NIMODIPINE capsule, liquid filled
Nimodipine by
Drug Labeling and Warnings
Nimodipine by is a Prescription medication manufactured, distributed, or labeled by McKesson Corporation dba SKY Packaging, Legacy Pharmaceutical Packaging, LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- Rx Only
-
BOXED WARNING
(What is this?)
DO NOT ADMINISTER NIMODIPINE CAPSULES INTRAVENOUSLY OR BY OTHER PARENTERAL ROUTES. DEATHS AND SERIOUS, LIFE THREATENING ADVERSE EVENTS HAVE OCCURRED WHEN THE CONTENTS OF NIMODIPINE CAPSULES HAVE BEEN INJECTED PARENTERALLY (See WARNINGS and DOSAGE AND ADMINISTRATION).
-
DESCRIPTION
Nimodipine capsules belongs to the class of pharmacological agents known as calcium channel blockers. Nimodipine is isopropyl 2 – methoxyethyl 1, 4 – dihydro – 2, 6 – dimethyl – 4 – (m-nitrophenyl) – 3, 5 – pyridinedicarboxylate. It has a molecular weight of 418.5 and a molecular formula of C21H26N2O7. The structural formula is:
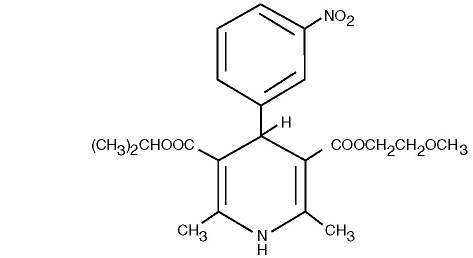
Nimodipine is a yellow crystalline substance, practically insoluble in water.
Nimodipine capsules are formulated as soft gelatin capsules for oral administration. Each liquid filled capsule contains 30 mg of nimodipine in a vehicle of glycerin, peppermint oil, purified water and polyethylene glycol 400. The soft gelatin capsule shell contains gelatin, glycerin, purified water, titanium dioxide and iron oxide black. -
CLINICAL PHARMACOLOGY
Mechanism of Action: Nimodipine is a calcium channel blocker. The contractile processes of smooth muscle cells are dependent upon calcium ions, which enter these cells during depolarization as slow ionic transmembrane currents. Nimodipine inhibits calcium ion transfer into these cells and thus inhibits contractions of vascular smooth muscle. In animal experiments, nimodipine had a greater effect on cerebral arteries than on arteries elsewhere in the body perhaps because it is highly liphophilic, allowing it to cross the blood-brain barrier; concentrations of nimodipine as high as 12.5 ng/mL have been detected in the cerebrospinal fluid of nimodipine-treated subarachnoid hemorrhage (SAH) patients.
The precise mechanism of action of nimodipine in humans is unknown. Although the clinical studies described below demonstrate a favorable effect of nimodipine on the severity of neurological deficits caused by cerebral vasospasm following SAH, there is no arteriographic evidence that the drug either prevents or relieves the spasm of these arteries. However, whether or not the arteriographic methodology utilized was adequate to detect a clinically meaningful effect, if any, on vasospasm is unknown.
Pharmacokinetics and Metabolism: In man, nimodipine is rapidly absorbed after oral administration, and peak concentrations are generally attained within one hour. The terminal elimination half-life is approximately 8 to 9 hours but earlier elimination rates are much more rapid, equivalent to a half-life of 1-2 hours; a consequence is the need for frequent (every 4 hours) dosing. There were no signs of accumulation when nimodipine was given three times a day for seven days. Nimodipine is over 95% bound to plasma proteins. The binding was concentration independent over the range of 10 ng/mL to 10 μg/mL. Nimodipine is eliminated almost exclusively in the form of metabolites and less than 1% is recovered in the urine as unchanged drug. Numerous metabolites, all of which are either inactive or considerably less active than the parent compound, have been identified. Because of a high first-pass metabolism, the bioavailability of nimodipine averages 13% after oral administration. The bioavailability is significantly increased in patients with hepatic cirrhosis, with Cmax approximately double that in normals which necessitates lowering the dose in this group of patients (see Dosage and Administration). In a study of 24 healthy male volunteers, administration of nimodipine capsules following a standard breakfast resulted in a 68% lower peak plasma concentration and 38% lower bioavailability relative to dosing under fasted conditions.
