STANDARDIZED MITE DERMATOPHAGOIDES FARINAE injection, solution STANDARDIZED MITE DERMATOPHAGOIDES PTERONYSSINUS injection, solution
Standardized Mite Dermatophagoides pteronyssinus by
Drug Labeling and Warnings
Standardized Mite Dermatophagoides pteronyssinus by is a Prescription medication manufactured, distributed, or labeled by Nelco Laboratories, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
BOXED WARNING
(What is this?)
WARNINGS
Standardized Allergenic Extract is intended for use by physicians who are experienced in the administration of standardized (AU/mL) allergenic extracts for immunotherapy and the emergency care of anaphylaxis, or for use under the guidance of an allergy specialist. Standardized allergenic extracts are not directly interchangeable with other allergenic extracts. The initial dose must be based on skin testing as described in the DOSAGE AND ADMINISTRATION section of this insert. Patients being switched from other types of extract to standardized allergenic extracts should be started as though they were coming under treatment for the first time. Standardized Mite extract is NOT directly interchangeable with non-standardized Mite extract.
This product should not be injected intravenously. Deep subcutaneous routes have proven to be safe. Sensitive patients may experience severe anaphylactic reactions resulting in respiratory obstruction, shock, coma and/or death.(14) Patients should be observed for at least 30 minutes following treatment and emergency measures and personnel trained in their use should be immediately available in the event of a life threatening reaction. (See Precautions)
Allergenic extracts may be used with caution for patients with unstable or steroid-dependent asthma or with underlying cardiovascular disease. (Contraindications)
Extreme caution should be taken when using allergenic extracts for patients who are taking beta-blocker medications. In the event of a serious adverse reaction associated with the use of allergenic extracts, patients receiving beta-blockers may not be responsive to epinephrine or inhaled bronchodialators.
Serious adverse reactions should be reported to Nelco Laboratories immediately and a report filed to: MedWatch, The FDA Medical Product Problem Reporting Program, at 5600 Fishers Lane, Rockville, Md. 20852-9787, call 1-800-FDA-1088.
-
DESCRIPTION
Standardized mite extract is a sterile injectable solution containing the extractable of Dermatophagoides farinae or Dermatophagoides pteronyssinus, 0.5% NaCl, 0.08% Na2HPO4, 0.036% KH2PO4, distilled water for injection, 0.4%, phenol as preservative and 50% glycerin by volume in sterile containers. All extracts are aseptically filled. Standardized mite extract is to be administered by prick-puncture or intradermal routes when used for diagnostic purposes and administered subcutaneously when used for immunotherapy injections.
It has been recognized that mites are one of the most common allergens in House Dust (1,2). Recent research and extensive clinical trials have shown that the mite component is important enough to separate it from the other antigenic components of House Dust. The two species of Dermatophagoides are found in the United States.(4)
Persons thought to be allergic to House Dust should be tested for sensitivity to mites. Standardized extracts have been prepared to diagnose and treat with D. farinae and D. pteronyssinus.
The Allergy Units are assigned to these extracts based on the relative potency by ELISA Inhibition to the Center for Biologics Evaluation and Research (CBER) reference. The CBER mite reference preparation has been assigned 10,000 AU/mL, based on quantitative skin assays.(11)
Extracts are prepared from supplied raw material containing greater than 99% pure adult mites and mite stages by actual count. The mites have been grown on a medium containing yeast and pork products. Cleaning of the raw material removes at least 99% of the medium. This medium contains no material of human origin. The extracting fluid contains 0.5% NaCl, 0.08% Na2HPO4, 0.036% KH2PO4, distilled water for injection, 0.4% phenol as preservative and 50% glycerin by volume as stabilizer.
