FACT SHEET FOR HEALTHCARE PROVIDERS ADMINISTERING VACCINE (VACCINATION PROVIDERS) EMERGENCY USE AUTHORIZATION (EUA) OF THE MODERNA COVID-19 VACCINE TO PREVENT CORONAVIRUS DISEASE 2019 (COVID-19)
Moderna COVID-19 Vaccine by
Drug Labeling and Warnings
Moderna COVID-19 Vaccine by is a Other medication manufactured, distributed, or labeled by Moderna US, Inc., ModernaTX, Inc., Catalent Indiana, LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
MODERNA COVID-19 VACCINE- cx-024414 injection, suspension
Moderna US, Inc.
----------
FACT SHEET FOR HEALTHCARE PROVIDERS ADMINISTERING VACCINE (VACCINATION PROVIDERS)
EMERGENCY USE AUTHORIZATION (EUA) OF THE MODERNA COVID-19 VACCINE TO PREVENT CORONAVIRUS DISEASE 2019 (COVID-19)
|
|
|
BOOSTER DOSE ONLY PRESENTATION |
The U.S. Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) to permit the emergency use of the unapproved product, Moderna COVID-19 Vaccine, for active immunization to prevent COVID-19 in individuals 6 months of age and older.
SPIKEVAX (COVID-19 Vaccine, mRNA) is an FDA-approved COVID-19 vaccine made by ModernaTX, Inc. that is indicated for active immunization to prevent COVID-19 in individuals 18 years of age and older.1
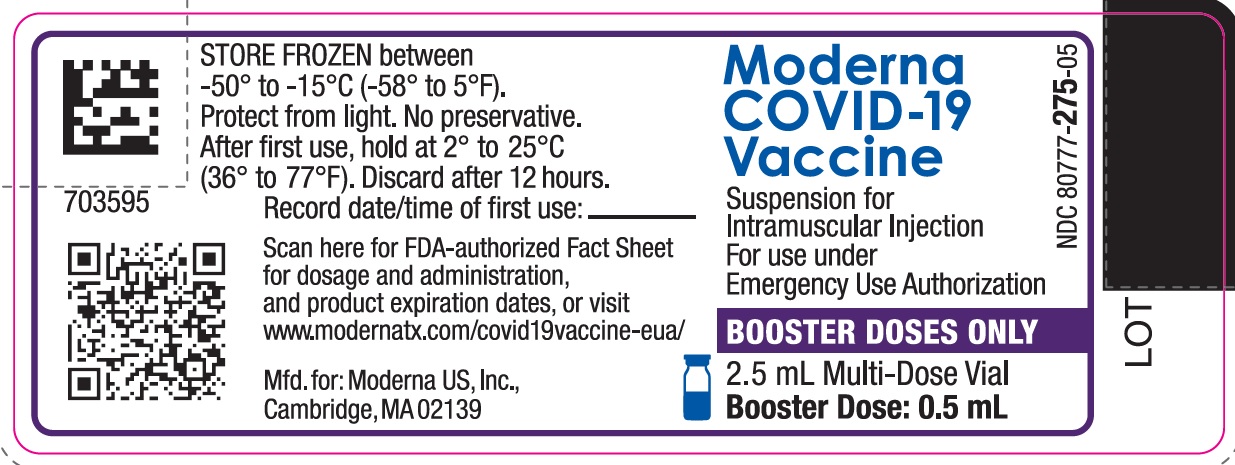
This Fact Sheet pertains only to the following authorized uses of Moderna COVID-19 Vaccine supplied in a multiple-dose vial with a dark blue cap and a label with a purple border:†
- a first booster dose to individuals 18 years of age and older who have completed a primary series with Moderna COVID-19 Vaccine or SPIKEVAX (COVID-19 Vaccine, mRNA);
- a first booster dose to individuals 18 years of age and older who have completed primary vaccination with another authorized or approved COVID-19 vaccine. The dosing interval for the heterologous booster dose is the same as that authorized for a booster dose of the vaccine used for primary vaccination;
- a second booster dose to individuals 50 years of age and older who have received a first booster dose of any authorized or approved COVID-19 vaccine; and
- a second booster dose to individuals 18 years of age and older with certain kinds of immunocompromise2 and who have received a first booster dose of any authorized or approved COVID-19 vaccine.
SUMMARY OF INSTRUCTIONS FOR COVID-19 VACCINATION PROVIDERS
Vaccination providers enrolled in the federal COVID-19 Vaccination Program must report all vaccine administration errors, all serious adverse events, cases of Multisystem Inflammatory Syndrome (MIS) in adults and children, and cases of COVID-19 that result in hospitalization or death following administration of the Moderna COVID-19 Vaccine. See “MANDATORY REQUIREMENTS FOR MODERNA COVID-19 VACCINE ADMINISTRATION UNDER EMERGENCY USE AUTHORIZATION” for reporting requirements.
The Moderna COVID-19 Vaccine is a suspension for intramuscular injection.
Primary Series
For primary series dose and schedule, see the Fact Sheet for the Moderna COVID-19 Vaccine presentation for the relevant age group (6 months through 5 years of age, 6 years through 11 years of age, or 12 years of age and older) or the prescribing information for SPIKEVAX (COVID-19 Vaccine, mRNA).
First Booster Dose
A first booster dose (0.5 mL) of the Moderna COVID-19 Vaccine supplied in a multiple-dose vial with a dark blue cap and a label with a purple border may be administered at least 5 months after completing a primary series of the Moderna COVID-19 Vaccine or SPIKEVAX (COVID-19 Vaccine, mRNA) to individuals 18 years of age or older.
A first booster dose (0.5 mL) of the Moderna COVID-19 Vaccine supplied in a multiple-dose vial with a dark blue cap and a label with a purple border may be administered to individuals 18 years of age and older as a heterologous booster dose following completion of primary vaccination with another authorized or approved COVID-19 vaccine. The dosing interval for the heterologous booster dose is the same as that authorized for a booster dose of the vaccine used for primary vaccination.
Second Booster Dose
A second booster dose (0.5 mL) of the Moderna COVID-19 Vaccine supplied in a multiple-dose vial with a dark blue cap and a label with a purple border may be administered to individuals 50 years of age and older at least 4 months after receipt of a first booster dose of any authorized or approved COVID-19 vaccine.
A second booster dose (0.5 mL) of the Moderna COVID-19 Vaccine supplied in a multiple-dose vial with a dark blue cap and a label with a purple border may be administered at least 4 months after receipt of a first booster dose of any authorized or approved COVID-19 vaccine to individuals 18 years of age and older with certain kinds of immunocompromise.
See this Fact Sheet for instructions for preparation and administration. This Fact Sheet may have been updated. For the most recent Fact Sheet, please see www.modernatx.com/covid19vaccine-eua.
For information on clinical trials that are testing the use of the Moderna COVID-19 Vaccine for active immunization against COVID-19, please see www.clinicaltrials.gov.
DESCRIPTION OF COVID-19
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by the novel coronavirus, SARS-CoV-2, that appeared in late 2019. It is predominantly a respiratory illness that can affect other organs. People with COVID-19 have reported a wide range of symptoms, ranging from mild symptoms to severe illness. Symptoms may appear 2 to 14 days after exposure to the virus. Symptoms may include: fever or chills; cough; shortness of breath; fatigue; muscle and body aches; headache; new loss of taste or smell; sore throat; congestion or runny nose; nausea or vomiting; diarrhea.
DOSAGE AND ADMINISTRATION
Storage and Handling
The information in this Fact Sheet supersedes the information on the vial and carton labels.
During storage, minimize exposure to room light, and avoid exposure to direct sunlight and ultraviolet light.
Frozen Storage
Store frozen between -50°C to -15°C (-58°F to 5°F).
Storage after Thawing
-
Storage at 2°C to 8°C (36°F to 46°F):
- o Vials may be stored refrigerated between 2°C to 8°C (36°F to 46°F) for up to 30 days prior to first use.
- o Vials should be discarded 12 hours after the first puncture.
-
Storage at 8°C to 25°C (46°F to 77°F):
- o Vials may be stored between 8°C to 25°C (46°F to 77°F) for a total of 24 hours.
- o Vials should be discarded 12 hours after the first puncture.
- o Total storage at 8°C to 25°C (46°F to 77°F) must not exceed 24 hours.
Do not refreeze once thawed.
Thawed vials can be handled in room light conditions.
Transportation of Thawed Vials at 2°C to 8°C (36°F to 46°F)
If transport at -50°C to -15°C (-58°F to 5°F) is not feasible, available data support transportation of one or more thawed vials for up to 12 hours at 2°C to 8°C (36°F to 46°F) when shipped using shipping containers which have been qualified to maintain 2°C to 8°C (36°F to 46°F) and under routine road and air transport conditions with shaking and vibration minimized. Once thawed and transported at 2°C to 8°C (36°F to 46°F), vials should not be refrozen and should be stored at 2°C to 8°C (36°F to 46°F) until use.
Dosing and Schedule
Primary Series
For primary series dose and schedule, see the Fact Sheet for the Moderna COVID-19 Vaccine presentation for the relevant age group (6 months through 5 years of age, 6 years through 11 years of age, or 12 years of age and older) or the prescribing information for SPIKEVAX (COVID-19 Vaccine, mRNA).
First Booster Dose
A first booster dose (0.5 mL) of the Moderna COVID-19 Vaccine supplied in a multiple-dose vial with a dark blue cap and a label with a purple border may be administered at least 5 months after completing a primary series of the Moderna COVID-19 Vaccine or SPIKEVAX (COVID-19 Vaccine, mRNA) to individuals 18 years of age or older.
A first booster dose (0.5 mL) of the Moderna COVID-19 Vaccine supplied in a multiple-dose vial with a dark blue cap and a label with a purple border may be administered to individuals 18 years of age and older as a heterologous booster dose following completion of primary vaccination with another authorized or approved COVID-19 vaccine. The dosing interval for the heterologous booster dose is the same as that authorized for a booster dose of the vaccine used for primary vaccination.
Second Booster Dose
A second booster dose (0.5 mL) of the Moderna COVID-19 Vaccine supplied in a multiple-dose vial with a dark blue cap and a label with a purple border may be administered to individuals 50 years of age and older at least 4 months after receipt of a first booster dose of any authorized or approved COVID-19 vaccine.
A second booster dose (0.5 mL) of the Moderna COVID-19 Vaccine supplied in a multiple-dose vial with a dark blue cap and a label with a purple border may be administered at least 4 months after receipt of a first booster dose of any authorized or approved COVID-19 vaccine to individuals 18 years of age and older with certain kinds of immunocompromise.
Preparation for Administration
- The Moderna COVID-19 Vaccine multiple-dose vial with a dark blue cap and a label with a purple border contains a volume of 2.5 mL and is supplied as a frozen suspension that does not contain a preservative and must be thawed prior to administration.
- Verify that the vial of Moderna COVID-19 Vaccine has a dark blue cap and a label with a purple border.
- Thaw each vial before use following the instructions below.
Thawing Instructions for Moderna COVID-19 Vaccine Multiple-Dose Vials with Dark Blue Caps and Labels with a Purple Border
|
Thaw in Refrigerator |
Thaw at Room Temperature |
|
Thaw between 2°C to 8°C (36°F to 46°F) for 2 hours. Let each vial stand at room temperature for 15 minutes before administering. |
Alternatively, thaw between 15°C to 25°C (59°F to 77°F) for 45 minutes. |
- After thawing, do not refreeze.
- Swirl vial gently after thawing and between each withdrawal. Do not shake. Do not dilute the vaccine.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
- The Moderna COVID-19 Vaccine is a white to off-white suspension. It may contain white or translucent product-related particulates. Do not administer if vaccine is discolored or contains other particulate matter.
- Each multiple dose vial with a dark blue cap and a label with a purple border contains 5 booster doses of 0.5 mL.
- If the amount of vaccine remaining in the vial cannot provide a full dose of 0.5 mL, discard the vial and contents. Do not pool excess vaccine from multiple vials.
- After the first 0.5 mL booster dose has been withdrawn, the vial should be held between 2°C to 25°C (36°F to 77°F). Record the date and time of first use on the Moderna COVID-19 Vaccine vial label. Discard vial after 12 hours. Do not refreeze.
CONTRAINDICATION
Do not administer the Moderna COVID-19 Vaccine to individuals with a known history of a severe allergic reaction (e.g., anaphylaxis) to any component of the Moderna COVID-19 Vaccine (see Full EUA Prescribing Information).
