MENOPUR- menotropins kit
Menopur by
Drug Labeling and Warnings
Menopur by is a Prescription medication manufactured, distributed, or labeled by Ferring Pharmaceuticals Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use MENOPUR ® safely and effectively. See full prescribing information for MENOPUR.
MENOPUR ® (menotropins for injection) for subcutaneous use.
Initial U.S. Approval: 1975INDICATIONS AND USAGE
MENOPUR ® (menotropins for injection) is a gonadotropin indicated for:
- Development of multiple follicles and pregnancy in ovulatory women as part of an Assisted Reproductive Technology (ART) cycle ( 1)
DOSAGE AND ADMINISTRATION
- Initial starting dose of the first cycle - 225 International Units per day, administered subcutaneously ( 2.2)
- Dosage adjustments after 5 days and by no more than 150 International Units at each adjustment ( 2.2)
- Do not administer doses greater than 450 International Units per day ( 2.2)
- MENOPUR may be administered together with BRAVELLE ® (urofollitropin for injection, purified). Only the total starting dose of 225 International Units (150 International Units of MENOPUR and 75 International Units of BRAVELLE or 75 International Units of MENOPUR and 150 International Units of BRAVELLE) was studied in a clinical trial. ( 2.2)
DOSAGE FORMS AND STRENGTHS
Lyophilized powder for injection: containing 75 IU FSH and 75 IU of LH activity, supplied as lyophilized powder or pellet in sterile vials with diluent vials and QCap ® vial adapters. ( 3)
CONTRAINDICATIONS
MENOPUR is contraindicated in women who exhibit:
- Prior hypersensitivity to MENOPUR or menotropins products or one of their excipients ( 4)
- High levels of FSH indicating primary ovarian failure ( 4)
- Pregnancy ( 4)
- Presence of uncontrolled non-gonadal endocrinopathies ( 4)
- Sex hormone dependent tumors of the reproductive tract and accessory organ ( 4)
- Tumors of pituitary gland or hypothalamus ( 4)
- Abnormal uterine bleeding of undetermined origin ( 4)
- Ovarian cyst or enlargement of undetermined origin, not due to polycystic ovary syndrome ( 4)
WARNINGS AND PRECAUTIONS
ADVERSE REACTIONS
The most common adverse reactions (≥2%) in ART include: abdominal cramps; abdomen enlarged; abdominal pain; headache; injection site pain and reaction; injection site inflammation; OHSS ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Ferring Pharmaceuticals Inc. at 1-888-FERRING (1-888-337-7464) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.DRUG INTERACTIONS
No drug/drug interaction studies have been conducted for MENOPUR in humans. ( 7)
USE IN SPECIFIC POPULATIONS
- Pregnancy Category X. Do not use MENOPUR in pregnant women. ( 4, 8.1)
- Nursing Mothers: It is not known whether this drug is excreted in human milk. ( 8.3)
- Pediatric Use: Safety and efficacy not established. ( 8.4)
- Renal and Hepatic Insufficiency: Safety, efficacy, and pharmacokinetics of MENOPUR in women with renal or hepatic insufficiency have not been established. ( 8.6)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 5/2018
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 General Dosing Information
2.2 Recommended Dosing for Assisted Reproductive Technology
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Abnormal Ovarian Enlargement
5.2 Ovarian Hyperstimulation Syndrome (OHSS)
5.3 Pulmonary and Vascular Complications
5.4 Ovarian Torsion
5.5 Multi-fetal Gestation and Birth
5.6 Congenital Malformations
5.7 Ectopic Pregnancy
5.8 Spontaneous Abortion
5.9 Ovarian Neoplasms
5.10 Laboratory Tests
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.6 Renal and Hepatic Insufficiency
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
17.1 Dosing and Use
17.2 Duration and Monitoring Required
17.3 Instructions Regarding a Missed Dose
17.4 Ovarian Hyperstimulation Syndrome
17.5 Multi-fetal Gestation and Birth
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
Development of Multiple Follicles and Pregnancy in Ovulatory Women as Part of an Assisted Reproductive Technology (ART) Cycle
Prior to initiation of treatment with MENOPUR ® (menotropins for injection):
- Perform a complete gynecologic and endocrinologic evaluation, and diagnose the cause of infertility
- Exclude the possibility of pregnancy
- Evaluate the fertility status of the male partner
- Exclude a diagnosis of primary ovarian failure
-
2 DOSAGE AND ADMINISTRATION
2.1 General Dosing Information
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
- Administer MENOPUR subcutaneously in the abdomen as described in Instructions for Use.
- MENOPUR may be administered together with BRAVELLE ® (urofollitropin for injection, purified).
2.2 Recommended Dosing for Assisted Reproductive Technology
The recommended dosing scheme for patients undergoing IVF follows a stepwise approach and is individualized for each woman. The recommended initial dose of MENOPUR for women who have received a GnRH agonist for pituitary suppression is 225 International Units. MENOPUR may be administered together with BRAVELLE and the total initial dose when the products are combined should not exceed 225 International Units (150 International Units of MENOPUR and 75 International Units of BRAVELLE or 75 International Units of MENOPUR and 150 International Units of BRAVELLE).
- Beginning on cycle day 2 or 3, a starting dose of 225 International Units of MENOPUR is administered subcutaneously daily. Adjust the dose after 5 days based on the woman's ovarian response, as determined by ultrasound evaluation of follicular growth and serum estradiol levels.
- Do not make additional dosage adjustments more frequently than every 2 days or by more than 150 International Units at each adjustment.
- Continue treatment until adequate follicular development is evident, and then administer hCG.
Withhold the administration of hCG in cases where the ovarian monitoring suggests an increased risk of OHSS on the last day of MENOPUR therapy [ see Warnings and Precautions (5.1, 5.2, 5.10)]. - Do not administer daily doses of MENOPUR or MENOPUR in combination with BRAVELLE that exceed 450 International Units .