The raw material is extracted with diluent, glycerinated, and the potency on the label is expressed in Allergy Units (AU/mL). Several manufacturers submitted intradermal skin test data on Biopol Laboratories mite medium extract using patients who were puncture test positive (Σ E ≥ 40 mm) to either D. farinae or D. pteronyssinus extracts. By intradermal testing, there was 1 positive (Σ E ≥ 20 mm) in 44 individuals at an estimated 1% level of medium contamination of mites and 4 positives in 40 individuals at an estimated 10% contamination.(5) Two of the individuals who were skin test positive to mite extract and who were also skin test positive to mite medium extract were also skin tested by the puncture method with an extract of yeast (Sacchoromyces spp) and were positive.
-
CLINICAL PHARMACOLOGY
The mode of action of allergenic extracts is still under investigation. The pharmacological action of allergenic extracts used diagnostically is based on the liberation of histamine and other substances when the allergen reacts with IgE antibodies attached to the mast cells. When allergen extracts are used for therapeutic immunotherapy, the effect is an increase in immunoglobulin G (IgG) and an increased T suppresser lymphocyte which interferes with the allergenic response.(15) Although immunotherapy may be considered as immunosuppression, in which the production of allergen-specific antibody is inhibited, the mechanism of the clinical effectiveness of immunotherapy remains under investigation.
-
INDICATIONS AND USAGE
Standardized mite allergenic extracts are intended for use in the diagnosis and therapy of D.farinae and D.pteronyssinus mite allergy, as established by allergy history and skin test reactivity (6,10). Standardized Mite extracts are not interchangeable with non standardized mite extracts. To select patients for a confirmation of allergic disease diagnosis and/or treatment with allergen extracts, screening tests should be done using in vivo identification testing methods (i.e. scratch or intradermal testing).(13)
Standardized mite extract containing equal parts of D.farinae and D.pteronyssinus is intended for therapy only. The use of standardized mites extract is indicated for hypersensitization treatment and may be used as part of the over-all management of the allergic patient. This treatment is particularly to be recommended when a patient's sensitivity to mite has been determined initially by scratch or intradermal skin tests.
-
CONTRAINDICATIONS
This product should not be used if the patient has asthma, cardiovascular disease, emphysema, diabetes, bleeding diathesis or pregnancy, unless a specific diagnosis of type 1 allergy to mite is made based on skin testing and the benefits of treatment outweigh the risks of an adverse reaction during testing or treatment. Mite extracts are not indicated for use in patients who are not clinically allergic to mite or who are not skin reactive to mite. Limitations on treatment using mite extract should be considered when treating very young patients, geriatric patients or patients suffering from auto-immune disorders or severe and unstable allergic conditions.
-
WARNINGS
Standardized Mites extract labeled in AU/mL are not interchangeable with non-standardized mite extracts.
Concentrated extracts must be diluted with sterile diluent prior to first use on a patient for treatment or intradermal testing.
DO NOT INJECT INTRAVENOUSLY. All concentrates of allergenic extracts have the ability to cause serious local and systemic reactions including death in sensitive patients. Sensitive patients may experience severe anaphylactic reactions resulting in respiratory obstruction, shock, coma and /or death. Allergenic extract should be temporarily withheld from patients or the dose of the extract adjusted downward if any of the following conditions exist: (1) Severe symptoms of rhinitis and/or asthma, (2) Infections or flu accompanied by fever and (3) Exposure to excessive amounts of clinically relevant allergen prior to a scheduled injection.
-
PRECAUTIONS
Epinephrine 1:1000 should be available as well as personnel trained in administering emergency treatment. Allergenic Extracts are not intended for intravenous injections. For safe and effective use of allergen extracts, sterile diluent, sterile vials, sterile syringes should be used and aseptic precautions observed when making a dilution and/or administering the allergen extract injection. A sterile tuberculin syringe graduated in 0.1 mL units to measure each dose for the prescribed dilution should be used. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
To reduce the risk of an occurrence of adverse reactions, begin with a careful personal history plus a physical exam. Confirm your findings with scratch or intradermal skin testing. Patients should be observed for 30 minutes after any test.
