PRAZIQUANTEL tablet, film coated
PRAZIQUANTEL by
Drug Labeling and Warnings
PRAZIQUANTEL by is a Prescription medication manufactured, distributed, or labeled by Par Pharmaceutical, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use PRAZIQUANTEL TABLETS safely and effectively. See full prescribing information for PRAZIQUANTEL TABLETS.
PRAZIQUANTEL tablets, for oral use
Initial U.S. Approval: 1982INDICATIONS AND USAGE
Praziquantel tablets are an anthelmintic indicated in patients aged one year and older for the treatment of the following infections: (1)
- Schistosomiasis due to all species of schistosoma (for example, Schistosoma mekongi, Schistosoma japonicum, Schistosoma mansoni and Schistosoma hematobium), and,
- Clonorchiasis and Opisthorchiasis due to the liver flukes, Clonorchis sinensis and Opisthorchis viverrini
DOSAGE AND ADMINISTRATION
- Schistosomiasis: 20 mg/kg body weight 3 times a day separated by 4 to 6 hours for 1 day only. (2.1)
- Clonorchiasis and Opisthorchiasis: 25 mg/kg 3 times a day separated by 4 to 6 hours for 1 day only. (2.1)
- Take with water during meals. Do not chew or keep segments in the mouth. (2.2)
- For pediatric patients under 6 years of age, the tablets may be crushed or disintegrated and mixed with semi-solid food or liquid. (2.2)
- For additional administration instructions see the full prescribing information.
DOSAGE FORMS AND STRENGTHS
- Tablets: 600 mg (with three scores (notches) on the tablet) (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Clinical Deterioration: Potentially life threatening clinical deterioration can occur in patients treated during the acute phase of schistosomiasis. (5.1)
- Central Nervous System (CNS) Effects: Praziquantel can exacerbate central nervous system pathology due to schistosomiasis. Consider whether to administer to individuals reporting a history of epilepsy and/or other signs of potential central nervous systems involvement such as subcutaneous nodules suggestive of cysticercosis. (5.2)
- Potential Lack of Efficacy for Acute Schistosomiasis: This has been reported in observational studies (5.3).
- Cardiac Arrhythmias: Bradycardia, ectopic rhythms, ventricular fibrillation, and AV blocks has been observed with praziquantel administration. Monitor patients with cardiac arrhythmias during treatment (5.4).
ADVERSE REACTIONS
The adverse reactions reported were malaise, headache, dizziness, abdominal discomfort (with or without nausea), pyrexia and urticaria. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Par Pharmaceutical at 1-800-828-9393 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- Other CYP 450 Inducers: Concomitant administration of other CYP450 inducers, for example, antiepileptic drugs and dexamethasone, may also reduce plasma levels concentrations of praziquantel. (7.1)
- CYP450 Inhibitors: Concomitant administration of CYP450 inhibitors, for example, cimetidine, ketoconazole, itraconazole, erythromycin. (7.2)
USE IN SPECIFIC POPULATIONS
- Pediatrics: Safety has not been established in pediatric patients younger than 1 year of age. (8.4)
- Hepatic Impairment: Monitor patients for adverse reactions when administering the recommended dose of praziquantel to hepatosplenic schistosomiasis patients with moderate to severe liver impairment (Child-Pugh Class B or C). (8.6)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 5/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
2.2 Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Clinical Deterioration
5.2 Central Nervous System (CNS) Effects
5.3 Potential Lack of Efficacy During the Acute Phase of Schistosomiasis
5.4 Cardiac Arrhythmias
5.5 Hepatic Impairment in Hepatosplenic Schistosomiasis Patients
5.6 Concomitant Administration with Strong Cytochrome P450 Inducers
6 ADVERSE REACTIONS
7 DRUG INTERACTIONS
7.1 CYP450 Inducers
7.2 CYP450 Inhibitors
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 Renal Impairment
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
Praziquantel tablets are indicated in patients aged 1 year and older for the treatment of the following infections:
- Schistosomiasis due to all species of schistosoma (for example, Schistosoma mekongi, Schistosoma japonicum, Schistosoma mansoni and Schistosoma hematobium), and
- Clonorchiasis and Opisthorchiasis due to the liver flukes, Clonorchis sinensis/Opisthorchis viverrini (approval of this indication was based on studies in which the two species were not differentiated)
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
Schistosomiasis The recommended dosage for the treatment of schistosomiasis is 20 mg/kg body weight administered orally three times a day separated by 4 to 6 hours, for 1 day only.
