COSOPT- dorzolamide hydrochloride and timolol maleate solution/ drops
COSOPT by
Drug Labeling and Warnings
COSOPT by is a Prescription medication manufactured, distributed, or labeled by Thea Pharma Inc., Akorn AG. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use COSOPT safely and effectively. See full prescribing information for COSOPT.
COSOPT ® (dorzolamide hydrochloride and timolol maleate ophthalmic solution), for topical ophthalmic use
Initial U.S. Approval: 1998INDICATIONS AND USAGE
- COSOPT is a combination of dorzolamide hydrochloride, a carbonic anhydrase inhibitor, and timolol maleate, a beta-adrenergic receptor blocking agent, indicated for the reduction of elevated intraocular pressure (IOP) in patients with open-angle glaucoma or ocular hypertension who are insufficiently responsive to beta-blockers.
- The IOP-lowering of COSOPT twice daily was slightly less than that seen with the concomitant administration of 0.5% timolol twice daily, and 2% dorzolamide three times daily. ( 1)
DOSAGE AND ADMINISTRATION
The dose is one drop of COSOPT in the affected eye(s) two times daily. ( 2)
DOSAGE FORMS AND STRENGTHS
Ophthalmic solution containing dorzolamide 20 mg/mL (2%) and timolol 5 mg/mL (0.5%). ( 3)
CONTRAINDICATIONS
COSOPT is contraindicated in patients with:
WARNINGS AND PRECAUTIONS
- Potentiation of Respiratory Reactions Including Asthma ( 5.1)
- Cardiac Failure ( 5.2)
- Sulfonamide Hypersensitivity ( 5.3)
- Obstructive Pulmonary Disease ( 5.4)
- Increased Reactivity to Allergens ( 5.5)
- Potentiation of Muscle Weakness ( 5.6)
- Masking of Hypoglycemic Symptoms in Patients with Diabetes Mellitus ( 5.7)
- Masking of Thyrotoxicosis ( 5.8)
- Renal and Hepatic Impairment ( 5.9)
- Impairment of Beta-Adrenergically Mediated Reflexes During Surgery ( 5.10)
ADVERSE REACTIONS
The most frequently reported adverse reactions were taste perversion (bitter, sour, or unusual taste) or ocular burning and/or stinging in up to 30% of patients. Conjunctival hyperemia, blurred vision, superficial punctate keratitis or eye itching were reported between 5 to 15% of patients. ( 6)
To report SUSPECTED ADVERSE REACTIONS, contact Thea Pharma Inc., at 1-833-838-4028 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- Potential additive effect of oral carbonic anhydrase inhibitor with COSOPT. ( 7.1)
- Potential acid-base and electrolyte disturbances. ( 7.2)
- Concomitant use with systemic beta-blockers may potentiate systemic beta-blockade. ( 7.3)
- Oral or intravenous calcium antagonists may cause atrioventricular conduction disturbances, left ventricular failure, and hypotension. ( 7.4)
- Catecholamine-depleting drugs may have additive effects and produce hypotension and/or marked bradycardia. ( 7.5)
- Digitalis and calcium antagonists, may have additive effects in prolonging atrioventricular conduction time. ( 7.6)
- CYP2D6 inhibitors may potentiate systemic beta-blockade. ( 7.7)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 5/2022
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
4.1 Asthma, COPD
4.2 Sinus Bradycardia, AV Block, Cardiac Failure, Cardiogenic Shock
4.3 Hypersensitivity
5 WARNINGS AND PRECAUTIONS
5.1 Potentiation of Respiratory Reactions Including Asthma
5.2 Cardiac Failure
5.3 Sulfonamide Hypersensitivity
5.4 Obstructive Pulmonary Disease
5.5 Increased Reactivity to Allergens
5.6 Potentiation of Muscle Weakness
5.7 Masking of Hypoglycemic Symptoms in Patients with Diabetes Mellitus
5.8 Masking of Thyrotoxicosis
5.9 Renal and Hepatic Impairment
5.10 Impairment of Beta-Adrenergically Mediated Reflexes During Surgery
5.11 Corneal Endothelium
5.12 Bacterial Keratitis
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Oral Carbonic Anhydrase Inhibitors
7.2 High-Dose Salicylate Therapy
7.3 Beta-Adrenergic Blocking Agents
7.4 Calcium Antagonists
7.5 Catecholamine-Depleting Drugs
7.6 Digitalis and Calcium Antagonists
7.7 CYP2D6 Inhibitors
7.8 Clonidine
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
COSOPT ® is indicated for the reduction of elevated intraocular pressure (IOP) in patients with open-angle glaucoma or ocular hypertension who are insufficiently responsive to beta-blockers (failed to achieve target IOP determined after multiple measurements over time). The IOP-lowering of COSOPT administered twice a day was slightly less than that seen with the concomitant administration of 0.5% timolol administered twice a day and 2% dorzolamide administered three times a day [see Clinical Studies (14)] .
-
2 DOSAGE AND ADMINISTRATION
The dose is one drop of COSOPT in the affected eye(s) two times daily.
If more than one topical ophthalmic drug is being used, the drugs should be administered at least five minutes apart [see Drug Interactions (7.3)] .
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
4.1 Asthma, COPD
COSOPT is contraindicated in patients with bronchial asthma, a history of bronchial asthma, or severe chronic obstructive pulmonary disease [see Warnings and Precautions (5.1)] .
4.2 Sinus Bradycardia, AV Block, Cardiac Failure, Cardiogenic Shock
COSOPT is contraindicated in patients with sinus bradycardia, second or third degree atrioventricular block, overt cardiac failure, and cardiogenic shock [see Warnings and Precautions (5.2)] .
4.3 Hypersensitivity
COSOPT is contraindicated in patients who are hypersensitive to any component of this product [see Warnings and Precautions (5.3)] .
