CLINDAMYCIN IN 5 PERCENT DEXTROSE injection, solution
Clindamycin in 5 Percent Dextrose by
Drug Labeling and Warnings
Clindamycin in 5 Percent Dextrose by is a Prescription medication manufactured, distributed, or labeled by Sandoz Inc. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
SPL UNCLASSIFIED SECTION
Rx Only
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Clindamycin in 5% Dextrose Injection and other antibacterial drugs, Clindamycin in 5% Dextrose Injection should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria.
Clindamycin in 5% Dextrose Injection in the Cryovac Plastic Container is a Sterile Solution for Intravenous Use Only
WARNING
Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including Clindamycin in 5% Dextrose Injection and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
Because Clindamycin in 5% Dextrose Injection therapy has been associated with severe colitis which may end fatally, it should be reserved for serious infections where less toxic antimicrobial agents are inappropriate, as described in the INDICATIONS AND USAGE section. It should not be used in patients with nonbacterial infections such as most upper respiratory tract infections. C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
-
DESCRIPTION
Clindamycin in 5% Dextrose Injection in the Cryovac plastic container for intravenous use is composed of clindamycin phosphate equivalent to 300, 600 and 900 mg of clindamycin premixed with 5% dextrose as a sterile solution. Disodium edetate has been added at a concentration of 0.04 mg/mL. The pH has been adjusted with sodium hydroxide and/or hydrochloric acid. Clindamycin is a semisynthetic antibiotic produced by a 7(S)-chloro-substitution of the 7(R)-hydroxyl group of the parent compound lincomycin.
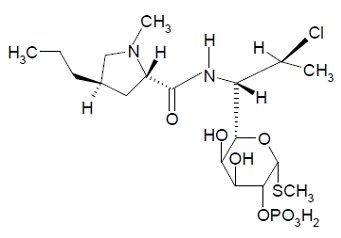
The chemical name of clindamycin phosphate is L-threo-α-D-galacto- Octopyranoside, methyl-7-chloro-6,7,8-trideoxy-6-[[(1-methyl-4-propyl-2-pyrrolidinyl) carbonyl] amino]-1-thio-, 2-(dihydrogen phosphate), (2S-trans)-.
The molecular formula is C18H34CIN208PS and the molecular weight is 504.97.
The structural formula is represented below:
The plastic container is fabricated from a specially designed multilayer plastic, M312A material. Solutions in contact with the plastic container can leach out certain of its chemical components in very small amounts within the expiration period. The suitability of the plastic has been confirmed in tests in animals according to the USP biological tests for plastic containers, as well as by tissue culture toxicity studies.
-
CLINICAL PHARMACOLOGY
Distribution
Biologically inactive clindamycin phosphate is converted to active clindamycin. By the end of short-term intravenous infusion, peak serum concentrations of active clindamycin are reached.
After intramuscular injection of clindamycin phosphate, peak concentrations of active clindamycin are reached within 3 hours in adults and 1 hour in pediatric patients. Serum concentration-time curves may be constructed from IV peak serum concentrations as given in Table 1 by application of elimination half-lives (see Excretion).
Serum concentrations of clindamycin can be maintained above the in vitro minimum inhibitory concentrations for most indicated organisms by administration of clindamycin phosphate every 8 to 12 hours in adults and every 6 to 8 hours in pediatric patients, or by continuous intravenous infusion. An equilibrium state is reached by the third dose.
No significant concentrations of clindamycin are attained in the cerebrospinal fluid even in the presence of inflamed meninges.
Metabolism
In vitro studies in human liver and intestinal microsomes indicated that clindamycin is predominantly metabolized by Cytochrome P450 3A4 (CYP3A4), with minor contribution from CYP3A5, to form clindamycin sulfoxide and a minor metabolite, N-desmethylclindamycin.
Excretion
Biologically inactive clindamycin phosphate disappears from the serum with 6 minutes of the average elimination half-life; however, the average serum elimination half-life of active clindamycin is about 3 hours in adults and 2½ hours in pediatric patients.
Specific Populations
Patients with Renal/Hepatic Impairment
The elimination half-life of clindamycin is increased slightly in patients with markedly reduced renal or hepatic function. Hemodialysis and peritoneal dialysis are not effective in removing clindamycin from the serum. Dosage schedules need not be modified in the presence of mild or moderate renal or hepatic disease.
