SHORT RAGWEED POLLEN injection, solution
Short Ragweed Pollen by
Drug Labeling and Warnings
Short Ragweed Pollen by is a Prescription medication manufactured, distributed, or labeled by Nelco Laboratories, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
BOXED WARNING
(What is this?)
WARNING
Diagnostic and therapeutic allergenic extracts are intended to be administered by a physician who is an allergy specialist and experienced in allergenic diagnostic testing and immunotherapy and the emergency care of anaphylaxis.
This product should not be injected intravenously. Deep subcutaneous routes have been safe. Sensitive patients may experience severe anaphylactic reactions resulting in respiratory obstruction, shock, coma and/or death. (See Adverse Reactions)
Serious adverse reactions should be reported to Nelco Laboratories immediately and a report filed to: MedWatch, The FDA Medical Product Problem Reporting Program, at 5600 Fishers Lane, Rockville, Md. 20852-9787, call 1-800-FDA-1088.
Extreme caution should be taken when using allergenic extracts for patients who are taking beta-blocker medications. In the event of a serious adverse reaction associated with the use of allergenic extracts, patients receiving beta-blockers may not be responsive to epinephrine or inhaled brochodialators.(1)(See Precautions)
Allergenic extracts should be used with caution for patients with unstable or steroid-dependent asthma or underlying cardiovascular disease. (See Contraindications)
-
DESCRIPTION
Allergenic extracts are sterile solutions consisting of the extractable components from various biological sources including pollens, inhalants, molds, animal epidermals and insects. Aqueous extracts are prepared using cocas fluid containing NaCl 0.5%, NaHCO3 0.0275%, WFI, preservative 0.4% Phenol. Glycerinated allergenic extracts are prepared with cocas fluid and glycerin to produce a 50% (v/v) allergenic extract. Allergenic Extracts are supplied as concentrations designated as protein nitrogen units (PNU) or weight/volume (w/v) ratio. Standardized extracts are designated in Bioequivalent Allergy Units (BAU) or Allergy Units (AU). (See product insert for standardized extracts)
For diagnostic purposes, allergenic extracts are to be administered by prick-puncture or intradermal routes. Allergenic extracts are administered subcutaneously for immunotherapy injections.
-
CLINICAL PHARMACOLOGY
The pharmacological action of allergenic extracts used diagnostically is based on the liberation of histamine and other substances when the allergen reacts with IgE antibodies attached to the mast cells. When allergenic extracts are used for immunotherapy, the effect is an increase in immunoglobulin G (IgG) and an increased T suppresser lymphocyte which interferes with the allergic response.(2) With repeated administration of allergenic extracts changes develop in regards to IgG and IgE production and mediator-releasing cells. The histamine release response is reduced in some patients.
-
INDICATIONS AND USAGE
Allergenic extracts are indicated for use in diagnostic testing and as part of a treatment regime for allergic disease, as established by allergy history and skin test reactivity.
Allergenic extracts are indicated for the treatment of allergen specific allergic disease for use as hyposensitization or immunotherapy when avoidance of specific allergens can not be attained. The use of allergenic extracts for therapeutic purpose has been established by well-controlled clinical studies. Allergenic extracts may be used as adjunctive therapy along with pharmacotherapy which includes antihistamines, corticosteroids, and cromoglycate, and avoidance measures. Allergenic extracts for therapeutic use should be given using only the allergen selection to which the patient is allergic, has a history of exposure and are likely to be exposed to again.
-
CONTRAINDICATIONS
Allergenic extracts should not be used if the patient has asthma, cardiovascular disease, emphysema, diabetes, bleeding diathesis or pregnancy, unless a specific diagnosis of type 1 allergic disease is made based on skin testing and the benefits of treatment outweigh the risks of an adverse reaction during testing or treatment. Allergenic extracts are not indicated for use in patients who are not clinically allergic or who are not skin reactive to an allergen. Allergenic extracts should be discontinued or the concentration of potency substantially reduced in patients who experience unacceptable adverse reactions.
-
WARNINGS
Epinephrine 1:1000 should be available.
Concentrated extracts must be diluted with sterile diluent prior to first use on a patient for treatment or intradermal testing. All concentrates of glycerinated allergenic extracts have the ability to cause serious local and systemic reactions including death in sensitive patients. Sensitive patients may experience severe anaphylactic reactions resulting in respiratory obstruction, shock, coma and /or death.(4)(See Adverse Reactions) An allergenic extract should be temporarily withheld from patients or the dose of the extract adjusted downward if any of the following conditions exist: (1) Severe symptoms of rhinitis and/or asthma (2) Infections or flu accompanied by fever and (3) Exposure to excessive amounts of clinically relevant allergen prior to a scheduled injection. When switching patients to a new lot of the same extract the initial dose should be reduced 3/4 so that 25% of previous dose is administered.
