EMPAVELI ®(pegcetacoplan) injection, for subcutaneous use These highlights do not include all the information needed to use EMPAVELI safely and effectively. See full prescribing information for EMPAVELI. Initial U.S. Approval: 2021
Empaveli by
Drug Labeling and Warnings
Empaveli by is a Prescription medication manufactured, distributed, or labeled by Cenexi HSC, Juzen Chemical Corporation, Bachem AG, Eurofins Lancaster Laboratories, Inc., Eurofins Advantar Laboratories, Inc., Cangene BioPharma, LLC, Nelson Laboratories, LLC, AndersonBrecon Inc. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
EMPAVELI- pegcetacoplan injection, solutionÂ
Cenexi HSC
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONEMPAVELI
®(pegcetacoplan) injection, for subcutaneous use
These highlights do not include all the information needed to use EMPAVELI safely and effectively. See full prescribing information for EMPAVELI. Initial U.S. Approval: 2021 WARNING: SERIOUS INFECTIONS CAUSED BY ENCAPSULATED BACTERIASee full prescribing information for complete boxed warning.EMPAVELI increases the risk of serious and life-threatening infections caused by encapsulated bacteria including Streptococcus pneumoniae, Neisseria meningitidisand Haemophilus influenzaetype B.
EMPAVELI is available only through a restricted program called EMPAVELI REMS. RECENT MAJOR CHANGESINDICATIONS AND USAGEEMPAVELI is a complement inhibitor indicated for the treatment of adult patients with paroxysmal nocturnal hemoglobinuria (PNH). ( 1) DOSAGE AND ADMINISTRATIONDOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONSWARNINGS AND PRECAUTIONS
ADVERSE REACTIONSMost common adverse reactions in patients with PNH (incidence ≥10%) were injection-site reactions, infections, diarrhea, abdominal pain, respiratory tract infection, pain in extremity, hypokalemia, fatigue, viral infection, cough, arthralgia, dizziness, headache, and rash. ( 6.1) To report SUSPECTED ADVERSE REACTIONS, contact Apellis Pharmaceuticals, Inc. at 1-833-866-3346 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. See 17 for PATIENT COUNSELING INFORMATION and Medication Guide. Revised: 2/2024 |
FULL PRESCRIBING INFORMATION
WARNING: SERIOUS INFECTIONS CAUSED BY ENCAPSULATED BACTERIA
EMPAVELI, a complement inhibitor, increases the risk of serious infections, especially those caused by encapsulated bacteria, such as Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzaetype B [see Warnings and Precautions (5.1)] . Life-threatening and fatal infections with encapsulated bacteria have occurred in patients treated with complement inhibitors. These infections may become rapidly life-threatening or fatal if not recognized and treated early.
- Complete or update vaccination for encapsulated bacteria at least 2 weeks prior to the first dose of EMPAVELI, unless the risks of delaying therapy with EMPAVELI outweigh the risk of developing a serious infection. Comply with the most current Advisory Committee on Immunization Practices (ACIP) recommendations for vaccinations against encapsulated bacteria in patients receiving a complement inhibitor. See Warnings and Precautions (5.1)for additional guidance on the management of the risk of serious infections caused by encapsulated bacteria.
- Patients receiving EMPAVELI are at increased risk for invasive disease caused by encapsulated bacteria, even if they develop antibodies following vaccination. Monitor patients for early signs and symptoms of serious infections and evaluate immediately if infection is suspected.
Because of the risk of serious infections caused by encapsulated bacteria, EMPAVELI is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called the EMPAVELI REMS [see Warnings and Precautions (5.2)] .
1 INDICATIONS AND USAGE
EMPAVELI ®is indicated for the treatment of adult patients with paroxysmal nocturnal hemoglobinuria (PNH).
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Vaccination and Prophylaxis
Vaccinate patients against encapsulated bacteria, including Streptococcus pneumoniaeand Neisseria meningitidis(serogroups A, C, W, Y and B), according to current ACIP recommendations at least 2 weeks prior to initiation of EMPAVELI therapy [see Warnings and Precautions (5.1)] .
If urgent EMPAVELI therapy is indicated in a patient who is not up to date with vaccines for Streptococcus pneumoniaeand Neisseria meningitidis, according to ACIP recommendations, provide the patient with antibacterial drug prophylaxis and administer these vaccines as soon as possible.
Healthcare professionals who prescribe EMPAVELI must enroll in the REMS for EMPAVELI [see Warnings and Precautions (5.2)] .
2.2 Recommended Dosage Regimen
The recommended dose of EMPAVELI is 1,080 mg administered subcutaneously twice weekly. EMPAVELI can be administered via a commercially available infusion pump with a reservoir of at least 20 mL or with EMPAVELI Injector.
Dosage for patients switching to EMPAVELI from C5 inhibitors
To reduce the risk of hemolysis with abrupt treatment discontinuation:
- For patients switching from eculizumab, initiate EMPAVELI while continuing eculizumab at its current dose. After 4 weeks, discontinue eculizumab before continuing on monotherapy with EMPAVELI.
- For patients switching from ravulizumab, initiate EMPAVELI no more than 4 weeks after the last dose of ravulizumab.
2.3 Administration
EMPAVELI is for subcutaneous administration using:
- an infusion pumpOR
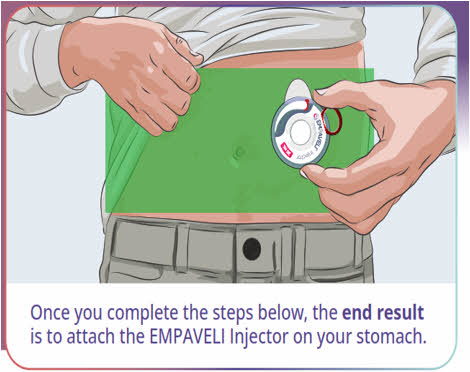
- EMPAVELI Injector, a single-use, disposable on body injector
EMPAVELI is intended for use under the guidance of a healthcare professional. Train patients and/or caregivers on how to prepare and administer EMPAVELI prior to use. After proper training a patient may self-administer, or the patient's caregiver may administer EMPAVELI, if a healthcare provider determines that it is appropriate.
Follow the steps below and use aseptic technique to prepare and administer EMPAVELI, either by an infusion pump or EMPAVELI Injector:
- Prior to use‚ allow EMPAVELI to reach room temperature for approximately 30 minutes. Keep the vial in the carton until ready for use to protect from light.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. EMPAVELI is a clear, colorless to slightly yellowish solution. Do not use if the liquid looks cloudy, contains particles, or is dark yellow.
- Discard any unused portion of EMPAVELI.
Preparation with Infusion Pump
- Refer to the EMPAVELI Instructions for Use and the infusion pump manufacturer's instructions for full preparation and administration information.
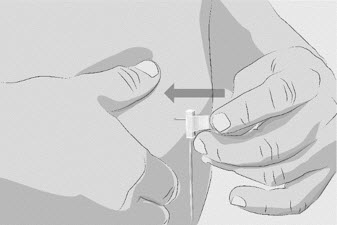
- Use a needleless transfer device (such as a vial adapter) or a transfer needle to fill the syringe.
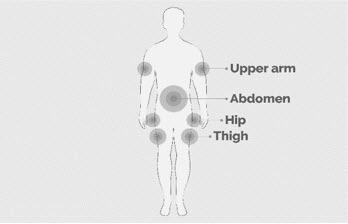
- Rotate infusion sites (i.e., abdomen, thighs, hips, upper arms) from one infusion to the next. Do not infuse where the skin is tender, bruised, red, or hard. Avoid infusing into tattoos, scars, or stretch marks.
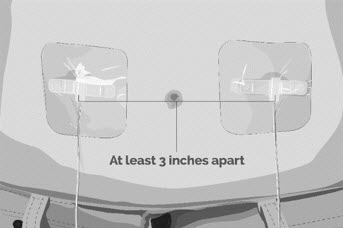
- If multi-infusion sets are needed, ensure the infusion sites are at least 3 inches apart.
- The typical infusion time is approximately 30 minutes (if using two infusion sites) or approximately 60 minutes (if using one infusion site).
Preparation with EMPAVELI Injector
- Refer to the EMPAVELI Injector Instructions for Use, which comes with the device.
- Use a needleless transfer device (such as a vial adapter).
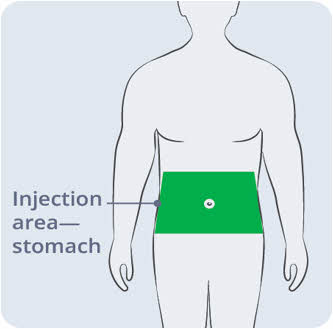
- EMPAVELI Injector is for abdominal subcutaneous use only. Rotate the site of each subcutaneous administration. Do not inject where the skin is tender, bruised, red, or hard. Avoid injecting into tattoos, scars, or stretch marks.
