GLIMEPIRIDE by International Laboratories, LLC / Dr. Reddy's Laboratories Limited GLIMEPIRIDE tablet
GLIMEPIRIDE by
Drug Labeling and Warnings
GLIMEPIRIDE by is a Prescription medication manufactured, distributed, or labeled by International Laboratories, LLC, Dr. Reddy's Laboratories Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use glimepiride safely and effectively. See full prescribing information for glimepiride.
GLIMEPIRIDE tablets, for oral use
Initial U.S. Approval: 1995INDICATIONS AND USAGE
DOSAGE AND ADMINISTRATION
Recommended starting dose is 1 or 2 mg once daily. Increase in 1 or 2 mg increments no more frequently than every 1 to 2 weeks based on glycemic response. Maximum recommended dose is 8 mg once daily (2.1).
Administer with breakfast or first meal of the day (2.1).
Use 1 mg starting dose and titrate slowly in patients at increased risk for hypoglycemia (e.g., elderly, patients with renal impairment) (2.1).DOSAGE FORMS AND STRENGTHS
Tablets (scored): 1 mg, 2 mg, 4 mg (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
Hypoglycemia: May be severe. Ensure proper patient selection, dosing, and instructions, particularly in at-risk populations (e.g., elderly, renally impaired) and when used with other anti-diabetic medications (5.1).
Hypersensitivity Reactions: Postmarketing reports include anaphylaxis, angioedema and Stevens-Johnson Syndrome. Promptly discontinue glimepiride, assess for other causes, institute appropriate monitoring and treatment, and initiate alternative treatment for diabetes (5.2).
Hemolytic Anemia: Can occur if glucose 6-phosphate dehydrogenase (G6PD) deficient. Consider a non-sulfonylurea alternative. (5.3).
Potential Increased Risk of Cardiovascular Mortality with Sulfonylureas: Inform patient of risks, benefits and treatment alternatives (5.4).
Macrovascular Outcomes: No clinical studies establishing conclusive evidence of macrovascular risk reduction with glimepiride or any other anti-diabetic drug (5.5).ADVERSE REACTIONS
Common adverse reactions in clinical trials (≥5% and more common than with placebo) include hypoglycemia, headache, nausea, and dizziness (6.1).
To report SUSPECTED ADVERSE REACTIONS, contact Dr. Reddy’s Laboratories, Inc. at 1-888-375-3784 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
Certain medications may affect glucose metabolism, requiring glimepiride tablets dose adjustment and close monitoring of blood glucose (7.1).
Miconazole: Severe hypoglycemia can occur when glimepiride and oral miconazole are used concomitantly. (7.2).
Cytochrome P450 2C9 interactions: Inhibitors and inducers of cytochrome P450 2C9 may affect glycemic control by altering glimepiride plasma concentrations (7.3).
Colesevelam: Coadministration may reduce glimepiride absorption. Glimepiride should be administered at least 4 hours prior to colesevelam (2.1, 7.4).USE IN SPECIFIC POPULATIONS
Pregnancy: Based on animal data, may cause fetal harm (8.1).
Nursing Mothers: Discontinue glimepiride or nursing taking into consideration the importance of glimepiride to the mother (8.3).
Pediatric Patients: Not recommended because of adverse effects on body weight and hypoglycemia (8.4).
Geriatric or Renally Impaired Patients: At risk for hypoglycemia with glimepiride. Use caution in dose selection and titration, and monitor closely (8.5, 8.6).See 17 for PATIENT COUNSELING INFORMATION.
Revised: 10/2017
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Important Limitations of Use
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosing
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hypoglycemia
5.2 Hypersensitivity Reactions
5.3 Hemolytic Anemia
5.4 Increased Risk of Cardiovascular Mortality with Sulfonylureas
5.5 Macrovascular Outcomes
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Drugs Affecting Glucose Metabolism
7.2 Miconazole
7.3 Cytochrome P450 2C9 Interactions
7.4 Concomitant Administration of Colesevelam
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Monotherapy
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
17.1 Information for Patients
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosing
Glimepiride tablets should be administered with breakfast or the first main meal of the day.
The recommended starting dose of glimepiride tablets are 1 mg or 2 mg once daily. Patients at increased risk for hypoglycemia (e.g., the elderly or patients with renal impairment) should be started on 1 mg once daily [see Warnings and Precautions (5.1) and Use in Specific Populations (8.5, 8.6)].
After reaching a daily dose of 2 mg, further dose increases can be made in increments of 1 mg or 2 mg based upon the patient’s glycemic response. Uptitration should not occur more frequently than every 1 to 2 weeks. A conservative titration scheme is recommended for patients at increased risk for hypoglycemia [see Warnings and Precautions (5.1) and Use in Specific Populations (8.5, 8.6)].
The maximum recommended dose is 8 mg once daily.
Patients being transferred to glimepiride tablets from longer half-life sulfonylureas (e.g., chlorpropamide) may have overlapping drug effect for 1 to 2 weeks and should be appropriately monitored for hypoglycemia.
When colesevelam is coadministered with glimepiride, maximum plasma concentration and total exposure to glimepiride is reduced. Therefore, glimepiride tablets should be administered at least 4 hours prior to colesevelam.