-
5 WARNINGS AND PRECAUTIONS
5.1 Potentiation of Respiratory Reactions Including Asthma
COSOPT contains timolol maleate, a beta-adrenergic blocking agent; and although administered topically, is absorbed systemically. Therefore, the same types of adverse reactions that are attributable to systemic administration of beta-adrenergic blocking agents may occur with topical administration. For example, severe respiratory reactions, including death due to bronchospasm in patients with asthma, and rarely death in association with cardiac failure, have been reported following systemic or ophthalmic administration of timolol maleate [see Contraindications (4.1)] .
5.2 Cardiac Failure
Sympathetic stimulation may be essential for support of the circulation in individuals with diminished myocardial contractility, and its inhibition by beta-adrenergic receptor blockade may precipitate more severe failure.
In patients without a history of cardiac failure continued depression of the myocardium with beta-blocking agents over a period of time can, in some cases, lead to cardiac failure. At the first sign or symptom of cardiac failure, COSOPT should be discontinued [see Contraindications (4.2)] .
5.3 Sulfonamide Hypersensitivity
COSOPT contains dorzolamide, a sulfonamide; and although administered topically, it is absorbed systemically. Therefore, the same types of adverse reactions that are attributable to sulfonamides may occur with topical administration of COSOPT. Fatalities have occurred, although rarely, due to severe reactions to sulfonamides including Stevens-Johnson syndrome, toxic epidermal necrolysis, fulminant hepatic necrosis, agranulocytosis, aplastic anemia, and other blood dyscrasias. Sensitization may recur when a sulfonamide is readministered irrespective of the route of administration. If signs of serious reactions or hypersensitivity occur, discontinue the use of this preparation [see Contraindications (4.3)] .
5.4 Obstructive Pulmonary Disease
Patients with chronic obstructive pulmonary disease (e.g., chronic bronchitis, emphysema) of mild or moderate severity, bronchospastic disease, or a history of bronchospastic disease (other than bronchial asthma or a history of bronchial asthma, in which COSOPT is contraindicated) should, in general, not receive beta-blocking agents, including COSOPT [see Contraindications (4.1)] .
5.5 Increased Reactivity to Allergens
While taking beta-blockers, patients with a history of atopy or a history of severe anaphylactic reactions to a variety of allergens may be more reactive to repeated accidental, diagnostic, or therapeutic challenge with such allergens. Such patients may be unresponsive to the usual doses of epinephrine used to treat anaphylactic reactions.
5.6 Potentiation of Muscle Weakness
Beta-adrenergic blockade has been reported to potentiate muscle weakness consistent with certain myasthenic symptoms (e.g., diplopia, ptosis, and generalized weakness). Timolol has been reported rarely to increase muscle weakness in some patients with myasthenia gravis or myasthenic symptoms.
5.7 Masking of Hypoglycemic Symptoms in Patients with Diabetes Mellitus
Beta-adrenergic blocking agents should be administered with caution in patients subject to spontaneous hypoglycemia or to diabetic patients (especially those with labile diabetes) who are receiving insulin or oral hypoglycemic agents. Beta-adrenergic receptor blocking agents may mask the signs and symptoms of acute hypoglycemia.
5.8 Masking of Thyrotoxicosis
Beta-adrenergic blocking agents may mask certain clinical signs (e.g., tachycardia) of hyperthyroidism. Patients suspected of developing thyrotoxicosis should be managed carefully to avoid abrupt withdrawal of beta-adrenergic blocking agents that might precipitate a thyroid storm.
5.9 Renal and Hepatic Impairment
Dorzolamide has not been studied in patients with severe renal impairment (CrCl <30 mL/min). Because dorzolamide and its metabolite are excreted predominantly by the kidney, COSOPT is not recommended in such patients.
Dorzolamide has not been studied in patients with hepatic impairment and should therefore be used with caution in such patients.
5.10 Impairment of Beta-Adrenergically Mediated Reflexes During Surgery
The necessity or desirability of withdrawal of beta-adrenergic blocking agents prior to major surgery is controversial. Beta-adrenergic receptor blockade impairs the ability of the heart to respond to beta-adrenergically mediated reflex stimuli. This may augment the risk of general anesthesia in surgical procedures. Some patients receiving beta-adrenergic receptor blocking agents have experienced protracted severe hypotension during anesthesia. Difficulty in restarting and maintaining the heartbeat has also been reported. For these reasons, in patients undergoing elective surgery, some authorities recommend gradual withdraw of beta-adrenergic receptor blocking agents.
If necessary during surgery, the effects of beta-adrenergic blocking agents may be reversed by sufficient doses of adrenergic agonists.
5.11 Corneal Endothelium
Carbonic anhydrase activity has been observed in both the cytoplasm and around the plasma membranes of the corneal endothelium. There is an increased potential for developing corneal edema in patients with low endothelial cell counts. Caution should be used when prescribing COSOPT to this group of patients.
5.12 Bacterial Keratitis
There have been reports of bacterial keratitis associated with the use of multiple-dose containers of topical ophthalmic products. These containers had been inadvertently contaminated by patients who, in most cases, had a concurrent corneal disease or a disruption of the ocular epithelial.
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
COSOPT was evaluated in 1,035 patients with elevated intraocular pressure treated for open-angle glaucoma or ocular hypertension for up to 15 months. Approximately 5% of all patients discontinued therapy because of adverse reactions.
The most frequently reported adverse reactions occurring in up to 30% of patients were taste perversion (bitter, sour, or unusual taste) or ocular burning and/or stinging. The following adverse reactions were reported in 5 to 15% of patients: conjunctival hyperemia, blurred vision, superficial punctate keratitis or eye itching.