In a single parallel-group study involving 24 elderly subjects (aged 59-79) and 24 younger subjects (aged 22-40), the observed AUC and Cmax of nimodipine was approximately 2-fold higher in the elderly population compared to the younger study subjects following oral administration (given as a single dose of 30 mg and dosed to steady-state with 30 mg t.i.d. for 6 days). The clinical response to these age-related pharmacokinetic differences, however, was not considered significant. (See PRECAUTIONS: Geriatric Use.)
Clinical Trials: Nimodipine has been shown, in 4 randomized, double-blind, placebo-controlled trials, to reduce the severity of neurological deficits resulting from vasospasm in patients who have had a recent subarachnoid hemorrhage (SAH). The trials used doses ranging from 20-30 mg to 90 mg every 4 hours, with drug given for 21 days in 3 studies, and for at least 18 days in the other. Three of the four trials followed patients for 3-6 months. Three of the trials studied relatively well patients, with all or most patients in Hunt and Hess Grades I-III (essentially free of focal deficits after the initial bleed) the fourth studied much sicker patients, Hunt and Hess Grades III-V. Two studies, one U.S., one French, were similar in design, with relatively unimpaired SAH patients randomized to nimodipine or placebo. In each, a judgment was made as to whether any late-developing deficit was due to spasm or other causes, and the deficits were graded. Both studies showed significantly fewer severe deficits due to spasm in nimodipine group; the second (French) study showed fewer spasm-related deficits of all severities. No effect was seen on deficits not related to spasm.
- * Hunt and Hess Grade
- † p=0.03
Patients Study Dose Grade* Number
AnalyzedAny Deficit
Due to SpasmNumbers with
Severe DeficitU.S. 20-30 mg I-III Nimodipine
Placebo56
6013
161
8†French 60 mg I-III Nimodipine
Placebo31
394
112
10†A third, large, study was performed in the United Kingdom in SAH patients with all grades of severity (but 89% were in Grades I-III). Nimodipine was dosed 60mg every 4 hours. Outcomes were not defined as spasm related or not but there was a significant reduction in the overall rate of infarction and severely disabling neurological outcome at 3 months:
- * p = 0.0444 – good and moderate vs severe and dead
- † p = 0.001 – severe disability
- ‡ p = 0.056 – death
Nimodipine Placebo
Total patients 278 276
Good recovery 199* 169
Moderate disability 24 16
Severe disability 12† 31
Death 43‡ 60 A Canadian study entered much sicker patients, (Hunt and Hess Grades III-V), who had a high rate of death and disability, and used a dose of 90 mg every 4 hours, but was otherwise similar to the first two studies. Analysis of delayed ischemic deficits, many of which result from spasm, showed a significant reduction in spasm-related deficits. Among analyzed patients (72 nimodipine, 82 placebo), there were the following outcomes.
- * p=0.001, nimodipine vs placebo
Delayed Ischemic
Deficits (DID)Permanent
Deficits
Nimodipine
n (%)Placebo
n (%)Nimodipine
n (%)Placebo
n (%)DID Spasm Alone 8 (11)* 25 (31) 5 (7)* 22 (27) DID Spasm Contributing 18 (25) 21 (26) 16 (22) 17 (21) DID Without Spasm 7 (10) 8 (10) 6 (8) 7 (9) No DID 39 (54) 28 (34) 45 (63) 36 (44) When data were combined for the Canadian and the United Kingdom studies, the treatment difference on success rate (i.e. good recovery) on the Glasgow Outcome Scale was 25.3% (nimodipine) versus 10.9% (placebo) for Hunt and Hess Grades IV or V. The table below demonstrates that nimodipine tends to improve good recovery of SAH patients with poor neurological status post-ictus, while decreasing the numbers with severe disability and vegetative survival.
- * p=0.045, nimodipine vs placebo
Glasgow Outcome* Nimodipine
(n=87)Placebo
(n=101)Good Recovery 22 (25.3%) 11 (10.9%) Moderate Disability 8 (9.2%) 12 (11.9%) Severe Disability 6 (6.9%) 15 (14.9%) Vegetative Survival 4 (4.6%) 9 (8.9%) Death 47 (54.0%) 54 (53.5%) A dose-ranging study comparing 30, 60 and 90 mg doses found a generally low rate of spasm-related neurological deficits but no dose response relationship.