-
3 DOSAGE FORMS AND STRENGTHS
Glimepiride tablets USP, are formulated as tablets of:
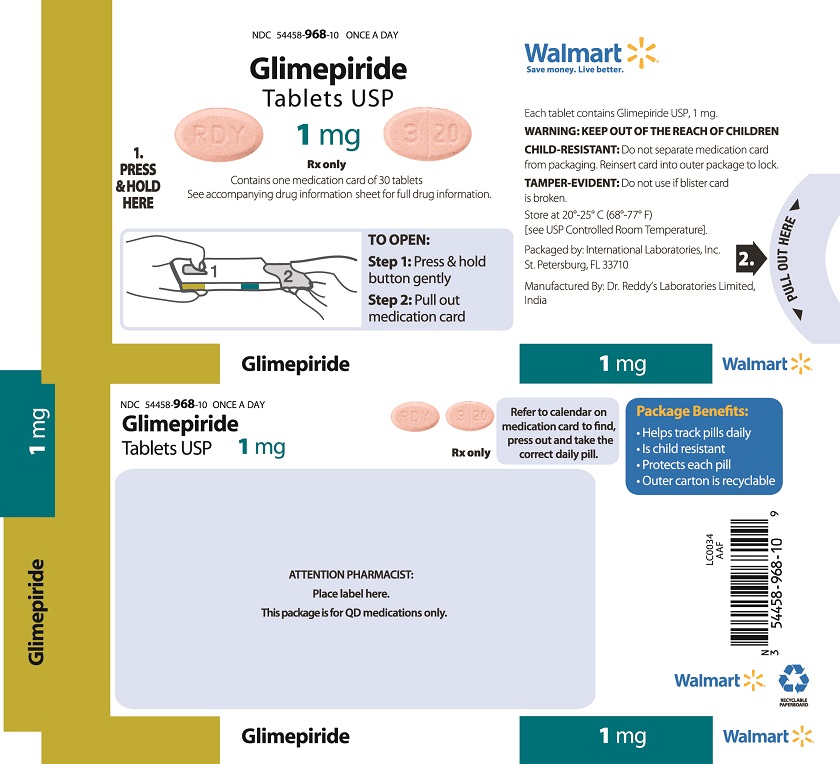
Glimepiride tablets USP, 1 mg are peach, oval, flat bevelled edged, uncoated tablets debossed “RDY” on one side and “320” separating “3” and “20” with bisect line scoring on the other side.
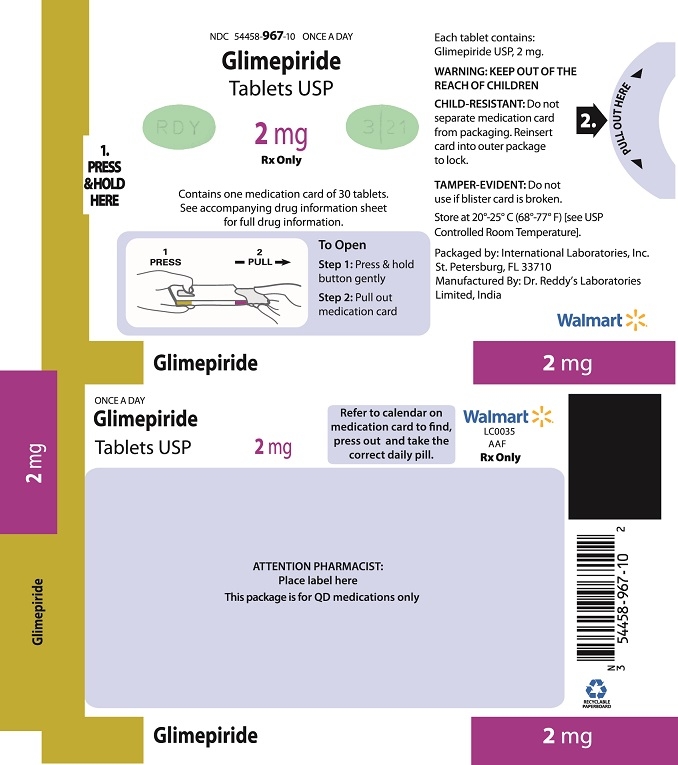
Glimepiride tablets USP, 2 mg are green, oval, flat bevelled edged, uncoated tablets debossed “RDY” on one side and “321” separating “3” and “21” with bisect line scoring on the other side.
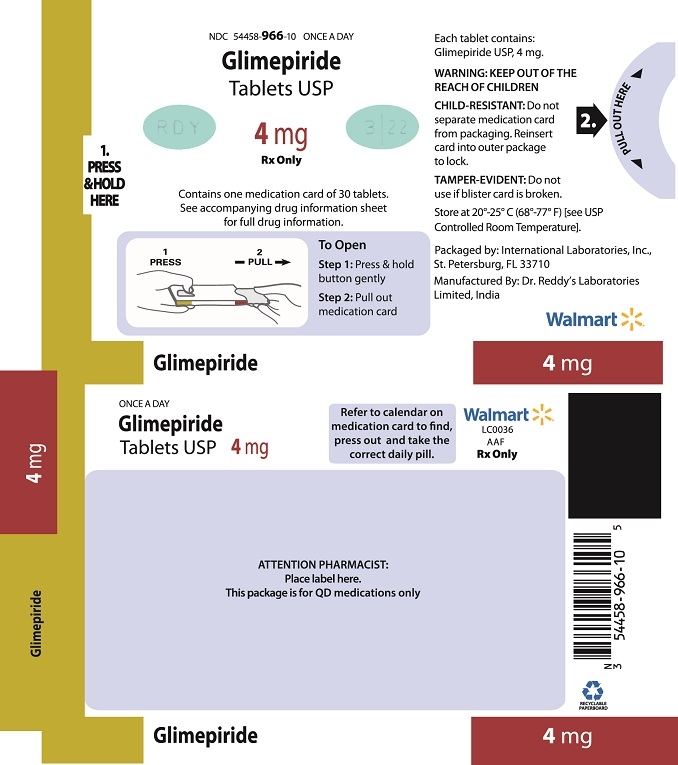
Glimepiride tablets USP, 4 mg are blue, oval, flat bevelled edged, uncoated tablets debossed “RDY” on one side and “322” separating “3” and “22” with bisect line scoring on the other side.
-
4 CONTRAINDICATIONS
Glimepiride tablets are contraindicated in patients with a history of a hypersensitivity reaction to:
- Glimepiride or any of the product’s ingredients [see Warnings and Precautions (5.2)].
Sulfonamide derivatives: Patients who have developed an allergic reaction to sulfonamide derivatives may develop an allergic reaction to glimepiride. Do not use glimepiride in patients who have a history of an allergic reaction to sulfonamide derivatives.
Reported hypersensitivity reactions include cutaneous eruptions with or without pruritus as well as more serious reactions (e.g. anaphylaxis, angioedema, Stevens-Johnson Syndrome, dyspnea) [see Warnings and Precautions (5.2) and Adverse Reactions (6.2)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Hypoglycemia
All sulfonylureas, including glimepiride, can cause severe hypoglycemia [see Adverse Reactions (6.1)]. The patient's ability to concentrate and react may be impaired as a result of hypoglycemia. These impairments may present a risk in situations where these abilities are especially important, such as driving or operating other machinery. Severe hypoglycemia can lead to unconsciousness or convulsions and may result in temporary or permanent impairment of brain function or death.