- Injection time is approximately 30 to 60 minutes.
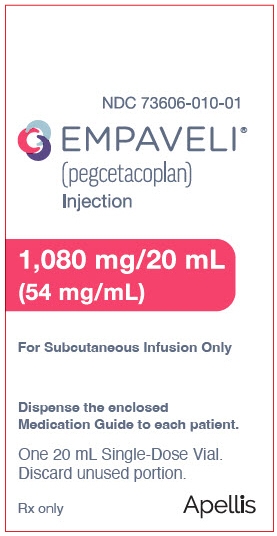
3 DOSAGE FORMS AND STRENGTHS
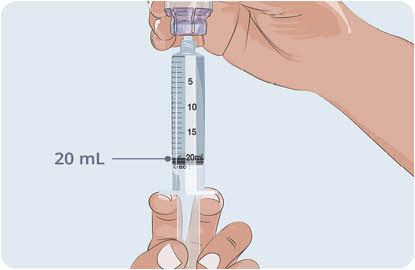
Injection: 1,080 mg/20 mL (54 mg/mL) clear, colorless to slightly yellowish solution in a single-dose vial.
4 CONTRAINDICATIONS
EMPAVELI is contraindicated:
- in patients with hypersensitivity to pegcetacoplan or to any of the excipients [see Warnings and Precautions (5.3)] .
- for initiation in patients with unresolved serious infection caused by encapsulated bacteria including Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzaetype B [see Warnings and Precautions (5.1)] .
5 WARNINGS AND PRECAUTIONS
5.1 Serious Infections Caused by Encapsulated Bacteria
EMPAVELI, a complement inhibitor, increases a patient's susceptibility to serious, life-threatening, or fatal infections caused by encapsulated bacteria including Streptococcus pneumoniae, Neisseria meningitidis(caused by any serogroup, including non-groupable strains), and Haemophilus influenzaetype B. Life-threatening and fatal infections with encapsulated bacteria have occurred in both vaccinated and unvaccinated patients treated with complement inhibitors. The initation of EMPAVELI treatment is contraindicated in patients with unresolved serious infection caused by encapsulated bacteria.
Complete or update vaccination against encapsulated bacteria at least 2 weeks prior to administration of the first dose of EMPAVELI, according to the most current ACIP recommendations for patients receiving a complement inhibitor. Revaccinate patients in accordance with ACIP recommendations considering the duration of therapy with EMPAVELI. Note that, ACIP recommends an administration schedule in patients receiving complement inhibitors that differs from the administration schedule in the vaccine prescribing information. If urgent EMPAVELI therapy is indicated in a patient who is not up to date with vaccines against encapsulated bacteria according to ACIP recommendations, provide the patient with antibacterial drug prophylaxis and administer these vaccines as soon as possible. Various durations and regimens of antibacterial drug prophylaxis have been considered, but the optimal durations and drug regimens for prophylaxis and their efficacy have not been studied in unvaccinated or vaccinated patients receiving complement inhibitors, including EMPAVELI. The benefits and risks of treatment with EMPAVELI, as well as the benefits and risks of antibacterial drug prophylaxis in unvaccinated or vaccinated patients, must be considered against the known risks for serious infections caused by encapsulated bacteria.
Vaccination does not eliminate the risk of serious encapsulated bacterial infections, despite development of antibodies following vaccination. Closely monitor patients for early signs and symptoms of serious infection and evaluate patients immediately if an infection is suspected. Inform patients of these signs and symptoms and instruct patients to seek immediate medical care if these signs and symptoms occur. Promptly treat known infections. Serious infection may become rapidly life-threatening or fatal if not recognized and treated early. Consider interruption of EMPAVELI in patients who are undergoing treatment for serious infections.
EMPAVELI is available only through a restricted program under a REMS [see Warnings and Precautions (5.2)].
5.2 EMPAVELI REMS
EMPAVELI is available only through a restricted program under a REMS called EMPAVELI REMS, because of the risk of serious infections caused by encapsulated bacteria [see Warnings and Precautions (5.1)] .
Notable requirements of the EMPAVELI REMS include the following:
- Prescribers must enroll in the REMS.
- Prescribers must counsel patients about the risk of serious infections caused by encapsulated bacteria.
- Prescribers must provide the patients with the REMS educational materials.
- Prescribers must assess patient vaccination status for encapsulated bacteria and vaccinate if needed according to current ACIP recommendations two weeks prior to the first dose of EMPAVELI.
- Prescribers must provide a prescription for antibacterial drug prophylaxis if treatment must be started urgently, and the patient is not up to date with vaccinations against encapsulated bacteria according to current ACIP recommendations at least two weeks prior to the first dose of EMPAVELI.
- Pharmacies that dispense EMPAVELI must be certified in the EMPAVELI REMS and must verify prescribers are certified.
- Patients must receive counseling from the prescriber about the need to receive vaccinations against encapsulated bacteria per ACIP recommendations, the need to take antibiotics as directed by the prescriber, and the signs and symptoms of serious infections.
- Patients must be instructed to carry the Patient Safety Card with them at all times during and for 2 months following treatment discontinuation with EMPAVELI.
Further information is available at www.empavelirems.com or 1-888-343-7073
5.3 Infusion-Related Reactions
Systemic hypersensitivity reactions (e.g., facial swelling, rash, urticaria) have occurred in patients treated with EMPAVELI. One patient (less than 1% in clinical studies) experienced a serious allergic reaction which resolved after treatment with antihistamines. If a severe hypersensitivity reaction (including anaphylaxis) occurs, discontinue EMPAVELI infusion immediately, institute appropriate treatment, per standard of care, and monitor until signs and symptoms are resolved.
5.4 Monitoring PNH Manifestations after Discontinuation of EMPAVELI
After discontinuing treatment with EMPAVELI, closely monitor for signs and symptoms of hemolysis, identified by elevated LDH levels along with sudden decrease in PNH clone size or hemoglobin, or reappearance of symptoms such as fatigue, hemoglobinuria, abdominal pain, dyspnea, major adverse vascular events (including thrombosis), dysphagia, or erectile dysfunction. Monitor any patient who discontinues EMPAVELI for at least 8 weeks to detect hemolysis and other reactions. If hemolysis, including elevated LDH, occurs after discontinuation of EMPAVELI, consider restarting treatment with EMPAVELI.
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are discussed in greater detail in other sections of the labeling:
- Serious Infections Caused by Encapsulated Bacteria [see Warnings and Precautions (5.1)]
- Infusion-Related Reactions [see Warnings and Precautions (5.3)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Paroxysmal Nocturnal Hemoglobinuria
Study in Complement-Inhibitor Experienced Adult Patients with PNH (Study APL2-302)
The data described below reflect the exposure in 80 adult patients with PNH who received EMPAVELI (n=41) or eculizumab (n=39) at the recommended dosing regimens for 16 weeks. Serious adverse reactions were reported in 7 (17%) patients with PNH receiving EMPAVELI. The most common serious adverse reaction in patients treated with EMPAVELI was infections (5%). The most common adverse reactions (≥10%) with EMPAVELI were injection-site reactions, infections, diarrhea, abdominal pain, respiratory tract infection, viral infection, and fatigue.
Table 1 describes the adverse reactions that occurred in ≥5% of patients treated with EMPAVELI in Study APL2-302.
| Adverse Reaction | EMPAVELI
(N=41) n (%) | Eculizumab
(N=39) n (%) |
|---|---|---|
|
|
||
| General disorders and administration site conditions | ||
| Injection-site reaction * | 16 (39) | 2 (5) |
| Fatigue * | 5 (12) | 9 (23) |
| Chest pain * | 3 (7) | 1 (3) |
| Infections and infestations | ||
| Infections * | 12 (29) | 10 (26) |
| Respiratory tract infection * | 6 (15) | 5 (13) |
| Viral Infection * | 5 (12) | 3 (8) |
| Gastrointestinal disorders | ||
| Diarrhea | 9 (22) | 1 (3) |
| Abdominal pain * | 8 (20) | 4 (10) |
| Musculoskeletal disorders | ||
| Back pain * | 3 (7) | 4 (10) |
| Nervous system disorders | ||
| Headache | 3 (7) | 9 (23) |
| Vascular disorders | ||
| Systemic hypertension * | 3 (7) | 1 (3) |
Clinically relevant adverse reactions in less than 5% of patients include:
- Intestinal ischemia
- Biliary sepsis
- Hypersensitivity pneumonitis
After the randomized control period, 77 patients continued the study, and all were treated with EMPAVELI monotherapy at the recommended dosing regimen for up to 48 weeks. Serious adverse reactions were reported in 18 patients (23%). Additional adverse reactions reported in >5% of patients treated with EMPAVELI during the open-label part of the study compared to the randomized controlled part in Table 1 were cough (12%), arthralgia (8%), oropharyngeal pain (8%), pyrexia (8%), pain in extremity (7%), thrombocytopenia (7%), abdominal distension (5%), acute kidney injury (5%), anxiety (5%), and myalgia (5%). One patient (1%) died due to COVID-19 infection.