- INDICATIONS AND USAGE
-
CONTRAINDICATIONS
The concomitant use of nimodipine with strong inhibitors of CYP3A4 such as some macrolide antibiotics (e.g., clarithromycin, telithromycin), some anti-HIV protease inhibitors (e.g., delaviridine, indinavir, nelfinavir, ritonavir, saquinavir), some azole antimycotics (e.g., ketoconazole, itraconazole, voriconazole) and some antidepressants (e.g., nefazadone) is contraindicated because of a risk of significant hypotension (see PRECAUTIONS, Drug Interactions).
-
WARNINGS
DEATH DUE TO INADVERTENT INTRAVENOUS ADMINISTRATION:
DO NOT ADMINISTER NIMODIPINE INTRAVENOUSLY OR BY OTHER PARENTERAL ROUTES. DEATHS AND SERIOUS, LIFE THREATENING ADVERSE EVENTS, INCLUDING CARDIAC ARREST, CARDIOVASCULAR COLLAPSE, HYPOTENSION, AND BRADYCARDIA, HAVE OCCURRED WHEN THE CONTENTS OF NIMODIPINE CAPSULES HAVE BEEN INJECTED PARENTERALLY (SEE DOSAGE AND ADMINISTRATION).Reduced Efficacy with CYP3A4 Inducers
Concomitant use of strong CYP3A4 inducers (e.g., rifampin, phenobarbital, phenytoin, carbamazepine, St John’s wort) and nimodipine should generally be avoided, as nimodipine plasma concentration and efficacy may be very significantly reduced (see PRECAUTIONS, Drug Interactions).Moderate and weak inducers of CYP3A4 may also reduce the efficacy of nimodipine to a lesser extent. Patients on these should be closely monitored for lack of effectiveness, and a nimodipine dosage increase may be required.
Moderate and weak CYP3A4 inhibitors include, for example: amprenavir, aprepitant, armodafinil, bosentan, efavirenz, etravirine, echinacea, modafinil, nafcillin, pioglitazone, prednisone and rufinamide.
-
PRECAUTIONS
General: Blood Pressure: Nimodipine has the hemodynamic effects expected of a calcium channel blocker, although they are generally not marked. However, intravenous administration of the contents of nimodipine capsules has resulted in serious adverse consequences including death, cardiac arrest, cardiovascular collapse, hypotension, and bradycardia. In patients with subarachnoid hemorrhage given nimodipine capsules in clinical studies, about 5% were reported to have had lowering of the blood pressure and about 1% left the study because of this (not all could be attributed to nimodipine). Nevertheless, blood pressure should be carefully monitored during treatment with nimodipine capsules based on its known pharmacology and the known effects of calcium channel blockers. (see WARNINGS and DOSAGE AND ADMINISTRATION).
Hepatic Disease: The metabolism of nimodipine capsules is decreased in patients with impaired hepatic function. Such patients should have their blood pressure and pulse rate monitored closely and should be given a lower dose (see DOSAGE AND ADMINISTRATION).
Intestinal pseudo-obstruction and ileus have been reported rarely in patients treated with nimodipine. A causal relationship has not been established. The condition has responded to conservative management.
Drug Interaction:
Nimodipine is metabolized via the cytochrome P450 3A4 system located both in the intestinal mucosa and in the liver. Drugs that are known to either inhibit or to induce this enzyme system may therefore alter the first pass or the clearance of nimodipine.In addition, the blood pressure lowering effects of antihypertensives could be enhanced when taken concomitantly with nimodipine.