-
PRECAUTIONS
GENERAL: Epinephrine 1:1000 should be available as well as personnel trained in administering emergency treatment. Allergenic Extracts are not intended for intravenous injections. For safe and effective use of allergenic extracts, sterile diluents, sterile vials, sterile syringes should be used and aseptic precautions observed when making a dilution and/or administering the allergenic extract injection. A sterile tuberculin syringe graduated in 0.1 ml units to measure each dose for the prescribed dilution should be used. To reduce the risk of an occurrence of adverse reactions, begin with a careful personal history plus a physical exam. Confirm your findings with scratch or intradermal skin testing.
Standardized extracts are those labeled in AU/ml units or BAU/ml units. Standardized extracts are not interchangeable with extracts previously labeled as wt/vol or PNU/ml. Before administering a standardized extract, read the accompanying insert contained with standardized extracts.
Information for Patients: All concentrates of allergenic extracts have the ability to cause serious local and systemic reactions including death in sensitive patients. Patients should be informed of this risk prior to skin testing and immunotherapy. Patients should be instructed to recognize adverse reaction symptoms that may occur and to report all adverse reactions to a physician. Patients should be instructed to remain in the office for 30 minutes during testing using allergenic extracts and at least 30 minutes after therapeutic injections using allergenic extracts.
DRUG INTERACTIONS: Some drugs may affect the reactivity of the skin; patients should be instructed to avoid medications, particularly antihistamines and sympathomimetic drugs, for at least 24 hours prior to skin testing. Antihistamines and Hydroxyzine can significantly inhibit the immediate skin test reactions as they tend to neutralize or antagonize the action of histamine.(3) This effect has been primarily documented when testing was performed within 1 to 2 hours after drug ingestion. Partial inhibition of the skin test reaction had been observed for longer periods. Epinephrine injection inhibits the immediate skin test reactions for several hours. Patients on delayed absorption antihistamine tablets should be free of such medication for 48 hours before testing. Patients using Astemizole (Hismanal) may experience prolonged suppression and should be free from such medication for up to 6 to 8 weeks prior to testing. Refer to package insert from an applicable long acting antihistamine manufacturer for additional information.
Extreme caution should be taken when using allergenic extracts on patients who are taking beta-blockers. Patients on non-selective beta blockers may be more reactive to allergens given for testing or treatment and may be unresponsive to the usual doses of epinephrine used to treat allergic reactions.
Carcinogenesis, mutagenesis, impairment of fertility:
Long term studies in animals have not been conducted with allergenic extracts to determine their potential carcinogenicity, mutagenicity or impairment of fertility.
Pregnancy: Category C: Animal reproduction studies have not been conducted with Allergenic Extracts. It is not known whether allergenic extracts can cause fetal harm when administered to pregnant women or can affect reproduction capacity. Allergenic extracts should be given to pregnant women only if clearly needed.
Nursing Mothers: It is not known whether this drug appears in human milk. Because many drugs are detected in human milk, caution should be exercised when Allergenic Extracts are administered to a nursing woman. There are no current studies on extract components in human milk, or their effect on the nursing infant.
Pediatric Use: Allergenic extracts have been used in children over two years of age.(5)
-
ADVERSE REACTIONS
Adverse systemic reactions usually occur within minutes and consist primarily of allergic symptoms such as: generalized skin erythema, urticaria, pruritus, angioedema, rhinitis, wheezing, laryngeal edema, itching of nose and throat, breathlessness, dyspnea, coughing, hypotension and marked perspiration. Less commonly, nausea, emesis, abdominal cramps, diarrhea and uterine contractions may occur. Severe reactions may cause anaphylaxis or shock and loss of consciousness and rarely death.
The treatment of systemic allergic reactions is dependent upon the system complex. Antihistamines may offer relief of recurrent urticaria, associated skin reactions and gastrointestinal symptoms. Corticosteroids may provide benefit if symptoms are prolonged or recurrent. (See Overdose section)
Local Reactions consisting of erythema, itching, swelling tenderness and sometimes pain may occur at the injection site. These reactions may appear within a few minutes to hours and persist for several days. Local cold applications and oral antihistamines may be effective treatment. For marked and prolonged local reactions the use of antihistamines or anti-inflammatory medications may be dictated. Serious adverse reactions should be reported to Nelco Laboratories immediately and a report can be filed to: MedWatch, The FDA Medical Product Problem Reporting Program, at 5600 Fishers Lane, Rockville, MD 20852-9787, call 1-800-FDA-1088.
-
OVERDOSAGE
Overdose can cause both local and systemic reactions. An overdose may be prevented by careful observation and questioning of the patient about the previous injection.
