LEVETIRACETAM tablet, film coated
Levetiracetam by
Drug Labeling and Warnings
Levetiracetam by is a Prescription medication manufactured, distributed, or labeled by Aurobindo Pharma Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use LEVETIRACETAM TABLETS safely and effectively. See full prescribing information for LEVETIRACETAM TABLETS.
LEVETIRACETAM tablets, for oral use
Initial U.S. Approval: 1999RECENT MAJOR CHANGES
INDICATIONS AND USAGE
Levetiracetam is indicated for the treatment of partial-onset seizures in patients 1 month of age and older (1.1)
Levetiracetam is indicated for adjunctive therapy for the treatment of:DOSAGE AND ADMINISTRATION
- Use the oral solution for pediatric patients with body weight ≤ 20 kg (2.1)
- For pediatric patients, use weight-based dosing for the oral solution with a calibrated measuring device (not a household teaspoon or tablespoon) (2.1)
Partial-Onset Seizures (monotherapy or adjunctive therapy)
- 1 Month to < 6 Months: 7 mg/kg twice daily; increase by 7 mg/kg twice daily every 2 weeks to recommended dose of 21 mg/kg twice daily (2.2)
- 6 Months to < 4 Years: 10 mg/kg twice daily; increase by 10 mg/kg twice daily every 2 weeks to recommended dose of 25 mg/kg twice daily (2.2)
- 4 Years to < 16 Years: 10 mg/kg twice daily; increase by 10 mg/kg twice daily every 2 weeks to recommended dose of 30 mg/kg twice daily (2.2)
- Adults 16 Years and Older: 500 mg twice daily; increase by 500 mg twice daily every 2 weeks to a recommended dose of 1500 mg twice daily (2.2)
Myoclonic Seizures in Adults and Pediatric Patients 12 Years and Older
- 500 mg twice daily; increase by 500 mg twice daily every 2 weeks to recommended dose of 1500 mg twice daily (2.3)
Primary Generalized Tonic-Clonic Seizures
- 6 Years to < 16 Years: 10 mg/kg twice daily, increase in increments of 10 mg/kg twice daily every 2 weeks to recommended dose of 30 mg/kg twice daily (2.4)
- Adults 16 Years and Older: 500 mg twice daily, increase by 500 mg twice daily every 2 weeks to recommended dose of 1500 mg twice daily (2.4)
Adult Patients with Impaired Renal Function
DOSAGE FORMS AND STRENGTHS
- 250 mg, 500 mg, 750 mg, and 1000 mg film-coated, scored tablets (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Behavioral abnormalities including psychotic symptoms, suicidal ideation, irritability, and aggressive behavior have been observed; monitor patients for psychiatric signs and symptoms (5.1)
- Suicidal Behavior and Ideation: Monitor patients for new or worsening depression, suicidal thoughts/behavior, and/or unusual changes in mood or behavior (5.2)
- Monitor for somnolence and fatigue and advise patients not to drive or operate machinery until they have gained sufficient experience on levetiracetam (5.3)
- Serious Dermatological Reactions: Discontinue levetiracetam at the first sign of rash unless clearly not drug related. (5.5)
- Coordination Difficulties: Monitor for ataxia, abnormal gait, and incoordination. Advise patients to not drive or operate machinery until they have gained experience on levetiracetam. (5.6)
- Withdrawal Seizures: Levetiracetam must be gradually withdrawn (5.7)
ADVERSE REACTIONS
Most common adverse reactions (incidence ≥ 5% more than placebo) include:
- Adult patients: somnolence, asthenia, infection and dizziness (6.1)
- Pediatric patients: fatigue, aggression, nasal congestion, decreased appetite, and irritability (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Aurobindo Pharma USA, Inc. at 1-866-850-2876 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 12/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Partial-Onset Seizures
1.2 Myoclonic Seizures in Patients with Juvenile Myoclonic Epilepsy
1.3 Primary Generalized Tonic-Clonic Seizures
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
2.2 Dosing for Partial-Onset Seizures
2.3 Dosing for Myoclonic Seizures in Patients 12 Years of Age and Older With Juvenile Myoclonic Epilepsy
2.4 Dosing for Primary Generalized Tonic-Clonic Seizures
2.5 Dosage Adjustments in Adult Patients with Renal Impairment
2.6 Discontinuation of Levetiracetam Tablets
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Behavioral Abnormalities and Psychotic Symptoms
5.2 Suicidal Behavior and Ideation
5.3 Somnolence and Fatigue
5.4 Anaphylaxis and Angioedema
5.5 Serious Dermatological Reactions
5.6 Coordination Difficulties
5.7 Withdrawal Seizures
5.8 Hematologic Abnormalities
5.9 Increase in Blood Pressure
5.10 Seizure Control During Pregnancy
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
10 OVERDOSAGE
10.1 Signs, Symptoms and Laboratory Findings of Acute Overdosage in Humans
10.2 Management of Overdose
10.3 Hemodialysis
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Partial-Onset Seizures
14.2 Myoclonic Seizures in Patients With Juvenile Myoclonic Epilepsy
14.3 Primary Generalized Tonic-Clonic Seizures
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
1.1 Partial-Onset Seizures
Levetiracetam tablets are indicated for the treatment of partial-onset seizures in patients 1 month of age and older.
-
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
Levetiracetam tablets are given orally with or without food. The levetiracetam dosing regimen depends on the indication, age group, dosage form (tablets or oral solution), and renal function.
Prescribe the oral solution for pediatric patients with body weight ≤ 20 kg. Prescribe the oral solution or tablets for pediatric patients with body weight above 20 kg.
When using the oral solution in pediatric patients, dosing is weight-based (mg per kg) using a calibrated measuring device (not a household teaspoon or tablespoon).
Levetiracetam tablets should be swallowed whole. Levetiracetam tablets should not be chewed or crushed.2.2 Dosing for Partial-Onset Seizures
The recommended dosing for monotherapy and adjunctive therapy is the same; as outlined below.
Adults 16 Years of Age and Older
Initiate treatment with a daily dose of 1000 mg/day, given as twice-daily dosing (500 mg twice daily). Additional dosing increments may be given (1000 mg/day additional every 2 weeks) to a maximum recommended daily dose of 3000 mg. There is no evidence that doses greater than 3000 mg/day confer additional benefit.
Pediatric Patients
1 Month to < 6 Months
Initiate treatment with a daily dose of 14 mg/kg in 2 divided doses (7 mg/kg twice daily). Increase the daily dose every 2 weeks by increments of 14 mg/kg to the recommended daily dose of 42 mg/kg (21 mg/kg twice daily). In the clinical trial, the mean daily dose was 35 mg/kg in this age group.
6 Months to < 4 Years:
Initiate treatment with a daily dose of 20 mg/kg in 2 divided doses (10 mg/kg twice daily). Increase the daily dose in 2 weeks by an increment of 20 mg/kg to the recommended daily dose of 50 mg/kg (25 mg/kg twice daily). If a patient cannot tolerate a daily dose of 50 mg/kg, the daily dose may be reduced. In the clinical trial, the mean daily dose was 47 mg/kg in this age group.
4 Years to < 16 Years
Initiate treatment with a daily dose of 20 mg/kg in 2 divided doses (10 mg/kg twice daily). Increase the daily dose every 2 weeks by increments of 20 mg/kg to the recommended daily dose of 60 mg/kg (30 mg/kg twice daily). If a patient cannot tolerate a daily dose of 60 mg/kg, the daily dose may be reduced. In the clinical trial, the mean daily dose was 44 mg/kg. The maximum daily dose was 3000 mg/day.
For levetiracetam tablet dosing in pediatric patients weighing 20 to 40 kg, initiate treatment with a daily dose of 500 mg given as twice daily dosing (250 mg twice daily). Increase the daily dose every 2 weeks by increments of 500 mg to a maximum recommended daily dose of 1500 mg (750 mg twice daily).
For levetiracetam tablet dosing in pediatric patients weighing more than 40 kg, initiate treatment with a daily dose of 1000 mg/day given as twice daily dosing (500 mg twice daily). Increase the daily dose every 2 weeks by increments of 1000 mg/day to a maximum recommended daily dose of 3000 mg (1500 mg twice daily).
Levetiracetam Oral Solution Weight-Based Dosing Calculation For Pediatric Patients
The following calculation should be used to determine the appropriate daily dose of oral solution for pediatric patients:
Daily dose (mg/kg/day) x patient weight (kg)
Total daily dose (mL/day) = ------------------------------------------------------
100 mg/mL
2.3 Dosing for Myoclonic Seizures in Patients 12 Years of Age and Older With Juvenile Myoclonic Epilepsy
Initiate treatment with a dose of 1000 mg/day, given as twice-daily dosing (500 mg twice daily). Increase the dosage by 1000 mg/day every 2 weeks to the recommended daily dose of 3000 mg. The effectiveness of doses lower than 3000 mg/day has not been studied.
2.4 Dosing for Primary Generalized Tonic-Clonic Seizures
Adults 16 Years of Age and Older
Initiate treatment with a dose of 1000 mg/day, given as twice-daily dosing (500 mg twice daily). Increase dosage by 1000 mg/day every 2 weeks to the recommended daily dose of 3000 mg. The effectiveness of doses lower than 3000 mg/day has not been adequately studied.
Pediatric Patients 6 to <16 Years of Age
Initiate treatment with a daily dose of 20 mg/kg in 2 divided doses (10 mg/kg twice daily). Increase the daily dose every 2 weeks by increments of 20 mg/kg to the recommended daily dose of 60 mg/kg (30 mg/kg twice daily). The effectiveness of doses lower than 60 mg/kg/day has not been adequately studied. Patients with body weight ≤20 kg should be dosed with oral solution. Patients with body weight above 20 kg can be dosed with either tablets or oral solution [see Dosage and Administration (2.1)]. Only whole tablets should be administered.2.5 Dosage Adjustments in Adult Patients with Renal Impairment
Levetiracetam tablet dosing must be individualized according to the patient’s renal function status. Recommended dosage adjustments for adults are shown in Table 1. In order to calculate the dose recommended for patients with renal impairment, creatinine clearance adjusted for body surface area must be calculated. To do this an estimate of the patient’s creatinine clearance (CLcr) in mL/min must first be calculated using the following formula:
[140-age (years)] x weight (kg)
CLcr = ----------------------------------------------(x 0.85 for female patients)
72 x serum creatinine (mg/dL)
Then CLcr is adjusted for body surface area (BSA) as follows:
CLcr (mL/min)
CLcr (mL/min/1.73 m2) = -------------------------- x 1.73
BSA subject (m2)
Table 1: Dosing Adjustment Regimen for Adult Patients with Renal Impairment Group Creatinine Clearance (mL/min/1.73 m2) Dosage
(mg)Frequency 1 Following dialysis, a 250 to 500 mg supplemental dose is recommended.
Normal
> 80
500 to 1,500
Every 12 hours
Mild
50 to 80
500 to 1,000
Every 12 hours
Moderate
30 to 50
250 to 750
Every 12 hours
Severe
< 30
250 to 500
Every 12 hours
ESRD patients using dialysis
----
500 to 1,0001
Every 24 hours1
2.6 Discontinuation of Levetiracetam Tablets
Avoid abrupt withdrawal from levetiracetam tablets in order to reduce the risk of increased seizure frequency and status epilepticus [see Warnings and Precautions (5.7)].
-
3 DOSAGE FORMS AND STRENGTHS
- Levetiracetam Tablets USP, 250 mg are blue oval shaped biconvex film-coated tablets debossed with a deep break line separating ‘E’ and ‘10’ on one side and plain on the other side.
- Levetiracetam Tablets USP, 500 mg are yellow oval shaped biconvex film-coated tablets debossed with a deep break line separating ‘E’ and ‘11’ on one side and plain on the other side.
