TREMFYA- guselkumab injection
TREMFYA by
Drug Labeling and Warnings
TREMFYA by is a Prescription medication manufactured, distributed, or labeled by Janssen Biotech, Inc., AndersonBrecon Inc., Janssen Pharmaceutica, NV, Jannsen Biologics B.V., Cilag AG, Biogen MA, Inc., PPD Development Ireland Ltd., Janssen Sciences Ireland UC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use TREMFYA safely and effectively. See full prescribing information for TREMFYA.
TREMFYA® (guselkumab) injection, for subcutaneous use
Initial U.S. Approval: 2017INDICATIONS AND USAGE
TREMFYA is an interleukin-23 blocker indicated for the treatment of adult patients with moderate-to-severe plaque psoriasis who are candidates for systemic therapy or phototherapy. (1)
DOSAGE AND ADMINISTRATION
100 mg administered by subcutaneous injection at Week 0, Week 4 and every 8 weeks thereafter. (2.1)
DOSAGE FORMS AND STRENGTHS
Injection: 100 mg/mL in a single-dose prefilled syringe or single-dose One-Press patient-controlled injector. (3)
CONTRAINDICATIONS
Serious hypersensitivity reactions to guselkumab or to any of the excipients. (4)
WARNINGS AND PRECAUTIONS
- Infections: TREMFYA may increase the risk of infection. Instruct patients to seek medical advice if signs or symptoms of clinically important chronic or acute infection occur. If a serious infection develops, discontinue TREMFYA until the infection resolves. (5.1)
- Tuberculosis (TB): Evaluate for TB prior to initiating treatment with TREMFYA. (5.2)
- Hypersensitivity Reactions: Serious hypersensitivity reactions may occur. (5.3)
ADVERSE REACTIONS
Most common (≥1%) adverse reactions associated with TREMFYA include upper respiratory infections, headache, injection site reactions, arthralgia, diarrhea, gastroenteritis, tinea infections, and herpes simplex infections. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Janssen Biotech, Inc. at 1-800-JANSSEN (1-800-526-7736) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
Avoid use of live vaccines in patients treated with TREMFYA. (7.1)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 4/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Dosage
2.2 Important Administration Instructions
2.3 Preparation for Use of TREMFYA Prefilled Syringe or One-Press Injector
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Infections
5.2 Pre-treatment Evaluation for Tuberculosis
5.3 Hypersensitivity Reactions
5.4 Immunizations
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Immunogenicity
6.3 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Live Vaccinations
7.2 CYP450 Substrates
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Dosage
TREMFYA is administered by subcutaneous injection. The recommended dose is 100 mg at Week 0, Week 4, and every 8 weeks thereafter.
2.2 Important Administration Instructions
Administer TREMFYA subcutaneously. Each prefilled syringe or One-Press injector is for single-dose only. Instruct patients to inject the full amount (1 mL), which provides 100 mg of TREMFYA.
Do not inject TREMFYA into areas where the skin is tender, bruised, red, hard, thick, scaly, or affected by psoriasis [see Instructions for Use].
TREMFYA is intended for use under the guidance and supervision of a physician. TREMFYA may be administered by a health care professional, or a patient may self-inject after proper training in subcutaneous injection technique.
The TREMFYA Instructions for Use contains more detailed patient instructions on the preparation and administration of TREMFYA [see Instructions for Use].
2.3 Preparation for Use of TREMFYA Prefilled Syringe or One-Press Injector
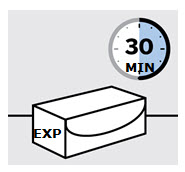
Before injection, remove TREMFYA prefilled syringe or One-Press injector from the refrigerator and allow TREMFYA to reach room temperature (30 minutes) without removing the needle cap.
Inspect TREMFYA visually for particulate matter and discoloration prior to administration. TREMFYA is a clear and colorless to light yellow solution that may contain small translucent particles. Do not use if the liquid contains large particles, is discolored or cloudy. TREMFYA does not contain preservatives; therefore, discard any unused product remaining in the prefilled syringe or One-Press injector.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
TREMFYA is contraindicated in patients with a history of serious hypersensitivity reaction to guselkumab or to any of the excipients [see Warnings and Precautions (5.3)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Infections
TREMFYA may increase the risk of infection. In clinical trials, infections occurred in 23% of subjects in the TREMFYA group versus 21% of subjects in the placebo group through 16 weeks of treatment. Upper respiratory tract infections, gastroenteritis, tinea infections, and herpes simplex infections occurred more frequently in the TREMFYA group than in the placebo group [see Adverse Reactions (6.1)]. The rate of serious infections for the TREMFYA group and the placebo group was ≤ 0.2%. Treatment with TREMFYA should not be initiated in patients with any clinically important active infection until the infection resolves or is adequately treated.
In patients with a chronic infection or a history of recurrent infection, consider the risks and benefits prior to prescribing TREMFYA. Instruct patients to seek medical help if signs or symptoms of clinically important chronic or acute infection occur. If a patient develops a clinically important or serious infection or is not responding to standard therapy, monitor the patient closely and discontinue TREMFYA until the infection resolves.
5.2 Pre-treatment Evaluation for Tuberculosis
Evaluate patients for tuberculosis (TB) infection prior to initiating treatment with TREMFYA. Initiate treatment of latent TB prior to administering TREMFYA. In clinical studies, 105 subjects with latent TB who were concurrently treated with TREMFYA and appropriate TB prophylaxis did not develop active TB (during the mean follow-up of 43 weeks). Monitor patients for signs and symptoms of active TB during and after TREMFYA treatment. Consider anti-TB therapy prior to initiating TREMFYA in patients with a past history of latent or active TB in whom an adequate course of treatment cannot be confirmed. Do not administer TREMFYA to patients with active TB infection.
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed in greater detail in other sections of labeling:
- Infections [see Warnings and Precautions (5.1)]
- Hypersensitivity Reactions [see Contraindications (4) and Warnings and Precautions (5.3)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In clinical trials, a total of 1823 subjects with moderate-to-severe plaque psoriasis received TREMFYA. Of these, 1393 subjects were exposed to TREMFYA for at least 6 months and 728 subjects were exposed for at least 1 year.
Data from two placebo- and active-controlled trials (VOYAGE 1 and VOYAGE 2) in 1441 subjects (mean age 44 years; 70% males; 82% white) were pooled to evaluate the safety of TREMFYA (100 mg administered subcutaneously at Weeks 0 and 4, followed by every 8 weeks).