WARNINGS
Management of Acute Allergic Reactions
Appropriate medical treatment to manage immediate allergic reactions must be immediately available in the event an acute anaphylactic reaction occurs following administration of the Moderna COVID-19 Vaccine.
Monitor Moderna COVID-19 Vaccine recipients for the occurrence of immediate adverse reactions according to the Centers for Disease Control and Prevention (CDC) guidelines (https://www.cdc.gov/vaccines/covid-19/clinical-considerations/managing-anaphylaxis.html).
Myocarditis and Pericarditis
Postmarketing data demonstrate increased risks of myocarditis and pericarditis, particularly within 7 days following the second dose. The observed risk is highest in males 18 through 24 years of age. Although some cases required intensive care support, available data from short-term follow-up suggest that most individuals have had resolution of symptoms with conservative management. Information is not yet available about potential long-term sequelae.
Some, but not all, observational analyses of postmarketing data suggest that there may be an increased risk of myocarditis and pericarditis in males under 40 years of age following the second dose of the Moderna COVID-19 Vaccine relative to other authorized or approved mRNA COVID-19 vaccines. Although postmarketing data following a booster dose of mRNA vaccines are limited, available evidence suggests a lower myocarditis risk following a booster dose relative to the risk following the primary series second dose.
The CDC has published considerations related to myocarditis and pericarditis after vaccination, including for vaccination of individuals with a history of myocarditis or pericarditis (https://www.cdc.gov/vaccines/covid-19/clinical-considerations/myocarditis.html).
Syncope
Syncope (fainting) may occur in association with administration of injectable vaccines. Procedures should be in place to avoid injury from fainting.
Altered Immunocompetence
Immunocompromised persons, including individuals receiving immunosuppressant therapy, may have a diminished immune response to the Moderna COVID-19 Vaccine.
Limitations of Vaccine Effectiveness
The Moderna COVID-19 Vaccine may not protect all vaccine recipients.
ADVERSE REACTIONS
Adverse Reactions in Clinical Trials
Adverse reactions reported in clinical trials following administration of the Moderna COVID-19 Vaccine include pain at the injection site, fatigue, headache, myalgia, arthralgia, chills, nausea/vomiting, axillary swelling/tenderness, fever, swelling at the injection site, erythema at the injection site, and rash. (See Full EUA Prescribing Information)
Adverse Reactions in Post-Authorization Experience
Anaphylaxis and other severe allergic reactions, myocarditis, pericarditis, and syncope have been reported following administration of the Moderna COVID-19 Vaccine outside of clinical trials.
Additional adverse reactions, some of which may be serious, may become apparent with more widespread use of the Moderna COVID-19 Vaccine.
USE WITH OTHER VACCINES
There is no information on the co-administration of the Moderna COVID-19 Vaccine with other vaccines.
INFORMATION TO PROVIDE TO VACCINE RECIPIENTS/CAREGIVERS
As the vaccination provider, you must communicate to the recipient or their caregiver, information consistent with the “Vaccine Information Fact Sheet for Recipients and Caregivers” (and provide a copy or direct the individual to the website www.modernatx.com/covid19vaccine-eua to obtain the Fact Sheet) prior to the individual receiving each dose of the Moderna COVID-19 Vaccine, including:
- FDA has authorized the emergency use of the Moderna COVID-19 Vaccine, which is not an FDA-approved vaccine.
- The recipient or their caregiver has the option to accept or refuse the Moderna COVID-19 Vaccine.
- The significant known and potential risks and benefits of the Moderna COVID-19 Vaccine, and the extent to which such risks and benefits are unknown.
- Information about available alternative vaccines and the risks and benefits of those alternatives.
For information on clinical trials that are evaluating the use of the Moderna COVID-19 Vaccine to prevent COVID-19, please see www.clinicaltrials.gov.
Provide a vaccination card to the recipient or their caregiver with the date when the recipient needs to return for the second dose of Moderna COVID-19 Vaccine.
Provide the v-safe information sheet to vaccine recipients/caregivers and encourage vaccine recipients to participate in v-safe. V-safe is a voluntary smartphone-based tool that uses text messaging and web surveys to check in with people who have been vaccinated to identify potential side effects after COVID-19 vaccination. V-safe asks questions that help CDC monitor the safety of COVID-19 vaccines. V-safe also provides second-dose reminders if needed and live telephone follow-up by CDC if participants report a significant health impact following COVID-19 vaccination. For more information, visit: www.cdc.gov/vsafe.
MANDATORY REQUIREMENTS FOR MODERNA COVID-19 VACCINE ADMINISTRATION UNDER EMERGENCY USE AUTHORIZATION7
In order to mitigate the risks of using this unapproved product under EUA and to optimize the potential benefit of the Moderna COVID-19 Vaccine, the following items are required. Use of unapproved Moderna COVID-19 Vaccine for active immunization to prevent COVID-19 under this EUA is limited to the following (all requirements must be met):
- 1. The Moderna COVID-19 Vaccine is authorized for use in individuals 6 months of age and older.
- 2. The vaccination provider must communicate to the individual receiving the Moderna COVID-19 Vaccine or their caregiver information consistent with the “Vaccine Information Fact Sheet for Recipients and Caregivers” prior to the individual receiving the Moderna COVID-19 Vaccine.
- 3. The vaccination provider must include vaccination information in the state/local jurisdiction’s Immunization Information System (IIS) or other designated system.
- 4.
The vaccination provider is responsible for mandatory reporting of the following to the Vaccine Adverse Event Reporting System (VAERS):
- vaccine administration errors whether or not associated with an adverse event,
- serious adverse events* (irrespective of attribution to vaccination),
- cases of Multisystem Inflammatory Syndrome (MIS) in adults and children, and
- cases of COVID-19 that result in hospitalization or death.
Complete and submit reports to VAERS online at https://vaers.hhs.gov/reportevent.html. For further assistance with reporting to VAERS, call 1-800-822-7967. The reports should include the words “Moderna COVID-19 Vaccine EUA” in the description section of the report.
- 5. The vaccination provider is responsible for responding to FDA requests for information about vaccine administration errors, adverse events, cases of MIS in adults and children, and cases of COVID-19 that result in hospitalization or death following administration of the Moderna COVID-19 Vaccine to recipients.
*Serious adverse events are defined as:
- Death;
- A life-threatening adverse event;
- Inpatient hospitalization or prolongation of existing hospitalization;
- A persistent or significant incapacity or substantial disruption of the ability to conduct normal life functions;
- A congenital anomaly/birth defect;
- An important medical event that based on appropriate medical judgement may jeopardize the individual and may require medical or surgical intervention to prevent one of the outcomes listed above.
OTHER ADVERSE EVENT REPORTING TO VAERS AND MODERNATX, INC.
Vaccination providers may report to VAERS other adverse events that are not required to be reported using the contact information above.
To the extent feasible, report adverse events to ModernaTX, Inc. using the contact information below or by providing a copy of the VAERS form to ModernaTX, Inc.
|
|
Fax number |
Telephone number |
|
1-866-599-1342 |
1-866-MODERNA (1-866-663-3762) |
ADDITIONAL INFORMATION
For general questions, visit the website or call the telephone number provided below.
To access the most recent Moderna COVID-19 Vaccine Fact Sheets, please scan the QR code or visit the website provided below.
|
Website |
Telephone number |
|
www.modernatx.com/covid19vaccine-eua 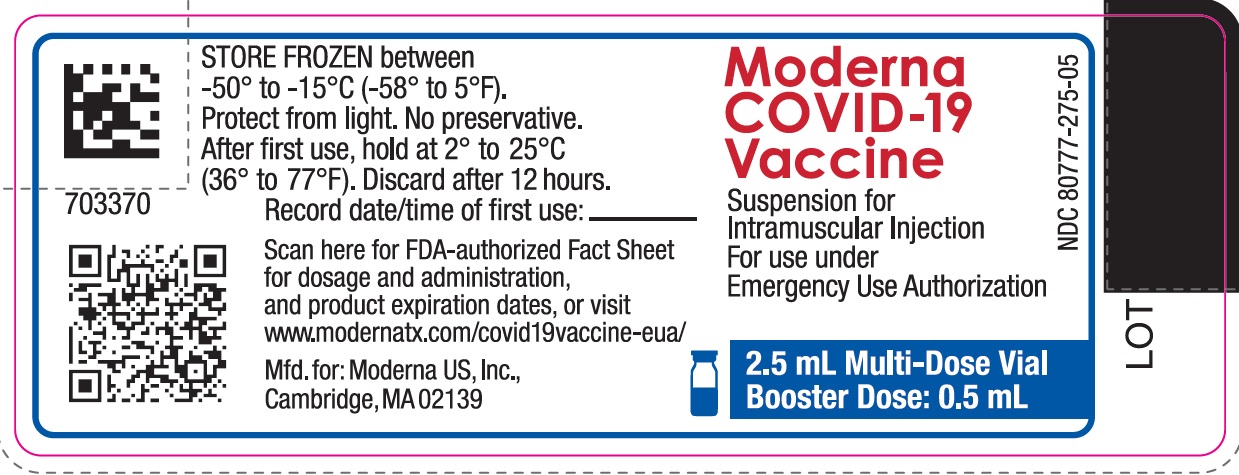 |
1-866-MODERNA (1-866-663-3762) |
AVAILABLE ALTERNATIVES
SPIKEVAX (COVID-19 Vaccine, mRNA) and COMIRNATY (COVID-19 Vaccine, mRNA) are FDA-approved vaccines to prevent COVID-19 caused by SARS-CoV-2. There may be clinical trials or availability under EUA of other COVID-19 vaccines.
FEDERAL COVID-19 VACCINATION PROGRAM
This vaccine is being made available for emergency use exclusively through the CDC COVID-19 Vaccination Program (the Vaccination Program). Healthcare providers must enroll as providers in the Vaccination Program and comply with the provider requirements. Vaccination providers may not charge any fee for the vaccine and may not charge the vaccine recipient any out-of-pocket charge for administration. However, vaccination providers may seek appropriate reimbursement from a program or plan that covers COVID-19 vaccine administration fees for the vaccine recipient (private insurance, Medicare, Medicaid, HRSA COVID-19 Uninsured Program for non-insured recipients). For information regarding provider requirements and enrollment in the CDC COVID-19 Vaccination Program, see https://www.cdc.gov/vaccines/covid-19/provider-enrollment.html.
Individuals becoming aware of any potential violations of the CDC COVID-19 Vaccination Program requirements are encouraged to report them to the Office of the Inspector General, U.S. Department of Health and Human Services, at 1-800-HHS-TIPS or TIPS.HHS.GOV.
AUTHORITY FOR ISSUANCE OF THE EUA
The Secretary of the Department of Health and Human Services (HHS) has declared a public health emergency that justifies the emergency use of drugs and biological products during the COVID-19 Pandemic. In response, the FDA has issued an EUA for the unapproved product, Moderna COVID-19 Vaccine, and for certain uses of FDA-approved SPIKEVAX (COVID-19 Vaccine, mRNA) for active immunization to prevent COVID-19.
FDA issued this EUA, based on ModernaTX, Inc.’s request and submitted data.
For the authorized uses, although limited scientific information is available, based on the totality of the scientific evidence available to date, it is reasonable to believe that the Moderna COVID-19 Vaccine and SPIKEVAX (COVID-19 Vaccine, mRNA) may be effective for the prevention of COVID-19 in individuals as specified in the Full EUA Prescribing Information.
This EUA for the Moderna COVID-19 Vaccine and SPIKEVAX (COVID-19 Vaccine, mRNA) will end when the Secretary of HHS determines that the circumstances justifying the EUA no longer exist or when there is a change in the approval status of the product such that an EUA is no longer needed.
For additional information about Emergency Use Authorization, visit FDA at: https://www.fda.gov/emergency-preparedness-and-response/mcm-legal-regulatory-and-policy- framework/emergency-use-authorization.
COUNTERMEASURES INJURY COMPENSATION PROGRAM
The Countermeasures Injury Compensation Program (CICP) is a federal program that has been created to help pay for related costs of medical care and other specific expenses to compensate people injured after use of certain medical countermeasures. Medical countermeasures are specific vaccines, medications, devices, or other items used to prevent, diagnose, or treat the public during a public health emergency or a security threat. For more information about CICP regarding the vaccines to prevent COVID-19, visit http://www.hrsa.gov/cicp, email cicp@hrsa.gov, or call: 1-855-266-2427.