Patients must be educated to recognize and manage hypoglycemia. Use caution when initiating and increasing glimepiride tablets doses in patients who may be predisposed to hypoglycemia (e.g., the elderly, patients with renal impairment, patients on other anti-diabetic medications). Debilitated or malnourished patients, and those with adrenal, pituitary, or hepatic impairment are particularly susceptible to the hypoglycemic action of glucose-lowering medications. Hypoglycemia is also more likely to occur when caloric intake is deficient, after severe or prolonged exercise, or when alcohol is ingested.
Early warning symptoms of hypoglycemia may be different or less pronounced in patients with autonomic neuropathy, the elderly, and in patients who are taking beta-adrenergic blocking medications or other sympatholytic agents. These situations may result in severe hypoglycemia before the patient is aware of the hypoglycemia.
5.2 Hypersensitivity Reactions
There have been postmarketing reports of hypersensitivity reactions in patients treated with glimepiride, including serious reactions such as anaphylaxis, angioedema, and Stevens-Johnson Syndrome. If a hypersensitivity reaction is suspected, promptly discontinue glimepiride, assess for other potential causes for the reaction, and institute alternative treatment for diabetes.
5.3 Hemolytic Anemia
Sulfonylureas can cause hemolytic anemia in patients with glucose 6-phosphate dehydrogenase (G6PD) deficiency. Because glimepiride tablets are a sulfonylurea, use caution in patients with G6PD deficiency and consider the use of a non-sulfonylurea alternative.
There are also postmarketing reports of hemolytic anemia in patients receiving glimepiride who did not have known G6PD deficiency [see Adverse Reactions (6.2)].
5.4 Increased Risk of Cardiovascular Mortality with Sulfonylureas
The administration of oral hypoglycemic drugs has been reported to be associated with increased cardiovascular mortality as compared to treatment with diet alone or diet plus insulin. This warning is based on the study conducted by the University Group Diabetes Program (UGDP), a long-term, prospective clinical trial designed to evaluate the effectiveness of glucose-lowering drugs in preventing or delaying vascular complications in patients with non-insulin-dependent diabetes. The study involved 823 patients who were randomly assigned to one of four treatment groups
UGDP reported that patients treated for 5 to 8 years with diet plus a fixed dose of tolbutamide (1.5 grams per day) had a rate of cardiovascular mortality approximately 2-1/2 times that of patients treated with diet alone. A significant increase in total mortality was not observed, but the use of tolbutamide was discontinued based on the increase in cardiovascular mortality, thus limiting the opportunity for the study to show an increase in overall mortality. Despite controversy regarding the interpretation of these results, the findings of the UGDP study provide an adequate basis for this warning. The patient should be informed of the potential risks and advantages of glimepiride and of alternative modes of therapy.
Although only one drug in the sulfonylurea class (tolbutamide) was included in this study, it is prudent from a safety standpoint to consider that this warning may also apply to other oral hypoglycemic drugs in this class, in view of their close similarities in mode of action and chemical structure.
-
6 ADVERSE REACTIONS
The following serious adverse reactions are discussed in more detail below and elsewhere in the labeling:
Hypoglycemia [see Warnings and Precautions (5.1)]
Hemolytic anemia [see Warnings and Precautions (5.3)]
In clinical trials, the most common adverse reactions with glimepiride were hypoglycemia, dizziness, asthenia, headache, and nausea.
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Approximately 2,800 patients with type 2 diabetes have been treated with glimepiride in the controlled clinical trials. In these trials, approximately 1,700 patients were treated with glimepiride for at least 1 year.
Table 1 summarizes adverse events, other than hypoglycemia, that were reported in 11 pooled placebo-controlled trials, whether or not considered to be possibly or probably related to study medication. Treatment duration ranged from 13 weeks to 12 months. Terms that are reported represent those that occurred at an incidence of ≥5% among glimepiride-treated patients and more commonly than in patients who received placebo.
Table 1. Eleven Pooled Placebo-Controlled Trials ranging from 13 weeks to 12 months: Adverse Events (Excluding Hypoglycemia) Occurring in ≥5% of glimepiride-treated Patients and at a Greater Incidence
than with Placebo*Glimepiride
N=745 %Placebo
N=294 %Headache
8.2
7.8
Accidental Injury†
5.8
3.4
Flu Syndrome
5.4
4.4
Nausea
5
3.4
Dizziness
5
2.4
* Glimepiride doses ranged from 1 to 16 mg administered daily
†Insufficient information to determine whether any of the accidental injury events were associated with hypoglycemia
Hypoglycemia:
In a randomized, double-blind, placebo-controlled monotherapy trial of 14 weeks duration, patients already on sulfonylurea therapy underwent a 3-week washout period then were randomized to glimepiride tablets 1 mg, 4 mg, 8 mg or placebo. Patients randomized to glimepiride tablets 4 mg or 8 mg underwent forced-titration from an initial dose of 1 mg to these final doses, as tolerated [see Clinical Studies (14.1)]. The overall incidence of possible hypoglycemia (defined by the presence of at least one symptom that the investigator believed might be related to hypoglycemia; a concurrent glucose measurement was not required) was 4% for glimepiride tablets 1 mg, 17% for glimepiride tablets 4 mg, 16% for glimepiride tablets 8 mg and 0% for placebo. All of these events were self-treated.
In a randomized, double-blind, placebo-controlled monotherapy trial of 22 weeks duration, patients received a starting dose of either 1 mg glimepiride tablets or placebo daily. The dose of glimepiride tablets was titrated to a target fasting plasma glucose of 90 to 150 mg/dL. Final daily doses of glimepiride tablets were 1, 2, 3, 4, 6 or 8 mg [see Clinical Studies (14.1)]. The overall incidence of possible hypoglycemia (as defined above for the 14-week trial) for glimepiride vs. placebo was 19.7% vs. 3.2%. All of these events were self-treated.
Weight gain: Glimepiride, like all sulfonylureas, can cause weight gain [see Clinical Studies (14.1)].
Allergic Reactions: In clinical trials, allergic reactions, such as pruritus, erythema, urticaria, and morbilliform or maculopapular eruptions, occurred in less than 1% of glimepiride-treated patients. These may resolve despite continued treatment with glimepiride. There are postmarketing reports of more serious allergic reactions (e.g., dyspnea, hypotension, shock) [see Warnings and Precautions (5.2)].