Clonorchiasis and Opisthorchiasis
The recommended dosage for the treatment of clonorchiasis and opisthorchiasis is 25 mg/kg body weight administered orally three times a day separated by 4 to 6 hours for 1 day only.
2.2 Administration
Take tablets with water during meals. Do not chew or keep the tablets (or parts of tablets) in the mouth; the bitter taste may cause gagging or vomiting. To prevent choking in pediatric patients under 6 years of age, the tablets may be crushed or disintegrated and mixed with semi-solid food or liquid. Use crushed or disintegrated tablets within 1 hour of mixing.
Praziquantel 600 mg tablets have three scores which can be split into four segments at the scores. When broken, each of the four segments contains 150 mg of praziquantel so that the dosage can be adjusted to the patient’s body weight. Segments are broken off by pressing the score (notch) with thumbnails. If one-quarter of a tablet is required, this is best achieved by breaking the segment from the outer end.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Praziquantel is contraindicated in:
- Patients who previously have shown hypersensitivity to praziquantel or any of the excipients in praziquantel tablets.
- Patients with ocular cysticercosis; since parasite destruction within the eye that occurs because of hypersensitivity reaction to the dead parasite after treatment may cause irreversible lesions, ocular cysticercosis must not be treated with praziquantel.
- Patients taking strong Cytochrome P450 (CYP450) inducers, such as rifampin, [see Warnings and Precautions (5.6) and Drug Interactions (7.1,7.2)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Clinical Deterioration
The use of praziquantel in patients with schistosomiasis may be associated with clinical deterioration (for example, paradoxical reactions, serum sickness Jarisch-Herxheimer like reactions: sudden inflammatory immune response suspected to be caused by the release of schistosomal antigens). These reactions predominantly occur in patients treated during the acute phase of schistosomiasis. They may lead to potentially life-threatening events, for example, respiratory failure, encephalopathy, papilledema, and/or cerebral vasculitis.
5.2 Central Nervous System (CNS) Effects
Praziquantel can exacerbate central nervous system pathology due to schistosomiasis, paragonimiasis, or Taenia solium cysticercosis. As a general rule, consider whether to administer praziquantel to individuals reporting a history of epilepsy and/or other signs of potential central nervous systems involvement such as subcutaneous nodules suggestive of cysticercosis unless the potential benefit justifies the potential risk. Hospitalize the patient for duration of treatment when schistosomiasis or fluke infection is found to be associated with cerebral cysticercosis.
5.3 Potential Lack of Efficacy During the Acute Phase of Schistosomiasis
Data from two observational cohort studies in patients indicate that treatment with praziquantel in the acute phase of infection may not prevent progression from asymptomatic infection to acute schistosomiasis, or from asymptomatic infection/acute schistosomiasis into chronic phase.
5.4 Cardiac Arrhythmias
Bradycardia, ectopic rhythms, ventricular fibrillation, and AV blocks has been observed with praziquantel administration. Monitor patients with cardiac arrhythmias during treatment.
5.5 Hepatic Impairment in Hepatosplenic Schistosomiasis Patients
Reduced hepatic metabolism of praziquantel results in higher and sustained plasma concentrations of unmetabolized praziquantel in patients with liver impairment [see Clinical Pharmacology (12.3)]. Monitor patients for adverse reactions when administering the recommended dose of praziquantel to hepatosplenic schistosomiasis patients with moderate or severe liver impairment (Child-Pugh Class B or C).