Weeks 0 to 16
In the 16-week placebo-controlled period of the pooled clinical trials (VOYAGE 1 and VOYAGE 2), adverse events occurred in 49% of subjects in the TREMFYA group compared to 47% of subjects in the placebo group and 49% of subjects in the U.S. licensed adalimumab group. Serious adverse events occurred in 1.9% of subjects in the TREMFYA group (6.3 events per 100 subject-years of follow-up) compared to 1.4% of subjects in the placebo group (4.7 events per 100 subject-years of follow-up), and in 2.6% of subjects in U.S. licensed adalimumab group (9.9 events per 100 subject-years of follow-up).
Table 1 summarizes the adverse reactions that occurred at a rate of at least 1% and at a higher rate in the TREMFYA group than in the placebo group during the 16-week placebo-controlled period.
Table 1: Adverse Reactions Occurring in ≥1% of Subjects through Week 16 in VOYAGE 1 and VOYAGE 2 TREMFYA*
100 mg
N=823
n (%)Adalimumab†
N=196
n (%)Placebo
N=422
n (%)- * Subjects receiving 100 mg of TREMFYA at Week 0, Week 4, and every 8 weeks thereafter
- † U.S. licensed adalimumab
- ‡ Upper respiratory infections include nasopharyngitis, upper respiratory tract infection (URTI), pharyngitis, and viral URTI.
- § Headache includes headache and tension headache.
- ¶ Injection site reactions include injection site erythema, bruising, hematoma, hemorrhage, swelling, edema, pruritus, pain, discoloration, induration, inflammation, and urticaria.
- # Gastroenteritis includes gastroenteritis and viral gastroenteritis.
- Þ Tinea infections include tinea pedis, tinea cruris, tinea infection, and tinea manuum infections.
- ß Herpes simplex infections include oral herpes, herpes simplex, genital herpes, genital herpes simplex, and nasal herpes simplex.
Upper respiratory infections‡ 118 (14.3) 21 (10.7) 54 (12.8) Headache§ 38 (4.6) 2 (1.0) 14 (3.3) Injection site reactions¶ 37 (4.5) 15 (7.7) 12 (2.8) Arthralgia 22 (2.7) 4 (2.0) 9 (2.1) Diarrhea 13 (1.6) 3 (1.5) 4 (0.9) Gastroenteritis# 11 (1.3) 4 (2.0) 4 (0.9) Tinea infectionsÞ 9 (1.1) 0 0 Herpes simplex infectionsß 9 (1.1) 0 2 (0.5) Adverse reactions that occurred in < 1% but > 0.1% of subjects in the TREMFYA group and at a higher rate than in the placebo group through Week 16 in VOYAGE 1 and VOYAGE 2 were migraine, candida infections, and urticaria.
Specific Adverse Reactions
Infections
Infections occurred in 23% of subjects in the TREMFYA group compared to 21% of subjects in the placebo group.
The most common (≥ 1%) infections were upper respiratory infections, gastroenteritis, tinea infections, and herpes simplex infections; all cases were mild to moderate in severity and did not lead to discontinuation of TREMFYA.
Elevated Liver Enzymes
Elevated liver enzymes were reported more frequently in the TREMFYA group (2.6%) than in the placebo group (1.9%). Of the 21 subjects who were reported to have elevated liver enzymes in the TREMFYA group, all events except one were mild to moderate in severity and none of the events led to discontinuation of TREMFYA.
6.2 Immunogenicity
As with all therapeutic proteins, there is the potential for immunogenicity with TREMFYA. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of incidence of antibodies to guselkumab with the incidences of antibodies to other products may be misleading.
Up to Week 52, approximately 6% of subjects treated with TREMFYA developed antidrug antibodies. Of the subjects who developed antidrug antibodies, approximately 7% had antibodies that were classified as neutralizing antibodies. Among the 46 subjects who developed antibodies to guselkumab and had evaluable data, 21 subjects exhibited lower trough levels of guselkumab, including one subject who experienced loss of efficacy after developing high antibody titers. Up to Week 156, approximately 9% of subjects treated with TREMFYA developed antidrug antibodies and of these subjects approximately 6% were classified as neutralizing antibodies. However, antibodies to guselkumab were generally not associated with changes in clinical response or development of injection-site reactions.
6.3 Postmarketing Experience
The following adverse reactions have been reported during post-approval of TREMFYA. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to TREMFYA exposure.
Immune system disorders: Hypersensitivity [see Warnings and Precautions (5.3)]
Skin and subcutaneous tissue disorders: Rash [see Warnings and Precautions (5.3)]
-
7 DRUG INTERACTIONS
7.1 Live Vaccinations
Avoid use of live vaccines in patients treated with TREMFYA [see Warnings and Precautions (5.3)].
7.2 CYP450 Substrates
The formation of CYP450 enzymes can be altered by increased levels of certain cytokines (e.g., IL-1, IL-6, IL-10, TNFα, interferon) during chronic inflammation.
Results from an exploratory drug-drug interaction study in subjects with moderate-to-severe psoriasis suggested a low potential for clinically relevant drug interactions for drugs metabolized by CYP3A4, CYP2C9, CYP2C19 and CYP1A2 but the interaction potential cannot be ruled out for drugs metabolized by CYP2D6. However, the results were highly variable because of the limited number of subjects in the study.
Upon initiation of TREMFYA in patients who are receiving concomitant CYP450 substrates, particularly those with a narrow therapeutic index, consider monitoring for therapeutic effect or drug concentration and consider dosage adjustment as needed [see Clinical Pharmacology (12.3)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no available data on TREMFYA use in pregnant women to inform a drug associated risk of adverse developmental outcomes. Human IgG antibodies are known to cross the placental barrier; therefore, TREMFYA may be transmitted from the mother to the developing fetus. In a combined embryofetal development and pre- and post-natal development study, no adverse developmental effects were observed in infants born to pregnant monkeys after subcutaneous administration of guselkumab during organogenesis through parturition at doses up to 30 times the maximum recommended human dose (MRHD). Neonatal deaths were observed at 6- to 30-times the MRHD (see Data). The clinical significance of these nonclinical findings is unknown.
All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Animal Data
In a combined embryofetal development and pre- and post-natal development study, pregnant cynomolgus monkeys were administered weekly subcutaneous doses of guselkumab up to 50 mg/kg (30 times the MRHD based on a mg/kg comparison) from the beginning of organogenesis to parturition. Neonatal deaths occurred in the offspring of one control monkey, three monkeys administered guselkumab at 10 mg/kg/week (6 times the MRHD based on a mg/kg comparison) and three monkeys administered guselkumab at 50 mg/kg/week (30 times the MRHD based on a mg/kg comparison). The clinical significance of these findings is unknown. No guselkumab-related effects on functional or immunological development were observed in the infants from birth through 6 months of age.
