PROMETHAZINE VC- promethazinehydrochloride and phenylephrine hydrochloride syrup
Promethazine VC by
Drug Labeling and Warnings
Promethazine VC by is a Prescription medication manufactured, distributed, or labeled by Preferred Pharmaceuticals, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
-
DESCRIPTION
Each 5 mL (one teaspoonful), for oral administration contains: Promethazine hydrochloride 6.25 mg; phenylephrine hydrochloride 5 mg. Alcohol 7%.
Inactive Ingredients: Apricot peach flavor, ascorbic acid, citric acid, FD&C yellow #6, menthol, methylparaben, propylene glycol, propylparaben, purified water, saccharin sodium, sodium benzoate, sodium citrate and sucrose.
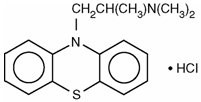
Promethazine hydrochloride, a phenothiazine derivative, is chemically designated as (±)-10-[2-(Dimethylamino)propyl] phenothiazine monohydrochloride.
Promethazine hydrochloride occurs as a white to faint yellow, practically odorless, crystalline powder which slowly oxidizes and turns blue on prolonged exposure to air. It is soluble in water and freely soluble in alcohol. It has a molecular weight of 320.88, a molecular formula of C17H20N2SHCI, and the following structural formula:
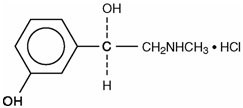
Phenylephrine hydrochloride is a sympathomimetic amine salt which is chemically designated as (-)-m-Hydroxy-α-[(methylamino)methyl] benzyl alcohol hydrochloride. It occurs as white or nearly white crystals, having a bitter taste. It is freely soluble in water and alcohol. Phenylephrine hydrochloride is subject to oxidation and must be protected from light and air. It has a molecular weight of 203.67, a molecular formula of C9H13NO2HCI, and the following structural formula:
-
CLINICAL PHARMACOLOGY
Promethazine:
Promethazine is a phenothiazine derivative which differs structurally from the antipsychotic phenothiazines by the presence of a branched side chain and no ring substitution. It is thought that this configuration is responsible for its relative lack (1/10 that of chlorpromazine) of dopamine antagonist properties.
Promethazine is an H1 receptor blocking agent. In addition to its antihistaminic action, it provides clinically useful sedative and antiemetic effects.
Promethazine is well absorbed from the gastrointestinal tract. Clinical effects are apparent within 20 minutes after oral administration and generally last four to six hours, although they may persist as long as 12 hours. Promethazine is metabolized by the liver to a variety of compounds; the sulfoxides of promethazine and N-demethylpromethazine are the predominant metabolites appearing in the urine.
Phenylephrine:
Phenylephrine is a potent postsynaptic α-receptor agonist with little effect on β-receptors of the heart. Phenylephrine has no effect on β-adrenergic receptors of the bronchi or peripheral blood vessels. A direct action at receptors accounts for the greater part of its effects, only a small part being due to its ability to release norepinephrine.
Therapeutic doses of phenylephrine mainly cause vasoconstriction. Phenylephrine increases resistance and, to a lesser extent, decreases capacitance of blood vessels. Total peripheral resistance is increased, resulting in increased systolic and diastolic blood pressure. Pulmonary arterial pressure is usually increased, and renal blood flow is usually decreased. Local vasoconstriction and hemostasis occur following topical application or infiltration of phenylephrine into tissues. The main effect of phenylephrine on the heart is bradycardia; it produces a positive inotropic effect on the myocardium in doses greater than those usually used therapeutically. Rarely, the drug may increase the irritability of the heart, causing arrhythmias. Cardiac output is decreased slightly. Phenylephrine increases the work of the heart by increasing peripheral arterial resistance.
Phenylephrine has a mild central stimulant effect.
Following oral administration or topical application of phenylephrine to the mucosa, constriction of blood vessels in the nasal mucosa relieves nasal congestion associated with allergy or head colds. Following oral administration, nasal decongestion may occur within 15 or 20 minutes and may persist for up to 4 hours.