Moderna US, Inc.
Cambridge, MA 02139
©2022 ModernaTX, Inc. All rights reserved.
Patent(s): www.modernatx.com/patents
Revised: June/17/2022
END SHORT VERSION FACT SHEET
Long Version (Full EUA Prescribing Information) Begins On Next Page
FULL EMERGENCY USE AUTHORIZATION (EUA) PRESCRIBING INFORMATION
MODERNA COVID-19 VACCINE
|
11 USE IN SPECIFIC POPULATIONS |
|
|
1 AUTHORIZED USE |
11.1 Pregnancy |
|
2 DOSAGE AND ADMINISTRATION |
11.2 Lactation |
|
2.1 Preparation for Administration |
11.3 Pediatric Use |
|
2.2 Administration |
11.4 Geriatric Use 13 DESCRIPTION |
|
2.3 Dosing and Schedule |
|
|
3 DOSAGE FORMS AND STRENGTHS |
14 CLINICAL PHARMACOLOGY |
|
4 CONTRAINDICATIONS |
14.1 Mechanism of Action |
|
5 WARNINGS AND PRECAUTIONS |
18 CLINICAL TRIAL RESULTS AND |
|
5.1 Management of Acute Allergic Reactions |
SUPPORTING DATA FOR EUA 18.1 Efficacy of Two-Dose Primary Series in Participants 18 Years and Older 18.2 Immunogenicity of a First Booster Dose Following a Moderna COVID-19 Vaccine Primary Series in Participants 18 Years and Older 18.3 Immunogenicity of a First Booster Dose Following Primary Vaccination with Another Authorized or Approved COVID-19 Vaccine 18.4 Immunogenicity of a Second Booster Dose 19 HOW SUPPLIED/STORAGE AND HANDLING 20 PATIENT COUNSELING INFORMATION 21 CONTACT INFORMATION *Sections or subsections omitted from the full prescribing information are not listed |
|
5.2 Myocarditis and Pericarditis |
|
|
5.3 Syncope |
|
|
5.4 Altered Immunocompetence |
|
|
5.5 Limitations of Vaccine Effectiveness |
|
|
6 OVERALL SAFETY SUMMARY |
|
|
6.1 Clinical Trials Experience |
|
|
6.2 Post-Authorization Experience |
|
|
8 REQUIREMENTS AND INSTRUCTIONS FOR REPORTING ADVERSE EVENTS AND VACCINE ADMINISTRATION ERRORS |
|
|
10 DRUG INTERACTIONS |
1 AUTHORIZED USE
Moderna COVID-19 Vaccine is authorized for use under an Emergency Use Authorization (EUA) for active immunization to prevent coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in individuals 6 months of age and older.
This EUA Prescribing Information pertains only to Moderna COVID-19 Vaccine supplied in a multiple-dose vial with a dark blue cap and a label with a purple border which is authorized for use for booster doses in individuals 18 years of age and older.
2 DOSAGE AND ADMINISTRATION
For intramuscular injection only.
The storage, preparation, and administration information in this EUA Prescribing Information apply to the Moderna COVID-19 Vaccine, supplied in a multiple-dose vial with a dark blue cap and a label with a purple border, which is authorized for use for booster doses in individuals 18 years of age and older.
2.1 Preparation for Administration
- The Moderna COVID-19 Vaccine multiple-dose vial with a dark blue cap and a label with a purple border contains a volume of 2.5 mL and is supplied as a frozen suspension that does not contain a preservative and must be thawed prior to administration.
- Verify that the vial of Moderna COVID-19 Vaccine has a dark blue cap and a label with a purple border.
- Thaw each vial before use following the instructions below.
Thawing Instructions for Moderna COVID-19 Vaccine Multiple-Dose Vials with Dark Blue Caps and Labels with a Purple Border
|
Thaw in Refrigerator |
Thaw at Room Temperature |
|
Thaw between 2°C to 8°C (36°F to 46°F) for 2 hours. Let each vial stand at room temperature for 15 minutes before administering. |
Alternatively, thaw between 15°C to 25°C (59°F to 77°F) for 45 minutes. |
- After thawing, do not refreeze.
- Swirl vial gently after thawing and between each withdrawal. Do not shake. Do not dilute the vaccine.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
- The Moderna COVID-19 Vaccine is a white to off-white suspension. It may contain white or translucent product-related particulates. Do not administer if vaccine is discolored or contains other particulate matter.
- Each multiple-dose vial with a dark blue cap and a label with a purple border contains 5 booster doses of 0.5 mL.
- If the amount of vaccine remaining in the vial cannot provide a full dose of 0.5 mL, discard the vial and contents. Do not pool excess vaccine from multiple vials.
- After the first 0.5 mL booster dose has been withdrawn, the vial should be held between 2°C to 25°C (36°F to 77°F). Record the date and time of first use on the Moderna COVID-19 Vaccine vial label. Discard vial after 12 hours. Do not refreeze.
2.3 Dosing and Schedule
Primary Series
For primary series dose and schedule, see the Fact Sheet for the Moderna COVID-19 Vaccine presentation for the relevant age group (6 months through 5 years of age, 6 years through 11 years of age, or 12 years of age and older) or the prescribing information for SPIKEVAX (COVID-19 Vaccine, mRNA).
First Booster Dose
A first booster dose (0.5 mL) of the Moderna COVID-19 Vaccine supplied in a multiple-dose vial with a dark blue cap and a label with a purple border may be administered at least 5 months after completing a primary series of the Moderna COVID-19 Vaccine or SPIKEVAX (COVID-19 Vaccine, mRNA) to individuals 18 years of age or older.
A first booster dose (0.5 mL) of the Moderna COVID-19 Vaccine supplied in a multiple-dose vial with a dark blue cap and a label with a purple border may be administered to individuals 18 years of age and older as a heterologous booster dose following completion of primary vaccination with another authorized or approved COVID-19 vaccine. The dosing interval for the heterologous booster dose is the same as that authorized for a booster dose of the vaccine used for primary vaccination.
Second Booster Dose
A second booster dose (0.5 mL) of the Moderna COVID-19 Vaccine supplied in a multiple-dose vial with a dark blue cap and a label with a purple border may be administered to individuals 50 years of age and older at least 4 months after receipt of a first booster dose of any authorized or approved COVID-19 vaccine.
A second booster dose (0.5 mL) of the Moderna COVID-19 Vaccine supplied in a multiple-dose vial with a dark blue cap and a label with a purple border may be administered at least 4 months after receipt of a first booster dose of any authorized or approved COVID-19 vaccine to individuals 18 years of age and older with certain kinds of immunocompromise.10
3 DOSAGE FORMS AND STRENGTHS
Moderna COVID-19 Vaccine supplied in a multiple-dose vial with a dark blue cap and a label with a purple border is a suspension for injection.
- The booster dose is 0.5 mL.
4 CONTRAINDICATIONS
Do not administer the Moderna COVID-19 Vaccine to individuals with a known history of severe allergic reaction (e.g., anaphylaxis) to any component of the Moderna COVID-19 Vaccine [see Description (13)].
5 WARNINGS AND PRECAUTIONS
5.1 Management of Acute Allergic Reactions
Appropriate medical treatment to manage immediate allergic reactions must be immediately available in the event an acute anaphylactic reaction occurs following administration of the Moderna COVID-19 Vaccine.
Monitor Moderna COVID-19 Vaccine recipients for the occurrence of immediate adverse reactions according to the Centers for Disease Control and Prevention (CDC) guidelines (https://www.cdc.gov/vaccines/covid-19/clinical-considerations/managing-anaphylaxis.html).
5.2 Myocarditis and Pericarditis
Postmarketing data demonstrate increased risks of myocarditis and pericarditis, particularly within 7 days following the second dose. The observed risk is highest in males 18 through 24 years of age. Although some cases required intensive care support, available data from short-term follow-up suggest that most individuals have had resolution of symptoms with conservative management. Information is not yet available about potential long-term sequelae.
Some, but not all, observational analyses of postmarketing data suggest that there may be an increased risk of myocarditis and pericarditis in males under 40 years of age following the second dose of the Moderna COVID-19 Vaccine relative to other authorized or approved mRNA COVID-19 vaccines. Although postmarketing data following a booster dose of mRNA vaccines are limited, available evidence suggests a lower myocarditis risk following a booster dose relative to the risk following the primary series second dose.
The CDC has published considerations related to myocarditis and pericarditis after vaccination, including for vaccination of individuals with a history of myocarditis or pericarditis (https://www.cdc.gov/vaccines/covid-19/clinical-considerations/myocarditis.html).
5.3 Syncope
Syncope (fainting) may occur in association with administration of injectable vaccines. Procedures should be in place to avoid injury from fainting.
6 OVERALL SAFETY SUMMARY
It is MANDATORY for vaccination providers to report to the Vaccine Adverse Event Reporting System (VAERS) all vaccine administration errors, all serious adverse events, cases of Multisystem Inflammatory Syndrome (MIS) in adults and children, and hospitalized or fatal cases of COVID-19 following vaccination with the Moderna COVID-19 Vaccine.11 To the extent feasible, provide a copy of the VAERS form to ModernaTX, Inc. Please see the REQUIREMENTS AND INSTRUCTIONS FOR REPORTING ADVERSE EVENTS AND VACCINE ADMINISTRATION ERRORS section for details on reporting to VAERS and ModernaTX, Inc.
Primary Series
In a clinical study, the adverse reactions in participants 18 years of age and older following administration of the primary series included pain at the injection site (92.0%), fatigue (70.0%), headache (64.7%), myalgia (61.5%), arthralgia (46.4%), chills (45.4%), nausea/vomiting (23.0%), axillary swelling/tenderness (19.8%), fever (15.5%), swelling at the injection site (14.7%), and erythema at the injection site (10.0%).
Booster Dose
In a clinical study, the adverse reactions in participants 18 years of age and older following administration of a booster dose included pain at the injection site (83.8%), fatigue (58.7%), headache (55.1%), myalgia (49.1%), arthralgia (41.3%), chills (35.3%), axillary swelling/tenderness (20.4%), nausea/vomiting (11.4%), fever (6.6%), swelling at the injection site (5.4%), erythema at the injection site (4.8%), and rash (1.8%).
Post-Authorization Experience
Anaphylaxis and other severe allergic reactions, myocarditis, pericarditis, and syncope have been reported following administration of the Moderna COVID-19 Vaccine outside of clinical trials.
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a vaccine cannot be directly compared with rates in the clinical trials of another vaccine and may not reflect the rates observed in practice.
Overall, 39,000 participants aged 6 months and older received at least one dose of Moderna COVID-19 Vaccine in five clinical trials (NCT04283461, NCT04405076, NCT04470427, NCT04649151, and NCT04796896).
Study 1 (NCT04470427) is a Phase 3 randomized, placebo-controlled, observer-blind clinical trial conducted in the United States involving 30,346 participants 18 years of age and older who received at least one dose of Moderna COVID-19 Vaccine12 (n=15,184) or placebo (n=15,162). Study 2 (NCT04405076) is a Phase 2, randomized, observer-blind, placebo-controlled, dose-confirmation study, which included an open-label phase involving 171 participants 18 years of age and older who received a booster dose of Moderna COVID-19 Vaccine 6 months (range of 5.8 months to 8.5 months) after receiving the second dose of the primary series. Study 3 (NCT04649151) is a Phase 2/3 randomized, placebo-controlled, observer-blind, clinical trial conducted in the United States involving 3,726 participants 12 years through 17 years of age who received at least one dose of Moderna COVID-19 Vaccine (n=2,486) or placebo (n=1,240). Study 4 (NCT04796896) includes an ongoing Phase 2/3 randomized, placebo-controlled, observer-blind clinical trial component conducted in the United States and Canada involving 10,390 participants 6 months through 11 years of age who received at least one dose of Moderna COVID-19 Vaccine (n=7,799) or placebo (n=2,591).
Two-Dose Primary Series in Participants 18 Years and Older
The safety of Moderna COVID-19 Vaccine was evaluated in an ongoing Phase 3 randomized, placebo-controlled, observer-blind clinical trial conducted in the United States involving 30,346 participants 18 years of age and older who received at least one dose of Moderna COVID-19 Vaccine (n=15,184) or placebo (n=15,162) (Study 1, NCT04470427). Upon issuance of the Emergency Use Authorization (December 18, 2020) for Moderna COVID-19 Vaccine, participants were unblinded in a phased manner over a period of months to offer placebo participants Moderna COVID-19 Vaccine. The median duration of follow up for safety after the second injection during the blinded phase was 4 months. The median duration of follow up for safety after the second injection including both the blinded phase and the open-label phase was 6 months.