8.2 Lactation
Risk Summary
There are no data on the presence of guselkumab in human milk, the effects on the breastfed infant, or the effects on milk production. Guselkumab was not detected in the milk of lactating cynomolgus monkeys. Maternal IgG is known to be present in human milk. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for TREMFYA and any potential adverse effects on the breastfed infant from TREMFYA or from the underlying maternal condition.
8.4 Pediatric Use
The safety and efficacy of TREMFYA in pediatric patients (less than 18 years of age) have not been established.
8.5 Geriatric Use
Of the 1823 subjects with plaque psoriasis exposed to TREMFYA, a total of 98 subjects were 65 years or older, and 6 subjects were 75 years or older. No overall differences in safety or effectiveness were observed between older and younger subjects who received TREMFYA. However, the number of subjects aged 65 years and older was not sufficient to determine whether they respond differently from younger subjects [see Clinical Pharmacology (12.3)].
- 10 OVERDOSAGE
-
11 DESCRIPTION
Guselkumab, an interleukin-23 blocker, is a human immunoglobulin G1 lambda (IgG1λ) monoclonal antibody. Guselkumab is produced in a mammalian cell line using recombinant DNA technology.
TREMFYA (guselkumab) injection is a sterile, preservative free, clear, colorless to light yellow solution that may contain small translucent particles. TREMFYA is supplied as a single-dose solution in a 1 mL glass syringe with a 27G, half inch fixed needle assembled in a passive needle guard delivery system or One-Press patient-controlled injector for subcutaneous use.
Each TREMFYA 1 mL prefilled syringe or One-Press patient-controlled injector contains 100 mg guselkumab, L-histidine (0.6 mg), L-histidine monohydrochloride monohydrate (1.5 mg), polysorbate 80 (0.5 mg), sucrose (79 mg) and water for injection at pH 5.8.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Guselkumab is a human monoclonal IgG1λ antibody that selectively binds to the p19 subunit of interleukin 23 (IL-23) and inhibits its interaction with the IL-23 receptor. IL-23 is a naturally occurring cytokine that is involved in normal inflammatory and immune responses. Guselkumab inhibits the release of proinflammatory cytokines and chemokines.
12.2 Pharmacodynamics
Guselkumab reduced serum levels of IL-17A, IL-17F and IL-22 relative to pre-treatment levels in evaluated subjects with psoriasis based on exploratory analysis of the pharmacodynamic markers. The relationship between these pharmacodynamic markers and the mechanism(s) by which guselkumab exerts its clinical effects is not fully understood.
12.3 Pharmacokinetics
Guselkumab exhibited linear pharmacokinetics in healthy subjects and subjects with psoriasis following subcutaneous injections. In subjects with psoriasis, following subcutaneous administration of 100 mg of TREMFYA at Weeks 0 and 4, and every 8 weeks thereafter, mean steady-state trough serum guselkumab concentration was approximately 1.2 mcg/mL.
Absorption
Following a single 100 mg subcutaneous injection in healthy subjects, guselkumab reached a mean (± SD) maximum serum concentration of 8.09 ± 3.68 mcg/mL by approximately 5.5 days post dose. The absolute bioavailability of guselkumab following a single 100 mg subcutaneous injection was estimated to be approximately 49% in healthy subjects.
Elimination
Apparent clearance in subjects with plaque psoriasis was 0.516 L/day. Mean half-life of guselkumab was approximately 15 to 18 days in subjects with plaque psoriasis across studies.
Metabolism
The exact pathway through which guselkumab is metabolized has not been characterized. As a human IgG monoclonal antibody, guselkumab is expected to be degraded into small peptides and amino acids via catabolic pathways in the same manner as endogenous IgG.
Specific Populations
No apparent differences in clearance were observed in subjects ≥ 65 years of age compared to subjects < 65 years of age, suggesting no dose adjustment is needed for elderly patients. Clearance and volume of distribution of guselkumab increases as body weight increases, however, observed clinical trial data indicate that dose adjustment for body weight is not warranted. No specific studies have been conducted to determine the effect of renal or hepatic impairment on the pharmacokinetics of guselkumab.
Drug Interactions
Population pharmacokinetic analyses indicated that concomitant use of ibuprofen, acetylsalicylic acid, or acetaminophen did not affect the clearance of guselkumab.
Cytochrome P450 Substrates
The effects of guselkumab on the pharmacokinetics of midazolam (metabolized by CYP3A4), warfarin (metabolized by CYP2C9), omeprazole (metabolized by CYP2C19), dextromethorphan (metabolized by CYP2D6), and caffeine (metabolized by CYP1A2) were evaluated in an exploratory study with 6 to 12 evaluable subjects with moderate-to-severe plaque psoriasis. Changes in AUCinf of midazolam, S-warfarin, omeprazole, and caffeine after a single dose of guselkumab were not clinically relevant. For dextromethorphan, changes in AUCinf after guselkumab were not clinically relevant in 9 out of 10 subjects; however, a 2.9-fold change in AUCinf was observed in one individual [see Drug Interactions (7.2)].
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Animal studies have not been conducted to evaluate the carcinogenic or mutagenic potential of TREMFYA.
No effects on fertility parameters were observed after male guinea pigs were subcutaneously administered guselkumab at a dose of 25 mg/kg twice weekly (15 times the MRHD based on a mg/kg comparison).
No effects on fertility parameters were observed after female guinea pigs were subcutaneously administered guselkumab at doses up to 100 mg/kg twice-weekly (60 times the MRHD based on a mg/kg comparison).
-
14 CLINICAL STUDIES
Four multicenter, randomized, double-blind trials (VOYAGE 1 [NCT02207231], VOYAGE 2 [NCT02207244], NAVIGATE [NCT02203032], and ORION [NCT02905331]) enrolled subjects 18 years of age and older with moderate-to-severe plaque psoriasis who were eligible for systemic therapy or phototherapy. Subjects had an Investigator's Global Assessment (IGA) score of ≥3 ("moderate") on a 5-point scale of overall disease severity, a Psoriasis Area and Severity Index (PASI) score ≥12, and a minimum affected body surface area (BSA) of 10%. Subjects with guttate, erythrodermic, or pustular psoriasis were excluded.