Information for Patients: All concentrates of allergen extracts including standardized pollen extracts, have the potential to cause serious local and systemic reactions including death, in sensitive patients. To minimize this potential hazard, the relative sensitivity of the patient must be assessed from an allergic history and from clinical observations. In certain individuals, life-threatening reactions may occur. Patients should be informed of this risk prior to skin testing and immunotherapy. Patients should be instructed to recognize adverse reaction symptoms that may occur and to report all adverse reactions to a physician. Patients should be told to wait in the office after injections for at least 30 minutes.
Drug Interaction: Antihistamines and Hydroxyzine can significantly inhibit the immediate skin test reactions as they tend to neutralize or antagonize the action of histamine (14). This effect has been primarily documented when testing was performed within 1 to 2 hours after drug ingestion. Although partial inhibition of the skin test reaction had been observed for longer periods, it was minor. Epinephrine injection inhibits the immediate skin test reactions for several hours. Patients on delayed absorption antihistamine tablets should be free of such medication for 48 hours before testing. Patients using Astemizole (Hismanal) may experience prolonged suppression and should be free from such medication for up to 6 to 8 weeks prior to testing. Refer to package insert from applicable long acting antihistamine manufacturers for additional information. In the event of a serious adverse reaction, patients receiving beta-blockers may not be responsive to epinephrine or inhaled bronchodilators.
Carcinogenesis, mutagenesis, impairment of fertility.
Long term studies in animals have not been conducted with allergenic extracts, especially mite extracts, to determine their potential carcinogenicity, mutagenicity or impairment of fertility.
Pregnancy: Category C. Animal reproduction studies have not been conducted with D. farinae or D. pteronyssinus mite extracts, it is not known whether this extract can incur fetal harm when administered to a pregnant women or can effect reproduction capacity. Standardized D.farinae or D.pteronyssinus Mite extract should be given to pregnant women and nursing mothers only if clearly needed.
Nursing Mothers: It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when Allergenic Extract, Standardized Mites, is administered to a nursing woman. There are no current studies on secretion of the extract components in human milk, or their effect on the nursing infant.
Pediatric Use: Children have been used extensively as patients in studies with mite extracts. However, it is recommended that children be treated only when indicated (6,7,8). Allergenic extracts have been tested in children over two years of age (9). (See WARNINGS and ADVERSE REACTIONS).
-
ADVERSE REACTIONS
Anaphylaxis and other systemic reactions may occur such as induced asthma, itching of nose and throat, breathlessness, urticaria and local reactions. Local reactions can be defined as an area of large erythema, swelling or pruritus at the injection site. Further indications of adverse reactions are edema, wheezing, dyspnea, locomotive impairment, marked perspiration, coughing, hypertension, shock and upper airway obstruction.
Adverse systemic reactions usually occur within minutes and consist primarily of allergic symptoms such as generalized skin erythema, urticaria, pruritus, angioedema, rhinitis, wheezing, laryngeal edema and hypotension. Less commonly, nausea, emesis, abdominal cramps, diarrhea and uterine contractions may occur. Severe reactions may cause shock and loss of consciousness. Fatalities have occurred rarely. These systemic reactions occur with varying frequency in different clinics. To some extent, the reaction rate is related to the type and dose of administered extract and to the degree of sensitivity of the patient. Despite all precautions, occasional reactions are unavoidable.
Reports from regulatory authorities in Sweden to the Center for Biologics Evaluation and Research (CBER) indicated that several deaths have been associated with the use of mite extracts. The CBER was subsequently informed that these deaths may have been related to use by physicians or other health professionals untrained in the administration of potent allergens rather than a product defect. It should be noted that anaphylaxis and deaths following the injection of mite extracts have also been reported by the British Committee on Safety in Medicine in the British Medical Journal, V293,pp948,1986.
Local reactions consisting of erythema, itching, swelling tenderness and sometimes pain may occur at the injection site. These reactions may appear within a few minutes to hours and persist for several days. Local cold applications and oral antihistamines may be effective treatment. For marked and prolonged local reactions steroids may be helpful.