Study in Complement-Inhibitor NaĂŻve Adult Patients with PNH (Study APL2-308)
The data described below reflect the exposure in adult patients with PNH who received EMPAVELI (n=46) or the control arm (supportive care excluding complement inhibitors) (n=18) in Study APL2-308 [see Clinical Studies (14.1)] . One patient (2%) who received EMPAVELI died due to septic shock. Serious adverse reactions were reported in 6 (13%) patients with PNH receiving EMPAVELI. The most common adverse reaction (≥10%) in patients treated with EMPAVELI were injection site reactions, infections, viral infection, pain in extremity, hypokalemia, arthralgia, dizziness, abdominal pain, rash, and headache.
Table 2 describes the adverse reactions that occurred in ≥5% of patients treated with EMPAVELI in Study APL2‑308.
| Adverse Reaction | EMPAVELI
(N=46) n (%) | Control Arm
*
(N=18) n (%) |
|---|---|---|
| Exposure Adjusted Rate (per 100 pt yrs) | Exposure Adjusted Rate (per 100 pt yrs) | |
| EMPAVELI (N=46) group includes patients who received EMPAVELI at any point during the study, including patients randomized to EMPAVELI (N=35) and patients randomized to the control arm and crossed over to EMPAVELI treatment (N=11). | ||
|
|
||
| General disorders and administration site conditions | ||
| Injection-site reaction †| 12 (26)
42 | 0
0 |
| Pyrexia | 4(9)
14 | 0
0 |
| Peripheral edema †| 3 (7)
11 | 0
0 |
| Infections and Infestations | ||
| Infections †| 9 (20)
32 | 4 (22)
74 |
| Viral infection †| 6 (13)
21 | 2 (11)
37 |
| Musculoskeletal and connective tissue disorders | ||
| Pain in extremity | 6 (13)
21 | 0
0 |
| Arthralgia | 5 (11)
18 | 0
0 |
| Musculoskeletal pain | 3 (7)
11 | 0
0 |
| Metabolism and nutrition disorders | ||
| Hypokalemia | 6 (13)
21 | 2 (11)
37 |
| Nervous system disorders | ||
| Dizziness | 5 (11)
18 | 0
0 |
| Headache | 5 (11)
18 | 0
0 |
| Somnolence | 3 (7)
11 | 0
0 |
| Gastrointestinal disorders | ||
| Abdominal pain †| 5 (11)
18 | 1 (6)
18 |
| Skin and subcutaneous tissue disorders | ||
| Rash †| 5(11)
18 | 0
0 |
| Ecchymosis | 3 (7)
11 | 0
0 |
| Erythema | 3 (7)
11 | 0
0 |
| Blood and lymphatic system disorders | ||
| Thrombocytopenia | 3 (7)
11 | 1 (6)
18 |
| Respiratory, thoracic and mediastinal disorders | ||
| Cough †| 4 (9)
14 | 0
0 |
| Epistaxis | 3 (7)
11 | 0
0 |
| Investigations | ||
| Blood creatinine increased | 3 (7)
11 | 0
0 |
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are insufficient data on EMPAVELI use in pregnant women to inform a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes. There are risks to the mother and fetus associated with untreated PNH in pregnancy (see Clinical Considerations) . The use of EMPAVELI may be considered following an assessment of the risks and benefits.
Treatment of pregnant cynomolgus monkeys with pegcetacoplan at a subcutaneous dose of 28 mg/kg/day (2.9 times human exposure based on AUC) from the gestation period through parturition resulted in a statistically significant increase in abortions or stillbirths compared to controls (see Data) .
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of major birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriages in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Disease-associated maternal and/or fetal/neonatal risk
PNH in pregnancy is associated with adverse maternal outcomes, including worsening cytopenias, thrombotic events, infections, bleeding, miscarriages and increased maternal mortality, and adverse fetal outcomes, including fetal death and premature delivery.
Data
Animal Data
Animal reproduction studies with pegcetacoplan were conducted in cynomolgus monkeys. Pegcetacoplan treatment of pregnant cynomolgus monkeys at a subcutaneous dose of 28 mg/kg/day (2.9 times human exposure based on AUC) from the gestation period through parturition resulted in a statistically significant increase in abortions and stillbirths compared to controls. No increase in abortions or stillbirths occurred at a dose of 7 mg/kg/day (1.3 times human exposure based on AUC). No maternal toxicity or teratogenic effects were observed in offspring delivered at term. No developmental effects were observed in infants up to 6 months postpartum. Systemic exposure to pegcetacoplan of less than 1% of maternal levels was detected in fetuses from monkeys treated with 28 mg/kg/day from the period of organogenesis through the second trimester.
8.2 Lactation
Risk Summary
It is not known whether pegcetacoplan is secreted in human milk or whether there is potential for absorption and harm to the infant. There are no data on the effects of pegcetacoplan on milk production. Pegcetacoplan is present in milk of lactating monkeys (see Animal Data) . Since many medicinal products are secreted into human milk, and because of the potential for serious adverse reaction in a breastfeeding child, breastfeeding should be discontinued during treatment and for 40 days after the last dose.
8.3 Females and Males of Reproductive Potential
Contraception
Females
EMPAVELI may cause embryo-fetal harm when administered to pregnant women [see Use in Specific Populations (8.1)] . Pregnancy testing is recommended for females of reproductive potential prior to treatment with EMPAVELI. Advise female patients of reproductive potential to use effective contraception during treatment with EMPAVELI and for 40 days after the last dose.
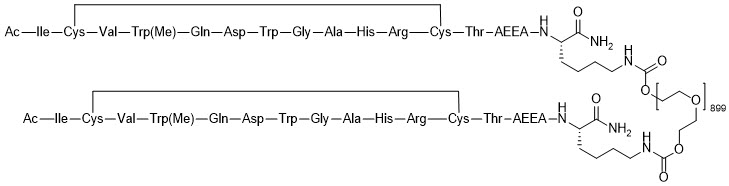
11 DESCRIPTION
EMPAVELI contains pegcetacoplan, a complement inhibitor. Pegcetacoplan is a symmetrical molecule comprised of two identical pentadecapeptides covalently bound to the ends of a linear 40-kiloDalton (kDa) PEG molecule. The peptide portions of pegcetacoplan contain 1-methyl-L-tryptophan (Trp(Me)) in position 4 and amino(ethoxyethoxy)acetic acid (AEEA) in position 14.
The molecular weight of pegcetacoplan is approximately 43.5 kDa. The molecular formula is C 1970H 3848N 50O 947S 4. The structure of pegcetacoplan is shown below.
EMPAVELI injection is a sterile, clear, colorless to slightly yellowish aqueous solution for subcutaneous use and is supplied in a 20-mL single-dose vial. Each 1 mL of solution contains 54 mg of pegcetacoplan, 41 mg of sorbitol, 0.384 mg of glacial acetic acid, 0.490 mg of sodium acetate trihydrate, and Water for Injection USP. EMPAVELI may also contain sodium hydroxide and/or additional glacial acetic acid for adjustment to a target pH of 5.0.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Pegcetacoplan binds to complement protein C3 and its activation fragment C3b, thereby regulating the cleavage of C3 and the generation of downstream effectors of complement activation. In PNH, extravascular hemolysis (EVH) is facilitated by C3b opsonization while intravascular hemolysis (IVH) is mediated by the downstream membrane attack complex (MAC). Pegcetacoplan acts proximally in the complement cascade controlling both C3b-mediated EVH and terminal complement-mediated IVH.
12.2 Pharmacodynamics
In patients with PNH administered multiple doses of pegcetacoplan, the mean C3 concentration increased from 0.94 g/L at baseline to 3.80 g/L at Week 16 and sustained through Week 48 (Study APL2-302). In study APL2-308, the mean C3 concentration increased from 0.95 g/L at baseline to 3.56 g/L at Week 26 [see Clinical Studies (14.1)] .
The percentage of PNH Type II + III RBCs increased from 66.2% at baseline to 93.9% at Week 16 and sustained through Week 48 (Study APL2-302). In Study APL2-308, the mean percentage of PNH Type II + III RBCs increased from 42.4% at baseline to 90.0% at Week 26.