VOYAGE 1 and VOYAGE 2
In VOYAGE 1 and VOYAGE 2, 1443 subjects were randomized to either TREMFYA (100 mg at Weeks 0 and 4 and every 8 weeks thereafter) administered with a prefilled syringe, placebo or U.S. licensed adalimumab (80 mg at Week 0 and 40 mg at Week 1, followed by 40 mg every other week thereafter).
Both trials assessed the responses at Week 16 compared to placebo for the two co-primary endpoints:
- the proportion of subjects who achieved an IGA score of 0 ("cleared") or 1 ("minimal");
- the proportion of subjects who achieved at least a 90% reduction from baseline in the PASI composite score (PASI 90).
Comparisons between TREMFYA and U.S. licensed adalimumab were secondary endpoints at the following time points:
- at Week 16 (VOYAGE 1 and VOYAGE 2), the proportions of subjects who achieved an IGA score of 0 or 1, a PASI 90, and a PASI 75 response;
- at Week 24 (VOYAGE 1 and VOYAGE 2), and at Week 48 (VOYAGE 1), the proportions of subjects achieving an IGA score of 0, an IGA score of 0 or 1, and a PASI 90 response.
Other evaluated outcomes included improvement in psoriasis symptoms assessed on the Psoriasis Symptoms and Signs Diary (PSSD) and improvements in psoriasis of the scalp at Week 16.
In both trials, subjects were predominantly men and white, with a mean age of 44 years and a mean weight of 90 kg. At baseline, subjects had a median affected BSA of approximately 21%, a median PASI score of 19, and 18% had a history of psoriatic arthritis. Approximately 24% of subjects had an IGA score of severe. In both trials, 23% had received prior biologic systemic therapy.
Clinical Response
Table 2 presents the efficacy results at Week 16 in VOYAGE 1 and VOYAGE 2.
Table 2: Efficacy Results at Week 16 in Adults with Plaque Psoriasis (NRI*) VOYAGE 1 VOYAGE 2 Endpoint TREMFYA
(N=329)
n (%)Placebo
(N=174)
n (%)TREMFYA
(N=496)
n (%)Placebo
(N=248)
n (%)- * NRI = Non-Responder Imputation
- † Co-Primary Endpoints
- ‡ IGA response of 0 (cleared) or 1 (minimal)
IGA response of 0/1†, ‡ 280 (85) 12 (7) 417 (84) 21 (8) PASI 90 response† 241 (73) 5 (3) 347 (70) 6 (2) Table 3 presents the results of an analysis of all the North America sites (i.e., U.S. and Canada), demonstrating superiority of TREMFYA to U.S. licensed adalimumab.
Table 3: Efficacy Results in Adults with Plaque Psoriasis (NRI*) VOYAGE 1 VOYAGE 2 Endpoint TREMFYA
(N=115)†
n (%)Adalimumab‡
(N=115)†
n (%)TREMFYA
(N=160)†
n (%)Adalimumab‡
(N=81)†
n (%)- * NRI = Non-Responder Imputation
- † Subjects from sites in the United States and Canada
- ‡ U.S. licensed adalimumab
IGA response of 0/1 (cleared or minimal) Week 16 97 (84) 70 (61) 119 (74) 50 (62) Week 24 97 (84) 62 (54) 119 (74) 46 (57) Week 48 91 (79) 62 (54) NA NA IGA response of 0 (cleared) Week 24 61 (53) 27 (23) 76 (48) 23 (28) Week 48 54 (47) 28 (24) NA NA PASI 75 response Week 16 105 (91) 80 (70) 132 (83) 51 (63) PASI 90 response Week 16 84 (73) 47 (41) 102 (64) 34 (42) Week 24 92 (80) 51 (44) 113 (71) 41 (51) Week 48 84 (73) 53 (46) NA NA An improvement was seen in psoriasis involving the scalp in subjects randomized to TREMFYA compared to placebo at Week 16.
Examination of age, gender, race, body weight, and previous treatment with systemic or biologic agents did not identify differences in response to TREMFYA among these subgroups.
Maintenance and Durability of Response
To evaluate maintenance and durability of response (VOYAGE 2), subjects randomized to TREMFYA at Week 0 and who were PASI 90 responders at Week 28 were re-randomized to either continue treatment with TREMFYA every 8 weeks or be withdrawn from therapy (i.e. receive placebo).
At Week 48, 89% of subjects who continued on TREMFYA maintained PASI 90 compared to 37% of subjects who were re-randomized to placebo and withdrawn from TREMFYA. For responders at Week 28 who were re-randomized to placebo and withdrawn from TREMFYA, the median time to loss of PASI 90 was approximately 15 weeks.
Patient Reported Outcomes
Greater improvements in symptoms of psoriasis (itch, pain, stinging, burning and skin tightness) at Week 16 in TREMFYA compared to placebo were observed in both trials based on the Psoriasis Symptoms and Signs Diary (PSSD). Greater proportions of subjects on TREMFYA compared to U.S. licensed adalimumab achieved a PSSD symptom score of 0 (symptom-free) at Week 24 in both trials.
NAVIGATE
NAVIGATE evaluated the efficacy of 24 weeks of treatment with TREMFYA in subjects (N=268) who had not achieved an adequate response, defined as IGA ≥2 at Week 16 after initial treatment with U.S. licensed ustekinumab (dosed 45 mg or 90 mg according to the subject's baseline weight at Week 0 and Week 4). These subjects were randomized to either continue with U.S. licensed ustekinumab treatment every 12 weeks or switch to TREMFYA 100 mg at Weeks 16, 20, and every 8 weeks thereafter. Baseline characteristics for randomized subjects were similar to those observed in VOYAGE 1 and VOYAGE 2.
In subjects with an inadequate response (IGA ≥2 at Week 16 to U.S. licensed ustekinumab), greater proportions of subjects on TREMFYA compared to U.S. licensed ustekinumab achieved an IGA score of 0 or 1 with a ≥2 grade improvement at Week 28 (31% vs 14%, respectively; 12 weeks after randomization).
ORION
ORION evaluated the efficacy, safety, and pharmacokinetics of TREMFYA administered with the One-Press injector. In this study, 78 subjects were randomized to receive either TREMFYA (100 mg at Weeks 0 and 4 and every 8 weeks thereafter) [N=62], or placebo [N=16]. Baseline characteristics for subjects were comparable to those observed in VOYAGE 1 and VOYAGE 2. The co-primary endpoints were the same as those for VOYAGE 1 and VOYAGE 2. Secondary endpoints included the proportion of subjects who achieved an IGA score of 0 at Week 16 and the proportion of subjects who achieved a PASI 100 response at Week 16.