If systemic or anaphylactic reaction, does occur, apply a tourniquet above the site of injection and inject intramuscularly or subcutaneously 0.3 to 0.5ml of 1:1000 Epinephrine Hydrochloride into the opposite arm. The dose may be repeated in 5-10 minutes if necessary. Loosen the tourniquet at least every 10 minutes. The Epinephrine Hydrochloride 1:1000 dose for infants to 2 years is 0.05 to 0.1 ml, for children 2 to 6 years it is 0.15 ml, for children 6-12 years it is 0.2 ml.
Patients unresponsive to Epinephrine may be treated with Theophylline. Studies on asthmatic subjects reveal that plasma concentrations of Theophylline of 5 to 20 µg/ml are associated with therapeutic effects. Toxicity is particularly apparent at concentrations greater than 20 µg/ml. A loading dose of Aminophylline of 5.8 mg/kg intravenously followed by 0.9 mg/kg per hour results in plasma concentrations of approximately 10 µg/ml for patients not previously receiving theophylline. (Mitenko and Ogilive, Nicholoson and Chick,1973)
Other beta-adrenergic drugs such as Isoproterenol, Isoetharine, or Albuterol may be used by inhalation. The usual dose to relieve broncho-constriction in asthma is 0.5 ml of the 0.5% solution for Isoproterenol HCl. The Albuterol inhaler delivers approximately 90 mcg of Albuterol from the mouthpiece. The usual dosage for adults and children would be two inhalations repeated every 4-6 hours. Isoetharine supplied in the Bronkometer unit delivers approximately 340 mcg Isoetharine. The average dose is one to two inhalations. Respiratory obstruction not responding to parenteral or inhaled bronchodilators may require oxygen, intubation and the use of life support systems.
-
DOSAGE AND ADMINISTRATION
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permits.
The dosage of allergenic extracts is dependent upon the purpose of the administration. Allergenic extracts can be administered for diagnostic use or for therapeutic use.
When allergenic extracts are administered for diagnostic use, the dosage is dependent upon the method used. Two methods commonly used are scratch testing and intradermal testing. Both types of tests result in a wheal and flare response at the site of the test which usually develops rapidly and may be read in 20-30 minutes.
Diagnostic Use: Scratch Testing Method
Scratch testing is considered a simple and safe method although less sensitive than the intradermal test. Scratch testing can be used to determine the degree of sensitivity to a suspected allergen before using the intradermal test. This combination lessens the severity of response to an allergen which can occur in a very sensitive patient.
The most satisfactory testing site is the patient's back or volar surface of the arms from the axilla to 2.5 or 5cm above the wrist, skipping the anti-cubital space. If using the back as a testing site, the most satisfactory area are from the posterior axillary fold to 2.5 cm from the spinal column, and from the top of the scapula to the lower rib margins.
Allergenic extracts for diagnostic use are to be administered in the following manner: To scratch surface of skin, use a circular scarifier. Do not draw blood. Tests sites should be 4 cm apart to allow for wheal and flare reaction. 1-30 scratch tests may be done at a time. A separate sterile scratch instrument is to be used on each patient to prevent transmission of homologous serum hepatitis or other infectious agents from one patient to another.
The recommended usual dosage for Scratch testing is one drop of allergen applied to each scratch site. Do not let dropper touch skin. Always apply a control scratch with each test set. Sterile Diluent (for a negative control) is used in exactly the same way as an active test extract. Histamine may be used as a positive control. Scratch or prick test sites should be examined at 15 and 30 minutes. To prevent excessive absorption, wipe off antigens producing large reactions as soon as the wheal appears. Record the size of the reaction.
Interpretation of Scratch Test
Skin tests are graded in terms of the wheal and erythema response noted at 10 to 20 minutes. Wheal and erythema size may be recorded by actual measurement as compared with positive and negative controls. A positive reaction consists of an area of erythema surrounding the scarification that is larger than the control site. For uniformity in reporting reactions, the following system is recommended. (6)
REACTION SYMBOL CRITERIA Negative - No wheal. Erythema absent or very slight (not more than 1 mm diameter). One Plus + Wheal absent or very slight erythema present (not more than 3 mm diameter). Two Plus ++ Wheal not more than 3mm or erythema not more than 5mm diameter. Three Plus +++ Wheal between 3mm and 5mm diameter, with erythema. Possible pseudopodia and itching. Four Plus ++++ A larger reaction with itching and pain. Diagnostic Use: Intradermal Skin Testing Method
Do not perform intradermal test with allergens which have evoked a 2+ or greater response to a Scratch test. Clean test area with alcohol, place sites 5 cm apart using separate sterile tuberculin syringe and a 25 gauge needle for each allergen. Insert needle tip, bevel up, into intracutaneous space. Avoid injecting into blood vessel, pull back gently on syringe plunger, if blood enters syringe change position of needle. The recommended dosage and range for intradermal testing is 0.05 ml of not more than 100 pnu/ml or 1:1000 w/v (only if puncture test is negative) of allergenic extract. Inject slowly until a small bleb is raised. It is important to make each bleb the same size.