- Levetiracetam Tablets USP, 750 mg are orange oval shaped biconvex film-coated tablets debossed with a deep break line separating ‘E’ and ‘12’ on one side and plain on the other side.
- Levetiracetam Tablets USP, 1000 mg are white to off-white modified oval shaped biconvex film-coated tablets debossed with a deep breakline separating ‘E’ and ‘13’ on one side and plain on the other side.
-
4 CONTRAINDICATIONS
Levetiracetam tablets are contraindicated in patients with a hypersensitivity to levetiracetam. Reactions have included anaphylaxis and angioedema [see Warnings and Precautions (5.4)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Behavioral Abnormalities and Psychotic Symptoms
Levetiracetam may cause behavioral abnormalities and psychotic symptoms. Patients treated with levetiracetam should be monitored for psychiatric signs and symptoms.
Behavioral abnormalities
In clinical studies, 13% of adult levetiracetam-treated patients and 38% of pediatric levetiracetam-treated patients (4 to 16 years of age) compared to 6% and 19% of adult and pediatric placebo-treated patients, experienced non-psychotic behavioral symptoms (reported as aggression, agitation, anger, anxiety, apathy, depersonalization, depression, emotional lability, hostility, hyperkinesias, irritability, nervousness, neurosis, and personality disorder).
A randomized double-blind, placebo-controlled study was performed to assess the neurocognitive and behavioral effects of levetiracetam as adjunctive therapy in pediatric patients (4 to 16 years of age). The results from an exploratory analysis indicated a worsening in levetiracetam-treated patients on aggressive behavior (one of eight behavior dimensions) as measured in a standardized and systematic way using a validated instrument, the Achenbach Child Behavior Checklist (CBCL/6 to 18).
In clinical studies in pediatric patients 1 month to < 4 years of age, irritability was reported in 12% of the levetiracetam-treated patients compared to 0% of placebo-treated patients.
In clinical studies, 1.7% of adult levetiracetam-treated patients discontinued treatment due to behavioral adverse reactions, compared to 0.2% of placebo-treated patients. The treatment dose was reduced in 0.8% of adult levetiracetam-treated patients and in 0.5% of placebo-treated patients. Overall, 11% of levetiracetam-treated pediatric patients experienced behavioral symptoms associated with discontinuation or dose reduction, compared to 6% of placebo-treated patients.
Psychotic symptoms
In clinical studies, 1% of levetiracetam-treated adult patients, 2% of levetiracetam-treated pediatric patients 4 to 16 years of age, and 17% of levetiracetam-treated pediatric patients 1 month to <4 years of age experienced psychotic symptoms, compared to 0.2%, 2%, and 5% in the corresponding age groups treated with placebo. In a controlled study that assessed the neurocognitive and behavioral effects of levetiracetam in pediatric patients 4 to 16 years of age, 1.6% of levetiracetam-treated patients experienced paranoia, compared to 0% of placebo-treated patients. In the same study, 3.1% of levetiracetam-treated patients experienced confusional state, compared to 0% of placebo-treated patients [see Use in Specific Populations (8.4)].
In clinical studies, two (0.3%) levetiracetam-treated adult patients were hospitalized and their treatment was discontinued due to psychosis. Both events, reported as psychosis, developed within the first week of treatment and resolved within 1 to 2 weeks following treatment discontinuation. There was no difference between drug and placebo-treated patients in the incidence of the pediatric patients who discontinued treatment due to psychotic and non-psychotic adverse reactions.
5.2 Suicidal Behavior and Ideation
Antiepileptic drugs (AEDs), including levetiracetam, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Patients treated with any AED for any indication should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted Relative Risk 1.8, 95% CI:1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43%, compared to 0.24% among 16,029 placebo-treated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated. There were four suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number is too small to allow any conclusion about drug effect on suicide.
The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed.
The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5 to 100 years) in the clinical trials analyzed. Table 2 shows absolute and relative risk by indication for all evaluated AEDs.
Table 2: Risk by Indication for Antiepileptic Drugs in the Pooled Analysis Indication Placebo Patients with Events Per 1000 Patients Drug Patients with Events Per 1000 Patients Relative Risk: Incidence of Events in Drug Patients/Incidence in Placebo Patients Risk Difference: Additional Drug Patients with Events Per 1000 Patients Epilepsy
1
3.4
3.5
2.4
Psychiatric
5.7
8.5
1.5
2.9
Other
1
1.8
1.9
0.9
Total
2.4
4.3
1.8
1.9
The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
Anyone considering prescribing levetiracetam or any other AED must balance the risk of suicidal thoughts or behaviors with the risk of untreated illness. Epilepsy and many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and an increased risk of suicidal thoughts and behavior. Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated.5.3 Somnolence and Fatigue
Levetiracetam may cause somnolence and fatigue. Patients should be monitored for these signs and symptoms and advised not to drive or operate machinery until they have gained sufficient experience on levetiracetam to gauge whether it adversely affects their ability to drive or operate machinery.
Somnolence
In controlled trials of adult patients with epilepsy experiencing partial-onset seizures, 15% of levetiracetam-treated patients reported somnolence, compared to 8% of placebo-treated patients. There was no clear dose response up to 3000 mg/day. In a study where there was no titration, about 45% of patients receiving 4000 mg/day reported somnolence. The somnolence was considered serious in 0.3% of levetiracetam-treated patients, compared to 0% in the placebo group. About 3% of levetiracetam-treated patients discontinued treatment due to somnolence, compared to 0.7% of placebo-treated patients. In 1.4% of levetiracetam-treated patients and 0.9% of placebo-treated patients, the dose was reduced, while 0.3% of the levetiracetam-treated patients were hospitalized due to somnolence.
Asthenia
In controlled clinical studies of adult patients with epilepsy experiencing partial-onset seizures, 15% of levetiracetam-treated patients reported asthenia, compared to 9% of placebo-treated patients. Treatment was discontinued due to asthenia in 0.8% of levetiracetam-treated patients as compared to 0.5% of placebo-treated patients. In 0.5% of levetiracetam-treated patients and in 0.2% of placebo-treated patients, the dose was reduced due to asthenia.
Somnolence and asthenia occurred most frequently within the first 4 weeks of treatment. In general, the incidences of somnolence and fatigue in the pediatric partial-onset seizure studies, and in pediatric and adult myoclonic and primary generalized tonic-clonic seizure studies were comparable to those of the adult partial-onset seizure studies.
5.4 Anaphylaxis and Angioedema
Levetiracetam can cause anaphylaxis or angioedema after the first dose or at any time during treatment. Signs and symptoms in cases reported in the postmarketing setting have included hypotension, hives, rash, respiratory distress, and swelling of the face, lip, mouth, eye, tongue, throat, and feet. In some reported cases, reactions were life-threatening and required emergency treatment. If a patient develops signs or symptoms of anaphylaxis or angioedema, levetiracetam should be discontinued and the patient should seek immediate medical attention. Levetiracetam should be discontinued permanently if a clear alternative etiology for the reaction cannot be established [see Contraindications (4)].
5.5 Serious Dermatological Reactions
Serious dermatological reactions, including Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), have been reported in both pediatric and adult patients treated with levetiracetam. The median time of onset is reported to be 14 to 17 days, but cases have been reported at least four months after initiation of treatment. Recurrence of the serious skin reactions following rechallenge with levetiracetam has also been reported. Levetiracetam should be discontinued at the first sign of a rash, unless the rash is clearly not drug-related. If signs or symptoms suggest SJS/TEN, use of this drug should not be resumed and alternative therapy should be considered.
5.6 Coordination Difficulties
Levetiracetam may cause coordination difficulties.
In controlled clinical studies in adult patients with partial-onset seizure studies, 3.4% of adult levetiracetam-treated patients experienced coordination difficulties, (reported as either ataxia, abnormal gait, or incoordination) compared to 1.6% of placebo-treated patients. A total of 0.4% of patients in controlled clinical studies discontinued levetiracetam treatment due to ataxia, compared to 0% of placebo-treated patients. In 0.7% of levetiracetam-treated patients and in 0.2% of placebo-treated patients, the dose was reduced due to coordination difficulties, while one of the levetiracetam-treated patients was hospitalized due to worsening of pre-existing ataxia. These events occurred most frequently within the first 4 weeks of treatment.
Patients should be monitored for these signs and symptoms and advised not to drive or operate machinery until they have gained sufficient experience on levetiracetam to gauge whether it could adversely affect their ability to drive or operate machinery.5.7 Withdrawal Seizures
As with most antiepileptic drugs, levetiracetam should generally be withdrawn gradually because of the risk of increased seizure frequency and status epilepticus. If withdrawal is needed because of a serious adverse reaction, rapid discontinuation can be considered.
5.8 Hematologic Abnormalities
Levetiracetam can cause hematologic abnormalities. Hematologic abnormalities occurred in clinical trials and included decreases in white blood cell (WBC), neutrophil, and red blood cell (RBC) counts; decreases in hemoglobin and hematocrit; and increases in eosinophil counts. Cases of agranulocytosis, pancytopenia, and thrombocytopenia have been reported in the postmarketing setting. A complete blood count is recommended in patients experiencing significant weakness, pyrexia, recurrent infections, or coagulation disorders.
Partial-Onset Seizures
Adults
Minor, but statistically significant, decreases compared to placebo in total mean RBC count (0.03 x 106/mm3), mean hemoglobin (0.09 g/dL), and mean hematocrit (0.38%), were seen in levetiracetam-treated patients in controlled trials.
A total of 3.2% of levetiracetam-treated and 1.8% of placebo-treated patients had at least one possibly significant (≤2.8 x 109/L) decreased WBC, and 2.4% of levetiracetam-treated and 1.4% of placebo-treated patients had at least one possibly significant (≤1 x 109/L) decreased neutrophil count. Of the levetiracetam-treated patients with a low neutrophil count, all but one rose towards or to baseline with continued treatment. No patient was discontinued secondary to low neutrophil counts.
Pediatric Patients 4 Years to < 16 Years
Statistically significant decreases in WBC and neutrophil counts were seen in levetiracetam-treated patients as compared to placebo. The mean decreases from baseline in the levetiracetam-treated group were -0.4 × 109/L and -0.3 × 109/L, respectively, whereas there were small increases in the placebo group. Mean relative lymphocyte counts increased by 1.7% in levetiracetam-treated patients, compared to a decrease of 4% in placebo patients (statistically significant).
In the controlled trial, more levetiracetam-treated patients had a possibly clinically significant abnormally low WBC value (3% of levetiracetam-treated patients versus 0% of placebo-treated patients), however, there was no apparent difference between treatment groups with respect to neutrophil count (5% of levetiracetam-treated patients versus 4.2% of placebo-treated patients). No patient was discontinued secondary to low WBC or neutrophil counts.
In the controlled cognitive and neuropsychological safety study, 5 patients (8.6%) in the levetiracetam-treated group and two patients (6.1%) in the placebo-treated group had high eosinophil count values that were possibly clinically significant (≥10% or ≥0.7 x 109/L).5.9 Increase in Blood Pressure
In a randomized, placebo-controlled study in patients 1 month to <4 years of age, a significantly higher risk of increased diastolic blood pressure was observed in the levetiracetam-treated patients (17%), compared to the placebo-treated patients (2%). There was no overall difference in mean diastolic blood pressure between the treatment groups. This disparity between the levetiracetam and placebo treatment groups was not observed in the studies of older children or in adults.
Monitor patients 1 month to <4 years of age for increases in diastolic blood pressure.
5.10 Seizure Control During Pregnancy
Physiological changes may gradually decrease plasma levels of levetiracetam throughout pregnancy. This decrease is more pronounced during the third trimester. It is recommended that patients be monitored carefully during pregnancy. Close monitoring should continue through the postpartum period especially if the dose was changed during pregnancy.
