CLINDAMYCIN PHOSPHATE lotion
Clindamycin Phosphate by
Drug Labeling and Warnings
Clindamycin Phosphate by is a Prescription medication manufactured, distributed, or labeled by Taro Pharmaceuticals U.S.A., Inc., Taro Pharmaceuticals Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
-
DESCRIPTION
Clindamycin Phosphate Topical Lotion, 1% contains clindamycin phosphate, USP, at a concentration equivalent to 10 mg clindamycin per milliliter.
Clindamycin phosphate is a water soluble ester of the semi-synthetic antibiotic produced by a 7(S)-chloro-substitution of the 7(R)-hydroxyl group of the parent antibiotic lincomycin.
The lotion contains cetostearyl alcohol (2.5%), glycerin, glyceryl stearate SE (with potassium monostearate), isostearyl alcohol (2.5%), methylparaben (0.3%), purified water, sodium lauroyl sarcosinate and stearic acid.
The structural formula is represented below:
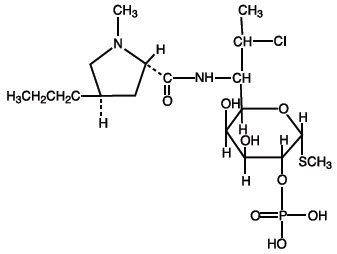
The chemical name for clindamycin phosphate is Methyl 7-chloro-6,7,8-trideoxy-6-(1-methyl- trans-4-propyl-L-2-pyrrolidinecarboxamido)-1-thio-L- threo-α-D- galacto-octopyranoside 2-(dihydrogen phosphate).
-
CLINICAL PHARMACOLOGY
Pharmacokinetics
Following multiple topical applications of clindamycin phosphate at a concentration equivalent to 10 mg clindamycin per mL in an isopropyl alcohol and water solution, very low levels of clindamycin are present in the serum (0 to 3 ng/mL) and less than 0.2% of the dose is recovered in urine as clindamycin.
Although clindamycin phosphate is inactive in vitro, rapid in vivohydrolysis converts this compound to the antibacterially active clindamycin.
Microbiology
Clindamycin inhibits bacterial protein synthesis by binding to the 23S RNA of the 50S subunit of the ribosome. Clindamycin is bacteriostatic.
Antimicrobial Activity
Clindamycin is active in vitroagainst most isolates of Propionibacterium acnes;however, the clinical significance is unknown.
Resistance
Resistance to clindamycin is most often caused by modification of specific bases of the 23S ribosomal RNA. Cross-resistance between clindamycin and lincomycin is complete. Because the binding sites for these antibacterial drugs overlap, cross-resistance is sometimes observed among lincosamides, macrolides and streptogramin B. Macrolide-inducible resistance to clindamycin occurs in some isolates of macrolide-resistant bacteria.
-
INDICATIONS AND USAGE
Clindamycin phosphate topical lotion is indicated in the treatment of acne vulgaris. In view of the potential for diarrhea, bloody diarrhea and pseudomembranous colitis, the physician should consider whether other agents are more appropriate (see CONTRAINDICATIONS, WARNINGSand ADVERSE REACTIONS).
- CONTRAINDICATIONS
-
WARNINGS
Orally and parenterally administered clindamycin has been associated with severe colitis which may result in patient death. Use of the topical formulation of clindamycin results in absorption of the antibiotic from the skin surface. Diarrhea, bloody diarrhea, and colitis (including pseudomembranous colitis) have been reported with the use of topical and systemic clindamycin.
Studies indicate a toxin(s) produced by clostridia is one primary cause of antibiotic-associated colitis. The colitis is usually characterized by severe persistent diarrhea and severe abdominal cramps and may be associated with the passage of blood and mucus. Endoscopic examination may reveal pseudomembranous colitis. Stool culture for Clostridium difficileand stool assay for C. difficiletoxin may be helpful diagnostically.
When significant diarrhea occurs, the drug should be discontinued. Large bowel endoscopy should be considered to establish a definitive diagnosis in cases of severe diarrhea.
Antiperistaltic agents such as opiates and diphenoxylate with atropine may prolong and/or worsen the condition. Vancomycin has been found to be effective in the treatment of antibiotic-associated pseudomembranous colitis produced by Clostridium difficile. The usual adult dosage is 500 milligrams to 2 grams of vancomycin orally per day in three to four divided doses administered for 7 to 10 days. Cholestyramine or colestipol resins bind vancomycin in vitro. If both a resin and vancomycin are to be administered concurrently, it may be advisable to separate the time of administration of each drug.
Diarrhea, colitis, and pseudomembranous colitis have been observed to begin up to several weeks following cessation of oral and parenteral therapy with clindamycin.
-
PRECAUTIONS
General
Clindamycin phosphate topical lotion should be prescribed with caution in atopic individuals.