Elderly Patients
Pharmacokinetic studies in elderly volunteers (61 to 79 years) and younger adults (18 to 39 years) indicate that age alone does not alter clindamycin pharmacokinetics (clearance, elimination half-life, volume of distribution, and area under the serum concentration-time curve) after IV administration of clindamycin phosphate. After oral administration of clindamycin hydrochloride, the average elimination half-life is increased to approximately 4 hours (range 3.4 to 5.1 h) in the elderly, compared to 3.2 hours (range 2.1 to 4.2 h) in younger adults. The extent of absorption, however, is not different between age groups and no dosage alteration is necessary for the elderly with normal hepatic function and normal (age-adjusted) renal function1.
Table 1. Average Peak and Trough Serum Concentrations of Active Clindamycin After Dosing with Clindamycin Phosphate Dosage Regimen Peak
mcg/mLTrough
mcg/mL- * Data in this group from patients being treated for infection.
Healthy Adult Males (Post equilibrium)
600 mg IV in 30 min q6h
10.9
2
600 mg IV in 30 min q8h
10.8
1.1
900 mg IV in 30 min q8h
14.1
1.7
Pediatric Patients (first dose)*
5 to 7 mg/kg IV in 1 hour
10
Microbiology
Mechanism of Action
Clindamycin inhibits bacterial protein synthesis by binding to the 23S RNA of the 50S subunit of the ribosome. Clindamycin is bacteriostatic.
Resistance
Resistance to clindamycin is most often caused by modification of specific bases of the 23S ribosomal RNA. Cross-resistance between clindamycin and lincomycin is complete. Because the binding sites for these antibacterial drugs overlap, cross-resistance is sometimes observed among lincosamides, macrolides and streptogramin B. Macrolide-inducible resistance to clindamycin occurs in some isolates of macrolide-resistant bacteria. Macrolide-resistant isolates of staphylococci and beta-hemolytic streptococci should be screened for induction of clindamycin resistance using the D-zone test.
Antimicrobial Activity
Clindamycin has been shown to be active against most of the isolates of the following microorganisms, both in vitro and in clinical infections [see INDICATIONS AND USAGE]:
Gram-positive Bacteria
- Staphylococcus aureus (methicillin-susceptible strains)
- Streptococcus pneumoniae (penicillin-susceptible strains)
- Streptococcus pyogenes
Anaerobic Bacteria
- Clostridium perfringens
- Fusobacterium necrophorum
- Fusobacterium nucleatum
- Peptostreptococcus anaerobius
- Prevotella melaninogenica
The following in vitro data are available, but their clinical significance is unknown. At least 90 percent of the following bacteria exhibit an in vitro minimum inhibitory concentration (MIC) less than or equal to the susceptible breakpoint for clindamycin against isolates of a similar genus or organism group. However, the efficacy of clindamycin in treating clinical infections due to these bacteria has not been established in adequate and well-controlled clinical trials.
Gram-positive Bacteria
- Staphylococcus epidermidis (methicillin-susceptible strains)
- Streptococcus agalactiae
- Streptococcus anginosus
- Streptococcus mitis
- Streptococcus oralis
Anaerobic Bacteria
- Actinomyces israelii
- Clostridium clostridioforme
- Eggerthella lenta
- Finegoldia (Peptostreptococcus) magna
- Micromonas (Peptostreptococcus) micros
- Prevotella bivia
- Prevotella intermedia
- Propionibacterium acnes
-
INDICATIONS AND USAGE
Clindamycin in 5% Dextrose Injection is indicated in the treatment of serious infections caused by susceptible anaerobic bacteria.
Clindamycin in 5% Dextrose Injection is also indicated in the treatment of serious infections due to susceptible strains of streptococci, pneumococci, and staphylococci. Its use should be reserved for penicillin-allergic patients or other patients for whom, in the judgment of the physician, a penicillin is inappropriate. Because of the risk of antibiotic-associated pseudomembranous colitis, as described in the BOXED WARNING, before selecting clindamycin the physician should consider the nature of the infection and the suitability of less toxic alternatives (e.g., erythromycin).
Bacteriologic studies should be performed to determine the causative organisms and their susceptibility to clindamycin.
Indicated surgical procedures should be performed in conjunction with antibiotic therapy.
