CALDOLOR- ibuprofen injection
Caldolor by
Drug Labeling and Warnings
Caldolor by is a Prescription medication manufactured, distributed, or labeled by Cumberland Pharmaceuticals Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use CALDOLOR® safely and effectively. See full prescribing information for CALDOLOR.
CALDOLOR (ibuprofen) injection, for intravenous use
Initial U.S. Approval: 1974WARNING: RISK OF SERIOUS CARDIOVASCULAR AND GASTROINTESTINAL EVENTS
See full prescribing information for complete boxed warning
- Non-steroidal anti-inflammatory drugs (NSAIDs) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use. (5.1)
- CALDOLOR is contraindicated in the setting of coronary artery bypass graft (CABG) surgery. (4, 5.1)
- NSAIDs cause an increased risk of serious gastrointestinal (GI) adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients and patients with a prior history of peptic ulcer disease and/or GI bleeding are at greater risk for serious GI events. (5.2)
INDICATIONS AND USAGE
DOSAGE AND ADMINISTRATION
- Use the lowest effective dosage for shortest duration consistent with individual patient treatment goals
- CALDOLOR Injection vials must be diluted before administration. (2.1)
- CALDOLOR Injection bags are ready to use. (2.1)
- Adult Pain: 400 mg to 800 mg intravenously over 30 minutes every 6 hours as necessary. (2.2)
- Adult Fever: 400 mg intravenously over 30 minutes, followed by 400 mg every 4 to 6 hours or 100-200 mg every 4 hours as necessary. (2.2)
- Pediatric (pain and fever) ages 12 to 17 years of age: 400 mg intravenously over 10 minutes every 4 to 6 hours as necessary (2.3)
- Pediatric (pain and fever) ages 6 months to 12 years of age: 10 mg/kg intravenously over 10 minutes up to a maximum single dose of 400 mg every 4 to 6 hours as necessary (2.3)
- CALDOLOR must be diluted before administration. (2.1)
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Hepatotoxicity: Inform patients of warning signs and symptoms of hepatotoxicity. Discontinue if abnormal liver tests persist or worsen or if clinical signs and symptoms of liver disease develop (5.3)
- Hypertension: Patients taking some antihypertensive medications may have impaired response to these therapies when taking NSAIDs. Monitor blood pressure (5.4, 7)
- Heart Failure and Edema: Avoid use of CALDOLOR in patients with severe heart failure unless benefits are expected to outweigh risk of worsening heart failure (5.5)
- Renal Toxicity: Monitor renal function in patients with renal or hepatic impairment, heart failure, dehydration, or hypovolemia. Avoid use of CALDOLOR in patients with advanced renal disease unless benefits are expected to outweigh risk of worsening renal function (5.6)
- Anaphylactic Reactions: Seek emergency help if an anaphylactic reaction occurs (5.7)
- Exacerbation of Asthma Related to Aspirin Sensitivity: CALDOLOR is contraindicate d in patients with aspirin-sensitive asthma. Monitor patients with preexisting asthma (without aspirin sensitivity) (5.8)
- Serious Skin Reactions: Discontinue CALDOLOR at first appearance of skin rash or other signs of hypersensitivity (5.9)
- Premature Closure of Fetal Ductus Arteriosus: Avoid use in pregnant women starting at 30 weeks gestation (5.10, 8.1)
- Hematologic Toxicity: Monitor hemoglobin or hematocrit in patients with any signs or symptoms of anemia (5.11, 7)
ADVERSE REACTIONS
The most common adverse reactions are nausea, flatulence, vomiting, headache, hemorrhage and dizziness (>5%).
The most common adverse reactions in pediatric patients are infusion site pain, vomiting, nausea, anemia and headache (≥2%). (6)
To report SUSPECTED ADVERSE REACTIONS, contact Cumberland Pharmaceuticals Inc. at 1-877-484-2700 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- Drugs that Interfere with Hemostasis (e.g. warfarin, aspirin, SSRIs/SNRIs): Monitor patients for bleeding who are concomitantly taking CALDOLOR with drugs that interfere with hemostasis. Concomitant use of CALDOLOR and analgesic doses of aspirin is not generally recommended (7)
- ACE Inhibitors, Angiotensin Receptor Blockers (ARB), or Beta-Blockers: Concomitant use with CALDOLOR may diminish the antihypertensive effect of these drugs. Monitor blood pressure (7)
- ACE Inhibitors and ARBs: Concomitant use with CALDOLOR in elderly, volume depleted, or those with renal impairment may result in deterioration of renal function. In such high risk patients, monitor for signs of worsening renal function (7)
- Diuretics: NSAIDs can reduce natriuretic effect of furosemide and thiazide diuretics. Monitor patients to assure diuretic efficacy including antihypertensive effects (7)
- Digoxin: Concomitant use with CALDOLOR can increase serum concentration and prolong half-life of digoxin. Monitor serum digoxin levels (7)
USE IN SPECIFIC POPULATIONS
Pregnancy: Use of NSAIDs during the third trimester of pregnancy increases the risk of premature closure of the fetal ductus arteriosus. Avoid use of NSAIDs in pregnant women starting at 30 weeks gestation (5.10, 8.1)
Infertility: NSAIDs are associated with reversible infertility. Consider withdrawal of CALDOLOR in women who have difficulties conceiving (8.3)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 1/2020
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: RISK OF SERIOUS CARDIOVASCULAR AND GASTROINTESTINAL EVENTS
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosage and Administration Instructions
2.2 Adults
2.3 Pediatric Patients
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Cardiovascular Thrombotic Events
5.2 Gastrointestinal Bleeding, Ulceration, and Perforation
5.3 Hepatotoxicity
5.4 Hypertension
5.5 Heart Failure and Edema
5.6 Renal Toxicity and Hyperkalemia
5.7 Anaphylactic Reactions
5.8 Exacerbation of Asthma Related to Aspirin Sensitivity
5.9 Serious Skin Reactions
5.10 Premature Closure of Fetal Ductus Arteriosus
5.11 Hematologic Toxicity
5.12 Masking of Inflammation and Fever
5.13 Laboratory Monitoring
5.14 Ophthalmological Effects
5.15 Aseptic Meningitis
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Analgesia (Pain)
14.2 Antipyretic (Fever)
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: RISK OF SERIOUS CARDIOVASCULAR AND GASTROINTESTINAL EVENTS
Cardiovascular Thrombotic Events
- Non-steroidal anti-inflammatory drugs (NSAIDs) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use. [see Warnings and Precautions (5.1)].
- CALDOLOR is contraindicated in the setting of coronary artery bypass graft (CABG) surgery [see Contraindications (4) and Warnings and Precautions (5.1)].
Gastrointestinal Bleeding, Ulceration and Perforation
- NSAIDs cause an increased risk of serious gastrointestinal (GI) adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients and patients with a prior history of peptic ulcer disease and/or GI bleeding are at greater risk for serious GI events [see Warnings and Precautions (5.2)].
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosage and Administration Instructions
Use the lowest effective dosage for the shortest duration consistent with individual patient treatment goals [see Warnings and Precautions (5)].
After observing the response to initial therapy with CALDOLOR, the dose and frequency should be adjusted to suit an individual patient's needs. Do not exceed 3200 mg total daily dose in adults. Do not exceed 40 mg/kg or 2,400 mg, whichever is less, total daily dose in pediatric patients less than 17 years of age.
To reduce the risk of renal adverse reactions, patients must be well hydrated prior to administration of CALDOLOR.
CALDOLOR injection 800 mg/8 mL (100 mg/mL) vials MUST BE DILUTED prior to administration.
