.5 mg/kg administered intravenously once every 3 weeks. The median age was 65 years (range: 39 to 85 years), 53% were male, 74% were White, and 16% were Black. Most patients (77%) were International Staging System (ISS) Stage II or III, 75% had received prior autologous stem cell transplantation (ASCT), and 16% had an Eastern Cooperative Oncology Group (ECOG) performance status of 2. High-risk cytogenetic factors (presence of t[4;14], t[14;16] and 17p13del) were present in 27% of patients. The median number of prior lines of therapy was 7 (range: 3 to 21).
Efficacy results are summarized in Table 6. The median time to first response was 1.4 months (95% CI: 1.0, 1.6). Seventy-three percent of responders had a duration of response ≥6 months.
| a NR = Not reached. | |
|
BLENREP N = 97 |
|
|
Overall response rate (ORR), n (%) (97.5% CI) |
30 (31%) (21%, 43%) |
|
Stringent complete response (sCR), n (%) |
2 (2%) |
|
Complete response (CR), n (%) |
1 (1%) |
|
Very good partial response (VGPR), n (%) |
15 (15%) |
|
Partial response (PR), n (%) |
12 (12%) |
|
Median duration of response in monthsa (range) |
NR [NR to NR] |
16 HOW SUPPLIED/STORAGE AND HANDLING
BLENREP (belantamab mafodotin-blmf) for injection is a sterile, preservative-free, white to yellow lyophilized powder for reconstitution and further dilution prior to intravenous use.
BLENREP is supplied in a carton containing one 100-mg single-dose vial with a rubber stopper (not made with natural rubber latex) and aluminum overseal with removable cap (NDC: 0173-0896-01).
Store vials refrigerated at 36ºF to 46ºF (2ºC to 8ºC).
BLENREP is a hazardous drug. Follow applicable special handling and disposal procedures.1
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Ocular Toxicity
- Advise patients that ocular toxicity may occur during treatment with BLENREP [see Warnings and Precautions (5.1)].
- Advise patients to administer preservative-free lubricant eye drops as recommended during treatment and to avoid wearing contact lenses during treatment unless directed by a healthcare professional [see Dosage and Administration (2.3), Warnings and Precautions (5.1)].
- Advise patients to use caution when driving or operating machinery as BLENREP may adversely affect their vision [see Warnings and Precautions (5.1)].
BLENREP REMS
BLENREP is available only through a restricted program called BLENREP REMS [see Warnings and Precautions (5.2)]. Inform the patient of the following notable requirements:
- Patients must complete the enrollment form with their provider.
- Patients must comply with ongoing monitoring for eye exams [see Warnings and Precautions (5.1)].
Thrombocytopenia
- Advise patients to inform their healthcare provider if they develop signs or symptoms of bleeding [see Warnings and Precautions (5.3)].
Infusion-Related Reactions
- Advise patients to immediately report any signs and symptoms of infusion-related reactions to their healthcare provider [see Warnings and Precautions (5.4)].
Embryo-Fetal Toxicity
- Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to inform their healthcare provider of a known or suspected pregnancy [see Warnings and Precautions (5.5), Use in Specific Populations (8.1, 8.3)].
- Advise women of reproductive potential to use highly effective contraception during treatment and for 4 months after the last dose [see Warnings and Precautions (5.5), Use in Specific Populations (8.3)].
- Advise males with female partners of reproductive potential to use effective contraception during treatment with BLENREP and for 6 months after the last dose [see Use in Specific Populations (8.3), Nonclinical Toxicology (13.1)].
Lactation
- Advise women not to breastfeed during treatment with BLENREP and for 3 months after the last dose [see Use in Specific Populations (8.2)].
Infertility
- Advise males and females of reproductive potential that BLENREP may impair fertility [see Use in Specific Populations (8.3)].
Pneumonitis
- Advise patients to immediately report any new or worsening unexplained pulmonary signs or symptoms to their healthcare provider [see Adverse Reactions (6.1)].
Trademarks are owned by or licensed to the GSK group of companies.
Manufactured by:
GlaxoSmithKline Intellectual Property Development Ltd. England
Brentford, Middlesex, UK TW8 9GS
U.S. License No. 2148
including by use of Potelligent technology licensed from BioWa, Inc.
For:
GlaxoSmithKline
Research Triangle Park, NC 27709
©2022 GSK group of companies or its licensor.
BRP:2PI
|
|
|
What is the most important information I should know about BLENREP? Before you receive BLENREP, you must read and agree to all of the instructions in the BLENREP Risk Evaluation and Mitigation Strategy (REMS). Before prescribing BLENREP, your healthcare provider will explain the BLENREP REMS to you and have you sign the Patient Enrollment Form. BLENREP can cause serious side effects, including: Eye problems. Eye problems are common with BLENREP. BLENREP can cause changes to the surface of your eye that can lead to dry eyes, blurred vision, worsening vision, severe vision loss, and corneal ulcer. Tell your healthcare provider if you have any vision changes or eye problems during treatment with BLENREP.
See “What are the possible side effects of BLENREP?” for more information about serious side effects. |
|
|
What is BLENREP? BLENREP is a prescription medicine used to treat adults with multiple myeloma who:
It is not known if BLENREP is safe and effective in children. |
|
|
Before receiving BLENREP, tell your healthcare provider about all of your medical conditions, including if you:
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. |
|
|
How will I receive BLENREP?
|
|
|
What are the possible side effects of BLENREP? BLENREP can cause serious side effects, including:
|
|
|
|
Tell your healthcare provider right away if you get new or worsening unexplained signs or symptoms of lung problems, including shortness of breath, chest pain, and cough. These are not all the possible side effects of BLENREP. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
|
|
General information about the safe and effective use of BLENREP. Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. You can ask your pharmacist or healthcare provider for information about BLENREP that is written for health professionals. |
|
|
What are the ingredients in BLENREP? Active Ingredient: belantamab mafodotin-blmf Inactive Ingredients: citric acid, disodium edetate dihydrate, polysorbate 80, trehalose dihydrate, trisodium citrate dihydrate. |
|
|
For: GlaxoSmithKline, Research Triangle Park, NC 27709 ©2022 GSK group of companies or its licensor. BRP:2MG |
|
For more information, call GlaxoSmithKline (GSK) at 1-888-825-5249. Trademarks are owned by or licensed to the GSK group of companies. |
|
This Medication Guide has been approved by the U.S. Food and Drug Administration. Revised: 2/2022
PRINCIPAL DISPLAY PANEL
NDC: 0173-0896-01
BLENREP
(belantamab mafodotin-blmf)
for injection
100 mg/vial
CAUTION: Hazardous Agent.
For intravenous infusion after reconstitution and dilution.
Single-dose vial.
Discard unused portion.
No preservative.
No U.S. standard of potency.
Dispense the enclosed Medication Guide to each patient.
©2020 GSK group of companies or its licensor.
Rev. 8/20
62000000041460
| BLENREP
belantamab injection, powder, lyophilized, for solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - GlaxoSmithKline LLC (167380711) |
Trademark Results [Blenrep]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 BLENREP 98155191 not registered Live/Pending |
Glaxo Group Limited 2023-08-29 |
 BLENREP 86451001 5258533 Live/Registered |
Glaxo Group Limited 2014-11-11 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.