- Therapy should not exceed 20 days.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
MENOPUR is contraindicated in women who exhibit:
- Prior hypersensitivity to MENOPUR or menotropins products or one of their excipients
- High levels of FSH indicating primary ovarian failure [see Indications and Usage (1)]
- Pregnancy
MENOPUR may cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)]. MENOPUR is contraindicated in women who are pregnant. If this drug is used during pregnancy, or if the woman becomes pregnant while taking this drug, the woman should be apprised of the potential hazard to a fetus. - Presence of uncontrolled non-gonadal endocrinopathies (e.g., thyroid, adrenal, or pituitary disorders) [see Indications and Usage (1)]
- Sex hormone dependent tumors of the reproductive tract and accessory organs
- Tumors of pituitary gland or hypothalamus
- Abnormal uterine bleeding of undetermined origin
- Ovarian cyst or enlargement of undetermined origin, not due to polycystic ovary syndrome
-
5 WARNINGS AND PRECAUTIONS
MENOPUR should only be used by physicians who are experienced in infertility treatment. MENOPUR contains gonadotropic substances capable of causing in women, Ovarian Hyperstimulation Syndrome (OHSS) with or without pulmonary or vascular complications [see Warnings and Precautions (5.2, 5.3)] and multiple births [see Warnings and Precautions (5.5)] . Gonadotropin therapy requires the availability of appropriate monitoring facilities [see Warnings and Precautions (5.10)] . Use the lowest effective dose.
5.1 Abnormal Ovarian Enlargement
In order to minimize the hazards associated with abnormal ovarian enlargement that may occur with MENOPUR therapy, treatment should be individualized and the lowest effective dose should be used [see Dosage and Administration (2.2)] . Use of ultrasound monitoring of ovarian response and/or measurement of serum estradiol levels is important to minimize the risk of ovarian stimulation [see Warnings and Precautions (5.10)] .
If the ovaries are abnormally enlarged on the last day of MENOPUR therapy, hCG should not be administered in order to reduce the chance of developing Ovarian Hyperstimulation Syndrome (OHSS) [see Warnings and Precautions (5.2)] . Prohibit intercourse in women with significant ovarian enlargement because of the danger of hemoperitoneum resulting from rupture of ovarian cysts [see Warnings and Precautions (5.2)] .
5.2 Ovarian Hyperstimulation Syndrome (OHSS)
OHSS is a medical event distinct from uncomplicated ovarian enlargement and may progress rapidly to become a serious medical event. OHSS is characterized by a dramatic increase in vascular permeability, which can result in a rapid accumulation of fluid in the peritoneal cavity, thorax, and potentially, the pericardium. The early warning signs of development of OHSS are severe pelvic pain, nausea, vomiting, and weight gain. Abdominal pain, abdominal distension, gastrointestinal symptoms including nausea, vomiting and diarrhea, severe ovarian enlargement, weight gain, dyspnea, and oliguria have been reported with OHSS. Clinical evaluation may reveal hypovolemia, hemoconcentration, electrolyte imbalances, ascites, hemoperitoneum, pleural effusion, hydrothorax, acute pulmonary distress, and thromboembolic reactions [see Warnings and Precautions (5.3)]. Transient liver function test abnormalities suggestive of hepatic dysfunction, with or without morphologic changes on liver biopsy, have been reported in association with OHSS.
OHSS occurs after gonadotropin treatment has been discontinued and it can develop rapidly, reaching its maximum about seven to ten days following treatment. Usually, OHSS resolves spontaneously with the onset of menses. If there is evidence that OHSS may be developing prior to hCG administration [see Warnings and Precautions (5.1)] , the hCG must be withheld.
Cases of OHSS are more common, more severe, and more protracted if pregnancy occurs; therefore, women should be assessed for the development of OHSS for at least two weeks after hCG administration.
If serious OHSS occurs, gonadotropins, including hCG, should be stopped and consideration should be given as to whether the woman needs to be hospitalized. Treatment is primarily symptomatic and overall should consist of bed rest, fluid and electrolyte management, and analgesics (if needed). Because the use of diuretics can accentuate the diminished intravascular volume, diuretics should be avoided except in the late phase of resolution as described below. The management of OHSS may be divided into three phases as follows:
- Acute Phase:
Management should be directed at preventing hemoconcentration due to loss of intravascular volume to the third space and minimizing the risk of thromboembolic phenomena and kidney damage. Fluid intake and output, weight, hematocrit, serum and urinary electrolytes, urine specific gravity, BUN and creatinine, total proteins with albumin: globulin ratio, coagulation studies, electrocardiogram to monitor for hyperkalemia, and abdominal girth should be thoroughly assessed daily or more often based on the clinical need. Treatment, consisting of limited intravenous fluids, electrolytes, human serum albumin, is intended to normalize electrolytes while maintaining an acceptable but somewhat reduced intravascular volume. Full correction of the intravascular volume deficit may lead to an unacceptable increase in the amount of third space fluid accumulation. - Chronic Phase:
After the acute phase is successfully managed as above, excessive fluid accumulation in the third space should be limited by instituting severe potassium, sodium, and fluid restriction. - Resolution Phase:
As third space fluid returns to the intravascular compartment, a fall in hematocrit and increasing urinary output are observed in the absence of any increase in intake. Peripheral and/or pulmonary edema may result if the kidneys are unable to excrete third space fluid as rapidly as it is mobilized. Diuretics may be indicated during the resolution phase, if necessary, to combat pulmonary edema.
Do not remove ascitic, pleural, and pericardial fluid unless there is the necessity to relieve symptoms such as pulmonary distress or cardiac tamponade.
OHSS increases the risk of injury to the ovary. Pelvic examination or intercourse may cause rupture of an ovarian cyst, which may result in hemoperitoneum, and should be avoided.
If bleeding occurs and requires surgical intervention, the clinical objective should be to control the bleeding and retain as much ovarian tissue as possible. A physician experienced in the management of this syndrome, or who is experienced in the management of fluid and electrolyte imbalances, should be consulted.
In the IVF clinical trial for MENOPUR, OHSS occurred in 7.2% of the 373 MENOPUR treated women.
5.3 Pulmonary and Vascular Complications
Serious pulmonary conditions (e.g. atelectasis, acute respiratory distress syndrome, and exacerbation of asthma) have been reported in women treated with gonadotropins. In addition, thromboembolic events both in association with, and separate from the Ovarian Hyperstimulation Syndrome (OHSS) have been reported in women treated with gonadotropins. Intravascular thrombosis and embolism, which may originate in venous or arterial vessels, can result in reduced blood flow to critical organs or the extremities. Women with generally recognized risk factors for thrombosis, such as personal or family history, severe obesity, or thrombophilia, may have an increased risk of venous or arterial thromboembolic events during or following treatment with gonadotropins. Sequelae of such reactions have included venous thrombophlebitis, pulmonary embolism, pulmonary infarction, cerebral vascular occlusion (stroke), and arterial occlusion resulting in loss of limb and rarely in myocardial infarctions. In rare cases, pulmonary complications and/or thromboembolic reactions have resulted in death. In women with recognized risk factors, the benefits of ovulation induction and assisted reproductive technology need to be weighed against the risks. Pregnancy also carries an increased risk of thrombosis.