The mean percentage of PNH Type II + III RBCs with C3 deposition decreased from 17.8% at baseline to 0.20% at Week 16 and sustained through Week 48 (Study APL2-302). In Study APL2-308, the mean percentage of PNH Type II + III RBCs with C3 deposition decreased from 2.85% at baseline to 0.09% at Week 26.
12.3 Pharmacokinetics
In patients with PNH, the serum pegcetacoplan concentrations achieved steady-state approximately 4 to 6 weeks following the first dose. The exposure of pegcetacoplan increased proportionally over a dose range from 45 to 1,440 mg (0.04 to 1.33 times the approved recommended dose). The mean (CV%) trough serum concentration observed at Week 16 was 706 (15.1%) mcg/mL and sustained through Week 48 (Study APL2-302). In Study APL2-308, mean (CV%) trough serum concentration was 744 (25.5%) mcg/mL at Week 26.
Absorption
The median T maxof pegcetacoplan is between 108 and 144 hours (4.5 to 6.0 days) after a single dose.
Distribution
The mean (CV%) volume of distribution of pegcetacoplan is approximately 3.98 L (32%) in patients with PNH.
Elimination
The estimated mean (CV%) of clearance (CL) is 0.36 L/day (30%) and median effective half-life of elimination (t 1/2) is 8.6 days in patients with PNH.
Specific Populations
There were no clinically significant differences on the pharmacokinetics of pegcetacoplan based on age (19 to 81 years old), sex, race (Asian vs. non-Asian), renal impairment, and hepatic function as evaluated by total bilirubin (0.06-8.8 mg/dL), albumin (3.0-5.5 g/dL), aspartate aminotransferase (6.0-302 IU/L), or alanine aminotransferase (4.0-209 IU/L).
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term animal carcinogenicity studies of pegcetacoplan have not been conducted.
Pegcetacoplan was not mutagenic when tested in an in vitrobacterial reverse mutation (Ames) and was not genotoxic in an in vitroassay in human TK6 cells or in an in vivomicronucleus assay in mice.
Effects of pegcetacoplan on fertility have not been studied in animals. There were no microscopic abnormalities in male or female reproductive organs in toxicity studies in rabbits and monkeys.
13.2 Animal Toxicology and/or Pharmacology
In toxicology studies in rabbits and cynomolgus monkeys, epithelial vacuolation and infiltrates of vacuolated macrophages were observed in multiple tissues, including the renal tubules, following daily subcutaneous doses of pegcetacoplan up to 7 times the human dose. These findings are attributable to uptake of the PEG moieties of pegcetacoplan. Renal degeneration was observed microscopically in rabbits at exposures (C maxand AUC) less than those for the human dose, and in monkeys at exposures approximately 2.7-fold those for the human dose. The clinical significance of these findings is uncertain.
14 CLINICAL STUDIES
14.1 Paroxysmal Nocturnal Hemoglobinuria
The efficacy and safety of EMPAVELI in patients with PNH were assessed in two open-label, randomized-controlled Phase 3 studies: Study APL2-302 (NCT03500549) and Study APL2-308 (NCT04085601). All patients who completed the studies were eligible to enroll in a separate long-term extension study.
In both studies, patients were vaccinated against Streptococcus pneumoniae, Neisseria meningitidistypes A, C, W, Y, and B, and Haemophilus influenzaetype B (Hib), either within 2 years prior to Day 1 or within 2 weeks after starting treatment with EMPAVELI. Patients vaccinated after initiation of treatment with EMPAVELI received prophylactic treatment with appropriate antibiotics until 2 weeks after vaccination. In addition, prophylactic antibiotic therapy was administered at the discretion of the investigator in accordance with local treatment guidelines for patients with PNH receiving treatment with a complement inhibitor.
A dose of 1,080 mg twice weekly was used for patients randomized to the EMPAVELI group of each study. If required, the dose of EMPAVELI could be adjusted to 1,080 mg every 3 days. EMPAVELI was administered as a subcutaneous infusion; the infusion time was approximately 20 to 40 minutes.
Study in Complement-Inhibitor Experienced Adult Patients with PNH (Study APL2-302)
The study enrolled patients with PNH who had been treated with a stable dose of eculizumab for at least the previous 3 months and with Hb levels less than 10.5 g/dL.
Eligible patients entered a 4-week run-in period during which they received EMPAVELI 1,080 mg subcutaneously twice weekly in addition to their current dose of eculizumab. Patients were then randomized in a 1:1 ratio to receive either 1,080 mg of EMPAVELI twice weekly or their current dose of eculizumab through the duration of the 16-week randomized controlled period (RCP).
Randomization was stratified based on the number of packed red blood cell (PRBC) transfusions within the 12 months prior to Day -28 (<4; ≥4) and platelet count at screening (<100,000/mm 3; ≥100,000/mm 3). Following completion of the RCP, all patients entered a 32-week open-label period (OLP) and received monotherapy with EMPAVELI. Patients initially randomized to eculizumab entered a second 4-week run-in period during which they received EMPAVELI in addition to eculizumab before continuing on to receive EMPAVELI monotherapy. All patients who completed the 48-week period were eligible to enroll in a separate long-term extension study.
A total of 80 patients were randomized to receive treatment, 41 to EMPAVELI and 39 to eculizumab. Demographics and baseline disease characteristics were generally well balanced between treatment groups (see Table 2). The median times from PNH diagnosis to Day -28 were 6.0 and 9.7 years, respectively, for EMPAVELI and eculizumab. The baseline mean total PNH RBC clone sizes (Type III) were 47% for EMPAVELI and 50% for eculizumab. Twenty-nine percent and 23% of patients had a history of major adverse vascular events, and 37% and 26% had a history of thrombosis for patients receiving EMPAVELI or eculizumab, respectively. Within 28 days prior to the first dose of EMPAVELI or eculizumab, respectively, 34% and 31% of patients used anti-thrombotic agents (anti-platelet and/or anticoagulants). During Study APL2-302, 37% and 36% of patients on EMPAVELI and eculizumab, respectively, used antithrombotic agents. A total of 38 patients in the group treated with EMPAVELI and 39 patients in the eculizumab group completed the 16-week RCP and continued into the 32-week OLP. Because of adverse reactions of hemolysis, 3 patients were discontinued from the EMPAVELI group during the RCP. Two out of 41 patients in the EMPAVELI group needed the dose adjustment to 1,080 mg every 3 days.
| Parameter | Statistics | EMPAVELI
(N=41) | Eculizumab
(N=39) |
|---|---|---|---|
| Age (years) | Mean (SD) | 50.2 (16.3) | 47.3 (15.8) |
| Sex | |||
| Â Â Female | n (%) | 27 (65.9) | 22 (56.4) |
| Race | |||
| Â Â Asian | n (%) | 5 (12.2) | 7 (17.9) |
| Â Â Black or African American | n (%) | 2 (4.9) | 0 |
| Â Â White | n (%) | 24 (58.5) | 25 (64.1) |
| Â Â Other | n (%) | 0 | 1 (2.6) |
| Â Â Not reported | n (%) | 10 (24.4) | 6 (15.4) |
| Ethnicity | |||
| Â Â Hispanic or Latino | n (%) | 2 (4.9) | 1 (2.6) |
| Â Â Not Hispanic or Latino | n (%) | 29 (70.7) | 32 (82.1) |
| Â Â Not reported | n (%) | 10 (24.4) | 6 (15.4) |
| Hemoglobin level (g/dL) | Mean (SD) | 8.7 (1.1) | 8.7 (0.9) |
| Absolute reticulocyte count
(10 9cells/L) | Mean (SD) | 218 (75.0) | 216 (69.1) |
| LDH level (U/L) | Mean (SD) | 257.5 (97.7) | 308.6 (284.8) |
| Number of transfusions in last 12 months prior to Day -28 | Mean (SD) | 6.1 (7.3) | 6.9 (7.7) |
| Â Â <4 | n (%) | 20 (48.8) | 16 (41.0) |
|   ≥4 | n (%) | 21 (51.2) | 23 (59.0) |
The efficacy of EMPAVELI was based on change from baseline to Week 16 (during RCP) in hemoglobin level. Baseline was defined as the average of measurements recorded prior to taking the first dose of EMPAVELI. Supportive efficacy data included transfusion avoidance, defined as the proportion of patients who did not require a transfusion during the RCP, and change from baseline to Week 16 in absolute reticulocyte count (ARC).