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed in more details in other sections of labeling:
- Behavior Abnormalities and Psychotic Symptoms [see Warnings and Precautions (5.1)]
- Suicidal Behavior and Ideation [see Warnings and Precautions (5.2)]
- Somnolence and Fatigue [see Warnings and Precautions (5.3)]
- Anaphylaxis and Angioedema [see Warnings and Precautions (5.4)]
- Serious Dermatological Reactions [see Warnings and Precautions (5.5)]
- Coordination Difficulties [see Warnings and Precautions (5.6)]
- Hematologic Abnormalities [see Warnings and Precautions (5.8)]
- Increase in Blood Pressure [see Warnings and Precautions (5.9)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Partial-Onset Seizures
Adults
In controlled clinical studies in adults with partial-onset seizures [see Clinical Studies (14.1)], the most common adverse reactions in patients receiving levetiracetam in combination with other AEDs, for events with rates greater than placebo, were somnolence, asthenia, infection, and dizziness. Of the most common adverse reactions in adults experiencing partial-onset seizures, asthenia, somnolence, and dizziness occurred predominantly during the first 4 weeks of treatment with levetiracetam.
Table 3 lists adverse reactions that occurred in at least 1% of adult epilepsy patients receiving levetiracetam in placebo-controlled studies and were numerically more common than in patients treated with placebo. In these studies, either levetiracetam or placebo was added to concurrent AED therapy.
Table 3: Adverse Reactions in Pooled Placebo-Controlled, Adjunctive Studies in Adults Experiencing Partial-Onset Seizures
Levetiracetam
(N=769)
%
Placebo
(N=439)
%
Asthenia
15
9
Somnolence
15
8
Headache
14
13
Infection
13
8
Dizziness
9
4
Pain
7
6
Pharyngitis
6
4
Depression
4
2
Nervousness
4
2
Rhinitis
4
3
Anorexia
3
2
Ataxia
3
1
Vertigo
3
1
Amnesia
2
1
Anxiety
2
1
Cough Increased
2
1
Diplopia
2
1
Emotional Lability
2
0
Hostility
2
1
Paresthesia
2
1
Sinusitis
2
1
In controlled adult clinical studies, 15% of patients receiving levetiracetam and 12% receiving placebo either discontinued or had a dose reduction as a result of an adverse reaction. Table 4 lists the most common (>1%) adverse reactions that resulted in discontinuation or dose reduction and that occurred more frequently in levetiracetam-treated patients than in placebo-treated patients.
Table 4: Adverse Reactions that Resulted in Discontinuation or Dose Reduction in Placebo-Controlled Studies in Adult Patients Experiencing Partial-Onset Seizures Adverse Reaction
Levetiracetam
(N=769)
%
Placebo
(N=439)
%
Somnolence
4
2
Dizziness
1
0
Pediatric Patients 4 Years to <16 Years
The adverse reaction data presented below was obtained from a pooled analysis of two controlled pediatric clinical studies in pediatric patients 4 to 16 years of age with partial-onset seizures. The most common adverse reactions in pediatric patients receiving levetiracetam in combination with other AEDs, for events with rates greater than placebo, were fatigue, aggression, nasal congestion, decreased appetite, and irritability.
Table 5 lists adverse reactions from the pooled pediatric controlled studies (4 to 16 years of age) that occurred in at least 2% of pediatric levetiracetam-treated patients and were numerically more common than in pediatric patients treated with placebo. In these studies, either levetiracetam or placebo was added to concurrent AED therapy.
Table 5: Adverse Reactions in Pooled Placebo-Controlled, Adjunctive Studies in Pediatric Patients Ages 4 to 16 Years Experiencing Partial-Onset Seizures
Levetiracetam
(N=165)
%
Placebo
(N=131)
%
Headache
19
15
Nasopharyngitis
15
12
Vomiting
15
12
Somnolence
13
9
Fatigue
11
5
Aggression
10
5
Cough
9
5
Nasal Congestion
9
2
Upper Abdominal Pain
9
8
Decreased Appetite
8
2
Abnormal Behavior
7
4
Dizziness
7
5
Irritability
7
1
Pharyngolaryngeal Pain
7
4
Diarrhea
6
2
Lethargy
6
5
Insomnia
5
3
Agitation
4
1
Anorexia
4
3
Head Injury
4
0
Altered Mood
3
1
Constipation
3
1
Contusion
3
1
Depression
3
1
Fall
3
2
Influenza
3
1
Affect Lability
2
1
Anxiety
2
1
Arthralgia
2
0
Confusional State
2
0
Conjunctivitis
2
0
Ear Pain
2
1
Gastroenteritis
2
0
Joint Sprain
2
1
Mood Swings
2
1
Neck Pain
2
1
Rhinitis
2
0
Sedation
2
1
In the controlled pooled pediatric clinical studies in patients 4 to 16 years of age, 7% of patients receiving levetiracetam and 9% receiving placebo discontinued as a result of an adverse reaction.
Pediatric Patients 1 Month to < 4 Years
In the 7-day, controlled pediatric clinical study in children 1 month to less than 4 years of age with partial-onset seizures, the most common adverse reactions in patients receiving levetiracetam in combination with other AEDs, for events with rates greater than placebo, were somnolence and irritability. Because of the shorter exposure period, incidences of adverse reactions are expected to be lower than in other pediatric studies in older patients. Therefore, other controlled pediatric data, presented above, should also be considered to apply to this age group.
Table 6 lists adverse reactions that occurred in at least 5% of pediatric epilepsy patients (ages 1 month to < 4 years) treated with levetiracetam in the placebo-controlled study and were numerically more common than in patients treated with placebo. In this study, either levetiracetam or placebo was added to concurrent AED therapy.
Table 6: Adverse Reactions in a Placebo-Controlled, Adjunctive Study in Pediatric Patients Ages 1 Month to < 4 Years Experiencing Partial-Onset Seizures
Levetiracetam
(N=60)
%
Placebo
(N=56)
%
Somnolence
13
2
Irritability
12
0
In the 7-day controlled pediatric clinical study in patients 1 month to < 4 years of age, 3% of patients receiving levetiracetam and 2% receiving placebo either discontinued or had a dose reduction as a result of an adverse reaction. There was no adverse reaction that resulted in discontinuation for more than one patient.
Myoclonic Seizures
Although the pattern of adverse reactions in this study seems somewhat different from that seen in patients with partial-onset seizures, this is likely due to the much smaller number of patients in this study compared to partial seizure studies. The adverse reaction pattern for patients with JME is expected to be essentially the same as for patients with partial seizures.
In the controlled clinical study in patients 12 years of age and older with myoclonic seizures [see Clinical Studies (14.2)], the most common adverse reactions in patients receiving levetiracetam in combination with other AEDs, for events with rates greater than placebo, were somnolence, neck pain, and pharyngitis.
Table 7 lists adverse reactions that occurred in at least 5% of juvenile myoclonic epilepsy patients experiencing myoclonic seizures treated with levetiracetam and were numerically more common than in patients treated with placebo. In this study, either levetiracetam or placebo was added to concurrent AED therapy.
Table 7: Adverse Reactions in a Placebo-Controlled, Adjunctive Study in Patients 12 Years of Age and Older with Myoclonic Seizures
Levetiracetam
(N=60)
%
Placebo
(N=60)
%
Somnolence
12
2
Neck pain
8
2
Pharyngitis
7
0
Depression
5
2
Influenza
5
2
Vertigo
5
3
In the placebo-controlled study, 8% of patients receiving levetiracetam and 2% receiving placebo either discontinued or had a dose reduction as a result of an adverse reaction. The adverse reactions that led to discontinuation or dose reduction and that occurred more frequently in levetiracetam-treated patients than in placebo-treated patients are presented in Table 8.
Table 8: Adverse Reactions that Resulted in Discontinuation or Dose Reduction in a Placebo-Controlled Study in Patients with Juvenile Myoclonic Epilepsy Adverse Reaction
Levetiracetam
(N=60)
%
Placebo
(N=60)
%
Anxiety
3
2
Depressed mood
2
0
Depression
2
0
Diplopia
2
0
Hypersomnia
2
0
Insomnia
2
0
Irritability
2
0
Nervousness
2
0
Somnolence
2
0
Primary Generalized Tonic-Clonic Seizures
Although the pattern of adverse reactions in this study seems somewhat different from that seen in patients with partial-onset seizures, this is likely due to the much smaller number of patients in this study compared to partial seizure studies. The adverse reaction pattern for patients with primary generalized tonic-clonic (PGTC) seizures is expected to be essentially the same as for patients with partial seizures.
In the controlled clinical study that included patients 4 years of age and older with PGTC seizures [see Clinical Studies (14.3)], the most common adverse reaction in patients receiving levetiracetam in combination with other AEDs, for events with rates greater than placebo, was nasopharyngitis.
Table 9 lists adverse reactions that occurred in at least 5% of idiopathic generalized epilepsy patients experiencing PGTC seizures treated with levetiracetam and were numerically more common than in patients treated with placebo. In this study, either levetiracetam or placebo was added to concurrent AED therapy.
Table 9: Adverse Reactions in a Placebo-Controlled, Adjunctive Study in Patients 4 Years of Age and Older with PGTC Seizures
Levetiracetam
(N=79)
%
Placebo
(N=84)
%
Nasopharyngitis
14
5
Fatigue
10
8
Diarrhea
8
7
Irritability
6
2
Mood swings
5
1
In the placebo-controlled study, 5% of patients receiving levetiracetam and 8% receiving placebo either discontinued or had a dose reduction during the treatment period as a result of an adverse reaction.
This study was too small to adequately characterize the adverse reactions that could be expected to result in discontinuation of treatment in this population. It is expected that the adverse reactions that would lead to discontinuation in this population would be similar to those resulting in discontinuation in other epilepsy trials (see tables 4 and 8).
In addition, the following adverse reactions were seen in other controlled adult studies of levetiracetam: balance disorder, disturbance in attention, eczema, memory impairment, myalgia, and blurred vision.
Comparison of Gender, Age and Race
The overall adverse reaction profile of levetiracetam was similar between females and males. There are insufficient data to support a statement regarding the distribution of adverse reactions by age and race.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of levetiracetam. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The following adverse reactions have been reported in patients receiving marketed levetiracetam worldwide. The listing is alphabetized: abnormal liver function test, acute kidney injury, anaphylaxis, angioedema, agranulocytosis, choreoathetosis, drug reaction with eosinophilia and systemic symptoms (DRESS), dyskinesia, erythema multiforme, hepatic failure, hepatitis, hyponatremia, muscular weakness, pancreatitis, pancytopenia (with bone marrow suppression identified in some of these cases), panic attack, thrombocytopenia, and weight loss. Alopecia has been reported with levetiracetam use; recovery was observed in majority of cases where levetiracetam was discontinued. -
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to antiepileptic drugs (AEDs), including levetiracetam, during pregnancy. Encourage women who are taking levetiracetam during pregnancy to enroll in the North American Antiepileptic Drug (NAAED) pregnancy registry by calling 1-888-233-2334 or visiting http://www.aedpregnancyregistry.org/.
Risk Summary
Prolonged experience with levetiracetam in pregnant women has not identified a drug-associated risk of major birth defects or miscarriage, based on published literature, which includes data from pregnancy registries and reflects experience over two decades [see Human Data]. In animal studies, levetiracetam produced developmental toxicity (increased embryofetal and offspring mortality, increased incidences of fetal structural abnormalities, decreased embryofetal and offspring growth, neurobehavioral alterations in offspring) at doses similar to human therapeutic doses [see Animal Data].
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively. The background risk of major birth defects and miscarriage for the indicated population is unknown.
Clinical Considerations
Levetiracetam blood levels may decrease during pregnancy [see Warnings and Precautions (5.10)].