Drug Interactions
Clindamycin has been shown to have neuromuscular blocking properties that may enhance the action of other neuromuscular blocking agents. Therefore, it should be used with caution in patients receiving such agents.
Pregnancy
Teratogenic effects
In clinical trials with pregnant women, the systemic administration of clindamycin during the second and third trimesters has not been associated with an increased frequency of congenital abnormalities. There are no adequate studies in pregnant women during the first trimester of pregnancy. Clindamycin should be used during the first trimester of pregnancy only if clearly needed.
Nursing Mothers
It is not known whether clindamycin is excreted in breast milk following use of clindamycin phosphate topical lotion. However, orally and parenterally administered clindamycin has been reported to appear in breast milk. Clindamycin has the potential to cause adverse effects on the breast-fed infant's gastrointestinal flora. Monitor the breast-fed infant for possible adverse effects on the gastrointestinal flora, such as diarrhea, candidiasis (thrush, diaper rash) or rarely, blood in the stool indicating possible antibiotic-associated colitis.
The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for clindamycin and any potential adverse effects on the breast-fed child from clindamycin or from the underlying maternal condition.
Pediatric Use
Safety and effectiveness in pediatric patients under the age of 12 have not been established.
Geriatric Use
Clinical studies for clindamycin phosphate did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients.
-
ADVERSE REACTIONS
In 18 clinical studies of various formulations of clindamycin phosphate using placebo vehicle and/or active comparator drugs as controls, patients experienced a number of treatment emergent adverse dermatologic events [see tablebelow].
Number of Patients Reporting Events Treatment Emergent Adverse Event Solution
n=553 (%)Gel
n=148 (%)Lotion
n=160 (%)- * not recorded
- † of 126 subjects
Burning 62 (11) 15 (10) 17 (11) Itching 36 (7) 15 (10) 17 (11) Burning/Itching 60 (11) *( – ) *( – ) Dryness 105 (19) 34 (23) 29 (18) Erythema 86 (16) 10 ( 7) 22 (14) Oiliness/Oily Skin 8 ( 1) 26 (18) 12 †(10) Peeling 61 (11) *( – ) 11 ( 7) Orally and parenterally administered clindamycin has been associated with severe colitis which may end fatally.
Cases of diarrhea, bloody diarrhea and colitis (including pseudomembranous colitis) have been reported as adverse reactions in patients treated with oral and parenteral formulations of clindamycin and rarely with topical clindamycin (see WARNINGS).
Abdominal pain, gastrointestinal disturbances, gram-negative folliculitis, eye pain and contact dermatitis have also been reported in association with the use of topical formulations of clindamycin.
-
OVERDOSAGE
Topically applied clindamycin phosphate can be absorbed in sufficient amounts to produce systemic effects (see WARNINGS).
- DOSAGE AND ADMINISTRATION
-
HOW SUPPLIED
Clindamycin Phosphate Topical Lotion, 1% containing clindamycin phosphate equivalent to 10 mg clindamycin per milliliter is available in the following size:
60 mLplastic squeeze bottle – NDC: 51672-1400-4
- SPL UNCLASSIFIED SECTION
-
PRINCIPAL DISPLAY PANEL - 60 mL Bottle Carton
60 mL
NDC: 51672-1400-4
Clindamycin
PhosphateTopical Lotion
1%
FOR TOPICAL
USE ONLYKeep this and all
medications out
of the reach of
children.Rx only
TARO
-
INGREDIENTS AND APPEARANCE
CLINDAMYCIN PHOSPHATE
clindamycin phosphate lotionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 51672-1400 Route of Administration TOPICAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CLINDAMYCIN PHOSPHATE (UNII: EH6D7113I8) (CLINDAMYCIN - UNII:3U02EL437C) CLINDAMYCIN PHOSPHATE 10 mg in 1 mL Inactive Ingredients Ingredient Name Strength CETOSTEARYL ALCOHOL (UNII: 2DMT128M1S) GLYCERIN (UNII: PDC6A3C0OX) GLYCERYL STEARATE SE (UNII: FCZ5MH785I) ISOSTEARYL ALCOHOL (UNII: Q613OCQ44Y) METHYLPARABEN (UNII: A2I8C7HI9T) SODIUM LAUROYL SARCOSINATE (UNII: 632GS99618) STEARIC ACID (UNII: 4ELV7Z65AP) WATER (UNII: 059QF0KO0R) Product Characteristics Color white (white to off-white) Score Shape Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 51672-1400-4 1 in 1 CARTON 06/28/2021 1 60 mL in 1 BOTTLE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA214526 06/28/2021 Labeler - Sun Pharmaceutical Industries, Inc. (146974886) Establishment Name Address ID/FEI Business Operations Sun Pharma Canada Inc. 243339023 manufacture(51672-1400)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.