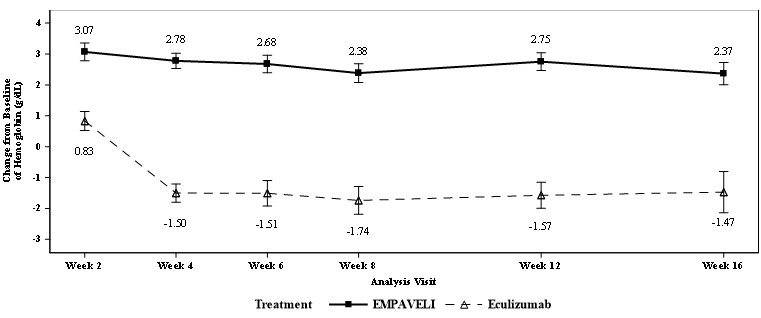
EMPAVELI was superior to eculizumab for the change from baseline in hemoglobin level at Week 16 ( p<0.0001). The adjusted mean change from baseline in hemoglobin level was 2.37 g/dL in the group treated with EMPAVELI versus -1.47 g/dL in the eculizumab group (Figure 1), demonstrating an adjusted mean increase of 3.84 g/dL with EMPAVELI compared to eculizumab at Week 16 (95% CI, 2.33-5.34).
|
|
|
Figure 1: Adjusted Mean (± SE) Change from Baseline to Week 16 in Hemoglobin (g/dL) in Study APL2-302 * |
|
|
Non-inferiority was demonstrated in the endpoints of transfusion avoidance and change from baseline in ARC at Week 16.
The adjusted means, treatment differences, and confidence intervals (CIs) for additional efficacy results are shown in Table 4.
| EMPAVELI
(N=41) | Eculizumab
(N=39) | Difference
(95% CI) |
|
|---|---|---|---|
|
|
|||
| Transfusion avoidance, n (%) | 35 (85%) | 6 (15%) | 63%
*
(48%, 77%) |
| Change from baseline in ARC(10 9cells/L), LS †mean (SE) ‡ | -136 (6.5) | 28 (11.9) | -164
(-189.9, -137.3) |
Efficacy was generally similar across subgroups based on sex, race, and age.
All 77 patients who completed the RCP entered the 32- week OLP, during which all patients received EMPAVELI, resulting in a total exposure of up to 48 weeks. Between Week 16 and Week 48, 10 patients discontinued the study, all due to adverse reactions, and thirteen patients had a dose adjustment to 1,080 mg every three days. The efficacy results at Week 48 were generally consistent with those at Week 16.
Study in Complement-Inhibitor NaĂŻve Adult Patients with PNH (Study APL2-308)
Study APL2-308 enrolled patients with PNH who had not been treated with any complement inhibitor within 3 months prior to enrollment and with Hb levels less than the lower limit of normal (LLN). Eligible patients were randomized in a 2:1 ratio to receive EMPAVELI or supportive care [excluding complement inhibitors (e.g., transfusions, corticosteroids, supplements such as iron, folate, and vitamin B 12), hereafter referred to as the control arm] through the duration of the 26-week treatment period. Randomization was stratified based on the number of packed red blood cell (PRBC) transfusions within the 12 months prior to Day -28 (<4; ≥4). At any point during the study, a patient assigned to the control arm treatment group who had Hb levels ≥2 g/dL below baseline or presented with a PNH associated thromboembolic event was offered cross-over to EMPAVELI for the remainder of the study.
A total of 53 patients were randomized, 35 to EMPAVELI and 18 to the control arm. Demographics and baseline disease characteristics were generally well balanced between treatment groups (see Table 4). The mean times from PNH diagnosis to Day 1 were 5.7 and 5.5 years, respectively, for EMPAVELI and the control arm. The baseline mean total PNH RBC clone sizes (Type III) were 31% for EMPAVELI and 28% for the control arm. In the EMPAVELI group, 2.9% of patients had a history of major adverse vascular events. Two patients (5.7%) in the EMPAVELI group and 3 patients (16.7%) in the control arm group had a history of at least 1 type of thrombosis. Within 28 days prior to the first dose of EMPAVELI or the control arm, respectively, 17.1% and 27.8% of patients used anti-thrombotic agents (anti-platelet and/or anticoagulants). During Study APL2-308, 8.6% and 0% of patients on EMPAVELI and the control arm, respectively, used antithrombotic agents. Eleven of 18 patients randomized to the control transitioned to cross-over therapy with EMPAVELI due to a decreased Hb level ≥2 g/dL below baseline. Three patients treated with EMPAVELI required dose adjustment to 1,080 mg every 3 days. Three patients (5.7%; two patients in the EMPAVELI group and one patient in the control arm group) discontinued the study, none due to an adverse reaction.
| Parameter | Statistics | EMPAVELI
(N=35) | Control Arm * |
|---|---|---|---|
| (N=18) | |||
|
|
|||
| Age (years) | Mean (SD) | 42.2 (12.7) | 49.1 (15.6) |
| Sex | |||
| Â Â Female | n (%) | 16 (45.7) | 8 (44.4) |
| Race | |||
| Â Â American Indian or Alaska | n (%) | 9 (25.7) | 2 (11.1) |
| Native | |||
| Â Â Asian | n (%) | 23 (65.7) | 16 (88.9) |
| Â Â Black or African American | n (%) | 2 (5.7) | 0 |
| Â Â Other | n (%) | 1 (2.9) | 0 |
| Ethnicity | |||
| Â Â Hispanic or Latino | n (%) | 12 (34.3) | 2 (11.1) |
| Â Â Not Hispanic or Latino | n (%) | 23 (65.7) | 16 (88.9) |
| Hemoglobin level (g/dL) | Mean (SD) | 9.4 (1.4) | 8.7 (0.8) |
| Absolute reticulocyte count (10 9cells/L) | Mean (SD) | 230.2 (81.0) | 180.3 (109.1) |
| LDH level (U/L) | Mean (SD) | 2151.0 (909.4) | 1945.9 (1003.7) |
| Number of transfusions in last 12 months prior to Day -28 | Mean (SD) | 3.9 (4.4) | 5.1 (5.0) |
| Â Â <4 | n (%) | 21 (60.0) | 8 (44.4) |
|   ≥4 | n (%) | 14 (40.0) | 10 (55.6) |
The efficacy of EMPAVELI was based on the percentage of patients achieving hemoglobin stabilization, defined as avoidance of a >1 g/dL decrease in hemoglobin levels from baseline in the absence of transfusion, and the change from baseline in LDH level. Supportive efficacy data included change from baseline in absolute reticulocyte count (ARC), change from baseline in hemoglobin, and transfusion avoidance, defined as the proportion of patients who did not require a transfusion through Week 26. Baseline was defined as the average of measurements recorded prior to taking the first dose of EMPAVELI or prior to randomization to the control arm treatment group.
Efficacy results are shown in Table 6 below.
| EMPAVELI
(N=35) | Control Arm * | Difference
(95% CI) |
|
|---|---|---|---|
| (N=18) | p-value | ||
| Data collected after cross-over from the control arm is excluded in analyses. | |||
|
|
|||
| Â | |||
| Hemoglobin Stabilization
â€
(n, %) | 30 (85.7%) | 0 (0%) | 73% (57%, 89%)
p<0.0001 ‡ |
| Change from Baseline in LDH §(LS ¶Mean CFB, SE #) | -1870 (101.0) | -400 (313.0) | -1470 (-2113.4, -827.3)
p<0.0001 |
| Â | Â | ||
| Change from baseline in ARC
§
(LS ¶Mean CFB, SE #) | -123 (9.2) | -19 (25.2) | -103 (-158.9, -48.7)
p = 0.0002 |
| Change from baseline in Hb
§
(LS ¶Mean CFB, SE #) | 2.9 (0.38) | 0.3 (0.76) | 2.7 (0.99, 4.35)
p = 0.0019 |
| Transfusion Avoidance
â€
(n, %) | 32 (91%) | 1 (6%) | 72% (56%, 89%)
p<0.0001 ‡ |
16 HOW SUPPLIED/STORAGE AND HANDLING
How Supplied
EMPAVELI injection is a clear, colorless to slightly yellowish aqueous solution for subcutaneous infusion supplied as 1,080 mg/20 mL (54 mg/mL) solution in 20-mL single-dose vials.
EMPAVELI is available in 20-mL single-dose vials individually packaged in cartons that are supplied in 8-count convenience cartons. NDC: 73606-010-01.
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide and Instructions for Use).
Serious Infections Caused by Encapsulated Bacteria
Advise patients of the risk of serious infection. Inform patients of the need to complete or update their vaccinations against encapsulated bacteria at least 2 weeks prior to receiving the first dose of EMPAVELI or receive antibacterial drug prophylaxis if EMPAVELI treatment must be initiated immediately and they have not been previously vaccinated. Inform the patient that they are required to be revaccinated according to current ACIP recommendations for encapsulated bacteria while on EMPAVELI therapy [see Warnings and Precautions (5.1)] .