5.6 Concomitant Administration with Strong Cytochrome P450 Inducers
Concomitant administration of strong CYP450 inducers, such as rifampin with praziquantel is contraindicated since therapeutically effective levels of praziquantel may not be achieved. [see Contraindications (4) and Drug Interactions (7.1)].
In patients receiving rifampin who need immediate treatment for schistosomiasis, alternative agents for schistosomiasis should be considered. However, if treatment with praziquantel is necessary, discontinue rifampin 4 weeks before administration of praziquantel. Treatment with rifampin can then be restarted one day after completion of praziquantel treatment [see Drug Interactions (7.1, 7.2)].
-
6 ADVERSE REACTIONS
The following serious or otherwise important adverse reactions are discussed elsewhere in the labeling:
- Clinical Deterioration [see Warnings and Precautions (5.1)]
- Central Nervous System (CNS) Effects [see Warnings and Precautions (5.2)]
- Potential Lack of Efficacy During the Acute Phase of Schistosomiasis [see Warnings and Precautions (5.3)]
- Cardiac Arrhythmias [see Warnings and Precautions (5.4)]
- Hepatic Impairment in Hepatosplenic Schistosomiasis Patients [see Warnings and Precautions (5.5)]
- Concomitant Administration with Strong Cytochrome P450 Inducers [see Warnings and Precautions (5.6)]
The following adverse reactions associated with the use of praziquantel were identified in clinical studies, published literature or postmarketing reports. Because some of these reactions were reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The following adverse reactions were observed in both adults and pediatric patients:
General disorders and administration site conditions: malaise, pyrexia
Nervous system disorders: headache, dizziness
Gastrointestinal disorders: abdominal discomfort, nausea
Skin and subcutaneous tissue disorders: urticaria
Such adverse reactions may be more frequent and/or serious in patients with a heavy worm burden.
Additional adverse reactions reported from worldwide post marketing experience and from publications with praziquantel and various formulations of praziquantel include:
Blood and lymphatic system disorders: eosinophilia
Cardiac disorders: arrhythmia (including bradycardia, ectopic rhythms, ventricular fibrillation, AV blocks)
Ear and labyrinth disorders: vertigo, tinnitus
Eye disorders: visual disturbance
Gastrointestinal disorders: abdominal pain, bloody diarrhea, vomiting
General disorders and administration site conditions: polyserositis, asthenia, fatigue, gait disturbance
Hepatobiliary disorders: hepatitis
Immune system disorders: allergic reaction, generalized hypersensitivity, anaphylactic reaction
Metabolism and nutrition disorders: anorexia
Musculoskeletal and connective tissue disorders: myalgia
Nervous system disorders: convulsion, somnolence, intention tremor
Respiratory, thoracic and mediastinal disorders: pneumonitis, dyspnea, wheezing
Skin and subcutaneous tissue disorders: pruritus, rash, Stevens-Johnson syndrome
Pediatric patients 1 to 17 years of age treated with praziquantel tablets and various formulations of praziquantel experienced similar adverse reactions as those observed in adult patients.
-
7 DRUG INTERACTIONS
7.1 CYP450 Inducers
Rifampin
Concomitant administration of rifampin, a strong CYP450 inducer, with praziquantel is contraindicated. In patients receiving rifampin, for example, as part of a combination regimen for the treatment of tuberculosis, alternative drugs for schistosomiasis should be considered. If treatment with praziquantel is necessary, treatment with rifampin should be discontinued 4 weeks before administration of praziquantel. Treatment with rifampin can then be restarted one day after completion of praziquantel treatment. [See Contraindications (4), Warnings and Precautions (5.6) and Clinical Pharmacology (12.3).]