Dilute to a final concentration of 4 mg/mL or less. Appropriate diluents include 0.9% Sodium Chloride Injection USP (normal saline), 5% Dextrose Injection USP (D5W), or Lactated Ringers Solution.
- 100 mg dose: Dilute 1 mL of CALDOLOR in at least 100 mL of diluent
- 200 mg dose: Dilute 2 mL of CALDOLOR in at least 100 mL of diluent
- 400 mg dose: Dilute 4 mL of CALDOLOR in at least 100 mL of diluent
- 800 mg dose: Dilute 8 mL of CALDOLOR in at least 200 mL of diluent
CALDOLOR injection 800 mg/200 mL (4 mg/mL) polypropylene flexible bags are ready to use, intended for 800 mg doses only.
For weight-based dosing at 10 mg/kg ensure that the concentration of CALDOLOR is 4 mg/mL or less.
Visually inspect parenteral drug products for particulate matter and discoloration prior to administration, whenever solution and container permit. If visibly opaque particles, discoloration or other foreign particulates are observed, the solution should not be used.
Diluted solutions are stable for up to 24 hours at ambient temperature (approximately 20° C to 25° C) and room lighting.
2.2 Adults
2.3 Pediatric Patients
Ages 12 to 17 years
The dose is 400 mg intravenously every 4 to 6 hours as necessary. Infusion time must be at least 10 minutes. Maximum daily dose is 2,400 mg.
Ages 6 months to 12 years
The dose is 10 mg/kg intravenously up to a maximum single dose of 400 mg every 4 to 6 hours as necessary. Infusion time must be at least 10 minutes. Maximum daily dose is 40 mg/kg or 2,400 mg, whichever is less.
Pediatric Dosing as Necessary for Fever and Pain * Maximum daily dose is 40 mg/kg or 2,400 mg, whichever is less
Age Group Dose Dosing Interval Min infusion time Max daily dose 6 months to less than 12 years 10 mg/kg up to 400 mg max Every 4 to 6 hours as necessary 10 minutes *40 mg/Kg or 2,400 mg 12 to 17 years 400 mg Every 4 to 6 hours as necessary 10 minutes 2,400 mg - 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
CALDOLOR is contraindicated in the following patients:
- Known hypersensitivity (e.g., anaphylactic reactions and serious skin reactions) to ibuprofen or any components of the drug product [see Warnings and Precautions (5.7, 5.9)]
- History of asthma, urticaria, or other allergic-type reactions after taking aspirin or other NSAIDs. Severe, sometimes fatal, anaphylactic reactions to NSAIDs have been reported in such patients [see Warnings and Precautions (5.7, 5.8)]
- In the setting of coronary artery bypass graft (CABG) surgery [see Warnings and Precautions (5.1)]
-
5 WARNINGS AND PRECAUTIONS
5.1 Cardiovascular Thrombotic Events
Clinical trials of several COX-2 selective and nonselective NSAIDs of up to three years duration have shown an increased risk of serious cardiovascular (CV) thrombotic events, including myocardial infarction (MI) and stroke, which can be fatal. Based on available data, it is unclear that the risk for CV thrombotic events is similar for all NSAIDs. The relative increase in serious CV thrombotic events over baseline conferred by NSAID use appears to be similar in those with and without known CV disease or risk factors for CV disease. However, patients with known CV disease or risk factors had a higher absolute incidence of excess serious CV thrombotic events, due to their increased baseline rate. Some observational studies found that this increased risk of serious CV thrombotic events began as early as the first weeks of treatment. The increase in CV thrombotic risk has been observed most consistently at higher doses.
To minimize the potential risk for an adverse CV event in NSAID-treated patients, use the lowest effective dose for the shortest duration possible. Physicians and patients should remain alert for the development of such events, throughout the entire treatment course, even in the absence of previous CV symptoms. Patients should be informed about the symptoms of serious CV events and the steps to take if they occur.
There is no consistent evidence that concurrent use of aspirin mitigates the increased risk of serious CV thrombotic events associated with NSAID use. The concurrent use of aspirin and an NSAID, such as ibuprofen, increases the risk of serious gastrointestinal (GI) events [see Warnings and Precautions (5.2)].
Status Post Coronary Artery Bypass Graft (CABG) Surgery
Two large, controlled clinical trials of a COX-2 selective NSAID for the treatment of pain in the first 10-14 days following CABG surgery found an increased incidence of myocardial infarction and stroke. NSAIDs are contraindicated in the setting of CABG [see Contraindications (4)].
Post-MI Patients
Observational studies conducted in the Danish National Registry have demonstrated that patients treated with NSAIDs in the post-MI period were at increased risk of reinfarction, CV-related death, and all-cause mortality beginning in the first week of treatment. In this same cohort, the incidence of death in the first year post-MI was 20 per 100 person years in NSAID-treated patients compared to 12 per 100 person years in non-NSAID exposed patients. Although the absolute rate of death declined somewhat after the first year post-MI, the increased relative risk of death in NSAID users persisted over at least the next four years of follow-up.
Avoid the use of CALDOLOR in patients with a recent MI unless the benefits are expected to outweigh the risk of recurrent CV thrombotic events. If CALDOLOR is used in patients with a recent MI, monitor patients for signs of cardiac ischemia.
5.2 Gastrointestinal Bleeding, Ulceration, and Perforation
NSAIDs, including ibuprofen, cause serious gastrointestinal (GI) adverse events including inflammation, bleeding, ulceration, and perforation of the esophagus, stomach, small intestine, or large intestine, which can be fatal. These serious adverse events can occur at any time, with or without warning symptoms, in patients treated with NSAIDs. Only one in five patients who develop a serious upper GI adverse event on NSAID therapy is symptomatic. Upper GI ulcers, gross bleeding, or perforation caused by NSAIDs occurred in approximately 1% of patients treated for 3-6 months and in about 2%-4% of patients treated for one year. However, even short-term therapy is not without risk.
Risk Factors for GI Bleeding, Ulceration and Perforation
Patients with a prior history of peptic ulcer disease and/or GI bleeding who used NSAIDs had a greater than 10-fold increased risk for developing a GI bleed compared to patients without these risk factors. Other factors that increase the risk of GI bleeding in patients treated with NSAIDs include longer duration of NSAID therapy; concomitant use of oral corticosteroids, aspirin, anticoagulants, or selective serotonin reuptake inhibitors (SSRIs); smoking; use of alcohol; older age; and poor general health status. Most postmarketing reports of fatal GI events occurred in elderly or debilitated patients. Additionally, patients with advanced liver disease and/or coagulopathy are at increased risk for GI bleeding.
Strategies to Minimize the GI Risks in NSAID-treated patients:
- Use the lowest effective dosage for the shortest possible duration.
- Avoid administration of more than one NSAID at a time.
- Avoid use in patients at higher risk unless benefits are expected to outweigh the increased risk of bleeding. For such patients, as well as those with active GI bleeding, consider alternate therapies other than NSAIDs.
- Remain alert for signs and symptoms of GI ulceration and bleeding during NSAID therapy.
- If a serious GI adverse event is suspected, promptly initiate evaluation and treatment, and discontinue CALDOLOR until a serious GI adverse event is ruled out.
- In the setting of concomitant use of low-dose aspirin for cardiac prophylaxis, monitor patients more closely for evidence of GI bleeding [see Drug Interactions (7)].
5.3 Hepatotoxicity
Elevations of ALT or AST (three or more times the upper limit of normal [ULN]) have been reported in approximately 1% of NSAID-treated patients in clinical trials. In addition, rare, sometimes fatal, cases of severe hepatic injury, including fulminant hepatitis, liver necrosis, and hepatic failure have been reported.