Interpretation of Intradermal Test:
The patient's reaction is graded on the basis of size of wheal and flare as compared to control. Use 0.05 ml sterile diluent as a negative control to give accurate interpretation. The tests may be accurately interpreted only when the saline control site has shown a negative response. Observe patient for at least 30 minutes. Tests can be read in 15-20 minutes. Edema, erythema and presence of pseudopods, pain and itching may be observed in 4 plus reactions. For uniformity in reporting reactions the following system is recommended. (6)
REACTION SYMBOL CRITERIA Negative - No increase in size of bleb since injection. No erythema. One Plus + An increase in size of bleb to a wheal not more than 5mm diameter, with associated erythema. Two Plus ++ Wheal between 5mm and 8mm diameter with erythema. Three Plus +++ Wheal between 8mm and 12mm diameter with erythema and possible pseudopodia and itching or pain. Four Plus ++++ Any larger reaction with itch and pain, and possible diffuse blush of the skin surrounding the reaction area. Therapeutic Use: Recommended dosage & range
Check the listed ingredients to verify that it matches the prescription ordered. When using a prescription set, verify the patient's name and the ingredients listed with the prescription order. Assess the patient's physical and emotional status prior to giving as injection. Do not give injections to patients who are in acute distress. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Dosage of allergenic extracts is a highly individualized matter and varies according to the degree of sensitivity of the patient, his clinical response and tolerance to the extract administered during the early phases of an injection regimen. The dosage must be reduced when transferring a patient from non-standardized or modified extract to standardized extract. Any evidence of a local or generalized reaction requires a reduction in dosage during the initial stages of immunotherapy as well as during maintenance therapy. After therapeutic injections patients should be observed for at least 20 minutes for reaction symptoms.
The following schedule may act as a guide. This schedule has not been proven to be safe or effective. Sensitive patients may begin with smaller doses of weaker solutions and the dosage increments can be less.
STRENGTH DOSE VOLUME Vial #1 1 0.05 1:100,000 w/v 2 0.10 10 pnu/ml 3 0.15 1 AU/ml 4 0.20 1 BAU/ml 5 0.30 6 0.40 7 0.50 Vial #2 8 0.05 1:10,000 w/v 9 0.10 100 pnu/ml 10 0.15 10 AU/ml 11 0.20 10 BAU/ml 12 0.30 13 0.40 14 0.50 Vial #3 15 0.05 1:1,000 w/v 16 0.10 1,000 pnu/ml 17 0.15 100 AU/ml 18 0.20 100 BAU/ml 19 0.30 20 0.40 21 0.50 Vial #4 22 0.05 1:100 w/v 23 0.07 10,000 pnu/ml 24 0.10 1,000 AU/ml 25 0.15 1,000 BAU/ml 26 0.20 27 0.25 Maintenance Refill 28 0.25 1:100 w/v 29 0.25 10,000 pnu/ml 30 0.25 1,000 AU/ml 31 0.25 1,000 BAU/ml 32 0.25 subsequent doses 33 0.25 All dilutions may be made using sterile buffered diluent. The calculation may be based on the following ratio:
Volume desired x Concentration desired = Volume needed x Concentration available.
Example 1: If a 1:10 w/v extract is available and it is desired to use a 1:1,000 w/v extract substitute as follows:
Using a sterile technique, remove 0.10 ml of extract from the 1:10 vial and place it into a vial containing 9.90 ml of sterile diluent. The resulting ratio will be a 10 ml vial of 1:1,000 w/v.
Example 2: If a 10,000 pnu/ml extract is available and it is desired to use a 100 pnu/ml extract substitute as follows:
Using a sterile technique, remove 0.10 ml of extract from the 10,000 pnu/ml vial and place it into a vial containing 9.90 ml of sterile diluent. The resulting concentration will be a 10 ml vial of 100 pnu/ml.
Example 3: If a 10,000 AU/ml or BAU/ml extract is available and it is desired to use a 100 AU/ml or BAU/ml extract substitute as follows: Vd x Cd = Vn x Ca
Using a sterile technique, remove 0.10 ml of extract from the 10,000 AU/ml or BAU/ml vial and place it into a vial containing 9.90 ml of sterile diluent. The resulting concentration will be 10ml vial of 100 AU/ml or BAU/ml.
Intervals between doses: The optimal interval between doses of allergenic extract has not been definitely established. The amount of allergenic extract is increased at each injection by not more than 50%-100% of the previous amount and the next increment is governed by the response to the last injection. There are three generally accepted methods of pollen hyposensitizing therapy.
Treatment starts each year 6 to 8 weeks before onset of seasonal symptoms. Maximal dose reached just before symptoms are expected. Injections discontinued during and following season until next year.