Clindamycin in 5% Dextrose Injection is indicated in the treatment of serious infections caused by susceptible strains of the designated organisms in the conditions listed below:
Lower respiratory tract infections including pneumonia, empyema, and lung abscess caused by anaerobes, Streptococcus pneumoniae, other streptococci (except E. faecalis), and Staphylococcus aureus.
Skin and skin structure infections caused by Streptococcus pyogenes, Staphylococcus aureus, and anaerobes.
Gynecological infections including endometritis, nongonococcal tubo-ovarian abscess, pelvic cellulitis, and postsurgical vaginal cuff infection caused by susceptible anaerobes.
Intra-abdominal infections including peritonitis and intra-abdominal abscess caused by susceptible anaerobic organisms.
Septicemia caused by Staphylococcus aureus, streptococci (except Enterococcus faecalis), and susceptible anaerobes.
Bone and joint infections including acute hematogenous osteomyelitis caused by Staphylococcus aureus and as adjunctive therapy in the surgical treatment of chronic bone and joint infections due to susceptible organisms.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Clindamycin in 5% Dextrose Injection and other antibacterial drugs, Clindamycin in 5% Dextrose Injection should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
- CONTRAINDICATIONS
-
WARNINGS
See BOXED WARNING.
Clostridium difficile Associated Diarrhea
Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including Clindamycin in 5% Dextrose Injection, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
Anaphylactic and Severe Hypersensitivity Reactions
Anaphylactic shock and anaphylactic reactions have been reported (see ADVERSE REACTIONS).
Severe hypersensitivity reactions, including severe skin reactions such as toxic epidermal necrolysis (TEN), drug reaction with eosinophilia and systemic symptoms (DRESS), and Stevens-Johnson syndrome (SJS), some with fatal outcome, have been reported (see ADVERSE REACTIONS).
In case of such an anaphylactic or severe hypersensitivity reaction, discontinue treatment permanently and institute appropriate therapy.
A careful inquiry should be made concerning previous sensitivities to drugs and other allergens.
-
PRECAUTIONS
General
Review of experience to date suggests that a subgroup of older patients with associated severe illness may tolerate diarrhea less well. When clindamycin is indicated in these patients, they should be carefully monitored for change in bowel frequency.
Clindamycin in 5% Dextrose Injection should be prescribed with caution in individuals with a history of gastrointestinal disease, particularly colitis.
Clindamycin in 5% Dextrose Injection should be prescribed with caution in atopic individuals.
Certain infections may require incision and drainage or other indicated surgical procedures in addition to antibiotic therapy.
The use of Clindamycin in 5% Dextrose Injection may result in overgrowth of nonsusceptible organisms- particularly yeasts. Should superinfections occur, appropriate measures should be taken as indicated by the clinical situation.
Clindamycin in 5% Dextrose Injection should not be injected intravenously undiluted as a bolus, but should be infused over at least 10 to 60 minutes as directed in the DOSAGE AND ADMINISTRATION section.
Clindamycin dosage modification may not be necessary in patients with renal disease. In patients with moderate to severe liver disease, prolongation of clindamycin half-life has been found. However, it was postulated from studies that when given every eight hours, accumulation should rarely occur. Therefore, dosage modification in patients with liver disease may not be necessary. However, periodic liver enzyme determinations should be made when treating patients with severe liver disease.
Prescribing Clindamycin in 5% Dextrose Injection in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Information for Patients
Patients should be counseled that antibacterial drugs including Clindamycin in 5% Dextrose Injection should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When Clindamycin in 5% Dextrose Injection is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by Clindamycin in 5% Dextrose Injection or other antibacterial drugs in the future.
Diarrhea is a common problem caused by antibiotics which usually ends when the antibiotic is discontinued. Sometimes after starting treatment with antibiotics, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibiotic. If this occurs, patients should contact their physician as soon as possible.
Laboratory Tests
During prolonged therapy periodic liver and kidney function tests and blood counts should be performed.
Drug Interactions
Clindamycin has been shown to have neuromuscular blocking properties that may enhance the action of other neuromuscular blocking agents. Therefore, it should be used with caution in patients receiving such agents.
Clindamycin is metabolized predominantly by CYP3A4, and to a lesser extent by CYP3A5, to the major metabolite clindamycin sulfoxide and minor metabolite N-desmethylclindamycin. Therefore, inhibitors of CYP3A4 and CYP3A5 may increase plasma concentrations of clindamycin and inducers of these isoenzymes may reduce plasma concentrations of clindamycin. In the presence of strong CYP3A4 inhibitors, monitor for adverse reactions. In the presence of strong CYP3A4 inducers such as rifampicin, monitor for loss of effectiveness.