Elevations of ALT or AST (less than three times ULN) may occur in up to 15% of patients treated with NSAIDs, including ibuprofen.
Inform patients of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, diarrhea, pruritus, jaundice, right upper quadrant tenderness, and "flu-like" symptoms). If clinical signs and symptoms consistent with liver disease develop, or if systemic manifestations occur (e.g., eosinophilia, rash, etc.), discontinue CALDOLOR immediately, and perform a clinical evaluation of the patient.
5.4 Hypertension
NSAIDs, including CALDOLOR, can lead to new onset of hypertension or worsening of preexisting hypertension, either of which may contribute to the increased incidence of CV events. Patients taking angiotensin converting enzyme (ACE) inhibitors, thiazide diuretics, or loop diuretics may have impaired response to these therapies when taking NSAIDs [see Drug Interactions (7)].
Monitor blood pressure (BP) during the initiation of NSAID treatment and throughout the course of therapy.
5.5 Heart Failure and Edema
The Coxib and traditional NSAID Trialists' Collaboration meta-analysis of randomized controlled trials demonstrated an approximately two-fold increase in hospitalizations for heart failure in COX-2 selective-treated patients and nonselective NSAID-treated patients compared to placebo-treated patients. In a Danish National Registry study of patients with heart failure, NSAID use increased the risk of MI, hospitalization for heart failure, and death.
Additionally, fluid retention and edema have been observed in some patients treated with NSAIDs. Use of ibuprofen may blunt the CV effects of several therapeutic agents used to treat these medical conditions (e.g., diuretics, ACE inhibitors, or angiotensin receptor blockers [ARBs]) [see Drug Interactions (7)].
Avoid the use of CALDOLOR in patients with severe heart failure unless the benefits are expected to outweigh the risk of worsening heart failure. If CALDOLOR is used in patients with severe heart failure, monitor patients for signs of worsening heart failure.
5.6 Renal Toxicity and Hyperkalemia
Renal Toxicity
Long-term administration of NSAIDs has resulted in renal papillary necrosis and other renal injury.
Renal toxicity has also been seen in patients in whom renal prostaglandins have a compensatory role in the maintenance of renal perfusion. In these patients, administration of an NSAID may cause a dose dependent reduction in prostaglandin formation and, secondarily, in renal blood flow, which may precipitate overt renal decompensation. Patients at greatest risk of this reaction are those with impaired renal function, dehydration, hypovolemia, heart failure, liver dysfunction, those taking diuretics and ACE inhibitors or ARBs, and the elderly. Discontinuation of NSAID therapy is usually followed by recovery to the pretreatment state.
No information is available from controlled clinical studies regarding the use of CALDOLOR in patients with advanced renal disease. The renal effects of CALDOLOR may hasten the progression of renal dysfunction in patients with preexisting renal disease.
Correct volume status in dehydrated or hypovolemic patients prior to initiating CALDOLOR. Monitor renal function in patients with renal or hepatic impairment, heart failure, dehydration, or hypovolemia during use of CALDOLOR [see Drug Interactions (7)]. Avoid the use of CALDOLOR in patients with advanced renal disease unless the benefits are expected to outweigh the risk of worsening renal function. If CALDOLOR is used in patients with advanced renal disease, monitor patients for signs of worsening renal function.
5.7 Anaphylactic Reactions
Ibuprofen has been associated with anaphylactic reactions in patients with and without known hypersensitivity to ibuprofen and in patients with aspirin-sensitive asthma [see Contraindications (4) and Warnings and Precautions (5.8)].
Seek emergency help if anaphylactic reaction occurs.
5.8 Exacerbation of Asthma Related to Aspirin Sensitivity
A subpopulation of patients with asthma may have aspirin-sensitive asthma which may include chronic rhinosinusitis complicated by nasal polyps; severe, potentially fatal bronchospasm; and/or intolerance to aspirin and other NSAIDs. Because cross-reactivity between aspirin and other NSAIDs has been reported in such aspirin-sensitive patients, CALDOLOR is contraindicated in patients with this form of aspirin sensitivity [see Contraindications (4)]. When CALDOLOR is used in patients with preexisting asthma (without known aspirin sensitivity), monitor patients for changes in the signs and symptoms of asthma.
5.9 Serious Skin Reactions
NSAIDs, including ibuprofen, can cause serious skin adverse reactions such as exfoliative dermatitis, Stevens-Johnson Syndrome (SJS), and toxic epidermal necrolysis (TEN), which can be fatal. These serious events may occur without warning. Inform patients about the signs and symptoms of serious skin reactions, and to discontinue the use of CALDOLOR at the first appearance of skin rash or any other sign of hypersensitivity. CALDOLOR is contraindicated in patients with previous serious skin reactions to NSAIDs [see Contraindications (4)].
5.10 Premature Closure of Fetal Ductus Arteriosus
Ibuprofen may cause premature closure of the fetal ductus arteriosus. Avoid use of NSAIDs, including CALDOLOR, in pregnant women starting at 30 weeks of gestation (third trimester) [see Use in Specific Populations (8.1)].
5.11 Hematologic Toxicity
Anemia has occurred in NSAID-treated patients. This may be due to occult or gross GI blood loss, fluid retention, or an incompletely described effect on erythropoiesis. If a patient treated with CALDOLOR has any signs or symptoms of anemia, monitor hemoglobin or hematocrit.
NSAIDs, including CALDOLOR may increase the risk of bleeding events. Co-morbid conditions such as coagulation disorder, concomitant use of warfarin, other anticoagulants, antiplatelet agents (e.g., aspirin), serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs) may increase this risk. Monitor these patients for signs of bleeding [see Drug Interactions (7)].
CALDOLOR must be diluted prior to use. Infusion of the drug product without dilution can cause hemolysis [see Dosage and Administration (2.3)].
5.12 Masking of Inflammation and Fever
The pharmacological activity of CALDOLOR in reducing inflammation, and possibly fever, may diminish the utility of diagnostic signs in detecting infections.
5.13 Laboratory Monitoring
Because serious GI bleeding, hepatotoxicity, and renal injury can occur without warning symptoms or signs, consider monitoring patients on long-term NSAID treatment with a CBC and a chemistry profile periodically [see Warnings and Precautions (5.2, 5.3, 5.6)].
5.14 Ophthalmological Effects
Blurred or diminished vision, scotomata, and changes in color vision have been reported with oral ibuprofen. Discontinue ibuprofen if a patient develops such complaints, and refer the patient for an ophthalmologic examination that includes central visual fields and color vision testing.
5.15 Aseptic Meningitis
Aseptic meningitis with fever and coma has been observed in patients on oral ibuprofen therapy. Although it is probably more likely to occur in patients with systemic lupus erythematosus and related connective tissue diseases, it has been reported in patients who do not have underlying chronic disease. If signs or symptoms of meningitis develop in a patient on ibuprofen, give consideration to whether or not the signs or symptoms are related to ibuprofen therapy.