A greater proportion of subjects in the guselkumab group achieved an IGA score of 0 or 1 or a PASI 90 response at Week 16 (81% and 76%, respectively) than in the placebo group (0% for both endpoints). The proportion of subjects who achieved an IGA score of 0 at Week 16 was higher in the guselkumab group compared to the placebo group (56% vs. 0%). The proportion of subjects who achieved a PASI 100 response at Week 16 was higher in the guselkumab group compared to the placebo group (50% vs. 0%).
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
TREMFYA (guselkumab) Injection is a clear and colorless to light yellow solution that may contain small translucent particles. TREMFYA is supplied as:
- Single-dose 100 mg/mL prefilled syringe (NDC: 57894-640-01)
- Single-dose 100 mg/mL One-Press patient-controlled injector (NDC: 57894-640-11)
-
17 PATIENT COUNSELING INFORMATION
Advise the patient and/or caregiver to read the FDA-approved patient labeling (Medication Guide and Instructions for Use) before starting TREMFYA therapy, and each time the prescription is renewed, as there may be new information they need to know.
Infections
Instruct patients of the importance of communicating any history of infections to the healthcare provider and contacting their healthcare provider if they develop any symptoms of an infection [see Warnings and Precautions (5.1)].
Hypersensitivity Reactions
Advise patients to discontinue TREMFYA and seek immediate medical attention if they experience any symptoms of serious hypersensitivity reactions [see Warnings and Precautions (5.3)].
Instruction on Injection Technique
Instruct patients or caregivers to perform the first self-injection under the supervision and guidance of a qualified healthcare professional for proper training in subcutaneous injection technique. Instruct patients who are self-administering to inject the full dose of TREMFYA [see Medication Guide and Instructions for Use].
Instruct patients or caregivers in the technique of proper needle and syringe disposal. Needles and syringes should be disposed of in a puncture-resistant container. Advise patients and caregivers not to reuse needles or syringes.
Remind patients if they forget to take their dose of TREMFYA to inject their dose as soon as they remember. They should then take their next dose at the appropriate scheduled time.
- SPL UNCLASSIFIED SECTION
-
MEDICATION GUIDE
This Medication Guide had been approved by the U.S. Food and Drug Administration. Revised: April/2019 Medication Guide
TREMFYA® (trem fye' ah)
(guselkumab)
injection, for subcutaneous useWhat is the most important information I should know about TREMFYA?
TREMFYA may cause serious side effects, including:
Infections. TREMFYA is a medicine that may lower the ability of your immune system to fight infections and may increase your risk of infections. Your healthcare provider should check you for infections and tuberculosis (TB) before starting treatment with TREMFYA and may treat you for TB before you begin treatment with TREMFYA if you have a history of TB or have active TB. Your healthcare provider should watch you closely for signs and symptoms of TB during and after treatment with TREMFYA.- Tell your healthcare provider right away if you have an infection or have symptoms of an infection, including:
- fever, sweats, or chills
- cough
- shortness of breath
- blood in your phlegm (mucus)
- muscle aches
- warm, red, or painful skin or sores on your body different from your psoriasis
- weight loss
- diarrhea or stomach pain
- burning when you urinate or urinating more often than normal
See "What are the possible side effects of TREMFYA?" for more information about side effects. What is TREMFYA?
TREMFYA is a prescription medicine used to treat adults with moderate to severe plaque psoriasis who may benefit from taking injections or pills (systemic therapy) or phototherapy (treatment using ultraviolet or UV light).
It is not known if TREMFYA is safe and effective in children under 18 years of age.Do not use TREMFYA if you have had a serious allergic reaction to guselkumab or any of the other ingredients in TREMFYA. See the end of this Medication Guide for a complete list of ingredients in TREMFYA. Before using TREMFYA, tell your healthcare provider about all of your medical conditions, including if you: - have any of the conditions or symptoms listed in the section "What is the most important information I should know about TREMFYA?"
- have an infection that does not go away or that keeps coming back.
- have TB or have been in close contact with someone with TB.
- have recently received or are scheduled to receive an immunization (vaccine). You should avoid receiving live vaccines during treatment with TREMFYA.
- are pregnant or plan to become pregnant. It is not known if TREMFYA can harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if TREMFYA passes into your breast milk.
How should I use TREMFYA?
See the detailed "Instructions for Use" that comes with TREMFYA for information on how to prepare and inject a dose of TREMFYA, and how to properly throw away (dispose of) used TREMFYA prefilled syringes or One-Press injectors.
- Use TREMFYA exactly as your healthcare provider tells you to use it.
- If you miss your TREMFYA dose, inject a dose as soon as you remember. Then, take your next dose at your regular scheduled time. Call your healthcare provider if you are not sure what to do.
What are the possible side effects of TREMFYA?
TREMFYA may cause serious side effects including:- See "What is the most important information I should know about TREMFYA?"
-
Serious allergic reactions. Stop using TREMFYA and get emergency medical help right away if you develop any of the following symptoms of a serious allergic reaction:
- feel faint
- swelling of your face, eyelids, lips, mouth, tongue or throat
- trouble breathing or throat tightness
- chest tightness
- skin rash, hives
The most common side effects of TREMFYA include: - upper respiratory infections
- joint pain (arthralgia)
- fungal skin infections
- headache
- diarrhea
- herpes simplex infections
- injection site reactions
- stomach flu (gastroenteritis)
These are not all the possible side effects of TREMFYA. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. General information about the safe and effective use of TREMFYA
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use TREMFYA for a condition for which it was not prescribed. Do not give TREMFYA to other people, even if they have the same symptoms that you have. It may harm them. You can ask your healthcare provider or pharmacist for information about TREMFYA that is written for health professionals.What are the ingredients in TREMFYA?
Active ingredient: guselkumab
Inactive ingredients: L-histidine, L-histidine monohydrochloride monohydrate, polysorbate 80, sucrose and water for injectionManufactured by: Janssen Biotech, Inc., Horsham, PA 19044, U.S. License Number 1864,
For more information, call 1-800-526-7736 or go to www.tremfya.com. -
Instructions for Use
TREMFYA®
(trem fye' ah)
(guselkumab)Prefilled Syringe

SINGLE-DOSE
Important
TREMFYA comes as a single-dose prefilled syringe containing one 100 mg dose. Each TREMFYA prefilled syringe can only be used one time. Throw the used prefilled syringe away (See Step 3) after one dose, even if there is medicine left in it. Do not reuse your TREMFYA prefilled syringe.