Laboratory Tests:
Elevated Serum Alanine Aminotransferase (ALT): In 11 pooled placebo-controlled trials of glimepiride, 1.9% of glimepiride-treated patients and 0.8% of placebo-treated patients developed serum ALT greater than 2 times the upper limit of the reference range.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of glimepiride. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Serious hypersensitivity reactions, including anaphylaxis, angioedema, and Stevens-Johnson Syndrome [see Warnings and Precautions (5.2)]
- Hemolytic anemia in patients with and without G6PD deficiency [see Warnings and Precautions (5.3)]
- Impairment of liver function (e.g. with cholestasis and jaundice), as well as hepatitis, which may progress to liver failure.
- Porphyria cutanea tarda, photosensitivity reactions and allergic vasculitis
- Leukopenia, agranulocytosis, aplastic anemia, and pancytopenia
- Thrombocytopenia (including severe cases with platelet count less than 10,000/μL) and thrombocytopenic purpura
- Hepatic porphyria reactions and disulfiram-like reactions
- Hyponatremia and syndrome of inappropriate antidiuretic hormone secretion (SIADH), most often in patients who are on other medications or who have medical conditions known to cause hyponatremia or increase release of antidiuretic hormone
-
7 DRUG INTERACTIONS
7.1 Drugs Affecting Glucose Metabolism
A number of medications affect glucose metabolism and may require glimepiride tablets dose adjustment and particularly close monitoring for hypoglycemia or worsening glycemic control.
The following are examples of medications that may increase the glucose-lowering effect of sulfonylureas including glimepiride, increasing the susceptibility to and/or intensity of hypoglycemia: oral anti-diabetic medications, pramlintide acetate, insulin, angiotensin converting enzyme (ACE) inhibitors, H2 receptor antagonists, fibrates, propoxyphene, pentoxifylline, somatostatin analogs, anabolic steroids and androgens, cyclophosphamide, phenyramidol, guanethidine, fluconazole, sulfinpyrazone, tetracyclines, clarithromycin, disopyramide, quinolones, and those drugs that are highly protein-bound, such as fluoxetine, nonsteroidal anti-inflammatory drugs, salicylates, sulfonamides, chloramphenicol, coumarins, probenecid and monoamine oxidase inhibitors. When these medications are administered to a patient receiving glimepiride, monitor the patient closely for hypoglycemia. When these medications are withdrawn from a patient receiving glimepiride, monitor the patient closely for worsening glycemic control.
The following are examples of medications that may reduce the glucose-lowering effect of sulfonylureas including glimepiride, leading to worsening glycemic control: danazol, glucagon, somatropin, protease inhibitors, atypical antipsychotic medications (e.g., olanzapine and clozapine), barbiturates, diazoxide, laxatives, rifampin, thiazides and other diuretics, corticosteroids, phenothiazines, thyroid hormones, estrogens, oral contraceptives, phenytoin, nicotinic acid, sympathomimetics (e.g., epinephrine, albuterol, terbutaline), and isoniazid. When these medications are administered to a patient receiving glimepiride, monitor the patient closely for worsening glycemic control. When these medications are withdrawn from a patient receiving glimepiride, monitor the patient closely for hypoglycemia.
Beta-blockers, clonidine, and reserpine may lead to either potentiation or weakening of glimepiride’s glucose-lowering effect.
Both acute and chronic alcohol intake may potentiate or weaken the glucose-lowering action of glimepiride in an unpredictable fashion.
The signs of hypoglycemia may be reduced or absent in patients taking sympatholytic drugs such as beta-blockers, clonidine, guanethidine, and reserpine.
7.2 Miconazole
A potential interaction between oral miconazole and sulfonylureas leading to severe hypoglycemia has been reported. Whether this interaction also occurs with other dosage forms of miconazole is not known.
7.3 Cytochrome P450 2C9 Interactions
There may be an interaction between glimepiride and inhibitors (e.g., fluconazole) and inducers (e.g., rifampin) of cytochrome P450 2C9. Fluconazole may inhibit the metabolism of glimepiride, causing increased plasma concentrations of glimepiride which may lead to hypoglycemia. Rifampin may induce the metabolism of glimepiride, causing decreased plasma concentrations of glimepiride which may lead to worsening glycemic control.
7.4 Concomitant Administration of Colesevelam
Colesevelam can reduce the maximum plasma concentration and total exposure of glimepiride when the two are coadministered. However, absorption is not reduced when glimepiride is administered 4 hours prior to colesevelam. Therefore, glimepiride should be administered at least 4 hours prior to colesevelam.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C
There are no adequate and well-controlled studies of glimepiride in pregnant women. In animal studies there was no increase in congenital anomalies, but an increase in fetal deaths occurred in rats and rabbits at glimepiride doses 50 times (rats) and 0.1 times (rabbits) the maximum recommended human dose (based on body surface area). This fetotoxicity, observed only at doses inducing maternal hypoglycemia, is believed to be directly related to the pharmacologic (hypoglycemic) action of glimepiride and has been similarly noted with other sulfonylureas. Glimepiride should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Because data suggest that abnormal blood glucose during pregnancy is associated with a higher incidence of congenital abnormalities, diabetes treatment during pregnancy should maintain blood glucose as close to normal as possible.
Nonteratogenic Effects: Prolonged severe hypoglycemia (4 to 10 days) has been reported in neonates born to mothers receiving a sulfonylurea at the time of delivery.
8.3 Nursing Mothers
It is not known whether glimepiride tablets are excreted in human milk. During pre- and post-natal studies in rats, significant concentrations of glimepiride were present in breast milk and the serum of the pups. Offspring of rats exposed to high levels of glimepiride during pregnancy and lactation developed skeletal deformities consisting of shortening, thickening, and bending of the humerus during the postnatal period. These skeletal deformations were determined to be the result of nursing from mothers exposed to glimepiride. Based on these animal data and the potential for hypoglycemia in a nursing infant, a decision should be made whether to discontinue nursing or discontinue glimepiride, taking into account the importance of glimepiride to the mother.
8.4 Pediatric Use
The pharmacokinetics, efficacy and safety of glimepiride have been evaluated in pediatric patients with type 2 diabetes as described below. Glimepiride tablets are not recommended in pediatric patients because of its adverse effects on body weight and hypoglycemia.