-
6 ADVERSE REACTIONS
The following serious adverse reactions are discussed in greater detail in other sections of the labeling:
- Cardiovascular Thrombotic Events [see Warnings and Precautions (5.1)]
- GI Bleeding, Ulceration and Perforation [see Warnings and Precautions (5.2)]
- Hepatotoxicity [see Warnings and Precautions (5.3)]
- Hypertension [see Warnings and Precautions (5.4)]
- Heart Failure and Edema [see Warnings and Precautions (5.5)]
- Renal Toxicity and Hyperkalemia [see Warnings and Precautions (5.6)]
- Anaphylactic reactions [see Warnings and Precautions (5.7)]
- Serious Skin Reactions [see Warnings and Precautions (5.9)]
- Hematologic Toxicity [see Warnings and Precautions (5.11)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be compared directly to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adult Population
During clinical development, 560 patients were exposed to CALDOLOR, 438 in pain and 122 with fever. In the pain studies, CALDOLOR was started intra-operatively and administered at a dose of 400 mg or 800 mg every six hours for up to three days. In the fever studies, CALDOLOR was administered at doses of 100 mg, 200 mg, or 400 mg every four or six hours for up to 3 days. The most frequent type of adverse reaction occurring with oral ibuprofen is gastrointestinal.
Pain Studies
The incidence rates of adverse reactions listed in the following table were derived from multi-center, controlled clinical studies in post-operative patients comparing CALDOLOR to placebo in patients also receiving morphine as needed for post-operative pain.
Table 1: Post-operative Patients with Adverse Reactions Observed in ≥ 3% of Patients in any CALDOLOR Treatment Group in Pain Studies* * All patients received concomitant morphine during these studies.
Event CALDOLOR Placebo
(N=287)400 mg
(N=134)800 mg
(N=304)Any Reaction 118 (88%) 260 (86%) 258 (90%) Nausea 77 (57%) 161 (53%) 179 (62%) Vomiting 30 (22%) 46 (15%) 50 (17%) Flatulence 10 (7%) 49 (16%) 44 (15%) Headache 12 (9%) 35 (12%) 31 (11%) Hemorrhage 13 (10%) 13 (4%) 16 (6%) Dizziness 8 (6%) 13 (4%) 5 (2%) Edema peripheral 1 (<1%) 9 (3%) 4 (1%) Urinary retention 7 (5%) 10 (3%) 10 (3%) Anemia 5 (4%) 7 (2%) 6 (2%) Decreased hemoglobin 4 (3%) 6 (2%) 3 (1%) Dyspepsia 6 (4%) 4 (1%) 2 (<1%) Wound hemorrhage 4 (3%) 4 (1%) 4 (1%) Abdominal discomfort 4 (3%) 2 (<1%) 0 Cough 4 (3%) 2 (<1%) 1 (<1%) Hypokalemia 5 (4%) 3 (<1%) 8 (3%) Fever Studies
Fever studies were conducted in febrile hospitalized patients with malaria and febrile hospitalized patients with varying causes of fever. In hospitalized febrile patients with malaria, the adverse reactions observed in at least two CALDOLOR-treated patients included abdominal pain and nasal congestion.
In hospitalized febrile patients (all causes), adverse reactions observed in more than two patients in any given treatment group are presented in the table below.
Table 2: Patients with Adverse Reactions Observed in ≥ 3% of Patients in any CALDOLOR Treatment Group in All-Cause Fever Study Event CALDOLOR Placebo
N=28100 mg
N=30200 mg
N=30400 mg
N=31Any Reaction 27 (87%) 25 (83%) 23 (74%) 25 (89%) Anemia 5 (17%) 6 (20%) 11 (36%) 4 (14%) Eosinophilia 7 (23%) 7 (23%) 8 (26%) 7 (25%) Hypokalemia 4 (13%) 4 (13%) 6 (19%) 5 (18%) Hypoproteinemia 3 (10%) 0 4 (13%) 2 (7%) Neutropenia 2 (7%) 2 (7%) 4 (13%) 2 (7%) Blood urea increased 0 0 3 (10%) 0 Hypernatremia 2 (7%) 0 3 (10%) 0 Hypertension 0 0 3 (10%) 0 Hypoalbuminemia 3 (10%) 1 (3%) 3 (10%) 1 (4%) Hypotension 0 2 (7%) 3 (10%) 1 (4%) Diarrhea 3 (10%) 3 (10%) 2 (7%) 2 (7%) Pneumonia bacterial 3 (10%) 1 (3%) 2 (7%) 0 Blood LDH increased 3 (10%) 2 (7%) 1 (3%) 1 (4%) Thrombocythemia 3 (10%) 2 (7%) 1 (3%) 0 Bacteremia 4 (13%) 0 0 0 Pediatric Population
A total of 143 pediatric patients ages 6 months and older have received CALDOLOR in controlled clinical trials. The most common adverse reactions (incidence greater than or equal to 2%) in pediatric patients treated with CALDOLOR were infusion site pain, vomiting, nausea, anemia and headache.
-
7 DRUG INTERACTIONS
See Table 3 for clinically significant drug interactions with ibuprofen.
Table 3: Clinically Significant Drug Interactions with Ibuprofen Drugs That Interfere with Hemostasis Clinical Impact: - Ibuprofen and anticoagulants such as warfarin have a synergistic effect on bleeding. The concomitant use of ibuprofen and anticoagulants have an increased risk of serious bleeding compared to the use of either drug alone.
- Serotonin release by platelets plays an important role in hemostasis. Case-control and cohort epidemiological studies showed that concomitant use of drugs that interfere with serotonin reuptake and an NSAID may potentiate the risk of bleeding more than an NSAID alone.
Intervention: Monitor patients with concomitant use of CALDOLOR with anticoagulants (e.g., warfarin), antiplatelet agents (e.g., aspirin), selective serotonin reuptake inhibitors (SSRIs), and serotonin norepinephrine reuptake inhibitors (SNRIs) for signs of bleeding [see Warnings and Precautions (5.11)]. Aspirin Clinical Impact: Controlled clinical studies showed that the concomitant use of NSAIDs and analgesic doses of aspirin does not produce any greater therapeutic effect than the use of NSAIDs alone. In a clinical study, the concomitant use of an NSAID and aspirin was associated with a significantly increased incidence of GI adverse reactions as compared to use of the NSAID alone [see Warnings and Precautions (5.2)]. Intervention: Concomitant use of CALDOLOR and analgesic doses of aspirin is not generally recommended because of the increased risk of bleeding [see Warnings and Precautions (5.11)].
CALDOLOR is not a substitute for low dose aspirin for cardiovascular protection.ACE Inhibitors, Angiotensin Receptor Blockers, and Beta-Blockers Clinical Impact: - NSAIDs may diminish the antihypertensive effect of angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), or beta-blockers (including propranolol).
- In patients who are elderly, volume-depleted (including those on diuretic therapy), or have renal impairment, co-administration of an NSAID with ACE inhibitors or ARBs may result in deterioration of renal function, including possible acute renal failure. These effects are usually reversible.
Intervention: - During concomitant use of CALDOLOR and ACE-inhibitors, ARBs, or beta- blockers, monitor blood pressure to ensure that the desired blood pressure is obtained.
- During concomitant use of CALDOLOR and ACE-inhibitors or ARBs in patients who are elderly, volume-depleted, or have impaired renal function, monitor for signs of worsening renal function [see Warnings and Precautions (5.6)].
- When these drugs are administered concomitantly, patients should be adequately hydrated. Assess renal function at the beginning of the concomitant treatment and periodically thereafter.