-
OVERDOSAGE
Overdose can cause both local and systemic reactions. Overdose is prevented by careful observation and questioning of the patient about the previous injection.
The treatment of systemic allergic reactions is dependent upon the symptom complex. In cases of an occurrence of a systemic or anaphylactic reaction, apply a tourniquet above the site of injection and inject intramuscularly or subcutaneously 0.3 to 0.5mL of 1:1000 Epinephrine Hydrochloride into the opposite arm. The dose may be repeated in 5-10 minutes if necessary. Loosen the tourniquet at least every 10 minutes. The Epinephrine Hydrochloride 1:1000 dose for infants to 2 years is 0.05 to 0.1 mL: for children 2 to 6 years it is 0.15 mL:, for children 6-12 years it is 0.2 mL.
Patients unresponsive to Epinephrine may be treated with Theophylline. Studies on asthmatic subjects reveal that plasma concentrations of Theophylline of 5 to 20 µg/mL are associated with therapeutic effects. Toxicity is particularly apparent at concentrations greater than 20 µg/mL. A loading dose of Aminophylline of 5.8 mg/kg intravenously followed by 0.9 mg/kg per hour results in plasma concentrations of approximately 10 µg/mL. (Mitenko and Ogilive, Nicholoson and Chick,1973)
Other beta-adrenergic drugs such as Isoproterenol, Isoetharine, or Albuterol may be used by inhalation. The usual dose to relieve broncho-constriction in asthma is 0.5 mL or the 0.5% solution for Isoproterenol HCl. The Albuterol inhaler delivers approximately 90 mcg of Albuterol from the mouthpiece. The usual dosage for adults and children would be two inhalations repeated every 4-6 hours. Isoetharine supplied in the Bronkometer unit delivers approximately 340 mcg Isoetharine. The average dose is one to two inhalations.
Respiratory obstruction not responding to parenteral or inhaled bronchodilators may require Theophylline, oxygen, intubation and the use of life support systems. Parenteral fluid and/or plasma expanders may be utilized for treatment of shock. Adrenocorticosteroids may be administered parenterally or intravenously.
Antihistamines may offer relief of recurrent urticaria, associated skin reactions and gastrointestinal symptoms. Persistent wheezing may necessitate intravenous aminophylline treatment. For profound shock and hypotension, intravenous fluids, vasopressor and oxygen may also be needed. Maintenance of a patent airway is critical if upper and lower airway obstruction is present. Corticosteroids may provide benefit if symptoms are prolonged or recurrent.
-
DOSAGE AND ADMINISTRATION
It is imperative that the physician determine the initial dose of the product by skin testing. Patients being switched from a Standardized Mite extract to a new Standardized Mite extract (both labeled in AU/mL) should be skin tested with both extracts to determine the relative potency of the extracts and the dosage adjusted accordingly.
For safe and effective use of allergen extracts, sterile solutions, vials, syringes, etc. should be used and aseptic precautions observed in making dilution's. The usual precautions to be observed in administering extracts are necessary. A sterile tuberculin syringe graduated in 0.1 mL units to measure each dose for the prescribed dilution should be used.
Recommended dosage and range:(Diagnostic) The concentration of Standardized Mite extract for Scratch or Prick-puncture testing is 10,000 AU/mL, glycerinated, supplied in 5 mL dropper vials. Skin tests are graded in terms of the wheal and erythema response noted at 10 to 20 minutes. Wheal and erythema size may be recorded by actual measurement or the extent of both responses.