5.4 Ovarian Torsion
Ovarian torsion has been reported after treatment with gonadotropins. This may be related to OHSS, pregnancy, previous abdominal surgery, past history of ovarian torsion, previous or current ovarian cyst, and polycystic ovaries. Damage to the ovary due to reduced blood supply can be limited by early diagnosis and immediate detorsion.
5.5 Multi-fetal Gestation and Birth
Multi-fetal gestation and births have been reported with all gonadotropin therapy including therapy with MENOPUR.
In the IVF clinical trial of MENOPUR, multiple pregnancy as diagnosed by ultrasound occurred in 35.3% (n=30) of 85 total pregnancies.
Before beginning treatment with MENOPUR, advise the woman and her partner of the potential risk of multi-fetal gestation and birth.
5.6 Congenital Malformations
The incidence of congenital malformations after some ART [specifically in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI)] may be slightly higher than after spontaneous conception. This slightly higher incidence is thought to be related to differences in parental characteristics (e.g., maternal age, maternal and paternal genetic background, sperm characteristics) and to the higher incidence of multi-fetal gestations after IVF or ICSI. There are no indications that the use of gonadotropins during IVF or ICSI is associated with an increased risk of congenital malformations.
5.7 Ectopic Pregnancy
Since infertile women undergoing ART often have tubal abnormalities, the incidence of ectopic pregnancy may be increased. Early confirmation of intrauterine pregnancy should be determined by β-hCG testing and transvaginal ultrasound.
5.8 Spontaneous Abortion
The risk of spontaneous abortion (miscarriage) is increased with gonadotropin products. However, causality has not been established. The increased risk may be a factor of the underlying infertility .
5.9 Ovarian Neoplasms
There have been infrequent reports of ovarian neoplasms, both benign and malignant, in women who have had multiple drug therapy for controlled ovarian stimulation; however, a causal relationship has not been established.
5.10 Laboratory Tests
In most instances, treatment of women with MENOPUR will result only in follicular growth and maturation. In the absence of an endogenous LH surge, hCG is given when monitoring of the woman indicates that sufficient follicular development has occurred. This may be estimated by ultrasound alone or in combination with measurement of serum estradiol levels. The combination of both ultrasound and serum estradiol measurement are useful for monitoring follicular growth and maturation, timing of the ovulatory trigger, detecting ovarian enlargement and minimizing the risk of the OHSS and multiple gestation.
The clinical confirmation of ovulation is obtained by direct or indirect indices of progesterone production as well as sonographic evidence of ovulation.
Direct or indirect indices of progesterone production:
- Urinary or serum luteinizing hormone (LH) rise
- A rise in basal body temperature
- Increase in serum progesterone
- Menstruation following the shift in basal body temperature
Sonographic evidence of ovulation:
- Collapsed follicle
- Fluid in the cul-de-sac
- Features consistent with corpus luteum formation
- Secretory endometrium
- Acute Phase:
-
6 ADVERSE REACTIONS
The following serious adverse reactions are discussed elsewhere in the labeling:
- Abnormal Ovarian Enlargement [see Warnings and Precautions (5.1)]
- Ovarian Hyperstimulation Syndrome [see Warnings and Precautions (5.2)]
- Atelectasis, acute respiratory distress syndrome and exacerbation of asthma [see Warnings and Precautions (5.3)]
- Thromboembolic events [see Warnings and Precautions (5.3)]
- Ovarian Torsion [see Warnings and Precautions (5.4)]
- Multi-fetal Gestation and Birth [see Warnings and Precautions (5.5)]
- Congenital Malformations [see Warnings and Precautions (5.6)]
- Ectopic Pregnancy [see Warnings and Precautions (5.7)]
- Spontaneous Abortion [see Warnings and Precautions (5.8)]
- Ovarian Neoplasms [see Warnings and Precautions (5.9)]
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trial of another drug and may not reflect the rates observed in practice.
In two single cycle, open label, multinational, multicenter, comparative trials, a total of 434 normal ovulatory infertile women were randomized and received subcutaneously administered MENOPUR as part of an in vitro fertilization (IVF) cycle (both trials) or intracytoplasmic sperm injection (ICSI) cycle (one of the two trials). All women received pituitary down-regulation with gonadotropin releasing hormone (GnRH) agonist before stimulation. Adverse Reactions occurring at an incidence of ≥ 2% in women receiving MENOPUR are shown in Table 1.
Table 1: MENOPUR Administered Subcutaneously in Women Undergoing IVF and ICSI. Adverse Reactions with Incidence of 2% or Greater Occurring on or After GnRH Administration. IVF
n=434Body System/Preferred Term N % Body as a whole Abdominal cramps 13 3.0 Abdomen enlarged 10 2.3 Abdominal pain 29 6.7 Headache 27 6.2 Injection site pain + reaction 17 3.9 Injection site inflammation 10 2.3 Urogenital Ovarian Hyperstimulation Syndrome (OHSS) 27 6.2 In addition, thrombophlebitis was reported in less than 1% of subjects.
In an open label, US, multicenter, comparative IVF and ICSI trial, MENOPUR and BRAVELLE were administered in the same syringe to 60 normal ovulatory infertile women. OHSS, post retrieval cramping and nausea and spontaneous abortion were the most common adverse reactions occurring at an incidence of ≥ 5% in women receiving the combination of MENOPUR and BRAVELLE.
In another open label, US multicenter, comparative trial for ovulation induction in anovulatory or oligovulatory infertile women, 76 subjects received subcutaneous or intramuscular injections of MENOPUR. The most common adverse reactions occurring at an incidence of ≥ 5% in women receiving MENOPUR were: headache; OHSS; injection site reaction, abdominal cramps, fullness and pain; and nausea.
6.2 Postmarketing Experience
The following adverse reactions have been reported during postmarketing use of gonadotropins. Because these reactions were reported voluntarily from a population of uncertain size, the frequency or a causal relationship to MENOPUR cannot be reliably determined.
Gastrointestinal disorders: abdominal pain, abdominal pain lower, abdominal distension, nausea, vomiting, abdominal discomfort
General disorders and administration site conditions: injection site reactions (most frequently reported injection site reaction was injection site pain), fatigue
Nervous system disorders: headache, dizziness
Reproductive system disorders: OHSS [see Warnings and Precautions (5.2)] , pelvic pain, ovarian cyst, breast complaints (including breast pain, breast tenderness, breast discomfort, and breast swelling)
Skin and subcutaneous tissue disorders: acne, rash
Vascular disorders: hot flush
- 7 DRUG INTERACTIONS
-
8 USE IN SPECIFIC POPULATIONS
8.3 Nursing Mothers
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in the nursing infant from MENOPUR, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
-
10 OVERDOSAGE
Aside from possible OHSS [see Warnings and Precautions (5.2)] and multiple gestations [see Warnings and Precautions (5.5)] , there is no additional information on the consequences of acute overdosage with MENOPUR.