Inducers of CYP3A4
Nimodipine plasma concentration and efficacy may be significantly reduced when concomitantly administered with strong CYP3A4 inducers. Therefore strong CYP3A4 inducers (e.g., rifampin, carbamazepine, phenobarbital, phenytoin, St. John’s Wort) should generally not be administered concomitantly with nimodipine (see WARNINGS). Other moderate and weak inducers of CYP3A4 may also reduce the efficacy of nimodipine, although the magnitude of decrease in nimodipine plasma concentrations is not known. Patients on these should be closely monitored for lack of effectiveness, and a nimodipine dosage increase may be required. Moderate and weak CYP3A4 inducers include: amprenavir, aprepitant, armodafinil, bosentan, efavirenz, etravirine, Echinacea, modafinil, nafcillin, pioglitazone, prednisone and rufinamide.Inhibitors of CYP3A4
Nimodipine plasma concentration can be significantly increased when concomitantly administered with strong inhibitors of the CYP3A4 system. As a consequence, the blood pressure lowering effect may be increased. Therefore strong CYP3A4 inhibitors should not be coadministered with nimodipine (see CONTRAINDICATIONS). Strong CYP3A4 inhibitors include some members of the following classes: - macrolide antibiotics (e.g., clarithromycin, telithromycin,), - HIV protease inhibitors (e.g., delavirdine, indinavir, nelfinavir, ritonavir, saquinavir), - azole antimycotics (e.g., ketoconazole, itraconazole, voriconazole), - antidepressants (e.g., nefazodone) - grapefruit juice: after intake of grapefruit juice and nimodipine, the blood pressure lowering effect may last for at least 4 days after the last ingestion of grapefruit juice. Ingestion of grapefruit / grapefruit juice is therefore not recommended while taking nimodipine (see DOSAGE AND ADMINISTRATION).Nimodipine plasma concentration can also be increased in the presence of moderate and weak inhibitors of CYP3A4. If nimodipine is concomitantly administered with these drugs, blood pressure should be monitored, and a reduction of the nimodipine dose may be necessary. Moderate and weak CYP3A4 inhibitors include amprenavir, aprepitant, atazanavir, amiodarone, alprozalam, cyclosporine, cimetidine, erythromycin, fluconazole, fluoxetine, isoniazid, oral contraceptives, quinuprestin/dalforpristin, and valproic acid.
Blood pressure lowering drugs
Nimodipine may increase the blood pressure lowering effect of concomitantly administered anti-hypertensives, such as:
- diuretics, - other calcium antagonists,
- β-blockers, - α-adrenergic blocking agents,
- ACE inhibitors, - PDE5 inhibitors,
- A1-antagonists, - α-methyldopa.Blood pressure should be carefully monitored, and dose adjustment of the blood pressure lowering drug(s) may be necessary.
Carcinogenesis, Mutagenesis, Impairment of Fertility:
In a two-year study, higher incidences of adenocarcinoma of the uterus and Leydig-cell adenoma of the testes were observed in rats given a diet containing 1800 ppm nimodipine (equivalent to 91 to 121 mg/kg/day nimodipine) than in placebo controls. The differences were not statistically significant, however, and the higher rates were well within historical control range for these tumors in the Wistar strain. Nimodipine was found not to be carcinogenic in a 91-week mouse study but the high dose of 1800 ppm nimodipine-in-feed (546 to 774 mg/kg/day) shortened the life expectancy of the animals. Mutagenicity studies, including the Ames, micronucleus and dominant lethal tests were negative.Nimodipine did not impair the fertility and general reproductive performance of male and female Wistar rats following oral doses of up to 30 mg/kg/day when administered daily for more than 10 weeks in the males and 3 weeks in the females prior to mating and continued to day 7 of pregnancy. This dose in a rat is about 4 times the equivalent clinical dose of 60 mg q4h in a 50 kg patient.
Pregnancy: Pregnancy Category C. Nimodipine has been shown to have a teratogenic effect in Himalayan rabbits. Incidences of malformations and stunted fetuses were increased at oral doses of 1 and 10 mg/kg/day administered (by gavage) from day 6 through day 18 of pregnancy but not at 3.0 mg/kg/day in one of two identical rabbit studies. In the second study an increased incidence of stunted fetuses was seen at 1.0 mg/kg/day but not at a higher doses. Nimodipine was embryotoxic, causing resorption and stunted growth of fetuses, in Long Evans rats at 100 mg/kg/day administered by gavage from day 6 through day 15 of pregnancy. In two other rat studies, doses of 30 mg/kg/day nimodipine administered by gavage from day 16 of gestation and continued until sacrifice (day 20 of pregnancy or day 21 post partum) were associated with higher incidences of skeletal variation, stunted fetuses and stillbirths but no malformations. There are no adequate and well controlled studies in pregnant women to directly assess the effect on human fetuses. Nimodipine should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nursing Mothers: Nimodipine and/or its metabolites have been shown to appear in rat milk at concentrations much higher than in maternal plasma. It is not known whether the drug is excreted in human milk. Because many drugs are excreted in human milk, nursing mothers are advised not to breast feed their babies when taking the drug.