Physiological changes during pregnancy may affect levetiracetam concentration. Decrease in levetiracetam plasma concentrations has been observed during pregnancy. This decrease is more pronounced during the third trimester. Dose adjustments may be necessary to maintain clinical response.
Data
Human Data
While available studies cannot definitively establish the absence of risk, data from the published literature and pregnancy registries have not established an association with levetiracetam use during pregnancy and major birth defects or miscarriage.
Animal Data
When levetiracetam (0, 400, 1200, or 3600 mg/kg/day) was administered orally to pregnant rats during the period of organogenesis, reduced fetal weights and increased incidence of fetal skeletal variations were observed at the highest dose tested. There was no evidence of maternal toxicity. The no-effect dose for adverse effects on embryofetal developmental in rats (1200 mg/kg/day) is approximately 4 times the maximum recommended human dose (MRHD) of 3000 mg on a body surface area (mg/m2) basis.
Oral administration of levetiracetam (0, 200, 600, or 1800 mg/kg/day) to pregnant rabbits during the period of organogenesis resulted in increased embryofetal mortality and incidence of fetal skeletal variations at the mid and high dose and decreased fetal weights and increased incidence of fetal malformations at the high dose, which was associated with maternal toxicity. The no-effect dose for adverse effects on embryofetal development in rabbits (200 mg/kg/day) is approximately equivalent to the MRHD on a mg/m2 basis.
Oral administration of levetiracetam (0, 70, 350, or 1800 mg/kg/day) to female rats throughout pregnancy and lactation led to an increased incidence of fetal skeletal variations, reduced fetal body weight, and decreased growth in offspring at the mid and high doses and increased pup mortality and neurobehavioral alterations in offspring at the highest dose tested. There was no evidence of maternal toxicity. The no-effect dose for adverse effects on pre- and postnatal development in rats (70 mg/kg/day) is less than the MRHD on a mg/m2 basis.
Oral administration of levetiracetam to rats during the latter part of gestation and throughout lactation produced no adverse developmental or maternal effects at doses of up to 1800 mg/kg/day (6 times the MRHD on a mg/m2 basis).
8.2 Lactation
Risk Summary
Levetiracetam is excreted in human milk. There are no data on the effects of levetiracetam on the breastfed infant, or the effects on milk production.
The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for levetiracetam and any potential adverse effects on the breastfed infant from levetiracetam or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of levetiracetam for the treatment of partial-onset seizures in patients 1 month to 16 years of age have been established [see Clinical Pharmacology (12.3) and Clinical Studies (14.1)]. The dosing recommendation in these pediatric patients varies according to age group and is weight-based [see Dosage and Administration (2.2)].
The safety and effectiveness of levetiracetam as adjunctive therapy for the treatment of myoclonic seizures in adolescents 12 years of age and older with juvenile myoclonic epilepsy have been established [see Clinical Studies (14.2)].
The safety and effectiveness of levetiracetam as adjunctive therapy for the treatment of primary generalized tonic-clonic seizures in pediatric patients 6 years of age and older with idiopathic generalized epilepsy have been established [see Clinical Studies (14.3)].
Safety and effectiveness for the treatment of partial-onset seizures in pediatric patients below the age of 1 month; adjunctive therapy for the treatment of myoclonic seizures in pediatric patients below the age of 12 years; and adjunctive therapy for the treatment of primary generalized tonic-clonic seizures in pediatric patients below the age of 6 years have not been established.
A 3-month, randomized, double-blind, placebo-controlled study was performed to assess the neurocognitive and behavioral effects of levetiracetam as adjunctive therapy in 98 (levetiracetam N=64, placebo N=34) pediatric patients, ages 4 to 16 years old, with partial seizures that were inadequately controlled. The target dose was 60 mg/kg/day. Neurocognitive effects were measured by the Leiter-R Attention and Memory (AM) Battery, which measures various aspects of a child's memory and attention. Although no substantive differences were observed between the placebo and drug treated groups in the median change from baseline in this battery, the study was not adequate to assess formal statistical non-inferiority of the drug and placebo. The Achenbach Child Behavior Checklist (CBCL/6 to 18), a standardized validated tool used to assess a child’s competencies and behavioral/emotional problems, was also assessed in this study. An analysis of the CBCL/6 to 18 indicated on average a worsening in levetiracetam-treated patients in aggressive behavior, one of the eight syndrome scores [see Warnings and Precautions (5.1)].
Juvenile Animal Toxicity Data
Studies of levetiracetam in juvenile rats (dosed on postnatal days 4 through 52) and dogs (dosed from postnatal weeks 3 through 7) at doses of up to 1800 mg/kg/day (approximately 7 and 24 times, respectively, the maximum recommended pediatric dose of 60 mg/kg/day on a mg/m2 basis) did not demonstrate adverse effects on postnatal development.
8.5 Geriatric Use
There were 347 subjects in clinical studies of levetiracetam that were 65 and over. No overall differences in safety were observed between these subjects and younger subjects. There were insufficient numbers of elderly subjects in controlled trials of epilepsy to adequately assess the effectiveness of levetiracetam in these patients.
Levetiracetam is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function [see Clinical Pharmacology (12.3)].8.6 Renal Impairment
Clearance of levetiracetam is decreased in patients with renal impairment and is correlated with creatinine clearance [see Clinical Pharmacology (12.3)]. Dose adjustment is recommended for patients with impaired renal function and supplemental doses should be given to patients after dialysis [see Dosage and Administration (2.5)].
-
10 OVERDOSAGE
10.1 Signs, Symptoms and Laboratory Findings of Acute Overdosage in Humans
The highest known dose of levetiracetam received in the clinical development program was 6000 mg/day. Other than drowsiness, there were no adverse reactions in the few known cases of overdose in clinical trials. Cases of somnolence, agitation, aggression, depressed level of consciousness, respiratory depression and coma were observed with levetiracetam overdoses in postmarketing use.
10.2 Management of Overdose
There is no specific antidote for overdose with levetiracetam. If indicated, elimination of unabsorbed drug should be attempted by emesis or gastric lavage; usual precautions should be observed to maintain airway. General supportive care of the patient is indicated including monitoring of vital signs and observation of the patient’s clinical status. A Certified Poison Control Center should be contacted for up to date information on the management of overdose with levetiracetam.
10.3 Hemodialysis
Standard hemodialysis procedures result in significant clearance of levetiracetam (approximately 50% in 4 hours) and should be considered in cases of overdose. Although hemodialysis has not been performed in the few known cases of overdose, it may be indicated by the patient's clinical state or in patients with significant renal impairment.
-
11 DESCRIPTION
Levetiracetam is an antiepileptic drug available as 250 mg (blue), 500 mg (yellow), 750 mg (orange), and 1000 mg (white to off-white) tablets for oral administration.
The chemical name of levetiracetam, a single enantiomer, is (-)-(S)-α-ethyl-2-oxo-1-pyrrolidine acetamide, its molecular formula is C8H14N2O2 and its molecular weight is 170.21. Levetiracetam is chemically unrelated to existing antiepileptic drugs (AEDs). It has the following structural formula:
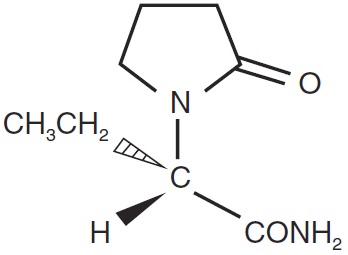
Levetiracetam USP is a white to off-white, crystalline powder with a faint odor and a bitter taste. It is very soluble in water (104 g/100 mL). It is freely soluble in chloroform (65.3 g/100 mL) and in methanol (53.6 g/100 mL), soluble in ethanol (16.5 g/100 mL), sparingly soluble in acetonitrile (5.7 g/100 mL) and practically insoluble in n-hexane. (Solubility limits are expressed as g/100 mL solvent.)
Levetiracetam tablets USP contain the labeled amount of levetiracetam. Inactive ingredients: corn starch, colloidal silicon dioxide, povidone, talc, magnesium stearate, hypromellose, titanium dioxide, polyethylene glycol, and purified water. In addition 250 mg contains FD&C Blue #2/indigo carmine aluminum lake, 500 mg contains iron oxide yellow, and 750 mg contains FD&C Yellow #6/sunset yellow FCF aluminum lake, FD&C Blue #2/indigo carmine aluminum lake, and iron oxide red.
Meets USP dissolution test 2. -
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The precise mechanism(s) by which levetiracetam exerts its antiepileptic effect is unknown.
A saturable and stereoselective neuronal binding site in rat brain tissue has been described for levetiracetam. Experimental data indicate that this binding site is the synaptic vesicle protein SV2A, thought to be involved in the regulation of vesicle exocytosis. Although the molecular significance of levetiracetam binding to SV2A is not understood, levetiracetam and related analogs showed a rank order of affinity for SV2A which correlated with the potency of their antiseizure activity in audiogenic seizure-prone mice. These findings suggest that the interaction of levetiracetam with the SV2A protein may contribute to the antiepileptic mechanism of action of the drug.12.2 Pharmacodynamics
Effects on QTc Interval
The effect of levetiracetam on QTc prolongation was evaluated in a randomized, double-blind, positive-controlled (moxifloxacin 400 mg) and placebo-controlled crossover study of levetiracetam (1000 mg or 5000 mg) in 52 healthy subjects. The upper bound of the 90% confidence interval for the largest placebo-adjusted, baseline-corrected QTc was below 10 milliseconds. Therefore, there was no evidence of significant QTc prolongation in this study.12.3 Pharmacokinetics
The pharmacokinetics of levetiracetam are similar when used as monotherapy or as adjunctive therapy for the treatment of partial-onset seizures.
Absorption and Distribution
Absorption of levetiracetam is rapid, with peak plasma concentrations occurring in about an hour following oral administration in fasted subjects. The oral bioavailability of levetiracetam tablets is 100% and the tablets and oral solution are bioequivalent in rate and extent of absorption. Food does not affect the extent of absorption of levetiracetam but it decreases Cmax by 20% and delays Tmax by 1.5 hours. The pharmacokinetics of levetiracetam are linear over the dose range of 500 to 5000 mg. Steady state is achieved after 2 days of multiple twice-daily dosing. Levetiracetam and its major metabolite are less than 10% bound to plasma proteins; clinically significant interactions with other drugs through competition for protein binding sites are therefore unlikely.
Metabolism
Levetiracetam is not extensively metabolized in humans. The major metabolic pathway is the enzymatic hydrolysis of the acetamide group, which produces the carboxylic acid metabolite, ucb L057 (24% of dose) and is not dependent on any liver cytochrome P450 isoenzymes. The major metabolite is inactive in animal seizure models. Two minor metabolites were identified as the product of hydroxylation of the 2-oxo-pyrrolidine ring (2% of dose) and opening of the 2-oxo-pyrrolidine ring in position 5 (1% of dose). There is no enantiomeric interconversion of levetiracetam or its major metabolite.
Elimination
Levetiracetam plasma half-life in adults is 7 ± 1 hour and is unaffected by either dose or repeated administration. Levetiracetam is eliminated from the systemic circulation by renal excretion as unchanged drug which represents 66% of administered dose. The total body clearance is 0.96 mL/min/kg and the renal clearance is 0.6 mL/min/kg. The mechanism of excretion is glomerular filtration with subsequent partial tubular reabsorption. The metabolite ucb L057 is excreted by glomerular filtration and active tubular secretion with a renal clearance of 4 mL/min/kg. Levetiracetam elimination is correlated to creatinine clearance. Levetiracetam clearance is reduced in patients with renal impairment [see Use in Specific Populations (8.6) and Dosage and Administration (2.5)].
Specific Populations
Elderly
Pharmacokinetics of levetiracetam were evaluated in 16 elderly subjects (age 61 to 88 years) with creatinine clearance ranging from 30 to 74 mL/min. Following oral administration of twice-daily dosing for 10 days, total body clearance decreased by 38% and the half-life was 2.5 hours longer in the elderly compared to healthy adults. This is most likely due to the decrease in renal function in these subjects.