Prick-puncture tests on Mite allergic subjects: 10 puncture tests (bifurcated needle) on mite allergic subjects yielded the following:
# Person Mean sum of wheal Range Mean sum of Erythema Range (mm) D. farinae 10 17.4 mm 12-21 mm 78.8 mm 63-97 mm D. pteronyssinus 10 18.0 mm 10-37 mm 68.7 mm 46-114 mm Intradermal tests (using 0.05 mL) on 10 puncture positive patients AU/mL to elicit 50 mm sum of dia. of erythema reaction (10)
# Persons Mean Range (AU/mL) D. farinae 10 0.029 AU/mL 0.077-0.005 AU/mL D. pteronyssinus 10 0.024 AU/mL 0.78-0.0004 AU/mL Patients with a negative scratch or prick-puncture test: Patients who do not react to a valid scratch or prick- puncture test should be tested intradermally with a 0.02 to 0.05 mL of a 50 AU/mL extract solution. If this test is negative, a second intradermal test may be performed using a 100 AU/mL extract dilution. The negative puncture test control must be diluted appropriately for ID use. It is supplied in 5 mL and 10 mL vials of 50% glycerin (v/v).
To prepare a 50 AU/mL dilution from 10,000 AU/mL vial:
Take 5.0mL of 10,000AU/mL + 5.0 mL of diluent = Vial A @5,000 AU/mL.
Take 1.0 of Vial A + 9.0 mL diluent = Vial B @ 500 AU/mL.
Take 1.0 of Vial B + 9.0 mL diluent = Vial C @ 50 AU/mL.
Patients tested only by the intradermal method: Patients being suspected of being highly allergic should be tested with 0.02 to 0.05 mL of a 0.1 AU/mL dilution.(3) A negative test should be followed by repeat tests using progressively stronger concentrations until the maximal recommended strength of 100 AU/mL is reached. The negative puncture test control must be diluted appropriately for intradermal use. It is supplied in 5 mL and 10 mL vials of 50% glycerin (v/v).
Recommended dosage and range: (Therapeutic) Dosage of allergenic extracts is a highly individualized matter and varies according to the degree of sensitivity of the patient, his clinical response and tolerance to the extract administered during the early phases of an injection regimen. In patients who appear to be highly sensitive by history and skin test, the initial dose of the extract should be 0.1 mL of 0.01 to 0.1 AU/mL. Patients with lesser sensitivity may be started at 1.0 to 10.0 AU/mL. The amount of allergenic extract is increased at each injection by not more than 50%-100% of the previous amount, and the next increment is governed by the response to the last injection. Large local reactions which persist longer than 24 hours are generally considered an indication for repeating the previous dose or reducing the dose. Any evidence of systemic reaction is an indication for a significant reduction (at least 50%) for the subsequent dose. Maximum dosage has not been established however, the upper limits of l mL of 10,000 AU/mL may be painful due to glycerin content. The dosage of allergenic extract does not vary significantly with the allergic disease under treatment.
After therapeutic injections patients should always be observed for at least 30 minutes. If adverse reactions appear, the next therapeutic injection of extract should be reduced to the dose which does not elicit a reaction and subsequent doses increased slowly. If local reactions occur, reduce subsequent injections to a dose which did not elicit this reaction.
Preparation Instructions: To prepare dilution for intradermal and therapeutic use, one starts with 10,000 AU/mL concentrate and makes a 1:10 dilution by adding 1.0 mL of the concentrate to 9.0 mL of sterile diluent. Subsequent dilution's are made in similar manner.
TEN-FOLD DILUTION SERIES Dilution Extract Diluent mL AU/mL 0 Concentrate 0 10,000 1 1 mL concentrate 9 1,000 2 1 mL dilution #1 9 100 3 1 mL dilution #2 9 10 4 1 mL dilution #3 9 1 5 1 mL dilution #4 9 0.1 6 1 mL dilution #5 9 0.01 Intervals between doses: The optimal interval between doses of allergenic extract has not been definitely established. However, as it is customary practiced, injections are given 1,2, or 3 times per week until the maintenance dose of extract is reached. At this time, the injection interval may be increased to 2 weeks, then 3 weeks and finally to 4 weeks. If the patient does not return for 6-8 weeks after the last injection, the dose should be reduced to 25% of the last dose. If longer than 8 weeks, a dose reduction of 1,2, or 3 dilution's may be made depending on a consideration of the components and the patient's sensitivity. The dosage and the interval between injections may need to be modified according to the clinical response of the patient. When switching patients to a fresh extract the initial dose should be reduced 3/4 so that 25% of previous dose is administered.(14)
Duration of Treatment: The usual duration of treatment has not been established. A period of two or three years of injection therapy constitutes an average minimum course of treatment.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
-
HOW SUPPLIED
Diagnostic Allergens- Scratch or Prick test: 10,000 AU/mL, 50% glycerin in 5 mL dropper vials.