The following adverse reactions were reported in 1 to 5% of patients: abdominal pain, back pain, blepharitis, bronchitis, cloudy vision, conjunctival discharge, conjunctival edema, conjunctival follicles, conjunctival injection, conjunctivitis, corneal erosion, corneal staining, cortical lens opacity, cough, dizziness, dryness of eyes, dyspepsia, eye debris, eye discharge, eye pain, eye tearing, eyelid edema, eyelid erythema, eyelid exudate/scales, eyelid pain or discomfort, foreign body sensation, glaucomatous cupping, headache, hypertension, influenza, lens nucleus coloration, lens opacity, nausea, nuclear lens opacity, pharyngitis, post-subcapsular cataract, sinusitis, upper respiratory infection, urinary tract infection, visual field defect, vitreous detachment.
Other adverse reactions that have been reported with the individual components are listed below:
Dorzolamide 2%
Angioedema, asthenia/fatigue, bronchospasm, contact dermatitis, epistaxis, eyelid crusting, ocular discomfort, photophobia, signs and symptoms of ocular allergic reaction, transient myopia.
Timolol (ocular administration)
Body as a Whole: Asthenia/fatigue; Cardiovascular: Arrhythmia, syncope, cerebral ischemia, worsening of angina pectoris, palpitation, cardiac arrest, pulmonary edema, edema, claudication, Raynaud's phenomenon, and cold hands and feet; Digestive: Anorexia, abdominal pain; Immunologic: Systemic lupus erythematosus; Nervous System/Psychiatric: Increase in signs and symptoms of myasthenia gravis, somnolence, insomnia, nightmares, behavioral changes and psychic disturbances including confusion, hallucinations, anxiety, disorientation, nervousness, and memory loss; Skin: Alopecia, psoriasiform rash or exacerbation of psoriasis; Hypersensitivity: Signs and symptoms of systemic allergic reactions, including anaphylaxis, angioedema, urticaria, and localized and generalized rash; Respiratory: Bronchospasm (predominantly in patients with pre-existing bronchospastic disease); Endocrine: Masked symptoms of hypoglycemia in diabetic patients; Special Senses: Ptosis, decreased corneal sensitivity, cystoid macular edema, visual disturbances including refractive changes and diplopia, pseudopemphigoid, and tinnitus; Urogenital: Retroperitoneal fibrosis, decreased libido, impotence, and Peyronie's disease; Musculoskeletal: Myalgia.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of COSOPT. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure: bradycardia, cardiac failure, cerebral vascular accident, chest pain, choroidal detachment following filtration surgery, depression, diarrhea, dry mouth, dyspnea, heart block, hypotension, iridocyclitis, myocardial infarction, nasal congestion, Stevens-Johnson syndrome, toxic epidermal necrolysis, paresthesia, photophobia, respiratory failure, skin rashes, urolithiasis, and vomiting.
Timolol (oral administration)
The following additional adverse reactions have been reported in clinical experience with ORAL timolol maleate or other ORAL beta-blocking agents and may be considered potential effects of ophthalmic timolol maleate: Allergic: Erythematous rash, fever combined with aching and sore throat, laryngospasm with respiratory distress; Body as a Whole: Extremity pain, decreased exercise tolerance, weight loss; Cardiovascular: Worsening of arterial insufficiency, vasodilatation; Digestive: Gastrointestinal pain, hepatomegaly, mesenteric arterial thrombosis, ischemic colitis; Hematologic: Nonthrombocytopenic purpura; thrombocytopenic purpura, agranulocytosis; Endocrine: Hyperglycemia, hypoglycemia; Skin: Pruritus, skin irritation, increased pigmentation, sweating; Musculoskeletal: Arthralgia; Nervous System/Psychiatric: Vertigo, local weakness, diminished concentration, reversible mental depression progressing to catatonia, an acute reversible syndrome characterized by disorientation for time and place, emotional lability, slightly clouded sensorium, and deceased performance on neuropsychometrics; Respiratory: Rales, bronchial obstruction; Urogenital: Urination difficulties.
-
7 DRUG INTERACTIONS
7.1 Oral Carbonic Anhydrase Inhibitors
There is a potential for an additive effect on the known systemic effects of carbonic anhydrase inhibition in patients receiving an oral carbonic anhydrase inhibitor and COSOPT. The concomitant administration of COSOPT and oral carbonic anhydrase inhibitors is not recommended.
7.2 High-Dose Salicylate Therapy
Although acid-base and electrolyte disturbances were not reported in the clinical trials with dorzolamide hydrochloride ophthalmic solution, these disturbances have been reported with oral carbonic anhydrase inhibitors and have, in some instances, resulted in drug interactions (e.g., toxicity associated with high-dose salicylate therapy). Therefore, the potential for such drug interactions should be considered in patients receiving COSOPT.
7.3 Beta-Adrenergic Blocking Agents
Patients who are receiving a beta-adrenergic blocking agent orally and COSOPT should be observed for potential additive effects of beta-blockade, both systemic and on intraocular pressure. The concomitant use of two topical beta-adrenergic blocking agents is not recommended.
7.4 Calcium Antagonists
Caution should be used in the coadministration of beta-adrenergic blocking agents, such as COSOPT, and oral or intravenous calcium antagonists because of possible atrioventricular conduction disturbances, left ventricular failure, and hypotension. In patients with impaired cardiac function, coadministration should be avoided.
7.5 Catecholamine-Depleting Drugs
Close observation of the patient is recommended when a beta-blocker is administered to patients receiving catecholamine-depleting drugs, such as reserpine, because of possible additive effects and the production of hypotension and/or marked bradycardia, which may result in vertigo, syncope, or postural hypotension.