Pediatric Patients
Pharmacokinetics of levetiracetam were evaluated in 24 pediatric patients (age 6 to 12 years) after single dose (20 mg/kg). The body weight adjusted apparent clearance of levetiracetam was approximately 40% higher than in adults.
A repeat dose pharmacokinetic study was conducted in pediatric patients (age 4 to 12 years) at doses of 20 mg/kg/day, 40 mg/kg/day, and 60 mg/kg/day. The evaluation of the pharmacokinetic profile of levetiracetam and its metabolite (ucb L057) in 14 pediatric patients demonstrated rapid absorption of levetiracetam at all doses with a Tmax of about 1 hour and a t1/2 of 5 hours across the three dosing levels. The pharmacokinetics of levetiracetam in children was linear between 20 to 60 mg/kg/day. The potential interaction of levetiracetam with other AEDs was also evaluated in these patients. Levetiracetam had no significant effect on the plasma concentrations of carbamazepine, valproic acid, topiramate or lamotrigine. However, there was about a 22% increase of apparent clearance of levetiracetam when it was co-administered with an enzyme-inducing AED (e.g., carbamazepine).
Following single dose administration (20 mg/kg) of a 10% oral solution to children with epilepsy (1 month to < 4 years), levetiracetam was rapidly absorbed and peak plasma concentrations were observed approximately 1 hour after dosing. The pharmacokinetic results indicated that half-life was shorter (5.3 h) than for adults (7.2 h) and apparent clearance was faster (1.5 mL/min/kg) than for adults (0.96 mL/min/kg).
Population pharmacokinetic analysis showed that body weight was significantly correlated to the clearance of levetiracetam in pediatric patients; clearance increased with an increase in body weight.
Pregnancy
Levetiracetam levels may decrease during pregnancy [see Warnings and Precautions (5.10) and Use in Specific Populations (8.1)].
Gender
Levetiracetam Cmax and AUC were 20% higher in women (N=11) compared to men (N=12). However, clearances adjusted for body weight were comparable.
Race
Formal pharmacokinetic studies of the effects of race have not been conducted. Cross-study comparisons involving Caucasians (N=12) and Asians (N=12), however, show that pharmacokinetics of levetiracetam were comparable between the two races. Because levetiracetam is primarily renally excreted and there are no important racial differences in creatinine clearance, pharmacokinetic differences due to race are not expected.
Renal Impairment
The disposition of levetiracetam was studied in adult subjects with varying degrees of renal function. Total body clearance of levetiracetam is reduced in patients with impaired renal function by 40% in the mild group (CLcr = 50 to 80 mL/min), 50% in the moderate group (CLcr = 30 to 50 mL/min) and 60% in the severe renal impairment group (CLcr <30 mL/min). Clearance of levetiracetam is correlated with creatinine clearance.
In anuric (end stage renal disease) patients, the total body clearance decreased 70% compared to normal subjects (CLcr >80 mL/min). Approximately 50% of the pool of levetiracetam in the body is removed during a standard 4-hour hemodialysis procedure [see Dosage and Administration (2.5)].
Hepatic Impairment
In subjects with mild (Child-Pugh A) to moderate (Child-Pugh B) hepatic impairment, the pharmacokinetics of levetiracetam were unchanged. In patients with severe hepatic impairment (Child-Pugh C), total body clearance was 50% that of normal subjects, but decreased renal clearance accounted for most of the decrease. No dose adjustment is needed for patients with hepatic impairment.
Drug Interactions
In vitro data on metabolic interactions indicate that levetiracetam is unlikely to produce, or be subject to, pharmacokinetic interactions. Levetiracetam and its major metabolite, at concentrations well above Cmax levels achieved within the therapeutic dose range, are neither inhibitors of, nor high affinity substrates for, human liver cytochrome P450 isoforms, epoxide hydrolase or UDP-glucuronidation enzymes. In addition, levetiracetam does not affect the in vitro glucuronidation of valproic acid.
Potential pharmacokinetic interactions of or with levetiracetam were assessed in clinical pharmacokinetic studies (phenytoin, valproate, warfarin, digoxin, oral contraceptive, probenecid) and through pharmacokinetic screening in the placebo-controlled clinical studies in epilepsy patients.
Phenytoin
Levetiracetam (3000 mg daily) had no effect on the pharmacokinetic disposition of phenytoin in patients with refractory epilepsy. Pharmacokinetics of levetiracetam were also not affected by phenytoin.
Valproate
Levetiracetam (1500 mg twice daily) did not alter the pharmacokinetics of valproate in healthy volunteers. Valproate 500 mg twice daily did not modify the rate or extent of levetiracetam absorption or its plasma clearance or urinary excretion. There also was no effect on exposure to and the excretion of the primary metabolite, ucb L057.
Other Antiepileptic Drugs
Potential drug interactions between levetiracetam and other AEDs (carbamazepine, gabapentin, lamotrigine, phenobarbital, phenytoin, primidone and valproate) were also assessed by evaluating the serum concentrations of levetiracetam and these AEDs during placebo-controlled clinical studies. These data indicate that levetiracetam does not influence the plasma concentration of other AEDs and that these AEDs do not influence the pharmacokinetics of levetiracetam.
Effect of AEDs in Pediatric Patients
There was about a 22% increase of apparent total body clearance of levetiracetam when it was co-administered with enzyme-inducing AEDs. Dose adjustment is not recommended. Levetiracetam had no effect on plasma concentrations of carbamazepine, valproate, topiramate, or lamotrigine.
Oral Contraceptives
Levetiracetam (500 mg twice daily) did not influence the pharmacokinetics of an oral contraceptive containing 0.03 mg ethinyl estradiol and 0.15 mg levonorgestrel, or of the luteinizing hormone and progesterone levels, indicating that impairment of contraceptive efficacy is unlikely. Coadministration of this oral contraceptive did not influence the pharmacokinetics of levetiracetam.
Digoxin
Levetiracetam (1000 mg twice daily) did not influence the pharmacokinetics and pharmacodynamics (ECG) of digoxin given as a 0.25 mg dose every day. Coadministration of digoxin did not influence the pharmacokinetics of levetiracetam.
Warfarin
Levetiracetam (1000 mg twice daily) did not influence the pharmacokinetics of R and S warfarin. Prothrombin time was not affected by levetiracetam. Coadministration of warfarin did not affect the pharmacokinetics of levetiracetam.
Probenecid
Probenecid, a renal tubular secretion blocking agent, administered at a dose of 500 mg four times a day, did not change the pharmacokinetics of levetiracetam 1000 mg twice daily. Cssmax of the metabolite, ucb L057, was approximately doubled in the presence of probenecid while the fraction of drug excreted unchanged in the urine remained the same. Renal clearance of ucb L057 in the presence of probenecid decreased 60%, probably related to competitive inhibition of tubular secretion of ucb L057. The effect of levetiracetam on probenecid was not studied.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Rats were dosed with levetiracetam in the diet for 104 weeks at doses of 50, 300, and 1800 mg/kg/day. Plasma exposure (AUC) at the highest dose was approximately 6 times that in humans at the maximum recommended daily human dose (MRHD) of 3000 mg. There was no evidence of carcinogenicity. In mice, oral administration of levetiracetam for 80 weeks (doses up to 960 mg/kg/day) or 2 years (doses up to 4000 mg/kg/day, lowered to 3000 mg/kg/day after 45 weeks due to intolerability) was not associated with an increase in tumors. The highest dose tested in mice for 2 years (3000 mg/kg/day) is approximately 5 times the MRHD on a body surface area (mg/m2)basis.
Mutagenesis
Levetiracetam was negative in in vitro (Ames, chromosomal aberration in mammalian cells) and in vivo (mouse micronucleus) assays. The major human metabolite of levetiracetam (ucb L057) was negative in in vitro (Ames, mouse lymphoma) assays.
Impairment of Fertility
No adverse effects on male or female fertility or reproductive performance were observed in rats at oral doses up to 1800 mg/kg/day, which were associated with plasma exposures (AUC) up to approximately 6 times that in humans at the MRHD.
-
14 CLINICAL STUDIES
14.1 Partial-Onset Seizures
Effectiveness in Partial-Onset Seizures in Adults
The effectiveness of levetiracetam for the treatment of partial-onset seizures in adults was established in three multicenter, randomized, double-blind, placebo-controlled clinical studies in patients who had refractory partial-onset seizures with or without secondary generalization. The tablet formulation was used in all these studies. In these studies, 904 patients were randomized to placebo, 1000 mg, 2000 mg, or 3000 mg/day. Patients enrolled in Study 1 or Study 2 had refractory partial-onset seizures for at least two years and had taken two or more classical AEDs. Patients enrolled in Study 3 had refractory partial-onset seizures for at least 1 year and had taken one classical AED. At the time of the study, patients were taking a stable dose regimen of at least one and could take a maximum of two AEDs. During the baseline period, patients had to have experienced at least two partial- onset seizures during each 4-week period.
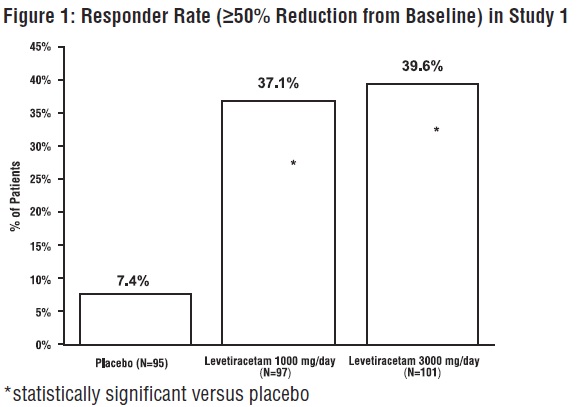
Study 1
Study 1 was a double-blind, placebo-controlled, parallel-group study conducted at 41 sites in the United States comparing levetiracetam 1000 mg/day (N=97), levetiracetam 3000 mg/day (N=101), and placebo (N=95) given in equally divided doses twice daily. After a prospective baseline period of 12 weeks, patients were randomized to one of the three treatment groups described above. The 18-week treatment period consisted of a 6-week titration period, followed by a 12-week fixed dose evaluation period, during which concomitant AED regimens were held constant. The primary measure of effectiveness was a between group comparison of the percent reduction in weekly partial seizure frequency relative to placebo over the entire randomized treatment period (titration + evaluation period). Secondary outcome variables included the responder rate (incidence of patients with ≥50% reduction from baseline in partial-onset seizure frequency). The results of the analysis of Study 1 are displayed in Table 10.Table 10: Reduction in Mean Over Placebo in Weekly Frequency of Partial-Onset Seizures in Study 1 *statistically significant versus placebo Placebo (N=95)
Levetiracetam
1000 mg/day
(N=97)
Levetiracetam
3000 mg/day
(N=101)
Percent reduction in partial seizure frequency over placebo
–
26.1%*
30.1%*
The percentage of patients (y-axis) who achieved ≥50% reduction in weekly seizure rates from baseline in partial-onset seizure frequency over the entire randomized treatment period (titration + evaluation period) within the three treatment groups (x-axis) is presented in Figure 1.
Study 2
Study 2 was a double-blind, placebo-controlled, crossover study conducted at 62 centers in Europe comparing levetiracetam 1000 mg/day (N=106), levetiracetam 2000 mg/day (N=105), and placebo (N=111) given in equally divided doses twice daily.