If your healthcare provider decides that you or a caregiver may be able to give your injections of TREMFYA at home, you should receive training on the right way to prepare and inject TREMFYA using the prefilled syringe before attempting to inject. Do not try to inject yourself until you have been shown the right way to give the injections by your healthcare provider.
Read this Instructions for Use before using your TREMFYA prefilled syringe and each time you get a refill. There may be new information. This leaflet does not take the place of talking with your healthcare provider about your medical condition or your treatment.
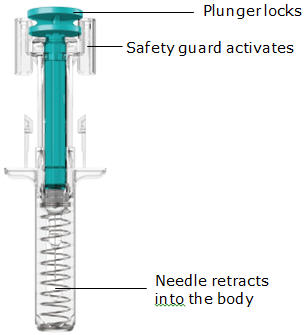
The TREMFYA prefilled syringe is intended for injection under the skin, not into the muscle or vein. After injection, the needle will retract into the body of the device and lock into place.
 Storage information
Storage information
Store in refrigerator at 36° to 46°F (2° to 8°C). Do not freeze TREMFYA prefilled syringe.
Keep TREMFYA prefilled syringe and all medicines out of reach of children.
Do not shake your TREMFYA prefilled syringe.
Keep TREMFYA prefilled syringe in the original carton to protect from light and physical damage.
Prefilled syringe parts
Before use
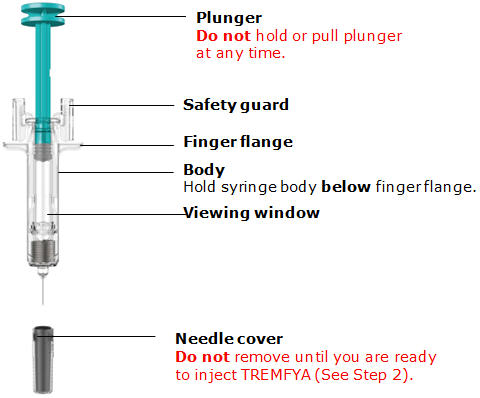
After use
You will need these supplies:
- 1 TREMFYA prefilled syringe
Not provided in the TREMFYA prefilled syringe carton:
- 1 Alcohol swab
- 1 Cotton ball or gauze pad
- 1 Adhesive bandage
- 1 Sharps container (See Step 3)
1. Prepare for your injection

Inspect carton
Remove your TREMFYA prefilled syringe carton from the refrigerator.
Keep the prefilled syringe in the carton and let it sit on a flat surface at room temperature for at least 30 minutes before use.
Do not warm the prefilled syringe any other way.
Check the expiration date ('EXP') on the back panel of the carton.
Do not use your prefilled syringe if the expiration date has passed.
Do not inject TREMFYA if the perforations on the carton are broken. Call your healthcare provider or pharmacist for a refill.

Choose injection site
Select from the following areas for your injection:
- Front of thighs (recommended)
- Lower stomach area (lower abdomen), except for a 2-inch area right around your navel (belly-button)
- Back of upper arms (only if someone else is giving you the injection)
Do not inject into skin that is tender, bruised, red, hard, thick, scaly or affected by psoriasis.

Clean injection site
Wash your hands well with soap and warm water.
Wipe your chosen injection site with an alcohol swab and allow it to dry.
Do not touch, fan, or blow on the injection site after you have cleaned it.
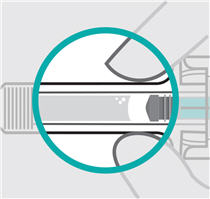
Inspect liquid
Take your TREMFYA prefilled syringe out of the carton.
Check the TREMFYA prefilled syringe liquid in the viewing window. It should be clear to slightly yellow and may contain tiny white or clear particles. You may also see one or more air bubbles. This is normal.
Do not inject if the liquid is cloudy or discolored, or has large particles. Call your healthcare provider or pharmacist for a refill.
2. Inject TREMFYA using prefilled syringe
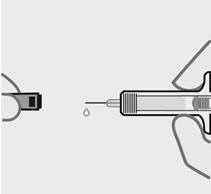
Remove needle cover
Hold your prefilled syringe by the body and pull needle cover straight off. It is normal to see a drop of liquid.
Inject TREMFYA within 5 minutes of removing the needle cover.
Do not put needle cover back on, as this may damage the needle or cause a needle stick injury.
Do not touch needle or let it touch any surface.
Do not use a TREMFYA prefilled syringe if it is dropped. Call your healthcare provider or pharmacist for a refill.
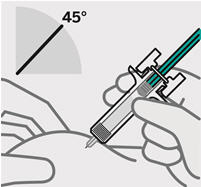
Position fingers and insert needle
Place your thumb, index and middle fingers directly under the finger flange, as shown.
Do not touch plunger or area above finger flange as this may cause the needle safety device to activate.
Use your other hand to pinch skin at the injection site. Position syringe at about a 45 degree angle to the skin.
It is important to pinch enough skin to inject under the skin and not into the muscle.
Insert needle with a quick, dart-like motion.
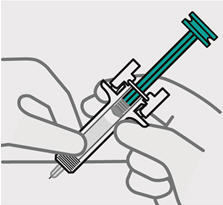
Release pinch and reposition hand
Use your free hand to grasp the body of the prefilled syringe.
Press plunger
Place thumb from the opposite hand on the plunger and press the plunger all the way down until it stops.

Release pressure from plunger
The safety guard will cover the needle and lock into place, removing the needle from your skin.

Dispose of your prefilled syringe
Put your used TREMFYA prefilled syringe in an FDA-cleared sharps disposal container right away after use.
Do not throw away (dispose of) your TREMFYA prefilled syringe in your household trash.
Do not recycle your used sharps disposal container.
For more information, see "How should I dispose of the used prefilled syringe?"

Check injection site
There may be a small amount of blood or liquid at the injection site. Hold pressure over your skin with a cotton ball or gauze pad until any bleeding stops.
Do not rub the injection site.
If needed, cover injection site with a bandage.
 Need help?
Need help?
Call your healthcare provider to talk about any questions you may have. For additional assistance or to share your feedback call 800-JANSSEN (800-526-7736).
How should I dispose of the used prefilled syringe?