7.6 Digitalis and Calcium Antagonists
The concomitant use of beta-adrenergic blocking agents with digitalis and calcium antagonists may have additive effects in prolonging atrioventricular conduction time.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic Effects. Developmental toxicity studies with dorzolamide hydrochloride in rabbits at oral doses of ≥2.5 mg/kg/day (37 times the recommended human ophthalmic dose) revealed malformations of the vertebral bodies. These malformations occurred at doses that caused metabolic acidosis with decreased body weight gain in dams and decreased fetal weights. No treatment-related malformations were seen at 1 mg/kg/day (15 times the recommended human ophthalmic dose).
Teratogenicity studies with timolol in mice, rats, and rabbits at oral doses up to 50 mg/kg/day (7,000 times the systemic exposure following the maximum recommended human ophthalmic dose) demonstrated no evidence of fetal malformations. Although delayed fetal ossification was observed at this dose in rats, there were no adverse effects on postnatal development of offspring. Doses of 1,000 mg/kg/day (142,000 times the systemic exposure following the maximum recommended human ophthalmic dose) were maternotoxic in mice and resulted in an increased number of fetal resorptions. Increased fetal resorptions were also seen in rabbits at doses of 14,000 times the systemic exposure following the maximum recommended human ophthalmic dose, in this case without apparent maternotoxicity.
There are no adequate and well-controlled studies in pregnant women. COSOPT should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
8.3 Nursing Mothers
It is not known whether dorzolamide is excreted in human milk. Timolol maleate has been detected in human milk following oral and ophthalmic drug administration. Because of the potential for serious adverse reactions from COSOPT in nursing infants, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
The safety and effectiveness of dorzolamide hydrochloride ophthalmic solution and timolol maleate ophthalmic solution have been established when administered individually in pediatric patients aged 2 years and older. Use of these drug products in these children is supported by evidence from adequate and well-controlled studies in children and adults. Safety and efficacy in pediatric patients below the age of 2 years have not be established.
-
10 OVERDOSAGE
Symptoms consistent with systemic administration of beta-blockers or carbonic anhydrase inhibitors may occur, including electrolyte imbalance, development of an acidotic state, dizziness, headache, shortness of breath, bradycardia, bronchospasm, cardiac arrest and possible central nervous system effects. Serum electrolyte levels (particularly potassium) and blood pH levels should be monitored. [see Adverse Reactions (6)] .
A study of patients with renal failure showed that timolol did not dialyze readily.
-
11 DESCRIPTION
COSOPT (dorzolamide hydrochloride and timolol maleate ophthalmic solution) is the combination of a topical carbonic anhydrase inhibitor and a topical beta-adrenergic receptor blocking agent.
Dorzolamide hydrochloride is described chemically as: (4 S-trans)-4-(ethylamino)-5,6-dihydro-6-methyl-4 H-thieno[2,3- b]thiopyran-2-sulfonamide 7,7-dioxide monohydrochloride. Dorzolamide hydrochloride is optically active. The specific rotation is:
[α] 25°C (C=1, water) = ~-17°. 405 nm Its empirical formula is C 10H 16N 2O 4S 3 ∙ HCl and its structural formula is:
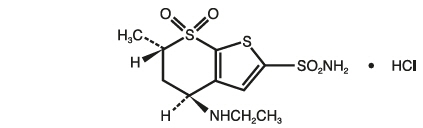
Dorzolamide hydrochloride has a molecular weight of 360.91. It is a white to off-white, crystalline powder, which is soluble in water and slightly soluble in methanol and ethanol.
Timolol maleate is described chemically as: (-)-1-( tert-butylamino)-3-[(4-morpholino-1,2,5-thiadiazol-3-yl)oxy]-2-propanol maleate (1:1) (salt). Timolol maleate possesses an asymmetric carbon atom in its structure and is provided as the levo-isomer. The optical rotation of timolol maleate is:
[α] 25°C in 1N HCl (C = 5) = -12.2° (-11.7° to -12.5°). 405 nm Its molecular formula is C 13H 24N 4O 3S ∙ C 4H 4O 4 and its structural formula is:
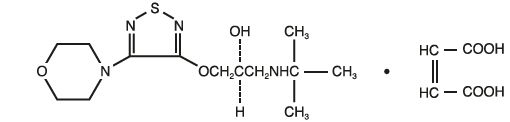
Timolol maleate has a molecular weight of 432.50. It is a white, odorless, crystalline powder which is soluble in water, methanol, and alcohol. Timolol maleate is stable at room temperature.
COSOPT is supplied as a sterile, clear, colorless to nearly colorless, isotonic, buffered, slightly viscous, aqueous solution. The pH of the solution is approximately 5.65, and the osmolarity is 242 to 323 mOsM. Each mL of COSOPT contains 20 mg dorzolamide (equivalent to 22.26 mg of dorzolamide hydrochloride) and 5 mg timolol (equivalent to 6.83 mg timolol maleate). Inactive ingredients are sodium citrate, hydroxyethyl cellulose, sodium hydroxide, mannitol, and water for injection. Benzalkonium chloride 0.0075% is added as a preservative.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
COSOPT is comprised of two components: dorzolamide hydrochloride and timolol maleate. Each of these two components decreases elevated intraocular pressure, whether or not associated with glaucoma, by reducing aqueous humor secretion. Elevated intraocular pressure is a major risk factor in the pathogenesis of optic nerve damage and glaucomatous visual field loss. The higher the level of intraocular pressure, the greater the likelihood of glaucomatous field loss and optic nerve damage.