The pharmacokinetics of a 1 mg single dose of glimepiride was evaluated in 30 patients with type 2 diabetes (male = 7; female = 23) between ages 10 and 17 years. The mean (± SD) AUC(0-last) (339±203 nghr/mL), Cmax (102±48 ng/mL) and t1/2 (3.1±1.7 hours) for glimepiride were comparable to historical data from adults (AUC(0-last) 315±96 nghr/mL, Cmax 103±34 ng/mL and t1/2 5.3±4.1 hours).
The safety and efficacy of glimepiride in pediatric patients was evaluated in a single-blind, 24-week trial that randomized 272 patients (8 to 17 years of age) with type 2 diabetes to glimepiride (n=135) or metformin (n=137). Both treatment-naïve patients (those treated with only diet and exercise for at least 2 weeks prior to randomization) and previously treated patients (those previously treated or currently treated with other oral antidiabetic medications for at least 3 months) were eligible to participate. Patients who were receiving oral antidiabetic agents at the time of study entry discontinued these medications before randomization without a washout period. Glimepiride was initiated at 1 mg, and then titrated up to 2, 4 or 8 mg (mean last dose 4 mg) through Week 12, targeting a self-monitored fasting fingerstick blood glucose < 126 mg/dL. Metformin was initiated at 500 mg twice daily and titrated at Week 12 up to 1000 mg twice daily (mean last dose 1365 mg).
After 24 weeks, the overall mean treatment difference in HbA1c between glimepiride and metformin was 0.2%, favoring metformin (95% confidence interval -0.3% to +0.6%).
Based on these results, the trial did not meet its primary objective of showing a similar reduction in HbA1c with glimepiride compared to metformin.
Table 2. Change from Baseline in HbA1C and Body Weight in Pediatric Patients Taking Glimepiride or Metformin
Metformin
Glimepiride
Treatment-Naïve Patients*
N=69
N=72
HbA1C (%)
Baseline (mean)
8.2
8.3
Change from baseline (adjusted LS mean) +
-1.2
-1
Adjusted Treatment Difference** (95%Cl)
0.2 (-0.3; 0.6)
Previously Treated Patients*
N=57
N=55
HbA1C (%)
Baseline (mean)
9
8.7
Change from baseline (adjusted LS mean) +
-0.2
0.2
Adjusted Treatment Difference** (95%Cl)
0.4 (-0.4; 1.2)
Body Weight (kg)*
N=126
N=129
Baseline (mean)
67.3
66.5
Change from baseline (adjusted LS mean)+
0.7
2
Adjusted Treatment Difference** (95% Cl)
1.3 (0.3; 2.3)
* Intent-to-treat population using last-observation-carried-forward for missing data (Glimepiride, n=127; metformin, n=126)
+ adjusted for baseline HbA1c and Tanner Stage
** Difference is glimepiride – metformin with positive differences favoring metformin
The profile of adverse reactions in pediatric patients treated with glimepiride was similar to that observed in adults [see Adverse Reactions (6)].
Hypoglycemic events documented by blood glucose values <36 mg/dL were observed in 4% of pediatric patients treated with glimepiride and in 1% of pediatric patients treated with metformin. One patient in each treatment group experienced a severe hypoglycemic episode (severity was determined by the investigator based on observed signs and symptoms).
8.5 Geriatric Use
In clinical trials of glimepiride, 1053 of 3491 patients (30%) were >65 years of age. No overall differences in safety or effectiveness were observed between these patients and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
There were no significant differences in glimepiride pharmacokinetics between patients with type 2 diabetes ≤65 years (n=49) and those >65 years (n=42) [see Clinical Pharmacology (12.3)].
Glimepiride is substantially excreted by the kidney. Elderly patients are more likely to have renal impairment. In addition, hypoglycemia may be difficult to recognize in the elderly [see Dosage and Administration (2.1) and Warnings and Precautions (5.1)]. Use caution when initiating glimepiride and increasing the dose of glimepiride tablets in this patient population.
8.6 Renal Impairment
To minimize the risk of hypoglycemia, the recommended starting dose of glimepiride tablets are 1 mg daily for all patients with type 2 diabetes and renal impairment [see Dosage and Administration (2.1) and Warnings and Precautions (5.1)].
A multiple-dose titration study was conducted in 16 patients with type 2 diabetes and renal impairment using doses ranging from 1 mg to 8 mg daily for 3 months. Baseline creatinine clearance ranged from 10 to 60 mL/min. The pharmacokinetics of glimepiride tablets were evaluated in the multiple-dose titration study and the results were consistent with those observed in patients enrolled in a single-dose study. In both studies, the relative total clearance of glimepiride increased when kidney function was impaired. Both studies also demonstrated that the elimination of the two major metabolites was reduced in patients with renal impairment [see Clinical Pharmacology (12.3)].
-
10 OVERDOSAGE
An overdosage of glimepiride tablets, as with other sulfonylureas, can produce severe hypoglycemia. Mild episodes of hypoglycemia can be treated with oral glucose. Severe hypoglycemic reactions constitute medical emergencies requiring immediate treatment. Severe hypoglycemia with coma, seizure, or neurological impairment can be treated with glucagon or intravenous glucose. Continued observation and additional carbohydrate intake may be necessary because hypoglycemia may recur after apparent clinical recovery [see Warnings and Precautions (5.1)].
-
11 DESCRIPTION
Glimepiride tablets USP, are an oral sulfonylurea that contains the active ingredient glimepiride USP. Chemically, glimepiride USP is identified as 1-[[p-[2-(3-ethyl-4-methyl-2-oxo-3-pyrroline-1-carboxamido) ethyl]phenyl]sulfonyl]-3-(trans-4-methylcyclohexyl)urea (C24H34N4O5S) with a molecular weight of 490.62. Glimepiride USP is a white to almost white powder, soluble in dimethyl formamide, sparingly soluble in methylene chloride, practically insoluble in water.
The structural formula is:
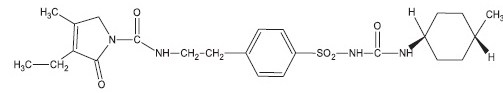
Structural Formula
Glimepiride tablets meets USP drug release test 2.