Diuretics Clinical Impact: Clinical studies, as well as post-marketing observations, showed that NSAIDs reduced the natriuretic effect of loop diuretics (e.g., furosemide) and thiazide diuretics in some patients. This effect has been attributed to the NSAID inhibition of renal prostaglandin synthesis. Intervention: During concomitant use of CALDOLOR with diuretics, observe patients for signs of worsening renal function, in addition to assuring diuretic efficacy including antihypertensive effects [see Warnings and Precautions (5.6)]. Digoxin Clinical Impact: The concomitant use of ibuprofen with digoxin has been reported to increase the serum concentration and prolong the half-life of digoxin. Intervention: During concomitant use of CALDOLOR and digoxin, monitor serum digoxin levels. Lithium Clinical Impact: NSAIDs have produced elevations in plasma lithium levels and reductions in renal lithium clearance. The mean minimum lithium concentration increased 15%, and the renal clearance decreased by approximately 20%. This effect has been attributed to NSAID inhibition of renal prostaglandin synthesis. Intervention: During concomitant use of CALDOLOR and lithium, monitor patients for signs of lithium toxicity. Methotrexate Clinical Impact: Concomitant use of NSAIDs and methotrexate may increase the risk for methotrexate toxicity (e.g., neutropenia, thrombocytopenia, renal dysfunction). Intervention: During concomitant use of CALDOLOR and methotrexate, monitor patients for methotrexate toxicity. Cyclosporine Clinical Impact: Concomitant use of CALDOLOR and cyclosporine may increase cyclosporine's nephrotoxicity. Intervention: During concomitant use of CALDOLOR and cyclosporine, monitor patients for signs of worsening renal function. NSAIDs and Salicylates Clinical Impact: Concomitant use of ibuprofen with other NSAIDs or salicylates (e.g., diflunisal, salsalate) increases the risk of GI toxicity, with little or no increase in efficacy [see Warnings and Precautions (5.2)]. Intervention: The concomitant use of ibuprofen with other NSAIDs or salicylates is not recommended. Pemetrexed Clinical Impact: Concomitant use of CALDOLOR and pemetrexed, may increase the risk of pemetrexed-associated myelosuppression, renal, and GI toxicity (see the pemetrexed prescribing information). Intervention: - During concomitant use of CALDOLOR and pemetrexed, in patients with renal impairment whose creatinine clearance ranges from 45 to 79 mL/min, monitor for myelosuppression, renal and GI toxicity.
- NSAIDs with short elimination half-lives (e.g., diclofenac, indomethacin) should be avoided for a period of two days before, the day of, and two days following administration of pemetrexed.
- In the absence of data regarding potential interaction between pemetrexed and NSAIDs with longer half-lives (e.g., meloxicam, nabumetone), patients taking these NSAIDs should interrupt dosing for at least five days before, the day of, and two days following pemetrexed administration.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Use of NSAIDs, including CALDOLOR, during the third trimester of pregnancy increases the risk of premature closure of the fetal ductus arteriosus. Avoid use of NSAIDs, including CALDOLOR, in pregnant women starting at 30 weeks gestation (third trimester).
There are no adequate and well-controlled studies of CALDOLOR in pregnant women. Data from observational studies regarding potential embryofetal risks of NSAID use in women in the first or second trimesters of pregnancy are inconclusive. In the general U.S. population, all clinically recognized pregnancies, regardless of drug exposure, have a background rate of 2-4% for major malformations, and 15-20% for pregnancy loss. In published animal reproduction studies, there were no clear developmental effects at doses up to 0.4-times the maximum recommended human dose (MRHD) in the rabbit and 0.5-times in the MRHD rat when dosed throughout gestation. In contrast, an increase in membranous ventricular septal defects was reported in rats treated on Gestation Days 9 & 10 with 0.8-times the MRHD. Based on animal data, prostaglandins have been shown to have an important role in endometrial vascular permeability, blastocyst implantation, and decidualization. In animal studies, administration of prostaglandin synthesis inhibitors such as ibuprofen, resulted in increased pre- and post-implantation loss. Advise a pregnant woman of the potential risk to a fetus.
Labor or Delivery
There are no studies on the effects of CALDOLOR during labor or delivery. In animal studies, NSAIDs, including ibuprofen, inhibit prostaglandin synthesis, cause delayed parturition, and increase the incidence of stillbirth.
Animal Data
In a published study, female rabbits given 7.5, 20, or 60 mg/kg ibuprofen (0.04, 0.12, or 0.36-times the maximum recommended human daily dose of 3200 mg of ibuprofen based on body surface area) from Gestation Days 1 to 29, no clear treatment-related adverse developmental effects were noted. This dose was associated with significant maternal toxicity (stomach ulcers, gastric lesions). In the same publication, female rats were administered 7.5, 20, 60, 180 mg/kg ibuprofen (0.02, 0.06, 0.18, 0.54-times the maximum daily dose) did not result in clear adverse developmental effects. Maternal toxicity (gastrointestinal lesions) was noted at 20 mg/kg and above.
In a published study, rats were orally dosed with 300 mg/kg ibuprofen (0.912-times the maximum human daily dose of 3200 mg based on body surface area) during Gestation Days 9 and 10 (critical time points for heart development in rats). Ibuprofen treatment resulted in an increase in the incidence of membranous ventricular septal defects. This dose was associated with significant maternal toxicity including gastrointestinal toxicity. One incidence each of a membranous ventricular septal defect and gastroschisis was noted in fetuses from rabbits treated with 500 mg/kg (3-times the maximum human daily dose) from Gestation Day 9-11.
8.2 Lactation
Risk Summary
No lactation studies have been conducted with CALDOLOR; however, limited published literature reports that, following oral administration, ibuprofen is present in human milk at relative infant doses of 0.06% to 0.6% of the maternal weight-adjusted daily dose. There are no reports of adverse effects on the breastfed infant and no effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for CALDOLOR and any potential adverse effects on the breastfed infant from the CALDOLOR or from the underlying maternal condition.
8.3 Females and Males of Reproductive Potential
Females
Based on the mechanism of action, the use of prostaglandin-mediated NSAIDs, including CALDOLOR, may delay or prevent rupture of ovarian follicles, which has been associated with reversible infertility in some women. Published animal studies have shown that administration of prostaglandin synthesis inhibitors has the potential to disrupt prostaglandin- mediated follicular rupture required for ovulation. Small studies in women treated with NSAIDs have also shown a reversible delay in ovulation. Consider withdrawal of NSAIDs, including CALDOLOR in women who have difficulties conceiving or who are undergoing investigation of infertility.
8.4 Pediatric Use
The safety and effectiveness of CALDOLOR for the treatment of pain and fever in pediatric patients ages 6 months and older is supported by evidence of fever reduction from a multi-center, open-label study of hospitalized febrile pediatric patients along with safety data from exposure to CALDOLOR in 143 pediatric patients ages 6 months and older in two pediatric fever studies and one pediatric pain study, supportive data from other ibuprofen products approved in pediatric patients, and evidence from adequate and well controlled studies in adults. The effectiveness of CALDOLOR for the treatment of pain and fever has not been studied in pediatric patients less than 6 months of age. [see DOSAGE AND ADMINISTRATION (2), Clinical Study Experience (6.1), Pharmacokinetics (12.3), CLINICAL STUDIES (14)].
8.5 Geriatric Use
Elderly patients, compared to younger patients, are at greater risk for NSAID-associated serious cardiovascular, gastrointestinal, and/or renal adverse reactions. If the anticipated benefit for the elderly patient outweighs these potential risks, start dosing at the low end of the dosing range, and monitor patients for adverse effects [see Warnings and Precautions (5.1, 5.2, 5.3, 5.6, 5.13)].
Clinical studies of CALDOLOR did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy. Elderly patients are at increased risk for serious GI adverse events.
-
10 OVERDOSAGE
Symptoms following acute NSAID overdosages have been typically limited to lethargy, drowsiness, nausea, vomiting, and epigastric pain, which have been generally reversible with supportive care. Gastrointestinal bleeding has occurred. Hypertension, acute renal failure, respiratory depression, and coma have occurred, but were rare [see Warnings and Precautions (5.1, 5.2, 5.4, 5.6)].