Geriatric Use: Clinical studies of nimodipine did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dosing in elderly patents should be cautious, reflecting the greater frequency of decreased hepatic, renal or cardiac function, and of concomitant disease of other drug therapy.
-
ADVERSE REACTIONS
Adverse experiences were reported by 92 of 823 patients with subarachnoid hemorrhage (11.2%) who were given nimodipine. The most frequently reported adverse experience was decreased blood pressure in 4.4% of these patients. Twenty-nine of 479 (6.1%) placebo treated patients also reported adverse experiences. The events reported with a frequency greater than 1% are displayed below by dose.
DOSE q4h
Number of Patients (%)
NimodipineSign/Symptom 0.35 mg/kg
(n=82)30 mg
(n=71)60 mg
(n=494)90 mg
(n=172)120 mg
(n=4)Placebo
(n=479)Decreased
Blood Pressure1 (1.2) 0 19 (3.8) 14 (8.1) 2 (50.0) 6 (1.2) Abnormal Liver
Function Test1 (1.2) 0 2 (0.4) 1 (0.6) 0 7 (1.5) Edema 0 0 2 (0.4) 2 (1.2) 0 3 (0.6) Diarrhea 0 3 (4.2) 0 3 (1.7) 0 3 (0.6) Rash 2 (2.4) 0 3 (0.6) 2 (1.2) 0 3 (0.6) Headache 0 1 (1.4) 6 (1.2) 0 0 1 (0.2) Gastrointestinal
Symptoms2 (2.4) 0 0 2 (1.2) 0 0 Nausea 1 (1.2) 1 (1.4) 6 (1.2) 1 (0.6) 0 0 Dyspnea 1 (1.2) 0 0 0 0 0 EKG Abnormalities 0 1 (1.4) 0 1 (0.6) 0 0 Tachycardia 0 1 (1.4) 0 0 0 0 Bradycardia 0 0 5 (1.0) 1 (0.6) 0 0 Muscle Pain/Cramp 0 1 (1.4) 1 (0.2) 1 (0.6) 0 0 Acne 0 1 (1.4) 0 0 0 0 Depression 0 1 (1.4) 0 0 0 0 There were no other adverse experiences reported by the patients who were given 0.35 mg/kg q4h, 30 mg q4h or 120 mg q4h. Adverse experiences with an incidence rate of less than 1% in the 60 mg q4h dose group were: hepatitis; itching; gastrointestinal hemorrhage; thrombocytopenia; anemia; palpitations; vomiting; flushing; diaphoresis; wheezing; phenytoin toxicity; lightheadedness; dizziness; rebound vasospasm; jaundice; hypertension; hematoma.
Adverse experience with an incidence rate less than 1% in the 90 mg q4h dose group were: itching, gastrointestinal hemorrhage; thrombocytopenia; neurological deterioration; vomiting; diaphoresis; congestive heart failure; hyponatremia; decreasing platelet count; disseminated intravascular coagulation; deep vein thrombosis.
As can be seen from the table, side effects that appear related to nimodipine use based on increased incidence with higher dose or a higher rate compared to placebo control, included decreased blood pressure, edema and headaches which are known pharmacologic actions of calcium channel blockers. It must be noted, however, that SAH is frequently accompanied by alterations in consciousness which lead to an under reporting of adverse experiences. Patients who received nimodipine in clinical trials for other indications reported flushing (2.1%), headache (4.1%) and fluid retention (0.3%), typical responses to calcium channel blockers. As a calcium channel blocker, nimodipine may have the potential to exacerbate heart failure in susceptible patients or to interfere with A-V conduction, but these events were not observed.
No clinically significant effects on hematologic factors, renal or hepatic function or carbohydrate metabolism have been causally associated with oral nimodipine. Isolated cases of non-fasting elevated serum glucose levels (0.8%), elevated LDH levels (0.4%), decreased platelet counts (0.3%), elevated alkaline phosphatase levels (0.2%) and elevated SGPT levels (0.2% have been reported rarely.