Inform patients that vaccination may not prevent serious infection and strongly advise patients to seek immediate medical attention if these signs or symptoms occur. These signs and symptoms include the following:
- fever with or without shivers or the chills
- fever with chest pain and cough
- fever with breathlessness/fast breathing
- fever with high heart rate
- headache and a fever
- headache with a stiff neck or stiff back
- fever and a rash
- confusion
- headache with nausea or vomiting
- body aches with flu-like symptoms
- clammy skin
- eyes sensitive to light
Inform patients that they will be given a Patient Safety Card for EMPAVELI that they should carry with them at all times. This card describes symptoms which, if experienced, should prompt the patient to seek immediate medical evaluation.
EMPAVELI REMS
EMPAVELI is available only through a restricted program called EMPAVELI REMS [see Warnings and Precautions (5.2)] .
Inform the patient of the following notable requirements:
- Patients must receive counseling about the risk of serious infections caused by encapsulated bacteria.
- Patients must receive written educational materials about this risk.
- Patients must be instructed to carry the Patient Safety Card with them at all times during and for 2 months following treatment with EMPAVELI.
- Patients must be instructed to complete or update vaccinations against encapsulated bacteria per ACIP recommendations as directed by the prescriber prior to treatment with EMPAVELI.
- Patients must receive antibiotics as directed by the prescriber if they are not up to date with vaccinations against encapsulated bacteria and have to start EMPAVELI right away.
Anaphylaxis and infusion-related reactions
Advise patients of the risk of anaphylaxis and infusion-related reactions. Inform patients that anaphylaxis is life-threatening and strongly advise patients to seek immediate medical attention if these signs or symptoms occur. These signs and symptoms include the following:
- difficulty breathing including shortness of breath and wheezing
- swollen tongue or throat
- feeling faint
- rapid heart rate
- skin reactions, including hives and itching
- nausea or vomiting
- confusion and anxiety
- dizziness or fainting
Discontinuation
Inform patients with PNH that they may develop hemolysis due to PNH when EMPAVELI is discontinued and that they will be monitored by their healthcare professional for at least 8 weeks following discontinuation of EMPAVELI.
Inform patients who discontinue EMPAVELI to keep the Patient Safety Card with them for 2 months after the last dose of EMPAVELI, because the increased risk of serious infection persists for several weeks following discontinuation of EMPAVELI.
Manufactured for:
Apellis Pharmaceuticals, Inc.
100 Fifth Avenue
Waltham, MA 02451
For patent information: www.apellis.com/productpatent
Copyright © 2021 Apellis Pharmaceuticals, Inc. All rights reserved.
EMPAVELI is a registered trademark of Apellis Pharmaceuticals, Inc.
EMP-PI-08Feb2024-5.0
| This Medication Guide has been approved by the U.S. Food and Drug Administration. | Revised:02/2024Â Â Â Â Â Â Â Â Â Â Â Â | |||
| MEDICATION GUIDE
EMPAVELI ®(em-puh-vel-ee) (pegcetacoplan) injection, for subcutaneous use |
||||
| What is the most important information I should know about EMPAVELI?
EMPAVELI is a medicine that affects your immune system. EMPAVELI may lower the ability of your immune system to fight infections.
|
||||
|
|
|||
| Your healthcare provider will give you a Patient Safety Card about the risk of serious infections.Carry it with you at all times during treatment and for 2 months after your last dose of EMPAVELI. Your risk of serious infections may continue for several weeks after your last dose of EMPAVELI. It is important to show this card to any healthcare provider who treats you. This will help them diagnose and treat you quickly.
EMPAVELI is only available through a program called the EMPAVELI Risk Evaluation and Mitigation Strategy (REMS). Before you can take EMPAVELI, your healthcare provider must:
|
||||
| What is EMPAVELI?
EMPAVELI is a prescription medicine used to treat adults with a disease called paroxysmal nocturnal hemoglobinuria (PNH). It is not known if EMPAVELI is safe and effective in children. |
||||
Do not take EMPAVELI if you:
|
||||
Before you take EMPAVELI, tell your healthcare provider about all of your medical conditions, including if you:
Know the medicines you take and the vaccines you receive. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine. |
||||
How should I take EMPAVELI?
|
||||
|
|
|||
| If you miss a dose of EMPAVELI, take the missed dose as soon as possible. Take your next dose at your regularly scheduled time. | ||||
| What are the possible side effects of EMPAVELI?
EMPAVELI can cause serious side effects including:
|
||||
|
|
|||
| Tell your healthcare provider about any side effect that bothers you or that does not go away. These are not all of the possible side effects of EMPAVELI. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
||||
How should I store EMPAVELI?
|
||||
| General information about the safe and effective use of EMPAVELI.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use EMPAVELI for a condition for which it was not prescribed. Do not give EMPAVELI to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about EMPAVELI that is written for health professionals. |
||||
| What are the ingredients in EMPAVELI?
Active ingredient:pegcetacoplan Inactive ingredients:sorbitol, glacial acetic acid, sodium acetate trihydrate, Water for Injection USP. EMPAVELI may also contain sodium hydroxide and/or additional glacial acetic acid for pH adjustment. Manufactured for: Apellis Pharmaceuticals, Inc. 100 Fifth Avenue Waltham, MA 02451 For patent information: www.apellis.com/productpatent Copyright © 2021 Apellis Pharmaceuticals, Inc. All rights reserved. EMPAVELI is a registered trademark of Apellis Pharmaceuticals, Inc. For more information, go to www.EMPAVELI.com or call 1-866-692-7527 EMP-MG-08Feb2024-5.0 |
||||
INSTRUCTIONS FOR USE
EMPAVELI
®(em-puh-vel-ee)
(pegcetacoplan)
injection, for subcutaneous use
infusion pump
Important Information
This Instructions for Use is for the infusion pump only. If using EMPAVELI Injector, follow the Instructions for Use that comes with the EMPAVELI Injector.
Read thisInstructions for Use before you start using EMPAVELI with an infusion pump and each time you get a refill as there may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or treatment. Your healthcare provider should show you or your caregiver how to infuse EMPAVELI the right way before you use it for the first time. Ask your healthcare provider about any instructions you do not understand.
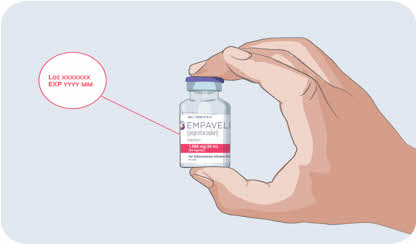
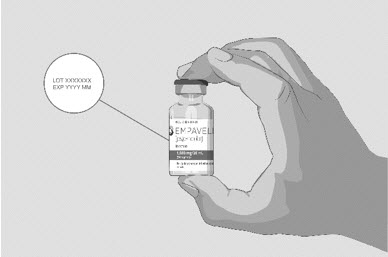
How should I store EMPAVELI?
- Store vials of EMPAVELI in the refrigerator between 36°F to 46°F (2°C to 8°C) in the original carton to protect from light.
- Do not use EMPAVELI past the expiration date stamped on the carton.
Keep EMPAVELI and all medicines out of the reach of children.
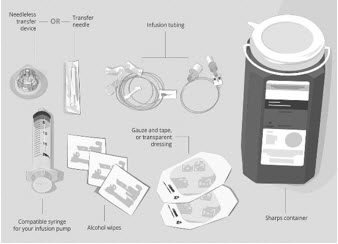
| Step 1 | Prepare for infusion
Before you start:
| |
Gather your supplies (See
Figure A):
| Figure A: Supplies
|
|
| Clean your work surface well using an alcohol wipe. | ||
| Wash your hands well with soap and water. Dry your hands. | ||
| Step 2 | Check the vial and liquid
| Figure B
|
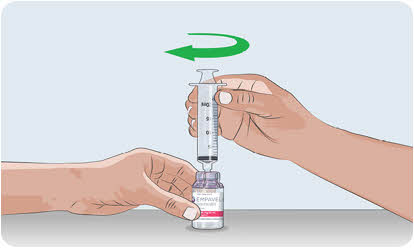
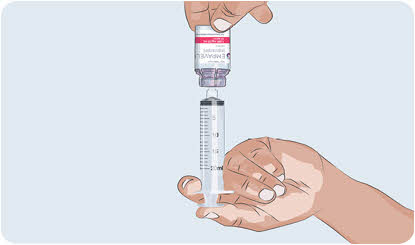
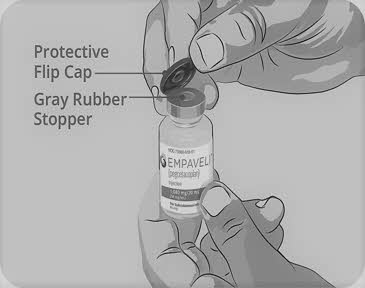
| Step 3 | Prepare and fill syringe
Do nottouch the exposed gray rubber stopper after wiping. | Figure C
|
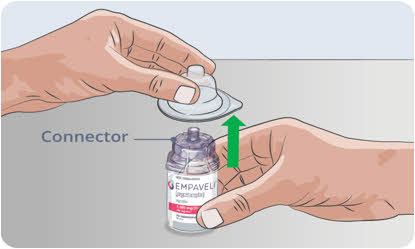
| Option 1:If using a needleless transfer device (such as a vial adapter), follow the instructions provided by the device manufacturer.