The first period of the study (Period A) was designed to be analyzed as a parallel-group study. After a prospective baseline period of up to 12 weeks, patients were randomized to one of the three treatment groups described above. The 16-week treatment period consisted of the 4-week titration period followed by a 12-week fixed dose evaluation period, during which concomitant AED regimens were held constant. The primary measure of effectiveness was a between group comparison of the percent reduction in weekly partial seizure frequency relative to placebo over the entire randomized treatment period (titration + evaluation period). Secondary outcome variables included the responder rate (incidence of patients with ≥50% reduction from baseline in partial-onset seizure frequency). The results of the analysis of Period A are displayed in Table 11.Table 11: Reduction in Mean Over Placebo in Weekly Frequency of Partial-Onset Seizures in Study 2: Period A *statistically significant versus placebo Placebo
(N=111)
Levetiracetam
1000 mg/day
(N=106)
Levetiracetam
2000 mg/day
(N=105)
Percent reduction in partial
seizure frequency over placebo
–
17.1%*
21.4%*
The percentage of patients (y-axis) who achieved ≥50% reduction in weekly seizure rates from baseline in partial -onset seizure frequency over the entire randomized treatment period (titration + evaluation period) within the three treatment groups (x-axis) is presented in Figure 2.
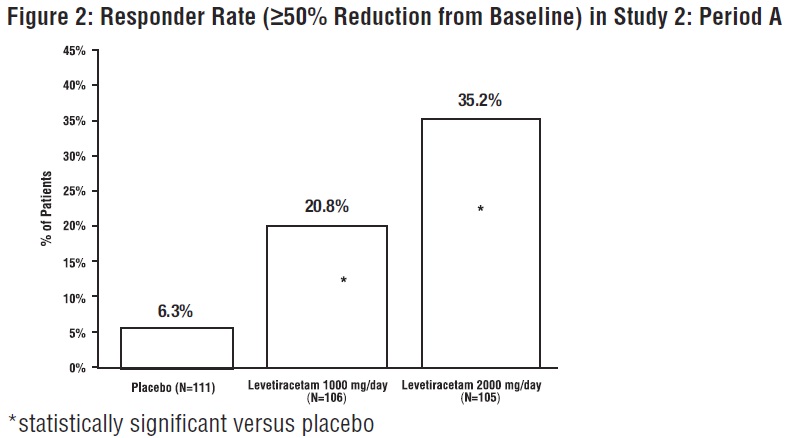
The comparison of levetiracetam 2000 mg/day to levetiracetam 1000 mg/day for responder rate was statistically significant (P=0.02). Analysis of the trial as a cross-over yielded similar results.
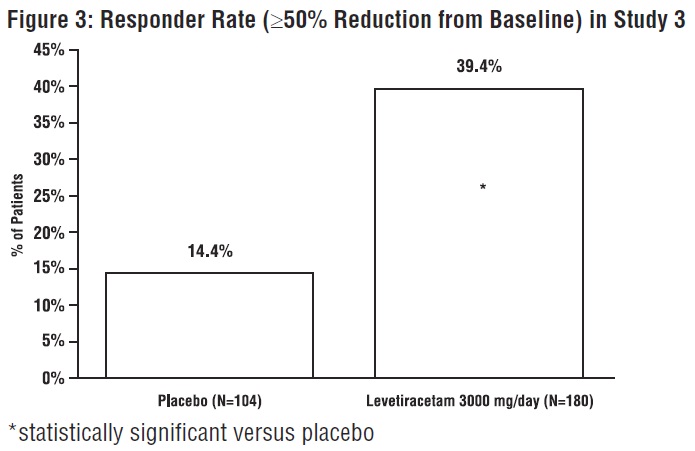
Study 3
Study 3 was a double-blind, placebo-controlled, parallel-group study conducted at 47 centers in Europe comparing levetiracetam 3000 mg/day (N=180) and placebo (N=104) in patients with refractory partial-onset seizures, with or without secondary generalization, receiving only one concomitant AED. Study drug was given in two divided doses. After a prospective baseline period of 12 weeks, patients were randomized to one of two treatment groups described above. The 16-week treatment period consisted of a 4-week titration period, followed by a 12-week fixed dose evaluation period, during which concomitant AED doses were held constant. The primary measure of effectiveness was a between group comparison of the percent reduction in weekly seizure frequency relative to placebo over the entire randomized treatment period (titration + evaluation period). Secondary outcome variables included the responder rate (incidence of patients with ≥50% reduction from baseline in partial-onset seizure frequency). Table 12 displays the results of the analysis of Study 3.
Table 12: Reduction in Mean Over Placebo in Weekly Frequency of Partial-Onset Seizures in Study 3 *statistically significant versus placebo Placebo
(N=104)
Levetiracetam
3000 mg/day
(N=180)
Percent reduction in partial seizure frequency over placebo
–
23%*
The percentage of patients (y-axis) who achieved ≥50% reduction in weekly seizure rates from baseline in partial-onset seizure frequency over the entire randomized treatment period (titration + evaluation period) within the two treatment groups (x-axis) is presented in Figure 3.
Effectiveness in Partial-Onset Seizures in Pediatric Patients 4 to 16 Years of Age
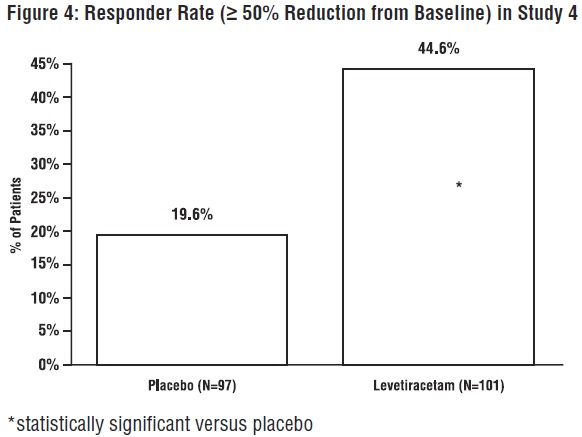
The effectiveness of levetiracetam for the treatment of partial-onset seizures in pediatric patients was established in one multicenter, randomized double-blind, placebo-controlled study (Study 4), conducted at 60 sites in North America, in pediatric patients 4 to 16 years of age with partial seizures uncontrolled by standard antiepileptic drugs (AEDs). Eligible patients on a stable dose of 1 to 2 AEDs, who still experienced at least 4 partial- onset seizures during the 4 weeks prior to screening, as well as at least 4 partial-onset seizures in each of the two 4-week baseline periods, were randomized to receive either levetiracetam or placebo. The enrolled population included 198 patients (levetiracetam N=101, placebo N=97) with refractory partial-onset seizures, whether or not secondarily generalized. The study consisted of an 8-week baseline period and 4-week titration period followed by a 10-week evaluation period. Dosing was initiated at a dose of 20 mg/kg/day in two divided doses. During the treatment period, levetiracetam doses were adjusted in 20 mg/kg/day increments, at 2-week intervals to the target dose of 60 mg/kg/day. The primary measure of effectiveness was a between group comparison of the percent reduction in weekly partial seizure frequency relative to placebo over the entire 14-week randomized treatment period (titration + evaluation period). Secondary outcome variables included the responder rate (incidence of patients with ≥ 50% reduction from baseline in partial-onset seizure frequency per week). Table 13 displays the results of this study.Table 13: Reduction in Mean Over Placebo in Weekly Frequency of Partial-Onset Seizures in Study 4 *statistically significant versus placebo Placebo
(N=97)
Levetiracetam (N=101)
Percent reduction in partial seizure frequency over placebo
-
26.8%*
The percentage of patients (y-axis) who achieved ≥ 50% reduction in weekly seizure rates from baseline in partial-onset seizure frequency over the entire randomized treatment period (titration + evaluation period) within the two treatment groups (x-axis) is presented in Figure 4.
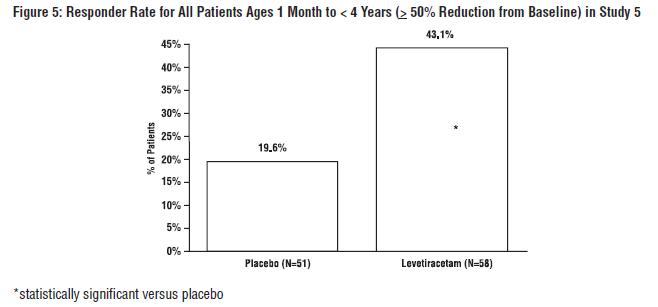
Effectiveness in Partial-Onset Seizures in Pediatric Patients 1 Month to <4 Years of AgeThe effectiveness of levetiracetam for the treatment of partial-onset seizures in pediatric patients was established in one multicenter, randomized double-blind, placebo-controlled study (Study 5), conducted at 62 sites in North America, South America, and Europe in pediatric patients 1 month to less than 4 years of age with partial seizures, uncontrolled by standard epileptic drugs (AEDs). Eligible patients on a stable dose of 1 to 2 AEDs, who experienced at least 2 partial -onset seizures during the 48-hour baseline video EEG were randomized to receive either levetiracetam or placebo. The enrolled population included 116 patients (levetiracetam N=60, placebo N=56) with refractory partial-onset seizures, whether or not secondarily generalized. Randomization was stratified by age range as follows: 1 month to less than 6 months of age (N=4 treated with levetiracetam), 6 months to less than 1 year of age (N=8 treated with levetiracetam), 1 year to less than 2 years of age (N=20 treated with levetiracetam), and 2 years to less than 4 years of age (N=28 treated with levetiracetam). The study consisted of a 5-day evaluation period which included a 1-day titration period followed by a 4-day maintenance period. Levetiracetam dosing was determined by age and weight as follows: children 1 month to less than 6 months old were randomized to a target dose of 40 mg/kg/day, and children 6 months to less than 4 years old were randomized to a target dose of 50 mg/kg/day. The primary measure of effectiveness was the responder rate (percent of patients with ≥ 50% reduction from baseline in average daily partial-onset seizure frequency) assessed by a blinded central reader using a 48-hour video EEG performed during the last two days of the 4-day maintenance period. A total of 109 patients were included in the efficacy analysis. A statistically significant difference between levetiracetam and placebo was observed (see Figure 5). The treatment effect associated with levetiracetam was consistent across age groups.
14.2 Myoclonic Seizures in Patients With Juvenile Myoclonic Epilepsy
The effectiveness of levetiracetam as adjunctive therapy in patients 12 years of age and older with juvenile myoclonic epilepsy (JME) experiencing myoclonic seizures was established in one multicenter, randomized, double-blind, placebo-controlled study (Study 6), conducted at 37 sites in 14 countries. Eligible patients on a stable dose of 1 antiepileptic drug (AED) experiencing one or more myoclonic seizures per day for at least 8 days during the prospective 8-week baseline period were randomized to either levetiracetam or placebo (levetiracetam N=60, placebo N=60). Patients were titrated over 4 weeks to a target dose of 3000 mg/day and treated at a stable dose of 3000 mg/day over 12 weeks (evaluation period). Study drug was given in 2 divided doses.
The primary measure of effectiveness was the proportion of patients with at least 50% reduction in the number of days per week with one or more myoclonic seizures during the treatment period (titration + evaluation periods) as compared to baseline. Of the 120 patients enrolled, 113 had a diagnosis of confirmed or suspected JME. Table 14 displays the results for the 113 patients with JME in this study.