-
11 DESCRIPTION
MENOPUR is a preparation of gonadotropins (FSH and LH activity), extracted from the urine of postmenopausal women, which has undergone additional steps for purification.
MENOPUR is a sterile, lyophilized powder intended for subcutaneous (SC) injection after reconstitution with sterile 0.9% Sodium Chloride Injection, USP. Each vial of MENOPUR contains 75 International Units of follicle-stimulating hormone (FSH) activity and 75 International Units of luteinizing hormone (LH) activity, plus 21 mg lactose monohydrate and 0.005 mg Polysorbate 20 and Sodium Phosphate Buffer (Sodium Phosphate Dibasic, Heptahydrate and Phosphoric Acid).
The biological activity of MENOPUR is determined using the bioassays for FSH (ovarian weight gain assay in female rats) and LH (seminal vesicle weight gain assay in male rats), modified to increase the accuracy and reproducibility of these assays. The FSH and LH activity assays are standardized using the Fourth International Standard for Urinary FSH and Urinary LH, November 2000, by the Expert Committee on Biological Standardization of the World Health Organization (WHO ECBS). Both FSH and LH are glycoproteins that are acidic and water-soluble. Human Chorionic Gonadotropin (hCG) is detected in MENOPUR.
MENOPUR has been mixed in vitro with BRAVELLE with no evidence of aggregation.
Therapeutic class: Infertility
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
MENOPUR, administered for 7 to 20 days, produces ovarian follicular growth and maturation in women who do not have primary ovarian failure. Treatment with MENOPUR in most instances results only in follicular growth and maturation. When sufficient follicular maturation has occurred, hCG must be given to induce ovulation.
12.3 Pharmacokinetics
Two open-label, randomized, controlled trials were conducted to assess the pharmacokinetics of MENOPUR. Study 2003-02 compared single doses of subcutaneous administration of the US and European (EU) formulations of MENOPUR in 57 healthy, pre-menopausal females who had undergone pituitary suppression. The study established that the two formulations are bioequivalent. Study 2000-03 assessed single and multiple doses of MENOPUR administered subcutaneously and intramuscularly in a 3 phase crossover design in 33 healthy, pre-menopausal females who had undergone pituitary suppression. The primary pharmacokinetic endpoints were FSH AUC and C max values. The results are summarized in Table 2.
Table 2: FSH Pharmacokinetic Parameters [Mean (SD)] Following MENOPUR Administration (Study 2000-03) PK Parameters Single Dose
(225 IU)Multiple Dose
(225 IU × 1 day then 150 IU × 6 days)Subcutaneous Intramuscular Subcutaneous Intramuscular - * Single dose C max, AUC 120 and multiple dose C maxss, AUC ss
C max* (mIU/mL) 8.5 (2.5) 7.8 (2.4) 15.0 (3.6) 12.5 (2.3) T max (hr) 17.9 (5.8) 27.5 (25.4) 8.0 (3.0) 9.0 (7.0) AUC†
(hr-mlU/mL)726.2 (243.0) 656.1 (233.7) 622.7 (153.0) 546.2 (91.2) - 13 NONCLINICAL TOXICOLOGY
-
14 CLINICAL STUDIES
The efficacy of MENOPUR was established in one randomized, open-label, multicenter, multinational (in Europe and Israel), comparative clinical trial of women undergoing in vitro fertilization (IVF) or IVF plus intracytoplasmic injection (ICSI) to achieve pregnancy.
All women began ovarian stimulation as part of an IVF cycle following pituitary suppression with a GnRH agonist. A total of 373 patients were randomized to the MENOPUR arm. Randomization was stratified by insemination technique [conventional IVF vs. ICSI]. Efficacy was assessed based on the primary efficacy parameter of continuing pregnancy. The initial daily dose of MENOPUR was 225 International Units administered subcutaneously for five days. Thereafter, the dose was individualized according to each patient's response, up to a maximum of 450 IU/day for a total maximum duration of stimulation of 20 days. Treatment outcomes are summarized in Table 3.
Table 3: Efficacy Outcome in IVF Study (one cycle of treatment) Parameter Subcutaneously Administered MENOPUR n=373 - * Continuing pregnancy was defined as ultrasound visualization of gestational sac with fetal heartbeat at ≥10 weeks after ET
- † Non-inferior to comparator recombinant human FSH based on a two-sided 95% confidence interval, intent-to-treat analysis
- ‡ Secondary efficacy parameter. Study was not powered to demonstrate differences in this parameter
Continuing Pregnancy (%) * 87 (23) † Clinical Pregnancy (%) 98 (26) ‡ -
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
MENOPUR (menotropins for injection) is supplied in sterile vials as a lyophilized, white to off-white powder or pellet.
Each vial of MENOPUR is accompanied by a vial of sterile diluent containing 2 mL of 0.9% Sodium Chloride for Injection, USP:
75 International Units FSH and 75 International Units of LH activity, supplied as
NDC: 55566-7501-2: Box of 5 vials + 5 vials diluent + 5 QCap vial adapters
-
17 PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling ( Patient Information and Instructions for Use).
17.1 Dosing and Use
Instruct women on the correct usage and dosing of MENOPUR [see Dosage and Administration (2.2)] . Caution women not to change the dosage or the schedule of administration unless she is told to do so by her healthcare provider.
17.2 Duration and Monitoring Required
Prior to beginning therapy with MENOPUR, inform women about the time commitment and monitoring procedures necessary for treatment [see Dosage and Administration (2.2) and Warnings and Precautions (5.10)] .
17.3 Instructions Regarding a Missed Dose
Inform the woman that if she misses or forgets to take a dose of MENOPUR, the next dose should not be doubled and she should call her healthcare provider for further dosing instructions.
17.4 Ovarian Hyperstimulation Syndrome
Inform women regarding the risks of OHSS [see Warnings and Precautions (5.2)] and OHSS-associated symptoms including lung and blood vessel problems [see Warnings and Precautions (5.3)] and ovarian torsion [see Warnings and Precautions (5.4)] with the use of MENOPUR.
17.5 Multi-fetal Gestation and Birth
Inform women regarding the risk of multi-fetal gestation and birth with the use of MENOPUR [see Warnings and Precautions (5.5)]
Vials of sterile diluent of 0.9% Sodium Chloride Injection, USP manufactured for Ferring Pharmaceuticals Inc.