Phenylephrine is irregularly absorbed from and readily metabolized in the gastrointestinal tract. Phenylephrine is metabolized in the liver and intestine by monoamine oxidase. The metabolites and their route and rate of excretion have not been identified. The pharmacologic action of phenylephrine is terminated at least partially by uptake of the drug into tissues.
- INDICATIONS AND USAGE
-
CONTRAINDICATIONS
Promethazine is contraindicated in comatose states, and in individuals known to be hypersensitive or to have had an idiosyncratic reaction to promethazine or to other phenothiazines.
Antihistamines are contraindicated for use in the treatment of lower respiratory tract symptoms, including asthma.
Phenylephrine is contraindicated in patients with hypertension or with peripheral vascular insufficiency (ischemia may result with risk of gangrene or thrombosis of compromised vascular beds). Phenylephrine should not be used in patients known to be hypersensitive to the drug or in those receiving a monoamine oxidase inhibitor (MAOI).
-
WARNINGS
WARNING:
PROMETHAZINE HYDROCHLORIDE SHOULD NOT BE USED IN PEDIATRIC PATIENTS LESS THAN 2 YEARS OF AGE BECAUSE OF THE POTENTIAL FOR FATAL RESPIRATORY DEPRESSION.
POSTMARKETING CASES OF RESPIRATORY DEPRESSION, INCLUDING FATALITIES, HAVE BEEN REPORTED WITH USE OF PROMETHAZINE HYDROCHLORIDE IN PEDIATRIC PATIENTS LESS THAN 2 YEARS OF AGE. A WIDE RANGE OF WEIGHT-BASED DOSES OF PROMETHAZINE HYDROCHLORIDE HAVE RESULTED IN RESPIRATORY DEPRESSION IN THESE PATIENTS.
CAUTION SHOULD BE EXERCISED WHEN ADMINISTERING PROMETHAZINE HYDROCHLORIDE TO PEDIATRIC PATIENTS 2 YEARS OF AGE AND OLDER. IT IS RECOMMENDED THAT THE LOWEST EFFECTIVE DOSE OF PROMETHAZINE HYDROCHLORIDE BE USED IN PEDIATRIC PATIENTS 2 YEARS OF AGE AND OLDER AND CONCOMITANT ADMINISTRATION OF OTHER DRUGS WITH RESPIRATORY DEPRESSANT EFFECTS BE AVOIDED.
Promethazine:
CNS Depression –
- Promethazine may impair the mental and/or physical abilities required for the performance of potentially hazardous tasks, such as driving a vehicle or operating machinery. The impairment may be amplified by concomitant use of other central nervous system depressants such as alcohol, sedatives/hypnotics (including barbiturates), narcotics, narcotic analgesics, general anesthetics, tricyclic antidepressants, and tranquilizers; therefore, such agents should either be eliminated or given in reduced dosage in the presence of promethazine HCl (see PRECAUTIONS - Information For Patients and Drug Interactions ).
Respiratory Depression –
Promethazine may lead to potentially fatal respiratory depression.
Use of promethazine in patients with compromised respiratory function (e.g., COPD, sleep apnea) should be avoided.
Lower Seizure Threshold –
Promethazine may lower seizure threshold. It should be used with caution in persons with seizure disorders or in persons who are using concomitant medications, such as narcotics or local anesthetics, which may also affect seizure threshold.
Bone Marrow Depression –
Promethazine should be used with caution in patients with bone marrow depression. Leukopenia and agranulocytosis have been reported, usually when promethazine HCl has been used in association with other known marrow toxic agents.
Neuroleptic Malignant Syndrome –
A potentially fatal symptom complex sometimes referred to as Neuroleptic Malignant Syndrome (NMS) has been reported in association with promethazine HCl alone or in combination with antipsychotic drugs. Clinical manifestations of NMS are hyperpyrexia, muscle rigidity, altered mental status and evidence of autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis and cardiac dysrhythmias).