Other CYP 450 Inducers
Concomitant administration of other drugs that are CYP450 inducers, for example, antiepileptic drugs (phenytoin, phenobarbital and carbamazepine), and dexamethasone, may also reduce plasma concentrations of praziquantel. [See Warnings and Precautions (5.6).]
7.2 CYP450 Inhibitors
Concomitant administration of drugs that decrease the activity of drug metabolizing liver enzymes (CYP450 inhibitors), for example, cimetidine, ketoconazole, itraconazole, erythromycin may increase plasma concentrations of praziquantel. In addition, grapefruit juice was also reported to produce a 1.6-fold increase in the Cmax and a 1.9-fold increase in the AUC of praziquantel. The effect of this exposure increase on the therapeutic effect and safety of praziquantel has not been systematically evaluated [see Dosage and Administration (2.2)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Published studies have not identified an association with praziquantel use during pregnancy and major birth defects, miscarriage or adverse maternal or fetal outcomes (see Data). In animal reproduction studies conducted in pregnant rats and rabbits no adverse developmental outcomes were observed with oral administration of praziquantel during organogenesis at approximately 0.65 times (rats) or 1.3 times (rabbits) the highest recommended human daily dose of 75 mg/kg/day, based on body surface area.
The estimated background risk of major birth defects and miscarriage for the indicated population are unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Human Data
Two randomized controlled clinical trials have been conducted using praziquantel for the treatment of schistosoma infection in pregnant women. In one randomized controlled trial in pregnant women with schistosoma (S. japonicum) infection, 186 pregnant women were treated with praziquantel compared to 184 women who received placebo. Treatment with praziquantel during pregnancy had no effect on birth weight, and there were no differences in rates of miscarriage, fetal death and major birth defects between the praziquantel-treated and control patients. In another randomized controlled trial that included 2,507 pregnant women in Uganda, 18% of women were infected with schistosoma infection. Treatment with praziquantel during pregnancy had no effect on mean birth weight, perinatal mortality or major birth defects.
In other published studies, including a retrospective observational study, case series and case reports, there have been no reports of major birth defects, stillbirths or other adverse pregnancy outcomes associated with the use of praziquantel during pregnancy.
Animal Data
No evidence of fetal harm was observed in rats and rabbits at praziquantel dose levels of 30 to 300 mg/kg body weight given repeatedly by oral administration during the period of organogenesis. These doses were up to 0.65 times (rats) or 1.3 times (rabbits) the highest recommended human daily dose of 75 mg/kg/day, based on body surface area.
8.2 Lactation
Risk Summary
Limited data from published literature reports the presence of praziquantel in human milk at low concentrations. There is no information on the effects of praziquantel in the breastfed infant or effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for praziquantel and any potential adverse effects on the breastfed infant from praziquantel or from the underlying maternal condition.
8.4 Pediatric Use
Safety and dosing recommendations of praziquantel in pediatric patients 1 to 17 years have been established. Safety of praziquantel in pediatric patients younger than 1 year of age has not been established.
Post-marketing experience and published literature indicates that pediatric patients 1 to 17 years of age treated with praziquantel experience similar adverse reactions as adults treated with praziquantel [see Adverse Reactions (6)].
8.5 Geriatric Use
Clinical studies of praziquantel did not include a sufficient number of subjects ages 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older patients cannot be ruled out. This drug is known to be substantially excreted by the kidney. Because elderly patients are more likely to have decreased renal function, the risk of toxic reactions to this drug may be greater in these patients [see Clinical Pharmacology (12.3)].
8.6 Hepatic Impairment
Following oral administration of praziquantel to patients with liver impairment, reduced hepatic metabolism of praziquantel results in higher and sustained plasma concentrations of unmetabolized praziquantel [see Clinical Pharmacology (12.3)]. Monitor patients for adverse reactions when administering the recommended dose of praziquantel to hepatosplenic schistosomiasis patients with moderate or severe liver impairment (Child-Pugh Class B or C).