Manage patients with symptomatic and supportive care following an NSAID overdosage. There are no specific antidotes. Forced diuresis, alkalinization of urine, hemodialysis, or hemoperfusion may not be useful due to high protein binding.
For additional information about overdosage treatment contact a poison control center at 1-800-222-1222.
-
11 DESCRIPTION
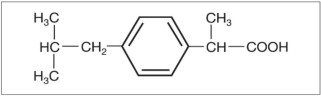
CALDOLOR (ibuprofen) Injection is a nonsteroidal anti-inflammatory drug, available as an 800 mg/8 mL single dose vial (100 mg/mL) and 800 mg/200 mL (4 mg/mL) polypropylene, single dose, ready-to-use, flexible bag for intravenous administration. The chemical name is ibuprofen, which is (±)-2-(p-isobutylphenyl) propionic acid. Ibuprofen is a white powder with a melting point of 74°C to 77°C. It has a molecular weight of 206.28. It is very slightly soluble in water (<1 mg/mL) and readily soluble in organic solvents such as ethanol and acetone. The structural formula of ibuprofen is represented below:
800 mg/8 mL vial: Each 1 mL of solution contains 100 mg of ibuprofen in Water for Injection, USP. The inactive ingredients in CALDOLOR include: 78 mg/mL arginine at a molar ratio of 0.92:1 arginine:ibuprofen. The solution pH is about 7.4.
800 mg/200 mL polypropylene flexible bag: Each 1 mL of solution contains 4 mg of ibuprofen in Water for Injection, USP. The inactive ingredients in CALDOLOR include: sodium phosphate, sodium hydroxide, and sodium chloride. The solution is iso-osmotic with an approximate pH of 7.4.
CALDOLOR is sterile and is intended for intravenous administration only.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Ibuprofen has analgesic, anti-inflammatory, and antipyretic properties.
The mechanism of action of CALDOLOR, like that of other NSAIDs, is not completely understood but involves inhibition of cyclooxygenase (COX-1 and COX-2).
Ibuprofen is a potent inhibitor of prostaglandin synthesis in vitro. Ibuprofen concentrations reached during therapy have produced in vivo effects. Prostaglandins sensitize afferent nerves and potentiate the action of bradykinin in inducing pain in animal models. Prostaglandins are mediators of inflammation. Because ibuprofen is an inhibitor of prostaglandin synthesis, its mode of action may be due to a decrease of prostaglandins in peripheral tissues.
12.3 Pharmacokinetics
Ibuprofen is a racemic mixture of [-]R- and [+]S-isomers. In vivo and in vitro studies indicate that the [+]S-isomer is responsible for clinical activity. The [-]R-form, while thought to be pharmacologically inactive, is slowly and incompletely (~60%) interconverted into the active [+]S species in adults. The [-]R-isomer serves as a circulating reservoir to maintain levels of active drug. The pharmacokinetic parameters of CALDOLOR determined in a study with volunteers are presented below.
Table 4: Pharmacokinetic Parameters of Intravenous Ibuprofen AUC = Area-under-the-curve
Cmax = Peak plasma concentration
CV = Coefficient of Variation
KEL = First-order elimination rate constant
T1/2 = Elimination half-life
* = 60 minute infusion time
400 mg* CALDOLOR
Mean (CV%)800 mg* CALDOLOR
Mean (CV%)Number of Patients 12 12 AUC (mcg·h/mL) 109.3 (26.4) 192.8 (18.5) Cmax (mcg/mL) 39.2 (15.5) 72.6 (13.2) KEL (1/h) 0.32 (17.9) 0.29 (12.8) T1/2 (h) 2.22 (20.1) 2.44 (12.9) The pharmacokinetic parameters of CALDOLOR determined in a study with febrile pediatric patients are presented in Table 5. It was observed that the median Tmax was at the end of the infusion and that CALDOLOR had a shorter elimination half-life in pediatric patients compared to adults. The volume of distribution and clearance increased with age.
Table 5: Pharmacokinetic Parameters of 10 mg/kg Intravenous Ibuprofen, Pediatric Patients, by Age Group *Median (minimum-maximum)
#WT: body weight (kg)
6 months to
<2 years
Mean (CV%)2 years to
<6 years
Mean (CV%)6 years to
16 years
Mean (CV%)Number of Patients 5 12 25 AUC (mcg·h/mL) 71.1 (37.1) 79.2 (37.0) 80.7 (36.9) Cmax (mcg/mL) 59.2 (34.8) 64.2 (34.3) 61.9 (26.6) Tmax (min)* 10 (10-30) 12 (10-46) 10 (10-40) T1/2 (h) 1.8 (29.9) 1.5 (41.8) 1.55 (26.4) Cl (mL/h) 1172.5 (38.9) 1967.3 (56.0) 4878.5 (71.0) Vz (mL) 2805.7 (20.1) 3695.8 (30.0) 10314.2 (67.4) Cl/WT# (mL/hr/kg) 133.7 (58.6) 130.1 (82.4) 109.2 (41.6) Vz/WT# (mL/kg) 311.2 (35.4) 227.2 (41.7) 226.8 (30.4) Ibuprofen, like most NSAIDs, is highly protein bound (>99% bound at 20 mcg/mL). Protein binding is saturable, and at concentrations >20 mcg/mL binding is nonlinear. Based on oral dosing data, there is an age- or fever-related change in volume of distribution for ibuprofen.
Drug Interaction Studies
Aspirin: When NSAIDs were administered with aspirin, the protein binding of NSAIDs were reduced, although the clearance of free NSAID was not altered. The clinical significance of this interaction is not known. See Table 3 for clinically significant drug interactions of NSAIDs with aspirin [see Drug Interactions (7)].
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Long-term studies in animals to evaluate the carcinogenic potential of ibuprofen have not been conducted.
Mutagenesis
In published studies, ibuprofen was not mutagenic in the in vitro bacterial reverse mutation assay (Ames assay).
Impairment of Fertility
In a published study, dietary administration of ibuprofen to male and female rats 8-weeks prior to and during mating at dose levels of 20 mg/kg (0.06-times the MRHD based on body surface area comparison) did not impact male or female fertility or litter size.
In other studies, adult mice were administered ibuprofen intraperitoneally at a dose of 5.6 mg/kg/day (0.0085-times the MRHD based on body surface area comparison) for 35 or 60 days in males and 35 days in females. There was no effect on sperm motility or viability in males but decreased ovulation was reported in females.
-
14 CLINICAL STUDIES
14.1 Analgesia (Pain)
The effect of CALDOLOR on acute pain was evaluated in two multi-center, randomized, double-blind, placebo-controlled studies.
In a study of women who had undergone an elective abdominal hysterectomy, 319 patients were randomized and treated with CALDOLOR 800 mg or placebo administered every 6 hours (started intra-operatively) and morphine administered on an as needed basis. Efficacy was demonstrated as a statistically significant greater reduction in the mean morphine consumption through 24 hours in patients who received CALDOLOR as compared to those receiving placebo (47 mg and 56 mg, respectively). The clinical relevance of this finding is supported by a greater reduction in pain intensity over 24 hours for patients treated with CALDOLOR, even though morphine was available on an as needed basis.
In a study of patients who had undergone an elective abdominal or orthopedic surgery, 406 patients (87 men, 319 women) were randomized to receive CALDOLOR 400 mg, CALDOLOR 800 mg, or placebo administered every 6 hours (started intra-operatively), and morphine on an as needed basis. This study failed to demonstrate a statistically significant difference in outcome between patients receiving CALDOLOR 800 mg or 400 mg and placebo, although there were trends favoring the active treatments.