In vitro studies indicate that clindamycin does not inhibit CYP1A2, CYP2C9, CYP2C19, CYP2E1 or CYP2D6 and only moderately inhibits CYP3A4.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Long term studies in animals have not been performed with clindamycin to evaluate carcinogenic potential. Genotoxicity tests performed included a rat micronucleus test and an Ames Salmonella reversion test. Both tests were negative.
Fertility studies in rats treated orally with up to 300 mg/kg/day (approximately 1.1 times the highest recommended adult human dose based on mg/m2) revealed no effects on fertility or mating ability.
Pregnancy
Teratogenic Effects
In clinical trials with pregnant women, the systemic administration of clindamycin during the second and third trimesters, has not been associated with an increased frequency of congenital abnormalities.
Clindamycin should be used during the first trimester of pregnancy only if clearly needed. There are no adequate and well-controlled studies in pregnant women during the first trimester of pregnancy. Because animal reproduction studies are not always predictive of the human response, this drug should be used during pregnancy only if clearly needed.
Reproduction studies performed in rats and mice using oral doses of clindamycin up to 600 mg/kg/day (2.1 and 1.1 times the highest recommended adult human dose based on mg/m2, respectively) or subcutaneous doses of clindamycin up to 250 mg/kg/day (0.9 and 0.5 times the highest recommended adult human dose based on mg/m2, respectively) revealed no evidence of teratogenicity.
Nursing Mothers
Limited published data based on breast milk sampling reports that clindamycin appears in human breast milk in the range of less than 0.5 to 3.8 mcg/mL at dosages of 150 mg orally to 600 mg intravenously. Clindamycin has the potential to cause adverse effects on the breast-fed infant's gastrointestinal flora. If oral or intravenous clindamycin is required by a nursing mother, it is not a reason to discontinue breastfeeding, but an alternate drug may be preferred. Monitor the breast-fed infant for possible adverse effects on the gastrointestinal flora, such as diarrhea, candidiasis (thrush, diaper rash) or rarely, blood in the stool indicating possible antibiotic-associated colitis.
The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for clindamycin and any potential adverse effects on the breast-fed child from clindamycin or from the underlying maternal condition.
Pediatric Use
When Clindamycin in 5% Dextrose Injection sterile solution is administered to the pediatric population (birth to 16 years) appropriate monitoring of organ system functions is desirable.
Usage in Newborns and Infants
The potential for the toxic effect in the pediatric population from chemicals that may leach from the single dose premixed IV preparation in plastic has not been evaluated. See WARNINGS.
Geriatric Use
Clinical studies of clindamycin did not include sufficient numbers of patients age 65 and over to determine whether they respond differently from younger patients. However, other reported clinical experience indicates that antibiotic-associated colitis and diarrhea (due to Clostridium difficile) seen in association with most antibiotics occur more frequently in the elderly (>60 years) and may be more severe. These patients should be carefully monitored for the development of diarrhea.
Pharmacokinetic studies with clindamycin have shown no clinically important differences between young and elderly subjects with normal hepatic function and normal (age-adjusted) renal function after oral or intravenous administration.
-
ADVERSE REACTIONS
The following reactions have been reported with the use of clindamycin.
Gastrointestinal
Antibiotic-associated colitis (see WARNINGS), pseudomembranous colitis, abdominal pain, nausea, and vomiting. The onset of pseudomembranous colitis symptoms may occur during or after antibacterial treatment (see WARNINGS). An unpleasant or metallic taste has been reported after intravenous administration of the higher doses of clindamycin phosphate.
Hypersensitivity Reactions
Maculopapular rash and urticaria have been observed during drug therapy. Generalized mild to moderate morbilliform-like skin rashes are the most frequently reported of all adverse reactions.
Severe skin reactions such as Toxic Epidermal Necrolysis, some with fatal outcome, have been reported (see WARNINGS). Cases of Acute Generalized Exanthematous Pustulosis (AGEP), erythema multiforme, some resembling Stevens-Johnson syndrome, have been associated with clindamycin. Anaphylactic shock, anaphylactic reaction and hypersensitivity have also been reported (see WARNINGS).