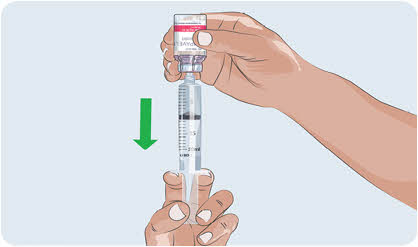
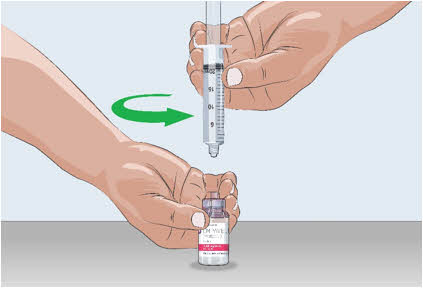
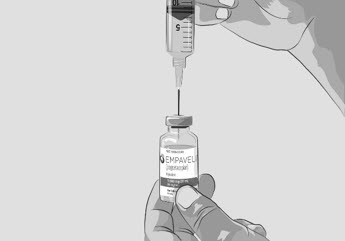
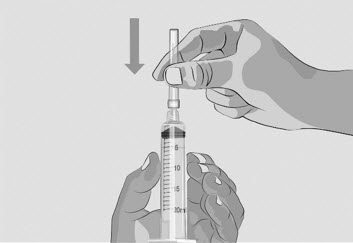
OR Option 2:If transfer is done using a transfer needle and a syringe, follow the instructions below:
| Figure D
|
|
| Figure F
|
|
| Figure G
|
|
| Figure H
|
|
| Figure I
|
|
| Figure J
|
|
| Step 4 | Prepare infusion pump and tubing
| |
| Step 5 | Prepare the infusion site(s)
| Figure K
|
| Figure L
|
|
| Figure M
|
|
| Step 6 | Insert and secure the infusion needle(s)
| Figure N
|
| Figure O
|
|
| Step 7 | Start infusion
| |
| Step 8 | Complete infusion
| |
| Step 9 | Record infusion
| |
| Step 10 | Clean up
| |
| Step 11 | Dispose of (throw away) used needles and syringes and EMPAVELI infusion tubing.
| Figure P
|
Call 1-866-692-7527 to speak with an Apellis representative.
Manufactured for:
Apellis Pharmaceuticals, Inc. 100 Fifth Avenue Waltham, MA 02451
Copyright © 2021 Apellis Pharmaceuticals, Inc. All rights reserved.
EMPAVELI is a registered trademark of Apellis Pharmaceuticals, Inc.
This Instructions for Use has been approved by the U.S. Food and Drug Administration.
Revised 09/2023
EMP-IFU-29Sep2023-4.0
INSTRUCTIONS FOR USE
EMPAVELI
®Injector
(pegcetacoplan)
injection, for subcutaneous use
Single-use on-body injector
Important Information
This Instructions for Use is for the EMPAVELI Injector only.
Read thisInstructions for Use before you start using the Injector and each time you get a refill as there may be new information. The EMPAVELI Injector is placed on your body to give medicine under the skin. This information does not take the place of talking to your healthcare provider about your medical condition or treatment. Your healthcare provider should show you or your caregiver how to inject EMPAVELI the right way before you use it for the first time. It is important that you do not try to give yourself or someone else the injection unless you have received training from your healthcare provider. Ask your healthcare provider about any instructions you do not understand.
If you have questions, concerns, or need of help, please call ApellisAssist ®at 1-866-MY-APL-ASSIST (1-866-692-7527).
| SIDE 1:
Filling the Syringe |
|
Start Here Complete these instructions on how to prepare EMPAVELI before completing EMPAVELI Injector administration instructions on the back of this page. |
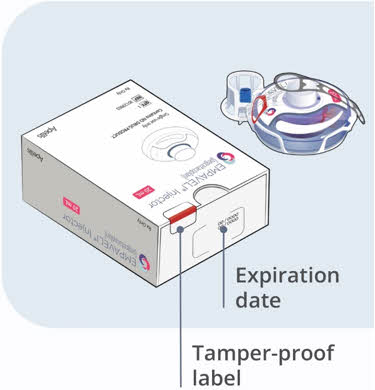
How should I store EMPAVELI?
- Store vials of EMPAVELI in the refrigerator between 36°F to 46°F (2°C to 8°C) in the original carton to protect from light.
- Do notuse EMPAVELI past the expiration date stamped on the carton.
Keep EMPAVELI, EMPAVELI Injector, and all medicines out of the reach of children.
|
|
| Prepare for injection | |
1
|
|
2
|
|
| Check the vial and liquid | |
| 3
|
|
| 4
|
|
| 5
|
|
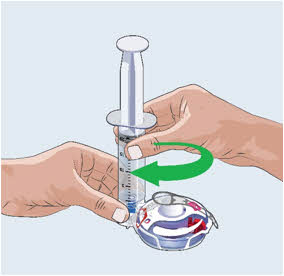
| Prepare and fill the syringe with EMPAVELI using a needleless transfer device (such as a vial adapter)
|
|
| 6
Always follow the Instructions for Use provided by the needleless transfer device's manufacturer (as they may differ from the following steps).
|
|
| 7
|
|
| 8
|
|
| 9
|
|
| 10
|
|
| 11
|
|
| 12
|
|
| 13
|
|
| 14
|
|
| 15
|
|
| 16
|
|
| SIDE 2:
Injector Administration |
| Complete these instructions for administering the EMPAVELI Injector after completing syringe filling instructions on the front of this page. |
|
|
Important information for administration with EMPAVELI Injector
General use:
| Using EMPAVELI Injector:
| During injection:
|
|
|
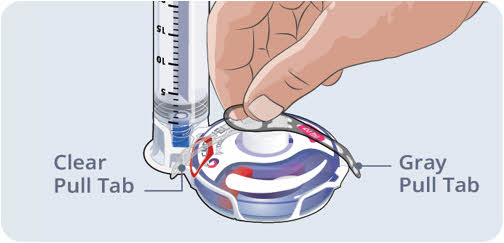
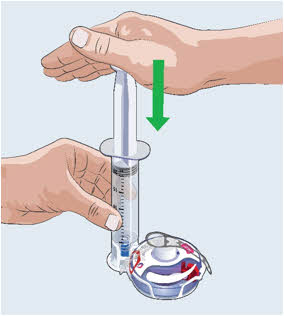
| Fill injector with EMPAVELI liquid | |
| 17
|
|
| 18
|
|
19
 |
|
| 20
|
|
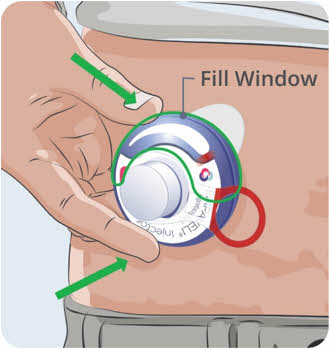
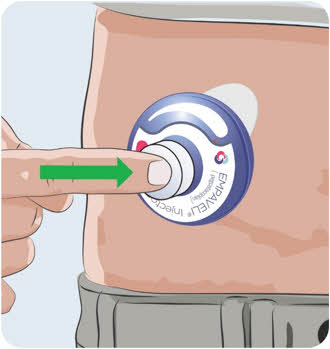
| Attach EMPAVELI Injector to stomach | |
| 21
|
|
| 22
|
|
| 23
|
|
| 24
|
|
| 25
|
|
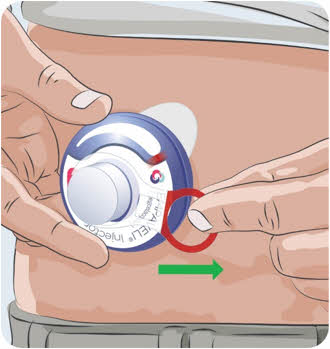
| Start Injection | |
| 26
|
|
| 27
|
|
| 28
|
|
| 29
|
|
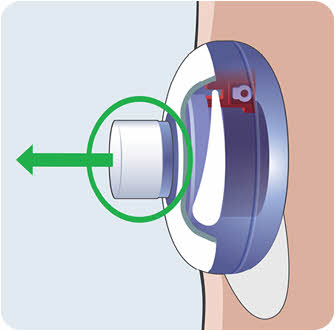
| Remove and dispose of EMPAVELI Injector | |
| 30
|
|
| 31
|
|
|
|
|
|
How to store the EMPAVELI Injector
|
|
| Questions and answers
Can I use more than 1 syringe to fill the EMPAVELI Injector? No, use only 1 syringe per EMPAVELI Injector. What should I do if the syringe plunger will not push down to fill the EMPAVELI Injector? You must firmly press down on the plunger to fill the EMPAVELI Injector. It will feel like there is resistance. Can I remove the EMPAVELI Injector from my stomach and put it on later to finish injection? No. The EMPAVELI Injector cannot be reattached. If you take it off, you may not get your full dose. How long should the injection take? The injection time is approximately 30 to 60 minutes. If the button has not popped out after 2 hours (120 minutes), press and hold the button while you remove the EMPAVELI Injector from your skin.