- SPL UNCLASSIFIED SECTION
-
Patient Information
MENOPUR ® (Men-oh-pyoor)
(menotropins for injection)
for subcutaneous useRead this Patient Information before you start using MENOPUR ® (menotropins for injection) and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or your treatment.
What is MENOPUR?
MENOPUR is a prescription medicine that contains follicle stimulating hormone (FSH) and luteinizing hormone (LH). MENOPUR causes your ovaries to make multiple (more than 1) eggs as part of an Assisted Reproductive Technology (ART) cycle.
Who should not use MENOPUR?
Do not use MENOPUR if you:
- are allergic to menotropins or any of the ingredients in MENOPUR. See the end of this leaflet for a complete list of ingredients in MENOPUR.
- have ovaries that no longer make eggs (primary ovarian failure)
- are pregnant or think you may be pregnant. If MENOPUR is taken while you are pregnant, it may harm your baby.
- have problems with your thyroid gland, adrenal gland or pituitary gland that are not controlled by taking medicine.
- have a tumor in your female organs, including your ovaries, breast, or uterus that may get worse with high levels of estrogen
- have a tumor of your pituitary gland or hypothalamus
- have abnormal bleeding from your uterus or vagina and the cause is not known
- have ovarian cysts or enlarged ovaries, not due to a problem called polycystic ovary syndrome (PCOS)
What should I tell my healthcare provider before using MENOPUR?
Before you use MENOPUR, tell your healthcare provider if you:
- have been told by a healthcare provider that you are at an increased risk for blood clots (thrombosis)
- have ever had a blood clot (thrombosis), or anyone in your family has ever had a blood clot
- had twisting of your ovary (ovarian torsion)
- had or have a cyst in your ovary
- have any other medical conditions
- are breast feeding or plan to breast feed. It is not known if MENOPUR passes into your breast milk. You and your healthcare provider should decide if you will use MENOPUR or breastfeed. You should not do both.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.
How should I use MENOPUR?
- Read the Instructions for Use at the end of this Patient Information about the right way to use MENOPUR or MENOPUR mixed with BRAVELLE ® (urofollitropin for injection, purified).
- Use MENOPUR exactly as your healthcare provider tells you to use it.
- Your healthcare provider will tell you how much MENOPUR to use and when to use it.
- Your healthcare provider may change your dose of MENOPUR if needed.
- If you miss a dose of MENOPUR, call your healthcare provider right away. Do not double the amount of MENOPUR you are using.
- You may need more than 1 vial of MENOPUR for your dose.
- MENOPUR may be mixed with BRAVELLE in the same syringe.
What are possible side effects of MENOPUR?
MENOPUR may cause serious side effects, including:
- ovaries that are too large. MENOPUR may cause your ovaries to be abnormally large. Symptoms of large ovaries include bloating or pain in your lower stomach (pelvic) area. If your ovaries become too large your healthcare provider may tell you that you should not have intercourse (sex) so you do not rupture an ovarian cyst.
-
ovarian hyperstimulation syndrome (OHSS). Using MENOPUR may cause OHSS. OHSS is a serious medical condition that can happen when your ovaries produce too many eggs (overstimulated). OHSS can cause fluid to suddenly build up in the area of your stomach, chest, heart, and cause blood clots to form. OHSS may also happen after you stop using MENOPUR. Stop using MENOPUR and call your healthcare provider or go to the nearest hospital emergency room right away if you have any of the following symptoms of OHSS:
- severe pelvic or stomach pain
- nausea
- vomiting
- sudden weight gain
- swollen stomach
- diarrhea
- trouble breathing
- decreased or no urine
- lung problems. MENOPUR may cause serious lung problems that can sometimes lead to death including fluid in the lungs, trouble breathing, and worsening of asthma.
-
blood clots. MENOPUR may increase your chance of having blood clots in your blood vessels. Blood clots can cause:
- blood vessel problems (thrombophlebitis)
- stroke
- loss of your arm or leg
- blood clot in your lung (pulmonary embolus)
- twisting (torsion) of your ovary. MENOPUR may increase the chance of your ovary twisting, if you already have certain conditions such as OHSS, pregnancy, and previous abdominal surgery. Twisting of your ovary may lead to blood flow being cut off to your ovary.
- pregnancy with and birth of multiple babies. MENOPUR may increase your chance of having a pregnancy with more than 1 baby. Having a pregnancy and giving birth to more than 1 baby at a time increases the health risk for you and your babies. Your healthcare provider should talk to you about your chances of multiple births before you start using MENOPUR.
- birth defects. Babies born after ART may have an increased chance of birth defects. Your age, certain sperm problems, your genetic background, and that of your partner, and a pregnancy with more than 1 baby at a time may increase the chance that your baby may have birth defects.
- ectopic pregnancy (pregnancy outside your womb). MENOPUR may increase your chance of having a pregnancy that is abnormally outside of your womb. Your chance of having a pregnancy outside of your womb is increased if you also have fallopian tube problems.
- miscarriage. Your chance of loss of an early pregnancy may be increased if you had difficulty becoming pregnant.
- tumors of the ovary. If you have used medicines like MENOPUR more than 1 time to get pregnant, you may have an increased chance of having tumors in your ovaries, including cancer.
The most common side effects of MENOPUR include:
- stomach cramps, fullness or pain
- headache
- injection site swelling, heat, redness and pain
These are not all the possible side effects of MENOPUR. For more information, ask your healthcare provider or pharmacist.
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
How should I store MENOPUR?
- Before mixing, store MENOPUR powder in the refrigerator or at room temperature between 37ºF to 77ºF (3ºC to 25ºC).
- Protect MENOPUR from light.
- MENOPUR should be used right after mixing.
- Throw away any unused MENOPUR.
Keep MENOPUR and all medicines out of the reach of children.
General Information about the safe and effective use of MENOPUR.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use MENOPUR for a condition for which it was not prescribed. Do not give MENOPUR to other people, even if they have the same condition you have. It may harm them.
This Patient Information summarizes the most important information about MENOPUR. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about MENOPUR that is written for health professionals.
For more information go to www.menopur.com, or call 1-888-FERRING (1-888-337-7464).
What are the ingredients in MENOPUR?
Active ingredient: menotropins
Inactive ingredients: lactose monohydrate, polysorbate, sodium phosphate buffer (sodium phosphate dibasic, heptahydrate and phosphoric acid)
-
Instructions for Use
MENOPUR ® (Men-oh-pyoor)
(menotropins for injection)
for subcutaneous use
Your healthcare provider should show you how to mix and inject MENOPUR ® (menotropins for injection) or MENOPUR mixed with BRAVELLE ® (urofollitropin for injection, purified) before you do it for the first time. Before using MENOPUR or MENOPUR mixed with BRAVELLE for the first time, read this Instructions for Use carefully. Keep this leaflet in a safe place and read it when you have questions.