The diagnostic evaluation of patients with this syndrome is complicated. In arriving at a diagnosis, it is important to identify cases where the clinical presentation includes both serious medical illness (e.g., pneumonia, systemic infection, etc.) and untreated or inadequately treated extrapyramidal signs and symptoms (EPS). Other important considerations in the differential diagnosis include central anticholinergic toxicity, heat stroke, drug fever and primary central nervous system (CNS) pathology.
The management of NMS should include 1) immediate discontinuation of promethazine HCl, antipsychotic drugs, if any, and other drugs not essential to concurrent therapy, 2) intensive symptomatic treatment and medical monitoring, and 3) treatment of any concomitant serious medical problems for which specific treatments are available. There is no general agreement about specific pharmacological treatment regimens for uncomplicated NMS.
Since recurrences of NMS have been reported with phenothiazines, the reintroduction of promethazine HCl should be carefully considered.
-
Use In Pediatric Patients
PROMETHAZINE PRODUCTS ARE CONTRAINDICATED FOR USE IN PEDIATRIC PATIENTS LESS THAN TWO YEARS OF AGE.
CAUTION SHOULD BE EXERCISED WHEN ADMINISTERING PROMETHAZINE PRODUCTS TO PEDIATRIC PATIENTS 2 YEARS OF AGE AND OLDER BECAUSE OF THE POTENTIAL FOR FATAL RESPIRATORY DEPRESSION. RESPIRATORY DEPRESSION AND APNEA, SOMETIMES ASSOCIATED WITH DEATH, ARE STRONGLY ASSOCIATED WITH PROMETHAZINE PRODUCTS AND ARE NOT DIRECTLY RELATED TO INDIVIDUALIZED WEIGHT-BASED DOSING, WHICH MIGHT OTHERWISE PERMIT SAFE ADMINISTRATION. CONCOMITANT ADMINISTRATION OF PROMETHAZINE PRODUCTS WITH OTHER RESPIRATORY DEPRESSANTS HAS AN ASSOCIATION WITH RESPIRATORY DEPRESSION, AND SOMETIMES DEATH, IN PEDIATRIC PATIENTS.
ANTIEMETICS ARE NOT RECOMMENDED FOR TREATMENT OF UNCOMPLICATED VOMITING IN PEDIATRIC PATIENTS, AND THEIR USE SHOULD BE LIMITED TO PROLONGED VOMITING OF KNOWN ETIOLOGY. THE EXTRAPYRAMIDAL SYMPTOMS WHICH CAN OCCUR SECONDARY TO PROMETHAZINE HYDROCHLORIDE ADMINISTRATION MAY BE CONFUSED WITH THE CNS SIGNS OF UNDIAGNOSED PRIMARY DISEASE, e.g., ENCEPHALOPATHY OR REYE'S SYNDROME. THE USE OF PROMETHAZINE PRODUCTS SHOULD BE AVOIDED IN PEDIATRIC PATIENTS WHOSE SIGNS AND SYMPTOMS MAY SUGGEST REYE'S SYNDROME OR OTHER HEPATIC DISEASES.
Excessively large dosages of antihistamines, including promethazine hydrochloride, in pediatric patients may cause sudden death (see OVERDOSAGE). Hallucinations and convulsions have occurred with therapeutic doses and overdoses of promethazine hydrochloride in pediatric patients. In pediatric patients who are acutely ill associated with dehydration, there is an increased susceptibility to dystonias with the use of promethazine HCl.
- Other Considerations
-
Phenylephrine:
Because phenylephrine is an adrenergic agent, it should be given with caution to patients with thyroid diseases, diabetes mellitus, and heart disease or those receiving tricyclic antidepressants.
Men with symptomatic, benign prostatic hypertrophy can experience urinary retention when given oral nasal decongestants.