In Study 1, the median age of the population was 52 years (range 18-95); 22,826 (75.2%) participants were 18 to 64 years of age and 7,520 (24.8%) participants were 65 years of age and older. Overall, 52.6% of the participants were male, 47.4% were female, 20.5% were Hispanic or Latino, 79.2% were White, 10.2% were African American, 4.6% were Asian, 0.8% were American Indian or Alaska Native, 0.2% were Native Hawaiian or Pacific Islander, 2.0% were other races, and 2.1% were Multiracial. Demographic characteristics were similar between participants who received Moderna COVID-19 Vaccine and those who received placebo.
Unsolicited Adverse Events
Participants were monitored for unsolicited adverse events for 28 days following each dose. Serious adverse events and medically attended adverse events will be recorded for the entire study duration (2 years). Among the 30,346 participants who had received at least 1 dose of vaccine (N=15,184) or placebo (N=15,162), unsolicited adverse events that occurred within 28 days following any vaccination were reported by 31.3% of participants (n=4,752) who received Moderna COVID-19 Vaccine and 28.6% of participants (n=4,338) who received placebo.
During the 28-day follow-up period following any dose, lymphadenopathy-related events were reported by 1.7% of vaccine recipients and 0.8% of placebo recipients. These events included lymphadenopathy, lymphadenitis, lymph node pain, vaccination-site lymphadenopathy, injection-site lymphadenopathy, and axillary mass.
During the 7-day follow-up period of any vaccination, hypersensitivity events of injection site rash or injection site urticaria, likely related to vaccination, were reported by 6 participants in the Moderna COVID-19 Vaccine group and none in the placebo group. Delayed injection site reactions that began >7 days after vaccination were reported in 1.4% of vaccine recipients and 0.7% of placebo recipients. Delayed injection site reactions included pain, erythema, and swelling and are likely related to vaccination.
In the blinded portion of the study, there were 8 reports of facial paralysis (including Bell’s palsy) in the Moderna COVID-19 Vaccine group, and 3 in the placebo group. In the 28-day follow-up period there were two cases of facial paralysis in the Moderna COVID-19 Vaccine group, which occurred on 8 and 22 days, respectively, after vaccination, and one in the placebo group, which occurred 17 days after vaccination. Currently available information on facial paralysis is insufficient to determine a causal relationship with the vaccine.
In the blinded portion of the study, there were 50 reports of herpes zoster in the Moderna COVID-19 Vaccine group, and 23 in the placebo group. In the 28-day period after any vaccination, there were 22 cases of herpes zoster in the SPIKEVAX group, and 15 in the placebo group. Currently available information on herpes zoster infection is insufficient to determine a causal relationship with the vaccine.
There were no other notable patterns or numerical imbalances between treatment groups for specific categories of adverse events (including other neurologic, neuro-inflammatory, and thrombotic events) that would suggest a causal relationship to Moderna COVID-19 Vaccine.
Serious Adverse Events
During the blinded phase of the study, serious adverse events were reported by 1.8% (n=268) of participants who received Moderna COVID-19 Vaccine and 1.9% (n=292) of participants who received placebo.
There were three serious adverse events of angioedema/facial swelling in the vaccine group in recipients with a history of injection of dermatological fillers. The onset of swelling was reported 1-2 days after the second dose and was likely related to vaccination.
There were no other notable patterns or imbalances between treatment groups for specific categories of serious adverse events (including neurologic, neuro-inflammatory, and thrombotic events) that would suggest a causal relationship to Moderna COVID-19 Vaccine.
First Booster Dose Following a Primary Series of Moderna COVID-19 Vaccine or SPIKEVAX (COVID-19 Vaccine, mRNA) in Participants 18 Years and Older
Study 2 is an ongoing Phase 2, randomized, observer-blind, placebo-controlled, dose-confirmation study to evaluate the safety, reactogenicity, and immunogenicity of the Moderna COVID-19 Vaccine in participants 18 years of age and older (NCT04405076). In this study, 198 participants received two doses 1 month apart of the Moderna COVID-19 Vaccine primary series. In an open label-phase, 171 of those participants received a single booster dose at least 6 months (range of 5.8 to 8.5 months) after receiving the second dose of the primary series. Safety monitoring after the booster dose was the same as that described for Study 1 participants who received the primary series.
Among the 171 booster dose recipients, the median age was 55 years (range 18-87), 39.2% were male and 60.8% were female, 95.9% were White, 5.8% were Hispanic or Latino, 2.9% were Black or African American, 0.6% were Asian, and 0.6% were American Indian or Alaska Native. Following the booster dose, the median follow-up time was 5.7 months (range of 3.1 to 6.4 months).
Solicited Adverse Reactions
presents the frequency and severity of reported solicited local and systemic adverse reactions among Study 2 Moderna COVID-19 Vaccine booster dose recipients 18 to <65 years of age and ≥65 years of age within 7 days of a booster vaccination.
| Participants
18 Years Through 64 Years (N=129) n (%) | Participants
≥65 Years (N=38) n (%) |
|
|---|---|---|
|
Local Adverse Reactions | ||
|
Pain |
111 (86.0) |
29 (76.3) |
|
Pain, Grade 3a |
4 (3.1) |
2 (5.3) |
|
Axillary swelling/tenderness |
32 (24.8) |
2 (5.3) |
|
Axillary swelling/tenderness, Grade 3a |
1 (0.8) |
0 (0) |
|
Swelling (hardness) ≥25 mm |
8 (6.2) |
1 (2.6) |
|
Swelling (hardness) ≥25 mm, Grade 3b |
0 (0) |
1 (2.6) |
|
Erythema (redness) ≥25 mm |
7 (5.4) |
1 (2.6) |
|
Erythema (redness), Grade 3b |
1 (0.8) |
0 (0.0) |
|
Systemic Adverse Reactions | ||
|
Fatigue |
80 (62.0) |
18 (47.4) |
|
Fatigue, Grade 3c |
4 (3.1) |
3 (7.9) |
|
Headache |
76 (58.9) |
16 (42.1) |
|
Headache, Grade 3d |
1 (0.8) |
1 (2.6) |
|
Myalgia |
64 (49.6) |
18 (47.4) |
|
Myalgia, Grade 3c |
4 (3.1) |
1 (2.6) |
|
Arthralgia |
54 (41.9) |
15 (39.5) |
|
Arthralgia, Grade 3c |
4 (3.1) |
1 (2.6) |
|
Chills |
52 (40.3) |
7 (18.4) |
|
Nausea/vomiting |
16 (12.4) |
3 (7.9) |
|
Fever |
9 (7.0) |
2 (5.4) |
|
Fever, Grade 3e |
2 (1.6) |
0 (0.0) |
|
Rash |
3 (2.3) |
0 (0) |
|
Use of antipyretic or pain medication |
64 (49.6) |
11 (28.9) |
|
* 7 days included day of vaccination and the subsequent 6 days. Events and use of antipyretic or pain medication were collected in the electronic diary (e-diary). † Absence of rows for Grade 3 or Grade 4 adverse reactions indicates no events were reported. a Grade 3 pain and axillary swelling/tenderness: Defined as any use of prescription pain reliever; prevents daily activity. b Grade 3 swelling and erythema: Defined as >100 mm / >10 cm. c Grade 3 fatigue, myalgia, arthralgia: Defined as significant; prevents daily activity. d Grade 3 headache: Defined as significant; any use of prescription pain reliever or prevents daily activity. e Grade 3 fever: Defined as ≥39.0° – ≤40.0°C / ≥102.1° – ≤104.0°F. |
||
In participants who received a booster dose, the median duration of solicited local and systemic adverse reactions was 2 to 3 days.
Unsolicited Adverse Events
Overall, the 171 participants who received a booster dose had a median follow-up time of 5.7 months after the booster dose to the cut-off date (August 16, 2021). Through the cut-off date, there were no unsolicited adverse events not already captured as solicited local and systemic reactions that were considered causally related to the Moderna COVID-19 Vaccine.
Serious Adverse Events
Of the 171 participants who received a booster dose of Moderna COVID-19 Vaccine, there were no serious adverse events reported from the booster dose through 28 days after the booster dose. Through the cut-off date of August 16, 2021, there were no serious adverse events following the booster dose considered causally related to the Moderna COVID-19 Vaccine.
First Booster Dose Following Primary Vaccination with Another Authorized or Approved COVID-19 Vaccine
The safety of a Moderna COVID-19 Vaccine booster dose in individuals who completed primary vaccination with another authorized or approved COVID-19 vaccine (heterologous booster dose) is inferred from the safety of a Moderna COVID-19 Vaccine booster dose administered following completion of a Moderna COVID-19 Vaccine primary series (homologous booster dose) and from data from an independent Phase 1/2 open-label clinical trial (NCT04889209) conducted in the United States that evaluated a booster dose of the Moderna COVID-19 Vaccine. The booster dose that study participants received contained twice the amount of mRNA compared to the authorized booster dose of the Moderna COVID-19 Vaccine. In this study, adults who had completed primary vaccination with a Moderna COVID-19 Vaccine 2-dose series (N=151), a Janssen COVID-19 Vaccine single dose (N=156), or a Pfizer-BioNTech COVID-19 Vaccine 2-dose series (N=151) at least 12 weeks (range 12 to 20 weeks) prior to enrollment and who reported no history of SARS-CoV-2 infection were randomized 1:1:1 to receive a booster dose of one of three vaccines: Moderna COVID-19 Vaccine, Janssen COVID-19 Vaccine, or Pfizer-BioNTech COVID-19 Vaccine. Adverse events were assessed through 28 days after the booster dose. An overall review of adverse reactions reported following the Moderna COVID-19 Vaccine heterologous booster dose did not identify any new safety concerns, as compared with adverse reactions reported following Moderna COVID-19 Vaccine primary series doses or homologous booster dose.
Second Booster Dose
In an independently conducted study (Gili Regev‑Yochay, Tal Gonen, Mayan Gilboa, et al. 2022 DOI: 10.1056/NEJMc2202542), the Moderna COVID-19 Vaccine was administered as a second booster dose to 120 participants 18 years of age and older who had received a 2-dose primary series and a first booster dose of Pfizer-BioNTech COVID-19 Vaccine at least 4 months prior. No new safety concerns were reported during up to three weeks of follow-up after the second booster dose.
6.2 Post-Authorization Experience
The following adverse reactions have been identified during post-authorization use of the Moderna COVID-19 Vaccine. Because these reactions are reported voluntarily, it is not always possible to reliably estimate their frequency or establish a causal relationship to vaccine exposure.
Cardiac Disorders: myocarditis, pericarditis
Immune System Disorders: anaphylaxis
Nervous System Disorders: syncope
8 REQUIREMENTS AND INSTRUCTIONS FOR REPORTING ADVERSE EVENTS AND VACCINE ADMINISTRATION ERRORS13
See Overall Safety Summary (Section 6) for additional information.
The vaccination provider enrolled in the federal COVID-19 Vaccination Program is responsible for the MANDATORY reporting of the listed events following Moderna COVID-19 Vaccine to the Vaccine Adverse Event Reporting System (VAERS)
- Vaccine administration errors whether or not associated with an adverse event
- Serious adverse events* (irrespective of attribution to vaccination)
- Cases of Multisystem Inflammatory Syndrome (MIS) in adults and children
- Cases of COVID-19 that results in hospitalization or death
*Serious Adverse Events are defined as:
- Death;
- A life-threatening adverse event;
- Inpatient hospitalization or prolongation of existing hospitalization;
- A persistent or significant incapacity or substantial disruption of the ability to conduct normal life functions;
- A congenital anomaly/birth defect;
- An important medical event that based on appropriate medical judgement may jeopardize the individual and may require medical or surgical intervention to prevent one of the outcomes listed above.
Instructions for Reporting to VAERS
The vaccination provider enrolled in the federal COVID-19 Vaccination Program should complete and submit a VAERS form to FDA using one of the following methods:
- Complete and submit the report online: https://vaers.hhs.gov/reportevent.html, or
- If you are unable to submit this form electronically, you may fax it to VAERS at 1-877-721-0366. If you need additional help submitting a report, you may call the VAERS toll-free information line at 1-800-822-7967 or send an email to info@vaers.org.