Table 14: Responder Rate (≥50% Reduction from Baseline) in Myoclonic Seizure Days per Week for Patients with JME in Study 6 Placebo
(N=59)Levetiracetam
(N=54)*statistically significant versus placebo
Percentage of responders
23.7%
60.4%*
14.3 Primary Generalized Tonic-Clonic Seizures
The effectiveness of levetiracetam as adjunctive therapy in patients 6 years of age and older with idiopathic generalized epilepsy experiencing primary generalized tonic-clonic (PGTC) seizures was established in one multicenter, randomized, double-blind, placebo-controlled study (Study 7), conducted at 50 sites in 8 countries. Eligible patients on a stable dose of 1 or 2 antiepileptic drugs (AEDs) experiencing at least 3 PGTC seizures during the 8-week combined baseline period (at least one PGTC seizure during the 4 weeks prior to the prospective baseline period and at least one PGTC seizure during the 4-week prospective baseline period) were randomized to either levetiracetam or placebo. The 8-week combined baseline period is referred to as “baseline” in the remainder of this section. Patients were titrated over 4 weeks to a target dose of 3000 mg/day for adults or a pediatric target dose of 60 mg/kg/day and treated at a stable dose of 3000 mg/day (or 60 mg/kg/day for children) over 20 weeks (evaluation period). Study drug was given in 2 equally divided doses per day. The primary measure of effectiveness was the percent reduction from baseline in weekly PGTC seizure frequency for levetiracetam and placebo treatment groups over the treatment period (titration + evaluation periods). The population included 164 patients (levetiracetam N=80, placebo N=84) with idiopathic generalized epilepsy (predominately juvenile myoclonic epilepsy, juvenile absence epilepsy, childhood absence epilepsy, or epilepsy with Grand Mal seizures on awakening) experiencing primary generalized tonic-clonic seizures. Each of these syndromes of idiopathic generalized epilepsy was well represented in this patient population.
There was a statistically significant decrease from baseline in PGTC frequency in the levetiracetam-treated patients compared to the placebo-treated patients.
Table 15: Median Percent Reduction from Baseline in PGTC Seizure Frequency per Week in Study 7 Placebo
(N=84)Levetiracetam
(N=78)*statistically significant versus placebo
Percent reduction in PGTC seizure frequency
44.6%
77.6%*
The percentage of patients (y-axis) who achieved ≥50% reduction in weekly seizure rates from baseline in PGTC seizure frequency over the entire randomized treatment period (titration + evaluation period) within the two treatment groups (x-axis) is presented in Figure 6.
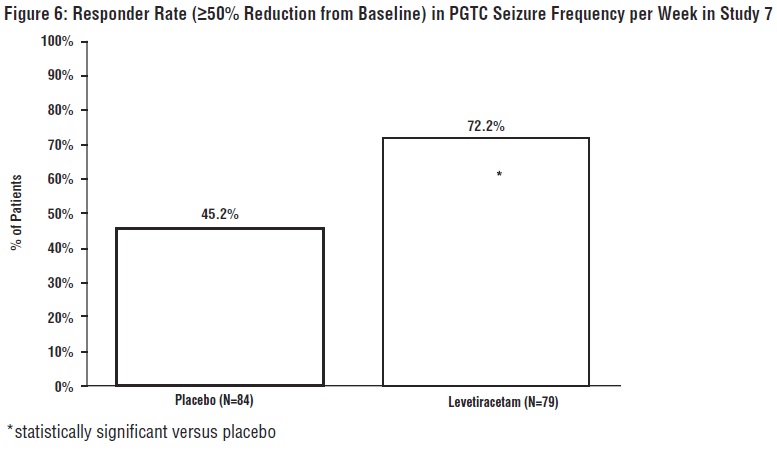
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Levetiracetam Tablets USP, 250 mg are blue oval shaped biconvex film-coated tablets debossed with a deep break line separating ‘E’ and ‘10’ on one side and plain on the other side.
Bottles of 120 NDC: 65862-245-08
Bottles of 500 NDC: 65862-245-05
Levetiracetam Tablets USP, 500 mg are yellow oval shaped biconvex film-coated tablets debossed with a deep break line separating ‘E’ and ‘11’ on one side and plain on the other side.
Bottles of 120 NDC: 65862-246-08
Bottles of 500 NDC: 65862-246-05
Levetiracetam Tablets USP, 750 mg are orange oval shaped biconvex film-coated tablets debossed with a deep break line separating ‘E’ and ‘12’ on one side and plain on the other side.
Bottles of 120 NDC: 65862-247-08
Bottles of 500 NDC: 65862-247-05
Levetiracetam Tablets USP, 1000 mg are white to off-white modified oval shaped biconvex film-coated tablets debossed with a deep breakline separating ‘E’ and ‘13’ on one side and plain on the other side.
Bottles of 30 NDC: 65862-315-30
Bottles of 60 NDC: 65862-315-60
Bottles of 500 NDC: 65862-315-05 -
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Psychiatric Reactions and Changes in Behavior
Advise patients that levetiracetam may cause changes in behavior (e.g., aggression, agitation, anger, anxiety, apathy, depression, hostility, and irritability) and psychotic symptoms [see Warnings and Precautions (5.1)].
Suicidal Behavior and Ideation
Counsel patients, their caregivers, and/or families that antiepileptic drugs (AEDs), including levetiracetam, may increase the risk of suicidal thoughts and behavior and advise patients to be alert for the emergence or worsening of symptoms of depression; unusual changes in mood or behavior; or suicidal thoughts, behavior, or thoughts about self-harm. Advise patients, their caregivers, and/or families to immediately report behaviors of concern to a healthcare provider [see Warnings and Precautions (5.2)].
Effects on Driving or Operating Machinery
Inform patients that levetiracetam may cause dizziness and somnolence. Inform patients not to drive or operate machinery until they have gained sufficient experience on levetiracetam to gauge whether it adversely affects their ability to drive or operate machinery [see Warnings and Precautions (5.3)].
Anaphylaxis and Angioedema
Advise patients to discontinue levetiracetam and seek medical care if they develop signs and symptoms of anaphylaxis or angioedema [see Warnings and Precautions (5.4)].
Dermatological Adverse Reactions
Advise patients that serious dermatological adverse reactions have occurred in patients treated with levetiracetam and instruct them to call their physician immediately if a rash develops [see Warnings and Precautions (5.5)].
Withdrawal of levetiracetam
Advise patients and caregivers not to discontinue use of levetiracetam without consulting with their healthcare provider. levetiracetam should normally be gradually withdrawn to reduce the potential of increased seizure frequency and status epilepticus [see Warnings and Precautions (5.7)].
Pregnancy
Advise patients to notify their healthcare provider if they become pregnant or intend to become pregnant during levetiracetam therapy. Encourage patients to enroll in the North American Antiepileptic Drug (NAAED) pregnancy registry if they become pregnant [see Use in Specific Populations (8.1)].
Dispense with Medication Guide available at: www.aurobindousa.com/product-medication-guides
Distributed by:
Aurobindo Pharma USA, Inc.
279 Princeton-Hightstown Road
East Windsor, NJ 08520
Manufactured by:
Aurobindo Pharma Limited
Hyderabad-500 038, India
Revised: 12/2019
-
MEDICATION GUIDE
Levetiracetam Tablets USP, for oral use
(lee'' ve tye ra' se tam)
Read this Medication Guide before you start taking levetiracetam tablets and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or treatment.
What is the most important information I should know about levetiracetam tablets?
Like other antiepileptic drugs, levetiracetam tablets may cause suicidal thoughts or actions in a very small number of people, about 1 in 500 people taking it.
Call a healthcare provider right away if you have any of these symptoms, especially if they are new, worse, or worry you:
- thoughts about suicide or dying
- attempts to commit suicide
- new or worse depression
- new or worse anxiety
- feeling agitated or restless
- panic attacks
- trouble sleeping (insomnia)
- new or worse irritability
- acting aggressive, being angry, or violent
- acting on dangerous impulses
- an extreme increase in activity and talking (mania)
- other unusual changes in behavior or mood
Do not stop levetiracetam tablets without first talking to a healthcare provider.
- Stopping levetiracetam tablets suddenly can cause serious problems. Stopping a seizure medicine suddenly can cause seizures that will not stop (status epilepticus).
- Suicidal thoughts or actions can be caused by things other than medicines. If you have suicidal thoughts or actions, your healthcare provider may check for other causes.
How can I watch for early symptoms of suicidal thoughts and actions?
- Pay attention to any changes, especially sudden changes, in mood, behaviors, thoughts, or feelings.
- Keep all follow-up visits with your healthcare provider as scheduled.
Call your healthcare provider between visits as needed, especially if you are worried about symptoms
What are levetiracetam tablets?
Levetiracetam tablets are a prescription medicine taken by mouth that is used to treat partial-onset seizures in people 1 month of age and older.
Levetiracetam tablets are a prescription medicine taken by mouth that is used with other medicines to treat:
- myoclonic seizures in people 12 years of age and older with juvenile myoclonic epilepsy.
- primary generalized tonic-clonic seizures in people 6 years of age and older with certain types of generalized epilepsy.
It is not known if levetiracetam tablets are safe or effective in children under:
- 1 month of age to treat partial-onset seizures
- 12 years of age to treat myoclonic seizures
- 6 years of age to treat primary generalized tonic-clonic seizures
Before taking your medicine, make sure you have received the correct medicine. Compare the name above with the name on your bottle and the appearance of your medicine with the description of levetiracetam tablets provided below. Tell your pharmacist immediately if you think you have been given the wrong medicine.
Who should not take levetiracetam tablets?
Do not take levetiracetam tablets if you are allergic to levetiracetam.
What should I tell my healthcare provider before starting levetiracetam tablets?
Before taking levetiracetam tablets, tell your healthcare provider about all of your medical conditions, including if you:
- have or have had depression, mood problems or suicidal thoughts or behavior.
- have kidney problems.
- are pregnant or planning to become pregnant. It is not known if levetiracetam tablets will harm your unborn baby. You and your healthcare provider will have to decide if you should take levetiracetam tablets while you are pregnant. If you become pregnant while taking levetiracetam tablets, talk to your healthcare provider about registering with the North American Antiepileptic Drug Pregnancy Registry. You can enroll in this registry by calling 1-888-233-2334 or go to http://www.aedpregnancyregistry.org. The purpose of this registry is to collect information about the safety of levetiracetam tablets and other antiepileptic medicine during pregnancy.
- are breastfeeding or plan to breastfeed. levetiracetam can pass into your breast milk. It is not known if the levetiracetam that passes into your breast milk can harm your baby. Talk to your doctor about the best way to feed your baby while you receive levetiracetam tablets.
Tell your healthcare provider about all the medicines you take, including prescription and over-the counter medicines, vitamins, and herbal supplements. Do not start a new medicine without first talking with your healthcare provider.
Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist each time you get a new medicine.
How should I take levetiracetam tablets?
- Take levetiracetam tablets exactly as your healthcare provider tells you to take them.
- Your healthcare provider will tell you how much levetiracetam tablets to take and when to take them. Levetiracetam tablets are usually taken 2 times each day.
- Your healthcare provider may change your dose. Do not change your dose without talking to your healthcare provider.
- Take levetiracetam tablets with or without food.
- Swallow the tablets whole. Do not chew or crush tablets. Ask your healthcare provider for levetiracetam oral solution if you cannot swallow tablets.
- If your healthcare provider has prescribed levetiracetam oral solution, be sure to ask your pharmacist for a medicine dropper or medicine cup to help you measure the correct amount of levetiracetam oral solution. Do not use a household teaspoon. Ask your pharmacist for instructions on how to use the measuring device the right way.
- If you take too much levetiracetam tablets, call your local Poison Control Center or go to the nearest emergency room right away.
What should I avoid while taking levetiracetam tablets?
Do not drive, operate machinery or do other dangerous activities until you know how levetiracetam tablets affect you. Levetiracetam tablets may make you dizzy or sleepy.
What are the possible side effects of levetiracetam tablets?
Levetiracetam tablets can cause serious side effects including:
See “What is the most important information I should know about levetiracetam tablets?”
Call your healthcare provider right away if you have any of these symptoms:
- mood and behavior changes such as aggression, agitation, anger, anxiety, apathy, mood swings, depression, hostility, and irritability. A few people may get psychotic symptoms such as hallucinations (seeing or hearing things that are really not there), delusions (false or strange thoughts or beliefs) and unusual behavior.