Phenylephrine can cause a decrease in cardiac output, and extreme caution should be used when administering the drug parenterally or orally to patients with arteriosclerosis, to elderly individuals, and/or to patients with initially poor cerebral or coronary circulation.
Phenylephrine should be used with caution in patients taking diet preparations, such as amphetamines or phenylpropanolamine, because synergistic adrenergic effects could result in serious hypertensive response and possible stroke.
-
PRECAUTIONS
Animal reproduction studies have not been conducted with the drug combination—promethazine and phenylephrine. It is not known whether this drug combination can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Promethazine and phenylephrine should be given to a pregnant woman only if clearly needed.
General:
Drugs having anticholinergic properties should be used with caution in patients with narrow-angle glaucoma, prostatic hypertrophy, stenosing peptic ulcer, pyloroduodenal obstruction, and bladder-neck obstruction.
Promethazine should be used cautiously in persons with cardiovascular disease or impairment of liver function.
Phenylephrine should be used with caution in patients with cardiovascular disease, particularly hypertension.
Information For Patients:
Promethazine and phenylephrine may cause marked drowsiness or may impair the mental and/or physical abilities required for the performance of potentially hazardous tasks, such as driving a vehicle or operating machinery. Ambulatory patients should be told to avoid engaging in such activities until it is known that they do not become drowsy or dizzy from promethazine and phenylephrine therapy. Children should be supervised to avoid potential harm in bike riding or in other hazardous activities.
The concomitant use of alcohol or other central nervous system depressants, including narcotic analgesics, sedatives, hypnotics, and tranquilizers, may have an additive effect and should be avoided or their dosage reduced.
Patients should be advised to report any involuntary muscle movements.
Avoid prolonged exposure to the sun.
Drug Interactions:
CNS Depressants –
Promethazine may increase, prolong, or intensify the sedative action of other central nervous system depressants, such as alcohol, sedatives/hypnotics (including barbiturates), narcotics, narcotic analgesics, general anesthetics, tricyclic antidepressants, and tranquilizers; therefore, such agents should be avoided or administered in reduced dosage to patients receiving promethazine HCl. When given concomitantly with promethazine, the dose of barbiturates should be reduced by at least one-half, and the dose of narcotics should be reduced by one-quarter to one-half. Dosage must be individualized. Excessive amounts of promethazine HCl relative to a narcotic may lead to restlessness and motor hyperactivity in the patient with pain; these symptoms usually disappear with adequate control of the pain.
Epinephrine –
Because of the potential for promethazine to reverse epinephrine's vasopressor effect, epinephrine should NOT be used to treat hypotension associated with promethazine overdose.
Anticholinergics –
Concomitant use of other agents with anticholinergic properties should be undertaken with caution.
Monoamine Oxidase Inhibitors (MAOI) –
Drug interactions, including an increased incidence of extrapyramidal effects, have been reported when some MAOI and phenothiazines are used concomitantly.
Phenylephrine
Drug
Phenylephrine with prior administration of monoamine oxidase inhibitors (MAOI).
Effect
Cardiac pressor response potentiated.
May cause acute hypertensive crisis.Drug
Phenylephrine with tricyclic antidepressants.
Effect
Pressor response increased.Drug
Phenylephrine with ergot alkaloids.
Effect
Excessive rise in blood pressure.Drug
Phenylephrine with bronchodilator sympathomimetic agents and with epinephrine or other sympathomimetics.
Effect
Tachycardia or other arrhythmias may occur.Drug
Phenylephrine with atropine sulfate.
Effect
Reflex bradycardia blocked; pressor response enhanced.Drug
Phenylephrine with prior administration of propranolol or other β-adrenergic blockers.
Effect
Cardiostimulating effects blocked.Drug
Phenylephrine with prior administration of phentolamine or other α-adrenergic blockers.
Effect
Pressor response decreased.Drug
Phenylephrine with diet preparations, such as amphetamines or phenylpropanolamine.