8.7 Renal Impairment
No dosage adjustment of praziquantel is necessary in patients with renal impairment. Nephrotoxic effects of praziquantel or its metabolites are not known [see Clinical Pharmacology (12.3)].
-
11 DESCRIPTION
Praziquantel, USP is an anthelmintic, trematodicide provided in tablet form for oral administration.
Praziquantel, USP is 2-(cyclohexylcarbonyl)-1,2,3,6,7,11b-hexahydro-4H-pyrazino[2,1-a] isoquinolin-4-one with the molecular formula; C19H24N2O2. The structural formula is as follows:
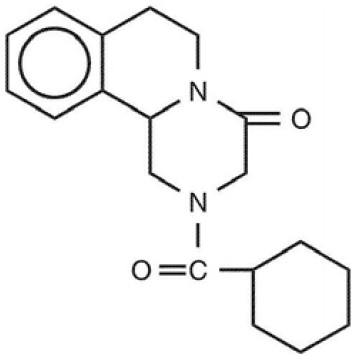
Praziquantel, USP is a white or almost white crystalline powder. The compound is stable under normal conditions and melts at 136°C to 142°C. The active substance is non-hygroscopic. Praziquantel, USP is freely soluble in ethanol (96 per cent) and in methylene chloride, practically insoluble in water.
Praziquantel tablets, USP contain 600 mg of praziquantel, USP. Inactive ingredients: corn starch, croscarmellose sodium, magnesium stearate, microcrystalline cellulose, povidone, sodium lauryl sulfate, polyethylene glycol, titanium dioxide and hypromellose.
-
12 CLINICAL PHARMACOLOGY
12.3 Pharmacokinetics
Absorption
After oral administration, 80% of an administered praziquantel dose is absorbed, with maximal serum concentrations of praziquantel achieved 1 to 3 hours after dosing.
Elimination
Following oral administration of praziquantel, the elimination half-life of praziquantel in serum ranges between 0.8 to 1.5 hours.
Metabolism
Praziquantel is rapidly metabolized by the cytochrome P450 enzyme system and undergoes a first pass effect after oral administration of praziquantel.
Excretion
Approximately 80% of an oral dose of praziquantel is excreted in the kidneys, almost exclusively (greater than 99%) in the form of praziquantel metabolites.
Specific Populations
Patients with Hepatic Impairment
The pharmacokinetics of praziquantel were studied in 40 patients with Schistosoma mansoni infections with varying degrees of hepatic impairment (See Table 1). In patients with schistosomiasis, the pharmacokinetic parameters did not differ significantly between those with normal hepatic function (Group 1) and those with mild (Child-Pugh class A) hepatic impairment. However, in patients with moderate-to-severe hepatic impairment (Child-Pugh class B and C), praziquantel half-life, Cmax, and AUC increased progressively with the degree of hepatic impairment. In Child-Pugh class B, the increases in mean half-life, Cmax, and AUC relative to Group 1 were 1.58-fold, 1.76-fold, and 3.55-fold, respectively. The corresponding increases in Child-Pugh class C patients were 2.82-fold, 4.29-fold, and 15-fold for half-life, Cmax, and AUC.
Table 1: Pharmacokinetic parameters of praziquantel in four groups of patients with varying degrees of liver function following administration of 40 mg/kg of praziquantel tablets under fasting conditions.