Intradermal test- 100 AU/mL in 5 mL or 10 mL sterile multiple dose vials.
Therapeutic allergens - In 5 mL, 10 mL, 50 mL multiple dose vials as individual allergens, stock mixture containing 5000 AU/mL of D. farinae plus 5000 AU/mL of D. pteronyssinus, or mixture prescribed by physician.
Dilution's of concentrate can be made with either buffered diluent with 0.4% phenol or 50% glycerin (v/v) with salts.
-
STORAGE
The expiration date of Standardized Mite extract containing 10,000 AU/mL in 50% glycerin (v/v) is listed on the container label. Store extracts upon arrival at 2° to 8°C and keep them in this range during office use.
WARRANTY: We warrant that this product was prepared and tested according to the standards of the FDA and is true to label. Because of biological differences in individuals and because allergenic extracts are manufactured to be potent and because we have no control over the conditions of use, we cannot and do not warrant either a good effect or against an ill effect following use.
-
REFERENCES
1. Wharton, G.W.: House Dust Mites, J.Med. Entomol.12:577,1976.
2. Vorhorst.R., M.Spieksnma and Varekamp: House Dust atopy and the house mite. Linden, Stafleu's Scientific Publishing Co.,1969.
3. Bear,H. :Allergy to House Dust Mites. Immuno Allergy Practice. 5:356, 1983.
4. Lang, J.D. and S.Mulla: Distribution and abundance of House Dust Mites.Dermatophagoides (Spp) in different zones of Southern California. Environmental Entomology 6:123, 1977.
5. Seltzer,J.M. Standardization and Relative Potency of D.farinae extract. Jour.Allergy and Clin.Immuno. Vol. 77 p204, 1986.
6. Murray,A.B. A.C. Ferguson, B.J. Morrison: Diagnosis of House Dust Mite Allergy in asthmatic children. J. Allergy Clin. Immuno. 71:21, 1983.
7. Warner,J.O., J.F.Price, J.F. Soothill, Controlled trials of hyposensitization to D.pteronyssinus in children with asthma. Lancet 2:912, 1978.
8. Smith, A.P. Hyposentization with D.pteronyssinus antigen. Trials in asthma induced by house dust. Br.Med.4.204,1971.
9. Glasser,J., Allergy in Childhood. C. Thomas, 29, 1956.
10. Pauli,G, J.C.Bessot, R.Thierry, A.Lamensons:Correlation between skin tests, inhalation tests and specific IgE in a study of 120 subjects allergic to house dust and D.pteronyssinus. Clin.Allergy 7:337,1977.
11. Quantitative Intradermal Procedure for Evaluation of Subject Sensitivity to Standardized Allergenic Extracts and for Assignment of Bioequivalent Allergy Units to Reference Preparations using the ID50EAL method. Methods & Procedures Manual, CBER, 1993.
12. Lockey,R., L.M.Benedict, P.C.Turkeltaub, S.O.Bukantz. Fatalities from immunotherapy and skin testing. J.Allergy Clin Immuno.,79(4), 1987.
13. Evans,R., H. Pence, H.Kaplan, R.Rockllin: The Effect of Immunotherapy on Humoral and Cellular Response in Ragweed Hayfever. J.Clin.Inv. 57, 1976.
14. Gleich, G., J.W. Younginger: The RAST test: A Method to Measure IgE Antiboides and the Potency of Allergy Extracts, N.Y. Acad. Sci.57 (7), 1981.