IMPORTANT: When reporting adverse events or vaccine administration errors to VAERS, please complete the entire form with detailed information. It is important that the information reported to FDA be as detailed and complete as possible. Information to include:
- Patient demographics (e.g., patient name, date of birth)
- Pertinent medical history
- Pertinent details regarding admission and course of illness
- Concomitant medications
- Timing of adverse event(s) in relationship to administration of Moderna COVID-19 Vaccine
- Pertinent laboratory and virology information
- Outcome of the event and any additional follow-up information if it is available at the time of the VAERS report. Subsequent reporting of follow-up information should be completed if additional details become available.
The following steps are highlighted to provide the necessary information for safety tracking:
- 1. In Box 17, provide information on Moderna COVID-19 Vaccine and any other vaccines administered on the same day; and in Box 22, provide information on any other vaccines received within one month prior.
- 2. In Box 18, description of the event:
- a. Write “Moderna COVID-19 Vaccine EUA” as the first line
- b. Provide a detailed report of vaccine administration error and/or adverse event. It is important to provide detailed information regarding the patient and adverse event/medication error for ongoing safety evaluation of this unapproved vaccine. Please see information to include listed above.
- 3. Contact information:
- a. In Box 13, provide the name and contact information of the prescribing healthcare provider or institutional designee who is responsible for the report.
- b. In Box 14, provide the name and contact information of the best doctor/healthcare professional to contact about the adverse event.
- c. In Box 15, provide the address of the facility where vaccine was given (NOT the healthcare provider’s office address).
Other Reporting Instructions
Vaccination providers may report to VAERS other adverse events that are not required to be reported using the contact information above.
To the extent feasible, report adverse events to ModernaTX, Inc. using the contact information below or by providing a copy of the VAERS form to ModernaTX, Inc.
|
|
Fax number |
Telephone number |
|
1-866-599-1342 |
1-866-MODERNA (1-866-663-3762) |
10 DRUG INTERACTIONS
There are no data to assess the concomitant administration of the Moderna COVID-19 Vaccine with other vaccines.
11 USE IN SPECIFIC POPULATIONS
11.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to Moderna COVID-19 Vaccine during pregnancy. Women who are vaccinated with Moderna COVID-19 Vaccine during pregnancy are encouraged to enroll in the registry by calling 1-866-MODERNA (1-866-663-3762).
Risk Summary
All pregnancies have a risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. Available data on Moderna COVID-19 Vaccine administered to pregnant women are insufficient to inform vaccine-associated risks in pregnancy.
In a developmental toxicity study, 0.2 mL of a vaccine formulation containing the same quantity of nucleoside-modified messenger ribonucleic acid (mRNA) (100 mcg) and other ingredients included in a single primary series dose of Moderna COVID-19 Vaccine for individuals 12 years of age and older was administered to female rats by the intramuscular route on four occasions: 28 and 14 days prior to mating, and on gestation days 1 and 13. No vaccine-related adverse effects on female fertility, fetal development, or postnatal development were reported in the study.
11.2 Lactation
Risk Summary
Data are not available to assess the effects of Moderna COVID-19 Vaccine on the breastfed infant or on milk production/excretion.
11.3 Pediatric Use
Moderna COVID-19 Vaccine is not authorized to provide booster doses for individuals younger than 18 years of age.
11.4 Geriatric Use
Clinical studies of Moderna COVID-19 Vaccine included participants 65 years of age and older receiving vaccine or placebo, and their data contribute to the overall assessment of safety and efficacy. In an ongoing Phase 3 clinical study (Study 1) of primary series dosing, 24.8% (n=7,520) of participants were 65 years of age and older and 4.6% (n=1,399) of participants were 75 years of age and older. Vaccine efficacy in participants 65 years of age and older was 86.4% (95% CI 61.4, 95.2) compared to 95.6% (95% CI 90.6, 97.9) in participants 18 to <65 years of age [see Clinical Trial Results and Supporting Data for EUA (18.1)]. Overall, there were no notable differences in the safety profiles observed in participants 65 years of age and older and younger participants [see Overall Safety Summary (6.1)].
In an ongoing Phase 2 clinical study (Study 2) of a single booster dose, 22.2% (n=38) of participants were 65 years of age and older. This study did not include sufficient numbers of participants 65 years of age and older to determine whether they respond differently than younger participants. Some local and systemic adverse reactions were reported in a lower proportion of participants 65 years of age and older compared to participants 18 through 64 years of age [see Overall Safety Summary (6.1)].
13 DESCRIPTION
Moderna COVID-19 Vaccine is provided as a white to off-white suspension for intramuscular injection.
Each 0.5 mL booster dose of Moderna COVID-19 Vaccine supplied in a multiple-dose vial with a dark blue cap and a label with a purple border contains 50 mcg of nucleoside-modified messenger RNA (mRNA) encoding the pre-fusion stabilized Spike glycoprotein (S) of SARS-CoV-2 virus. Each 0.5 mL dose of the Moderna COVID-19 Vaccine supplied in a multiple-dose vial with a dark blue cap and a label with a purple border contains the following ingredients: a total lipid content of 1.01 mg (SM-102, polyethylene glycol [PEG] 2000 dimyristoyl glycerol [DMG], cholesterol, and 1,2-distearoyl-sn-glycero-3-phosphocholine [DSPC]), 0.25 mg tromethamine, 1.2 mg tromethamine hydrochloride, 0.021 mg acetic acid, 0.10 mg sodium acetate trihydrate, and 43.5 mg sucrose.
Moderna COVID-19 Vaccine does not contain a preservative.
The vial stoppers are not made with natural rubber latex.
14 CLINICAL PHARMACOLOGY
14.1 Mechanism of Action
The nucleoside-modified mRNA in the Moderna COVID-19 Vaccine is formulated in lipid particles, which enable delivery of the nucleoside-modified mRNA into host cells to allow expression of the SARS-CoV-2 S antigen. The vaccine elicits an immune response to the S antigen, which protects against COVID-19.
18 CLINICAL TRIAL RESULTS AND SUPPORTING DATA FOR EUA
18.1 Efficacy of Two-Dose Primary Series in Participants 18 Years and Older
Study 1 is an ongoing Phase 3 randomized, placebo-controlled, observer-blind clinical trial to evaluate the efficacy, safety, and immunogenicity of the Moderna COVID-19 Vaccine in participants 18 years of age and older in the United States (NCT04470427). Randomization was stratified by age and health risk: 18 to <65 years of age without comorbidities (not at risk for progression to severe COVID-19), 18 to <65 years of age with comorbidities (at risk for progression to severe COVID-19), and 65 years of age and older with or without comorbidities. Participants who were immunocompromised and those with a known history of SARS-CoV-2 infection were excluded from the study. Participants with no known history of SARS-CoV-2 infection but with positive laboratory results indicative of infection at study entry were included. The study allowed for the inclusion of participants with stable pre-existing medical conditions, defined as disease not requiring significant change in therapy or hospitalization for worsening disease during the 3 months before enrollment, as well as participants with stable human immunodeficiency virus (HIV) infection. A total of 30,420 participants were randomized equally to receive 2 doses of the Moderna COVID-19 Vaccine or saline placebo 1 month apart. Participants will be followed for efficacy and safety until 24 months after the second dose.
The primary efficacy analysis population (referred to as the Per-Protocol Set) included 28,207 participants who received two doses at 0 and 1 month of either Moderna COVID-19 Vaccine (n=14,134) or placebo (n=14,073) and had a negative baseline SARS-CoV-2 status. In the Per-Protocol Set, 47.4% were female, 19.7% were Hispanic or Latino; 79.5% were White, 9.7% were African American, 4.6% were Asian, and 2.1% other races. The median age of participants was 53 years (range 18-95) and 25.3% of participants were 65 years of age and older. Of the study participants in the Per-Protocol Set, 18.5% were at increased risk of severe COVID-19 due to at least one pre-existing medical condition (chronic lung disease, significant cardiac disease, severe obesity, diabetes, liver disease, or HIV infection) regardless of age. Between participants who received Moderna COVID-19 Vaccine and those who received placebo, there were no notable differences in demographics or pre-existing medical conditions.
Efficacy Against COVID-19
COVID-19 was defined based on the following criteria: The participant must have experienced at least two of the following systemic symptoms: fever (≥38ºC / ≥100.4°F), chills, myalgia, headache, sore throat, new olfactory and taste disorder(s); or the participant must have experienced at least one of the following respiratory signs/symptoms: cough, shortness of breath or difficulty breathing, or clinical or radiographical evidence of pneumonia; and the participant must have at least one NP swab, nasal swab, or saliva sample (or respiratory sample, if hospitalized) positive for SARS-CoV-2 by RT-PCR. COVID-19 cases were adjudicated by a Clinical Adjudication Committee.
The median length of follow-up for efficacy for participants in the study was 9 weeks post Dose 2. There were 11 COVID-19 cases in the Moderna COVID-19 Vaccine group and 185 cases in the placebo group, with a vaccine efficacy of 94.1% (95% confidence interval of 89.3% to 96.8%).
|
Moderna COVID-19 Vaccine |
Placebo |
% Vaccine Efficacy (95% CI)† |
||||
|
Participants (N) |
COVID-19 Cases (n) |
Incidence Rate of COVID-19 per 1,000 Person-Years |
Participants (N) |
COVID-19 Cases (n) |
Incidence Rate of COVID-19 per 1,000 Person-Years |
|
|
14,134 |
11 |
3.328 |
14,073 |
185 |
56.510 |
94.1 (89.3, 96.8) |
|
* COVID-19: symptomatic COVID-19 requiring positive RT-PCR result and at least two systemic symptoms or one respiratory symptom. Cases starting 14 days after Dose 2. † VE and 95% CI from the stratified Cox proportional hazard model. |
||||||
The subgroup analyses of vaccine efficacy are presented in Table 3.
|
Age Subgroup (Years) |
Moderna COVID-19 Vaccine |
Placebo |
% Vaccine Efficacy (95% CI)† |
||||
|
Participants (N) |
COVID-19 Cases (n) |
Incidence Rate of COVID-19 per 1,000 Person-Years |
Participants (N) |
COVID-19 Cases (n) |
Incidence Rate of COVID-19 per 1,000 Person-Years |
||
|
18 to <65 |
10,551 |
7 |
2.875 |
10,521 |
156 |
64.625 |
95.6 (90.6, 97.9) |
|
≥65 |
3,583 |
4 |
4.595 |
3,552 |
29 |
33.728 |
86.4 (61.4, 95.2) |
|
* COVID-19: symptomatic COVID-19 requiring positive RT-PCR result and at least two systemic symptoms or one respiratory symptom. Cases starting 14 days after Dose 2. † VE and 95% CI from the stratified Cox proportional hazard model. |
|||||||
Severe COVID-19 was defined based on confirmed COVID-19 as per the primary efficacy endpoint case definition, plus any of the following: Clinical signs indicative of severe systemic illness, respiratory rate ≥30 per minute, heart rate ≥125 beats per minute, SpO2 ≤93% on room air at sea level or PaO2/FIO2 <300 mm Hg; or respiratory failure or ARDS (defined as needing high-flow oxygen, non-invasive or mechanical ventilation, or ECMO), evidence of shock (systolic blood pressure <90 mmHg, diastolic BP <60 mmHg or requiring vasopressors); or significant acute renal, hepatic, or neurologic dysfunction; or admission to an intensive care unit or death.
Among all participants in the Per-Protocol Set analysis, which included COVID-19 cases confirmed by an adjudication committee, no cases of severe COVID-19 were reported in the Moderna COVID-19 Vaccine group compared with 30 cases reported in the placebo group (incidence rate 9.138 per 1,000 person-years). One PCR-positive case of severe COVID-19 in a vaccine recipient was awaiting adjudication at the time of the analysis.
18.2 Immunogenicity of a First Booster Dose Following a Moderna COVID-19 Vaccine Primary Series in Participants 18 Years and Older
Effectiveness of a booster dose of the Moderna COVID-19 Vaccine was based on assessment of neutralizing antibody titers (ID50) against a pseudovirus expressing the SARS-CoV-2 Spike protein from a USA_WA1/2020 isolate carrying the D614G mutation. Immunogenicity analyses compared the ID50 following the booster dose to the ID50 following the primary series.