Patient is first treated during season with symptoms. Low initial doses are employed to prevent worsening of condition. This is followed by an intensive schedule of therapy (i.e. injections given 2 to 3 times per week). Fewer Allergists are resorting to this Co-seasonal therapy because of the availability of more effective, symptomatic medications that allow the patient to go through a season relatively symptom free.
Initially this is the same as pre seasonal. The allergen is administered twice weekly or weekly for about 20 injections to achieve the maximum tolerated dose. Then, maintenance therapy may be administered once a week or less frequently.
Duration of Treatment: The usual duration of treatment has not been established. A period of two or three years of injection therapy constitutes an average minimum course of treatment.
-
HOW SUPPLIED
Allergenic extracts are supplied with units listed as: Weight/volume (W/V), Protein Nitrogen Units (PNU/ml), Allergy Units (AU/ml) or Bioequivalent Allergy Units (BAU/ml).
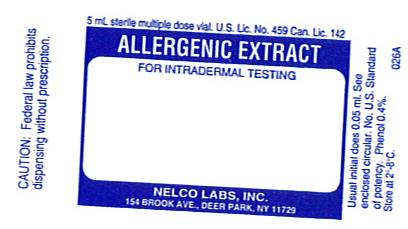
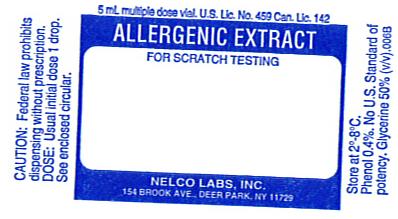
Diagnostic Scratch: 5 ml dropper application vials
Diagnostic Intradermal: 5 ml or 10 ml vials.
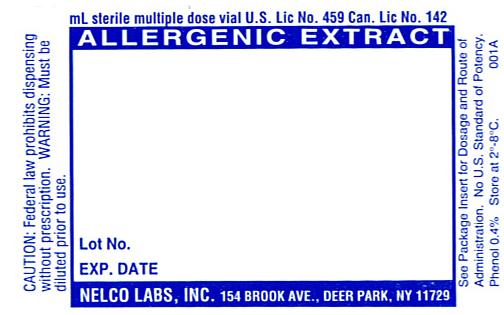
Therapeutic Allergens: 5 ml, 10 ml, 50 ml multiple dose vials.
-
STORAGE
The expiration date of allergen extracts is listed on the container label. Store extracts upon arrival at 2° to 8°C and keep them in this range during office use.
WARRANTY:We warrant that this product was prepared and tested according to the standards of the FDA and is true to label. Because of biological differences in individuals and because allergenic extracts are manufactured to be potent and because we have no control over the conditions of use, we cannot and do not warrant either a good effect or against an ill effect following use.
-
REFERENCES
1 Jacobs, Robert L., Geoffrey W.Rake,Jr., et.al. Potentiated Anaphylaxis in Patients with Drug-induced Beta-adrenergic Blockade. J.Allergy & Clin. Immunol., 68(2): 125-127. August 1981.
2 Ishizaka,K.: Cellular Events in the IgE Antibody Response. Adv. in Immuno. 23:50-75, 1976.
3. Lockey, R.F., Bukantz, S.C., Allergen Immunotherapy. New York,NY: Marcel Dekker Inc., 1991.
4. Reid,M.J., Lockey,R.F., Turkeltaub,P.C., Platts-Mills,T.A.E., Survey of fatalities from skin testing and immunotherapy 1985-1989. Journal of Allergy Clin. Immunol. 92 (1): 6-15, July 1993.
5. Murray, A.B., Ferguson, A., Morrison, B., The frequency and severity of cat allergy vs dog allergy in atopic children. J. Allergy Clin. Immunolo: 72, 145-9, 1983.
6. Lockey, R.F., Bukantz, S.C., Allergen Immunotherapy. New York,NY: Marcel Dekker Inc., 1991.
ADDITIONAL INSTRUCTIONS DOSAGE FORM AND ROUTE OF ADMINISTRATION FOR USE OF ALLERGENIC EXTRACTS CONTAINING SHORT RAGWEED POLLEN
This is a supplement to Directions for Use and Suggested Dosage Schedule for Therapeutic Allergenic Extracts
INFORMATION RELATING TO ANTIGEN E
Antigen E Content in Concentrate: This product is compounded and diluted on a PNU or W/V basis. Extracts containing Short Ragweed Pollen also bear a labeled potency in terms of Antigen E content. The amount of Antigen E is expressed as units of Antigen E per mL of extract. Antigen E units are approximately equal to micrograms previously used to measure Antigen E concentration. Antigen E assay provides a measure of extract potency related to the E antigen in Short Ragweed, rather than only an expression of extract strength such as Protein Nitrogen Units (PNU) or Weight/Volume (W/V).