Skin and Mucous Membranes
Pruritus, vaginitis, angioedema, and rare instances of exfoliative dermatitis have been reported (see Hypersensitivity Reactions).
Liver
Jaundice and abnormalities in liver function tests have been observed during clindamycin therapy.
Renal
Although no direct relationship of clindamycin to renal damage has been established, renal dysfunction as evidenced by azotemia, oliguria, and/or proteinuria has been observed.
Hematopoietic
Transient neutropenia (leukopenia) and eosinophilia have been reported. Reports of agranulocytosis and thrombocytopenia have been made. No direct etiologic relationship to concurrent clindamycin therapy could be made in any of the foregoing.
Immune System
Drug reaction with eosinophilia and systemic symptoms (DRESS) cases have been reported.
Local Reactions
Thrombophlebitis has been reported after intravenous infusion. Reactions can be minimized by avoiding prolonged use of indwelling intravenous catheters.
Cardiovascular
Cardiopulmonary arrest and hypotension have been reported following too rapid intravenous administration (see DOSAGE AND ADMINISTRATION).
-
OVERDOSAGE
Significant mortality was observed in mice at an intravenous dose of 855 mg/kg and in rats at an oral or subcutaneous dose of approximately 2,618 mg/kg. In the mice, convulsions and depression were observed.
Hemodialysis and peritoneal dialysis are not effective in removing clindamycin from the serum.
-
DOSAGE AND ADMINISTRATION
If diarrhea occurs during therapy, this antibiotic should be discontinued (see WARNING box).
Adults
Parenteral (IV Administration)
Serious infections due to aerobic gram-positive cocci and the more susceptible anaerobes (NOT generally including Bacteroides fragilis, Peptococcus species and Clostridium species other than Clostridium perfringens):
600 to 1,200 mg/day in 2, 3 or 4 equal doses.
More severe infections, particularly those due to proven or suspected Bacteroides fragilis, Peptococcus species, or Clostridium species other than Clostridium perfringens:
1,200 to 2,700 mg/day in 2, 3 or 4 equal doses.
For more serious infections, these doses may have to be increased. In life-threatening situations due to either aerobes or anaerobes these doses may be increased. Doses of as much as 4,800 mg daily have been given intravenously to adults. See IV Infusion Rates section below.
Alternatively, drug may be administered in the form of a single rapid infusion of the first dose followed by continuous IV infusion as follows:
To Maintain Serum Clindamycin Levels Rapid Infusion Rate Maintenance Infusion Rate Above 4 mcg/mL
10 mg/min for 30 min
0.75 mg/min
Above 5 mcg/mL
15 mg/min for 30 min
1 mg/min
Above 6 mcg/mL
20 mg/min for 30 min
1.25 mg/min
Neonates (less than 1 month)
15 to 20 mg/kg/day in 3 to 4 equal doses. The lower dosage may be adequate for small prematures.
Pediatric patients 1 month of age to 16 years
Parenteral (IV) Administration: 20 to 40 mg/kg/day in 3 or 4 equal doses. The higher doses would be used for more severe infections. As an alternative to dosing on a body weight basis, pediatric patients may be dosed on the basis of square meters body surface: 350 mg/m2/day for serious infections and 450 mg/m2/day for more severe infections.
Parenteral therapy may be changed to oral clindamycin palmitate hydrochloride flavored granules or clindamycin hydrochloride capsules when the condition warrants and at the discretion of the physician.
In cases of β-hemolytic streptococcal infections, treatment should be continued for at least 10 days.
IV Infusion Rates
Infusion rates for Clindamycin in 5% Dextrose Injection should not exceed 30 mg per minute. The usual infusion rates are as follows:
Dose Strength Time 300 mg/50 mL
6 mg/mL
10 min
600 mg/50 mL
12 mg/mL
20 min
900 mg/50 mL
18 mg/mL
30 min
Administration of more than 1,200 mg in a single 1-hour infusion is not recommended.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Compatibility
No incompatibility has been demonstrated with the antibiotics cephalothin, kanamycin, gentamicin, penicillin or carbenicillin.
DIRECTIONS FOR USE
Clindamycin in 5% Dextrose Injection in Cryovac Plastic Container
Premixed Clindamycin in 5% Dextrose Injection is for intravenous administration using sterile equipment. Check for minute leaks prior to use by squeezing bag firmly. If leaks are found, discard solution as sterility may be impaired. Do not add supplementary medication. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit. Do not use unless solution is clear and seal is intact.