Glimepiride tablets USP, contain the active ingredient glimepiride USP and the following inactive ingredients: lactose monohydrate, magnesium stearate, microcrystalline cellulose, povidone and sodium starch glycolate. In addition, glimepiride 1 mg tablets contain ferric oxide red, glimepiride 2 mg tablets contain lake blend green (contains D&C yellow # 10 aluminium lake and FD&C blue #1/ brilliant blue FCF aluminium lake) and glimepiride 4 mg tablets contain lake blend blue (contains D&C yellow # 10 aluminium lake and FD&C blue # 1/ brilliant blue FCF aluminium lake).
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Glimepiride primarily lowers blood glucose by stimulating the release of insulin from pancreatic beta cells. Sulfonylureas bind to the sulfonylurea receptor in the pancreatic beta-cell plasma membrane, leading to closure of the ATP-sensitive potassium channel, thereby stimulating the release of insulin.
12.2 Pharmacodynamics
In healthy subjects, the time to reach maximal effect (minimum blood glucose concentrations) was approximately 2 to 3 hours after single oral doses of glimepiride tablets. The effects of glimepiride on HbA1c, fasting plasma glucose, and post-prandial glucose have been assessed in clinical trials [see Clinical Studies (14)].
12.3 Pharmacokinetics
Absorption: Studies with single oral doses of glimepiride in healthy subjects and with multiple oral doses in patients with type 2 diabetes showed peak drug concentrations (Cmax) 2 to 3 hours post-dose. When glimepiride was given with meals, the mean Cmax and AUC (area under the curve) were decreased by 8% and 9%, respectively.
Glimepiride does not accumulate in serum following multiple dosing. The pharmacokinetics of glimepiride does not differ between healthy subjects and patients with type 2 diabetes. Clearance of glimepiride after oral administration does not change over the 1 mg to 8 mg dose range, indicating linear pharmacokinetics.
In healthy subjects, the intra- and inter-individual variabilities of glimepiride pharmacokinetic parameters were 15-23% and 24-29%, respectively.
Distribution: After intravenous dosing in healthy subjects, the volume of distribution (Vd) was 8.8 L (113 mL/kg), and the total body clearance (CL) was 47.8 mL/min. Protein binding was greater than 99.5%.
Metabolism: Glimepiride is completely metabolized by oxidative biotransformation after either an intravenous or oral dose. The major metabolites are the cyclohexyl hydroxy methyl derivative (M1) and the carboxyl derivative (M2). Cytochrome P450 2C9 is involved in the biotransformation of glimepiride to M1. M1 is further metabolized to M2 by one or several cytosolic enzymes. M2 is inactive. In animals, M1 possesses about one-third of the pharmacological activity of glimepiride, but it is unclear whether M1 results in clinically meaningful effects on blood glucose in humans.
Excretion: When 14C-glimepiride was given orally to 3 healthy male subjects, approximately 60% of the total radioactivity was recovered in the urine in 7 days. M1 and M2 accounted for 80-90% of the radioactivity recovered in the urine. The ratio of M1 to M2 in the urine was approximately 3:2 in two subjects and 4:1 in one subject. Approximately 40% of the total radioactivity was recovered in feces. M1 and M2 accounted for about 70% (ratio of M1 to M2 was 1:3) of the radioactivity recovered in feces. No parent drug was recovered from urine or feces. After intravenous dosing in patients, no significant biliary excretion of glimepiride or its M1 metabolite was observed.
Geriatric Patients: A comparison of glimepiride pharmacokinetics in patients with type 2 diabetes ≤65 years and those >65 years was evaluated in a multiple-dose study using glimepiride tablets 6 mg daily. There were no significant differences in glimepiride pharmacokinetics between the two age groups. The mean AUC at steady state for the older patients was approximately 13% lower than that for the younger patients; the mean weight-adjusted clearance for the older patients was approximately 11% higher than that for the younger patients.
Gender: There were no differences between males and females in the pharmacokinetics of glimepiride when adjustment was made for differences in body weight.
Race: No studies have been conducted to assess the effects of race on glimepiride pharmacokinetics but in placebo-controlled trials of glimepiride in patients with type 2 diabetes, the reduction in HbA1C was comparable in Caucasians (n = 536), blacks (n = 63), and Hispanics (n = 63).
Renal Impairment: A single-dose, open-label study glimepiride tablets 3 mg was administered to patients with mild, moderate and severe renal impairment as estimated by creatinine clearance (CLcr): Group I consisted of 5 patients with mild renal impairment (CLcr > 50 mL/min), Group II consisted of 3 patients with moderate renal impairment (CLcr = 20 to 50 mL/min) and Group III consisted of 7 patients with severe renal impairment (CLcr < 20 mL/min). Although, glimepiride serum concentrations decreased with decreasing renal function, Group III had a 2.3-fold higher mean AUC for M1 and an 8.6-fold higher mean AUC for M2 compared to corresponding mean AUCs in Group I. The apparent terminal half-life (T1/2) for glimepiride did not change, while the half-lives for M1 and M2 increased as renal function decreased. Mean urinary excretion of M1 plus M2 as a percentage of dose decreased from 44.4% for Group I to 21.9% for Group II and 9.3% for Group III.
Hepatic Impairment: It is unknown whether there is an effect of hepatic impairment on glimepiride pharmacokinetics because the pharmacokinetics of glimepiride has not been adequately evaluated in patients with hepatic impairment.
Obese Patients: The pharmacokinetics of glimepiride and its metabolites were measured in a single-dose study involving 28 patients with type 2 diabetes who either had normal body weight or were morbidly obese. While the tmax, clearance, and volume of distribution of glimepiride in the morbidly obese patients were similar to those in the normal weight group, the morbidly obese had lower Cmax and AUC than those of normal body weight. The mean Cmax, AUC0-24, AUC0-∞ values of glimepiride in normal vs. morbidly obese patients were 547 ± 218 ng/mL vs. 410 ± 124 ng/mL, 3210 ± 1030 hoursng/mL vs. 2820 ± 1110 hoursng/mL and 4000 ± 1320 hoursng/mL vs. 3280 ± 1360 hoursng/mL, respectively.