15. Ishizaka,K.: Cellular Events in the IgE Antibody Response. Adv. in Immuno. 23:50-75, 1976.
16. Bousquet.J.,Djoukadar, F.Hewitt, B.Guerin, B.Michel, Comparison of the stability of a mite and a pollen extract stored in normal conditions of use.Clin.Allergy, 15,1985.
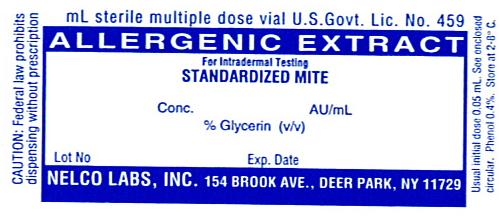
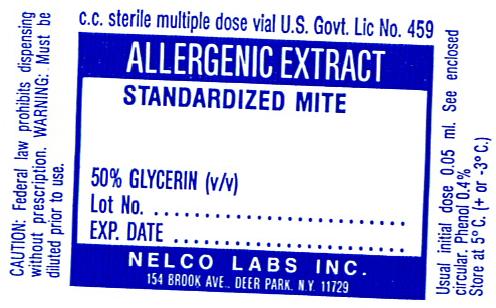
- CONTAINER LABELING
-
INGREDIENTS AND APPEARANCE
STANDARDIZED MITE DERMATOPHAGOIDES FARINAE
standardized mite dermatophagoides farinae injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 36987-1844 Route of Administration SUBCUTANEOUS, INTRADERMAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength DERMATOPHAGOIDES FARINAE (UNII: PR9U2YPF3Q) (DERMATOPHAGOIDES FARINAE - UNII:PR9U2YPF3Q) DERMATOPHAGOIDES FARINAE 10000 [AU] in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) SODIUM PHOSPHATE, DIBASIC (UNII: GR686LBA74) POTASSIUM PHOSPHATE, MONOBASIC (UNII: 4J9FJ0HL51) WATER (UNII: 059QF0KO0R) PHENOL (UNII: 339NCG44TV) GLYCERIN (UNII: PDC6A3C0OX) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 36987-1844-1 5 mL in 1 VIAL, MULTI-DOSE 2 NDC: 36987-1844-2 10 mL in 1 VIAL, MULTI-DOSE 3 NDC: 36987-1844-3 30 mL in 1 VIAL, MULTI-DOSE 4 NDC: 36987-1844-4 50 mL in 1 VIAL, MULTI-DOSE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA102193 06/12/1987 STANDARDIZED MITE DERMATOPHAGOIDES PTERONYSSINUS
standardized mite dermatophagoides pteronyssinus injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 36987-1845 Route of Administration SUBCUTANEOUS, INTRADERMAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength DERMATOPHAGOIDES PTERONYSSINUS (UNII: 57L1Z5378K) (DERMATOPHAGOIDES PTERONYSSINUS - UNII:57L1Z5378K) DERMATOPHAGOIDES PTERONYSSINUS 10000 [AU] in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) SODIUM PHOSPHATE, DIBASIC (UNII: GR686LBA74) POTASSIUM PHOSPHATE, MONOBASIC (UNII: 4J9FJ0HL51) WATER (UNII: 059QF0KO0R) PHENOL (UNII: 339NCG44TV) GLYCERIN (UNII: PDC6A3C0OX) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 36987-1845-1 5 mL in 1 VIAL, MULTI-DOSE 2 NDC: 36987-1845-2 10 mL in 1 VIAL, MULTI-DOSE 3 NDC: 36987-1845-3 30 mL in 1 VIAL, MULTI-DOSE 4 NDC: 36987-1845-4 50 mL in 1 VIAL, MULTI-DOSE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA102194 02/22/1990 Labeler - Nelco Laboratories, Inc. (054980867) Registrant - Nelco Laboratories, Inc. (054980867) Establishment Name Address ID/FEI Business Operations Nelco Laboratories, Inc. 054980867 manufacture
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.