Effect
Synergistic adrenergic response.Drug/Laboratory Test Interactions:
The following laboratory tests may be affected in patients who are receiving therapy with promethazine hydrochloride.
Carcinogenesis, Mutagenesis, Impairment Of Fertility:
Promethazine:
Long-term animal studies have not been performed to assess the carcinogenic potential of promethazine, nor are there other animal or human data concerning carcinogenicity, mutagenicity, or impairment of fertility with this drug. Promethazine was nonmutagenic in the Salmonella test system of Ames.
Phenylephrine:
A study which followed the development of cancer in 143,574 patients over a four-year period indicated that in 11,981 patients who received phenylephrine (systemic or topical), there was no statistically significant association between the drug and cancer at any or all sites.
Long-term animal studies have not been performed to assess the carcinogenic potential of phenylephrine, nor are there other animal or human data concerning mutagenicity.
A study of the effects of adrenergic drugs on ovum transport in rabbits indicated that treatment with phenylephrine did not alter incidence of pregnancy; the number of implantations was significantly reduced when high doses of the drug were used.
Pregnancy:
Teratogenic Effects –
Promethazine:
Teratogenic effects have not been demonstrated in rat-feeding studies at doses of 6.25 and 12.5 mg/kg of promethazine HCl. These doses are from approximately 2.1 to 4.2 times the maximum recommended total daily dose of promethazine for a 50-kg subject, depending upon the indication for which the drug is prescribed. Daily doses of 25 mg/kg intraperitoneally have been found to produce fetal mortality in rats.
Specific studies to test the action of the drug on parturition, lactation, and development of the animal neonate were not done, but a general preliminary study in rats indicated no effect on these parameters. Although antihistamines have been found to produce fetal mortality in rodents, the pharmacological effects of histamine in the rodent do not parallel those in man. There are no adequate and well-controlled studies of promethazine in pregnant women.
Phenylephrine:
A study in rabbits indicated that continued moderate overexposure to phenylephrine (3 mg/day) during the second half of pregnancy (22nd day of gestation to delivery) may contribute to perinatal wastage, prematurity, premature labor, and possibly fetal anomalies; when phenylephrine (3 mg/day) was given to rabbits during the first half of pregnancy (3rd day after mating for seven days), a significant number gave birth to litters of low birth weight. Another study showed that phenylephrine was associated with anomalies of aortic arch and with ventricular septal defect in the chick embryo.
Promethazine and phenylephrine should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Labor And Delivery:
Administration of phenylephrine to patients in late pregnancy or labor may cause fetal anoxia or bradycardia by increasing contractility of the uterus and decreasing uterine blood flow.
See also "Nonteratogenic Effects."
Nursing Mothers:
It is not known whether promethazine or phenylephrine are excreted in human milk.
Caution should be exercised when promethazine and phenylephrine is administered to a nursing woman.
Pediatric Use:
PROMETHAZINE HYDROCHLORIDE AND PHENYLEPHRINE HYDROCHLORIDE SYRUP IS CONTRAINDICATED FOR USE IN PEDIATRIC PATIENTS LESS THAN TWO YEARS OF AGE (see WARNINGS – Black Box Warning and Use In Pediatric Patients).
Promethazine hydrochloride and phenylephrine hydrochloride syrup should be used with caution in pediatric patients 2 years of age and older (see WARNINGS – Use In Pediatric Patients).
Geriatric Use:
Clinical studies of promethazine hydrochloride and phenylephrine hydrochloride syrup did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal or cardiac function, and of concomitant disease or other drug therapy.
Sedating drugs may cause confusion and over-sedation in the elderly; elderly patients generally should be started on low doses of promethazine hydrochloride and phenylephrine hydrochloride syrup and observed closely.