In an open-label phase of Study 2, participants 18 years of age and older received a single booster dose at least 6 months after completion of the primary series (two doses 1 month apart). The primary immunogenicity analysis population included 149 booster dose participants in Study 2 (including one individual who had only received a single dose of the primary series) and a random subset of 1,055 participants from Study 1 who received two doses 1 month apart of Moderna COVID-19 Vaccine. Study 1 and 2 participants included in the analysis population had no serologic or virologic evidence of SARS-CoV-2 infection prior to the first primary series dose and prior to the booster dose, respectively. Among participants assessed for immunogenicity, 60.4% were female, 6.7% were Hispanic or Latino; 95.3% were White, 3.4% were Black or African American, 0.7% were Asian, and 0.7% were American Indian or Alaskan Native; 9.4% were obese (body mass index ≥30 kg/m2). The median age of Study 2 participants was 56 years of age (range 18-82) and 24.8% of participants were 65 years of age and older. Study 2 participants included in the primary immunogenicity analysis population did not have pre-existing medical conditions that would place them at risk of severe COVID-19. Study 1 participants included in the primary immunogenicity analysis population were a stratified random sample which reflected the overall primary efficacy analysis population with regards to demographics and pre-existing medical conditions with a higher percentage of those ≥65 years of age (33.6%), with risk factors for severe COVID-19 (39.4%), and communities of color (53.5%).
Immunogenicity analyses included an assessment of ID50 geometric mean titer (GMT) ratio and difference in seroresponse rates. The analysis of the GMT ratio of ID50 following the booster dose compared to the primary series met the immunobridging criteria for a booster response. Seroresponse for a participant was defined as achieving a ≥4-fold rise in ID50 from baseline (before the booster dose in Study 2 and before the first dose of the primary series in Study 1). The lower limit of the 2-sided 95% CI for the difference in seroresponse rates between Study 1 and Study 2 was -16.7%, which did not meet the immunobridging criterion for a booster response (lower limit of 2-sided 95% CI for the percentage difference of ≥ -10%). These analyses are summarized in Table 4 and .
|
Study 2 Booster Dose Na=149 GMTb (95% CI) |
Study 1 Primary Series Na=1053 GMTb (95% CI) |
GMT Ratio (Study 2/Study 1) |
Met Success Criteriac |
|
1802 (1548, 2099) |
1027 (968, 1089) |
1.8 (1.5, 2.1) |
Lower limit of 95% CI ≥0.67 Criterion: Yes Point Estimate ≥1.0 Criterion: Yes |
|
* Per-Protocol Immunogenicity Set included all subjects who had both baseline (or Study 2 Day 1 for Study 2) and post-vaccination immunogenicity samples, did not have SARS-CoV-2 infection at baseline (or Study 2 Day 1 for Study 2), did not have a major protocol deviation that impacted immune response, and had post-injection immunogenicity assessment at timepoint of primary interest (Day 29 for Study 2 and Day 57 for Study 1). a Number of subjects with non-missing data at the corresponding timepoint. b Given the lack of randomization in Study 2, the statistical analysis plan pre-specified an analysis of covariance model for estimating the geometric mean titer that adjusts for differences in age groups (<65 years, ≥65 years). c Immunobridging is declared if the lower limit of the 2-sided 95% CI for the GMR is >0.67 and the point estimate of the GLSM ratio is ≥1.0. Note: Antibody values < the lower limit of quantitation (LLOQ) are replaced by 0.5 × LLOQ. Values > the upper limit of quantitation (ULOQ) are replaced by the ULOQ if actual values are not available. GLSM = Geometric least squares mean GMR = Geometric mean ratio |
|||
|
Study 2 Booster Seroresponsea Nb=149 n (%) (95% CI)c |
Study 1 Primary Series Seroresponsea Nb=1050 n (%) (95% CI)c |
Difference in Seroresponse Rate (Study 2-Study 1) % (95% CI)d |
Met Success Criterione |
|
131 (87.9) (81.6, 92.7) |
1033 (98.4) (97.4, 99.1) |
-10.5 (-16.7, -6.1) |
Lower limit of 95% CI ≥-10% Criterion: No |
|
* Per-Protocol Immunogenicity Set included all subjects who had both baseline (or Study 2 Day 1 for Study 2) and post-vaccination immunogenicity samples, did not have SARS-CoV-2 infection at baseline (or Study 2 Day 1 for Study 2), did not have a major protocol deviation that impacted immune response, and had post-injection immunogenicity assessment at timepoint of primary interest (Day 29 for Study 2 and Day 57 for Study 1). a Seroresponse is defined as ≥4-fold rise of pseudovirus neutralizing antibody titers (ID50) from baseline (pre-booster dose in Study 2 and pre-Dose 1 in Study 1), where baseline titers < LLOQ are set to LLOQ for the analysis. b Number of subjects with non-missing data at both baseline and the post-baseline timepoint of interest. c 95% CI is calculated using the Clopper-Pearson method. d 95% CI is calculated using the Miettinen-Nurminen (score) confidence limits. e Immunobridging is declared if the lower limit of the 2-sided 95% CI for the percentage difference is > -10%. |
|||
Study 2 participants who met the ≥4-fold increase in titer post-booster dose (87.9%) had a lower baseline GMT of 109 (range of individual titers 9, 4393), whereas Study 2 participants who did not meet the ≥4-fold increase in titers post-booster had a higher baseline GMT of 492 (range of individual titers 162, 2239).
An additional descriptive analysis evaluated seroresponse rates using baseline neutralizing antibody titers prior to Dose 1 of the primary series. As shown in Table 6 below, the booster dose seroresponse rate, with seroresponse defined as at least a 4-fold rise relative to the pre-Dose 1 titer, was 100%. The difference in seroresponse rates in this post-hoc analysis was 1.6% (95% CI -0.9, 2.6).
|
Study 2 Booster Seroresponsea Nb=148 n (%) (95% CI)d |
Study 1 Primary Series Seroresponsea Nc=1050 n (%) (95% CI)d |
Difference in Seroresponse Rate (After Booster-After Primary Series) % (95% CI)e |
|
148 (100) (97.5, 100) |
1033 (98.4) (97.4, 99.1) |
1.6 (-0.9, 2.6) |
|
* Per-Protocol Immunogenicity Set included all subjects who had non-missing data at baseline (before Dose 1) and 28 days post-booster in Study 2 or 28 days post-Dose 2 in the primary series in Study 1, respectively, did not have SARS-CoV-2 infection at pre-booster in Study 2 or baseline in Study 1, did not have a major protocol deviation that impacted immune response, and had post-injection immunogenicity assessment at timepoint of primary interest. a Seroresponse is defined as ≥4-fold rise of pseudovirus neutralizing antibody titers (ID50) from pre-Dose 1, where baseline titers < LLOQ are set to LLOQ for the analysis. b Number of subjects with non-missing data at baseline (before Dose 1) and 28 days post-booster in Study 2. c Number of subjects with non-missing data at baseline (before Dose 1) and 28 days post-Dose 2 in the primary series in Study 1. d 95% CI is calculated using the Clopper-Pearson method. e 95% CI is calculated using the Miettinen-Nurminen (score) confidence limits. |
||
18.3 Immunogenicity of a First Booster Dose Following Primary Vaccination with Another Authorized or Approved COVID-19 Vaccine
Effectiveness of a Moderna COVID-19 Vaccine booster dose in individuals who completed primary vaccination with another authorized or approved COVID-19 vaccine (heterologous booster dose) is inferred from immunogenicity data supporting effectiveness of a Moderna COVID-19 Vaccine booster dose administered following completion of a Moderna COVID-19 Vaccine primary series and from immunogenicity data from an independent Phase 1/2 open-label clinical trial (NCT04889209) conducted in the United States that evaluated a booster dose of the Moderna COVID-19 Vaccine. The booster dose that study participants received contained twice the amount of mRNA compared to the authorized booster dose of the Moderna COVID-19 Vaccine. In this study, adults who had completed primary vaccination with a Moderna COVID-19 Vaccine 2-dose series (N=151), a Janssen COVID-19 Vaccine single dose (N=156), or a Pfizer-BioNTech COVID-19 Vaccine 2-dose series (N=151) at least 12 weeks (range 12 to 20 weeks) prior to enrollment and who reported no history of SARS-CoV-2 infection were randomized 1:1:1 to receive a booster dose of one of three vaccines: Moderna COVID-19 Vaccine, Janssen COVID-19 Vaccine, or Pfizer-BioNTech COVID-19 Vaccine. Neutralizing antibody titers, as measured by a pseudovirus neutralization assay using a lentivirus expressing the SARS-CoV-2 Spike protein with D614G mutation, were assessed on Day 1 prior to administration of the booster dose and on Day 15 after the booster dose. A booster response to the Moderna COVID-19 Vaccine was demonstrated regardless of the vaccine used for primary vaccination.
18.4 Immunogenicity of a Second Booster Dose
Immunogenicity data from an ongoing, open-label, non-randomized clinical study in healthcare workers at a single center in Israel were provided in a publication (Gili Regev‑Yochay, Tal Gonen, Mayan Gilboa, et al. 2022 DOI: 10.1056/NEJMc2202542). In this study, 120 individuals 18 years of age and older who had received primary vaccination and a first booster dose with Pfizer-BioNTech COVID-19 Vaccine were administered a second booster dose of Moderna COVID-19 Vaccine at least 4 months after the first booster dose. Among these individuals, approximately 7- to 16-fold increases in geometric mean neutralizing antibody titers against wild-type virus and Delta and Omicron variants, were reported at two weeks after the second booster as compared to 5 months after the first booster dose.
19 HOW SUPPLIED/STORAGE AND HANDLING
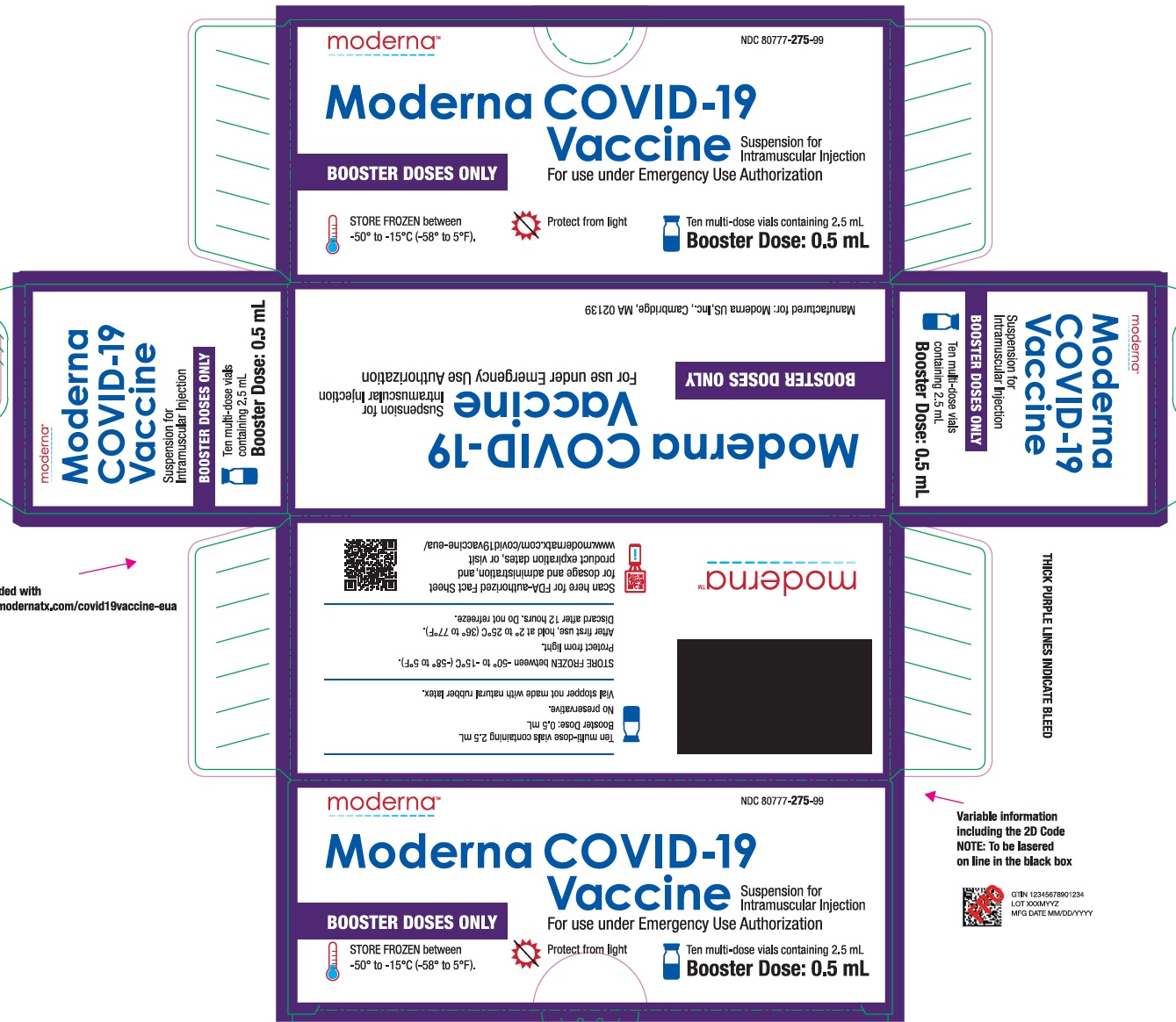
The information in this section applies to the Moderna COVID-19 Vaccine that is supplied in multiple-dose vials with dark blue caps and labels with a purple border. These multiple-dose vials are supplied as follows:
NDC: 80777-275-99 Carton of 10 multiple-dose vials, each containing 2.5 mL
During storage, minimize exposure to room light, and avoid exposure to direct sunlight and ultraviolet light.