If you do not have an FDA-cleared sharps disposal container, you may use a household container that is:
- made of a heavy-duty plastic
- can be closed with a tight-fitting, puncture-resistant lid, without sharps being able to come out
- upright and stable during use
- leak-resistant
- properly labeled to warn of hazardous waste inside the container
When your sharps disposal container is almost full, you will need to follow your community guidelines for the right way to dispose of your sharps disposal container. There may be state or local laws about how you should throw away used needles and syringes.
For more information about safe sharps disposal, and for specific information about sharps disposal in the state that you live in, go to the FDA's website at: www.fda.gov/safesharpsdisposal
This Instructions for Use has been approved by the U.S. Food and Drug Administration.
Manufactured by:
Janssen Biotech, Inc. Horsham, PA 19044
US License No. 1864Approved: December 2017
-
Instructions for Use
TREMFYA®
(trem fye' ah)
(guselkumab)One-Press Patient-Controlled Injector

SINGLE-DOSE
Important
TREMFYA comes in a single-dose One-Press injector containing one 100 mg dose. Each One-Press injector can only be used one time. Throw away (See Step 3) after one dose, even if there is medicine left in it. Do not reuse your One-Press injector.
If your healthcare provider decides that you or a caregiver may be able to give your injections of TREMFYA at home, you should receive training on the right way to prepare and inject TREMFYA using the One-Press injector. Do not try to inject yourself until you have been trained by your healthcare provider.
Please read this Instructions for Use before using your One-Press injector and each time you get a new One-Press injector. There may be new information. This leaflet does not take the place of talking with your healthcare provider about your medical condition or your treatment.
 Storage information
Storage information
Store in refrigerator at 36° to 46°F (2° to 8°C).
Do not freeze your One-Press injector.
Keep your One-Press injector and all medicines out of reach of children.
Do not shake your One-Press injector.
Keep your One-Press injector in the original carton to protect from light and physical damage.
 Need help?
Need help?
Call your healthcare provider to talk about any questions you may have. For additional assistance or to share your feedback call 800-JANSSEN (800-526-7736).
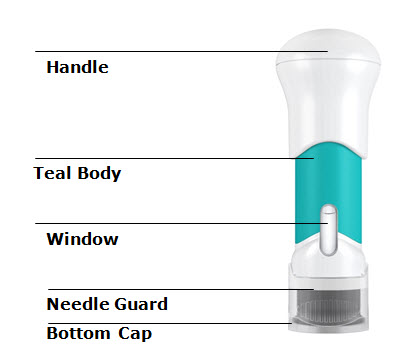
One-Press injector parts
You will need: - 1 One-Press injector
- 1 Alcohol swab
- 1 Cotton ball or gauze pad
- 1 Adhesive bandage
- 1 Sharps container (See Step 3)
1. Prepare for your injection
Inspect carton
Remove your One-Press injector carton from the refrigerator.
Keep your One-Press injector in the carton and let it sit on a flat surface at room temperature for at least 30 minutes before use.
Do not warm your One-Press injector any other way.
Check the expiration date ('EXP') on the carton.
Do not use your One-Press injector if the expiration date has passed.
Do not inject TREMFYA if the perforations on the carton are broken. Call your healthcare provider or pharmacist for a new One-Press injector.

Choose injection site
Select from the following areas for your injection:
- Front of thighs (recommended)
- Lower stomach area (lower abdomen), except for a 2-inch area right around your navel (belly-button)
- Back of upper arms (only if someone else is giving you the injection)
Do not inject into skin that is tender, bruised, red, hard, thick, scaly, or affected by psoriasis.

Wash hands
Wash your hands well with soap and warm water.
Clean injection site
Wipe your chosen injection site with an alcohol swab and allow it to dry.
Do not touch, fan, or blow on the injection site after you have cleaned it.

Inspect liquid in window
Take your One-Press injector out of the carton.
Check the liquid in the window. It should be clear to slightly yellow and may contain tiny white or clear particles. You may also see one or more air bubbles. This is normal.
Do not inject if the liquid is cloudy or discolored, or has large particles. Call your healthcare provider or pharmacist for a new One-Press injector.
2. Inject TREMFYA using the One-Press injector
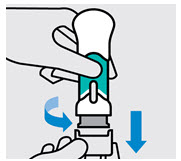
Twist and pull off bottom cap
Keep hands away from the needle guard after the cap is removed.
Inject TREMFYA within 5 minutes of removing the cap.
Do not put the cap back on, this could damage the needle.
Do not use a One-Press injector if it is dropped after removing the cap. Call your healthcare provider or pharmacist for a new One-Press injector.
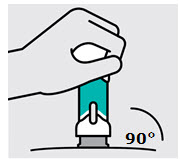
Place on skin
Position the One-Press injector straight onto the skin (about 90 degrees relative to injection site).
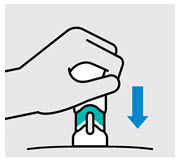
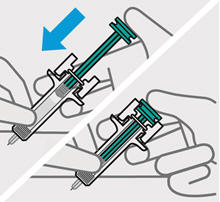
Push handle straight down
Medication injects as you push. Do this at a speed that is comfortable for you.
Do not lift the One-Press injector during the injection. The needle guard will lock and the full dose will not be delivered.
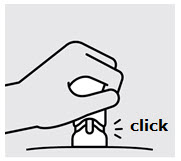
Complete injection
Injection is complete when the handle is pushed all the way down, you hear a click, and the teal body is no longer visible.
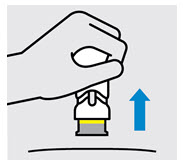
Lift straight up
The yellow band indicates that the needle guard is locked.

Dispose of your One-Press injector
Put your used One-Press injector in an FDA-cleared sharps disposal container right away after use.
Do not throw away (dispose of) your One-Press injector in your household trash.
Do not recycle your used sharps disposal container.
For more information, see "How should I dispose of the used One-Press injector?".
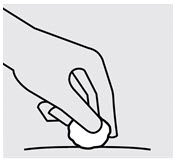
Check injection site
There may be a small amount of blood or liquid at the injection site. Hold pressure over your skin with a cotton ball or gauze pad until any bleeding stops.
Do not rub the injection site.
If needed, cover injection site with a bandage.
How should I dispose of the used One-Press injector?
If you do not have an FDA-cleared sharps disposal container, you may use a household container that is:
- made of a heavy-duty plastic
- can be closed with a tight-fitting, puncture-resistant lid, without sharps being able to come out
- upright and stable during use
- leak-resistant
- properly labeled to warn of hazardous waste inside the container
When your sharps disposal container is almost full, you will need to follow your community guidelines for the right way to dispose of your sharps disposal container. There may be state or local laws about how you should throw away used needles and syringes.