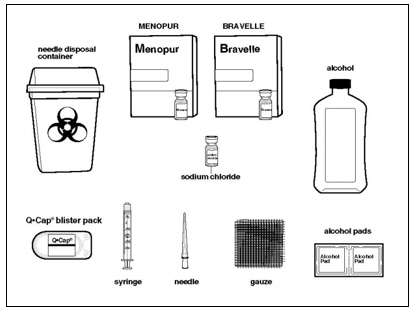
Supplies you will need to give your injection of MENOPUR or MENOPUR mixed with BRAVELLE. See Figure A.
- a clean, flat surface to work on, like a table
- vials of MENOPUR powder (and BRAVELLE powder if you are going to mix the 2 medicines)
- 1 vial of 0.9% Sodium Chloride, USP used for mixing the medicine
- alcohol pads
- rubbing alcohol
- gauze pads
- 1 sterile syringe and 1 sterile needle with cap. Your healthcare provider should tell you which syringe and needle to use.
- the QCap ® (vial adapter) that comes with your medicine
- a sharps disposal container for throwing away your used needles and syringes. See " Disposing of your used needles and syringes" at the end of these instructions.
Step 1. Preparing your MENOPUR or MENOPUR mixed with BRAVELLE.
- Wash your hands well with soap and water and dry them with a clean towel.
- Place all the supplies you need on the clean surface you already prepared.
- Check the vial(s) of MENOPUR (and BRAVELLE if needed) to make sure there is powder or a pellet in the vial(s). If you do not see any powder in the vial(s) do not use the vial and call your pharmacist or healthcare provider.
- Check the 0.9% Sodium Chloride, USP vial to make sure that the liquid is clear and does not contain any particles. If you see any particles in the liquid or the liquid is discolored, do not use the vial and call your pharmacist or healthcare provider.
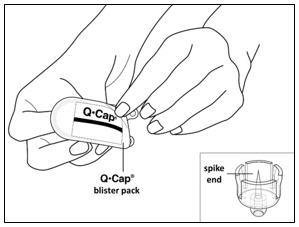
- Check the QCap blister pack package to make sure it is intact. Do not use if the package is damaged.
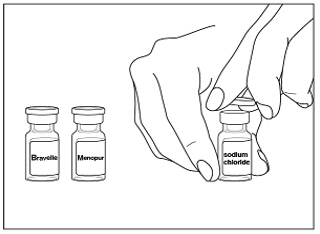
- Remove the plastic cap(s) from the vial(s) of MENOPUR (and BRAVELLE if needed) and 0.9% Sodium Chloride, USP vial(s). See Figure B.
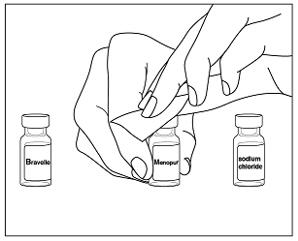
- Wipe the tops of the vials with alcohol and allow them to dry. Do not touch the tops of the vials after you have wiped them. See Figure C.
- Place the vial of 0.9% Sodium Chloride, USP on the table.
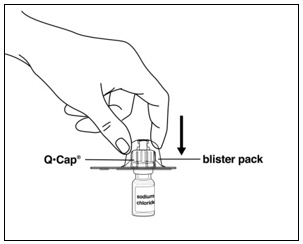
- Open the QCap blister pack by peeling back the lidding (See Figure D) . Do not take the QCap out of the blister pack at this time. Do not touch the spike or connector (luer) ends of the QCap.
- Hold the 0.9% Sodium Chloride, USP vial in 1 hand. With your other hand, hold the sides of the QCap blister pack, turn the QCap blister pack over, and place it on top of the vial. Push the QCap straight down into the rubber stopper of the vial until the QCap spike pierces the top of the vial and snaps into place.
See
Figure E.
- Do not use the QCap if it falls out of the blister pack. Throw it away and get a new one.
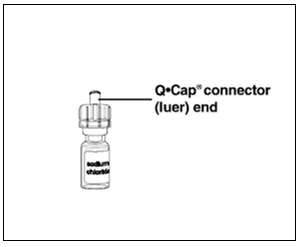
- Remove the blister pack and throw it away in your household trash. Do not touch the connector end (luer) of the QCap. See Figure F.
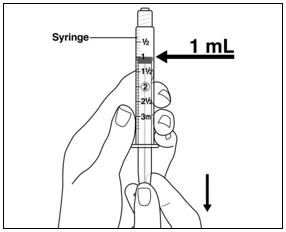
- Take the syringe and pull down on the syringe plunger rod until you have reached the line that corresponds with amount of 0.9% Sodium Chloride, USP that your healthcare provider told you to use (typically 1 mL). Air is just being drawn into the syringe at this step.
See
Figure G.
NOTE: The usual amount of 0.9% Sodium Chloride, USP used to mix your MENOPUR is 1 mL .
-
- Be very careful not to touch the syringe plunger during this step.
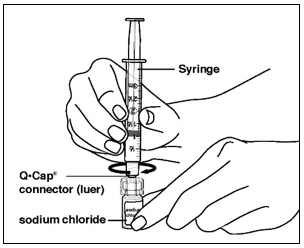
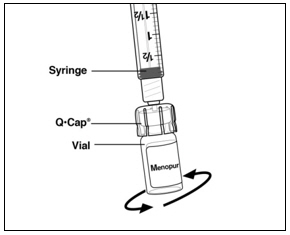
- Place the tip of the syringe into the connector end (luer) of the QCap then twist the syringe clockwise until it is tight. Be careful not to overtighten the syringe. See Figure H.
- Slowly push down on the syringe plunger to push the air from the syringe into the vial. See Figure I.
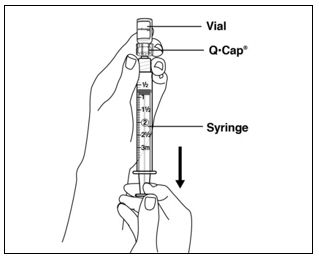
- Keeping the syringe and QCap together, turn the vial upside down and pull down on the syringe plunger to withdraw the right amount of 0.9% Sodium Chloride, USP from the vial. Your healthcare provider should tell you the right amount of 0.9% Sodium Chloride, USP to use. See Figure J.