Patient
Group
Half-life
(hr)
Tmax
(hr)
Cmax
(mcg/mL)
AUC
(mcg/mL* hr)
Normal hepatic function
(Group 1)
2.99 ± 1.28
1.48 ± 0.74
0.83 ± 0.52
3.02 ± 0.59
Child-Pugh A
(Group 2)
4.66 ± 2.77
1.37 ± 0.61
0.93 ± 0.58
3.87 ± 2.44
Child-Pugh B (Group 3)
4.74 ± 2.16a
2.21 ± 0.78a,b
1.47 ± 0.74a,b
10.72 ± 5.53a,b
Child-Pugh C
(Group 4)
8.45 ± 2.62a,b,c
3.2 ± 1.05a,b,c
3.57 ± 1.30a,b,c
45.35 ± 17.50a,b,c
a) p<0.05 compared to Group 1
b) p<0.05 compared to Group 2
c) p<0.05 compared to Group 3
Patients with Renal Impairment
Excretion of praziquantel following oral administration of praziquantel might be delayed in patients with impaired renal function, but accumulation of unchanged drug would not be expected.
Drug Interaction Studies
Rifampin (CYP450 Inducer)
In a crossover study with a 2-week washout period, 10 healthy subjects ingested a single 40 mg/kg oral dose of praziquantel following pre-treatment with oral rifampin (600 mg daily for 5 days). Plasma praziquantel concentrations were undetectable in 7 out of 10 subjects. When a single 40 mg/kg oral dose of praziquantel was administered to these same healthy subjects two weeks after discontinuation of rifampin, the mean praziquantel AUC and Cmax were 23% and 35% lower, respectively, than when praziquantel was given alone.
12.4 Microbiology
Praziquantel induces a rapid contraction of schistosomes by a specific effect on the permeability of the cell membrane. The drug further causes vacuolization and disintegration of the schistosome tegument. However, the mechanism of action is unknown.
Praziquantel is active against schistosoma (for example, Schistosoma mekongi, Schistosoma japonicum, Schistosoma mansoni and Schistosoma hematobium), and infections due to the liver flukes, Clonorchis sinensis/Opisthorchis viverrini [see Indications and Usage (1)]. Published in vitro data have shown a potential lack of efficacy of praziquantel against migrating schistosomulae [see Warnings and Precautions (5.3)].
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Mutagenicity studies of praziquantel published in the scientific literature are inconclusive. Long term oral carcinogenicity studies in rats and golden hamsters did not reveal any carcinogenic effect at doses up to 250 mg/kg/day (about half of the human daily dose based on body surface area). Praziquantel had no effect on fertility and general reproductive performance of male and female rats when given at oral doses ranging from 30 to 300 mg/kg body weight (up to 0.65 times the human daily dose based on body surface area).
-
16 HOW
SUPPLIED/STORAGE AND HANDLING
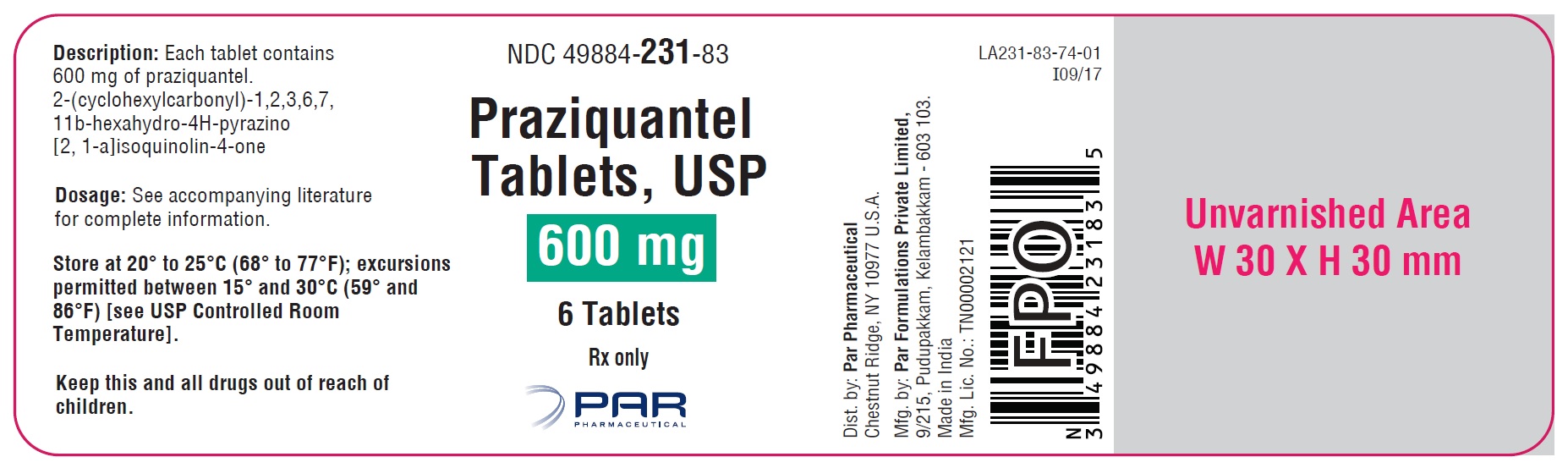
Praziquantel tablets, USP are supplied as 600 mg tablets containing praziquantel, USP. The tablets are white to off white, film-coated, oblong tablet with three scores coded with “PAR” on one side “231” on the reverse side.