Example: Short Ragweed pollen extracted at 1:10 W/V usually assays within a range Of 70,000-100,000 PNU/mL and 100-400 AgE Units. (Analytical accuracy of the Antigen E assay is ±25%) Most treatment programs are W/V concentration of 1:100 to 1:20 or a PNU/mL concentrate of 20,000 to 40,000.
This would give a 70-100 AgE unit/mL concentration of Short Ragweed extract (Tall and Short Ragweed mix would be 1/2 this value).
New extraction lots of Short Ragweed will be labeled ac¬cording to W/V or PNU in addition to Antigen E content.
Antigen E Content in Mixtures: The Antigen E value applies only to the concentration of the Short Ragweed antigens contained in a concentrate. The Antigen E value does not express the total potency of the extract if Short Ragweed is mixed with another allergenic extract. Labeled Antigen content of extracts containing Short Ragweed at a concentration more dilute than a concentrate is determined by calculation. The formulae used for such calculations is given by:
V1 = Volume of extract you wish to prepare
V2 = Volume of extract you need for dilution
C1 = Concentration (W/V, PNU/mL, units Antigen E/mL) you wish to prepare
C2 = Concentration of extract to be used
Therapeutic allergens are available in l0mL and 50mL sterile multiple dose vials as individual allergens, stock mixture or mixture prescribed by the physician. Therapeutic allergens are standardized according to weight/volume.
Antigen E Short Ragweed and Tall and Short Ragweed mixture allergenic extracts are available in l0mL and 50mL dose vials at 1:10 and 40,000 PNU/mL aqueous or 1:20 and 20,000 PNU/mL with 50% glycerin.
SHORT RAGWEED AND MIXED RAGWEED
(Mixed Ragweed/equal parts ofShort and Tall)
WARNING: This product is intended for use by or under the guidelines of physicians experienced and trained in the use allergenic extracts for hyposensitization and who are experienced in the emergency treatment of anaphylaxis.
The practitioner should have available the following: Epinephrine, tourniquet, parenteral fluids, bronchodilators, cardioactive drugs, as well as adequate oxygenation required for endotracheal intubation, emergency cricothyrotomy, or transtracheal catheterization if patient cannot be intubated.
In the event of systemic reactions characterized by one or more of the following: sneezing, mild to severe generalized urticaria, itching other than at the injection site, extensive or generalized edema, wheezing, asthma, dyspnea, cyanosis, tachycardia, lacrimation, marked perspiration, cough, hypotension, syncope, shock and upper airway obstruction, all of which may result in death, the following steps should taken: application of a tourniquet above the injection site and administration of 0.2 mL to 1.0 mL of Epinephrine Injection 1:1000 are recommended. Maximal recommended dose children under 2 years of age is 0.3 mL. Maximal recommended dose for children between 2 and 12 years of age is 0.5 mL. Following customary technique, the tourniquet is gradually released. The tourniquet should not be left in place without loosening for 90 seconds every 15 minutes. Volume expanders and vasopressor agents may be required to reverse hypotension. Inhaled bronchodialators and parenteral aminophylline may be required to reverse bronospasm.
Pregnancy Category C (Short Ragweed) - Animal reproduction studies have not been conducted with Short Ragweed. It is also not known whether Short Ragweed can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Short Ragweed should be given to a pregnant woman only if clearly needed.
Pediatricis use: There is conflicting evidence as to the effectiveness of AgE extracts in children. Some studies have shown a decrease in clinical symptomatology.
1. Extract should be inspected visually for particulate matter and discoloration prior to administration whenever solution and product container permit.
2. In addition to the active ingredients - Short Ragweed pollen extract - this product contains 0.4% phenol as a preservative and as inactive ingredients - 0.5% NaCl and 0.275% NaHCO3.
3. All extracts are aseptically filled.
4. This product should be stored upon arrival at 2º C to 8º C as determined by stability data furnished by the FDA showing rapid drop in potency at temperatures above refrigerated temperatures for non-glycerinated products. 50% glycerin extracts maintain AgE stability much longer.
Cumulative AgE dosage of less than 0.1 unit is not immunizing for most patients. This should not be interpreted as meaning that 0.1 unit is the maximum tolerated dosage. It has been shown that moderately sensitive patients may tolerate a dosage of ten to fifty times greater. For extremely sensitive patients who do not respond to treatment, the physician might consider immunotherapy with an alternative to the conventional aqueous allergenic extract.
This product is intended for use in the amelioration of symptoms associated with Short Ragweed allergy. If this is adjunctive therapy, beware of any regimen which might interfere with existing medications. Studies show that sufficient antigen dosage immunotherapy gives moderate or significant relief from Ragweed hayfever in adults.
Justification for use of this therapy can be derived from patient questionaires, daily diaries, respiratory function tests of airflow and lung volume and by immunological tests such as: leukocyte histamine release, measurement of allergenic specific IgE. lgG and IgA antibodies in serum and secretions, allergen provocation tests to skin, nose and lung.