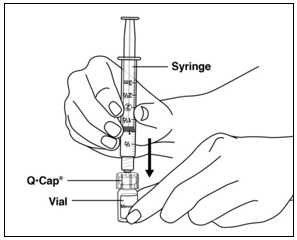
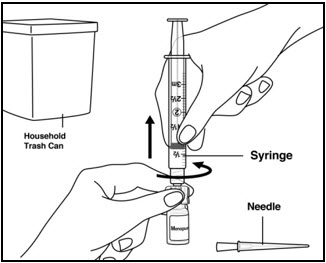
- Separate the QCap and syringe from the vial by pulling up on the syringe barrel. Do not pull the plunger to remove the QCap. Throw away 0.9% Sodium Chloride, USP vial in your household trash. See Figure K.
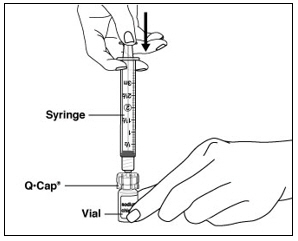
- Hold the vial of MENOPUR powder in 1 hand. With your other hand, hold the sides of the syringe with the QCap attached and place the tip of the QCap over the top of the vial. Push the tip of the QCap into the rubber stopper on the top of the vial until it stops and snaps into place. Be careful not to push down on the syringe plunger during this step. See Figure L. You may see the powder dissolve as the QCap snaps into place, but continue with the steps listed below.
- Slowly push down on the syringe plunger to push the 0.9% Sodium Chloride, USP into the vial with the MENOPUR powder in it. The entire amount of the 0.9% Sodium Chloride, USP in the syringe should be added . Gently swirl the vial until the MENOPUR powder is completely dissolved. Do not shake the vial as this will cause bubbles. See Figure M.
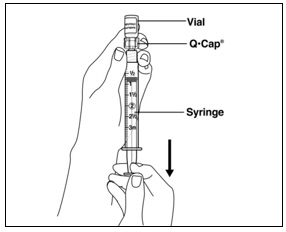
- As soon as the powdered medicine has completely dissolved, push the plunger down to empty any remaining air from the syringe, then turn the vial upside down and slowly pull down on the plunger to withdraw all of the MENOPUR into the syringe.
See
Figure N.
- Be careful not to pull the plunger stopper all the way out of the syringe barrel.
If your healthcare provider tells you to use more than 1 vial of MENOPUR or tells you to mix your MENOPUR with BRAVELLE in the same syringe:
- Mix your first vial of MENOPUR powder or BRAVELLE powder with 0.9% Sodium Chloride, USP. Do not inject your dose yet.
- Use the liquid in the syringe you have just mixed to mix the next vial of MENOPUR or BRAVELLE. See Figures K through M.
- You can use the liquid in the syringe to mix up to 5 more vials of medicine.
- Your healthcare provider will tell you how many vials of MENOPUR and BRAVELLE to use.
Step 2. Removing the QCap and adding your needle for injection.
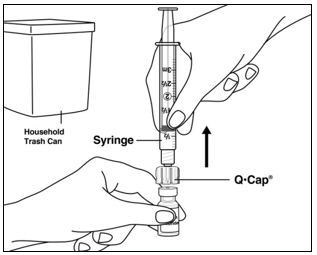
- When you have finished mixing the last vial needed for your injection and have withdrawn all the medicine into the syringe, remove the syringe from the QCap by twisting the syringe counter-clockwise while holding the QCap steady. See Figure O. Throw away the QCap with the attached vial into your household trash.
- You are now ready to attach the needle to the syringe for your injection.
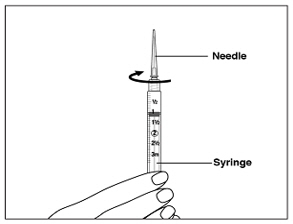
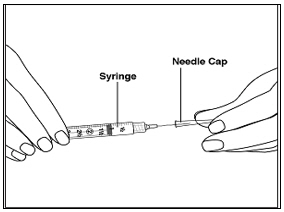
Your healthcare provider will tell you what needle you should use for your injection. - While holding the syringe with the syringe tip pointing up, place the needle on the top of the syringe. Gently push down on the needle and twist the needle onto the syringe in a clockwise direction until it is tight. See Figure P.
-
Do not remove the needle cap until you are ready for your injection. (
See
Step 4)
- Carefully set the syringe with the needle down on the table. See Figure Q.
Step 3. Prepare Injection site for MENOPUR or MENOPUR mixed with BRAVELLE.
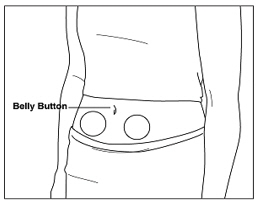
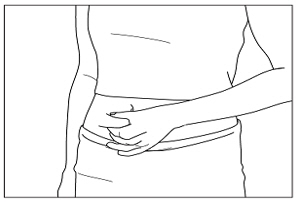
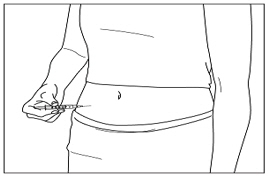
- Select a site to inject MENOPUR or MENOPUR mixed with BRAVELLE on your stomach area (abdomen).
- Pick a site on your lower abdomen, 1-2 inches below the navel, alternating between left and right sides.
- Each day, inject in a different site to help reduce soreness and skin problems. For example, on day 1, inject yourself on the right side of your abdomen. The next day, inject yourself on the left side of your abdomen. Changing your injection sites every day will help reduce soreness and skin problems. See Figure R.
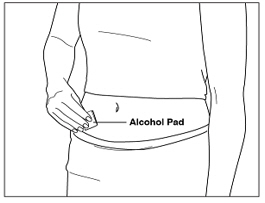
- Clean your injection site with an alcohol pad. Let the alcohol dry. See Figure S.
- Carefully remove the needle cap from the syringe. See Figure T.
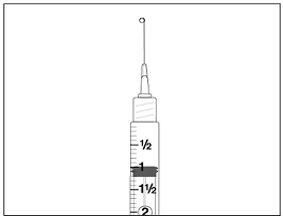
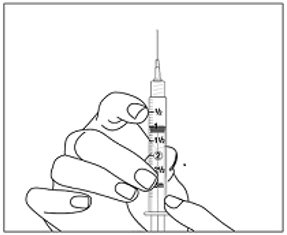
- Hold the syringe with the needle pointing straight up. Pull down slightly on the plunger and tap the barrel of the syringe so that any air bubbles rise to the top. Slowly press the plunger up until all the air is out of the syringe and a small drop of liquid is seen at the tip of the needle. See Figure U.