Praziquantel tablets, USP 600 mg are available in bottles of 6 tablets (NDC: 49884-231-83).
Store at 20° to 25°C (68° to 77°F); excursions permitted between 15° and 30°C (59° and 86°F) [see USP Controlled Room Temperature].
-
17 PATIENT COUNSELING INFORMATION
- Advise patients to take praziquantel during meals as directed [see Dosage and Administration (2.2)].
- Advise patients not to chew tablets and to take them with water [see Dosage and Administration (2.2)]
- Advise patients that tablets may be crushed or disintegrated and mixed with semi-solid food or liquid or disintegrated to prevent choking in children under 6 years of age. Crushed or disintegrated tablets should be used within 1 hour of mixing [see Dosage and Administration (2.2)].
- Advise patients not to take praziquantel tablets if they are allergic to praziquantel or any of its components [see Contraindications (4)].
- Advise patients not to take praziquantel if they are taking rifampin [see Contraindications (4) and Warnings and Precautions (5.6, 7.1, 7.2)].
- Advise patients that the use of praziquantel can be associated with clinical deterioration during the acute phase of schistosomiasis [see Warnings and Precautions (5.1)].
- Advise patients that praziquantel should not be used if they have epilepsy or other CNS effects [see Warnings and Precautions (5.2)].
- Advise patients to report any cardiac irregularities to their healthcare provider [see Warnings and Precautions (5.4)].
- Advise patients not to drive a car and not to operate machinery on the day of praziquantel treatment and the following day.
Dist. by:
Par Pharmaceutical
Chestnut Ridge, NY 10977 U.S.A.
Mfg. by:
Par Formulations Private Limited,
9/215, Pudupakkam, Kelambakkam - 603 103.
Made in India
Mfg. Lic. No.: TN00002121
OS231-01-74-02
Revised: 05/2019
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
PRAZIQUANTEL
praziquantel tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 49884-231 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PRAZIQUANTEL (UNII: 6490C9U457) (PRAZIQUANTEL - UNII:6490C9U457) PRAZIQUANTEL 600 mg Inactive Ingredients Ingredient Name Strength STARCH, CORN (UNII: O8232NY3SJ) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) POVIDONE (UNII: FZ989GH94E) SODIUM LAURYL SULFATE (UNII: 368GB5141J) POLYETHYLENE GLYCOL 1000 (UNII: U076Q6Q621) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) HYPROMELLOSE 2208 (100 MPA.S) (UNII: B1QE5P712K) Product Characteristics Color WHITE (white to off white) Score 4 pieces Shape RECTANGLE (oblong) Size 22mm Flavor Imprint Code PAR;231 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 49884-231-83 6 in 1 BOTTLE; Type 0: Not a Combination Product 11/27/2017 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA208820 11/27/2017 Labeler - Par Pharmaceutical, Inc. (092733690)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.