Drug Interactions:
Aspirin: In a randomized, double-blind, two-period, crossover study, healthy subjects were given either placebo or aspirin 1 gram three times daily for a total treatment period of 5 days. On Day 4 of each study period, a single 1 mg dose of glimepiride tablets was administered. The glimepiride tablets doses were separated by a 14-day washout period. Co-administration of aspirin and glimepiride resulted in a 34% decrease in the mean glimepiride AUC and a 4% decrease in the mean glimepiride Cmax.
Colesevelam: Concomitant administration of colesevelam and glimepiride resulted in reductions in glimepiride AUC0-∞ and Cmax of 18% and 8%, respectively. When glimepiride was administered 4 hours prior to colesevelam, there was no significant change in glimepiride AUC0-∞ or Cmax, -6% and 3%, respectively [see Dosage and Administration (2.1) and Drug Interactions (7.4)].
Cimetidine and Ranitidine: In a randomized, open-label, 3-way crossover study, healthy subjects received either a single 4 mg dose of glimepiride tablets alone, glimepiride with ranitidine (150 mg twice daily for 4 days; glimepiride was administered on Day 3), or glimepiride with cimetidine (800 mg daily for 4 days; glimepiride was administered on Day 3). Co-administration of cimetidine or ranitidine with a single 4 mg oral dose of glimepiride tablets did not significantly alter the absorption and disposition of glimepiride.
Propranolol: In a randomized, double-blind, two-period, crossover study, healthy subjects were given either placebo or propranolol 40 mg three times daily for a total treatment period of 5 days. On Day 4 or each study period, a single 2 mg dose of glimepiride tablets was administered. The glimepiride tablets doses were separated by a 14-day washout period. Concomitant administration of propranolol and glimepiride significantly increased glimepiride Cmax, AUC, and T1/2 by 23%, 22%, and 15%, respectively, and decreased glimepiride CL/f by 18%. The recovery of M1 and M2 from urine was not changed.
Warfarin: In an open-label, two-way, crossover study, healthy subjects received 4 mg of glimepiride tablets daily for 10 days. Single 25 mg doses of warfarin were administered 6 days before starting glimepiride and on Day 4 of glimepiride administration. The concomitant administration of glimepiride did not alter the pharmacokinetics of R- and S-warfarin enantiomers. No changes were observed in warfarin plasma protein binding. Glimepiride resulted in a statistically significant decrease in the pharmacodynamic response to warfarin. The reductions in mean area under the prothrombin time (PT) curve and maximum PT values during glimepiride treatment were 3.3% and 9.9%, respectively, and are unlikely to be clinically relevant.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Studies in rats at doses of up to 5000 parts per million (ppm) in complete feed (approximately 340 times the maximum recommended human dose, based on surface area) for 30 months showed no evidence of carcinogenesis. In mice, administration of glimepiride for 24 months resulted in an increase in benign pancreatic adenoma formation that was dose-related and was thought to be the result of chronic pancreatic stimulation. No adenoma formation in mice was observed at a dose of 320 ppm in complete feed, or 46 to 54 mg/kg body weight/day. This is about 35 times the maximum human recommended dose of 8 mg once daily based on surface area.
Glimepiride was non-mutagenic in a battery of in vitro and in vivo mutagenicity studies (Ames test, somatic cell mutation, chromosomal aberration, unscheduled DNA synthesis, and mouse micronucleus test).
There was no effect of glimepiride on male mouse fertility in animals exposed up to 2500 mg/kg body weight (>1,700 times the maximum recommended human dose based on surface area). Glimepiride had no effect on the fertility of male and female rats administered up to 4000 mg/kg body weight (approximately 4,000 times the maximum recommended human dose based on surface area).
-
14 CLINICAL STUDIES
14.1 Monotherapy
A total of 304 patients with type 2 diabetes already treated with sulfonylurea therapy participated in a 14-week, multicenter, randomized, double-blind, placebo-controlled trial evaluating the safety and efficacy of glimepiride monotherapy. Patients discontinued their sulfonylurea therapy then entered a 3-week placebo washout period followed by randomization into 1 of 4 treatment groups: placebo (n=74), glimepiride tablets 1 mg (n=78), glimepiride tablets 4 mg (n=76) and glimepiride tablets 8 mg (n=76). All patients randomized to glimepiride tablets started 1 mg daily. Patients randomized to glimepiride tablets 4 mg or 8 mg had blinded, forced titration of the glimepiride tablets dose at weekly intervals, first to 4 mg and then to 8 mg, as long as the dose was tolerated, until the randomized dose was reached. Patients randomized to the 4 mg dose reached the assigned dose at Week 2. Patients randomized to the 8 mg dose reached the assigned dose at Week 3. Once the randomized dose level was reached, patients were to be maintained at that dose until Week 14. Approximately 66% of the placebo-treated patients completed the trial compared to 81% of patients treated with glimepiride 1 mg and 92% of patients treated with glimepiride 4 mg or 8 mg. Compared to placebo, treatment with glimepiride tablets 1 mg, 4 mg and 8 mg daily provided statistically significant improvements in HbA1C compared to placebo (Table 3).
Table 3. 14-week Monotherapy Trial Comparing Glimepiride to Placebo in Patients Previously Treated
With Sulfonylurea Therapya
Placebo
(N=74)
Glimepiride1 mg (N=78)
4 mg (N=76)
8 mg (N=76)
HbA1C (%) n=59
n=65
n=65
n=68
Baseline (mean)
8
7.9
7.9
8
Change from Baseline (adjusted meanb)
1.5
0.3
-0.3
-0.4
Difference from Placebo (adjusted meanb) 95% confidence interval
-1.2*
(-1.5, -0.8)-1.8*
(-2.1, -1.4)-1.8*
(-2.2, -1.5)Mean Baseline Weight (kg) n=67
n=76
n=75
n=73
Baseline (mean)
85.7
84.3
86.1
85.5
Change from Baseline (adjusted meanb)
-2.3
-0.2
0.5
1
Difference from Placebo (adjusted meanb) 95% confidence interval
2*
(1.4, 2.7)2.8*
(2.1, 3.5)3.2*
(2.5, 4)aIntent-to-treat population using last observation on study
bLeast squares mean adjusted for baseline value
*p<0.001A total of 249 patients who were treatment-naïve or who had received limited treatment with antidiabetic therapy in the past were randomized to receive 22 weeks of treatment with either glimepiride (n=123) or placebo (n=126) in a multicenter, randomized, double-blind, placebo-controlled, dose-titration trial. The starting dose of glimepiride tablets was 1 mg daily and was titrated upward or downward at 2-week intervals to a goal FPG of 90 to 150 mg/dL. Blood glucose levels for both FPG and PPG were analyzed in the laboratory. Following 10 weeks of dose adjustment, patients were maintained at their optimal dose (1, 2, 3, 4, 6 or 8 mg) for the remaining 12 weeks of the trial. Treatment with glimepiride provided statistically significant improvements in HbA1C and FPG compared to placebo (Table 4).