- Tap the syringe to remove the small drop of liquid at the tip of the needle. Do not let the needle touch anything to keep it sterile. See Figure V.
- The medicine is now ready for you to inject. See Figure V.
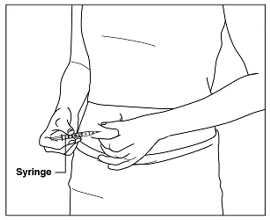
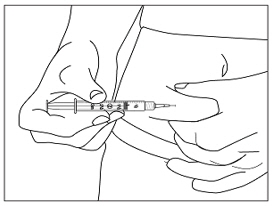
- Hold the syringe in 1 hand. Use your other hand to gently pinch a fold of cleaned skin where you will insert your needle. Hold the skin between your thumb and index finger. See Figure W.
- Hold your syringe at a right angle to your skin. Quickly insert the needle all the way into your skin fold. See Figure X.
- Push down the plunger of the syringe with a steady motion. Keep pushing until all the fluid is injected into your skin. See Figure Y.
- Let go of your skin fold and pull the needle straight out of your skin. See Figure Z.
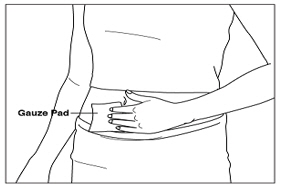
- If there is any bleeding at your injection site, place a gauze pad over your injection site. Apply gentle pressure to stop the bleeding. Do not rub the site. See Figure AA.
- If your injection site becomes sore or red, you may put ice on your injection site for 1 minute and then take it off for 3 minutes. If needed, you may repeat this 3 or 4 times.
Step 6. Disposing of your used needles and syringes.
- Put your used needles and syringes in a FDA-cleared sharps disposal container right away after use. Do not throw away loose needles and syringes in your household trash.
- If you do not have a FDA-cleared sharps disposal container, you may use a household container that:
- is made of a heavy-duty plastic,
- can be closed with a tight-fitting, puncture-resistant lid, without sharps being able to come out,
- remains upright and stable during use,
- is leak-resistant, and
- is properly labeled to warn of hazardous waste inside the container.
- When your sharps disposal container is almost full, you will need to follow your community guidelines for the right way to dispose of your sharps disposal container. There may be state or local laws about how you should throw away used needles and syringes. For more information about safe sharps disposal, and for specific information about sharps disposal in the state that you live in, go to the FDA's website at: http://www.fda.gov/safesharpsdisposal.
Do not dispose of your used sharps disposal container in your household trash unless your community guidelines permit this. Do not recycle your used sharps disposal container.
This Instructions for Use has been approved by the U.S. Food and Drug Administration.
- SPL UNCLASSIFIED SECTION
-
PRINCIPAL DISPLAY PANEL - Kit Carton
NDC: 55566-7501-2
Menopur® 75 IU
(menotropins for injection)5 single dose vials of Menotropins for Injection
5 single dose vials of 0.9% Sodium Chloride Injection, USP, 2 mL
5 QCap ® Vial AdaptersFOR SUBCUTANEOUS
INJECTION ONLYRx only
QCap®
Vial Adapters
for Needle-Free
ReconstitutionFor exclusive use with
Ferring reproductive health productsFERRING
PHARMACEUTICALS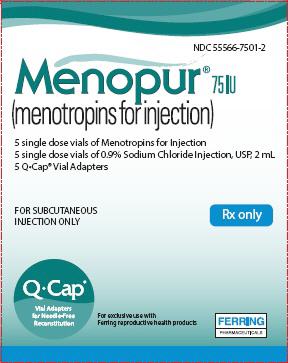
-
INGREDIENTS AND APPEARANCE
MENOPUR
menotropins kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 55566-7501 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 55566-7501-2 1 in 1 CARTON; Type 0: Not a Combination Product 10/29/2004 Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 5 VIAL 5 mL Part 2 5 VIAL 10 mL Part 1 of 2 MENOPUR
menotropins injection, powder, lyophilized, for solutionProduct Information Item Code (Source) NDC: 55566-7502 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength FOLLITROPIN (UNII: 076WHW89TW) (FOLLITROPIN - UNII:076WHW89TW) FOLLITROPIN 75 [iU] in 1 mL LUTEINIZING HORMONE (UNII: 8XA4VN1LH4) (LUTEINIZING HORMONE - UNII:8XA4VN1LH4) LUTEINIZING HORMONE 75 [iU] in 1 mL Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) 11.5 mg in 1 mL POLYSORBATE 20 (UNII: 7T1F30V5YH) SODIUM PHOSPHATE, DIBASIC, HEPTAHYDRATE (UNII: 70WT22SF4B) Product Characteristics Color white Score Shape Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 55566-7502-0 1 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA021663 10/29/2004 Part 2 of 2 SODIUM CHLORIDE
sodium chloride injectionProduct Information Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) (CHLORIDE ION - UNII:Q32ZN48698, SODIUM CATION - UNII:LYR4M0NH37) SODIUM CHLORIDE 9 mg in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 2 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA021663 10/29/2004 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA021663 10/29/2004 Labeler - Ferring Pharmaceuticals Inc. (103722955) Establishment Name Address ID/FEI Business Operations Ferring Production Inc. 079510999 label(55566-7501) , pack(55566-7501) , manufacture(55566-7501) Establishment Name Address ID/FEI Business Operations Sharp Corporation 143696495 pack(55566-7501) Establishment Name Address ID/FEI Business Operations Jubilant HollisterStier General Partnership 246762764 manufacture(55566-7501) , pack(55566-7501) Establishment Name Address ID/FEI Business Operations Ferring GmbH 328609615 manufacture(55566-7501) , pack(55566-7501) Establishment Name Address ID/FEI Business Operations Patheon Italia S.p.a. 338336589 manufacture(55566-7501) Establishment Name Address ID/FEI Business Operations Patheon Italia S.p.A. 434078638 manufacture(55566-7501) Establishment Name Address ID/FEI Business Operations Hikma Pharmaceuticals USA Inc. 946499746 manufacture(55566-7501) Establishment Name Address ID/FEI Business Operations F.M. Howell & Company 962888116 pack(55566-7501) Establishment Name Address ID/FEI Business Operations Instituto Massone S.A. 970053831 api manufacture(55566-7501)
Trademark Results [Menopur]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 MENOPUR 88228425 not registered Live/Pending |
Ferring B.V. 2018-12-13 |
 MENOPUR 76458482 2989995 Live/Registered |
Ferring B.V. 2002-10-16 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.