Frozen Storage
Store frozen between -50°C to -15°C (-58°F to 5°F).
Storage after Thawing
-
Storage at 2°C to 8°C (36°F to 46°F):
- o Vials may be stored refrigerated between 2°C to 8°C (36°F to 46°F) for up to 30 days prior to first use.
- o Vials should be discarded 12 hours after the first puncture.
-
Storage at 8°C to 25°C (46°F to 77°F):
- o Vials may be stored between 8°C to 25°C (46°F to 77°F) for a total of 24 hours.
- o Vials should be discarded 12 hours after the first puncture.
- o Total storage at 8°C to 25°C (46°F to 77°F) must not exceed 24 hours.
Do not refreeze once thawed.
Thawed vials can be handled in room light conditions.
Transportation of Thawed Vials at 2°C to 8°C (36°F to 46°F)
If transport at -50°C to -15°C (-58°F to 5°F) is not feasible, available data support transportation of one or more thawed vials for up to 12 hours at 2°C to 8°C (36°F to 46°F) when shipped using shipping containers which have been qualified to maintain 2°C to 8°C (36°F to 46°F) and under routine road and air transport conditions with shaking and vibration minimized. Once thawed and transported at 2°C to 8°C (36°F to 46°F), vials should not be refrozen and should be stored at 2°C to 8°C (36°F to 46°F) until use.
20 PATIENT COUNSELING INFORMATION
Advise the recipient or caregiver to read the Vaccine Information Fact Sheet for Recipients and Caregivers.
The vaccination provider must include vaccination information in the state/local jurisdiction’s Immunization Information System (IIS) or other designated system. Advise recipient or caregiver that more information about IISs can be found at: https://www.cdc.gov/vaccines/programs/iis/about.html.
21 CONTACT INFORMATION
For general questions, send an email or call the telephone number provided below.
|
|
Telephone number |
|
1-866-MODERNA (1-866-663-3762) |
This EUA Prescribing Information may have been updated. For the most recent Full EUA Prescribing Information, please visit www.modernatx.com/covid19vaccine-eua.
Moderna US, Inc.
Cambridge, MA 02139
©2022 ModernaTX, Inc. All rights reserved.
Patent(s): www.modernatx.com/patents
Revised: June/17/2022
VACCINE INFORMATION FACT SHEET FOR RECIPIENTS AND CAREGIVERS
ABOUT SPIKEVAX (COVID-19 VACCINE, mRNA) AND THE MODERNA COVID-19 VACCINE TO PREVENT CORONAVIRUS DISEASE 2019 (COVID-19) IN INDIVIDUALS 12 YEARS OF AGE AND OLDER
|
FOR 12 YEARS OF AGE AND OLDER |
You are being offered either SPIKEVAX (COVID-19 Vaccine, mRNA) or the Moderna COVID-19 Vaccine to prevent Coronavirus Disease 2019 (COVID-19) caused by SARS-CoV-2.
This Vaccine Information Fact Sheet for Recipients and Caregivers comprises the Fact Sheet for the authorized Moderna COVID-19 Vaccine and also includes information about the FDA-licensed vaccine, SPIKEVAX (COVID-19 Vaccine, mRNA) for use in individuals 12 years of age and older.14
The FDA-approved SPIKEVAX (COVID-19 Vaccine, mRNA) and the Moderna COVID-19 Vaccine authorized for Emergency Use Authorization (EUA) for individuals 12 years of age and older can be used interchangeably, when used according to their respective instructions for use.15
SPIKEVAX (COVID-19 Vaccine, mRNA) is an FDA-approved COVID-19 vaccine made by ModernaTX, Inc. It is approved as a two-dose series for prevention of COVID-19 in individuals 18 years of age and older. It is also authorized under EUA to provide:
- a two-dose primary series to individuals 12 years through 17 years of age;
- a third primary series dose to individuals 12 years of age and older who have been determined to have certain kinds of immunocompromise;
- a first booster dose to individuals 18 years of age and older who have completed a primary series with Moderna COVID-19 Vaccine or SPIKEVAX (COVID-19 Vaccine, mRNA);
- a first booster dose to individuals 18 years of age and older who have completed primary vaccination with another authorized or approved COVID-19 vaccine. The booster schedule is based on the labeling information of the vaccine used for the primary series;
- a second booster dose to individuals 50 years of age and older who have received a first booster dose of any authorized or approved COVID-19 vaccine; and
- a second booster dose to individuals 18 years of age and older with certain kinds of immunocompromiseand who have received a first booster dose of any authorized or approved COVID-19 vaccine.
The Moderna COVID-19 Vaccine has received EUA from FDA to provide:
- a two-dose primary series to individuals 12 years of age and older;
- a third primary series dose to individuals 12 years of age and older with certain kinds of immunocompromise;
- a first booster dose to the individuals 18 years of age and older who have completed a primary series with the Moderna COVID-19 Vaccine or SPIKEVAX (COVID-19 Vaccine, mRNA);
- a first booster dose to individuals 18 years of age and older who have completed primary vaccination with another authorized or approved COVID-19 vaccine. The booster schedule is based on the labeling information of the vaccine used for the primary series;
- a second booster dose to individuals 50 years of age and older who have received a first booster dose of any authorized or approved COVID-19 vaccine; and
- a second booster dose to individuals 18 years of age and older with certain kinds of immunocompromise and who have received a first booster dose of any authorized or approved COVID-19 vaccine.
This Vaccine Information Fact Sheet contains information to help you understand the risks and benefits of SPIKEVAX (COVID-19 Vaccine, mRNA) and the Moderna COVID-19 Vaccine, which you may receive because there is currently a pandemic of COVID-19. Talk to your vaccination provider if you have questions.
The Moderna COVID-19 Vaccine and SPIKEVAX (COVID-19 Vaccine, mRNA) may not protect everyone.
This Fact Sheet may have been updated. For the most recent Fact Sheet, please visit www.modernatx.com/covid19vaccine-eua.
WHAT YOU NEED TO KNOW BEFORE YOU GET THIS VACCINE
WHAT IS COVID-19?
COVID-19 is caused by a coronavirus called SARS-CoV-2. This type of coronavirus has not been seen before. You can get COVID-19 through contact with another person who has the virus. It is predominantly a respiratory illness that can affect other organs. People with COVID-19 have had a wide range of symptoms reported, ranging from mild symptoms to severe illness. Symptoms may appear 2 to 14 days after exposure to the virus. Symptoms may include: fever or chills; cough; shortness of breath; fatigue; muscle or body aches; headache; new loss of taste or smell; sore throat; congestion or runny nose; nausea or vomiting; diarrhea.
HOW IS SPIKEVAX (COVID-19 VACCINE, mRNA) RELATED TO THE MODERNA COVID-19 VACCINE?
SPIKEVAX (COVID-19 Vaccine, mRNA) can be used interchangeably.
For more information on EUA, see the “What is an Emergency Use Authorization (EUA)?” section at the end of this Fact Sheet.
WHAT SHOULD YOU MENTION TO YOUR VACCINATION PROVIDER BEFORE YOU GET THE VACCINE?
Tell your vaccination provider about all of your medical conditions, including if you:
- have any allergies
- have had myocarditis (inflammation of the heart muscle) or pericarditis (inflammation of the lining outside the heart)
- have a fever
- have a bleeding disorder or are on a blood thinner
- are immunocompromised or are on a medicine that affects your immune system
- are pregnant or plan to become pregnant
- are breastfeeding
- have received another COVID-19 vaccine
- have ever fainted in association with an injection
WHO SHOULD NOT GET THE VACCINE?
You should not get the vaccine if you:
- had a severe allergic reaction after a previous dose of this vaccine
- had a severe allergic reaction to any ingredient of this vaccine
WHAT ARE THE INGREDIENTS IN THE VACCINE?
The Moderna COVID-19 Vaccine and SPIKEVAX (COVID-19 Vaccine, mRNA) contain the following ingredients: messenger ribonucleic acid (mRNA), lipids (SM-102, polyethylene glycol [PEG] 2000 dimyristoyl glycerol [DMG], cholesterol, and 1,2-distearoyl-sn-glycero-3-phosphocholine [DSPC]), tromethamine, tromethamine hydrochloride, acetic acid, sodium acetate trihydrate, and sucrose.
HOW IS THE VACCINE GIVEN?
The Moderna COVID-19 Vaccine or SPIKEVAX (COVID-19 Vaccine, mRNA) will be given to you as an injection into the muscle.
Primary Series: The vaccine is administered as a two-dose series, 1 month apart. A third primary series dose may be administered at least 1 month after the second dose to individuals with certain kinds of immunocompromise.
Booster Dose:
- A first booster dose of the vaccine may be administered at least 5 months after completion of a primary series of the Moderna COVID-19 Vaccine or SPIKEVAX (COVID-19 Vaccine, mRNA) in individuals 18 years of age and older.
- A first booster dose of the vaccine may be administered to individuals 18 years of age and older who have completed primary vaccination with another authorized or approved COVID-19 vaccine. Please check with your healthcare provider regarding timing of the booster dose.
- A second booster dose of the Moderna COVID-19 Vaccine may be administered to individuals 50 years of age and older at least 4 months after receipt of a first booster dose of any authorized or approved COVID-19 vaccine.
- A second booster dose of the Moderna COVID-19 Vaccine may be administered, at least 4 months after receipt of a first booster dose of any authorized or approved COVID-19 vaccine to individuals 18 years of age and older with certain kinds of immunocompromise.
HAS THE VACCINE BEEN USED BEFORE?
Yes. In clinical trials, approximately 30,000 individuals 12 years of age and older have received at least 1 dose of the vaccine. Data from these clinical trials supported the Emergency Use Authorization of Moderna COVID-19 Vaccine and the approval of SPIKEVAX (COVID-19 Vaccine, mRNA). Millions of individuals have received the vaccine under EUA since December 18, 2020.
WHAT ARE THE BENEFITS OF THE VACCINE?
The vaccine has been shown to prevent COVID-19. The duration of protection against COVID-19 is currently unknown.
WHAT ARE THE RISKS OF THE VACCINE?
There is a remote chance that the vaccine could cause a severe allergic reaction. A severe allergic reaction would usually occur within a few minutes to one hour after getting a dose of the vaccine. For this reason, your vaccination provider may ask you to stay at the place where you received your vaccine for monitoring after vaccination. Signs of a severe allergic reaction can include:
- Difficulty breathing
- Swelling of your face and throat
- A fast heartbeat
- A bad rash all over your body
- Dizziness and weakness
Myocarditis (inflammation of the heart muscle) and pericarditis (inflammation of the lining outside the heart) have occurred in some people who have received the vaccine, most commonly in adult males under 40 years of age than among females and older males. In most of these people, symptoms began within a few days following receipt of the second dose of the vaccine. The chance of having this occur is very low. You should seek medical attention right away if you have any of the following symptoms after receiving the vaccine:
- Chest pain
- Shortness of breath
- Feelings of having a fast-beating, fluttering, or pounding heart
Side effects that have been reported in clinical trials with the vaccine include:
- Injection site reactions: pain, tenderness and swelling of the lymph nodes in the same arm of the injection, swelling (hardness), and redness
- General side effects: fatigue, headache, muscle pain, joint pain, chills, nausea and vomiting, fever, and rash
Side effects that have been reported during post-authorization use of the vaccine include:
- Severe allergic reactions
- Myocarditis (inflammation of the heart muscle)
- Pericarditis (inflammation of the lining outside the heart)
- Fainting in association with injection of the vaccine
These may not be all the possible side effects of the vaccine. Serious and unexpected side effects may occur. The possible side effects of the vaccine are still being studied in clinical trials.