Dorzolamide hydrochloride is an inhibitor of human carbonic anhydrase II. Inhibition of carbonic anhydrase in the ciliary processes of the eye decreases aqueous humor secretion, presumably by slowing the formation of bicarbonate ions with subsequent reduction in sodium and fluid transport. Timolol maleate is a beta 1 and beta 2 (non-selective) adrenergic receptor blocking agent that does not have significant intrinsic sympathomimetic, direct myocardial depressant, or local anesthetic (membrane-stabilizing) activity. The combined effect of these two agents administered as COSOPT twice daily results in additional intraocular pressure reduction compared to either component administered alone, but the reduction is not as much as when dorzolamide administered three times daily and timolol twice daily are administered concomitantly. [see Clinical Studies (14)] .
12.3 Pharmacokinetics
Dorzolamide Hydrochloride
When topically applied, dorzolamide reaches the systemic circulation. To assess the potential for systemic carbonic anhydrase inhibition following topical administration, drug and metabolite concentrations in RBCs and plasma and carbonic anhydrase inhibition in RBCs were measured. Dorzolamide accumulates in RBCs during chronic dosing as a result of binding to CA-II. The parent drug forms a single N-desethyl metabolite, which inhibits CA-II less potently than the parent drug but also inhibits CA-I. The metabolite also accumulates in RBCs where it binds primarily to CA-I. Plasma concentrations of dorzolamide and metabolite are generally below the assay limit of quantitation (15nM). Dorzolamide binds moderately to plasma proteins (approximately 33%).
Dorzolamide is primarily excreted unchanged in the urine; the metabolite also is excreted in urine. After dosing is stopped, dorzolamide washes out of RBCs nonlinearly, resulting in a rapid decline of drug concentration initially, followed by a slower elimination phase with a half-life of about four months.
To simulate the systemic exposure after long-term topical ocular administration, dorzolamide was given orally to eight healthy subjects for up to 20 weeks. The oral dose of 2 mg twice daily closely approximates the amount of drug delivered by topical ocular administration of dorzolamide 2% three times daily. Steady state was reached within 8 weeks. The inhibition of CA-II and total carbonic anhydrase activities was below the degree of inhibition anticipated to be necessary for a pharmacological effect on renal function and respiration in healthy individuals.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In a two-year study of dorzolamide hydrochloride administered orally to male and female Sprague-Dawley rats, urinary bladder papillomas were seen in male rats in the highest dosage group of 20 mg/kg/day (250 times the recommended human ophthalmic dose). Papillomas were not seen in rats given oral doses equivalent to approximately 12 times the recommended human ophthalmic dose. No treatment-related tumors were seen in a 21-month study in female and male mice given oral doses up to 75 mg/kg/day (~900 times the recommended human ophthalmic dose). The increased incidence of urinary bladder papillomas seen in the high-dose male rats is a class-effect of carbonic anhydrase inhibitors in rats. Rats are particularly prone to developing papillomas in response to foreign bodies, compounds causing crystalluria, and diverse sodium salts.
No changes in bladder urothelium were seen in dogs given oral dorzolamide hydrochloride for one year at 2 mg/kg/day (25 times the recommended human ophthalmic dose) or monkeys dosed topically to the eye at 0.4 mg/kg/day (~5 times the recommended human ophthalmic dose) for one year.
In a two-year study of timolol maleate administered orally to rats, there was a statistically significant increase in the incidence of adrenal pheochromocytomas in male rats administered 300 mg/kg/day (approximately 42,000 times the systemic exposure following the maximum recommended human ophthalmic dose). Similar differences were not observed in rats administered oral doses equivalent to approximately 14,000 times the maximum recommended human ophthalmic dose.
In a lifetime oral study of timolol maleate in mice, there were statistically significant increases in the incidence of benign and malignant pulmonary tumors, benign uterine polyps and mammary adenocarcinomas in female mice at 500 mg/kg/day, (approximately 71,000 times the systemic exposure following the maximum recommended human ophthalmic dose), but not at 5 or 50 mg/kg/day (approximately 700 or 7,000, respectively, times the systemic exposure following the maximum recommended human ophthalmic dose). In a subsequent study in female mice, in which post-mortem examinations were limited to the uterus and the lungs, a statistically significant increase in the incidence of pulmonary tumors was again observed at 500 mg/kg/day.
The increased occurrence of mammary adenocarcinomas was associated with elevations in serum prolactin which occurred in female mice administered oral timolol at 500 mg/kg/day, but not at doses of 5 or 50 mg/kg/day. An increased incidence of mammary adenocarcinomas in rodents has been associated with administration of several other therapeutic agents that elevate serum prolactin, but no correlation between serum prolactin levels and mammary tumors has been established in humans. Furthermore, in adult human female subjects who received oral dosages of up to 60 mg of timolol maleate (the maximum recommended human oral dosage), there were no clinically meaningful changes in serum prolactin.
The following tests for mutagenic potential were negative for dorzolamide: (1) in vivo (mouse) cytogenetic assay; (2) in vitro chromosomal aberration assay; (3) alkaline elution assay; (4) V-79 assay; and (5) Ames test.
Timolol maleate was devoid of mutagenic potential when tested in vivo (mouse) in the micronucleus test and cytogenetic assay (doses up to 800 mg/kg) and in vitro in a neoplastic cell transformation assay (up to 100 mcg/mL). In Ames tests the highest concentrations of timolol employed, 5,000 or 10,000 mcg/plate, were associated with statistically significant elevations of revertants observed with tester strain TA100 (in seven replicate assays), but not in the remaining three strains. In the assays with tester strain TA100, no consistent dose response relationship was observed, and the ratio of test to control revertants did not reach 2. A ratio of 2 is usually considered the criterion for a positive Ames test.
Reproduction and fertility studies in rats with either timolol maleate or dorzolamide hydrochloride demonstrated no adverse effect on male or female fertility at doses up to approximately 100 times the systemic exposure following the maximum recommended human ophthalmic dose.