This product should not be used if the patient has a considerable identifiable risk such as asthma, cardiovascular disease, emphysema, diabetes or pregnancy, unless a specific diagnosis of type 1 allergy is made based on skin testing and the benefits of treatment are felt to outweigh the risks of an adverse reaction during testing or treatment.
Defined as undesirable effects that are reasonably associated with product use, such as the following effects on various organ systems: erythema and pruritis of the skin, asthma effecting the lungs, tachycardia and angioedema of the heart and rhinitis of the nasal membranes.
Those reactions are mainly due to the interaction of allergen (antigen) with IgE specific antibodies, but other causes have not been excluded. For example, endotoxins, other types of reactions resuiting from prolonged immunotherapy, such as immune complex disease have been suggested as theoretical possibilities but not documented.
General Precautions: Sterile solutions, vials, syringes, etc. should be used and aseptic precautions observed in making dilutions. Dilution preparations should be tested for sterility. The usual precautions to be observed in administering extracts are necessary.
A sterile tuberculin syringe graduated in 0.1 mL units to measure each dose from the prescribed dilution should be used.
A treatment schedule is related directly to patient's sensitivity as determined first by skin testing and continuously by response to therapeutic doses. The potency of the intial injections should be adjusted to the patient's sensitivity. 1/10 of the lowest concentration producing positive ID skin test is usually safe.
Injections are administered subcutaneously, care to avoid injecting into blood vessels should be observed (Withdraw plunger gently. If blood appears, use a new injection site). A separate heat sterilized or sterile disposable syringe and needle should be used for each individual patient to prevent the transmission of homologous serum hepatitis and other infectious agents from one person to another.
Patient should always be observed for at least 30 minutes after any injection. If adverse reactions appear, the next therapeutic injection of extract should be reduced to the dose which does not elicit a reaction and subsequent doses increased more slowly.
A. 0.01 AgE/mL B. (0.005 AgE/mL) 0.1 AgE/mL (0.05 AgE/mL) 1.0 AgE/mL (0.5 AgE/mL) 10 AgE/mL (5 AgE/mL) 100 AgE/mL (50 AgE/mL) Dose No. Dose mL Dose No. Dose mL Dose No. Dose mL Dose No. Dose mL Dose No. Dose mL 1 .03 7 .03 13 .03 19 .03 25 .03 2 .05 8 .05 14 .05 20 .05 26 .05 3 .08 9 .08 15 .08 21 .08 27 .08 4 .12 10 .12 16 .12 22 .12 28 .12 5 .20 11 .20 17 .20 23 .20 29 .20 6 .30 12 .30 18 .30 24 .30 30 .30 Frequently dilutions of 1:100,000 W/V are prepared as the initial dilution or, in terms of Antigen E concentration, approximately 0.01 to 0.05 AgE units. For individuals which are hypersensitive, a more dilute extract is recommended, e.g. 1:1,000,000 W/V or 0.001 to 0.005 Antigen E/mL. A dose of 0.03 to 0.05 mL of this initial concentration is used initially and gradually increased in units of 0.03 mL (see above schedule) until a tolerance dose is reached or symptoms are controlled. Should a marked local reaction occur, the dosage should be lowered to a non-reactive dose before increasing once again.
Allergenic extracts become less potent with age. Should it therefore become necessary to treat a patient with a vial bearing a later expiration date, the initial dose of the extract should be lowered to a safe, non-reacting level.
Extremely sensitive patients may react to 0.01 units AgE or less on intradermal skin testing. For these patients a safe dose may be between 0.0004 and 0.0008 units of AgE requiring 100 fold dilution from dose one listed in the recommended table.
In transferring patients from unstandardized to standardized product, the physician should establish the potency relationship, perhaps by comparative skin testing at equal concentration, prior to injecting the first standardized dose.