WHAT SHOULD I DO ABOUT SIDE EFFECTS?
If you experience a severe allergic reaction, call 9-1-1, or go to the nearest hospital.
Call the vaccination provider or your healthcare provider if you have any side effects that bother you or do not go away.
Report vaccine side effects to FDA/CDC Vaccine Adverse Event Reporting System (VAERS). The VAERS toll-free number is 1-800-822-7967 or report online to https://vaers.hhs.gov/reportevent.html. Please include either “SPIKEVAX (COVID-19 Vaccine, mRNA)” or “Moderna COVID-19 Vaccine EUA,” as appropriate, in the first line of box #18 of the report form.
In addition, you can report side effects to ModernaTX, Inc. at 1-866-MODERNA (1-866-663-3762).
You may also be given an option to enroll in v-safe. V-safe is a voluntary smartphone-based tool that uses text messaging and web surveys to check in with people who have been vaccinated to identify potential side effects after COVID-19 vaccination. V-safe asks questions that help CDC monitor the safety of COVID-19 vaccines. V-safe also provides second-dose reminders if needed and live telephone follow-up by CDC if participants report a significant health impact following COVID-19 vaccination. For more information on how to sign up, visit: www.cdc.gov/vsafe.
WHAT IF I DECIDE NOT TO GET SPIKEVAX (COVID-19 VACCINE, mRNA) OR THE MODERNA COVID-19 VACCINE?
Under the EUA, it is your choice to receive or not receive the vaccine. Should you decide not to receive it, it will not change your standard medical care.
ARE OTHER CHOICES AVAILABLE FOR PREVENTING COVID-19 BESIDES SPIKEVAX (COVID-19 VACCINE, mRNA) OR THE MODERNA COVID-19 VACCINE?
Another choice for preventing COVID-19 is COMIRNATY (COVID-19 Vaccine, mRNA), an FDA-approved COVID-19 vaccine. Other vaccines to prevent COVID-19 may be available under EUA.
CAN I RECEIVE SPIKEVAX (COVID-19 VACCINE, mRNA) OR THE MODERNA COVID-19 VACCINE AT THE SAME TIME AS OTHER VACCINES?
Data have not yet been submitted to FDA on administration of SPIKEVAX (COVID-19 Vaccine, mRNA) or the Moderna COVID-19 Vaccine at the same time as other vaccines. If you are considering receiving SPIKEVAX (COVID-19 Vaccine, mRNA) or the Moderna COVID-19 Vaccine with other vaccines, discuss your options with your healthcare provider.
WHAT IF I AM IMMUNOCOMPROMISED?
If you are immunocompromised, you may receive a third primary series dose of the vaccine. The third dose may still not provide full immunity to COVID-19 in people who are immunocompromised, and you should continue to maintain physical precautions to help prevent COVID-19. In addition, after you received a first booster dose, you may receive a second booster dose of the vaccine if you are 18 years of age and older. Your close contacts should be vaccinated as appropriate.
WHAT IF I AM PREGNANT OR BREASTFEEDING?
If you are pregnant or breastfeeding, discuss your options with your healthcare provider.
WILL THE VACCINE GIVE ME COVID-19?
No. The vaccine does not contain SARS-CoV-2 and cannot give you COVID-19.
KEEP YOUR VACCINATION CARD
When you receive your first dose, you will get a vaccination card to show you when to return for your next dose(s) of the vaccine. Remember to bring your card when you return.
ADDITIONAL INFORMATION
If you have questions, visit the website or call the telephone number provided below.
To access the most recent Fact Sheets, please scan the QR code provided below.
|
Moderna COVID-19 Vaccine website |
Telephone number |
|
www.modernatx.com/covid19vaccine-eua 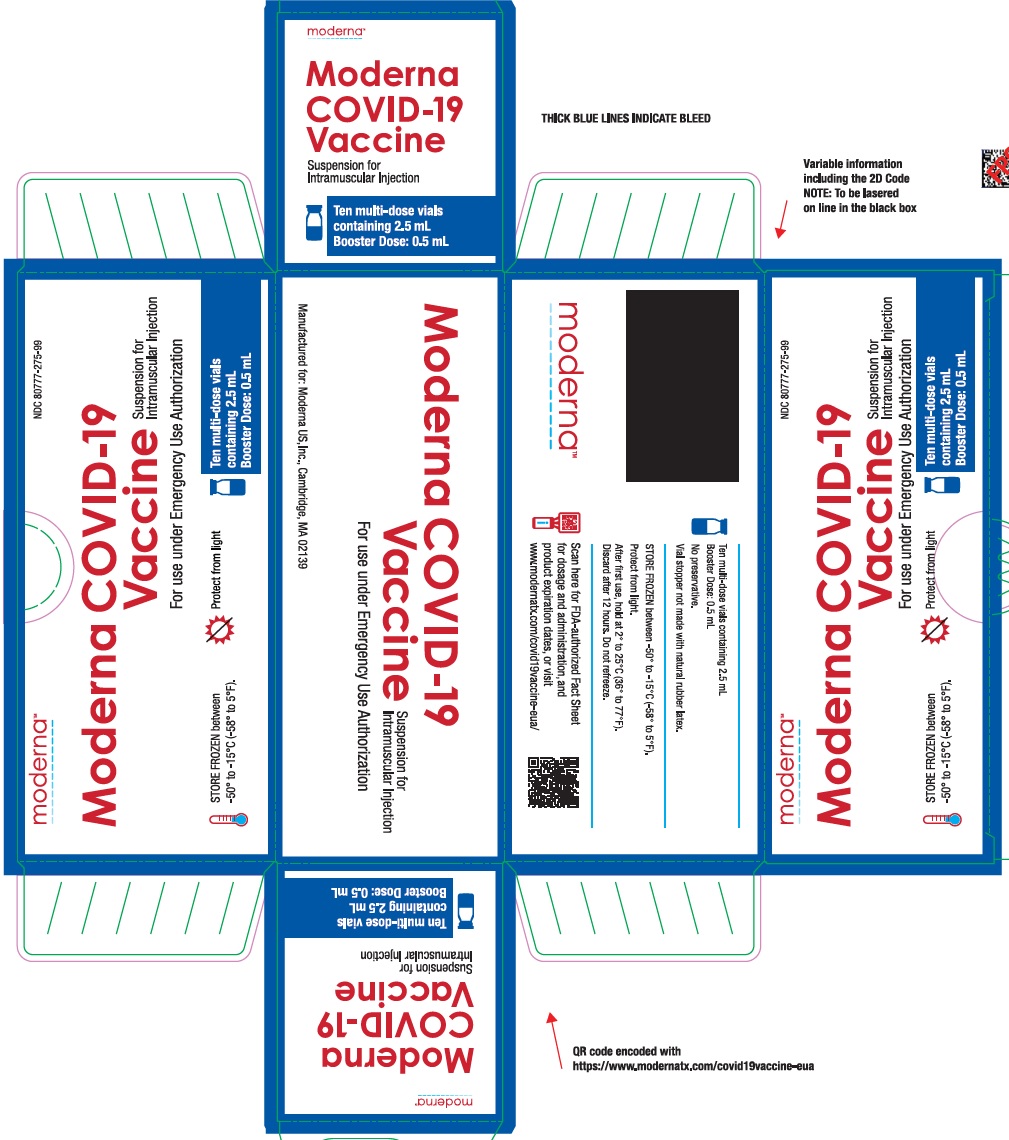 |
1-866-MODERNA (1-866-663-3762) |
HOW CAN I LEARN MORE?
- Ask the vaccination provider
- Visit CDC at https://www.cdc.gov/coronavirus/2019-ncov/index.html
- Visit FDA at https://www.fda.gov/emergency-preparedness-and-response/mcm-legal- regulatory-and-policy-framework/emergency-use-authorization
- Contact your state or local public health department
WHERE WILL MY VACCINATION INFORMATION BE RECORDED?
The vaccination provider may include your vaccination information in your state/local jurisdiction’s Immunization Information System (IIS) or other designated system. This will ensure that you receive the same vaccine when you return for the second dose. For more information about IISs, visit: https://www.cdc.gov/vaccines/programs/iis/about.html.
CAN I BE CHARGED AN ADMINISTRATION FEE FOR RECEIPT OF THE COVID-19 VACCINE?
No. At this time, the provider cannot charge you for a vaccine dose and you cannot be charged an out-of-pocket vaccine administration fee or any other fee if only receiving a COVID-19 vaccination. However, vaccination providers may seek appropriate reimbursement from a program or plan that covers COVID-19 vaccine administration fees for the vaccine recipient (private insurance, Medicare, Medicaid, HRSA COVID-19 Uninsured Program for non-insured recipients).
WHERE CAN I REPORT CASES OF SUSPECTED FRAUD?
Individuals becoming aware of any potential violations of the CDC COVID-19 Vaccination Program requirements are encouraged to report them to the Office of the Inspector General, U.S. Department of Health and Human Services, at 1-800-HHS-TIPS or TIPS.HHS.GOV.
WHAT IS THE COUNTERMEASURES INJURY COMPENSATION PROGRAM?
The Countermeasures Injury Compensation Program (CICP) is a federal program that may help pay for costs of medical care and other specific expenses of certain people who have been seriously injured by certain medicines or vaccines, including this vaccine. Generally, a claim must be submitted to the CICP within one (1) year from the date of receiving the vaccine. To learn more about this program, visit www.hrsa.gov/cicp/ or call 1-855-266-2427.
WHAT IS AN EMERGENCY USE AUTHORIZATION (EUA)?
An EUA is a mechanism to facilitate the availability and use of medical products, including vaccines, during public health emergencies, such as the current COVID-19 pandemic. An EUA is supported by a Secretary of Health and Human Services (HHS) declaration that circumstances exist to justify the emergency use of drugs and biological products during the COVID-19 pandemic. A product authorized for emergency use has not undergone the same type of review by FDA as an FDA approved product.
FDA may issue an EUA when certain criteria are met, which includes that there are no adequate, approved, and available alternatives. In addition, the FDA decision is based on the totality of the scientific evidence available showing that the product may be effective to prevent COVID-19 during the COVID-19 pandemic and that the known and potential benefits of the product outweigh the known and potential risks of the product. All of these criteria must be met to allow for the product to be used during the COVID-19 pandemic.
An EUA is in effect for the duration of the COVID-19 EUA declaration justifying emergency use of this product, unless terminated or revoked (after which the product may no longer be used).
Moderna US, Inc.
Cambridge, MA 02139
©2022 ModernaTX, Inc. All rights reserved.
Patent(s): www.modernatx.com/patents
Revised: June/17/2022
Package/Label Display Panel
NDC: 80777-275-05
Moderna COVID-19 Vaccine
Suspension for Intramuscular Injection
For use under Emergency Use Authorization
BOOSTER DOSES ONLY
2.5 mL Multi-Dose Vial
Booster Dose: 0.5 mL
Package/Label Display Panel
NDC: 80777-275-99
Moderna COVID-19 Vaccine
Suspension for Intramuscular Injection
For use under Emergency Use Authorization
BOOSTER DOSES ONLY
STORE FROZEN between -50° to -15°C (-58° to 5°F).
Protect from light
Ten multi-dose vials containing 2.5 mL
Booster Dose: 0.5 mL
| MODERNA COVID-19 VACCINE
cx-024414 injection, suspension |
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
| Labeler - Moderna US, Inc. (117626450) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| ModernaTX, Inc. | 116912313 | ANALYSIS(80777-275) , API MANUFACTURE(80777-275) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Catalent Indiana, LLC | 172209277 | MANUFACTURE(80777-275) , ANALYSIS(80777-275) , LABEL(80777-275) , PACK(80777-275) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Patheon Manufacturing Services, LLC | 079415560 | MANUFACTURE(80777-275) , ANALYSIS(80777-275) , LABEL(80777-275) , PACK(80777-275) | |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.