14.2 Antipyretic (Fever)
The effect of CALDOLOR on fever was evaluated in two randomized, double-blind studies in adults and in one open-label study in pediatric patients.
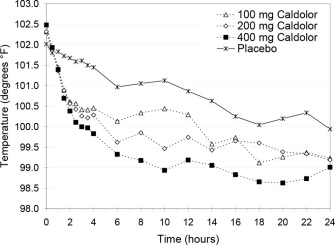
In a multi-center study, 120 hospitalized patients (88 men, 32 women) with temperatures of 101°F or greater were randomized to CALDOLOR 400 mg, 200 mg, 100 mg or placebo, administered every 4 hours for 24 hours. Each of the three CALDOLOR doses, 100 mg, 200 mg, and 400 mg, resulted in a statistically greater percentage of patients with a reduced temperature (<101°F) after 4 hours, compared to placebo (65%, 73%, 77% and 32%, respectively). The dose response is shown in the figure below.
Figure 1: Temperature Reduction by Treatment Group, Hospitalized Febrile Patients
In a single-center study, 60 hospitalized patients (48 men, 12 women) with uncomplicated P. falciparum malaria having temperatures ≥100.4°F were randomized to CALDOLOR 400 mg or placebo, administered every 6 hours for 72 hours of treatment. There was a significant reduction in fever within the first 24 hours of treatment, measured as the area above the temperature 98.6°F vs. time curve for patients treated with CALDOLOR.
In a multi-center, open-label study, 100 hospitalized pediatric patients 6 months of age and older with temperatures of 101.0ºF or greater were randomized and treated with 10 mg/kg of CALDOLOR or a low dose of an active comparator every 4 hours as needed for fever.
Efficacy was demonstrated as a statistically significant greater reduction in temperature for the primary endpoint, an area under the curve analyses of temperature versus time for the first 2 hours, as well as over the entire dosing interval. Seventy-four percent of CALDOLOR treated patients became afebrile (temperature <99.5ºF) by the end of first dosing interval.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
CALDOLOR (ibuprofen) Injection is a clear, colorless, non-pyrogenic, aqueous solution supplied as follows:
- 800 mg/8 mL (100 mg/mL) single dose vial. Carton of 25 vials, NDC: 66220-287-08
- 800 mg/200 mL (4 mg/mL) single dose, ready-to-use polypropylene flexible bag. Case of 20 bags, NDC: 66220-284-22. Individual bag, NDC: 66220-284-11.
Storage
Store at controlled room temperature 20 °C to 25 °C (68 °F to 77 °F); excursions permitted between 15 °C to 30 °C (59 °F to 86 °F) [see USP Controlled Room Temperature]. Discard the unused portion.
The stopper in the CALDOLOR vial does not contain natural rubber latex, dry natural rubber, or blends of natural rubber.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide) that accompanies each prescription dispensed. Patients, families, or their caregivers should be informed of the following information before initiating therapy with CALDOLOR and periodically during the course of ongoing therapy.
Cardiovascular Thrombotic Events
Advise patients to be alert for the symptoms of cardiovascular thrombotic events, including chest pain, shortness of breath, weakness, or slurring of speech, and to report any of these symptoms to their health care provider immediately [see Warnings and Precautions (5.1)].
Gastrointestinal Bleeding, Ulceration, and Perforation
Advise patients to report symptoms of ulcerations and bleeding, including epigastric pain, dyspepsia, melena, and hematemesis to their health care provider. In the setting of concomitant use of low-dose aspirin for cardiac prophylaxis, inform patients of the increased risk for and the signs and symptoms of GI bleeding [see Warnings and Precautions (5.2)].
Hepatotoxicity
Inform patients of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, pruritus, diarrhea, jaundice, right upper quadrant tenderness, and “flu-like” symptoms). If these occur, instruct patients to stop CALDOLOR and seek immediate medical therapy [see Warnings and Precautions (5.3)].
Heart Failure and Edema
Advise patients to be alert for the symptoms of congestive heart failure including shortness of breath, unexplained weight gain, or edema and to contact their healthcare provider if such symptoms occur [see Warnings and Precautions (5.5)].
Anaphylactic Reactions
Inform patients of the signs of an anaphylactic reaction (e.g., difficulty breathing, swelling of the face or throat). Instruct patients to seek immediate emergency help if these occur [see Contraindications (4) and Warnings and Precautions (5.7)].
Serious Skin Reactions
Advise patients to stop CALDOLOR immediately if they develop any type of rash and to contact their healthcare provider as soon as possible [see Warnings and Precautions (5.9)].
Female Fertility
Advise females of reproductive potential who desire pregnancy that NSAIDs, including CALDOLOR, may be associated with a reversible delay in ovulation [see Use in Specific Populations (8.3)]
Fetal Toxicity
Inform pregnant women to avoid use of CALDOLOR and other NSAIDs starting at 30 weeks gestation because of the risk of the premature closing of the fetal ductus arteriosus [see Warnings and Precautions (5.10) and Use in Specific Populations (8.1)].
Avoid Concomitant Use of NSAIDs
Inform patients that the concomitant use of CALDOLOR with other NSAIDs or salicylates (e.g., diflunisal, salsalate) is not recommended due to the increased risk of gastrointestinal toxicity, and little or no increase in efficacy [see Warnings and Precautions (5.2) and Drug Interactions (7)]. Alert patients that NSAIDs may be present in “over the counter” medications for treatment of colds, fever, or insomnia.
Use of NSAIDS and Low-Dose Aspirin
Inform patients not to use low-dose aspirin concomitantly with CALDOLOR until they talk to their healthcare provider [see Drug Interactions (7)].
Manufactured for:
Cumberland Pharmaceuticals Inc.
Nashville, TN 37203
US Patent Number 6,727,286, 8,871,810, 8,735,452, 9,012,508, 9,072,661, 9,072,710, 9,114,068, 9,138,404, 9,295,639, and 9,649,284
CALDOLOR® is a registered trademark of Cumberland Pharmaceuticals Inc. -
PRINCIPAL DISPLAY PANEL
Principal Display Panel - 8 mL Vial Label
NDC: 66220-287-08 Rx Only
Caldolor®
(ibuprofen) Injection800 mg/8 mL
(100 mg/mL)
FOR INTRAVENOUS USE. MUST DILUTE BEFORE USE.
Store at controlled room temperature,
20°C - 25°C (68° - 77°F).Single dose vial, discard unused portion.