Table 4. 22-Week Monotherapy Trial Comparing Glimepiride to Placebo in Patients Who Were
Treatment-Naïve or Who Had No Recent Treatment with Antidiabetic TherapyaPlacebo (N=126)
Glimepiride (N=123)
HbA1C (%)
n=97
n=106
Baseline (mean)
9.1
9.3
Change from Baseline (adjusted meanb)
-1.1*
-2.2*
Difference from Placebo (adjusted meanb)
95% confidence interval-1.1*
(-1.5, -0.8)Body Weight (kg) n=122
n=119
Baseline (mean)
86.5
87.1
Change from Baseline (adjusted meanb)
-0.9
1.8
Difference from Placebo (adjusted meanb)
95% confidence interval2.7
(1.9, 3.6)aIntent to treat population using last observation on study
bLeast squares mean adjusted for baseline value
*p<0.0001 -
16 HOW SUPPLIED/STORAGE AND HANDLING
Glimepiride tablets USP, are available in the following strengths and package sizes:
Glimepiride tablets USP, 2 mg are green, oval, flat bevelled edged, uncoated tablets debossed “RDY” on one side and “321” separating “3” and “21” with bisect line scoring on the other side and are supplied in adherence packages of 30.
Bottles of 30 NDC: 54458-967-16
Glimepiride tablets USP, 4 mg are blue, oval, flat bevelled edged, uncoated tablets debossed “RDY” on one side and “322” separating “3” and “22” with bisect line scoring on the other side and are supplied in adherence packages of 30.
Bottles of 30 NDC: 54458-966-16
Store at 20°-25°C (68°-77°F) [see USP Controlled Room Temperature].
-
17 PATIENT COUNSELING INFORMATION
17.1 Information for Patients
Inform patients about the importance of adherence to dietary instructions, of a regular exercise program, and of regular testing of blood glucose.
Inform patients about the potential side effects of glimepiride including hypoglycemia and weight gain.
Explain the symptoms and treatment of hypoglycemia as well as conditions that predispose to hypoglycemia. Patients should be informed that the ability to concentrate and react may be impaired as a result of hypoglycemia. This may present a risk in situations where these abilities are especially important, such as driving or operating other machinery.
Patients with diabetes should be advised to inform their healthcare provider if they are pregnant, contemplating pregnancy, breastfeeding, or contemplating breastfeeding.
Rx only
Manufactured by:
Dr. Reddy's Laboratories Limited
Bachupally - 500 090 India
or
Dr. Reddy's Limited Laboratories
Srikakulam - 532 409 India
Packaged for:
International Laboratories, LLC
Seminole, FL 33777
Distributed by:
Walmart
Bentonville, AR 72716
Rev. 10/17 LI0012
- PACKAGE LABEL PRINCIPAL DISPLAY PANEL
- PACKAGE LABEL PRINCIPAL DISPLAY PANEL
- PACKAGE LABEL PRINCIPAL DISPLAY PANEL
- PACKAGE LABEL. PRINCIPAL DISPLAY PANEL
- PACKAGE LABEL PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
GLIMEPIRIDE
glimepiride tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 54458-966 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength GLIMEPIRIDE (UNII: 6KY687524K) (GLIMEPIRIDE - UNII:6KY687524K) GLIMEPIRIDE 4 mg Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POVIDONE (UNII: FZ989GH94E) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) D&C YELLOW NO. 10 (UNII: 35SW5USQ3G) FD&C BLUE NO. 1 (UNII: H3R47K3TBD) Product Characteristics Color BLUE Score 2 pieces Shape OVAL Size 8mm Flavor Imprint Code RDY;3;22 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 54458-966-10 30 in 1 BLISTER PACK; Type 0: Not a Combination Product 02/06/2009 2 NDC: 54458-966-16 30 in 1 BOTTLE; Type 0: Not a Combination Product 07/17/2017 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA077091 02/06/2009 GLIMEPIRIDE
glimepiride tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 54458-968 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength GLIMEPIRIDE (UNII: 6KY687524K) (GLIMEPIRIDE - UNII:6KY687524K) GLIMEPIRIDE 1 mg Inactive Ingredients Ingredient Name Strength FERRIC OXIDE RED (UNII: 1K09F3G675) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POVIDONE (UNII: FZ989GH94E) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) Product Characteristics Color PINK (Peach) Score 2 pieces Shape OVAL Size 8mm Flavor Imprint Code RDY;3;20 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 54458-968-10 30 in 1 BLISTER PACK; Type 0: Not a Combination Product 02/06/2009 02/25/2019 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA077091 02/06/2009 02/25/2019 GLIMEPIRIDE
glimepiride tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 54458-967 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength GLIMEPIRIDE (UNII: 6KY687524K) (GLIMEPIRIDE - UNII:6KY687524K) GLIMEPIRIDE 2 mg Inactive Ingredients Ingredient Name Strength D&C YELLOW NO. 10 (UNII: 35SW5USQ3G) FD&C BLUE NO. 1 (UNII: H3R47K3TBD) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POVIDONE (UNII: FZ989GH94E) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) Product Characteristics Color GREEN Score 2 pieces Shape OVAL Size 8mm Flavor Imprint Code RDY;3;21 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 54458-967-10 30 in 1 BLISTER PACK; Type 0: Not a Combination Product 02/06/2009 2 NDC: 54458-967-16 30 in 1 BOTTLE; Type 0: Not a Combination Product 08/02/2017 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA077091 02/06/2009 Labeler - International Laboratories, LLC (023569924) Establishment Name Address ID/FEI Business Operations Dr. Reddy's Laboratories Limited 918608162 MANUFACTURE(54458-966, 54458-968, 54458-967)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.