-
ADVERSE REACTIONS
Promethazine:
Central Nervous System – Drowsiness is the most prominent CNS effect of this drug. Sedation, somnolence, blurred vision, dizziness; confusion, disorientation, and extrapyramidal symptoms such as oculogyric crisis, torticollis, and tongue protrusion; lassitude, tinnitus, incoordination, fatigue, euphoria, nervousness, diplopia, insomnia, tremors, convulsive seizures, excitation, catatonic-like states, hysteria. Hallucinations have also been reported.
Cardiovascular – Increased or decreased blood pressure, tachycardia, bradycardia, faintness.
Dermatologic – Dermatitis, photosensitivity, urticaria.
Hematologic – Leukopenia, thrombocytopenia, thrombocytopenic purpura, agranulocytosis.
Gastrointestinal – Dry mouth, nausea, vomiting, jaundice.
Respiratory – Asthma, nasal stuffiness, respiratory depression (potentially fatal) and apnea (potentially fatal). (See WARNINGS – Promethazine; Respiratory Depression.)
Other – Angioneurotic edema. Neuroleptic malignant syndrome (potentially fatal) has also been reported. (See WARNINGS – Promethazine;Neuroleptic Malignant Syndrome.)
Paradoxical Reactions – Hyperexcitability and abnormal movements have been reported in patients following a single administration of promethazine HCI. Consideration should be given to the discontinuation of promethazine HCl and to the use of other drugs if these reactions occur. Respiratory depression, nightmares, delirium, and agitated behavior have also been reported in some of these patients.
Phenylephrine:
Nervous System – Restlessness, anxiety, nervousness, and dizziness.
Cardiovascular – Hypertension (see "WARNINGS").
Other – Precordial pain, respiratory distress, tremor, and weakness.
-
OVERDOSAGE
Promethazine:
Signs and symptoms of overdosage with promethazine HCl range from mild depression of the central nervous system and cardiovascular system to profound hypotension, respiratory depression, unconsciousness, and sudden death. Other reported reactions include hyperreflexia, hypertonia, ataxia, athetosis, and extensor-plantar reflexes (Babinski reflex).
Stimulation may be evident, especially in children and geriatric patients. Convulsions may rarely occur. A paradoxical reaction has been reported in children receiving single doses of 75 mg to 125 mg orally, characterized by hyperexcitability and nightmares.
Atropine-like signs and symptoms – dry mouth, fixed dilated pupils, flushing, as well as gastrointestinal symptoms, may occur.
Phenylephrine:
Signs and symptoms of overdosage with phenylephrine include hypertension, headache, convulsions, cerebral hemorrhage, and vomiting. Ventricular premature beats and short paroxysms of ventricular tachycardia may also occur. Headache may be a symptom of hypertension. Bradycardia may also be seen early in phenylephrine overdosage through stimulation of baroreceptors.
Treatment:
The treatment of overdosage with promethazine and phenylephrine is essentially symptomatic and supportive. Only in cases of extreme overdosage or individual sensitivity do vital signs including respiration, pulse, blood pressure, temperature, and EKG need to be monitored. Activated charcoal orally or by lavage may be given, or sodium or magnesium sulfate orally as a cathartic. Attention should be given to the re-establishment of adequate respiratory exchange through provision of a patent airway and institution of assisted or controlled ventilation. Diazepam may be used to control convulsions. Acidosis and electrolyte losses should be corrected. Note that any depressant effects of promethazine are not reversed by naloxone. Avoid analeptics which may cause convulsions.
Severe hypotension usually responds to the administration of norepinephrine or phenylephrine. EPINEPHRINE SHOULD NOT BE USED, since its use in a patient with partial adrenergic blockade may further lower the blood pressure.
Limited experience with dialysis indicates that it is not helpful.
-
DOSAGE AND ADMINISTRATION
Promethazine hydrochloride and phenylephrine hydrochloride syrup is contraindicated for children under 2 years of age (see WARNINGS – Black Box Warning and Use In Pediatric Patients).