DOSAGE: See package insert for dosage,
dilution, and administration information. -
PRINCIPAL DISPLAY PANEL
Principal Display Panel - 8 mL Carton Label
NDC: 66220-287-08
25 x 8 mL Vials
800 mg/8 mL
For Intravenous Use
Must Dilute Before Use
Caldolor®
(ibuprofen) Injection800 mg/8 mL
(100 mg/mL)
-
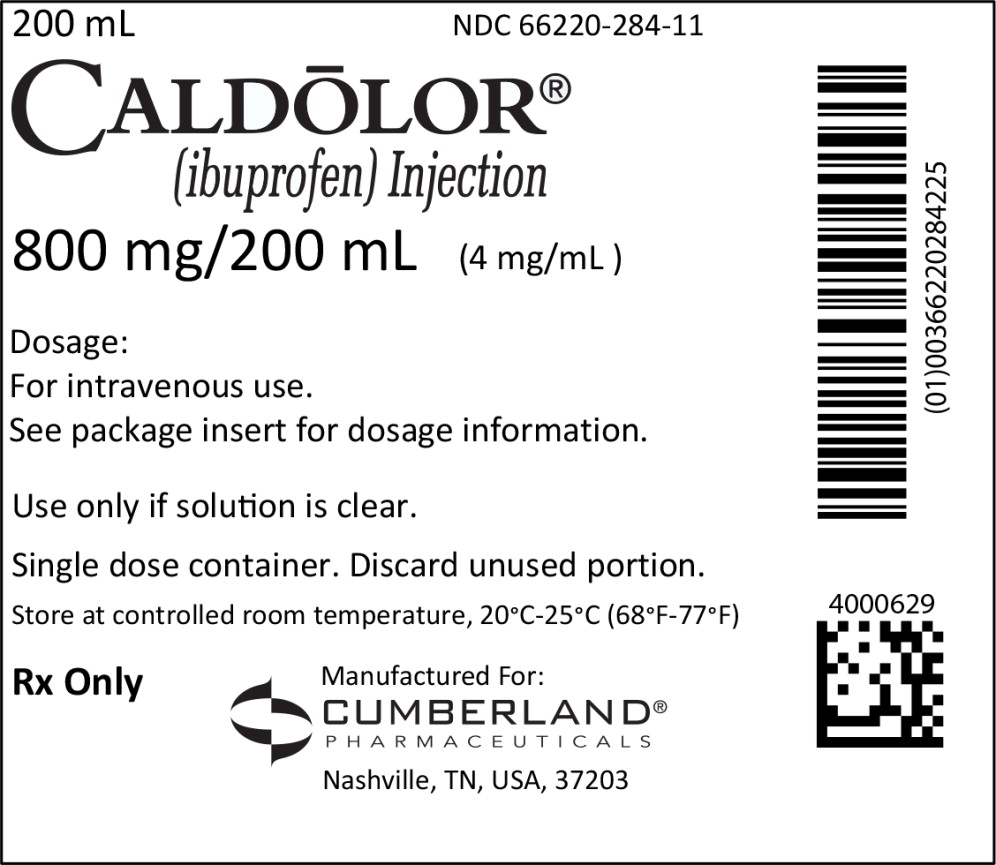
PRINCIPAL DISPLAY PANEL
Principal Panel Display – Bag Label
200 mL NDC: 66220-284-11
CALDOLOR®
(ibuprofen) Injection
800 mg/200 mL (4 mg/mL)
Dosage:
For intravenous use.
See package insert for dosage information.
Use only if solution is clear.
Single dose container. Discard unused portion.
Store at controlled room temperature, 20°C-25°C (68°F-77°F)
Rx Only
Manufactured For:
CUMBERLAND®
PHARMACEUTICALS
Nashville, TN, USA, 37203
-
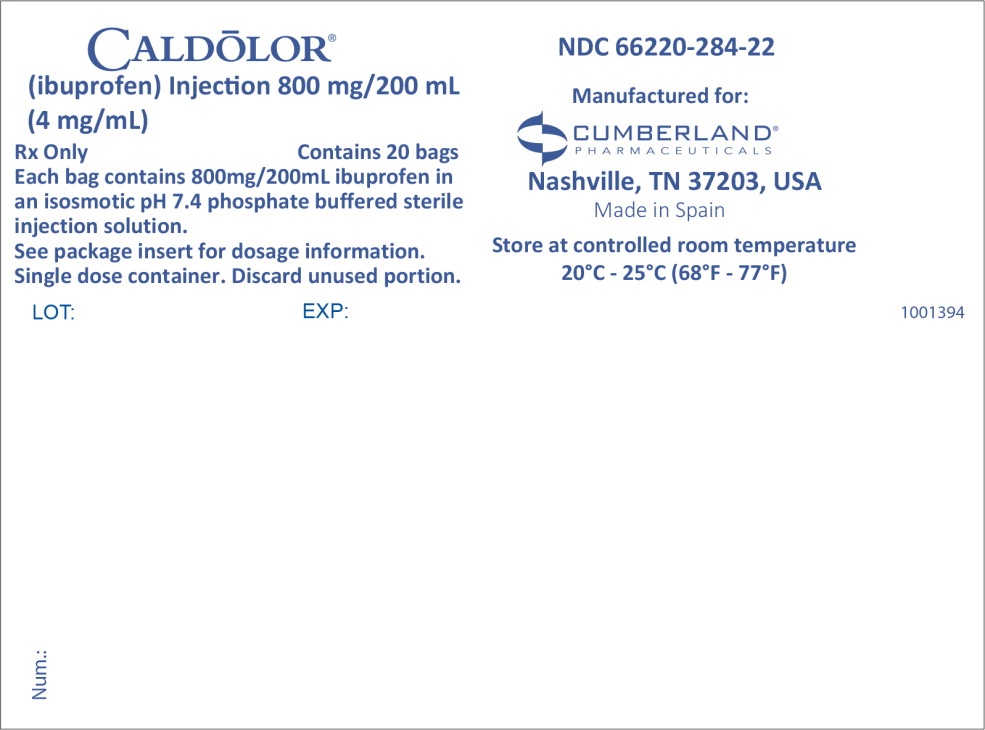
PRINCIPAL DISPLAY PANEL
Principal Panel Display – Case Label
CALDOLOR®
(ibuprofen) Injection 800 mg/200 mL
(4 mg/mL)
Rx Only Contains 20 bags
Each bag contains 800 mg/200 mL ibuprofen in
an isosmotic pH 7.4 phosphate buffered sterile
injection solution.See package insert for dosage information.
Single dose container. Discard unused portion.
LOT: EXP:
NDC: 66220-284-22
Manufactured For:
CUMBERLAND®
PHARMACEUTICALS
Nashville, TN, USA, 37203
Made in Spain
Store at controlled room temperature
20°C - 25°C (68°F - 77°F)
-
INGREDIENTS AND APPEARANCE
CALDOLOR
ibuprofen injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 66220-287 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ibuprofen (UNII: WK2XYI10QM) (ibuprofen - UNII:WK2XYI10QM) ibuprofen 800 mg in 8 mL Inactive Ingredients Ingredient Name Strength water (UNII: 059QF0KO0R) arginine (UNII: 94ZLA3W45F) hydrochloric acid (UNII: QTT17582CB) nitrogen (UNII: N762921K75) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 66220-287-08 25 in 1 CARTON 06/11/2009 1 8 mL in 1 VIAL; Type 0: Not a Combination Product 2 NDC: 66220-287-24 20 in 1 CASE 04/01/2019 09/03/2020 2 NDC: 66220-287-11 200 mL in 1 BAG; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA022348 06/11/2009 CALDOLOR
ibuprofen injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 66220-284 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ibuprofen (UNII: WK2XYI10QM) (ibuprofen - UNII:WK2XYI10QM) ibuprofen 800 mg in 200 mL Inactive Ingredients Ingredient Name Strength sodium phosphate, dibasic, unspecified form (UNII: GR686LBA74) water (UNII: 059QF0KO0R) sodium chloride (UNII: 451W47IQ8X) sodium hydroxide (UNII: 55X04QC32I) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 66220-284-22 20 in 1 CASE 01/01/2020 1 NDC: 66220-284-11 200 mL in 1 BAG; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA022348 01/01/2020 Labeler - Cumberland Pharmaceuticals Inc. (069532880)
Trademark Results [Caldolor]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 CALDOLOR 77559307 3659228 Live/Registered |
Cumberland Pharmaceuticals Inc. 2008-08-29 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.