Caution
Do not use plastic containers in series connections. Such use could result in air embolism due to residual air being drawn from the primary container before administration of the fluid from the secondary container is complete.
Preparation for Administration
- 1. Suspend container from eyelet support.
- 2. Remove protector from outlet port at bottom of container.
- 3. Attach administration set. Refer to complete directions accompanying set.
-
HOW SUPPLIED
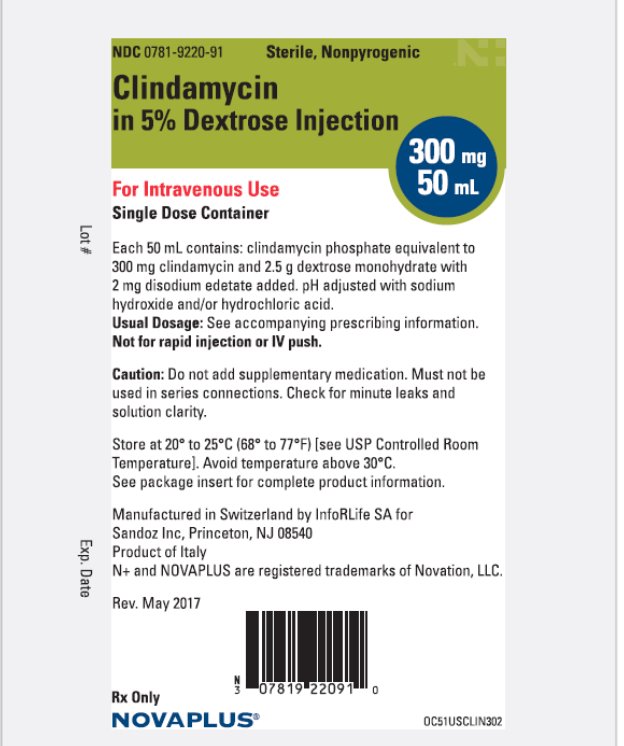
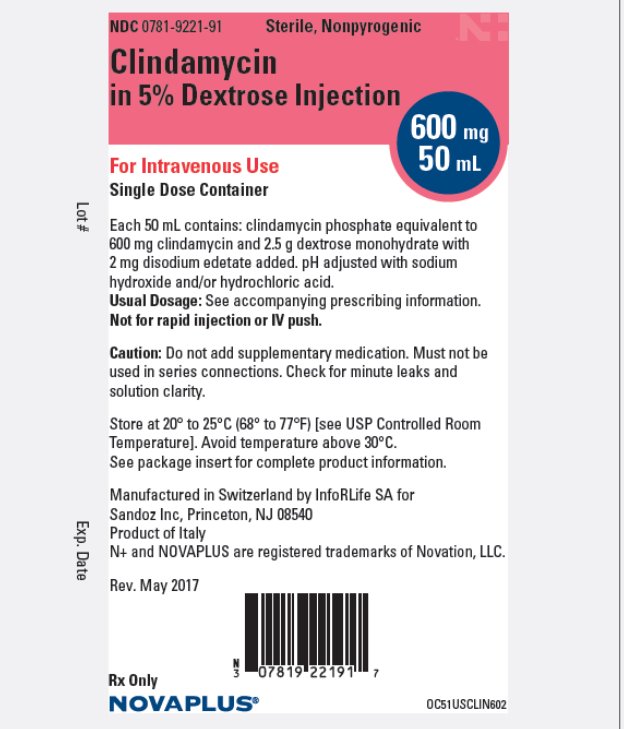
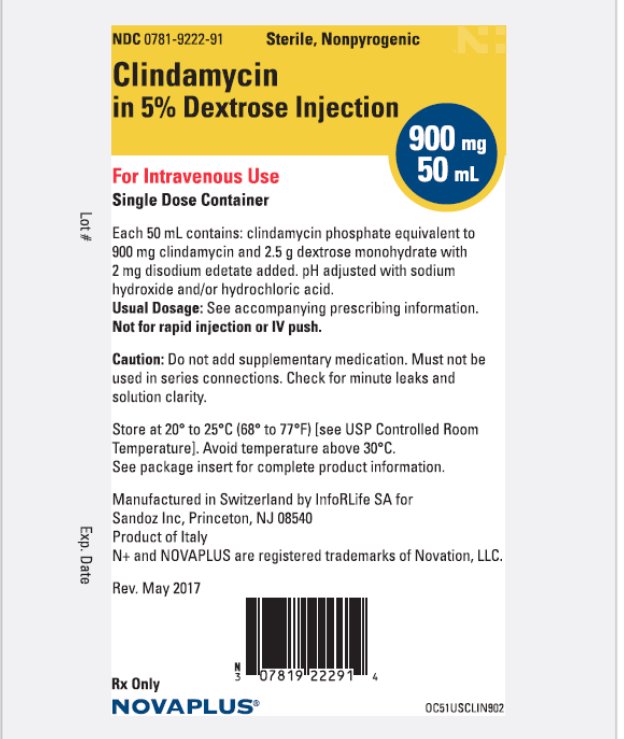
Clindamycin in 5% Dextrose Injection in Cryovac plastic containers is a sterile solution of clindamycin phosphate with 5% dextrose. Each 50 mL contains clindamycin phosphate equivalent to 300 mg, 600 mg or 900 mg clindamycin. The single dose Cryovac plastic containers are available as follows:
300 mg/50 mL, Carton of 24 minibags
NDC: 0781-9220-09
600 mg/50 mL, Carton of 24 minibags
NDC: 0781-9221-09
900 mg/50 mL, Carton of 24 minibags
NDC: 0781-9222-09
Exposure of pharmaceutical products to heat should be minimized. It is recommended that Cryovac plastic containers be stored at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature]. Avoid temperatures above 30° C.
- REFERENCES
- SPL UNCLASSIFIED SECTION
- Package/Label Display Panel
- Package/Label Display Panel
- Package/Label Display Panel
-
INGREDIENTS AND APPEARANCE
CLINDAMYCIN IN 5 PERCENT DEXTROSE
clindamycin in 5 percent dextrose injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0781-9220 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CLINDAMYCIN (UNII: 3U02EL437C) (CLINDAMYCIN - UNII:3U02EL437C) CLINDAMYCIN 6 mg in 1 mL Inactive Ingredients Ingredient Name Strength DEXTROSE MONOHYDRATE (UNII: LX22YL083G) 50 mg in 1 mL