1.Lowell. F.C., et. al., "Journal of Allergy" 34, 165 (1963)
2.Ibid. "New Eng. Journal of Medicine" 273, 675 (1965)
3.Lichtenstein, L.M. et. al., "American Journal of Medicine" 44, 514 (1968)
4.Lichtenstein, L.M. et. al., "Journal of Allergy and Clinical Immunology" 61, 370 (1978)
5.Van Metre, T.E. and Lichtenstein, L.M. et. al., "Journal of Allergy and Clinical Immunology" 60, 181 (1982)
6.Lessof and Lippincott, "Immunologic Apsects of Allergy" 81, 300 (1981)
- CONTAINER LABELING
-
INGREDIENTS AND APPEARANCE
SHORT RAGWEED POLLEN
short ragweed pollen injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 36987-3384 Route of Administration INTRADERMAL, SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AMBROSIA ARTEMISIIFOLIA POLLEN (UNII: K20Y81ACO3) (AMBROSIA ARTEMISIIFOLIA POLLEN - UNII:K20Y81ACO3) AMBROSIA ARTEMISIIFOLIA POLLEN 20000 [PNU] in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) SODIUM BICARBONATE (UNII: 8MDF5V39QO) PHENOL (UNII: 339NCG44TV) WATER (UNII: 059QF0KO0R) GLYCERIN (UNII: PDC6A3C0OX) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 36987-3384-1 5 mL in 1 VIAL, MULTI-DOSE 2 NDC: 36987-3384-2 10 mL in 1 VIAL, MULTI-DOSE 3 NDC: 36987-3384-3 30 mL in 1 VIAL, MULTI-DOSE 4 NDC: 36987-3384-4 50 mL in 1 VIAL, MULTI-DOSE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA102203 04/08/1983 SHORT RAGWEED POLLEN
short ragweed pollen injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 36987-3385 Route of Administration INTRADERMAL, SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AMBROSIA ARTEMISIIFOLIA POLLEN (UNII: K20Y81ACO3) (AMBROSIA ARTEMISIIFOLIA POLLEN - UNII:K20Y81ACO3) AMBROSIA ARTEMISIIFOLIA POLLEN 40000 [PNU] in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) SODIUM BICARBONATE (UNII: 8MDF5V39QO) PHENOL (UNII: 339NCG44TV) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 36987-3385-1 5 mL in 1 VIAL, MULTI-DOSE 2 NDC: 36987-3385-2 10 mL in 1 VIAL, MULTI-DOSE 3 NDC: 36987-3385-3 30 mL in 1 VIAL, MULTI-DOSE 4 NDC: 36987-3385-4 50 mL in 1 VIAL, MULTI-DOSE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA102203 04/08/1983 SHORT RAGWEED POLLEN
short ragweed pollen injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 36987-3387 Route of Administration INTRADERMAL, SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AMBROSIA ARTEMISIIFOLIA POLLEN (UNII: K20Y81ACO3) (AMBROSIA ARTEMISIIFOLIA POLLEN - UNII:K20Y81ACO3) AMBROSIA ARTEMISIIFOLIA POLLEN 0.05 g in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) SODIUM BICARBONATE (UNII: 8MDF5V39QO) PHENOL (UNII: 339NCG44TV) WATER (UNII: 059QF0KO0R) GLYCERIN (UNII: PDC6A3C0OX) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 36987-3387-1 5 mL in 1 VIAL, MULTI-DOSE 2 NDC: 36987-3387-2 10 mL in 1 VIAL, MULTI-DOSE 3 NDC: 36987-3387-3 30 mL in 1 VIAL, MULTI-DOSE 4 NDC: 36987-3387-4 50 mL in 1 VIAL, MULTI-DOSE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA102203 04/08/1983 SHORT RAGWEED POLLEN
short ragweed pollen injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 36987-3388 Route of Administration INTRADERMAL, SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AMBROSIA ARTEMISIIFOLIA POLLEN (UNII: K20Y81ACO3) (AMBROSIA ARTEMISIIFOLIA POLLEN - UNII:K20Y81ACO3) AMBROSIA ARTEMISIIFOLIA POLLEN 0.1 g in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) SODIUM BICARBONATE (UNII: 8MDF5V39QO) PHENOL (UNII: 339NCG44TV) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 36987-3388-1 5 mL in 1 VIAL, MULTI-DOSE 2 NDC: 36987-3388-2 10 mL in 1 VIAL, MULTI-DOSE 3 NDC: 36987-3388-3 30 mL in 1 VIAL, MULTI-DOSE 4 NDC: 36987-3388-4 50 mL in 1 VIAL, MULTI-DOSE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA102203 04/08/1983 SHORT RAGWEED POLLEN
short ragweed pollen injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 36987-3453 Route of Administration INTRADERMAL, SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AMBROSIA ARTEMISIIFOLIA POLLEN (UNII: K20Y81ACO3) (AMBROSIA ARTEMISIIFOLIA POLLEN - UNII:K20Y81ACO3) AMBROSIA ARTEMISIIFOLIA POLLEN 0.1 g in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) SODIUM BICARBONATE (UNII: 8MDF5V39QO) PHENOL (UNII: 339NCG44TV) WATER (UNII: 059QF0KO0R) GLYCERIN (UNII: PDC6A3C0OX) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 36987-3453-1 5 mL in 1 VIAL, MULTI-DOSE 2 NDC: 36987-3453-2 10 mL in 1 VIAL, MULTI-DOSE 3 NDC: 36987-3453-3 30 mL in 1 VIAL, MULTI-DOSE 4 NDC: 36987-3453-4 50 mL in 1 VIAL, MULTI-DOSE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA102203 04/08/1983 Labeler - Nelco Laboratories, Inc. (054980867) Registrant - Nelco Laboratories, Inc. (054980867) Establishment Name Address ID/FEI Business Operations Nelco Laboratories, Inc. 054980867 manufacture
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.