For more information about safe sharps disposal, and for specific information about sharps disposal in the state that you live in, go to the FDA's website at: www.fda.gov/safesharpsdisposal
This Instructions for Use has been approved by the U.S. Food and Drug Administration.
Manufactured by:
Janssen Biotech, Inc. Horsham, PA 19044
US License No. 1864Approved: January 2019
-
PRINCIPAL DISPLAY PANEL - 100 mg/mL Syringe Carton
Tremfya®
(guselkumab)
Injection100 mg/mL
FOR SUBCUTANEOUS USE ONLY
Rx only
NDC: 57894-640-11
Single-dose One-Press
patient-controlled injectorDiscard unused portion
Contains no preservativeATTENTION: Dispense the enclosed
Medication Guide to each patient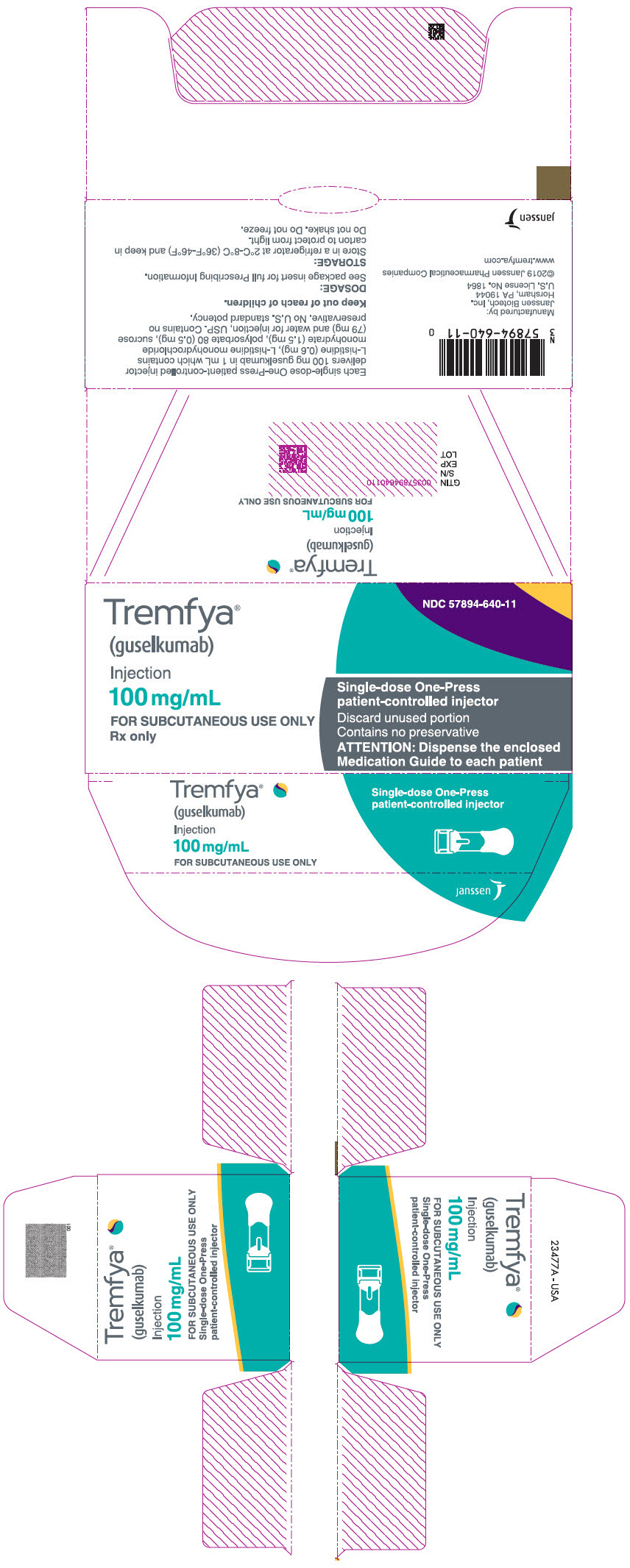
-
INGREDIENTS AND APPEARANCE
TREMFYA
guselkumab injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 57894-640 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Guselkumab (UNII: 089658A12D) (Guselkumab - UNII:089658A12D) Guselkumab 100 mg in 1 mL Inactive Ingredients Ingredient Name Strength Histidine (UNII: 4QD397987E) 0.6 mg in 1 mL Histidine Monohydrochloride Monohydrate (UNII: X573657P6P) 1.5 mg in 1 mL Polysorbate 80 (UNII: 6OZP39ZG8H) 0.5 mg in 1 mL Sucrose (UNII: C151H8M554) 79 mg in 1 mL Water (UNII: 059QF0KO0R) Product Characteristics Color YELLOW (clear and colorless to light yellow) Score Shape Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 57894-640-01 1 in 1 CARTON 07/13/2017 1 1 mL in 1 SYRINGE; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) 2 NDC: 57894-640-04 1 in 1 CARTON 07/13/2017 2 1 mL in 1 SYRINGE; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) 3 NDC: 57894-640-11 1 in 1 CARTON 01/28/2019 3 1 mL in 1 SYRINGE; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) 4 NDC: 57894-640-99 1 in 1 CARTON 01/28/2019 4 1 mL in 1 SYRINGE; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA761061 07/13/2017 Labeler - Janssen Biotech, Inc. (099091753) Establishment Name Address ID/FEI Business Operations Janssen Sciences Ireland UC 986030167 API MANUFACTURE(57894-640) , ANALYSIS(57894-640) Establishment Name Address ID/FEI Business Operations Cilag AG 483237103 MANUFACTURE(57894-640) , ANALYSIS(57894-640) , PACK(57894-640) Establishment Name Address ID/FEI Business Operations Janssen Biologics B.V. 409612918 ANALYSIS(57894-640) Establishment Name Address ID/FEI Business Operations AndersonBrecon Inc. 053217022 PACK(57894-640) Establishment Name Address ID/FEI Business Operations PPD Development Ireland Ltd. 985036175 ANALYSIS(57894-640) Establishment Name Address ID/FEI Business Operations Janssen Biotech, Inc. 038978363 API MANUFACTURE(57894-640) Establishment Name Address ID/FEI Business Operations Biogen MA Inc. 841087823 API MANUFACTURE(57894-640)
Trademark Results [TREMFYA]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 TREMFYA 86799255 5297001 Live/Registered |
JOHNSON & JOHNSON 2015-10-26 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.