-
14 CLINICAL STUDIES
Clinical studies of 3 to 15 months duration were conducted to compare the IOP-lowering effect over the course of the day COSOPT twice daily (dosed morning and bedtime) to individually and concomitantly administered 0.5% timolol twice daily and 2% dorzolamide twice and three times daily. The IOP-lowering effect of COSOPT twice daily was greater (1 to 3 mmHg) than that of monotherapy with either 2% dorzolamide three times daily or 0.5% timolol twice daily. The IOP-lowering effect of COSOPT twice daily was approximately 1 mmHg less than that of concomitant therapy with 2% dorzolamide three times daily and 0.5% timolol twice daily.
Open-label extensions of two studies were conducted for up to 12 months. During this period, the IOP-lowering effect of COSOPT twice daily was consistent during the 12 month follow-up period.
- 16 HOW SUPPLIED/STORAGE AND HANDLING
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-Approved patient labeling (Patient Information and Instructions for Use).
Potential for Exacerbation of Asthma and COPD
COSOPT may cause severe worsening of asthma and COPD symptoms including death due to bronchospasm. Advise patients with bronchial asthma, a history of bronchial asthma, or severe chronic obstructive pulmonary disease not to take this product. [see Contraindications (4.1)] .
Potential of Cardiovascular Effects
COSOPT may cause worsening of cardiac symptoms. Advise patients with sinus bradycardia, second or third degree atrioventricular block, or cardiac failure not to take this product. [see Contraindications (4.2)] .
Sulfonamide Reactions
COSOPT contains dorzolamide (which is a sulfonamide) and, although administered topically, is absorbed systemically. Therefore the same types of adverse reactions that are attributable to sulfonamides may occur with topical administration, including severe skin reactions. Advise patients that if serious or unusual reactions or signs of hypersensitivity occur, they should discontinue the use of the product and seek their physician's advise. [see Warnings and Precautions (5.3)] .
Handling Ophthalmic Solutions
Instruct patients that ocular solutions, if handled improperly or if the tip of the dispensing container contacts the eye or surrounding structures, can be contaminated by common bacteria known to cause ocular infections. Serious damage to the eye and subsequent loss of vision may result from using contaminated solutions [see Warnings and Precautions (5.12)] .
Intercurrent Ocular Conditions
Advise patients that if they have ocular surgery or develop an intercurrent ocular condition (e.g., trauma or infection), they should immediately seek their physician's advice concerning the continued use of the present multidose container.
- SPL UNCLASSIFIED SECTION
-
PATIENT INFORMATION
COSOPT
® (CO-sopt)
(dorzolamide hydrochloride and timolol maleate ophthalmic solution)
for topical ophthalmic use
What is COSOPT?
COSOPT is a prescription eye drop solution that contains two medicines, dorzolamide hydrochloride called an ophthalmic carbonic anhydrase and timolol maleate called a beta-blocker.
COSOPT is used to lower high pressure in the eye in people with open-angle glaucoma or ocular hypertension when a beta-blocking medicine alone does not work to control the eye pressure. It is not known if COSOPT is safe and effective in children 2 years of age and younger.
Do not use COSOPT if you:
- have or have had asthma.
- have chronic obstructive pulmonary disease (COPD) which emphysema, chronic bronchitis or both.
- have heart problems including a slow heartbeat, heart block, heart failure, or your heart muscle suddenly becomes weak due to a severe heart attack or other heart problem that caused heart damage (cardiogenic shock).
- are allergic to any of the ingredients in COSOPT. See the end of this Patient Information leaflet for a complete list of ingredients in COSOPT.
Before using COSOPT, tell your healthcare provider about all your medical conditions, including if you:
- have or have had allergies to sulfa drugs
- have a history of anaphylactic reactions to allergens
- have atopy (genetic disposition to develop allergic reactions)
- have or have had muscle weakness or myasthenia gravis
- have diabetes
- have thyroid disease
- have or have had kidney or liver problems
- plan to have any type of surgery
- wear contact lenses
- are using any other eye drops
- have an eye infection or eye trauma
- are pregnant or plan to become pregnant. It is not know if COSOPT will harm your unborn baby. Tell your healthcare provider right away if you become pregnant while using COSOPT. You and your healthcare provider will decide if you should use COSOPT while you are pregnant.
- are breastfeeding or plan to breastfeed. It is not known if COSOPT passes into breastmilk. Talk to your healthcare provider about the best way to feed your baby while using COSOPT.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
COSOPT may affect the way medicines work, and other medicines may affect how COSOPT works. Do not start a new medicine without first talking to your healthcare provider.
Ask your healthcare provider or pharmacist for a list of medicines you are using, if you are not sure. Know the medicines you take. Keep a list of them and show it to your healthcare provider and pharmacist when you get a new medicine.
How should I use COSOPT?
- See the complete Instructions for Use at the end of this Patient Information leaflet for detailed instructions about the right way to use COSOPT.
- Use COSOPT exactly as your healthcare provider tells you.
- Use 1 drop of COSOPT in the affected eye or both eyes if needed, 2 times each day. 1 drop in the morning and 1 drop in the evening.
- If you are using COSOPT with another eyedrop, wait at least 5 minutes before or after using COSOPT.
- If you have eye surgery or have any problems with your eye such as trauma or an infection, talk to your healthcare provider about continuing to use the bottle (multidose) that contains COSOPT.
- COSOPT contains a preservative called benzalkonium chloride. The preservative may be absorbed by soft contact lenses. If you wear contact lenses, remove them before using COSOPT. The lenses can be placed back into your eyes 15 minutes after using COSOPT.
- Do not touch your eye or eyelid with the dropper tip. Eye medicines, not handled the right way, can become contaminated by bacteria that can cause eye infections. Serious damage to the eye and followed by loss of vision may happen from using contaminated eye medicines. If you think your COSOPT medicine may be contaminated, or if you develop an eye infection, contact your healthcare provider right away about continuing to use your bottle of COSOPT.