- extreme sleepiness, tiredness, and weakness
- allergic reactions such as swelling of the face, lips, eyes, tongue, and throat, trouble swallowing or breathing, and hives.
- a skin rash. Serious skin rashes can happen after you start taking levetiracetam tablets. There is no way to tell if a mild rash will become a serious reaction.
- problems with muscle coordination (problems walking and moving)
The most common side effects seen in people who take levetiracetam tablets include:
- sleepiness
- weakness
- infection
- dizziness
The most common side effects seen in children who take levetiracetam tablets include, in addition to those listed above include:
- tiredness
- acting aggressive
- decreased appetite
- nasal congestion
- irritability
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of levetiracetam tablets. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store levetiracetam tablets?
- Store levetiracetam tablets at room temperature, 15° to 30°C (59° to 86°F) away from heat and light.
- Keep levetiracetam tablets and all medicines out of the reach of children.
General information about the safe and effective use of levetiracetam tablets.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use levetiracetam tablets for a condition for which it was not prescribed. Do not give levetiracetam tablets to other people, even if they have the same symptoms that you have. They may harm them. You can ask your pharmacist or healthcare provider for information about levetiracetam tablets that is written for health professionals.
What are the ingredients in levetiracetam tablets?
Active ingredient: levetiracetam
Inactive ingredients: corn starch, colloidal silicon dioxide, povidone, talc, magnesium stearate, hypromellose, titanium dioxide, polyethylene glycol, purified water and additional agents listed below:
250 mg tablets: FD&C Blue #2/indigo carmine aluminum lake
500 mg tablets: iron oxide yellow
750 mg tablets: FD&C Yellow #6/sunset yellow FCF aluminum lake, FD&C Blue #2/indigo carmine aluminum lake and iron oxide red.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Dispense with Medication Guide available at: www.aurobindousa.com/product-medication-guides
Distributed by:
Aurobindo Pharma USA, Inc.
279 Princeton-Hightstown Road
East Windsor, NJ 08520
Manufactured by:
Aurobindo Pharma Limited
Hyderabad-500 038, India
Revised: 12/2019 -
PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 250 mg (500 Tablets Bottle)
NDC: 65862-245-05
Rx only
Levetiracetam
Tablets USP
250 mg
PHARMACIST: PLEASE DISPENSE WITH
MEDICATION GUIDE PROVIDED
SEPARATELY
AUROBINDO 500 Tablets
-
PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 500 mg (500 Tablets Bottle)
NDC: 65862-246-05
Rx only
Levetiracetam
Tablets USP
500 mg
PHARMACIST: PLEASE DISPENSE WITH
MEDICATION GUIDE PROVIDED
SEPARATELY
AUROBINDO 500 Tablets
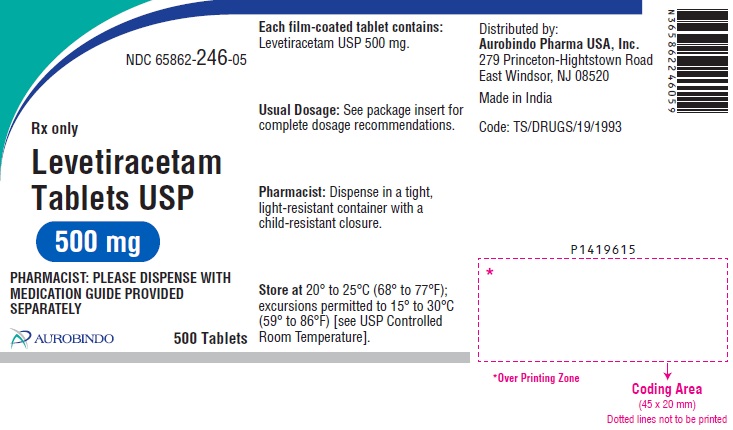
-
PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 750 mg (500 Tablets Bottle)
NDC: 65862-247-05
Rx only
Levetiracetam
Tablets USP
750 mg
PHARMACIST: PLEASE DISPENSE WITH
MEDICATION GUIDE PROVIDED
SEPARATELY
AUROBINDO 500 Tablets
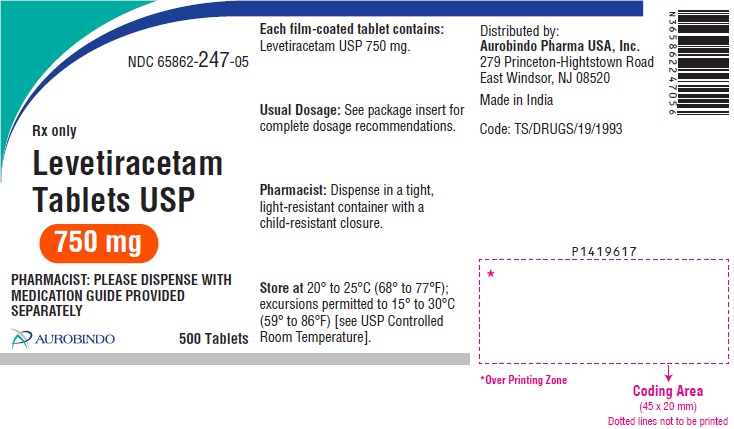
-
PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 1000 mg (500 Tablets Bottle)
NDC: 65862-315-05
Rx only
Levetiracetam
Tablets USP
1000 mg
PHARMACIST: PLEASE DISPENSE WITH
MEDICATION GUIDE PROVIDED
SEPARATELY
AUROBINDO 500 Tablets
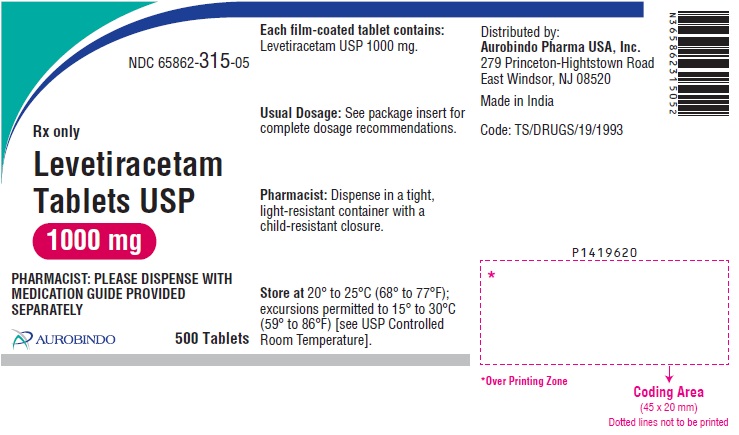
-
INGREDIENTS AND APPEARANCE
LEVETIRACETAM
levetiracetam tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 65862-245 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LEVETIRACETAM (UNII: 44YRR34555) (LEVETIRACETAM - UNII:44YRR34555) LEVETIRACETAM 250 mg Inactive Ingredients Ingredient Name Strength STARCH, CORN (UNII: O8232NY3SJ) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) POVIDONE K30 (UNII: U725QWY32X) TALC (UNII: 7SEV7J4R1U) MAGNESIUM STEARATE (UNII: 70097M6I30) HYPROMELLOSE 2910 (3 MPA.S) (UNII: 0VUT3PMY82) HYPROMELLOSE 2910 (6 MPA.S) (UNII: 0WZ8WG20P6) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL 4000 (UNII: 4R4HFI6D95) WATER (UNII: 059QF0KO0R) FD&C BLUE NO. 2 (UNII: L06K8R7DQK) Product Characteristics Color BLUE Score 2 pieces Shape OVAL (Biconvex) Size 15mm Flavor Imprint Code E;10 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 65862-245-08 120 in 1 BOTTLE; Type 0: Not a Combination Product 01/15/2009 2 NDC: 65862-245-05 500 in 1 BOTTLE; Type 0: Not a Combination Product 01/15/2009 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA078993 01/15/2009 LEVETIRACETAM
levetiracetam tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 65862-246 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LEVETIRACETAM (UNII: 44YRR34555) (LEVETIRACETAM - UNII:44YRR34555) LEVETIRACETAM 500 mg Inactive Ingredients Ingredient Name Strength STARCH, CORN (UNII: O8232NY3SJ) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) POVIDONE K30 (UNII: U725QWY32X) TALC (UNII: 7SEV7J4R1U) MAGNESIUM STEARATE (UNII: 70097M6I30) HYPROMELLOSE 2910 (3 MPA.S) (UNII: 0VUT3PMY82) HYPROMELLOSE 2910 (6 MPA.S) (UNII: 0WZ8WG20P6) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL 4000 (UNII: 4R4HFI6D95) WATER (UNII: 059QF0KO0R) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) Product Characteristics Color YELLOW Score 2 pieces Shape OVAL (Biconvex) Size 18mm Flavor Imprint Code E;11 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 65862-246-08 120 in 1 BOTTLE; Type 0: Not a Combination Product 01/15/2009 2 NDC: 65862-246-05 500 in 1 BOTTLE; Type 0: Not a Combination Product 01/15/2009 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA078993 01/15/2009 LEVETIRACETAM
levetiracetam tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 65862-247 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LEVETIRACETAM (UNII: 44YRR34555) (LEVETIRACETAM - UNII:44YRR34555) LEVETIRACETAM 750 mg Inactive Ingredients Ingredient Name Strength STARCH, CORN (UNII: O8232NY3SJ) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) POVIDONE K30 (UNII: U725QWY32X) TALC (UNII: 7SEV7J4R1U) MAGNESIUM STEARATE (UNII: 70097M6I30) HYPROMELLOSE 2910 (3 MPA.S) (UNII: 0VUT3PMY82) HYPROMELLOSE 2910 (6 MPA.S) (UNII: 0WZ8WG20P6) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL 4000 (UNII: 4R4HFI6D95) WATER (UNII: 059QF0KO0R) FD&C YELLOW NO. 6 (UNII: H77VEI93A8) FD&C BLUE NO. 2 (UNII: L06K8R7DQK) FERRIC OXIDE RED (UNII: 1K09F3G675) Product Characteristics Color ORANGE Score 2 pieces Shape OVAL (Biconvex) Size 20mm Flavor Imprint Code E;12 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 65862-247-08 120 in 1 BOTTLE; Type 0: Not a Combination Product 01/15/2009 2 NDC: 65862-247-05 500 in 1 BOTTLE; Type 0: Not a Combination Product 01/15/2009 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA078993 01/15/2009 LEVETIRACETAM
levetiracetam tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 65862-315 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LEVETIRACETAM (UNII: 44YRR34555) (LEVETIRACETAM - UNII:44YRR34555) LEVETIRACETAM 1000 mg Inactive Ingredients Ingredient Name Strength STARCH, CORN (UNII: O8232NY3SJ) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) POVIDONE K30 (UNII: U725QWY32X) TALC (UNII: 7SEV7J4R1U) MAGNESIUM STEARATE (UNII: 70097M6I30) HYPROMELLOSE 2910 (5 MPA.S) (UNII: R75537T0T4) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL 400 (UNII: B697894SGQ) WATER (UNII: 059QF0KO0R) Product Characteristics Color WHITE (White to Off-white) Score 2 pieces Shape OVAL (Modified Oval, Biconvex) Size 22mm Flavor Imprint Code E;13 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 65862-315-30 30 in 1 BOTTLE; Type 0: Not a Combination Product 01/15/2009 2 NDC: 65862-315-60 60 in 1 BOTTLE; Type 0: Not a Combination Product 01/15/2009 3 NDC: 65862-315-05 500 in 1 BOTTLE; Type 0: Not a Combination Product 01/15/2009 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA078993 01/15/2009 Labeler - Aurobindo Pharma Limited (650082092) Establishment Name Address ID/FEI Business Operations Aurobindo Pharma Limited 918917642 ANALYSIS(65862-245, 65862-246, 65862-247, 65862-315) , MANUFACTURE(65862-245, 65862-246, 65862-247, 65862-315)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.