EDETATE DISODIUM (UNII: 7FLD91C86K) 0.04 mg in 1 mL HYDROCHLORIC ACID (UNII: QTT17582CB) SODIUM HYDROXIDE (UNII: 55X04QC32I) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0781-9220-09 24 in 1 CARTON 03/01/2014 1 NDC: 0781-9220-91 50 mL in 1 BAG; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA201692 03/01/2014 CLINDAMYCIN IN 5 PERCENT DEXTROSE
clindamycin in 5 percent dextrose injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0781-9221 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CLINDAMYCIN (UNII: 3U02EL437C) (CLINDAMYCIN - UNII:3U02EL437C) CLINDAMYCIN 12 mg in 1 mL Inactive Ingredients Ingredient Name Strength DEXTROSE MONOHYDRATE (UNII: LX22YL083G) 50 mg in 1 mL EDETATE DISODIUM (UNII: 7FLD91C86K) 0.04 mg in 1 mL HYDROCHLORIC ACID (UNII: QTT17582CB) SODIUM HYDROXIDE (UNII: 55X04QC32I) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0781-9221-09 24 in 1 CARTON 03/01/2014 1 NDC: 0781-9221-91 50 mL in 1 BAG; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA201692 03/01/2014 CLINDAMYCIN IN 5 PERCENT DEXTROSE
clindamycin in 5 percent dextrose injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0781-9222 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CLINDAMYCIN (UNII: 3U02EL437C) (CLINDAMYCIN - UNII:3U02EL437C) CLINDAMYCIN 18 mg in 1 mL Inactive Ingredients Ingredient Name Strength DEXTROSE MONOHYDRATE (UNII: LX22YL083G) 50 mg in 1 mL EDETATE DISODIUM (UNII: 7FLD91C86K) 0.04 mg in 1 mL HYDROCHLORIC ACID (UNII: QTT17582CB) SODIUM HYDROXIDE (UNII: 55X04QC32I) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0781-9222-09 24 in 1 CARTON 03/01/2014 1 NDC: 0781-9222-91 50 mL in 1 BAG; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA201692 03/01/2014 Labeler - Sandoz Inc (005387188)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.