- If you use too much COSOPT you may have dizziness, headaches, shortness of breath, slow heartbeats, or problems breathing. If you have any of these symptoms call your healthcare provider or go to the nearest hospital emergency room right away.
What are the possible side effects of COSOPT?
COSOPT may cause serious side effects, including:
- severe breathing problems. These breathing problems can happen in people who have asthma, chronic obstructive pulmonary disease, or heart failure and can cause death. Tell your healthcare provider right away if you have breathing problems while using COSOPT.
-
heart failure. This can happen in people who already have heart failure and in people who have never had heart failure before. Tell your healthcare provider right away if you get any of these symptoms of heart failure while taking COSOPT:
- shortness of breath
- irregular heartbeat (palpitations)
- swelling of your ankles or feet
- sudden weight gain
-
serious sulfa (sulfonamide) reactions. Serious reactions including death can happen in people who are allergic to sulfonamide medicines like one of the medicines in COSOPT. Other serious reactions can include:
- severe skin reactions
- liver problems
- blood problems
- swelling of your face, lips, mouth, or tongue
- trouble breathing
- wheezing
- severe itching
- skin rash, redness, or swelling
- dizziness or fainting
- fast heartbeat or pounding in your chest
- sweating
-
increased allergic reactions. People who have a genetic history of developing allergies (atopy) or who have a history of severe anaphylactic reactions from different allergens may have increased allergic reactions while taking beta-blockers, like one of the medicines in COSOPT. Your usual dose of epinephrine used to treat your anaphylactic reactions may not work as well.
Stop using COSOPT and call your healthcare provider or get emergency help right away if you get any of these symptoms of an allergic reaction:
- swelling of your face, lips, mouth or tongue
- trouble breathing
- wheezing
- severe itching
- skin rash, redness, or swelling
- dizziness or fainting
- fast heartbeat or pounding in your chest
- sweating
- worsening muscle weakness. Muscle weakness symptoms including double vision or drooping eyelids can happen while using COSOPT. Muscle weakness can get worse in people who already have problems with muscle weakness like myasthenia gravis.
- swelling of eye. Some people with low counts of certain types of cells in the eye have developed corneal edema when using COSOPT. Call your healthcare provider if you have swelling in your eyes.
The most common side effects of COSOPT include:
- eye burning
- eye stinging
- eye redness
- blurred vision
- eye tearing
- eye itching
- a bitter, sour, or unusual taste after putting in your eyedrops
These are not all the possible side effects of COSOPT.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store COSOPT?
- Store at 68° to 77°F (20° to 25°C).
- Protect from light.
- Do not use COSOPT after the expiration date on the bottle.
Keep COSOPT and all medicines out of the reach of children.
General information about the safe and effective use of COSOPT.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use COSOPT for a condition for which it was not prescribed. Do not give COSOPT to other people, even if they have the same symptoms that you have. It may harm them.
You can ask your pharmacist or healthcare provider for information about COSOPT that is written for health professionals.
What are the ingredients in COSOPT?
Active ingredients: dorzolamide hydrochloride and timolol maleate
Inactive ingredients: sodium citrate, hydroxyethyl cellulose, sodium hydroxide, mannitol, water for injection and benzalkonium chloride added as a preservative.
This Patient Package Information has been approved by the U.S. Food and Drug Administration | 11/2020
-
INSTRUCTIONS FOR USE
COSOPT
® (CO-sopt)
(dorzolamide hydrochloride and timolol maleate ophthalmic solution)
for topical ophthalmic use
Read this Instructions for Use before you start using COSOPT and each time you get a refill. There may be new information. This leaflet does not take the place of talking to your healthcare provider about your medical condition or treatment.
Important Information:
- COSOPT is for use in the eye.
- If you are using COSOPT with another eyedrop, wait at least 5 minutes before or after using COSOPT.
- If you wear contact lenses, remove them before using COSOPT. The lenses can be placed back into your eyes 15 minutes after using COSOPT.
- Do not touch your eye or eyelid with the dropper tip. Eye medicines, not handled the right way, can become contaminated by bacteria that can cause eye infections. Serious damage to the eye and followed by loss of vision may happen from using contaminated eye medicines. If you think your COSOPT medicine may be contaminated, or if you develop an eye infection, contact your healthcare provider right away about continuing to use your bottle of COSOPT.
- Wash your hands before each use to make sure you do not infect your eyes while using COSOPT.
- Before using the eyedrops for the first time, be sure the Safety Seal around the cap is not broken. If the Safety Seal is broken, call your pharmacist to get a new bottle of COSOPT.
Step 1. Tear off the Safety Seal. Step 2. To open the COSOPT bottle, unscrew the cap by turning counterclockwise. Step 3. Tilt your head back. Gently pull your lower eyelid downwards to form a pocket between your eyelid and your eye, look up (See Figure A). 
Step 4. Turn the COSOPT bottle upside down. Step 5. Place the dropper tip of the COSOPT bottle close to your eye but be careful not to touch your eye with it. Gently press the COSOPT bottle lightly with your thumb or index finger until 1 drop of COSOPT falls into your eye (See Figure B). 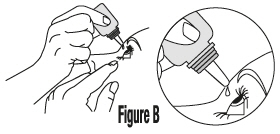
Step 6. Repeat Steps 4 and 5 with the other eye if instructed to do so by your healthcare provider. Step 7. Replace the cap by turning until it is firmly touching the bottle. Do not overtighten the cap. Step 8. If you use contact lenses, wait at least 15 minutes before placing them back into your eyes. - The dropper tip is made to give a single drop of COSOPT. Do not enlarge the hole of the dropper tip.
- After you have used all of your doses of COSOPT, there will be some COSOPT left in the bottle.