The recommended doses are given in the following table:
Adults And Children 12 Years And Over
1 teaspoonful (5 mL) every 4 to 6 hours, not to exceed 6 teaspoonsful (30 mL) in 24 hours.
Children 6 To Under 12 Years Of Age
½ to 1 teaspoonful (2.5 to 5 mL) every 4 to 6 hours, not to exceed 6 teaspoonsful (30 mL) in 24 hours.
Children 2 To Under 6 Years Of Age
¼ to ½ teaspoonful (1.25 to 2.5 mL) every 4 to 6 hours.
- HOW SUPPLIED
- SPL UNCLASSIFIED SECTION
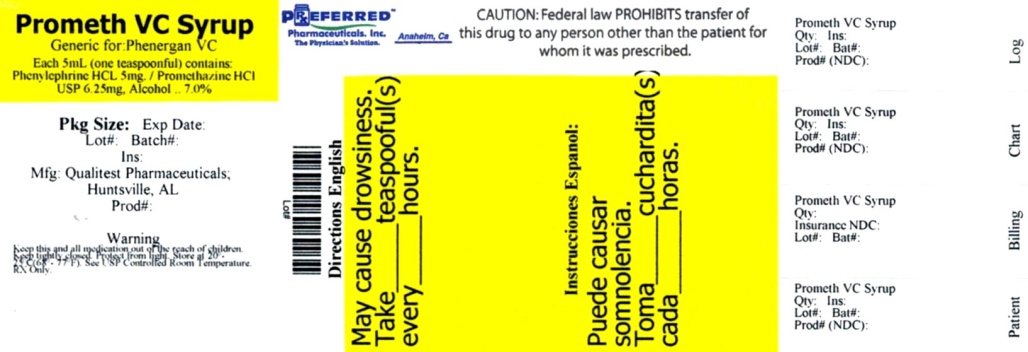
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
PROMETHAZINE VC
promethazinehydrochloride and phenylephrine hydrochloride syrupProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 68788-6763(NDC: 0603-1587) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PROMETHAZINE HYDROCHLORIDE (UNII: R61ZEH7I1I) (PROMETHAZINE - UNII:FF28EJQ494) PROMETHAZINE HYDROCHLORIDE 6.25 mg in 5 mL PHENYLEPHRINE HYDROCHLORIDE (UNII: 04JA59TNSJ) (PHENYLEPHRINE - UNII:1WS297W6MV) PHENYLEPHRINE HYDROCHLORIDE 5 mg in 5 mL Inactive Ingredients Ingredient Name Strength ALCOHOL (UNII: 3K9958V90M) ASCORBIC ACID (UNII: PQ6CK8PD0R) CITRIC ACID MONOHYDRATE (UNII: 2968PHW8QP) FD&C YELLOW NO. 6 (UNII: H77VEI93A8) MENTHOL, UNSPECIFIED FORM (UNII: L7T10EIP3A) METHYLPARABEN (UNII: A2I8C7HI9T) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) PROPYLPARABEN (UNII: Z8IX2SC1OH) WATER (UNII: 059QF0KO0R) SACCHARIN SODIUM (UNII: SB8ZUX40TY) SODIUM BENZOATE (UNII: OJ245FE5EU) SODIUM CITRATE, UNSPECIFIED FORM (UNII: 1Q73Q2JULR) SUCROSE (UNII: C151H8M554) Product Characteristics Color YELLOW (Yellowish-Orange) Score Shape Size Flavor APRICOT (Apricot-Peach) Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 68788-6763-1 118 mL in 1 BOTTLE; Type 0: Not a Combination Product 07/25/2012 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA040654 07/25/2012 Labeler - Preferred Pharmaceuticals, Inc. (791119022) Registrant - Preferred Pharmaceuticals, Inc. (791119022) Establishment Name Address ID/FEI Business Operations Preferred Pharmaceuticals, Inc. 791119022 RELABEL(68788-6763)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.