Make sure that you have taken off the Red Safety Tab. If the Red Safety Tab is removed, make sure you have tried to push the Button in all the way. If you still cannot push the button all the way in, then the EMPAVELI Injector is damaged. Remove your EMPAVELI Injector and set aside. Open a new EMPAVELI Injector and start over. Call ApellisAssist at 1-866-MY-APL-ASSIST (1-866-692-7527). What if the EMPAVELI Injector falls off of my body? If the EMPAVELI Injector falls off of your body, pick it up carefully. Do not touch the needle or any medicine that may be on the EMPAVELI Injector. Set the EMPAVELI Injector aside and out of the reach of children. Call ApellisAssist at 1-866-MY-APLASSIST (1-866-692-7527) right away. Is it normal for skin to be bumpy or irritated during an injection? No. Your body may be sensitive to the adhesive on the EMPAVELI Injector or to the medicine. Call your healthcare provider right away. Is it normal for skin to be red after an injection? Your skin may be slightly red after adhesive removal. If the redness does not go away after 1-2 days, call your healthcare provider. |
Manufactured for:
Apellis Pharmaceuticals, Inc. 100 Fifth Avenue Waltham, MA 02451
Manufactured by:
Enable Injections, Inc. 2863 E. Sharon Road Cincinnati, OH 45421, USA
10130600 Rev 04
Patent:EnableInjections.com/patent
Copyright © 2023 Apellis Pharmaceuticals, Inc. All rights reserved.
APELLIS, APELLISASSIST, EMPAVELI, and their respective logos are registered trademarks of Apellis Pharmaceuticals, Inc.
This Instructions for Use has been approved by the U.S. Food and Drug Administration.
Issued: 09/2023
EMP INJ-IFU-29Sep2023-1.0
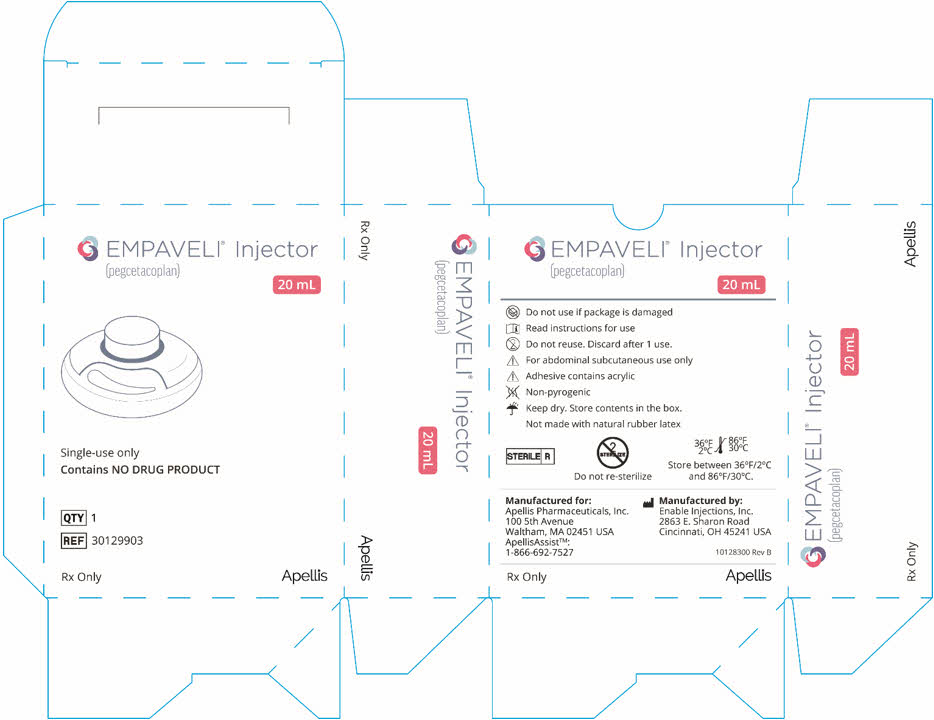
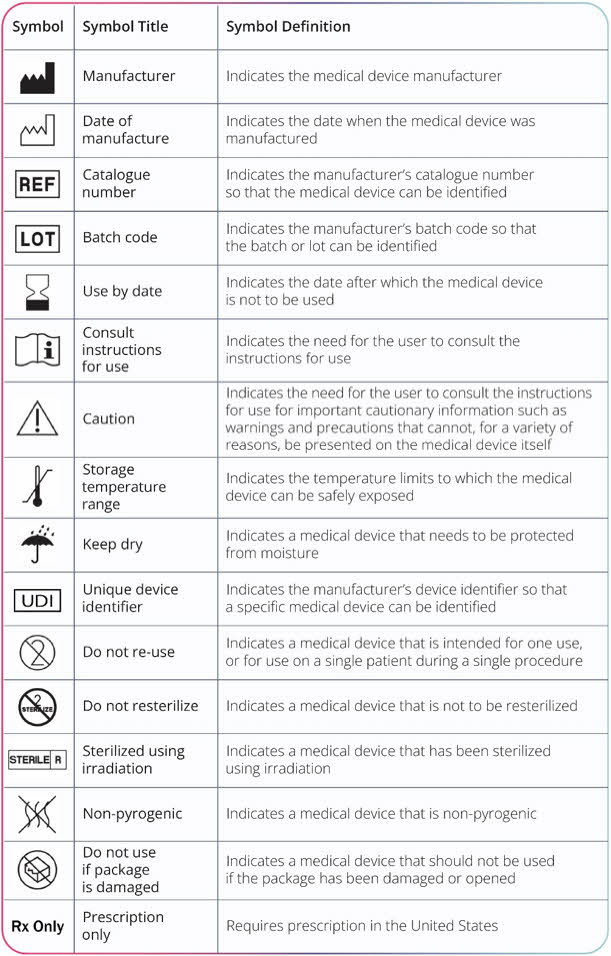
PRINCIPAL DISPLAY PANEL - 1,080 mg/20 mL Vial Carton
NDC: 73606-010-01
EMPAVELI
®
(pegcetacoplan)
Injection
1,080 mg/20 mL
(54 mg/mL)
For Subcutaneous Infusion Only
Dispense the enclosed
Medication Guide to each patient.
One 20 mL Single-Dose Vial.
Discard unused portion.
Rx only
Apellis
| EMPAVELIÂ
pegcetacoplan injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler -Â Cenexi HSC (268155718) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Juzen Chemical Corporation | 691036974 | api manufacture(82454-0010) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Bachem AG | 482220311 | api manufacture(82454-0010) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Eurofins Lancaster Laboratories, Inc. | 069777290 | analysis(82454-0010) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Eurofins Advantar Laboratories, Inc. | 849636258 | analysis(82454-0010) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Cangene BioPharma, LLC | 050783398 | manufacture(82454-0010) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Nelson Laboratories, LLC | 151663234 | analysis(82454-0010) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| AndersonBrecon Inc | 053217022 | pack(82454-0010) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Cenexi HSC | 268155718 | manufacture(82454-0010) | |
Trademark Results [Empaveli]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 EMPAVELI 97460836 not registered Live/Pending |
Apellis Pharmaceuticals, Inc. 2022-06-15 |
 EMPAVELI 90505492 not registered Live/Pending |
Apellis Pharmaceuticals, Inc. 2021-02-02 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.










 Â
Â