- DRUG ABUSE AND DEPENDENCE
-
OVERDOSAGE
There have been no reports of overdosage from the oral administration of nimodipine capsules. Symptoms of overdosage would be expected to be related to cardiovascular effects such as excessive peripheral vasodilation with marked systemic hypotension. Clinically significant hypotension due to nimodipine capsules overdosage may require active cardiovascular support with pressor agents. Specific treatments for calcium channel blocker overdose should also be given promptly. Since nimodipine is highly protein-bound, dialysis is not likely to be of benefit.
-
DOSAGE AND ADMINISTRATION
DO NOT ADMINISTER NIMODIPINE CAPSULES INTRAVENOUSLY OR BY OTHER PARENTERAL ROUTES (see WARNINGS).
If nimodipine is inadvertently administered intravenously, clinically significant hypotension may require cardiovascular support with pressor agents. Specific treatments for calcium channel blocker overdose should also be given promptly.
Nimodipine capsules are given orally in the form of gray opaque colored, soft gelatin 30 mg capsules for subarachnoid hemorrhage.
The recommended oral dose is 60 mg (two 30 mg capsules) every 4 hours for 21 consecutive days. In general, the capsules should be swallowed whole with a little liquid, preferably not less than one hour before or two hours after meals. Grapefruit juice is to be avoided (see PRECAUTIONS, Drug Interactions). Oral nimodipine capsules therapy should commence as soon as possible within 96 hours of the onset of subarachnoid hemorrhage.
If the capsule cannot be swallowed, e.g., at the time of surgery, or if the patient is unconscious, a hole should be made in both ends of the capsule with an 18 gauge needle, and the contents of the capsule extracted into a syringe. A parenteral syringe can be used to extract the liquid inside the capsule, but the liquid should always be transferred to a syringe that cannot accept a needle and that is designed for administration orally or via a naso-gastric tube or PEG. To help minimize administration errors, it is recommended that the syringe used for administration be labeled “Not for IV Use”. The contents should then be emptied into the patient’s in situ naso-gastric tube and washed down the tube with 30 mL of normal saline (0.9%).
Severely disturbed liver function, particularly liver cirrhosis, may result in an increased bioavailability of nimodipine due to a decreased first pass capacity and a reduced metabolic clearance. The reduction in blood pressure and other adverse effects may be more pronounced in these patients. Dosage should be reduced to one 30 mg capsule every 4 hours with close monitoring of blood pressure and heart rate; if necessary, discontinuation of the treatment should be considered. Strong inhibitors of CYP3A4 should not be administered concomitantly with nimodipine (see CONTRAINDICATIONS).
Strong inducers of CYP3A4 should generally not be administered with Nimodipine (see WARNINGS). Patients on moderate and weak inducers of CYP3A4 should be closely monitored for lack of effectiveness, and a nimodipine dose increase may be required. Patients on moderate and weak CYP3A4 inhibitors may require a nimodipine dose reduction in case of hypotension (see PRECAUTIONS, Drug Interactions).
- HOW SUPPLIED
- Nimodipine
-
INGREDIENTS AND APPEARANCE
NIMODIPINE
nimodipine capsule, liquid filledProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 63739-797(NDC:67877-297) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength NIMODIPINE (UNII: 57WA9QZ5WH) (NIMODIPINE - UNII:57WA9QZ5WH) NIMODIPINE 30 mg Inactive Ingredients Ingredient Name Strength GLYCERIN (UNII: PDC6A3C0OX) PEPPERMINT OIL (UNII: AV092KU4JH) WATER (UNII: 059QF0KO0R) POLYETHYLENE GLYCOL 400 (UNII: B697894SGQ) GELATIN, UNSPECIFIED (UNII: 2G86QN327L) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FERROSOFERRIC OXIDE (UNII: XM0M87F357) Product Characteristics Color gray (gray opaque) Score no score Shape capsule (softgel capsule) Size 15mm Flavor Imprint Code A297 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 63739-797-33 3 in 1 BOX, UNIT-DOSE 12/29/2016 1 10 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA090103 01/01/2015 Labeler - McKesson Corporation dba SKY Packaging (140529962) Establishment Name Address ID/FEI Business Operations McKesson Corporation dba RX Pak 025183281 REPACK(63739-797)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.