- There is an extra amount of COSOPT that has been added to the bottle. You will get the full amount of COSOPT that your doctor prescribed.
- Do not try to remove the extra COSOPT medicine from the bottle.
This Instructions for Use has been approved by the U.S. Food and Drug Administration | 11/2020
Manufactured for: Thea Pharma Inc. Waltham, MA 02451
Made in Switzerland© 2023. Thea Pharma Inc. All rights reserved
The COSOPT trademarks are owned by Merck Sharp & Dohme Corp. and are being used with permission.
Rev. 05/2023Revised: 5/2023
Thea Pharma Inc.
-
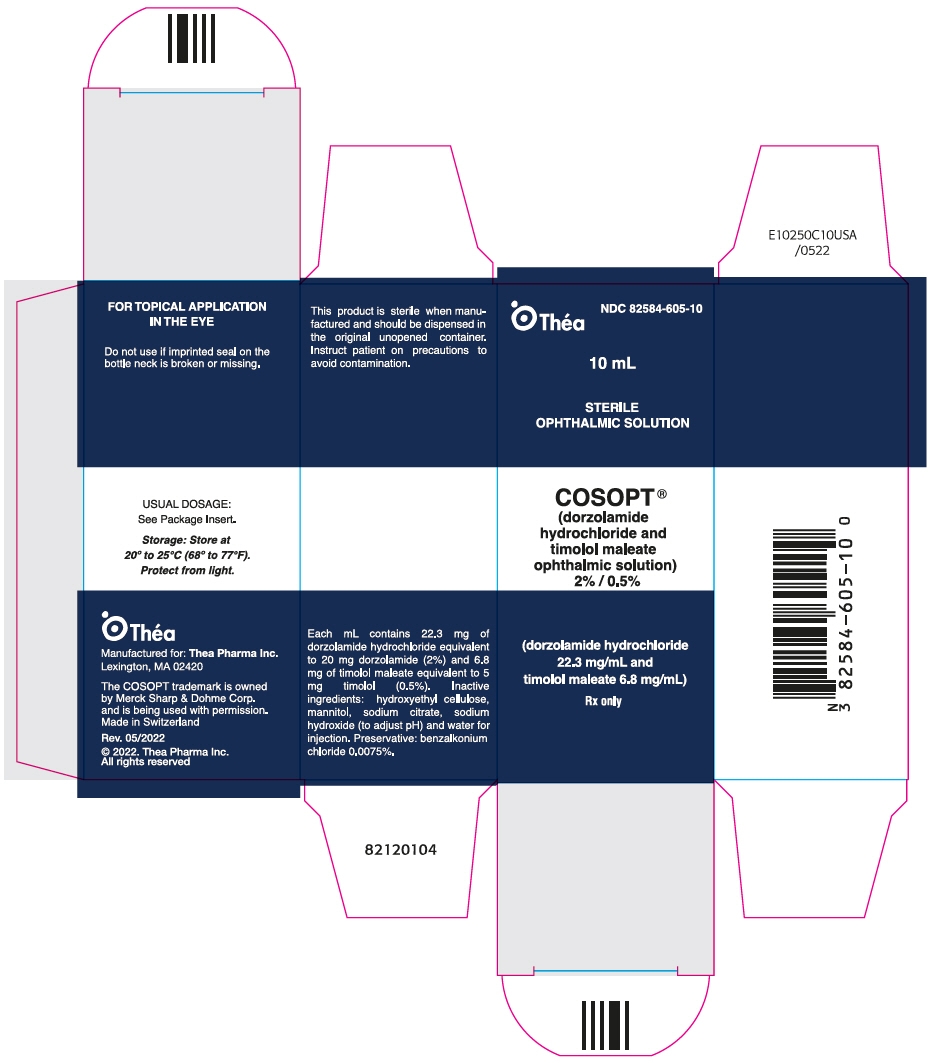
PRINCIPAL DISPLAY PANEL - 10 mL Bottle Carton
NDC: 82584-605-10
Théa
10 mL
STERILE
OPHTHALMIC SOLUTIONCOSOPT ®
(dorzolamide
hydrochloride and
timolol maleate
ophthalmic solution)
2% / 0.5%(dorzolamide hydrochloride
22.3 mg/mL and
timolol maleate 6.8 mg/mL)Rx only
-
INGREDIENTS AND APPEARANCE
COSOPT
dorzolamide hydrochloride and timolol maleate solution/ dropsProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 82584-605 Route of Administration OPHTHALMIC Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength DORZOLAMIDE HYDROCHLORIDE (UNII: QZO5366EW7) (DORZOLAMIDE - UNII:9JDX055TW1) DORZOLAMIDE 20 mg in 1 mL TIMOLOL MALEATE (UNII: P8Y54F701R) (TIMOLOL ANHYDROUS - UNII:5JKY92S7BR) TIMOLOL ANHYDROUS 5 mg in 1 mL Inactive Ingredients Ingredient Name Strength HYDROXYETHYL CELLULOSE (2000 MPA.S AT 1%) (UNII: S38J6RZN16) MANNITOL (UNII: 3OWL53L36A) SODIUM CITRATE, UNSPECIFIED FORM (UNII: 1Q73Q2JULR) SODIUM HYDROXIDE (UNII: 55X04QC32I) WATER (UNII: 059QF0KO0R) BENZALKONIUM CHLORIDE (UNII: F5UM2KM3W7) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 82584-605-10 1 in 1 CARTON 11/10/2022 1 10 mL in 1 BOTTLE, DROPPER; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020869 11/10/2022 Labeler - Thea Pharma Inc. (117787029)
Trademark Results [COSOPT]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 COSOPT 74714427 2173319 Live/Registered |
MERCK SHARP & DOHME CORP. 1995-08-11 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.